Abnormalities of prothrombin: a review of the pathophysiology
advertisement

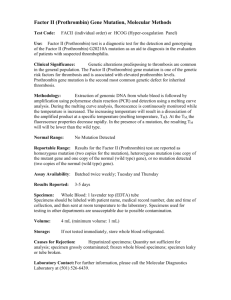
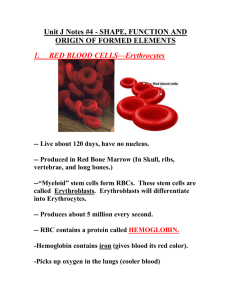
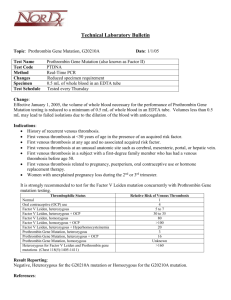
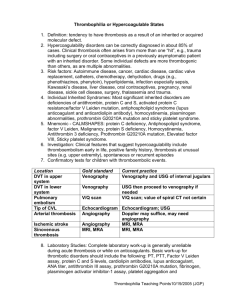
Haemophilia (2008), 14, 1159–1163 DOI: 10.1111/j.1365-2516.2008.01832.x ORIGINAL ARTICLE Abnormalities of prothrombin: a review of the pathophysiology, diagnosis, and treatment S. L. MEEKS and T. C. ABSHIRE Aflac Cancer Center and Blood Disorders Service, ChildrenÕs Healthcare of Atlanta and Emory University, Atlanta, GA, USA Summary. Prothrombin (factor II) deficiency is a rare autosomal recessive coagulation disorder that occurs in approximately 1 in 1–2 million people. Prothrombin is activated to thrombin, which in turn proteolytically cleaves fibrinogen to fibrin and contributes to forming a stable fibrin clot. The haemostatic level of prothrombin is thought to be between 20 and 40%, and the half-life is approximately 3 days. There are more than 40 known mutations in prothrombin. Both hypoprothrombinemia and dysprothrombinemia have been described. Low prothrombin activity typically prolongs both the activated partial thromboplastin time and prothrombin time. Clinical manifestations are predominantly mucosal or surgical- or trauma-associated bleeding, but joint bleeding and intracranial haemorrhages have been reported. No purified prothrombin products are available for replacement therapy. Both fresh frozen plasma and prothrombin complex concentrates contain prothrombin and may be used for treatment. Introduction Materials and methods Prothrombin (factor II) deficiency is a rare coagulation disorder first reported by Quick in 1947 and further described in 1955 and 1962. In 1969, Shapiro reported the first prothrombin abnormality, prothrombin Cardeza, in [1]. We now know that the zymogen prothrombin, when activated to thrombin, is instrumental in converting fibrinogen to fibrin and forming a stable fibrin clot. Homozygous prothrombin deficiency is exceedingly rare, occurring in approximately 1 in 1–2 million people. This review summarizes our current knowledge of the pathophysiology, diagnosis, and treatment of prothrombin deficiency (Fig. 1). Also included is a brief review of the prothrombin 20210 mutation, an abnormality associated with thrombosis rather than bleeding. A systematic review of the PubMed database was undertaken using ÔprothrombinÕ and Ôfactor IIÕ as the initial keywords searched. Review articles and original reports were included. An internet-based search was also performed. Correspondence: Shannon L. Meeks, MD, Aflac Cancer Center and Blood Disorders Service, ChildrenÕs Healthcare of Atlanta/ Emory University, 2015 Uppergate Dr. NE, 4th Floor, Atlanta, GA 30322, USA. Tel.: 404-727-1608; fax: 404-727-4451; e-mail: shannon.meeks@choa.org Accepted after revision 5 July 2008 2008 The Authors Journal compilation 2008 Blackwell Publishing Ltd Keywords: bleeding, coagulation, factor II, haemostasis, prothrombin, thrombophilia Incidence, racial/ethnic predilection Like most autosomal recessive disorders, prothrombin deficiency is reportedly higher in regions and ethnic groups with increased rates of consanguinity [2]. Indeed, many of the patients who have been genotyped are homozygous for the same mutation rather than being compound heterozygotes. In the North American Rare Bleeding Disorder Registry, 62% of the patients with heterozygous or homozygous factor II deficiency were Latinos, 25% Caucasian, and 12% other [3]. This increase in Latino patients was not accounted for by the baseline percentage of Latinos in the overall study population. Pathophysiology Thrombin, which is derived from the Greek word thrombos, meaning Ôto clotÕ, is a serine protease 1159 1160 S. L. MEEKS and T. C. ABSHIRE Prothrombin (factor ll) deficiency Clinical Mucosal bleeding Surgical- or trauma-related bleeding Rare-joint bleeding, ICH Laboratory FII level <10% ↑ aPTT; ↑↑ PT Treatment FFP PCC Fig. 1. Summary of prothrombin deficiency. synthesized in the liver as the inactive zymogen prothrombin. Prothrombin is a 72-kDa, vitamin Kdependent glycoprotein with a plasma concentration of approximately 100 lg mL)1. In the coagulation cascade, factor Xa is made as a product of both the tissue factor and the contact factor pathways. In the presence of calcium, factor Xa, as part of the prothrombinase complex with factor Va and phospholipid, sequentially cleaves two peptide bonds in prothrombin to form thrombin [4]. Thrombin in turn proteolytically cleaves fibrinogen to fibrin and contributes to forming a stable fibrin clot. Thrombin also acts on a variety of other substances in the haemostatic pathway. It promotes platelet activation, activates factor XIII to cross-link the fibrin clot, enhances clot stability by activating thrombin-activatable fibrinolysis inhibitor (TAFI), and up-regulates its own production by activating factors IX, VIII, and V [5–7]. Regulation of thrombinÕs procoagulant activity is necessary to generate enough fibrin to stop bleeding but at the same time prevent excessive clot formation. When bound to thrombomodulin, thrombin down-regulates the coagulation cascade by activating protein C, which in turn inactivates factors VIIIa and Va. In addition, antithrombin, heparin cofactor II, and protease nexin I, all members of the serine protease inhibitor (serpin) superfamily, inhibit the catalytic activity of thrombin, thus limiting clot formation. The activity of these serpins is increased in the presence of glycosaminoglycans such as heparin [6]. Thrombin interacts via proteinase-activated receptors on endothelial cells, leading to tissue plasminogen activator (tPA) release and up-regulation of cell surface molecules, which increase the rate of tPA conversion of plasminogen to plasmin and Haemophilia (2008), 14, 1159–1163 thus enhances thrombolysis [8]. There are additional effects of thrombin on cytokine production and vessel wall biology, including regulation of vessel tone, smooth muscle cell proliferation, angiogenesis, atherogenesis, and vascular development [9–11]. There are two types of inherited prothrombin deficiency. Type I or hypoprothrombinemia occurs when there is a decreased level of normally functioning protein, characterized by a proportional decrease in protein antigen and activity. Type II or dysprothrombinemia occurs when there is a normal antigen level but a decreased level of activity. The haemostatic level of prothrombin is thought to be between 20 and 40%. The half-life is approximately 3 days [2,12]. No reports are in the literature of aprothrombinemia, and complete deficiency is thought to be incompatible with life. In a murine factor II knock-out model, complete prothrombin deficiency resulted in either embryonic or neonatal death [13]. Acquired prothrombin deficiency can occur in vitamin K deficiency, liver disease, and warfarin therapy and in the presence of inhibitors similar to those seen with the lupus anticoagulant. Genetics The prothrombin gene is composed of 20.3 kb and found on chromosome 11p11.2. The deficiency is inherited in an autosomal recessive fashion, either as a single or a combination of defects within the prothrombin gene. Combined deficiencies of the vitamin K-dependent proteins, factors II, VII, IX, and X, can occur when there is an abnormality in the gamma-glutamyl carboxylase gene or the vitamin K epoxide reductase complex [14]. More than 40 different mutations have been identified in patients with prothrombin deficiency [1,15,16]. The Human Gene Mutation Database at the Institute of Medical Genetics in Cardiff contains a large collection of mutations, leading to prothrombin deficiency, including 35 missense/nonsense, 2 splicing, 4 small deletion, and 1 small insertion [17]. The mutations associated with dysprothrombinemia can be divided into two groups: those that produce defects in prothrombin activation and those with defects in the thrombin molecule that is formed. In the first group, prothrombin activation by factor Xa in the prothrombinase complex is diminished, but the thrombin that is generated is fully functional. In the second group, the function of the thrombin produced is abnormal either because of altered interactions with fibrinogen or abnormalities in the catalytic region of thrombin itself [1,18]. 2008 The Authors Journal compilation 2008 Blackwell Publishing Ltd ABNORMALITIES OF PROTHROMBIN Clinical manifestations Patients who are homozygous or compound heterozygous for defects in the prothrombin gene can have moderate to severe bleeding symptoms. Given the small number of cases reported in the literature, the genotype/phenotype correlation is difficult to ascertain, but in general, the lower the levels of protein, the more severe the bleeding. A spectrum of bleeding symptoms have been reported, including easy bruising, mucosal bleeding, surgical bleeding, traumarelated bleeding, haemarthroses, and intracranial haemorrhage [2,3,19]. In the newborn period, patients can present with haematomas, bleeding after circumcision, and umbilical cord bleeding. Heterozygotes are typically asymptomatic; however, bleeding has been reported after tonsillectomy and tooth extraction [1,2]. In the North American Registry, most heterozygotes who had their conditions diagnosed after haemorrhage or abnormal preoperative screening laboratory test results reported bleeding symptoms entirely in the skin or mucous membranes [3]. In terms of prognosis and chronic disease-related complications, the North American Registry reported that 49% of the patients with homozygous prothrombin deficiency had anaemia, 17% had musculoskeletal complications such as target joints or muscle contractures, and 11% had central nervous system complications, including intracranial bleeding and stoke [3]. Chronic arthropathy was also reported in a series of patients from Iran and Italy [15,16]. Diagnosis Patients with prothrombin deficiency typically demonstrate both a prolonged prothrombin time and partial thromboplastin time from a screening laboratory panel often drawn as part of a preoperative evaluation. However, the increase may be minimal and reagent-dependent. If the index of suspicion for prothrombin deficiency is high, a factor II assay (usually a functional or activity level) should be checked. Activity testing is most often performed using a one-stage assay, which uses a tissue thromboplastin as the activating agent and a prothrombinfree substrate. Factor II antigen testing can be performed using an immunoassay. When considering a dysprothrombinemia, it is important to consider that the different prothrombin-activating agents, including tissue thromboplastin and various snake venoms, all demonstrate varying requirements for the presence of factor V, phospholipid, and calcium in the activation of prothrombin to thrombin and 2008 The Authors Journal compilation 2008 Blackwell Publishing Ltd 1161 will manifest different activity levels, depending on where the defect in prothrombin is located [1,18]. In the first months of life, prothrombin deficiency must be differentiated from haemorrhagic disease of the newborn, in which all of the vitamin K-dependent factors are low. Many clinical coagulation laboratories perform the prothrombin time-based assay for factor II activity levels and molecular testing for the prothrombin 20210 mutation. However, molecular testing for types I and II prothrombin deficiency is much more complicated. Genotyping has only been performed on a small number of patients in the rare bleeding disorders registries. Given the small number of known recurring mutations, complete analysis of the prothrombin gene and flanking regions may be necessary if a familial mutation is not already known. This molecular analysis is currently only available in the research setting. Prenatal diagnosis on DNA samples obtained by chronic villous sampling or amniocentesis is feasible if the genotype of the prothrombin abnormality is known [2,20]. Management Treatments currently available Acute bleeding episodes can be treated with fresh frozen plasma (FFP) at 15–20 mL kg)1, which will usually raise the factor level by 25%. As stated previously, this level should be haemostatic for those with homozygous factor II deficiency. For surgical procedures or more severe bleeding episodes, a loading dose of 15–20 mL kg)1 of FFP followed by 3 mL kg)1 every 12–24 h is usually adequate for haemostasis [21]. The volume of FFP needed can be prohibitive for patients with severe fluid restriction. Another option is prothrombin complex concentrates (PCC) at a dose of 20–30 IU kg)1 based on factor IX units. PCC contain factors II, VII, IX, and X and vary in the amounts of each factor from product-to-product and lot-to-lot. For example, Bebulin VH (Baxter, Deerfield, IL, USA) is a PCC with more factor X (factor X > factor II > factor IX) and Profilnine SD (Grifols, Los Angeles, CA, USA) has more factor II (factor II > factor IX > factor X) [22]. However, these products are labelled based on factor IX units, and the exact amount of factor II in these products is unknown. The recommended dosing of 20–30 U kg)1 of factor IX usually raises the factor II to haemostatic levels. However, as other vitamin K-dependent factors are present in PCC, treatment of factor II deficiency with these products Haemophilia (2008), 14, 1159–1163 1162 S. L. MEEKS and T. C. ABSHIRE may potentially lead to supertherapeutic levels of these factors. These high factor levels may increase the risk of thrombosis [16]. No pure factor II concentrates are available [18,23]. Antifibrinolytic therapies such as -aminocaproic acid or tranexamic acid can be administered orally or intravenously to treat mucosal bleeding. Typically antifibrinolytics are not used in conjunction with PCC because of the risk of thrombosis. Hormonal therapy with oestrogens and/or progesterones may help reduce menstrual blood loss in patients with menorrhagia [2]. Successful prophylaxis of a patient with severe prothrombin deficiency with onceweekly home administration of PCC has been reported [24]. both procoagulant and anticoagulant activities. Abnormal levels of prothrombin antigen or activity can lead to excessive bleeding or, in the case of the 20210 mutation, thrombosis. These abnormalities of prothrombin demonstrate the delicate balance of procoagulant and anticoagulant activities in maintaining appropriate haemostasis. Given the small numbers of patients with prothrombin deficiency, it is essential to continue collaborative efforts with international registries to expand our knowledge of this and other rare coagulation disorders. Disclosures The authors stated that they had no interests which might be perceived as posing a conflict or bias. Research Registries for rare bleeding disorders have been established in many countries [3,16]. The International Society of Thrombosis and Hemostasis (ISTH) has a scientific subcommittee working group on rare bleeding disorders and an international database has been established [12,25]. The World Federation of Hemophilia (WFH) also collects basic epidemiological data on patients with bleeding disorders. The international community is working together to standardize data collection to increase the power of these databases. More information about rare bleeding disorders and the registries can be found at the ISTH or WFH web sites: http://www.ISTH.org and http://www.WFH.org. Prothrombin and thrombosis The prothrombin 20210 guanine to adenine mutation has been associated with an increased risk of thrombosis. First described in 1996, this mutation, in the 3¢ untranslated region, results in higher baseline levels of prothrombin [26]. Studies have demonstrated a three- to fivefold increased risk of venous thromboembolus in heterozygotes with an even higher risk in the homozygote [26,27]. This mutation is found in 2–3% of Caucasians and in 4–8% of subjects presenting with a first venous thromboembolus [5,26]. The prevalence of the prothrombin 20210 mutation was also significantly higher in a group of pregnant women with venous thromboemboli than in those without [28,29]. Conclusion Prothrombin is the inactive zymogen that when cleaved forms thrombin, a serine protease that has Haemophilia (2008), 14, 1159–1163 References 1 Girolami A, Scarano L, Saggiorato G, Girolami B, Bertomoro A, Marchiori A. Congenital deficiencies and abnormalities of prothrombin. Blood Coagul Fibrinolysis 1998; 9: 557–69. 2 Mannucci PM, Duga S, Peyvandi F. Recessively inherited coagulation disorders. Blood 2004; 104: 1243–52. 3 Acharya SS, Coughlin A, Dimichele DM. Rare Bleeding Disorder Registry: deficiencies of factors II, V, VII, X, XIII, fibrinogen and dysfibrinogenemias. J Thromb Haemost 2004; 2: 248–56. 4 Bianchini EP, Orcutt SJ, Panizzi P, Bock PE, Krishnaswamy S. Ratcheting of the substrate from the zymogen to proteinase conformations directs the sequential cleavage of prothrombin by prothrombinase. Proc Natl Acad Sci USA 2005; 102: 10099–104. 5 Goodnight S, Hathaway W. Disorders of Hemostasis and Thrombosis – A Clinical Guide, 2nd edn. New York: The McGraw-Hill Companies, 2001. 6 Davie EW, Kulman JD. An overview of the structure and function of thrombin. Semin Thromb Hemost 2006; 32(Suppl 1): 3–15. 7 Sambrano GR, Weiss EJ, Zheng YW, Huang W, Coughlin SR. Role of thrombin signalling in platelets in haemostasis and thrombosis. Nature 2001; 413: 74–8. 8 Peterson EA, Sutherland MR, Nesheim ME, Pryzdial EL. Thrombin induces endothelial cell-surface exposure of the plasminogen receptor annexin 2. J Cell Sci 2003; 116(Pt 12): 2399–408. 9 Coughlin SR. Thrombin signalling and protease-activated receptors. Nature 2000; 407: 258–64. 10 Griffin CT, Srinivasan Y, Zheng YW, Huang W, Coughlin SR. A role for thrombin receptor signaling in endothelial cells during embryonic development. Science 2001; 293: 1666–70. 11 Patterson C, Stouffer GA, Madamanchi N, Runge MS. New tricks for old dogs: nonthrombotic effects of 2008 The Authors Journal compilation 2008 Blackwell Publishing Ltd ABNORMALITIES OF PROTHROMBIN 12 13 14 15 16 17 18 19 20 21 22 23 24 thrombin in vessel wall biology. Circ Res 2001; 88: 987–97. Peyvandi F, Kaufman RJ, Seligsohn U et al. Rare bleeding disorders. Haemophilia 2006; 12(Suppl 3): 137–42. Sun WY, Witte DP, Degen JL et al. Prothrombin deficiency results in embryonic and neonatal lethality in mice. Proc Natl Acad Sci USA 1998; 95: 7597–602. Brenner B. Hereditary deficiency of vitamin K-dependent coagulation factors. Thromb Haemost 2000; 84: 935–6. Akhavan S, Mannucci PM, Lak M et al. Identification and three-dimensional structural analysis of nine novel mutations in patients with prothrombin deficiency. Thromb Haemost 2000; 84: 989–97. Peyvandi F, Duga S, Akhavan S, Mannucci PM. Rare coagulation deficiencies. Haemophilia 2002; 8: 308– 21. Stenson PD, Ball EV, Mort M et al. Human Gene Mutation Database (HGMD): 2003 update. Hum Mutat 2003; 21: 577–81. Bolton-Maggs PH, Perry DJ, Chalmers EA et al. The rare coagulation disorders –review with guidelines for management from the United Kingdom Haemophilia Centre DoctorsÕ Organisation. Haemophilia 2004; 10: 593–628. Strijks E, Poort SR, Renier WO, Gabreels FJ, Bertina RM. Hereditary prothrombin deficiency presenting as intracranial haematoma in infancy. Neuropediatrics 1999; 30: 320–4. Peyvandi F, Jayandharan G, Chandy M et al. Genetic diagnosis of haemophilia and other inherited bleeding disorders. Haemophilia 2006; 12(Suppl 3): 82–9. Di Paola J, Nugent D, Young G. Current therapy for rare factor deficiencies. Haemophilia 2001; 7(Suppl 1): 16–22. http://www.hemophilia.org. http://www.wfh.org. Lobel JS, Majumdar S, Kovats-Bell S. Successful prophylactic treatment for bleeding in a girl with severe 2008 The Authors Journal compilation 2008 Blackwell Publishing Ltd 25 26 27 28 29 1163 hereditary prothrombin deficiency using a prothrombin complex concentrate (Bebulin VH). J Pediatr Hematol Oncol 2004; 26: 480–3. http://www.rbdd.org. Poort SR, Rosendaal FR, Reitsma PH, Bertina RM. A common genetic variation in the 3¢-untranslated region of the prothrombin gene is associated with elevated plasma prothrombin levels and an increase in venous thrombosis. Blood 1996; 88: 3698–703. Brown K, Luddington R, Williamson D, Baker P, Baglin T. Risk of venous thromboembolism associated with a G to A transition at position 20210 in the 3¢-untranslated region of the prothrombin gene. Br J Haematol 1997; 98: 907–9. Gerhardt A, Scharf RE, Beckmann MW et al. Prothrombin and factor V mutations in women with a history of thrombosis during pregnancy and the puerperium. N Engl J Med 2000; 342: 374–80. Samama MM, Rached RA, Horellou MH et al. Pregnancy-associated venous thromboembolism (VTE) in combined heterozygous factor V Leiden (FVL) and prothrombin (FII) 20210 A mutation and in heterozygous FII single gene mutation alone. Br J Haematol 2003; 123: 327–34. Links to organizations http://www.ISTH.org – International Society of Thrombosis and Hemostasis website; http://www.wfh.org – World Federation of Hemophilia website; http://www.hgmd.cf.ac.uk – The Human Gene Mutation Database at the Institute of Medical Genetics at Cardiff website; http://www.rbdd.org – An international database for rare bleeding disorders. Haemophilia (2008), 14, 1159–1163