Food Services and Nutrition Management Year Two Semester Two

Food Services and Nutrition Management
Year Two Semester Two
Study Guide
2013-2014
© 2013 Canadian Healthcare Association. All rights reserved.
No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise without expressed permission of the publisher.
Canadian Healthcare Association
17 York Street, Suite 100
Ottawa, Ontario
K1N 9J6 www.cha.ca
© 2013 Canadian Healthcare Association. All rights reserved. 2
Food Services and Nutrition Management
Year Two Semester Two
2013-2014
Table of Contents
Unit 7: Nutrition Therapy II- Nutritional Management of Gastrointenstinal Disorders, Surgery and
Unit 8: Nutrition Therapy III- Nutritional Management of Heart Disease, Renal and Gallbladder
© 2013 Canadian Healthcare Association. All rights reserved. 3
FSNM Yr 2 Se 2 Introduction
Introduction
The Food Service and Nutrition Management (FSNM) program is fully accredited by the
Canadian Society of Nutrition Management (CSNM) . The two-year program is designed for individuals currently working in food services in health care or other institutional settings who wish to pursue a career in food service management.
A food service nutrition manager is involved with the day-to-day operation of the food and nutrition/dietary department and is an active member of the management team. He/she provides the much needed link between administrative and food service personnel. The role of this manager is to incorporate education and experience in co-ordinating and supervising operations of the food service department and to provide quality, economical meal service. The emphasis on cost control, quality assurance, accreditation, menu planning, patient counseling and safe food handling makes for a stimulating and challenging program.
The first year of study focuses on food management, while the second year explores nutrition and diet therapy and focuses on the clinical aspects of the food service and nutrition manager’s role.
Learning Objectives
Upon completion of the Food Services and Nutrition Management Program, will be able to:
1. Understand the basic physiological processes of digestion,
2. Identify the food sources of the key nutrients and their functions in the body,
3. Understand the relationship between nutrition and maintenance of good health,
4. Understand the principles involved in menu planning,
5. Understand the rationale for therapeutic nutrition modifications, and
6. Follow established procedures for writing modified diets for various disorders of the human body.
Program Components
The Food Services and Nutrition Management Year Two Semester Two program includes:
Four structured study units, with written assignments to be completed between
September and December
30 Supervisory Hours per months
75 hours Practical Nutrition Experience
Intramural Attendance Compulsory
Study Units
Each study unit includes learning objectives, required readings, suggested supplementary readings and an assignment.
© 2013 Canadian Healthcare Association. All rights reserved. 4
FSNM Yr 2 Se 2 Introduction
The study units in the program are:
5. Nutritional Care
6. Nutrition Therapy 1 -Weight Management, Diabetes, Cancer and AIDS
7. Nutrition Therapy 2 - Nutritional Management of G.I. Disorders, Surgery and
Supplemental Feedings
8. Nutrition Therapy 3 - Nutritional Management of Heart Disease, Renal and Gallbladder
Disorders and Pancreatitis
Unit Assignments
Unit assignments are available individually on the Gateway. Students must upload all completed assignments directly to the Gateway for grading.
© 2013 Canadian Healthcare Association. All rights reserved. 5
FSNM Yr 2 Se 2 Unit 5
Food Services and Nutrition Management
Year Two Semester Two
Unit 5: Nutritional Care
© 2013 Canadian Healthcare Association. All rights reserved. 6
FSNM Yr 2 Se 2 Unit 5
Nutritional Care
Objectives
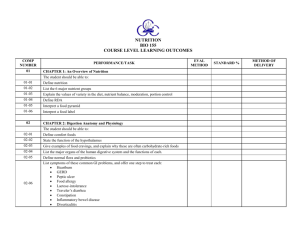
Upon completion of this unit, the learner will:
List chronic disease afflicting the North American population and cite risk factors, both dietary and non-dietary;
Understand the importance of nutrition in relation to disease prevention;
Explain the impact of illness on patient's food acceptance and nutritional status;
Identify the roles of the members of the health care team in establishing a coordinated patient care plan and the nutrition care plan;
Understand how components of assessment are used to develop nutrition care plans, and be able to perform a nutritional assessment;
Utilize the nutritional assessment to develop a nutrition care plan;
Differentiate between nutrition /diet therapy instruction and nutrition/ diet therapy counselling;
Outline the steps comprising the dietary counselling process;
Conduct a nutrition counselling session on general nutrition;
Be able to adjust general meal patterns to meet individual needs.
Introduction to Nutritional Care
Dramatic progress is occurring in attaining better health for Canadians. Much of this progress has been due to the control of preventable diseases and nutrition has played a large part. More and more attention is being focused on preventative medicine or protective health than on curative measures. There are programs for the prevention of cardiovascular disease, cancer and osteoporosis.
More recently, it has been accepted that healthy eating is a significant factor in reducing the risk of developing nutrition-related problems, including: heart disease, cancer, obesity, hypertension
(high blood pressure), osteoporosis, anemia, dental decay and some bowel disorders.
"Nutritional care is the process of meeting stable or changing nutritional needs. The type of care depends on the presence of disease or potential disease, the environment and the state of growth and development of the individual. The nutritional care process consists of (1) assessing nutritional status, (2) identifying nutritional needs or problems, (3) planning and prioritizing objectives of nutritional care to meet these needs, (4) implementing nutritional activities necessary to meet the objectives, and (5) evaluating nutritional care outcomes".
1
© 2013 Canadian Healthcare Association. All rights reserved. 7
FSNM Yr 2 Se 2 Unit 5
Reducing Risk means that the chances of developing a disease are lowered. It does not guarantee that a disease will be prevented. Since several factors are involved in the development of disease, risk reduction usually involves several different strategies or approaches. For instance, healthy eating is one positive action that may help to avoid a potential problem. " Prevention refers to activities and approaches which reduce the likelihood that a disease or disorder will affect an individual, interrupt or slow the progress of the disorder, or reduce disability."
2
There is no single way of determining if a person is at risk for certain diseases. There are numerous assessment techniques that are used by clinicians. The nutritional assessment is one such technique. If a person is found to be at nutritional risk, then appropriate assessments and care plans must be developed in conjunction with that person. A thorough nutritional assessment also includes consideration of dietary history and intake data, biochemical
(laboratory) data, clinical examination and pertinent health history, anthropometric data and psychosocial data. Besides adding to the assessment of health, this information will give the health professional information for anticipating problems and preventing poor nutrition before it develops.
The Health Care Team
"Health care settings are complex environments, serving clients with multiple and diverse health care needs. The aging population and the increasing number of persons with chronic illnesses demand a blend of services to meet medical, nursing, rehabilitation, psychological and recreational needs. No one discipline has the expertise and capability to provide the necessary services. Interdisciplinary teams, who can work together in a collaborative manner, are an essential requirement to meet the current and future needs of the patient population"
3
The food supervisor/ diet technician and the dietitian are important members of the health care team. They contribute their expertise on nutrition and help to integrate the nutritional care of the individual with the other care plans. At times these goals and strategies may conflict and a compromise is required to ensure that the overall goals for the care of the client or patient is achieved. An example of conflicting goals would be between the speech therapist who has assessed a patient and determined that they should only consume very small amounts of soft foods to avoid aspiration. The food supervisor is concerned because the patient is nutritionally compromised and needs to consume more calories and protein. Together, the speech therapist and the FSS need to create a plan for the patient. Perhaps a few more days with a less than adequate diet is acceptable to avoid the problems of aspiration or perhaps a tube feeding could be considered.
8 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5
Nutrition & Disease Prevention
Osteoporosis
Over the past few years, the fear of developing osteoporosis - a disease affecting mostly women where there is a reduction in the quantity of bone - has fuelled much interest in the nutritional requirements of calcium. The benefits of calcium in the treatment of osteoporosis are currently controversial, but it is known that calcium plays an important role in the development and maintenance of bones throughout life.
Adequate calcium intake, especially during bone development, will help ensure that there are adequate reserves to withstand the accelerated bone loss later in life. Other factors involved in determining a person's risk of developing osteoporosis are bone structure, hormonal status, drug therapy, genetic background and exercise. Current health promotion for reducing the risk of osteoporosis is adequate dietary intake of calcium throughout life along with exercise and a healthy life style.
Cardiovascular Disease
Cardiovascular disease is a major cause of death and an increasing health care cost in Canada.
Certain major risk factors have been linked to this disease. See Figure 1. Some of these factors, such as family history cannot be controlled but several others, such as smoking, obesity and lack of exercise are controllable. Through various health promotion programs, these risk factors are being targeted. Diet and nutrition intervention for the general population in terms of prevention of heart disease will be an ongoing initiative of the health ministries in Canada.
Canada's Guidelines to Healthy Living recommends that a person's daily fat intake be less than
30% of the total calorie intake, that alcohol be restricted to two drinks or less and that salt intake be lowered.
Figure 1 - Risk Factors - Cardiovascular Disease
KNOWN RISKS OTHER RISKS
1. Increased blood pressure
2. Smoking
3. High Blood Pressure
4. Diabetes
5. Family history
1. Diet
2. Stress
3. Obesity
4. Lack of exercise
9 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5
CVD - Multifactorial Disease o Smoke - risk is 2-6 times greater o High serum cholesterol - risk is 3-5 times greater
The sum of these risks mathematically is 5-11 times, but in reality the risk is much greater, that is 14-16 times greater.
Therefore, the risk is greater than the mere sum of the risks (it is multifactorial).
Cancer
Research is continually being done on the causes of various types of cancer. Much of what we know about diet and cancer has been learned from epidemiological studies, the studies of distribution and causes of diseases. It is difficult to prove relationships between certain foods and cancer because of various factors, including:
Cancer is a very slow developing disease and it may be 20 plus years after a number of people are exposed to a cancer-causing agent before there is any evidence or increase in the incidence.
Some substances may cause the change in the body's cells which can lead to cancer, while other substances may promote or encourage that change,
Many cancers develop due to a combination of factors.
All recommendations to date regarding cancer prevention emphasize following Canada's Food
Guide. As well, several studies have indicated that vegetables from the Brassica or cabbage family may reduce the risk of cancer of the colon. The Brassica vegetables include cabbage, broccoli, cauliflower, brussel sprouts and rutabaga. Other studies have shown a link between vitamin A intake and a reduced incidence of cancer of the lung, mouth, larynx and esophagus. It is not known whether it is the vitamin itself or another component of carotene-containing foods that is helpful in reducing the risk of these cancers. Studies have also shown that eating vitamin
C containing foods may lower the risk of gastric and esophageal cancers. Fibre-containing foods appear to provide some protection against cancers of the colon, rectum and stomach.
In all cases of the above research studies, it has been recommended that food sources of these nutrients provide the best protection from the disease. Not enough research has been done to evaluate the effect of extra vitamin and mineral supplementation.
In unit one you read about the determinants of heath. In that reading the authors cite various factors which have been studied to determine the effect on the health of a population. Take a minute to review the determinants of health. Many of these factors influence the nutritional status of an individual or population. Being aware of these factors will assist the health professional while counselling clients.
© 2013 Canadian Healthcare Association. All rights reserved. 10
FSNM Yr 2 Se 2 Unit 5
Nutritional Screening & Assessment
Nutrition screening is a process which healthcare institutions use to determine which clients are likely to be at nutritional risk and would therefore need a more complete assessment of their nutritional status. Food Supervisors or Diet Technicians are often the individuals who perform such nutrition screening. The screening should only take 10-15 minutes to complete and this information is used to determine if the client is at high moderate or low nutritional risk. Figure 2 is an example of a screening form used in a long term care facility. Figure 3 is a description of
Resident Nutritional Risk Screening Criteria.
The nutrition screen determines which patients require a more detailed nutritional assessment.
Nutritional assessment is a process that involves collecting data to establish a client's nutritional status. From this assessment the nutritional problems are identified and a plan developed to overcome these problems. A full nutritional assessment includes: dietary history, biochemical markers (serum albumin, serum pre-albumin, serum transferring, total lymphocyte count etc.), anthropometric assessment (weight, height, BMI, triceps skinfold thickness, mid-arm circumference etc.) and medical history. The data may come from the patient or client or from other health professionals. For example a social worker may have determined that a patient is receiving social assistance. The FSS or the dietitian would use that information in assessing the nutritional status and might ask the client if it was difficult to budget for groceries. They would not ask questions directly related to income.
A thorough nutritional assessment includes two main types of data:
1) Subjective Data - this data is based on thoughts, feelings or beliefs and is provided by the patient/resident, their family or caregiver. It includes dietary intake, food likes and dislikes, social information including any socioeconomic or cultural information which is relevant to the nutritional status.
2) Objective Data - this is actual measurable data. It includes height and weight, weight patterns and ideal body weight, laboratory data of nutritional significance, medications of nutritional significance, past medical history which is relevant to the nutritional status.
Besides adding to the assessment of health, the information in a nutritional assessment will give the health professional information for anticipating problems and preventing poor nutrition before it develops.
A food and nutrition manager may be involved in doing the initial nutrition screening but the more complex assessments such as physical and anthropometric assessment requires the expertise of a dietitian who has advanced training. Anthropometric measures to determine body size and proportion require the use of standardized measurement protocols, instruments which
11 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5 are calibrated and a trained person to do the measurements. Appendix E in your textbook elaborates further on skin calibre measurements.
Pediatric nutrition assessment also requires the expertise of dietitians and/or physicians who have specialized training and knowledge. The food and nutrition manager should be aware of the types of assessments which the dietitian and/or physician may use.
Biochemical analyses provide information about protein-energy nutrition, vitamin and mineral status, fluid and electrolyte balance and organ function. Most tests are based on analyses of blood and urine samples. Table 14-7 (pp.393) in your textbook describes common blood tests with nutritional implications.
In the evaluation of body weight a weight to hip ratio may be used in clinical practice although research in Canada has shown that abdominal girth measurements provide sufficient information. Measures such as mid-upper arm circumference are not used routinely in clinical practice but are useful in research and clinical trials. A variety of measurements would be taken to take into account the differing body shapes and distribution of fat.
Measuring Body Weight - Body Mass Index (BMI) is an index of weight-to-height (kg/m²). BMI is not a direct measure of body fat or lean tissue, but it is a reliable indicator of health risks associated with underweight, overweight and obesity.
Desirable weight has traditionally been based on figures published in height and weight tables . However, the body mass index (BMI) is currently considered the best measure of weight status for healthy Canadians between the ages of 20 and 65 years of age because it has been shown to have a high correlation with body fat.
BMI = weight(kg) ÷ height(m)
2
Health Risk Classification According to Body Mass Index (BMI)
Classification
BMI Category
(kg/m
2
)
< 18.5
Risk of developing health problems
Increased Underweight
Normal Weight
Overweight
18.5 - 24.9
25.0 - 29.9
30.0 - 34.9
Least
Increased
High
35.0 - 39.9
>= 40.0
Very high
Extremely high
Source: Health Canada. (2003 ). Canadian Guidelines for Body Weight Classification in Adults . Ottawa, Canada:
Minister of Public Works and Government Services Canada.
12 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5
An example of a calculated BMI follows:
Female weighs 60 Kg and is 157 cm tall
BMI = 60 60
1.57 x 1.57 = 2.4649 = 24.34 or a BMI of 24
A BMI of 24 tells us that this women is in a healthy weight range and her weight is a low contributor for risk of developing health problems
The calculation is exactly the same for males and females. Try working out your own body mass index . Knowing that healthy weight falls between a BMI of 18.5-24.9, you can use the formula above to calculate your healthy weight range.
For example: for the female above who is 157 cm tall:
A BMI of 18.5 gives her a weight of: 45.6 kg
X(wt)
(1.57)
2
= 18.5, therefore: 18.5 x (1.57)
2
= (wt) = 45.6 kg.
A BMI of 24.9 gives her a weight of: 61.4 kg
X(wt)
(1.57)
2
= 24.9, therefore: 24.9 x (1.57)
2
= (wt) = 61.4 kg.
Her healthy weight range is: 45.6 kg – 61.4 kg
Calculate your own healthy weight range – compare it to the chart in the back of your textbook
See your Health Canada handout, “Canadian guidelines for body weight classification in adults’ – quick reference tool for professionals.”
13 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5
The use of BMI is not without limitations. BMI should only be used in men and women ages 18-
65, not for children, older adults, pregnant or breastfeeding women or very muscular individuals.
A BMI in the range of 25-29.9 is classified as overweight, while a BMI equal to or greater than
30 is classified as obese. The higher the BMI the greater the risk for developing health problems including Type 2 diabetes, elevated cholesterol, hypertension, coronary heart disease, gallbladder disease, obstructive sleep apnea, and certain cancers.
4
For persons 65 years and older the 'normal' range may begin slightly above BMI 18.5 and extend into the 'overweight' range (25-29.9). In general BMI in the upper range of the overweight category is suggestive of increased relative heart risk.
Your textbook also introduces the concepts of % Ideal body weight and % Usual body weight as measures or assessment tools for adults with illnesses that have lead to weight loss.
© 2013 Canadian Healthcare Association. All rights reserved. 14
FSNM Yr 2 Se 2 Unit 5
Figure 2
NUTRITIONAL RISK SCREENING
Resident’s Name:
Admission Date:
Review Dates:
Signature:
RISK INDICATORS
Room:
Diagnosis:
Physician:
YES NO RISK INDICATORS
1. Has the resident had an unplanned weight change 5% or more in one month, 7.5 % or more in 3 months, 10% or more in 6 months
2. Has there been reported a minimal food/fluid intake in the last 3 days.
5. Does the resident have any of the following problems:
diarrhea for 3 or more days
nausea or vomiting
choking/coughing when eating
choking/coughing when drinking
poor fluid intake
food allergies/intolerance
blood in stool *
6. Is the resident able to feed him/herself?
3. Has the resident had major changes in his/her appetite in the last three months.
4. Does the resident have any of the following medical conditions?
kidney problems
skin sores (ulcers) that won't heal
long lasting or frequent infections
high blood pressure
heart problems
diabetes
controlled (fasting blood glucose = 3.3-12)
uncontrolled
chronic constipation
7. Does the resident require feeding aids?
8. Does the resident have a serum albumin level less than 35 g/L (if available check lab results)
YES NO
15 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5
RATING:
HIGH RISK MODERATE RISK LOW RISK
*
Please refer to the Nutritional Risk Screening Criteria to determine the residents nutritional risk level rating. All residents at HIGH RISK must be referred to Dietitian.
Information available from client record or nursing observations
© 2013 Canadian Healthcare Association. All rights reserved. 16
FSNM Yr 2 Se 2 Unit 5
Figure 3
RESIDENT NUTRITIONAL RISK SCREENING CRITERIA
The following categories have been developed to determine the degree of nutritional risk level for each resident.
High Nutritional Risk Moderate Risk
unplanned weight loss
/gain 5 % or more in 1 month
7.5% or more in 3 months
obesity hypertension
chronic constipation
10% or more in 6 months
diabetes mellitus
slow continual weight loss
minimal food/fluid intake in last 3 days.
(controlled, insulin or non insulin dependent)
dysphagia
inability to feed oneself
(need feeding aids, chewing problems)
diabetes mellitus uncontrolled food allergies
kidney disease - need for protein restricted diet
lactose intolerance
poor fluid intake
continuing nausea, continuing, diarrhea or blood in the stool
poor or changed appetite
decubitus ulcers
low serum albumin
combination of four or more indicators listed as examples in moderate risk category
Low Risk
no recent significant weight change
eats independently
consumes most of an average portion of food and fluid
consumes a variety of foods in all food groups
PRIORITY # 1 - HIGH NUTRITIONAL RISK
Requires further assessment and follow up by the clinical dietitian.
PRIORITY # 2 - MODERATE NUTRITIONAL RISK
17 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2
Follow up assessment by the FSS or Diet Tech and verbal review with dietitian.
PRIORITY # 3 - LOW RISK
Quarterly assessment by FSS or Diet Tech.
Unit 5
KEY NOTE: RESIDENT'S NUTRITIONAL STATUS AND PRIORITY MAY CHANGE AT ANY
TIME
© 2013 Canadian Healthcare Association. All rights reserved. 18
FSNM Yr 2 Se 2 Unit 5
Dietary interviews provide the foundation for the collection of information about individual food habits. The information collected must be accurate and complete. Skilful interviewing requires strong listening and verbal communication skills, combined with a supportive attitude. It requires planning, objectives and the use of direct, open-ended questions.
The interviewing process contains 4 major steps.
Preparation
Collect background information on the client before the interview from the health record or a health professional.
Information needed: age, height, weight, medical history, medications, laboratory data of nutritional significance, occupation.
Build Rapport
The interviewer introduces himself/herself and begins to develop rapport with the client.
Suggestions are: discussion of the weather, the client's dress, jewellery, etc., then explanation of the reason for the interview and the objectives for this first interview.
Data Collection
The interviewer questions the client about food habits based on the previously established objectives of the interview.
It is best to ask open-ended, non-judgmental questions.
This part of the interview can be based around one or more of the tools for collecting data;
24-hour recall, food frequency questionnaire, dietary history and food record.
Closing
The interviewer must summarize the interview for the client to check how complete and accurate the interview was.
The interviewer then tells the client what will be done with the information.
Finally the interviewer tells the client when they will be contacted for follow up - either teaching, or presentation of the data collected, etc.
A sample nutritional assessment form for a long term care facility is shown in Figure 6. The nutritional assessment form shown in Figure 7 is one, which could be used in an active treatment facility. In each of these two cases, it is important to note pertinent medications that a person is taking when completing the assessment, as well as all related laboratory results. A partial list of drugs that can interfere with nutrients is shown in Figure 8. Drug-nutrient interactions are common in the elderly.
Using the strategies as described above the interviewer needs to interview the resident or patient to determine their usual patterns and habits concerning their diet.
© 2013 Canadian Healthcare Association. All rights reserved. 19
FSNM Yr 2 Se 2 Unit 5
Assessing nutritional and individual needs
This includes obtaining knowledge of food habits, medical history, resources (e.g. financial, cooking facilities, etc.), meanings and values attributed to food, specific food preferences and preparation methods. During the interview, the client will give you many clues to about how willing they are to make changes in their diet. This information will be important later as you develop a plan with the client. At this stage of the interview, it is vital that you avoid making any judgements about the information the client is sharing with you. Your role is to listen, encourage and elicit information.
Consider this scenario:
Joan is an executive secretary and has come to a nutritionist for counselling regarding a reduced sodium intake for her hypertension. She has begun to tell the counsellor that she usually buys a toasted bacon sandwich for breakfast with a coffee at the restaurant in her office building. The nutrition counsellor raises her eyebrows and says "Not only is the sandwich very high in salt but it is loaded with fat. Surely you know that is an unhealthy breakfast!!!" Joan who had looked forward to information which would help her avoid taking medications subconsciously decides to tell the nutrition counsellor only about her healthy food choices.
By making a judgmental statement during the interview, the nutritionist has defeated the purpose of gathering accurate information. Without a true picture of what the client is eating she will not be able to identify the changes that the client may be willing to make.
There are several methods for obtaining dietary information. These include:
24-hour Recall
This is the easiest and most popular method for obtaining an idea of a person's dietary intake however the interviewer must be experienced in interviewing. It gives qualitative information about an individual's diet. The person is asked for a complete listing of the foods they ate in the past 24 hours. They may not be able to recall accurately the amounts of food eaten, the previous day's intake may not be typical or they may not tell the truth about the day's intake.
Food Frequency Questionnaire
This enables the interviewer to be selective with questions about foods suspected of being deficient or excessive in the diet. It aids in validating the accuracy of the 24-hour recall data.
20 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5
This questionnaire does not give quantitative data on intake and it usually relies on the person's memory for determining how often a food is eaten.
Food Diary or Record
The patient is asked to keep a record of all they eat for at least three days. They may also supply information on lifestyle, meal eating atmosphere, etc. It is most complete and accurate if the individual records the information immediately after eating. Because several days intake are recorded, there is a better representation of a person's eating habits than with the 24-hour recall method.
It is very time consuming for both the individual to record and the professional to analyze than any other method. It also may be inaccurate because foods are forgotten if they are not recorded immediately after eating.
Dietary History
This is a combination of both 24-hour recall and food frequency questionnaire with additional personal information supplied. It helps the interviewer to assess the nutritional/dietary knowledge that the individual has in order to prepare for the type of counselling that is needed.
The interviewer must be as objective as possible and not prejudice the individual when asking the questions. It is very time-consuming to complete.
Because a patient/resident needs your help to solve a nutrition related problem, it is not surprising to find that the steps involved in nutrition assessment and counselling incorporate many problem solving techniques.
Identifying the problem and developing a plan of care
Once the assessment has identified the major problems relating to nutrition, they need to be prioritized. The greatest attention should be devoted to the problem with the highest priority. The patient should be involved in determining the priority and the goals for intervention. Choosing the most crucial problem and focusing on the major issue is crucial to your success as a counsellor. Most authorities recommend that a course of action is planned and is one that both you and the client feel will motivate the individual and result in success.
"As consumers become more vocal and knowledgeable, they wish to be actively involved in decisions affecting their own health"
5
The goals for a client may include both short term and long term objectives.
Implementing the plan of care
Implementation of the plan includes: setting realistic goals (e.g. planning gradual changes in eating habits), communicating effectively (e.g. using simple language, listening, etc.), and actively involving the patient/resident in planning, execution and evaluation of the change.
The information recorded in the first interview will provide baseline information around which
© 2013 Canadian Healthcare Association. All rights reserved. 21
FSNM Yr 2 Se 2 Unit 5 planning will be done. Identify the needs of the patient/resident and the goals for the instruction.
(e.g. the client suffers from constipation so the goal is to alleviate this problem, increase the client's intake of fluids and fibre-containing foods based on the dietary intake data obtained.)
Assess the knowledge of the learner regarding these needs.
Arranging for follow up care
During an initial hospital stay, the counsellor should arrange to follow up on the results of the care provided. However, with the shortened length of stay of most hospital patients, follow up care may be provided on an outpatient basis or by other care providers such as home care.
Evaluate results
Evaluating what you have done is one way to check that your counselling has been appropriate.
For example, you could ask yourself the following questions: a) Is there a need for a change in approach? b) Is there a lack of motivation? c) Is food preparation too difficult? d) Has my teaching been practical? e) How can I improve?
Figure 6 Nutrition Assessment
Name
Admission Date
Diagnosis/Previous Medical History
Room
Physician
Birth date
Gender
Mental Status
M F
Personal History
Height
Desirable Weight
Weight
BMI
Percentage of Desirable Weight
Percentage of Recent Weight Loss
Mobility
Hearing
© 2013 Canadian Healthcare Association. All rights reserved.
Average Wt. for age and Ht.
Goal Weight
Weight History
Percentage of Usual Weight
Vision
Dentition
22
FSNM Yr 2 Se 2
Skin Integrity
Problems related to Eating:
Choking Chewing
Gastrointestinal
Admission Diet
Dining Room Placement
Eating:
Independent
Total Feed
Assistance
Assistive Devices
Nutrition History
Bowel Function
Swallowing
Laboratory Data
Sore Mouth
Medications of Nutritional Significance
Unit 5
Food Allergy
Food Intake
Figure 6 (continued)
Food Intolerance
Fluid Intake
Nutrition Risk Screening
Low Risk Moderate Risk High Risk
No significant wt change
Eats independently
Consumes most of food and
fluid
Consumes variety of food
from all food groups
Food Allergies
Texture Modified Diet
Feeding devices
Chronic constipation
Unplanned weight loss or gain ( 10% x 6 mo)
Poor appetite
Poor fluid intake
Controlled Diabetes
Lactose Intolerance
Hypertension
Nutrition Risk Assessment
No/ Low Risk Moderate Risk High Risk
Unplanned weight loss greater than 10% over 6 months
Dysphagia
Uncontrolled diabetes
Renal Disease
Severe Decubitus ulcers
23 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2
Intervention Planned
Unit 5
Date:
WEIGHT GRAPH
Signature:
© 2013 Canadian Healthcare Association. All rights reserved. 24
FSNM Yr 2 Se 2 Unit 5
Figure 7
Department of Nutrition and Food Services
Nutrition Assessment Worksheet / Department Record
Room: Admission: Name:
Consult:
Problem relating to eating:
Chewing
Swallowing
Gastrointestinal
Intake: Normal
No change in usual intake
Degree of abnormal intake:
Starvation
Suboptimal solid diet
Full liquid diet
Hypocaloric diet
Hypercaloric
Yes
Abnormal
No
Team Conference
Diagnosis and nutritionally significant medical history
Choking
Sore Mouth
Food Aversion
Salivation
Menu Selection:
Family Assistance
Nut & Food Service
Independence of Feeding:
Self
Assistance
Total Feed
Feeding Aids
Daily
Yes
Weekly
No
Present Diet Order:
Medication of Nutritional Significance:
Previous Diets:
Height measured)
Usual Weight
Desirable Weight
(estimated or
Current Weight
Goal Weight
25 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5 by
BMI Wt. (kg)
Ht
2
(m)
Unintentional Weight loss/gain Yes No
BMI less than 18.5 underweight at risk
BMI 18.5-24.9
healthy weight range
Percentage of Desirable Weight
80-90% = mild 70-79% = moderate 0-69% = severe
If yes,
Percentage of Usual Weight
Less than 5%= small loss
5-10% = potential significance
Greater than 10% loss = definite significance
kg within past months
BMI 25-29.9
caution zone
BMI over 30 overweight , at risk of health problems
Percentage of Usual Weight
85-95% = mild 75-84% = moderate 0-74% = severe
Percentage of Recent Weight Loss
Significant Weight Loss =
-2% over 1 week months
Food Allergies Food Intolerances
Figure 7 (continued)
Functional Capacity or Energy Level: No Dysfunction (full capacity)
Ambulatory Degree: Working suboptimaly
Skin Integrity
(Comment on any decubitus ulcers and duration)
Dysfunction
Bedridden
26 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5
Laboratory Data
1. Hemoglobin
3. Hematocrit
4. Total Lymphocyte count
g/L (117-157) 2. Serum Albumin
g/L (.350-.470 g/L)
X91 (1.0 - 4.8 x 91)
5. Other
Consultation or Team Conference - Recommendations:
Special Menu Request/Requirements
Breakfast Lunch
g/L (34-52)
Nourishment - AM Nourishment - PM
Dinner
Nourishment - HS
Adequacy of Present Intake:
(Comment on pt acceptance of diet, consistency, nutritional adequacy as compared to Canada's Food Guide to
Healthy Eating, consumption of nourishments, comments from meal rounds and meal intake records)
Calculated Meal Plan
Protein
Starch
Calculated Meal Pattern
B AM L PM D HS PRO FAT CHO
CHO
PRO
FAT
%
%
%
27 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2
Milk
Fruit&Veg
Fats&Oils
Extras
Other
Unit 5
SODIUM
FLUID
POSTASSIUM
ESTIMATED DAILY REQUIRMENTS
ENERGY
PROTIEN
FLUID
COMMENTS
SIGNATURE DATE
© 2013 Canadian Healthcare Association. All rights reserved. 28
FSNM Yr 2 Se 2 Unit 5
Figure 8
DRUGS THAT INTERFERE WITH NUTRIENTS
Drug Nutrients Affected
Antilipemia
Cholestyramine
Chlofibrate
Antiparkinson
Levodopa
Anti-ulcer
Tagamet
Aspirin
Decreases absorption of cholesterol, vitamins A, D, K,
B12, folic acid and calcium.
Drug
Alcohol
Nutrients Affected
Decreased absorption B1, B12, and folic acid.
Increased excretion of
Magnesium and Zinc
Decreases absorption of cholesterol, carotene, glucose, iron and B 12.
Anti-arthritic
Penicillamine
Increased excretion of zinc, iron, copper and B6.
Increased need for Vitamin C and B6.
Decreased absorption of tryptophan and amino acids
Antibodies
Penicillin
Increased excretion of potassium.
Decreased absorption of
Calcium, Iron, Magnesium and
Zinc.
Bacterial overgrowth in stomach with decreased acid secretion, possible malabsorption
Tetracyclines Decreased synthesis of Vitamin
K.
Neomycin
Increased excretion of Vitamin
C, B2, B6, folic acid and nitrogen
Decreased absorption of fat, nitrogen, lactose, sucrose, potassium, calcium, iron, B12,
Vitamins A, D, and K
Anticoagulants Antagonist of vitamin K
1-3 grams cause 2 mg iron loss, may alter CHO metabolism; antagonist of vitamin K
Antiinflammatory
Increased need of Calcium,
Vitamins D. C & B6,
29 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2
Decreases serum folate
Unit 5
Cardiovascular
Digitalis
Diuretics*
* Potassium sparing diuretics:
Aldactone,
Dyazide,
Aldactazide
*Potassium wasting diuretics:
Lasix, Diural,
Hydrodiuril,Thia zide
Hypotensive
Hydralizine
Increased urinary excretion of potassium, magnesium and calcium.
Increased urinary excretion of
B1, B6, Ca, Mg.
Inactivates B6 and increases urinary excretion
Corticosteroid
Glucocorticoid
Fluid Retention
Increased need for vitamins B6,
C, D, folic acid.
Increased absorption of calcium and potassium.
Nutritional Care Plan
The nutrition care plan flows from the nutrition screening and assessment. The care plan includes a problem statement, realistic and observable (or measureable) goals, suggested interventions and time frames for review. Interventions may include a special diet or feeding regimen, patient education, monitoring of the special diet and evaluation of progress on the diet or in the education program. The Nutritional Care Plan is part of the overall care plan for the patient/resident. The central person in the process is the patient/resident who must be involved and should participate as much as possible in planning for and implementing all care.
6
This is referred to as patient centered care .
30 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5
See Figure 9 for a sample Nutrition Care Plan displayed in the form of a Health Care Record display.
Providing optimal nutrition for any patient in hospital or resident in a long term care facility requires a coordinated team approach. The basic team members are the physician, dietitian/food service supervisor and nurse. Other members may include the pharmacist, social worker, physiotherapist and occupational therapist. This team may meet weekly or monthly at
Multidisciplinary Rounds to discuss patient problems. The accreditation standards from CCHSA require that there be teams developed to work together to ensure quality care.
Some teams are developing care maps . A care map is a standardized care plan for a patient's stay depending on the procedure or diagnosis and is based on the expectations of the progress of uncomplicated cases. For example the care map of a post operative appendectomy, patient may have their diet as clear fluid on Day 1 and progressed to a general diet on Day 2.
Provision of Nutritional Care
Meals are usually the highpoint of the day for patients/residents in any type of health care facility. It is through the food served to patients/residents that nutritional care is provided.
Successful results in a nutritional care plan are developed from the patient/resident eating the food provided for his/her benefit and the food service department ensuring that the meals provided meet the needs of the patients/residents.
Nutritional care must be based on individual patient/resident needs. This does not require individual diets or meals for each person because those persons with similar needs may be grouped together. For example, all residents in a nursing home who have ill-fitting dentures may receive chopped or dental-soft foods.
However, each of these residents will have a different nutritional status - some may be overweight, others at nutritional risk because of disease or illness. Attention to these other needs will be important in the provision of nutritional care.
© 2013 Canadian Healthcare Association. All rights reserved. 31
FSNM Yr 2 Se 2 Unit 5
Figure 9
Health Care Record Display – Sample of computerized care plan system
Resident: Mrs. Smith Room/Bed 216/A Care Unit: Oak
Care Plan: Indicators of Moderate Nutritional Risk Present
Created by: Goodman
On 09 may 2010 14:39
Last update: Goodman
20 Aug 2010 09:24
Goals active: 10 Complete: 0
Inactive: 0 Discipline: DIET
Next Review: 30 -11-
2010
Concerns Goals Interventions
RELATED TO:
AS EVIDENCED BY:
Status: A, 09 May, 2010 Provide Full diet with Regular texture
Who: DIET, NUR
Meet kcal, protein and fluid needs.
Estimated energy requirement =
1500-1600 kcal. Estimated protein requirement = 52-57 gm protein (1.0-
1.1 gm/kg); Fluid requirements =
1500 ml fluid; BMI = 19.7. Goal to maintain weight within GWR and BMI within normal range
Provide and encourage intake of 1500 ml fluid at meals and/or snacks Who: DIET,
NUR
Monitor weight monthly and report weight changes > 2 kg to Nutrition Manager
Who: NUR
Record and review intake of all meals and snacks. Who: NUR
Involve Mrs. Smith in menu selection. She doesn’t like liver. Who: DIET, NUR
The above nutrition interventions have been discussed with Mrs. Smith and/or substitute decision maker Who: DIET
Self-feeding difficulty related to not completing
Status: A, 09 May, 2010
Mrs. Smith will consume > 75% of
Mrs. Smith requires assistance in the form of cutting meats, opening cartons, opening packages Who: NUR
32 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5 meals
Constipation meals and snacks,
Status: A, 09 May, 2010
Maintain self-feeding
Status: A, 09 May, 2010
At least 3 soft formed stools weekly
Provide assistance as needed Who: NUR
Offer 125 ml prune juice at breakfast daily
Who: DIET, NUR
Status: A, 09 May, 2010
Reduce use of suppositories and laxatives
Status: A, 09 May, 2010
Serve whole grain breads Who: DIET,
NUR
Potential for skin breakdown.
Osteoporosis
Maintain skin integrity
Potential for weight loss
Status: A, 09 May, 2010
Mrs. Smith will eat sufficient food to maintain weight in GWR of 49.0-59.9 kg
Abnormal lab values
Status: A, 09 May, 2010
Maintain acceptable lab values for
Hgb, Hct, RBC
Provide high energy high protein snacks i the form of 125 ml milkshake at PM and
HS snack Who: DIET, NUR
Mrs. Smith is encouraged to complet protein portion at meals. She does not want supplements at this time.
DIET, NUR
Who:
MD aware of abnormal levels. Who: DOC
NUR
Status: A, 09 May, 2010
Maintain communication with wound care team to be aware of any skin breakdown
Who: NUR
Maintain bone health
Provide calcium rich snacks in the form of milk, pudding, yogurt, cheese, salmon, and other calcium rich foods Who: DIET,
NUR
Recommend multivitamin/mineral supplement daily Who: DOC NUR
33 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5
Nutrition Counselling
Give a man a fish and he eats for a day. Teach him how to fish and he eats for a lifetime. Proverb
Nutrition counselling is defined as "the total process of providing individualized guidance so that the client acquires the ability to self-mange his/her own nutrition care, i.e. successfully effect behaviour change that results in more healthy behaviours."
7
There is a big difference between diet instruction and nutrition counselling. Instruction is giving the client the knowledge about the dietary modifications, counselling goes beyond instruction in that the counsellor assists the client develop the strategies to incorporate the desired changes into their lifestyle.
Change is difficult for most people and behaviour change is even more difficult. One mistaken belief regarding dietary change is that "dietary change can be effected by short-term counselling. Nothing could be further from the fact. Changing one's behaviour takes time and can be achieved only via long-term, individualized efforts in most instances in which the client becomes involved. Nutrition counselling is effective only when the client accepts and practices improved behaviours. Compliance, then, is a behavioural outcome that mediates nutrition counselling, appropriate and desired behaviour, and positive health outcome."
8
In the article "Steps to take in primary care for achieving lasting dietary change" the author
Johanna Dwyer identifies some steps to incorporate in the counselling process for dietary change. She advises that one step in the process is to inform and motivate the patient.
"Motivation is an inward prompting or an impulse that brings forth an action."
9
As a counsellor it is important to discuss the client's reasons for a dietary change. An example of using motivation to improve health is the practice of a large teaching hospital to offer the children of patients having had a heart attack the opportunity to have an assessment of their cardiac risk factors in the outpatient clinic. Motivation to avoid coronary artery disease is very high at this point in their lives and any health or nutrition counselling is likely to produce more sustained lifestyle changes. It is important for counsellors to realize while they are facilitators for their clients, it is the client themselves who need to take the responsibility for the change process.
In your reading “Tailor your counselling with the Stages of Change model" there is an excellent discussion of the stages of motivational readiness. The type of information and the methods to use when counselling people at the various steps is very valuable to the nutrition counsellor.
Tailoring your counselling to this model will help the client to move along the stages until they can begin to make changes in their diet. Some individuals will have moved through some of these steps prior to seeing a counsellor.
One of the most successful strategies in assisting clients in changing their dietary behaviours is to ensure that they are successful in their first goals. Some clients are unrealistic and want to achieve major change very quickly. The effective counsellor will assist the client in identifying
34 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5 realistic and achievable goals. The client needs to be assured that the goals will change as they move towards the desired outcome.
Counsellors need to give the client the information the client needs to know rather than the information which is nice to know. Information concerning which foods are the best food choices, how to prepare their foods and how to choose a meal in a restaurant is the information the client needs to know in order to be successful in dietary change. As the client moves through the stages of change, they may require more technical information.
Another function of the counsellor is to identify potential obstacles to the client's success. These may require the counsellor to change their way of imparting knowledge. A dietitian in a teaching hospital told of a teaching session she had with a blind patient. The dietitian was prepared to involve another member of the patient's family in the teaching session or to use a tape recorder for the patient. When she discussed it with the patient, the patient preferred that the dietitian simply explain the information verbally. In the follow up session, the patient had retained most of the important points the dietitian had explained. The dietitian was amazed until the patient explained that he had memorized information for many years and this skill was well developed to overcome his loss of sight.
Once an individual has made dietary changes, the next step is for them to maintain the changes over the long term. "Dietary lapses are less likely to result form a lack of skills in food selection and preparation than from new, altered or continuing barriers to dietary change in the patient's social and physical environment."
10
The counsellor can assist the client in identifying strategies to overcome these barriers. Clients need to be assured that they have not sabotaged their efforts by deviating from the improved behaviour on occasion. A common saying is "It's not what you eat between Christmas and New Year that is important, but what you eat between New
Year and Christmas."
In health care today, a common theme is evaluation. This is also true for nutrition counselling.
Consider the strategies that you and the client have utilized. What worked? What could be improved? What would I do differently?
As food service supervisors, you may be responsible for nutritional counselling of patients/residents in your facility. It is generally accepted that the FSS /Diet Tech are capable of normal nutrition counselling and diets in which their is one dietary modification, e.g. cholesterol lowering diet, or a reduced sodium diet. It is important for the FSS/Diet Tech to evaluate their own level of knowledge and confidence concerning a specific diet. If you are unsure, a referral to a dietitian is indicated.
As health care professionals, there is an obligation to provide the best treatment possible in the form of high quality care and consistent support for individual change over time.
35 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5
Documentation
In a hospital and many long term care facilities, nutritional information and nutritional status of a patient is recorded in a medical record or chart. A dietitian, food service supervisor, or diet technician will record this information so that other members of the health care team will be aware of the nutritional care plan and nutrition related activities. The nutrition information recorded may include diet orders, diet history, a report of the patient's acceptance and tolerance of the diet, communication between the dietary staff and other members of the health care team concerning the patient, request for diet consultations, nutritional care discharge plans.
In some facilities, the medical chart is organized according to the patient's major problems. They include a data base, problem list and progress notes. Entries are organized according to the
SOAP format. This can be outlined as:
S - subjective information; e.g. lack of appetite
O - objective; e.g. actual weight
A - assessment; e.g. inadequate intake of calories
P - plan; e.g. have patient eat between-meal-snacks. This section should also include how you will evaluate the success of your intervention and the follow up planned.
The following information was adapted from the Clinical Nutrition Policy and Procedure Manual of Dartmouth General Hospital in Nova Scotia. Include the following information under these headings when charting.
S Subjective Information, Patient's Comments (use direct quotes if possible)
attitude
previous diets, previous dietary instructions, successes of failures
pertinent information from diet history ( e.g. meal pattern)
pertinent lifestyle information (e.g. cooking facilities, eating away from home, shift work)
activity pattern
O Objective Data, Clinical Findings and Observed Behaviour
age, height weight, ideal weight, calculated BMI, initial goal weight , weight changes ( in follow up notes record only weight changes)
diet order
calculated energy intake ( from energy counts/intake sheets}
nutritionally significant medical history
medications of nutritional significance
laboratory data of nutritional significance
observed behaviours on the nursing unit or in the cafeteria or dining room
36 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5
A Assessment of the Subjective and Objective Data to arrive at the Determination of the
Nutritional Status of the Individual and to Formulate a Nutrition Care Plan
assessment of nutritional status including problems noted in diet history
appropriateness of diet order (e.g. energy level, nutritional adequacy, consistency)
patient's tolerance and/or acceptance of diet
patient's understanding of need for diet
patient's motivation and predicted compliance
need for resources (e.g. Meals on Wheels, Homemaker services)
progress made ( e.g. makes appropriate food choices, weight changes)
P Plan or Suggestions for Coping or overcoming the Problem
objective to be achieved with nutrition intervention (e.g. ideal weight, improved nutritional status)
obtain more information (e.g. recommend energy count, monitor food intake)
nutrition intervention recommended(e.g. change in diet order, supplemental feedings, consultation with other health professionals)
patient education, description of diet instructions
follow up in hospital or after discharge
Over the years, the SOAP format has been modified. The acronyms SOAPIE and SOAPIER refer to formats that add interventions, evaluation and revision.
I
E
Interventions refer to the specific interventions that have actually been performed by the caregiver
Evaluation includes client responses to interventions and medical treatments. This is primarily reassessment data.
R Revision reflects care plan modifications suggested by the evaluation. Changes may be made in desired outcomes, interventions or target dates
When charting in the medical record there are some generally accepted rules to follow. The medical record is a legal document and all entries need to be accurate, clear and concise.
Entries should be in black ink, be legible and should be dated and signed at the time of the entry. If an error occurs when you are writing a chart note, the correct procedure for corrections is to put a line through the entry and initial and date the error. An example is given below:
Weight 158 lb error P.S 96/0403
37 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5
Figure 10 lists common abbreviations approved for use in medical charts. Figure 9 shows an example of a SOAP note as part of the medical record. Table 15-1 on page 413 of your textbook lists terms prohibited on clinical documentation.
In some long term care facilities and hospitals, a kardex system or notebook may be used to organize information about the nutritional and/or nursing care plans for a resident/patient. It may also be stored in a computer information system where the information is easily assessed regarding patient's likes/dislikes, eating habits and sample meal plan.
© 2013 Canadian Healthcare Association. All rights reserved. 38
FSNM Yr 2 Se 2 Unit 5
Figure 10 SOAP NOTE
Date Time COMMENTS
March 2, 1997 13:00 h S: Patient states that appetite is poor. "I just don't have any appetite" At home normally ate three meals per day and did not snack. Has never been on a special diet. He is concerned about the recent weight loss. Dislikes the supplements offered and would prefer something less sweet.
O: Weight 130 lb (59 kg). Height 6 feet (182 cm)
Calculated BMI 18, Recent Weight loss of 18 lb.
Usual Weight 148 lb ( 67 kg) Albumin 2.2 g/dl
A: Significant weight loss of 18 lb since admission. Jan 19,
1996. Probably related to decreased caloric consumption and increased needs due to acute stage of illness. Low albumin indicative of low protein intake. At moderate to severe nutrition risk.
P: Will request dietitian do a complete nutrition assessment.
High protein snacks will be offered TID.
Energy/ protein assessment will be conducted for 3 days.
Will calculate intake on March 6 and follow up with further recommendations as per dietitian consult.
Roberta Smith, FSS
39 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5
Figure 11 COMMON APPROVED MEDICAL ABBREVIATIONS abd abdomen e without a.c. ad lib
AIDS
AKA aq.
ASHD
Ba before meals as desired
Acquired Immunodeficiency syndrome above-knee amputation water arteriosclerotic heart disease barium
ECG, EKG
EEG
ENT
ER f
FBS
Fe electrocardiogram electroencephalogram ear, nose, and throat emergency room
Fahrenheit fasting blood sugar iron
BaE b.i.d.
BMR
BP c barium enema twice a day (bis in die) basal metabolic rate blood pressure with (cum)
FH
F/u
GB
GI g family history follow-up gallbladder gastrointestinal gram gr. grain(s)
Grav.1,2,3 first, second, third pregnancy
C.A.
Ca
CAD
CAPD
CAT scan computed (axial) tomography
CBC complete blood count cc
CCU chem
CHF chronological age calcium; cancer coronary artery disease continuous ambulatory peritoneal dialysis cubic centimeter coronary care unit chemotherapy congestive heart failure
GTT
GYN
Hb(hgb) h.d. h/o
H
2
O h.s. hx
IDDM glucose tolerance test
Gynecology
Hemoglobin at bedtime (hora decubitus) history of water at bedtime (hora somni) history insulin dependent diabetes mellitus chr chronic
40 © 2013 Canadian Healthcare Association. All rights reserved.
CPR
CR ct.
CVA
CVS
C/W
CXR
DD
DM
DOB
DT
D
FSNM Yr 2 Se 2 c.gl. cm
CNS
CO
2
C0PD correction with glasses centimeter central nervous system carbon dioxide chronic obstructive pulmonary disease cardiopulmonary resuscitation chronic renal failure count cerebrovascular accident cardiovascular system compare with chest x-ray discharge diagnostic diabetes mellitus date of birth delirium tremens diagnosis inj.
I.Q.
IV (i.v.)
Kg;kg
L
LAT;lat
L&W
M.A.
MAO mEq/L mg
MH
Ml mL mm
Na
NED neg.
NG tube
NIDDM
Unit 5 injection intelligence quotient intravenous (injection) kilogram liter; left; lower lateral living and well mental age monoamine oxidase milliequivalent per liter milligram marital history myorcardial infarction milliliter millimeter sodium no evidence of disease negative nasogastric tube non-insulin dependent diabetes mellitus
41 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5
Figure 11 (continued)
OB obstetrics
OR os oz. p.c.
PD
PE pH
PKU
PM p/o po pos. operating room opening; mouth; bone ounce after meals peritoneal dialysis physical examination alkalinity and acidity measurement phenylketonuria afternoon (post meridian) postoperative
Orally (per os) positive preoperative as required (pro re nata) protocol q.n.s.
R.,r.,rt.
R/O
Rx s
SOB sol. st. stat.
Sx
T t.i.d.
TPN
TPR quantity not sufficient
Right rule out treatment; therapy without (sine) shortness of breath solution stage (of disease) immediately (statim) symptoms temperature three times daily (ter in die) total parenteral nutrition pre-op p.r.n. prot. pt.
PTA q.d. q.h. patient prior to admission every day (quaque die) every hour (quaqua hora)
Tx w/f w/m y/o temperature, pulse, and
respiration treatment white female white male year old q.i.d. q.n. four times daily (quater in die) every night (quaque nox)
Reference: Chabner, D. (1985). The Language of Medicine . Toronto, ON: W.B. Saunders Co.
(Your facility may have another list of approved abbreviations. You should follow the rules of your facility when using abbreviations)
© 2013 Canadian Healthcare Association. All rights reserved. 42
FSNM Yr 2 Se 2 Unit 5
Confidentiality
Any caregiver in a hospital or long term care facility has access to information on patients/residents that must be kept confidential. The medical record or resident/client record will document the course of the patient's health care, personal information and acts as a method of communication among all the members of the health care team.
In the text Medical Record Management Huffman states that: "In order to fulfil these purposes, significant amounts of data must be revealed and recorded. The patient must be assured that information shared with health care professionals will remain confidential; otherwise the patient may withhold critical information which could affect the quality of care provided". Patients and residents expect their privacy to be respected. Care must be taken that such medical and personal information related to patients and clients, is shared only with those individuals providing care and who have a need to know such information.
Health care professionals must be careful of the manner in which information is transmitted.
Conversations regarding a patient or resident must nor take place in areas where the conversation may be overheard. Written information must be kept in a confidential manner.
Information stored in a database must be secure from unauthorized access.
There are usually specific instructions in each facility regarding recording of information on residents and storage of this information. To discard any information, it may have to be shredded.
Standard Hospital Diets
The normal diet is the foundation diet for an institution. In some instances the normal diet is modified for texture and consistency. Other conditions require modification in energy and/or one or more nutrients; eg. sodium restricted, modified fat. These diet alterations will be discussed in the following units of the Study Guide.
1. General diet
also known a normal, regular, full or house diet
planned for the healthy "average" Canadian with no restriction in foods
2. Fluid diets
two types: clear fluid and full fluid
these diets do not provide all the nutrients needed by the body. Appropriate commercial supplemental feeds should be provided if the patient/resident is unable to progress to solid food within two to three days.
clear fluid
"The clear or restricted liquid diet is frequently ordered for post operative patients/residents to furnish fluids, some electrolytes and small amounts of energy
43 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5 prior to the return of gastrointestinal function. It is an inadequate diet composed chiefly of water and carbohydrates and therefore is used for a very short period of time."
11
composed of clear liquids such as tea, broth, carbonated beverages, popsicles, strained fruit juice (if tolerated), and gelatin.
no milk or milk products
full fluid
used post-operatively or whenever solid food cannot be tolerated or there is a difficulty with chewing and swallowing solid foods.
composed of foods that are liquid at body temperature.
milk and milk products such as yogurt, puddings, custard and ice cream are permitted as well as refined cooked cereals and strained cream.
soups in addition to liquids permitted on the clear fluid diet.
nutritionally inadequate supplementation required.
Refer to the Manual of Clinical Dietetics for specific restrictions.
3. Texture modifications in diets
Any diet can be modified in texture depending on the requirements of the patient/resident.
At one time, "Dental Soft" was the term used for these diets. Now there can be variations in this dental soft diet ranging from bite-size foods to pureed consistency. There is also a soft fibre-restricted diet available in some hospitals that is used between the full-liquid and regular diet. It is nutritionally adequate and includes soft foods that are easy to chew and digest without harsh fibre, stimulating flavourings or excessive richness.
The detailing of specific food textures under bite size, mechanical soft, minced, pureed and blenderized aids in understanding the slight differences that may be needed by certain patients.
Information is also given on dysphagia and common eating problems with developmentally handicapped persons.
The article by Fernie gives practical information for the assessment and feeding techniques for the resident with dysphasia. Unit 7 contains more information regarding dysphasia.
44 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 5
Conclusion
Satisfactory nutrition of patients/residents requires a team approach with the patient or resident, physician, nurse and dietitian or food service supervisor being the key participants. Nutritional screening or assessment identifies those persons at risk. Dietary counselling is an essential aspect of therapy as well as development of a nutritional care plan for the patient/resident.
Appropriate documentation in the chart or kardex will ensure that all members of the team are aware of the nutritional interactions.
Diet therapy involves modifying the patient's/resident's normal nutritional needs to meet the demands imposed by a specific condition or disease. Careful assessment and the development of an individualized meal plan help to enhance the success of nutritional management and diet therapy.
This unit described modifying the consistency of the house or regular diet. Fluid diets are used pre and postoperatively and whenever there is difficulty chewing and swallowing. Texture modified diets are used for residents with ill-fitting dentures, neuro-motor difficulties, young children and for dysphagia.
© 2013 Canadian Healthcare Association. All rights reserved. 45
FSNM Yr 2 Se 2 Unit 5
Endnotes
1
Mahan, L and Escott-Stump. (1996). Food, Nutrition & Diet Therapy , Philadelphia, PA: W.B.
Saunders Co., p.403.
2
Health and Welfare Canada. (1992). Enhancing Prevention in the Practice of Health
Professionals . Ottawa, ON: Health and Welfare Canada, p.30.
3
Hibbert, J.M., and Kyle, M. (1994). Nursing Management in Canada . Toronto, ON: W.B.
Saunders Canada, p.501.
4
Health Canada. (2003). Canadian Guidelines for Body Weight Classification in Adults . Ottawa,
ON: Her Majesty the Queen in Right of Canada, p. 7.
5
Ibid. P 511
6
Robinson, C., Weigley, E.S., and Mueller, D.H. (1993). Basic Nutrition and Diet Therapy . New
York, NY: MacMillan Publishing Co., p.287.
7
Vickery, C.E. and Hodges, P.M.(1986). Counselling strategies for dietary management:
Expanded possibilities for effecting behaviour change , Journal of the American Dietetic
Association , 86, 924-928.
8
Ibid, pp 924-925
9
Dwyer, J. (1991). Steps to take in primary care for achieving lasting dietary change, Topics in
Clinical Nutrition , 6(4), 22-3.
10
Ibid p. 30
11
Krause, M. and Mahan, L. (1984). Food, Nutrition and Diet Therapy.
Philadelphia, PA: W.B.
Saunders Co., p 401.
© 2013 Canadian Healthcare Association. All rights reserved. 46
FSNM Yr 2 Se 2 Unit 5
Required reading
Textbook(s)
DeBruyne, L.K., Pinna, E. & Whitney, E.N. (2012).
Nutrition and diet therapy (8th ed.). Belmont,
CA: Wadsworth/Thomson Learning.
Chapter 14 “Illness and Nutrition Care”, pp. 381-409
Chapter 15
Chapter 17
“Medications, Herbal Supplements, and Diet-Drug Interactions”, pp. 410-
428
“Consistency-Modified & Upper GI Disorders – only first section on modified diets and dysphagia”, pp. 460-463.
Appendix E Nutrition Assessment: Supplemental Information
Readings from Course Reader
Health Canada (2003). Canadian Guidelines for Body Weight Classification in Adults
–
Quick Reference Tool for Health Professionals . Ottawa, ON: Her Majesty the Queen in
Right of Canada.
Anderson, D. (2003). Improving nutrition screening and assessments in long term care.
Long Term Care , 13(2),15-18.
Cleary Stuart, C. (2007). Current approaches to managing feeding and swallowing disorders for residents with dementia. Canadian Nursing Home , 18, 11-16.
Becel, Heart Health Information Bureau. (1997). Heart Headlines™ Tailor you counselling with Stages of Change model, 4(2).
Dietitians of Canada – Client Education Handout series; Soft Diet
47 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2
Unit 5 Assignment located on the Gateway
To complete the Unit 5 assignment, please access your account on the Gateway at www.cha.ca. The assignment is available in Word format on the Gateway for you to download. Once completed, please upload your assignment into the designated location.
Unit 5
© 2013 Canadian Healthcare Association. All rights reserved. 48
FSNM Yr 2 Se 2 Unit 6
Food Services and Nutrition Management
Year Two Semester Two
Unit 6: Nutrition Therapy I - Weight
Management & Nutritional Management of
Diabetes, Cancer and AIDS
49 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 6
Nutrition Therapy I - Weight Management & Nutritional
Management of Diabetes, Cancer and AIDS
Objectives
Upon completion of this unit, the learner will:
Use BMI to assess an individual’s health risks and list the major health risks associated with underweight and overweight/obesity;
Discuss the importance of body composition and fat distribution for assessing health risks associated with body weight;
Discuss the complex factors that determine body weight;
Explain the principles of weight management for overweight/obesity and discuss these with a client or patient;
Plan weight management menus and physical activity plans based on Canada’s Food
Guide, CDA’s Beyond the Basics and Canada’s Physical Activity Guide
;
Discuss the factors that influence body image and suggest strategies to help individuals establish a positive body image;
Discuss the continuum of eating disorders including anorexia nervosa, bulimia nervosa and binge-eating disorder and explain the treatment approach for each;
Explain the causes of underweight, the nutritional care of underweight and formulate suggestions for promoting weight gain;
Differentiate the characteristics of the types of diabetes mellitus;
Describe the methods for monitoring diabetes mellitus;
Summarize the nutrition recommendations for diabetes mellitus;
Categorize foods into the Canadian Diabetic Association Beyond the Basics meal planning for healthy eating program and be familiar with serving sizes;
Plan menus according to specified meal patterns and correct selective menus;
Outline the current etiologies of cancer and HIV/AIDS;
Explain the nutritional requirements in the disease states of cancer and AIDS;
Suggest dietary strategies for individuals with cancer to overcome the side effects of the disease/treatment and enable them to optimize their nutritional status.
50 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 6
Introduction to Nutrition Therapy I
This unit is the first unit in which nutrition therapy is used to alter a disease state or to overcome the nutritional problems resulting from a disease. Nutrition therapy is the cornerstone of the treatment of weight management (obesity, overweight /underweight) and is a major factor in the management of diabetes. In cancer and HIV/AIDS individuals have nutrition related problems, and the skilful management of these problems will enhance the quality of life for patients and may improve their ability to undergo treatment.
"Healthy weight is a vital part of a healthy life. Those who are at a healthy weight feel better, are less likely to develop chronic diseases, and enjoy a better quality of life. On the other hand, an unhealthy weight – being either underweight or overweight or obese – is a serious threat to health and wellbeing.” 1
In Canada almost 50% of adults are either overweight or obese. These epidemic rates have serious consequences for the health of Canadians. Both overweight and obesity are recognized risk factors for Type 2 diabetes, elevated cholesterol, hypertension, coronary heart disease, gallbladder disease, obstructive sleep apnea, and certain cancers.
2
Body weight is determined by the relationship between energy intake and energy output as well as the influences of a complex combination of biological, lifestyle, socio-economic, cultural and environmental factors. Weight management involves a commitment to healthy eating, physical activity and behaviour modification. An important part of this process is to establish a positive body image that accepts a range of body shapes and weights as attractive and healthy.
Unrealistic ideals of thinness are partially to blame for the increasing prevalence of eating disorders in North America including anorexia nervosa, bulimia nervosa and binge-eating disorder."
3
Diabetes mellitus is a chronic disease of the endocrine system. Currently over one million
Canadians have diabetes and about one in 20 Canadians can expect to develop it during their lifetime. This unit will cover the types of diabetes in relation to nutritional management
Weight Management
The regulation of body weight depends on a balance between energy intake and energy output.
Energy intake is the amount of fuel (calories) taken in through consumption of carbohydrates, proteins, fats, and alcohol. Food intake is regulated by feelings of hunger, appetite and satiety.
Energy output is the amount of calories expended, mainly for basic body functions, the processing of food, and physical activity.
An imbalance between energy intake and energy output leads to weight gain or weight loss. The energy imbalance that results from overeating and inactivity is responsible for much of Canada’s overweight and obesity epidemic. The percentage of Canadians who are overweight or obese has risen dramatically in recent years.
4
According to the 2004 Canadian Community Health
Survey, 23.1% of adult Canadians are obese. An additional 36.1% are overweight.
5
The rates of childhood overweight and obesity are also on the rise. In recent years the rates of obesity in
© 2013 Canadian Healthcare Association. All rights reserved. 51
FSNM Yr 2 Se 2 Unit 6 children ages seven to thirteen has tripled.
6
Overweight and obesity are major public health challenges. Scientists speculate that the rising rates of obesity will soon reverse the increases in life expectancy that occurred throughout the twentieth century.
7
As the waistlines of North American’s have expanded so has the weight loss and dieting industry. American estimates suggest that the revenues of the commercial weight loss industry total more than $30 billion (US) from diet centres, specialty foods, medications, exercise clubs and weight loss books and magazines. Fad diets continue to engage the public, often with outlandish and unrealistic claims.
8
Overweight and Obesity
The World Health Organization (WHO) defines obesit y as “a condition of excessive body fat accumulation to an extent that health may be compromised.”
The Canadian Guidelines for Body
Weight Classification in Adults , developed by Health Canada provides a system for categorizing health risk according to body weight, as measured by body mass index (BMI), and level of abdominal fat, as measured by waist circumference (WC). Take a moment to review calculating
BMI which was covered in Unit 5.
Waist Circumference (WC) provides an independent indicator of health risk associated with abdominal fatness. A waist circumference at or above 102 cm (40 inches) for men and at or above 88 cm (35 inches) for women is associated with increased risk of cardiovascular disease, elevated cholesterol, type 2 diabetes and hypertension.
9
Reading: Canadian Guidelines for Body Weight Classification in Adults Executive
Summary and Quick Reference Tool for Professionals summarizes this information and provides a quick reference for interpreting Body Mass Index and Waist Circumference.
Body weight consists of water, skeletal tissue, muscles, organs, blood and other body fluids and fat tissue (also known as adipose tissue). The adipose tissue is the storage site for the energy reserves of the body. Some adipose tissue is necessary for normal function of the body (see study unit 2). Body fat values of 10-22% in men and 20-32% in women are generally considered satisfactory.
10
Several methods exist to assess body composition. These include underwater weighing, bioelectrical impedance and fatfold measurements.
Distribution of body fat is even more important than the amount of body fat for assessing health risks. Intra-abdominal fat that collects deep within the abdominal area and around the organs is more likely to lead to health problems than subcutaneous fat that is stored just under the skin. Intraabdominal fat creates the “apple” shape that is common in men and post-menopausal
52 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 6 women. The apple shape presents a greater health risk than the “pear” shape where fat is distributed around the hips and thighs.
Factors Influencing Body Weight
Although body weight is a relationship between energy intake and energy output, body weight is also influenced by a complex combination of biological, lifestyle, socio-economic, cultural and environmental factors.
Reading: Chapter IV of the 2004 Chief Medical Officer of Health Report: Healthy Weights,
Healthy Lives discusses the mix of factors that determine weight.
Healthy Weight Management
Just as each person has a unique set of interrelated factors that lead to weight gain, approaches to weight management are just as complex. To be effective they must be tailored to the individual. The American Dietetic Association defines weight management as “the adoption of healthful and sustainable eating and exercise behaviours indicated for reduced disease risk and improved feelings of energy and wellbeing.” Healthy approaches to weight management emphasize overall health and fitness rather than a specific weight loss goal. In many cases, a modest amount of weight loss (about 10 percent) can reduce health risks.
11
A combination of diet modification, physical activity and behavioural therapy is the approach recommended by qualified weight management professionals (physicians, dietitians, psychologists, etc.). Dietary recommendations are based on Canada’s Food Guide to Healthy
Eating and emphasize moderation and a balanced diet that is low in fat and high in healthful foods such as vegetables, fruits and whole grains. Recommendations for physical activity are based on Cana da’s Physical Activity Guide
and involve incorporating regular moderate physical activities as part of a healthy lifestyle. Behaviour change is seen as an ongoing process that requires new skills for maintaining a healthy lifestyle. A healthy approach also builds in strategies to enhance self-esteem and aims to reduce the social pressures that make people strive for extreme thinness.
Reading: The three Healthy Measures fact sheets provide tips for achieving and maintaining a healthy body weight through active living, healthy eating and behaviour modification.
Other more dramatic approaches to treating obesity have been used by the medical community with varying degrees of success. These include anti-obesity prescription medications, behavioural therapies, commercial programs, very low calorie diets (VLCD), meal replacements, and bariatric surgery such as gastroplasty and gastric bypass surgery.
Fuelled by the weight loss and diet industry, many overweight Canadians are on a perpetual quest for the miracle s olution to weight loss. It seems every few years there is a new ‘fad’ that goes against the healthy approach to weight management. In recent years the low carbohydrate
© 2013 Canadian Healthcare Association. All rights reserved. 53
FSNM Yr 2 Se 2 Unit 6 or very low carbohydrate fad diets have prevailed. Sadly, without a commitment to permanent lifestyle change and improving physical, social and psychological wellbeing, most individuals will regain any weight lost.
Reading: The Dietitian’s of Canada article, Beyond the low carb hype: Should I try a low carbohydrate diet to lose weight?
explores the dangers of low carbohydrate diets.
Underweight
From a public health standpoint, in Canada, underweight is much less of a problem than obesity. However, underweight people are at increased risk of developing health problems such as undernutrition, osteoporosis, infertility and compromised immune function. Underweight may also be an indication of an eating disorder or an underlying illness, such as cancer.
12
The
Canadian Guidelines for Body Weight Classification in Adults defines underweight as a BMI less than 18.5. For seniors age 65 and over, the risks associated with underweight may be evident at a BMI somewhat higher than for younger adults. For seniors, BMIs in the low 20s and below suggest the need for additional health assessment to rule out underlying conditions such as undernutrition, osteoporosis and cancer. For young adults who have not reached full growth or for naturally lean adults a BMI somewhat less than 18.5 is not necessarily an indication of health problems.
13
The causes of underweight are varied. Chronic disease such as cancer may be associated with general malnutrition and wasting. Illnesses, infections and certain medications can speed up metabolic rate and interfere with appetite and digestion. Hormonal disturbances such as hyperthyroidism may also play a role in underweight. Addiction to alcohol and street drugs is yet another cause of underweight.
An inadequate food intake may be multifactorial. Causes may include depression and other psychological factors which cause a person to refuse to eat, a loss of appetite or inadequate resources to obtain and prepare food. In addition, familial attitudes towards eating that are indifferent may result in learned behaviours that contribute to underweight. Malabsorption may also contribute to underweight. If individuals are unable to effectively absorb nutrients they will not be able to maintain the energy supply required to maintain a healthy weight. Excessive exercise without adequately compensating with increased food intake may also cause underweight.
The dietary treatment of underweight requires an assessment of the reasons for the underweight and correcting any underlying medical problems (if at all possible). The nutritional care should be individualized to the particular circumstances of the patient or client.
Practitioners need to be sensitive to the personal, living and economic situation of the underweight person. Strategies to increase the caloric density of the diet and the overall nutritional quality must be coordinated with these special circumstances. Prescription medications such as appetite stimulants, medications to speed stomach emptying or digestive
54 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 6 enzymes replacements may be helpful for some. Exercise also has an important role in weight gain as a strategy to increase muscle mass.
Body Image and Eating Disorders
Body image is a person’s mental concept of his or her physical appearance and the associated feelings and judgements of that concept.
14
Sometimes this mental concept can be very inaccurate and has little to do with how a person actually looks or how others see them. Body image can have a dramatic effect on how people feel about themselves – their self-esteem.
Many factors influence body image including culture, family and friends, and individual personality. There are incredible pressures on people, especially women, to buy into the idealized body image promoted by the media and fashion industries. The overall message presented is that thin people are successful, in control, popular, healthy and happy and that anyone willing to work hard enough can be thin. As a result, many people set unrealistic goals for the way their bodies should look which ultimately leads to frustration, guilt and body image dissatisfaction.
Establishing positive body image starts with challenging unrealistic ideals of thinness. It means accepting that healthy, good-looking bodies come in a range of weights, shapes and sizes.
There is no one singe ‘best weight’ for a particular age group or body type. Rather, there is a range of weights that are healthy. Provided healthy foods are eaten and physical activity is included, the body will naturally settle at a weight that is healthy for each individual. Learning to love and accept oneself and being a good role model for others is the best way to foster positive body image.
Eating Disorders
Eating disorders are a spectrum of abnormal eating patterns that eventually may endanger a person’s health. Eating disorders are divided into three categories that form a continuum, with self-starvation at one end and compulsive overeating at the other.
15
Anorexia
Nervosa
Bulimia
Nervosa
Binge-eating
Disorder self-starvation binge & purge compulsive overeating
55 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 6
On the surface it may appear that eating disorders result from the societal pressures to be thin.
However, the causes of eating disorders are complex and not fully understood. The current view is that certain people appear to have a predisposition to eating disorders that may be rooted in complex interactions between social, biological and psychological factors.
Anorexia Nervosa is a self-imposed starvation syndrome that is triggered by a severely distorted body image. Even when dangerously underweight, people with anorexia typically see themselves as fat. Anorexia nervosa is characterized by a preoccupation with dieting and thinness that leads to excessive weight loss, usually to less than 85% of expected weight for height or a BMI less than or equal to 17.5. Other symptoms include muscle and bone wasting, cessation of menstrual cycle, abnormal heart rhythm, lowered body temperature, development of a downy hair known as languna and depression.
The typical anorexia sufferer is an upper-class Caucasian female adolescent, although more recently, it is affecting people from a wider range of social and ethnic backgrounds. Most experts doubt that patients with anorexia can ever be cured, however, with intensive therapy patients can achieve a normal weight. Severe cases may be hospitalized in inpatient treatment programs. Less severe cases may be treated in outpatient programs. Effective treatment should involve support from a multidisciplinary team of physicians, psychologists, psychiatrists and dietitians.
Bulimia Nervosa is a pattern of binge eating and then purging the body of the food before it is digested and absorbed. The purges may be in the form of self-induced vomiting, the use of laxatives, and/or excessive exercise. The average person with bulimia is an unmarried
Caucasian woman in her twenties or thirties with a normal or near normal weight. The complications of bulimia include electrolyte imbalances, damage to the enamel of the teeth, inflammation of the esophagus, kidney damage and damage to the gastrointestinal tract.
Bulimics often have a great sense of guilt over their behaviour and hide their behaviour from friends and family.
Bulimia appears to be easier to treat than anorexia, perhaps because bulimic patients tend to recognize that their behaviour is abnormal. More than half of patients report an improvement in their binge-eating and coping behaviours following treatment with dietary and behaviour therapies.
Binge-eating disorder is the most common eating disorder seen in people of all ages and backgrounds. Like people with bulimia, those with binge-eating disorder consume excessive quantities of food in a relatively short period of time. Unlike bulimia, those with binge-eating disorder do not attempt to compensate by purging or other means. Not all binge eaters are obese, although many obese people binge. Most binge eaters are people who have not learned to cope with their emotions and seek solace in food. People who have binge-eating disorder usually require therapy to help them identify and cope with emotions. Some benefit from antidepressant medications.
56 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 6
Reading: The article, Eating Disorders and Body Image, from BC Partners for Mental
Health and Addictions Information discusses the prevalence of eating disorders and body image dissatisfaction in Canada and the complexities of managing these disorders.
Diabetes Mellitus
Diabetes mellitus is a chronic disease of the endocrine system characterized by changes in carbohydrate, protein and fat metabolism.
16
There are three main types of this disease. The basic principles of diet management are similar.
Type 1 Diabetes
This class of diabetes is sometimes called IDDM (Insulin-Dependant Diabetes Mellitus). These persons are dependent on daily insulin injections, which may be given in single doses, multiple doses, or continuously with an insulin pump. Type 1 Diabetes is usually diagnosed in children/youth.
Reading: Type 1 Diabetes - Things You Should Know . Go to Canadian Diabetes website – in addition to this reading about type 1 diabetes, there is an audio recording about the information on that section. http://www.diabetes.ca/files/type1-basics.pdf
Type 2 Diabetes
This is also known as NIDDM (Non-Insulin-Dependant Diabetes Mellitus). The vast majority of people in this class are older and overweight. The symptoms may improve with weight loss.
Reading: Type 2 Diabetes - Things You Should Know , http://www.diabetes.ca/files/Type2Basics.pdf
Also see handout on Type 2 diabetes – the basics.
Gestational diabetes
Approximately 2-4% of all pregnant women in North America will develop glucose intolerance during the pregnancy. This is known as gestational diabetes and usually occurs in the second or third trimester. Women who have pre-existing diabetes prior to their pregnancy are not classified as having gestational diabetes.
Recently, increasing numbers of children and youth in high-risk populations are being diagnosed with type 2 diabetes. This emphasizes the importance of teaching healthy eating and physical activity to delay and prevent the onset of diabetes mellitus.
57 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 6
Human beings require energy and the major source of energy is glucose , which is a form of sugar. (Other sources of energy are fats and proteins). The principles underlying the diabetic diet are not difficult to understand if the role of food and glucose in relation to insulin is explained. Our bodies cannot manufacture glucose so it must be obtained from the food we eat.
Carbohydrate containing foods are broken down in the gut into smaller components called glucose which is absorbed in the small intestine and released into the blood circulation. Blood transports glucose to the cells and tissues.
At this point, a hormone called insulin is released from the pancreas to facilitate the entrance of glucose into cells where it is used as a fuel to supply the body with energy. It acts as the "key" to open the "cell door" for glucose to enter.
If glucose is not required immediately for energy, it is stored in the liver as glycogen until required. For example, glycogen is often released into the blood to provide energy between meals. Glycogen is also stored in muscle to be readily available when energy is needed during physical activity.
"It is essential that the level of blood glucose remains within a certain range. One very important reason for this is that glucose is the brain's major source of energy, and if the blood glucose falls rapidly and remains below a certain level, the brain is "starved" and will cease to function.
This, of course, means death."
17
In diabetes, there is either a partial or total lack of insulin or a resistance of the cells to the action of the insulin. Insulin is responsible for "opening the doors" of the cells and therefore, if this hormone is not produced by the pancreas, glucose is unable to enter the cells. Glucose builds up in the bloodstream (outside of the "cell doors") and the result is an increased blood glucose level called hyperglycemia . Some of the "excess" glucose is filtered through the kidneys, where its presence can be detected using simple urine tests.
If, on the other hand, too much insulin is present, more glucose will enter the cells. If the serum glucose level happens to be low at this time (for example, because food was not eaten due to a missed or delayed meal) too much available glucose will leave the bloodstream and this can lead to a low serum glucose level or hypoglycemia . Exercise facilitates the uptake of glucose by the cells. When a person with diabetes exercises more than normal, they need to compensate for the exercise by eating a snack to prevent hypoglycemia.
The above description is an over simplification of the actual process. However, it does serve to emphasize the importance of insulin and diet in controlling blood glucose levels.
Medical Nutrition Therapy
The goals of medical nutrition therapy for the treatment of diabetes are to:
1. Control blood glucose levels to avoid both hyperglycemia and hypoglycemia.
58 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 6
2. Control body weight to optimal or a reasonable weight range.
3. Control or prevent complications of diabetes such as:
Repeated infections
Cardiovascular diseases (coronary heart disease and hypertension)
Nephropathy (compromised kidney function)
Retinopathy (retinal degeneration and loss of vision)
Neuropathy (damage to the nerves)
4. Promote overall health of the individual.
Energy needs of individuals with diabetes are the same as for other persons of the same age, activity and height. The energy level of the diet needs to be sufficient to allow a normal growth rate for children and adolescents.
The recommended protein intake should be 15% - 20% of total calories. Fat content of the diet should be less than 35% of the total calories of the diet. As diabetes is a major risk factor for the development of cardiovascular disease, a reduced fat intake is beneficial to help prevent the development of cardiovascular disease. Saturated fats should be restricted to less than 7% of total energy daily intake and trans fatty acids should be kept to a minimum. Polyunsaturated fats should also be limited to less than 10% of energy intake. When possible, meal plans should favour monounsaturated fats and include foods rich in polyunsaturated omega-3 fatty acids (e.g. fatty fish) and plant oils (e.g. canola, walnut, flax).
The carbohydrate content of the diabetic diet should be 45-60% of the total energy level of the diet. The amount and source of carbohydrate in meal planning should be considered. The glycemic index (GI) is a scale that ranks carbohydrate rich foods by how much they raise blood glucose levels compared to a standard food. Low glycemic index foods raise blood glucose levels slower and lower. High glycemic index foods raise blood glucose faster and higher.
Therefore, it is recommended to consume low GI foods in place of high GI foods within the same food category to help control blood glucose levels.
Reading: Nutrition Therapy – CDA 2008 Clinical Practice Guidelines. See table 3; pg.S43.
How and when sugar is included in the diet has important effects on blood sugar control. Added sugar can be permitted in amounts of 10% of total calories. For example up to 40 - 45 g of sucrose (5 tsp.) in an 1800 kcal diet. This is the amount of added sugar currently in the typical
Canadian diet.
The use of sugar in the diabetic diet is optional, and portions of sugar choice are small. The inclusion of sugar choices should be spread throughout the day and be part of a mixed meal, (a meal that contains starch, protein and fats & oils). This will slow the absorption of the glucose and permit good blood glucose control.
© 2013 Canadian Healthcare Association. All rights reserved. 59
FSNM Yr 2 Se 2 Unit 6
Nutrition thera py and meal planning should be individualized to accommodate the person’s preferences, age, needs, culture, lifestyle, economic status, activity level and readiness to change. In general, people with diabetes should follow the healthy diet recommended for the general population in Eating Well with Canada’s Food Guide . Foods should be low in energy density (high in nutrient density) to optimize satiety and discourage overconsumption, help attain and maintain healthy body weight, and ensure an adequate intake of carbohydrate, fibre, protein, essential fatty acids, vitamins and minerals.
Pharmacological Treatment
Insulin
As indicated earlier, insulin injections are required for the person with Type 1 diabetes; however insulin is used in some Type 2 diabetics to achieve tighter control of the blood sugar when oral hypoglycemic and diet therapy have not achieved the optimal blood sugar for the individual. In addition, at times of acute illness or surgery, insulin may be required for a period of time.
There are several categories of insulin related to the onset and duration of action. Regular insulin is short acting insulin with a short onset of activity and a peak activity in 2-3 hours. The duration of the activity is 3-6 hours. Intermediate acting insulins are NPH and Lente . Ultralente insulin is a long acting insulin with an onset of activity of 6-10 hours after injection and a duration of effect of 18-24 hours. Individuals with diabetes may take a combination of insulins to optimize their blood glucose control. A recent study of intensive treatment of diabetes showed that the tight control of blood glucose levels delays or prevents the complications of diabetes.
One method of this intense control was multiple injections of insulin.
Insulin therapy and the dietary management of diabetes need to be carefully orchestrated with the timing of meals and snacks to provide a source of carbohydrate and the onset of insulin activity and to cover the peak effect of the insulin.
Reading: Canadian Diabetes readings on insulin and commonly used diabetes pills.
Oral hypoglycemics
Individuals with Type 2 Diabetes who do not achieve adequate blood sugar control with dietary modifications and exercise may require an oral hypoglycemic agent. The sulfonylureas act to cause the pancreas to secrete insulin. Biguanides increase the body's ability to utilize glucose.
© 2013 Canadian Healthcare Association. All rights reserved. 60
FSNM Yr 2 Se 2 Unit 6
Other medications used to treat diabetes reduce the cell's resistance to insulin or by slowing the absorption of carbohydrates. However the sulfonylureas and biguanides are the most common medications used for Type 2 blood glucose control.
Your text is the source of your background information on the metabolic disorder of diabetes mellitus. Carbohydrate counting has become more popular with persons with diabetes to manage their blood sugars and their medication whether on insulin or oral hypoglycemics.
The American guidelines for diet in the text are similar, but different to the Canadian ones, so use the CDA ‘Beyond the Basics” for diet therapy and carbohydrate counting. Also note that the normal and target levels for blood glucose on page 549 of your text, differ from the Canadian levels. American blood glucose levels are measured in mg/dl and Canadian blood glucose levels are measured in mmol/l. The following information reflects the 2013 Canadian Clinical
Practice Guidelines.
Figure 1
Recommended Blood Glucose Targets for People With Diabetes*
AIC
A1C Fasting blood glucose / blood glucose before meals
(mmol/L)
Blood glucose two hours after eating
(mmol/L)
Target for Type 1 & Type 2 patients with diabetes
=7.0% 4.0 to 7.0 5.0 to 10.0
5.0 to 8.0
(if AIC target not being met)
The website for the Canadian Diabetes Association, www.diabetes.ca
, is an excellent up to date resource for all information about diabetes. “Just the basics”, “Basic Carbohydrate Counting” and “The Glycemic Index Resource” are just a few of the instruction sheets that you can download for yourself, as a student, or later, as an educator, and for patients. On the website, you will also find the 2013 Clinical Practice Guidelines
( http://guidelines.diabetes.ca/Browse.aspx
). The Nutrition Therapy chapter from the guidelines is re-printed in your readings.
The article by Paula Blagrave looks at diabetic meal planning in long term care.
© 2013 Canadian Healthcare Association. All rights reserved. 61
FSNM Yr 2 Se 2 Unit 6
Hypoglycemia
Hypoglycemia may occur in individuals who are not diabetic. There are two types of hypoglycemia in non diabetic individuals; reactive hypoglycemia occurs when symptoms develop one to five hours after a meal and fasting or post-absorptive hypoglycemia occurs when symptoms develop after fasting for at least six hours. Exercise, alcohol and some medications may contribute to the condition. There is no specific diet for the post-absorptive hypoglycemia, treatment consist of determining the underlying cause and treating it.
Hypoglycemia is considered to be present when the blood glucose levels are less than 3.3 mmol / L and the person experiences symptoms. The symptoms may range from sweating, tremors, increased heart rate, anxiety, pallor, hunger, dizziness, headache, to confusion. In addition to the measurement of blood glucose levels a serum insulin level that is high is also part of the diagnostic work up for hypoglycemia. A high serum insulin level causes the glucose to leave the blood and enter the cells.
Nutritional management of the reactive hypoglycemia centers around a diet which is 50-55% of calories from carbohydrate and avoiding all concentrated sources of simple sugars. It is thought that individuals, who have hypoglycemia, produce excess insulin from the pancreas in the presence of simple carbohydrates in the diet. This results in a rebound hypoglycemia. Complex carbohydrates however are absorbed more slowly and the release of insulin is not as great. The diet should have no more than 30% of calories from fat and the remainder of the calories from protein. Alcohol and caffeine intake should be moderate. Some people will require between meal snacks and most require an evening snack. Each meal should have one portion of a high protein food as this will stabilize the blood sugar fluctuations.
Complications – From Head to Toe
Diabetes strikes nearly every part of the body. Studies show that good management and aggressive treatment of the disease can curb the damage.
Eyes
– Diabetes is the leading cause of blindness among adults aged 20-74. Every 1% reduction in A1C (from 8% to 7%, for example) lowers the risk of eye, kidney and nerve disease by 40%.
(Excerpt from Nutrition Action Health Letter – June 2004)
Brain – People with diabetes are more likely to be diagnosed with dementia. Researchers don’t know if the dementia is due to diabetes or to multiple mini strokes (common in people with diabetes) that gradually impair mental function over time. If it’s mini-strokes, lowering blood pressure might protect the brain. (Excerpt from Nutrition Action Health Letter – June 2004)
Heart – Cardiovascular disease is responsible for up to 80% of deaths in people with diabetes and is among the most devastating complications of diabetes. Effective management and prevention of complications is vital for decreasing the burden of diabetes and improving the
© 2013 Canadian Healthcare Association. All rights reserved. 62
FSNM Yr 2 Se 2 Unit 6 quality of life of people who have it. Lifestyle interventions, including weight reduction, physical activity and smoking cessation, remain key strategies for CVD prevention and diabetes management. A well-balanced, energy-restricted diet that is low in saturated and trans fats, dietary cholesterol and refined carbohydrates is considered essential
Kidneys - Diabetes is the fastest growing cause of end-stage renal disease. Obesity is linked to type 2 diabetes and a report by the Canadian Institute for Health Information released in
February 2007 found that diabetes is a major risk factor for kidney failure. The report, Treatment of End-Stage Organ Failure in Canada, 1995 to 2004 showed that over a 10-year period the number of newly diagnosed kidney failure patients with diabetes increased by 114%. That jump correlates with an increase in the incidence of diabetes in the Canadian population overall. In addition, among kidney failure patients with type 2 diabetes, 30% were determined to be obese.
Nerves – As estimated six out of ten people with diabetes have nerve damage that can cause problems like numbness or pain in the feet or hands, carpal tunnel syndrome (in the wrist), and delayed digestion of food. (Excerpt from Nutrition Action Health Letter – June 2004)
Feet – diabetes causes more than 60% of foot and leg amputations that are not caused by accidents. (Excerpt from Nutrition Action Health Letter – June 2004)
The Canadian Diabetes Association (CDA) Food Choice System:
Beyond the Basics: Meal Planning for Healthy Eating, Diabetes Prevention and Management
In March 2005, launched the CDA Beyond the Basics meal planning guide, replacing the former
Good Health Eating Guide. The CDA food choice system is based on Canada’s Food Guide with some changes to meet the needs of people with diabetes. In this system, foods are divided into groups according to the amount of carbohydrate, protein and fat they contain. The new meal planning guide has several features. Firstly, portion sizes and types of foods have been adjusted. Food items reflect current thinking on heart health, glycemic index and carbohydrate counting. Where possible, portions are also more similar to those in Canada’s Food Guide and to the Quebec and US meal planning systems. You need to be familiar with this information and know which foods fall under each category, serving sizes, and grams of carbohydrate, protein, fat, and energy for each category.
Beyond the Basics makes it easier for consumers to include a variety of foods at mealtimes while keeping carbohydrate fairly constant. While Beyond the Basics was created for the adult with type 2 diabetes, anyone with diabetes can use this tool.
© 2013 Canadian Healthcare Association. All rights reserved. 63
FSNM Yr 2 Se 2
Beyond the basics (2005)
FOOD GROUPS Beyond the Basics kcal (KJ)
15 g carb
Grains &
Starches
3 g protein 70 (290)
0 g fat
Fruits
15 g carb
1 g protein
0 g fat
65 (275)
Milk &
Alternatives
15 g carb
8 g protein variable fat
Skim – 90 (380)
1% – 110 (460)
2% – 130 (550)
Whole
– 140 (590)
Other Choices
Vegetables
Meat &
Alternatives
15 g carb variable fat & protein
<5 g carb**
2 g protein
0 g fat
0 g carb
7 g protein
3-5 g fat
See Nutrition Facts
Table on food label
30 (130)
(considered free in meal planning)
55-75 (230-315)
Fats
Extras
0 g carb
0 g protein
5 g fat
<5 g carb**
50 (200)
<20 (90)
© 2013 Canadian Healthcare Association. All rights reserved.
Unit 6
64
FSNM Yr 2 Se 2 Unit 6
Organization of food groups
(Reference: Canadian Diabetes Association, Helpful hints for educators using B eyond the
Basics, Meal Planning for Healthy Eating, Diabetes Prevention and Management . http://www.diabetes.ca/files/BeyondTheBasicsTips.pdf
)
1. All food groups containing carbohydrate (CHO) have been re-evaluated to provide approximately 15 g of available CHO per serving. Available carbohydrate is carbohydrate that remains after the dietary fibre and half the value of the sugar alcohols has been subtracted. Sugar alcohols can raise blood glucose thus only half their value should be subtracted.
2. Multicultural foods have been added to more accurately reflect Canada’s multicultural population and Canadians’ love of diverse cuisines.
3. Although consumers are able to select all their recommended portions of CHO according to their own preferences and cultural background, educators are encouraged to reinforce healthy eating habits that include choosing a variety of foods from all food groups.
4. Names of food groups have been changed to more accurately reflect foods included in each group. Items which do not obviously belong in a specific food group have been placed according to their most common usage (e.g. potatoes and yams in
Grains & Starches, soy beverages in Milk & Alternatives, legumes in Meats &
Alternatives). Corn remains in the Grains and Starches group as it is classified botanically as a grain. Legumes (peas, beans, and lentils), are a good source of protein but also contain about 15 g of available carbohydrate per serving, so they also must be counted as a Grains and Starches serving.
5. Foods in green boxes should be chosen more often because they are lower in fat, higher in fibre, and/or have a lower GI value. Foods to choose less often have been placed in amber boxes, in general due to their higher fat, higher sugar or higher GI values.
6. Most vegetables are now classified as “free”. This move was made to encourage consumption of vegetables for their nutritional benefits. Also, vegetables such as carrots and beets have less available carbohydrate than popularly believed because of the large amount of fibre (e.g. 22 mini carrots have 15 g available carbohydrate).
On the other hand, parsnips, peas, and winter squash provide 15 g of available CHO per 1 cup serving. Consumers who eat these vegetables on a regular basis should be taught how to account for the carbohydrate.
7. Blackberries, raspberries, and strawberries are very high in fibre, so a 2 cup serving yields only about 15 g of available carbohydrate.
65 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 6
8. Canned fruit is in a green box because although it has less fibre than fresh fruit, it is a good choice for an emergency shelf or in communities with less access to fresh produce. For ease of use, all fruit juices have been listed as a 125 mL (1/2 cup) serving. According to the nutrient data, most of the juices provided between 12 and
18g of available CHO per 125 mL. Those juices with a larger number of grams of carbohydrate in this size serving generally had a lower Glycemic Index, so this rounding has resulted in a similar Glycemic Load.
9. The Sugars group has been renamed “Other Choices” and includes a variety of sweet and snack foods. The 2003 CDA Clinical Practice Guidelines state that up to
10% of daily calories may be consumed as sugar without causing a deleterious effect on glycemic or lipid control.
10. Educators should remind patients of the importance of limiting saturated and trans fat because these fats are implicated in increasing the risk of cardiovascular disease.
Butter, however, has been placed in a green box because it contains Conjugated
Linoleic Acid (CLA). CLA is believed to be less harmful to heart health.
11. Items such as coffee, tea, diet soda, spices, vinegar, mustard and other condiments contain few calories and carbohydrates. Educators may wish to provide a list of foods commonly considered as “extras”.
12. The beige-shaded section of the meal planning chart highlights all the carbohydratecontaining foods. Carbohydrate containing foods may be counted as carbohydrate
“choices” or in grams. For example, educators may suggest that breakfast has 3
Carbohydrate choices, or 45 g carbohydrate, whichever works better for the client.
© 2013 Canadian Healthcare Association. All rights reserved. 66
FSNM Yr 2 Se 2 Unit 6
Figure 3 shows a sample diabetic meal plan and a menu that has been marked for an individual following this plan.
Meal Plan
1500 Calories
Breakfast
AM
Snack
Lunch
PM
Snack
Dinner
HS
Snack
Total
Choices
Carbohydrate
(grams / choices)
45g
3 Choices
60g 15g
4
Choices
1
Choice
2
75g 15g
5
Choices
1
Choice
2 1
210g
14
Choices
6 Grain &
Starches
Fruits
1
1
Milk &
Alternatives
Other Choices
1
Vegetables
Meat &
Alternative
1
1
1
1
1
1
1
1
3
1
4
3
1
6
Fats
Extra
1
1
2
67 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 6
1500 Calorie Menu
6 grain; 4 fruit; 3 milk; 6 meat; 2 fat, 1 other choice
Breakfast
125 ml Grapefruit Juice
1 Poached Egg
1 slice W.W. toast
(1 Fruit)
(1 Meat & alt)
(1 Grain)
Lunch
175 ml Vegetable soup
4 small Soda Crackers
Tuna Salad Plate
5 ml margarine
250 ml 1% milk
(1 Fat)
(1 Milk)
- 60 ml Tuna
- 125 ml macaroni salad
1 coffee (Extra)
- 15 ml mayonnaise (light)
- tomato slices, lettuce
Dinner
Broth
125 ml tomato juice
90 g Chicken Breast with
(Extra)
(1 Fruit)
(3 meat & alt)
- dill pickle
1 medium apple
250 ml 1% milk
Tea
PM. Snack
1 medium orange
15 ml BBQ sauce
1 Parsley Potato
125 ml Mixed Vegetables
2 broccoli spears
(Extra)
(2 Grain)
(Veg)
(veg)
H.S. Snack
30 g Cheddar cheese
½ whole pita
175 ml Plain low fat Yogurt
1 tbs. maple syrup
(1 Milk)
(1 other)
Tea (extra)
© 2013 Canadian Healthcare Association. All rights reserved.
(1/2 Grain)
(1/2 Grain)
-
(1 Meat & alt)
(1 Grain)
(1 Fat)
(veg)
(extra)
(1 Fruit)
(1 milk)
Extra
(1 fruit.)
(1 Grain)
(1 Meat & Alt.)
68
FSNM Yr 2 Se 2 Unit 6
For an accurate calculation, individuals are encouraged to use food labels. However, Beyond the Basics Meal Planning tools provide a guideline for assessing meal plans.
Calculations for the previous 1500 kcal menu.
FOOD
Beyond the Basics
GROUPS
Total
Choices
CHO g
FAT g
PRO g
Grains &
Starches
15 g carb
3 g protein
Grain &
Starches
Fruits
6
4
90
60
18
4
Fruits
0 g fat
15 g carb
1 g protein
0 g fat
Milk &
Alternatives
Other
Choices
3
1
45
15
3 24
Milk &
Alternatives
8 g protein
Other
Choices
15 g carb variable fat
15 g carb variable fat & protein
Vegetables FREE
Meat &
Alternative
Fats
Extra
6
2
24
10
42
<5 g carb**
Vegetables 2 g protein
Total Grams 210 37 88
Total Calories (1525) 840 333 352
% of total calories 55% 22% 23%
0 g fat
0 g carb
Meat &
Alternatives
7 g protein
3-5 g fat
% are based on Beyond the Basic guidelines
Fats
0 g carb
0 g protein
5 g fat
Extras <5 g carb**
© 2013 Canadian Healthcare Association. All rights reserved. 69
FSNM Yr 2 Se 2 Unit 6
Available Carbohydrate
Reading Food Labels:
The carbohydrate that remains after the dietary fibre has been subtracted.
18 g carbohydrate
– 2 g fibre
= 16 g available carbohydrate
A 125 ml serving of this product contains
16g of CHO and 3g of Protein.
Figure 4 on the next page, provides sample meal plans based on the Beyond the Basics Meal
Planning for Healthy Eating. They are meant to be used as guides only and are intended for temporary use. An individualized pattern should be developed for each person.
© 2013 Canadian Healthcare Association. All rights reserved. 70
FSNM Yr 2 Se 2 Unit 6
Figure 4 Sample Meal Plans
Total Energy kcal
Protein
Fat
Carbohydrate
Grains & Starches
Fruits
Milk & Alternatives
Other Choice
Vegetables
Meat & Alternatives
Fats & Oils
Extra
Grains & Starches
Fruits
Milk & Alternatives
Grains & Starches
Fruits
Milk & Alternatives
Other Choice
Vegetables
Meat & Alternatives
Fats & Oils
Extra
Grains & Starches
Fruits
Milk & Alternatives
Grains & Starches
Fruits
Milk & Alternatives
Other Choice
Vegetables
Meat & Alternatives
Fats & Oils
Extra
Grains & Starches
Fruits
Milk & Alternatives
Meat & Alternatives
Grains & Starches
Fruits
Milk & Alternatives
Other Choice
Vegetables
Meat & Alternatives
Fats & Oils
Total Protein, g
Total Fat, g
Total CHO, g
© 2013 Canadian Healthcare Association. All rights reserved.
1200
23%
23%
53%
2
1
0.5
2
1
0.5
1
1
1
3
1
1
1
1
6
3
2
0
5
2
72
32
165
2
1
1
1500
23%
22%
55%
2
1
1
2
1
1
3
1
2
1
1
1
6
4
3
1
6
2
88
37
210
1
0.5
1800
23%
25%
52%
2
1
0.5
1
2
0.5
2
1
3
2
1
0.5
1
3
1
1
1
9
3
3
1
7
4
103
51
240
1
1
2
1
1
2000
22%
24%
53%
3
1
1
3
1
2
1
4
2
2
1
1
10
3
3
2
8
4
113
55
270
1
1
2
1
3
1
1
2800
23%
27%
50%
2
1
1
2
1
1
1
3
2
2
1
2
5
3
2
1
1
1
11
5
4
3
12
6
154
82
345
71
1
2
1
2
1
1
2400
23%
22%
55%
1
1
3
1
1
3
1
1
1
1
1
4
1
4
1
1
1
11
5
4
2
10
3
140
59
330
FSNM Yr 2 Se 2 Unit 6
Total Calories 1236 1525 1831 2027 2411 2734
Cancer- Nutritional Management
There are important connections between cancer and prevention which have been noted in your
Study Guide in the previous unit. In this section, nutritional considerations in relation to therapy for various cancers will be discussed. "The adverse effects of cancer can be severe and may be compounded by the effects of the therapeutic regimes and the psychological impact of cancer.
The result is often a profound state of depletion. Data suggest an association between weight loss and shortened survival (Langstein and Norton, 1991) and imply a very subtle relationship between nutritional status and the outcome of malignant disease."
18
Some of the nutritional effects of the cancer include cancer cachexia . This is progressive weight loss with anorexia, loss of strength, weakness, anemia and abnormalities of protein, lipid and carbohydrate metabolism.
Weight loss may be related to a reduced energy intake or increased energy requirements. In addition the metabolism of protein, fats and carbohydrates are altered by the growth of the tumour. There is an increased demand for carbohydrate, as well as for amino acids to support the tumour growth. Lipid metabolism is also altered with a depletion of total body fat.
Fluid and electrolyte imbalances are common in advanced cancer. Patients with metastases to the bone may exhibit hypercalcemia. Excessive vomiting and diarrhea are contributory causes of some of the fluid and electrolyte imbalances.
A common complaint of cancer patients is an alteration in the taste and smell of food. These taste abnormalities can themselves lead to food aversions and reduced intake. It is important to understand that all types of cancer therapy require some form of nutritional support. The following problems encountered by patients and suggestions regarding nutritional intervention are important to know. The skill of the FSS/Diet tech in assisting clients to overcome these nutritional problems will aid the client to optimize the nutritional status.
Weight Loss - Despite the measures available to prevent it, weight loss still occurs in many patients/residents. Dietary supplementation can help to minimize or prevent malnutrition.
Continuation of the regular diet as much as possible is desirable.
Suggestions:
1)
2)
3)
Rely on well liked foods.
Arrange food attractively.
Provide a pleasant atmosphere.
72 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 6
4)
5)
6)
7)
8)
9)
Suggest light exercise before meals.
Try to add extra proteins and kilocalories to foods without increasing the quantity.
Use several small meals including snacks.
Keep a food diary on the patient/resident.
Weigh patient/resident regularly (e.g. weekly).
Nutritional supplements can be added as required using a variety of recipes to enhance aroma and appearance.
2)
3)
4)
5)
Nausea and Vomiting - Nausea and vomiting are common side effects of chemotherapy. The results can lead to dehydration and electrolyte imbalance.
Suggestions:
1) Avoid using foods which are offensive to patient/resident (e.g. hot, spicy, strong smelling or fried greasy foods).
Provide dry, salty or bland foods (e.g. crackers, toast before meals).
Supply larger portions when nausea subsides.
Serve bland, easy to digest meals several hours before treatment.
Try using cold meals to minimize food odours.
6)
7)
Include foods that are quickly and easily digested (e.g. reduce amount of fatty food, increase number of starchy food items).
Suggest to the patient/resident that they eat slowly and rest with their head elevated after eating to allow digestion to occur.
Separate dry and liquid foods. Serve fluids one hour before or after meals. 8)
9) Sipping small amounts of fluid continuously may also help to reduce nausea. Broth, fruit juice, and ginger ale (if kept down) will provide sufficient water and electrolytes for short term problems with vomiting.
Sore Mouth and Throat - Sore mouth and throat may occur because of radiotherapy or chemotherapy. In some cases, patients will develop mouth sores due to fungal infections.
Suggestions:
1) Try offering soft food and liquids that are cold or at room temperature, e.g. canned fruit, melon, gelatin, ice cream, and popsicles.
73 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 6
2)
3)
4)
5)
6)
7)
Avoid acidic foods (i.e. citrus fruit and juice). Try nectars and imitation fruit drinks with added Vitamin C to replace these juices.
Avoid serving highly seasoned foods and condiments (e.g. pepper, chilli, hot sauce, spicy meat sauce).
Avoid using rough crunchy foods.
Provide a straw for liquids to make swallowing easier.
Use extra butter, cream sauce or gravy to moisten food.
Prepare high protein, high calorie drinks (e.g. nutritional liquid supplements, milkshakes, eggnogs, etc.).
8) Local anesthetic/antiseptic mouth washes may be used to numb the area, thus enabling the patient/resident to eat with less difficulty.
Dry Mouth - Dry mouth may occur because of side effects due to radiotherapy or a reduced or altered saliva production.
Suggestions:
1)
2)
Liquids and very moist soft foods are usually easier to swallow. Dry foods can be moistened with gravy, broth, sauces or melted butter.
Use tender cuts of meat or soft alternates (e.g. fish, soft cheese, eggs, puddings, ice cream, cream soup).
3)
4)
Puree cooked meat, fruit and vegetables (only if required).
Serve cooked cereal with margarine, butter or cream.
5) Try offering soft rolls and bread (no seeds). Avoid dry snack foods, dry coarse cereal, crackers. "Dunking" foods such as cookies in tea, coffee or milk, helps to moisten the food.
Do not provide milk products when saliva is thick. 6)
7) Suggest that the patient/resident rinse their mouth frequently. If oral tissues degenerate, sweet and sticky foods should be discouraged.
Hard, sugarless candy or chewing gum may stimulate saliva production. 8)
Anorexia (Reduced or No Appetite)
Suggestions:
74 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 6
1)
2)
3)
4)
5)
6)
7)
8)
Serve well liked foods.
Arrange food attractively and serve in pleasant atmosphere.
If possible, try suggesting light exercise before meals.
Serve small, frequent feedings.
Try to add extra protein and energy without increasing the quantity of food.
Use smaller dishes and glasses.
If there is a "best time" during the day to eat, make the most of this.
Liquids or soft foods may by preferable to solids.
Early Satiety
Suggestions:
1) Provide small, frequent meals. Suggest that the patient/resident chew his/her food well and eat slowly in a relaxed atmosphere.
2)
3)
4)
5)
Avoid foods which are very high in fat (e.g. rich sauces).
Offer clear liquids 30 to 60 minutes before or after meals (instead of with meals).
"Hold" dessert for a snack when it can be enjoyed.
If bloating is a problem, avoid serving gas forming foods such as cabbage, onions, nuts, beer and colas.
Altered Taste Sensations
Suggestions:
1) If there is an aversion to meat dishes, try to serve them cold high protein substitutes for meat such as eggs, cheese, fish, poultry, milk or milk products may be better tolerated.
2)
3)
Marinate meat, fish or poultry.
Experiment with different spices and seasonings to accentuate the flavour.
4) Try stronger seasonings.
5) Use ketchup, relish or savoury sauces to enhance bland foods.
© 2013 Canadian Healthcare Association. All rights reserved. 75
FSNM Yr 2 Se 2 Unit 6
6)
7)
8)
9)
Experiment with texture or temperature.
Sugar tones down salty and acidic foods.
Salt tones down sweet and acidic foods.
Offer liquids or candies to suck to help reduce bad taste in the mouth.
Diarrhea -Diarrhea may be related to radiation therapy and chemotherapy.
Suggestions:
1)
2)
Avoid serving whole grain bread and cereals, bran, fruits with seeds and skins, dried fruit, prune juice, raw vegetables, nuts and seeds.
Highly seasoned foods, fried foods, sauces, gravy and foods of extreme temperatures may not be well tolerated.
Provide small meals at frequent intervals. 3)
4) Avoid foods and activities which may cause gas (e.g. beer, soft drinks, baked beans, cabbage, spicy foods, chewing gum, and skipping meals).
Replace fluid loss with liquids taken between meals. 5)
6) If diarrhea persists, milk and milk products should also be avoided (yogurt or buttermilk may still be tolerated).
Your textbook has information on development of cancerous cells as well as therapies and nutritional management.
Your provincial Nutritional Care Manual will supply information on nutritional assessments for those persons undergoing cancer therapy and the care of persons in palliative care, which is increasing in importance these days. There is also a summary of common side effects with the various types of chemical and radiation therapy.
AIDS-Nutritional Management
Since 1981, when the acquired immune deficiency syndrome (AIDS) was identified, considerable research has been conducted on the transmission and treatment of the syndrome and new treatment therapies are continually being developed and tested.
AIDS is caused by the human immunodeficiency virus (HIV); it destroys a type of T-cell in the immune system. The infections that develop are caused by ordinary harmless organisms which
"exploit the opportunity" of an incomplete immune system. People with immunodeficiency
© 2013 Canadian Healthcare Association. All rights reserved. 76
FSNM Yr 2 Se 2 Unit 6 disorders are at high risk of food borne infections. Presently there is no cure for AIDS, although some drugs will slow the replication of the virus.
"Acquired immunodeficiency syndrome (AIDS) and its complications remain a national concern and a major priority in health care management. Patients infected with the AIDS virus are frequently malnourished, and the etiologies of the protein-energy malnutrition in these patients with AIDS are multifactoral. The findings in these patients are consistent with those of undernourished patients without AIDS. Optimal management of these patients requires the same working knowledge and skilful management of nutrition as required in non-AIDS patients, but in combination with the knowledge of the multiple additional symptoms, complications and infections associated with progressive AIDS. It is suggested that aggressive early nutritional intervention can benefit even asymptomatic patient infected with the human immunodeficiency virus (HIV) with prolonged survival, sustained functional level and overall well being."
19
AIDS progresses at different rates with varying symptoms affecting organs and systems. One of the most common symptoms is difficulty or pain with chewing and swallowing due to candidiasis, a fungal infection of the mouth.
20
Anorexia, oral and esophageal pain and/or dysphagia, and nausea and vomiting are all causes of decreased intake of nutrients. In addition some individuals may exhibit neurological changes which result in decreased food intake.
AIDS patients may have diarrhea and malabsorption which may be the result of infestations of the GI tract, bacterial overgrowth (in the stomach and upper GI tract may be related to decreased gastric acid secretions), and specific malabsorbtive problems such as lactose intolerance. In addition, the HIV may have a direct intestinal injury which results in diarrhea. The result of the diarrhea is malabsorption of all nutrients and losses of fluids and electrolytes.
An increased metabolic rate is a significant factor in the weight loss and wasting common in
AIDS. The presence of fever and infections increases the nutritional requirements and further increases the rate of weight loss.
A nutritional assessment should be done when the HIV-positive diagnosis is confirmed in order that the patient realizes the importance of adequate diet and food safety. As the disease progresses, any dietary intervention depends on the type of symptoms and the patient's tolerance.
21
The textbook explains the various symptoms that develop, including infections, malnutrition and neurological problems. Therapy is very similar to that for cancer patients.
Reading: Nutrition Intervention in the care of persons with HIV infection: Position of the
American Dietetic Association and Dietitians of Canada.
77 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 6
Endnotes
1
Basrur, S. (2004).
Chief Medical Officer of Health Report: Healthy Weights, Healthy Lives ,
Ministry of Health and Long Term Care, p. 4.
2
Health Canada (2003) Canadian Guidelines for Body Weight Classification in Adults , Her
Majesty the Queen in Right of Canada, p. 7.
3
Health Canada. (2003). Canadian Guidelines for Body Weight Classification in Adults , Her
Majesty the Queen in Right of Canada, p. 7.
4
Heart and Stroke Foundation of Canada, Federation Policy Statement on Obesity , June 2005. p. 1.
5
Tjepkema, M. (2005) Measured obesity. Adult obesity in Canada: Measured height and weight,
Nutrition: Findings from the Canadian Community Health Survey, Issue no. 1, Statistics Canada,
Retreived from: http://www.statcan.ca/english/research/82-620-MIE/2005001/pdf/aobesity.pdf
6
Basrur, S. (2004) Chief Medical Officer of Health Report: Healthy Weights, Healthy Lives ,
Ministry of Health and Long Term Care, p. 28.
7
Insel, P., Turner, R.E., Ross, D. (2006). Discovering Nutrition , 2nd ed., Jones and Bartlett
Publishers, p. 289.
8
Dietitians of Canada. (2004). 2005 National Nutrition Month Campaign Backgrounder for
Dietitians and Community Leaders , Dietitians of Canada, p. 20.
9
Health Canada. (2003). Canadian Guidelines for Body Weight Classification in Adults , Her
Majesty the Queen in Right of Canada, p. 15.
10
Dietitians of Canada. (2004). 2005 National Nutrition Month Campaign Backgrounder for
Dietitians and Community Leaders , Dietitians of Canada, p. 10.
11
Insel, P., Turner, R.E., Ross, D. (2006). Discovering Nutrition , 2nd ed., Jones and Bartlett
Publishers., p. 291.
12
Health Canada. (2003). Canadian Guidelines for Body Weight Classification in Adults , Her
Majesty the Queen in Right of Canada, p. 7.
13
Health Canada. (2003). Canadian Guidelines for Body Weight Classification in Adults , Her
Majesty the Queen in Right of Canada, p. 16.
14
BC Partners for Mental Health and Addictions Information, (2003). Eating Disorders and Body
Image , 2003.
15
Insel, P., Turner, R.E., Ross, D. (2006). Discovering Nutrition , 2nd ed., Jones and Bartlett
Publishers., p. 486.
78 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 6
16
Robinson, C.H., Weigley, E.S. and Mueller, D.H. (1993) Basic Nutrition and Diet Therapy .
MacMillan Publishing Co. New York, NY, p.383.
17
Doran, R., and Lum-Doran, P. (1984). Diabetes . Toronto, ON: Copp Clark Pittman Ltd, p.2.
18
Mahan, L. and Escott-Stump, S. (1996). Food Nutrition & Diet Therapy, 9 th. ed .,
Philadelphia, Penn. , W.B. Saunders Co., p 813
19
Alpers, D.H., Stenson, W.F. and.Bier, D.M. (1995). Manual of Medical Therapeutics, 3 rd ed .,
Boson, Mass: Little Brown and Co., p 499
20
Robinson, C., Weigley E.S. and Mueller, D.H. (1993). Basic Nutrition and Diet Therapy. New
York, NY: MacMillan Publishing Co., p.355.
21
Robinson, C., Weigley E.S. and Mueller, D.H. (1993). Basic Nutrition and Diet Therapy. New
York, NY: MacMillan Publishing Co., p.356.
© 2013 Canadian Healthcare Association. All rights reserved. 79
FSNM Yr 2 Se 2 Unit 6
Required Readings
Textbook(s)
DeBruyne, L.K., Pinna, E. & Whitney, E.N. (2012).
Nutrition and diet therapy (8th ed.).
Belmont, CA: Wadsworth/Thomson Learning.
Chapter 6 “Metabolism and Energy Balance”, pp. 145-151 (Body weight, body composition and health)
Chapter 7 “Weight Management: Overweight and Underweight” pg. 160-187
Chapter 25
“Energy and Protein Modified Diets for Cancer and HIV Infection” pg. 637-
655
Chapter 21 “Carbohydrate Controlled Diets for Diabetes Mellitus, pp. 542-567.
Appendix B – Canada’s Meal Planning for Healthy Eating, pp. B8-B12
Readings from Course Reader
Health Canada. (2003). Canadian guidelines for body weight classification in adults :
Quick reference tool for health professionals . Ottawa, ON: Her Majesty the Queen in
Right of Canada.
Dietitians of Canada. (2006). Beyond the low carb hype: Should I try a low carbohydrate diet to lose weight?
Dietitians of Canada.
Nutrition Resource Centre (2003). Healthy measures fact sheets: Eat well, be active, be yourself.
Nutrition Resource Centre. http://www.healthymeasures.ca/eng_tip_sheets.html
Nutrition Resource Centre (2003). Healthy measures fact sheets: Eat 10 steps to a healthier you.
Nutrition Resource Centre. http://www.healthymeasures.ca/eng_tip_sheets.html
BC Partners for Mental Health and Addictions Information. (2003). Eating disorders and body image .
Canadian Diabetes Association (2013). Nutrition therapy –, Clinical Practice
Guidelines Expert Committee, pp. S45 –S55. Retrieved from http://download.journals.elsevierhealth.com/pdfs/journals/1499-
2671/PIIS1499267113000208.pdf
July, 2013.
© 2013 Canadian Healthcare Association. All rights reserved. 80
FSNM Yr 2 Se 2 Unit 6
Dietitians of Canada. (2004). Nutrition intervention in the care of persons with human immunodeficiency virus infection. Position statement of the American Dietetic
Association and Dietitians of Canada. Canadian Journal of Dietetic Practice
Research , 65: 132-135.
Blagrave, P. (2008). Diabetes care in 2008: The long-t erm care resident’s perspective.
Canadian Nursing Home , vol. 19 (2).
Dietitians of Canada – Client Education Handout series; High –Calorie, High-Protein
Diet/ Recipes/ Tips; Iron Rich Diet/ Sources of Iron/ Recipes; Calcium-Rich Diet/
Foods/ Recipes.
Internet readings:
Basrur, S. (2004). 2004 Chief Medical Officer of Health Report: Healthy Weights,
Healthy Lives , Ministry of Health and Long Term Care, Chapter IV. The Complex Factors that Affect Weight , pp. 33-42 http://www.mhp.gov.on.ca/en/heal/healthy_weights.pdf
If you scroll down this web page, you can download this publication.
Canadian Diabetes Association: www.diabetes.ca
Visit : Diabetes and you/ nutrition. Look at all the tabs in this section
Visit : For professionals/ resources/ nutrition and then go to Beyond the Basics sections for meal planning reference. http://www.diabetes.ca/for-professionals/resources/nutrition/beyond-basics/#hints
Canadian Diabetes Association Factsheets:
Just the Basics: Tips for Healthy Eating, Diabetes Prevention and Management http://www.diabetes.ca/files/JTB17x_11_CPGO3_1103.pdf
Glycemic Index 2013 http://www.diabetes.ca/documents/about-diabetes/GlycemicIndex_09_final2.pdf
Basic Carbohydrate Counting for Diabetes Management http://www.diabetes.ca/files/CarbCounting_0909_Boehringer.pdf
81 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2 Unit 6
Sugars and Sweeteners 2013 http://www.diabetes.ca/documents/about-diabetes/121020_04-198_sugars-andsweeteners_0413_lc_final.pdf
Alcohol and Diabetes http://www.diabetes.ca/documents/about-diabetes/111025_08-369_alcohol-anddiabetes_0413_lc_V2_final.pdf
Type 1 Diabetes: the basics http://www.diabetes.ca/documents/for-professionals/112007_08-399_type-1-diabetes-thebasics_0413_lc_final.pdf
Type 2 diabetes: the basics http://www.diabetes.ca/documents/for-professionals/112020_08-399_type-2-diabetes-thebasics_0413_lc_final.pdf
Cholesterol and Diabetes 2013 http://www.diabetes.ca/documents/about-diabetes/111036_08-369_cholesterol-anddiabetes_0413_lc_final_060413.pdf
Managing Weight and Diabetes 2013 http://www.diabetes.ca/documents/aboutdiabetes/BMI_and_WC_0413_lc_final.pdf
High Blood Pressure and Diabetes 2013 http://www.diabetes.ca/documents/about-diabetes/111066_09-424_high-blood-pressure-anddiabetes_0413_lc_final.pdf
Mailed Handout’s (sent to you at beginning of Year 2)
Beyond the Basics Poster – you have been provided (you also need to bring this to
Intramural)
Due to space restrictions, the Beyond the Basic Poster contains only a limited number of foods. A longer list of foods, listed within their food group in alphabetical order, with the
“choose more often” choices can be found at http://www.diabetes.ca/forprofessionals/resources/nutrition/beyond-basics/#hints
The longer list is useful for developing menus and answering assignment questions.
82 © 2013 Canadian Healthcare Association. All rights reserved.
FSNM Yr 2 Se 2
Unit 6 Assignment located on the Gateway
To complete the Unit 6 assignment, please access your account on the Gateway at www.cha.ca. The assignment is available in Word format on the Gateway for you to download. Once completed, please upload your assignment into the designated location.
Unit 6
© 2013 Canadian Healthcare Association. All rights reserved. 83
FSNM Yr 2 Se 2 Unit 7
Food Services and Nutrition Management
Year Two Semester Two
Unit 7: Nutrition Therapy II- Nutritional
Management of Gastrointestinal Disorders,
Surgery and Supplemental Feedings
2013 Canadian Healthcare Association. All rights reserved.
84
FSNM Yr 2 Se 2 Unit 7
Nutrition Therapy II- Nutritional Management of
Gastrointestinal Disorders, Surgery and Supplemental
Feedings
Objectives
Upon completion of this unit, the learner will:
Discuss the nutritional management of patients/residents with gastrointestinal disorders and be able to use these factors to plan menus appropriate for various gastrointestinal disorders;
Differentiate between the terms crude fiber, dietary fiber, and residue and classify foods as either high or low in dietary fibre;
Differentiate the terms food allergy and intolerance and be able to explain the difference to a client;
Identify those foods which are suitable and those to be avoided for various food sensitivities including lactose intolerance and be able to plan/ modify menus for these sensitivities;
Identify those foods which are suitable and those to be avoided on various allergen-free diets and be able to plan / modify menus for these diets;
Identify foods containing gluten and be able to plan a menu suitable for a gluten free diet;
Describe the special nutritional needs of patients undergoing surgery and be able to plan menus for the progression of diets from clear fluids to a regular diet;
Explain pertinent aspects of the composition and characteristics of nutritional supplements and enteral formulas;
Debate the advantages and disadvantages of oral intake vs. enteral feedings vs. parenteral nutrition.
Introduction to Nutrition Therapy II
"Gastrointestinal diseases account for about 15 percent of all absences from work in the 17 to
64 year old age group, thus representing an important economic loss to both employers and employees".
1
It is important to realize that everything we eat and drink is handled by this very intricate system and if anything goes wrong, it affects the whole human body.
Allergic conditions can produce sensitivity to certain food components which in turn can affect the digestive tract. If the gastrointestinal tract is functioning but a person is unable to be adequately nourished by the normal means of chewing food and swallowing it, supplemental feedings are considered. These feedings can be given orally or by tube to help patients/residents with certain conditions to maintain or improve their nutritional status.
2013 Canadian Healthcare Association. All rights reserved.
85
FSNM Yr 2 Se 2 Unit 7
Gastrointestinal Disorders
The open-ended digestive system begins at the mouth and ends at the anus (See Figure 1).
Linking them together is the 30-foot long gastrointestinal tract . Teeth, tongue and saliva prepare food for its descent through the throat into the esophagus , which carries the softened substance into the stomach .
"Stomach muscles churn the ingested food, and gastric glands in the lining infuse it with digestive juices, resulting in a semifluid mass known as chyme . The stomach stores partly digested food that is thoroughly processed by the small intestine . In the small intestine chyme is mixed with bile from the liver and juices from the pancreas. Valuable nutrients are sent on to the bloodstream. Waste is transported to the five foot colon , or large intestine, where it's further broken down by bacteria before moving on to the rectum , the end of the colon, and finally to the outside world."
2
A review of the process of digestion is recommended before progressing with this unit.
Gastrointestinal disease may occur at any spot along the digestive tract.
Figure 1 Major Organs Involved in Digestion
2013 Canadian Healthcare Association. All rights reserved.
86
FSNM Yr 2 Se 2 Unit 7
Gastroesophageal Reflux
Gastroesophageal Reflux Disease (GERD) occurs because of the reflux (backward flow) of the stomach contents into the esophagus. This can be due to:
incompetent gastric sphincter - a sphincter is a circular muscle which regulates an opening. When relaxed, a sphincter allows materials to pass through the opening. When contracted this structure closes the opening
the presence of a hiatus hernia (a protrusion of a structure, often a portion of the stomach, through an opening in part of the esophagus which runs through the diaphragm.
increased abdominal pressure caused by obesity or ascites (excess fluid in the space between the membranes lining the abdomen and abdominal organs (the peritoneal cavity).
Complication of GERD includes esophageal ulcers and esophagitis (which results from an inflammation of the esophagus).
Figure 2 Hiatus Hernia
There are a number of sphincters along the digestive tract that aid digestion. If one does not function properly, it is referred to as an incompetent gastric sphincter. See Figure 17.3 on page 467 of the textbook.
The primary factor for the development of gastroesophageal reflux is a reduced lower esophageal sphincter (LES) pressure. When the pressure of the LES is inadequate the reflux of the acidic gastric contents into the esophagus occurs.
Aachlasia , on the other hand is a motor disorder of the esophagus characterized by complete loss of peristalsis. The lower esophageal sphincter fails to relax and allow foods to pass from the espophagus to the stomach. Symptoms are somewhat similar to GERD. Treatment focuses on removing the resistance of the LES with medication or surgery.
The goals of nutritional care of the individual with gastroesophageal reflux disease are to prevent further irritation of the esophageal mucosa and to allow the esophagus to heal by preventing the reflux. The recommendations for changes in diet are based on the need to avoid further decreased LES pressure. Foods which reduce LES pressure and must be avoided are:
alcohol
caffeine
2013 Canadian Healthcare Association. All rights reserved.
87
FSNM Yr 2 Se 2 Unit 7
chocolate
fats (the diet avoids high fat foods)
spearmint
peppermint
High fat meals tend to decrease LES pressure and delay gastric emptying, thereby increasing esophageal exposure time to gastric acid and the volume available for reflux. Decreasing dietary fat and weight loss is generally recommended as treatment to control reflux for those over weight.
Figure 2 is a diagram of the stomach and esophagus with a hiatus hernia and shows the location of the LES in this disorder.
Ulcers
Ulcerations of the gastric mucosa (lining) may occur throughout the upper GI tract. The term peptic ulcer refers to an ulceration of either the gastric or duodenal mucosa while the term gastric ulcer refers only to ulcers within the stomach area. Duodenal ulcers are the most common form of ulcers and are most frequently found in the first portion of the duodenum known as the duodenal bulb.
The lining of the stomach and duodenum is protected by the mucosal barrier. This mucosal barrier is mucus which protects the stomach and duodenum from the breakdown of its protein structure. Ulcers occur when there is "an imbalance between two factors: (1) amount of gastric acid and pepsin (a powerful gastric enzyme for digestion of protein) secretions, and (2) degree of tissue resistance to these secretions."
3
Another causative factor for ulcers is the presence of
Heliobacter pylori in the GI tract which results in an impaired mucosal defence. The most common symptom of ulcers is pain after eating, due to the contact of gastric juices with the ulcer.
The medical and nutritional therapy for ulcers is aimed at:
reducing acid secretion by the stomach,
neutralizing stomach acids,
maintaining the protective function of the gastric mucosa, and
eliminating heliobacter pylori
“In uncomplicated disease, the role of diet may be insignificant in comparison to treatment with antibiotics and antacids.” 4
Dietary restrictions are based on individual tolerances. For this reason, the diet should be primarily a well-balanced, regular diet.
General diet recommendations include:
eat a well-balanced diet; Good nutrition is important for ulcers to heal.
2013 Canadian Healthcare Association. All rights reserved.
88
FSNM Yr 2 Se 2 Unit 7
include a wide variety of whole grains, vegetables and fruits, meats and meat alternatives (like dried beans, peas, and lentils), and milk and milk alternatives)
A diet high in soluble or viscous fibre may help to prevent ulcers from coming back. Try to eat sources of soluble or viscous fibre more often. Lentils and dried beans, oatmeal and oat bran, barley, peanut butter, nuts, vegetables and fruit are good sources of soluble fibre.
Eat your meals slowly, in a relaxed atmosphere.
Limit foods that cause ulcer pain or discomfort. There is little evidence for completely eliminating a specific food from the diet unless it causes repeated discomfort.
Use of antacid preparations and/or other medications to help neutralize the gastric juices already produced.
Avoid foods and activities which may irritate the stomach lining, including alcohol, cigarette smoking, salicylates (aspirin), and other non-steroidal anti-inflammatory drugs (NSAID) agents.
Consistency-modified diets
Modified consistency diets provide foods physically altered in texture and firmness. Consistency modified diets include liquid, pureed, chopped, tender-cooked and soft whole foods. Diets are based on the individual’s food tolerances. Persons with a decreased ability to chew may benefit from the modified consistency diet. Some conditions that warrant the use of this diet include absence of teeth, loose dentures, sore gums and head and neck injuries or surgeries, and persons with upper GI abnormalities. Although the consistency may appear bland, the taste need not be.
Your text, Nutrition and Diet Therapy, 8 th edition, provides information on a range of consistency modified diets, from clear liquid through to mechanical soft.
Terminology to describe texture characteristics of food
Hardness
Hardness is the energy necessary to attain a given deformation. It can be judged as the force required to penetrate a substance with molar teeth. As an example, an oatmeal cookie can be very tender to very hard depending on the recipe. Hardness is typically described as soft, firm and hard.
2013 Canadian Healthcare Association. All rights reserved.
89
FSNM Yr 2 Se 2 Unit 7
Cohesiveness
The strength of the internal bonds making up the product or the degree to which a product holds it shape describes cohesiveness. As an example, stirred yogurt products are less cohesive than firm yogurt. Stirred yogurt shows greater flowability and therefore has less cohesiveness than firm yogurt.
Viscosity
Viscosity refers to the rate of flow or resistance to flow. The scale ranges from water to condensed milk. Another illustration is the presentation of foods such as juices in the range from regular juice to those thickened to nectar-like juice, honey-like juice and spoon-thick/puddinglike juice. Terms used to describe viscosity include thin and viscous.
Adhesiveness
The force required to remove the material that adheres to the mouth. This scale is illustrated by foods ranging from vegetable oil to cream cheese to peanut butter and is also demonstrated by comparing the mouth-feel when eating peanut butter and when eating whipped cream products.
Popular terms for describing adhesiveness include sticky, tacky and gooey.
Other descriptors:
Size and shape of particles: gritty, grainy and coarse.
Shape and orientation of particles include fibrous, cellular and crystalline.
Moisture content descriptive terms include dry, moist, wet and water.
Fat content may be described in terms of oiliness and greasiness.
Inflammatory Bowel Diseases
Inflammatory bowel disease is a painful disease with no known cause or cure. "The term inflammatory bowel disease (IBD) refers to two chronic inflammatory conditions: Crohn's disease and ulcerative colitis. Although two distinct diseases, Crohn's disease and ulcerative colitis are similar in that they are chronic (recurring or occurring over a long period of time) inflammation involving various areas and layers of the gastrointestinal tract. The gastrointestinal tract is the organ of nutrient digestion and absorption. It is the disruption of this organ by inflammation and the associated symptoms of pain, nausea and diarrhea that contribute to the high incidence of poor nutrition associated with these diseases."
5
2013 Canadian Healthcare Association. All rights reserved.
90
FSNM Yr 2 Se 2 Unit 7
Crohn's disease is characterized by inflammation which penetrates the entire thickness of the bowel wall. Inflammation may occur at any point of the G.I. tract from the mouth to the anus and it is usually segmental (affects various segments of the G.I. tract with healthy tissue in between).
Ulcerative Colitis is a chronic inflammation and ulceration of the colon lining. (See Figure 2).
Colitis can be life threatening.
The symptoms of IBD can include:
bloody diarrhea
abdominal pain
weight loss
fever
fatigue
malnutrition
Patients/residents with IBD develop multiple nutritional deficiencies because of:
reduced food intake ( this may be a result of a poor appetite, fear of eating due to the pain and diarrhea, or because of altered taste sensations)
decreased utilization or absorption of food
increased loss of protein and energy due to steattorhea (greater than normal amounts of fat in the stool) and diarrhea. Steatorrhea also promotes the loss of calcium, magnesium and zinc.
The diet for IBD is planned to supply sufficient nutrients, restore and maintain normal nutrition and to avoid injury to the fragile intestinal lining. The energy and protein intake of the diet should be increased with a range of 40-50 Kcal of ideal body weight and a protein of 1.0 - 1.5 g per kg
IBW. Some individuals with IBD will develop a secondary lactose intolerance, although they may be able to tolerate some lactose in the diet. Lactose restriction is not required for all individuals with IBD. More information relating to the lactose restricted diet is included under the discussion of food intolerances. Diets should be individualized and undue restrictions avoided. Many individuals can consume a normal diet.
Fluids and dietary protein are increased to replace losses due to diarrhea. Two food groups are emphasized to include foods containing high quality protein:
milk and milk products
meat and alternates
2013 Canadian Healthcare Association. All rights reserved.
91
FSNM Yr 2 Se 2 Unit 7
Menu items incorporating foods from these two groups will increase the protein intake. High protein supplements may also be used.
Fibre does not need to be restricted in the case of Ulcerative Colitis. However, in Crohn's
Disease fibre intake may need to be restricted during periods of acute inflammation or if an obstruction has occurred. Consuming raw fruits and vegetables may increase diarrhea and gas so some individuals may temporarily restrict their intake and then return to a normal or high fibre diet.
Low fibre diets (also referred to as low residue diets) have been prescribed in the past for such conditions as pre-surgery preparation, post surgical period for bowel surgery, and acute inflammation of the gastrointestinal tract.
It has been found that a temporary clear fluid diet is sufficient for pre and post surgical situations and that when complete bowel rest is required, total parenteral nutrition or an elemental diet is preferred. The prevention of malnutrition is of main concern in long term therapy. The material from Dietitians@Work - Client Education Handouts contains a good overview of the nutrition therapy in IBD.
Constipation
"The definition of constipation is varied, but the condition can generally be described as the irregular, difficult or sluggish passage of stools. Often stools are dry, small in size and difficult to expel. Constipation can be an infrequent problem or an ongoing daily concern and can be caused by a number of disorders."
6
Current research indicates that fibre intake is an important part of good nutrition. Evidence indicates that a lack of fibre in the diet may contribute to many diseases such as:
bowel cancer haemorrhoids,
diabetes mellitus
atherosclerosis
gallstones
varicose veins obesity diverticulitis
When fibre is consumed it is not completely broken down, digested or absorbed by the body's digestive enzymes or secretions. Residue is the amount of fecal content remaining in the intestinal tract following digestion (after food has passed through the small and large bowel).
Residue contains undigested and unabsorbed food (e.g. dietary fibre) as well as metabolic and bacterial products .All foods leave some digestive residue. Even if no food is eaten, some residue would still be present in the colon as a result of normal metabolic processes.
2013 Canadian Healthcare Association. All rights reserved.
92
FSNM Yr 2 Se 2 Unit 7
The term "roughage" is no longer used because the word implies that dietary fibre acts as an inert filler in the large intestine and has an abrasive effect. Such descriptions are inaccurate.
Constipation refers to the infrequent or difficult passage of feces. Constipation may occur for a number of reasons including:
poor eating habits (e.g. insufficient fibre in the diet)
inadequate fluid intake (leading to the formation of hard, dry feces)
insufficient dietary fat (for lubrication)
low food intake (producing insufficient bulk for stool formation)
lack of physical activity (leading to poor muscle tone of the G.I. tract)
repeatedly failing to respond to normal bowel stimulus when the "urge" occurs.
Nutritional management of constipation includes increasing the intake of dietary fibre and stressing the importance of regular eating and exercise patterns. Increasing dietary fibre intake should be done gradually. Too much fibre, introduced too fast, may cause a bowel obstruction.
The colon cannot be expected to adjust to such rapid change. Good eating habits are stressed with regular timing of meals.
An increased fluid intake should accompany any increase in dietary fibre. A glass of water before breakfast (when the stomach is empty) will help the water pass rapidly down to the colon and excite peristaltic waves which gets the bowel working. Take a moment and read the article by Pilon to see how one facility introduced a flax program to combat constipation and improve the quality of life of residents.
Irritable Bowel Syndrome
Irritable Bowel Syndrome (IBS) - (also known as spastic colon, colitis) is characterized by a fluctuation between periods of diarrhea and constipation. "The cause of IBS is unknown, but possible mechanisms are:
(1) exaggerated gastrocolic reflex,
(2) abnormal colonic sensitivity to stretching, and
(3) dietary intolerances
Contributing causes include excessive use of laxatives and caffeine, previous gastrointestinal illness, antibiotic therapy, and lack of regularity in sleep, rest, fluid intake and bowel movements."
7
A gradual increase in fibre is recommended to establish a high fibre intake sufficient to relieve the constipation. Increased fluid intake is stressed, as are regular rest, work, meal, and
2013 Canadian Healthcare Association. All rights reserved.
93
FSNM Yr 2 Se 2 Unit 7 elimination habits. It is recommended that individuals avoid foods and beverages which are likely to precipitate diarrhea such as excessive consumption of coffee, tea, cola, cocoa, alcoholic beverages or the use of spicy foods. Some foods have also been implicated in causing abdominal cramps.
Diverticulosis
Diverticula are tiny pockets in the mucosal lining of the intestine, usually the colon. These pockets develop at points of weakened muscles in the bowel wall. It has been found that a diet low in fibre increases the pressure needed to move the fecal mass through the colon.
8
The dietary management of diverticulosis is a high fiber diet with adequate fluid intake. The fibre promotes the formation of large bulky stools and which move through the colon easily. This decreases the pressure on the colon walls and helps to prevent the formation of new diverticula.
The presence of these pockets is called diverticulosis . If these pockets become infected, it is a condition called diverticulitis . During a period of diverticulitis, a liquid diet to give the bowel rest is recommended. Then a gradual increase in the amount of fibre in the diet is usually prescribed.
Diarrhea
Diarrhea is not a disease but a symptom of various disorders. It is defined as the passage of liquid or semisolid stools of greater that normal volume and frequency.
9
Diarrhea may be categorized as osmotic, secretory or exudative. Osmotic diarrhea is caused by the presence of osmotically active (able to draw fluid into the intestinal tract) solutes. This is the type of diarrhea an individual with lactose intolerance would experience.
The diarrhea which occurs with the secretion of electrolytes and water by the intestinal epithelium is classified as secretory diarrhea. Causes of secretory diarrhea include the presence of bacterial exotoxins, viruses and increased intestinal hormone secretion.
Exudative diarrhea is caused by damage to the intestinal mucosa and results in the output of mucus, blood and plasma proteins. An example of exudative diarrhea is the diarrhea of ulcerative colitis.
Acute diarrhea is not usually a concern because it begins abruptly and ends within hours to a few days. Usual causes are dietary excesses, anxiety and food borne illness. Prolonged diarrhea leads to serious losses of fluids, electrolytes and body weight. The cause must be identified and removed and the G.I. tract is allowed to rest. Fluids and electrolytes are usually given intravenously.
2013 Canadian Healthcare Association. All rights reserved.
94
FSNM Yr 2 Se 2 Unit 7
Allergies and Intolerances
Food allergies may be defined as a sensitivity which is the body's defence reaction to a foreign substance or allergen . In other words, the immune system reacts abnormally to substances in our environment.
Allergens gain access to the body through direct contact (e.g. touching), injection, inhalation or ingestion. The response to the food allergen may manifest itself in many different ways such as hives, eczema, asthma or gastrointestinal symptoms. In a person who experiences allergic reactions, the body's immune system , for unknown reasons, behaves in an abnormal manner.
Normally, the function of the immune system is to protect the body against disease. White blood cells produce proteins known as antibodies , which combine with harmful bacteria and viruses to render them harmless. However, in allergy prone individuals, the immune system springs into action to challenge the presence of allergens resulting in a variety of undesirable symptoms.
The allergic reaction may take place in any area of the body but characteristic sites include:
respiratory system (cough, asthma)
skin (rash, eczema)
gastrointestinal system (diarrhea, vomiting)
neurological (fatigue, headache)
Usually the allergen is a protein (eggs, milk) but carbohydrate, lipids and various chemicals such as food additives may be responsible for a reaction occurring.
Any food may cause an allergic reaction but the most common offenders are: eggs corn white potato milk wheat citrus fruit tomatoes chocolate strawberries fish (shellfish) nuts bananas
The most reliable, objective method of testing for a food allergy is to eliminate the suspected offending food from the diet for a period of time, and observing any improvement in symptoms.
The suspected food is then reintroduced to check for reoccurrence of symptoms.
When a child is young, it is usually relatively simple to determine which food is responsible for producing an allergic reaction. For older children, as for adults, the diagnosis of allergy becomes more complicated because of the variety of foods eaten.
Dietary treatment in food allergies is the elimination of food causing the allergic reaction or altering the allergen by denaturing so that it no longer evokes the allergic reaction or substituting
2013 Canadian Healthcare Association. All rights reserved.
95
FSNM Yr 2 Se 2 Unit 7 another food to which the person is not allergic. For individuals with multiple food allergies, planning a nutritionally adequate diet is challenging. It is quite easy to eliminate strawberries from a meal plan but more difficult to remove staple food items such as milk, eggs or wheat which are found in a variety of food products.
Some infants cannot tolerate cow's milk or cow's milk formulas. In these cases goat's milk or special formulas are often well tolerated.
Sometimes, the denatured protein will cease to act as an allergen. Therefore, a person sensitive to raw milk or lightly boiled eggs may be able to tolerate boiled milk or an egg that has been hard cooked for ten minutes.
(note: patients/residents may be able to tolerate eating egg yolk but not egg white. This is because the egg white contains most of the protein found in eggs.)
Substitution of other food items within the same food group may allow the individual to enjoy foods which are similar but not exactly the same as the one containing the allergen. For example, soy, potato, rice or rye flours may be substituted for wheat flour; soy milk formulas for regular cow's milk, etc. It is important to remember that an allergy to wheat includes an allergy to all parts of the wheat grain. Gluten free products may have the protein of the wheat removed but may still have the wheat starch.
The "Choices" fact sheet explains the differences between allergies and food intolerances.
Food Intolerances
Certain food intolerances result from underlying genetic abnormalities. Examples are lactose intolerance, celiac disease and sprue.
Lactose intolerance involves the inability to produce sufficient lactase , the enzyme required to digest the milk sugar called lactose. Any undigested lactose remains in the small intestine and is acted upon by intestinal bacteria. This results in bloating, diarrhea, gas and abdominal cramps.
Lactase deficiencies include a primary deficiency of the enzyme lactase or a secondary lactase deficiency as a result of gastrointestinal disorders. Infants have a high level of lactase, however the levels of lactase and its' activity declines with age. Primary lactase deficiency is common in among people of Asian, South American and African descent. Secondary lactase deficiency may occur with malabsorption syndromes, infections of the GI tract and in inflammatory bowel disease. In both primary and secondary lactase deficiency the ingested lactose is not metabolized to glucose and galactose but remains intact in the gastrointestinal tract. The lactose in the GI tract draws water into the intestinal tract, and as well bacteria start to ferment the lactose and lactic acid, Hydrogen gas and carbon dioxide are produced. These two actions result in the symptoms of cramps, diarrhea, bloating and flatulence.
2013 Canadian Healthcare Association. All rights reserved.
96
FSNM Yr 2 Se 2 Unit 7
A restricted lactose diet is used for patients/residents with lactose deficiencies. The diet includes the removal of milk and milk products and the use of lactose free commercial items such as Lacteeze and Lactaid.
Most individuals with lactose intolerance can digest small quantities of lactose at any one time.
Tolerance to lactose must be individually determined by first following the restricted lactose recommendations. If symptom free, foods containing small amounts of lactose may be added gradually until the level of tolerance is reached.
2013 Canadian Healthcare Association. All rights reserved.
97
FSNM Yr 2 Se 2 Unit 7
Celiac Disease
Gluten-free diets are provided for those persons who have intolerance to gluten. Gluten is a protein found in the cereal grains of wheat, rye, barley, oats and triticale.
The presence of gluten in the diet of sensitive individuals causes decreased absorption of sugars, fats and amino acids. The stools are foul smelling and foamy due to fermentation of undigested carbohydrates. Untreated persons show signs of malnutrition such as: weight loss, stunting growth in children, muscle wasting, bone pain, sore mouth.
Celiac disease is the name given this gluten intolerance if it occurs in children and nontropical sprue , if it occurs in adults.
Along with your textbook, The Canadian Celiac Society website provides a description of the disease and details of the diet. The Dietitians@Work client education handout provides more details about gluten-free diets, sources of gluten and acceptable as well as questionable foods for celiacs.
Metabolic Stress, Infections, Trauma, & Surgery
When people suffer a major trauma whether from an accident, burn, major infection or surgery, there is a metabolic response to the injury. This response results in metabolic alterations which begin when the trauma occurs and changing metabolic responses continue until the healing is complete. In the initial stages after injury, shock with a decreased metabolic rate, diminished perfusion of the body tissues with oxygen, decreased blood pressure and a decreased body temperature occurs. After the initial response is treated by fluid replacement and the restoration of the transportation of oxygen to the body tissues, the body enters a catabolic phase. The metabolic rate is increased, oxygen uptake by the tissues is increased and there is an increased excretion of nitrogen. To further complicate the nutritional status, there is an impaired utilization of energy from carbohydrate, protein and fat. As recovery and healing occur the adaptive response begins and the body enters an anabolic phase. The metabolic rate diminishes and the body is able to restore and repair tissues. Optimal recovery is dependent on adequate nutrient intake.
The care of the surgical patient will evolve around two periods. The preoperative period is one in which the nutritional status of the patient needs to be maintained or enhanced. Nutrition screening preoperatively for elective admissions will detect individuals at high risk for malnutrition and provide for early intervention.
Good nutritional status before and after surgery is associated with effective wound healing, fewer infections, shorter hospital stays and decreased complications.
2013 Canadian Healthcare Association. All rights reserved.
98
FSNM Yr 2 Se 2 Unit 7
Preoperative Nutrition -Maintaining nutrient reserves
The incidence of protein-energy malnutrition in hospitalized patients is well known. The causes of this may be related to the illness or to treatments. In surgery there is protein loss through the loss of blood as well as from the damage to the body tissues. A diet with optimal protein intake will ensure that protein reserves in the tissues and blood plasma are adequate to meet the needs in the post-operative period.
In addition enough energy must be included in the diet to spare the protein in the diet for tissue maintenance and repair. Underweight individuals need to increase their weight to as close as possible to their ideal body weight with an increase in lean body mass. Oral nutrition is the preferred method of enhanced nutritional support. Overweight individuals may be advised to lose weight prior to certain types of surgery to minimize the surgical risks. Such weight loss must not be at the expense of the nutritional status of the individual.
During the preoperative phase an optimal vitamin and mineral status should be maintained.
Fluid and electrolyte balance is also important.
The immediate pre-op orders will usually require that a patient is NPO for at least eight hours to prevent vomiting and aspiration of food particulates after an anesthetic. Food within the stomach may increase the risk of the development of postoperative gastric retention and expansion.
Abdominal surgery will require that the colon is free of residue to reduce the presence of colon bacteria and to help prevent infections after the surgery.
Postoperative Nutrition Care - Restoring nutritional status
In the immediate post-operative period the patient will be NPO until they are fully conscious and it is determined that the gut is functional. The patient will usually begin with a clear fluid diet and progress to full fluids and then to diet as tolerated.
Protein is required after any surgery to replace the protein lost during the surgical procedure and to allow for tissue healing. After major surgery, the body enters a phase of catabolism and a negative nitrogen balance of up to 20 g/day may occur. This represents a loss of tissue protein of 1 lb. per day. The loss of protein also comes from various body losses or exudates.
The patient requires protein for wound healing which requires the formation of large amounts of new body tissue. For this to occur, adequate amounts of all the essential amino acids as well as the non-essential amino acids must be present.
In order to prevent shock there must be an adequate amount of the blood plasma proteins and in particular, albumin . If the plasma proteins drop, fluid leaks from the blood capillaries and the blood volume drops. The result is shock, which can be life threatening. The fluid, which leaked form the capillaries, enters the cells of the body and edema or swelling of the tissues occurs.
Edema can have serious effects on the heart and respiratory systems.
2013 Canadian Healthcare Association. All rights reserved.
99
FSNM Yr 2 Se 2 Unit 7
Protein is also required to resist infection. Protein is a major component of the body's immune system in the form of lymphocytes (white blood cells), and antibodies. Proteins carry fats to the tissues for wound healing. Fats form the center of cell walls and have other important functions in other necessary metabolic activities.
An adequate energy intake is necessary to ensure that protein is spared for tissue healing. The provision of adequate carbohydrate calories is essential to spare the protein for tissue building and repair.
There are several types of surgery involving the gastrointestinal tract, which require specific dietary adjustments.
Gastric Surgery
Gastrectomy
A gastrectomy is the surgical removal of part or all of the stomach. Some individuals experience what is known as dumping syndrome following a gastrectomy. Since the reservoir capacity of the stomach is diminished, the partially digested food may be dumped into the jejunum. This rapid deposit of large amounts of food in a short period results in a solution in the jejunum which is hypertonic. Through osmosis, fluid is drawn through the wall of the intestine.
Due to the large amount of fluid required to dilute the intestinal contents the circulating blood volume is decreased. The result is the patient/resident experiences a rapid heart rate, weakness, sweating, early satiety, cramps, diarrhea, nausea and vomiting. The individual becomes reluctant to eat and presents a picture of a typically malnourished person.
A post gastrectomy diet is ordered after gastric surgery has been performed and/or if dumping syndrome (nausea, weakness and perhaps diarrhea after ingestion of food) is experienced. The textbook provides a good description of the dumping syndrome, as well as nutritional care and diet plans for both dumping syndrome and post-gastric surgeries.
Colostomies and Ileostomies
If the colon is removed, an opening into the abdominal wall is made from either the ileum - the first section of the large intestine ( ileostomy ) or further along the large intestine
( colonostomy ). An appliance to contain the discharge must be worn. Coping with any "ostomy" is difficult and patients need support and practical help in learning about self-care. There are local chapters of the United Ostomy Association, which provide this support. Refer to the diet manual for the specific nutrition management of colostomies and ileostomies.
Gastroplasty
2013 Canadian Healthcare Association. All rights reserved.
100
FSNM Yr 2 Se 2 Unit 7
Gastroplasty (gastric stapling) and gastric bypass are surgical procedures used for persons with severe obesity. The principal surgery procedure is to reduce the space for food in the stomach and limit appetite and eating. Figure 3 is a summary of the diets for the various gastrointestinal disorders.
Figure 3
Disorder
Comparison of diets for gi disorders
Diet Highlights
Ulcers - duodenal
- peptic
Gastritis
Gastroesophageal Reflux Encourage weight loss/control.
Encourage low fat snacks.
Avoid coffee, tea, cola drinks, chocolate.
Avoid alcohol and smoking.
Do not lie down for 2 to 3 hours after eating.
Inflammatory Bowel Disease Small frequent feedings
- Crohn's Disease
- Ulcerative Colitis
Avoid snacking, especially at bedtime.
Avoid coffee, tea, cola drinks, chocolate.
Avoid alcohol and smoking.
Encourage high fibre foods.
Adequate calorie intake to maintain weight.
Increase protein to 1.5 g/kg body weight.
Fat restriction if steatorrhoea occurs in Crohn's Disease.
Encourage well balanced diet with normal fibre content (15-20 g/day).
Multivitamin supplementation may be required.
Irritable Bowel Syndrome
Diverticulitis
Encourage well balanced diet with normal to higher fibre content
(20 g/day).
Avoid coffee, tea, cola drinks and alcohol.
Encourage adequate fluid intake.
In acute stage, clear fluid diet to give bowel a rest.
Encourage well balanced diet with normal to higher fibre content
(20-25 g/day).
2013 Canadian Healthcare Association. All rights reserved.
101
FSNM Yr 2 Se 2
Encourage adequate fluid intake.
Unit 7
Gastric Surgery Progress from clear fluid diet to full fluid diet to light or soft foods.
Reduce carbohydrate content, particularly simple sugars.
Increase protein and fat content to meet the calorie needs.
Encourage small frequent meals.
Separate solids from liquids so that liquids are consumed 30 minutes before or after meals.
Multivitamin supplementation may be required.
- dumping syndrome Limit simple sugars.
- steatorrhoea
- colostomy
- ileostomy
Restrict fat and/or lactose.
Chew foods well to prevent blockage.
Adequate fluid intake with electrolytes.
2013 Canadian Healthcare Association. All rights reserved.
102
FSNM Yr 2 Se 2 Unit 7
Nutrition Support
During acute or chronic illness many patients/residents will be unable to consume an adequate diet composed of solid foods and will require supplemental oral feedings or, in some cases, tube feeding to restore and maintain adequate nutrition.
There are two types of nutrition support or supplemental feeding available to your patients/residents:
enteral nutrition and
parenteral nutrition
In enteral nutrition, feeds are given orally or by tube. There are many commercial nutrition support products available on the market. These may be used as is or altered by the Nutrition and Food Services Department to adjust the protein, fat or carbohydrate content. In parenteral nutrition, sterile protein, fat, and carbohydrate solutions are administered directly into the blood through surgically inserted tubes in a central vein. These solutions are prepared by the pharmacy department.
Nutritional Products for Oral Supplementation
Oral Supplements
Oral supplements may be used for a patient/resident who needs extra energy and/or protein.
They are often administered as a beverage between meals but can also be used as a meal replacement. Oral nutritional supplements are very similar in consistency to blenderized milkshakes but contain added nutrients and are administered to patients/residents who have digestive capability but will not or cannot eat.
Oral nutritional supplements can be flavoured and are best served cold. Individual taste preference plays an important role in the acceptance of these products. These are therapeutic foods and not just milkshakes! The products are often more readily accepted by patients/residents if they understand that the supplement is part of their treatment and if health care staff show a positive attitude toward the supplement when administering them.
There are numerous brands and flavours of supplements commercially available. Your facility may stock several flavours and/or types of supplements (i.e. some are more like the consistency of a milkshake while others are thinner in consistency and fruitier in taste). If patients/residents can find a supplement they enjoy, their acceptance and intake of the product may increase.
2013 Canadian Healthcare Association. All rights reserved.
103
FSNM Yr 2 Se 2 Unit 7
When deciding on the types of oral supplements a facility will stock, there are numerous factors to consider. The density of the nutrients supplied should be compared to the cost of the product, the texture or form of the supplement (supplements may be available in the form of a cookie, drink, pudding or soup), taste preferences of your patients or residents, and the ability of a particular group of residents to tolerate the ingredients of the supplement. For example a patient population of elderly residents may be intolerant to the lactose in some supplements, patients with dysphagia may tolerate a pudding better and cancer patients may prefer a supplement which is not too sweet.
At a volume of 1500 mL, most supplements are nutritionally complete. They can be given orally or by tube to the patient/resident unable to ingest by mouth, but who has a fully functional digestive system. The nutrients in these feedings are available in a form that requires digestion.
They contain intact proteins which must be broken down before they can be digested and absorbed.
Some products for tube feeding are designed for that specific purpose and they may not have an appetizing taste. For these products feeding by tube is preferable, although some patients who are highly motivated to avoid a tube may take them orally.
Elemental Feedings or Chemically Defined Formulas
Elemental diets provide a nutritionally complete liquid diet for the individual with a nonfunctioning digestive system.
The nutrients provided require minimal digestion (for example, protein is available in the form of individual amino acids). The diet is therefore pre-digested and leaves little or no residue in the bowel.
Elemental feedings promote optimal nitrogen retention. This is important for malnourished individuals who are in a state of negative nitrogen balance. In addition, there is no substantial secretion of digestive enzymes with elemental feedings. This helps rest organs involved in diseased states (e.g. most chemically defined formulas are low in lactose and residue).
Problems with elemental diets may occur because of their high osmolality. Osmolality is the osmotic pressure of a solution. It is expressed as osmols and is the quantity of a substance in solution, i.e., molecules, ions or both .The higher the osmolality the greater the movement of fluid across a semipermeable membrane. The intestinal wall is a semipermeable membrane.
"The osmolarity of elemental diets depends upon the formulation, dilution and flavouring....
Osmolarity is important in relation to diet administration. Tolerance of diet therapy depends to a large extent on osmolarity, especially the osmolar load delivered per unit of time. The osmolarity depends upon the carbohydrate and nitrogen sources. Diets containing more and smaller molecules have higher osmolalities."
10
2013 Canadian Healthcare Association. All rights reserved.
104
FSNM Yr 2 Se 2 Unit 7
Enteral Nutrition Support
Nutrition support is an integral part of medical therapy and must be implemented if patients are to receive maximum benefit from their medical therapy.
11
Many think of nutrition support as enteral or parenteral nutrition; however, it can range from the addition of a snack to a patient's meal pattern to the more complex modalities of enteral nutrition (EN) or Total Parenteral
Nutrition (TPN). Upon admission to any healthcare facility a nutrition screening will reveal those individuals who require nutrition intervention. The following diagram will help to show the decision-making tree involved in such screening.
Admission to Healthcare Facility
Screening
Chart Review- height, weight, physical exam, diagnoses or problems, laboratory data, medications, vital signs, diet order
Patient Interview- usual weight, weight changes and patterns, previous diets, allergies and food intolerances and diet history
Nutritional Deficits
High Risk
Assess Nutritional Needs
Nutritional Care Plan
Implemented
Moderate Risk
Assess Nutritional Needs
Nutritional Care Plan
Implemented
No Nutritional Deficits
Low Risk
No further screening unless there is a change in status or the individual exceeds the expected length of stay
Monitor
Reassess
Monitor
Reassess
2013 Canadian Healthcare Association. All rights reserved.
105
FSNM Yr 2 Se 2 Unit 7
Redefine Risk Category
Possible referral to
Nutritional Support Team
Redefine Risk Category
Some factors which will determine whether a person is at high or moderate risk:
Weight Loss- A weight loss of 5 % in less than one month or weight loss of 10% or more in 6 months are indicators of high nutritional risk; however a weight loss that is planned will need to be evaluated as it in fact could be a positive factor in the health of the person.
Laboratory data is another factor to consider. Albumin levels of less than 30 g/l are indicative of high nutritional risk. Serum albumin is a good indicator for malnutrition with protein depletion. It indicates protein deficiencies which have occurred over a long period of time. Once albumin is synthesized in the body it remains stable for about 14-20 days before being broken down. Thus it will not be a good indicator for acute protein depletion. In considering the serum albumin levels, it is necessary to consider the hydration status of the individual as serum albumin levels rise in dehydration and fall when there is significant fluid overload.
The diagnosis of the individual is another aspect which should be considered in the nutritional assessment. Significant disease of kidney, liver, pancreas, gastrointestinal tract and neurosurgery are all associated with a high nutritional risk. These diseases may require a very specialized approach to the nutritional support and requires the skill of a clinical dietitian.
The ability of the individual to consume an adequate diet is also a factor which contributes to the nutritional risk. If physical or other barriers prevent a person from consuming an adequate diet, malnutrition will result.
If as a result of the nutritional assessment, it becomes evident that nutrition support is required the decision must be made concerning how the nutrition support will be provided. The choices for nutrition support vary from providing oral supplements to tube feedings to total parenteral nutrition. "The optimal method of support depends on the degree of stress, functional capacity of the gastrointestinal tract, the severity of pre-existing malnutrition and the risk of refeeding/feeding complications."
12
A common expression among nutrition support teams is "if the gut works use it".
2013 Canadian Healthcare Association. All rights reserved.
106
FSNM Yr 2 Se 2 Unit 7
The following diagram outlines the decision process in determining the route of nutrition support.
Yes
Ability to take orally
Functional Gut
No
Parenteral
Yes
Solid Food & supplements
No
Tube Feeding
Peripheral
Central
Monitor
Reassess
Monitor
Reassess
Once the decision relating to the form of the nutritional support is made, then the actual composition of the supplied nutrition must be determined. The first step is to determine the energy requirements of the individual. Energy requirements are affected by the activity of the person and the degree of illness. Various metabolic studies have determined a range of factors for various conditions.
2013 Canadian Healthcare Association. All rights reserved.
107
FSNM Yr 2 Se 2 Unit 7
Stress Factors for Adjusting Basal Energy Requirements
Condition
Post operative recovery with no complications
Fractures of long bones
Multiple trauma
Brain Injury
Stress Factor
1.00 - 1.05
1.25 - 1.30
1.30 - 1.55
Sedated, paralysed, drug induced coma
Non sedated, non paralysed
Peritonitis
0.90
1.40
1.05 - 1.25
Severe infection with sepsis
Cancer
1.30 - 1.55
1.10 - 1.45
Even with the hospitalized patient the activity factors must also be considered. The following table summarizes the suggested activity factors.
Activity Factors for Hospitalized Patients to adjust Basal Energy Requirements
Patient Status Activity Factor
Critically ill, on mechanical ventilation and/ or paralysed or heavily sedated
Bed rest or non ambulatory
1.0 - 1.1
1.1 - 1.2
Ambulatory 1.2 - 1.3
The total energy requirements are determined by multiplying the calculated basal energy requirements by the stress factor and by the activity factor. As there is a range in each of the categories, it requires considerable clinical judgement for the determination of total energy requirements. It is important to avoid over feeding the patient to avoid a very serious complication known as refeeding syndrome . Refeeding syndrome occurs because of metabolic imbalances and can lead to death.
2013 Canadian Healthcare Association. All rights reserved.
108
FSNM Yr 2 Se 2 Unit 7
Protein requirements also vary depending on the degree of illness or trauma. "Because all protein serves a vital cellular or enzymatic function and thus there are no protein reserves, preserving body protein mass and thereby supporting organ and body function during illness or injury is extremely important."
13
The range of protein requirements are from 1.0 g of protein per kilogram of body weight per day after an uncomplicated elective surgery to 2.0 - 2.5 g per kilogram of body weight per day for complicated conditions such as sepsis and brain injury.
The fluid requirement for patients who are confined to bed and are being enterally fed is usually calculated as 1 mL of free water for each calorie of energy intake. The water content of the formula should be considered in determining how much supplemental water is to be provided.
Selection of Tube Feeding Formula
There are many commercially prepared formulas on the market suitable for a tube feeding. In assessing which formula to select consideration is given to the osmolality, the viscosity or thickness of the formula in relation to the size of the tube to be used, the nutrient profile of the formula and the nutrition needs of the patient and the cost of the formula. The following table taken from Krause's Food, Nutrition & Diet Therapy is a concise review of the factors to consider.
Factors to Consider when Choosing a Feeding Formula
Integrity of the patient's gastrointestinal system.
The type of protein, fat, carbohydrate, and fiber in the formula as related to the patients' digestive and absorptive capacity.
Caloric and protein density of the formula (i.e. kcal/mL, g protein/ mL and kcal: nitrogen ratio.
Ability of the formula, taken in the amounts tolerated to meet the patient's nutritional requirements.
Sodium, potassium and phosphorus content of the formula, especially for patients with renal, hepatic, or cardiac dysfunction
Viscosity of the formula related to the type of tube-feeding equipment
Cost of the formula (i.e. per g protein, per kcal, per mL)
To prevent constipation, adequate water intake is required. There are fibre containing formulas which help in preventing both constipation and diarrhea. Diarrhea can also occur if the feeding rate is too rapid, the formula is hypertonic (the osmolality is too high), or the patient has an intolerance to lactose.
The major goal in the tube feeding of a patient is to prevent dehydration, starvation and subsequent fluid and electrolyte disturbances, especially when the tube feeding is for prolonged periods of time. Early detection and correction of dehydration is important because often, the patient/resident is not aware of their need for fluids (e.g. do not feel thirsty).
2013 Canadian Healthcare Association. All rights reserved.
109
FSNM Yr 2 Se 2 Unit 7
Tube Feeding Routes
There are three routes which can be used for tube feedings: nasogastric (or gavage feeding) the tube is inserted through the nose into the stomach. This is the most common type of tube feeding used for brief periods of time (e.g. for those who are unable to swallow or refuse to eat, premature infants with immature swallowing and gag reflexes, etc.).
The major complication with this type of tube feeding is aspiration . This occurs when the patient/resident inhales enteral feedings mucous or vomit into the respiratory tract where it enters the lungs and causes choking. gastrostomy where the tube is inserted through an artificial opening made through the abdominal wall into the stomach. The mouth and esophagus are bypassed and food can therefore be administered directly into the stomach. The tube is inserted surgically and can be used for short term, intermittent feeding or for continuous feeding on a long-term basis. jejunostomy where the tube is inserted surgically through an artificial opening made through the abdominal wall into the jejunum (part of the small intestine). This type of feeding is for those who are unable to take food into their stomach. This facilitates postoperative feeding by bypassing the stomach and/or permits feeding in the presence of any problem occurring between the mouth and the site of tube insertion.
Formula Administration
Enteral nutrition formulas may be administered as, intermittent feeds or continuous feeds.
Intermittent feedings are quantities of 250 - 500 mL of the enteral product being administered several times a day over a time period of at least half an hour or longer. The number of feeds will depend on the quantity of formula required and the ability of the patient or resident to tolerate the volume at each feed. This method of feeding is often the choice when patients/residents are able to ambulate and allows them the freedom to enjoy normal activities.
In addition, the feeding is usually administered into the stomach and the stomach acts as a reservoir and delays the transit of the feeding into the small intestine. This helps to prevent diarrhea and bacteria growth in the stomach.
Continuous feedings are given at a slow rate over a period of 10 to 24 hours. In the acute care setting it is most common to have infusion pumps which control the precise quantity of formula dripped per minute. It is acceptable to use a gravity drip method as well. Because the feedings are given over a longer period of time a greater volume of feeding is able to be tolerated.
Occasionally a combination of continuous and intermittent feeds may be utilized. People with very high nutrient requirements who are able to ambulate and engage in normal daily activities may have intermittent feedings during the day and make up the volume of enteral feeds during the night with continuous feeds.
2013 Canadian Healthcare Association. All rights reserved.
110
FSNM Yr 2 Se 2 Unit 7
Once the decision has been made relating to the site of tube feeding, the method of administration and the type of enteral product, a protocol for the initiation of tube feeding must be recommended. In the past it was common to start isotonic feedings diluted with water at a low rate. This has several drawbacks as it delayed the patient receiving adequate calories and nutrients.
Now the most common practice is to start the enteral feedings (those with an energy concentration of 1.0- 1.1 calories per mL and a low osmolality) at a low volume such as 30-50 mL hour and to monitor the patient for tolerance and to increase the volume several times during a 24 hour period until the patient is able to tolerate the required volume.
Assessment
The assessment of the patient during the initiation of tube feeding center on the gastrointestinal tolerance of the feeding. Such parameters as the presence of bowel sounds, gastric distension, absence of vomiting and nausea are all used to evaluate the tolerance of the feed before it is increased in volume. In the clinical setting the determination of gastric residuals is done to assess the gastric motility and the rate of gastric emptying. The determination of gastric residuals is done by using a large syringe to draw out the contents of the stomach and to measure the volume. The contents of the syringe are then returned to the stomach as it contains significant amounts of potassium and other necessary gastric juices.
A large residual of 200- 300 mL would indicate that the patient has delayed gastric emptying and the feeding should be reduced or stopped until the gastric residuals normalize. The volume and consistency of bowel movements is also evaluated daily.
The longer term evaluation of the tube fed patient includes the evaluation of gastrointestinal tolerance but also includes the assessment of the nutritional and hydration status of the patient.
In acute care the assessment of electrolyte status may be done on a daily basis until it is known that the patient will tolerate the feeding.
Patients who are nutritionally stable may be transferred to a long term care facility or if they are capable to a home care program. The frequency of the evaluation of their nutritional status will be determined on a case by case basis, but it should be a regular part of the health care of the person.
Complications of Enteral Nutrition Support
The complications associated with enteral nutrition support may be related to the physical capability of the delivery of the solution or gastrointestinal and other physiological changes in the patient. The most common complication is the blockage of the feeding tube. Since smaller tubes cause less irritation for the patient, smaller tubes are most often utilized. The most common cause of blocked tubes is the administration of medications through the tube.
2013 Canadian Healthcare Association. All rights reserved.
111
FSNM Yr 2 Se 2 Unit 7
Aspiration is another complication which may occur. The placement of a feeding tube into the stomach affects the lower esophageal sphincter and allows gastroesophageal reflux. In addition, high gastric residuals may also cause aspiration. The aspiration of the stomach contents into the lungs may result in pneumonia. Aspiration may also be caused if the feeding tube is incorrectly placed and allows the enteral formula to enter the lungs. To prevent aspiration, the head of the bed should be elevated 30 - 45º during the feeding and for between one half to one hour after feeding, gastric residuals should be checked regularly and each time the feeding tube is placed, the placement should be checked by an x-ray.
Diarrhea may occur as a result of tube feeding. There are, however, many other causes of diarrhea the most common of which is the administration of medications via the feeding tube. In addition, the use of antibiotics may contribute to the incidence of diarrhea. Commercial enteral feeding solutions, which are unopened, are sterile. Once the feeding is opened and poured into the bag for administration of the feed, bacterial growth can begin. It is important that the feeding bags and tubing are changed frequently. In acute care settings it is common for these to be changed every 24 hours.
Support Team
Enteral nutrition support requires the skill and expertise of the health care team. It is common to have a physician skilled in nutrition support, the dietitian and the nursing care team all participate in the decision making concerning the initiation and monitoring of the patient when they are acutely ill. The food service and nutrition manager may be involved in the care of the patient once they are stable and tolerating the feeding well. Whenever there is a change in the health of the patient or complications relating to the tube feeding occur, a reassessment of the patient by persons with greater skill in the area of nutrition support should be initiated. In a long term care facility, which does not have the services of a dietitian on a full time basis, the physician or the nursing team leader may be the person to consult with the nutrition support team.
Formula Available
There are many commercial products available for enteral nutrition support. Most companies, which manufacture enteral products, will have a full line of products available to choose from.
The standard enteral products are usually 1.0- 1.2 cal/ mL and are of low osmolality of between 300-500 mOsm/kg. They are usually lactose free. An example of a standard product is Isocal.
2013 Canadian Healthcare Association. All rights reserved.
112
FSNM Yr 2 Se 2 Unit 7
Fiber containing products are for long term feeding with a fully functional GI tract.
These formula contain soy polysaccharides and provide approximately 15 g of fiber per liter of formula. These are usually lactose free and contain 1.0- 1.2 cal/mL. Jevity is one example of a fiber containing product.
Energy dense products are designed to provide between 1.5- 2.0 cal/mL and may be used when there is an unusually high energy requirement of in cases when fluid must be restricted. An example would be Nutren.
High Nitrogen products are designed for conditions requiring very high protein content.
The protein content is approximately 17 % of the kcal. Ensure Plus HN is a high nitrogen product.
Defined products are for individuals with a compromised GI tract who are unable to digest and absorb intact proteins. The nutrients are partly hydrolysed to aid in absorption. An example of a defined product is Peptamen.
Elemental products are also for individuals with a compromised GI tract. In an elemental formula the protein is in the form of free amino acids, the carbohydrate is in the form of malto dextrin and modified starch. These products are usually very low in fat. They are high in osmolality. Vivonex is an elemental product.
Specialized products are designed for specific conditions such as diabetes, pulmonary disease or for specific organ dysfunction. These products are very expensive. An example of such a product is Glucerna.
Modular Formulas can be assembled in various proportions depending on the patient/residents nutrition requirements. Protein, fat, carbohydrate, electrolytes and vitamins/micronutrients are available in separate forms. These can be added together to form a new formula or added on an individual basis to an existing formula.
Medium chain triglycerides bypass the portal system and are absorbed directly into the lymphatic system. They are used for individuals who do not efficiently digest and absorb conventional long chain fatty acids. MCT oil is available and may also be added to other food products.
2013 Canadian Healthcare Association. All rights reserved.
113
FSNM Yr 2 Se 2 Unit 7
Long chain glucose polymers such as Polycose or Caloreen are available to add extra energy to products without increasing the sweetness of the product. The foods/liquids should not be baked or boiled as this will break the long chains and cause an increase in sweet taste.
Protein powder, Promod, Promix or skim milk powder may be added to increase the protein content of the food or beverage.
Supplemental and tube feeding are sometimes considered "formula" diets in textbooks. TPN is the name for central parenteral nutrition where feeding by the digestive system is not at all possible and TPN solutions are administered through a vein. This requires sophisticated management of the nutritional and medical care of the patient and requires individuals with specialized training to assess the patient and prescribe the formula.
2013 Canadian Healthcare Association. All rights reserved.
114
FSNM Yr 2 Se 2 Unit 7
Conclusion
"Many dietary recommendations have been made for the management of gastrointestinal diseases. Any proposed dietary modifications should take into consideration the possible effects of ingested food upon: 1) the secretory activity of the stomach, small intestine, pancreas, liver and gallbladder; 2) motility of the gut; 3) the bacterial flora; 4) the comfort and ease of digestion and 5) the maintenance and repair of the mucosal structures."
14
When patients/residents are unable to consume an adequate diet, supplemental and/or tube feedings may be prescribed. It is generally accepted that if the G.I. tract is functioning, it should be used.
Various diet adjustments for gastrointestinal problems have been mentioned in this unit. It is important to remember this information should be used as reference when dealing with persons with these disorders. Hospitals may have specific diets that vary from these references. As well, each p erson’s intestinal tract differs and his or her tolerance level for different foods will vary. It is especially important to individualize diets for persons with gastrointestinal disease.
2013 Canadian Healthcare Association. All rights reserved.
115
FSNM Yr 2 Se 2 Unit 7
Endnotes
1
Almy, T.P. et al. (1985). Prevalence and significance of digestive disease. Gastroenterology .
68, p.1351.
2
Burrows, E. (1984). The digestive system. Chatelaine , 38.
3
Williams, S.R. (1992), Basic Nutrition and Diet Therapy, 9 th. ed ., St. Louis, Miss, p. 272
4
American Dietetic Association. (2000). Dietitians of Canada, Manual of Clinical Dietetics , 6th ed., Chicago, Illinois, p. 421
5
Greenwood, J.K. (1992). The IBD Nutrition Book . New York, NY: John Wiley & Sons Inc., p xiii
6
Greenwood, J.K. (1992). The IBD Nutrition Book . New York, NY: John Wiley & Sons Inc., p 64
7
Mahan, K.L. and Escott-Stump, S. (1996). Krause's Food Nutrition and Diet Therapy . 9th. ed.
Philadelphia, Penn., p. 632.
8
Robinson, C.H., Weigley, E.S. and Mueller, D.H. (1993). Basic Nutrition and Diet Therapy .
New York, NY: MacMillan Publishing Co., p.369.
9
Robinson, C.H., Weigley, E.S. and Mueller, D.H.(1993) Basic Nutrition and Diet Therapy . New
York, NY: MacMillan Publishing Co., p.361.
10
Russell, R (1981). Elemental Diets . Boca Raton, Florida: C.R.C. Press.
11
Grant, A. and DeHoog, S. (1985). Nutritional Assessment and Support , 3rd ed.
12
Ibid p.131
13
British Columbia Dietitians' and Nutritionists' Association. (1992). Estimating Energy, Protein and Fluid Requirements in the Manual of Nutritional Care , 4 th ed., p. 92
14
Robinson, C. and Lawler, M. (1982). Normal & Therapeutic Nutrition . New York. MacMillan
Publishing, p.522
2013 Canadian Healthcare Association. All rights reserved.
116
FSNM Yr 2 Se 2 Unit 7
Required Readings
Textbook(s)
DeBruyne, L.K., Pinna, E. & Whitney, E.N. (2012).
Nutrition and diet therapy (8th ed.).
Belmont, CA: Wadsworth/Thomson Learning.
Chapter 16 “Specialized Nutrition Support: Enteral and Parenteral Nutrition”, pp. 429-
455
Chapter 17 “Consistency-modified and other diets for upper GI tract disorders,” pp. 460-
483
Chapter 18 “Fibre-modified diets for lower gastrointestinal tract disorders”, pp. 484-
497
Chapter 19 “Carbohydrate and Fat-modified diets for malabsorption”, pp 502-520
Chapter 24 “Energy and Protein Modified Diets for metabolic and respiratory stress”, pp.619-
633
Readings from Course Reader
Canadian Food Inspection Agency – Fact Sheet: Labelling of Foods Causing Allergies and Sensitivities.
Pilon, Jody (2007). Natural Bowel Care. A Case Study From Espanola Nursing Home .
Long Term Care Magazine, September/October 2007, pp. 11-12.
Olynyk, Andrea (2008). To Supplement or Not to Supplement ? Long Term Care
Magazine, December 2008, pp. 37-38.
Dietitians of Canada – Client Education Handout series; Gluten-Free Diet; Gluten Free
Substitutions; Gluten-Free Diet by Food Groups.
Dietitians of Canada – Client Education Handout series; Diet to Control Heartburn; Highfibre diet; Sources of Fibre; High Fibre Recipes; Inflammatory Bowel Disease Diet.
Dietitians of Canada – Client Education Handout series; Diet for Ileostomy; Food Tips for
Ileostomy; Low-lactose diet; Lactose Content of Common Foods and Beverages; Low-
Fat Diet.
2013 Canadian Healthcare Association. All rights reserved.
117
FSNM Yr 2 Se 2 Unit 7
Internet readings:
Health Canada has developed a web page with information about food allergies and links to the new Government of Canada brochures with information on each of the nine priority food allergens in Canada. This information can be found at the following address: http://www.hc-sc.gc.ca/fn-an/securit/allerg/index-eng.php
Canadian Celiac Association. Disease and Diet section of the website: http://www.celiac.ca
Crohn’s & Colitis Foundation of Canada website at http://www.ccfc.ca/site/c.ajIRK4NLLhJ0E/b.6319851/k.BDBF/Home.htm
Website: Gastrointestinal Society; Canadian society of Intestinal Research: www.badgut.org
2013 Canadian Healthcare Association. All rights reserved.
118
FSNM Yr 2 Se 2
Unit 7 Assignment located on the Gateway
To complete the Unit 7 assignment, please access your account on the Gateway at www.cha.ca. The assignment is available in Word format on the Gateway for you to download. Once completed, please upload your assignment into the designated location.
Unit 8
2013 Canadian Healthcare Association. All rights reserved.
119
FSNM Yr 2 Se 2 Unit 8
Food Services and Nutrition Management
Year Two Semester Two
Unit 8: Nutrition Therapy III- Nutritional
Management of Heart Disease, Renal and
Gallbladder Disorders and Pancreatitis
2013 Canadian Healthcare Association. All rights reserved.
120
FSNM Yr 2 Se 2 Unit 8
Nutrition Therapy III- Nutritional Management of Heart
Disease, Renal and Gallbladder Disorders and
Pancreatitis
Objectives
Upon completion of this unit, the learner will:
Understand the symptoms, causes and types of heart disease and the role of nutritional management in treating this disorder;
Summarize the stepwise dietary approach to lowering lipids;
Given a calculated dietary pattern be able to plan menus for reduced energy, fat and cholesterol intake;
Explain methods to reduce the lipid content of food;
Plan diet patterns and sample menus for reduced sodium intake;
Identify foods that are high in sodium content and recommend methods to reduce the sodium content of food;
Name the major structural units of the kidney and explain the functions of the kidney;
List and describe the common diseases of the kidney;
Describe the implications of renal disorders and the importance of the nutritional management of each type of kidney disease;
Given a calculated meal pattern, plan and adjust menus to be suitable for patients with renal disease;
Know the types of nutritional management required for patients/residents with liver, gallbladder or pancreatic disorders.
Introduction to Nutritional Management III
"The 20th century man has become more reluctant to accept deterioration of coronary arteries and subsequent development of atherosclerosis as a necessary accompaniment of the aging process or of his personal being or so called constitution. In a search for associated factors from his mode of life, diet has become one of the focal points of inquiry.
Gradually, the question has become, not whether diet can be associated with coronary heart disease, but to what extent diet influences the development of coronary heart disease in man."
1
"The important function of the kidneys is to maintain the normal composition and volume of the blood. They accomplish this by the excretion of nitrogenous and other metabolic wastes, by regulation of electrolyte and fluid excretion so that water balance is maintained, by making the
2013 Canadian Healthcare Association. All rights reserved.
121
FSNM Yr 2 Se 2 Unit 8 final adjustment of acid base balance, and by the synthesis of enzymes and other substances that influence metabolic activities."
2
In other words the kidneys play a major role in ensuring that the internal environment remains balanced and stable.
The liver performs many functions that influence one's nutritional state. Diseases of this large and complex organ dramatically affect a patient's/resident's health.
The incidence of gallbladder disease increases with age and obesity. Certain G.I. gastrointestinal orders and drug consumption also contributes to gallbladder disease.
Disorders of the pancreas usually involve inadequate enzyme production which leads to problems with digestion.
Liver Disease
"The liver has the most varied and extensive function of any organ and is one of the most important organs involved in the metabolism and storage of nutrients. It is a central regulatory site for most of the end-products of digestion that are absorbed across the intestinal mucosa into the portal circulation. In addition to dietary substrates, the liver receives endogenous substances such as free fatty acids and amino acids derived form other tissues and metabolic processes".
3
The biliary tract includes:
the liver (which produces bile),
the gallbladder (which stores bile) and
the hepatic and bile ducts (which secrete bile into the small intestine)
Bile is a fluid produced by the liver, concentrated and stored in the gall bladder and poured into the small intestine via the bile ducts when needed for digestion. One of the major roles of bile is in the emulsification, digestion and absorption of fats. Liver infection or disease, inflammation of the gallbladder or gallstones can disturb the flow of bile.
The liver is the largest and most complex organ in the body and is essential to life. The liver performs dozens of functions, many of which directly influence one's nutritional state such as:
secretion of bile (which aids in the digestion especially of dietary fats);
supply of glucose to the body;
conversion of excess sugar into fat;
conversion of sugars into glycogen (which can form glucose when necessary to maintain steady blood glucose levels). The liver can store up to 20 percent of its weight in glycogen;
2013 Canadian Healthcare Association. All rights reserved.
122
FSNM Yr 2 Se 2 Unit 8
conversion of protein and fat into glucose if required and excess sugar into fat (after which the fat is sent for storage into other parts of the body);
building (synthesis) of many essential proteins;
detoxification (reduction of the poisonous substances) of drugs, alcohol and environmental poisons. This is a protective function of the liver.
storing vitamins such as C, A, D, K and B complex, and minerals such as copper and iron (for release into the bloodstream when levels in blood fall too low). These liver reserves can last many months.
metabolizing alcohol. One litre of alcohol can be metabolized each day by the liver.
In liver disease protein, carbohydrate and fat metabolism are altered. A typical symptom of biliary tract disease is jaundice which is a yellow pigment of the skin and body tissues caused by the accumulation of bile (a yellow coloured fluid) pigments in the blood.
Hepatitis
The two major types of hepatitis (or inflammation of the liver) are:
drug induced hepatitis - due to alcoholism, use of certain drugs (such as heroin, hashish or marijuana), ingestion of poisonous substances or hypersensitivity to sulfa compounds or penicillin.
viral hepatitis - Type A (HAV) which is infectious and transmitted through fecal contamination of water or food. Poor sanitary procedures when parenteral nutrition is used enhances the likelihood of contracting viral hepatitis.
Type B (HBV) which creates more serious problems than Type A. Traditionally hepatitis
B was believed to be transmitted through contact with blood and blood products
(e.g. through blood transfusions, contaminated needles, etc.). It is now known that the virus can be transmitted via such body fluids as tears, saliva and semen.
In addition, there is a so called "vertical" transmission by which an infant is infected by its mother either during pregnancy or after birth.
Whereas HAV usually has been eliminated from the body by the time jaundice appears, the body is not always able to rid itself of HBV so easily. This virus can persist in body fluids for years or even a lifetime.
Through the work of the Nobel prize winner Baruch Blumberg and his colleagues, it is now known that there is a direct link between cancer of the liver and HBV.
Nutritional problems of hepatitis include:
loss of appetite
2013 Canadian Healthcare Association. All rights reserved.
123
FSNM Yr 2 Se 2
vomiting after meals
fever, headache and fatigue
abdominal discomfort
Unit 8
The objectives of dietary treatment in hepatitis is to aid the regeneration of the liver tissue and to prevent further liver damage. This can be accomplished by providing a nutritious diet and enticing the patient/resident to eat. Foods must be well prepared and attractively served with consideration given to the individual's food preferences.
During the acute states a liquid diet or one of soft consistency may be required with progression to a normal diet to include the following:
sufficient kilocalories to maintain or attain weight, to furnish the energy demands of tissue regeneration and to compensate for losses caused by fever.
sufficient dietary carbohydrate to ensure that enough glucose is provided to restore glycogen reserves and to meet the energy demands of the disease process.
adequate fat to make the food palatable. (Former regimens limiting the amount of fat on the basis of preventing fat accumulation in the diseased liver are no longer used.)
adequate protein to overcome negative nitrogen balance and promote tissue regeneration.
Small to moderate portions with between meal supplements are usually better tolerated than larger meals.
Cirrhosis
In cirrhosis, liver cells are gradually replaced by fibrous connective tissue. The liver becomes smaller and loses its ability to function properly (degenerates).
The most common cause of cirrhosis is chronic alcoholism in association with malnutrition. The onset of cirrhosis may be gradual with G.I. disturbances (e.g. anorexia, nausea, vomiting, pain and distension). As the disease progresses, jaundice and other serious changes occur (e.g. fat is not removed from the liver as it should be and accumulates, damaging the liver).
Nutritional management of cirrhosis includes:
sufficient protein to promote liver regeneration
dietary fat is restricted only if fat malabsorption is present.
vitamin and mineral supplementation (to replace those poorly absorbed or lost from vomiting, diarrhoea, etc.)
2013 Canadian Healthcare Association. All rights reserved.
124
FSNM Yr 2 Se 2
sodium restriction if edema (fluid retention) is present.
alcohol is eliminated.
Unit 8
When ammonia (a by-product of protein metabolism) is not removed from the body by the liver, it enters the circulation of the brain and can cause ammonia intoxication which can result in altered mental function in the patient/resident, with the eventual possible occurrence of hepatic coma . Nutritional treatment recommends a high calorie diet with at least .8g protein per kg body weight per day, but preferably 1.2-1.5g per kg body weight per day to ensure nitrogen balance.
Protein restriction, which was formerly believed to prevent encephalopathy or progression of liver dysfunctions can further malnourish the patient and is not recommended.
The patient's/resident's intake of non-protein food sources such as sugar, hard candies, butter and oil are encouraged to ensure adequate energy intake.
Biliary Tract Diseases and Pancreatitis
Biliary Tract Diseases include the formation of gallstones and /or an inflammation of the gallbladder.
The gallbladder is a pear shaped organ located below the liver. The gallbladder serves as a storage place for bile (a fluid which is required for the absorption and digestion of fat).
The reason why gallstones (hard, calcified substances) form in the gallbladder is unknown, although there has been some indication of a link between obesity and gallstone formation.
Complications occur when the gallstone travels through or blocks the bile duct causing severe pain.
Cholecystitis - inflammation of the gallbladder - is usually caused by gallstones. Other causes include typhoid fever or a malignant tumour blocking the biliary tract.
Characteristic symptoms of biliary tract disease are indigestion after eating accompanied by flatulence (gas) and nausea, vomiting and pain. The symptoms are more pronounced after a large meal or one which is high in fat.
Nutritional management includes spacing meals (so that large amounts of food are not consumed at one time) and use of a restricted fat diet as tolerated. In the case of asymptomatic cholelithiasis a restricted fat diet is usually of limited benefit.
In pancreatitis - inflammation of the pancreas - protein and fat are not digested or absorbed properly. Total parenteral nutrition is often used in cases of acute pancreatitis. As the condition improves oral feedings are resumed. If steatorrhea (fatty diarrhea due to malabsorption of fat) is present, a restricted fat diet can be of benefit although the primary treatment is the use of pancreatic enzymes.
The Nutritional Care Manual details specific diet modifications for liver disease.
2013 Canadian Healthcare Association. All rights reserved.
125
FSNM Yr 2 Se 2
Heart Disease
Unit 8
The heart is a pear shaped muscular organ about the size of your closed fist. The heart's job is to supply nutrients and oxygen contained in the blood to every organ and tissue of the body.
The heart pumps about 5-6 quarts (5-6 liters) of blood each minute and may increase its output to more than 20 quarts (20 liters) during exercise. Carrying out this work requires a continually available, adequate supply of energy to the heart muscle, which is provided by the nutrients and oxygen carried in the blood. Nutrients may be stored within the heart for later use but oxygen cannot be stored. The heart muscle therefore cannot tolerate interruption of its blood supply for long periods."
Students should review the functions and general anatomy of the cardiovascular system in a reference of their choice. Figure 1 shows a diagram of the major blood vessels in the body.
Cardiovascular disease refers to the many conditions or disorders of the heart and blood vessels (the circulatory system).
Coronary heart disease (CHD) is one form of cardiovascular disease. Coronary heart disease is the diminished flow of blood to the blood vessels surrounding the heart and providing oxygen to the heart muscle or myocardium. The most common cause of the decreased blood supply is the narrowing of the coronary arteries by fatty deposits called plaque.
The risk factors for Coronary Heart Disease were listed in Unit 5. Most experts agree that CHD is a multi factorial disease, and that individuals who exhibit more than one of the risk factors have a CHD risk that is much greater than the simple sum of the two factors (for example, smokers with a family history of heart disease).
Arteriosclerosis includes a variety of conditions which cause the artery walls to calcify, become thick and hard and to lose their elasticity. The most common type of arteriosclerosis is atherosclerosis , a disease in which the artery walls become clogged with fatty deposits, such as cholesterol. Atherosclerosis is a disease which takes many years for the slow progressive damage to the arteries to become evident and produce symptoms. Atherosclerosis can begin in childhood or early adulthood. When the blood flow to the myocardium is not sufficient for the demand for oxygen, the individual experiences a dull squeezing or crushing sensation in the chest known as angina .
A heart attack occurs when there is a complete blockage of one of the coronary arteries or a branch of a coronary artery and the complete lack of oxygen and nutrients to the cells of the heart muscle supplied by that coronary artery. Often the artery walls have already been damaged from the buildup of cholesterol deposits. The results are some of the cells of the myocardium being starved of oxygen and these cells die. The purpose of the immediate care of a person suffering from a heart attack is to prevent further damage to the heart muscle and to allow for scar tissue to form.
2013 Canadian Healthcare Association. All rights reserved.
126
FSNM Yr 2 Se 2 Unit 8
If blood vessels rupture in the brain or if a blood clot has cut off oxygen supplies and nutrients to the brain, a stroke is the result.
Nutritional management is required for most people that have coronary heart disease. The type of intervention will depend on the stage of development. When a person's blood lipid levels are found to be elevated, they may be counselled to restrict their overall fat intake or restrict cholesterol. If the person is overweight, they may need counselling on weight reduction. If the individual has to stop smoking, dietary monitoring may be necessary as smoking cessation sometimes leads to an increased food intake and weight gain.
2013 Canadian Healthcare Association. All rights reserved.
127
FSNM Yr 2 Se 2
Figure 1
Unit 8
2013 Canadian Healthcare Association. All rights reserved.
128
FSNM Yr 2 Se 2 Unit 8
Blood lipids include cholesterol, triglycerides and phospholipids. Cholesterol is a fat like substance found in all body cells. As discussed in Unit 2, cholesterol has many important functions in the body. We manufacture cholesterol in our bodies as well as obtain it from foods of animal origin. For the lipids to be transported in the blood they must be bound to a protein molecule. They are then called lipoproteins . The problem arises when there is an excess of cholesterol in the blood stream or an imbalance in the types of lipoproteins. Lipoproteins are classified by their density. Hyperlipoproteinemia is the term for elevated levels of these lipoproteins. The two most commonly discussed in relation to heart disease are the low density lipoprotein (LDL) and the high density lipoprotein (HDL) . The LDL is the transporter of cholesterol in the blood stream and if there is too much LDL-cholesterol in the blood stream, deposits of the cholesterol are left on the walls of the arteries. The HDL, on the other hand, carries cholesterol from the arteries and tissues to the liver where it can be eliminated.
Triglycerides are the form of fat which we see as the fat on a steak or the fat under the skin of poultry. There has been conflicting research on the risk of heart disease from elevated triglycerides; however, a high triglyceride level is often associated with a high total cholesterol and a high LDL-cholesterol and a low HDL-cholesterol level.
Individuals with a family history of cardiovascular disease, or with known abnormalities of blood lipids, or with multiple risk factors for cardiovascular disease should have a blood test to measure the levels of total cholesterol and LDL and HDL cholesterol. The following table gives
Canadian values for Blood Cholesterol Levels.
Figure 2
Blood Cholesterol Levels
Cholesterol Level
TOTAL BLOOD CHOLESTEROL
Below 5 mmol/L (200 mg/dl)
Between
Above
5 & 6 mmol/L
6 mmol/L
LDL CHOLESTEROL
Classification
Desirable
(200 -240 mg/dl) Borderline
(240 mg/dl) High Risk
Below 3.4 mmol/L
Between 3.4 & 4 mmol/L
Above 4 mmol/L
HDL CHOLESTEROL *
Below 1.0 mmol/L
(130 mg/dl) Desirable
(130-155 mg/dl) Borderline
(155 mg/dl) High Risk
(40 mg/dl) High Risk
2013 Canadian Healthcare Association. All rights reserved.
129
FSNM Yr 2 Se 2
Between 1.0 & 1.3 mmol/L (40-50 mg/dl) Borderline
Unit 8
Above 1.3 mmol/L (50 mg/dl) Desirable
Nutritional management of an elevated cholesterol level includes the following modifications:
a reduction in the total fat intake to 30% or less of total calories
a reduction of cholesterol from animal foods to 250 mg (6.4 mmol) or less per day
(which includes limiting egg yolk consumption to a maximum of 2 per week)
replacement of foods high in saturated fats with products high in polyunsaturated fats and monounsaturated fats
a reduction in energy intake if overweight
an increase in dietary fibre intake
In order to increase the levels of HDL the strategies are to lose weight, cessation of smoking and increasing aerobic exercise. Weight loss, exercise, reduced alcohol intake and good control of diabetes often lowers triglyceride levels.
Two diet plans referred to as Step I and Step II are used in the management of elevated cholesterol levels. The diet plans becomes increasingly restrictive in the amount of total fat, saturated fat, and cholesterol permitted.
2013 Canadian Healthcare Association. All rights reserved.
130
FSNM Yr 2 Se 2
Dietary Therapy for High Blood Cholesterol
Nurtient
Recommended Intake
Step 1 Diet Step II Diet
Unit 8
Total Fat
Saturated fatty acids
Polyunsaturated fatty acids
Monounsaturated fatty acids
30% of total calories
8-10% of total calories
Up to 10% of total calories
Up to 15% of total calories
< 7% of total calories
Carbohydrates
Protein
Cholesterol
Total Calories
55% or more of total calories
Approximately 15% of total calories
< 300 mg/dL < 200 mg/dL
To achieve and maintain desirable body weight
Source: Manual of Clinical Dietetics, 6th Edition, 2000, pp. 272
Dietary and lifestyle changes are the first methods of management of hyperlipoprotenemias. If the person does not respond to these methods various medications may be used to lower cholesterol and LDL-cholesterol levels while raising HDL-cholesterol. These medications are particularly useful in persons with inherited disorders of lipid metabolism.
As food service supervisors you do not need to know all of the symptoms and other medical data related to lipid abnormalities. However, you should be able to counsel a patient on a cholesterol lowering diet and be able to advise them on ways to prepare foods with reduced quantities of fat, cholesterol and saturated fat. It is recommended that you go to the website of the Heart and Stroke Foundation of Canada and review the information on Dietary Fat and
Cholesterol: http://www.heartandstroke.com/site/c.ikIQLcMWJtE/b.3484237/k.D734/Healthy_living__Dietary_ fats_oils_and__cholesterol.htm
.
Some supervisors need to be more knowledgeable in the area of nutrition and heart disease, especially if a large number of patients/residents in the health care facility are being treated for certain types of hyperlipoproteinemias.
The reduction of total fat in the diet is still the most important advice to give people. The two following short articles are from the Healthy Living/Healthy Eating section on Heart and Stroke
Foundation website http://ww2.heartandstroke.ca
. On the Heart and Stroke website, you have to first go to your province, and then look through the healthy eating and healthy living sections.
2013 Canadian Healthcare Association. All rights reserved.
131
FSNM Yr 2 Se 2
Separating fat from fiction
Unit 8
With so much conflicting nutritional information out there, planning a heart healthy diet can be confusing. To help you separate the truth about fat – and other dietary components – from fiction, two leading researchers give you the straight goods about heart healthy eating. Here’s what you need to know:
Fat
– the good, the bad and the ugly
Over the years, fat has developed a bad reputation. And, while it’s true that certain types of fat can contribute to obesity, atherosclerosis, heart disease and other health concerns, the reality is, not all fat is bad.
In fact, polyunsaturated and monounsaturated fats (The Good), found in vegetable oils, nuts and fish can actually reduce cholesterol levels. On the other hand, saturated fat (The Bad), found primarily in red meat and high-fat dairy products, raises cholesterol and along with it, heart disease risk.
But clearly, the most damaging kind of fat is trans fat (The Ugly). Frequently found in hard ma rgarines, baked goods and fried foods, these fats are particularly “ugly” because they actually raise bad cholesterol (LDL cholesterol) levels and lower levels of good cholesterol (HDL cholesterol).
“We have to be more concerned about the kind of fats we’re eating,” explains Dr. David Jenkins, professor and Canada Research Chair in Nutrition and Metabolism, department of nutritional sciences at the University of Toronto.
A big fat Greek diet
Several recent studies focusing on Mediterranean-style diets, which contain lots of olive oil, fish, vegetables, fruit and whole grains, show they can significantly reduce heart disease risk.
One study found that the traditional diet on the Greek island of Crete significantly reduced heart disease risk, even though fat made up 40% of the calories. In fact, subjects eating this type of diet had an even lower incidence of heart disease when compared to those consuming a traditional Japanese diet, where only 10% of calories come from fat and where the incidence of heart disease is already low. Researchers attribute this to the fact that the majority of fat in the Greek diet is monounsaturated.
4
The evidence to support consuming a Mediterranean diet is strong and getting stronger, says
Dr. David Spence, Heart and Stroke Foundation researcher and head of the Stroke Prevention and Atherosclerosis Research Centre in London, Ontario.
For instance, he says, one study from Lyon, France found that for patients with heart disease, a
Mediterranean diet reduced the risk of a second heart attack or stroke by 50% to 70% within
2013 Canadian Healthcare Association. All rights reserved.
132
FSNM Yr 2 Se 2 Unit 8 four years, while another from India found that for patients with, or at high risk of heart disease, a Mediterranean-style diet reduced their risk by 50% within two years.
5
Since heart disease is the leading cause of death in Canada, says Dr. Spence, all of us could reduce our risk if we consumed more fruit, vegetables, whole grains, fish, monounsaturated oil and nuts emphasized in the Mediterranean diet and outlined in Canada’s Food Guide to Healthy
Eating.
Nuts no longer taboo
There has been a complete reversal of the view on nuts, says Dr.
Jenkins. They used to be thought of as taboo because of their high fat content, but the truth is, the fat they contain is mainly monounsaturated
(The Good). Dry-roasted or raw nuts are best.
Some nuts, like almonds, are high in vegetable protein, and have been found to reduce coronary heart disease risk factors . Walnuts are a good source of omega-3 fatty acids, which also have heart-healthy benefits.
What’s more, people who eat nuts are actually less likely to be obese since eating them seems to significantly reduce the intake of other, less healthy, snack foods.
6
Refining the carbohydrate message
There is a widespread perception that carbohydrates are a healthier alternative to fat. But this is not necessarily the case. Refined carbohydrates such as white bread, rice and potatoes can cause a dramatic rise, and equally dramatic drop, in blood sugar levels which can lead to feelings of hunger, contribute to overeating and increase the risk of obesity, diabetes and heart disease. It is best, say the experts, to replace refined carbohydrates with their whole grain counterparts.
Vegetables and fruit – more is more!
A high intake of vegetables and fruit is a healthy choice, but one that many Canadians still haven’t bought in to. Research shows plant foods – including soy-based products such as tofu – not only protect against heart disease, they help lower blood pressure,
7
boost the immune system, guard against certain types of birth defects and are a vital source of many of the vitamins necessary for overall good health. Current recommendations call for five to 10 servings of vegetables and fruit per day. But, say the experts, when it comes to this food group, you can’t really overindulge!
2013 Canadian Healthcare Association. All rights reserved.
133
FSNM Yr 2 Se 2
How to slash the fat
Unit 8
A healthy diet contains between 20 and 35% of total daily calories from fat. For a woman this means about 45 - 75 grams of fat a day.
For a man this means about 60 - 105 grams of fat a day. But reducing the fat doesn’t mean you have to give up the flavour. Follow these tips to make sure you stay heart healthy for life!
Cut down on the amount of fats and oils you use in cooking. Use a non-stick pan and spray with vegetable oil.
Or use chicken or vegetable broth instead of oil, or a mixture of both.
Use flavourful oils in small amounts for the most taste per spoonful. For example, add a splash of sesame oil to your stir-fry.
If you’re cooking with cheese, mix a lower-fat version in with a stronger-tasting cheese.
Increase the amount of vegetables and decrease the amount of meat in stews and casseroles.
Always pour oil onto a teaspoon before adding to food to keep track of the amount.
Substitute applesauce, mashed banana and prune puree for the fat in many baked goods.
Replace some of the oil in salad dressings with seasoned rice vinegar, vegetable stock or even water.
Choose low-fat versions of fried foods such as baked tortilla and potato chips.
Sauté in water, vegetable stock, wine or dry sherry instead of fat.
Use fresh herbs, spices and other condiments to boost flavour and nutrition without adding any fat or calories. If you’re short on time, add some bottled condiments, such as chopped ginger, garlic, Dijon mustard, horseradish or a variety of vinegars.
Instead of frying foods try baking, barbecuing, broiling, braising, microwaving, poaching, roasting or stir-frying. Allow excess fat to drip off while foods are cooking.
Reference: http://www.heartandstroke.ca - 6/16/2006 2006 Heart and Stroke Foundation
Hypertension and Congestive Heart Failure
Congestive Heart Failure (CHF) is a condition which results from several types of heart problems including atherosclerotic heart disease and disease of the valves of the heart. In
2013 Canadian Healthcare Association. All rights reserved.
134
FSNM Yr 2 Se 2 Unit 8 congestive heart failure, the pumping action of the heart becomes lessened and the heart is not able to pump as large volumes of blood and a series of adjustments occur. As a result of these adaptations there is an abnormal accumulation of fluid. This fluid can accumulate in the lungs, the legs and body tissues. This accumulation of fluid is known as edema. The treatment of CHF includes a restriction in the sodium content of the diet and at times may include a fluid restriction. Patients may be on diuretics, some of which can cause potassium depletion.
Hypertension or high blood pressure is a symptom that acts as an indicator to signal that the risks are high for developing medical complications (e.g. heart attack, stroke, kidney or liver problems, etc.)
When the heart contracts the resulting pressure on the artery walls is called systolic pressure .
Systolic pressure is normally in the range of 110 140 (mm Hg). When the heart rests between beats the rate of pressure on the artery walls is referred to as diastolic pressure - normally in the range of 60 90 (mm Hg).
There is a misconception that those with high blood pressure are nervous, excitable, irritable, tense, etc. Hypertension is a medical problem. A contributing factor to high blood pressure may be long term dietary intake of sodium. The kidneys are able to excrete large amounts of excess sodium but kidney "overloading" over time may result in functional changes to this organ with the result that the kidney retains too much sodium. Along with sodium retention, water also accumulates in the body producing edema.
Sodium is an essential mineral that is required daily in small but nutritionally significant amounts. It is found naturally in most plants and animals that we use as foods. Salt contains sodium and chloride and it is the sodium not the chloride, that is a concern in hypertension.
Sodium is also found in many food additives. For example, sodium benzoate is used as a preservative in pickles and sodium alginate gives a smooth texture to ice cream and chocolate milk.
One third of the average sodium intake is from foods which naturally contain sodium (where sodium has not been added by man, such as meat, fish, poultry, eggs, cheese and milk).
Another third of our sodium consumption comes from salt added to foods during processing (to enhance flavour, for preservation etc.). The final third occurs when salt is added to foods by the consumer (e.g. using a salt shaker at the table or during the preparation process).
2013 Canadian Healthcare Association. All rights reserved.
135
FSNM Yr 2 Se 2
Figure 2
How to shake the salt habit
Unit 8
We all need some sodium in our diet to maintain good health. But eating too much may raise blood pressure and increase the risk of heart disease in some people.
Salt, sodium — what’s the difference?
Sodium is a mineral that is essential in our diet. The body requires a small amount of sodium to be healthy, but most people eat too much. Sodium is an ingredient in table salt, and is also found in additives and preservatives, such as monosodium glutamate (MSG).
Salt usually refers to common white table salt, which is a mixture of 40% sodium and 60% chloride. Table salt is also called sodium chloride.
How much is too much
According to the Institute of Medicine, the adequate intake (AI) for sodium is 1,500 mg per day.
This is the amount that our body requires for normal functioning. Most Canadians consume much more than this. The salt we shake onto our meals or add to our cooking accounts for only about 10% to 15% of the sodium we consume. An astounding 75% to 80% comes from eating processed foods. That’s because salt is added to almost all processed foods as a preservative and a flavour enhancer.
Salty dogs Strategies for losing your salty tooth
The following foods are particularly high in sodium, so they should be eaten in moderation. You can also look for “lower s odium” or “unsalted” versions:
Follow these strategies when you’re trying to reduce the amount of salt you eat.
Salty snacks like pretzels, chips and packaged popcorn.
Foods containing monosodium glutamate and other preservatives made from sodium.
Processed and packaged foods, including canned goods, frozen meals, processed meats (hot dogs, salami and luncheon meats, bacon, ham, corned beef), pickles and olives.
Do it gradually . It takes a couple of months for your taste buds to adjust. By cutting back a little at a time, you’ll hardly notice the change.
Use other flavourings . Cook at home more often, using enhancers such as flavoured vinegars, lemon and lime juice and zest, fresh garlic, ginger and herbs, chipotle peppers, black pepper and other spices.
Read labels . Prepackaged foods list the sodium content in the Nutrition Facts panel.
Remember to adjust that amount if you eat more than the stated serving size.
Condiments such as barbecue sauce, ketchup, mustard, gravies and salad
Eat in more often . Foods prepared in restaurants are often high in salt. By cooking more meals yourself, you can control the
2013 Canadian Healthcare Association. All rights reserved.
136
FSNM Yr 2 Se 2 dressings.
Unit 8 ingredients that you choose and the amount of salt that you add.
Instead of this highsodium food…
Soups made with bouillon cubes or canned stock
Processed cheddar cheese, parmesan or feta
Sea salt, rock salt, kosher salt or table salt
Caesar, Greek or taco salad
Choose this lowersodium option…
Soups made with low-sodium bouillon cubes or home-made stock
Mozzarella or Swiss
Garlic powder or spice mixes
Ketchup, mustard or mayonnaise on sandwiches or burgers
Regular butter or margarine
Fruit, mixed green or spinach salad
Tomato, cucumber or lettuce on sandwiches or burgers
Becel Salt Free margarine
There is enough sodium which occurs naturally in foods to supply our individual daily needs for sodium.
It is generally accepted that hypertensive individuals can benefit from a dietary increase in vegetables, fruits, fiber, and non-fat dairy, as well as a reduction in sodium.
Recommendation for treatment and Prevention of Hypertension
Reduce sodium to 2400mg/day (100mmol) or less.
Your textbook (Table 22-5 p. 584) introduces you to the DASH diet. The DASH eating plan was the test diet used in a study called Dietary Approaches to Stop Hypertension.
The DASH diet recommends:
Eat lots of vegetables & fruit (potassium),
Add low-fat milk products (calcium),
Beans and nuts (magnesium).
Lower fat and sugar
2013 Canadian Healthcare Association. All rights reserved.
137
FSNM Yr 2 Se 2
Other:
Weight loss of 5-10% of current wt. if overweight.
Increase exercise.
Limit alcohol.
Unit 8
2013 Canadian Healthcare Association. All rights reserved.
138
FSNM Yr 2 Se 2 Unit 8
A routine diet provided by a health care facility usually provides 3 - 5 grams of sodium a day
(130 mmol - 270 mmol). This general diet is then modified to four different levels for those on sodium restricted diets:
Weights & Measures no added salt (NAS)
-
-
(3g or 130 mmol sodium)
omit excessively salty foods mild sodium restriction
-
-
little or no salt is added at the table or in cooking
use all salt free foods except bread, butter and margarine
(2 g or 87 mmol sodium)
most common level ordered
There are two main methods of describing concentrations: by weight, and by molecular count. Weights are in grams, molecular counts in moles. (If you really want to know, a mole is 6.022*10^23 molecules.) In both cases, the unit is usually modified by milli- or micro- or other prefix, and is always "per" some volume, often a liter. This means that the conversion factor depends on the molecular weight of the substance in question.
some foods should be eaten in limited amounts because of the natural sodium they contain (e.g. 500 mL milk, meat, etc.)
omit excessively salty foods
Conversion factors for minerals:
potassium, mg ÷ 39 = mmol;
magnesium, mg ÷ 24 = mmol;
calcium, mg ÷ 40 = mmol;
sodium, mg ÷ 23 = mmol. moderate sodium restriction (1 g or 44 mmol)
-
-
-
use all salt free foods
limit milk intake to 2 cups (500 mL) per day
omit excessively salty foods
For example: a sport drink has 23 mmol/liter of sodium. This converts to 529 mg/liter (23 x 23). So, a 500mL bottle of the drink has 265 mg of sodium or .265g. severe sodium restriction (500 mg or 22 mmol)
90 mmol of sodium is roughly 2g
60 mmol of potassium is roughly (2340 mg) or 2.3 g
use all salt free foods
limit milk intake to 2 cups (500 mL) per day
limit meat intake to 5 exchanges per day
omit sherbet and flavoured gelatin
omit vegetables known to contain higher levels of sodium. ( see p 777 of diet manual)
2013 Canadian Healthcare Association. All rights reserved.
139
FSNM Yr 2 Se 2
omit excessively salty foods
Unit 8
Meal planning for those on sodium restricted diets is based on individual needs. Some foods such as meat, milk, eggs, fish and poultry are permitted even during severe sodium restriction because they are nutritionally essential (e.g. high in protein). The patient/resident should understand that:
it is sodium and not salt that causes fluid retention
salt contains sodium
sodium also occurs naturally in foods
many foods contain sodium and reading product labels is important
that the taste for highly salted foods in the diet is an acquired taste, and with time, the patient/resident will come to enjoy the flavour of foods without added salt.
The food service and nutrition manager requires patience and creativity to plan menus for individuals which are restricted in sodium.
Some special dietetic products available for those on restricted sodium diets include:
Salt substitutes and leavening agents
Salt substitutes usually contain small amounts of sodium. Their main ingredient, however, is potassium chloride. They should be used only if approved by a physician or dietitian.
Some drug stores may prepare sodium free baking powder and baking soda or they may be found in health food stores; however, they can be difficult to obtain. These can be sifted into flour near the end of the baking period. It is important not to overbeat these products and to bake the item containing them right away. (12 teaspoons = 1 teaspoon of the regular leavening agent). Store the special leavening agents in airtight containers for short periods of time.
These products replace sodium with potassium as the major ingredient and are unsuitable for those with renal (kidney) damage. Salt substitutes should not be placed on the table for use in place of salt in long term care facilities because other patients/residents may use the substitute when it is inappropriate for their needs. Excess potassium intake can alter electrolyte balance and create cardiac problems.
2013 Canadian Healthcare Association. All rights reserved.
140
FSNM Yr 2 Se 2
Dietetic Canned Products
Unit 8
These products are more expensive because they must be analyzed for their sodium content which is then specified on the label. Salt free tomato catsup, salad dressings, pickles, peanut butter, tomato juice, butter, bread, cheese, etc. are available.
As food service and nutrition managers, you need to survey the grocery stores and health food stores in your area to determine what products are available in your area.
Renal Disease
Urine production begins in the kidneys , two bean shaped organs (located near the back above the waist) that extract impurities from the bloodstream. Blood flows continuously through each kidney's filtering units, the nephrons . Each kidney contains more than 1 million nephrons which remove waste chemicals and excess water from the blood. Approximately 180 L of fluid are filtered through the kidneys each day, the kidney then reabsorbs most of the filtered fluid and the blood constituents with approximately 1- 1.5 L of the remaining fluid and waste forming the urine. Urine passes from the kidneys through the ureters to the bladder. The bladder expands as urine enters and contracts to expel it through an exit tube called the urethra . On page 595 of the text the components of the urinary system and the structure of the nephron are shown in figure 23-1.
The kidneys have a complex role to play in maintaining the homeostasis of the body. They have a regulatory effect on many of the body's internal controls. The kidneys excrete metabolic wastes, regulate fluid balance, regulate electrolyte balance, assist in the regulation of acid-base balance and blood pressure, influence the production of red blood cells and converts calcidol to calcitrol. The functions of the kidney are outlined throughout the text.
Two of the important hormones the kidney produces are:
rennin - which has the property of increasing blood pressure. In some kidney conditions, too much renin is produced resulting in elevated blood pressure levels
(hypertension).
Erythropoietin - which controls the rate at which red blood cells are made by the body.
If too little of this substance is released into the blood, anemia occurs.
When kidney function declines significantly, the amount of water, salt and other ingested substances does not match the amount excreted in the urine. This results in an increase in the volume of water in the body and swelling of the tissues (edema). Without specialized treatment by dialysis (which filters waste products from the blood), the composition of the body fluids changes steadily and progressively and can eventually lead to death.
2013 Canadian Healthcare Association. All rights reserved.
141
FSNM Yr 2 Se 2
Renal Failure
Unit 8
Renal failure may be classified as Early Renal Insufficiency (ERI) when the kidney function starts to decrease and Chronic Kidney Disease (CKD) when the kidney function continues to decline. Renal failure may be acute; an example of acute renal failure is renal failure occurring after surgery for an unrelated condition, or chronic (progressing over months or years).
Symptoms of renal failure include:
Uremia - the presence of excess amounts of urea and other nitrogen containing end products of protein metabolism in the blood. The presence of these substances can be measured and the amount present is referred to as the B.U.N. (blood urea nitrogen) level.
hyperkalemia - which is an abnormally high level of potassium in the blood.
Hyperkalemia can produce heart and muscle problems. Hyperkalemia occurs in chronic renal failure when the kidney cannot clear potassium adequately and it builds up to the point where it may prevent heart action. A proper balance between sodium, calcium and potassium is necessary for proper functioning of the heart. A low potassium diet is prescribed when hyperkalemia is present.
hypokalemia - When the fluid intake exceeds the ability of the kidney to excrete it and causes dilution of the blood, or when there are high urinary losses of potassium, hypokalemia (low blood potassium) occurs. Poor appetite or potassium losses that occur with vomiting and diarrhea, and G.I. problems associated with kidney failure; alter the absorption of many nutrients. A high potassium diet is prescribed for hypokalemia.
Nutritional Therapy
The nutritional therapy for early renal insufficiency (ERI) and chronic kidney disease (CKD) is designed to help ease the workload of the kidneys. The diet plan will try to slow or stop the decline in kidney function. Restrictions in protein, sodium and phosphorus are found in an ERI diet plan. protein & energy protein is broken down to urea which cannot be excreted when the kidneys malfunction. When the excreting mechanism is damaged, a low protein diet is used to minimize the work of the kidney. When protein restriction is necessary, much of the protein used should be of high biological value.
Energy intake is increased by adding foods which contain fat, sugar and less commonly by using commercially available low protein products (e.g.
2013 Canadian Healthcare Association. All rights reserved.
142
FSNM Yr 2 Se 2 low protein flour, bread, noodles, desserts, etc.)
Unit 8 sodium calcium and phosphorus the damaged kidneys are unable to remove excess sodium from the body creating fluid retention and swelling
Reduction of phosphorus extcretion may lead to hyperphosphatemia (high phosphorus levels) and hypocalcemia (low calcium levels). Intake of milk and milk products is restricted to 125-250 mL/day and cheese is limited to
3 oz/week due to their high phosphorus content. fluid the damaged kidneys are unable to remove water properly leading to decreased urine output, fluid retention, increased blood pressure and possible heart failure. Fluid restriction becomes necessary and includes limiting the intake of any food item which is liquid at body temperature (e.g. ice cream, jello, syrups, gravy, soup etc.) Fruit juices are often limited because of their high potassium content.
The exchange lists for the renal diet differ from those of the diabetic diet mainly in the potassium content of the foods (i.e., fruits and vegetables). The renal diet counts vegetables separately as the protein content is higher than that of fruit
The control of the actual number of grams of protein is much more important in renal disease than in uncomplicated diabetes. Students are not expected to know the serving sizes and protein content of the renal diet. If a nutrition manager works in an institution which has a great many of these types of patients then they should be familiar with this information. Each institution that provides renal menus will have the food lists followed at that institution.
Treatment for End-Stage Renal Disease (ESRD) includes diet, drugs and dialysis. In ESRD the kidney can no longer remove waste products so a machine must replace the function of the kidney. This is known as dialysis . The types of dialysis include hemodialysis, intermittent peritoneal dialysis and continuous ambulatory peritoneal dialysis (CAPD). Please refer to the
Canadian Kidney Foundation website under publications, http://www.kidney.ca
- Check the information in publications pertaining to Haemodialysis and Peritoneal Dialysis. Both provide excellent descriptions and graphics. Other topics are listed there as well. The Nutrition in
Practice in Chapter 23, pp. 616-618 also describes the different types of dialysis.
The diet for hemodialysis involves control of protein, sodium, fluid, phosphorus and potassium intake. Waste products tend to accumulate in the blood between hemodialysis treatments. This
2013 Canadian Healthcare Association. All rights reserved.
143
FSNM Yr 2 Se 2 Unit 8 can lead to symptoms such as nausea, vomiting, headaches and loss of appetite which pose a particular challenge when trying to encourage ESRD patients to consume a nutritionally adequate food intake. Patients with a diet restricted in potassium may have an inadequate intake of water soluble vitamins as these are usually found in higher amounts in fruits and vegetables which are also good sources of potassium and need to be restricted. Water soluble vitamins are removed from the blood stream during dialysis. For these reasons, a special renal vitamin supplement is prescribed for kidney patients.
Continuous ambulatory peritoneal dialysis (CAPD) removes wastes from the body daily so the diet plan is more liberal than in hemodialysis.
Kidney Stones or Urinary Calculi
Kidney stones vary in size from fine gravel to large stones and may develop in the ureter, bladder or urethra. Most calculi contain calcium. The cause of kidney stones is unknown.
Nutritional management is directly related to the composition of the kidney stone involved:
calcium stones - accounts for most cases of urinary calculi. A controlled calcium diet is used which provides 800 mg Ca/day. A lower sodium diet will cause less calcium to be excreted in the urine.
uric acid stones - common in cases of gout. Uric acid is produced from purines.
Foods high in purines include kidney, liver, sweetbreads, sardines, anchovies and meat extracts. Today, medication usually controls uric acid levels.
Conclusion
In coronary heart disease many factors interrelate to increase the risk involved. These risks include raised serum cholesterol levels, hypertension and cigarette smoking. Dietary adjustments are made for those with ischemic heart disease, hyperlipoprotenemia and hypertension.
In view of the central role of the kidneys in maintaining the constant internal environment it is not surprising that renal disease and eventually renal failure affect every system and tissue in the body.
"Protection of the parenchymal cells is the foremost consideration in all types of liver injury.
Since the liver is so intimately involved in the metabolism of foodstuffs, a nutritious diet is an important part of therapy and should be designed to protect the liver from stress and to enable it to function as efficiently as possible."
8
Diseases of the gallbladder may require dietary medical or surgical intervention. The principle dietary aim is to provide a restricted fat diet to minimize discomfort.
2013 Canadian Healthcare Association. All rights reserved.
144
FSNM Yr 2 Se 2 Unit 8
Pancreatitis usually leads to digestive problems as evidenced by the presence of "excess fat and undigested protein in the stools. Dietary treatment of pancreatic disorders depends on the nature and extent of digestive impairment rather than on the disease itself".
9
Endnotes
1
Goodhart, R., and Skills, M. (1980). Modern Nutrition in Health and Disease . NY, NY: Lea and
Febiger, p.1046.
2
Robinson, C. and Lawler, M. (1982). Normal and Therapeutic Nutrition , NY, NY: MacMillan
Publishing Co., p.659.
3
Mahan, L.K. and Escott-Stump, S. (1996). Krause's Food Nutrition & Diet Therapy, 9th. ed .,
Philadelphia, Penn.: W.B. Saunders Co., p 642
4
Willett, W.C., Stampfer M.(2003). Rebuilding the food pyramid, Scientific American ,
Hu, F. (2003). The Mediterranean diet and mortality: Olive oil and beyond. New England
Journal of Medicine , 348(26), 2599-2608.
Hu, F., Willet, W.C. (2002). Optimal diets for prevention of coronary heart disease. JAMA ,
288(20), 2569-2578.
5
de Lorgeril, M., Salen, P., Martin, J., et al. (1999). Lyon diet heart study, Circulation , 99, 779-
785.
5
Singh, R.B., Dubnov, G., Niaz, M.A.,, et al. (2002). Effect of an Indo-Mediterranean diet on progression of coronary artery disease in high risk patients, Lancet , 360, 1455-61.
6
Willett, W.C., Stampfer, M. (2003). Rebuilding the food pyramid, Scientific American .
7
Akita, S., Sacks, F.M., Conlin, P.R., et al. (2003). DASH diet acts through diuretic effect to lower blood pressure. Hypertension /
8
Robinson, C. and Lawler, M. (1982). Normal & Therapeutic Nutrition . New York, NY:
MacMillan Publishing Co., p.563.
9
Robinson, C. and Lawler, M. (1982). Normal & Therapeutic Nutrition . New York, NY:
MacMillan Publishing Co.
2013 Canadian Healthcare Association. All rights reserved.
145
FSNM Yr 2 Se 2
Required Readings
Textbook(s)
DeBruyne, L.K., Pinna, E. & Whitney, E.N. (2012).
Nutrition and diet therapy (8th ed.). Belmont, CA: Wadsworth/Thomson Learning.
Chapter 19 “Carbohydrate and Fat-modified diets for malabsorption”, pp. 502-
520
Chapter 20 “Nutrition therapy for liver and gallbladder diseases”, pp. 521-541
Chapter 22
“Fat-controlled, mineral-modified diets for cardiovascular d iseases”, pp. 568-593
Chapter 23 “Protein, mineral, and fluid-modified diets for kidney diseases”, pp.
594-618
Readings from Course Reader
Colbeck, J. (2006). N utrition for dialysis: Don’t be scared. Food service & nutrition, Canadian Society of Nutrition Management , Vol 2, Issue 4.
Beck, L. (2008). The teetotaller’s liver disease.
Health: Food for thought: the facts about fatty tissue: a new epidemic? Globe and Mail , March 5, 2008.
Dietitians of Canada – Client Education Handout series; Low-Fat Diet; Low-
Potassium Diet/ Potassium content-vegetables/fruits; low-Sodium Diet;
Potassium-Rich Diet/Recipes; Heart-Healthy Eating Cholesterol/ Triglycerides/
Recipes/ Sample Menu.
Unit 8
2013 Canadian Healthcare Association. All rights reserved.
146
FSNM Yr 2 Se 2
Unit 8 Assignment located on the Gateway
To complete the Unit 8 assignment, please access your account on the Gateway at www.cha.ca. The assignment is available in Word format on the Gateway for you to download. Once completed, please upload your assignment into the designated location.
Unit 8
2013 Canadian Healthcare Association. All rights reserved.
147