CHRONIC OBSTRUCTIVE PULMONARY DISEASE
by
Kevin T. Martin
BVE, RRT, RCP
RC Educational Consulting Services, Inc.
16781 Van Buren Blvd, Suite B, Riverside, CA 92504-5798
(800) 441-LUNG / (877) 367-NURS
www.RCECS.com
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
BEHAVIORAL OBJECTIVES
UPON COMPLETION OF THE READING MATERIAL, THE PRACTITIONER WILL BE
ABLE TO:
1. Identify the pulmonary diseases classified as chronic obstructive pulmonary disease (COPD).
2. Define chronic bronchitis.
3. Define emphysema.
4. List complications of chronic obstructive pulmonary disease.
5. List the physical findings the clinician notes during assessment of the COPD patient.
6. List pertinent data that is included in the general clinical history of the COPD patient.
7. Explain how jugular vein distention is used in the assessment of COPD.
8. Describe the CRX of a patient with COPD.
9. Describe the pathology of COPD.
10. Explain the structural changes in COPD patients.
11. Detail the functional changes in COPD patients.
12. Describe specific therapies that would prevent further deterioration in COPD.
13. Identify the therapies that improve the daily function for COPD patients.
14. Identify other obstructive pulmonary diseases.
15. Define Asthma.
16. Classify severe persistent asthma.
17. Describe the pathology of Bronchiectasis.
18. Explain the pathology of Cystic Fibrosis.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
2
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
COPYRIGHT © September, 1990 By RC Educational Consulting Services, Inc.
COPYRIGHT © April, 2000 By RC Educational Consulting Services, Inc.
REVISED 1994, 1995, BY KEVIN T. MARTIN, BEV, RRT, RCP
REVISED 1999 BY MICHAEL R. CARR, BA, RRT, RCP
REVISED 2002 BY SUSAN JETT LAWSON, RCP, RRT-NPS
REVISED 2005 BY HELEN SCHAAR CORNING, RRT, RCP
REVISED 2008 BY MICHAEL R. CARR, BA, RRT, RCP
(# TX 0-480-589)
ALL RIGHTS RESERVED
This course is for reference and education only. Every effort is made to ensure that the clinical
principles, procedures and practices are based on current knowledge and state of the art
information from acknowledged authorities, texts and journals. This information is not intended
as a substitution for a diagnosis or treatment given in consultation with a qualified health care
professional
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
3
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
TABLE OF CONTENTS
INTRODUCTION ...........................................................................................................................7
RISK FACTORS .............................................................................................................................7
DEFINITIONS.................................................................................................................................8
CHRONIC BRONCHITIS ...........................................................................................................8
EMPHYSEMA .............................................................................................................................8
COPD............................................................................................................................................8
DIAGNOSING COPD...........................................................................................................8
CLASSIFICATION OF COPD BY SEVERITY ..................................................................9
EPIDEMIOLOGY .........................................................................................................................10
PATHOLOGY ...............................................................................................................................11
CHRONIC BRONCHITIS .........................................................................................................12
EMPHYSEMA ...........................................................................................................................13
COPD..........................................................................................................................................14
ETIOLOGY ...................................................................................................................................16
CHRONIC BRONCHITIS .........................................................................................................16
EMPHYSEMA ...........................................................................................................................16
COPD..........................................................................................................................................18
STRUCTURAL VS FUNCTIONAL CHANGES.........................................................................19
CLINICAL HISTORY...................................................................................................................19
SYMPTOMS AND DIAGNOSIS .................................................................................................20
ACUTE EXACERBATION .......................................................................................................22
PHYSICAL EXAMINATION ...................................................................................................22
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
4
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
ABG’s.........................................................................................................................................24
PULMONARY FUNCTION TESTS (PFT'S) ...........................................................................24
CHEST X-RAY (CXR) ..............................................................................................................25
SYMPTOMS ..............................................................................................................................25
TREATMENT ...............................................................................................................................26
SPECIFIC THERAPY................................................................................................................26
SYMPTOMATIC THERAPY....................................................................................................26
SUMMARY OF VARIOUS MEDICATION SIDE EFFECTS.................................................32
SECONDARY THERAPY ........................................................................................................34
COMPLICATIONS .......................................................................................................................38
SLEEP ABNORMALITIES.......................................................................................................38
ACUTE RESPIRATORY FAILURE (ARF) .............................................................................38
COR PULMONALE ..................................................................................................................40
PNEUMOTHORAX...................................................................................................................40
GIANT BULLAE .......................................................................................................................40
VENESECTION.........................................................................................................................40
PROGNOSIS .............................................................................................................................41
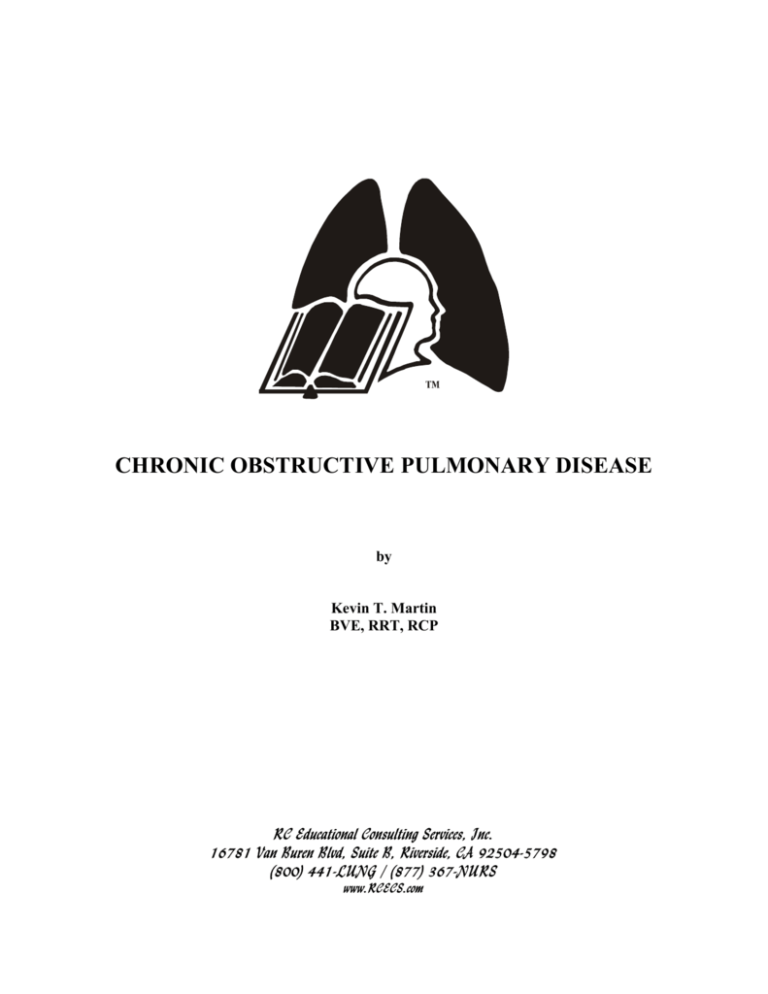
THE GLOBAL INITIATIVE FOR CHRONIC OBSTRUCTIVE LUNG DISEASE (GOLD)....41
OTHER OBSTRUCTIVE DISEASES ..........................................................................................42
ASTHMA.......................................................................................................................................42
ETIOLOGY ................................................................................................................................42
PATHOPHYSIOLOGY..............................................................................................................42
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
5
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
CLINICAL SIGNS AND SYMPTOMS.....................................................................................43
CLASSIFICATION OF ASTHMA ...............................................................................................43
CLASSIFICATION of PHARMACOLOGIC THERAPY ........................................................45
MANAGEMENT OF ASTHMA................................................................................................46
CYSTIC FIBROSIS (MUCOVISCIDOSIS) .................................................................................47
ETIOLOGY ................................................................................................................................47
PATHOPHYSIOLOGY...........................................................................................................47
LABORATORY STUDIES........................................................................................................48
TREATMENT ............................................................................................................................49
BRONCHIECTASIS .....................................................................................................................49
ETIOLOGY ................................................................................................................................49
PATHOPHYSIOLOGY..............................................................................................................50
CLINICAL SIGNS AND SYMPTOMS.....................................................................................50
TREATMENT ............................................................................................................................51
SUMMARY...................................................................................................................................52
CLINICAL PRACTICE EXERCISE ............................................................................................53
PRACTICE EXERCISE DISCUSSION .......................................................................................55
SUGGESTED READING AND REFERENCES .........................................................................56
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
6
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
INTRODUCTION
C
hronic Obstructive Pulmonary Disease (COPD) is a “catch-all” phrase describing a
process characterized by chronic airway obstruction that is not fully reversible. The
airflow inadequacy is usually both progressive and associated with an abnormal
inflammatory response of the lungs to noxious particles or gases. The American Lung
Association classifies emphysema and chronic bronchitis as COPD1. Over the years, chronic
asthma has sometimes been included in the term COPD. However, asthma is not classified as
COPD unless there is a diagnosis of chronic bronchitis or emphysema in conjunction with the
asthma. There are also other obstructive lung diseases, some of which are chronic, but are not
included in the American Lung Association classification of COPD. The other obstructive lung
diseases include asthma, cystic fibrosis, and bronchiectasis, which will also be discussed in this
course.
Very rarely does one find a “pure” chronic bronchitic or emphysemic patient. Most patients
have a mixture of both diseases. The airway obstruction most commonly associated with chronic
bronchitis and emphysema may be partly reversible. Very few patients fall into the precise
definitions of chronic bronchitis or emphysema so COPD is a more common diagnosis. COPD
is defined in the National Lung Health Education Program (NLHEP) and the Global Initiative for
Chronic Obstructive Lung Disease as a set of breathing related symptoms. These symptoms are
chronic cough, expectoration, various degrees of exertional dyspnea and a significant and
progressive reduction in airway flow. The mechanisms for obstruction to airflow are different in
each disease entity, but overlapping of the diseases is common. Many guidelines that are
evidence based use specific values for the evaluation of obstruction such as the FEV1/VC ratio.
The diagnosis of COPD identifies a process, rather than a specific disease entity. Most patients
exhibit symptoms of both chronic bronchitis and emphysema. They may, however, exhibit more
symptoms of one than the other. COPD is associated with impaired gas exchange and changes in
mechanical properties of the lung. These result in an increase in the work of breathing and a
change in the geometry of the lung.
Emergency department visits and hospitalization statistics in 2000 show about 1.5 million
emergency department visits by adults 25 and older. Females made more visits than males
(898,000 vs. 651,000). Hospitalizations for COPD were about 726,000 of which 404,000 were
female and 322,000 were male.
RISK FACTORS
C
igarette smoking continues to be the most significant contributing factor for the
development of COPD. In other countries pipes, cigars, and other types of tobacco,
which are also key risk factors, replace the less popular cigarette. At every possible
opportunity individuals who smoke should be encouraged to quit.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
7
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
DEFINITIONS
C
HRONIC BRONCHITIS - Chronic bronchitis is defined as: “the presence of a chronic
productive cough for three months of the year, for a successive two years, after other
causes of cough have been ruled out.” Chronic bronchitis is further defined as an
inflammation and eventual scarring of the lining of the bronchial tubes.
EMPHYSEMA - Emphysema is defined as: “abnormal, permanent enlargement of the
airspaces distal to the terminal bronchioles accompanied by destruction of the walls, and without
obvious fibrosis.” The walls between the air sacs in the lungs lose the ability to stretch and
recoil. When elasticity of the lung tissue is lost, air is trapped in the air sacs and impairs the
exchange of oxygen and carbon dioxide. The support of the airways is lost, causing obstruction
of airflow.
COPD - COPD is a process characterized by chronic bronchitis or emphysema that leads to
development of airway obstruction that may be partly reversible. A clinical definition is: “a
state of dyspnea on exertion with objective evidence of decreased airflow not explained by
specific heart or lung disease.”
DIAGNOSING COPD25
Key Indicators for Considering a COPD Diagnosis
Present intermittently or every day.
Chronic cough:
Often present throughout the day; seldom only nocturnal.
Any pattern of chronic production may indicate COPD.
Chronic sputum production:
Repeated episodes.
Acute bronchitis:
Progressive (worsens over time).
Dyspnea that is:
Persistent (present every day).
Worse on exercise.
Worse during respiratory infections.
Tobacco smoke (including popular local preparations).
History of exposure to risk factors:
Occupational dust and chemicals.
Smoke from home cooking and heating fuel.
When performing spirometry, measure:
•
Forced Vital Capacity (FVC) and
•
Forced Expiratory Volume in one second (FEV1)
•
Calculate the FEV1/FVC ratio.
•
Spirometric results are expressed as % Predicted using appropriate normal values for the
person’s sex, age, and height.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
8
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Normal
COPD
FEV1
4.150
2.350
FVC
5.200
3.900
FEV1/FVC
80%
60%
Figure 1: Examples of spirometric tracings and calculation of FEV1, FVC and FEV1/FVC ratio.
Patients with COPD typically show a decrease in both FEV1 and FEV1/FVC. The degree of
spirometric abnormality generally reflects the severity of COPD. However, both symptoms and
spirometry should be considered when developing an individualized management strategy for
each patient.
CLASSIFICATION of COPD by SEVERITY25
Stage O: At Risk – Chronic cough and sputum production; lung function is still normal.
Stage I: Mild COPD – Mild airflow limitation (FEV1/FVC < 70% but FEV1 > 80% predicted)
and usually, but not always, chronic cough and sputum production.
•
At this stage, the individual may not be aware that his or her lung function is
abnormal
Stage II: Moderate COPD – Worsening airflow limitation (50% < FEV1 < 80% predicted), and
usually the progression of symptoms, with shortness of breath typically developing on exertion.
Stage III: Severe COPD – Further worsening of airflow limitation (30% < FEV1 < 50%
predicted), increased shortness of breath, and repeated exacerbations which have an impact on
patient’s quality of life.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
9
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
•
Exacerbations of symptoms, which have an impact on a patient’s quality of life and
prognosis, are especially seen in patients with FEV1 < 50% predicted.
Stage IV: Very Severe COPD – Severe airflow limitation (FEV1 < 30% predicted) or FEV1 <
50% predicted plus chronic respiratory failure. Patients may have very severe (Stage IV) COPD
even if the FEV1 is > 30% predicted, whenever these complications are present.
•
At this stage, quality of life is very appreciably impaired and exacerbations may be
life-threatening.
DIFFERENTIAL DIAGNOSIS:
Diagnosis
COPD
Asthma
Congestive Heart Failure
Bronchiectasis
Tuberculosis
Differential Diagnosis of COPD
Suggestive Features
Onset in mid-life.
Symptoms slowly progressive.
Long smoking history.
Dyspnea during exercise.
Largely irreversible airflow limitation.
Onset early in life (often childhood).
Symptoms vary from day to day.
Symptoms at night/early morning.
Allergy, rhinitis, and/or eczema also present.
Family history of asthma.
Largely reversible airflow limitation.
Fine basilar crackles on auscultation.
Chest X-ray shows dilated heart, pulmonary edema.
Pulmonary function test indicate volume restriction,
not airflow limitation.
Large volumes of purulent sputum.
Commonly associated with bacterial infection.
Coarse crackles/CT shows bronchial dilation,
bronchial wall thickening.
Onset all ages.
Chest X-ray shows lung infiltrate or nodular lesions.
Microbiological confirmation.
High local prevalence of tuberculosis.
EPIDEMIOLOGY
C
OPD is the fourth leading cause of death in the United States according to 2000 statistics
and is projected to be the third leading cause of death for both males and females by the
year 2020, claiming the lives of 119,000 adults ages 25 and older annually1. Statistics
reported in the year 2003 reveal the annual cost of COPD to the nation is approximately $32
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
10
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
billion, which includes healthcare costs of $18 billion, and indirect costs of $14 billion. COPD is
also the leading cause of illness and disability in the United States. Approximately 80% to 90%
of COPD cases are the result of smoking. Other causes are air pollutants in the workplace, and
in the home, respiratory infections, genetic factors, and asthma.
Between 1980 and 2000, the COPD death rate for women grew much faster than the death rate
for men. Furthermore, the year 2000 was the first year that more women than men died from
COPD.2 The overall age-adjusted death rate for COPD remained higher for males in 2000. The
age-adjusted COPD death rate was about 46 percent higher in males than females and 63 %
higher in whites than blacks. Approximately 14 million adults were diagnosed with COPD in
2001.
In COPD, the incidence and mortality are inversely related to socioeconomic status and
educational level. Those with higher incomes and more education have less COPD than the poor
or uneducated. COPD tends to aggregate somewhat in families.
It is important to note that, unlike many other conditions, the death rate from COPD is
increasing. In the past 20 years, death rates from COPD has increased 22%. During this same
period, overall death rates from all other causes has decreased. The mortality rate for COPD is
increasing faster than any other leading cause of death. This is despite efforts to reduce smoking
and to provide clean work environments.
PATHOLOGY
T
he pathology of chronic bronchitis is described first, then it’s followed by the pathology of
emphysema. This is the most effective way of describing the cumulative changes that
occur in COPD. One should keep in mind that most patients will have a mixture of the
lesions described for chronic bronchitis and emphysema. A brief review of the normal
mucociliary escalator mechanism is provided for comparison to the changes that occur with
chronic bronchitis.
MUCOCILIARY ESCALATOR
Gel Layer
Sol Layer
Cilia
Goblet Cell
Ciliated Epithhelium
Bronchial Gland
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
11
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Normally, bronchial glands secrete a thin watery secretion to bathe the cilia. This is known as
the “sol” layer of mucus. Resting atop the sol layer is a “gel” layer of very thick, sticky mucus
produced by the goblet cells. The gel layer traps foreign matter, which is then transported out of
the lungs via the cilia. The watery sol layer allows for easy ciliary movement.
CHRONIC BRONCHITIS - Bronchial glands increase in size and volume and their ducts
dilate in chronic bronchitis. Glands in the bronchi hypertrophy first. This is followed by an
increase in goblet (surface-secreting) cells and their appearance in peripheral airways. The
appearance of goblet cells in peripheral (small) airways is an important feature and the most
significant determinant of disability in the patient. Mucus gland volume in the adult is
approximately 4 ml. Volume of the goblet cells is approximately 0.1 ml. A threefold increase in
gland cell thickness is not uncommon in COPD. A threefold increase in thickness results in a
27-fold increase in volume. Therefore, hypertrophy of the glands and goblet cells result in
considerably more mucus. The glands contribute much more to sputum than the goblet cells, but
the latter are the most related to the amount of disability experienced by the patient. This is
because the goblet cells begin secreting mucus in the small airways that are normally free of it.
This leads to airway obstruction due to the small lumen size.
CHRONIC BRONCHITIS
Thickened
Gel Layer
Sol Layer
Loss of
Cilia
Enlarged
Goblet
Enlarged
Bronchial Glands
Patchy areas of squamous epithelium appear in the airway and replace the normal ciliated
epithelium. Airways less than 2 mm show varying degrees of plugging with mucus. There is
also goblet cell metaplasia, inflammation, an increase in smooth muscle, and distortion of the
airways due to fibrosis.
Functionally, the hallmark of chronic bronchitis is hypersecretion, which may or may not be
purulent. Hypersecretion begins in the large airways and is not initially associated with airway
obstruction. As the disease progresses, excess mucus is produced in the small airways and
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
12
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
obstruction develops. For all practical purposes, increased sputum volume reflects changes in
the large airways and airway obstruction reflects changes in the small airways.
Mucus secretion is a normal function of the tracheobronchial tree, but the volume produced is
not enough to produce “sputum”. Sputum is a mixture of secretions from the airway epithelium,
tissue fluid, and serum. Secretions from the epithelium have large acid glycoproteins consisting
of polypeptide chains and oligosaccharide side chains. There is a small amount of disulfide
bonds in the main amino acids. Mucus glycoprotein is what gives sputum its viscoelastic
properties. In chronic bronchitis, the concentration of mucus glycoproteins is higher than in
normal secretions making it more viscous.
EMPHYSEMA - Emphysema results in a destruction of the lung parenchyma. The elastic
structure of the lung is destroyed and alveoli develop fenestrae. This leads to alveolar rupture.
Capillaries are destroyed and surface area for gas exchange is lost. The lungs enlarge and alveoli
become distended. The connective tissue that holds small airways open is destroyed. This
results in collapse at low expiratory lung volumes and airtrapping. A loss of elastic recoil also
contributes to air trapping. The diaphragm becomes flattened from the trapped air and this
inhibits its ability to contract effectively. The chest cage is stretched and increases in
anterior-posterior diameter. Severe emphysema results in a barrel-shaped chest.
NORMAL
EMPHYSEMA
Fractured connective tissue
Overdistended
alveoli
The specific lesion site is dependent upon the type of emphysema present. There are many types
of emphysema, differentiated by where the “abnormal permanent enlargement” is located.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
13
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
However, by definition, all types fall distal to the terminal bronchiole. The primary lesion can be
in the subpleural or intrapleural area, in the alveoli, or in the respiratory bronchiole. The
following is a brief description of the various types of emphysema.
Centriacinar emphysema involves enlargement at the center of the acinus (the portion of the lung
distal to the terminal bronchiole). Centriacinar emphysema results in scarring and focal
dilatation of the respiratory bronchioles and adjacent alveoli. Focal emphysema is a widespread
form of centriacinar. Focal emphysema occurs in individuals having heavy exposure to
biologically inactive dust, such as, coal dust. In this form of emphysema, there are many
pigment-laden macrophages uniformly distributed throughout the lung.
Centrilobular emphysema is also a type of centriacinar. It is most often associated with cigarette
smoking and no unusual dust exposure. Centrilobular emphysema involves the upper and
posterior portions of the lung more than the lower portions. Panacinar emphysema results in
dilatation of all spaces of the acinus. It may be focal or diffuse. In the focal form, lesions are
more common in the bases and in older patients. The diffuse form is most often associated with
alpha one protease inhibitor deficiency (commonly called alpha one antitrypsin deficiency). This
is discussed in detail in the following section on “etiology”.
Distal acinar emphysema is also known as paraseptal or subpleural emphysema. It is usually
localized along fibrous interlobular septa or beneath the pleura. Pulmonary function may be
normal in this form since the rest of the lung is spared. This form can cause apical bullae and
spontaneous pneumothorax. Bullae are areas of marked focal dilatation. They may be a result of
coalescence of adjacent areas, locally severe panacinar, or may develop from a ball-valve type of
obstruction. (Ball-valve obstructions allow air to enter but not leave.) Bullae are particularly
likely in distal acinar. Blebs are intrapleural collections of air. They are a form of interstitial
emphysema. Blebs also can rupture producing a pneumothorax. Subcutaneous emphysema,
compensatory emphysema, and pulmonary interstitial emphysema (in infants) are other types of
emphysema but will not be discussed here.
COPD - COPD patients have a combination of the lesions described above. Some will have
more chronic bronchitis and others more emphysema. There will be varying degrees of airway
inflammation and edema, mucus secretion, loss of connective tissue, alveolar rupture,
airtrapping, and loss of gas exchange surface area. The following illustration schematically
describes these changes and compares them to the normal airway.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
14
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
NORMAL
COPD
Fractured elastic
connective tissue
Connective
tissue
Mucus
layer
Airway lumen
Epithelial layer
Excessive
secretions
Edematous
epithelium
Narrowed
airway lumen
On the left is a normal airway. This shows a relatively thin airway wall and layer of mucus.
Connective tissue is intact and holding the airway open. On the right is the COPD airway. It
reveals a very small lumen due to an edematous airway wall and hypersecretion of mucus.
Airway connective tissue is lost, leading to early collapse on expiration. Work of breathing is
tremendously increased and air is trapped in alveoli.
COPD PATHOLOGY
•
Increase in gland size and volume
•
Hypersecretion of thick, viscous mucus
•
Loss of ciliated epithelium
•
Lung enlargement and airtrapping
•
Alveolar rupture
•
Loss of gas exchange surface area
•
Loss of connective tissue
•
Airway inflammation and edema
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
15
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
ETIOLOGY
T
he etiology of COPD, chronic bronchitis, and emphysema, according to the Global
Initiative for Chronic Obstructive Lung Disease, are not fully understood. However, the
contributing factors are known to be smoking (cigarette smoking, pipe, cigar and other
types of tobacco smoking popular in many countries are also risk factors for COPD), exposure to
air pollutants, respiratory infections, asthma, and genetic factors. Delineating causes are
compounded by a tremendous variability in amount of changes and disability between patients.
Using animal models, both chronic bronchitis and emphysema have been reproduced. The
mechanisms outlined from these models may or may not be the same as for humans.
CHRONIC BRONCHITIS - Chronic bronchitis appears to be related to some type of chronic
bronchial injury, such as, smog, tobacco smoke, or repeated infections. In animals, inhalation of
irritant gases causes various lesions depending upon the gas, its concentration, and duration of
exposure. Sulfur dioxide produces central airway lesions, increases the size of submucosal
glands, and increases the proportion of goblet cells. Cigarette smoke increases mucus-secreting
cells throughout the airway, particularly in small airways. Ozone and nitrogen dioxide damage
junctions of conducting airways and adjacent respiratory bronchioles in the centriacinar region.
Ciliated mucus-secreting cells in the small membranous bronchioles appear the most susceptible
to injury. With continued exposure, inflammatory cells also appear in the bronchioles. In
animals, breathing air for extended periods tends to reverse the changes.
Various substances have been injected into the airway to try and produce chronic bronchitis.
Injection into the airway of enzymes (proteases), endotoxins, and dilute nitric, sulfuric, or
hydrochloric acids all produce secretory cell changes. (It is of interest that sulfuric and nitric
acids are important components of air pollution.)
In humans, there also may be a hereditary component to the development of chronic bronchitis.
It appears that relatives of bronchitis have an increased incidence in chronic bronchitis than the
normal population. Siblings of bronchitis also have a higher incidence than their spouses and
monozygotic twins have a higher incidence than dizygotic twins.
EMPHYSEMA - Animal experiments with alpha-one protease inhibitor deficiency suggest that
lung elastin is deranged in emphysema. This has led to a theory of an imbalance between lung
enzymes and antienzymes (elastase/antielastase theory) as the cause of emphysema.
Elastase is an enzyme produced as an immune response to foreign matter or infection. It aids in
destroying foreign particles and microorganisms. To prevent the destruction of normal tissue
from elastase, antielastase is produced. Without the presence of antielastase, elastase destroys
lung elastin and causes emphysema. It is postulated that those who develop emphysema have an
imbalance between the amount of elastase and antielastase.
Some disease states affecting elastic tissue also support this theory. Infants with cutis laxa, for
example, have emphysema and generalized defects of elastin. Marfan’s syndrome causes
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
16
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
abnormal elastic tissue and emphysema is frequent. Other diseases causing destruction of elastic
tissues also tend to result in emphysema.
Emphysema has been experimentally produced in animals via several mechanisms. Injection of
pancreatic elastase into the trachea of hamster’s causes destruction of elastic fibers, alveolar
septal rupture and hemorrhage resulting in a loss of elastic recoil. The air spaces enlarge and
within 24 hours the total elastic content of the lungs is decreased to less than half. Elastic
content returns to normal after approximately 21 days, but the structural changes described
remain. A decrease in the number of alveoli and alveolar surface area also remain.
Functional changes that occur with an injection of elastase are an increase in lung compliance
and an increase in the functional residual capacity (FRC), residual volume (RV), and total lung
capacity (TLC). Forced expiratory flows are decreased, as is diffusion. There is hypoxemia
without CO2 retention and right ventricular hypertrophy. To a lesser degree injection of human
neutrophil elastase causes the same changes.
There is a very strong association between cigarette smoking and emphysema but tobacco smoke
inconsistently produces emphysema. Two to seven cigarettes a day times 2-4 months produced
emphysema in dogs, but the severity of the changes did not correlate with the amount of
cigarettes smoked.
Emphysema also has been produced by administration of beta-aminoproprionitrile (BAPN).
BAPN inhibits lysyl oxidase, an enzyme important in cross-linking of elastic molecules in the
lung. A decrease in lysyl oxidase results in a decrease in the number of alveoli, an increase in
average alveolar volume and an increase in lung compliance.
Individuals who are homozygous for the “z” variant of alpha one protease inhibitor develop
emphysema prematurely. These patients are deficient in what is commonly known as alpha-one
antitrypsin. Alpha-one antitrypsin (AAT) is a serum protein produced by the liver capable of
inhibiting several types of proteolytic enzymes including elastase. Alpha-one antitrypsin plays
an important role in inflammatory states by protecting lung tissue from substances released by
the immune system. Normally, it increases during pregnancy, infection, burns, after typhoid
vaccination, and in the presence of malignant tumors. Smoking increases alpha-one antitrypsin
by as much as 20% in defense against the smoke. Alpha-one antitrypsin inhibits pancreatic
trypsin, chymotrypsin, elastase, proteases from some microorganisms, and some other
proteolytic enzymes.
Deficient individuals do not demonstrate a rise in alpha-one antitrypsin in response to
inflammation. This means the enzymes released during inflammation, from smoking, from
microorganisms, or other conditions cause more damage in the deficient individual than in a
normal person. The deficient individual prematurely develops severe emphysema, particularly if
they smoke. Alpha-one antitrypsin deficiency significantly decreases survival and life
expectancy. At present, alpha-one antitrypsin deficiency is the only clear biochemical clue to
emphysema. It should be suspected in a patient who develops emphysema before the age of 50.
An estimated 50,000 to 100,000 Americans have AAT deficiency emphysema. This accounts for
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
17
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
less than 5% of the total emphysema cases. AAT deficiency is most common in persons of
northern European descent.1
COPD - Cigarette smokers have a higher prevalence of chronic bronchitis, emphysema,
obstructive airway disease, lung function abnormalities and respiratory symptoms than the
general population. Smokers also have a greater average decline in the forced expiratory volume
in one second (FEV1). Normally, the FEV1 decreases 25-30 ml per year past age 25-30. The
decline is much greater for smokers. Children of smokers also have a higher prevalence for
respiratory disease and symptoms than children of nonsmokers, smoker’s account for 80-90% of
COPD.
In comparison to nonsmokers, smokers have an increase in the number of neutrophils and other
cells in their lungs. These cells are attracted by the chronic irritation from the smoke. This is a
normal response of the immune system. Sampling the cellular content of smoker’s lungs via
bronchoalveolar lavage reveals they have 4-5 times the number of cells present as a nonsmoker.
This is of particular interest considering the effect pancreatic and neutrophilic elastase have on
destroying normal lung tissue. More cells means more elastase. More elastase means more
damage. There is evidence of increased elastase-like activity in lavage fluid from smokers.
In humans, air pollution initiates respiratory disease and predisposes those with COPD to
exacerbations. Mortality, morbidity, respiratory symptom prevalence, lung function, and sick
time from work all correlate with smog levels. Oxidants, nitrogen oxides, and hydrocarbons tend
to cause less damage than particles or sulfur dioxide.
Occupational dust and contaminants also play a role in respiratory disease. Sandstone workers,
tin and copper miners, cotton-strippers, grinders and coal miners have a high incidence of
chronic bronchitis and emphysema. Chronic cadmium poisoning from industrial fumes causes
emphysema. (Cigarette smoke also contains cadmium.) Short-order cooks exposed to smoke
and factory workers involved with sulfur-containing coke have a high incidence of emphysema.
It is believed carbon particles from the smoke carry caustic chemicals into the lungs.
COPD ETIOLOGY
•
Chronic bronchial irritation
•
Increase in proteolytic enzymes (elastase)
•
Cigarette smoking
•
Air pollution
•
Occupational dust and contaminants
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
18
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
PATHOLOGICAL TRIAD OF COPD
Secretions
Bronchospasm
Inflammation
STRUCTURAL VS FUNCTIONAL CHANGES
T
here is often little correlation between structural and functional changes in the chronic
bronchitic. The main changes are an increase in the size and number of glands. This may
or may not be associated with an increase in secretion. The glands can enlarge and
produce more, but not necessarily secrete more. In fact, the backing up of mucus within the
gland may be the cause of the enlargement. On the other hand, if secretion matches production,
there may be no enlargement.
There is a significant correlation between structural and functional changes in emphysema. The
degree of emphysema is moderately correlated to FEV1, FEV1/FVC (forced vital capacity) ratio,
and forced mid-expiratory flow rate. In less severe emphysema, there is a strong correlation
between airflow limitation and bronchiolar pathology.
There is a wide range in severity of emphysema for patients that exhibit obstructive airway
disease. Smokers also exhibit a wide range in the type and extent of lesions, with varying
degrees of obstruction. There is marked individual variability in response to smoking.
CLINICAL HISTORY
D
yspnea, or an acute chest illness, usually bring the COPD patient to the doctor between
the fifth and seventh decade of their lives. A chronic cough, expectoration and wheezing
usually precede the appearance of dyspnea. At this point, dyspnea is primarily on
exertion. This dyspnea on exertion (DOE) has been insidious in development, as have been the
other symptoms. Most patients will not notice respiratory symptoms except for the last few
years. However, family members will often confirm their presence for many years. Patients
generally blame their symptoms on getting old, smog, dust, etc. Sputum production is insidious
and usually does not exceed 60 ml per 24 hours.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
19
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Initially, sputum is sterile on being cultured and mucoid. (It is purulent if infection is present.)
Patients who have predominantly emphysema may have no significant sputum production.
Sputum production decreases sharply and disappears with the cessation of smoking. However,
in the long-term heavy smoker, sputum production may initially increase greatly in the first few
days and weeks of smoking cessation.
Hemoptysis may occur with chronic bronchitis, but also raises the possibility of cancer in a
smoker. Cough is a frequent symptom of COPD. It should not be suppressed by medications,
particularly if the cough is productive. The disappearance of cough in a COPD patient indicates
they are severely ill and retaining secretions. The cough reflex can be impaired by fatigue or
central nervous system (CNS) depression. This leads to secretion retention. An acute decrease
in sputum production and expectoration is an ominous sign in COPD. It indicates that secretion
retention and acute airway obstruction is taking place.
The patient generally has a history of at least one to two chest illnesses a year. During an acute
exacerbation or infection, one can expect to see “normal” symptoms worsen. (An exception may
be sputum production and cough that may actually decrease as a result of retention of secretions.)
Patients appear hypoxic and may be cyanotic. Insomnia, somnolence, personality changes, and
morning headaches indicate severe ABG disturbances. One significant difference to note
between the COPD patient and a normal patient is that rarely will the COPD patient exhibit a
significant fever or increase in white blood cells (WBC’s) with an infection.
SYMPTOMS AND DIAGNOSIS
T
he patient who has predominantly emphysematic is described as a “pink puffer” because
of their appearance. The patient does not exhibit hypoxia or cyanosis but is usually
“pink”. They achieve this by rapid breathing or “puffing”. They are emaciated because
they use up all of their energy breathing. These patients use their accessory muscles extensively
and exhale through pursed lips. They brace themselves with their arms sitting in a chair or on
the side of the bed to get maximum use of the accessory muscles. These patients have enlarged
lungs and a relatively small heart with no evidence of heart failure.
The patients who suffer primarily from chronic bronchitics are described as “blue bloaters”.
They do not maintain adequate blood gases and appear hypoxic or cyanotic. They chronically
hypoventilate and retain CO2. They appear well-nourished to the point of obesity. These
patients often have peripheral edema from their CHF. There is an enlarged heart with recurrent
bouts of congestive heart failure. These patients are polycythemic to compensate for the chronic
hypoxia.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
20
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
PATIENT PORTRAITS
CATEGORY
Definition
“PINK PUFFER”
EMPHYSEMA
Destruction of the airways distal to
the terminal bronchioles
Mechanism of obstruction
Functional lung units destroyed
Physiologic response to the
specific disease process
Destruction of alveolar septae and
pulmonary capillary bed = decreased
ability to oxygenate blood = limited
blood flow through a fairly well
oxygenated lung
Decreased
Hypoxemia
Polycythemia absent
Hyperventilation
Normal
Cardiac output
Oxygenation
CBC
Ventilation
Pulmonary pressures
Ventilation/Perfusion
Acid-base balance
Cough
Pulmonary Infection
Physical frame
Edema
Progression
Accessory muscle use
Breath sounds
Tactile Fremetis
Diaphragmatic Excursion
Cyanosis
Heart sounds
Serum chemistry
V/Q mismatch
Normal
Long history of progressive dyspnea
with late onset of infrequent,
nonproductive cough
Occasional mucopurulent relapses
Muscle wasting, weight loss, thin,
cachextic
Absent
Respiratory failure
Present
Barrel chest, tripod position, pursed
lip breathing
Hyperresonant, wheezing
Decreased
Impaired/decreased
Absent
Distant
Tend to retain Na
“BLUE BLOATER”
CHRONIC BRONCHITIS
Excessive mucus production with airway
obstruction and notable hyperplasia of
mucus-producing glands
Inflammation
Secretions
Decreased ventilation, increased cardiac
output = rapid circulation in a poorly
ventilated lung
Increased
Hypoxemia
Polycythemia present
Hypercapnia-Hypoventilation
Pulmonary artery vasoconstriction = cor
pulmonale (right heart failure)
V/Q mismatch
Respiratory acidosis
Frequent, productive cough, with
progression over time to intermittent
dyspnea
Frequent and recurrent infections
Obesity common
Present
Progressive cardio-respiratory failure over
time
Present
Coarse rhonchi and wheezing
Decreased
Impaired/decreased
Present
Normal
Tend to retain Na
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
21
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
CXR
Small heart, hyperinflation/
Hyperlucent, flat hemidiaphragms,
possible bullous changes,
Increased AP diameter,
Increased retrosternal space
ECG
Underlying cardiac disease is highly
likely, look for ischemia due to
hypoxia
Decreased FEV1
Decreased FEV1/FVC
Poor/absent reversibility with
bronchodilators
FVC normal or decreased
Normal or increased TLC
Increased RV
Decreased DLCO
Pulmonary function testing
Flattened hemidiaphragms, slightly
increased AP diameter, Increased
bronchovascular markings (enlarged
proximal pulmonary arteries and
prominent interstitial markings) and
cardiomegaly (specifically right
ventricular enlargement)
Underlying cardiac disease is highly
likely, look for ischemia due to hypoxia
Decreased FEV1
Decreased FEV1/FVC
Some reversibility with bronchodilators
FVC normal or decreased
TLC normal or increased
Increased RV
Normal or decreased DLCO
COPD patients have a decrease in exercise tolerance that has been developing for years. Most
have ignored it in the past, explaining it by “getting old”. When it finally becomes intolerable,
they seek medical help. Dyspnea at rest indicates very advanced disease or an acute
exacerbation, usually an infection.
COPD patients have a productive cough, which has been present for many years. Breath sounds
are very difficult to hear because of airtrapping and an enlarged chest. There is a decrease in
blood gas exchange, as evidenced by a decrease in PaO2 and increase in PaCO2. Bicarbonate
levels increase to buffer the additional CO2 so pH should be in a normal range. Depending upon
the degree of blood gas abnormality, they have CNS symptoms. These vary from simple
irritability to confusion to lethargy.
ACUTE EXACERBATION - A recent study concluded that of those patients admitted to the
hospital with exacerbation of their COPD, about 50% were admitted with respiratory infection,
25% due to congestive heart failure and approximately 30% with no known cause. Exacerbation
symptoms generally include patient complaints of increasing SOB, decreasing ability to perform
activities of daily living (ADL’s). Often they have increased sputum production, fever and
tachypnea. Hyperinflated chest, long expiratory times and wheezing are likely to be observed
during assessment.
PHYSICAL EXAMINATION - The COPD patient has some distinctive physical findings that
separate him/her from other patients. Because the airway obstruction primarily affects
expiration, there is significant airtrapping. Over a period of years, this deforms the chest cage
causing an increase in anterior-posterior diameter. The patient will appear “barrel-chested”. The
chest becomes fixed in an inflated position. There is minimal chest movement with breathing.
They may exhale through pursed lips. Pursed-lip breathing provides a slight backpressure to
keep airways open on expiration.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
22
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
BARREL CHEST
NORMAL AP
DIAMETER
INCREASED AP
DIAMETER
Airtrapping flattens the diaphragm, making it ineffective as a muscle for breathing. Flattening
shortens the muscle fibers and results in less muscle force during contraction. (In emphysema,
the fibers both shorten and decrease in number.) To compensate, the COPD patient relies upon
the accessory muscles of inspiration. The sternocleidomastoid, scalene and pectoralis muscles
become very prominent and hypertrophy from increased use. This hypertrophy, coupled with
tremendous negative pressures generated on inspiration, cause supraclavicular and suprasternal
notches to be very prominent.
Airtrapping impedes venous return resulting in jugular venous distention. Jugular venous
distention (JVD) or jugular venous pressure (JVP) is an estimation by examination of the height
of the blood column in the jugular veins. This estimation reflects the volume and pressure of
venous blood in the right side of the heart. When a patient lies in the supine position, a normal
person’s neck veins are full. If the head of the bed is elevated to a 45-degree angle, the column
of blood decreases to no greater than a few centimeters above the clavicle. If a patient has
increased venous pressure, the neck veins may be distended as high as the angle of the jaw, even
when the patient is in high fowler’s position. This assessment tool may be difficult to use for the
obese patient, as the veins may not be visible. Some clinicians prefer to observe both internal
and external jugular, but the internal is more reliable for assessment. The measurement should
be taken at the end of exhalation as jugular pressure may vary with breathing. The degree of
distention is graded as normal, increased, and markedly increased.
Chronic hypoxia results in pulmonary hypertension, leading to right ventricular hypertrophy.
(Cor pulmonale also contributes to venous distention.) There also may be pitting edema.
Chronic hypoxia results in clubbing of the digits. Chronic hypoxia also produces polycythemia
to increase O2 carrying capacity. The patient may be irritable or confused due to lack of oxygen
in the brain.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
23
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
DIGITAL CLUBBING
NORMAL
MILD
SEVERE
ABG’s - ABG’s reveal a lower than normal PaO2 (less than 80 mm Hg) on room air. It is not
uncommon for a COPD patient’s normal PaO2 to be in the 50-60 mm Hg range. PaCO2 is higher
than the normal 35-45 mm Hg range. It can be very high if obstruction is severe and causes
considerable airtrapping. Since the PaCO2 has gradually increased over a period of years, the
body increases bicarbonate levels proportionally to maintain pH and this results in a
pH of 7.35-7.45.
An acute exacerbation results in an acute rise in PaCO2 and respiratory acidosis. It is very
important to gauge the severity of the acute problem in the COPD patient by the abnormal pH,
rather than only assessing the PaCO2. The “normal” pH and PaCO2 of the COPD patient can be
quite different than what is normal in the healthy adult without pulmonary disease. One should
not be too hasty in instituting mechanical ventilation (or overzealous in its application) just
because the patient has an elevated PaCO2 or a mild respiratory acidosis. COPD patients tolerate
respiratory acidosis considerably better than the normal patient. It is wise to pursue other therapy
aggressively prior to mechanical ventilation. COPD patient’s can be difficult to wean once
intubated. They are often mechanically hyperventilated until they have a normal PaCO2. When
weaning is attempted the PaCO2 starts to return to their normally high level.
PULMONARY FUNCTION TESTS (PFT’s) - PFT’s definitively diagnosis COPD and help to
differentiate the primarily emphysemic from chronic bronchitic. Both have lower flow rates and
forced expiratory volumes (FEV’s) than normals. The FEV1 being indicative of large airways
decreases more in chronic bronchitis than emphysema. The FEV3 is indicative of smaller
airways. A decrease in FEV3 indicates small airway disease from advanced chronic bronchitis or
emphysema.
Both chronic bronchitis and emphysema cause an increase in airtrapping and closing volume
(CV). (Closing volume measures the point at which small airways collapse on expiration. An
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
24
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
increase indicates airways are closing sooner than normal and trapping air.) The increase in CV
is more severe with emphysema since it causes a loss of connective tissue. Connective tissue is
essential to hold small airways open. Airtrapping increases total lung capacity (TLC), residual
volume (RV), and functional residual capacity (FRC).
Emphysema decreases diffusion due to its destruction of alveoli and capillaries. Therefore, the
diffusion of carbon monoxide (DLCO) will be decreased. The DLCO is often the definitive test
for emphysema. A significant finding in emphysema compared to other lung disease is an
increase in compliance, particularly the static compliance. Static compliance reflects
distensibility of the lung parenchyma. Since emphysema affects this area by fracturing the
elastic tissue and alveoli, the lung becomes more distensible and compliance increases.
CHEST X-RAY (CXR) - The CXR of the emphysemic reveals very large, hyperinflated,
avascular lungs. Bullae may be present and there is an increase in the retrosternal space. The
CXR of the chronic bronchitic reveals an increase in bronchovascular markings and an enlarged
heart. There may be an increase in the size of the main and branching pulmonary arteries. Both
the emphysemic and chronic bronchitic show flattened diaphragms and a widening of the
costaphrenic angle. The COPD patient has a mixture of these changes. Generally, they have
hyperinflated, congested lungs with flattened diaphragms and an enlarged heart.
SYMPTOMS
•
Decreased exercise tolerance
•
Productive cough
•
Accessory muscles in use
•
Increased chest anterior-posterior diameter
•
Jugular venous distention
•
Pulmonary hypertension
•
Chronic hypoxia and hypercarbia
•
Compensated respiratory acidosis
•
Lowered expiratory flowrates and volumes
•
Flattened diaphragms
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
25
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
TREATMENT
T
reatment can be divided into several categories: specific, symptomatic, or secondary.
Specific therapy is treatment aimed at reversing the disease or preventing further
deterioration. Symptomatic therapy is aimed at the relief of specific symptoms, but
doesn’t alter the actual disease process. Secondary therapy is used to improve the quality of life
for the patient. Secondary therapy improves patient function, but does not alter the status of the
disease. (Some treatments, such as oxygen therapy, can be put in more than one category
depending upon the current status of the patient.)
SPECIFIC THERAPY - This begins with removal and avoidance of occupational or
environmental irritants. Avoidance of smoke, dust, smog, and cold air are examples of common
irritants. Since most exacerbations occur after viral infections (colds) an annual influenza
vaccine is recommended. Pneumococcal vaccination is highly suggested as well. Avoidance of
the large germ pool found in crowds is also highly recommended.
Quite possibly the most important specific therapy is smoking cessation. This is particularly
important if the disease has only progressed to a mild to moderate airflow obstruction. Mild PFT
abnormalities can be reversed if the patient stops smoking. A simple one to two minutes of
advice from the physician can cause approximately 5% of smokers to quit. The rest should be
referred to clinics and stop-smoking programs. (Unfortunately, even the best programs have a
success rate of less than 25% after one year.) Nicotine gum has been shown to enhance the
outcome of other interventions but is not particularly valuable as a sole intervention. The alphaadrenergic agonist clonidine is also effective in smoking cessation. Buproprion (Wellbutrin) has
shown excellent results in assisting patients with smoking cessation.
One should take a strong and active approach with the patient regarding smoking cessation. One
should tell the patient they must quit smoking not that they should quit smoking. Personalize the
message by emphasizing you are talking about their health, not just a bunch of statistics. Give
the patient a “quit date” to signify when smoking will cease. The simple acts of personalizing
the message and setting a quit date substantially increases cessation rate.
SYMPTOMATIC THERAPY - This is therapy aimed at the reversible elements of hypoxia
and airway obstruction. O2 therapy is used for the former and discussed extensively in the
following section. This section will discuss therapy to relieve increased secretions,
bronchospasm, and cellular infiltration/inflammation.
For increased secretions, the simplest treatment is water. The patient should be instructed to
drink 6-8 glasses of water per day (assuming there are no congestive heart problems). They
should drink enough water to keep the urine pale, except upon arising in the morning. Water
hydrates and thins the mucus making it easier to expectorate.
A mucolytic-expectorant, such as, iodinated glycerol, can be useful. Iodinated glycerol increases
secretion of the sol layer of mucus. This thins and dilutes the mucus much like systemic
hydration. A majority of COPD patients with excess mucus will benefit from the use of
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
26
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
iodinated glycerol. Ease of expectoration and overall condition improve and acute exacerbations
are shortened with its use. Up to eight weeks of therapy may be necessary to show improvement
with iodinated glycerol. If there is no improvement in this time, discontinue its use.
Chest physical therapy (CPT), or postural drainage and percussion, is also used to mobilize
secretions and aid expectoration. The newer lung oscillating/vibratory devices such as the
Flutter® device and Acapella PEP® are very effective substitutes for traditional CPT in most
cases. Many patients can perform this therapy independently. It is especially beneficial for the
patient to be instructed on these types of devices while in the hospital, and continue use as
needed after returning home.
Medications7,8. The most frequently used medications for COPD and asthma are listed here by
classification:
Beta2 specific fast-acting bronchodilators with a duration of 4 to 8 hours. These are given via
nebulizer, MDI, DPI, tablets or syrup depending on availability of the drug in differing delivery
devices:
Albuterol (Proventil®, Ventolin®)
Bitolterol (Tornalate®),
Levalbuterol (Xopenex®),
Pirbuterol (Maxair®)
Also note:
Salmeterol (Serevent®) and Formoterol (Foradil®) are also beta2 specific
bronchodilators, but are slow to act (approximately 20 minutes to onset), and the
duration is long at approximately 12 hours.
*Anticholinergic bronchodilator:
Ipratropium bromide (Atrovent®) given via nebulizer or MDI
Xanthine drugs:
Theophylline (Theo-Dur®, Theovent®, Slo Bid®) given via pill
Aminophylline given intravenously
Anti-Inflammatory Medications:
Corticosteroids given via MDI or DPI:
Beclomethasone (Beclovent®, Vanceril®, QVAR®)
Budesonide (Pulmicort®)
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
27
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Fluticasone (Flovent®)
Flunisolide (Aerobid®)
Triamcinolone (Azmacort®)
Systemic Corticosteroids given via pill, IM, or IV:
Hydrocortisone, prednisone, and methylprednisolone
Nonsteroidal anti-inflammatory agents given via MDI or nebulizer:
Cromolyn sodium (Intal®)
Nedocromil sodium (Tilade®)
Leukotriene inhibitors given via pill:
Zileuton (Zyflo®)
Zafirlukast (Accolate®)
Montelukast (Singulair®)
Mucolytic:
Acetylcysteine (Mucomyst®) given via nebulizer mixed with a beta2 drug.
*Cholinergic Antagonists. Cholinergically-induced bronchospasm in the central airways
decrease with the use of atropine and ipratropium bromide (Atrovent). Ipratropium can be a
more effective bronchodilator than the beta 2 drugs for many patients with COPD, particularly
the bronchitic patient. Cholinergic antagonists have an additive effect to the beta 2 agonists so
they can be used in combination for maximum effectiveness.
Combination Therapy: β adrenergic and Anticholinergic
IPRATROPIUM BROMIDE and ALBUTEROL (Combivent).
Ipratropium bromide and albuterol is a combination MDI product, with the usual doses of each
agent released from the valve (21 mcg of ipratropium, 100 mcg of albuterol base as 120 mcg of
albuterol sulfate). The combination therapy has been shown to be more effective in stable COPD
than other agents alone.
Corticosteroids - Approximately 10-20% of patients with COPD are capable of responding to
steroids for airway inflammation. Patients who respond are generally those that demonstrate an
increase of greater than 25% in the FEV1 after bronchodilator therapy. A trial using doses in the
range of 0.5 mg/kg of prednisone or its equivalent can be done on patients responding poorly to a
bronchodilator regimen. A trial of two weeks should be given. Discontinue if spirometry and/or
ABG’s have not improved. (One should look for an improvement in FEV1 more than 20%.)
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
28
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Taper the medication to the lowest level that maintains an improvement. If there is no
improvement, discontinue the medication.
For those who show an improvement, gradually taper the oral corticosteroid while replacing it
with an inhaled corticosteroid. Inhaled corticosteroids have minimal systemic absorption so side
effects of long-term use are minimized. They have potent local effects, so their dosage is 16 to
20 times less than that required for oral corticosteroids. Triamcinolone, beclomethasone and
flunisolide are the most common inhaled corticosteroids.
Patients need to be instructed that corticosteroids are not “bronchodilators” and maximum
benefit is obtained with regular use. They are not a PRN medication. Some patients also may
need calcium supplementation to prevent osteoporosis. A few will not respond to inhaled
corticosteroids as well as oral preparations.
Combination Therapy: β adrenergic and Corticosteroid
ADVAIR DISKUS (salmeterol xinafoate/fluticasone propionate inhalation powder), combines
an inhaled corticosteroid and a long acting inhaled bronchodilator to simultaneously treat both of
the underlying causes of asthma symptoms: inflammation (swelling and irritation of the lungs’
airways) and bronchoconstriction (tightening of the smooth muscle surrounding the airways).
Advair Diskus combines two leading asthma controller medications Serevent® (salmeterol
xinafoate), a long-acting inhaled bronchodilator, and Flovent® (fluticasone propionate), an
inhaled corticosteroid, in a single asthma medication. It is intended for the maintenance
treatment of asthma as prophylactic therapy in patients 12 years and older where combination
therapy is appropriate.
SYMBICORT is available in MDI. This contains the two medicines budesonide and formoterol
in the same single inhaler. It is used to treat asthma.
The reason for putting the two medicines together in one single inhaler is that they work on
different aspects of asthma:
•
budesonide is a type of medicine called a glucocorticosteroid, which treats the chronic,
underlying part of asthma. This is the inflammation - the “quiet part” of asthma that you
cannot hear, see, or feel. When it is left untreated, inflammation can worsen. The lungs
can become more inflamed and asthma symptoms and attacks can increase.
•
formoterol is a fast and long-acting bronchodilator. Bronchodilators are medicines that
open up the bronchial tubes (air passages) of the lungs. They are used to treat the
symptoms of bronchial asthma, chronic bronchitis, emphysema, and other lung diseases.
They relieve cough, wheezing, shortness of breath, and troubled breathing by allowing an
increased flow of air through the bronchial tubes.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
29
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Used together, budesonide and formoterol provide better control of asthma, decreasing the
number of asthma attacks. Symbicort provides both medications in the same single inhaler, so
that treatment is more convenient for the patient.
September 18, 2000 - 3M Pharmaceuticals announced that the U.S. Food and Drug
Administration (FDA) has granted approval for QVAR™ (beclomethasone dipropionate HFA)
Inhalation Aerosol for the treatment of asthma.
QVAR, a unique aerosol metered dose inhaler (MDI) which contains beclomethasone
dipropionate (BDP) in a solution and no chlorofluorocarbon (CFC) propellant, is the first inhaler
designed to deliver smaller-particle-sized medication to the large, intermediate and small
airways. This allows QVAR to control asthma at a lower dose than conventional CFCcontaining BDP inhalers.
New QVAR is indicated for the preventive management of asthma for people over the age of 12
and contains the safe and effective corticosteroid, beclomethasone dipropionate.
“Both the large and small airways in the lungs play an important role in asthma, but current
inhalers fail to deliver medication to the smallest airways. This new drug represents a potential
breakthrough for patients with asthma”, said Sally Wenzel, M.D., a leading Pulmonologist from
the National Jewish Medical and Research Center in Denver, Colorado.
The efficacy of inhaled corticosteroids for the treatment of asthma is well established, both
nationally and internationally, with treatment guidelines recommending their use as first-line
therapy. Corticosteroids, such as QVAR, for the treatment of asthma are usually administered
by inhalation through a metered dose inhaler.
Recent studies have shown that, in contrast to CFC-beclomethasone dipropionate (CFC-BDP)
inhalers, QVAR delivers more medication to the lungs, where it is needed, and deposits less in
the throat. With QVAR, approximately 50 percent of the drug is administered to the lungs.
Clinical trials have shown QVAR to be effective to conventional BDP at a lower dose.(25,26,32,33)
At recommended doses, QVAR was not associated with any clinically relevant systemic side
effects in adults.(33)
QVAR is the first CFC-free metered dose inhaler containing a corticosteroid. QVAR is a
formulation of the anti-inflammatory drug BDP, which uses the ozone friendly propellant
hydrofluoroalkane (HFA). All CFC-containing inhalers will eventually be phased out in the
United States. Thus, QVAR is a CFC-free BDP that has been developed to meet this change.
Common side effects associated with the use of QVAR and placebo in clinical trials include, but
are not limited to, headache (12 percent and 9 percent, respectively) and pharyngitis (8 percent
and 4 percent, respectively). QVAR is not a bronchodilator and is not indicated for rapid relief
of bronchospasm. Caution: Adrenal insufficiency may occur when transferring patients
from systemic steroids.
Antibiotics - the patient needs to be taught the difference between mucoid and purulent
secretions. When the sputum changes to purulent they should have a supply of antibiotics to
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
30
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
take. Prompt treatments of acute infections are essential in COPD. Common antibiotics are
ampicillin, tetracycline, amoxicillin, doxycycline, and sulfamethoxazole-trimethoprim. A course
of 7-14 days is usually given. Antibiotics should not be given prophylactically in COPD. They
should be reserved for acute exacerbations only.
COPD MEDICATIONS
Mucolytic-expectorant
trial x 8 weeks
Effective?
Inhaled ipratropium and/or
beta 2 adrenergic agonists
Effective?
Antibiotics for
acute exacerbation
Yes
No
Yes
No
Continue
Discontinue
Continue
Corticosteroids
Effective?
Yes
Taper and change
to inhaled steroid
Effective?
Yes
Continue and withdraw
oral steroids
No
Discontinue
No
Discontinue inhaled steroid,
continue oral steroid
Theophylline - Theophylline is widely used for the relief of bronchospasm, despite little
objective evidence of its efficacy in patients with severe COPD. Oral preparations are used for
the ambulatory patient and IV preparations for the acutely ill.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
31
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Theophylline has numerous side effects, such as, nausea, vomiting, headache, insomnia,
arrhythmias, and seizures. These are minimal if the patient is kept within the therapeutic range
of 10-20 mcg/ml. Side effects rise in proportion to the plasma level, so it’s best to keep levels as
low as possible. A target level of 10 mcg/ml is wise. Theophylline has an additive effect to the
beta 2 agonists. When used together, low doses of each can minimize toxicity.
Theophylline has several effects that may be beneficial to the COPD patient in addition to
bronchodilation. They are: increased diaphragm contractility, increased hypoxic drive to
respiration, increased right and left ventricular ejection fractions and direct myocardial
stimulation. There may be nonbronchodilating advantages to theophylline use in subjects with
COPD who also have cardiac disease or cor pulmonale. Theophylline can increase cardiac
output, decrease pulmonary vascular resistance and improve myocardial muscle perfusion in
ischemic regions.
An advantage to oral theophylline is that it is absorbed slowly from the GI tract. Therefore,
reasonably stable serum concentrations can be maintained. Dosage can be at 8-12 hour intervals.
There are also once-daily preparations but these can cause surges in blood levels after eating.
Many factors can affect theophylline plasma levels; smoking, smog, caffeine, high protein diets,
fever, pneumonia, CHF, propranolol, cimetidine, quinolones, and erythromycin are a few.
Dosage will have to be adjusted based upon their presence. Because of the narrow therapeutic
range and numerous side effects of theophylline, its role in COPD is limited to a few patients.
SUMMARY OF VARIOUS MEDICATION SIDE EFFECTS
Cholinergic Antagonists
•
Cough
•
Dyspnea
•
Dry mouth
•
Flulike symptoms
•
Nervousness
•
Bronchitis
•
Irritation
•
Upper respiratory infections
•
Dizziness
•
Nausea
•
Headache
•
Occasional bronchoconstriction
•
Palpitation
•
Eye pain
•
Rash
•
Urinary retention (< 3%)
•
Pharyngitis
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
32
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
ß2-Adrenergic Agonists
•
Tremor
•
Dizziness
•
Palpitations and tachycardia
•
Nausea
•
Headache
•
Tolerance (tachyphylaxis)
•
Insomnia
•
•
Rise in blood pressure
•
Worsening ventilation-perfusion
ratio
Hypokalemia
•
Nervousness
•
Propellant (CFC) induced
bronchospasm
Corticosteroids
Systemic Administration
•
HPA suppression
•
Fluid retention
•
Immunosuppression
•
Hypertension
•
Psychiatric reactions
•
Increased white cell count
•
Cataract formation
•
Dermatologic changes
•
Myopathy of skeletal muscle
•
Growth retardation
•
Osteoporosis
•
Increased glucose levels
•
Peptic ulcer
Inhaled aerosol corticosteroids
Systemic
•
Adrenal insufficiency
•
HPA suppression
•
Extrapulmonary allergy
•
Growth retardation
•
Acute asthma
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
33
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Local (topical)
•
Oropharyngeal fungal infection
•
Cough, bronchoconstriction
•
Dysphonia
•
Incorrect use of MDI
Antibiotics
•
Bacterial resistance
•
Local airway irritation
•
Allergies
SECONDARY THERAPY - Secondary therapy is designed to improve daily functioning, but
doesn’t alter disease status. Much of it is related to patient education and overlaps specific and
symptomatic therapies. Secondary therapy primarily consists of oxygen therapy and
rehabilitation/physical therapy.
Oxygen Therapy - COPD patient’s having severe airflow obstruction, cor pulmonale, and a PaO2
of 40-60 mm Hg should be provided continuous oxygen therapy. Continuous O2 therapy will
increase survival rate for these patients. COPD patients having a resting PaO2 of less than or
equal to 55 mm Hg (after being on an optimal bronchodilator regimen for one month) should be
provided oxygen, particularly for ambulation. Oxygen also should be provided the COPD
patient recovering from acute respiratory failure (ARF) for up to 30 days at home. They should
then be re-evaluated. Generally, a PaO2 of 60-80 mm Hg is desired. This is usually
accomplished with a flow of 1-3 lpm via nasal cannula. A venturi mask can also be used for an
exact FIO2 at a higher flow.
PaO2’s of 60-80 mm Hg may be too high for some COPD patients. Some COPD patients
function on a “hypoxic drive” for ventilatory stimulation. Should their PaO2 exceed a specific
threshold level they will hypoventilate. When the hypoventilation causes the PaO2 to drop below
the threshold level they start breathing again. This is rarely a significant problem, but should be
documented if it occurs and PaO2/flow adjusted accordingly. Never withhold oxygen from a
patient who needs it for fear of knocking out their hypoxic drive. If this occurs, it can be easily
remedied. However, the effects of prolonged hypoxia may not be so easily reversed.
A nasal cannula is the most common method of oxygen delivery. Transtracheal catheters are
being used more frequently for outpatients in recent years. They have the advantage of being
less conspicuous and use less oxygen per level of activity. There have been some complications
associated with the catheters, so additional studies are needed before they are routinely
recommended. Oxygen simple masks, venturi masks, tents and other delivery devices are used
when appropriate.
Rehabilitation/Physical Therapy - COPD patients become dyspneic on exertion early in their
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
34
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
disease process. Therefore, they stop exerting themselves to avoid dyspnea. This leads to
skeletal muscle deconditioning due to inactivity. Deconditioning then causes dyspnea at smaller
and smaller levels of activity. A vicious cycle is thus created where dyspnea and inactivity feed
each other. Participation in an exercise program can result in numerous positive effects for the
COPD patient.
In normal subjects, participation in a well-designed exercise program results in an increase in
maximum O2 uptake; an increase in muscle strength, endurance, and muscle mass; improvements
in coordination and sense of well-being; and a decrease in fat tissue. COPD patients get similar
results, depending upon severity of disease. Those with mild to moderate disease get the same
effects as those with normal pulmonary status. Those with severe disease get improved exercise
endurance and sensation of well-being but little to no change in maximum O2 uptake. Virtually
all COPD patients can benefit from some type of graded exercise program.
There are three principles regarding muscle training one should be aware of: specificity,
intensity/duration, and the detraining effect. The first refers to the fact that training provides
benefits specific to the muscles being trained. Arm exercises improve the arms and leg exercises
improve the legs for example. The type of training is also specific to its benefits. Strength
training improves strength and endurance training improves endurance. Weightlifting improves
strength and aerobics improve endurance for example. A well-designed exercise program for the
COPD patient should include arm and leg exercises to build both strength and endurance.
The second, intensity and duration, affect the degree of the training effect, the greater the
intensity and duration, the greater the training effect. Athletes train at their maximal or nearmaximal exercise capacity. Normal persons may train at 80% of their capacity. COPD patients
may begin training at 30-50% of their capacity and increase as tolerated. (Patients have better
results at 50% than 30% and some programs even go as high as 70% for their COPD patients).
Programs should be designed with an initial intensive phase for learning purposes followed by a
maintenance phase to keep the training effect.
The detraining effect refers to the fact that if one stops exercising, the training effect is lost. This
also applies to the patient who doesn’t exercise but is recovering from prolonged bed rest due to
an acute exacerbation. In a normal subject the maximal O2 uptake is decreased after 21 days of
rest. It takes from 10 to 50 days for the muscles to return to their former condition. One can
assume it can take the COPD patient the same or more time to return to normal. If the patient
participates in a regular exercise program, and then stops, the benefits of training are lost about
one month after quitting. This is why the maintenance phase of an exercise program is so
important.
An exercise program can be provided on an inpatient or outpatient basis with little to no
specialized equipment. Walking or cycling can perform leg exercises. Lifting wooden dowels,
dumbbells, or other common objects can perform arm exercises. Treadmills, weight machines,
arm or leg ergometers, etc. can be used if finances permit. Prior to beginning the program,
evaluate the patient’s exercise capacity by measuring the distance walked/cycled in 6 or 12
minutes or how many steps they can go up without stopping to rest. Also have the patient rate
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
35
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
their “dyspnea level” at a given level of activity using a scale of 1 to 10. This is an extremely
important measurement because the patient’s perception of dyspnea is the most problematic
symptom and the most influential in their physical limitations. The above measurements are
critical in determining the patient’s exercise capacity and their response to training. They
provide excellent feedback to the patient and are very motivating.
Arm exercises are more tiring to the patient than leg exercises. Simply raising the arms 90o
causes an increase in heart rate, minute ventilation, O2 consumption and CO2 production in the
COPD patient. This is because many of the muscles of the chest and shoulder girdle have a dual
function. They can be used in ventilation or posture/positioning. In the latter function, they help
support the arms and shoulders and exert a pulling force on the rib cage when the arms are used.
In COPD, when the diaphragm becomes ineffective these muscles are used for ventilation.
Unsupported arm exercises detract from this function causing dyspnea. But arm training, like leg
training, reduces the ventilatory requirement for the same amount of work. Since many of the
activities of daily living require the arms, they should not be overlooked in training.
Breathing retraining also is used to improve efficiency of the ventilatory muscles. It is a
valuable adjunct to exercise conditioning. Breathing retraining offers patients a useful coping
mechanism for times of acute dyspnea. The patient is taught to relax the accessory muscles and
“mobilize” the diaphragm through diaphragmatic breathing exercises. Airtrapping flattens the
diaphragm and makes it relatively useless for breathing. Before practicing diaphragmatic
breathing some patients need to do some neck exercises to relax the accessory muscles.
Relaxing the accessory muscles make it easier to work the diaphragm. Have them turn the head
from side to side, up and down, and rotate it slowly several times. The first step in breathing
retraining is to make the patient aware of the diaphragm. They are instructed to become more
aware of their breathing and to take slow, deep, controlled inspirations. Inspiration should be
through the nose to filter, warm, and humidify the air. Expiration should be through pursed lips
to minimize air trapping.
To demonstrate diaphragm movement to the patient, have them place one hand on the abdomen
and the other on the upper chest. Then instruct them to “sniff” the air. Sniffing is a diaphragm
activity. The hand on the abdomen moves and detects the diaphragm movement while the hand
on the chest remains motionless. The patient is then instructed to exhale while pressing on the
abdomen with the lower hand. As they inhale the abdomen should push the lower hand out.
Instruct them to keep the upper hand relatively immobile until the latter part of inspiration.
Contract the abdominal muscles to push the diaphragm up on expiration and relax them to pull
the diaphragm down on inspiration.
When exercising, the patient should return to a controlled breathing pattern prior to becoming
dyspneic. For example, they should take several breaths, walk up a few stairs and then stop.
Take a few more breaths and then continue. Make the patient aware that they can control their
breathing, rather than the reverse.
How to perform activities of daily living without becoming dyspneic are also taught. An
example is the one above of walking up stairs. Another example is reaching for items on a top
shelf. Raising the arms above the head stresses the accessory muscles and makes breathing
difficult. A footstool should be used for items on upper shelves. Items used often should be
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
36
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
placed on lower shelves. Another example is a change of eating habits to 5-6 small meals a day,
rather than the customary 3 large ones. Large meals interfere with diaphragm movement and
burn more oxygen in the digestion process than smaller meals. These and other techniques help
the COPD patient perform daily activities with a minimum of distress.
All of the above therapies should be tailored to the individual patient. They should be applied in
a graded manner that is dependent on the severity of the airway obstruction. Therapy
during exacerbations should be increased and then decreased as they improve. Maintain therapy
at the lowest effective level that relieves symptoms or shows an improvement.
Psychological management is an aspect of therapy often overlooked in the COPD patient.
Dyspnea, mucus obstruction, expectoration and other symptoms of chronic lung disease
adversely affect psychological well-being. Symptoms of COPD produce fear, panic, fatigue,
depression, and embarrassment to the patient. They are compounded if there is a poor
therapeutic response due to under treatment, improper medication dosing, poor compliance, or
incorrect use of MDI’s, the more severe the symptoms, the greater the psychological impact.
Proper treatment of the anxiety, depression, loss of self-esteem and sense of isolation that is
common in COPD can tremendously improve the patient’s quality of life.
Numerous instruments are available to measure emotional and psychological symptoms of
COPD. Repeat measurements are used to monitor response to treatment. The Quality of WellBeing Scale assigns a score to level of physical activity, mobility, and social activity. It
classifies patients as having any of 22 symptoms or problems that might affect function. The
scale takes into account clinical problems, symptoms, and levels of activity.
The Sickness Impact Profile asks the patient to answer 136 questions regarding physical,
psychosocial, and behavioral function. The Profile of Mood States has the patient rate 65 items
for mood, tension, depression, and anger. The Chronic Respiratory Disease Questionnaire rates
89 items on dyspnea, fatigue, emotional function and mastery. Others are the Minnesota
Multiphasic Personality Inventory, Likert Scale, Bronchitis-Emphysema Symptom Checklist,
Katz Adjustment Scale, and Beck Depression Inventory Scale.
Each instrument measures different items of emotional, functional, and perceptual response to
illness. Combined uses of the scales provide a good indication of quality of life for the COPD
patient. The Sickness Impact Profile provides the broadest measure of quality of life for these
patients because it examines the combined effects of age, social class, neuropsychological
functioning, and physiologic functioning to life quality.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
37
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
SPECIFIC THERAPY
SYMPTOMATIC THERAPY
SECONDARY THERAPY
Avoid irritants
Annual influenza vaccine
SMOKING CESSATION!
Water
Chest physical therapy
Mucolytic-expectorants
Ipratropium bromide
Beta two adrenergic agonists
Theophylline?
Corticosteroids?
Antibiotics
Oxygen therapy
Oxygen therapy
Graded muscle exercises
Breathing retraining
ADL instruction
COMPLICATIONS
T
here are many complications of COPD. Some, such as, decreased exercise tolerance,
repeated infections, hypoxia, chest cage deformity, CNS disturbances, etc., have been
mentioned. Several others will now be discussed.
SLEEP ABNORMALITIES - Normally, there is a decrease in alveolar ventilation, decrease in
PaO2, and increase in PaCO2 during sleep. These changes are greatest during the rapid eye
movement (REM) phase of sleep. The severities of the changes tend to get worse as the night
wears on. Most people tolerate these well but the degree of ABG changes are much greater in
the COPD patient. Supplemental oxygen decreases the severity of sleep-induced hypoxia and
accompanying arrhythmias. This can improve the quality of sleep for a COPD patient.
Fortunately, absolute sleep apnea is relatively uncommon. However, many COPD patients wake
up repeatedly due to hypoxia or to cough up accumulating secretions.
ACUTE RESPIRATORY FAILURE (ARF) - acute infections are thought to be the cause of
ARF in up to 55% of the cases. ARF in the COPD patient results in a PaCO2 greater than 50 or a
PaO2 less than 50 mm Hg. Patients usually get to the hospital awake and having a PaCO2 less
than 80 mm Hg. Uncontrolled oxygen therapy can cause hypoventilation and the PaCO2 to
increase in a patient on hypoxic drive. This complication usually does not occur until PaO2
exceeds 60 mm Hg. A useful clinical goal is to obtain a PaO2 of 50-60 mm Hg and % sat around
90% to avoid hypoventilation and tissue hypoxia. A 24-28% venturi mask or nasal cannula at
1-2 lpm is usually sufficient. As long as the pH remains above 7.25, COPD patients generally do
well. Intubation should be avoided, if possible. If hypoxia and hypercapnia continue to worsen,
mechanical ventilation may be necessary. It is important to avoid overzealousness in mechanical
ventilation by decreasing the PaCO2 too rapidly. COPD patients have a high bicarbonate level
from chronic hypercapnia. Too rapid of a reduction in CO2 can cause a severe alkalosis. The
result can be seizures, coma, or death.
In the past, it was recommended to perform a tracheostomy after 3-7 days of intubation. Today,
an endotracheal tube can be left in place up to 30 days before a tracheostomy procedure. A
tracheostomy causes as many problems as it solves, with infection being the most prominent. If
it is felt the patient will be extubated within a few weeks, tracheostomy should be avoided.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
38
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
It is important to ensure the patient is provided adequate nutrition while being ventilated. There
is usually significant muscle atrophy after recovery from ARF. These muscles need to be
repaired with proper nutrition and conditioning. High carbohydrate diets should be avoided.
Carbohydrates produce CO2 when metabolized thereby increasing the ventilatory workload.
This can be a problem in some patients, particularly during weaning.
Once hypoxia and hypercapnia are relieved, one should concentrate on relieving the precipitating
airway obstruction (whether on or off a ventilator). Adequate hydration, bronchodilators,
mucolytic-expectorants, and antibiotics should be provided, if necessary. Patients should be
re-evaluated frequently. Sputum cultures and gram stains also should be done.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
39
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
COR PULMONALE - Cor pulmonale is defined as an “enlargement of the right ventricle due
to an increase in the right ventricular afterload from diseases of the lung and pulmonary
circulation”. Pulmonary artery pressure (PAP) can go up to a mean of 60 mm Hg in COPD. The
major cause of this is hypoxemic vasoconstriction. (It also can be related to a loss of the
capillary bed in the emphysemic patient.) It is not clear why hypoxemic vasoconstriction does
this, but it may be from vasoconstrictor agents released from endothelial cells. If the patient is
acidotic, the condition is increased. Transmission of increased intrathoracic pressure caused by
chronic airway obstruction also can increase the PAP. A combination of the above can be
present in COPD leading to cor pulmonale.
Successful treatment consists of appropriate management of the underlying lung disease.
Hypoxia should be corrected with oxygen. Airway obstruction must be relieved as much as
possible. Diuretics may be necessary to decrease fluid levels. Pulmonary vasodilators are still
experimental.
PNEUMOTHORAX - Spontaneous pneumothorax in the normal patient causes minimal
symptoms or lung dysfunction. In the COPD patient a pneumothorax can be life-threatening. It
can also result in a persistent air leak making treatment very difficult. Pneumothorax should be
suspected if the patient experiences a sudden, severe exacerbation of dyspnea. Decreased or
absent breath sounds are the most important clinical symptom, but in COPD the breath sounds
are already diminished. A CXR, taken at full expiration for maximum sensitivity, is needed. If a
pneumothorax is present, intercostal chest tubes with water seal drainage may be needed.
Negative pressure also may be needed to re-expand the lung. Most leaks close after several days
but some need surgical closure. If surgery is too risky, instillation of tetracycline into the pleural
space may be given a trial. This causes a pleurodesis and adheres the pleura to close the hole.
GIANT BULLAE - Bullae occupying 1/3 to 1/2 of the hemithorax can cause mild to severe lung
dysfunction, depending upon the amount of normal vs. diseased lung tissue that is compressed.
Bullae may continue to enlarge over time if there is a check-valve mechanism that allows air to
enter but not leave.
Bullae are most often seen in smokers and most often in the upper lung zones. There is a two-toone preponderance for the right lung. Should the patient have significant symptoms, the bullae
should be excised. The most important prognostic sign is evidence of compression of lung tissue
and displacement of vascular structures on the CXR. If the compressed lung tissue is
emphysematous there is little gain from resection.
VENESECTION - As you are well aware, chronic hypoxemia may result in secondary
polycythemia. This increases blood viscosity as well as right ventricular load. If the patient’s
hematocrit exceeds 65%, venesection to improve hemodynamics can be considered.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
40
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
PROGNOSIS
M
ild airway obstruction has a favorable prognosis. Smoking cessation usually causes
expectoration to subside in the patient with chronic bronchitis. An approximate
mortality rate of 30% at one year, and 95% at ten years occurs in patients with an FEV1
severely below normal. (Normal FEV1 is 75% to 83% of FVC).
Many patients with severe disease survive for many years beyond the average. This is related to
the successful therapy of acute exacerbations. Patients who survive heart failure or ARF may
survive for many years. Death is generally from overwhelming infection, pneumonia, and
retained secretions with atelectasis, pneumothorax, cardiac arrhythmias, or pulmonary embolism.
THE GLOBAL INITIATIVE FOR CHRONIC OBSTRUCTIVE LUNG DISEASE
(GOLD)
A
s we have discussed in this course Chronic Obstructive Pulmonary Disease (COPD) is a
major cause of chronic morbidity and death throughout the world. A committee
composed of health professionals, public health authorities, and the general public was
formed to address the issues of management and improvement of prevention for the ailment.
This is a worldwide effort, which will generate scientific reports on COPD, encourages
dissemination and adoption of the reports, and promotes international collaboration on COPD
research.
Chronic bronchitis and emphysema were discussed together because they are overlapping
conditions usually due to heavy cigarette smoking. COPD is more often used to indicate chronic
bronchitis and/or emphysema, which have a similar etiology. Asthma, cystic fibrosis and
bronchiectasis are clearly different diseases. Asthma may be a lifelong disease, but tends to be
more severe in children and young adults. Cystic fibrosis is actually a disease of the exocrine
glands with severe detrimental pulmonary effects. Bronchiectasis is really a complication of
previous disease rather than a disease in itself.
OVERLAP OF COPD
EMPHYSEMA
CHRONIC
BRONCHITIS
ASTHMA
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
41
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
OTHER OBSTRUCTIVE DISEASES
ASTHMA
A
sthma is recognized as a complex disorder of the airways, This chronic inflammatory
disease affects more than 22 million people in the United States.2 These figures may be
an underestimate of actual number of asthma patients.
It is now recognized that not all asthma is completely reversible, and there is renewed emphasis
on the role of inflammation in the disease. The pathogenesis of asthma that occurs in the
pediatric patient does not differ from that in the adult. The highest incidence of asthma is noted
in urban settings; among blacks in all geographic locations; and among children who were born
to mothers who smoked cigarettes, children living in poverty, children who had low birth weight,
and children born to mothers under 20 years old.
ETIOLOGY
Extrinsic asthma (allergic asthma)
Extrinsic asthma begins in childhood. The causes can be verified and include but are not limited
to the inhalation of airborne antigens such as dust and pollens. Often exercise can precipitate
bronchospasm in these potential patients.
Intrinsic asthma (nonallergic asthma)
Intrinsic asthma may be considered a nonseasonal, nonallergic form of asthma that occurs in
adult life. Precipitating factors include such pollutants as dust, fumes, smoke and many others.
Infections and emotional crisis can initiate an attack.
PATHOPHYSIOLOGY
Stimulation of mast cells in the tracheal bronchial tree causes the release of:
•
Histamine
•
Leukotrienes
•
Slow - reacting substance of anaphylaxis
•
Eosinophilic chemotactic factor of anaphylaxis
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
42
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
•
Prostaglandins
As a result of the release of these substances the following occurrences begin:
•
Bronchoconstriction
•
Mucosal edema
•
Increased mucus production
•
Accumulation of eosinophils in blood
•
Vasodilation
CLINICAL SIGNS AND SYMPTOMS
The symptoms may start with mild wheezing and cough initially, which may progress to severe
dyspnea if the attack is not controlled. The patient may not have a productive cough initially,
however, this may change later. If laboratory examinations of the secretions reveal high
eosinophil levels (1% to 3% is considered normal), the etiology of asthma is most likely allergic.
Severe attacks will cause the patient to use their accessory muscles to breathe and display
intercostal and supraclavicular retractions. The presents of pulsus paradoxus (systolic blood
pressure is 10 torr higher on expiration than on inspiration) may indicate severe air trapping,
cardiac tamponade, advanced heart failure and other conditions. Tachycardia and tachypnea are
part of the early signs and symptoms of asthma. Initial ABG results reveal hypoxemia and
hypocapnia. If the patient’s condition deteriorates and work of breathing increase they will
develop hypercapnia indicating the need for intubation. Cyanosis, if present, indicates a severe
decrease in oxygen saturation
X-ray Characteristics
Hyperinflation (hyperlucency of lung fields) is present with air trapping. Atelectasis may be
present, however, it is uncommon. Possible pulmonary infiltrates may also be observed.
Pulmonary Function Studies
Pulmonary function studies will usually reveal a decreased PEF and FEV1, FVC, FEV1/FVC
ratio will also be decreased. Asthmatics will have an increase in their residual volume resulting
from air trapping.
CLASSIFICATION OF ASTHMA
Several expert panel reports are used by the National Asthma Education Program (NAEP) to
establish the following guidelines for classification of asthma.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
43
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Mild Intermittent
•
< 1 times per week
•
Brief exacerbations
•
Nighttime symptoms < 2 times per month
•
Asymptomatic with normal lung function between exacerbations
•
FEV1 and PEF < 80% of predicted
•
PEF variability < 20%
Mild Persistent
•
Symptoms > 2 times per week, but < 1 time per day
•
Exacerbations may affect activity
•
Nighttime symptoms > 3 times per month
•
FEV1 and PEF < 80% predicted
•
PEF variability 20-30%
Moderate Persistent
•
Daily symptoms
•
Exacerbation < 2 times per week affecting activity
•
Nighttime asthma symptoms > 1 times per week
•
Daily use of short-acting beta-agonist
•
FEV1 and PEF > 60% and < 80% of predicted
•
PEF variability > 30%
Severe Persistent
•
Continuous symptoms
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
44
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
•
Frequent exacerbations
•
Frequent nighttime symptoms
•
Limited activity
•
FEV1 and PEF < 60% of predicted
•
PEF variability >30%
CLASSIFICATION OF PHARMACOLOGIC THERAPY
Quick Relief Medication
•
Short-acting beta-agonist
•
Inhaled anticholinergics
•
Systemic corticosteroids
Long-term Control Medications
•
Corticosteroids
•
Leukotriene modifiers
•
Cromolyn sodium, nedocromil
•
Long-acting inhaled beta-agonists
•
Methylxanthines
The National Institute of Health has established guidelines for the pharmacological management,
control, and prevention of asthma. 9 The following is a stepwise approach used for management
of asthma based on the severity of symptoms. The patient’s response to the treatments should be
reviewed every 1 to 6 months. If the patient is managing their symptoms with sustained control
for at least 3 months, a gradual stepwise reduction in treatment may be indicated. If the patient is
unable to manage their symptoms, as evidenced by using the fast-acting beta2 bronchodilator
every day, then a step up in treatment may be necessary.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
45
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
MANAGEMENT OF ASTHMA.9
Severity of Symptoms
Step 1. Mild Intermittent
Symptoms occur less than once per week, nocturnal symptoms occur less than twice per month,
asymptomatic between exacerbations.
Fast Relief:
Fast-acting beta2 bronchodilator as needed for symptoms.
Long-term Control:
No daily medications needed.
Step 2. Mild Persistent
Symptoms occur two or more times per week, nocturnal symptoms occur three or more times per
month.
Fast Relief:
Fast-acting beta2 bronchodilator as needed for symptoms.
Long-term Control:
Inhaled anti-inflammatory medications in low doses:
Corticosteroid, cromolyn or nedocromil,
OR
Oral sustained-release theophylline to serum concentration of 5 to 15 mcg/mL,
OR
A leukotriene inhibitor may be considered (position in therapy is not fully established).
Step 3. Moderate Persistent
Symptoms occur daily, nocturnal symptoms occur two or more times per week.
Fast Relief:
Fast-acting beta2 bronchodilator as needed for symptoms.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
46
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Long-term Control:
Inhaled anti-inflammatory corticosteroid medication in medium dose,
OR
Inhaled corticosteroid in low to medium dose,
PLUS
A long-acting bronchodilator (especially for nocturnal symptoms),either a long-acting
beta2agonist, or sustained release theophylline.
Step 4. Severe Persistent
Continuous symptoms, frequent nocturnal symptoms, severity of symptoms limit activities of
daily living.
Fast Relief:
Fast-acting beta2 bronchodilator as needed for symptoms.
Long-term Control:
Inhaled anti-inflammatory corticosteroid in high dose,
PLUS
A long-acting bronchodilator; either a long acting beta2 drug, or sustained-release
theophylline,
PLUS
Oral corticosteroid tablets or syrup.
CYSTIC FIBROSIS (MUCOVISCIDOSIS)
ETIOLOGY
C
ystic Fibrosis is a disease that was not clinically reported until 1936. It is a major cause
of chronic lung disease and death in children. Approximately 1 in every 2000 live births
of Caucasians, and 1 in 17,000 live births in blacks are diagnosed with the disease. Both
parents must carry the genetic mutation for the disease to be transmitted to their children. Cystic
fibrosis is an autosomal recessive disorder characterized by thick secretions that lead to
obstruction of the airways. This disease process affects several organs of the body. Principal
problems associated with cystic fibrosis are bronchiectasis, pancreatic exocrine insufficiency,
and an elevated sweat electrolyte concentration. In past decades, patients with cystic fibrosis
rarely survived past the age of 20. With recent advances in medicine, these patients can now
survive into their 30’s or 40’s.8
Pathophysiology
Three common findings are associated with cystic fibrosis. They are referred to as the triad of
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
47
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
cystic fibrosis, they are:
1. Chronic pulmonary disease
2. Pancreatic deficiency
3. High sweat electrolyte concentration
A generalized disorder of exocrine gland function impairs the clearance of secretions from
various organs in the body. Hypertrophy of the goblet cells cause hypersecretion of mucus,
which leads to mucus plugging, increased airway resistance and atelectasis. At birth the function
of the pancreas may be normal. After the first few months’ secretions become thick and cause
dilation and destruction of the exocrine ducts. Stool size and number may increase because of
the fibrosis and fatty infiltration of the pancreas. The defect of epithelial fluid and electrolyte
exchange due to a faulty chloride channel is the basic pathophysiology of abnormality. Chloride
sweat test is used to make a definitive diagnosis. Levels above 60 mEq/L in children and 80
mEq/l in adults in the proper clinical setting are diagnostic of cystic fibrosis.
Some cystic fibrosis infants will sweat excessively. Failure of the sweat glands to reabsorb
sodium, chloride, and potassium lead to elevated electrolyte levels. After kissing an infant and
noticing a salty taste may be a physical finding of significance and prompt a call for medical
consultation.
LABORATORY STUDIES
Genetic testing
The gene for cystic fibrosis has been localized to chromosome 7. The gene can now be detected
as early as the 10th week of gestation, using chorionic villus (placental tissues) sampling and
DNA analysis.
Pulmonary function testing
Simple spirometry reveals an obstructive defect. Expiratory flow rates are decreased with an
increase in FRC and TLC, particularly in the advanced disease state.
Sputum cultures
Sputum cultures are very beneficial in identifying the specific pathogen causing the infection.
Arterial blood gas analysis
Blood gases can be normal or reveal mild hypoxemia during periods of disease stability. Disease
progression will result in chronic hypoxemia and hypercarbia.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
48
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
Chest radiograph
Radiograph can:
•
monitor the degree of hyperinflation
•
monitor the size of the heart
•
identify and localize areas of consolidation
•
rule out a pneumothorax
TREATMENT
Treatment plans should be individually designed based on the severity of the disease and the
existing symptoms. A respiratory treatment plan should include:
•
Bronchial hygiene program that includes chest physiotherapy and postural drainage.
•
PEP mask therapy, autogenic drainage (AD) and flutter valve therapy.
•
Intravenous antibiotics to enhance the treatment of gram-negative bacterial infections.
•
Aerosolizated antibiotics to enhance the treatment of gram-negative bacterial
infections.
Prophylactic immunization for measles, pertussis, and influenza reduce the incidence
of pulmonary infection.
•
BRONCHIECTASIS
B
ronchiectasis is an irreversible dilation of the lumen of bronchi and bronchioles, chronic
in nature, that results in inflammation and destruction to the walls of these airway.
Because of the impairment of bronchial clearance, increased bronchial secretion becomes
stagnant and secondarily infected. Destruction of bronchial structure and dilation continue
resulting in a self-sustaining, sometimes progressively advancing, pathologic process.
ETIOLOGY
It is not clear what exact basic abnormality puts in motion the pathologic changes of
bronchiectasis. It is known that some diseases or condition that occur in childhood may be
predisposing factor, even though bronchiectasis can develop at any age. Some examples are
chronic respiratory infections, tuberculous lesions, and patients with cystic fibrosis and patients
that may have had obstruction of the bronchus due to a foreign object, such as a peanut. With
the increased use of computed tomography (CT) imaging technology for investigation of lung
disease, bronchiectasis has been recognized to be a complication of such condition as rheumatoid
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
49
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
lung disease, acquired immunodeficiency syndrome (AIDS), smoke inhalation and transplant
rejection.
PATHOPHYSIOLOGY
It is not known whether the chronic dilation is a result of destructive changes in the bronchial
walls due to inflammation and infection or possibly a congenital defect of the airways.
Bronchial obstruction may render the mucociliary transport system ineffective, leading to an
accumulation of thick secretions. The bronchial wall is destroyed, with resultant atrophy of the
mucosal layer.
CLINICAL SIGNS AND SYMPTOMS
The most common symptoms of bronchietasis are cough and expectoration. The cough is
generally productive with large amount of thick purulent secretions; may be foul smelling; often
a layering of the sputum occurs. Hemoptysis may also be present. Some patient will have
copious amounts of sputum ( > several hundred milliliters per day) and some much less, while
others may not have any at all. Bronchiectasis without increased sputum production is referred
to as dry bronchiectasis. Recurrent pulmonary infections as a result of secretion retention are
very common. Hypoxemia occurs in both the early and advanced stages can lead to the
development of cyanosis. Ventilatory efforts in the early stages produce respiratory alkalosis,
while in the advanced stages of the disease the patient will develop respiratory acidosis. A barrel
chest may develop because of airway trapping resulting from airway obstruction.
X-ray characteristics
Findings of the chest x-ray will show the following:
•
Increased lung markings
•
Flattened diaphragm
•
Segmental atelectasis
•
Peribronchial fibrosis
•
Occasional multiple air-fluid levels
Sputum smear
Results:
•
Increased WBC
•
Gram-positive and gram-negative
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
50
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
•
Aerobic and anaerobic bacteria
•
Common organisms
haemophilus influenzae
staphylococcus pneumoniae
moraxella catarrhalis
mycobacterium avium
aspergillus
Pulmonary function studies
Many patients with mild to moderate bronchiectasis will have no abnormality detectable by
routine spirometry and arterial blood gas analysis. However, with advanced disease, patients
may show deterioration in lung volumes, ventilation mechanics, ventilation perfusion (V/Q)
mismatching.
TREATMENT
When designing the respiratory care plan the following therapeutic modalities should be
included:
•
Chest physical therapy
•
Aerosol therapy
•
Bronchodilator therapy
•
Mucolytics
•
Antibiotics
•
Oxygen therapy
•
Expectorants
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
51
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
SUMMARY
C
OPD is most commonly associated with the disease processes of chronic bronchitis and
emphysema. Most patients have components of both. Emphysema results in a
permanent enlargement and destruction of the lung parenchyma. Chronic bronchitis
results in chronic hypersecretion and a productive cough with inflammation and scarring of the
lining of the bronchial tubes. COPD can be defined as a state of dyspnea on exertion with
objective evidence of decreased airflow not explained by specific heart or lung disease.
The pathology of chronic bronchitis includes hyperplasia, hypertrophy and dilation of bronchial
gland ducts. There are inflammatory changes in the airways and hypersecretion is present.
There is a loss of ciliated epithelium. The pathology of emphysema includes destruction of
alveolar walls and pulmonary capillaries. The connective tissue and elastic structure of the lung
are destroyed. There is a loss of elastic recoil and significant airtrapping. Surface area for gas
exchange is lost.
The pathogenesis of chronic bronchitis appears to be related to chronic bronchial injury.
Tobacco smoke and infection are the most common causes of chronic injury. The exact cause of
emphysema is unknown but animal experiments suggest an imbalance of lung elastase/
antielastase. Tobacco smoke has been implicated as a cause. Cigarette smokers have a higher
incidence of emphysema than the general population. In the United States, smoking accounts for
80-90% of the risk for developing COPD.
Specific therapy for COPD primarily consists of avoiding inhaled irritants. Smoking cessation is
the most important specific therapy. Symptomatic therapy is used to decrease mucosal
congestion and edema, decrease secretion, decrease bronchospasm, and decrease cellular
infiltration and inflammation. Water, bronchodilators, mucolytics, anticholinergics,
corticosteroids, antibiotics, and chest physical therapy are used.
Oxygen therapy can be used to treat both acute and chronic hypoxia. When used for the former,
it is considered symptomatic therapy. When used for the latter, it is considered secondary
therapy. Additional secondary therapies consist of rehabilitation and physical therapy. Graded
muscle exercises, breathing retraining, and instruction in the performance of activities of daily
living are examples of secondary therapy.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
52
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
CLINICAL PRACTICE EXERCISE
The following practice exercise is discussed at the end of the course.
1. The patient is a 70-year-old female admitted for increasing shortness of breath and congested
nonproductive cough times 3 days. The patient has smoked cigarettes for 45 years and normally
has a productive cough of small amounts of thick white-pale yellow mucus. Physical
examination reveals use of accessory muscles on inspiration with little to no discernible chest
movement. Breath sounds are bilaterally decreased and absent in the left lower lobe. The neck
veins are distended and there is no fever. Evaluate this information and make recommendations.
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
2. ABG’s reveal pH 7.34, PaCO2 70, PaO2 51, HCO3 32, % sat 82%. CXR reveals hyperinflated
lungs, widening of costaphrenic angle, and a left lower lobe infiltrate. WBC’s are normal,
hemoglobin is 16 grams. Patient refuses to perform spirometry. Evaluate this information and
make specific, symptomatic, and secondary therapy suggestions.
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
______________________________________________________________________________
3. This patient is a 53-year-old woman with emphysema and congestive heart failure. She is on
a chronic regime of digitalis, Lasix, and steroids. She presents to the emergency department
with weakness and shortness of breath. The following blood gases, vital signs, blood work, and
electrolytes were reported in the emergency department: ABG’s reveal, FIO2 0.21, pH 7.43,
PaCO2 78 mm Hg, HCO3 50 mEq/L, PaO2 51 mm Hg, SaO2 88%; Vital Signs, Pulse 126/min,
BP 110/80, Temperature 37o C, RR 26/min, Bloodwork WBC 8000 mm3, Hb 16 g%, Hct 48%;
Plasma Electrolytes, Na+ 142 mEq/L, CO2 51 mEq/L, Cl- 80 mEq/L, K+ 2.6 mEq/L
a. Classify the arterial blood gas.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
53
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
b. State any conditions that are present that might alert the clinician to the potential that a mixed
disturbance exists.
c. Is the patient receiving any drugs that could cause metabolic alkalosis? If so, name them.
d. Are there any electrolyte abnormalities that could contribute to metabolic alkalosis in this
patient? Explain.
e. Is it possible that congestive heart failure (disease itself) can cause metabolic alkalosis?
Explain.
f. What drugs that this patient is receiving could lead to hypokalemia?
g. How should the metabolic alkalosis be treated in this patient?
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
54
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
h. Is oxygen therapy indicated? If so, what is the target PaO2?
i. What FIO2 is indicated?
j. What could explain the weakness in this patient?
PRACTICE EXERCISE DISCUSSION
1. Patient’s age, smoking history, and chronic productive cough indicate underlying COPD. Use
of accessory muscles in breathing and lack of chest movement is compatible with an ineffective
diaphragm. This is probably related to air trapping. Bilateral decreased breath sounds and
distended neck veins are also compatible with air trapping. Infection is the most common reason
for COPD admissions so work patient up for left lower lobe pneumonia. Lack of fever in the
COPD patient does not rule out infection. Suggest CXR, ABG, CBC, and bedside spirometry for
further diagnosis and baseline values. Suggest low flow O2 for dyspnea.
2. CXR is indicative of COPD with left lower lobe pneumonia. ABG indicative of chronic
hypercapnia with acute decompensation and hypoxia. Lack of elevated WBC in acute infection
in COPD not uncommon. Elevated hemoglobin probably is in response to chronic hypoxia. For
specific treatment, recommend stop smoking and influenza vaccine. For symptomatic treatment,
recommend O2, encourage fluids, chest physical therapy to left lower lobe, trial bronchodilator
treatment to assess reversibility of obstruction; attempt to get sputum sample for cultures. For
secondary treatment, evaluate patient for home O2, breathing retraining, and if cooperative,
graded exercises and instruction in activities of daily living.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
55
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
SUGGESTED READING AND REFERENCES
1. The American Lung Association (2003). Chronic Obstructive Pulmonary Disease. American
Lung Association Fact Sheet. (On-Line). Available: lungusa.org/diseases/copd_factsheet.html.
2. The Center for Disease Control (CDC). (2004). Facts About Chronic Obstructive Pulmonary
Disease. (On-Line). Available: cdc.gov/nceh/cond/condfaq.htm.
3. Murray, John F., et al. (2000). Textbook of Respiratory Medicine. 3rd Edition. Publisher:
WB Saunders Company.
4. Gold, Warren M., et al. (2002). Atlas of Procedures in Respiratory Medicine. Publisher: WB
Saunders Company.
5. Lewis, Sharon, et al. (2003). Medical Surgical Nursing. Publisher: Elsevier Science.
6. Wyka, Kenneth A., et al. (2001). Foundations of Respiratory Care. Publisher: Delmar
Learning.
7. Arky, Ronald MD, et al, Medical Economics Staff. (2004). Physicians' Desk Reference. 58th
Edition. Medical Economics Company, Inc.
8. Damico, Christine M., RM, MSN, CPNP, et al. (2004). Nursing 2004 Drug Handbook.
Springhouse Corporation.
9. The National Institute of Health and the National Heart, Lung, & Blood Institute. (2001).
Guidelines for the Diagnosis and Management of Asthma. (On-Line). Available:
nhlbi.nih.gov/guidelines/asthma/asthgdln.htm.
10. DHD Healthcare Corporation. (2004). Acapella® Vibratory PEP Therapy System.
Wampsville, NY.
11. Axcan Scandipharm Company. (2004). Flutter® Mucus Clearance Device. (On-Line).
Available: axcanscandipharm.
12. Muller, Nestor L., et al. (2001). Radiologic Diagnosis of Diseases of the Chest. 1st Edition.
Publisher: WB Saunders Company.
13. Miller-Keane Medical Dictionary. (2000). Pulmonary Function Tests. (On-Line).
Available: my.webmd.com/content/assert/miller_keane_27551.
14. Whitaker, Kent B. (2000). Comprehensive Perinatal and Pediatric Respiratory Care.
Publisher: Delmar Learning.
15. Oakes, Dana F. (2000). Neonatal/Pediatric Respiratory Care. Health Educator Publications,
Inc.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
56
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
16. Oakes, Dana F. (2000). Clinical Practitioners Pocket Guide to Respiratory Care. Health
Educator Publications, Inc.
17. Klenschmidt, P. Chronic Obstructive Pulmonary Disease and Emphysema from Emergency
Medicine/Pulmonary. Emedicine.com, 2001.
18. Nosworthy, J. and the Working Party Membership of Royal Melbourne Hospital,
GUIDELINES FOR THE HOSPITAL MANAGEMENT OF CHRONIC OBSTRUCTIVE
PULMONARY DISEASE, 2000.
19. National Center for Health Statistics. National Health Interview Survey: Research for the
1995-2004 redesign. Hyattsville, MD: US Department of Health and Human Services, CDC,
NCHS. Vital and Health Stat 2(126), 1999. Available at
http://cdc.gov/nchs/about/major/nhis/hisredesign.htm.
20. National Center for Health Statistics. National Health Interview Survey: Hyattsville, MD:
US Department of Health and Human Services, CDC, NCHS, 2001. Available at
http://cdc.gov/nchs/nhis.htm.
21. National Center for Health Statistics. National Hospital Discharge Survey. Hyattsville, MD:
US Department of Health and Human Services, CDC, NCHS. Vital and Health Stat: series 13
(issues from 1995-2000). Available at http://cdc.gov/nchs/about/major/hdasd/nhds.htm.
22. National Center for Health Statistics. National Hospital Ambulatory Medical Care Survey.
Hyattsville, MD: US Department of Health and Human Services, CDC, NCHS, 1995-2000.
Available at http://cdc.gov/nchs/about/major/ahcd/ahcd1.htm.
23. National Center for Health Statistics. National Vital Statistics System. Hyattsville, MD: US
Department of Health and Human Services, CDC, NCHS, 1995-2000. Available at
http://cdc.gov/nchs/nvss.htm.
24. National Heart, Lung, and Blood Institute. Morbidity and Mortality: 2002. Chartbook on
Cardiovascular, Lung, and Blood Diseases. Bethesda, MD: US Department of Health and
Human Services, NIH, NHLBI. May 2002. Available at
http://www.nhlbi.nih.gov/resources/docs/02_chtbk.pdf.
25. Global Initiative for Chronic Obstructive Lung Disease. Available at
http://www.goldcopd.com
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
57
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
POST TEST
DIRECTIONS: IF COURSE WAS MAILED TO YOU, CIRCLE THE MOST CORRECT
ANSWERS ON THE ANSWER SHEET PROVIDED AND RETURN TO: RCECS, 16781
VAN BUREN BLVD, SUITE B, RIVERSIDE, CA 92504-5798 OR FAX TO: (951) 789-8861.
IF YOU ELECTED ONLINE DELIVERY, COMPLETE THE TEST ONLINE – PLEASE
DO NOT MAIL OR FAX BACK.
1. A definition of emphysema is:
a. Acute reversible airway obstruction.
b. Presence of a chronic productive cough for 3 months in each of two
successive years.
c. Acute small airways inflammation.
d. Abnormal permanent enlargement of the distal air spaces with destruction of
alveolar walls.
2. A definition of chronic bronchitis is:
a. Acute reversible airway obstruction.
b. Presence of a chronic productive cough for 3 months in each of 2 successive
years.
c. Abnormal permanent enlargement of the distal air spaces with destruction of
alveolar walls.
d. Acute small airways inflammation.
3. Secondary therapy (therapy that improves daily functioning) for COPD consists of:
a.
b.
c.
d.
Graded muscle exercises.
Breathing retraining.
Instruction in the performance of daily activities.
All of the above.
4. What does the CXR in COPD generally reveal?
a.
b.
c.
d.
Hyperinflation.
Congested lungs.
Flattened diaphragms.
All the above.
5. Which is a complication of COPD?
a.
b.
c.
d.
Premature atrial contractions.
Renal failure.
Acute respiratory failure.
Tachycardia.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
58
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
6. Leukotriene modifiers are considered as long-term control medication in the asthmatic
patient.
a. True.
b. False.
7. A distinctive physical finding on the COPD patient is:
1.
2.
3.
4.
a.
b.
c.
d.
airtrapping.
use of the accessory muscles.
increase in the chest A-P diameter.
deep vein thrombosis.
1, 2, 3.
2, 3, 4.
2, 4.
1, 2, 3, 4.
8. Jugular venous distention in the COPD patient may be caused by:
a.
b.
c.
d.
e.
Diabetes.
Chronic respiratory acidosis.
Airtrapping.
Frequent infections.
c & d.
9. Which of the following is specific therapy aimed at preventing further deterioration in
COPD?
1.
2.
3.
4.
a.
b.
c.
d.
removes and avoids irritants.
stop smoking.
annual influenza vaccine.
bronchodilators.
1, 3, 4
1, 2, 3
1, 2, 4
1, 2, 3, 4
10. COPD, as classified by the American Lung Association, includes emphysema and
chronic bronchitis.
a. True
b. False
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
59
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
11. The pathology of COPD consists of:
1.
2.
3.
4.
a.
b.
c.
d.
e.
loss of connective tissue.
airway inflammation.
airtrapping.
loss of gas exchange surface area.
1, 2, 3, 4
1 only
1, 3
2, 3
2, 3, 4
12. Patients diagnosed with asthma, who also have chronic bronchitis, are classified as
COPD patients by the American Lung Association.
a. True
b. False
13. Major pathological changes that take place in chronic bronchitis are:
1.
2.
3.
4.
a.
b.
c.
d.
e.
increase in bronchial gland size.
destruction of lung parenchyma.
hypersecretion.
increase goblet cells.
1, 2, 3
1, 2, 3, 4
1, 3, 4
2, 3
2, 3, 4
14. Genetic testing can be performed as early as the 5th week of gestation to determine cystic
fibrosis.
a. True.
b. False.
15. A patient classified as severe persistent asthma will have all of the following signs or
symptoms except:
a.
b.
c.
d.
limited activity.
FEV1 and/or PEF > 80% of predicted.
PEF variability > 30%.
frequent nighttime symptoms.
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
60
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
16. Treatment of the patient with bronchiectasis includes:
a.
b.
c.
d.
Bronchial hygiene techniques
Oxygen therapy
Antibiotics
All of the above
17. The general clinical history of the COPD patient usually DOES NOT include:
a.
b.
c.
d.
Chronic cough
Dyspnea on exertion
Fever
Wheezing
18. Asthma is defined as a:
a.
b.
c.
d.
Disease of the exocrine glands
Complication of chronic bronchitis
Chronic inflammatory disease
None of the above
19. Bronchiectasis results in:
a.
b.
c.
d.
Tuberculosis
Dilation of bronchi and bronchioles
Cystic fibrosis
Transplant rejection
20. Which of the following statements are TRUE when discussing structural vs.
functional changes in the COPD patient?
a. There is little correlation between structural and functional changes in the
chronic bronchitic.
b. There is a poor correlation between airflow limitation and bronchiolar
pathology in the emphysema patient.
c. There is an insignificant correlation between structural and functional changes
in the emphysema patient.
d. The main change in the chronic bronchitic is a decrease in the size and
number of mucus glands.
KM: Test Version F
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
61
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
ANSWER SHEET
NAME____________________________________ STATE LIC #__________________
ADDRESS_________________________________ AARC# (if applic.)_____________
DIRECTIONS: (REFER TO THE TEXT IF NECESSARY – PASSING SCORE FOR CE
CREDIT IS 70%). IF COURSE WAS MAILED TO YOU, CIRCLE THE MOST CORRECT
ANSWERS AND RETURN TO:
RCECS, 16781 VAN BUREN BLVD, SUITE B,
RIVERSIDE, CA 92504-5798 OR FAX TO: (951) 789-8861. IF YOU ELECTED ONLINE
DELIVERY, COMPLETE THE TEST ONLINE – PLEASE DO NOT MAIL OR FAX BACK.
1.
a b c d
16. a b c d
2.
a b c d
17. a b c d
3.
a b c d
18. a b c d
4.
a b c d
19. a b c d
5.
a b c d
20. a b c d
6.
a b
7.
a b c d
8.
a b c d e
9.
a b c d
10. a b
11. a b c d e
12. a b
13. a b c d e
14. a b
15. a b c d
KM: Test Version F
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
62
CHRONIC OBSTRUCTIVE PULMONARY DISEASE
EVALUATION FORM
NAME:____________________________________________ DATE:______________
AARC # (if applic.)________________________ STATE LICENSE #:______________
RC Educational Consulting Services, Inc. wishes to provide our clients with the highest quality
CE materials possible. Your honest feedback helps us to continually improve our courses and
meet CE regulations in many states. Please complete this form and return/submit it with your
answer sheet. Thank you.
YES
NO
Were the objectives of the course met?
Was the material clear and understandable?
Was the material well-organized?
Was the material relevant to your job?
Did you learn something new?
Was the material interesting?
Were the illustrations, if any, helpful?
Would you recommend this course to a friend?
What was the most valuable portion of the material?
________________________________________________________________________
What was the least valuable portion of the material?
________________________________________________________________________
Suggestions for future courses: ______________________________________________
Comments: ______________________________________________________________
________________________________________________________________________
What is your specialty area?______________________________ Credentials?________
How did you hear about RCECS?____________________________________________
This material is copyrighted by RC Educational Consulting Services, Inc. Unauthorized duplication is prohibited by law.
63