Blood blood liquid connective tissue consist of plasma and formed
advertisement

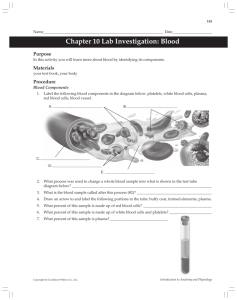
Blood blood liquid connective tissue consist of plasma and formed elements(red blood cells,white blood cells and platelets) Plasma is the liquid medium for carrying various substances in the blood. It also distributes the heat generated as a by-product of metabolism, particularly muscle contraction. About 91% of plasma is water The remaining 9% of plasma consists of various salts (ions) and organic molecules. Salts are dissolved in plasma As mentioned previously, salts and plasma proteins maintain the osmotic pressure of blood. Salts also function as buffers that help maintain blood pH. Small organic molecules such as glucose and amino acids are nutrient in the cells; urea is a nitrogenous waste product on its way to the kidneys for excretion. The most abundant organic molecules in blood are called the plasma proteins. The liver produces the majority of the plasma proteins. The plasma proteins have many functions that help maintain homeostasis. Like salts, they are able to take up and release hydrogen ions. Therefore, they help keep blood pH around 7.4. Plasma proteins are too large to pass through capillary walls. They remain in the blood, establishing an osmotic gradient between blood and tissue fl uid. This osmotic pressure is a force that prevents excessive loss of plasma from the capillaries into tissue fl uid. Three major types of plasma proteins are the albumins, globulins, and fi brinogen. Albumins are the most abundant plasma proteins and contribute most to plasma’s osmotic pressure. They also combine with and help transport other organic molecules. The globulins are of three types called alpha, beta, and gamma globulins. Alpha and beta globulins also combine with and help transport substances in the blood such as hormones, cholesterol, and iron. Gamma globulins are also known as antibodies and are produced by white blood cells called lymphocytes, not by the liver. Gamma globulins are important in fi ghting disease- causing pathogens .Fibrinogen is an inactive plasma protein. Once activated, fi brinogen forms a blood clot Red Blood Cells Carry Oxygen Red blood cells are highly specialized for oxygen (O2) transport. RBCs contain hemoglobin (Hb), a pigment that makes red blood cells and blood red. The globin portion of hemoglobin is a protein that contains four highly folded polypeptide chains. The heme part of hemoglobin is an iron-containing group in the center of each polypeptide chain . Each hemoglobin molecule can transport four molecules of O2 , and each RBC contains about 280 million hemoglobin molecules. Red blood cells are an excellent example of structure suiting function. They have no nucleus; their biconcave shape comes about because they lose their nucleus during maturation . The biconcave shape of RBCs gives them a greater surface area for the of the internal space of RBCs is used for transport of oxygen, RBCs also lack most organelles including mitochondria. RBCs anaerobically produce ATP, and they do not consume any of the oxygen they transport. When oxygen binds to heme in the lungs, hemoglobin assumes a slightly different shape and is called oxyhemoglobin. In the tissues, heme gives up this oxygen, and hemoglobin resumes its former shape, called deoxyhemoglobin The released oxygen diffuses out of the blood into tissue fl uid and then into cells Red Blood Cells Help Transport Carbon Dioxide After blood picks up carbon dioxide (CO2) in the tissues,about 7% is dissolved in plasma., hemoglobin directly transports about 25% of CO2, combining it with the globin protein. Hemoglobin-carrying CO2 is termed carbaminohemoglo bin The remaining CO2 (about 68%) is transported as the bicarbonate ion (HCO3 –) in the plasma. Consider this equation CO2 + H2O H2CO3 H+ + HCO3 When Carbon dioxide moves into RBCs, combining with cellular water to form carbonic acid. An enzyme found inside RBCs, called carbonic anhydrase, speeds the reaction. Carbonic acid quickly separates, or dissociates, to form hydrogen ions (H+) and bicarbonate ions (HCO3 –). The bicarbonate ions diffuse out of the RBCs to be carried in the plasma. The H+ from this equation binds to globin, the protein portion of hemoglobin. Thus, hemoglobin assists plasma proteins and salts in keeping the blood pH constant. . When blood reaches the lungs, the reaction is reversed Hydrogen ions and bicarbonate ions reunite to re-form carbonic acid. The carbonic anhydrase enzyme also speeds this reverse reaction. Carbon dioxide diffuses out of the blood and into the airways of the lungs, to be exhaled from the body. The RBC stem cells in the bone marrow divide and produce new cells that differentiate into mature RBCs. As red blood cells mature, they lose their nucleus and acquire hemoglobin. Because they lack a nucleus, RBCs are unable to replenish important proteins and repair cellular damage. Therefore, red blood cells only live about 120 days. When they age, red blood cells are phagocytized by white blood cells (macrophages) in the liver and spleen It is estimated that about 2 million RBCs are destroyed per second, and therefore, an equal number must be produced to keep the red blood cell count in balance. When red blood cells are broken down, hemoglobin is released The globin portion of hemoglobin is broken down into its component amino acids, which are recycled by the body. The majority of the iron is recovered and returned to the bone marrow for reuse, although some is lost and must e replaced in the diet. The rest of the heme portion of the molecule undergoes chemical degradation and is excreted by the liver and kidneys. If the liver fails to excrete heme, it accumulates in tissues, causing a condition called jaundice.In jaundice, the skin and whites of the eyes turn yellow. . The kidneys release a hormone called erythropoietin that stimulate the production of RBCs in bone marrow in process called erythropoiesis Disorders Involving Red Blood Cells When there is an insufficient number of red blood cells or the cells do not have enough hemoglobin, the individual suffers from anemia and has a tired, run-down feeling. Iron, vitamin B12, and folic acid are necessary for the production of red blood cells. Iron-defi ciency anemia is the most common form. It results from inadequate intake of dietary iron, which causes insufficient hemoglobin synthesis. A lack of vitamin B12 causes pernicious anemia, in which stem-cell activity is reduced due to inadequate DNA production. As a consequence, fewer red blood cells are produced. Folic-acid-defi ciency anemia also leads to a reduced number of RBCs, particularly during pregnancy.Pregnant women should increase their intake of folic acid, because a defi ciency can lead to birth defects in the newborn. Hemolysis is the rupturing of red blood cells. In hemolytic anemia, the rate of red blood cell destruction increases. Sickle-cell disease is a hereditary condition in which the individual has sickle-shaped red blood cells that tend to rupture as they pass through the narrow capillaries.. The problem arises because the protein in two of the four chains making up hemoglobin is abnormal. The life expectancy of sickleshaped red blood cells is about 90 days instead of 120 days White blood cells (leukocytes)WBCs WBCs differ from red blood cells in that they are usually larger, have a nucleus, lack hemoglobin, and are translucent unless stained. White blood cells are not as numerous as red blood cells. There are only 5,000– 11,000 per mm3 of blood. White blood cells are derived from stem cells in the red bone marrow, where most types mature. There are several types of white blood cells and the production of each type is regulated by a protein called a colony-stimulating factor (CSF). In a person with normally functioning bone marrow, the numbers of white blood cells can double within hours, if needed. White blood cells are able to squeeze through pores in the capillary wall; therefore, they are also found in tissue fl uid and lymph White blood cells fight infection; thus, they are an importantpart of the immune system. WBCs divided to: Granular Leukocytes The granular leukocytes include neutrophils, eosinophils and basophils 1- Neutrophils account for 50–70% of all white blood cell Therefore, they are the most abundant of the white blood cells. They have a multilobed nucleus, so they are called polymorphonuclear leukocytes, or “polys.” The granules of neutrophils are not easily stained with acidic red dye, nor with basic purple dye. (This accounts for their name, neutrophil. Neutrophils can be recognized by their numerous light-pink granules. Neutrophils are usually fi rst responders to bacterial infection, and their intense phagocytic activity is essential to overcoming an invasion by a pathogen. 2-Eosinophils have a bilobed nucleus. Their large, abundant for their name,eosinophil.) Not much is known specifi cally about the function of eosinophils, but they increase in number in the event of a parasitic worm infection or an allergic reaction 3-Basophils have a U-shaped or lobed nucleus. Their granules take up the basic stain and become a dark-blue color. (This accounts for their name, basophil.) In the connective tissues, basophils (and similar cells called mast cells) release histamine associated with allergic reactions. Histamine dilates blood vessels but constricts the air tubes that lead to the lungs, which is what happens during an asthma attack when someone has diffi culty breathing. Agranular Leukocytes The agranular leukocytes include the lymphocytes and the monocytes. Lymphocytes and monocytes do not have granules and have nonlobular nuclei. They are sometimes called the mononuclear leukocytes 1-Lymphocytes account for 25–35% of all white blood cells. Therefore, they are the second most abundant type of white blood cell. Lymphocytes are responsible for specifi c immunity to particular pathogens and toxins ( poisonous substances). The lymphocytes are of two types: B cells and T cells. Mature B cells called plasma cells produce antibodies, the proteins that combine with target pathogens and mark them for destruction. Some T cells (cytotoxic T cells) directly destroy pathogens. The AIDS virus attacks one of several types of T cells. In this way, the virus causes immune defi ciency, an inability to defend the body against pathogens 2-Monocytes are the largest of the white blood cells. After taking up residence in the tissues, they differentiate into even larger macrophages. In the skin, they become dendritic cells. Like the neutrophils, macrophages and dendritic cells are active phagocytes, destroying pathogens, old cells, and cellular debris Macrophages and dendritic cells also stimulate other white blood cells, including lymphocytes, to defend the body Disorders Involving White Blood Cells Cancer is due to uncontrolled cell growth. Leukemia, which means “white blood,” refers to a group of cancers that involve uncontrolled white blood cell proliferation. Most of these white blood cells are abnormal or immature. Therefore, they are incapable of performing their normal defense functions. Each type of leukemia is named for the type of cell dividing out of control. For example, lymphocytic leukemia involves abnormal lymphocyte proliferation. Immune defi ciencies are sometimes inherited. Children have severe combined immunodefi ciency disease (SCID) when the stem cells of white blood cells lack an enzyme called adenosine deaminase. Without this enzyme, B and T lymphocytes do not develop and the body cannot fi ght infections. About 100 children are born with the disease each year. Injections of the missing enzyme can be given twice weekly, but a bone marrow transplant from a compatible donor is the best way to cure the disease An Epstein–Barr virus (EBV) infection of lymphocytes is the cause of infectious mononucleosis, so named because the lymphocytes are mononuclear. EBV, a member of the herpes virus family, is one of the most common human viruses. Symptoms of infectious mononucleosis are fever ,sore throat, and swollen lymph glands Blood Clotting Platelets (thrombocytes) result from fragmentation of certain large cells, called megakaryocytes, in the red bone marrow.Platelets are produced at a rate of 200 billion a day, and the blood contains 150,000–300,000 per mm3. These formed elements are involved in the process of blood clotting, or coagulation.When a blood vessel in the body is damaged Stages of Blood Clotting There are at least 12 clotting factors that participate in the formation of a blood clot. We will discuss the roles played by fibrinogen, prothrombin, and thrombin. Fibrinogen and prothrombin are proteins manufactured and deposited in blood by the liver. Vitamin K, found in green vegetables and also formed by intestinal bacteria, is necessary for the production of prothrombin, and if by chance this vitamin is missing from the diet, hemorrhagic disorders occure * When a break occurs in a blood vessel, damaged tissue releases tissue thromboplastin, a blood clotting factor that initiates a series of reactions involving several clotting factors and calcium ions (Ca). * These reactions lead to production of prothrombin activator which converts prothrombin to thrombin. This reaction also requires Ca. *Thrombin, in turn, acts as an enzyme that convers fibrinogento long threads of fibrin. * Fibrin threads wind around the platelet plug in the damaged area of the blood vessel and provide the framework for the clot. Red blood cells also are trapped within the fibrin threads; these cells make a clot appear red. A fibrin clot is present only temporarily. As soon as blood vessel repair is initiated, an enzyme called plasmin destroys the fibrin network and restores the fluidity of plasma. If blood is allowed to clot in a test tube, a yellowish fluid develops above the clotted material. This fluid is called serum, and it contains all the components of plasma except fibrinogen. Hemophilia is an inherited clotting disorder due to a deficiency in a clotting factor.. Bleeding into muscles can lead to nerve damage and muscular atrophy The most frequent cause of death is bleeding into the brain with accompanying neurological damage. ABO System The most common system for typing blood is the ABO system In the ABO system, the presence or absence of type A and type B antigens on red blood cells determines a person’s blood type. For example, if a person has type Ablood, the A antigen is on his or her red blood cells. This molecule is not an antigen to this individual, although it can be an antigen to a recipient who does not have type A blood. In the simplified ABO system, there are four types of blood: A, B, AB, and O . Within the plasma, there are antibodies to the antigens that are not present on the person’s red blood cells. These antibodies are called anti-A and anti-B It is reasonable that type Ablood would have anti-B and not anti-A antibodies in the plasma. If anti-A antibodies were present in plasma, agglutination, of red blood cells, would occur. Agglutination of red blood cells can cause blood to stop circulating in small blood vessels, and this leads to organ damage. It also is followed by hemolysis, which may cause the death of the individual . For a recipient to receive blood from a donor, the recipient’s plasma must not have an antibody that causes the donor’s cells to agglutinate to determine each person’s blood type. Figure 6.10 demonstrates a way to use the antibodies derived from plasma to determine the blood type. If clumping occurs after a sample of blood is exposed to a particular antibody, the person has that type of blood Today, blood transfusions are a matter of concern not only because blood types should match, but also because each person wants to receive blood that is of good quality and free of infectious agents. Blood is tested for the more serious agents such as those that cause AIDS, hepatitis, and syphilis. Rh System Another important antigen in matching blood types is the Rh factor. Eighty-five percent of the U.S. population have this particular antigen on the red blood cells and are Rh (Rh positive). Fifteen percent do not have this antigen and are Rh (Rh negative). Rh individuals normally do not have antibodies to the Rh factor, but they may make them when exposed to the Rh factor. To test whether an individual is Rh or Rh, blood is mixed with anti-Rh antibodies. When Rh blood is mixed with anti-Rh antibodies, agglutination occurs The designation of blood type usually also includes whether the person has or does not have the Rh factor on the red blood cells. During pregnancy, if the mother is Rh and the father is Rh, the child may be Rh. The Rh red blood cells may begin leaking across the placenta into the mother’s cardiovascular system, as placental tissues normally break down before and at birth. The presence of these Rh antigens causes the mother to produce anti-Rh antibodies. In this or a subsequent pregnancy with another Rh baby, anti-Rh antibodies produced by the mother may cross the placenta and destroy the child’s red blood cells. This is called hemolytic disease of the newbor n (HDN) because hemolysis continues after the baby is born. Due to red blood cell destruction, excess bilirubin in the blood can lead to brain damage and mental retardation or even death The Rh problem is prevented by giving Rh women an Rh immunoglobulin injection. This injection contains anti-Rh antibodies that attack any of the baby’s red blood cells in the mother’s blood before these cells can stimulate her immune system to produce her own antibodies. This injection is not beneficial if the woman has already begun to produce antibodies; therefore, the timing of the injection is most important The Blood Vessels The cardiovascular system has three types of blood vessels the arteries (and arterioles), which carry blood away from the heart to the capillaries; the capillaries, which permit exchange of material with the tissues; and the veins (and venules), which return blood from the capillaries tothe heart. The Arteries The arterial wall has three layers. The inner layer is a simple squamous epithelium called endothelium with a connective tissue basement membrane that contains elastic fibers. The middle layer is the thickest layer and consists of smooth muscle that can contract to regulate blood flow and blood pressure. The outer layer is fibrous connective tissue near the middle layer, but it becomes loose connective tissue at its periphery. Some arteries are so large that they require their own blood vessels Arterioles are small arteries just visible to the naked eye. The middle layer of arterioles has some elastic tissue but is composed mostly of smooth muscle whose fibers encircle the arteriole. When these muscle fibers are contracted,the vessel has a smaller diameter (is constricted); when these muscle fibers are relaxed, the vessel has a larger diameter (is dilated). Whether arterioles are constricted or dilated affects blood pressure. The greater the number of vessels dilated, the lower the blood pressure The Capillaries Arterioles branch into capillaries. Each capillary is an extremely narrow, microscopic tube with one-cell-thick walls composed only of endothelium with a basement membrane. Capillary beds (networks of many capillaries) are present in all regions of the body; consequently, a cut to any body tissue draws blood. Capillaries are a very important part of the human cardiovascular system because an exchange of substances takes place across their thin walls. Oxygen and nutrients, such as glucose, diffuse out of a capillary into the tissue fluid that surrounds cells. Wastes, such as carbon dioxide, diffuse into the capillary. The relative constancy of tissue fluid is absolutely dependent upon capillary exchange Venules are small veins that drain blood from the capillaries and then join to form a vein. The walls of venules (and veins) have the same three layers as arteries, but there is less smooth muscle and connective tissue . Veins often have valves, which allow blood to flow only toward the heart when open and prevent the backward flow of blood when closed. Since the walls of veins are thinner, they can expand to a greater extent At any one time, about 70% of the blood is in the veins. In this way, the veins act as a blood reservoir. The heart is a cone-shaped, muscular organ located between the lungs, The major portion of the heart is the interior wall of tissue called the myocardium, consisting largely of cardiac muscle tissue. The muscle fibers of myocardium are branched. Each fiber is tightly joined to neighboring fibers by structures called intercalated disks The intercalated disks also include cell junctions like gap junctions and desmosomes. The heart is surrounded by the pericardium, a thick, membranous sac that supports and protects the heart. The inside of the pericardium secretes pericardial fluid (a lubrication fluid), and the pericardium slides smoothly over the heart’s surface as it pumps the blood Internally, a wall called the septum separates the heart into a right side and a left side (Fig. 5.4a). The heart has four chambers. The two upper, thin-walled atria (sing., atrium) are called the right atrium and the left atriumThe two lower chambers are the thick-walled ventricles, called the right ventricle and the left ventricle Heart valves keep blood fl owing in the right direction and prevent its backward movement. The valves that lie between the atria and the ventricles are called the atrioventricula (AV) valves. These valves are supported by strong fi brous strings called chordae tendineae. The chordae tendineae are attached to papillary muscles that project from the ventricular walls. The AV valve on the right side is called the tricuspid valve because it has three fl aps, or cusps. The AV valve on the left side is called the bicuspid valve because it has two fl aps the semilunar valves, with fl aps shaped like half-moons. These valves lie between the ventricles and their attached vessels. The semilunar valves are named for their attached vessels: The pulmonary semilunar lve lies between the right ventricle and the pulmonary trunk. The aortic semilunar valve lies between the left ventricle and the aorta . Disorders of cardiovascular system Hypertension occurs when blood moves through the arteries at a higher pressure than normal atherosclerosis . Atherosclerosis is caused by formation of lesions, or atherosclerotic plaques, on the inside of blood vessels. The plaques narrow blood vessel diameter, choking off blood and oxygen supply to the tissues As long as the clot remains stationary, it is called a thrombus When blood moves along with the blood, it is called an embolus A thromboembolism consists of a clot fi rst carried in the bloodstream that then becomes completely stationary stroke, often results when a small cranial arteriole bursts or is blocked by an embolus myocardial infarction (MI), also called a heart attack occurs when a portion of the heart muscle dies due to lack of oxygen. If a coronary artery becomes partially blocked the individual may then suffer from angina pectoris.