Priming and Flushing • Tubing and Pumps
advertisement

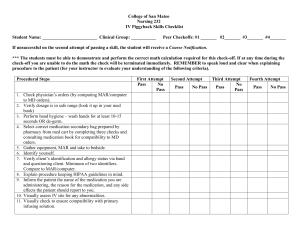
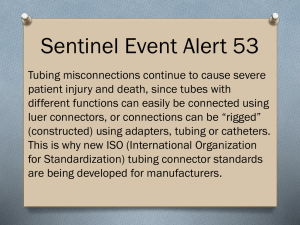
Small Volumes, Big Problems: A Patient Safety Approach to Secondary IV Medications Tonja G. Schroder, BSN, RN, CPN and Julie Bell, MS, RN, CPN Situation If you asked ten nurses on our pediatric units how they set up, infused and flushed a small volume intermittent medication, you would get ten variations, all within policy. Background • Priming and Flushing - Nurses might prime tubing with medication or normal saline (NS), creating variance in when the medication reached the patient, especially at low rates - Flushes might be infused by pump or pushed possibly at a different rate than the medication infused (e.g., bolus push of NS) - Nurses who floated to Pediatric units from NICU had a different protocol for priming and flushing • Tubing and Pumps - Tubing was changed with each intermittent medication and connected at a Y-port near the insertion site • Frequent opening of line may increase infection possibility • Manipulation of the line close to the insertion site may increase risk of dislodging catheter • Frequent tubing changes increases cost - Some small volume medications were administered via secondary (“piggyback” infusion set with large volume tubing) and some were administered by syringe pump with various tubing volumes Assessment • Multiple opportunities for improvement existed • A work group of staff nurses, nursing professional development specialists, and pharmacists from pediatrics, pediatric ICU, and neonatal ICU developed a unique solution Medication Safety: • Accurate delivery rate and volume Standardized flush procedure • Medication & flush infusions supported by smart pump • Nurses know next step when pump alarms Infection Control: • Decrease opening line Closed system • Decrease infections • Decrease manipulation of line Cost Savings: • Standardize tubing volume Streamline tubing • Decrease tubing changes to save money • Save nursing time Outcomes Implications for Nursing Practice • Standardized flush and procedure – Improved consistency of process for nurses – Medications delivered at ordered rate • Infection control – closed system – Loss of peripheral lines were minimal before and after implementation – Compliance with maintaining closed system high • Cost savings – One unit’s medication tubing costs (3 months) Before implementation................................... $894 After implementation..................................... $216 Cost savings...................................................... $678 Implementation Pump: Use the syringe channel rather than piggybacks for all secondary IV medications < 60 mL Tubing: Use microbore (1 mL) tubing; use a multi-lumen extension set when needed. Only one set of tubing is needed for all intermittent medications for 72 hours, saving an average of 6 sets of tubing per day for 3 days. Closed system with less manipulation at site: Both the medication and flush syringes are attached at the end of the microbore tubing rather than at a Y-port near the insertion site. The flush syringe remains in place until the next medication to keep the site closed. Priming: The first mL of the next medication is pushed and the pump is programmed for the rate and volume prescribed for the medication. Flush: When the medication has infused, a new pre-filled NS flush syringe is attached and 1.5 mL is infused at the same rate as the medication by using <resume> function on pump. Standardization: Any nurse responding to the pump alarm, seeing that an intermittent medication is complete, knows to attach the NS flush, restore the rate, and set the volume. Any nurse responding and seeing that the flush has infused, also knows to turn off the syringe pump channel (large volume IV continues at programmed rate). Staff Education – Quick Tips IV Medication Delivery Meds ≤ 60 mL use Closed Med System Syringe Microbore tubing (1 mL) Push 1st mL Infuse Flush 1.5 mL at same rate as med Tubing lasts 72 hours if not removed from Y-port & capped Meds > 60 mL Piggyback Secondary tubing Back prime Infuse Leave tubing connected; primary resumes Tubing lasts 24 hours •Improving medication safety, decreasing infection risks, standardizing nursing process, and decreasing cost were all realized by this improvement •Sharing this trans-disciplinary, multi-unit process and the procedure with nurse colleagues can assist them in achieving these same outcomes Transdisciplinary Team Pediatric/PICU Staff Nurses •Karen Joyce, BSN, RN, CPN, Pediatrics •Meg Kerr, BSN, RN, CPN, Pediatrics Nursing Supervisor •John Liberatos, BS, RN, PICU •Donna Lingerfelt, BSN, RN, CPN, Pediatrics •Elaine Mordenti, BSN, RN, CPN, Pediatrics Nursing Supervisor •Lisa Penland, RN, CPN, PICU •Allison Taylor, BSN, RN, CPN, Pediatrics Pediatric Pharmacists •Marci Bemis, PharmD •Jamie Hogerheide, PharmD Nursing Professional Development Specialists •Tonja Schroder, BSN, RN, CPN •Julie Bell, MS, RN, CPN NICU Colleagues •Anne Ramirez, MSN, RN, Clinical Nurse Specialist •Brianna Bridges, BSN, RN