Module 2 Intravenous Insertion Learning Package
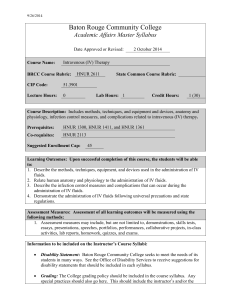
advertisement

Module 2 Peripheral Intravenous Insertion Learning Package August 2007 Revised November 2011 & January 2013 Table of Contents Introduction and Competency 3 Objectives 4 Indications for IV therapy 5 Professional Practice Considerations 6 Standards of Care 7 Anatomy & Physiology 8-11 Peripheral veins appropriate for IV initiation 12-14 Equipment used for peripheral IV initiation 15-20 Special considerations before initiating peripheral I.V. therapy 21-23 Steps to initiating I.V therapy 24-42 Complications of I.V. Insertion and therapy 43-46 References 47-48 Appendix A Competency Skills Check List 49 Appendix B Algorithm for IV initiation 50 Appendix C Post test 51-53 Peripheral Intravenous (I.V.) Initiation 2 Introduction and Competency The purpose of this module is to provide information to the Registered Practical Nurse (RPN) and the Registered Nurse (RN) with regards to peripheral intravenous (I.V.) initiation/insertion. Process of Competency: This is a self-directed learning package. To provide evidence that you have completed this module, you must: 1. Complete Module 2 – Peripheral Intravenous (I.V.) Initiation/Insertion 2. Complete written test (80% pass) to your Clinical Nurse Educator or your Clinical Team Manager within one month of receiving the package. 3. Attend a teaching/didactic session by the Clinical Nurse Educator or a trained I.V. certified nurse. 4. Successfully initiate 3 - 5 intravenous (I.V) and signed off by competent nurses certified to initiate I.Vs using the Competency Skills Check List (See Appendix F). Nurses who were IV certified in other organizations will successful initiate 3 IVs. You will receive a Certificate of Intravenous (I.V) Initiation/Insertion once you have completed all of the above. See Appendix A Please Note: The Clinical Nurse Educator may require of you additional study or practice until 100% competence is acheived. Continuing Competency Competency will be maintained through: 1. On-going practice. 2. Self reflection and review of learning package if ongoing practice or opportunities not available. 3. Two (2) successful intravenous (I.V) initiation per month as per documented patient MRN in the Unit Based IV Competency Binder. 4. Monitoring of I.V. practices through unit-based I.V audits. It is your professional obligation to determine if you have the knowledge, skill and ability to continue practicing safely. Please contact your Clinical Nurse Educator or Clinical Team Manager if you have any learning needs. Additional copies of this package may been obtained from the Educator. Peripheral Intravenous (I.V.) Initiation 3 Objectives By the end of this self-directed learning module, the nurse will be able to: 1. 2. 3. 4. 5. 6. Describe the indications for intravenous therapy Describe standards of care and maintenance of peripheral intravenous (PIV) therapy. Describe basic anatomy of veins and skin. Identify complications of intravenous therapy. Demonstrate how to succesfully initiate IV therapy. Describe components of documentation regarding IV initation. Peripheral Intravenous (I.V.) Initiation 4 Indications for Intravenous Therapy Indications for initiating intravenous therapy include: a) b) c) d) e) f) maintenance of fluid & electrolyte balance blood & blood products administration medication administration parenteral nutrition (short term) to provide access for diagnostic tests and/or procedures resuscitation Peripheral Intravenous (I.V.) Initiation 5 Professional Practice Considerations Nurses have a professional responsibility to ensure care and maintenance of peripheral intravenous (PIV) therapy in their clinical setting. These include: 1. Evidence-based theoretical and practical knowledge to enable safe practice 2. Maintaining practical competency and practice in accordance with NYGH policy and procedures 3. Patients receive education of signs and symptoms and potential complications related to intravenous therapy 4. Maintaining ongoing documentation of care and maintenance, initiation and discontinuation related to intravenous therapy. Adapted from http://www.cancernursing.org Peripheral Intravenous (I.V.) Initiation 6 Standards of Care Both RNs and RPNs are responsible for care & maintenance of the IV site. In the event of complications, it is your responsibility to assess, consult when necessary, take action and document. You are required to be knowledgeable in the care of patients with peripheral intravenous sites and therapy. As per the NYGH Policy and Procedures – Intravascular Care and Maintenance II-240 & Peripheral IV Initiation Competency II- 245 and as per the Medical Directive – http://www.nygh.on.ca/nygh_test/XII_138_Initiate___Discontinue_Saline_Lock.pdf According to the Journal of Infusion Nursing (2011), The RNAO Best Practice Guidelines (2008), the Center for Disease Control (2011), and NYGH Policy and Procedures, it is your responsibility to perform the following: Hand Washing • • Perform hand hygiene in accordance to NYGH Infection Prevention and Control Policy and Procedures. Wear personal protective equipment. Assess patient risk factors and use personal protective equipment when needed (to either protect the patient, as in immunosuppressed patients or to protect you, in case of contact with body fluids). Peripheral Intravenous (I.V.) Initiation 7 Anatomy and Physiology Skin The skin consists of two main layers, the epidermis and the dermis which lies over the superficial fascia. The epidermis is the layer that acts as a defense mechanism. Its thickness varies with age and exposure to elements such as wind and sun. The dermis, a much thicker layer, is located directly below the epidermis. The dermis consists of blood vessels, hair follicles, sweat glands, sebaceous glands, small muscles, and nerves. As a result, it reacts quickly to painful stimuli, temperature changes, and pressure sensation. (http://health.yahoo.com/media/mayoclinic/images/image_popup/skin_type.jpg) Peripheral Intravenous (I.V.) Initiation 8 Sensory Receptors Phillips (2005) describes five types of sensory receptors, four of which affects parental therapy. Sensory receptors related to parental therapy includes a. Mechanoreceptors: which process the skin tactile sensation and deep tissue sensation. b. Thermoreceptors: which process cold, warmth and pain (application of heat and cold) c. Noiceptors: which process pain (puncture of the vein fro insertion of the cannula) d. Chemoreceptors: which process osmotic changes in the blood and decrease arterial pressure (decrease circulating blood volume) (http://fig.cox.miami.edu/~cmallery/150/neuro/c7.49.3.skin.jpg) Peripheral Intravenous (I.V.) Initiation 9 Characteristics of Veins and Artery Tissue Layers Tunica Intima The Inner Layer Tunica Media The Middle Layer Vein Characteristics Elastic endothelial lining Smooth surface allows cells and platelets to flow through the vessels • Damage to this layer encourages thrombus formation Artery Characteristics • Elastic endothelial lining • Smooth surface allows cells and platelets to flow through the vessels • Damage to this layer encourages thrombus formation • Muscular and elastic tissues Contains constrictors and vasodilators nerve fibers Not as strong and stiff Allows vein to collapse or distend with pressure changes Areolar connective tissues surrounds and supports the vessels • Veins have valves to permit only unidirectional blood flow towards the heart. Usually found superficial Blood will appear dark red Blood will flow from cannula Does NOT have a palpable pulse • • • • • • Tunica Adventitia The Outer Layer • Valves • Other differences • • • • • • • • • • • • Muscular and elastic tissues Contains constrictors and vasodilators nerve fibers Strong and stiff Arteries DO NOT collapse or distend with pressure changes Areolar connective tissues surrounds and supports the vesselsBut thicker in arteries due to greater pressure No Valves Usually found deep and surrounded by muscles Blood will appear bright red Blood will pulsate from the IV cannula Has a palpable pulse Peripheral Intravenous (I.V.) Initiation 10 (http://www.sci.sdsu.edu/class/bio590/pictures/lect5/artery-vein.jpeg) Peripheral Intravenous (I.V.) Initiation 11 Peripheral Veins Appropriate For IV Initiation Peripheral Intravenous (I.V.) Initiation 12 Veins of the Arms Vein and Location Digital Lateral and dorsal portions of the fingers Metacarpal and Dorsal Dorsal surface of the hand Cephalic Radial portion of the lower arm along the radial bone of the forearm from the wrist to the Anticubital fossa • • • • • Good site to begin IV therapy Easily visualized Avoid if infusing antibiotics, potassium chloride or chemotherapeutic agents • • Large vein, easy to access First use most distal section and work upward for long term therapy Useful for infusing blood and chemically irritating medications Puncture at the wrist may cause mechanical irritation from joint movement • • Accessory Cephalic Branches off the cephalic along the radial bone • • • Upper Cephalic Radial aspect of the upper arm above the elbow Basilic Ulnar aspect of the lower arm and runs up the ulnar bone Considerations Use a padded tongue blade to splint the finger Use solutions that are Isotonic and with out additives, to decrease the risk of infiltration Medium to large size, easy to stabilize and access Difficult to palpate in persons with large amounts of adipose tissue Valves at the cephalic junction may prohibit cannula advancement (use a shorter cannula, 1inch) • • Difficult to visualize Great site for confused patients, who tend to pull at their I.V. line • • Difficult area to access Large vein, easily palpated, but moves easily, therefore needs to be stabilized Often available when other sites have been exhausted • Peripheral Intravenous (I.V.) Initiation 13 Median Antebrachial Extends up ulnar side of anterior forearm from the median Anticubital veins • • Anticubital Fossa In the bend of the elbow • • • • • Vein is readily accessible Area has many nerve endings and should be avoided Infiltration occurs easily Should be reserved for blood draws for laboratory analysis Uncomfortable placement site, due to unnatural positioning of the arm Difficult to splint with an arm board If used in an emergent situation (e.g. dehydration, blood loss, arrest) change site within 24 hours Peripheral Intravenous (I.V.) Initiation 14 Equipment Used for I.V. Initiation I.V. Catheters: There are various companies and types of peripheral I.V. catheters used. A catheter is another term for tube that can be inserted into the body for the delivery or removal of fluid. When choosing the correct size catheter, for your patient, the following should be considered: age, level of activity, venous status, type of solution, type of medications being administered, the length of therapy, and the procedure/surgery to be performed when deciding. In the medicine and surgical units, the BD NEXIVA CLOSED CATHETER SYSTEM – SINGLE PORT is used. For more information, read pages 17-20. Catheter Lengths: ¾ inch-1 ¼ inch • 24 gauge • 22 -20 gauge • • • • • 18 gauge • • • • • • Considerations Use the shortest length and the smallest gauge that allows for proper administration of prescribed therapy Use in infants, children, older adults and adults with extremely small or fragile veins Difficult to insert in tough skin 22 gauge: For fragile veins in elderly persons if unable to place a 20 gauge catheter 20 gauze: Medical or surgical patient requiring medication and fluid replacement Blood may be given to patients with 22 gauge catheter on a pump (i.e. IVAC pump) 20 gauge: preferred for cardiac patients and for blood administration Immediate post-op surgical patients Obstetrical patients Blood and blood product administration TPN and viscous solutions CT Scan procedures Patients requiring resuscitation Peripheral Intravenous (I.V.) Initiation 15 Gloves: Gloves are the recommended standard precaution whenever exposure to blood and bodily is likely. Latex and vinyl gloves protect wearers from contact with blood and body fluids. See Policy IV-a-85 for latex awareness Skin Cleansing Solution: A tincture of 2% chlorhexidine gluconate and 70% isopropyl alcohol significantly reduces the chance of nosocomial infection. Recommended by the CDC (2011) guidelines. Scrub insertion site using side to side, up and down friction. Let it dry for 30 seconds and apply the dressing. Dressings & Site Securing: A clear transparent dressing is the standard (i.e. Tegaderm). When a patient is diaphoretic, sterile skin prep is available and can be used after catheter insertion to secure the dressing to the skin. Tapes: Tape must NOT to be used over the insertion site as it will hinder the ability to assess and visualize the site. Use tape to anchor the tubing and hub. Paper tape is best used on patients that are allergic to plastic tape and for patients with thin skin that are prone to skin tares. Tourniquet: A disposable tourniquet must be used and discarded after each patient to decrease the transfer of infection to other patients (INS, 2000) Needleless Connector: Hospira’s Microclave Clear Needleless Connector(“cap”) must be primed and attached to the end of the Nexiva single port catheter. Then flush using the stop/start and positive pressure technique before clamping the catheter. IV Tubing: New tubing must be used after each IV initiation. See page 21 for IV tubing changes. Sharp Disposal: See NYGH Policy IV-a-90 Peripheral Intravenous (I.V.) Initiation 16 Peripheral Intravenous (I.V.) Initiation 17 Peripheral Intravenous (I.V.) Initiation 18 Peripheral Intravenous (I.V.) Initiation 19 Peripheral Intravenous (I.V.) Initiation 20 Special Considerations Site selection a. The site selection should be readily visible and roller bandages should never be used around the catheter site (INS, 2000) b. Select an area without flexion: movements may cause irritation, resulting in phlebitis and or infiltration. An area of flexion may interfere with the flow rate and it may cause irritation and pain c. Avoid areas of skin irritation, this may increase the risk of infection and embolus d. Avoid the lower extremities, especially in patients who are diabetic and/or have peripheral vascular disease (PVD). Initiating an IV will increase the risk of ulcer formation related to poor healing Vein selection a. Vein selection shall include assessment of the patient’s condition, age and diagnosis, the condition of the vein, the size and location and the duration of therapy. The vein should be able to accommodate the gauge and length of the cannula required by the prescribed therapy (INS, 2000) b. A suitable vein should feel relatively smooth, pliable with valves well spaced. c. Start with distal veins and work proximally. d. Veins that feels bumpy, like running your fingers over a cat’s tail, are usually thrombosed or extremely valvular (Phillips, 2005) Geriatric Considerations a. Due to the decrease in subcutaneous tissue the veins loss stability and roll away from needle. To stabilize the vein, apply traction to the skin below the projected insertion point b. Use the smallest gauge possible (22- 24 gauge for fluid and medication administration, less traumatic) c. Avoid the back of the hands – it interferes with independence d. Sclerotic and fragile veins are common in the elderly population, approach venipuncture gently and evaluate the need for a tourniquet (Fabian, 1995) Peripheral Intravenous (I.V.) Initiation 21 Overweight Considerations: a. If you are unable to palpate or see the vein, create a visual image of the venous anatomy and select a longer catheter b. According to Weinstein (2001), double or triple tourniquets are recommended. Pediatric Considerations (see Pediatric IV SDLM) a. Infants do no have accessible sites; this is related to an increased body fat. Hence, veins in the hands, feet and antecubital region may be the only accessible sites. b. Peripheral routes for pediatric IV include scalp vein, veins in the dorsum of the hand, forearm and foot c. The major superficial scalp veins (frontal best access), perauricular, supraorbital and occipital can be used fro children up to 18months of age. Only RNs with added competencies may initiate scalp veins IV d. The major superficial veins of the scalp are easily visualized, readily dilates because it has no valves; hands are kept free e. The dorsum of the hand and forearm, f. A flashlight or transilluminator device placed beneath the extremity helps to illuminates tissue surrounding the vein; the veins are better outlines for better visualization (Frey, 2001) Psychological Considerations: a. Anxiety, stress and fear will increase stress response and causes vasoconstriction and may inhibit cannulation Physiological Considerations: a. Thermoregulation: Veins distends when warm and constricts when cold b. Hypovolemic: In severe shock, veins will collapse c. Previous trauma: Repeated cannulation or drug therapy can result in damage veins Chemotherapy Considerations: • Veins suitable for IV administration of chemotherapeutic agents must be smooth and non-sclerotic. When selecting veins for chemotherapeutic, it is recommended to use the distal veins of the hands and arm first. However, large veins of the forearm are preferable. Veins commonly used are including Peripheral Intravenous (I.V.) Initiation 22 the basilica, cephalic and metacarpal veins. Do not use the antecubital fossa or the wrist. Peripheral Intravenous (I.V.) Initiation 23 Steps to IV initiation - Adapted from (Philips, 2005) Precannulation 1. Check the physician’s orders: a. validate the order for IV insertion or document the medical directive used b. determine the need for venous access based on nursing judgment 2. Hand hygiene a. Scrub hands vigorously with an antimicrobial agents for 15- 20 seconds before and after all clinical procedures 3. Equipment preparation: a. Prepare and prime IV tubing using aseptic technique. b. Gather equipments and select vascular access device base on needs 4. Patient assessment and psychological preparation: a. Provide privacy b. Explain the procedure to minimize anxiety c. Instruct the patient regarding the purpose, the procedure, mobility limitation and potential complications d. Assess the psychological preparedness for the IV procedure such as fear of blood or needles and pain. 5. Site selection and veins dilation: a. Based on age, diagnosis, vein conditions types and duration of therapy b. The following list provides suggested ways to dilate the vein i. Gravity: position the extremities below the heart ii. Fist clenching: instruct the patients to open and close the fist squeezing a rubber ball or rolled washcloth works well iii. Tapping: using the thumb and the second finger; flick the vein. This enhance the release of histamines beneath the skin and causes dilation. iv. Warm compress: Apply warm towel to the extremities for 10- 15 minutes will result in vasodilatation and enhance cannulation (Walling and Lenhardt, 2003) v. Tourniquet: Apply the tourniquet 6 to 8 inches (10 – 15cm) above the intended insertion site. If the blood pressure is within normal Peripheral Intravenous (I.V.) Initiation 24 l step) method For direct (one Indirect entry (two –steps method) i limits, place the tourniquet lower with hypotensive patients and higher with hypertensive patients. Do not leave the tourniquet in place for longer than 2-3 minutes. Patients with fragile veins do not require tourniquets Cannulation 6. Needle selection : (See page 15 & 20) 7. Gloves: Recommended routine standard of practice. 8. Site preparation: a. Clip excessive hair only if necessary, shaving is not recommended because of the potential for microabrasion. Using a tincture of 2% chlorhexidine gluconate and 70% isopropyl alcohol significantly reduces the chance of nosocomial infection. Prepare the site using vigorous circular motion, working from the center outwards to a diameter 2 – 3 inches for 20 seconds. The solution should be allowed to air dry 9. Cannulation: Direct vs. Indirect Direct: Insert the catheter directly over the vein at a 15 to 25° angle; penetrating all layers of the vein with one motion. Not suitable for small veins due to hematoma potential. Indirect: Cannula is inserted “through skin below the point where vein is visible but above the vein. This approach depresses the vein, obscuring its position. The catheter is adjacent to the vein, but has not penetrated the vessel wall. Gently locate the vein, decrease the catheter angle and enter the vessel.” NOTE: In the medicine and surgical units, BD NEXIVA CLOSED CATHETER SYSTEM – SINGLE PORT is used. For more information, read pages 29 - 41. Peripheral Intravenous (I.V.) Initiation 25 a) Wash hands. a) Wash hands & stabilize vein b) pull the skin below the puncture b) Insert the cannula at a 15 to 25° site to stabilize the skin and angle to the skin along the vein; prevent the rolling of the vein gently insert the cannula distal to c) Insert the needle of choice bevel up at a 15 - 25° angle, depending on the vein location the point at which the needle will enter the vein c) After the bevel enters the vein and catheter, while applying and blood flashback occurs, traction on the vein to keep skin lower the angle of the catheter taut. For superficial veins, a and stylet (needle) as one unit lower angle of 5° is and advance into the vein. recommended. (CINA, 1999) a. Insert the catheter by d) After the catheter tip and bevel are in the vein, advance the direct or indirect method catheter forward of the stylet and with a steady motion. into the vein. e) After the vein is entered, cautiously advance the cannula into the vein lumen. Hold the catheter hub with your thumb and middle finger and use the index finger to advance the catheter f) While the stylet is still partially inside the catheter, release the tourniquet g) Remove the stylet h) Connect the adapter to the administration set to the hub of the catheter Peripheral Intravenous (I.V.) Initiation 26 10. Catheter stabilization and dressing management a. The catheter should be stabilized in a manner that does not interfere with visualization and evaluation of the site. Stabilization reduces the risk of complications related to IV therapy. b. Cover the insertion site and the catheter hub with a transparent dressing. Secure the lines to prevent excessive movements Post Cannulation 11. Attach primed needleless connector to end of single port of catheter. Then flush using the stop/start and positive pressure technique before clamping the catheter (See page 42). 12. Labeling a. IV set up must be labeled in three areas: the insertion site, the tubing and the solution container/ bag b. The venipuncture site must be labeled on the side of the transparent dressing or across the hub with the date, time, size of catheter and nurse’s initials. 13. Equipment disposal a. Sharps must be placed in the sharps container 14. Patient education a. Inform the patient of any limitation on movement or mobility b. Instruct the patient to call for assistance if the venipuncture site becomes tender or sore or if redness or swelling develops c. Advise the patient that the site will be checked by the nurse 15. Rate calculation a. Accurately calculate the rate, the drop per minute should be calculated based on the drop factor. (See Self directed learning Module on Care and Maintenance of intravascular therapy ) 16. Documentation a. Monitor the patient’s response to the therapy, document procedure performed, how the patient tolerated the venipuncture, and what instructions were given. b. Document the size and length of the catheter and difficulties during the procedure, and site and vein. Including the solution and rate/ saline lock. Peripheral Intravenous (I.V.) Initiation 27 BD Nexiva Points to Practice – Initiation Peripheral Intravenous (I.V.) Initiation 28 BD NEXIVA CLOSED CATHETER SYSTEM – SINGLE PORT Peripheral Intravenous (I.V.) Initiation 29 Peripheral Intravenous (I.V.) Initiation 30 Peripheral Intravenous (I.V.) Initiation 31 Peripheral Intravenous (I.V.) Initiation 32 Peripheral Intravenous (I.V.) Initiation 33 Peripheral Intravenous (I.V.) Initiation 34 Peripheral Intravenous (I.V.) Initiation 35 Peripheral Intravenous (I.V.) Initiation 36 Peripheral Intravenous (I.V.) Initiation 37 Peripheral Intravenous (I.V.) Initiation 38 Peripheral Intravenous (I.V.) Initiation 39 Peripheral Intravenous (I.V.) Initiation 40 Peripheral Intravenous (I.V.) Initiation 41 BD Nexiva’s IV Closed System Catheter-Single Port with Hospira’s Microclave Clear Needleless Connector and/or Bifurcated Extension Set Hospira’s Microclave Clear Needleless Connector(“cap”) This new needleless connector requires no change in practice with stop/start and positive pressure technique. Practice change related to starting an IV: 1. Retrieve a single port Nexiva IV Closed Catheter system and a Hospira Microclave Needleless Connector. Note: If you need to use 2 ports- bring Hospira’s bifurcated extension set(Important- the needleless connectors on the bifurcated extension set are bonded to the tubing-see picture below). 2. Wash hands and apply gloves(follow Infection Prevention and Control standards). 3. Scrub the Microclave needleless connector hub for 30 seconds using 70% alcohol swab and attach prefilled 0.9% saline syringe. Prime the Microclave needleless connector with 0.05mls 0.9%normal saline. 4. Insert the single port Nexiva IV Closed Catheter System(follow guidelines for IV insertion) 5. Add the primed Microclave needleless connector to the end of the Nexiva single port catheter. Flush using the stop/start and positive pressure techniques and clamp the catheter. 6. If 2 ports are required, scrub the Microclave needleless connector hubs on the bifurcated extension set for 30 seconds using 70% alcohol swab and attach prefilled 0.9% saline syringe. Prime the bifurcated extension set with 1.4mLs 0.9% normal saline. 7. Scrub the Microclave needleless connector (already attached to the IV catheter) and attach the bifurcated extension set. Flush using the stop/start and positive pressure techniques and clamp the catheter. Peripheral Intravenous (I.V.) Initiation 42 Complications of IV Insertion and Therapy An important part of IV therapy is the ongoing evaluation. There can be several complications that may occur and require immediate recognition and nursing intervention. Complication Definition Causes Infiltration *Leaking of nonvesicant solution/medication into the surrounding tissue *Trauma to vein with insertion *Cannula is positioned outside vein *Large volume infiltrate Extravasation *Leaking of vesicant solution/medication into the surrounding tissue (vesicant solution can cause blister formation and possible tissue necrosis) *Trauma to vein with insertion *Cannula is positioned outside vein *Large volume infiltrate Signs and Symptoms *Swelling and pain to the area *Alerted flow rate *Blanching and coolness of the skin area *Leaking at the site *Swelling and pain to the area *Alerted flow rate *Blanching and coolness of the skin area *Leaking at the site *Sloughing off of tissue Nursing Interventions *Stop infusion *Remove IV cannula *Elevate limb and apply warm compresses *Restart IV in unaffected area *Document *Stop Infusion *Contact MD for orders *Change tubing at hub *Infuse antidote as per MD order *Remove IV cannula *Cover with dry sterile dressing *Document (http://pharmlabs.unc.edu/parenterals/routes/intravenous_sites.jpg) Peripheral Intravenous (I.V.) Initiation 43 Complication Definition Causes Arterial Puncture *Accidental puncture of artery Phlebitis *Inflammation of the Intima; inner lining of the vein Thrombophlebitis *Inflammation of vessel due to formation of thrombus *Inappropriate site selection *Inability to distinguish between vein/artery *Mechanical: - Inflammation causes by trauma or IV catheter, manipulation of the catheter *Chemical: -vein becomes irritated by medications or solution *Bacterial: -caused by breakage of skin barrier pathogens have access *See causes for phlebitis Signs and Symptoms *Blood pulsing from site *Inability to thread IV due to high pressure Nursing Interventions *Remove IV cannula *Apply direct pressure to site *Document *Pain at the site *Area is warm to touch *Inflammation of the vein, erythema, edema *Bacterial phlebitis may have purulent discharge, and fever *Stop infusion *Remove IV cannula *Clean area with antimicrobial agent and apply dry dressing *Apply warm/cold compress to area *Document *Contact MD if Bacterial phlebitis is suspected *Pain and inflammation at the site *Hard cord like vein *Altered infusion flow rate *Limb may be cool and discolored *Stop infusion *Remove IV cannula *Clean area with antimicrobial agent and apply dry dressing *Apply COLD compress to area to decrease flow *Followed by WARM Compress and elevate arm *Instruct client against rubbing area – may cause EMBOLI Peripheral Intravenous (I.V.) Initiation 44 (http://www.postgradmed.com/issues/2004/11_04/slaughter.htm) Complication Definition Causes Embolism *A thrombus is formed and becomes dislodged *Emboli can be dislodged due -to forced flushing with syringe -manipulation of cannula Occlusion *An emboli formed within or at the tip of the cannula *Prolonged interruption of the flow of IV fluids Signs and Symptoms *Pain in arm *Hypotension, cyanosis, tachycardia weak pulse *Rise in venous pressure *Decreased GCS *Unable to resume flow of IV fluids *Blood may back up into tubing Nursing Interventions *Apply tourniquet above IV site *Check vital signs *Place client in Trendelenberg position *Have another staff member call the MD *Do not leave client *Do not flush IV (may cause emboli) *Remove IV cannula *Document Peripheral Intravenous (I.V.) Initiation 45 Complication Definition Causes Pain *As defined by the client *Insertion site may be tender *Infusion may be too rapid *Infiltrate may be too concentrated Speed Shock *A systemic reaction that occurs due to rapid introduction of a medication *Large volume infused too fast which permits toxic levels of medication in the plasma Fluid Overload *Venous pressure is increased due to circulatory overload *Large volume infused to fast Signs and Symptoms *Client states that they are in pain and indicate IV site as the source *Immediate complaint of headache *May complain of face flushing, chest pain *Rare cases – loss of consciousness, anaphylactic shock or cardiac arrest *Hypertension *Distended jugular veins *SOB *Crackles to lung fields *Possible Pulmonary Edema Nursing Interventions *If pain is extreme remove cannula *dilute solution if possible *reposition tubing *Slow infusion rate *Stop infusion *Put client in Trendelenberg *Provide O2 by non-rebreather mask *Notify MD *Slow rate to TKVO *Position client in Semi-fowlers if possible *Notify MD *Document Peripheral Intravenous (I.V.) Initiation 46 References BD Nexiva Closed IV Catheter System. College of Nurses of Ontario (2005). The Standards of Practice for Nurses. Retrieved March 20, 2006 from www.cno.org Center for Disease Control (2011). Guidelines for the Prevention of Intravascular Catheter-Related Infections. Center for Disease Control (2002). Guidelines for the Prevention of Intravascular Catheter- Related Infections. Morbidity and Mortality Weekly Report. 51 (10) Fabian, B. (1998). Basic I.V. skills: Adult and Pediatric. National Academy Presentation: November 1998, Pheonix, AZ Infusion Nurses Society, 2011. Infusion Nursing Standards of Practice. Journal of Infusion Nursing 34(1S). Hibbard, J.S. Mulberry, G., & Brady, A. (2002). A clinical study comparing the Skin antisepsis and safety of chloraprep, 70 isopropyl alcohol and aqueous chlorhexidine. Journal of Infusion Nursing, 25 (4) 244- 249 Infusion Nursing Society (2000). Revised intravenous standards of practice. Journal of Intravenous Nursing, 21 (65) North York General Nospital (2005) Policy and Procedure on Infection control North York General Hospital (2005). Policy and Procedure on Latex Gloves North York General Hospital (2006?) Self Directed Learning Module on Chemotherapy and Biotherapy Philips, D (2005). The Manual of I.V therapeutic. 4th Ed. F.A Davis Philadelphia Peripheral Intravenous (I.V.) Initiation 47 Potter, & Perry (2004). Clinical Nursing Skills & Technique. 5th Ed. Mosby Register Nurses Association of Ontario (2006). Best Practice Guideline: Assessment and Selection of Vascular access device. Retrieved March 20, 2006 from www.rnao.org Weinstein, S. (2004) .Plumer’s Intravenous Therapy. 7th ED. Lippincott. Philadelphia Walling, A & Lenhardt, R. (2003). Local warming and insertion of peripheral Venous cannulas: Single blinded prospective randomized controlled trial and a single blinded randomized crossover trail. American Family Physician 67 (2), 401 Vanek,V. (2002). the In and Outs of venous access: Part 1. Nutrition in Clinical Practice 17(2) 85- 98 Peripheral Intravenous (I.V.) Initiation 48 Appendix A Competency Skills Check List Name: _________________ Unit ____________________ S= Satisfactory; U = Unsatisfactory The RN/RPN must successfully initiate 3- 5 IVs to be competent Number of successful starts Criteria 1 2 3 4 5 6 7 Comments 1. Check the physician’s order 2. Collection of all the necessary equipment 3. Hand Hygiene 4. Explain the procedure to the patient 5. Proper positioning of the patient 6. Applies Tourniquet 3-4” above the site of insertion 7. Proper cleansing of the site based on aseptic technique 8. Maintain standard precaution (gloves) 9. Check proper functioning of the catheter 10. Anchor patient’s limb/ vein appropriately 11. Insert the needle 12. Observe for flash back, withdrawal of needle, advance the catheter 13. Proper stabilization of the site with tape and transparent dressing 14. Proper adjustment of Flow rate 15. Proper labeling of IV site/ Tubing 16. Disposal of sharps 17. Hand hygiene 18. Appropriate documentation on Powerchart 19. Initials of Trainer Most Responsible Educator______________________ Date:_______________ Peripheral Intravenous (I.V.) Initiation 49 Appendix B ALGORITHM for IV Initiation IV INSERTION ORDERED ↓ RN/RPN (knowledge, skills and resources available to manage outcome) ↓ RN/RPN assesses Patient & Purpose for IV ↓ No Contraindications ↓ Determine the right gauge & site selection ↓ INSERT IV Once, if unsuccessful ↓ Utilize unit resources or champions and attempt again ↓ Still unsuccessful ↓ Page Vascular Access Nurse (Write Request in Book) ↓ Ensure IV tubing is primed and labeled Peripheral Intravenous (I.V.) Initiation 50 Appendix C Post Test Name: ________________________ Unit:_______ Date:_______________ 1. Which of the following types of patients should have a minimum 18-gauge intravenous initiated as per hospital guidelines a) Multiple trauma patients, L & D patients pre- operative patients only b) Pediatric patients, dehydrate patients and chemotherapy patients c) Patients receiving transfusions of blood and blood products, multiple trauma patients, and all L & D and preoperative patients 2. Thrombophlebitis is: a) a painful inflamed area along the length of the vein or surrounding area around the site of the catheter b) Swelling noted distally to the catheter insertion site c) A large area of discoloration proximal to hand d) Pain, numbness, or a decrease sensation of the extremities 3. Intravenous cannulation should progress from the: a) Dorsal surface of the hand towards the antecubital space b) Lateral surface of the hand towards the antecubital space c) Antecubital space towards the finger d) None of the above 4. Veins commonly used for peripheral IV therapy are: a) The veins at the point of flexion b) Veins in the antecubital fossa c) Basilic, Cephalic and Metacarpals d) Veins on the inner aspect of the forearm 5. A peripheral saline lock must be flushed: a) after medication b) Between medication c) Before giving a medication d) All of the above 6. A patient complains of pain and has redness with swelling near the site of the I.V. The action the nurse should take is to: a) Rub or massage the reddened area b) Change the IV tubing c) Stop the infusion and resite the cannula d) Splint the site to make it more comfortable for the patient Peripheral Intravenous (I.V.) Initiation 51 Post Test Please Answer True (T) or False (F) 1) If there is blood “flash back” during intravenous cannulation, advance the stylet back into the catheter and adjust the positioning of the needle to locate the vein 2) Under the new RHPA guidelines, intravenous initiation is considered an added nursing skill. 3) When an IV is blocked, the nurse should milk the tubing a few times to unblock it. 4) You should turn the patient on the left to trendelenberg position if you suspect the existence of an air embolism. 5) If there is a lack of blood flash back during intravenous cannulation, wiggle the needle around to center the bevel in the vein 6) The healthcare provider must follow the hospital policies and procedures regarding IV therapy before and after initiating an IV. 7) Saline locks and IV sites are changed every 4 days. Match column A to definitions found in Column B 1. Arteries a) Free floating 2. Veins b) Usually superficial and palpable but may be deep 3. Infection c) sensitivity to IV catheter 4. Allergic Reaction d) No valves present 5. Pulmonary Embolism e) Redness, tenderness, swelling at IV site Symptom Identification Place an (I) infiltration and/ or (P) phlebitis beside the symptom most commonly associated with infiltration or phlebitis 1. Blanching _____________ 2. Cold skin _____________ 3. Hot skin _____________ 4. Palpable cord _____________ 5. Pain _____________ 6. Redness ______________ 7. Sensation of heaviness _____________ 8. Swelling _____________ 9. Tenderness _____________ 10. Burning Sensation _____________ Peripheral Intravenous (I.V.) Initiation 52 Short Answer 1. Identify FOUR purposes of IV infusion a) ____________________________ b) ____________________________ c) ____________________________ d) _____________________________ 2. The first line of defense against nosocomial infection is _______________ 3. List 3 characteristic of Veins and arteries Veins a) _________________ b) _________________ c) _________________ Arteries ________________ ________________ _________________ Post Test score: __________ PLEASE RETURN TO YOUR CLINICAL NURSE EDUCATOR – THANK YOU Peripheral Intravenous (I.V.) Initiation 53