Occupational exposure to aluminium phosphide and phosphine gas
advertisement

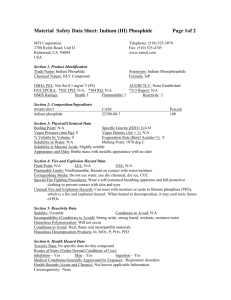
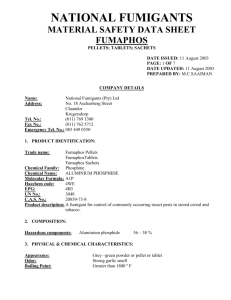
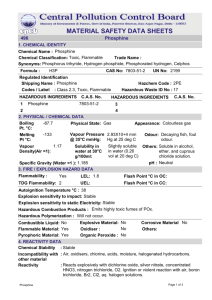
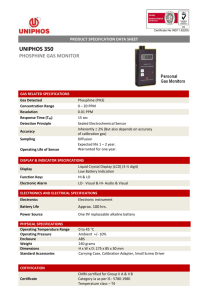
Human & Experimental Toxicology (2005) 24: 27 /33 www.hetjournal.com Occupational exposure to aluminium phosphide and phosphine gas? A suspected case report and review of the literature DL Sudakin* Department of Environmental and Molecular Toxicology, Oregon State University, Corvallis, OR, USA The manufacture and application of aluminium phosphide fumigants pose risks of inhalation exposure to phosphine gas. This article presents a case report of suspected inhalation exposure to phosphine gas in a manufacturing facility for aluminium phosphide fumigants, which was associated with acute dyspnoea, hypotension, bradycardia and other signs of intoxication. These symptoms resolved within several hours after removal from exposure. A review of the data on human exposures to phosphide fumigants identifies both pesticide applicators and individuals in the vicinity of application to be at risk of accidental exposure and injury from phosphine inhalation. More recent reports have identified risks of phosphine gas inhalation in association with the clandestine production of methamphetamine. Toxicodynamic effects of phosphine result from the inhibition of cytochrome c oxidase and subsequent generation of reactive oxygen species. There remain unanswered questions relating to the toxicokinetics of phosphine, as well as the assessment of human exposure utilizing biomarkers. As initial signs and symptoms of intoxication from phosphine gas may be nonspecific and transient, there is a need for improved recognition of the potential hazards associated with phosphide fumigants and phosphine gas. Human & Experimental Toxicology (2005) 24, 27 /33 Key words: environmental; epidemiology; fumigant; human; occupational; phosphide; phosphine; poisoning; toxicodynamics; toxicokinetics; toxicology Introduction Aluminium phosphide is a pesticide registered in the USA and many other countries for the indoor fumigation of agricultural commodities, animal feeds, processed foods and structural as well as outdoor pest control. The chemical is usually formulated in pellets, granules or as a dust. Upon contact with moisture in the environment, aluminium phosphide undergoes a chemical reaction yielding phosphine gas, which is the active pesticidal component (Figure 1). In addition to these chemical properties, phosphine may spontaneously ignite in the presence of oxygen at concentrations above a threshold limit range of 0.48 /1.9% (v/v).1 Phosphine gas has been variably described as having a garlic or fishy odour, although exposures to toxicologically relevant concentrations of phosphine can occur in the absence of obvious odour detection.2 In the USA, the occupational Permissi*Correspondence: Daniel L Sudakin, Department of Environmental and Molecular Toxicology, Oregon State University, 333 Weniger, Corvallis, OR 97331-6502, USA E-mail: sudakind@ace.orst.edu Received 7 August 2004; revised 18 November 2004; accepted 22 November 2004 – 2005 Edward Arnold (Publishers) Ltd ble Exposure Limit (PEL) for phosphine gas is 0.3 ppm. Exposure to aluminium phosphide is a relatively common cause of poisoning from agricultural chemical exposures in many countries.3 5 The risks of major morbidity and mortality associated with both accidental and intentional exposure to aluminium phosphide fumigants have been well described.6 9 Despite these risks, intoxication from phosphine inhalation can be difficult to confirm and is frequently a diagnosis of exclusion when reliable biomarkers of exposure and environmental measurements are not available.10 Risks from phosphide fumigants may increase in the future, as they are considered an alternative to the use of methyl bromide, which is currently being phased out of use as a fumigant in many countries throughout the world. The purpose of this article is to present a case of suspected occupational exposure to phosphine gas in a manufacturing facility for phosphide fumigants, and to update the available information on the epidemiology and clinical toxicology of accidental human exposures to aluminium phosphide and phosphine. Emphasis is 10.1191/0960327105ht496oa Exposure to aluminium phosphide and phosphine gas DL Sudakin 28 OH moisture Al P + aluminum phosphide 3 H2O HO + Al OH PH3 phosphine Figure 1 Aluminium phosphide and liberation of phosphine gas. placed on the need for improved recognition of individuals at risk of occupational exposure. Case report A 42-year-old male had been employed at a manufacturing facility for aluminium phosphide fumigants for over 14 years. His work involved rotation through several different steps in the manufacturing process. This process included mixing of aluminium phosphide with ammonium carbonate, tumbling of the mixture, transferring the product to a hopper, and subsequently adding talc and zinc to generate a pellet formulation. The worker described workplace safety concerns including air filters that frequently became clogged with dust generated through the manufacturing process, infrequent monitoring and documentation of phosphine gas concentrations, poor compliance with the use of required respiratory protective gear, and previous incidents of hoppers that had exploded in the workplace (Figure 2). Figure 2 Storage container for aluminium phosphide, which had previously exploded. On a day when the worker was having difficulty removing the solid product during the blending process, he acutely developed symptoms of chest pain, shortness of breath, weakness, dizziness, disorientation and nausea with an episode of vomiting. He did not experience abdominal pain or dyspepsia. The worker was not wearing respiratory protection at the time, and did not recall noticing an odour. He was taken to the company physician, who noted the worker was alert and responsive with a normal respiratory rate, but appeared pale, sweaty and acutely ill. On initial examination, the heart rate was described as very slow with distant heart sounds. The initial blood pressure was 78/58 mmHg, and a rhythm strip indicated a junctional bradycardia (58 beats/min). He was transported via ambulance to an emergency room, and it was suspected that he was having a myocardial infarction. An initial ECG showed normal sinus rhythm with nonspecific ST and T-wave abnormalities. No arrhythmias were apparent. Laboratory analyses revealed an elevated creatine phosphokinase (CK 247 U/L), with a normal CK-MB index and a normal troponin I. Other laboratory values, including a complete blood count, amylase, and renal and liver function, were within normal limits. Serum magnesium was not measured. Chest and abdominal X-rays were unremarkable. The worker had a history of gastro-oesophageal reflux disease for which he was taking medication, but no known prior history of cardiovascular disease, and a recent exercise stress test, which was unremarkable. He was admitted to the hospital with a diagnosis of acute chest pain, ruling out unstable angina. His clinical condition improved rapidly while in the emergency room, and his symptoms resolved over the next 6 hours. He did not develop arrhythmias or other clinical or laboratory signs of cardiac injury while under observation. A repeat ECG showed no significant change from the previous study. Consultation by a gastroenterology specialist revealed no evidence that the episode was gastrointestinal in origin. He was subsequently discharged to home the next day. He returned to the duties of his job, reporting changes in workplace safety procedures. These included improved engineering controls, routine monitoring for phosphine gas and appropriate use of respiratory protective equipment. The worker reported that an investigation to determine concentrations of phosphine gas in his immediate work area was not conducted on the date that he became acutely ill. Exposure to aluminium phosphide and phosphine gas DL Sudakin 29 Epidemiology of exposure to phosphide fumigants and phosphine gas The epidemiology of occupational and environmental exposure to phosphine gas in association with phosphide fumigants has been reviewed by the National Institute of Occupational Safety and Health (NIOSH).11 Relevant findings in a 10-year study of 205 symptomatic exposures included the observation that 75% of cases occurred among individuals who were not directly handling or applying the fumigants. In 63% of cases among applicators, and 45% of cases among nonapplicators, symptomatic exposure was reported to have occurred from the normal handling of phosphide fumigants (consistent with the product labelling). In this case series, approximately 25% of exposures to aluminium phosphide among applicators occurred in the context of a misapplication (handling violations).11 There were no reported occupational cases occurring among individuals involved in the manufacturing process of phosphide fumigants in this series. Another epidemiological study investigated health endpoints among Indian workers engaged in fumigation of stored grains.12 The mean duration of employment among these workers was 11.1 years, and workplace concentrations of phosphine gas ranged from 0.17 to 2.11 parts per million (ppm) during the period of investigation. In this study, workers did not use facemasks, gloves or aprons as personal protective equipment. The most frequently reported symptoms reported immediately after completing fumigation activities included headache (31.8%), dyspnoea (31.8%) and chest tightness (27.3%). Physical examinations of these workers were unremarkable, and no significant abnormalities were observed in tests of motor and sensory nerve conduction.12 Outside of the workplace, phosphide fumigants are frequently implicated in association with epidemiological reports of accidental morbidity and mortality. A three-year (1999 /2001) analysis of childhood poisonings in India found that 9% of all cases resulted from exposure to agricultural pesticides, and aluminium phosphide fumigants were the most frequently implicated classification (29.67% of cases). Most of these cases involved ingestion pathways of exposure resulting from improper storage of fumigants.3 Medical outcomes were not reported in this study. In another longitudinal, retrospective review of acute poisoning deaths in northern India, aluminium phosphide fumigants were identified as the most commonly implicated poison associated with fatalities (65% of 4 cases). In this investigation, the incidence of cases resulting in death from aluminium phosphide increased during the period of observation (1972 / 1997). This study did not provide further analysis of demographics or circumstances surrounding exposures resulting in fatalities. Morbidity and mortality have also been reported from phosphine inhalation in association with the in-transit fumigation of ships and railways.13,14 In one such report, two children and 29 of 31 adults aboard a grain freighter developed acute and severe symptoms of headache, nausea, vomiting and shortness of breath when phosphine gas escaped from a cargo hold and was transmitted to forward areas of the vessel. One child died after this exposure, and another child had evidence of myocardial injury as evidenced by abnormal ECG, echocardiography and transient elevation of creatine phosphokinase.14 A review of more recent epidemiological reports demonstrates that occupational and environmental exposure to phosphine may also occur from scenarios that do not involve phosphide fumigants. Case reports of inhalation exposure to phosphine gas have been described in association with the clandestine synthesis of methamphetamine, as phosphine can be produced from phosphorous acid that is formed when iodine and red phosphorus are combined in aqueous media. WillersRusso reported three fatalities from acute inhalation of phosphine gas, which occurred in a motel room where methamphetamine was being synthesized.15 Burgess described a case of transient symptoms of dizziness, headache, cough and diarrhoea in a law enforcement official who was investigating a clandestine methamphetamine laboratory.16 In this case, the affected individual was exposed to phosphine gas at a concentration of 2.7 ppb for 20 /30 min. Exposure assessment: phosphine gas Epidemiological reports of accidental incidents involving phosphide fumigants and phosphine gas demonstrate the difficulties that can be encountered in predicting inhalation exposure. Industrial hygiene studies provide further evidence of these challenges. A study of aluminium phosphide fumigations in grain elevators reported considerable temporal variation in the concentration of phosphine gas liberated in enclosed bins, with ambient temperature and air movement conditions significantly influencing the concentrations.17 Ventilation practices including the use of fans and aerating windows were found to reduce the phosphine gas concentrations to less than 0.3 ppm in most cases, Exposure to aluminium phosphide and phosphine gas DL Sudakin 30 although the potential for accumulation of phosphine gas to concentrations more than 0.3 ppm was noted to occur in worker areas after weekends, when windows and other ventilation systems were normally closed or not operating.17 Earlier environmental monitoring studies conducted during grain fumigations have measured concentrations of phosphine gas up to 52 ppm,18 a level which exceeds the immediately dangerous to life and health (IDLH) value of 50 ppm established by the NIOSH. A minimum set of respiratory protective measures has been recommended by NIOSH, although the implementation of effective engineering controls is considered the primary goal and means to prevent worker exposure to phosphine gas from phosphide fumigations.11 Toxicology of phosphine The clinical toxicology of aluminium phosphide and phosphine gas have been previously reviewed.19 Phosphine, a nucleophile which acts as a strong reducing agent, is capable of interacting with and inhibiting critical cellular enzymes involved in metabolic processes. Early studies of phosphine demonstrated specific inhibitory effects on mitochondrial cytochrome c oxidase.20 Experimental and observational studies have subsequently demonstrated that the inhibition of cytochrome c oxidase and other enzymes leads to the generation of superoxide radicals and cellular peroxides, and subsequent cellular injury through lipid peroxidation and other oxidant mechanisms.21,22 Results of animal studies suggest that glutathione, melatonin, vitamin C, beta-carotene and possibly other antioxidants may play an important role in reducing the effects of reactive oxidant species caused by phosphine.23,24 The four-hour inhalation LC50 of phosphine gas is 11 ppm (approximately 0.014 mg/L) in animal (rat) studies, which places it in the highest toxicity category (E.P.A. signal word ‘Danger’) for acute inhalation exposure.25 Mutagenic effects resulting from oxidative damage to DNA have been reported in vitro. 26 A cytogenetic study of phosphide fumigant applicators reported a significantly higher incidence of chromatid gaps and deletions in comparison to controls.27 A more recent investigation of genetic damage among phosphide fumigant applicators reported no significant difference in multiple endpoints (fluorescence in situ hybridization and the glycophorin A assay) between exposed and control individuals, a finding that may be partly explained by improved use of personal protective equipment.28 Accidental or intentional ingestion of aluminium phosphide results in the rapid onset of gastrointestinal signs and symptoms, including epigastric pain and recurrent, profuse vomiting.19,29 Cardiovascular manifestations of acute ingestion or inhalation exposures include hypotension and bradycardia.19 Nonspecific ST-T wave changes on electrocardiogram have been frequently reported, as well as left ventricular systolic dysfunction on echocardiogram during the initial phases of human intoxication.30 Myocardial and skeletal muscle injury can occur as a result of high level inhalation or ingestion pathways of exposure.31 Increased CK with a normal CK-MB fraction has been previously reported.32 Pulmonary injury and oedema have been described after ingestion of aluminium phosphide, as well as from environmental and occupational exposure to phosphine gas.33,34 Neurological manifestations following acute exposure include headache and dizziness,35 frequently accompanied by a normal mental state.19 Acute renal and liver injury can also develop.19,36 The prognosis from suicidal ingestion of aluminium phosphide is poor. A case fatality rate of 77.2% was reported in a case series of 408 patients.37 Very little information is available relating to the toxicokinetics of phosphine in humans. In an investigation of a series of patients with intoxication from aluminium phosphide, indicators of oxidative stress (malonyldialdehyde levels, superoxide dismutase and catalase activity) appeared to peak within 48 hours of exposure, with normalization of most indicators occurring by day 5.38 Reliable biomarkers of exposure to phosphine are not readily available,39 but one investigation reported a correlation of blood phosphine concentrations with clinical grades of toxicity in individuals with severe intoxication.40 A bedside test has been described for the diagnosis of aluminium phosphide ingestion, using gastric aspirates and paper strips impregnated with silver nitrate.41 The test was found to be positive in 100% of cases of aluminium phosphide ingestion, and negative in all controls in one case series.42 The same test was also investigated to detect phosphine in the exhaled air of patients with intoxication from aluminium phosphide ingestion, and the results were positive in 50% of cases.43 Clinical management of phosphine gas exposure The clinical management of intoxication from aluminium phosphide is supportive. The administra- Exposure to aluminium phosphide and phosphine gas DL Sudakin 31 tion of H2 receptor antagonists has been recommended after aluminium phosphide ingestion to reduce the gastric acidity and prevent further liberation of phosphine gas. As hypomagnesemia is a frequent complication of acute intoxication from phosphine gas exposure,42 and intracellular magnesium plays an important role as a co-factor in the synthesis and activity of glutathione and other antioxidants, the administration of intravenous magnesium has been investigated in cases of aluminium phosphide poisoning. In an unblinded trial of 50 patients, individuals receiving repeated doses of intravenous magnesium had significant improvement in indicators of oxidative stress (malonyldialdehyde, reduced glutathione) and a lower incidence of mortality (20%) in comparison to control subjects (44% mortality).43 More recently, the oral administration of the anti-ischaemic drug trimetazidine, which works through a metabolic mechanism of decreasing the production of oxygen-derived free radicals and stimulating the oxidative metabolism of glucose,44,45 was temporally associated with clinical improvement in a case report of occupational inhalation exposure to phosphine gas from aluminium phosphide.46 Case discussion While most of the epidemiological reports of occupational exposure to phosphide fumigants have involved pesticide applicators, risks among workers involved in the manufacturing of phosphide fumigants have not been previously described. In the current case report, a worker acutely developed severe symptoms in the course of their job duties in the production of aluminium phosphide fumigants. They were not wearing respiratory protection at the time the symptoms developed. Symptoms consistent with acute inhalation to phosphine gas included the sudden onset of chest pain, shortness of breath, weakness, dizziness, disorientation and nausea. Signs consistent with overexposure to phosphine included vomiting, hypotension, bradycardia and an abnormal elevation in the CK (with a normal CK-MB). Although the worker did not recall an odour at the time he developed symptoms, other studies have reported the absence of detectable odours among workers exposed to phosphine concentrations exceeding 50 ppm.2 A significant limitation in exposure assessment in this case is that phosphine concentrations were apparently not investigated at the time the worker became symptomatic. The role that occupational exposure to phosphine may have had in the aetiology of the worker’s symptoms was not immediately considered or investigated by the treating physicians in this case. Based upon the worker’s occupation, however, acute inhalation exposure to phosphine was plausible and the observed signs and symptoms were consistent. The rapid resolution of symptoms following removal from exposure and the apparent ruling out of alternative explanations provide additional evidence suggestive of acute intoxication from phosphine gas. Risks associated with phosphide fumigants have recently been reassessed in the USA. In 1998, the US E.P.A. completed a re-registration eligibility decision (RED) for aluminium phosphide fumigants.47 The risk assessment process identified concerns with respect to handlers (applicators) performing aeration and fumigation tasks without the use of respiratory protective equipment. Similar concerns were identified with respect to the potential risks of nonapplicators (in the vicinity of the application). A Memorandum of Agreement amending the aluminium phosphide RED was subsequently issued by E.P.A., which outlined a series of provisions intended to mitigate risks.48 These provisions include fumigant exposure monitoring studies, improved training and education for applicators, the development of fumigation management plans, and plans to review and determine whether current exposure standards for phosphine should be lowered from the current limit of 0.3 ppm. While these provisions were intended to reduce risks in the general population, this case report suggests that workers involved in the manufacture of aluminium phosphide fumigants should be considered individuals at high risk of exposure. Conclusions Inhalation exposure to phosphine gas liberated from aluminium phosphide fumigants presents risks of major morbidity and mortality. The rapid progression to life-threatening symptoms and limited data on the efficacy of therapeutic interventions pose challenges to the clinical toxicologist. This case report describes a scenario consistent with acute intoxication from the inhalation of phosphine gas at a manufacturing facility for phosphide fumigants, and adds to the more recent literature demonstrating that accidental inhalation of phosphine gas may occur from processes other than phosphide fumigation. There is a growing need for improved awareness of these risks with an emphasis on recognition, management and prevention. Exposure to aluminium phosphide and phosphine gas DL Sudakin 32 References 1 Kondo S, Tokuhashi K, Nagai H, Iwasaka M, Kaise M. Spontaneous ignition limits of silane and phosphine. Combustion Flame 1995; 101: 170. 2 Zaebst DD, Blade LM, Burroughs GE, Morelli-Schroth P, Woodfin WJ. Phosphine exposures in grain elevators during fumigations with aluminum phosphide. Appl Ind Hyg 1988; 3: 146 /54. 3 Gupta SK, Peshin SS, Srivastava A, Kaleekal T. A study of childhood poisoning at National Poisons Information Centre, All India Institute of Medical Sciences, New Delhi. J Occup Health 2003; 45: 191 /96. 4 Singh D, Jit I, Tyagi S. Changing trends in acute poisoning in Chandigarh zone: a 25-year autopsy experience from a tertiary care hospital in northern India. Am J Forensic Med Pathol 1999; 20: 203 /10. 5 Abder-Rahman HA, Battah AH, Ibraheem YM, Shomaf MS, el Batainch N. Aluminum phosphide fatalities, new local experience. Med Sci Law 2000; 40: 164 /68. 6 Deaths associated with exposure to fumigants in railroad cars / United States. Morb Mortal Wkly Rep 1994; 43: 489 /91. 7 Abder-Rahman HA, Battah AH, Ibraheem YM, Shomaf MS, el Batainch N. Aluminum phosphide fatalities, new local experience. Med Sci Law 2000; 40: 164 /68. 8 Anger F, Paysant F, Brousse F, Le N, I, Develay P, Gaillard Y, Baert A, Le Gueut MA, Pepin G, Anger JP. Fatal aluminum phosphide poisoning. J Anal Toxicol 2000; 24: 90 /92. 9 Popp W, Mentfewitz J, Götz R, Voshaar T. Phosphine poisoning in a German office. Lancet 2002; 359: 1574. 10 Schoonbroodt D, Guffens P, Jousten P, Ingels J, Grodos J. Acute phosphine poisoning? A case report and review. Acta Clin Belg 1992; 47: 280 /84. 11 National Institute of Occupational Safety and Health. NIOSH alert: preventing phosphine poisoning and explosions during fumigation . Columbus, OH: NIOSH, 2003: 99 /126, 1 /16. 12 Misra UK, Bhargava SK, Nag D, Kidwai MM, Lal MM. Occupational phosphine exposure in Indian workers. Toxicol Lett 1988; 42: 257 /63. 13 Feldstein A, Heumann M, Barnett M. Fumigant intoxication during transport of grain by railroad. J Occup Med 1991; 33: 64 /65. 14 Wilson R, Lovejoy FH, Jaeger RJ, Landrigan PL. Acute phosphine poisoning aboard a grain freighter. Epidemiologic, clinical, and pathological findings. JAMA 1980; 244: 148 /50. 15 Willers-Russo LJ. Three fatalities involving phosphine gas, produced as a result of methamphetamine manufacturing. J Forensic Sci 1999; 44: 647 /52. 16 Burgess JL. Phosphine exposure from a methamphetamine laboratory investigation. J Toxicol Clin Toxicol 2001; 39: 165 /68. 17 Reed C. Influence of environmental, structural, and behavioral factors on the presence of phosphine in worker areas during fumigations in grain elevators. J Agric Saf Health 2001; 7: 21 /34. 18 Zaebst DD, Blade LM, Burroughs GE, Morelli-Schroth P, Woodfin WJ. Phosphine exposures in grain elevators during fumigations with aluminum phosphide. Appl Ind Hyg 1988; 3: 146 /54. 19 Gupta S, Ahlawat SK. Aluminum phosphide poisoning / a review. J Toxicol Clin Toxicol 1995; 33: 19 /24. 20 Chefurka W, Kashi KP, Bond EJ. The effect of phosphine [gas toxic to insects] on electron transport in mitochondria. Pestic Biochem Physiol 1976; 6: 65 /84. 21 Bolter CJ, Chefurka W. Extramitochondrial release of hydrogen peroxide from insect and mouse liver mitochondria using the respiratory inhibitors phosphine, myxothiazol, and antimycin and spectral analysis of inhibited cytochromes. Arch Biochem Biophys 1990; 278: 65 /72. 22 Chugh SN, Arora V, Sharma A, Chugh K. Free radical scavengers and lipid peroxidation in acute aluminium phosphide poisoning. Indian J Med Res 1996; 104: 190 /93. 23 Hsu CH, Chi BC, Liu MY, Li JH, Chen CJ, Chen RY. Phosphine-induced oxidative damage in rats: role of glutathione. Toxicology 2002; 179: 1 /8. 24 Hsu CH, Han BC, Liu MY, Yeh CY, Casida JE. Phosphine-induced oxidative damage in rats: attenuation by melatonin. Free Radic Biol Med 2000; 28: 636 / 42. 25 United States Environmental Protection Agency, Office of Prevention Pesticides and Toxic Substances. Reregistration Eligibility Decision: Aluminum and Magnesium Phosphide. Washington, DC: US EPA, 1998. 26 Hsu CH, Quistad GB, Casida JE. Phosphine-induced oxidative stress in Hepa 1c1c7 cells. Toxicol Sci 1998; 46: 204. 27 Garry VF, Nelson RL, Danzl TJ, Cervenka J, Krueger LA, Griffith J, Whorton E. Human genotoxicity in phosphine-exposed fumigant applicators. Prog Clin Biol Res 1990; 340C: 367 /76. 28 Tucker JD, Moore DH, Ramsey MJ, Kato P, Langlois RG, Burroughs B, Long L, Garry VF. Multi-endpoint biological monitoring of phosphine workers. Mutat Res 2003; 536: 7 /14. 29 Singh S, Dilawari JB, Vashist R, Malhotra HS, Sharma BK. Aluminium phosphide ingestion. Br Med J (Clin Res Ed) 1985; 290: 1110 /11. 30 Gupta MS, Malik A, Sharma VK. Cardiovascular manifestations in aluminium phosphide poisoning with special reference to echocardiographic changes. J Assoc Physicians India 1995; 43: 773 /80. 31 Khosla SN, Nand N, Kumar P, Trehan V. Muscle involvement in aluminium phosphide poisoning. J Assoc Physicians India 1988; 36: 289 /90. 32 Dueñas A, Pérez-Castrillon JL, Cobos MA, Herreros V. Treatment of the cardiovascular manifestations of phosphine poisoning with trimetazidine, a new antiischemic drug. Am J Emerg Med 1999; 17: 219 /20. 33 Chugh SN, Ram S, Mehta LK, Arora BB, Malhotra KC. Adult respiratory distress syndrome following aluminium phosphide ingestion. Report of 4 cases. J Assoc Physicians India 1989; 37: 271 /72. 34 Willers-Russo LJ. Three fatalities involving phosphine gas, produced as a result of methamphetamine manufacturing. J Forensic Sci 1999; 44: 647 /52. 35 National Institute of Occupational Safety and Health. NIOSH alert: preventing phosphine poisoning and Exposure to aluminium phosphide and phosphine gas DL Sudakin 33 36 37 38 39 40 41 42 explosions during fumigation. Columbus, OH: NIOSH, 2003: 99 /126, 1 /16. Arora B, Punia RS, Kalra R, Chugh SN, Arora DR. Histopathological changes in aluminium phosphide poisoning. J Indian Med Assoc 1995; 93: 380 /81. Chugh SN, Dushyant, Ram S, Arora B, Malhotra KC. Incidence and outcome of aluminium phosphide poisoning in a hospital study. Indian J Med Res 1991; 94: 232 /35. Chugh SN, Arora V, Sharma A, Chugh K. Free radical scavengers and lipid peroxidation in acute aluminium phosphide poisoning. Indian J Med Res 1996; 104: 190 /93. Singh S. Serial blood phosphine levels in aluminium phosphide [ALP] poisoning. J Assoc Physicians India 1996; 44: 841 /42. Chugh SN, Pal R, Singh V, Seth S. Serial blood phosphine levels in acute aluminium phosphide poisoning. J Assoc Physicians India 1996; 44: 184 /85. Chugh SN, Ram S, Chugh K, Malhotra KC. Spot diagnosis of aluminium phosphide ingestion: an application of a simple test. J Assoc Physicians India 1989; 37: 219 /20. Chugh SN, Kamar P, Sharma A, Chugh K, Mittal A, Arora B. Magnesium status and parenteral magnesium 43 44 45 46 47 48 sulphate therapy in acute aluminum phosphide intoxication. Magnes Res 1994; 7: 289 /94. Chugh SN, Kolley T, Kakkar R, Chugh K, Sharma A. A critical evaluation of anti-peroxidant effect of intravenous magnesium in acute aluminium phosphide poisoning. Magnes Res 1997; 10: 225 /30. de Leiris J, Boucher F. Rationale for trimetazidine administration in myocardial ischaemia-reperfusion syndrome. Eur Heart J 1993; 14: 34 /40. Lopaschuk GD. Treating ischemic heart disease by pharmacologically improving cardiac energy metabolism. Am J Cardiol 1998; 82: 14K /17K. Dueñas A, Pérez-Castrillon JL, Cobos MA, Herreros V. Treatment of the cardiovascular manifestations of phosphine poisoning with trimetazidine, a new antiischemic drug. Am J Emerg Med 1999; 17: 219 /20. United States Environmental Protection Agency, Office of Prevention Pesticides and Toxic Substances. Reregistration Eligibility Decision: Aluminum and Magnesium Phosphide. US EPA, 1998. United States Environmental Protection Agency, Office of Prevention Pesticides and Toxic Substances. Fact Sheet on Memorandum of Agreement Amending Aluminum and Magnesium Phosphide RED. US EPA, 2001.