CalWHO
2014
Theme Guide
Reproductive Rights
The CalWHO 2014 Theme Guide on Reproductive Rights was created and
designed by Leah Shipton, Erin Bell, Leah Schmidt, Vidhya Bavanala and
Daniela Urrego.
Images used throughout the document are not the property of CalWHO.
Contents
Introduction to Reproductive Rights
2
Section 1: Sexual Health
1.1 Female Genital Mutilation (FGM)
Definition
Policy Timeline
Current Topic Status
Impact
3
1.2 Sexually Transmitted Infections (STIs)
Definition
Policy Timeline
Current Topic Status
Impact
Section 2: Family Planning
2.1 Contraceptions
Definition
Policy Timeline
Current Topic Status
Impact
2.2 Abortion
Definition
Policy Timeline
Current Topic Status
Impact
Section 3: Maternal Care
3.1 Prenatal Care
Definition
Policy Timeline
Current Topic Status
Impact
3.2 Postnatal Care
Definition
Policy Timeline
Current Topic Status
Impact
4
5
6
8
9
10
11
14
16
17
18
19
21
22
23
24
26
28
29
30
31
33
34
35
36
38
2
Section I:
Sexual Health
1.1 Defining FGM
Female genital mutilation (FGM) involves any practice, which partially or fully removes external female
genitalia for non-medical purposes (UNICEF, 2013). It is done for traditional, cultural or religious reasons
most often between infancy and age 15. Today over 125 million girls have been cut worldwide.
The WHO is firmly against FGM because:
(1) it shows deep-rooted inequalities between men and women;
(2) it is carried out on minors, which violates their rights; and
(3) it violates a person’s rights to health, security and physical integrity, right to be free from torture and
inhumane treatment, and the right to life when the procedure results in death.
FGM was once called female circumcision, but was changed to mutilation to distinguish from male
circumcision and to reflect the severity of the act that is greater than what male circumcision comprises
(UNFPA).
Possible immediate and long term health implications of FGM include: severe acute and chronic pain,
excessive bleeding, difficulty urinating, infections (eg. urogenital, sexually transmitted, etc.) death,
psychological trauma, reduced quality of sexual life, and birth complications (WHO, 2014).
The four major types of FGM are (UNICEF, 2013):
(1) Clitoridectomy: partial or total removal of the clitoris,
(2) Excision: partial or total removal of the clitoris and labia minora and sometimes the labia majora,
(3) Infibulation: narrowing of the vaginal canal to create a seal by cutting and repositioning the inner or
outer labia, sometimes clitoris is removed; and
(4) any other harmful procedures for non-medical purposes including pricking, piercing, scraping, and
incising
How should the healthcare systems of Western nations support victims of FGM?
How does FGM complicate reproduction?
What are the competing perceptions of FGM in African communities?
How does migration influence FGM practices?
What are the roles of healthcare workers in the practice of FGM?
How do men perceive FGM in their communities?
What are the long term psychological consequences of FGM?
How does FGM influence a woman’s sexuality?
4
Policy Timeline
1999
2002
2012
February 1, 1999 - Member Nations
• Developed and implemented legislation and policies prohibiting
traditional practices that harm health of girls, including FGM
• Mandated education about the harmful effects of FGM using various
media in local communities
• Promoted discussion of female empowerment through inclusion of
harmful traditional practices education in school curricula and health
personnel training
• Encouraged inclusion of all stakeholders in publicity campaigns
January 30, 2002 - Member Nations
Developed initiatives to:
• Collect and disseminate basic data on the prevalence of traditional
practices affecting the health of women and children, including FGM;
• Develop, adopt, implement national policy that prohibits harmful
traditional practices and persecutes the perpetrators;
• Establish a mechanism for policy implementation such as law
enforcement;
• Establish and strengthen support services for women and girls harmed
by traditional practices by training health providers capable of
assisting at all stages of such practices; and
• Promote economic opportunities for women to strengthen their
independence and capacity to protect themselves from forced
traditional practices.
December 20, 2012 - Member Nations
Developed initiatives to:
• Engage boys and girls to develop programs and promote
investment from religious organizations and educational institutions;
• Ensure all programs and policies implements to prevent and eliminate
FGM have indicators that allow for effective monitoring and impact
assessment;
• Implement programs to prevent and treat FGM in communities with
refugee and immigrant women; and
• Engage communities to work on ways to prevent and eliminate FGM
practices, in particular ways for those performing traditional practices
to find another livelihood.
5
Current Topic Status
Continent
Social &
Cultural Issues
• Social workers aren’t
necessarily educated about
the practice or how to
assist refugees who have
experienced the practice
and need physical and
psychological health
support (UNHCR, 2013).
• FGM practices are not
uniform within countries,
for example the prevalence
rate in Gambia is 78%, but
in some ethnic groups the
prevalence rate is 99%. It
is important for health
professionals to
understanding the different
practices of cultural
groups so that they know
what to look for in their
patients.
• Thought that 9.1% of
asylum seeking female
applicants are affected by
FGM.
• Based on limited
statistical data it is thought
that 20% of applicants are
seeking asylum for
FGM-related reasons.
Health Issues
Political Issues
• Women don’t like to be
examined in that area
because they feel
uncomfortable, and often
they need to have a
translator or their husband
in the room because of
the language barrier so
they don’t have
confidentiality (UNHCR,
2013).
• Member States
accepting asylum seekers
need to establish health
system policies that
recognize FGM as a form
of torture, in particular its
chronic impact because
women endure pelvic
infections, pain,
reproductive system
infections, delivery and
obstetrics complications,
and emotional and
psychological
disturbances.
• Health professionals in
asylum seeking
communities need to have
training in FGM so they
can provide appropriate
treatment and are able to
identify women who
suffer from FGM.
Training ethnic minorities
from FGM practicing
countries is an idea of
how to expand cultural
understanding in the
health care system.
• Country of Origin
(COI) document is not
tailored to understand and
address the specific
cultural and social
considerations for each
country, steps need to be
made to ensure
asylum-seekers from
FGM-practicing countries
will have their health
concerns addressed
(UNHCR, 2013)
• COI document should
assume an “FGM lens” in
which case the ‘safe
countries of origin’
depend on the gender
context of the applicant
(eg. Nigeria would not be
considered a safe country
of origin for a female
asylum seeker).
• Policies that facilitate
information and
knowledge exchange
between health
professionals addressing
these issues within the EU
would be beneficial.
• Require policies that
protect refugee girls
settled in EU communities
from FGM domestically
or outside of the country.
6
• FGM correlates with
ethnicity, not nationality
therefore it is important to
adjust elimination
strategies based on the
significance of FGM to
each community.
• FGM has been practiced
for centuries in many
communities, so the
decision to end it must
come from the men,
women, and community
leaders (WHO, 2008).
• History shows that when
interventions seek to
eradicate FGM without
community involvement
and consent a great
distrust can form between
the community and the
foreign parties.
• Patriarchy, culture, and
marriageability are three
social-level variables
enforcing FGM in
communities.
• It is feared that uncut
girls will not receive offers
of marriage, which is
particularly important in
some communities for
social and economic
protection. It becomes
important that
intra-marrying
communities begin a
dialogue about FGM and
how it pertains to
cultural/social
expectations, but also how
it relates to human rights
• If FGM is considered a
prerequisite to marriage
then it is crucial that
intra-marrying
communities decide to end
the practice together
• Where FGM is practiced
and accepted anyone who
refuses to participate faces
ostracization,
• In Egypt, Somalia and
Sudan FGM is
consistently carried out by
health workers (called
medicalization of FGM),
so creating medical
councils is crucial to
educating about the harm
of FGM (WHO, 2008).
• Health workers need to
be trained and have the
resources to treat the
physical and psycho-social
consequences of FGM in
the communities they
serve.
• In areas of countries
where health resources are
scarce it is important that
health professionals are
able to prevent and treat
FGM - training in treating
medical complications of
FGM as well as in health
promotion are crucial in
remote regions.
• Birth complications
increase as a result of
FGM, namely postpartum
haemorrhage, C-Section,
episiotomy, extended
hospital stay, and death.
• Convention on the
Elimination of Violence
Against Women passed a
bill in 1990 that all
Member States take action
against FGM. All but
Sudan and Somalia signed
the bill. Since national
policy and effective and
committed legal instruments are crucial to
eliminating FGM, it is
concerning that these
Member States did not
sign the bill (WHO, 2008).
• Involving stakeholders
at grassroots level and
religious/traditional
leaders in the development
of national policy and
legal proceedings is crucial
and has been an approach
used in The Gambia.
• Countries such as
Ethiopia, Kenya, and
Guinea-Bissau have
developing national
policies for the elimination
of FGM through Ministries of Justice.
• Creation of a national
policy eliminating FGM
and it’s media coverage is
only the first step, and acts
as a way for the government to show the population it’s commitment to
the issue and the repercussions. Media of prosecution cases are a way for
the government to reiterate the consequences of
performing FGM.
• Countries who’ve
developed national
policies for FGM are
varied in their enforcement.
• Often parents are
convicted of committing
FGM on their daughters,
which proves to complicate the family dynamics.
7
The Impact
My experience as a young girl was not
unlike other girls in Somalia. Experiencing
female genital mutilation is a necessary
passage to womanhood in my culture,
especially to be seen as appropriate for
marriage. Witnessed by my mother and
aunts, I was cut by an elderly woman in my
community. Only when I left Somalia for
asylum in France many years later did I
realize that the educational campaigns
against FGM implemented by other
African nations were absent in my home.
These messages of FGM as a human rights
violation, causing immense psychological
and physical health issues, did not reach
my community in time to prevent my
mutilation. After great struggle I have
found a doctor in France who understands
FGM and the long-lasting health
consequences, which is more important
now than ever because I am pregnant with
my first child. My doctor has explained the
numerous birth complications possible
due to FGM, and it makes me so nervous
and angry to see my life still plagued by my
childhood violation.
In Cameroon
95% of boys
and men think
FGM should be
discontinued
3 million girls
are at risk of
undergoing
FGM annually
In Egypt 77% of
all cutting was
done by
healthcare
providers
Daughters of
mothers who
have been cut
are more likely
to be cut
1.2 Defining STIs
Sexually transmitted infections (STIs) are a category of over 30 kinds of bacteria, viruses, and parasites
contracted primarily through sexual exchanges and to a lesser degree non-sexual contact (WHO, 2013).
The prevention of STIs includes counselling for safer sex practices, sexual education, promoting condom
use and targeting vulnerable populations with culturally appropriate interventions. Vaccines schedules for
HPV and Hepatitis B have been introduced as regular childhood and adolescent immunization regimes in
high and middle income countries. Diagnosing STIs varies with the resources available. In developed
countries facilities for testing all STIs are more available with appropriate counselling services.
Alternatively, low resource settings are privy to utilizing rapid STI tests to maximize convenience. In low
resource settings syndromic management is used as an alternative to expensive laboratory testing.
Syndromic management relies on identifying symptoms to diagnose infections. The four most prevalent
curable STIs are syphilis, chlamydia, gonorrhoea, and trichomoniasis; which are treated with relative ease
using antibiotics. Unfortunately, Herpes Simplex 2 and HIV are incurable, but can be regulated with
appropriate treatment regimens.
WHO seeks to improve the approaches to STI control by improving testing technologies, refining case
management procedures, and establishing Hepatitis B and HPV vaccination schedules in low income
countries. Prevention strategies must be multidimensional, utilizing biomedical and social knowledge to
restructure health cares systems to appropriately address STIs. Technologies effective in low resource
contexts are a crucial direction for research.
What groups are at most risk for STIs?
How do STIs effect the capacity of healthcare systems?
How does government policy influence the prevention and treatment of STIs?
Why is it difficult and controversial to address STIs, such as vaccinating for
HPV?
How does an individual context affect the experience and outcome of an STI?
How do healthcare systems prioritize which STIs to address?
9
Policy Timeline
Medieval
Era
15th-16th
Century
17th-19th
Century
1983
1987
2000
2007
• Connections between STIs and sexual activity established, but
symptoms are perceived as belonging to one disease (Venereol).
• Colombus and his fleet bring syphilis from the ‘Old World’ to ‘New
World’. Soldiers spread upon there return, sourcing an epidemic in
Europe.
• Unethical experiments on syphilis and gonorrhea patients stems
inaccurate myths and misinterpretations of illness etiology.
• The first assembly to address the AIDS epidemic (AIDS.gov, 2014).
• WHO launches the Global Program on AIDS, intentioned to raise
awareness, develop policies, provide support to struggling countires,
uphold human rights, and initiate research.
• UN Security Council discuss the impact of AIDS on African peace and
security
• WHO releases report outlining recommendations for health care
systems to address HIV/AIDS
10
Current Topic Status
Continent
Social &
Cultural Issues
• Seeking care for syphilis
is accompanied with
similar stigma to other
STIs. Receiving a syphilis
diagnosis and treatment
incurs judgment of
character and isolation
• Greater stigma is
assigned to vertical
transmission, when a
mother with HIV or
syphilis passes the disease
to her child
• Involving partners of
pregnant women with the
treatment process may be
difficult if economic or
social circumstances inhibit
their participation
Health Issues
Political Issues
• At 3.9% Latin America
has the highest maternal
syphilis rate in the world,
causing 165,000 to
350,000 cases of
congenital syphilis
annually with a 30-50%
mortality rate
• Improved maternal and
child health services which
screen and test for syphilis
in populations with
minimal access to health
care is necessary,
particularly to reduce
mother to child
transmission (MTCT) of
syphilis
• As HIV and syphilis
have similar prevention
and treatment patterns
developing programs and
policies that address them
in tandem is thought to be
more effective than
addressing them separately
• Establishing
comprehensive
surveillance of STIs
across the region to
monitor vulnerable
populations is important
to allocate health services
and intervention
appropriately and increase
the uptake of best
practices and the exchange
of clinical care lessons,
improving treatment and
prevention of STIs.
• Diagnosing syphilis
requires a serology test. If
a pregnant woman tests
• Political commitment to
educating vulnerable
regions about syphilis is an
important tool for
encouraging health
seeking behavior and
preventing transmission
• Policies to address
syphilis should capitalize
on the public health
efforts established by
governments to address
HIV in various
communities
• Governments need to
advocate and target
marginalized populations
with prevention and
treatment strategies for
STIs, particularly syphilis,
so that equitable access to
health services is
improved. Currently
countries that are
addressing the syphilis and
HIV epidemics effectively
still experience high rates
in their marginalized
populations (Elimination?)
• Syphilis should be
regarded as a serious
public health issue by
politicians and
government officials so
that concrete efforts are
taken to address the
epidemic.
11
• MSM and transgender
populations are often
addressed together, making
it difficult to target the
unique needs for prevention
and treatment strategies for
each group (WHO, 2013)
• Transgender people are
often involved in numerous
high-risk behaviors such as
sex work and drug use, this
should be considered when
seeking to understand their
risk to STIs and how to
prevent and treat them
appropriately
• Self-stigmatization for
HIV positive people is high
in this region, 23%
experiencing suicidal
thoughts (UNAIDS, 2013)
• Women with HIV report
higher experiences of
violence then those who do
not, particularly women
from minority groups such
as sex workers, female drug
users, and transgender
women. For example, in
India married women
sexually and physically
abused by their husbands
have a higher prevalence of
HIV
• Sex trafficking is a major
human rights violation in
countries of SEA and sex
workers are at an increased
risk for acquiring STIs. The
sex tourism and trafficking
industry perpetuates the risk
for young women and girls.
• In Southeast Asia transgender women are rarely
acknowledged for their
reproductive and sexual
health concerns pertaining
to STIs. leading to little
regarding how transgender
populations access services
for STIs. They require
special health services that
cannot be provided at
regular clinics, often they
resort to street vendors for
hormone therapy or medical transitions, increasing
the risk of STI transmission. (WHO, 2013)
• Many vulnerable populations rely on friends and the
internet for health information because they cannot
afford health services, fear
stigmatization, or in the
case of transgender populations, know that health care
professionals have little
information about their
health issues and how to
address their needs appropriately
• Many HIV clinics do not
have counseling services, so
the psychological repercussions of a diagnosis are not
addressed
• Expanding epidemics of
injection drug use are
increasing HIV rates in
Pakistan, Nepal, and Philippines (UNAIDS, 2013)
• MSM are still the fastest
growing HIV epidemic in
SEA
• Antiretroviral treatment
provision only covers 51%
of the region, far behind
the global coverage rate
• Community-based HIV
testing and counseling has
proven more effective at
drawing patients and
connecting them with
appropriate care
• Law is necessary to
protect transgender and
other vulnerable populations, to increase their
rights to employment and
health care services. For
example, punishing
discrimination or hate
crimes against transgender
populations to decrease
marginalization would
encourage their participation in mainstream society
(UNAIDS, 2013)
• Governments need to
acknowledge transgender
identity by having gender
fluidity on documents
such as passports, national
ID, and birth certificates.
Governments recognizing
their transgender populations are more effective at
reducing STI epidemics
and conducting ethical
research
• China, Fiji, Vietnam and
Mongolia are countries
who’ve removed policy
that criminalizes HIV
transmission as well as
minority group such as sex
worker and MSM have
witnessed reduction of
stigma and disease prevalence. Punitive laws hinder
effective population-level
responses to STI transmission.
• The Stigma Index
allows countries to generate policies and programs
that decrease barriers to
HIV testing and treatment
• Policy addressing the
domestic violence and
HIV should be enforced
extensively to prevent
transmission and improve
access to testing, counseling, and treatment.
12
• In the arctic regions
resident spend their summer
far from their communities
whaling and hunting, which
isolates their access to
health services (Law et al,
2008).
• Arctic residents inhabit a
very small community, so
there is a perception that
privacy and confidentiality
can be breached easily. This
makes accessing STI
servicing fearful.
• Discussing STIs with a
partner may be considered
taboo in the arctic as some
cultural norms view talking
about an issue as
synonymous with wishing
said issue upon someone.
This makes it difficult for
couples to have
conversations about safe sex
to uphold their sexual and
human rights
• The arctic regions of
Canada, Greenland and the
United States have higher
rates of gonorrhea and
Chlamydia than southern
regions. Highest rates are
among young aboriginal
women (Law et al, 2008).
• The extent to which
arctic populations are
educated about STI symptoms, treatment and
prevention techniques is
unknown
• Many arctic communities
are very remote and require
fly-in health services so
receiving treatment and
diagnostic care for STIs is
difficult.
• Health-seeking behavior
varies among the arctic
region, and the health care
systems of each nation may
influence how populations
access care for STIs.
Greenland and Alaska, USA
have universal healthcare
for aboriginal populations.
Canada has universal health
care, but the extent of
benefits vary between
aboriginals living on versus
off reserves
• Poor reproductive health
data is available for arctic
communities because of
limited surveillance,
blinding professionals to
future research directions
and areas of concern
• Historically, health
research has been conducted by outsiders on aboriginal communities, rather
than in a partnership.
Engaging aboriginal communities to identify areas of
concern pertaining to
various issues, including
STIs is important to highlight avenues of improvement.
• Convention on the
Elimination of Violence
Against Women passed a
bill in 1990 that all
Member States take action
against FGM. All but
Sudan and Somalia signed
the bill. Since national
policy and effective and
committed legal instruments are crucial to
eliminating FGM, it is
concerning that these
Member States did not
sign the bill (WHO, 2008).
• Involving stakeholders
at grassroots level and
religious/traditional
leaders in the development
of national policy and
legal proceedings is crucial
and has been an approach
used in The Gambia.
• Countries such as
Ethiopia, Kenya, and
Guinea-Bissau have
developing national
policies for the elimination
of FGM through Ministries of Justice.
• Creation of a national
policy eliminating FGM
and it’s media coverage is
only the first step, and acts
as a way for the government to show the population it’s commitment to
the issue and the repercussions. Media of prosecution cases are a way for
the government to reiterate the consequences of
performing FGM.
• Countries who’ve
developed national
policies for FGM are
varied in their enforcement.
• Often parents are
convicted of committing
FGM on their daughters,
which proves to complicate the family dynamics.
13
The Impact
I entered a relationship with someone who wanted
to get STI testing together, she said she’d feel
more comfortable knowing we were both ‘clean’.
Although I’ve never been tested for any STIs I
assumed I’d be fine, I’d never felt sick or had any
symptoms. When the clinic phoned with my
results I was so shocked, and immediately
embarrassed when they told me I had Chlamydia.
I also felt responsible to tell my partner about the
infection, and she reacted with distrust and
judgment. We broke up immediately, and her
reaction made me so nervous to be stigmatized by
other people that I delayed seeking treatment for
a couple months. Eventually I went to my doctor
and he treated the Chlamydia with relative ease
using antibiotics. I’ve now learned how risky
delayed treatment of STIs can be for my overall
health, these are consequences I don’t feel I was
aware of because mainstream media makes
discussion of STIs so uncomfortable and taboo.
Syphilis leads to
305 000 fetal
and neonatal
deaths annually
More than 1
million people
acquire an STI
every day
Few low-income
countries
administer a
national
immunization
program
More than 340
million new
cases of STIs
occur annually
References
Burg, G. (2012). History of sexually transmitted infections (STI). Giornale Italiano di Dermatologia e Venereologia. 147(4), 329-340.
Law, D. G., Rink, E., Mulvad, G., & Koch, A. (2008). Sexual Health and Sexually Transmitted Infections in the North American Arctic.
Emerging Infectious Diseases. 14(1), 4-9.
UNAIDS. (2013). HIV in Asia and the Pacific. Bangkok, Thailand.
UNHCR. (2013). Too Much Pain: Female Mutilation & Asylum in the European Union. Geneva, Switzerland.
UNICEF & UNFPA. (2012). Joint Programme on Female Genital Mutilation/Cutting: Acelerating Change. New York, USA.
UNICEF. (2011). Clinical Guideline for the Elimination of Mother to Child Transmission of HIV and Congenital Syphilis in Latin America and the
Caribbean. Montevideo, Uruguay.
UNICEF. (2013). Female Genital Mutilation/Cutting: A statistical overview and exploration of the dynamics of change. New York, USA.
United Nations. (1999). General Assembly resolution 53/117, Traditional or customary practices affecting the health of women and girls,
A/RES53/117 (1 February 1999), available from undocs.org/A/RES/53/117
United Nations. (2002). General Assembly resolution 56/128, Traditional or customary practices affecting the health of women and girls,
A/RES/56/128 (30 January 2002), available from undocs.org/A/RES/56/128
United Nations. (2012). General Assembly , Intensifying global efforts for the elimination of female genital mutilations, A/C.3/67/L.21/Rev1 (16
November 2012), available from http://www.un.org/ga/search/view_doc.asp?symbol=A/C.3/67/L.21/Rev.1
US Department of Health and Human Services. (n.d.). A timeline of AIDS. Retrieved October 14, 2014, from
http://www.aids.gov/hiv-aids-basics/hiv-aids-101/aids-timeline/
WHO. (2007). Global strategy for the prevention and control of sexually transmitted infections: 2006-2015. Geneva, Switzerland.
WHO. (2008). Eliminating Female genital mutilation. Geneva, Switzerland.
WHO. (2011). An update on WHO’s work on female genital mutilation (FGM). Geneva, Switzerland.
WHO. (2013). Regional Assessment of HIV, STI and other Health Needs of Transgender People in Asia and the Pacific. Geneva, Switzerland.
WHO. (2013). Sexually transmitted infections. Retrieved October 14, 2014, from
http://www.who.int/mediacentre/factsheets/fs110/en/
WHO. (2013). Sexually transmitted infections (STIs). Retrieved October 14, from
http://apps.who.int/iris/bitstream/10665/82207/1/WHO_RHR_13.02_eng.pdf
WHO. (2014). Female genital mutilation. Retrieved October 14, from
http://www.who.int/mediacentre/factsheets/fs241/en/
WHO. (2014). Sexual and Reproductive Heath. Retrieved October 14, 2014, from
http://www.who.int/reproductivehealth/topics/fgm/health_consequences_fgm/en/
15
Section II:
Family Planning
2.1 Defining
Contraception
Family planning care, services and information dissemination as a component of reproductive and sexual
health care is recognized as a fundamental human right by the World Health Organization (WHO, 2013).
Family planning services and availability of reproductive and sexual health information are key to
improving and attaining adequate health standards for women and their children (WHO, 2013). Family
planning involves controlling or spacing pregnancies through methods of contraception, abortion and
infertility treatments. This section will focus on global family planning initiatives involving contraception
and abortion. Contraception is a term that represents a number of different methods all with the same
purpose; to prevent pregnancy. Some methods are administered prior to sexual intercourse, such as male
and female condom use, or birth control medication, while others known as emergency contraception
(WHO, 2012), such as the morning after pill, are taken post-coital.
Contraception is a component of family planning, that prevents unintended pregnancies through a variety
of methods. Contraceptive use has shown to decrease the number of unintended pregnancies globally, in
turn, reducing maternal and infant morbidity and mortality (WHO, 2014). Adequate access to
contraceptive methods additionally allows individuals to take control of their own reproductive rights and
sexuality, in turn, improving and meeting the needs of their sexual health.
Contraceptive methods can be administered pre or post-coital. Pre-coital contraceptive methods include
condom use, birth control pills, patches or internal rings and intrauterine devices. Post coital contraception
methods, intended for failed contraceptive use, lack of pre-coital contraceptive use or rape and coerced
intercourse, involve emergency contraception, which include emergency contraception pills also known as
the morning after pill, and copper bearing intrauterine devices (WHO, 2012).
How does access to contraception correlate with STIs and unplanned pregnancies?
What are the repercussions of social stigma against contraception?
How do NGOs influence access and perception of contraception?
Does government policy regarding contraception translate effectively at the
community level?
How does contraception use vary between sexual relationships?
How does formal and informal sexual education affect contraceptive use?
17
Policy Timeline
Antiquity
16th-17th
Century
19th
Century
1900s
1960s
2004
2012
• The ancient Egyptians used natural ingredients as means of
contraception, including acacia, honey and dates molded into a block
and inserted into the vagina (Quarini, 2005).
• The oldest known condoms are dated back to this era. Discovered in
Birmingham, England, these condoms were constructed of animal
intestines and were primarily used to prevent transmission of STIs
• Various products made of animal parts and vulcanized rubber was
used to produce condoms and prevent conception. Along with the
production of condoms, cervical caps, intrauterine devices and
douching syringes were produced with the goal of preventing
conception (Quarini, 2005).
• Contraception and family planning initiatives were criminalized in the
United States. Global use of contraception was recorded to be 54%
(WHO, 2013).
• FDA approval of the contraceptive pill is granted, however only for use
of menstruation disorders and not for means of pregnancy prevention.
• WHO released guideline recommendations for global contraceptive
use. These guidelines address the unmet need for family planning
worldwide and set standards for those who can practice contraceptive
methods on individuals (WHO, 2004).
• Global use of contraception has risen to 57%, but continues to remain
low in sub-Saharan Africa at 24% (from 23% in 2008), unchanged in
Asia at 62% and increased slightly in Latin America to 67% (from 64% in
2008) (WHO, 2013).
18
Current Topic Status
Continent
Social &
Cultural Issues
• There is an unmet need
of family planning and
contraception availability in
these regions impacting
economic development,
education for young
women, an increase in
unsafe abortions,
prevalence of STIs and
HIV/AIDS and higher
infant and maternal
mortality and morbidity
(WHO, 2010).
• Women with higher
income are more likely to
use long term
contraception compared to
those in the lower income
range, due to affordability,
accessibility, and availability
(WHO, 2011).
• Lack of contraceptive
use among individuals
living in Africa include
concerns of health and
side effects with
contraception as well as
the belief that they are not
at risk for getting pregnant
(WHO, 2012).
• Young adolescent
women have a more
difficult time accessing
contraception and
contraceptive information
compared to those women
of older age and who are
married, largely due to the
stigma associated with
pre-marital sexual
relationships (Guttmacher,
2012).
Health Issues
Political Issues
• 30% of all pregnancies
and births are unintended,
due to inadequate family
planning initiatives (WHO,
2010). This leads to severe
physical and mental health
issues, particularly if the
women is of adolescent
age.
• Health issues can
include risk of high blood
pressure, complications
during pregnancies, unsafe
abortion, obstructed labor,
excessive bleeding and
death.
• With an unmet need for
contraception, the number
of unintended
pregnancies rises, leading
to high rates of abortions,
maternal and infant
mortality as well as
disability or complications
during and after the
birthing process
(Guttmacher, 2012)
• Family planning services
including the delivery and
distribution of
contraceptives have been
successful in some areas –
when a grassroots
program is collaboratively
implemented (WHO, 2010
– family planning)
• In some regions, like
Zimbabwe and Central
African Republic, although
adolescents under the age
of 18 years may be legally
permitted to consent and
engage in sexual
intercourse, but they are
not legally allowed to seek
contraception and STI
Services (IPPF, 2007).
19
• Research has indicated
that many North Americans
may not be using their
method of contraception
correctly or consistently –
increasing their risk of
unintended pregnancy or
contraction of STIs (CFSH,
2007).
• Reasons explaining why
some North Americans
refrain from purchasing and
using condoms as they
perceive them as
embarrassing to purchase or
were too expensive, belief
that intercourse is less
enjoyable with condom use
(CFSH, 2007).
• Many adolescents also
believe that if they are in a
monogamous sexually active
relationship that they are
not at risk for contracting
an STI, thus may refrain
from using condom as a
form of contraception
(CFSH, 2007).
• Cost barriers exist for
economically disadvantaged
women trying to access
emergency contraception
(CFSH, 2007).
• Adolescents who do not
have access to or do not use
contraception on their first
sexual encounter are twice
as likely to become pregnant in their adolescent
years than those who do
practice contraceptive
methods (Guttmacher,
2014)
• Many women report
relying solely on oral
contraceptive methods
during their sexual encounters – potentially putting
them at risk for contracting
an STI or unintended
pregnancy, through lack of
condom use (CFSH, 2007)
• US supreme court
extended rights to privacy
of a minor’s desire to
obtain contraception,
improving access to
contraception and increasing the chances of them
practicing safe sex (Guttmacher, 2005)
• Some religious based
organizations have influenced government in the
United States to fund only
particular forms of sexual
education for adolescents
in the public school
system- hindering effective
dissemination of contraceptive information and
services (IPPF, 2012)
• Sexual activity before
marriage is stigmatized in
many regions, hindering the
effectiveness of
contraception use
(Guttmacher, 2009).
• Lack of education, living
in rural settings, and
number of children have
been identified as
contributing factors to poor
use of contraception
(Guttmacher, 2009).
• In some regions, such as
Saudi Arabia, women are
required to seek consent of
their spouse in order to
access and obtain
contraception (IPPf, 2007).
• The termination of
USAID’s vast provision of
contraceptives to regions in
Asia, has presented challenges for individuals,
particular the most
economically disadvantaged, to access contraception in these regions (Guttmacher, 2009).
• In some countries, it is
legally required for women
to obtain spousal consent in
order to undergo certain
forms of contraception,
such as sterilization (IPPF,
2007).
• Individuals who are not
able to practice contraception due to various factors
such as economic status,
education, religion, and
policies are at higher risk
of unintended pregnancy,
contraction of STI,
poverty, hunger, poor
mental health and many
other health issues.
20
The Impact
When I was sixteen, I was forced to drop out
of high school because me and my boyfriend
Jamie became unintentionally pregnant. I
mean, they always talked in school about
using protection, but Jamie and I had been
dating for a year and we stopped worrying
about sexually transmitted infections (STIs) a
while ago, plus Jamie always said condoms
made it less enjoyable and we had our own
methods of pregnancy prevention. After
learning Jamie was not as faithful as I
believed him to be - and one syphilis infection
later, I’d wished I could spread the message
to all adolescents about proper contraceptive
use. Contraception for pregnancy prevention
is critical, especially as a sexually active
adolescent – monogamous relationship or
not.
But, condom use as a form of
contraception is critical in also protecting
your body against STIs. Thankfully my baby
was born healthy, but that is not to say her
and I don’t still struggle day to day financially
to get by. With not even a high school
education, finding a decent paying job to put
a roof over our heads and food on the table,
in this city is a burden.
In 2012 37% of
pregnancy-related
deaths were
women with
unintended
pregnancies
222 million women
have unmet
contraception needs.
Highest areas of need
have the highest
maternal mortality
54 million unintended
pregnancies, 16 million
unsafe abortions, 7 million
miscarriages, 79000 maternal
deaths and 1.1 million infant
deaths could be prevented if
adequate access to
contraceptive information and
methods were provided
44% of unmarried
women lack access
to contraception
compared to 24% of
married women
2.2 Defining
Abortion
Abortion is a measure of contraception that involves termination of a pregnancy. It can occur at different
stages of the pregnancy and through different methods, primarily safe and unsafe abortions.
Safe abortions (WHO, 2012) involve those, which are done by a medical or health professional. This
includes medical or non-surgical abortions, which involve the use of pharmacological drugs to terminate
the pregnancy; typically mifepristone and misoprostol, which administered up to 84 days after conception.
Surgical abortions are another form of safe abortion, which involve a more invasive procedure such as,
vacuum aspiration and dilatation and evacuation, performed within 12-14 weeks of gestation (WHO, 2012
– safe abortion doc).
The World Health Organization (WHO) defines unsafe abortion as the termination of a pregnancy by an
unqualified individual, or an abortion performed in an environment that does not meet the WHO medical
standards or a combination of these two situations (WHO, 2011). Furthermore, lack of pre and post
abortion counseling, induced abortion by unskilled individual, in unhygienic or outside a health care
setting, through violent abdominal massages, insertions of objects into the woman’s uterus and
inappropriate use of medications or hazardous substances all fall under the umbrella of the term unsafe
abortion (WHO 2011).
How does foreign aid policy impact access to abortion in low and middle
income countries?
Does secularity affect domestic policies targeted at abortion?
What social stigma is assigned to abortions and why?
What are the physical and mental repercussions of unsafe abortions?
How do the moral standards of healthcare professionals conflict with government abortion policy?
What options do women have in nations where abortion is illegal?
22
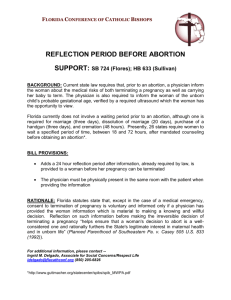
Policy Timeline
1967
1971
1988
1997-2008
2012
• The Abortion Act in the UK is developed. This act states among other
things that doctors are legally permitted to terminate pregnancies and
that doctors are permitted to refuse to perform abortions if he or she
has a conscientious objection to abortion, but he or she is obligated to
provide the necessary medical treatment in times of emergency and
when the woman needs it (IPPF, 2013)
• Medical Termination of Pregnancy Act in India was granted, permitting
women to undergo abortion on the grounds of health (IPPF, 2013)
• Supreme Court recognized that it was women’s rights to decide
whether or not to continue or terminate a pregnancy and that it is
protected by the Canadian Charter of rights and Freedom (CFSH,
2007).
• The legalization of abortion expanded to include 17 new countries;
Benin, Bhutan, Cambodia, Chad, Colombia, Ethiopia, Guinea, Iran,
Mali, Nepal, Niger, Portugal, Saint Lucia, Swaziland, Switzerland,
Thailand and Togo. El Salvador and Nicaragua changed their
restrictive abortion laws to prohibition of abortion entirely. Poland
• The World Health Organization developed policy guidelines for safe
abortion practices globally, granted that 22 million abortions
continued to be administered unsafely annually resulting in the death
of approximately 47, 000 women (WHO, 2012). Recognizing that many
of these abortions could have been prevented, this document was
developed for policy makers and health care professionals to inform
quality sexual education programs, contraception methods and safe,
qualified abortion services.
23
Current Topic Status
Continent
Social &
Cultural Issues
• Religious views are a
major determinant of
whether or not women
undergo abortion in these
regions
• Poor and rural women
tend to rely more on
traditional or untrained
individuals to carryout
their abortions – increasing
their risk of adverse health
effects (Guttmacher, 2012)
• Some women delay
getting post abortion care
services because they are
worried about the stigma
associated with abortion
and that health
professionals may be
hostile towards them
(Guttmacher 2012)
Health Issues
Political Issues
• 460 per 100,000 women
will die from undergoing
unsafe abortions
(Guttmacher, 2012).
• Women undergoing
unsafe abortions, will be at
high risk for medical
complications and often
will not receive the post
abortive care that they
need to address these
health issues (Guttmacher,
2012).
• Health complications
from unsafe abortion
include incomplete
abortion, excessive
bleeding and infection
(Guttmacher 2012)
• A lack of post abortion
services can also have a
large negative impact a
women’s mental
well-being
• In some regions,
abortion is only permitted
in cases where its purpose
is to save the woman’s life
(IPPF, 2012)
• In some regions, such as
Gabon, abortion is
restricted due to the
governments concerns
regarding their countries
falling fertility and
population growth rates
(IPPF, 2012).
24
• Many women fear the
stigma surrounding
abortion in society, and
refrain from accessing
abortion services and
procedures (CFSH, 2007).
• Geographical setting is a
major contributor to
hindering the access to
abortion services (CFSH,
2007).
• Confidentiality has been
recognized as a key barrier
to women accessing
abortion services (CFSH,
2007).
• Parental consent has been
recognized as a barrier for
those young females who
may be attempting to access
abortion services (CFSH,
2007)
• Adolescents that may be
forced into informing their
parents or guardians about
their pregnancy or abortion
(due to the law concerning
parental consent) – may be
placed at risk for physical or
verbal abuse and violence
(Guttmacher, 2005).
• There are some states
where adolescents require
parental consent to obtain
an abortion, - which can
result in adverse health
and mental health
outcomes (Guttmacher,
2005)
• The Canadian government acknowledges
abortion as a form of
medically necessary health
care service and has been
made universal and
publically funded –
barriers however still exist,
for instance, geographical
factors have been found
to affect the accessibility
of these services (CFSH,
2007).
•
Socioeconomic status
is a major determinant of
whether or not women will
undergo safe or unsafe
abortions (Guttmacher,
2012)
• Poor post-abortion
services exists in these
areas, due to lack of
governmental funding for
these services. This can
increase the risk of poor
mental and physical
well-being among the
women undergoing abortion procedures (Guttmacher, 2012).
• Abortion is illegal in
some parts of Asia, such
as the Philippines which
forces many women to
undergo unsafe and
underground abortion
procedures (Guttmacher,
2009)
• In some regions, abortion is only permitted in
cases where its purpose is
to save the woman’s life
(IPPF, 2012)
25
The Impact
Being
Being a
a young
young woman
woman from
from my
my village
village in
in
Angola,
my
family
expects
me
to
get
Angola, my family expects me to get married
married
to
to a
a man
man of
of their
their approval,
approval, bear
bear many
many
children
and
raise
them
to
carry
on
our
children and raise them to carry on our kin.
kin.
Last
Last year,
year, II was
was in
in great
great fear
fear when
when II learned
learned
that
that II was
was carrying
carrying my
my boyfriend’s
boyfriend’s child.
child. II
could
not
have
my
family
find
out
about
could not have my family find out about this
this
but
I
also
did
not
know
where
to
turn
because
but I also did not know where to turn because
abortions
abortions are
are illegal
illegal in
in my
my country.
country. II spoke
spoke
with
with a
a girl
girl in
in my
my village
village that
that told
told me
me about
about a
a
traditional
healer
who
terminates
traditional
healer
who
terminates
pregnancies
pregnancies for
for young
young women
women like
like me.
me. II
turned
turned to
to an
an underground
underground abortion
abortion and
and the
the
health
complications
I
later
endured
were
health complications I later endured were
agonizing.
agonizing. Looking
Looking back
back II realize
realize that
that
restrictive
abortion
laws,
lack
of
qualified
restrictive abortion laws, lack of qualified
health
health professionals,
professionals, and
and the
the fear
fear of
of being
being
ostracized
by
my
community,
pushed
me
ostracized by my community, pushed me into
into
putting
my
body
at
risk
and
undergoing
such
putting my body at risk and undergoing such
a
a traumatic
traumatic experience.
experience
Highly
Highly restrictive
restrictive
abortion
abortion laws
laws are
are
not
associated
not associated
with
with lower
lower
abortion
abortion rates
rates
98%
98% of
of abortions
abortions
occur
occur in
in the
the
developing
developing world,
world,
nearly
half
nearly half
deemed
deemed unsafe
unsafe
In
In 2008
2008 97%
97% of
of
abortions
in
Africa
abortions in Africa
were
were considered
considered
unsafe
unsafe by
by World
World
Health
Organization
Health Organization
Standards
Standards
It
It is
is estimated
estimated that
that
$341
million
goes
$341 million goes
to
to post-abortion
post-abortion
care
care in
in the
the
developing
developing world
world
References
Creanga, A. A., Gillespie, D., Karklins, S., & Tsui, A. O. (2011). Low use contraception among poor women in Africa: an equity issue. Bulletin of
the World Health Organization, 89(4), 258-266.
Canadian Federation for Sexual Health (2007). Sexual Health in Canada. Retrieved October 14, 2014, from:
http://www.cfsh.ca/files/Publications/Resources_to_download/Sex
al_Hea th_in_Canada_Baseline_2007_FINAL.pdf\
Guttmacher Institute (2012). Costs and Benefits of Investing in Contraceptive Services in the Developing World. Retrieved October 14, 2014, from:
http://www.guttmacher.org/pubs/FB-Costs-Benefits Contraceptives.html
Guttmacher Institute (2012). Facts on Induced Abortion Worldwide International Planned Parenthood Federation (2013). Abortion.
Retrieved from: http://www.ippf.org/our-work/what-we-do/abortion/advocacy-abortion
Quarini, C. A. (2005). History of contraception. Women's Health Medicine, 2(5), 28-30.
Singh, S., & Darroch, J. E. (2012). Adding it up: Costs and benefits of contraceptive services. Guttmacher Institute and UNFPA.
TIME Magazine (2010). A Brief History of Birth Control. Retrieved from:
http://content.time.com/time/magazine/article/0,9171,1983970,0.html
World Health Organization. (2004). Medical eligibility criteria forcontraceptive use World Health Organization. Geneva, Switzerland, 176.
World Health Organization. (2004). Selected practice recommendations for contraceptive use.
World Health Organization. (2008). Repositioning family planning: guidelines for advocacy action. Washington DC: WHO, USAID.
World Health Organization. (2011). Unsafe abortion: global and regional estimates of incidence of unsafe abortion and associated mortality in 2008.
Geneva, Switzerland.
World Health Organization, (2012). Emergency Contraception Fact Sheet #244. Retrieved October 14, 2014, from:
http://www.who.int/mediacentre/factsheets/fs244/en/
World Health Organization. (2012). Safe abortion: technical and policy guidance for health systems.
World Health Organization, (2013). Family Planning Fact Sheet #351. Retrieved October 14, 2014, from:
http://www.who.int/mediacentre/factsheets/fs351/en/
World Health Organization. (2014). Ensuring human rights in the provision of contraceptive information and services: guidance and recommendations.
27
Section III:
Maternal Care
3.1 Defining
Prenatal Care
Maternal Health is defined broadly within the World Health Organization (WHO) as “the health of women
during pregnancy, childbirth, and the postpartum period,” (WHO, 2014). Pregnancy is recognized by the
World Health Organization (WHO, 2014) as the key development period in ensuring maternal, newborn,
and infant health. Focusing on evidence-based healthcare and the necessity of ensuring the skilled
healthcare workers are able to attend to the expectant or post-partum mother (WHO, 2014), the World
Health Organization is dedicated to providing access to a number of key areas of need; including
generalized antenatal care, as well as more specialized areas of pregnancy crisis events, including
hypertension, anemia, perennial trauma, post-partum trauma, and controlling the mother-child
transmission of STIs (WHO, 2014).
Pregnancy is defined by the World Health Organization as “the nine months or so for which a woman
carries a developing embryo and fetus in her womb” (WHO, 2014). While this period may have biological
inconsistencies between individuals, the healthcare required by both the mother and fetus remain
consistent enough between cases for the World Health Organization to have developed cross-sectional
global policy on areas such as general antenatal care (WHO, 2014), pregnancy medical crises (WHO, 2014),
prenatal fetus diagnoses (WHO, 2014), and pregnancy complications (WHO, 2014). Healthcare during this
period is intrinsic to not only the quality of life for mother and fetus, but also for their survival (WHO,
2006). Approximately 16 million adolescent girls, and 192 million women worldwide (Guttmacher Institute,
2011) become pregnant each year; and of these girls and women, approximately 800 women die each day
from preventable pregnancy-related health issues (Guttmacher Institute, 2011). This rate of maternal and
fetus mortality is not consistent globally; and the areas of higher rates are often influenced by unequal
access to healthcare resources and inconsistent maternal health education (WHO, 2014).
What is “pregnancy” in international policy?
What are the primary health considerations of for pregnant women?
How do socio-cultural perceptions of pregnancy affect maternal health?
What complexities do pregnant women in rural communities face during the
pre-natal period?
How does nutritional recommendations for pregnant women vary by
geography?
What are the physical and psycho-social health outcomes of miscarriages?
What role does the health system play in preventing preterm birth?
29
Policy Timeline
1990
2000
2010
Member Nations
• Formed the Maternal Mortality Estimation Inter-Agency Group
(MMEIG) in a collaboration between WHO, United Nations Children’s
Fund, United Nations Population Fund, the UN Population Division
and The World Bank
• Called for increased research on the causes and forms of maternal
mortality
• Recognized the pressing need to develop policy specific to
adolescent mothers
• Created a global system of collecting maternal birth and death data
from civil registration, surveys, surveillance systems, censuses, sample
registration systems, and others
Member Nations
• Adopted “Maternal Health” as the fifth of eight Millennium
Development Goals (MDGs), with the aim of reducing maternal
mortality ratio by three quarters by 2015 and achieving universal
access to reproductive health by 2015
• Accepted the UN Secretary-General’s launching of a Global Strategy
for women’s and children’s health
• Called for a mobilization by governments, civil society organizations,
and development partners to increase progress
• Launched the Global Plan towards the Elimination of New HIV
Infections Among Children by 2015 and Keeping their Mothers Alive
with the goal of strengthening civil partnerships with states to reduce
deaths of HIV-positive women by half
Member Nations
• Launched Global Strategy for Women’s and Children’s Health created
by Secretary-General Ban Ki-moon, as a means to strengthen
nation-led healthcare policy development
• Called for increased partner-centric training for healthcare personnel
and promoting accountability for health-care resources in order to
meet the MDGs by 2015
• Pledged to reduce maternal mortality by 75-80% by 2035 through
reducing abortion-related deaths, as well as adolescent pregnancy
• Created Essential Interventions, Commodities and Guidelines for
Reproductive, Maternal, Newborn and Child Health the first-ever
global consensus on the needs of mothers and newborns.
30
Current Topic Status
Continent
Social &
Cultural Issues
• Recent shifts in South
America, including
economic (increased
industrialization and
urbanization), cultural
(shift from the
nuclear-family structure),
and gender (increasing
presence of women in the
workforce), mean that
increased family-planning
campaigns and policies are
becoming accessible.
• The majority of teenage
mothers in the region
struggle to combine
parenting with earning an
income, and most still live
in their parent’s household.
• There is increased
reports of single parents,
and extended family
members taking on
childrearing responsibilities
in these situations.
Patriarchal households
remain the norm.
• Despite high rates of
fertility and unintended
pregnancy amongst South
American indigenous
populations, research
amongst this population
focusing on access to
reproductive health care is
limited.
Health Issues
Political Issues
• South America’s average
Low Birth Rate rate is
9.6% . The total number
of Low Birth Rate infants
in South America is nearly
double that in all of
North America.
• Neonatal mortality
varied from 5 per 1,000 in
Chile to 23 per 1,000 in
Bolivia in 2010.
• 72 maternal deaths
occurred per 100,000 live
births in 2010 in Latin
America.
• In South America, the
risk of maternal death is 1
in 520, compared to 1 in
3800 in the Global North.
• Being a person of
Indigenous descent in
South America is a
significant risk factor for
unwanted pregnancy and
unsafe abortion.
• 8% of women receive
late or no prenatal care in
South America.
• In Latin America,
untreated preeclampsia is
the main cause of prenatal
death for expectant
women
• Recent deterioration of
the labour market, as well
as an increase in unequal
income distribution, mean
that many families
struggle to meet
healthcare costs.
• Massive political change
in the past three decades
in this area, particularly
the shift from
dictatorships to
democracy in the 1980’s,
has led to increased debate
on social policy addressing
marginalized groups
(women, children, etc.)
Neoliberal policies
introduced in the 90’s have
further cut funding to
these areas.
• Cross-continent, there
are higher rates of
cohabitation and divorce,
combined with a higher
average education level for
women, which is affecting
the decreasing fertility
rates.
• Access to reproductive
resources and healthcare is
slowly increasing, however
strong oppositional forces
(including conservative
governments and the
Catholic Church) have
strongly opposed these
reforms, making transition
slow.
31
• Cross-cultural binary
gender roles have led to
decreased education on
reproductive health issues,
as well as economic
priorities outside of
maternal care.
• Due to religious
restrictions, many women in
the region will only see a
female healthcare provider;
and lack of trained female
medical aides mean that
clinics are often
short-staffed, leading to
under-served prenatal
women.
• Cultural stigmatization
leads to increased pressure
for women to become
mothers, leading to earlier
marriages and birth .
• Women in refugee camps
or in areas of conflict often
have little or no access to
medical supplies; and
transport to medical centers
for birth or pregnancy
complications can lead to
long-term injuries.
.
• In developing countries
in the region, complications
during pregnancy and
childbirth are the leading
cause of death and disability among women.
• About half of the 10
million women who give
birth every year in the
Middle East and North
Africa experience some
kind of complication, with
more than 1 million of
them suffering from serious
injuries that often lead to
long-term illness
• More than half of all
maternal deaths in the
region occur within 24
hours of delivery, mostly
due to postpartum hemorrhage.
• Less than 70% of pregnant women have at least
one antenatal check-up, and
even fewer women receive
multiple checkups.
• Lack of access to sanitary
water for bathing and
unsanitary medical practices
during delivery in rural
regions can lead to women
in this region suffering
from reproductive tract
infections, which complicate the birth process
further and can lead to
life-threatening complications.
• In North Africa and the
Middle East, around 30%
of adolescent girls are, on
average, married by the
age of 18. Over half of
these girls will have their
first child by age 18.
• Three out of five
maternal deaths in the
region occur in four
countries: Egypt, Iraq,
Morocco, and Yemen.
Only Kuwait and the
United Arab Emirates
have maternal mortality
ratios that meet World
Health Organization
standards.
• Very high wealth disparities between the rich and
the poor, as well as wealth
differences between family
living in rural areas, mean
that monitoring and
quality of prenatal healthcare varies substantially.
• The majority of women
in the region (from 25% in
Yemen to a high of 74%
in Iran) practice family
planning, instead of other
types of contraception, as
their main method of
preventing unwanted
pregnancies
32
The Impact
I spent my entire pregnancy in my home, several
miles outside of Todos Santos Cuchumatan, in the
Cuchumatanes mountains. As an indigenous
woman, all of the women of my village who have
children, including my mother, stay in this area for
their entire pregnancy. My cousin, who lives in the
city, says that she went to her local NGO for health
checks before the birth, including disease tests and
nutrition services. Because my village is a day’s horse
ride away from the closest town, on a very bumpy
mountainous road, I cannot get to a clinic for these
tests, or go back down for test results. I need to stay
in our village and look after my children while my
husband is away working in San Martin Cuchumatán.
My mother, before she passed away, used to be a
very good traditional midwife, but she did not train a
replacement and we have little access to new
medical supplies. While I wait for my homebirth, it is
my hope that my child will not be stillborn, as some
of my previous children have been. I am exhausted
by pregnancy, and I want to discuss sterilization with
my husband after this birth. I do not think he will
agree to it.
96.5% of the
world’s low birth
weight infants are
born in less
developed
countries
Women in
developing
countries are
seven times more
likely to develop
Every year, 529,000
women die from
pregnancy and
childbirth
complications, 99% of
these deaths in
developing countries
Only one third of
pregnant women in
low-income countries
obtain adequate
prenatal care
2.2 Defining
Postnatal Care
The post-natal, or post-partum, period is a culturally-dependent concept. Globally, it can be defined as
between up to 6 weeks following the birth or up to one year following the birth (Postpartum/Postnatal
Services Review Working Group, 2002). From a medical perspective, the World Health Organization
(WHO) generally defines it as “the days and weeks following childbirth”, with the highest-risk periods
being first defined as the first 24 hours following the birth, and then the first three weeks following the
birth (WHO, 2010; WHO, 2013).
From a cultural perspective, the postnatal period is generally around 40 days, and surrounded by specific
cultural customs for both the mother and infant (Eberhard-Gran, Nordhagen, Heiberg, Eskild, Bergsjo,
2003). This period is also the time where the highest risk of maternal and infant mortality occurs: of the 2.9
million newborn deaths that occurred globally in 2012, close to half of them occurred within the first 24
hours after birth (WHO, 2014). Risk factors such as asphyxiation of the infant or premature births, and
hemorrhaging, fistulas, and prolapsed uteruses of the mothers are at high risk in this period (WHO, 2014).
In rural and developing areas, under-prepared health professionals and clinics, a lack of hygiene, and some
traditional cultural practices can turn even a low-risk childbirth into a life-threatening process (WHO,
2014). This critical phase is often the most-neglected period for the provision of quality care and relevant
policy, with the WHO stating that “the postpartum and postnatal period [consistently] receives less
attention from health care providers than pregnancy and childbirth” (WHO, 2013).
How does the medical capacity of birthing settings vary, and how does this
affect complications during birth?
How do cultural expectations affect breastfeeding practices?
How does the value attributed to maternal health by government policy influence care standards and cultural perceptions of pregnancy?
How does the treatment of post-partum depression vary culturally?
How does access to proper treatment vary within marginalized groups of
women?
34
Policy Timeline
1998
2004
2008
Member Nations
• Published the Postpartum Care of the Mother and Newborn: A
Practical Guide, which began to call for recognition of postpartum
depression, as well as the value of breastfeeding
• Called for culturally-sensitive immediate post-partum services globally,
particularly in rural areas and encouraging referral services
• Recognized that harmful traditional practices determined by gender of
the newborn and cultural taboos around the mother’s activity following
birth, require a change of practice
Member Nations
• Pregnancy, Childbirth, Postpartum and Newborn Care: A Guide for
Essential Practice was updated in 2004 to include practices based
around evidence-based policies (WHO, 2013)
• Called for increased practice of contagious disease screenings,
including malaria, tuberculosis, HIV, and lung diseases, for both the
mother and newborn
• Recognized an increased need for trained infant feeding counseling
for mothers
• Recommended increased attention paid to confidentiality and privacy
for the patient’s treatment
Member Nations
• Called for a technical consultation on the issue of post-natal care,
which led to the furthering of the “Maternal Health” United Nations
Millennium Development Goal (MDGs)
• Recognized that the postpartum and postnatal period receive less
focus from health care providers than birth and pregnancy
• Recommended a reworking of the early 20th century models of
post-partum care, in that these services should now provide emotional,
social, and cultural support following the birth as well
35
Current Topic Status
Continent
Social &
Cultural Issues
• Despite a high national
GDP, American women
face extreme shortages in
health care providers, high
cost of health care,
bureaucratic and financial
barriers, and lack of
autonomy in the birthing
process.
• Over the last 50 years,
African American women
in the United States have
been four times as likely to
die in the post-natal period
as white women, due to
differences in experiencing
prenatal-crisis
complications, as well as
being more likely to be in
communities with
under-funded health
facilities.
• Every six hours in
Mexico, a woman dies in
labour or due to a
pregnancy-related
complication, often due to
poverty-induced factors.
• In Mexico, a lack of
social support, low
education levels,
unplanned pregnancy, and
giving birth to a girl-child
have been cited as some
causes for the current 14%
rate of postpartum
depression.
Health Issues
Political Issues
• Over 56 studies in
North America over the
past 20 years, it has been
determined that the rate
of postpartum depression
sits at 13%, on average.
• In the United States,
according to the Centers
for Disease Control and
Prevention, almost one in
three women deliver via a
cesarean section.
• In 2010, the United
States was ranked as 50th
in the world for rates of
maternal mortality,
ranking with higher ratios
than many European,
Asian, and Middle Eastern
nations.
• Low-income women are
less likely to have
insurance prior to
pregnancy, and more likely
to suffer chronic health
conditions due to
pregnancy. Getting health
coverage is made more
difficult by bureaucratic
barriers and delays, and
the inability to find
insurance providers who
will accept them.
• American law does not
protect physicians who
refuse to perform
medically-unnecessary
cesarean sections on
patients, particularly if
there is complications in
the birth.
• In both Canada and the
United States, incarcerated
women and adolescents
who are expecting face a
policy gap with regards to
treatment. In the United
States, thirty-eight states
have no or inadequate
policies on prenatal care
for incarcerated women,
and forty-one states do
not require prenatal
nutrition counseling.
• In the United States, the
“International Cesarean
Awareness Network”
stresses that the choice of
an elective caesarian
section is “never
autonomous”, and that
women are
under-informed on the
risks of c-sections.
• In Canada, post-partum
depression is still a
relatively new diagnosis;
and existing infrastructure
is not equipped to handle
those expectant women
who experience
depression during
pregnancy, as well as in the
post-partum period.
36
• In China and South-East
Asia, open discussion about
sexuality and the birth
process are often considered
a taboo.
• A doctor of the same sex
is preferred by most Asian
patients, particularly
women.
• In Nepal, a combination
of social status, ethnicity,
and poverty lead to
increased belief in
traditional postnatal care,
and women are more likely
to seek out traditional
healers over Western
physicians.
• Cultural practices around
birth in some rural areas of
the continent, including
maternal seculusion and
community involvement,
lead to decreased utilization
of Western medical
practices.
• In rural Asia, particularly
the central Republics and
South Asia, the proportion
of women who had
received postnatal care after
delivery was around 34%,
and only 19% of women
received care within 48
hours of giving birth.
• The most common
health in the postnatal
period were weakness
(27%), mastitis (27%),
vaginal bleeding (20%),
fever (13%), vaginal pain
(13%) and a prolapsed
uterus (7%).
• Statistical evidence from
South Asian communities
of poverty suggest that
home-visits by community
health workers in the few
days following the birth, as
well as pre-birth education
and nutritional resources,
provided positive results in
reducing maternal and
infant mortality.
• In South-East Asia,
booking follow-up appointments following the birth is
the responsibility of the
mother, and some clinics
may refuse to see the
mother before the
two-week check-up point.
• The Philippines have not
managed to meet the UN’s
Millennium Development
• In rural areas of Asia,
around 50% of the
women are typically
illiterate, with the remainder having some level of
primary or secondary
education, and most
having some level of work
experience in farming.
• In Japan, delivery and
hospitalization are not
covered by National
Health Insurance, unless
there are complications.
Some parents can receive
government subsidies, but
need to inquire with their
local political office prior
to the birth to qualify.
• The prevalence of
postpartum depression
peaks in Pakistan, where
the recorded rate is
currently 63.3%. Risk
factors in Asia for postpartum depression include
unwanted pregnancy,
poverty, and infant gender
preference. Traditional
post-partum practices
were not shown as providing positive psychological
benefits for the women.
37
The Impact
I had my first child at the age of 14 in the Gaspard
Kamara Health Centre. My doctors, who were trained by
World Health Organization, made a point to incorporate
my cultural beliefs into my medical care after the birth.
My child was premature and very tiny, so they used the
“kangaroo” position, where she was secured to my chest
using a blanket, to keep her warm and so that I could tell
the nurses if she became feverish. I am lucky that my
husband got me to the Health Centre in time; my
cousins, who live in the rural area outside of Sangalkam,
often have to travel many kilometers in order to reach a
clinic, while in labour. If I had to do the same, my
premature daughter might not have survived the journey.
I am also lucky that my doctors had a conversation with
me about family planning and depression, following the
birth. They say that when I come back to get my
daughter immunized, I can also receive some
contraceptive tools and talk to them about how I am
feeling. My daughter’s birth was well-supported, and as a
woman in urban Dakar, I was one of the few women who
had the opportunity to receive that level of care.
In South Asia, 2.6
million infants die
each year during
the neonatal
period, or the
month of life
Only 13% of South
American women
receive a postnatal
visit within two
days of birth
96.5% of the
world’s LBW
infants are born in
less developed
countries
Over 60% of
maternal deaths
occur in the first
48 hours after
childbirth
References
Angelle, A. (2010). Modern Medicine: Unncessary C-Sections on the Rise. Retrieved October 14, 2014, from
http://www.livescience.com/11218-modern-medicine-unnecessary-sections-rise.html
Angloinfo. (2014). Post-natal Care in India. Retrieved October 14, 2014, from http://india.angloinfo.com/healthcare/pregnan
cy-birth/postnatal-care/
Angloinfo. (2014). Post-natal Care in Japan. Retrieved October 14, 2014, from http://japan.angloinfo.com/healthcare/pregnan
cy-birth/post-natal-care/
Coeytaux, F., Bingham, D., & Strauss, N. (2011). Maternal Mortality in the United States: A Human Rights Failure. 83(3), 189-193.
Child Trends Databank. (2014). Late or no prenatal care. Retrieved October 14, 2014, from http://www.childtrends.org/?indica
tors=late-or-no-prenatal-care
Dhakal, S., Chapman, G.N., Simkhada, P., van Teijlingen, E.R., Stephens, J., & Raja, A.E. (2007). Utilisation of postnatal care among rural
women in Nepal. BioMed Central Pregnancy and Childbirth. 7(19), 1-9.
Eberhard-Gran, M., Nordhagen, R., Heiberg, E., Bergsjo, P., & Eskild, A. (2003). Postnatal care in cross-cultural and historical perspec
tive. Journal of the Norwegian Medical Association. 123(24), 3553-3556.
Jelin, E & Diaz-Munoz, A. (2003). Major trends affecting families: South America in perspective.
Jewell, T. R. (2009). Prenatal care and birthweight production: evidence from South America. Applied Economics. 39(4), 415-426.
Klainin, P & Arthur D.G. (2009). Postpartum depression in Asian cultures: a literature review. International Journal of Nursing Studies.
46(10), 1355-1373.
Mann, S., Colbourn, T., Barros, H., Lopes, S., & Duysburgh, E. (2012). Post-partum mother and child-care: a comparison of four African
countries. The Lancet. 380, S17.
Newman, Lucia. (1996). Poor acces to health care endangers pregnant Mexican women. CNN World News. Retrieved October 14,
2014, from http://edition.cnn.com/WORLD/9607/25/mexico.healthcare/
Nova Scotia Department of Health. (2002). Healthy Babies, Health Families: Postpartum & Postnatal Guidelines.
Population Council. (2008). Strengthening Postnatal Care Services Including Postpartum Family Planning in Kenya.
Preelampisa Foundation. (2014). Preeclampsia and Maternal Mortality: a Global Burden. Retrieved October 14, 2014, from,
http://www.preeclampsia.org/component/content/article/149-ad
vocacy-awareness/332-preeclampsia-and-maternal-mortality-a-global-burden
Public Health Agency of Canada. (2012). Depression in Pregnancy. Retrieved October 14, 2014, from http://www.phac-aspc.gc.
ca/mh-sm/preg_dep-eng.php
Queensland Government. (n.d.). Chinese Ethnicity and Background. Retrieved October 14, 2014, from http://www.health.qld.gov
.au/multicultural/health_workers/Chinese-preg-prof.pdf
Robertson, E., Celasun, N., & Stewart D.E. (2003). Maternal Mental Health & Child Health and Development: Literature review of risk
factors and interventions.
Sims-Place, J.M., Billings, D.L., & de Castro, F. (2014). Postnatal Depression: What should we know about? Retrieved October 14, 2014,
from http://www.mhtf.org/category/discover/topics/postnatal-care/
39
References
WHO. (2014). Saving Mother’s Lives. Retrieved on October 14, 2014, from http://www.who.int/reproductivehealth/publications/moni
toring/infographic/en/
Woodhouse, C., Camelo, J. L., & Wehby, G.L. (2014). A Comparative Analysis of Prenatal Care and Fetal Growth in Eight South American
Countries. PLoS ONE. 9(3): 10.1371/journal.pone.0091292
Wurtz, H. (2012). Indigenous Women of Latin America: Unintended Pregnancy, Unsafe Abortion, and Reproductive Health Outcomes.
Pimatisiwin. 10(3): 271-282.
Yamashita, Tadashi., Suplido, S.A., Ladines-Llave, C., Tanaka, Y., Senba, N., & Matsuo, H. (2014). A Cross-Sectional Analytic Study of
Postpartum Health Care Service Utilization in the Philippines. PLoS ONE. 9(1): doi:10.1371/journal.pone.0085627.
41
References
Stevens, E.E., Patrick, T.E., & Pickler, R. (2009). A History of Infant Feeding. Journal of Perinatal Education. 18(2), 32-39.
The American College of Obstetricians and Gynecologists. (2011). ACOG Committee Opinion No. 511: Health care for pregnant and
postpartum incarcerated women and adolescent females. 118(5), 1198-19202.
The Obstetrics and Gynecology Risk Research Group., Kukla, R., Kuppermann, M., Little, M., Lyerly, A.D., Mitchell, L.M., Armstrong,
E.M., & Harris, L. (2009). Finding Autonomy in Birth. Bioethics. 23(1), 1-8.
UN Chronicle. (2007). Newborns in Sub-Saharan Africa: How to Save These Fragile Lives. Retrieved October 14, 2014, from
http://unchronicle.un.org/article/newborns-sub-saharan-africa-how-save-these-fragile-lives/
UNICEF. (n.d.). Maternal Mortality. Retrieved October 14, 2014, from http://www.unicef.org/specialsession/about/sgreportpdf/09_MaternalMortality_D7341Insert_English.pdf
UNICEF. (2004). Surviving Childbirth and Pregnancy in South Asia. Kathmandu, Nepal.
UNICEF. (2007). Teenage motherhood in Latin America and the Caribbean. Chile, Santiago.
UNICEF. (2014). Tackling the hidden issue of adolescent pregnancy in Asia-Pacific. Retrieved from http://unicefeapro.blogspot.
ca/2014/09/tackling-hidden-issue-of-adolescent_19.html
United Nations. (2013). The Millennium Development Goals Report: Poverty and hunger reduced Latin America and Caribbean with
advances on Millennium Development Goals. New York, USA.
United Nations. (2014). Millennium Development Goals and Beyond 2015. Retrieved on October 14, 2014, from http://www.un.org/millenniumgoals/
UNFPA. (2012). Trends in maternal mortality: 1999 to 2010. Geneva, Switzerland.
WHO. (n.d.) Opportunities for Africa’s Newborns.
WHO. (2007). Adolescent pregnancy - Unmet needs and undone deeds. Geneva, Switzerland.
WHO. (2010). WHO Technical Consultation on Postpartum and Postnatal Care. Geneva, Switzerland.
WHO. (2013). World Health Statistics 2013. Geneva, Switzerland.
WHO. (2014). Ending disrespect and abuse during facility-based childbirth. Retrieved on October 14, 2014, from http://www.who.int/reproductivehealth/topics/maternal_perinatal/en/
WHO. (2014). Maternal Health. Retrieved on October 14, 2014, from http://www.who.int/topics/maternal_health/en/
WHO. (2014). Maternal, newborn, child and adolescent health: Postnatal care. Retrieved October 14, 2014, from http://www.who.int/maternal_child_adolescent/topics/newborn/postnatal_care/e n/
WHO. (2014). Maternal mortality. Retrieved on October 14, 2014, from
http://www.who.int/mediacentre/factsheets/fs348/en/
WHO. (2014). MDG 5: improve maternal health. Retrieved on October 14, 2014, from http://www.who.int/topics/millennium_development_goals/maternal_health/en/
WHO. (2014). Postnatal care of the mother and newborn. Geneva, Switzerland.
40