How does cholecystokinin stimulate exocrine pancreatic secretion
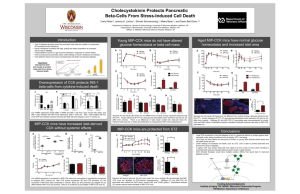
advertisement

Am J Physiol Regul Integr Comp Physiol 292: R666 –R678, 2007. First published October 19, 2006; doi:10.1152/ajpregu.00131.2006. Invited Review How does cholecystokinin stimulate exocrine pancreatic secretion? From birds, rodents, to humans Bi Jue Wang and Zong Jie Cui Institute of Cell Biology, Beijing Normal University, Beijing, China Wang BJ, Cui ZJ. How does cholecystokinin stimulate exocrine pancreatic secretion? From birds, rodents, to humans. Am J Physiol Regul Integr Comp Physiol 292: R666–R678, 2007. First published October 19, 2006; doi:10.1152/ajpregu.00131.2006.— The field of cholecystokinin (CCK) stimulation of exocrine pancreatic secretion has experienced major changes in the recent past. This review attempts to summarize the present status of the field. CCK production in the intestinal I cells, the molecular forms of CCK produced and subsequently circulated in the blood, the presence or absence of CCK receptors on the isolated pancreatic acinar cells and the associated signaling for acinar cell secretion, and the actual circuits and sites of action for CCK regulation of exocrine pancreatic secretion in vivo are reviewed in different animal species with an emphasis on birds, rodents, and humans. Clear differences in the relative importance of neural and direct modes of CCK action on pancreatic acinar cells were identified. Rodents seem to be endowed with both modes of action, whereas in humans the neural mode may predominate. In birds, such as duck, the direct mode needs further assistance from pituitary adenylate cyclaseactivating peptide/VIP receptors. However, much further work needs to be directed to the neural mode to map out all sites of CCK action and details of the full circuits, and we foresee a major revival for this field of research in the near future. pancreatic acinar cells; vagal afferent nerves; plasma cholecystokinin concentration; species specificity cholecystokinin (CCK) as a gut hormone is an important endogenous secretagogue in exocrine pancreatic secretion. CCK also stimulates gallbladder contraction and enhances growth of the exocrine pancreas (63, 115, 138). CCK is produced and released by the intestinal mucosal I cells (78). This source of CCK may travel through the circulation to target tissues that include the exocrine pancreas and gallbladder (65, 78). CCK peptides are also found in large quantities in neurons, but neuronal CCK contributes negligibly to CCK concentration in the circulation (118). This general picture has been changed drastically by the recent findings that CCK can also stimulate exocrine pancreatic secretion by the excitation of sensory nerves and vagovagal and enteropancreatic reflexes, and this may be the only pathway in humans (65, 105). In addition, major differences have been found in the traditional humoral pathway, depending on the animal species (35, 149). Therefore, the purpose of this review is to present the current status of CCK regulation of exocrine pancreatic secretion with a particular emphasis on species specificity as shown in birds, rodents, and humans. IT IS GENERALLY ACCEPTED THAT GUT CCK-SECRETING CELL CCK is produced by I cells of the intestinal mucosa, which in rodents are concentrated in the duodenum and proximal jejunum (31, 78). I cells are flask shaped, with their microvilliabundant apical surface oriented toward the intestine lumen (109); their secretory granules, which are ⬃250 nm in size and Address for reprint requests and other correspondence: Z. J. Cui, Institute of Cell Biology, Beijing Normal Univ., Beijing 100875, China (e-mail: zjcui@bnu.edu.cn). R666 contain packaged CCK, are concentrated around the basolateral surfaces of the cell (13). Because CCK-secreting cells are diffusely scattered in intestinal mucosa, I cell studies are rather limited to immortalized cell lines (44). The neuroendocrine cell line STC-1 was derived from the murine gut and established as a model system for rodent I cell CCK secretion (120). In STC-1 cells, SNARE proteins syntaxin-1, synaptosome-associated protein of 25 kDa (SNAP-25), and vesicle-associated membrane polypeptide 2 (VAMP-2) have been found to be involved in Ca2⫹-induced CCK secretion (100), and the GTPbound form of rab3A has been found to be a negative clamp for exocytosis (39). The most potent stimulants of CCK secretion are digestive products of fats and proteins, with carbohydrates being less potent. Of triglyceride hydrolysis products, fatty acids with longer acyl chains (ⱖ12 carbon atoms) are potent secretagogues for CCK secretion; of protein breakdown products, tryptophan and phenylanaline are the most potent (79). Soybean agglutinin stimulates CCK release by opening L-type Ca2⫹ channels in cultured rabbit jejunal cells (62). Fatty acids elicit a marked increase in intracellular Ca2⫹ concentration ([Ca2⫹]i) and CCK secretion in STC-1 cells; both responses are blocked by nicardipine (88). In STC-1 and GLUTag cells, fatty acid induces both [Ca2⫹]i increases and CCK secretion (129). Sodium oleate has been found to stimulate CCK release in enriched rat mucosal cells and in STC-1 cells (18). It was found early on that diversion of bile-pancreatic juice and infusion of trypsin inhibitors into the intestine of rats led to enormous increases in pancreatic secretion and CCK release (45); this formed the basis of negative feedback regulation of CCK release. The hypothesis postulated that trypsin-sensitive 0363-6119/07 $8.00 Copyright © 2007 the American Physiological Society http://www.ajpregu.org Invited Review R667 SPECIES DIFFERENCES IN EXOCRINE PANCREAS SECRETION intestinal-releasing factors were present in the small intestine lumen, and, when pancreatic proteases were absent, endogenously produced releasing factors are intact and would interact with the CCK cell to stimulate CCK release (79). This idea led to the discovery of luminal CCK-releasing factor (LCRF), isolated from rat intestinal washings (133), and diazepambinding inhibitor (DBI), isolated from porcine intestine (47). Both LCRF and DBI are involved in the negative feedback regulation of CCK secretion because they are intact and functional in the absence of the pancreatic proteases. However, such mode of CCK feedback regulation may be restricted to rats because there is no spontaneous release of LCRF in humans. In humans, the release of LCRF requires the stimulation of luminal amino acids and fatty acids (78). A peptide isolated from rat pancreatic juice when infused into rat intestine also stimulated CCK secretion, and this led to the discovery of the monitor peptide (77, 78, 82). Monitor peptide, also known as pancreatic secretory trypsin inhibitor I-61, is produced by pancreatic acinar cells. Monitor peptidebinding sites were found in rodent small intestine mucosa (89). The monitor peptide monitors the status in the intestinal lumen, and its increased presence after pancreatic secretion stimulates CCK release from I cells to trigger more pancreatic secretion and therefore is involved in a form of positive feedback loop (77). The synthetic fragments LCRF(1– 41) and LCRF(1–35) have similar potency and efficacy for CCK release in conscious rats (134). Tarasova et al. (137) reported that endogenous LCRF was present throughout the gut, including in the pancreas, stomach, duodenum, jejunum, ileum, and colon, with the highest concentration in small intestine, supporting the notion that LCRF is secreted into intestinal lumen to stimulate CCK release from mucosal CCK cells. In dispersed human intestinal mucosal cells and in STC-1 cells, LCRF markedly stimulated CCK release (141). Porcine intestinal DBI could also stimulate CCK release when administered intraduodenally in rat (47). The biologically active DBI fragment DBI(33–50) induces Ca2⫹ oscillations and CCK secretion in STC-1 cells (151). In addition to luminal factors, neuropeptide bombesin (101, 131, 136), -adrenergic receptor agonist (127), GABA (44, 54), and orexins (69) could all stimulate I cell CCK secretion. Both radioligand binding studies and Northern blot analyses suggested the presence of bombesin-like receptors in CCK cells (131). Bombesin-stimulated CCK secretion from STC-1 cells was PKC dependent and involved the MAPK pathway (101) and calmodulin (136). Liddle and colleagues (127) demonstrated the presence of -adrenergic receptors in STC-1 cells, the stimulation of which led to cAMP production and CCK release (127). Addition of GABA depolarizes STC-1 cells, activating voltage-gated Ca2⫹ channels and subsequent CCK release (44). Further work found that, in addition to GABAA receptors (44), functional GABAC receptors were also present on STC-1 cells (54), and both played important roles in CCK secretion. Neuropeptide orexin stimulates CCK release in STC-1 cells, via orexin1 and orexin2 receptors (69). The distribution of CCK-immunoreactive cells is similar in birds and mammals (111). In ostrich, CCK is mainly produced in duodenum, whereas, in chicken, CCK production is concentrated at the transit from jejunum to ileum (61). Chicken CCK cell secretory granules are ⬃230 nm in diameter (111). In chicken, both dietary proteins and amino acids are potent AJP-Regul Integr Comp Physiol • VOL stimulators of CCK release (37, 150). In addition, two DBIs have been purified from chicken intestine (19). PLASMA CCK CONCENTRATION Hormones classically exert their effect through the circulation (115). Therefore, measurement of plasma CCK is an important parameter in CCK physiology. Plasma CCK concentration can be measured by bioassay and radioimmunoassay (114) with the use of antibodies. Plasma CCK concentrations are usually in the picomolar range in each of the animal species examined (see Table 1). In humans, premeal plasma CCK concentration measured by bioassays or by radioimmunoassays in different studies varied from 1.1 ⫾ 0.1 to 2.8 ⫾ 0.5 pM; after a meal, plasma CCK concentration varied from 4.6 ⫾ 0.6 to 8.2 ⫾ 1.3 pM (see Table 1). An exception is a report that human basal CCK level was 8.3 ⫾ 2.5 pM and after a meal was 24.4 ⫾ 6.5 pM (14). The variation of plasma CCK concentration is partly because of different techniques and different antibodies used and the ingested food used to elevate CCK concentration. Before meals, rat plasma CCK concentrations were found to be in the range of 0.5 ⫾ 0.2 to 2.5 ⫾ 0.3 pM; after feeding, concentrations increased to 4.4 ⫾ 0.8 to ⬃13.4 ⫾ 3.8 pM (29, 30, 81, 84, 128). Basal CCK plasma concentration in chicken was found to be 5–10 pM; after feeding, this increased to 15– 40 pM (37, 86). Table 1. Plasma CCK concentration in different animal species Plasma CCK concentration, pM Before meal After meal Reference Human 2.0⫾0.2 2.0⫾0.2 1.0⫾0.2 8.3⫾2.5 2.8⫾0.5 1.5⫾0.5 1.7⫾0.7 1.1⫾0.1 1.13⫾0.10 7.4⫾0.7 4.6⫾0.–7.3⫾1.0 6.0⫾1.6 24.4⫾6.5 6.5⫾0.7 6.3⫾1.7* 29.8⫾2.9† 8.2⫾1.3 4.92⫾0.34 1.9⫾0.3 2.5 0.5⫾0.2 0.85⫾0.1 2.5⫾0.3 13.4⫾3.8 9.7⫾1.6 7.9⫾1.9 8.2⫾1.1 8.9⫾0.6 16 1.8⫾0.9 5.3⫾0.6 45 4.6⫾1 9.4⫾1.6 10.6⫾1.4 10–30 27.6⫾4.8 80–100 0.5⫾0.3 12.3⫾1.5 15 63 80 14 50 53 53 55 114 Rat 84 29 81 128 30 Dog 33 85 135 Cat 7 6 Pig 17 Chicken 5–10 15–40 37–86 Values are means ⫾ SE. *Medium-chain triglyceride meal; †long-chain triglyceride meal. 292 • FEBRUARY 2007 • www.ajpregu.org Invited Review R668 SPECIES DIFFERENCES IN EXOCRINE PANCREAS SECRETION Fig. 1. Rat proCCK sequence written in single amino acid format. CCK peptides are numbered backward from the COOH terminus of CCK octapeptide (CCK-8). The NH2 terminus of the major molecular forms of amidated CCK peptides is indicated. Three tyrosine residues are sulfated in the proCCK sequence. Amino acid residues not contained in the active fragments are numbered ⫺1 to ⫺12. [Modified from Beinfeld (11).] DIFFERENT MOLECULAR FORMS OF PLASMA CCK CCK is a heterogeneous hormone and present in different molecular forms in mammals: CCK-83, CCK-58, CCK-39, CCK-33, CCK-22, and CCK-8 (Fig. 1). The different forms are all carboxyamidated and O-sulfated and are all ligands for the CCK1 receptor (11, 93, 114, 115). The endoproteolysis of proCCK occurs mainly at monoarginyl sites, but the presence of CCK-22 shows that the Lys-61 site is also cleaved (11, 115). Processing of proCCK is cell specific (11, 115). The plasma CCK originates almost entirely from I cells in small intestinal mucosa (78), which contain a mixture of medium-sized CCK molecules (CCK-58, CCK-33, CCK-22, and CCK-8) that are released into the blood circulation (11, 115). CCK is also a widespread neurotransmitter in the nervous system (114), and neurons mainly release CCK-8 (117). Thus brain and gut contain drastically different molecular forms of CCK. This is because proCCK is processed by different isoforms of the prohormone convertase. Prohormone convertase 1 is present in the intestines, whereas prohormone convertase 2 processes proCCK in the brain (116). Different animal species also have their plasma CCK in diverse forms (Table 2). CCK-33 was found to be the predominant form in human plasma, CCK-22 being the second most abundant, with CCK-58 less abundant (118). Moderate amounts of CCK-8 in human plasma have also been reported (114). CCK-58 is the major circulating form of Table 2. Plasma CCK forms in different animal species Plasma CCK Molecular Forms Reference Rat CCK-58* 112 Human CCK-58, CCK-33,* CCK-22, CCK-8 114, 118 Canine CCK-58* 32, 135 Cat CCK-58, CCK-33, CCK-8 7 Pig CCK-58, CCK-33, CCK-22,* CCK-8 17 Rabbit CCK-33, CCK-22,* CCK-8* 113 Chicken, intestine CCK-70 CCK-8* CCK-7* 61 Ostrich, intestine CCK-70 CCK-8* CCK-7* 61 *Indicates the most abundant form of CCK in blood. AJP-Regul Integr Comp Physiol • VOL CCK in canine blood (32, 135). The most abundant forms of CCK in cat plasma were found to be CCK-8, CCK-33, and CCK-58 (7). In pig plasma, the bioactive species comprised CCK-58, CCK-33, CCK-22, and CCK-8, with CCK-22 being predominant (17). Substantial amounts of CCK-22- and CCK8-like peptides were reported in rabbit plasma, with a small amount of CCK-33-like peptide (113). The plasma forms of CCK in ostrich and chicken are not certain, but analysis of intestinal extracts indicated that some CCK-70 was present, and the dominant forms were CCK-8 and CCK-7 (61). Human preproCCK shares 55% identity with chicken amino acid sequence, further suggesting that CCK is highly conserved among different vertebrate species (60). It may be worthwhile to note here that strict blood collection procedures may be needed to prevent possible degradation of CCK during sample processing. With this new method, Reeve et al. (112) found that CCK-58 was the only major endocrine form of CCK in the rat. CCK RECEPTOR IN DIFFERENT ANIMAL SPECIES CCK binds to CCK1 receptors (CCK1R) on vagal fibers (75) or pancreatic acinar cells (93, 103, 142, 152) to evoke pancreatic enzyme secretion and to CCK receptors in the gastrointestinal tract to regulate gastrointestinal motility (46, 70, 87, 99). Receptors for CCK and gastrin are members of the G-protein-coupled receptor superfamily. Two receptor subtypes for CCK and gastrin have been classified (93, 103, 142). CCK1R, found in gall bladder, exocrine pancreas, and limited areas of the central nervous system, is highly selective for sulfated CCK analogs, whereas the CCK2 receptor (CCK2R), present in widespread areas in the brain and stomach, has high affinity for both sulfated and nonsulfated CCK and gastrin analogs (142). In rodent pancreatic acinar cells, CCK1Rs are coupled to heterotrimeric G proteins of the Gq family, especially Gq and G11, which activate PLC-mediated phosphatidylinositol 4,5bisphosphate breakdown to increase inositol trisphosphate and diacylglycerol formation and eventually to stimulate pancreatic zymogen granule exocytosis (57, 148). CCK1Rs are highly conserved among different animal species. The amino acid sequences of CCK1Rs in rat, mouse, rabbit, guinea pig, dog, human, and cynomolgus monkey are shown in Fig. 2. Rat and mouse CCK1Rs were first characterized in the 1990s, the protein sequences being 95% identical and 98% similar (40, 144). Such sequence differences may have important functional significance. Differences in two amino acid residues in rat and mouse CCK1Rs (Leu-43 and Ileu-50 in rat and Val-43 and Phe-50 in mouse), for example, led to completely opposite effects in MAP/ERK kinase kinasemediated Jun activation (52). The guinea pig CCK1R was found to be 89% homologous to the rat CCK1R sequence (26). 292 • FEBRUARY 2007 • www.ajpregu.org Invited Review SPECIES DIFFERENCES IN EXOCRINE PANCREAS SECRETION Human CCK1R has ⬎90% homology to the rat and guinea pig CCK1R (25). CCK1R of cynomolgus monkey is 98% identical to the human CCK1R (49). Rabbit CCK1R is 92% homologous (87% identity) to the rat CCK1R sequence (8, 119). Canine gallbladder CCK1R is 89% identical to the human and 85% identical to the rat CCK1R (97). Different animal species share ⬃90% identity in their CCK1R amino acid sequence (102). It is noteworthy that there was a seven-amino acid insertion (GGGGGGS) in the predicted third intracellular loop of the mouse receptor that has not been seen in CCK receptors from any other species (40) (see Figs. 2 and 3). The major differences in the sequences are in predicted intracellular domains, with the third intracellular loop being predominant and with the COOH-terminal tail also harboring several differences (40, 49). Like other members of the G-protein-coupled receptor superfamily, CCK1R has a heptahelical transmembrane (TM) structure (4, 24, 91, 143) (Fig. 3). Mierke and colleagues (43) built a model of the human CCK1R. The TM motifs each form an ␣-helix that embeds into the lipid bilayer (42, 107). There is a disulfide bond between C18 and C29 in the NH2 terminus [CCK1R(1– 47)] (107). The first and second extracellular loops are connected by a disulfide bond (C114 –C196), which plays an important structural role. The extracellular loops and the NH2 terminus are vital for both recognition and binding of CCK (91). The COOH-terminal portion of the third cytoplasmic loop of CCK1R contains a stretch of charged residues that are thought to form an amphipathic ␣-helical extension of the sixth transmembrane domain in a critical orientation for G protein activation (143). Theoretical models of CCK1R have also been built by others (3, 28). CCK receptors are present in chicken brain, pancreas, cecum, hypothalamus, and gallbladder, all with a dissociation constant (Kd) of 1 nM (121). In chicken, two CCK receptor subtypes exist: a central subtype in brain and hypothalamus that resembles the mammalian CCK2R in agonist binding and a peripheral subtype in pancreas, gallbladder, and cecum that resembles the mammalian CCK1R in agonist binding (102, 121, 140). These similarities notwithstanding, however, rodent CCK1 antagonist L-364,718 behaves as a chicken CCK2R antagonist, whereas rodent CCK2 antagonist L-365,260 has very low affinity for both receptor subtypes in chicken (121). At the amino acid level, chicken brain CCK receptor (CCKCk) shared ⬃50% homology with mammalian and Xenopus laevis CCK receptors (102) (see Fig. 2). CCK-Ck resembled rodent CCK2Rs regarding agonist binding (CCK-8, CCK-4, gastrin-17). However, CCK-Ck showed higher affinity for the rodent CCK1R antagonist devazepide than for the rodent CCK2R antagonist L-365,260 (102, 121, 140). Human and canine CCK2/gastrin receptors share 90% amino acid sequence identity and have similar agonist affinities (10, 66, 71). However, human and canine receptor binding affinities for antagonists L-365,260 and L-364,718 differ by 20-fold. Beinborn et al. (10) found that a single amino acid in the sixth transmembrane domain of the CCK2/gastrin receptor corresponding to Val-319 in the human homologue was critical in determining binding affinity for antagonists L-365,260 and L-364,718. Substitution of Val-319 by leucine decreases affinity for L-365,260 20-fold and increases affinity for L-364,718; an isoleucine in the same position of human receptor selectively increases affinity for L-364,718 (10). Kopin et al. (67) identified eight amino acid AJP-Regul Integr Comp Physiol • VOL R669 residues in membrane domains adjacent to the cell surface; these residues project into a putative ligand-binding pocket of the human CCK2R, and this pocket is very important for ligandreceptor interaction. These data suggest that ligand-binding amino acid residues, particularly antagonist-binding residues in avian CCK receptors, may be different than those in mammals. Theoretical model building for the avian CCK receptor may help to understand this difference. Early work indicated that a common ancestor CCK receptor diverged into CCK1R and CCK2R at or before the level of the divergence of birds and mammals from reptiles (104, 140). The evolution of CCK probably followed the evolution of CCK receptors. Johnsen (60) reviewed the sequence variations of CCK molecules in lower animals. More detailed studies on CCK receptors in lower animals are obviously needed. CCK STIMULATION OF EXOCRINE PANCREATIC SECRETION: DIRECT AND INDIRECT PATHWAYS Physiologists have used different models to investigate exocrine pancreatic secretion, including the in situ pancreas perfusion model and isolated pancreatic acini. The latter model makes it possible to study pancreatic acinar cell responses without influence from neural or humoral factors, and single cell responses can be easily investigated. Comparison of data from these two general models revealed significant variations in the in-born mechanisms in different animal species. Rodents. CCK-stimulated amylase release in isolated rodent pancreatic acinar cells is typically “bell-shaped.” At lower CCK concentrations, amylase release increased progressively with increasing concentrations, whereas, at higher CCK concentrations, amylase release gradually diminished with increasing CCK concentrations. This results in a maximal stimulating CCK concentration of ⬃100 pM (57, 122, 123). This bell shape may be due to simultaneous occupation in different proportions of high-affinity (Kd ⫽ 26 pM), low-capacity and low-affinity (Kd ⫽ 2.2 nM), high-capacity CCK1R states (123). Further examination of the dose-response curve revealed that rodent CCK1Rs are exceptionally sensitive to CCK, with a threshold concentration at 1 pM (23, 57, 115, 149). Picomolar CCK concentrations induced significant amylase secretion in all isolated rodent (rat, mouse, and guinea pig) pancreatic acini, and maximal stimulating CCK concentration was 100 pM (149). CCK concentration of 10 pM typically induces regular Ca2⫹ oscillations in individual rat pancreatic acinar cells in intact acini (2). This also applies to mouse and rabbit pancreatic cells (5, 146). Atropine does not alter secretory responses to CCK in isolated rodent pancreatic acini (2, 56, 147), indicating that CCK’s effect on rat pancreatic enzyme secretion in isolated pancreatic acini is not dependent on cholinergic stimulation. Hence, in rodents, physiological concentrations of CCK could stimulate pancreatic enzyme secretion by direct stimulation of CCK1Rs on pancreatic acinar cells (51, 124). CCK, however, could also influence exocrine pancreatic secretion in vivo by a neural pathway in rodents. Bilateral vagotomy, pretreatment with atropine or hexamethonium, or perivagal treatment with capsaicin in anesthetized rats completely abolished pancreatic protein secretion in response to low doses of CCK, suggesting that CCK at physiological levels stimulates pancreatic enzyme secretion via a capsaicin-sensitive afferent vagal pathway originating from the gastroduode292 • FEBRUARY 2007 • www.ajpregu.org Invited Review R670 SPECIES DIFFERENCES IN EXOCRINE PANCREAS SECRETION AJP-Regul Integr Comp Physiol • VOL 292 • FEBRUARY 2007 • www.ajpregu.org Invited Review SPECIES DIFFERENCES IN EXOCRINE PANCREAS SECRETION R671 Fig. 3. Structure of human CCK1 receptor (CCK1R), CCK-8, and CCK-8-CCK1R interaction. Middle: serpentine representation of the CCK1R. The NH2-terminal CCK1R(1– 47), third extracellular loop CCK1R(329 –357), and residues (W39, Q40, A334, Y338) involved in interaction with CCK-8 are denoted (91). Top left: complex of CCK1R(1– 47) with CCK-8. Receptor fragment is shown as blue and CCK-8 as red ribbons. W39, Q40 of CCK1R(1– 47), Tyr-27, and Met-28 of CCK-8 are displayed as ball-and-stick representation (107). Top right: structure of CCK1R(329 –357). Transmembrane domain 7 (TM7) and TM6 are depicted on the left and right, respectively. Residues of receptor fragment are color coded according to hydrophobicity (blue ⫽ polar, red ⫽ hydrophobic) (42). Bottom left: structure of CCK-8. Helix-like loop in center of CCK-8 is highlighted by ribbon diagram. Protons involved in intermolecular interaction with NH2 terminus of CCK1R are denoted as spheres (91). Bottom right: interactions of CCK-8 (gray ribbon) with NH2 terminus and third extracellular loop (EC3) of CCK1R (black ribbon). The side chains of the amino acids of CCK-8 and CCK1R stabilizing the CCK-8-CCK1R complex are illustrated as ball-and-sticks and sticks, respectively. The residues of CCK-8 are denoted by three-letter code and those of CCK1R by one-letter code (42). nal mucosa (74). In both rats and guinea pigs, atropine decreased CCK-evoked pancreatic secretory response in vivo (110). In vivo infusion of CCK-JMV-180 (a CCK analog), the high-affinity agonist of CCK1R, causes dose-dependent increases in pancreatic protein secretion in rats blockable by CCK1R antagonist L-364,718, and acute vagotomy in anesthetized rats and perivagal application of capsaicin in conscious rats will abolish pancreatic secretory responses to CCK-JMV180, demonstrating that CCK acts through high-affinity CCK1Rs on nerves to mediate pancreatic protein secretion (73, 105). CCK receptors have been detected in rat vagus nerves with the use of in vitro receptor autoradiography, and these receptors are transported toward peripheral nerve endings from the nodose ganglia (153). CCK1Rs and axonal transport are found in vagal trunks and all abdominal vagal branches (95). Both CCK1R and CCK2R have been found to be present in the cervical vagus and the nucleus of the solitary tract (20). Furthermore, the existence of functional CCK1Rs in the nodose ganglion has been confirmed (12, 145). Both CCK1R and CCK2R have been found to be synthesized in nodose ganglion cells, and these receptors can be transported to the periphery along afferent fibers in both rats and humans (96). CCK may also act on low-affinity CCK1Rs to trigger Ca2⫹ influx into vagal afferent neurons, which in turn may result in acute activation of vagal afferent neurons (130). Electrophysiological evidence showed that both high- and low-affinity CCK1Rs exist on rat vagal afferent fibers, and the vagal CCK-receptor field includes the regions innervated by the gastric, celiac, and hepatic vagal branches (76). Recent work Fig. 2. Alignment of CCK receptor sequences in different species. Amino acid sequences of CCK1 receptor from mouse (CCK-M1), rat (CCK-R1), cynomolgus monkey (CCK-Mk1), guinea pig (CCK-Gp1), rabbit (CCK-Rb1), dog (canine) (CCK-Cn1), and human (CCK-H1); of CCK2 receptors from human (CCK-H2); and of CCK receptors from chicken brain (CCK-Ck) and Xenopus laevis (CCK-Xp) are shown. Completely identical residues in all receptor homologues are indicated in white letters on black background, identical residues in a few species are indicated in black letters on gray background, and distinct residues are indicated in black letters on white background. Compiled from Refs. 40, 49, 97, and 102. AJP-Regul Integr Comp Physiol • VOL 292 • FEBRUARY 2007 • www.ajpregu.org Invited Review R672 SPECIES DIFFERENCES IN EXOCRINE PANCREAS SECRETION indicates that CCK1Rs exist in both high- and low-affinity states in rat nodose ganglia cells. Activation of high-affinity CCK1Rs in isolated rat nodose ganglia cells elicits regular Ca2⫹ oscillations, whereas stimulation of low-affinity CCK1Rs evokes a Ca2⫹ transient followed by a small and sustained Ca2⫹ plateau. Such Ca2⫹ signaling involves both Gq and L-type Ca2⫹ channels (68). CCK acts through high-affinity CCK1Rs on rat vagal afferent fibers to mediate pancreatic secretion (73). The above observations provide evidence for a role for CCK receptors in vagal afferent fibers in pancreatic digestive enzyme secretion. CCK receptors are also present on rabbit vagus nerve, and vagal CCK receptors include both CCK1 and CCK2/gastrin subtypes (83). In rabbit vagal afferent (nodose) ganglion, high concentrations of CCK- and neuropeptide Y-binding sites have been found in 10.6% and 9.2% of the nodose ganglion neurons, respectively; both CCK (CCK1/2) and neuropeptide Y (Y1/2) receptor binding sites are expressed by discrete populations of neurons in the nodose ganglia (41). These data suggest that CCK released from peripheral tissues (mainly from I cells in the small intestinal mucosa) may interact with CCK receptors in vagal afferent fibers to modulate a neural circuit. In addition, it has been found that CCK (10 nM to 10 M) stimulates [3H]acetylcholine release from rat pancreatic lobules, which was blocked by TTX, by Ca2⫹-free medium, and by CCK antagonist L-364,718, suggesting that CCK may act by stimulation of neural acetylcholine release (132). This provides an additional site for CCK action through the neural pathway, but apparently with much lower affinity, because at least nanomolar CCK concentrations were needed to stimulate acetylcholine release from the rat pancreatic lobules (132). Together, these findings suggest that in both rodents and other animals (rabbit) CCK can act both directly on acinar cells and through neural pathways to stimulate exocrine pancreatic secretion (Fig. 4A). Humans. Quantitative RT-PCR indicated that, in human pancreas, CCK1R mRNA was ⬃30 times lower than CCK2R mRNA, which was ⬃10 times further lower than M3 muscarinic acetylcholine receptor mRNA (58). In situ hybridization completely failed to detect either CCK1R or CCK2R mRNA in adult human pancreas (58, 59). In isolated human pancreatic acini, CCK or secretin stimulation did not produce any functional responses, and no significant specific binding for CCK Fig. 4. CCK stimulates physiological exocrine pancreatic secretion through different pathways: species dependence. CCK is released from intestinal mucosal I cells, which in turn exert its role via different pathways. A: in rodents such as rat, CCK released from I cells is transported to pancreas via circulation, directly stimulating the CCK1 receptors on pancreatic acinar cells. CCK can also activate sensory nerve fibers to activate the long vagovagal and short enteropancreatic reflexes. B: in humans, released CCK activates CCK receptors in the intestinal sensory nerve fibers to excite both the long vagovagal and short enteropancreatic reflexes. Efferent vagal nerve terminals eventually release neurotransmitters such as ACh to stimulate pancreatic acinar cells secretion. The lack of CCK1Rs on human pancreatic acinar cells dictates that circulating CCK does not stimulate digestive enzyme secretion. C: in ducks, circulating CCKs in the presence of neurotransmitter vasoactive intestinal peptide (VIP)/pituitary adenylate cyclase-activating peptide (PACAP) stimulate pancreatic acinar cell secretion. Dashed lines indicate that more work needs to be done before confirmation of the reflexes. DVC, dorsal vagal complex; NG, nodose ganglia; VIP, vasoactive intestinal polypeptide. Drawn with the use of an initial template (64, 65). AJP-Regul Integr Comp Physiol • VOL 292 • FEBRUARY 2007 • www.ajpregu.org Invited Review SPECIES DIFFERENCES IN EXOCRINE PANCREAS SECRETION receptors was found (58, 59, 94). This is in contrast to the high density of CCK1Rs revealed by microautoradiography in the mucosa and in smooth muscles in the human duodenum (94). However, after adenoviral-mediated transfection of either CCK1R or CCK2R gene to human pancreatic acinar cells, these cells became responsive to CCK stimulation (58). These data indicate that human pancreatic acinar cells do not respond to CCK stimulation due to insufficient levels of CCK1R gene expression. With advanced quantitative RT-PCR technology, CCK1R transcription in human pancreas has now become detectable (38), although the cell type expressing it was not determined. In vivo human studies found that the highly specific CCK1R antagonist MK-329 (also known as L-364,718 and devazepide) only slightly affected pancreatic enzyme secretion and gastric emptying but significantly inhibited bile secretion, indicating that CCK is not an essential mediator of postprandial pancreatic enzyme secretion in humans (16). Others found that CCK in vivo stimulated pancreatic secretion by interacting with neural cholinergic system. Atropine in human subjects completely suppressed low-dose CCK-induced digestive enzyme secretion, indicating that CCK-mediated exocrine pancreatic secretion required a cholinergic tone in vivo (108). Atropine blocked significantly meal-stimulated pancreatic digestive enzyme secretion, and the response to graded doses of exogenous CCK was significantly inhibited by both atropine and loxiglumide, a CCK1R antagonist, suggesting that pancreatic enzyme secretion is predominantly dependent on a cholinergic tone and that CCK modulates the enzymesecretory response in human (1). Atropine (5 g 䡠 kg⫺1 䡠 h⫺1) reduced the CCK-stimulated increase in pancreatic enzyme secretion and essentially blocked postprandial enzyme secretion (9). In another study, trypsin output stimulated by physiological doses of CCK was inhibited by atropine by 84.0%, whereas lipase output was inhibited by 78.6% in humans (132). Thus the human exocrine pancreas is crucially dependent on a cholinergic background, with CCK only modulating this secretory response (9). The above data suggest that CCK can act on vagal afferent fibers, which explains how physiological plasma CCK levels act via vagal cholinergic pathways to stimulate pancreatic secretion. Although knowledge of vagal CCK1Rs has come from rodents, other work suggests that this information is also applicable to humans (105). The fact that CCK1Rs exist in human duodenum seems to support such a notion (possibly mediating both vagal afferent input and duodenal-pancreas reflex) (34). Therefore, physiological levels of CCK appear to act entirely via vagal cholinergic pathways to mediate pancreatic secretion in humans (Fig. 4B). Birds. The case for avian CCK stimulation of exocrine pancreatic secretion is different from that for both rats and humans, although the plasma CCK levels seem to be similar in all animal species. Proteins and fatty acids are the major luminal dietary stimuli for CCK release in rat (29, 30, 72, 81, 84). Duodenal infusion of casein, for example, resulted in elevation of plasma CCK from fasting levels of 0.5 ⫾ 0.1 to 3.8 ⫾ 0.4 pM (72). This picomolar postprandial plasma CCK concentration is sufficient to stimulate enzyme secretion and trigger Ca2⫹ oscillation in rat pancreatic acini (2, 21–23, 149). Soya proteins and amino acid mixtures mimicking soya protein composition could increase gut CCK release in chicks AJP-Regul Integr Comp Physiol • VOL R673 (150). In chickens, plasma CCK increases from a basal level (control diet) of 9.6 ⫾ 0.6 to 13.4 ⫾ 0.6 and to 18.1 ⫾ 0.8 pM 90 min after ingestion of a diet supplemented with 100 and 1,000 mg soybean trypsin inhibitor, respectively (37). Plasma CCK concentration is also significantly enhanced in chicks fed medium-chain triglycerides but not in chicks fed long-chain triglycerides (86). However, in chickens, such picomolar CCK Fig. 5. Simultaneous activation of VIP/PACAP and CCK receptor systems results in physiological stimulation of exocrine pancreatic secretion. A. leftward expansion by VIP/PACAP of CCK dose-response curve for amylase secretion from freshly isolated Peking duck pancreatic acini. Acini were incubated with CCK alone (circles), CCK plus PACAP 1 nM (squares), or CCK plus VIP 10 nM (triangles) for 30 min. Amylase secreted into the extracellular medium was then measured and expressed as a percentage of total amylase present in acini before stimulation. PACAP (1 nM) and VIP (10 nM) alone had little effect on amylase secretion. *Lowest CCK concentration at which statistically significant stimulation of amylase secretion was observed. Note the 3 orders of magnitude difference in the absence and presence of PACAP/VIP. Redrawn from data published in Ref. 149. B: low, physiological concentrations of CCK alone do not stimulate amylase secretion in freshly isolated duck pancreatic acini; only when CCK concentration reaches supraphysiological levels will it have a stimulatory effect on amylase secretion, with a maximal stimulatory concentration of 10 nM (solid blue line). Similarly, not until CCK concentration reaches 100 pM will it induce regular Ca2⫹ oscillations. In the presence of physiological concentrations of VIP/PACAP, low physiological concentrations of CCK start to induce significant amylase secretion, higher CCK concentrations induce more amylase secretion, and supraphysiolgical CCK concentrations result in a reduction in amylase secretion (solid black line). Also, in the presence of VIP/PACAP, low physiological concentrations of CCK induce regular Ca2⫹ oscillations. The CCK doseresponse curve in the presence of VIP/PACAP could possibly be broken down into 2 components: at high CCK concentrations, VIP and PACAP serve the purpose of priming zymogen granules for exocytosis (dashed green line); at low CCK concentrations, VIP and PACAP not only prime zymogen granules but also serve to sensitize Ca2⫹ signal generation (dashed yellow line). 292 • FEBRUARY 2007 • www.ajpregu.org Invited Review R674 SPECIES DIFFERENCES IN EXOCRINE PANCREAS SECRETION concentrations do not stimulate pancreatic acini secretion; CCK concentrations 100 times higher are required to elicit secretory response from isolated chicken pancreatic acini. This has led to the belief that endogenous CCK does not have any important role in digestive enzyme secretion from exocrine pancreas in birds (35, 36, 98, 125). In the isolated duck pancreatic acini, picomolar concentrations of CCK do not stimulate either an increase in [Ca2⫹]i or digestive enzyme secretion. CCK at 1 nM was required for stimulation of amylase secretion, with a maximal effect being achieved at 10 nM (149). Vasoactive intestinal peptide (VIP)/ pituitary adenylate cyclase-activating peptide (PACAP) receptor (VPAC) agonists such as PACAP38 and PACAP27 and VIP alone had little effect on amylase secretion in duck pancreatic acini but could make picomolar concentrations of CCK effective. Furthermore, PACAP27 and VIP shifted the maximal stimulating CCK concentrations from 10 to 1 nM (149). Subthreshold CCK (10 pM) in the presence of VPAC agonists induced Ca2⫹ spikes. CCK (10 nM)-induced secretion was inhibited by CCK1R antagonist FK-480 (1 M). Gastrin did not stimulate amylase secretion and did not induce [Ca2⫹]i increase (149). These data suggest that duck pancreatic acini possess both CCK1 and VPAC receptors and that simultaneous activation of both is required for each to play a physiological role (149) (Fig. 5A). As such, VIP/PACAP sensitization of CCK stimulation could probably be broken down into two components. At higher CCK concentrations, VIP/PACAP may primarily serve the purpose of priming zymogen granules for exocytosis; at lower CCK concentrations, VIP/PACAP may also sensitize Ca2⫹ signal generation (Fig. 5B). The presence of VIP/PACAP innervation in avian exocrine pancreas provides a direct line of evidence that VIP or VIP-like receptors are likely to have a physiological role in exocrine pancreatic secretion. In situ studies show that chicken VIP increased the flow of pancreatic juice in turkey (27). Vaillant et al. (139) identified VIP in the gut and pancreas of turkey. Mensah-Brown and Pallot (90) found that Houbara Bustard (Chlamydotis undulata) exocrine pancreas was innervated by VIP, galanin, neuropeptide Y, and some other neurotransmitters. Mirabella et al. (92) found that, in duck, both PACAP38 and PACAP27 are present in neurons and fibers of the enteric nervous system, and PACAP is colocalized with VIP. Peeters et al. (106) also suggested that PACAP receptor exists in chicken pancreas. The well-established innervation of VIP/ PACAP and related receptors in avian pancreas lend support to a role for VIP/PACAP receptors in avian exocrine pancreatic secretion (149). Presently, there is scant information about vagal reflexes and their potential role in exocrine pancreatic secretion in birds. However, there is evidence to indicate that chicken exocrine pancreatic secretion is controlled by the vagus nerve (48). In addition, turkey pancreatic secretion may be controlled by a cholinergic pathway (126). Therefore, neural or vagal reflexes may also exist in avian species. Figure 4C depicts the presently known situation for exocrine pancreatic secretion in birds. CONCLUSIONS AND PERSPECTIVES The hormone CCK is the most important mediator of postprandial pancreatic secretion, particularly concerning digestive AJP-Regul Integr Comp Physiol • VOL enzyme output. Pancreatic secretion can be influenced by CCK either directly via actions on pancreatic acinar cells or indirectly via actions on afferent vagus nerves. The mechanisms of action are species specific. In rodents, CCK acts both directly through the blood and neurally to mediate pancreatic secretion. In humans, CCK appears to act entirely via vagal cholinergic pathways to mediate pancreatic secretion. In birds, VIP/ PACAP and CCK are mutually dependent to directly stimulate exocrine pancreatic secretion at physiological concentrations. This latter conclusion implies mutual dependence of the endocrine and nervous systems. In birds, whether VIP/PACAP and CCK are also needed together to excite the sensory nerves, triggering vagovagal and enteropancreatic reflexes to stimulate pancreatic enzyme secretion, remains unclear. This will require future studies. Avian CCK receptors have not received much attention before, largely because of the uncertainty about its physiological role in exocrine pancreatic secretion. Now that its role is established and significant differences in CCK receptors of bird and mammals are quite obvious both structurally and functionally, more attention should be directed to that respect in the future. ACKNOWLEDGMENTS We thank the anonymous reviewers for suggestions for improving our manuscript. We are gratefully to Prof. Dale Mierke of Brown University for kindly providing the original high-resolution files for Fig. 3. GRANTS This work was supported by Natural Science Foundation of China Grants 39825112, 30070286, 30472048, and 30540420524, by Ministry of Education Grant 104186, and by Natural Science Foundation Beijing Grant 6062014. REFERENCES 1. Adler G, Beglinger C, Braun U, Reinshagen M, Koop I, Schafmayer A, Rovati L, Arnold R. Interaction of the cholinergic system and cholecystokinin in the regulation of endogenous and exogenous stimulation of pancreatic secretion in humans. Gastroenterology 100: 537– 543, 1991. 2. An YP, Xiao R, Cui H, Cui ZJ. Selective activation by photodynamic action of cholecystokinin receptor in the freshly isolated rat pancreatic acini. Br J Pharmacol 139: 872– 880, 2003. 3. Archer-Lahlou E, Escrieut C, Clerc P, Martinez J, Moroder L, Logsdon C, Kopin A, Seva C, Dufresne M, Pradayrol L, Maigret B, Fourmy D. Molecular mechanism underlying partial and full agonism mediated by the human cholecystokinin-1 receptor. J Biol Chem 280: 10664 –10674, 2005. 4. Archer-Lahlou E, Tikhonova I, Escrieut C, Dufresne M, Seva C, Pradayrol L, Moroder L, Maigret B, Fourmy D. Modeled structure of a G-protein-coupled receptor: the cholecystokinin-1 receptor. J Med Chem 48: 180 –191, 2005. 5. Ashby MC, Camello-Almaraz C, Gerasimenko OV, Petersen OH, Tepikin AV. Long distance communication between muscarinic receptors and Ca2⫹ release channels revealed by carbachol uncaging in cell-attached patch pipette. J Biol Chem 278: 20860 –20864, 2003. 6. Backus RC, Howard KA, Rogers QR. The potency of dietary amino acids in elevating plasma cholecystokinin immunoreactivity in cats is related to amino acid hydrophobicity. Regul Pept 72: 31– 40, 1997. 7. Backus RC, Rogers QR, Rosenquist GL, Calam J, Morris JG. Diets causing taurine depletion in cats substantially elevate postprandial plasma cholecystokinin concentration. J Nutr 125: 2650 –2657, 1995. 8. Bayle D, Weeks D, Sachs G. Identification of membrane insertion sequences of the rabbit gastric cholecystokinin-A receptor by in vitro translation. J Biol Chem 272: 19697–19707, 1997. 9. Beglinger C, Hildebrand P, Adler G, Werth B, Luo H, Delco F, Gyr K. Postprandial control of gallbladder contraction and exocrine pancreatic secretion in man. Eur J Clin Invest 22: 827– 834, 1992. 292 • FEBRUARY 2007 • www.ajpregu.org Invited Review SPECIES DIFFERENCES IN EXOCRINE PANCREAS SECRETION 10. Beinborn M, Lee YM, McBride EW, Quinn SM, Kopin AS. A single amino acid of the cholecystokinin-B/gastrin receptor determines specificity for non-peptide antagonists. Nature 362: 348 –350, 1993. 11. Beinfeld MC. Biosynthesis and processing of pro CCK: recent progress and future challenges. Life Sci 72: 747–757, 2003. 12. Broberger C, Holmberg K, Shi TJ, Dockray G, Hokfelt T. Expression and regulation of cholecystokinin and cholecystokinin receptors in rat nodose and dorsal root ganglia. Brain Res 903: 128 –140, 2001. 13. Buchan AM, Polak JM, Solcia E, Capella C, Hudson D, Pearse AG. Electron immunohistochemical evidence for the human intestinal I cell as the source of CCK. Gut 19: 403– 407, 1978. 14. Byrnes DJ, Henderson L, Borody T, Rehfeld JF. Radioimmunoassay of cholecystokinin in human plasma. Clin Chim Acta 111: 81– 89, 1981. 15. Cantor P. Evaluation of a radioimmunoassay for cholecystokinin in human plasma. Scand J Clin Lab Invest 46: 213–221, 1986. 16. Cantor P, Mortensen PE, Myhre J, Gjorup I, Worning H, Stahl E, Survill TT. The effect of the cholecystokinin receptor antagonist MK329 on meal-stimulated pancreaticobiliary output in humans. Gastroenterology 102: 1742–1751, 1992. 17. Cantor P, Rehfeld JF. Cholecystokinin in pig plasma: release of components devoid of a bioactive COOH-terminus. Am J Physiol Gastrointest Liver Physiol 256: G53–G61, 1989. 18. Chang CH, Chey WY, Chang TM. Cellular mechanism of sodium oleate-stimulated secretion of cholecystokinin and secretin. Am J Physiol Gastrointest Liver Physiol 279: G295–G303, 2000. 19. Chen ZW, Bergman T, Jornvall H, Bonetto V, Norberg A, Mutt V, Longone P, Costa E, Efendic S, Ostenson CG. Full-length and Nterminally truncated chicken intestinal diazepam-binding inhibitor. Purification, structural characterization and influence on insulin release. Regul Pept 69: 63– 68, 1997. 20. Corp ES, McQuade J, Moran TH, Smith GP. Characterization of type A and type B CCK receptor binding sites in rat vagus nerve. Brain Res 623: 161–166, 1993. 21. Cui ZJ, He XH. The pre-synaptic blocker toosendanin does not inhibit secretion in exocrine cells. World J Gastroenterol 8: 918 –922, 2002. 22. Cui ZJ, Kanno T. Photodynamic triggering of calcium oscillation in the isolated rat pancreatic acini. J Physiol 504: 47–55, 1997. 23. Cui ZJ, Kanno T. Cholecystokinin analog JMV-180-induced intracellular calcium oscillations are mediated by inositol 1,4,5-trisphosphate in rat pancreatic acini. Acta Pharmacol Sin 21: 377–380, 2000. 24. Dawson ES, Henne RM, Miller LJ, Lybrand TP. Molecular models for cholecystokinin-A receptor. Pharmacol Toxicol 91: 290 –296, 2002. 25. De Weerth A, Pisegna JR, Huppi K, Wank SA. Molecular cloning, functional expression and chromosomal localization of the human cholecystokinin type A receptor. Biochem Biophys Res Commun 194: 811– 818, 1993. 26. De Weerth A, Pisegna JR, Wank SA. Guinea pig gallbladder and pancreas possess identical CCK-A receptor subtypes: receptor cloning and expression. Am J Physiol Gastrointest Liver Physiol 265: G1116 – G1121, 1993. 27. Dimaline R, Dockray GJ. Potent stimulation of the avian exocrine pancreas by porcine and chicken vasoactive intestinal peptide. J Physiol 294: 153–163, 1979. 28. Ding XQ, Pinon DI, Furse KE, Lybrand TP, Miller LJ. Refinement of the conformation of a critical region of charge-charge interaction between cholecystokinin and its receptor. Mol Pharmacol 61: 1041–1052, 2002. 29. Douglas BR, Jansen JB, de Jong AJ, Lamers CB. Effect of various triglycerides on plasma cholecystokinin levels in rats. J Nutr 120: 686 – 690, 1990. 30. Douglas BR, Woutersen RA, Jansen JB, de Jong AJ, Lamers CB. The influence of different nutrients on plasma cholecystokinin levels in the rat. Experientia 44: 21–23, 1988. 31. Dubois PM, Paulin C, Chayvialle JA. Identification of gastrin-secreting cells and cholecystokinin-secreting cells in the gastrointestinal tract of the human fetus and adult man. Cell Tissue Res 175: 351–356, 1976. 32. Eysselein VE, Eberlein GA, Hesse WH, Singer MV, Goebell H, Reeve JR Jr. Cholecystokinin-58 is the major circulating form of cholecystokinin in canine blood. J Biol Chem 262: 214 –217, 1987. 33. Fried GM, Ogden WD, Swierczek J, Greeley GH Jr, Rayford PL, Thompson JC. Release of cholecystokinin in conscious dogs: correlation with simultaneous measurements of gallbladder pressure and pancreatic protein secretion. Gastroenterology 85: 1113–1119, 1983. AJP-Regul Integr Comp Physiol • VOL R675 34. Funakoshi A, Fukamizu Y, Miyasaka K. Mechanism of cholecystokinin-A receptor antagonist on human pancreatic exocrine secretion. Localization of CCK-A receptor in the human duodenum. Digestion 60: 75– 80, 1999. 35. Furuse M. Release and endogenous actions of the gastrin/cholecystokinin (CCK) family in the chicken. J Exp Zool 283: 448 – 454, 1999. 36. Furuse M, Choi YH, Satoh S, Okumura J. The action of the cholecystokinin-A receptor antagonist, devazepide, on the digestive system of the chicken. Experientia 52: 353–356, 1996. 37. Furuse M, Yang SI, Muramatsu T, Okumura J. Enhanced release of cholecystokinin by soya-bean trypsin inhibitor in chickens. Scand J Gastroenterol 25: 1242–1246, 1990. 38. Galindo J, Jones N, Powell GL, Hollingsworth SJ, Shankley N. Advanced qRT-PCR technology allows detection of the cholecystokinin 1 receptor (CCK1R) expression in human pancreas. Pancreas 31: 325– 331, 2005. 39. Gevrey JC, Laurent S, Saurin JC, Nemoz-Gaillard E, Regazzi R, Chevrier AM, Chayvialle JA, Abello J. Rab3a controls exocytosis in cholecystokinin-secreting cells. FEBS Lett 503: 19 –24, 2001. 40. Ghanekar D, Hadac EM, Holicky EL, Miller LJ. Differences in partial agonist action at cholecystokinin receptors of mouse and rat are dependent on parameters extrinsic to receptor structure: molecular cloning, expression and functional characterization of the mouse type A cholecystokinin receptor. J Pharmacol Exp Ther 282: 1206 –1212, 1997. 41. Ghilardi JR, Allen CJ, Vigna SR, McVey DC, Mantyh PW. Cholecystokinin and neuropeptide Y receptors on single rabbit vagal afferent ganglion neurons: site of prejunctional modulation of visceral sensory neurons. Brain Res 633: 33– 40, 1994. 42. Giragossian C, Mierke DF. Intermolecular interactions between cholecystokinin-8 and the third extracellular loop of the cholecystokinin A receptor. Biochemistry 40: 3804 –3809, 2001. 43. Giragossian C, Suggs EE, Szewczyk JR, Mierke DF. Intermolecular interactions between peptidic and nonpeptidic agonists and the third extracellular loop of the cholecystokinin 1 receptor. J Med Chem 46: 3476 –3482, 2003. 44. Glassmeier G, Herzig KH, Hopfner M, Lemmer K, Jansen A, Scherubl H. Expression of functional GABAA receptors in cholecystokinin-secreting gut neuroendocrine murine STC-1 cells. J Physiol 510: 805– 814, 1998. 45. Green GM, Lyman RL. Feedback regulation of pancreatic enzyme secretion as a mechanism for trypsin inhibitor-induced hypersecretion in rats. Proc Soc Exp Biol Med 140: 6 –12, 1972. 46. Grider JR. Role of cholecystokinin in the regulation of gastrointestinal motility. J Nutr 124: 1334S-1339S, 1994. 47. Herzig KH, Schon I, Tatemoto K, Ohe Y, Li Y, Folsch UR, Owyang C. Diazepam binding inhibitor is a potent cholecystokinin-releasing peptide in the intestine. Proc Natl Acad Sci USA 93: 7927–7932, 1996. 48. Hiramatsu K, Watanabe T. Ultrastructural and morphometric studies on the peripheral course of the vagus in the domestic fowl, with particular reference to the cholinergic innervation of the pancreas. Ann Anat 175: 335–341, 1993. 49. Holicky EL, Hadac EM, Ding XQ, Miller LJ. Molecular characterization and organ distribution of type A and B cholecystokinin receptors in cynomolgus monkey. Am J Physiol Gastrointest Liver Physiol 281: G507–G514, 2001. 50. Hopman WP, Jansen JB, Rosenbusch G, Lamers CB. Effect of equimolar amounts of long-chain triglycerides and medium-chain triglycerides on plasma cholecystokinin and gallbladder contraction. Am J Clin Nutr 39: 356 –359, 1984. 51. Hosotani R, Chowdhury P, Doi R, Rayford PL. Characterization of interactions between CCK-33 and CCK receptors in isolated dispersed pancreatic acini. J Cell Physiol 153: 523–527, 1992. 52. Ibarz G, Oiry C, Carnazzi E, Crespy P, Escrieut C, Fourmy D, Galleyrand JC, Gagne D, Martinez J. Cholecystokinin 1 receptor modulates the MEKK1-induced c-Jun trans-activation: structural requirements of the receptor. Br J Pharmacol 147: 951–958, 2006. 53. Isaacs PE, Ladas S, Forgacs IC, Dowling RH, Ellam SV, Adrian TE, Bloom SR. Comparison of effects of ingested medium- and long-chain triglyceride on gallbladder volume and release of cholecystokinin and other gut peptides. Dig Dis Sci 32: 481– 486, 1987. 54. Jansen A, Hoepfner M, Herzig KH, Riecken EO, Scherubl H. GABAC receptors in neuroendocrine gut cells: a new GABA-binding site in the gut. Pflügers Arch 441: 294 –300, 2000. 292 • FEBRUARY 2007 • www.ajpregu.org Invited Review R676 SPECIES DIFFERENCES IN EXOCRINE PANCREAS SECRETION 55. Jansen JB, Lamers CB. Radioimmunoassay of cholecystokinin in human tissue and plasma. Clin Chim Acta 131: 305–316, 1983. 56. Jaworek J, Konturek SJ. Effects of pirenzepine and atropine on amylase response to various secretagogues from the rat pancreatic acini. Digestion 36: 175–181, 1987. 57. Jensen RT, Wank SA, Rowley WH, Sato S, Gardner JD. Interaction of CCK with pancreatic acinar cells. Trends Pharmacol Sci 10: 418 – 423, 1989. 58. Ji B, Bi Y, Simeone D, Mortensen RM, Logsdon CD. Human pancreatic acinar cells lack functional responses to cholecystokinin and gastrin. Gastroenterology 121: 1380 –1390, 2001. 59. Ji B, Bi Y, Simeone D, Mortensen RM, Logsdon CD. Human pancreatic acinar cells do not respond to cholecystokinin. Pharmacol Toxicol 91: 327–332, 2002. 60. Johnsen AH. Phylogeny of the cholecystokinin/gastrin family. Front Neuroendocrinol 19: 73–99, 1998. 61. Jonson L, Schoeman N, Saayman H, Naude R, Jensen Hanne, Johnsen AH. Identification of ostrich and chicken cholecystokinin cDNA and intestinal peptides. Peptides 21: 1337–1344, 2000. 62. Jordinson M, Beales IL, Calam J. Soybean agglutinin stimulated cholecystokinin release from cultured rabbit jejunal cells requires calcium influx via L-type calcium channels. Peptides 19:1541–1547, 1998. 63. Kerstens PJ, Lamers CB, Jansen JB, de Jong AJ, Hessels M, Hafkenscheid JC. Physiological plasma concentrations of cholecystokinin stimulate pancreatic enzyme secretion and gallbladder contraction in man. Life Sci 36: 565–569, 1985. 64. Konturek PC, Konturek SJ. The history of gastrointestinal hormones and the Polish contribution to elucidation of their biology and relation to nervous system. J Physiol Pharmacol 54: 83–98, 2003. 65. Konturek SJ, Pepera J, Zabielski K, Konturek PC, Pawlik T, Szlachcic A, Hahn EG. Brain-gut axis in pancreatic secretion and appetite control. J Physiol Pharmacol 54: 293–317, 2003. 66. Kopin AS, Lee YM, McBride EW, Miller LJ, Lu M, Lin HY, Kolakowski LF Jr, Beinborn M. Expression cloning and characterization of the canine parietal cell gastrin receptor. Proc Natl Acad Sci USA 89: 3605–3609, 1992. 67. Kopin AS, McBride EW, Quinn SM, Kolakowski LF Jr, Beinborn M. The role of the cholecystokinin-B/gastrin receptor transmembrane domains in determining affinity for subtype-selective ligands. J Biol Chem 270: 5019 –5023, 1995. 68. Lankisch TO, Tsunoda Y, Lu Y, Owyang C. Characterization of CCK-A receptor affinity states and Ca2⫹ signal transduction in vagal nodose ganglia. Am J Physiol Gastrointest Liver Physiol 282: G1002– G1008, 2002. 69. Larsson KP, Akerman KE, Magga J, Uotila S, Kukkonen JP, Nasman J, Herzig KH. The STC-1 cells express functional orexin-A receptors coupled to CCK release. Biochem Biophys Res Commun 309: 209 –216, 2003. 70. Ledeboer M, Masclee AA, Biemond I, Lamers CB. Gallbladder motility and cholecystokinin secretion during continuous enteral nutrition. Am J Gastroenterol 92: 2274 –2279, 1997. 71. Lee YM, Beinborn M, McBride EW, Lu M, Kolakowski LF Jr, Kopin AS. The human brain cholecystokinin-B/gastrin receptor. Cloning and characterization. J Biol Chem 268: 8164 – 8169, 1993. 72. Lewis LD, Williams JA. Regulation of cholecystokinin secretion by food, hormones, and neural pathways in the rat. Am J Physiol Gastrointest Liver Physiol 258: G512–G518, 1990. 73. Li Y, Hao Y, Owyang C. High-affinity CCK-A receptors on the vagus nerve mediate CCK-stimulated pancreatic secretion in rats. Am J Physiol Gastrointest Liver Physiol 273: G679 –G685, 1997. 74. Li Y, Owyang C. Vagal afferent pathway mediates physiological action of cholecystokinin on pancreatic enzyme secretion. J Clin Invest 92: 418 – 424, 1993. 75. Li Y, Owyang C. Endogenous cholecystokinin stimulates pancreatic enzyme secretion via vagal afferent pathway in rats. Gastroenterology 107: 525–531, 1994. 76. Li Y, Zhu J, Owyang C. Electrical physiological evidence for high and low-affinity vagal CCK-A receptors. Am J Physiol Gastrointest Liver Physiol 277: G469 –G477, 1999. 77. Liddle RA. Regulation of cholecystokinin secretion by intraluminal releasing factors. Am J Physiol Gastrointest Liver Physiol 269: G319 – G327, 1995. 78. Liddle RA. Cholecystokinin cells. Annu Rev Physiol 59: 221–242, 1997. AJP-Regul Integr Comp Physiol • VOL 79. Liddle RA. Regulation of cholecystokinin secretion in humans. J Gastroenterol 35: 181–187, 2000. 80. Liddle RA, Goldfine ID, Rosen MS, Taplitz RA, Williams JA. Cholecystokinin bioactivity in human plasma. Molecular forms, responses to feeding, and relationship to gallbladder contraction. J Clin Invest 75: 1144 –1152, 1985. 81. Liddle RA, Green GM, Conrad CK, Williams JA. Proteins but not amino acids, carbohydrates, or fats stimulate cholecystokinin secretion in the rat. Am J Physiol Gastrointest Liver Physiol 251: G243– G248, 1986. 82. Liddle RA, Misukonis MA, Pacy L, Balber AE. Cholecystokinin cells purified by fluorescence-activated cell sorting respond to monitor peptide with an increase in intracellular calcium. Proc Natl Acad Sci USA 89: 5147–5151, 1992. 83. Lin CW, Miller TR. Both CCK-A and CCK-B/gastrin receptors are present on rabbit vagus nerve. Am J Physiol Regul Integr Comp Physiol 263: R591–R595, 1992. 84. Linden A, Carlquist M, Hansen S, Uvnas-Moberg K. Plasma concentrations of cholecystokinin, CCK-8, and CCK-33, 39 in rats, determined by a method based on enzyme digestion of gastrin before HPLC and RIA detection of CCK. Gut 30: 213–222, 1989. 85. Linden A, Uvnas-Moberg K. Plasma levels of cholecystokinin (CCK-8 and CCK-33–39) in response to feeding and during pregnancy in dogs. Scand J Gastroenterol 22: 859 – 864, 1987. 86. Mabayo RT, Furuse M, Yang SI, Okumura J. Medium-chain triacylglycerols enhance release of cholecystokinin in chicks. J Nutr 122: 1702–1705, 1992. 87. Martin MT, Fernandez E, Rodriguez-Sinovas A, Gonalons E. Effects of cholecystokinin on chicken cecal motility: mechanisms involved. Life Sci 56: 601– 610, 1995. 88. McLaughlin JT, Lomax RB, Hall L, Dockray GJ, Thompson DG, Warhurst G. Fatty acids stimulate cholecystokinin secretion via an acyl chain length-specific, Ca2⫹-dependent mechanism in the enteroendocrine cell line STC-1. J Physiol 513: 11–18, 1998. 89. McVey DC, Romac JM, Clay WC, Kost TA, Liddle RA, Vigna SR. Monitor peptide binding sites are expressed in the rat liver and small intestine. Peptides 20: 457– 464, 1999. 90. Mensah-Brown EP, Pallot DJ. Peptidergic and aminergic neurotransmitters of the exocrine pancreas of the Houbara Bustard (Chlamydotis undulata). J Morphol 244: 23–29, 2000. 91. Mierke DF, Giragossian C. Peptide hormone binding to G-proteincoupled receptors: structural characterization via NMR techniques. Med Res Rev 21: 450 – 471, 2001. 92. Mirabella N, Squillacioti C, Colitti M, Germano G, Pelagalli A, Paino G. Pituitary adenylate cyclase activating peptide (PACAP) immunoreactivity and mRNA expression in the duck gastrointestinal tract. Cell Tissue Res 308: 347–359, 2002. 93. Miyasaka K, Funakoshi A. Cholecystokinin and cholecystokinin receptors. J Gastroenterol 38: 1–13, 2003. 94. Miyasaka K, Shinozaki H, Jimi A, Funakoshi A. Amylase secretion from dispersed human pancreatic acini: neither cholecystokinin A nor cholecystokinin B receptors mediate amylase secretion in vitro. Pancreas 25: 161–165, 2002. 95. Moran TH, Smith GP, Hostetler AM, McHugh PR. Transport of cholecystokinin (CCK) binding sites in subdiaphragmatic vagal branches. Brain Res 415: 149 –152, 1987. 96. Moriarty P, Dimaline R, Thompson DG, Dockray GJ. Characterization of cholecystokinin A and cholecystokinin B receptors expressed by vagal afferent neurons. Neuroscience 79: 905–913, 1997. 97. Morton MF, Pyati J, Dai H, Li L, Moreno V, Shankley NP. Molecular cloning, expression and pharmacological characterization of the canine cholecystokinin 1 receptor. Br J Pharmacol 145: 374 –384, 2005. 98. Murai A, Satoh S, Okumura J, Furuse M. Factors regulating amylase secretion from chicken pancreatic acini in vitro. Life Sci 66: 585–591, 2000. 99. Muramatsu S, Sonobe K, Mizumoto A, Yamada T, Itoh Z. Relationship between gallbladder bile concentration and motility in conscious dogs: role of cholecystokinin. Peptides 18: 111–118, 1997. 100. Nemoz-Gaillard E, Bosshard A, Regazzi R, Bernard C, Cuber JC, Takahashi M, Catsicas S, Chayvialle JA, Abello J. Expression of SNARE proteins in enteroendocrine cell lines and functional role of tetanus toxin-sensitive proteins in cholecystokinin release. FEBS Lett 425: 66 –70, 1998. 292 • FEBRUARY 2007 • www.ajpregu.org Invited Review SPECIES DIFFERENCES IN EXOCRINE PANCREAS SECRETION 101. Nemoz-Gaillard E, Cordier-Bussat M, Filloux C, Cuber JC, Van Obberghen E, Chayvialle JA, Abello J. Bombesin stimulates cholecystokinin secretion through mitogen-activated protein-kinase-dependent and -independent mechanisms in the enteroendocrine STC-1 cell line. Biochem J 331: 129 –135, 1998. 102. Nilsson IB, Svensson SP, Monstein HJ. Molecular cloning of an unusual bicistronic cholecystokinin receptor mRNA expressed in chicken brain: a structural and functional expression study. Regul Pept 114: 37– 43, 2003. 103. Noble F, Wank SA, Crawley JN, Bradwejn J, Seroogy KB, Hamon M, Roques BP. International Union of Pharmacology. XXI. Structure, distribution, and functions of cholecystokinin receptors. Pharmacol Rev 51: 745–781, 1999. 104. Oliver AS, Vigna SR. CCK-A- and CCK-B-like receptors in the gallbladder and stomach of the alligator (Alligator mississippiensis). Gen Comp Endocrinol 105: 91–101, 1997. 105. Owyang C, Logsdon CD. New insights into neurohormonal regulation of pancreatic secretion. Gastroenterology 127: 957–969, 2004. 106. Peeters K, Gerets HH, Princen K, Vandesande F. Molecular cloning and expression of a chicken pituitary adenylate cyclaseactivating polypeptide receptor. Brain Res Mol Brain Res 71: 244 – 255, 1999. 107. Pellegrini M, Mierke DF. Molecular complex of cholecystokinin-8 and N-terminus of the cholecystokinin A receptor by NMR spectroscopy. Biochemistry 38: 14775–14783, 1999. 108. Pfeffer F, Nauck M, Reinert A, Benz S, Schareck W, Hopt UT. Influence of the extrinsic nervous system on exocrine pancreatic secretion in the human. Langenbecks Arch Chir Suppl Kongressbd 115: 437– 442, 1998. 109. Polak JM, Bloom SR, Rayford PL, Pearse AG, Buchan AM, Thompson JC. Identification of cholecystokinin-secreting cells. Lancet 2: 1016 –1018, 1975. 110. Pozo MJ, Estevez MJ, Alcon S, Camello PJ, Pariente JA, Salido GM. Cholinergic dependence of pancreatic response to cholecystokinin in rats and guinea pigs. Gen Pharmacol 26: 843– 850, 1995. 111. Rawdon BB, Andrew A. Gut endocrine cells in birds: an overview, with particular reference to the chemistry of gut peptides and the distribution, ontogeny, embryonic origin and differentiation of the endocrine cells. Prog Histochem Cytochem 34: 3– 82, 1999. 112. Reeve JR Jr, Green GM, Chew P, Eysselein VE, Keire DA. CCK-58 is the only detectable endocrine form of cholecystokinin in rat. Am J Physiol Gastrointest Liver Physiol 285: G255–G265, 2003. 113. Rehfeld JF. The molecular nature of cholecystokinin in plasma. An in vivo immunosorption study in rabbits. Scand J Gastroenterol 29: 110 – 121, 1994. 114. Rehfeld JF. Accurate measurement of cholecystokinin in plasma. Clin Chem 44: 991–1001, 1998. 115. Rehfeld JF. Clinical endocrinology and metabolism. Cholecystokinin. Best Pract Res Clin Endocrinol Metab 18: 569 –586, 2004. 116. Rehfeld JF, Bungaard JR, Friis-Hansen L, Goetze JP. On the tissuespecific processing of procholecystokinin in the brain and gut: a short review. J Physiol Pharmacol 54: S73–S79, 2003. 117. Rehfeld JF, Hansen HF, Marley PD, Stengaard-Pedersen K. Molecular forms of cholecystokinin in the brain and the relationship to neuronal gastrins. Ann NY Acad Sci 448: 11–23, 1985. 118. Rehfeld JF, Sun G, Christensen T, Hillingso JG. The predominant cholecystokinin in human plasma and intestine is cholecystokinin-33. J Clin Endocrinol Metab 86: 251–258, 2001. 119. Reuben M, Rising L, Prinz C, Hersey S, Sachs G. Cloning and expression of the rabbit gastric CCK-A receptor. Biochim Biophys Acta 1219: 321–327, 1994. 120. Rindi G, Grant SG, Yiangou Y, Ghatei MA, Bloom SR, Bautch VL, Solcia E, Polak JM. Development of neuroendocrine tumors in the gastrointestinal tract of transgenic mice. Heterogeneity of hormone expression. Am J Pathol 136: 1349 –1363, 1990. 121. Rodriguez-Sinovas A, Fernandez AG, Gonalons E. Central and peripheral cholecystokinin receptors in chickens differ from those in mammals. Regul Pept 60: 47–54, 1995. 122. Rogers J, Hughes RG, Matthews EK. Cyclic GMP inhibits protein kinase C-mediated secretion in rat pancreatic acini. J Biol Chem 263: 3713–3719, 1988. 123. Sankaran H, Goldfine ID, Bailey A, Licko V, Williams JA. Relationship of cholecystokinin receptor binding to regulation of biological AJP-Regul Integr Comp Physiol • VOL 124. 125. 126. 127. 128. 129. 130. 131. 132. 133. 134. 135. 136. 137. 138. 139. 140. 141. 142. 143. R677 functions in pancreatic acini. Am J Physiol Gastrointest Liver Physiol 242: G250 –G257, 1982. Sarri E, Ramos B, Salido GM, Claro E. The cholecystokinin analogs JMV-180 and CCK-8 stimulate phospholipase C through the same binding site of CCK (A) receptor in rat pancreatic acini. Br J Pharmacol 133: 1227–1234, 2001. Satoh S, Furuse M, Choi YH, Okumura J. Cholecystokinin is not a major regulator in the digestive system in the chicken. Experientia 50: 812– 814, 1994. Satoh S, Furuse M, Okumura J. Factors influencing the intestinal phase of pancreatic exocrine secretion in the turkey. Experientia 51: 249 –251, 1995. Scott L, Prpic V, Capel WD, Basavappa S, Mangel AW, Gettys TW, Liddle RA. Beta-adrenergic regulation of cholecystokinin secretion in STC-1 cells. Am J Physiol Gastrointest Liver Physiol 270: G291–G297, 1996. Sharara AI, Bouras EP, Misukonis MA, Liddle RA. Evidence for indirect dietary regulation of cholecystokinin release in rats. Am J Physiol Gastrointest Liver Physiol 265: G107–G112, 1993. Sidhu SS, Thompson DG, Warhurst G, Case RM, Benson RS. Fatty acid-induced cholecystokinin secretion and changes in intracellular Ca2⫹ in two enteroendocrine cell lines, STC-1 and GLUTag. J Physiol 528: 165–176, 2000. Simasko SM, Wiens J, Karpiel A, Covasa M, Ritter RC. Cholecystokinin increases cytosolic calcium in a subpopulation of cultured vagal afferent neurons. Am J Physiol Regul Integr Comp Physiol 283: R1303– R1313, 2002. Snow ND, Prpic V, Mangel AW, Sharara AI, McVey DC, Hurst LJ, Vigna SR, Liddle RA. Regulation of cholecystokinin secretion by bombesin in STC-1 cells. Am J Physiol Gastrointest Liver Physiol 267: G859 –G865, 1994. Soudah HC, Lu Y, Hasler WL, Owyang C. Cholecystokinin at physiological levels evokes pancreatic enzyme secretion via a cholinergic pathway. Am J Physiol Gastrointest Liver Physiol 263: G102–G107, 1992. Spannagel AW, Green GM, Guan D, Liddle RA, Faull K, Reeve JR Jr. Purification and characterization of a luminal cholecystokinin-releasing factor from rat intestinal secretion. Proc Natl Acad Sci USA 93: 4415– 4420, 1996. Spannagel AW, Reeve JR Jr, Greeley GH Jr, Yanaihara N, Liddle RA, Green GM. Bioactivity of intraduodenally and intravenously infused fragments of luminal cholecystokinin releasing factor (LCRF). Regul Pept 773: 161–164, 1998. Sun G, Chang TM, Xue WJ, Wey JF, Lee KY, Chey WY. Release of cholecystokinin and secretin by sodium oleate in dogs: molecular form and bioactivity. Am J Physiol Gastrointest Liver Physiol 262: G35–G43, 1992. Takahashi A, Tanaka S, Miwa Y, Yoshida H, Ikegami A, Niikawa J, Mitamura K. Involvement of calmodulin and protein kinase C in cholecystokinin release by bombesin from STC-1 cells. Pancreas 21: 231–239, 2000. Tarasova N, Spannagel AW, Green GM, Gomez G, Reed JT, Thompson JC, Hellmich MR, Reeve JR Jr, Liddle RA, Greeley GH Jr. Distribution and localization of a novel cholecystokinin-releasing factor in the rat gastrointestinal tract. Endocrinology 138: 5550 –5554, 1997. Thomas RP, Hellmich MR, Townsend CM, Evers BM. Role of gastrointestinal hormones in the proliferation of normal and neoplastic tissues. Endocr Rev 24: 571–599, 2003. Vaillant C, Dimaline R, Dockray GJ. The distribution and cellular origin of vasoactive intestinal polypeptide in the gastrointestinal tract and pancreas. Cell Tissue Res 211: 511–523, 1980. Vigna SR, Thorndyke MC, Williams JA. Evidence for a common evolutionary origin of brain and pancreas cholecystokinin receptors. Proc Natl Acad Sci USA 83: 4355– 4359, 1986. Wang Y, Prpic V, Green GM, Reeve JR Jr, Liddle RA. Luminal CCK-releasing factor stimulates CCK release from human intestinal endocrine and STC-1 cells. Am J Physiol Gastrointest Liver Physiol 282: G16 –G22, 2002. Wank SA. Cholecystokinin receptors. Am J Physiol Gastrointest Liver Physiol 269: G628 –G646, 1995. Wank SA. G-protein-coupled receptors in gastrointestinal physiology. I. CCK receptors: an exemplary family. Am J Physiol Gastrointest Liver Physiol 274: G607–G613, 1998. 292 • FEBRUARY 2007 • www.ajpregu.org Invited Review R678 SPECIES DIFFERENCES IN EXOCRINE PANCREAS SECRETION 144. Wank SA, Harkins R, Jensen RT, Shapira H, de Weerth A, Slattery T. Purification, molecular cloning, and functional expression of the cholecystokinin receptor from rat pancreas. Proc Natl Acad Sci USA 89: 3125–3129, 1992. 145. Widdop RE, Krstew E, Mercer LD, Carlberg M, Beart PM, Jarrott B. Electrophysiological and autoradiographical evidence for cholecystokinin A receptors on rat isolated nodose ganglia. J Auton Nerv Syst 46: 65–73, 1994. 146. Willems PH, Van Emst-de Vries SE, De Pont JJ. Cholecystokininstimulated enzyme secretion from dispersed rabbit pancreatic acinar cells: phosphorylation-dependent changes in potency and efficacy. Pflügers Arch 430: 626 – 635, 1995. 147. Williams JA, Korc M, Dormer RL. Action of secretagogues on a new preparation of functionally intact, isolated pancreatic acini. Am J Physiol Endocrinol Metab Gastrointest Physiol 235: E517–E524, 1978. 148. Williams JA, Sans MD, Tashiro M, Schafer C, Bragado MJ, Dabrowski A. Cholecystokinin activates a variety of intracellular signal AJP-Regul Integr Comp Physiol • VOL 149. 150. 151. 152. 153. transduction mechanisms in rodent pancreatic acinar cells. Pharmacol Toxicol 91: 297–303, 2002. Xiao R, Cui ZJ. Mutual dependence of VIP/PACAP and CCK receptor signaling for a physiological role in duck exocrine pancreatic secretion. Am J Physiol Regul Integr Comp Physiol 286: R189 –R198, 2004. Yang SI, Furuse M, Muramatsu T, Okumura J. Enhanced release of cholecystokinin by dietary amino acids in chicks (Gallus domesticus). Comp Biochem Physiol A 92: 319 –322, 1989. Yoshida H, Tsunoda Y, Owyang C. Diazepam-binding inhibitor33–50 elicits Ca2⫹ oscillation and CCK secretion in STC-1 cells via L-type Ca2⫹ channels. Am J Physiol Gastrointest Liver Physiol 276: G694–G702, 1999. Yule DI, Williams JA. CCK antagonists reveal that CCK-8 and JMV180 interact with different sites on the rat pancreatic acinar cell CCKA receptor. Peptides 15: 1045–1051, 1994. Zarbin MA, Wamsley JK, Innis RB, Kuhar MJ. Cholecystokinin receptors: presence and axonal flow in the rat vagus nerve. Life Sci 29: 697–705, 1981. 292 • FEBRUARY 2007 • www.ajpregu.org