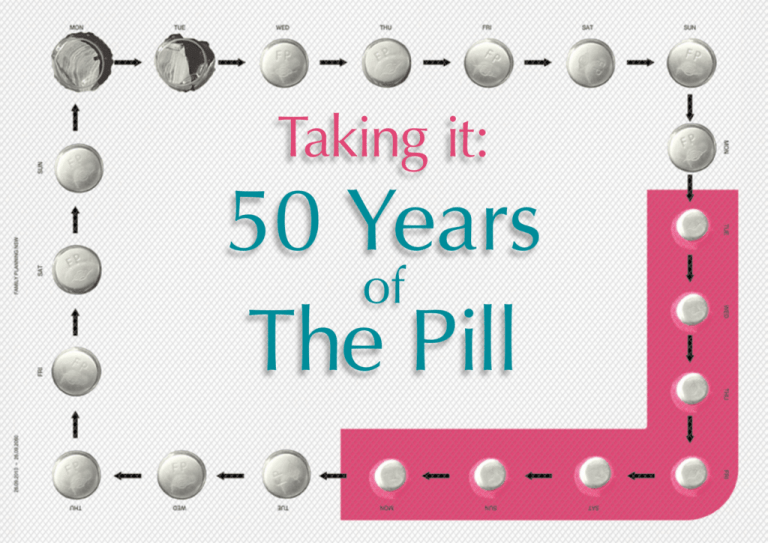
Taking it:
50 Years
of
The Pill
A model of synthetic oestrogen.
Co n te n t s
Introduction
Personal Reactions
The Future
01
29
41
Chris Udy
Nina Funnell
Ann Brassil
Dr Devora Lieberman
32
43
History
Wendy McCarthy AO
Foreword –
Family Planning NSW
07
A potted history
of hormonal contraception
Dr Terri Foran
13
50 years of the Pill – A medical, social and
political commentary
Dr Edith Weisberg OAM
I rarely marry virgins anymore…
The Pill and I — A personal
and political reflection
35
50 years of taking it
Jane Caro
37
There is a long way to go…
Hopes and dreams: six wishes
for the future of contraception
in Australia
Dr Caroline Harvey
47
Fifty years from now
Dr Christine Read
How the Pill changed my
life — Reflections of a
Generation X teenager
Sophie McCarthy
17
Pills, sex and family planning…
Dr Deborah Bateson
19
The Pill is 50 years old…
Professor Gab Kovacs
23
The medicalisation
and democratisation
of contraception Dr Stefania Siedlecky AM
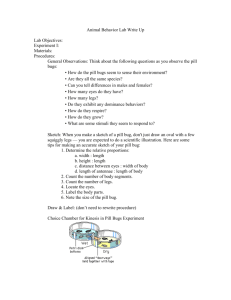
“Taking It: 50 years of The Pill” 2010.
A collection of essays published by Family Planning NSW to celebrate the 50th anniversary of the oral contraceptive pill.
Edited by: Christine Read MBBS ThA FAChSHM Grad Cert PH
Published by: Family Planning NSW, 328-336 Liverpool Rd, Ashfield 2131
F o rew Or d
“Access to contraception has been one of the
defining influences in my own life, particularly
in allowing me to choose the timing and
spacing of my own children and the impacts
this has had on my ability to pursue a
professional career and support my family”
Ann Brassil
Chief Executive Officer
Family Planning NSW
The 50 year commemoration of the launch of
the first oral contraceptive pill in Australia is an
important anniversary in so many ways.
It defines the moment in time from which
women could easily and efficiently manage their
fertility, it signals the point from which human
scientific endeavour created a way for society
to manage population growth effectively with a
culture of invention and enquiry that is ongoing,
it allowed a whole generation of baby boomers
to make choices about their futures with a
certainty their parents never enjoyed and it was
controversial and led to intense examination of
sexuality, women’s rights, society’s accepted
conventions and moral judgements. It became
a political issue and caused changes in health
service provision and the spread of the family
planning movement.
Virtually all of these issues have become intrinsic
to our mainstream culture, yet we still have a
long way to go.
There is a sexual ‘double standard’ in Australia.
There is inequity of reproductive and sexual
healthcare between indigenous and non
indigenous peoples and for a range of
marginalised groups such as the young and
people from some cultural backgrounds.
Some states have taken a sensible ‘health
based’ approach to abortion legislation but it
still remains within the Crimes Act in NSW and
a young woman and her partner are
facing possible imprisonment for procuring an
abortion under Queensland’s antiquated law.
The implementation of comprehensive
reproductive and sexual health education in
schools in Australia remains a challenge.
Access to contraception has been one of the
defining influences in my own life, particularly in
allowing me to choose the timing and spacing
of my own children, and the impacts this has
had on my ability to pursue a professional
career and support my family. This publication,
composed of essays and the personal opinion
of its contributors provides a fascinating window
into history, personal experiences, intellectual
grappling and questions for the future. I hope
you enjoy it and find the articles as compelling
as we have.
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 3
“I feel fortunate to never have lived in a
time or place when I did not have easy
access to reliable, affordable contraception,
and the right to decide what to do about
an unplanned pregnancy should that
contraception fail. I hope that it doesn’t
take another 50 years for all women to
be able to feel the same”
Dr Devora Lieberman
President
Family Planning NSW
When I first started working as a contraception
and abortion counsellor at Planned Parenthood
of New York City in 1984 (my summer job for
three years during Uni), I was given a Zip-Loc
bag full of all of the available contraceptive methods
for demonstration purposes. There was a condom,
a can of spermicidal foam, a diaphragm, yellowed
with age and with a hole in the middle so it
wouldn’t be stolen, a Lippes Loop IUD with a
blue nylon string attached, a Today sponge and,
of course, plastic dial packs of lolly-coloured
pills. The yellow packs contained the 50 mcg
pills, and the peach the 35. The options were
few, the hassles and side effects, many.
Much has changed in the last 25 years! Lippes
Loops disappeared in the mid-eighties when
sales were decimated following the disaster that
was the Dalkon Shield. And who could forget
the Seinfeld episode when Elaine scoured every
pharmacy in New York when they stopped
making sponges? Pills have gone through
myriad formulations – lower doses, multiphases, newer progestins – whose introduction
was always carefully timed with patent expiry.
The first decade of the new millennium has seen
a resurgence of contraceptive technology.
Implanon in 2000, followed quickly by Mirena,
offered women extremely reliable “set and
forget” contraception. NuvaRing® in 2005 gave
the monthly option, with the advantage of being
able to stop it without seeing a doctor.
I feel fortunate to never have lived in a time
or place when I did not have easy access to
reliable, affordable contraception, and the right
to decide what to do about an unplanned
pregnancy should that contraception fail.
I hope that it doesn’t take another 50 years
for all women to be able to feel the same.
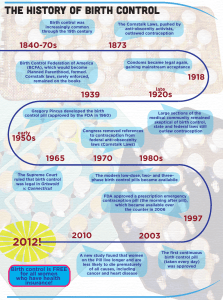
A Timeline for 50 Years of The Pill
1960
• The oral contraceptive pill, Enovid
(Searle) launched in the United
States May 1960.
2002
• Packaged levonorgestrel
emergency contraceptive
pill available in Australia.
2003
1961
• Anovlar
(Schering)
marketed in
Australia – the
second country
in the world to
have the oral
contraceptive pill.
2001
1965
• The US Supreme Court ruled that
married women have a constitutional
right to privacy that allows them to
obtain contraception.
1998
• Contraceptive implant containing
progestogen only –­ etonogestrel
available in Australia and on PBS.
• Lower dose (20mcg)
oestrogen pills become
available in Australia.
• A hormone releasing
progestogen only (levonorgestrel)
intrauterine device available
in Australia and goes on PBS
in 2003.
• “Sex and the Law” – The first
health workers’ guide to sex
and legal matters is published
by Family Planning NSW.
2004
2005
• United States FDA approves a
prepackaged pill regimen with
four placebo breaks per year.
• Emergency contraceptive
pill available over the counter
at pharmacies.
• Australian fertility rate: 1.75 births
per woman.
• The “Baby bonus” is
introduced to raise
Australia’s birth rate.
• It was noted that only 15.9% of
countries, which were identified in
2005 as failing to achieve gender
parity in both primary and secondary
schools, will achieve this Millennium
Development goal by 2015.
1966
• Margaret
Sanger,
birth control
pioneer dies.
1995
• Venous thromboembolism
(bloodclots) media stories in UK
about third generation progestogen
containing – lead women to cease
taking their pills and a marked rise
in the abortion rate.
2006
• Combined hormonal vaginal ring
available in Australia.
• Australian teenage birthrate:
17.3 per 1000 women.
1967
• Prof Rodney Shearman reports to
WHO meeting: Australia has the
highest rate of use of The Pill in
the world.
1994
• International Conference
on Population Development
in Cairo commits to ensure
reproductive health rights for
all, including family planning
and sexual health.
2007
• UN Millennium Development Goal 5(b)
is introduced: to achieve universal
access to reproductive health services
by 2015.
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 5
1968
TIMELINE
• Papal encyclical – Humanae vitae
“On the Regulation of Birth” –
Reaffirmed the positive value of
sex (in marriage), but rejected
contraception for Catholics.
1992
• Pills containing cyproterone acetate
is available, licensed specifically for
treatment of acne and androgenic
symptoms, the first recognition of
non contraceptive benefits with oral
contraceptives.
1969
1970
• Man lands on the Moon.
1971
• “The Female Eunuch” by Germaine
Greer is published.
• L ow dose oestrogen (30 mcg ethinyl
oestradiol) pills are available.
1987
• Australian teenage birthrate:
55.5 per 1000 women average
of 2.95 births per woman.
• 38% Australian women taking
the Pill.
1985
• Medicare introduced to
Australia and card available
to 15 year olds.
• Pills containing
“third generation”
progestogens;
desogestrel
and gestodene
available.
• Biphasic and triphasic pills
available, mimicing the
hormone pattern in the
menstrual cycle and reducing
the overall load of hormone.
1980
• The 20th
anniversary of
the Pill described
as “unhappy”
in the Sunday
Telegraph.
Women are
interviewed about adverse effects,
but still enormously popular.
2008
2009
2010
• Pill with a regimen of 24 active
pills and 4 placebo tablets
launched in Australia.
• The first oestradiol (natural
form of oestrogen) pill available
in Australia.
• J ulia Gillard – First female
Prime Minister of Australia.
• Worldwide 1 in every
10 women has an unmet
need for contraception.
1972
• L uxury tax removed
and Pharmaceutical
Benefits Schedule
(PBS) listing of the
Pill by Whitlam
government.
1973
• Family Planning Association
branches appear in each state
of Australia.
• Legal maturity reduced from
21 to 18 years.
The
Future
• New ways of packaging pills with bleeding breaks to be
potentially under the woman’s control, plus new delivery
methods such as a wafer that dissolves on the tongue.
• More work to be done on reproductive rights worldwide
and removing abortion from criminal codes.
• Family planning services and meeting Millennium
Development Goals in developing countries.
Hormone production before the 1950’s.
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 7
A p otted History of H o rm o n a l Co n trac e pti o n
“In his dystopian 1932 novel Brave New World
Aldous Huxley described a future in which sex was
depersonalised and social order maintained by the use
of the psychoactive medication “soma.” Twenty eight
years later he was asked to write a commentary on
the state of contemporary society through the prism of
his earlier predictions. It was in this subsequent work,
Brave New World revisited, that the term “the Pill” –
with its distinctive capital P-came into existence.”1
Terri Foran
Sexual Health Physician, Lecturer
School of Women’s and Children’s Health,
Medical Faculty, University of New South Wales
Since the dawn of time humans have sought
to control their fertility. Initially women relied
mainly on amulets and superstition but even
in the ancient world contraceptive douches,
pessaries and sponges were used across many
civilisations and religions. Christianity developed
its official position in the 5th century when
St Augustine declared that sex without the
intention to procreate was unconditionally
immoral and illicit, thus effectively prohibiting any
form of contraception. And this influential early
Church philosopher knew quite a bit about sex,
having had several mistresses and one 14-year
common law relationship prior to his conversion
to Christianity. During these libidinous years
Augustine’s self confessed maxim was “Grant
me chastity…but not yet.”
It would appear that the majority of the
mediaeval population identified more closely
with the early, pre-sanctified Augustine when it
came to sex and continued to utilise traditional
contraceptive practices with varying degrees of
success. However, it was the advent of cheap
mass-produced vulcanised rubber condoms
in the mid 1800s which really took effective
contraception to the general population.
Couples took full advantage of this new
opportunity to limit the size of their families.
In the 1800s the average American woman gave
birth seven times, by 1900 that rate had halved,
remaining stable until 1960 at which point it
halved again with the release of the Pill.2
The concept of hormonal contraception also
has a long history. Mexican women traditionally
consumed Barbasco yams as a means of
avoiding unintended pregnancy. This tuber is
rich in plant hormones and was the original
source of the steroids used in modern
contraceptive pills and menopause therapy,
until these could be synthetised more cheaply.
The early women settlers in New Brunswick
in Canada borrowed from a local indigenous
tradition and relied on a monthly brew of dried
beaver’s testicles steeped in alcohol for their
contraceptive needs. There is even an
antipodean connection, though not a human
one, in the discovery by Australian farmers in
the 1940s that ewes grazing on hormone-rich
red clover produced significantly fewer lambs
the following season.
The Contraceptive Pioneers
The late 19th century saw a tension between
the neo-Malthusians, who advocated population
control as a means of managing limited world
resources, and the religious and pro-natalist
groups, who linked a growing population with
traditional family values and economic success.
In much of the world this debate was managed
politely. Continental gynaecologists quietly
developed more effective contraceptive
methods, such as stem pessaries and
individually-fitted diaphragms for their wealthier
patients, while in the United Kingdom the
botanist Marie Stopes founded women’s clinics
and daringly advocated sexual pleasure as a
female right.
Page 8 | Ta k i n g i t – 5 0 y e a r s o f t h e p i l l
The first Australian birth control clinic opened
its doors in Sydney in 1933, under the auspices
of the Racial Hygiene Association of New South
Wales. This organisation advocated “the
selective breeding of future generations for the
elimination of hereditary disease and defects”
and most of the early birth control pioneers had
a similarly eugenic philosophy. The belief that
the people most likely to have the largest
families were those least able to care for them
was widely-held and for this reason most of the
population control efforts were directed towards
the socially disadvantaged. When examined
through 21st century eyes these beliefs smack
heavily of classism and racism and it is
understandable then that the writings of many
of these early pioneers of birth control are now
open to modern criticism. Marie Stopes, for
example, was an ardent admirer of Hitler,
and in 1939 sent him a copy of her own
sentimental love poems complete with a
gushing covering letter.3
It was, perhaps, inevitable that a more hostile
clash occurred in the United States where
positions were even more polarised. One of the
more interesting characters in this struggle was
Margaret Sanger, who is actually credited with
coining the term “birth control”. One of 11
children, Sanger was born in 1879 into the strict
Catholic Higgins family. Her mother, who she
idolised, died at only 50 years of age from
tuberculosis. The young Margaret however
attributed the death to her mother’s eighteen
pregnancies and held her father directly to
blame. “You caused this.” she accused him.
“Mother is dead from having too many children”.
She later worked as a community nurse in the
slums of New York. Distressed by the numbers
of women in her care who died as a result of
numerous pregnancies or from the
complications of backyard abortions, she
later wrote “No woman can call herself free
who does not own and control her own body.
No woman can call herself free until she can
choose consciously whether or not she will be
a mother.”4
Scientific Advances and Hormonal Contraception
As early as 1921 the German physiologist
Haberlandt had demonstrated the possibility
of hormonal contraception when he rendered
rabbits infertile by injecting them with corpus
luteum extract.5 Researchers in the 1930s and
40s, such as Inhoffen, Hohlweg, Russell,
Makepeace and Djerassi, developed the steroid
hormones which were later to become the basic
ingredients of oral contraceptives.
These experiences acted as a personal
catalyst for Sanger and by 1910 she was
going door‑to‑door teaching women about
contraception. In 1916, she established the first
birth control clinic in the United States and by
the 1940s there were 800 similar clinics across
the country. To a woman as passionate as
Sanger however, the diaphragms, condoms and
pessaries available at the time were frustratingly
fallible. As early as 1912 she had begun to refer
to the “magic pill” in her writings – a pill which
would allow couples the ultimate choice in when
and whether they reproduced. It was not until
the 1950s however that advances in steroid
chemistry allowed that vision to become a
reality. Sanger lived just long enough to see the
US Supreme Court rule in 1965 that “the use of
contraception is a constitutional right”. After this
announcement friends propped the terminally ill
86-year-old rebel up in her bed, and it is
recorded that she celebrated the event by
drinking vintage champagne through a straw.
In 1951 Margaret Sanger was by chance
introduced to the brilliant but abrasive
physiologist Gregory Pincus who had
recently set up his own research facility after
a disagreement with his Harvard colleagues.
Pincus and his collaborator, the infertility
specialist John Rock, were experimenting
with hormones that might assist conception.
Sanger realised that this work might finally be
the key to the development of her “magic pill”
and persuaded her wealthy collaborator,
Katharine McCormick to endow the research
facility with enough funds to enable an entirely
new project. Pincus and Rock were charged
with investigating whether hormones could
also be used as an effective way of preventing
pregnancy. Since it was still a felony at that time
to administer contraception in their home state
of Massachusetts, the pair was forced to
conduct their early pill trials in Puerto Rico.
Poster for the Racial Hygiene Association
of NSW 1933.
Margaret Sanger, established the first birth control clinic in the
United States.
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 9
The first contraceptive formulation administered
to the women in the trials contained only
progestogen. Though this preparation effectively
prevented ovulation there was a high rate of
unpredictable vaginal bleeding which severely
limited its acceptability as a contraceptive.
However at some point during the early trials
a batch of pills was inadvertently contaminated
during the manufacturing process by a small
amount of synthetic oestrogen. The women
receiving this batch had significantly less
bleeding than the other women on the trial and
so, through sheer serendipity, the concept of a
combined pill was born. A descendent of this
accidental combination was later to become
“Enovid,” the first contraceptive pill to be
approved for use in the United States.
Pincus and Rock also made a decision to
schedule a regular break from hormone tablets
every four weeks. This was partly from a desire
to provide women with a regular menstrual-like
bleed but also because the devoutly Catholic
Rock believed that this would make their
preparation akin to natural family planning and
therefore acceptable to his Church. He was
later to be proved wrong when the 1968 papal
encyclical “Humanae Vitae” reiterated its
complete objection to oral contraceptives and
all other “artificial” methods of birth control.
Rock however maintained his position until he
died, despite a great deal of personal pressure
and the threat of excommunication. One angry
woman wrote to him not long after the Pill was
approved “You should be afraid to meet your
Maker!” “My dear madam,” Rock wrote back,
“in my faith, we are taught that the Lord is with
us always. When my time comes, there will be
no need for introductions”.
Marketing the Pill in America and Beyond
In late 1957 the pharmaceutical company
Searle received regulatory approval to
market Enovid in the United States for the
treatment of menstrual disorders. Following
a virtual epidemic of this condition, the
product was subsequently given an official
indication for contraception in May 1960.
Australia was only the second country
in the world to approve a combined
preparation for contraceptive use with the
release of the Schering product, Anovlar,
in February 1961.
All these early formulations contained much
higher hormonal doses than those found in
modern contraceptives. They also had a higher
rate of side effects, including the more serious
complications of clots and strokes, and on the
whole both regulatory authorities and the
medical profession took a fairly conservative
position on their use. Initially the Pill was
restricted to married women and even then,
was often prescribed only after the woman had
completed her family. Searle executives were
however supremely optimistic as to the Pill’s
wider potential. An early in-house newsletter
exhorted their sales team to “weed out all the
negative points and convince doctors to get
patients started on Enovid today…”
Few would suggest that the Pill initiated the
sexual revolution but there is no doubt it fell
on fertile social ground. The 60s saw the
rise of the Women’s Movement in which
activists sought increasing freedom on
many fronts: political, legislative, workplace
as well as reproductive. By the late 1960s
women centred health clinics had been
established in most Western countries.
These were usually left leaning in philosophy
and challenged conventional perceptions
about women’s sexuality. Many of the health
professionals in these centres had no objection
to providing contraception to sexually active
young women regardless of their marital status.
Even fundamentally more conservative doctors
recognised in the Pill a more scientific method
of contraception which did not require the
previously “messy” business of fitting a
diaphragm. Thus as the historian Beth Bailey
observed “the Pill was a wonder drug not simply
because of its effectiveness for women but
because of its convenience to those who
prescribed it”.7
What has been the social impact
of the Pill on Women and Society?
During the years of the Second World War,
unprecedented numbers of women were
encouraged to assume roles in industry and
commerce in order to support the war effort.
With the end of hostilities most resumed their
previous domestic roles, but it could not be
expected that such an immense social upheaval
would not have an impact. The leitmotif of the
1950s was home, family and conservatism.
At least for some women, however, this cosy
domesticity masked what was in effect a galling
lack of freedom and opportunity. This was a
time when Australian women were forbidden
from entering a public bar and automatically
forfeited their public service employment upon
marriage. Premarital sex was at once forbidden
and widespread and if an unmarried woman
was unlucky enough to get pregnant she had
only three choices – public shame and adoption
of the child, a shot-gun marriage to the often
unwilling father or a hazardous illegal abortion.
1961 – The first oral contraceptive pill released in Australia.
Page 10 | Ta k i n g i t – 5 0 y e a r s o f t h e p i l l
One of the problems in examining the true
impact of the Pill is untangling it from the social
events which were occurring at the time of its
genesis. The post-war period was a hive of
industry, invention and an overwhelming
optimism that there was no problem which
medical and technological advances could not
address. The 60s and 70s saw immense social
change – a time when long-accepted social
mores were held up to question. It was the era
of the sexual revolution, peace and civil rights
movements and a growing youth culture which
sought to distance itself from the values of its
parents. Germaine Greer’s totemic ‘The Female
Eunich8’ was published in 1970 and prompted
many women to question the gender roles and
societal expectations previously imposed on
them and to develop aspirations beyond that
of being someone’s wife or mother. The Pill
effectively separated the concepts of sex and
reproduction, made contraception “modern”
and laced it under the woman’s own control.
Increasingly, women chose to exercise this
control in order to enter higher education,
to aspire to careers and to delay marriage and
family. Employers too, saw the disappearance
of one of the last excuses for not employing
young women – that they would simply leave
when they fell pregnant. The Pill did not cause
these changes but it certainly enabled and
sustained them.
The Pill saw contraception transformed into a
more esoteric process in which the mechanics
of sex itself need never be mentioned, thereby
enabling wider discussion and debate. This shift
to a more “scientific” focus, and the inevitable
controversy surrounding the Pill’s release, made
it a prime subject for coverage in the press and
on the television sets which were gradually
finding a place in most living rooms. One of the
fathers of hormonal contraception, Carl Djerassi,
was to reflect in a 2007 interview “No one
expected that women would accept oral
contraceptives in the manner in which they did
in the 60s. The explosion was much faster than
anyone expected”.9 And explode it did, with the
use of the Pill in the United States climbing from
400,000 women in 1961 to over 3.5 million only
four years later.2 Australians also responded
enthusiastically to the idea of more effective
contraception and by 1971, 38% of women of
reproductive age were taking the Pill.10 The
removal of sales tax and the addition of the Pill
to the Australian Pharmaceutical Benefits
Scheme in 1972 further increased its availability
and use in this country.
In 1969 the British-American anthropologist
Ashley Montagu ranked the Pill’s
importance with “the discovery of fire”
and went on to predict that “the Pill would
not only emancipate women and make
premarital sex acceptable”, but would
“allow for the overall rehumanisation
of mankind”.11
Hyperbole perhaps, but there is no doubt that
the past 50 years have seen women claiming
both economic equality and the right to
explore a sexuality outside the boundaries of a
traditional marital relationship. Western countries
saw a growing acceptance of premarital sex,
single-parenting, alternative family units and
dual-income households. More couples made
a conscious decision to remain childless and
those that did have children usually opted for
smaller families and had them later in life. This
trend has in fact continued to the point where
many now feel this delay has been pushed
almost beyond biological limits, with statistics
indicating that age-related infertility is now the
commonest reason for referral to Australian
fertility clinics. We may also be in the throes of a
reaction to the demands that such an enormous
social change has placed on the population.
The early 21st century has seen a growing
number of women questioning the desirability
of frantically juggling both career and family
commitments and opting for a more traditional
stay-at-home approach to parenting.
For some social commentators there has been
a continual reassessment of the Pill’s impact.
In her first article for Esquire Magazine in 1962
the influential US feminist Gloria Steinham took
as her theme the Pill’s potential to revolutionise
the lives of women.12 Importantly she also
cautioned that for such a revolution to be
effective there must be a corresponding change
in the attitude of men. Steinham famously later
described the Pill’s impact as “overrated”, but
when interviewed recently on the occasion of
the Pill’s 50th anniversary it appeared she had
again reconsidered her view “There have always
been methods of contraception, but this was
much more dramatic, complete and public”
she said. “It really changed the image of
women and of women’s lives”.13
And it is true that feminists have long had an
uneasy relationship with the Pill. On one hand
it offers the freedom and female reproductive
control promised by Sanger and the other early
contraceptive pioneers. Many feminists however
hold a profound distrust of a medical and
scientific paradigm which they view as malegendered in its focus and motivated by control.
It is also undeniably and shamefully true that
some authorities have sought to impose
contraception on women least able to make
an informed choice or as a matter of national
population control policy. Another potent
suspicion held by many feminist commentators
is that the risks of hormonal contraception are
minimised by big pharma in an attempt to
maintain and boost sales of their products.
Research published in March 2010 perhaps
provides a degree of reassurance on this matter.
A study conducted by the Royal College of
General Practitioners in the United Kingdom
examined the health of a group of women over
nearly 40 years of pill use.2,14 These researchers
found an overall positive effect and concluded
that women on the Pill had lower rates of death
from all cancers (notably bowel, uterine and
ovarian) as well as lower rates of heart disease.
There are many conservative groups, the
most vocal being the Catholic Church, who
maintain strong objections to the Pill and to the
reproductive freedoms it enables. Such groups
link the availability of effective contraception to
immorality, promiscuity, the objectification of
women and the erosion of traditional family
structure and values. It is easy to dismiss these
objections as being relevant only to a small and
diminishing minority and it is true that even
practising Catholics are often able to separate
the religious from the personal. Catholic Italy, for
instance, has one of the lowest birth rates in the
world and a 2002 survey in the United States
showed that the contraceptive use of Catholic
women aged 15-44 years was virtually identical
to that of US woman in general.15 It is, however,
in the developing world, where Christian
doctrine remains more influential and
unchallenged, that pronouncements against
contraception may have a profound impact
on the lives of women. In the words of the
controversial Swiss Catholic theologian Hans
Kung, “This teaching has laid a heavy burden
on the conscience of innumerable people,
even in industrially developed countries with
declining birth rates. But for the people in many
under-developed countries, especially in Latin
America, it constitutes a source of incalculable
harm, a crime in which the Church has
implicated itself”.16
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 11
In the West it is now hard to imagine life without
the Pill. Yet there are countless women in many
parts of the world who have been bypassed
by the choices now seen as a right by their
Western sisters. These women remain trapped
by poverty and restriction. They would be
unable to afford effective contraception even
if their culture and religion allowed it and many
still experience the dangers of multiple
pregnancy and illegal abortion which would
have been immediately recognisable to the
young Margaret Sanger a century ago.
Perhaps it is only when all women across the
world, regardless of their race, colour or religion
have equal access to reproductive rights that
we will truly be able to assess the final impact
of the Pill.
The final word should again go to Huxley.
In a series of lectures on population control
delivered at the University of California in
1959 he commented on the inescapable
link between science and philosophy when
examining the impact of contraceptive
technologies. “The problem of the control
of the birth rate is infinitely complex”,
he said. “It is not merely a problem in
medicine, in chemistry, in biochemistry,
in physiology; It is also a problem in
sociology, in psychology, in theology and in
education.”17 More than half a century later
we are still grappling with the same issues.
References
1. Huxley A. Brave new world revisited. New York:
Harper and Row, 1958: p138-139
2. Gibbs N. The Pill at 50 Sex, Freedom and Paradox.
Time Magazine May 2010. Accessed June 2010
at- http://www.time.com/time/
printout/0,8816,1983712,00.html
3. Warner G, Marie Stopes is forgiven racism
and eugenics because she was anti-life, in:
The Telegraph, Aug. 28th, 2008. Accessed June
2010 at- http://blogs.telegraph.co.uk/news/
geraldwarner/5051109/Marie_Stopes_is_forgiven_
racism_and_eugenics_because_she_was_antilife/
4. Sanger M. Woman and the New Race. Chapter 8.
Birth Control – A Parent’s Problem or Woman’s?
New York. Brentano’s. 1920.
5. Haberlandt L. Hormonal sterilistaion of female
animals. Munchner Med Wochenschr 1921; 68:
p1577-1588
6. Solinger R. Pregnancy and Power: a short history of
Reproductive Politics in America. NYU Press, New
York. 2005 p173
7. Bailey B. Prescribing the Pill: Politics, Culture,
and the Sexual Revolution in America’s Heartland.
Journal of Social History. 1997; 30 (4): p827-856
8. Greer G. The Female Eunich. Paladin. London 1970.
9. Wood G. Father of the Pill. The Observer.
Sunday April 15, 2007. Accessed June 2010 at
http://www.djerassi.com/observer2007/index.html
10. Ware H. Australian Family Formation Project,
Department of Demography, Australian National
University, Canberra. 1973
11. Montagu A. Sex, Man and Society. G. P. Putnam’s,
New York. 1969. p13
12. Steinham G. The Moral Disarmament of Betty Coed.
Esquire. September 1962. p155
13. The Pill Turns 50-Marking Its Golden Anniversary,
Gloria Steinem, Hilary Swank, Dr. Jennifer Ashton
Discuss Its Impact, Future. The Early Show CBS
News, May 6, 2010. Accessed June 2010 at http://
www.cbsnews.com/stories/2010/05/06/earlyshow/
health/main6465686.shtml
14. Hannaford PC, Macfarlane TV, Elliott AM, Angus V,
Lee AJ. Mortality among contraceptive pill users:
cohort evidence from Royal College of General
Practitioners’ Oral Contraception Study. BMJ 2010;
340:c927
15. Ohlendorf J, Fehring RJ. The Influence of Religiosity
on Contraceptive Use among Roman Catholic
Women in the United States. The Linacre Quarterly
74.2 (2007): p135-144
16. Mumford SD, The Life and Death of NSSM 200:
How the destruction of Political will doomed a
US population policy, Center for Research on
Population and Security, Box 13067, Research
Triangle Park, NC 27709); 1994; p203.
17. Huxley A. The population explosion. In: the human
situation, a series of lectures delivered at the
University of California, Santa Barbara, in 1959.
Edited by Piero Ferrucci. Originally published
New York: Harper and Row, 1977.
Contraceptive options.
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 13
5 0 y ear s of the pill – A m e d i ca l , s o c i a l a n d po l i t i cal c o mme n ta ry
“Modern contraception has given women
the potential to plan their lives, complete
their education, and make career decisions.
Motherhood is an option to be exercised not
a compulsion. Pregnancies can be planned
and adequately spaced, improving the health
of both mother and child.”
Dr Edith Weisberg
Director Research
Family Planning NSW
As recently as 1905, President Theodore
Roosevelt attacked birth control and condemned
the tendency towards smaller families as “decadent,
a sign of moral disease”. Most countries passed
anti-contraception laws at some time and many
were not repealed until the mid 1900s. Initially both
the Anglican and Catholic churches opposed birth
control. But by 1930, the Anglican bishops had
approved the use of contraceptives for clearly felt
moral obligations to limit or avoid parenthood or
for avoiding complete abstinence. The Catholic
Church officially still only condones the use of
periodic abstinence. Until the 1960’s the word
“contraception” was not allowed to be used on
Australian radio.
Contraception Today
The present generations of women in their
reproductive years find it difficult to contemplate
what life was like for women without access to
modern contraceptive methods. The advent of
the oral contraceptive pill for the first time
enabled women to reliably control their fertility
with a method unrelated to intercourse. The first
pill, Enovid, released in the US on 11th May
1960, contained high levels of the oestrogen,
mestranol (150µg) and the progestogen,
norethynodrel (9.58mg). High doses were used as
there was no information on which to base the
minimal effective dose. The initial high doses
resulted in unpleasant side effects for some
women, such as breast tenderness and
bloating. It was associated with serious health
risks such as raised blood pressure, heart attack
and venous thrombosis.
In Australia the Pill, released in 1961, was
expensive as there was a 27.5% luxury tax
added, which was only removed in 1972 by
the Whitlam government.
Contraceptive choices
The modern woman now has the choice of
many other safe effective contraceptive options.
The development of long-acting methods,
which no longer require daily action on the part
of the user, have increased efficacy to a level
similar to sterilisation. For women who cannot
tolerate oestrogen or have medical
contraindications to its use, the progestogenonly methods offer a number of options ranging
from a daily pill, three monthly injections, an
under the skin implant lasting three years or an
intrauterine system lasting five years. The major
disadvantage of progestogen only methods is
an unpredictable effect on menstruation.
However, the majority of users of these
methods, apart from the Pill, will have either
no bleeding or light irregular bleeding.
For women who prefer regular cycles but
want a longer acting method the low dose
contraceptive vaginal ring that is left in place
for three weeks is available. In some countries,
a skin patch is available which releases
both oestrogen and progestogen and is
changed weekly.
Page 14 | Ta k i n g i t – 5 0 y e a r s o f t h e p i l l
For women who do not want to use hormonal
methods, copper IUDs provide effective
contraception lasting 5 to 10 years, but may
increase the volume or duration of menstrual
bleeding in some women. An alternative is the
vaginal diaphragm which can provide effective
contraception if used meticulously with each
intercourse. The condom has the added
advantage of protecting against both pregnancy
and sexually transmitted infection.
For women who have completed their families
sterilisation of either themselves or their partner
is an option. Modern surgical techniques
provide minimally invasive outpatient or day-only
procedures for both sexes.
Has the Pill made a difference?
The advent of the Pill, followed by
a plethora of other highly effective
contraceptive methods, has changed
the lives of women and indeed of the
whole community. Gone are the days
where women, especially poor women,
worn out by constant child bearing lived
in fear of pregnancy and often subjected
themselves to unsafe abortion with its
risk of infection, infertility and even death.
With the introduction of the Pill, women
could reliably control their fertility and
their lives were no longer controlled by
their reproductive potential.
Modern contraception has given women the
potential to plan their lives, complete their
education, and make career decisions.
Motherhood is an option to be exercised not
a compulsion. Pregnancies can be planned
and adequately spaced, improving the health
of both mother and child. Limiting family size
enables each child to be provided with
adequate nutrition, education and care
allowing development to its full capacity.
The ability to effectively control fertility has
had a profound effect on western society.
In the majority of relationships sex is a
recreational not a procreational activity, equally
to be enjoyed by both sexes. Women are able
to express their sexuality and enjoy it without
fear of pregnancy. Relationships have changed
drastically since the pre-Pill era where women
were expected to marry young, have children
and become stay at home housewives and
mothers. Moral perceptions have changed.
Premarital sex is accepted and expected;
marriage is no longer the gold standard.
De-facto relationships are common even
when children are involved. There is no stigma
in being an unmarried mother, indeed the state
offers support to single mothers. Women can
choose not to have children and still have
satisfying sexual relationships.
However, as with everything in life there are
down sides to having choices. The modern
woman faces many dilemmas and stresses not
experienced by women in pre-Pill eras. How to
balance career needs with the desire for children.
If she has children, balancing work, home and
child needs while still allowing some time for
recreation and her relationship with her partner.
The biggest dilemma is when to start a family.
Having the ability to control fertility at will has
led women to believe that they can also become
pregnant at will. They expect that as soon as
they stop contraception pregnancy will
immediately follow. Hormonal contraceptives
apart from depot medroxyprogesterone acetate
(DMPA) do not delay the return of fertility.
Irrespective of former hormonal contraceptive
use, it normally takes up to six months for the
majority of couples (70%) to produce a
pregnancy and up to 12 months to two years
for the remainder to conceive. The time to
conception increases with age as fertility starts
to decline in women from 35 years of age.
Modern contraception can prevent
childbearing by young adolescent women
who are likely to suffer more complications
than older women. However, it can make
the decision about when to have a child
more difficult for older women, who may
delay pregnancy because of career needs,
financial needs or find it difficult to accept
the change in lifestyle required once they
have a child.
Future Contraception
Despite the improvements and advancements in
contraception over the last 50 years we still do
not have an ideal contraceptive which is cheap,
100% effective, easily reversible, has no side
effects or health risks and requires little or no
medical intervention.
This holy grail is probably unattainable but
the research continues especially into male
contraception. Although a male pill is highly
unlikely, under the skin implants, injections,
or combinations of the two are likely within
the next five years. These will contain similar
progestogens to those used in female
contraception accompanied by replacement
testosterone. How acceptable these methods
will be to either sex remains to be seen.
Exploration of this issue in a number of different
cultures suggests that it will be high in some
groups but with wide variability, determined by a
number of factors including cultural background
and current contraceptive usage.
Contraceptive vaccines have been researched
for many years but as yet, no successful readily
reversible vaccine has been developed but may
be available in the future.
Compounds which are effective microbicides
as well as spermicides are being researched
which will act as effective local vaginal
contraceptives and prevent sexually
transmissible infections such as HIV,
chlamydia and herpes. Better one-size fits
all diaphragms will enable over the counter
purchase, decreasing cost by avoiding
medical consultation. The development of
long-acting biodegradable contraceptive
implants will mean that users will require only
an insertion procedure but these may pose
difficulty if removal is necessary before the
expiration of the device.
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 15
There is an increasing tendency for women
to want bleed-free contraception. This can
already be provided by back-to-back oral,
vaginal ring or skin patch combined hormonal
methods. However, there is a need to find more
effective oestrogen/progestogen combinations,
which result in a stable uterine lining to prevent
the occasional erratic bleeding episodes,
which occur with back-to-back use of
existing methods.
Public policy
Australia has always had a pro-natalist
government policy. Following the post World
War II baby boom, fertility rates dropped below
replacement levels in 1976, reaching a level of
1.75 in 2003, leading to concerns about a
shrinking workforce and a rapidly aging
population. This led in 2004 to the introduction
of a baby bonus of $3,000 per new child,
gradually increasing to $5,000 per child in 2008.
These payments were not means tested until
2009 when families with an income of more
than $150,000 a year were excluded and
instead of a lump sum, the payments were
made in thirteen bi-weekly payments. It is
likely that the baby bonus has in part been
responsible for the increase in the birth rate
from 1.72 in 2003/4 to 1.98 in the financial year
2008/9. However, it remains to be seen whether
the changes made in 2009 to the baby bonus
will sustain this increase.
There is insufficient public discussion
about options for enabling women to
fulfill both their maternal and work goals.
These include better access to affordable
childcare, adequate paid maternity leave,
flexible working hours which are
compatible with family needs and setting up
systems which allow women to temporarily
leave the workforce and return without loss
of career opportunities.
Although overall Australian women have good
access to a variety of fertility control methods,
there is still inequity. The pharmaceutical
benefits scheme (PBS) provides a range of
subsidised contraceptive methods such as pills,
implants and the intrauterine system. However,
poorer women may not have the same choices
as wealthier women. The only pills subsidised by
the PBS are the early second-generation pills.
The newer pills, the contraceptive vaginal ring
and emergency contraception are not
subsidised and may well be beyond the means
of women with healthcare cards, limiting their
choices in finding a suitable method.
Abortion is still within the criminal law in
many states with the present threat of
court action under the criminal code for
both doctors and women. It is time that
abortion is decrimalised and treated as the
medical procedure it is. This would allow
women to discuss the pros and cons
relating to their personal situation and
provide informed consent for abortion as is
the case for any other medical procedure.
A global view Although in Australia, there are inequities in
access to some contraceptive methods these
pale into insignificance when the plight of
women in the developing world is considered.
About 50% of conceptions worldwide are
unplanned and about 25% unwanted. It is
estimated that 300 million couples do not
have access to family planning services.
The unmet need for contraception is estimated
at 17% of currently married women with no
figures on the need of unmarried women.
In developing countries 137 million women
would like to stop childbearing or space their
next birth, but are not using a modern
contraceptive method because they lack access
to information, education, counselling on family
planning, and cannot access services, or face
other social, economic, or cultural barriers.
At the 1994, International Conference on
Population and Development in Cairo there was a
commitment to ensure reproductive health and
health rights for all, including family planning and
sexual health. The wealthy countries pledged
major investments in family planning, sexual
health, safe motherhood and child survival
programs. However, these wealthy countries
and most notably the United States have
provided less than half the amount promised
in Cairo. The United Nations Commission on
Population and Development stated in 2005
that funding for family planning services
decreased in absolute dollar amounts from
$723 million in 1995 to $461 million in 2003,
a decrease of 36%. The Alan Guttmacher
Institute estimates that to meet at a minimum
the ICPD commitments USD 20.5 billion is
required in 2010 and USD 21.7 billion in 2015.
Worldwide, 800,000 women die from
complications of pregnancy and childbirth
annually, all but 4,000 of whom are in the
developing world. This is more than four times
the death toll of the Aceh tsunami. For every
woman that dies up to 10 more women will
have significant morbidity. Many of these
complications last her lifetime. In Australia,
women have a lifetime risk of 1 in 6,500 of dying
of a pregnancy related cause but the risk is five
times greater for indigenous women. Eastern
and Southern African women have a 1 in 15 risk
while in South Asia the risk is 1 in 43. One
quarter to one third of maternal deaths in
the world are due to complications of
unsafe abortion. Of the 150,000 pregnancies
terminated daily one third are done in unsafe,
adverse conditions.
Among the millennium goals set in 2000 to
be achieved by 2015 were the eradication
of poverty and hunger, promoting gender
equality, reducing child mortality and
improving maternal health while also
ensuring environmental sustainability.
At the time, no mention was made of the
obvious link between these goals and
reproductive and sexual health.
To achieve goal 5, improving maternal
health, contraceptive services are needed
to effectively save lives by preventing
unplanned and high-risk pregnancies.
Averting unwanted pregnancies will also avert
unsafe abortions. Emergency obstetric care and
pre and post-natal care are critical to safe
motherhood. Preventing high-risk pregnancies and
providing pre-natal care reduces infant and child
mortality. Smaller families and better birth spacing
allow families to provide better nutrition and health
care. Unwanted pregnancies can put infants and
children at risk of neglect or abandonment.
Page 16 | Ta k i n g i t – 5 0 y e a r s o f t h e p i l l
To achieve goal 3, the promotion of
gender equality, controlling the timing
of childbearing is critical to women’s
empowerment, including educational
attainment and paid employment.
Smaller families may reduce gender inequities
in nutrition, education, health care and other
family investments in children.
To achieve the goal of environmentally
sustainable and equitable development,
delayed childbearing, wider birth intervals
and smaller families are necessary to slow the
momentum of population growth. Control over
childbearing can also help families emerge from
poverty. Lower fertility levels can permit higher
per capita investments.
Meeting global family planning needs will
save the lives of an additional 1.5 million women
and children each year, reduce the number of
induced abortions by 64% by averting 52 million
pregnancies, preventing 142,000 pregnancy
related deaths (including 53,000 from unsafe
abortion) and preventing 505,000 new orphans.
The transformation of reproductive and
sexual rights and health into reality requires
political will, increased and sustained
national and international financing for
reproductive and basic health services.
There needs to be equality and adherence to
human rights which encompass advocacy for
reproductive rights. There is a need for
intersectorial action nationally and internationally
to link progress in the development of health,
education, poverty alleviation and human rights.
Conclusion
While western women celebrate 50 years
of the Pill and the freedoms they have achieved
through effective fertility control, even if gender
equality is not yet fully achieved, we need to be
aware how fortunate we are. For the most part,
we have a range of affordable contraceptives,
excellent sexual and reproductive health
services and maternal and childcare facilities.
We should not take this for granted but work
towards a worldwide recognition that access
to reproductive and sexual health and related
services are a human right.
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 17
A REFLEC TION: Pills, sex a n d fam i ly pl a n n i n g …
“It would be wonderful if sexually active young
people could all confidently access services and
receive comprehensive and accurate information
at school as well as via new avenues such as
the internet and social media. But this is not of
course always the case, particularly in our rural
and remote areas, and amongst Aboriginal and
migrant women.”
Dr Deborah Bateson
Medical Director
Family Planning NSW
When invited to write these short reflections,
I could not help thinking back to my own first
contraceptive experience. As a teenager,
growing up in Liverpool in the UK in the mid
70s, I experienced a serious pregnancy scare
just before my A-level exams.
Luckily my mother and I could talk about such
things and, after the scare proved unfounded,
she decided that a visit to the family GP was
in order. He was a kind, and in hindsight,
enlightened doctor and I can remember every
detail of the consultation in which we all
enthusiastically agreed that the Pill would be
terribly useful for my “menstrual migraines” and
never once mentioned the word contraception
let alone anything to do with boys or sex.
Everyone was satisfied with this solution and
I was able to get through those exams and go
off to university with control over my fertility. It
would be wonderful if, 30 years later, sexually
active young people could all confidently access
services and receive comprehensive and
accurate information at school as well as via
new avenues such as the internet and social
media. But this is not of course always the case,
particularly in our rural and remote areas, and
amongst Aboriginal and migrant women.
Women’s Suffrage.
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 19
t h e pill i s 5 0 years old …
“The Pill is 50 years old – but has it fulfilled
our expectations? Where have we come with
contraception and family planning in the last
half a century?”
Professor Gab Kovacs AM, MB, BS HONS, MD.,
FRCOG, FRANZCOG, CREI, FAICD, Grad Dip Mgt (Macq)
Professor of Obstetrics and Gynaecology Monash University.
Honorary Consultant, Family Planning Victoria
The medical evolution of the modern pill
In 1949 Carl Djerassi joined Syntex, and with
his colleagues prepared norethisterone from
19-nor-testosterone in 1951. This had twice
the potency of progesterone,1 and in contrast
to progesterone which had to be administered
parenterally, it was orally active. This was the
first of several ethinylated testosterone derivates
which have been used in oral contraceptives.
In the USA it is known as norethindrone, and
the rest of world knows it as norethisterone.
This new progestin was first tested clinically
for the treatment of menstrual disorders by
Dr. Hertz at the NIH at Bethesda, USA in 1954.
Simultaneously, Dr Frank Cotton at G D Searle
patented another synthetic progestin,
norethynodrel, which was astonishingly similar
to norethisterone, the only difference being one
double bond between two of the carbon atoms.
Yet they were synthesised by different methods
and slightly different biological actions.
Although it had been recognised since the 1940s
that ovulation could be mostly inhibited by the
administration of oestrogen the addition of oral
progestin resulted in better efficacy and cycle
control. It was Rock, Garcia and Pincus who
found that the potent new progestin
norethynodrel at 30mg per day, administered
from day 5 to 25 of the cycle was an effective
contraceptive.2 These findings were first
presented at an International Planned Parenthood
Federation meeting in Tokyo in October 1955.3
Field trials were established in Puerto Rico, using
the Searle product norethynodrel.
It was believed that only the progestin was
necessary for contraception, and the “impurity”
oestrogen was eventually removed by the Searle
chemists. This led to a loss of cycle control and
decreased efficacy. It then became recognized
that oestrogen was necessary, and was
reintroduced in precise amounts.
The first oral contraceptive
These studies led to the approval of the first oral
contraceptive, Enovid (Searle, USA) in 1959.
Enovid contained 9.58mg of norethynodrel and
150ug of the synthetic oestrogen, mestranol.
The first oral contraceptive on the European
market was Anovlar (Schering, Germany).
This contained 4mg of nor-ethisterone as
the progestin, and 0.05mg of ethinyl oestradiol
in 1961.
Soon a more potent progestin, norgestrel was
developed, requiring only 0.5mg to be effective,
compared to 10-15mg norethindrone. It became
known as a “second generation” progestin.
When first introduced, norgesterel was a mixture
of the d and l isomers, and it subsequently
became recognised that the pharmacological
activity was exclusively from its levo form.
Page 20 | Ta k i n g i t – 5 0 y e a r s o f t h e p i l l
the Pharmaceutical Benefits Scheme (PBS),
they never captured significant market share
in Australia.
The next phase
What I call the “fourth generation” progestin
is drospirenone, a progestin derived from
17a-spirolactone with a pharmacological profile
similar to that of natural progesterone with potent
progestogenic, anti-mineralocorticoid, and
anti-androgenic activities and no oestrogenic
activity. It is available in Yasmin® and Yaz®.
One must not forget the cyproterone acetate/
ethinyl oestradiol containing oral contraceptive
which in Australia is approved for use in the
treatment of acne and “not indicated for
contraception alone.”
Dr Gregory Pincus.
In order to reduce the dose of progestin
further, its active levo-isomer was isolated
and subsequently used as levo-norgestrel,
without affecting efficacy.
Third generation pills
The next phase in the development of
progestins in oral contraceptives was the
development of a novel group of gonane
progestins with minimal androgenic activity.
These are called the “third generation”
progestins, and include desogestrel (active
metabolite 3-keto-desogestrel), gestodene and
norgestimate. The former two are now readily
available in oral contraceptives. These
preparations combine high progestogenic
efficacy with low androgenic activity.4
Unfortunately, combined oral contraceptives
(COC) utilising these third generation
progestogens were caught up in the Venous
Thrombo Embolism (VTE) controversy of 1995.5
Consequently, and as they were not listed on
Nevertheless, it is an efficient contraceptive,
and is the COC of choice for women with
androgenic symptoms, and many women
with Polycystic Ovary Syndrome (PCOS)
The oestrogen component
The only oestrogens used in a COC for the
past 50 years were either ethynyloestradiol (EE) or
mestranol – which is metabolised to EE. We went
through the fight to have “natural” oestrogens used
in Hormone Replacement Therapy (HRT) on the
PBS because they had fewer side effects, and we
have waited 50 years to have COC containing a
natural oestrogen rather than EE. We now have a
natural oestrogen containing COC on the market,
Qlaira®, an oral contraceptive with four sequential
phases comprising differing levels of the oestrogen,
estradiol valerate, and the progestogen, dienogest,
in a oestrogen step-down and progestogen
step-up regimen.6
Next year another natural oestrogen pill
containing 17b-oestradiol, with nomegestrol
acetate as the progestogen in a monophasic
preparation will be available in Australia.
Phasic pills
Although the initial pill preparations contained
the same concentration of oestrogen and
progestogen, in the early 1980s it was
recognised that the dose of hormone could
be reduced if they were administered in a
sequential step up manner, where the progestin
dose increases from 50ug per day to 125ug per
day.7 The triphasic preparation resulted in a 39%
reduction in the dose of levonorgestrel ingested
each month. By minimising the amount of
levonorgestrel, the triphasic preparation was
found to increase Sex Hormone Binding
Globulin (SHBG), and did not change HDL
cholesterol, and had less effect on HDL
cholesterol: total cholesterol ratio than the
monophasic version, and in summary has less
negative effects on lipid metabolism.8 Though
initially popular, it was soon recognised that its
disadvantages outweighed its benefits.
Duration of pill taking
When the Pill was first released it was marketed
on a 21 days of hormones, 7 days pill free
regimen, as a marketing ploy, so that every
woman who took it would be a “perfect 28 day
woman”. There is absolutely no physiological
reason for this, and it could have easily been
a six weekly or three monthly cycle. The
“trimonthly regimen” was piloted in Australia
in 1994, with the only disadvantage being an
increased incidence of break through bleeding.9
It was subsequently marketed in the USA
as “Seasonale®” a 30ug EE and 150ug
levonorgestrel pill, packaged as 84 active tablets
followed by 7 placebos. It again was reported to
have less bleeding days, but more unscheduled
bleeding. In 2007 the US FDA approved Lybrel®,
a continuous combined oral contraceptive pill
containing 20ug of EE and 90ug of levonorgestrel.
Non-contraceptive benefits of the Pill
Quality of life: one of the greatest noncontraceptive benefits of the combined oral
contraceptive pill is the relief of dysmenorrhoea
or painful periods. This is thought to be due to
the inhibition of ovulation and the absence of
a corpus luteum. The corollary of this is that if
dysmenorrhoea persists despite the use of
the Pill, then a pathological cause such as
endometriosis should be considered.
Another non contraceptive benefit of highly
significant proportions is the decrease in
menstrual blood flow with consequent
decrease in the incidence of anaemia.
Not only does the Pill decrease menstrual loss,
but it gives a woman the ability to control when
she menstruates.
Longevity: research in which the “chance of
dying” among women who have ever used oral
contraceptives was compared to that of never
users. This prospective cohort study started in
1968 and 46,112 women were observed for up
to 39 years, resulting in 378,006 woman years
of observation among never users of oral
contraception and 819,175 among ever users.
It was reported that ever users of oral
contraception had a significantly lower rate of
death from any cause (adjusted relative risk
0.88, 95% confidence interval 0.82 to 0.93) with
an estimated absolute reduction in all causes of
mortality among ever users of oral contraception
of 52 per 100 000 woman years.10
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 21
Cancers and the Pill
There is unequivocal evidence that both
ovarian and endometrial cancers are significantly
decreased in current and past users of the COC.
The incidence of cervical cancer is difficult to
assess because of confounding factors of condom
use, number of partners, sexual activity and HPV
incidence, but current studies do show that there
may be a slight increase.11 The studies on the
incidence of breast cancer are conflicting, and
the results are confounded by individual risk
factors, including genetic predisposition.
When combined in a meta-analysis they show
a significant but modest increased risk of
premenopausal breast cancer in general (OR,
1.19; 95% CI, 1.09-1.29) and across various
patterns of OC use, especially with use before
first full term pregnancy in parous women.12
Venous thromboembolism and the Pill
Although the COC was only released on the
market in 1960, by 1961 the first report of a
thrombo-embolic complication was published.
It was recognised that the risk was related to
the oestrogen dose, and there has since been
a steady decrease in the oestrogen dose from
150ug to as low as 15ug. There also has been
much discussion about the degree of risk, and
the possible increased risk with various
progestogens, especially the “third generation”.
Some thoughts 50 years on…
The population explosion
One of the world’s greatest problems is
conservation – how can we feed, house and
supply water for the exploding population
especially in developing countries?
On a worldwide basis we have made great
progress with the birth rate steadily decreasing:
Table 1. Change in birth rates 2003-2004.14
Percent
Change
Date of
Information
Year
Birth rate*
2003
20.43
2004
20.30
-0.64 %
2004 est.
2005
20.15
-0.74 %
2005 est.
2006
20.05
-0.50 %
2006 est.
2007
20.09
0.20 %
2007 est.
2008
20.18
0.45 %
2008 est.
2009
19.95
-1.14 %
2009 est.
2010
19.86
-0.45 %
2009 est.
2003 est.
* The average annual number of births during a year per 1,000
persons in the population at midyear; also known as crude birth
rate. The birth rate is usually the dominant factor in determining
the rate of population growth. It depends on both the level of
fertility and the age structure of the population.
The average child per couple worldwide is
now at a weighted average of 2.8 children
born per woman, with an average of 1.5 for
the European Union.
There is still a disproportion in developing
countries with 7.34 born per woman in Mali,
and 7.29 in Niger, 6.58 in Afghanistan.
However countries like India have reduced
their population growth to 2.76 and China
to 1.77 per woman, due to population
control measures.14
Thus on a global level population control
has made a difference.
Unplanned pregnancies
Unfortunately the advances in contraception
have had little effect on the number of
unplanned pregnancies in most developed
countries. It is reported that one in 10 Dutch
women has had a termination of pregnancy.
Firm data for Australian women is not available,
but statistics from Britain for 2009 record
189,100 abortions.
Figure 1. United States abortion rates,
1960-2005.15
There is no doubt that all COC are associated
with an increased incidence of venous thromboembolic (VTE) events, but overall VTE is a rare
event, so whilst being statistically significant,
is it clinically significant? Dinger illustrates this
elegantly in his research showing that the risk
of VTE in non-pregnant women not using any
oestrogen containing COC is 4.4/10,000 woman
years, those using low dose pills is 8.9/10,000
and during pregnancy 29.5/10,000.13
Why are we still having an epidemic of
unplanned pregnancies when there are
so many contraceptive choices?
Barriers to obtaining contraceptive advice
In 1970, my “engaged” but not yet married
sister in law attended a General Practitioner
for a repeat prescription of the combined
contraceptive pill. He threw her out after giving
her a lecture on “pre-marital” sex. I would be
very surprised if that would still happen today,
and there are many facilities for young single
women to obtain contraceptives, such as family
planning clinics, student health centres and
teenager friendly practices. Condoms are
available not only in supermarkets but also
from vending machines, so accessibility of
contraceptives is not a problem. Many oral
contraceptives are subsidised by the
Pharmaceutical Benefits Scheme and available
to socially disadvantaged women on a Health
Care Card for $5.30 a prescription, which
includes the etonogestrel implant (Implanon®)
for three years of contraception, and the
levonorgestrel intrauterine system (Mirena®)
for five years of protection.
Some couples have unprotected intercourse
because they think that “it won’t happen to
them”. Just once can’t possibly get them
pregnant, or they just decide to risk take,
especially if under the influence of alcohol
or drugs.
We must continue to educate that once is
enough, and also make condoms readily
available. It is good to see vending machines
in hotels, clubs and airports. We must also keep
re-enforcing the message that a well applied
condom properly used is an effective
contraceptive, as well as being a reasonable
barrier to most sexually transmitted infections.
It is hard to determine what proportion of these
were unplanned, but one can presume, most.
Page 22 | Ta k i n g i t – 5 0 y e a r s o f t h e p i l l
Barriers to the effective use of contraceptives,
especially the Pill.
When considering the effectiveness of any
contraceptive there are three levels of efficacy:
1. Perfect use or theoretical efficacy; using
the method correctly and consistently (this is
quoted at less than 0.55% for 30ug pills and
up to 1.26% for 20mcg pills.)16
2. Typical use; the efficacy one would expect
from actual users in a clinical trial who follow
all instructions. This is quoted at up to
1.19% for 30mcg and up to 1.6% for
20ug pills.16
3. Imperfect use – which is also described
as “patient failure” where users do not
follow the instructions. The Pearl Index
for imperfect use is unlimited.
With oral contraceptives there is great
opportunity for imperfect use, forgetting to
take the tablets every day, taking it later than
the twenty-four hour rule permits, or not
following the “seven day rule” after an
indiscretion. There is also the possibility that
there has been some interaction resulting in
malabsorption, or large bowel reabsorption,
such as vomiting, diarrhoea or drug interactions
inducing liver enzymes or interfering with
steroid reabsorption.
The non-oral administration of combined
oestrogen:progestogen overcomes some
of these possible risks for “imperfect use”,
an example being the contraceptive vaginal
ring (NuvaRing®).
The efficacy of hormonal contraceptives has
been improved by minimising imperfect use by
administering them as a Long Acting Reversible
Contraceptives (LARC). Unfortunately these are
currently only available for progestogen only
methods (implant, intrauterine system,
injectable) which in contrast to controlling
menstruation (see non-contraceptive benefits
of the Pill), result in irregular, unpredictable
bleeding, or even amenorrhoea. Apart from the
combined oestrogen:progestogen vaginal ring
which is medium term contraceptive, there are
no LARCS containing both hormones.
My final thought is: have we been too
successful at providing contraceptive
options, and has this resulted in women
delaying childbirth for too long, resulting in
an increased need for fertility intervention
due to advancing maternal age?
References
1. Kovacs GT.The pharmacology of progestins used
in oral contraceptives – An historical review to
contemporary prescribing. Aust and N Z J of Obst
and Gynaecol. 2003;43: p4-9.
2. Rock J, Garcia C R, Pincus G. Synthetic progestins
in the normal human menstrual cycle. Recent Progr
Horm Res 1957;13:323.
3. Pincus G G. Some effects of progesterone and
related compounds upon reproduction and early
development in mammals. In: The 5th International
Conference on Planned Parenthood. Tokyo. Report
of Proceedings, p175-184.
4. Elstein M editor Gestodne, development of a new
gestodene-containing low-dose oral contraceptive.
Carnforth: Parthenon, 1987.
5. Weiss N. Third-generation oral contraceptives:
how risky? Lancet 1995; 346:1570.
6. Endrikat J, Parke S, Trummer et al. Ovulation
inhibition with four variations of a four-phasic
estradiol valerate/dienogest combined oral
contraceptive:results of two prospective,
randomized, open-label studies. Contraception
2008: 78; p218-25.
7. Lachnit-Fixson U.The rationale for a new
triphasic contraceptive. In: Greenblatt R D, editor.
The development of a new triphasic contraceptive.
Lancaster:MTP Press Limited,1980: p23-29.
8. Larsson-Cohn U, Fahreus L, Wallentin L,
Zador G. Effects of some ethinyloestradiol/
levonorgestrel combinations on SHBG and on
lipid metabolism. In:Greenblatt R D, editor.
The development of a new triphasic contraceptive.
Lancaster:MTP Press Limited,1980: p69-77.
9. Kovacs G., Rusden J., Evans, A. A trimonthly
regimen for oral contraceptives. Br J of Fam Plan
19: p274-275.
10. Hannaford PC, Iversen L, Macfarlane TV, Elliott AM,
Angus V, Lee AJ. Mortality among contraceptive pill
users: cohort evidence from Royal College of
General Practitioners’ Oral Contraception Study.
BMJ. 2010;340:c927.
11. Hannaford PC, Selvaraj S, Elliott AM, Angus V,
Iversen L, Lee AJ.Cancer risk among users of oral
contraceptives: cohort data from the Royal College
of General Practitioner’s oral contraception study.
BMJ. 2007;335:651.
12. Kahlenborn C, Modugno F, Potter DM, Severs WB.
Oral contraceptive use as a risk factor for
premenopausal breast cancer: a meta-analysis.
Mayo Clin Proc. 2006;81:1290-302.
13. Dinger JC, Heinemann LA, Kühl-Habich D.The
safety of a drospirenone-containing oral
contraceptive: final results from the European Active
Surveillance Study on oral contraceptives based on
142,475 women-years of observation.
Contraception. 2007;75: p344-54.
14. CIA World Factbook - Unless otherwise noted,
information on this page is accurate as of
February 19, 2010.
15. Compiled by Wm. Robert Johnston last modified
17 February 2008.
16. Mansour D. Efficacy of contraceptive methods.
A review of the literature. Eu J Contracept Reprod
Health Care 2010; 15: p4-16.
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 23
T h e medi calisation an d d e m ocrat i sat i o n of co n t r ace p t i o n
“I have often told my students that the
introduction of the Oral Contraceptive Pill
resulted in medicalisation and democratisation
of contraception. But this was not achieved
overnight or with ease. This is an attempt to
tell a fascinating history in a few pages.”
Dr Stefania Siedlecky AM MBBS (Hons 2) Sydney,
MSc Medical Demography
London School of Hygiene and Tropical Medicine
In ancient classical writings, some of the herbal
drugs referred to were recommended to expel
the afterbirth or a dead foetus, or to overcome
uterine inertia. There was some confusion
between what constituted contraception and
what constituted abortion. Over time the idea
was extended to taking medication to avoid the
actual pregnancy. How effective some of these
early methods were is unknown but certainly
there were various levels of fertility control,
which became one of the factors affecting
population growth.
In the mid 19th century the vulcanisation of
rubber led to diaphragms and cervical caps and
more reliable condoms than the previous penile
sheaths; douching was introduced. The 1904
Royal Commission on the Decline of the
Birthrate and the Mortality of Infants in NSW
reported a cervical stud, one of the early
intrauterine devices (IUDs).1 By the mid 1960s
there were innumerable IUDs, at first nonchemical but later the copper containing and
more recently hormone containing IUDs.
In Australia it was originally considered that IUDs
did not have a medical effect, and they were not
subject to drug evaluation until it was found
necessary to test other devices such as artificial
heart valves. These advances meant a greater
involvement of medical practitioners. Meanwhile
official and religious attitudes to contraceptive
use became more prohibitive.
Medical attitudes to contraception
In 1897, the Catholic gynaecologist,
Dr Michael O’Sullivan, in a Presidential
address to the Victorian Branch of the
British Medical Association, stated that:
“Criminal abortion, performed generally by
illiterate and uncleanly charlatans of either sex,
claims numberless victims and consigns them
to permanent invalidism. But the most potent for
evil is the prevention of conception”.2
Ten years later, he warned somewhat
ambiguously of the use of birth control by
married couples: “But when a wife defiles the
marriage bed with the devices and equipment of
the brothel, and interferes with nature’s mandate
by cold-blooded preventives and safeguards;
when she consults her almanac, and refuses to
admit the approaches of her husband except at
stated times; when a wife behaves in so
unwifelike and unnatural a manner, can it be
otherwise than that estrangements and painful
suspicions of faithfulness should from time to
time occur? Can a home with such environment
be a happy one? Many husbands so situated
are, I fear, tempted to seek elsewhere the
pleasures denied them at home. Such are
nature’s reprisals; such indeed her
unfailing retributions”.3
Page 24 | Ta k i n g i t – 5 0 y e a r s o f t h e p i l l
Into the early 1900s, the English medical
press opposed contraceptive use on
ethical and moral grounds and some
doctors emphasised the harmful effects of
contraception including galloping cancer,
sterility and nymphomania in women, and
mental decay, amnesia and cardiac
palpitations in men. The Lancet called
it a sin against physiology.4 Similar
accusations are still made by opponents
of contraception.
Social attitudes to contraception
During the nineteenth century, laws were
introduced in many countries to make abortion
and the advertising and sale of contraceptives
illegal. Some birth control pioneers faced legal
action but the movement persisted and women
continued to try to avoid pregnancy.
In 1900, the NSW government, alarmed
at the declining birthrate and decline in
immigration, set up a Royal Commission on
“the Decline of the Birthrate and the Mortality
of Infants”. The Commission interviewed mostly
men: doctors, clergy, police, and pharmacists
and reported in 1904.They considered the main
cause was avoidance of childbearing:
“…we have been…driven to the conclusion
that the people… led astray by false and
pernicious doctrine into the belief that personal
interests and ambitions, a high standard of
ease, comfort and luxury, are the essential
aims of life…have neglected their true duty to
themselves, to their fellow countrymen, and to
posterity”.5 The second volume of their report
which gave details of contraceptive use and
abortion was considered so scandalous that
only twelve copies were published and were
not available for distribution.
Their recommendations included licensing of
maternity hospitals, restrictions on the import,
distribution and advertising of abortifacients and
contraceptives and emphasis on the clergy for
the teaching of moral behaviour.
While some pharmacists admitted to selling
emmenagogues, they denied selling
abortifacients although they knew that women
used emmenagogues as such. There was
considerable reticence about contraception
not confined to the pharmacists alone. In 1842
Thomas Beecham, of Beecham’s Pills fame,
started selling Pills called “Female’s Friend,”
made from his own secret formula, in Wigan,
England. He became a wealthy pharmacist and
Beecham’s Pills became internationally known
and aggressively marketed; Beecham’s became
the largest advertiser in the United Kingdom.
Beecham was also the grandfather of the noted
conductor, Sir Thomas Beecham.
One famous Beecham’s Pills advertisement
showed a mother counselling her daughter,
and stated: “Their fame has reached to the
uttermost ends of the earth. Their curative
power is universally acknowledged to a
degree unprecedented in the annals of
physical science and it is echoed from
shore to shore that for Bilious and Nervous
Disorders, Indigestion with its dreaded
allies, and for assisting nature in her
wondrous functions, they are WORTH
A GUINEA A BOX”.6 Possibly to avoid
embarrassment to the family, the words
in italics were omitted in the version
reproduced in the biography of
Thomas Beecham written by his
great‑granddaughter.7
In 1905, the Dunlop Rubber Company
Chairman, the Honourable Nicholas Fitzgerald,
a devout Catholic and Papal Knight, decided
that his firm would cease making condoms.
The equipment was bought by Eric Ansell. In
the early years of the Ansell Rubber Company,
condoms were referred to as the “A” products
and the condom machine was the “A”
machine.8 In America, Goodyear Rubber had
never advertised its condom business despite a
$150 million market in 1958.9 It was rumoured
condoms could be bought from a barber or
from a petrol station, as well as a pharmacist.
Australia: the challenge of managing fertility
in the depression and war years
The large decline in births during the years
of the Depression in the 1930s indicated that
many women were practising some type of birth
control. I recall that my mother, who suffered
from mitral stenosis, had two children in the
first four years of marriage and was advised
to have no more. At night going to bed, she
boiled up a jug of Condy’s Crystals (potassium
permanganate). Only years later did I realise
she was using a douche, and I found it
amazing to picture my mother leaping out
of bed after sex to do this.
As medical students during World War II
we were given little information on birth
control, even though there were many
women who had love affairs with the
American soldiers and ended up with
illegal, sometimes fatal, abortions.
Our Gynaecology lecturer, Dr (later Sir) Herbert
Schlink devoted four pages to the subject in
his gynaecology text book for medical students,
merely to prepare them for the “numerous
questions which would be put to them by
their patients” and also so that they would not
“unjustifiably act as aiders and abettors of a
practice that will never be entirely stopped,
but that is not altogether wise if you care for the
future of the white races”. He further wrote that
“Mankind would be happier and healthier if
nature were allowed to decide these issues.
Famine, flood and disease will see to it that
the world is not over-populated.”10 When we requested further information from
our Obstetrics tutor, Dr Ida Saunders, her reply,
quoted also by other students was “I’m here to
teach you how to deliver babies, not how to
prevent them”.
Professor Bruce Mayes in his 1950 Obstetrics
textbook mentions briefly only the safe period
as a method of enhancing the chance of
pregnancy or of avoiding pregnancy.11
As a resident at Crown St Women’s hospital
in 1944, I found that women who suffered
complications during pregnancy or labour
were advised not to have another
pregnancy for two years, but no advice
was given about how to manage that.
Fortunately a fellow doctor, Dr Doris Selby,
taught me how to fit a diaphragm. When I
was later in practice in the Blue Mountains,
other doctors referred women to me for a
diaphragm. Condoms, creams, self-made
pessaries, douching, rhythm and
withdrawal were the methods mostly used
to avoid pregnancy.
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 25
The fight for women’s rights
The first wave of feminism in the early 1900s
was mainly concerned with women’s rights to
vote, and only later with the rights of women
to control their fertility. The Race Improvement
Society was set up in 1923 to become the
Racial Hygiene Association (RHA) in 1927 and
the Family Planning Association of Australia
(FPAA) in 1960. Its original aims were sex
education, eradication of venereal disease and
education along eugenist lines. They opened
their first birth control clinic in Sydney in 1933,
aimed at married women only. Over the past
70 years, every international conference on
population or on women has included in its
recommendations that women and couples
should have the right to determine their
own fertility.
Family planning services in Australia
In 1967 Professor Rodney Shearman reported
to a World Health Organisation meeting that
Australia had the highest rate of oral
contraceptive usage of any country in the world.
Hospital family planning clinics were rare and
most prescriptions were provided privately,
which made it difficult to organize clinical
trials.12 The National Health and Medical
Research Council recommended in 1969
that family planning facilities should be made
readily available and by 1973 there were FPAA
branches in each state. Shearman also set up
a National Medical Advisory Panel. The FPAA
branches ran clinics in Baby Health Centres
and hospital out-patient departments. I recall
working in at least six different centres in Sydney
in the early 1970s. In North Sydney the Mayor
was a Catholic doctor and would not approve
a clinic in the Baby Health Centre, which he
considered would encourage promiscuity
among young people. It was only after a new
mayor was elected that a clinic was opened
in North Sydney.
General practitioners came to realize that there
was a considerable demand for and income in
prescribing the Pill. A survey of general
practitioners only, showed that the number of
prescriptions for the Pill, had increased from
839,000 in 1970-71 to 2,032,000 in 1974.13
The National Association of General
Practitioners resented the FPAA opening further
clinics and wrote in the Australian Medical
Association (AMA) Gazette that “the delivery
of contraceptive services through the Family
Planning Associations in many respects is very
wasteful of resources and money that can be
more economically and adequately provided
through the existing primary health care system
in Australia”.14
After discussions, the AMA and the FPAA
drew up a code of ethics aimed at ensuring
there was no conflict between clinic doctors
and general practitioners including “Before oral
contraceptives are prescribed, the patient’s
doctor should be informed”.15
During the early 1970s, representations
were made by family planning organisations
and others to have the sales tax on
contraceptives lifted and the Pill added to
the PBS, a move supported by the NHMRC.
Politicians used Question Time in the
Federal Parliament to raise family planning
issues such as support for international
family planning organisations (Everingham,
7 September 1971), illegality of sterilisation
in Queensland (Klugman, 23 November
1971), and advertising of contraceptives
in the Australian Capital Territory (ACT)
(Enderby, 2 November 1971).
Although many Liberal parliamentarians
supported family planning, Prime Minister
William McMahon feared a reaction from
Catholic and DLP voters. The Sun Herald
in March, 1972, carried a headline “Liberals
Split over Bid to End Tax on Pill”.
Within the first two weeks of winning
the December 1972 election, the Whitlam
Government removed the sales tax on the
Pill and had it added to the Pharmaceutical
Benefits list; lifted the sales tax on all
contraceptives; announced a grant of
$300,000 for international birth control
programs; and lifted the prohibition on
contraceptive advertising in the ACT.16
Stefania Siedlecky (R) and Diana Wyndham launch their history of the family planning movement, ‘Populate & Perish’.
Page 26 | Ta k i n g i t – 5 0 y e a r s o f t h e p i l l
In 1973 abortion was added to the services
covered by health insurance (and later
Medibank); the age of legal maturity was
lowered from twenty one to eighteen years;
and the Commonwealth Family Planning
Program (FPP) was established. Under this,
funds were made available for the FPAA and
Catholic Social Welfare Commission for
provision of services; money set aside for
research and doctor education programs and
grants were made to the Family Life Movement
(1973) and the Family Planning Association,
South Australia (1975) to make films for family
life education. In 1974, I was appointed as
Consultant in Family Planning to provide advice
on the FPP.
With the introduction of Medibank, and the
later introduction of Medicare and bulk billing,
contraceptive advice was now available to all
women at low cost, a significant move towards
democratization.
In 1973, the Sydney University Postgraduate
Representative Association (SUPRA) for the first
time published a comprehensive booklet on
contraception, sexually transmitted diseases
and abortion, which was continued for several
years.17 It gave emphasis to the Pill although it
dealt with all methods.
1960’s Brochure handout at universities.
Family planning services for unmarried women
Within FPAA, the debate on whether to extend
services to unmarried women and minors
continued into the early 1970s. In 1965-66,
the FPAA Annual Report stated that “it is not
the policy of the Association to moralise”, but
official attitudes remained fearful of public
reaction. Some single women, including women
under age 21, already did attend FPAA clinics,
and staff arranged that they were referred to the
more liberal minded doctors as some, even in
FPAA, were uncomfortable with prescribing for
minors. A change in the philosophy of the
Association was reflected in this statement in
the 1970-71 report “Services provided at the
clinics include: Help with birth control for
everyone over the age of consent, married or
unmarried, male or female”.
Treating young women under the age of consent
A more difficult problem was treating young
women under the age of consent. One speaker
at a FPAA symposium in 1972 declared that
girls under age 21 who still lived at home,
should not be given contraceptive advice
without the consent of their parents.
In 1971, the Queensland Branch of the AMA
decided to adopt the ruling of the AMA Federal
Council that it was: “the inalienable right of any
doctor to prescribe what he considers to be in
the best interests of his patient” (regarding the
prescription of oral contraceptives to unmarried
minors, each case should be considered on its
merits, and provided that State law permitted,
the ultimate decision should be left to the
individual doctor’s conscience).18
Over the next year there was considerable
correspondence in the Medical Journal of
Australia (MJA) on the subject of minors.
One doctor declared that it was not the “duty
of the medical profession to prescribe oral
contraceptives to un-married minors of Spockmarked parents” to avoid an unwanted
pregnancy which could lead to an abortion,
adding “This sort of thing only makes doctors
party to fornication or prostitution”.
Another doctor said: “I have felt constrained
on occasions to express the point of view that
I did not do a six years medical course merely
for the sake, inter alia, of providing the young
bucks with a means of having their pleasure
without responsibility”.
Sex education programs for schools in NSW
and other states were developed by FPAA.
On one occasion the question was vigorously
debated at a Parents and Citizens meeting at
my son’s prestigious high school but other
parents considered that only parents should
teach their children about sex. The acting
headmaster came to me in some anger after the
meeting to say that in his opinion high school
was “no place for teaching boys how to fuck”.
A boy from that school made his girlfriend
pregnant, his parents were Jewish and marriage
was out of the question, but they offered to pay
for an abortion which the girl’s parents refused.
The relationship broke up, the girl sat and
passed her Higher School Certificate; but she
developed toxaemia of pregnancy, had to have
a Caesarean section and the baby died. A tragic
introduction to adulthood.
About the same time I was asked to give
nurses’ lectures on gynaecology, and found that
in the notes I inherited there was nothing about
sexuality or contraception. Visiting another
hospital, I was told by some of the nurses that
at school when they studied from Harry Messel’s
new science book, the pages on sexuality and
contraception had been removed.
An editorial in the MJA in 1973 commented on
the need to clarify the law regarding prescribing
the Pill for minors and estimated that one in
every two pregnancies was unwanted and that
one third of all women of reproductive age were
taking the Pill. At this time, a hundred articles on
the contraceptive Pill in two leading Melbourne
newspapers in 1970 had been biased five to
one against the Pill. The MJA editorial urged the
establishment of more Family Planning Centres
and better education of doctors.19
Teenage births peaked in 1971, and where the
bride and groom were both aged less than
nineteen, 80% of girls were already pregnant.
Data from South Australia, the only state which
recorded abortions, showed that by 1977 the
teenage birth rate had dropped by over a third
and the decline was related more to the
improved use of contraception which reduced
pregnancies than an increase in abortions which
reduced births.20
The Royal Commission on Human
Relationships, in its final report in 1977 urged
clarification regarding services for minors and
recommended that a doctor prescribing
contraceptives or performing an abortion on a
person aged 14 years and with the person’s
consent, should not incur criminal or civil liability
by the virtue of the absence of parental consent,
and that under age 14, the principles of maturity
should apply, in the best interest of the patient
and where it is impracticable to obtain
parental consent.21
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 27
In 1980, the Standing Committee of the
Attorneys General, requested the Law Reform
Association of Western Australia develop
recommendations for uniform Australian
legislation. Their guidelines were re-written
to cover WA only.22 The other states have
developed different guidelines, but basically
in line with the RCHR. This indicates that all
women, even minors, now have access to the
Pill and other hormone preparations, ie the Pill
as been democratised.
When Medicare was introduced in 1985,
the Hawke government announced that
minors from age 15 could apply for their
own Medicare card.
There are some difficulties arising. Newer versions
of the Pill are more expensive and have been
excluded from the Pharmaceutical Benefits
Scheme which may mean that young people
cannot afford them. Also Tony Abbott, as
Minister for Health in the Howard Government,
announced that his government was developing
legislation to give parents access to Health
Insurance Commission information about their
children and their Medicare records, irrespective
of whether they had their own Medicare cards.
He stated:
“Doctors ought to be pointing out that there
are risks to youthful sexual experimentation
and they really need to consider a bit of parental
guidance. As a society we ought not to be
sanctioning open slather sexual activity of
15-16 year olds”.23
Socio-demographic effects of the Pill
How has the introduction of the Pill changed our
society? The Pill has played a large part in the
demographic and social changes over the 50
years since it was developed. Australian women
were already effective in controlling births in the
1930s but the Pill brought advantages, safe and
almost 100% reliable contraception, available to
all women, and available on the PBS.
Where once it was thought that the Pill
would enable women to marry earlier and
postpone childbirth, now it has resulted in
postponing marriage as well. Australian
Bureau of Statistics (ABS) data show that
the total fertility rate (TFR) has declined
since 1971 from 2.95 births per woman to
1.81 in 2006, with a slight rise to 1.97 in
2008. The major reason for the decline has
been the shift in births to older women.
The teenage fertility rate in 1971 peaked at
55.5 per 1000 women and has declined with
slight variations to 17.3 per 1000 in 2008.
The highest fertility rate for 2008 was among
women aged 30-34 years and the median
age for births has risen from 25.4 years in
1971 to 32.6 years in 2008. These changes
have been due to better contraceptive use
rather than to any increase in abortions
especially if one considers that by postponing
births a woman faces a longer period of risk of
unplanned pregnancy.
These figures reflect the opportunities young
women have for completing university and other
training (particularly in medicine incidentally),
participating in the workforce before
childbearing and planning the timing of the
births so that they can continue careers after
childbearing. The large entry of women into
the workforce has played a major role in the
economy: a family without a working mother
is disadvantaged.
10. Schlink, Herbert. 1939. Textbook of Gynaecology
Angus and Robertson, Sydney.
Women have been able to participate more
widely in all areas of social activity even
though there is still much to be done,
especially as women are still paid less
than men and still occupy fewer high status
positions. So women have won the right to
determine their own fertility in developed
countries at least, but there are still
feminist battles ahead to ensure that the
gains are not undermined.
15. Full text available in Siedlecky and Wyndham
Populate and Perish. 1990. p171. Allen and Unwin.
References
1. Royal Commission on the Decline of the Birthrate
and the Mortality of Infants vol II; p386.
2. O’Sullivan, M.U. (1897) President’s address to the
British Medical Society, Victorian Branch.
Intercolonial Medical Journal of Australasia vol II
no 1, p11-21.
3. O’Sullivan, M.U. (1907) Presidential address to
the Medical Society of Victoria, Medical Journal
of Australasia Vol XII no 2, p57-74.
4. Peel, J Potts M. 1970. Cambridge University Press.
Textbook of Contraceptive Practice. p5-6.
5. Royal Commission on the Decline of the Birthrate
and the Mortality of Infants vol I; Conclusion; p52.
6. Davis, Geoffrey. 1974. Interception of Pregnancy.
Angus and Robinson,Sydney. Frontispiece.
7. Francis, Anne. 1962. A Guinea a Box. Hale, London:
opposite. p81.
8. Johnston, Marjorie. 1990 .Ansell: Portrait of
a Company. Maryborough. Vict. p8.
9. McLaughlin, Loretta. The Pill, John Rock
and the Church. Little, Brown and Co. Boston,
Toronto. p134.
11. Mayes, Bruce. 1950. A Textbook of Obstetrics
.Australasian Publishing Company, Sydney; p60.
12. Shearman, Rodney. 1967. Hormonal Steroids in
Fertility Regulation. WHO October.
13. Lamont, John.1976. Oral Contraceptives. The
Medical Journal of Australia Special Supplement.
2 October; p27.
14. NAGPA Forum. 1978. reported in AMA Gazette
13 April p40.
16. Whitlam, Gough.1985. The Whitlam Government
1972-75. Viking Penguin, Victoria; p19-21.
17. Sydney University Postgraduate Representative
Association. 1974; Sex.
18. Report AMA, Qld Branch, 1971:p2.
19. Editorial, 1973. Family Planning in Australia.
MJA vol 2 no 10, p4738 Sept.
20. Siedlecky, Stefania.1979.Trend to more, better
contraceptive use by young. Health; vol 29; p16-21.
21. Royal Commission on Human Relationships. 1977.
Final Report vol.3. p226-231.
22. Siedlecky, Stefania. 2005. Minors’Right to Privacy in
NSW. New Doctor 82; p15-19.
23. Phillip Hudson. New Push to Give Parents Right to
Know. Sunday Age. 4 April 2004
WHEN IT COMES TO CONTRACEPTION OUR THERAPIES
HAVE BEEN THERE SINCE THE BEGINNING
It is now half a century since the first
ever contraceptive pill was launched. It’s
maker, Searle, later became part of the
Pfizer family.
In the decades since, Pfizer has quietly
and steadily expanded its range of
contraceptives, and were pioneers in
bringing hormonal long-acting reversible
contraception to Australian women.
We are not only committed to providing
contraceptive options for women, but also
in providing therapy choices in the areas
of endometriosis, management of heavy
periods and period pain, vaginal infection,
hormone therapy and more.
Much has changed over the last 50
years, but the importance of providing
therapeutic choices in Women’s Health
hasn’t.
Pfizer Australia Pty Ltd (ABN 50 008 422 348)
38-42 Wharf Rd, West Ryde, NSW 2114
Pfizer Medical Information: 1800 675 229.
www.pfizer.com.au
WORKING TOGETHER FOR A HEALTHIER WORLD.
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 29
P e r son al reflect ions
“I rarely marry virgins anymore.
By the time they come to me they’re
almost always experienced, and their
usual motive for seeking me out is not
because they want morally sanctioned
sex, but because they want to settle
down and make babies.”
Chris Udy
Minister of the Uniting Church in Australia
I’m a minister of the Uniting Church in Australia
so, unlike the Roman Catholic Church, marriage
is not a sacrament for us; it’s not one of the two
community celebrations Jesus asked his
disciples to observe (Baptism and Communion)
– but wedding services figure prominently
among the high points of my work. The service
calls a man and a woman “to love each other
with respect, tenderness and delight”, and
describes the purpose of marriage as helping to
provide “the companionship and comfort (that)
enables the full expression of physical love
between husband and wife”. It says that
marriage partners “share the life of a home,
and may be entrusted with the gift and care of
children”. It also says that marriage is “founded
on God’s loving nature”, and a “reflect(ion) of
the love of Christ for his Church”. That’s an
interesting connection, given that Jesus (as far
as we know) never had sex, and had no
children. But more about that later.
The Pill began a double revolution. In the
public and secular sphere it set off exultant
and sometimes explosive celebrations of liberty.
Women especially were released from the
anxieties of unplanned and unwelcomed
pregnancy, and that increased control has had
repercussions, not only in personal sexual
confidence and freedom, but in family dynamics
and in the workplace. Most men seem to have
welcomed the change as beneficiaries and
enthusiastic partners, not only personally and
physically, but also in social and economic
collaboration. Some may still be grieving the
loss of clear, hierarchical gender roles, and
unfortunately some have conscripted religious
texts to promote and defend their reactionary
yearnings, but most of us have embraced the
flexibility and depth of egalitarian partnerships at
home, and many have discovered the balanced
richness of social and work environments where
both genders are represented.
The material I use to work with a couple
preparing for marriage, despite being developed
for use across the wide range of Christian
traditions – conservative and evangelical to
liberal and progressive – also assumes that
those who want to celebrate their wedding know
enough about each others’ bodies and sexual
response to identify possible problems and be
willing to raise them with a minister of religion.
Premarital conversations about sex are no longer
introductory, awkward and euphemistic, and
counselling a couple wanting to marry is as likely
to be about addressing problems of fertility as
encouraging a healthy sexuality.
In Christian communities the revolution is as
deep and as pervasive – but the response is
more ambivalent, and not always enthusiastic.
Official and authoritative Church statements still
assume that the proper expression of sexuality
will be in marriage. The accepted simple
scenario is that each person will have one
sexual partner in life, to whom we will come as
virgins, and with whom we will remain “til death
do us part”.
Page 30 | Ta k i n g i t – 5 0 y e a r s o f t h e p i l l
Death adds the first complication – especially
death that occurs while the survivor can still be
sexually active and fertile. No-one would want to
suggest that a young widow or widower should
not find someone else to love and marry – but
finding a second partner, especially if there are
children around, isn’t always easy. Divorce
complicates things further, and conservative
Christian communities deal with that by frowning
at it furiously, denying its moral validity and
punishing those they believe have succumbed
to weakness. Sex outside marriage, either
premarital or extra-marital, is simply prohibited.
In that simple moral scenario, the Pill – or any
effective contraception – has a minimal and
controversial place. It may have allowed for
planned pregnancies, but even that possibility
wasn’t always welcomed. Better, in some
minds, to allow God’s sovereignty full reign,
and allow God’s mysterious purpose to unfold.
Biblically, humanity’s first role in creation was
“to be fruitful and multiply; to fill the earth and
subdue it”. Human competition was, at first,
with nature – but when the primary threat to
survival changed, and began to come from
other humans, God’s purpose also apparently
changed. It wasn’t enough for humanity to
prosper, now it was God’s chosen people,
Abraham’s family, Israel’s clan and race, who
were to become as numerous as the stars are in
the sky. Then came the first century AD (or CE),
when Jesus and the early Christian movement
dislocated God’s purpose from any particular
race or culture, and took the question of survival
into philosophical and political spheres.
For a short time that movement expected the
world to end “any day now”, and having children
seemed a less appropriate response than
celibacy and abstinence – but as the centuries
passed and the world continued; as other
religious movements emerged or were
discovered, and as secularisation apparently
undermined any religious view of the world,
Christian survival seemed to require unfettered
fertility. God’s purpose wasn’t only that human
babies were required, or that babies of a
particular family or race would survive, but that
Christian babies would be born to populate and
inherit the earth.
In a competitive world it makes little sense to
limit your production. The Pill was a threat,
not only to the sovereign will of God, but also
to the vision of a world where Christian values,
Christian influence and Christian institutions
held sway. Even more, it suggested that the
“holy struggle”, the life-long battle with sex that
surrounded celibate religious vocations with a
sacrificial aura, no longer needed waging.
The Pill effectively separated sex from making
babies. It forced us to re-examine sexuality and
gender, and profoundly affected by that radical
rethinking is family, community, society – and
the earth.
The Pill requires us to ask: if sex is not only for
making babies, then what is it for?
Obviously, for pleasure. Sex removed from
procreation – from reproduction, the replication
of genes and species survival – is, even so,
exciting, enjoyable, absorbing, delightful,
overwhelming. Sex is fundamentally pleasurable
– for many, the essence and definition of
pleasure. The brainstorm that is orgasm is a
primary desire. We’re made for it; hard-wired for
it, and it is powerfully attractive. But the pleasure
of sex doesn’t come on its own. It comes with
and through connections: images, sensations,
ideas – relationships, roles. And it’s in those
connections that the deeper ethical issues
of sex emerge.
Thankfully, since the Pill arrived, the
pleasure of sex has had more positive
press, not only in the public and secular
sphere, but also in religious communities.
Some have long traditions of sensual
affirmation – like Jewish Rabbis who taught
that Sabbath celebrations were incomplete
without wives and husbands making love.
Others have only recently overcome their
ambivalence on sexuality, adopting
statements that recognised that sex
is good for more than procreation.
In Christian theological conversations
the first and clearest affirmation of sexual
pleasure came in December 1930, when
Pope Pius XI promulgated an encyclical
entitled Casti Connubii “Of Chastity in
Marriage”. There, in addition (and
subordinate) to procreation, sex in
marriage was officially acknowledged
as having a unitive purpose and validity
“mutual aid, the cultivating of mutual
love, and the quieting of concupiscence”.
It recognised that sex can help to create,
express, reinforce and heal the connections
between husband and wife. Sex between
anyone other than a husband and a wife
was forcefully forbidden, as was sex with
any suggestion of violence or compulsion,
but the power of sex in attraction and
attachment was, for the first time, affirmed.
Unfortunately the primary purpose of Casti
Connubii was to establish an anti-contraception
position for the Roman Catholic Church, one
that was further entrenched with the
promulgation of Humanae Vitae “Of Human
Life” a few years after the Pill was first made
available. Humanae Vitae is subtitled “On the
regulation of birth”, and appeared in July 1968.
Positively, it reaffirmed and strengthened the
unitive purpose of sex, giving its pleasure and
expression of intimacy equal recognition with
the purpose of making babies. Less helpfully,
it maintained a firm rejection of all contraception
as artificial intervention into the natural order,
a position consistently maintained ever since.
In its manual for Confessors in the Roman
Catholic Church, the Pontifical Council for the
Family says: “The Church has always taught the
intrinsic evil of contraception, that is, of every
marital act intentionally rendered unfruitful.
This teaching is to be held as definitive and
irreformable. Contraception is gravely opposed
to marital chastity; it is contrary to the good of
the transmission of life (the procreative aspect
of matrimony), and to the reciprocal self-giving
of the spouses (the unitive aspect of matrimony);
it harms true love and denies the sovereign role
of God in the transmission of human life.”
This is not an occasion for sectarian polemic,
but that certainly wasn’t and isn’t the last word
in the ethical conversation on contraception.
Deep divisions remain between the official
Catholic statements and those of protestant
and orthodox theologians and ethicists.
The conversation within the Roman Catholic
Church is also lively, and began almost
immediately after Humanae Vitae appeared,
with the Canadian Conference of Catholic
Bishops releasing a statement within months,
appealing for the primacy of conscience in
decisions on contraception, and arguing that
Humanae Vitae would drive a wedge between
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 31
the moral teaching of the Church and the
pragmatic decisions of many Catholic women.
Sadly, that has been the result, and recent
opposition from Rome to the use of condoms
even in the face of HIV/AIDS has deepened
the divide.
Ironically, an inflexible determination to maintain
the connection between the possibility of
reproduction and the experience of sexual
pleasure has seriously compromised the
connection between sexual activity and ethical
conversation. Stalling that conversation in an
argument about contraception misses the
bigger picture. Sex is more than mechanical.
It’s about images, sensations, ideas – roles and
relationships – and the cliché remains true: the
most powerful sexual organ is the brain.
The brain needs to be engaged for sex to be
good, and the role of the brain is neither passive
nor constrained. It’s the brain that processes
visual information, tactile information, information
about role and relationship, risk and responsibility
– and turns on or turns off our sexual response.
It constructs scenarios, populates fantasies,
generates strategies of arousal and seduction.
It’s aware of power, adept at creating and
interpreting symbols, able to focus themes of
global consciousness and cosmic significance
into an act of personal expression and
interaction. When we make love “the earth
moves”. The deeper we move into intimacy,
the more clearly we reflect “the image of God”.
And if the brain is so creatively and profoundly
involved in these unitive, relational aspects of
sexuality, why shouldn’t it be as helpfully
engaged in the procreative and physical?
Human brains now understand the chemical
and hormonal rhythms and cycles that influence
fertility. Creativity in technology gives us the
means to regulate and assist fertility. We are
no longer naïve about where babies come from,
or about their impact on the world. Choosing to
have children, and planning when to have them,
is no longer just a personal decision – or even
a decision that impacts only on a couple or a
family. Family planning will inevitably be affected
by community, national and global issues,
events and conditions, and our societies at
every level are affected by where and when
children are being born. We can no longer
“leave it to God” to produce the supply of
babies at the rate and in the places where they
will best be cared for, and are most needed.
We are now aware of the world’s limitations;
we understand the pressures and stresses
population levies on resources and ecosystems.
We are now powerful and responsible agents,
architects of our future, co-creators and
collaborators with God.
It’s at the global resolution that these issues
are most clear. Around the world there’s a very
strong correlation between poverty, political
instability, and the inaccessibility of family
planning and contraception. It’s in sub-Saharan
Africa, Latin America and the Caribbean,
where nearly one in four women say they would
like to delay or avoid having children, but can’t
access or don’t use contraceptives, that poverty
(people living on less than US$1.25 a day)
remains endemic. It’s also in those areas where
rates of adolescent pregnancy are highest,
leading to missed opportunities for education
and the likelihood that more children will be born
than can be cared for. The UN’s Millennium
Development Goals, formulated by world
leaders in 2000 to be achieved by 2015,
are reported as being significantly undermined
by the lack of family planning. Death during
pregnancy and childbirth in the developing
world remains static at 500,000 each year;
one quarter of all children in developing
countries are underweight and undernourished;
only 18 of 113 countries identified in 2005 as
failing to achieve gender parity in both primary
and secondary schools will achieve the
goal by 2015. The vicious cycle that traps
households in poverty is triggered and
accelerated by early and unwanted pregnancy,
and a crucial key to liberty and development is
family planning education and the availability of
reliable contraception.
Nor are those problems confined to the
developing world. We now know that the
earth is an ecosystem where pressures at
one point build to explosions at another.
Unplanned growth in population can only
exacerbate the uncertainties posed by peak
oil, global warming, financial interconnectedness,
unchecked pollution, competition for clean
water and finite mineral resources. The earth
is well and truly “subdued”, and humanity has
“filled” it – if not with bodies, then with their
detritus. The effects of over-population, or of
inappropriate population, can’t be contained.
They will influence and complicate the lives of
Christian, Jewish, Muslim, Hindu, atheist and
agnostic babies and families every bit as much
as they do any other.
Sex is procreative, and issues of family
planning need to be considered with
intelligence and compassion. Contraception
and the Pill will necessarily play a part in that.
Sex is also unitive. It builds connections
between partners. It establishes relationships
– even if only for a very short time.
In the developed world, for a short
time, it looked like the Pill and other
contraception might separate sex from
procreation, leaving us free to enjoy the
pleasure of sex without complication.
But pleasure is relational, and there are
indications that our relationships are not
as healthy as we might wish them to be.
The early sexualisation of girls; anecdotal
reports of increased pressure on young
women for casual sex; the continuing
incidence of sexually transmitted diseases
and HIV/AIDS; declining fertility and an
increasing reliance on IVF technology for
couples “who’ve left it too late”; family
instability and an unsustainable “work/life
balance” – these are trends that suggest
we need further reflection on the powerful
effects of sexual pleasure in the way we
form identity, family and community.
Withholding contraceptive protection
and control is no solution, but nor can we
conclude our ethical conversation at the
point of providing condoms and the Pill.
We are no longer “virgins”, naïve and innocent
about the effects of our sexual behaviour.
We’ve “eaten from the tree of knowledge”
– we are experienced, aware, able to see
the implications of our actions, not only for
ourselves, but for our partners, our families,
our communities and the world. The Pill has
been and continues to be a powerful tool for
the regulation of our fertility, but life is more
than fertility. Contemporary Christian theology
focuses on God as Trinity – as essentially and
fundamentally relational – and says our purpose
and hope is to reflect the nature of God in the
way we live. It’s up to us to use our intelligence,
experience, creativity, and compassion as we
care for the planet and for each other; to build
communities of justice and peace, and “to
love each other with respect, tenderness
and delight”.
Page 32 | Ta k i n g i t – 5 0 y e a r s o f t h e p i l l
T h e Pill and I – A perso n a l a n d po l i ti ca l re f l e c t i o n
“It was in March 1964 that I swallowed my first
oral contraceptive pill thoughtfully provided by
a friend. I was 22 yrs old, in love and had already
survived one unplanned pregnancy. The idea that
I could be in charge of my own fertility by taking
a pill which provided total protection against
pregnancy and was not related to the sexual
moment was breathtaking.”
Wendy McCarthy AO
Company Director
Social Commentator and Mentor
Better still, it was medically endorsed and
therefore could be assumed to be safe.
After all it was the sixties and no one questioned
doctors. Our trust in the medical profession was
absolute and the risks seemed minimal. The risk
of an unplanned pregnancy was far greater for
most young women. Access to abortion was
secretive and limited, and the procedure was
often dangerous. Women still died from
backyard abortions. Becoming a single mother
or having to adopt a child out meant private
anguish and public loss of reputation.
I duly presented myself to the recommended
Gynecologist who advised I begin a course of
Anovlar a week before our wedding and dated
the prescription accordingly. He said he would
not do a pelvic examination as I was a virgin and
warned me of the inferior National Health
Service in the UK. If consequences in terms of
side effects were discussed I did not hear. I had
no idea how to raise the issue of my abortion or
my immediate contraceptive needs. How could
I admit to being sexually active? I could not wait
to exit the appointment.
I was lucky that when faced with an
unintended pregnancy, I had a committed
partner who had a pharmacist friend who
recommended a safe abortion clinic and as
two professional people we could afford the fee
(63 guineas). On reflection it is extraordinary that
despite its expensive fees no one recommended
I use birth control when I was discharged.
Instead I was encouraged to think of myself as
victim of a man’s sexual needs and was advised
to not let him have his way with me again.
There was no acknowledgement of an equal
relationship and my own sexual feelings. I was
incapable of expressing my needs and views
and happy to no longer be pregnant.
When I related the experience to my friend she
devised the perfect solution. She would lose her
script and ask her doctor for another and I could
take her existing six months supply. By then
I would be a married woman and entitled to
proper service and choices. In the interim the
plan worked and without the benefits of either
medical advice or physical examination I began
my life with the Pill. I loved this pill for the life
choices it gave me.
The Pill was a recurring topic of conversation
with my peer group who were marrying and a
newly married friend told me she was taking
the Pill and suggested I make a premarital
appointment so I could start using it. It seems
extraordinary to recall that at this time only
married women were prescribed it.
In retrospect I know that the early dosages
were high but that meant nothing at the time
for I had no benchmarks and I relied on medical
advice. I wanted safe and reliable contraception
and a sexual life. For me it was never about a
lack of desire for children. I wanted to be a
mother. Terminating the pregnancy was about
timing; I was not ready to be a parent. I loved
my teaching career and motherhood would
end that as the women in my staff room
demonstrated daily.
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 33
For married women the career options were
single and permanent, or married/parent
and casual.
After completing three years of teaching
I married and left to work in the UK and
the USA. It was not our intention to have
children until we returned and I would be
reliant on the Pill. Despite the warnings of
the Sydney doctor, I enrolled in the British
National Health Service to find it was
efficient in family planning matters.
My new GP said he did not really want to
waste his time with contraception as the
Family Planning Association was much
better and I was directed to the Family
Planning clinic in Notting Hill. How I loved
that it all seemed so normal and you were
praised for being responsible just for being
there. I felt empowered and liberated and
for two years was a regular client and a
happy pill consumer. It was also the
beginning of my long relationship with
the Family Planning Association whose
advice I trusted.
Access to contraceptive services was not
so easy in the US medical system and I was
grateful to have supplies with me. Turning
homewards and looking forward to being
pregnant it came as an extraordinary surprise
to find that I was not as fertile as I imagined.
I did not conceive in the first three months
after I stopped taking the Pill and privately
assumed this was related to my still private
abortion as I had not revealed this in any
medical consultation. The Pittsburgh
gynecologist commented that this was a
common side effect and if after returning to
Australia I was not pregnant I should apply
to adopt a child. I was 26.
Such drastic action was not required as within
six months I was pregnant and back in Australia.
Encouraged by my obstetrician in my desire to
have a drug free birth I joined the Childbirth
Education Association and began a political
life around choices in childbirth, abortion,
sex education and feminism. Three years
away from Australia helped me see other lives
and especially the choices women made.
Glad as I was to be back home, I was a very
different person.
What was private became political and public.
The abortion was no longer a matter of private
shame but a public statement and with others
advertised in a national newspaper inviting
police to arrest us for our illegal activity.
They did not respond and we were encouraged
to be braver. We marched for safe reliable
contraception and the right to choose whether or
not to be parents; for equal pay and education.
The Pill was no longer my private method of
contraception but rather as a method which
should be available to all women.
I became one of the NSW convenors of the
newly formed Women’s Electoral Lobby (WEL)
and part of the takeover campaign for the
Family Planning Association. No longer just a
private consumer with WEL, I campaigned for
the removal of the luxury tax on the Pill so that
it was available to more women. We read the
newest literature from the US and dreamed and
planned to ensure that women had more
choices. Our Bodies Ourselves from the Boston
Women’s Health Collective forced us to consider
health in a broader context. However even as I
read this and campaigned for access and
information for all, I stuck with the Pill.
I accepted the contemporary advice on two
year child spacing and like most of my peers
I resumed taking the Pill despite the unpredicted
consequence of losing my milk. I needed
certainty so that I could return to work and
manage an activist community life.
Three children later it was time to think of
contraception for the rest of my fertile years.
I had pill fatigue. I could not imagine taking a daily
tablet for another 20 years. The Pill had fulfilled
its promise and I decided on tubal ligation.
I was lucky to have my private reproductive
decision making informed and supported by my
professional life. As a feminist passionate about
family planning and education in late 1975 I left
my teaching career to pursue those passions
and became the Education, Media and
Information Officer for Family Planning NSW.
It was a heady time. I taught sex education
and family planning/personal development in
schools, community settings and universities
for a nearly a decade. I wrote the Cleo magazine
sex advice column and became the conduit
between its readers and the family planning
association. These conversations were nearly
always about the Pill.
The Pill was the contraceptive of choice for
Australian women and the public discourse
around contraception reflected this. Teenagers
wrote asking for information and the names of
doctors who would “put them on the Pill”.
Communities wrote saying their local doctors
would not prescribe the Pill and how could they
acquire a Family Planning clinic. This was a far
cry from the 60s.
From 1978 to 1983 I was Executive Director
of the national family planning body AFFPA.
Simultaneously I was a member of the National
Women’s Advisory Council advising the then
Prime Minister Malcolm Fraser on women’s
affairs, an appointment influenced significantly
by my Family Planning role. AFFPA was the
Australian member of the International Planned
Parenthood Federation and was regional and
global in outlook. It had been the lead agency
in family planning becoming a Human Right and
was tenacious in its advocacy for the rights of
women and families in the developing world.
This remains unfinished business.
Today despite some recent improvement
maternal mortality is the leading cause of
death among young women aged 15 to 19
in the developing world. For the last thirteen
years I have been a director of Plan International
– a child rights agency – and worked in over
thirty countries where access to family
planning education or clinical services is
inadequate. When I see the burden of
unplanned pregnancies, the under nourished
babies I compare with my healthy grandchildren
I am impatient with the rate of change.
Why is the pill, 50 years on yet to reach parts of
Africa and India? Why should these women be
denied a proven method of contraception when
we know that condoms and other forms of birth
control and AIDS prevention are still far too
difficult to obtain in many areas?
Without access to contraception there is no
gender equality and without gender equality
none of the 8 Millennium Development Goals
will be achieved. Millennium Development
Goal 5 – Improve maternal health has as its
target to reduce by three-quarters by 2015 the
maternal mortality rate. Currently it is the least
likely to be achieved.
Page 34 | Ta k i n g i t – 5 0 y e a r s o f t h e p i l l
America’s widely respected Guttmacher
Institute, which conducts research on
reproductive health, says that 215 million
women around the world are sexually active
and don’t want to become pregnant – but
are not using modern forms of contraception.
If contraception were broadly available in poor
countries, the report said, more than 50 million
unwanted pregnancies could be averted
annually. One result would be 25 million fewer
abortions per year. Another would be saving
the lives of as many as 150,000 women who
now die annually in childbirth.
Australia’s newest Companion of the Order
of Australia Dame Valerie Beral, a Professor
of Epidemiology at Oxford University, was
honoured for her work in breast cancer.
In her longitudinal study of breast cancer,
First ladies of the Pill – circa 1980.
Professor Beral found that the Pill offered
protection against ovarian cancer. She stated
“The Pill when it is being taken does have some
adverse effects on blood clots and breast
cancer. But for women taking the Pill in their
20s and 30s these are small effects, and
when they stop taking it the protection against
ovarian cancer goes on for the rest of their life.
The net effect is good.” (Sydney Morning Herald
interview June 14, 2010)
This should be good news for young women
across the world. However being a teenager
in a developing country means a new host of
challenges for girls. Over 80 million girls will be
married before their eighteenth birthday and
they may just keep on producing babies.
The Pill is not available for them.
Margaret Sanger, American social reformer
and founder of the birth control movement,
said in 1883 “No woman can call herself free
who does not own and control her own body.
No woman can call herself free until she can
choose consciously whether or not she will be
a mother”. The words are as true now as they
were then.
She could never have imagined the freedom
resulting from the invention of the Pill which
has enabled us to be both mothers and
workers. It is a choice which the rest of the
women in the world deserve.
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 35
5 0 y ear s of taking it
“Australia’s first female Prime Minister – Julia Gillard, is 48 years old and the Pill is 50.
Are these two facts related? You bet they are!”
Jane Caro
Co-author (with Catherine Fox) of “The F Word:
How we Learned to Swear by Feminism”
and author, broadcaster and advertising writer
While the slow (sometimes painfully slow) march
towards full and equal rights for women has
been in progress for over 300 years, it has
really gathered pace and momentum only in the
last half century. And there is one fundamental
reason for this; the modern ability women have
to control their fertility and separate sexual
intercourse from having children, in other words,
the invention of an effective, easy to use female
contraceptive pill. So important was its advent
for half the world’s population that, no matter
how many millions of different types of pills there
are this is the only one to almost instantly earn
the right to have the word “the” in front of the
word “Pill”. Given my 30 years writing ads for all
sorts of brands (some of them were even pills)
I can tell you this is the Holy Grail in productland.
Apted then filmed the fourteen every seven
years. The latest film is 49Up and 56Up is due
out soon. But when Apted chose the original
fourteen he only chose four girls. Why? Because
in 1963, while it was assumed boys would go on
to have varied and interesting lives, it was also
assumed girls would simply become wives and
mothers – and nothing else – just as they had for
millennia. The Pill was only three years old, back
then, and its profound impact on the shape of
women’s lives had not yet become apparent.
When PM Gillard was born, few women
continued to pursue careers after marriage
and motherhood, girls education was often
neglected because they were seen as
automatically growing up to become wives
and mothers. And their status and success
were defined by their relationship to a man.
If you don’t believe me, may I recommend
you check out the following?
But can the rise in the status and opportunities
of women, possibly the most important change
in the human condition since the invention of
fire, really be the product of just one small pill?
First, the brilliant and ground-breaking 7Up series
by Michael Apted. As a young TV doco producer,
Apted took on the assignment for the TV show
Panorama to choose and film fourteen British
seven year olds from different backgrounds to
explore the Jesuit adage “give me a boy until he
is seven and I will show you the man”.
Second; there is the remarkable AMC drama
series “Madmen”. If you want to know what it
was like to be a woman in the early years of the
60s, watch it and weep with relief that you were
born a little later in the century.
Yes, but there is more to it than that.
Advertising practitioners – whose stuff in trade
is changing behaviour – are becoming well
aware of just how such fundamental change
tends to take place.
The most cited example is community and
government attempts to discourage motorists
from drinking and driving. For decades, various
concerned groups – including State and Federal
Governments – spent many millions of dollars
running communication and advertising
campaigns designed to change attitudes
to drinking and driving.
Page 36 | Ta k i n g i t – 5 0 y e a r s o f t h e p i l l
They then tested those campaigns in focus
groups. And, over many decades, discovered
that they had, indeed, succeeded in changing
attitudes to being pissed behind the wheel.
Virtually unanimously, when drivers were asked
by market researchers whether they should
drink and drive, they all agreed they should not.
However, when they were asked whether they
did drink and drive, most agreed that indeed
they did, despite the fact they knew it was
wrong. The communication campaigns had
changed attitudes alright, but not behaviour.
Drivers only stopped drinking and driving in any
great numbers, with the introduction of random
breath testing. Something other than simply
attitudes had to change before people’s actions
matched their beliefs.
So perhaps we should just have brought
random breath testing in straight away and
saved – not just millions of dollars – but many
lives. Trouble is, without the precursor of the
changed attitudes, governments would probably
never have had community permission to bring
in random breath testing, so it is likely that for
really revolutionary, long-lasting behaviour
change there needs to be a considerable
investment in changing attitudes before it is
possible to institute the physical changes that
will drive behaviour.
We could mount the same argument in terms
of the progress of women. The 300 years since
Mary Wollstonecraft, inspired by the Enlightenment
and the French Revolution, penned “A Vindication
of the Rights of Woman”, included many feminist
figures who fought tremendous odds to break
through centuries old barriers to women’s
educational, occupational, economic and political
opportunities. Laws changed over that time.
Women gained the right to an education, to
their own children, to their own earnings and
inheritance and, eventually, the right to vote,
but most women continued to live much as
women had always done.
However, the trailblazers had begun to change
attitudes. By the time women gained the right to
vote, in most western countries fairly early in the
20th Century, there were many more people
willing to recognise that women were fully human
and entitled to human rights. In the west, at least,
few objected to girls going to school, or to single
women earning a living. The furore over the vote,
so vicious on both sides at the time, died away
almost as soon as the vote was granted.
Attitudes had changed, but just as with drink
driving, behaviour hadn’t kept pace. When a
woman married and had children, she lost
her autonomy.
Then, came the Pill and what is now often
referred to as the second wave of feminism.
I believe that the Pill worked for women and
their rights in the same way as random breath
testing worked to curtail drink driving. It was
only possible to sell such a contraceptive on the
open market because attitudes to women, and,
indeed, to sex, had already changed. It was
already unacceptable to try to control the
freedom of women in ways that had been quite
unremarkable in the past. And once women
could uncouple their sexuality from their fertility
the major barrier to their autonomy had been
toppled. Simone de Beauvoir famously defined
civilization as the distance we can place
between ourselves and our shit, and that
women have traditionally been seen as
inherently less civilized because we remained
out of control of our bodies and our biology.
More like animals, in other words, ruled by
instinct rather than intellect. The Pill, bless its
little hormonal heart, changed all that.
It is also important to remember that separating
sex from reproduction freed women from more
than merely the drudgery and lack of control of
constant child-bearing and rearing. Childbirth,
until relatively recently, was uniquely dangerous
and difficult for human females because of the
disproportionate size of the infant’s head.
There is a reason there are so many
stepmothers in fairy tales, it is because so many
women died agonizing deaths in childbirth. In
14th Century England, for example, men had a
life expectancy of about fifty and women just
thirty. For most of human history sexual
intercourse could have devastating
consequences for women. And, thanks to the
concept of conjugal rights, for most of that time
women also had no legal right to refuse their
husband sex. Marriage, in effect, was a kind of
legal prostitution.
The terrifying consequences of sexual
intercourse for women remain a reality for many
women in the third world. We occasionally hear
dry statistics about maternal mortality in
developing countries and watch documentaries
about noble doctors treating fistulas and forget
that – not so long ago – that was the reality for
our female ancestors, as well.
Medical science and hygiene have both played
a vital part in making childbirth much safer, but
the ability of women to space their family and
maintain their health and energy should not be
underestimated. It has saved lives as well as
marriages and relationships. At the turn of the
last century, a paleobotanist and a doctor of
both science and philosophy, Marie Stopes,
was horrified to discover that despite her
education she knew nothing about sexual
intercourse. She only found out about it when
she sought reasons for her infertility. Such was
her outrage she wrote a famous and scandalous
book called “Married Love” to help both men
and women understand their own bodies.
The mail she received in response (you can read
much of it in “Dear Dr. Stopes. Sex in the 1920’s.”
by Ruth Hall, 1982, Penguin) is heartbreaking.
People were desperate for contraceptive advice,
something that was illegal at the time. Women
wrote of being warned by their doctor that they
would die if they had more children, but being
given no advice on how to avoid pregnancy other
than to rely on the goodwill and self control of
their husband. Men wrote of their frustrated love
for their wife and their fear of causing her
permanent damage or even death. Stopes
became a crusading pioneer for contraception,
how she would have loved and applauded the
Pill. And Stopes – and many like her – must also
be given credit for helping to change attitudes and
create the climate where such an invention could
be contemplated and made widely available.
The ability of women to control their fertility has
also led to smaller families and all the economic,
emotional benefits that followed. Wanted, loved,
well-fed and cared for children with parents who
have (just) enough energy to pay attention to
them are the norm now, they weren’t once.
Fan of it that I am, the Pill is no magic bullet.
Human suffering and difficulty remain, and
women still have far to go before we enjoy
full and equal status with men, but whenever
anyone asks me what I think the most
important inventions of the 20th century have
been, I don’t think of the internal combustion
engine or nuclear fusion. I silently toss up
between the tampon and the Pill. I really
can’t imagine what my life would have
been like without either of them, can you?
And, whether she would give them credit or
not, they have made Julia Gillard’s path to
the Prime Ministership much easier than it
otherwise would have been.
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 37
H ow Th e Pill changed m y l i f e – R e f l e c ti o n s o f a G e n X t e e n a g e r
“I think we all understood going on the Pill to
be a rite of passage. It was a departure from
childhood and enabled you to have a safe and
enjoyable sex life. The only problem was that we
romanticised this transition, assuming we would
know when the right time was to embark upon
our new grown up status. Prince Charming aka
Patrick Swayze or Rob Lowe would sweep into
our lives to the sound of trumpets and we would
be in love.”
On 10 February 2006 I was in Australia’s
Parliament House fighting for access to a Pill.
It was not the Pill but RU486, or mifepristone,
and my journey to that day campaigning for
more reproductive choices for Australian
women possibly started 20 years earlier when
I mismanaged my own contraception and did
not take the Pill.
I am Gen X and was a teenager in the early
1980s. The Bay City Rollers had been replaced
by new romantics Duran Duran and the global
force of Madonna soon transformed us all into
hilarious looking urchins wearing pointy shoes,
tube skirts, off the shoulder t-shirts, teased
fringes and fluorescent socks and gloves. I grew
up in a leafy suburb on the lower north shore of
Sydney and attended a girl’s high school. I was
an average student with working parents and
life was full of sport, school, girlfriends and
weekends in the country – fairly uncomplicated.
By 1984 aged sixteen we spent many Saturday
nights pacing Oxford Street trying to get into
clubs – very unsuccessfully. Most nights we
were happy with a hot chocolate in a cafe
nearby with our other under aged mates and
the odd cigarette gave us all a thrill.
Sophie McCarthy
General Manager
McCarthy Mentoring
We’d all read Puberty Blues but our lives had
little similarity. Despite the fact that I was raised
by a working mother, feminist, who taught sex
education, wrote books on sex and was the
Cleo adviser, our sex lives were non-existent.
In Year 10 the Pill was for fast girls but by Year
12 it was becoming a sensible option. The Pill
was discussed among my friends and some
mothers had taken their daughters to the GP
for their script, “just to be careful” or to fix mild
acne. This was a more palatable explanation.
I think we all understood going on the Pill to be
a rite of passage. It was a departure from
childhood and enabled you to have a safe and
enjoyable sex life. The only problem was that we
romanticised this transition, assuming we would
know when the right time was to embark upon
our new grown up status. Prince Charming aka
Patrick Swayze or Rob Lowe would sweep into
our lives to the sound of trumpets and we would
be in love.
As a result of naivety, denial and misguided
notions of romance I received my first script for
the Pill at Preterm after the termination of an
unplanned pregnancy aged eighteen. It was my
first real boyfriend, my first sexual experience
and despite education, knowledge and
information about family planning services
and the Pill, I somehow lacked the maturity or
wherewithal to take myself to a clinic and get a
script. The boyfriend wasn’t much help either.
That experience changed my life.
Page 38 | Ta k i n g i t – 5 0 y e a r s o f t h e p i l l
Three years later I was working as a receptionist
at the family planning clinic in Canberra and did
my political science thesis at ANU on the
politics of abortion. After finishing my degree
I travelled to South America and felt shocked
and ashamed at the role of women in poor
countries dominated by the Catholic Church
and autocratic governments. Poverty, religion
and culture seemed to conspire against women
and offered them very few choices in life.
Through my young eyes it seemed women
worked in the fields, markets, shops and
streets while looking after children and the men
sat around smoking and drinking coffee. I saw
great poverty, desperation and hopelessness
in Bolivia and Peru where bad situations were
compounded by martial law and the growth
of terrorist groups.
The lives of so many women and their families
could be different if they had access to the Pill
and were able to manage the size of their
families and reduce their chances of dying in
labour. Today millions of women around the
world still die from complications in pregnancy,
labour and unsafe abortions. It is one of the
greatest killers in the modern world and
significantly preventable. Despite poor
communities around the world having
access to mobile phones and microfinance,
contraception in some form is still illegal,
too expensive, against god’s wishes or a
combination of all three.
Around the world women’s access to
contraception has and continues to be
determined by dominant social, religious
and political forces, such as the Vatican.
Medical wonders remain only that unless
they are sanctioned legally, politically
and economically.
It is perhaps a measure of Australia’s
success in managing this debate that
today most young women don’t consider
the battles that preceded the Pill’s
availability. As they pop that pill into
their mouths they are given choices their
grandmother’s would have killed for and
that millions of women around the world
today in 2010 still can only dream about.
Throughout my 20s I went on to work as
a researcher in public health and then for an
overseas aid and development organisation.
In 2000 when I was pregnant with my first
child I was approached to join the Board of the
NSW Family Planning Association Foundation.
This body was responsible for raising funds
for sexual and reproductive health projects
and allocating the funds responsibly to
research, infrastructure, health promotion
and education projects.
One of the highlights of that experience
was organising an event to celebrate the
80th anniversary of Family Planning NSW in
2006. Almost 200 people came together at
Women’s College at the University of Sydney.
The panel included my mother who had been
a sex educator with FPA NSW and Executive
Director of the Australian Federation of Family
Planning Associations in the 1970s-80s,
columnist and former CLEO Editor Mia
Freedman and Dr Edith Weisberg.
The key note speech was given by former
Australian Prime Minister Gough Whitlam whose
government on its third day in office removed the
sales tax on oral contraceptives in December
1972. This act and many other changes that his
Government introduced such as maternity leave,
child care, community health centres, free tertiary
education, equal pay for women, appointing
women to leadership roles in the judiciary,
government and public service, brought about
huge change for Australian society and yet is not
widely known amongst my generation. Lifting the
tax on the Pill was a milestone for Australian
women, family planning services and in Australian
politics and it was a personal privilege to help
organise a celebration to thank the many people
who had made it happen.
In 2010 the Pill is 50 years old. Today young
Australian women have many opportunities and
still have the blessed advantage that being born in
a wealthy country like Australia affords. Women
have access to education, the vote, freedom of
expression, access to high quality contraception
and sexual health information. These are human
rights and have been achieved through years of
social and political debate, protest and
negotiation.We saw another milestone for
Australian women as our first woman Prime
Minister Julia Gillard was sworn in by our first
female Governor General, Quentin Bryce.
In the world’s poorest countries particularly
sub-Saharan Africa there is very little access
to contraception and reproductive health
services and the low standard of living reflects
this. All the research shows that contraceptive
use promotes economic development and that
an investment in this area saves millions of
women’s lives and millions of dollars on services
for growing populations.
Access to contraception is fundamental to
achieving the Millennium Development Goals
however one in every 10 women – 137 million
– still had an unmet need for contraception
(Guttmacher 2008).
As a former client, employee and now donor
of a scholarship for nurses in sexual and
reproductive health working with Aboriginal
communities in remote NSW I have a personal
connection and gratitude to family planning
services in this country. It has been a part of my
life since I toiled in my mother’s office as a kid.
Indeed sexual and reproductive health is a part
of every woman’s story. I am delighted that
taking the Pill is no longer a clandestine act in
Australia, but a sign of a woman’s independence
and responsibility. It is my hope that it won’t be
another 50 years until this can be the experience
for all women around the world.
Since
1961 to 2011
& beyond...
Bayer Schering Pharma is proud to support Family
Planning NSW in commemorating 50 years of the
availability of the oral contraceptive pill in Australia.
It was Schering AG, now part of Bayer Schering Pharma that
brought the first pill to Australia, this was Anovlar in February 1961.
Since this time the company has been at the forefront
of innovation in hormonal contraception. Firsts include:
• the progressive lowering of dosage
• new advances in packaging and presentation
• new progestogens offering the addition of
non contraceptive benefits
It all started with Anovlar!
Our commitment...
Women’s health and particularly contraception remain a strategic
focus of the company’s research and development. In this regard
Australian prescribers and patients can be assured of continuing
availability of state of the art products and support.
Note: Anovlar (ethinyloestradiol / norethisterone
acetate) was launched in Australia 50 years
ago and is now no longer available globally.
Bayer Australia Limited. ABN 22 000 138 714, 875 Pacific Highway, Pymble, NSW 2073.
BA615 The Pill Mag Ad v2.indd 1
6/9/10 5:16:33 PM
Front Page of the Daily Telegraph, February 10, 2006.
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 41
T h e r e’ s a long way to g o …
“But while we should acknowledge this significant
milestone, it is important that young women
continue to fight to expand and consolidate our
reproductive rights. While it is hard for women
my age and younger to even imagine what it
was like to live in the pre-Pill, backyard-abortion
era of the fifties, we cannot become complacent
about our reproductive rights now.”
Nina Funnell
Researcher in the Journalism and Media Research Centre
University of NSW and a regular media commentator
I recently attended an exhibition about female
criminals titled “Femme Fatale”. The exhibition
was spread over two rooms housed at Sydney’s
Justice and Police Museum. The first room
charted the history of deviant females starting
– predictably – with that evil biblical temptress
“Eve”. The vain, sexually rapacious Queen from
Snow White and the Seven Dwarfs also got a
mention as did the female sex workers who
patrol Kings Cross each night.
My friend and I sniggered contemptuously at
the way the exhibition so transparently paralleled
and equated female sexuality with female
deviancy. After all, this was supposed to be an
exhibition about crime and yet there was barely
any analysis of how social factors such as
education, literacy, class and poverty impact
on rates of female criminality.
But when we got to the second room we
stopped dead in our tracks. There was a
disclaimer outside the room advising visitors
that the contents of the room may be disturbing.
There was also an explanation that the entire
room was devoted to the issue of abortion
because abortion is the one crime that
Australian women are most frequently involved
in and it is one of the only crimes that always
involves a woman.
And then the penny dropped. This exhibition
was not simply equating female sexuality with
female deviancy; it was documenting and
exposing the ways in which our current culture
and laws already do.
My friend and I walked silently through the
second room, reflecting soberly on the fact
that Australian women still do not have
complete rights over our own bodies.
As a young woman it is easy to fall into the trap
of assuming that women’s reproductive rights
have been secured and that these rights are
not at risk or being eroded by right wing,
conservative idealogues. On both counts we
would be wrong.
Last year, a nineteen year old woman and
her boyfriend were charged with procuring
an abortion. If they are found guilty under
Queensland law they face seven years jail
time. Meanwhile, QLD Premier, Anna Bligh,
has refused to reform abortion laws.
Aside from the fact that abortion is still a
criminalised offence in most Australian states
and territories, we also need to remember that
not all women can legally access the
contraception they desire.
In the Northern Territory, for example, doctors
can be fined up to $20 000 for failing to report on
sexually active teenagers (below the age of 16)
who request the morning after pill or the
contraceptive pill. Apparently they are eager
for more teenage mums in the top end.
Page 42 | Ta k i n g i t – 5 0 y e a r s o f t h e p i l l
Similarly there are many pharmacists who – on
moral or religious grounds – refuse to administer
the morning after pill to women. Two years ago,
when I was a staff member at the University of
Sydney, I was outraged to learn that one of the
campus chemists refused to provide the
morning after pill. After all, university is often a
time of sexual experimentation (and sexual slip
up). It is absolutely unethical for chemists to
deny young women the emergency
contraception they require.
There are also many pharmacists who continue
to give patronising, moralising sermons to young
women who request emergency contraception.
On more than one occasion I have had
to comfort rape survivors who have been
lectured and judged by arrogant, unthinking
pharmacists who have scolded them when
they came in to purchase the morning after
pill, having just been raped. And then there
are the ongoing fights over the emergency
contraception, RU486.
But it is not all doom and gloom. This year
marks the 50th anniversary of the public
availability of the contraceptive pill. And what a
prime opportunity to reflect on the undeniable
impact that this product has had on peoples
lives. While initially the Pill was only prescribed
to married women, it is now far more readily
available. It has enabled women to manage
and control their fertility and this in turn has
given them greater control and choice over
their lives and bodies.
But while we should acknowledge this
significant milestone, it is important that
young women continue to fight to expand and
consolidate our reproductive rights. While it is
hard for women my age and younger to even
imagine what it was like to live in the pre-Pill,
backyard-abortion era of the fifties, we cannot
become complacent about our reproductive
rights now.
Of course these issues do not apply to
Australian women alone. There are many
countries around the world where women’s
reproductive rights are abused as a matter of
course, and where they have little or no access
to the reproductive technologies that might
empower them to control their fertility.
There is clearly work ahead.
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 43
H opes a nd dreams: S ix w i s h e s f o r t h e f u t u r e of co n t r ac e p t i o n
i n A u str alia
“The upcoming anniversary of 50 years of
availability of the Pill in Australia gives pause
for thought on what’s gone before. But where
should we now go and what could improve
contraception provision as part of our health
care systems?”
Caroline Harvey
Medical Director
Family Planning Queensland
1. A National Sexual and Reproductive
Health Strategy
Australia has never had a comprehensive national
sexual and reproductive health strategy. In 2008,
The Australian Public Health Association in
collaboration with Australian Reproductive Health
Alliance and Sexual Health & Family Planning
Australia put forward a document calling for a
national strategy to be developed.
The document clearly outlines the issues and
the potential scope for such a policy. Whilst there
is a plethora of current policies and strategies
addressing particular aspects of sexual and
reproductive health, they are not well integrated
and in particular there is a notable absence of
policy which acknowledges strategies to
meaningfully address the prevention and
management of unwanted pregnancy.
The Australian Government partnership,
preventative and rights approaches to HIV/AIDS
have been recognized as best practice in sexual
health promotion worldwide. “Strong national
leadership ensured that local and sometimes
parochial views did not influence unduly the
major planks of the strategy”. Is it too much to
hope that at some point such sense and
leadership could similarly ever prevail in ensuring
sex education, contraception services and
abortion access are incorporated into national
health policy?
See http://www.phaa.net.au/documents/SRH_
background_paper.pdf
accessed 9 July 2010
2. Australian evidence based contraception
policies and guidelines
Many countries are recognising the need to
increase the use of long acting contraceptives,
especially by women under thirty, as a specific
population based strategy to reduce unplanned
pregnancy. The National Collaborating Centre
for Women’s and Children’s Health in the UK
have produced a comprehensive guideline on
Long Acting Reversible Contraception, key
concepts of which could easily be translated to
the Australian setting
See http://www.nice.org.uk/nicemedia/
live/10974/29912/29912.pdf
accessed 9 July 2010
While Sexual Health and Family Planning
Australia have published an evidence based
Australian handbook on contraception for
clinicians, there would be benefits in the
development and funding of a formal national
contraception guidelines process. This should
involve other key organisations and experts and
have as its aim, web based readily accessible
national guidelines to support practitioners,
particularly general practitioners.
Page 44 | Ta k i n g i t – 5 0 y e a r s o f t h e p i l l
3. Community discussion with young people
about their needs relating to sexuality and
sexual health services
Young people have sexual and reproductive
health needs that differ from adults in important
ways. These needs are often poorly understood
by health services, and are also affected by
assumptions and beliefs about the rights of
young people to information, to make choices
and decisions about their bodies and sexuality.
Having an openness in the community to listen
to what young people say they want, to listen to
the pragmatic and well-intentioned choices they
make would radically transform the shame and
stigma that gets in the way of good health care.
Imagine a community in which fears about early
sexualisation were transformed by the power
of acting upon the evidence that well informed
young people can assess, laugh at, and critique
the messages they receive and make
appropriate decisions. Imagine if openness and
information about relationships, pleasure and
desire removed the need for furtive, hurried and
unsatisfying encounters. Imagine a place where
young people felt supported to choose what
works for them, and barriers of cost and
access simply melted away.
4. More high quality “head to head” research
trials for the Pill
A higher level of evidence is needed to guide
decisions about combined oral contraceptive pill
choices both for individual prescribers and for
Pharmaceutical Benefits Scheme (PBS) funding
decisions for different oral contraceptive
formulations. Cochrane reviews to date, on the
effects of combined oral contraceptives on
period pain, weight gain, and acne have either
found insufficient evidence to compare and
make conclusions about benefits of different pill
formulations or not found significant differences
between them. Managing pill prescription choice
based on users’ side effects or intercurrent
clinical conditions is therefore often based at
best on “good science” but not strong evidence
of advantages of one pill formulation over
another. This is particularly problematic for
Australian women with current large cost
differentials between formulations for pill users.
5. Decriminalisation of abortion
Unplanned pregnancy is an issue that has
significant health consequences. The possibility
of an unplanned pregnancy is a reality that
women face throughout their reproductive
years. There is no contraceptive method that is
100% effective, and many new contraceptive
products are not available in Australia.
Accessibility to safe and affordable abortion
services ensures the rights of women to
reproductive self determination.
In Queensland, a woman and her partner
have been charged over an abortion and
face a combined ten years in jail if convicted.
This case was committed to trial at a hearing in
September 2009, with the couple to face court
again at a date still yet to be set. Doctors in
Queensland’s public hospitals have suspended
abortion services, mostly provided in cases of
severe foetal abnormality or maternal illness,
meaning some women have had to travel
interstate to access these procedures.
The availability of medical abortion around
the state remains inconsistent, despite the
Government’s recent amendments to section
282 of the state’s Criminal Code. The results of
recent independent opinion polling continue to
show high levels of support for decriminalisation,
with 79% of Queenslanders wanting the law
changed so abortion is no longer a crime.
Contraception:
an Australian
clinical practice
handbook
Second edition
◘◘◘
It is time for abortion to be regulated under
health laws where performed by qualified health
professionals and be removed from the criminal
codes of all state jurisdictions in Australia.
◘◘◘
◘◘◘
◘◘◘
6. Non hormonal contraception options
While the safety and non contraceptive
benefits of hormonal contraception are clearly
established, there is little doubt that some
women still harbour doubts and distrust about
the use of exogenous hormones. One only has
to read a few blogs on the subject to get a feel
for the variety of beliefs and thoughts on the
fears about “hormones”. These fears prompt
cessation of contraception and contribute to
unplanned pregnancy. As well as providing
accurate information to reassure and challenge
myths, we also need to ensure that the current
options of a range of copper intrauterine
devices, male and female barrier methods, and
both male and female sterilisation remain readily
available, affordable and accessible particularly
as new non hormonal methods do not seem to
be anywhere on the horizon.
Sexual Health & Family Planning Australia’s
‘Contraception: An Australian Clinical Practice Handbook’.
◘◘◘
Ta k i n g i t – 5 0 y e a r s o f t h e p i l l | Page 45
F i f ty y ears from now
“A number of critical elements; ideas, behaviours
and attitudes are required to provide a ‘tipping
point’ that produces an innovation as unique as
the Pill. It’s a compelling process reviewing the
steps that lead to an idea becoming a reality.
To have a look into the future, I felt a need
to appraise the people and the elements that
fused to create this moment in time and then
to project those thoughts into the future.”
Christine Read
Sexual Health Physician
Consultant in Family Planning,
Reproductive and Sexual Health
Scientists are the enquirers, fascinated by the
physiological and biochemical intricacies of the
human body and driven to understand them.
The biochemistry of reproductive hormones and
the physiology of the interconnected brain and
ovaries are beautifully balanced. It must have
been quite a moment when the early pioneers
realised they could potentially manipulate female
fertility using the female hormones, oestrogen
and progesterone. I imagine they must have felt
as if they were “playing God”.
Clinicians are driven to solve the practical
problems of their patients. In the early half of the
20th century, medicine was still dependent on a
physician’s skill in diagnosis, investigative
processes were fairly crude and the outcome
was still a bit of a lottery. People were used to
illness, disability and death – it was part of their
daily lives. Doctors, developing a relationship
of mutual respect with scientists, began to aim
higher, looking for ways to make outcomes
more certain and to prevention rather than cure.
Vaccines, antibiotics and anaesthetics
all showed us that there were ways to manipulate
the forces of disease. The discipline of public
health was born. For doctors and midwives it
must have seemed an unattainable promised
land to gain some form of control over
untrammelled fertility, maternal and infant
mortality and instead to have every pregnancy
healthy, planned and wanted. How challenging
it must have been to see the results of
unwanted pregnancy day after day. Was good
and safe contraception possible? And again
was it right to use human skill to prevent
procreation? For that generation there were
many challenges.
Women were both the victims and the
champions of the times. Born to reproduce,
their life span was limited by the joy and the
threat of maternity. As a woman, did you have
a choice? Apparently not if you listened to
orthodox voices, but yes, there was a way if you
listened to the change agents. Political freedom
in the form of votes had come to women,
at least in some parts of the world and Marie
Stopes and Margaret Sanger were set to free
women from their reproductive physiology.
They had set up birth control clinics where
simple barrier contraceptives were sold.
They were both loved and hated, but always
tenacious and resilient. Financial and moral
support would interestingly come from a
childless woman with a strong desire to support
and strengthen the community by ridding
women of the burden of unwanted childbirth,
Katharine McCormick.
Page 46 | Ta k i n g i t – 5 0 y e a r s o f t h e p i l l
Religion, politics and society’s rules
all played their part. There were concerns
about population control on a large scale.
The emerging economic imperatives made
the importance of women’s contributions to
household income so vital; the social revolution
was on the horizon after the first and second
world wars – education and careers for women.
And not least, the freedom and importance of
the expression of sexuality as part of human
relationships was just starting to be recognised.
1. The developed world. The newer forms of
contraception being developed and licensed
over the next ten years include; a wafer that
dissolves on the tongue, a new implant that
is radio opaque and able to be located by
X-ray, a new device for inserting implants,
an electronic device and contraceptive
dispenser that allows women to decide
when and if they will have a bleed, newer,
smaller intrauterine devices, self injections
and the list goes on.
Entrepreneurs provided commercial gain,
without which the story would have been short.
Pharmaceutical companies were only just
starting to realise their potential. Moving from
the era of “snake oil” practitioners and
pharmacists making their own drugs to that of
the pharmaceutical chemists looking for the
next big research development. To start the ball
rolling, managing menstrual disorders was a
“natural” way to go. The realisation that women
really did want the positive side effects of
contraception must have caused some
consternation and interest among the (probably
mostly male) businessmen running companies
like Syntex and Searle as they started to realise
what they had – and they took a risk in funding
and floating a product that did not treat disease,
but intervened in a complex natural function – it
was unknown territory.
2. The developing world. Needs are different,
geographical, cultural and religious issues
are challenging, individuals are less in control
of their immediate situation, population
explosions are political minefields and fertility
rates have been addressed in significantly
different ways from the developed world.
Contraception methods like the Pill are often
available over the counter, rather than by
prescription. This works well in some
countries – Thailand, for instance, but poorly
in Korea, where there is a traditional use of
condoms and withdrawal – male dominated
methods. Abortion rates and gender issues
are huge topics for international family
planning programs.
What about the future?
Science, medical practice, women’s needs,
population management and commercial
interests were all critical factors in the birth of
the Pill – what can they tell us about the future?
The scientists will not stop until they have
developed the perfect contraceptive, delivering
efficient contraception but with many additional
benefits to health and wellbeing. The question
is the perfect contraceptive for whom?
3. The least developed world. Places where
people are often only just surviving, the
question of contraception must seem like
a luxury, yet it is the area of most pressing
need. In Africa, women still have so little
choice. The methods that work have been
developed, but bigger issues are cost and
access and the HIV/AIDS epidemic.
Over the next 50 years we will certainly have
multiple fantastic choices for the developed
world. These products should in some way
be developed in a socially responsible manner:
part of the profits going towards the
development and distribution of acceptable
contraceptives for the least developed
countries. The science is there, but in the
language of the corporate world. We need to
understand and segment the market to meet
the needs of women, clinical services,
governments and the commercial sector to
provide appropriate contraceptive methods at
reasonable cost to where they are needed most.
In many cultures, contraception is still a male
practice and fecundity is part of a woman’s
identity and essential if she is to have any role
in the community. Contraception must somehow
manage these needs. Women should not die
because of unsafe childbirth or abortion, and all
should have access to the best care: before,
during and after delivery.
Over the next 50 years, we need to get this
part right – human rights, women’s roles and the
issues of maternal health. Contraception has a
huge part to play and sex education and sexual
health literacy are vital. Large foundations, such
as that endowed by Bill and Melinda Gates will
play a critical role, but other sources of support
with solid public health and project management
skills must come to the forefront to help build
sustainability and capacity on the ground.
Do doctors care? Yes! Do they know how to make
a difference? Not always. In 50 years how will
family planning practice look? At present it is seen
as an “add on” to medical studies (and often of far
lesser importance to the study of disease).
Interestingly it is in family planning, sexual and
reproductive health consultations that doctors’
really have to challenge their own assumptions,
their inherent judgemental attitudes and their
feelings about their own and others cultural identity.
Sex and fertility management touch on people’s
innermost taboos. Medical practitioners, especially
in the western world, are sometimes accused of
having a “disease focused” or “medical model” of
practice. This takes away from the individual and
gives power to the medical professional.
The passion that led many clinicians to campaign
for family planning in the developed world is often
described as unnecessary and “past its use by
date”. Yet there is so much we still do not
understand and will not if we do not take this
area of health seriously. In the developed world,
more than 50% of pregnancies are still unplanned
– why? We need to understand better the reasons,
and more public health and qualitative research is
needed to tease out the answers.
We all say we want freedom from repression,
from rules and of expression. What do we
mean? I think what we really want is freedom
of choice AND the means to make those
choices properly, effectively and with
confidence. In the world of health, this means
health literacy – and in the world of fertility
management, or family planning, this means
“sexual health literacy”.
Science can give us a better life, and doctors
and other health care practitioners are the
arbiters of good health care. Both women and
men must be engaged in their own reproductive
and sexual health. Yet, for the future of
contraception you need all the factors to get to
the “tipping point”. We need the entrepreneurs,
the pharmaceutical companies, the promoters
of conferences, the PR companies, the
advertising executives – the commercial arm of
medicine. Why do we find the nexus between
science, medicine, human rights and
commercialism so difficult? My guess it’s the
element of risk. Entrepreneurs take risks and
sometimes when those risks fail, human frailty
takes over. BUT, if no risks are ever taken,
where would we be?
We need to look at where we are and ask,
how do we get to the next stage? To get there
in 50 years we must all have the same goal –
efficient, appropriate, affordable and respectful
management of human reproduction.
Aboriginal artwork commissioned for Family Planning NSW clinic in Dubbo.
PB 03-001 MSD FULL PAGE AD 25-8-10
27/8/10
10:48 AM
Page 1
Welcome
to the next 50 years
of contraception innovation
50
years ago women were
offered a choice…half
a century later women
have changed, and so
have their choices.
Australian women now choose from daily and longer term reversible options,
including hormonal options in the form of the pill, the implant, the ring, the
injection or the intrauterine system, and non-hormonal options including the
coil and male or female condoms.
MSD, through its Organon heritage, is proud to have provided innovative and
ground breaking contraceptive options to Australian women.
MSD has also launched www.whatcontraceptiveareyou.com.au
an educational resource that informs Australian women about the contraceptive
options available to them.
And looking to the next 50 years, we are committed to the innovation of more
contraceptive options to suit women’s ever changing lifestyles.
Today's MSD is a global healthcare leader working to help the world be well. MSD is a tradename of Merck & Co., Inc., with headquarters in Whitehouse Station, N.J., U.S.A. Through our
prescription medicines, vaccines, biologic therapies, and consumer care and animal health products, we work with customers and operate in more than 140 countries to deliver innovative
health solutions. We also demonstrate our commitment to increasing access to healthcare through far-reaching policies, programs and partnerships. MSD. Be well. For more information,
visit www.msd-australia.com.au. Merck Sharp & Dohme (Australia) Pty Limited. Level 4, 66 Waterloo Road, North Ryde NSW 2113. WOHE-10-AUS-6526-O August 2010.
Acknowledgements
Writing and preparing a book for publication is a complex task. There are many
people in the team before it finally comes to life. The editor and publisher would like
to acknowledge the contributions, help and support of;
The Authors
Lindsey Parks, Manager Communications and Marketing Officer Family Planning NSW
Charlie Aarons, Publications Officer, Family Planning NSW
Ann Brassil, CEO, Family Planning NSW
Designed and printed by GEON print & communication solutions
Bayer Schering Pharma for providing images from their library
Dr Stefania Siedlecky for generously lending newspaper clippings of historical interest.
Emma Haslam, Librarian Family Planning NSW.
This Publication is subject to Copyright
All rights reserved by Family Planning NSW © Family Planning NSW 2010
No part of this publication may be reproduced, stored in a retrieval system or transmitted in any
form or by any means, electronic, mechanical, photocopying, recording or otherwise without the
prior permission of the publisher in writing.
ISBN 978-1-877026-19-5
“It was in March 1964 that I swallowed my first oral contraceptive pill
thoughtfully provided by a friend. I was 22 years old, in love and had already
survived one unplanned pregnancy. The idea that I could be in charge of
my own fertility by taking a pill which provided total protection against
pregnancy and was not related to the sexual moment was breathtaking.”
Wendy McCarthy AO, Company Director, Social Commentator and Mentor
14 perspectives on the impact of the oral contraceptive pill.