Chapter 48
advertisement
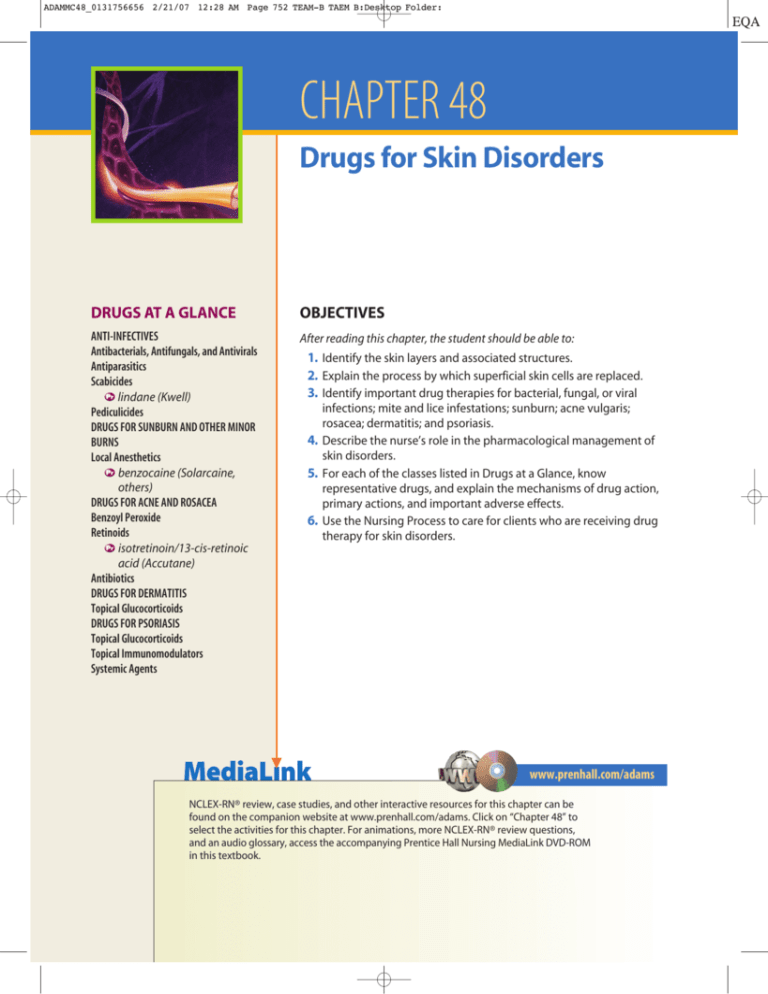
ADAMMC48_0131756656 2/21/07 12:28 AM Page 752 TEAM-B TAEM B:Desktop Folder: CHAPTER 48 Drugs for Skin Disorders DRUGS AT A GLANCE OBJECTIVES ANTI-INFECTIVES Antibacterials, Antifungals, and Antivirals Antiparasitics Scabicides lindane (Kwell) Pediculicides DRUGS FOR SUNBURN AND OTHER MINOR BURNS Local Anesthetics benzocaine (Solarcaine, others) DRUGS FOR ACNE AND ROSACEA Benzoyl Peroxide Retinoids isotretinoin/13-cis-retinoic acid (Accutane) Antibiotics DRUGS FOR DERMATITIS Topical Glucocorticoids DRUGS FOR PSORIASIS Topical Glucocorticoids Topical Immunomodulators Systemic Agents After reading this chapter, the student should be able to: 1. Identify the skin layers and associated structures. 2. Explain the process by which superficial skin cells are replaced. 3. Identify important drug therapies for bacterial, fungal, or viral infections; mite and lice infestations; sunburn; acne vulgaris; rosacea; dermatitis; and psoriasis. 4. Describe the nurse’s role in the pharmacological management of skin disorders. 5. For each of the classes listed in Drugs at a Glance, know representative drugs, and explain the mechanisms of drug action, primary actions, and important adverse effects. 6. Use the Nursing Process to care for clients who are receiving drug therapy for skin disorders. www.prenhall.com/adams NCLEX-RN® review, case studies, and other interactive resources for this chapter can be found on the companion website at www.prenhall.com/adams. Click on “Chapter 48” to select the activities for this chapter. For animations, more NCLEX-RN® review questions, and an audio glossary, access the accompanying Prentice Hall Nursing MediaLink DVD-ROM in this textbook. ADAMMC48_0131756656 2/21/07 12:28 AM Page 753 TEAM-B TAEM B:Desktop Folder: Chapter 48 Drugs for Skin Disorders KEY TERMS acne vulgaris page 761 comedone page 761 dermatitis page 765 eczema page 765 erythema page 754 excoriation page 765 keratolytic page 761 nits page 756 pediculicides page 757 pruritus page 753 psoralen page 768 retinoid page 762 rhinophyma page 761 rosacea page 761 scabicides page 757 seborrhea page 761 vitiligo page 753 753 T he integumentary system consists of the skin, hair, nails, sweat glands, and oil glands. The largest and most visible of all organs, the skin normally provides an effective barrier between the outside environment and the body’s internal organs. At times, however, external conditions become too extreme, or conditions within the body change, resulting in unhealthy skin. When this occurs, pharmacotherapy may be utilized to improve the skin’s condition. The purpose of this chapter is to examine the broad scope of skin disorders and the drugs used for skin pharmacotherapy. 48.1 Structure and Function of the Skin To understand the actions of dermatologic drugs, it is necessary to have a thorough knowledge of skin structure. The skin comprises three primary layers: the epidermis, dermis, and subcutaneous layer. The epidermis is the visible, outermost layer that constitutes only about 5% of the skin depth. The middle layer is the dermis, which accounts for about 95% of the entire skin thickness. The subcutaneous layer lies beneath the dermis. Some textbooks consider the subcutaneous layer as being separate from the skin, and not one of its layers. Each layer of skin is distinct in form and function and provides the basis for how drugs are injected or topically applied (Chapter 4 ). The epidermis has either four or five sublayers depending on its thickness. The five layers from the innermost to outermost are stratum basale (also referred to as the stratum germinativum), stratum spinosum, stratum granulosum, stratum lucidum, and the strongest layer, the stratum corneum. The stratum corneum is referred to as the horny layer because of the abundance of the protein keratin, which is also found in the hair, hooves, and horns of many mammals. Keratin forms a barrier that repels bacteria and foreign matter, and most substances cannot penetrate it. The largest amount of keratin is found in those areas subject to mechanical stress, for example, the soles of the feet and the palms of the hands. The deepest epidermal sublayer, the stratum basale, supplies the epidermis with new cells after older superficial cells have been damaged or lost through normal wear. Over time, these newly created cells migrate from the stratum basale to the outermost layers of the skin. As these cells are pushed to the surface they are flattened and covered with a water-insoluble material, forming a protective seal. On average, it takes a cell about 3 weeks to move from the stratum basale to the body surface. Specialized cells within the deeper layers of the epidermis, called melanocytes, secrete the dark pigment melanin, which offers a degree of protection from the sun’s ultraviolet rays. The number and type of melanocytes determine the overall pigment of the skin. The more melanin, the darker the skin color. In areas where the melanocytes are destroyed, there are milk-white areas of depigmented skin referred to as vitiligo. The second primary layer of skin, the dermis, provides a foundation for the epidermis and accessory structures such as hair and nails. Most receptor nerve endings, oil glands, sweat glands, and blood vessels are found within the dermis. Beneath the dermis is the subcutaneous layer, or hypodermis, consisting mainly of adipose tissue, which cushions, insulates, and provides a source of energy for the body. The amount of subcutaneous tissue varies in an individual, and is determined by nutritional status and heredity. 48.2 Causes of Skin Disorders Of the many types of skin disorders, some have vague, generalized signs and symptoms, and others have specific and easily identifiable causes. Pruritus, or itching, is a general condition associated with dry, scaly skin, or it may be a symptom of mite or lice infestation (Section 48.4). Inflammation, a characteristic ADAMMC48_0131756656 2/21/07 12:28 AM Page 754 TEAM-B TAEM B:Desktop Folder: 754 Unit 9 The Integumentary System Eyes/Ears TABLE 48.1 Classification of Skin Disorders Type Examples infectious Bacterial infections: boils, impetigo, infected hair follicles Fungal infections: ringworm, athlete’s foot, jock itch, nail infection Parasitic infections: ticks, mites, lice Viral infections: cold sores, fever blisters (herpes simplex), chicken pox, warts, shingles (herpes zoster), measles (rubeola), and German measles (rubella). inflammatory Injury and exposure to the sun such as sunburn and other environmental stresses Disorders marked by a combination of overactive glands, increased hormone production, and/or infection such as acne, blackheads, whiteheads, rosacea Disorders marked by itching, cracking, and discomfort such as eczema (atopic dermatitis), other forms of dermatitis (contact dermatitis, seborrheic dermatitis, stasis dermatitis), and psoriasis. neoplastic Types of skin cancers: squamous cell carcinoma, basal cell carcinoma, and malignant melanoma. Malignant melanoma is the most dangerous. Benign neoplasms include keratosis and keratoacanthoma. of burns and other traumatic disorders, occurs when damage to the skin is extensive. Local erythema or redness accompanies inflammation and many other skin disorders. Trauma to deeper tissues may cause additional symptoms such as bleeding, bruising, and infections. Skin disorders are diverse and difficult to classify. These disorders are summarized in Table 48.1. One simple method is to group them into the following general categories. Infectious: Bacterial, fungal, viral, and parasitic infections of the skin and mucous membranes are relatively common, and are frequent indications for anti-infective pharmacotherapy. A brief overview is presented in Sections 48.3 and 48.4; however, greater detail may be found in the anti-infective chapters of this text (Chapters 34–36 ). ● Inflammatory: Inflammatory disorders encompass a broad range of pathology that includes acne, burns, eczema, dermatitis, and psoriasis. Pharmacotherapy of inflammatory skin disorders includes many of the agents discussed in Chapter 43 , such as glucocorticoids. ● Neoplastic: Neoplastic disease includes malignant melanoma and basal cell carcinoma, which are treated with the therapies described in Chapter 37 . ● Dermatologic signs and symptoms may reflect disease processes occurring elsewhere in the body. Skin abnormalities including color, sizes, types, and character of surface lesions, and skin turgor and moisture may have systemic causes such as liver or renal impairment, cardiovascular insufficiency, metastatic tumors, recent injury, and poor nutritional status. The relationship between the integumentary system and other body systems is depicted in ● Figure 48.1. Common symptoms associated with a range of conditions are listed in Table 48.2. Although there are many skin disorders, some warrant only localized or short-term pharmacotherapy. Examples include lice infestation, sunburn with minor irritation, and acne. Eczema, dermatitis, and psoriasis are more serious disorders requiring extensive and sometimes prolonged therapy. SKIN INFECTIONS The skin is normally populated with microorganisms or flora that include a diverse collection of viruses, fungi, and bacteria. As long as the skin remains healthy and intact, it provides an effective barrier against infection from these organisms. The skin is very dry, and keratin is a poor energy source for microbes. Although perspiration often provides a wet environment, its high salt content discourages microbial growth. Furthermore, the outer layer is continually being sloughed off, and the microorganisms go with it. 48.3 Pharmacotherapy of Bacterial, Fungal, and Viral Skin Infections Bacterial skin diseases can occur when the skin is punctured or cut, or when the outer layer is abraded through trauma or removed through severe burns. Some bacteria also infect hair follicles. The two most common bacterial infections of the skin are caused by Staphylococcus and Streptococcus, which are normal skin inhabitants. S. aureus is responsible for furuncles, carbuncles, and abscesses of the skin. Both S. aureus and S. pyogenes can PHARMFACTS Skin Disorders ■ ■ ■ ■ ■ An estimated 3 million people with new cases of lice infestation are treated each year in the United States. Nearly 17 million people in the United States have acne, making it the most common skin disease. More than 15 million people in the United States have symptoms of dermatitis. Of infants and young children, 10% experience symptoms of dermatitis; roughly 60% of these infants continue to have symptoms into adulthood. Psoriasis affects 1% to 2% of the U.S. population. This disorder occurs in all age groups—adults mainly—affecting about the same number of men as women. ADAMMC48_0131756656 2/21/07 12:28 AM Page 755 TEAM-B TAEM B:Desktop Folder: Chapter 48 Drugs for Skin Disorders Endocrine system Hormones influence glandular activity, calcium homeostasis, and skin health. The integumentary system Respiratory system The lungs provide oxygen to all cells in the body. Lymphatic system Helps fight diseases and infections of the skin. Skeletal system The bones are a storage site for calcium, an important mineral connected with vitamin D function. Digestive system Proper nutrition is important for healthy skin. ● Figure 48.1 Nervous system Emotions affect skin coloration. The skin is a sensory organ. Cardiovascular system The blood carries oxygen and carbon dioxide, factors that influence skin health and coloration. Muscular system The skin and muscles are important for proper body movement and expression. Urinary system The accumulation of toxic substances in the bloodstream will affect the skin adversely. 755 For all systems The skin forms a protective barrier against hazardous conditions. Reproductive system The skin covers external genitalia. Sex hormones influence skin health. Interrelationships of the integumentary system with other body systems TABLE 48.2 Signs and Symptoms Associated With Changing Health, Age, or a Weakened Immune System Sign Description delicate skin, wrinkles, and hair loss Many degenerative changes occur in the skin; some are found in elderly clients; others are genetically related (fragile epidermis, wrinkles, reduced activity of oil and sweat glands, male pattern baldness, poor blood circulation); hair loss may also be linked to medical procedures, for example, radiation and chemotherapy. discoloration of the skin Discoloration is often a sign of an underlying medical disorder (for example, anemia, cyanosis, fever, jaundice, or Addison’s disease); some medications have photosensitive properties, making the skin sensitive to the sun and causing erythema. scales, patches, and itchy areas Some symptoms may be related to a combination of genetics, stress, and immunity; other symptoms are due to a fast turnover of skin cells; some symptoms develop for unknown reasons. seborrhea/oily skin and bumps This condition is usually associated with younger clients; examples include cradle cap in infants and an oily face, chest, arms, and back in teenagers and young adults; pustules, cysts, papules, and nodules represent lesions connected with oily skin. tumors Tumors may be genetic or may occur because of exposure to harmful agents or conditions. warts, skin marks, and moles Some skin marks are congenital; others are acquired or may be linked to environmental factors. ADAMMC48_0131756656 2/21/07 12:28 AM Page 756 TEAM-B TAEM B:Desktop Folder: 756 Unit 9 The Integumentary System Eyes/Ears cause impetigo, a skin disorder commonly occurring in school-age children. Although many skin bacterial infections are self-limiting, others may be serious enough to require pharmacotherapy. When possible, pharmacotherapy utilizes topical agents applied directly to the infection site. Topical agents offer the advantage of causing fewer side effects, and many are available OTC for self-treatment. If the infection is deep within the skin, affects large regions of the body, or has the potential to become systemic, then oral or parenteral therapy is indicated. Chapter 34 provides a complete discussion of antibiotic therapy. Some of the more common topical antibiotics include the following: Bacitracin ointment (Baciguent) ● Chloramphenicol cream (Chloromycetin) ● Erythromycin ointment (EryDerm, others) ● Gentamicin cream and ointment (Garamycin) ● Mupirocin (Bactroban) ● Neomycin (Myciguent) or neomycin with polymyxin B (Neosporin), cream and ointment ● Tetracycline (Topicycline) ● Fungal infections of the skin or nails commonly occur in warm, moist areas of the skin covered by clothing, such as tinea pedis (athlete’s foot) and tinea cruris (jock itch). Tinea capitis (ringworm of the scalp) and tinea unguium (nails) are also common. These pathogens are responsive to therapy with topical OTC antifungal agents such as undecylenic acid (Cruex, Desenex, others). More serious fungal infections of the skin and mucous membranes, such as Candida albicans infections that occur in immunocompromised clients, require systemic antifungals (Chapter 35 ). Clotrimazole (Mycelex, Lotrimin, others) and miconazole (Monistat, others) are common antifungals used for a variety of dermatologic mycoses. Some viral infections of the skin are considered diseases of childhood. These include varicella (chicken pox), rubeola (measles), and rubella (German measles). Usually, these infections are self-limiting and nonspecific, so treatment is directed at controlling the extent of skin lesions. Viral infections of the skin in adults include herpes zoster (shingles) and herpes simplex (cold sores and genital lesions). Pharmacotherapy of severe or persistent viral skin lesions may include topical or oral antiviral therapy with acyclovir (Zovirax), as discussed in Chapter 36 . ● Figure 48.2 Scabies Source: Courtesy of Dr. Jason L. Smith. is intense itching; vigorous scratching may lead to secondary infections. Scabies is readily spread through contact with upholstery and shared bed and bath linens. Lice are larger than mites, measuring from 1 to 4 mm in length. They are readily spread by infected clothing or close personal contact. These parasites require human blood for survival and die within 24 hours without the blood of a human host. Lice (singular: louse) often infest the pubic area or the scalp and lay eggs, referred to as nits, which attach to body hairs. Head lice are referred to as Pediculus capitis (● Figure 48.3), body lice as P. corpus, and pubic lice as Phthirus pubis. The pubic louse is referred to as a crab louse, because it looks like a tiny crab when viewed under the microscope. Individuals with pubic lice will sometimes say that they have “crabs.” Pubic lice may produce sky-blue SKIN PARASITES Common skin parasites include mites and lice. Scabies is an eruption of the skin caused by the female mite, Sarcoptes scabiei, which burrows into the skin to lay eggs that hatch after about 5 days. Scabies mites are barely visible without magnification and are smaller than lice. Scabies lesions most commonly occur between the fingers, on the extremities, in axillary and gluteal folds, around the trunk, and in the pubic area, as shown in ● Figure 48.2. The major symptom ● Figure 48.3 L. Smith. Pediculus capitis Source: Courtesy of Dr. Jason ADAMMC48_0131756656 2/21/07 12:28 AM Page 757 TEAM-B TAEM B:Desktop Folder: Chapter 48 Drugs for Skin Disorders macules on the inner thighs or lower abdomen. The bite of the louse and the release of saliva into the wound lead to intense itching followed by vigorous scratching. Secondary infections can result from scratching. 48.4 Pharmacotherapy With Scabicides and Pediculicides Scabicides are drugs that kill mites, and pediculicides are drugs that kill lice. Some drugs are effective against both types of parasites. The choice of drug may depend on where the infestation is located, as well as other factors such as age, pregnancy, or breast-feeding. The current drug of choice for lice is permethrin, a chemical derived from chrysanthemum flowers and formulated as a 1% liquid (Nix). This drug is considered the safest agent, especially for infants and children. Pyrethrin (RID, others) is a related product also obtained from the chrysanthemum plant. Permethrin and pyrethrins, which are also widely used as insecticides on crops and livestock, kill lice and their eggs on contact. These agents are effective in about 90% to 99% of clients, although a repeat application may be needed. Side effects are generally minor and include stinging, itching, or tingling. Malathion (Ovide) is an alternative for resistant organisms. Permethrin is also a preferred agent for scabies. The 5% cream (Elimite) is applied to the entire skin surface and allowed to remain for 8 to 14 hours before bathing. A single application cures 95% of the clients, although itching may PROTOTYPE DRUG Lindane (Kwell) continue for several weeks as the dead mites are removed from the skin. Crotamiton (Eurax) is an alternative scabicide available by prescription as a 10% cream. The traditional drug of choice for many decades for both mites and lice was lindane (Kwell, Scabene). Lindane was also widely used as an agricultural pesticide in the 1950s and 1960s, causing pollution of waterways and prompting restrictions on its use. Because lindane has the potential to cause serious nervous system toxicity, it is prescribed only after other less toxic drugs have failed to produce a therapeutic response. All scabicides and pediculicides must be used strictly as directed, because their excessive use can cause serious systemic effects and skin irritation. Drugs for the treatment of lice or mites must not be applied to the mouth, open skin lesions, or eyes, because this will cause severe irritation. NURSING CONSIDERATIONS The role of the nurse in scabicide and pediculicide therapy involves careful monitoring of a client’s condition and providing education as it relates to the prescribed drug treatment. Before assessing the client, be sure to don gloves. Assess the client’s hair and skin for evidence of lice, nits, or scabies. Assess the axilla, neckline, hairline, groin, and beltline areas for evidence of lice, such as visualization of nits, erythema, and pruritus. Look for evidence of scabies— small, pimplelike areas of redness noted in these areas and in webbing between fingers, on wrist, in skin folds, and in genital areas. Scabicide/Pediculocide ACTIONS AND USES Lindane is marketed as a cream or lotion for mites, and as a shampoo for head lice. Lindane cream or lotion takes longer to produce its effect; therefore, it is usually left on the body for about 8 to 12 hours before rinsing. Lindane shampoo is applied and left on for at least 5 minutes before rinsing. Clients should be aware that penetration of the skin with mites causes itching, which lasts up to 2 or 3 weeks even after the parasites have been killed. Lindane is absorbed directly into lice, mites, and their eggs, producing seizure and death of the parasites. Treatment may be reapplied in 24 hours when there is evidence of live lice or in 7 days for continued evidence that live mites are present. ADMINISTRATION ALERTS ■ Do not use on premature infants and children younger than 2 years. ■ Do not use on areas of skin that have abrasions, rash, or inflammation. ■ Pregnancy category C. PHARMACOKINETICS Onset: Rapid Peak: Unknown Half-life: 18 h Duration: 3 h 757 ADVERSE EFFECTS Lindane is absorbed across the skin and can cause systemic effects. CNS adverse effects include restlessness, dizziness, tremors, or convulsions (usually after misuse or accidental ingestion), and local irritation. If inhaled, lindane may cause headaches, nausea, vomiting, or irritation of the ears, nose, or throat. Contraindications: Topical lindane is contraindicated for premature neonates, clients crusted scabies and those with hypersensitivity to the drug. It is also contraindicated for clients with known seizure disorders. INTERACTIONS Drug–Drug: No clinically significant interactions have been documented. Lab Tests: Unknown. Herbal/Food: Unknown. Treatment of Overdose: Oral overdose causes CNS excitation and possibly convulsions that can be reversed with diazepam or a barbiturate. ADAMMC48_0131756656 2/21/07 12:28 AM Page 758 TEAM-B TAEM B:Desktop Folder: 758 Unit 9 The Integumentary System Eyes/Ears SPECIAL CONSIDERATIONS Follow application instructions exactly. After treatment for head lice, remove all nits from the hair shaft with a nit comb or a fine-tooth comb. Remove all nits manually to ensure that the parasite does not recur. ● Notify those who may have been exposed to or have been in close contact with the individual who is infected. ● For a child in day care, notify caregivers so that others may be assessed for possible infestation. ● Keep medication out of reach of children, because it is highly toxic if swallowed or inhaled. ● If breast-feeding, use another source of milk for a minimum of 4 days after using medication. ● If applying medication such as lindane to an infant’s skin, do not allow the medication to touch other skin areas. ● To prevent further infestation or recurrence, wash all bedding in hot water and dry in the dryer on maximum heat. If materials are nonwashable, have them dry cleaned. ● Place stuffed animals or other objects that cannot be washed in plastic bags, and ensure that they are sealed completely for 2 weeks. ● Vacuum all carpets and upholstered surfaces, discard the vacuum bag or empty the container, and place in trash outside the household, ● Keep the environmental temperature at 68F to 72F and at low humidity to reduce itching and drying of skin. ● ● Psychosocial and Community Impact of Scabies and Pediculosis MediaLink The American Academy of Dermatology Children and parents, particularly those in relatively affluent areas, may express feeling unclean or that their self-esteem has been lowered when they are diagnosed with scabies or pediculosis. Some clients think that only homeless persons or people of low income get these disorders. Educate the client and family members about the ways in which people contract scabies or pediculosis and the ways in which these infestations may be prevented. Help those affected to maintain their self-esteem and adopt a healthy attitude. Persons with scabies or pediculosis may tend to isolate socially, but this is unnecessary if precautions are taken to not share clothing, combs, or other hygiene supplies or have bodily contact with others. Scabies or lice can rapidly spread in a school, nursing home, residential treatment center, or hospital and become a community health problem. School nurses must assess the potential for students or clients contacting scabies or lice and take preventive measures. This may include frequent assessments of the hair, scalp, and exposed skin, and elimination of coat and hat racks and opportunities to share or swap clothing and/or towels. School children and their families need education on prevention and treatment. Clients and their families reporting scabies or pediculosis to the nurse should be treated in an accepting, professional, helpful manner. Obtain a thorough history regarding onset of symptoms and possible exposure to others. Take a history of epilepsy, pregnancy, lactation, allergies, and use of over-the-counter (OTC) or other home remedies to treat the current condition. If the client has lesions, assess the skin for abrasions, rashes, and open areas to determine any sites that might be prone to irritation from the topical medication. Follow application instructions, and wear gloves when applying medication. Cleanse the lesions and surrounding areas with warm water and soap, and dry thoroughly prior to applying medication. Cleansing of the lesions prior to and between applications of medication reduces the risk of secondary infections. If the medication is applied incorrectly or ingested, the client may experience headaches, nausea, vomiting, dizziness, tremors, restlessness, convulsions, and irritation of the nose, ears, or throat. Lifespan Considerations. Most medications for the treatment of skin parasites are contraindicated or should be used cautiously in pregnant or lactating women and young children. Assess women of childbearing age for the possibility of pregnancy, and ask if they are breast-feeding. Lindane (Kwell) is contraindicated in premature infants and should not be applied to children younger than 2 years of age because of increased risk of central nervous system (CNS) toxicity. Lindane is used cautiously in children ages 2 to 10 and only after other agents have been unsuccessful in treating the condition. Lower dosages are typically prescribed for children and elderly clients. Client Teaching. Client teaching regarding scabicides and pediculicides should include the goals of the therapy, the reasons for obtaining baseline data such as vital signs and the existence of underlying disorders, and possible drug side effects. Include the following points when teaching clients about scabicides or pediculicides: SUNBURN AND MINOR BURNS Burns are a unique type of stress that may affect all layers of the skin. Minor, first-degree burns affect only the outer layers of the epidermis, are characterized by redness, and are analogous to sunburn. Sunburn results from overexposure of the skin to ultraviolet light, and is associated with light skin complexions, prolonged exposure to the sun during the more hazardous hours of the day (10 A.M. until 3 P.M.), and lack of protective clothing when outdoors. Chronic sun exposure can result in serious conditions, including eye injury, cataracts, and skin cancer. 48.5 Pharmacotherapy of Sunburn and Minor Skin Irritation The best treatment for sunburn is prevention. Clients must be reminded of the acute and chronic hazards of exposure to direct sunlight. Liberal application of a lotion or oil having a very high SPF (sun protection factor) that protects against UVA and UVB rays, to areas of skin directly exposed to sunlight is strongly recommended. In addition to producing local skin damage, sun overexposure releases toxins that may produce systemic effects. The signs and symptoms of sunburn include erythema, intense pain, nausea, vomiting, chills, edema, and headache. These symptoms usually resolve within a matter of hours or days, depending on the severity of the exposure. Once ADAMMC48_0131756656 2/21/07 12:28 AM Page 759 TEAM-B TAEM B:Desktop Folder: Chapter 48 Drugs for Skin Disorders 759 NURSING PROCESS FOCUS Clients Receiving Lindane (Kwell) Assessment Potential Nursing Diagnoses Prior to administration: Obtain a complete history including age, allergies, drug history, possible drug interactions, and seizure disorders. Obtain a social history of close contacts, including household members and sexual partners. Assess vital signs. Assess skin for presence of lice and/or mite infestation, skin lesions, raw or inflamed skin, and open areas. Assess pregnancy and lactation status. ■ ■ ■ ■ ■ Knowledge, Deficient, related to no previous experience with lice or mite treatment Noncompliance, Potential for, related to knowledge deficit and embarrassment Skin Integrity, Impaired, related to lesions and pruritus ■ ■ ■ Planning: Client Goals and Expected Outcomes The client will: Be free of lice or mites and experience no reinfestation of self or other family members. Verbalize an understanding of how lice and mites are spread, proper administration of lindane, necessary household hygiene, and the need to notify household members, sexual partners, and other close contacts, such as classmates, of infestation. Exhibit skin that is intact and free of secondary infection and irritation. Demonstrate an understanding of the drug’s action by accurately describing drug side effects and precautions. ■ ■ ■ ■ Implementation Interventions and (Rationales) ■ Client Teaching/Discharge Planning Monitor for presence of lice or mites. (This determines the effectiveness of drug therapy.) Instruct client and caregiver to: Examine for nits on hair shafts; lice on skin or clothes, inner thigh areas, seams of clothes that come in contact with axilla, neckline, or beltline. Examine for mites between the fingers, on the extremities, in axillary and gluteal folds, around the trunk, and in the pubic area. ■ ■ ■ Apply lindane properly. (Proper application is critical to eliminating infestation.) Instruct client and caregiver: To wear gloves during application. To remove all skin lotions, creams, and oil-based hair products completely by scrubbing the whole body well with soap and water, and drying the skin prior to application To apply lindane to clean and dry affected body area as directed, using no more than 2 oz per application. To avoid contact with the product on an infant’s skin. That eyelashes can be treated with the application of petroleum jelly twice a day for 8 days followed by combing to remove nits. To comb affected hair with a fine-tooth comb, following lindane application, making sure to remove all nits. To treat all household members and sexual contacts immediately. To recheck affected hair or skin daily for 1 week after treatment. ■ ■ ■ ■ ■ ■ ■ ■ ■ Inform client and caregivers about proper care of clothing and equipment. (Contaminated articles will cause reinfestation.) Instruct client and caregiver to: Wash all bedding and clothing in hot water, and to dry-clean all nonwashable items that came in close contact with client. Clean combs and brushes with lindane shampoo and rinse thoroughly. ■ ■ Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that client goals and expected outcomes have been met (see “Planning”). Client and significant others are free of lice or mites and reinfestation. Client verbalizes an understanding of how lice and mites are spread, proper administration of lindane, and necessary household hygiene, and has notified household members, sexual partners, and other close contacts, such as classmates, of infestation. The client’s skin is intact and free of secondary infection and irritation. The client demonstrates an understanding of the drug’s action by accurately stating drug side effects and precautions. ■ ■ ■ ■ ADAMMC48_0131756656 2/21/07 12:28 AM Page 760 TEAM-B TAEM B:Desktop Folder: 760 Unit 9 The Integumentary System Eyes/Ears PROTOTYPE DRUG Benzocaine (Solarcaine, others) ACTIONS AND USES Benzocaine is an ester-type local anesthetic that provides temporary relief for pain and discomfort in cases of sunburn, pruritus, minor wounds, and insect bites. Its pharmacological action is caused by local anesthesia of skin receptor nerve endings. Preparations are also available to treat specific areas such as the ear, mouth, and throat, and rectal and genital areas. ADMINISTRATION ALERTS Do not use benzocaine to treat clients with open lesions or traumatized mucosal lesions. ■ Clients should use preparations only in areas of the body for which the medication is intended. ■ Pregnancy category C. ■ PHARMACOKINETICS Onset: Immediate Peak: 1 min Half-life: Unknown Duration: 15–30 min sunburn has occurred, medications can only alleviate the symptoms; they do not speed recovery time. Treatment for sunburn consists of addressing symptoms with soothing lotions, rest, prevention of dehydration, and topical anesthetic agents, if needed. Treatment is usually done on an outpatient basis. Topical anesthetics for minor burns include benzocaine (Solarcaine), dibucaine (Nupercainal), lidocaine (Xylocaine), and tetracaine HCl (Pontocaine). Aloe vera is a popular natural therapy for minor skin irritations and burns. These same agents may also provide relief from minor pain due to insect bites and pruritus. In more severe cases, oral analgesics such as aspirin or ibuprofen may be indicated. NURSING CONSIDERATIONS The role of the nurse in drug therapy for sunburn and minor skin irritation involves careful monitoring of a client’s condition and providing education as it relates to the prescribed drug treatment. Assess the sunburn, including location, portion of body surface area, edema, erythema, and blistering. For severe cases, especially those sunburns that affect a large portion of the body surface area, assess for fever, chills, weakness, and shock. Obtain a thorough history including sunburn and tanning history, the amount of time the client usually spends in the sun, how easily the client burns, and what type of sun protection is used. If the client uses a sunscreen, obtain the SPF rating. As part of the history, obtain allergies to any medications and use of OTC products or home remedies to treat the sunburn. If topical anesthetics or ointments are ordered, assess the skin for secondary infections, in which these medications are contraindicated. Topical benzocaine (Solarcaine) may cause a Topical Anesthetic ADVERSE EFFECTS Benzocaine has a low toxicity; anaphylaxis is rare, though possible. There are some reports of methemoglobinemia in infants. If prescribed in a spray form, avoid inhalation. Inhalation of benzocaine may cause methemoglobinemia. Contraindications: This drug is contraindicated in clients with hypersensitivity to “caine” anesthetics or to sunscreens containing PABA. INTERACTIONS Drug–Drug: Benzocaine may interfere with the activity of some antibacterial sulfonamides. Lab Tests: Unknown. Herbal/Food: Unknown. Treatment of Overdose: Overdose by the topical route is unlikely. See the Companion Website for a Nursing Process Focus specific to this drug. hypersensitivity reaction. For clients using the medication for the first time, a trial application on a small area of skin should be conducted to assess for an allergic reaction. If no adverse effects occur within 30 to 60 minutes, the medication may be applied to the entire area of sunburn. Lifespan Considerations. Education regarding sunburn prevention in clients of all ages is important. Infants and young children are vulnerable to sun exposure and should always be protected with a sunscreen with an SPF of 15 or higher. Client Teaching. Client education as it relates to sunburn and minor skin irritation should include the goals of therapy, the reasons for obtaining baseline data such as vital signs and the existence of underlying disorders, and possible drug side effects. Include the following points when teaching clients about sunburn and minor skin irritations: Avoid applying medication to open or infected areas of skin. ● Drink plenty of water to avoid dehydration. ● Report severe, persistent pain. ● Avoid sun exposure while receiving treatment. ● Prevent sunburn in the future by wearing protective clothing such as long-sleeved shirts and large-brim hats, and by using sunscreen with an SPF of 15 or greater. ● Follow the directions regarding use and reapplication of sunscreen after swimming or sweating. ● Refrigerate topical lotions so they will provide a soothing, cooling effect when applied. ● Avoid the use of benzocaine on infants and young children. ● ADAMMC48_0131756656 2/21/07 12:28 AM Page 761 TEAM-B TAEM B:Desktop Folder: Chapter 48 Drugs for Skin Disorders 761 ACNE AND ROSACEA Acne vulgaris is a common condition, affecting 80% of adolescents. Although acne occurs most often in teenagers, it is not unusual to find clients with acne who are older than 30 years, a condition referred to as mature acne or acne tardive. Acne vulgaris is more common in men but tends to persist longer in women. Factors associated with acne vulgaris include seborrhea, the overproduction of sebum by oil glands, and abnormal formation of keratin that blocks oil glands. The bacterium Propionibacterium acnes grows within oil gland openings and changes sebum to an acidic and irritating substance. As a result, small inflamed bumps appear on the surface of the skin. Other factors associated with acne include androgens, which stimulate the sebaceous glands to produce more sebum. This is clearly evident in teenage boys and in clients who are administered testosterone. Acne lesions include open and closed comedones. Blackheads, or open comedones, occur when sebum has plugged the oil gland, causing it to become black because of the presence of melanin granules. Whiteheads, or closed comedones, develop just beneath the surface of the skin and appear white rather than black. Rosacea is another skin disorder with lesions affecting mainly the face. Unlike acne, which most commonly affects teenagers, rosacea is a progressive disorder with an onset between 30 and 50 years of age. Rosacea is characterized by small papules or inflammatory bumps without pus that swell, thicken, and become painful, as shown in ● Figure 48.4. The face takes on a reddened or flushed appearance, particularly around the nose and cheek area. With time, the redness becomes more permanent, and lesions resembling acne appear. ● Figure 48.4 Rosacea Source: Courtesy of Dr. Jason L. Smith. The soft tissues of the nose may thicken, giving the nose a reddened, bullous, irregular swelling called rhinophyma. Rosacea is exacerbated by factors such as sunlight, stress, increased temperature, and agents that dilate facial blood vessels including alcohol, spicy foods, skin care products, and warm beverages. It affects more women than men, although men more often develop rhinophyma. 48.6 Pharmacotherapy of Acne and Acne-related Disorders Medications used for acne and related disorders are available OTC and by prescription. Because of their increased toxicity, prescription agents are reserved for more severe, persistent cases. These drugs are listed in Table 48.3. Benzoyl peroxide (Benzalin, Fostex, others) is the most common topical OTC medication for acne. Benzoyl peroxide has a keratolytic effect, which helps dry out and shed the TABLE 48.3 Drugs for Acne and Acne-related Disorders Drug Remarks OTC AGENT benzoyl peroxide (Benzacin, Benzamyclin, others) Sometimes combined with tetracycline, erythromycin, or clindamycin in severe cases, to fight bacterial infection PRESCRIPTION AGENTS (TOPICAL) adapalene (Differin) Retinoid-like compound used to treat acne formation azelaic acid (Azelex, Finacea, others) For mild to moderate inflammatory acne sulfacetamide sodium (Cetamide, Klaron, others) For sensitive skin; sometimes combined with sulfur to promote peeling, as in the condition rosacea; also used for conjunctivitis tretinoin (Retin-A, others) To prevent clogging of pore follicles; also used for the treatment of acute promyelocytic leukemia and wrinkles PRESCRIPTION AGENTS (ORAL) ethinyl estradiol (Estinyl) Oral contraceptives are sometimes used for acne; example: ethinyl estradiol plus norgestimate (Ortho Tri-Cyclen-28). doxycycline (Doryx, Vibramycin) Antibiotic; refer to Chapter 34 isotretinoin (Accutane) For acne with cysts or acne formed in small, rounded masses; pregnancy category X tetracycline hydrochloride (Achromycin, Panmycin, Sumycin) (see page 495 for the Prototype Drug box ) Antibiotic; refer to Chapter 34 . . ADAMMC48_0131756656 2/21/07 12:28 AM Page 762 TEAM-B TAEM B:Desktop Folder: 762 Unit 9 The Integumentary System Eyes/Ears outer layer of epidermis. In addition, this drug suppresses sebum production and exhibits rapid bacteriostatic action against P. acnes. Benzoyl peroxide is available as a topical lotion, cream, or gel in various percent concentrations. The drug is very safe, with local redness, irritation, and drying being the most common side effects. Other keratolytic agents used for severe acne include resorcinol, salicylic acid, and sulfur. Retinoids are a class of drug closely related to vitamin A that are used in the treatment of inflammatory skin conditions, dermatologic malignancies, and acne. The topical formulations are often drugs of choice for clients with mild to moderate acne. Tretinoin (Retin-A) is an older drug with an irritant action that decreases comedone formation and increases extrusion of comedones from the skin. Tretinoin also has the ability to improve photodamaged skin and is for wrinkle removal. Other retinoids include isotretinoin (Accutane), an oral vitamin A metabolite medication that aids in reducing the size of sebaceous glands, thereby decreasing oil production and the occurrence of clogged pores. Therapy with retinoids may require 8 to 12 weeks to achieve maximum PROTOTYPE DRUG Isotretinoin (Accutane) ACTIONS AND USES The principal action of isotretinoin is regulation of skin growth and turnover. As cells from the stratum germinativum grow toward the surface, skin cells are lost from the stratum pore openings, and their replacement is slowed. Isotretinoin also decreases oil production by reducing the size and number of oil glands. Symptoms take 4 to 8 weeks to improve, and maximum therapeutic benefit may take 5 to 6 months. Because of potentially serious adverse effects, this drug is most often reserved for cystic acne or severe keratinization disorders. ADMINISTRATION ALERTS Do not use in clients with a history of severe depression or suicidal ideation. ■ Take with meals to minimize GI distress. ■ Pregnancy category X. effectiveness. Common reactions to retinoids include burning, stinging, and sensitivity to sunlight. Adapalene (Differin) is a third-generation retinoid that causes less imitation than the older agents. Additional retinoid-like agents and related compounds used to treat acne are listed in Table 48.3. Antibiotics are sometimes used in combination with acne medications to lessen the severe redness and inflammation associated with the disorder. Doxycycline (Vibramycin, others) and tetracycline (Achromycin) have been the traditional antibiotics used in acne therapy. Topical erythromycin is an alternative for clients with microorganisms resistant to tetracyclines. Oral contraceptives containing ethinyl estradiol and norgestimate are also used to help clear the skin of acne. The agents are reserved for women who are unable to take oral antibiotics or when antibiotic therapy has proved ineffective. For the actions and contraindications of oral contraceptives, see Chapter 45 . Pharmacotherapy for rosacea includes a number of drugs given for acne vulgaris, including isotretinoin (Accutane), topical azelaic acid 20% cream (Finacea, Finevin), sulfacetamide Antiacne Agent/Retinoid ADVERSE EFFECTS Isotretinoin is a toxic metabolite of retinol or vitamin A. Common adverse effects are conjunctivitis, dry mouth, inflammation of the lips, dry nose, increased serum concentrations of triglycerides (by 50% to 70%), bone and joint pain, and photosensitivity. Liver function, serum glucose, and serum triglyceride tests should be obtained when taking isotretinoin. Contraindications: This drug causes birth defects and is contraindicated during lactation, pregnancy, or suspected pregnancy. Pregnancy testing is advised before starting therapy in female clients of childbearing age. Isotretinoin is also contraindicated in clients who have leucopenia or neutropenia or who are hypersensitive to the drug. ■ PHARMACOKINETICS Onset: Unknown Peak: 3.2 h Half-life: 10–20 h Duration: Unknown INTERACTIONS Drug–Drug: Use with vitamin A supplements increases the toxicity of isotretinoin. Tetracycline or minocycline use may increase risk of pseudotumor cerebri. concurrent use of hypoglycemic agents may lead to loss of glycemic control as well as increased risk for cardiovascular disease, secondary to elevated triglyceride levels. Isotretinoin decreases blood levels of carbamazepine, possibly leading to increased seizure activity. Isotretinoin is suspected of decreasing the effectiveness of certain contraceptives; therefore, it is critical that female clients of childbearing potential use two forms of effective contraception simultaneously. Lab Tests: The following values may be increased: plasma triglycerides, cholesterol, alkaline phosphatase (ALP), aspartate aminotransferase (AST), alanine aminotransferase (ALT), lactate dehydrogenase (LDH), fasting blood glucose, creatine phosphokinase (CPK), and serum uric acid. The following values may be decreased: serum HDL, white blood cells, and platelets. Herbal/Food: The oral absorption of isotretinoin is increased if taken with a high-fat meal. St. John’s wort should not be taken with isotretinoin because concurrent use may cause depression. In addition, pregnancies have been reported by users of certain contraceptives who also used St. John’s wort. Treatment of Overdose: Symptoms of overdose are nonspecific and resolve with symptomatic treatment. ADAMMC48_0131756656 2/21/07 12:28 AM Page 763 TEAM-B TAEM B:Desktop Folder: Chapter 48 Drugs for Skin Disorders 763 NURSING PROCESS FOCUS Clients Receiving Isotretinoin (Accutane) Assessment Potential Nursing Diagnosesm Prior to administration: Obtain a complete health history including allergies, drug history, and possible drug interactions. Obtain pregnancy and lactation status. Assess for history of psychiatric disorders. Assess vital signs to obtain baseline information. ■ ■ ■ ■ ■ ■ ■ ■ Body Image, Disturbed, related to presence of acne and possible worsening of symptoms after initiation of treatment Decisional Conflict, related to desire for pregnancy, and necessity of preventing pregnancy during therapy with isotretinoin Noncompliance, related to length of treatment time or failure to use effective contraception Skin Integrity, Impaired, related to inflammation, redness, and scaling secondary to treatment Planning: Client Goals and Expected Outcomes The client will: Experience decreased acne, without side effects or adverse reactions. Demonstrate acceptance of body image. Demonstrate an understanding of the drug’s action by accurately describing drug side effects and precautions. Use contraceptive measures to prevent pregnancy while taking medication. Comply with treatment regimen by keeping all scheduled appointments and laboratory visits for testing. ■ ■ ■ ■ ■ Implementation Interventions and (Rationales) ■ ■ Monitor lab studies during treatment, including blood glucose. (Monitoring of lab values is important in determining complications or serious side effects.) Discuss potential adverse reactions to drug therapy. (Understanding of drug effects is important for compliance.) Client Education/Discharge Planning ■ Instruct client to keep laboratory appointments prior to therapy and periodically during therapy, and if diabetic, to perform home blood glucose monitoring. Instruct client: To use two forms of reliable birth control for 1 month before beginning treatment, during treatment, and for 1 month following completion of treatment. Not to donate blood during treatment and for a minimum of 4 weeks after completion of treatment; isotretinoin in donated blood could cause fetal damage if given to a pregnant woman. To talk with pediatrician about alternative methods of feeding, if breast-feeding. To avoid use of vitamin A products. ■ ■ ■ ■ ■ ■ ■ ■ Monitor for cardiovascular problems. (Use isotretinoin with caution in clients with heart block, especially if client is also taking a beta-blocker.) Monitor emotional health. (Client may become depressed secondary to acne itself, length of treatment, possibility of worsening symptoms at beginning of treatment, changed body image, or drug itself.) Monitor CBC, blood lipid levels, glucose levels, liver function tests, eye exam, GI status, and urinalysis. (Monitoring of lab values is important in assessing for complications or serious side effects.) Monitor for vision changes. (Corneal opacities and/or cataracts may develop as result of isotretinoin use. Dryness of eyes during treatment is common. Night vision may be diminished during treatment.) ■ Discuss with client importance of complete disclosure regarding medical history and medications. Instruct client: To report signs of depression immediately and discontinue isotretinoin. To report any feelings of suicide. ■ ■ ■ Teach client importance of a complete workup prior to starting isotretinoin therapy and periodically during course of treatment. Instruct client: To report any decreased vision and discontinue use of isotretinoin. To avoid driving at night if possible. That use of artificial tears may relieve dry eyes. That use of contact lenses may need to be discontinued during therapy. ■ ■ ■ ■ ■ Monitor alcohol use. (Alcohol use with isotretinoin leads to increased triglyceride levels.) Advise client to: Eliminate or greatly reduce alcohol use, including alcohol-containing preparations such as mouthwashes or OTC medications, especially products containing acetaminophen. Read labels for alcohol content. ■ ■ (Continued) ADAMMC48_0131756656 2/21/07 12:28 AM Page 764 TEAM-B TAEM B:Desktop Folder: 764 Unit 9 The Integumentary System Eyes/Ears NURSING PROCESS FOCUS Clients Receiving Isotretinoin (Accutane) (Continued) Implementation Client Education/Discharge Planning Interventions and (Rationales) ■ Monitor skin problems. (This will determine the effectiveness of drug therapy.) Advise client: That acne may worsen during beginning of treatment. To monitor skin for improvement in 4 to 8 weeks; if no improvement is noted, client should contact primary healthcare provider. ■ ■ ■ Monitor for side effects. (Side effects may point to potential complications and noncompliance with drug regimen.) ■ Instruct client to be aware of and to report headache (especially if accompanied by nausea and vomiting), fatigue, depression, lethargy, severe diarrhea, rectal bleeding, abdominal pain, visual changes, dry mouth, hematuria, proteinuria, and liver dysfunction (jaundice, pruritus, dark urine). Evaluation of Outcome Criteria Evaluate the effectiveness of drug therapy by confirming that client goals and expected outcomes have been met (see “Planning”). The client reports decreased acne, without side effects or adverse reactions. The client verbalizes acceptance of body image. The client demonstrates an understanding of the drug’s action by accurately drug side effects and precautions. The client uses contraceptive measures to prevent pregnancy while taking medication. The client keeps all scheduled appointments and laboratory visits for testing. ■ ■ ■ ■ ■ preparations, and systemic antibiotics. Metronidazole 0.75% to 1% topical preparation (MetroGel, MetroCream), an antibacterial and antiprotozoal preparation is often the drug of choice for rosacea. Crotamiton (Eurax) 10% cream or lotion may also be prescribed if hair follicle mites are present. In addition to medications, some clients receive vascular or carbon dioxide laser surgery for rhinophyma. NURSING CONSIDERATIONS The role of the nurse in drug therapy for acne-related disorders includes careful monitoring of a client’s condition and providing education as it relates to the prescribed drug treatment. Have the client undress so you can examine the extent of acne. Wear gloves when assessing the skin. Assess the anterior and posterior thorax, because many acne lesions may be found in these areas. Obtain a thorough history including onset of acne, treatments used and their effects, and whether the client is pregnant. Ask about allergies, past medical history, and current medications. Isotretinoin (Accutane) is contraindicated in individuals with a history of depression and suicidal ideation and during pregnancy. Individuals who are prescribed isotretinoin should sign a consent regarding the understanding of suicidal risks prior to treatment. Obtain a pregnancy test in all female clients of childbearing years. Isotretinoin is also contraindicated for individuals taking carbamazepine for seizures because the drug may decrease the serum levels of carbamazepine, resulting in increased seizure activity. Use of isotretinoin with hypoglycemic agents may lead to a loss of glycemic control and cardiovascular risks, because isotretinoin raises serum triglyceride levels. Lifespan Considerations. Some acne medications are contraindicated during pregnancy because they may have teratogenic effects to the fetus. Therefore, verification of pregnancy in those individuals who are sexually active is critical in treatment. If assessing a teenager, rapport must be established, because many are embarrassed or have altered body image or low self-esteem issues related to their acne. Establishing rapport prior to assessing and taking a health history allows the client to become comfortable with answering questions. Client Teaching. Client education as it relates to drugs used to treat acne should include the goals of therapy, the reasons for obtaining baseline data such as vital signs and the existence of underlying psychiatric disorders, and possible drug side effects. Include the following points when teaching clients about drugs to treat acne: Report use of any OTC medications or herbal supplements to treat acne. ● Take medications exactly as prescribed and for the designated length of time. ● Practice reliable contraception and notify your healthcare provider if pregnancy is planned or suspected. ● If breast-feeding, select a different method of feeding your baby while on medications to control acne. If you have stopped taking the acne medications, contact your healthcare provider to determine when breast-feeding may resume. ● Immediately report unusual bleeding, bruising, yellow coloration of the skin or eyes, pale stools, and darkened urine. ● If taking isotretinoin, do not donate blood for 30 days after discontinuing the medication. ● If taking isotretinoin and wearing contacts, unusual dryness of the eyes may be experienced while on this medication. ● Keep a food diary to determine foods that may make acne worse, and avoid those foods. ● ADAMMC48_0131756656 2/21/07 12:28 AM Page 765 TEAM-B TAEM B:Desktop Folder: Chapter 48 Drugs for Skin Disorders 765 NATURAL THERAPIES HOME & COMMUNITY CONSIDERATIONS Burdock Root for Acne and Eczema Skin Disorders and Self-Esteem Burdock root, Arctium lappa, comes from a thick, flowering plant sometimes found on the roadsides of Great Britain and North America. It contains several active substances such as bitter glycosides and flavonoids, and it has a range of potential actions in the body: anti-infective, diuretic, mild laxative, and skin detoxifier. Burdock root is sometimes described as an attacker of skin disorders from within because it fights bacterial infections, reduces inflammation, and treats some stages of eczema, particularly the dry and scaling phases. Some claim that it is also effective against boils and sores. Burdock root is considered safe, having few side effects or drug interactions. It contains 50% inulin, a fiber widely distributed in vegetables and fruits, and is consumed as a regular part of the daily diet in many Asian countries. In many cases, burdock root is combined with other natural products for a better range of effectiveness. Such products include sarsaparilla (Smilax officinalis), yellow dock (Rumex crispus), licorice root (Glycyrrhiza glabra), echinacea (Echinacea purpurea), and dandelion (Taraxacum officinale). Avoid products that will dry or irritate the skin such as cologne, perfumes, and other alcohol-based products. ● Report severe skin irritation or inflammation that develops while taking these medications, and discontinue use. ● DERMATITIS Dermatitis is an inflammatory skin disorder characterized by local redness, pain, and pruritus. Intense scratching may lead to excoriation, scratches that break the skin surface and fill with blood or serous fluid to form crusty scales. Dermatitis may be acute or chronic. Atopic dermatitis, or eczema, is a chronic, inflammatory skin disorder with a genetic predisposition. Clients presenting with eczema often have a family history of asthma and hay fever as well as allergies to a variety of irritants such as cosmetics, lotions, soaps, pollens, food, pet dander, and dust. About 75% of clients with atopic dermatitis have had an initial onset before 1 year of age. In those babies predisposed to eczema, breast-feeding seems to offer protection, as it is rare for a breast-fed child to develop eczema before the introduction of other foods. In infants and small children, lesions usually begin on the face and scalp, and then progress to other parts of the body. A frequent and prominent symptom in infants is the appearance of red cheeks. Contact dermatitis can be caused by a hypersensitivity response, resulting from exposure to specific natural or synthetic allergens such as plants, chemicals, latex, drugs, metals, or foreign proteins. Accompanying the allergic reaction may be various degrees of cracking, bleeding, or small blisters. Seborrheic dermatitis is sometimes seen in newborns and in teenagers after puberty, and is characterized by yellowish, oily and crusted patches of skin that appear in areas of the face, scalp, chest, back, or pubic area. Bacterial infection or dandruff may accompany these symptoms. Stasis dermatitis, a condition found primarily in the lower extremities, results from poor venous circulation. Redness and scaling may be observed in areas where venous circulation is impaired or where deep venous blood clots have formed. The individual who has skin disorders must adhere to the medical regimen to achieve the desired result. An individual’s appearance is very important to self-esteem; therefore, skin lesions may cause embarrassment and the potential for limited social contact. Educate clients about the complexity of the skin disorder, the importance of compliance with the medical regimen and lifestyle changes, which are crucial to success in managing the disorder. 48.7 Pharmacotherapy of Dermatitis Pharmacotherapy of dermatitis is symptomatic and involves lotions and ointments to control itching and skin flaking. Antihistamines may be used to control inflammation and reduce itching, and analgesics or topical anesthetics may be prescribed for pain relief. Atopic dermatitis can be controlled, but not cured, by medications. Part of the management plan must include the identification and elimination of allergic triggers that cause flare-ups. Topical glucocorticoids are the most effective treatment for controlling the inflammation and itching of dermatitis. Creams, lotions, solutions, gels, and pads containing glucocorticoids are specially formulated to penetrate deep into the skin layers. These dermatologic agents are classified by potency, as listed in Table 48.4. The high-potency agents are TABLE 48.4 Topical Glucocorticoids for Dermatitis and Related Symptoms Generic Name Trade Names HIGHEST LEVEL OF POTENCY betamethasone Benisone, Diprosone, Valisone clobetasol Dermovate, Temovate diflorasone Florone, Maxiflor, Psorcon MIDDLE LEVEL OF POTENCY amcinonide Cyclocort desoximetasone Topicort, Topicort LP fluocinonide Lidex, Lidex-E, others halcinonide Halog mometasone Elocon triamcinolone Aristocort, Kenalog, others LOWER LEVEL OF POTENCY clocortolone Cloderm fluocinolone Fluolar, Synalar, others flurandrenolide Cordran, Cordran SP fluticasone Flonase hydrocortisone Hytone, Locoid, Westcort, others LOWEST LEVEL OF POTENCY alclometasone Aclovate desonide DesOwen, Tridesilon dexamethasone Decaderm, Decadron, others ADAMMC48_0131756656 2/21/07 12:28 AM Page 766 TEAM-B TAEM B:Desktop Folder: 766 Unit 9 The Integumentary System Eyes/Ears all skin surfaces (including face and neck) because they have fewer side effects than the topical glucocorticoids. Side effects include burning and stinging on broken skin. Although these drugs are not approved for long-term therapy, research has supported their safety over several years of use. PSORIASIS ● Figure 48.5 Psoriasis Source: Courtesy of Dr. Jason L. Smith. used to treat acute flare-ups and are limited to 2 to 3 weeks of therapy. The moderate-potency formulations are for more prolonged therapy of chronic dermatitis. The lowpotency glucocorticoids are prescribed for children. Long-term glucocorticoid use may lead to irritation, redness, hypopigmentation, and thinning of the skin. Highpotency formulations are not advised for the head or neck regions because of potential adverse effects. If absorption occurs, topical glucocorticoids may produce undesirable systemic effects including adrenal insufficiency, mood changes, serum imbalances, and loss of bone mass, as discussed in Chapter 43 . To avoid serious adverse effects, careful attention must be given to the amount of glucocorticoid applied, the frequency of application, and how long it has been used. Several alternatives to the glucocorticoids are available. Clients with persistent atopic dermatitis that does not respond to glucocorticoids may benefit from oral immunosuppressive agents, such as cyclosporine. This drug is generally used for the short-term treatment of severe disease. The topical calcineurin inhibitors pimecrolimus 1% (Elidel) and tacrolimus 0.03%, 0.1% (Protopic) are available for clients older than 2 years of age. These medications may be used over Psoriasis is a chronic, noninfectious, inflammatory disorder characterized by red, raised patches of skin covered with flaky, thick, silver scales called plaques, as shown in ● Figure 48.5. These plaques shed the scales, which are sometimes grayish. The reason for the appearance of plaques is an extremely fast skin turnover rate, with skin cells reaching the surface in 4 to 7 days instead of the usual 14 days. Plaques are ultimately shed from the surface, while the underlying skin becomes inflamed and irritated. Lesion size varies, and the shape tends to be round. Lesions are usually discovered on the scalp, elbows, knees, and extensor surfaces of the arms and legs, sacrum, and occasionally around the nails. The various forms of psoriasis are described in Table 48.5. The etiology of psoriasis is incompletely understood. About 50% of the cases have a genetic basis, with a close family member also having the disorder. One theory of causation is that psoriasis is an autoimmune condition, because overactive immune cells release cytokines that increase the production of skin cells. There is also a strong environmental component to the disease: factors such as stress, smoking, alcohol, climate changes, and infections can trigger flare-ups. In addition, certain drugs act as triggers, including angiotensin-converting enzyme (ACE) inhibitors, beta-adrenergic blockers, tetracyclines, and nonsteroidal anti-inflammatory drugs (NSAIDs). 48.8 Pharmacotherapy of Psoriasis Psoriasis is cosmetically disfiguring, and clients may experience anxiety, embarrassment, or depression, causing them to avoid social interactions. The pharmacological TABLE 48.5 Types of Psoriasis Form of Psoriasis Description Most Common Location of Lesions Comments guttate (droplike) or eruptive psoriasis lesions smaller than those of psoriasis vulgaris upper trunk and extremities more common in early-onset psoriasis; can appear and resolve spontaneously a few weeks following a streptococcal respiratory infection psoriatic arthritis resembles rheumatoid arthritis fingers and toes at distal interphalangeal joints; can affect skin and nails about 20% of clients with psoriasis also have arthritis. psoriasis vulgaris lesions are papules that form into erythematous plaques with thick, silver or gray plaques that bleed when removed; plaques in dark-skinned individuals often appear purple skin over scalp, elbows, and knees; lesions possible anywhere on the body most common form; requires long-term specialized management psoriatic erythroderma or exfoliative dermatitis generalized scaling; erythema without lesions all body surfaces least common form pustular psoriasis eruption of pustules; presence of fever trunk and extremities; can appear on palms, soles, and nail beds average age of onset is 50 years ADAMMC48_0131756656 2/21/07 12:28 AM Page 767 TEAM-B TAEM B:Desktop Folder: Chapter 48 Drugs for Skin Disorders goal of psoriasis pharmacotherapy is to reduce erythema, plaques, and scales to improve the cosmetic appearance of the client, leading to more normal lifestyle activities. The condition is lifelong, and there is no pharmacological cure. 767 A number of prescription and OTC drugs are available for the treatment of psoriasis, including both topical and systemic agents, as listed in Table 48.6. Combination therapy with two or more agents is common, and drugs are often rotated to achieve the maximum therapeutic response. TABLE 48.6 Drugs for Psoriasis and Related Disorders Drug Route and Adult Dose (max dose where indicated) Adverse Effects Topical: Apply thin layer to lesions 1–2 times/day Burning, stinging, folliculitis, itching TOPICAL MEDICATIONS* calcipotriene (Dovonex) No serious adverse effects tacrolimus (Protopic) Topical: Apply thin layer to affected area bid Oral: Start with 0.05 mg/kg/day; increase to 0.1 mg/kg/day at Week 3 and to 0.15 mg/kg/day at Week 6 The following may occur if the drug is administered PO or IV: Oliguria, nausea, constipation, diarrhea, headache, abdominal pain, insomnia, peripheral edema, fever Infections, hypertension, nephrotoxicity, neurotoxicity (tremors, paresthesia, psychosis), hyperkalemia, anemia, hyperglycemia tazarotene (Tazorac) Acne: Apply thin film to clean dry area daily Plaque psoriasis: Apply thin film daily in the evening Pruritus, burning, stinging, skin irritation, transient worsening of psoriasis No serious adverse effects SYSTEMIC MEDICATIONS acitretin (Soriatane) PO; 10–50 mg/day with the main meal Dry mouth Increased triglycerides and cholesterol, paresthesias, rigors, arthralgia cyclosporine (Sandimmune, Neoral) (see page 466 for the Prototype Drug box PO; 1.25 mg/kg bid (max: 4 mg/kg/day) Hirsutism, tremor, vomiting ) Hypertension, MI, nephrotoxicity, hyperkalemia etanercept (Enbrel) Subcutaneous: 25 mg twice/wk or 0.08 mg/kg or 50 mg once/wk Local reactions at injection site (pain, erythema, myalgia), abdominal pain, vomiting, headache Infections, pancytopenia, MI, heart failure etretinate (Tegison) PO: 0.75–1 mg/kg/day (max: 1.5 mg/kg/day) Fever, headache, fatigue, double vision, nosebleeds, appetite change, sore tongue, nausea, photosensitivity, arthralgia Pseudotumor cerebri, cardiac thrombotic obstructive events, increased triglycerides and cholesterol, hepatotoxicity, malignant neoplasms hydroxyurea (Hydrea) PO: 80 mg/kg q3days or 20–30 mg/kg/day Headache, dizziness, fever, chills, nausea, vomiting Bone marrow depression, convulsions, nephrotoxicity methotrexate (Mexate, Folex) (see page 562 for the Prototype Drug box PO; 2.5–5 mg bid for 3 doses each week (max: 25–30 mg/wk) ) Headache, glossitis, gingivitis, mild leukopenia, nausea Ulcerative stomatitis, myelosuppression, aplastic anemia, hepatic cirrhosis, nephrotoxicity, sudden death, pulmonary fibrosis *See Table 48.4 for topical glucocorticoids for psoriasis. Italics indicate common adverse effects; underlining indicates serious adverse effects. ADAMMC48_0131756656 2/21/07 12:28 AM Page 768 TEAM-B TAEM B:Desktop Folder: MediaLink The National Psoriasis Foundation 768 Unit 9 The Integumentary System Eyes/Ears TOPICAL THERAPIES Topical glucocorticoids are a primary treatment for psoriasis. Examples include betamethasone (Diprosone) ointment, lotion, or cream and hydrocortisone acetate (Cortaid, Caldecort, others) cream or ointment. Topical glucocorticoids reduce the inflammation associated with fast skin turnover. As in the treatment of dermatitis, high-potency agents are used for acute flare-ups for 2 to 3 weeks. Moderate-and low-potency glucocorticoids are used for chronic therapy. Topical immunomodulators (TIMS) are another class of agents that suppress the immune system. One example is the calcineurin inhibitor tacrolimus (Protopic) ointment. Other agents applied topically are retinoid-like compounds such as calcipotriene (Dovonex), a synthetic vitamin D ointment, cream, or scalp solution; and tazarotene (Tazorac), a vitamin A derivative gel or cream. These drugs provide the same benefits as topical glucocorticoids but exhibit a lower incidence of adverse effects. Calcipotriene may produce hypercalcemia if applied over large areas of the body or used in higher doses than recommended. This drug is usually not used on an extended basis. Other skin therapy techniques may be used with or without additional psoriasis medications. These include various forms of tar treatment (coal tar) and anthralin, which are applied to the skin’s surface. Tar and anthralin inhibit DNA synthesis and arrest abnormal cell growth. These are considered second-line therapies. SYSTEMIC THERAPIES The most often prescribed systemic drug for severe psoriasis is methotrexate. Methotrexate (Folex) is used in the treatment of a variety of disorders, including carcinomas and rheumatoid arthritis, in addition to being used for the treatment of psoriasis. Methotrexate is discussed as a prototype drug on page in Chapter 37 . Other systemic drugs for psoriasis include acitretin (Soriatane) and etretinate (Tegison). These drugs are taken orally to inhibit excessive skin cell growth. Additionally, drugs used for different disorders, but which provide relief of severe psoriatic symptoms, include hydroxyurea (Hydrea) and cyclosporine (Sandimmune, Neoral). Hydroxyurea is a drug used for sickle-cell anemia. Cyclosporine is an immunosuppressive agent that was presented as a prototype drug on page in Chapter 32 . Etanercept (Enbrel) and infliximab (Remicade), which are biological therapies approved for other autoimmune conditions, have been found to improve symptoms of psoriasis. Etanercept and infliximab are classified as tumor necrosis factor (TNF) blockers. NONPHARMACOLOGICAL THERAPIES Phototherapy with UVB and UVA light is used in cases of severe psoriasis. UVB therapy is less hazardous than UVA therapy. The wavelength of UVB is similar to sunlight, and it reduces lesions covering a large area of body that normally resist topical treatments. With close supervision, this type of phototherapy can be administered at home. Keratolytic pastes are often applied between treatments. The second type of phototherapy is referred to as PUVA therapy because psoralens are often administered in conjunction with phototherapy. Psoralens are oral or topical agents that when exposed to UV light produce a photosensitive reaction. This reaction reduces the number of lesions, but unpleasant side effects such as headache, nausea, and skin sensitivity still occur, limiting the effectiveness of this therapy. Immunosuppressant drugs such as cyclosporine are not used in conjunction with PUVA therapy, because they increase the risk of skin cancer. CHAPTER REVIEW KEY CONCEPTS The numbered key concepts provide a succinct summary of the important points from the corresponding numbered section within the chapter. If any of these points are not clear, refer to the numbered section within the chapter for review. 48.1 Three layers of skin, epidermis, dermis, and subcuta48.5 The pharmacotherapy of sunburn includes the symptoneous layer, provide effective barrier defenses for the matic relief of pain using soothing lotions, topical anesbody. thetics, and analgesics. 48.2 Skin disorders that may benefit from pharmacotherapy are acne, sunburns, infections, dermatitis, and psoriasis. 48.6 The pharmacotherapy of acne includes treatment with benzoyl peroxide, retinoids, and antibiotics. Therapies for rosacea include retinoids and metronidazole. 48.3 When the skin integrity is compromised, bacteria, viruses, and fungi can gain entrance and cause infections. Anti-infective therapy may be indicated. 48.7 The most effective treatment for dermatitis is topical glucocorticoids, which are classified by their potency. 48.4 Scabicides and pediculicides are used to treat parasitic mite and lice infestations, respectively. Permethrin is an agent of choice for these infections. 48.8 Both topical and systemic drugs, including glucocorticoids, immunomodulators, and methotrexate, are used to treat psoriasis. ADAMMC48_0131756656 2/21/07 12:28 AM Page 769 TEAM-B TAEM B:Desktop Folder: Chapter 48 Drugs for Skin Disorders 769 NCLEX-RN® REVIEW QUESTIONS 1 The client is treated for head lice with lindane (Kwell). Following treatment, the nurse reinforces instructions to: 1. Remain isolated for 48 hours. 2. Inspect the hair shaft, checking for nits daily for 1 week following treatment. 3. Shampoo with Kwell three times per day. 4. Wash linens with cold water and bleach. 2 Careful attention to directions for application of lindane (Kwell) is emphasized by the nurse. Signs of overapplication include (select all that apply): 1. Nausea and vomiting. 2. Headache. 3. Eye irritation. 4. Diaphoresis. 5. Restlessness. 3 The nurse evaluates the client’s understanding of the procedure for application of lindane (Kwell). Which of the following statements requires intervention by the nurse? 1. “The cream should be left on for 8 to 12 hours before rinsing.” 2. “I will leave the shampoo on 5 minutes before rinsing.” 3. “I will leave the lotion on about 30 minutes before rinsing.” 4. “The lotion takes longer to work.” 4 The teaching plan for a 24-year-old female receiving isotretinoin (Accutane) for treatment of acne must include: 1. Avoiding the use of oral contraceptives while taking this drug. 2. Avoiding pregnancy while taking this drug. 3. Avoiding using makeup until the treatment is completed. 4. Washing the face with cool water only. 5 Methotrexate (Amethopterin) is prescribed for a client with psoriasis vulgaris. During the physical examination, the nurse expects to find the lesions on the client’s: 1. Scalp, elbows, and knees. 2. Upper trunk and extremities. 3. Fingers and toes at distal interphalangeal joints. 4. Palms of hands, soles of feet. CRITICAL THINKING QUESTIONS 1. A senior nursing student is participating in well-baby screenings at a public health clinic. While examining a 4month-old infant, the student notes an extensive, confluent diaper rash. The baby’s mother is upset and asks the student nurse about the use of OTC corticosteroid ointment and wonders how she should apply the cream. How should the student nurse respond? 2. A 14-year-old girl has been placed on oral doxycycline (DoxyCaps) for acne vulgaris because she has not responded to topical antibiotic therapy. After 3 weeks of therapy, the client returns to the dermatologist’s office complaining about episodes of nausea and epigastric pain. The nurse learns that the client is “so busy with school activities” that she often forgets a morning dose and “doubles up” on the drug before bedtime. Devise a teaching plan relevant to drug therapy that takes into consideration the major side effects of this drug and the cognitive abilities of this client. 3. A 37-year-old woman is referred to a dermatologist for increasing redness and painful “acne” lesions. The client is frustrated with her attempts to camouflage her “teenage face” with makeup. She relates to the nurse that she had acne as a teen but had no further problem until the last 11 months. After consultation, the dermatologist suggests a 3-month trial of isotretinoin (Accutane). What are the specific reproductive considerations for this client? What information should this client be provided in relation to reproductive concerns? See Appendix D for answers and rationales for all activities. www.prenhall.com/adams NCLEX-RN® review, case studies, and other interactive resources for this chapter can be found on the companion website at www.prenhall.com/adams. Click on “Chapter 48” to select the activities for this chapter. For animations, more NCLEX-RN® review questions, and an audio glossary, access the accompanying Prentice Hall Nursing MediaLink DVD-ROM in this textbook. PRENTICE HALL NURSING MEDIALINK DVD-ROM ■ ■ Audio Glossary NCLEX-RN® Review COMPANION WEBSITE NCLEX-RN® Review Dosage Calculations ■ Case Study: Acne and rosacea ■ Care Plan: Client with head lice ■ ■