ICD10 and MT - The Perfect Storm
advertisement

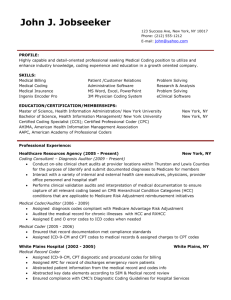
ICD-10 and Medical Transcription The Perfect Storm Copyright, C. Tessier, 2012 Claudia Tessier RHIA May 4, 2012 Full Disclosure • I am a consultant with an international firm (ID Information and Documentation in Healthcare) that designs coding software and is introducing its ICD-10 software into the US. • Thus, much of my ICD-10 knowledge comes from them – BUT I learned and taught ICD-9 coding years ago. • Of course, you know where my MT knowledge comes from! And I am here as your advocate. The Strategic View of Medical Transcription • “Evolving” medical transcription practice and business models • Increasing adoption of technologies: EMR, SR, CAC, NLP... • Impending transition to ICD-10 • Need for qualified coders Integrate Medical Coding with Transcription The Perfect Storm of Opportunity Just what is ICD-10? • ICD: International Classification of Diseases – Standard classification: general epidemiological reporting, also health management and clinical purposes – Started in 1850s, 1st edition 1893: International List of Causes of Death – WHO became responsible in 1948 with 6th revision - first edition to include morbidity causes in addition to mortality • ICD-9 – adopted in 1977 • ICD-10 – Endorsed by 43rd World Health Assembly in 1990 – Adopted by WHO member states in 1994 – US is among last few countries to adopt ICD-10 • Initial adoption date: October 1, 2013 • HHS has proposed delay to October 1, 2014 Why not stay with ICD-9? Because it’s… • Designed for reporting morbidity and mortality • Lacks structure and granularity for clinical decision making and research • Matches imperfectly in more than 95% of cases • Can’t keep up with advances in medicine and healthcare • Can’t be relied on to support continuity of care and management The ICD-10 Challenge • • • • Increase from 17,000 to 155,000 codes 25% to 50% decrease in coder productivity Increase in 3 % error rate to 6% to 10% Denial rate increase 10% to 25%2 • 10%+ charts will not have documentation specific enough for coding2 Huge changes and demands Increased specificity in ICD-10-CM • • • • • • • • • • • • • • Laterality Episode of care – initial subsequent, sequelae CC/MCC Acuity Anatomic detail Supporting lab values Qualifiers: severity, chronic/acute, accompanying conditions, etiology, fracture type, etc. Causative agents, drugs, diseases, genetics Disease processes connected to common manifestations Alcohol, tobacco, and drugs Expanded codes for injury, diabetes, alcohol/substance abuse, postoperative complications Updated clinical terminology (e.g. diabetes mellitus, malignant/benign hypertension - e.g., 6 diabetes mellitus categories Changes in time frames specified in certain codes, e.g., trimesters Lack of specificity more physician queries Benefits of ICD-10 • That increased specificity will – Improve cost analyses and resource utilization – Enhance comparability for volume, cost, morbidity and mortality – Facilitate opportunities for quality improvement – Improved revenue stream resulting from documentation improvement – Enhance disease management and protocol development – Support meaningful use – Facilitate strategic positioning – Facilitate epidemiological and bio-surveillance activities Source: Rose Dunn “Better Late than Never: How to Catch up with ICD10-CM/CPS in 2012,” AHIMA ICD-10 Summit, April 2012 Convergence of Initiatives ICD-10 Meaningful Use Clinical Analytic Dashboards (BI) Lower Medicare reimbursements ACOs Medical Homes PQRI DRG-driven reimbursement cutbacks Value-based purchasing Better Documentation = Improved Coding and Improved Information for Patient Care and Reimbursement Changing Regulatory Environment • Federal/state payment initiatives and reforms impact documentation and coding • ICD-10 will bring greater demands – Clinical documentation must be more specific – Coder productivity will drop – Training will take coders and CDI specialists away from daily workflow Relationship between EHRs and ICD-10 • Some EHRs are successful without structured documentation BUT • Specific structured clinical data are needed to achieve meaningful use AND • ICD-10 clinical documentation must be highly structured • Therefore, the documents you transcribe will become increasingly structured ICD-9 to ICD-10 Transition Impacts Coders • Coders need expanded clinical, medical language, anatomy and physiology, pharma, lab data knowledge. • Intelligent coding is the key to accuracy ICD-10 and Clinical Documentation • Data integrity is the Issue – Must capture specificity in documentation – So, how to improve documentation accuracy • Predicted 10% to 20% increase in documentation in response to ICD-10 • Denials will increase initially Medical Transcriptionists as Coders • Both require knowledge of • • • • • • • • • medical language anatomy and physiology clinical assessments diagnoses, treatments procedures pharmacology pathophysiology laboratory practice • Both must be able to – Read and understand patient medical records – Abstract patient information quickly and accurately – Research clinical information effectively Impact of Connecting Coding with Transcription • Expanded pool of qualified coders • Delayed or incomplete coding instances reduced • Diagnoses and procedures supplemented by MTs’ knowledge of and access to content • Coding process facilitated and streamlined • Improved clinical documentation • Reimbursement based on more accurate, complete, and timely coding • Delayed reimbursement due to requests for supporting documentation to support diagnoses diminished • Clients potential for revenue increased • More accurate, complete, and timely coding • Clinical documentation services will provide valued service to clients potential for increased revenue Coding Resources • The usual – medical dictionaries, word books, pharma and lab resources, etc. • Plus – – – – – – CAC – computer assisted coding NLP – natural language processing Remote coding EHR-supported coding Automated feedback CDI efforts - clinical documentation improvement Use of Patient Documents Coders Medical Transcriptionists • • • • • History and physicals Discharge summaries Consultations Progress notes Operative and procedure reports • Radiology reports • Pathology reports Coding with ICD-10 Crosswalk: ICD-9 to ICD-10 Clinical Documentation Improvement • Migrating paper records to electronic via hybrids • Deliberately discourages – Copy and paste – Handwriting – Free text narratives • Partial solutions – Templates – Speech recognition – Direct entry via pick lists, pull-down menus… Clinical Documentation Improvement • Physician clinical documentation goals – Standardized content and streamlined workflow – Address quality and regulatory considerations – Avoid financial penalties for poor documentation – Enhance clinical value • Technology advancements • Workflow changes Workflow Changes • Documentation in multiple locations vs centralized records • Automated feedback to clinicians as they document • CDI (clinical documentation improvement) programs • Transcription-supported coding • Concurrent coding via EMR • Electronic queries generated within EMR • Remote coding, chart reviews/audits • Include query response TAT within suspension process • Final coding Concurrent CDI and Coding • The route toward data improvement and integrity • Documentation leads to coding • Ergo… Opportunity! Technology Changes Impact Coding • Increased use of technology improves productivity, compliance, consistency of documentation and therefore of coding – CAC, NLP – ICD-10 crosswalks and mapping – DRG Grouper – Optimization of EHR-supported coding – Electronic queries and templates What is Computer-assisted Coding? • “…the use of computer software that automatically generates a set of medical codes for review, validation, and use based upon clinical documentation provided by healthcare practitioners.” – Delving into Computer-assisted Coding (AHIMA Practice Brief, 2004) Impact of CAC on Coding • First 9 months, expected 50% decrease in efficiency • CAC can offer gains up to 30%, reducing impact to 20% • Staff augmentation necessary • Increase coder efficiency – – – – Potential code alerts Reports/results accessible online Reduce paper shuffling Automated workflow CAC Goals • • • • • • • • • • • • • • • • • Solid foundation for ICD-10 readiness Seamless integration Improved documentation Improved quality Greater productivity Greater consistency Real-time coding Automation/integration of critical documentation data, e.g., POA, ROM, SOI Reduce labor and outsourcing costs Generate correct, compliant billing Reduction in denials Reduce A/R days and DNFB Improves capture of patient severity Facilitates identification of PSI/HAC Integrates with CDI and improves DRG accuracy and potential queries to physicians Improves coder and CDI staff satisfaction Facilitate communication between coders, CDIS, clinicians, MTS NLP and CAC • CAC with natural language processing as single platform is best solution • Improves workflow and production • Facilitates achieving CAC goals What is NLP? • A form of artificial intelligence • Reads text and understands meaning from standard dictation/transcription, SR, and templates with free-text fields – Most cannot read images of text or handwritten documents • • • • • Word-search functions for terms to support clinical findings Compares new and old documents Identify query opportunities improve productivity and accuracy Auto-suggest codes Crosswalk ICD-10 and guidelines to alert for additional specificity needed • Different types – Rules-based – Statistics-based – Combination • May give overwhelming feedback – need to discriminate NLP: Stage 1 – Documents Uploaded NLP Stage 2: Analysis and Action Begin Major Concern re Transition to ICD-10 • Coder shortage and productivity • Reactions/solutions – Training • • • • Advance At implementation Ongoing Sometimes funded – Retention bonuses – Sign-on bonuses Opportunity! What is Needed for MTs? • Training for coding • Understanding of computer-assisted coding tools • Understanding how NLP can be integrated • Marketing of new value to transcription and to its users MTs have a Key Advantage MTs do not have to unlearn ICD-9 Training Requirements • Variable depending on clinical knowledge and knowledge of coding systems • Medical transcriptionists • Already have clinical knowledge • Need to gain in-depth knowledge of coding systems but do not have to unlearn ICD-9 • Need course work plus lab time Training Options • • • • • • • • Internal resources Colleges/community colleges/technical schools Apprentice programs Online programs Websites YouTube Professional associations MT resources, e.g. MT Tools Online Coding Training • AHIMA – approved coding certificate program directory – Find sites athttp://www.ahima.org/careers/college_search/se arch.aspx – Search by state and by whether onsite or distance learning Coding Credentials for Hospitals or Physician’s Offices – AHIMA* • CCA – certified coding associate – first-level • CCS: certified coding specialist – mastery-level • CCS-P: certified coding specialist--physician-based Note: The U.S. Department of Labor's Bureau of Labor Statistics projects a 20% increase in employment before 2018 for the Medical Coding and Billing field, which includes medical coding and billing professionals. This represents more than 37,000 new jobs. • AHIMA coding credentials are the only ones currently accredited by the National Commission of Certifying Agencies Coding Credentials for Physician Offices and Outpatient Hospitals – AAPC* • CPC: certified professional coder – physician’s office • CPC-H: certified professional coder – outpatient hospital • CPC-P: certified professional coder – payer • CIRCC: certified interventional radiology cardiovascular coder • Multiple specialty coding credentials *American Academy of Professional Coders 2008 AHIMA Salary Survey for Coders Coders working in consulting services • average salary of $57,700. Otherwise, averages range from • $36,502 for coders in home health or hospice to • $48,115 for those in nonprovider settings. Medical Coder Salaries: 2011 AAPC survey • Average for CPC was $46,900 (up $1400 from previous year). Over half the respondents reported earning more than $40,000. Recent Postings: Medical Coder Salaries • • • • • • • • Inpatient/DRG Coder Remote coder Coding Supervisor Traveling IP Coders, Full travel Home-based Lead Coder Inpatient Coder Corporate Coder Senior IP/DRG Coder $38-$59K $43-$75K $50-$60K $50-$60K Up to $60K $56-$78K $65-$75K $68K MT Salaries • AHDI May 2002 salary survey: $31,400 • Occupational Outlook Handbook, Bureau of Labor Statistics – 2010 Median Pay $32,900 per year $15.82 per hour • PayScale.com – national pay data 2012 – – – – Hourly rate: $9.89 - $19.42 Overtime: $11.73 - $29.71 Bonus: $0 - $12,83 Total: $19,135 - $41,771 Remember? • Three levels of medical transcriptionists (per 1999 Hay Study) • With integrated coding skills, medical transcriptionists can create and enter the Fourth Level New career opportunity Evolution of the MT Profession Coding, CAC, NLP, and CDI Capturing clinicians’ voice and transcribing 1970s-1990s Word processing, computers, internet, speech recognition, and EMRs Trad’l capturing of clinicians’ voice and transcribing 1990s-2012 Computers, internet, speech recognition, EMRs, structured data entry Trad’l capturing of clinicians’ voice and transcribing What’s Next To Quote a Colleague • The Potential for MTs – I really believe this [coding] is something many MTs can pick up on easily. It’s such an easy transition because we have the basic fund of knowledge that’s required in terminology, anatomy and physiology, pharmacology, and pathophysiology. – The rest really is about learning the rules for coding and learning how to use your books to find the right codes…[e.g., being] able to identify what the primary diagnosis is in an encounter. I believe we’ve been doing that for a long time. – If you’re looking for a transition, I think this one has great potential. • Kathy Nicholls, Coding Corner Update, MT Tools Online, April 24, 2012 What do we need? • A project that addresses both training and integration of coding with transcription to address – Coding education requirements for MTs – Process and flow requirements for integrating coding into medical documentation/transcription – Business models • Rebranding! Questions • How much do we have to invest in training? • How much of transcription productivity will be lost due to coding? • How much coding productivity and value will be gained? • How much can be charged for the integrated process? • How much can MT/coders expect to be paid? • What will it affect status and value of MT? Of coding? • How will it affect patient care, reimbursement, CDI, etc.? • How will it affect our future? So… who will benefit from this perfect storm? Those with Blue Sky Thinking! Thank you! • For a copy of the slides and to learn more – c.tessier@id-diacos.com – 617-816-7513 Glossary of Abbreviations • • • • • • • • • • • • • • • • • • 5010 – upgrade of HIPAA 4010. Revised medical billing/coding data of ICD-10-CM & ICD-10-PCS will be accommodated by all covered entities in a better manner. ACA – Accountable Care Act ACO –accountable care organization ADR – adverse drug reaction, additional documentation request AHRQ – Agency for Healthcare Research and Quality CAC – computer assisted coding CC/MCC – complication/co-morbidity - major CC CDC – Centers for Disease Control and Prevention CERT – Comprehensive Error Rate Testing CMS – Centers for Medicare and Medicaid Services CPT – Current Procedural Terminology DNFB – discharged, not final billed DRG and MS-DRG – Diagnosis-related Group, Medical Severity DRG GEM – General Equivalence Mappings HAC – Health Administration Center (VA) HEAT – Health Care Fraud Prevention and Enforcement Action Team HCPCS – Healthcare Common Procedure Coding System HEDIS – Healthcare Effectiveness Data and Information Set Glossary of Abbreviations • • • • • • • • • • • • • • • • • • • HHS – (US Department of) Health and Human Services ICD – International Classification of Diseases ICD-10-CM – ICD-Clinical Modification ICD-10-PCS – ICD-Procedure Coding System NCHS – National Center for Health Statistics MAC - Medicare Administrative Coordinator MIC – Medical Inefficiency Committee MUE – medically unlikely edits NCCI – National Correct Coding Initiative OAG –Office of Inspector General POA – present on admission QIC –qualified independent contractor, Quality Improvement Council RAC – Recovery Audit Contractors ROM – risk of mortality SNOMED-CT – Systemized Nomenclature of Medicine – Clinical Terms SDX – secondary diagnosis SOI – severity of illness WHO – World Health Organization ZPIC – Zone Program Integrity Coordinators