Today - Oregon State University
advertisement

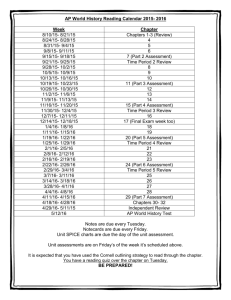
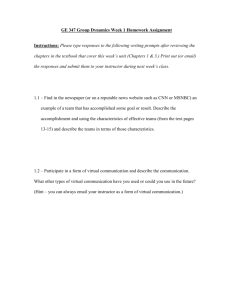
Chapters 18 - 20: Cardiovascular System P Exam I Exam II Today: A. Leukocytes B. Platelets Blood C. Hemostatis D. Heart Anatomy Mariners Tigers 3 4 Blood Components - Erythrocytes: • Balance of RBCs important: • Low = tissue hypoxia • High = viscous blood • Iron and B-complex vitamins crucial for RBC development • Vitamin B12 and folic acid = Proper DNA synthesis • Iron = Hemoglobin synthesis • Stored as ferritin and hemosiderin • Transported in blood via transferrins • Reserves = hemoglobin (80%), cells (20%), blood (<1%) • Controlled hormonally by erythropoietin • Produced by kidney (~ 85%) and liver (~ 15%) Chapters 18 - 20: Cardiovascular System Chapters 18 - 20: Cardiovascular System Blood Components - Erythrocytes: Blood Components - Erythrocytes: Hypoxia Lo wB loo d OOxygen Level Normal Blood xyg en Le vel Increased O2 Level in Blood 1) RBC loss 2) Low O2 3) Exercise Normal Blood Oxygen Level Reduced O2 Level in Blood Erythropoietin Stimulates Bone Marrow RBCs Mature More Rapidly Kidney Releases Erythropoietin Chapters 18 - 20: Cardiovascular System Increased O2 Level in Blood RBCs Mature More Rapidly Reduced O2 Level in Blood Erythropoietin Stimulates Bone Marrow Kidney Releases Erythropoietin Chapters 18 - 20: Cardiovascular System Lifecycle of RBCs: Blood Components - Erythrocytes: Erythrocyte Disorders: 1) Anemias (↓ oxygen carrying capacity) • Decreased RBCs (e.g. blood loss, marrow destruction) • Decreased Hemoglobin (e.g. iron / B12 deficiency) • Abnormal Hemoglobin (e.g. Thalassemia; Sickle-cell anemia) 2) Polycythemia (↑ RBCs) • Bone marrow cancer • High altitude living • Blood doping (artificial) (Figure 18.7) Whole Blood EPO Chapters 18 - 20: Cardiovascular System Chapters 18 - 20: Cardiovascular System Blood Components - Leukocytes: Granulocytes (contain granules): Blood Components: 3) Leukocytes (White Blood Cells - WBCs) • Complete cell • Function in defense against disease • Utilize blood for transport • Perform most functions in tissue (exit = diapedesis) • Produced in bone marrow • Produced/mobilize quickly • Generally < 1 day in circulation 1) Neutrophils (55-65%) • Small granules (hydrolytic enzymes/defensins) • Multi-lobed nuclei • Engulf bacteria/fungi (respiratory burst) 2) Eosinophils (1-4%) • Large granules (lysosomes) • Bi-lobed nuclei • Attack parasitic worms (e.g. tapeworms) 3) Basophils (< 1%) • Large granules (histamines) • U-shaped nuclei • Vasodilate vessels/attract WBCs Chapters 18 - 20: Cardiovascular System Chapters 18 - 20: Cardiovascular System Blood Components - Leukocytes Leukopoiesis (Figure 18.11): Blood Components - Leukoocytes: Agranulocytes (lack granules): proerythroblast 1) Lymphocytes (25-35%) • Large nuclei • Few in blood (lymph nodes/spleen) • Immunity function (Life span = years) • T lymphocytes (virus-infected/tumor cells) • B lymphocytes (antibodies) Hemocytoblast Myeloid stem cell Hormones: Interleukins Colony-stimulating factors (+) Lymphoid stem cell Myeloblast Monoblast Lymphoblast Eosinophils Basophils Neutrophils Monocytes Lymphocytes 2) Monocytes (3-7%) • Largest of WBCs • Large U-shaped nuclei • Macrophages (phagocytosis) Chapters 18 - 20: Cardiovascular System Chapters 18 - 20: Cardiovascular System Blood Components - Leukocytes: Leukocyte Disorders: 1) Overproduction of WBCs • Leukemias (cancers of WBCs) Lymphocytic leukemia • Mononucleosis (Epstein-Barr virus - high agranulocyte counts) 2) Underproduction of WBCs (Leukopenia) • Induced by drugs (glucocorticoids / anticancer) Blood Components: 4) Platelets (thrombocytes) • Cytoplasmic fragments (anucleate) • Function in blood clotting • Granules → clotting chemicals • Short-lived (~ 10 days) Chapters 18 - 20: Cardiovascular System Chapters 18 - 20: Cardiovascular System Blood Components - Platelets: Thrombopoietin Platelet Production: Megakaryocyte Megakaryoblast proerythroblast Hemocytoblast Platelets (+) (+) Myeloid stem cell Lymphoid stem cell Myeloblast Monoblast Lymphoblast Eosinophils Basophils Neutrophils Monocytes Lymphocytes (Figure 18.12) Chapters 18 - 20: Cardiovascular System Hemostasis (“Stoppage of blood flow”): • Series of fast, localized reactions to halt blood loss Phases: 1) Vascular Spasms (Vasoconstriction of damaged vessel) • Significantly reduces blood loss • Activated by: (a) Direct injury to smooth muscle (b) Chemical release (c) Nociceptors 2) Formation of Platelet Plug • Temporarily seals vessel break (Positive feedback loop) Chapters 18 - 20: Cardiovascular System Chapters 18 - 20: Cardiovascular System Hemostasis - Platelet Plug Formation: Hemostasis (“Stoppage of blood flow”): Rupture of vessel Phases: 3) Coagulation (Blood clotting) • Blood converted from liquid to gel (3-6 minutes) Collagen exposed Attracts more platelets Step 1: Formation of prothrombin activator (+) Platelets stick to site Vascular spasms • Intrinsic pathway → outside of body (minutes) • Extrinsic pathway → in tissues (seconds) Step 2: Platelets release contents Prothrombin (protein) Adenosine Diphosphate (ADP) Prothrombin activator Thrombin (enzyme) Aspirin Thromboxane A2 Serotonin Step 3: Thrombin Fibrinogen (protein) Fibrin mesh (seals hole) Events in coagulation: Chapters 18 - 20: Cardiovascular System • Produced in liver • Most require vitamin K (Figure 18.13) Chapters 18 - 20: Cardiovascular System Chapters 18 - 20: Cardiovascular System Hemostasis (“Stoppage of blood flow”): Hemostasis (“Stoppage of blood flow”): Clot Retraction and Removal: 1) Platelets draw wound together (Actin/myosin fibers) Factors preventing undesirable clotting: 1) Endothelium → smooth walls 2) Prostacyclin (PGI2) and Heparin (anticoagulants) • Inhibit platelet aggregation (produced by endothelial wall) Thromboembolytic Disorders (Undesirable clot formation): • Thrombus: Clot develops in unbroken vessel • Embolus: Clot floats freely in vessels 2) Platelet-derived Growth Factor (PDGF - Platelets) • Stimulates vessel to rebuild (smooth muscle/fibroblasts) 3) Plasminogen converted to Plasmin • Dissolves clot (fibrinlysis) • Plasmin activated by tPA (tissue plasminogen activator) • Drug treatment = Aspirin, heparin, warfarin Bleeding Disorders (e.g. Hemophilia - coagulation factor deficiency) Chapters 18 - 20: Cardiovascular System Chapters 18 - 20: Cardiovascular System Transfusion and Blood Replacement: Transfusion and Blood Replacement: 1) ABO Blood Groups 2) Rh Blood Groups • Presence / absence of 1 glycoprotein • Presence / absence of 2 glycoproteins (antigens) Type Rh+ Type A Type B Type AB • Blood has pre-formed antibodies opposite blood type • Type O blood = Universal Donor • Type AB blood = Universal Recipient Type Rh- Type O • Antibodies formed after initial contact with antigen Ø Hemolytic disease of the newborn Chapters 18 - 20: Cardiovascular System Transfusion Reactions: 1) Clumping of foreign RBCs: 2) RBCs rupture/are destroyed: Hemoglobin Treatment = Alkaline fluids (dilute/dissolve hemoglobin) Diuretics Kidneys