CARDIOVASCULAR SYSTEM: Blood: Chapter 19
advertisement

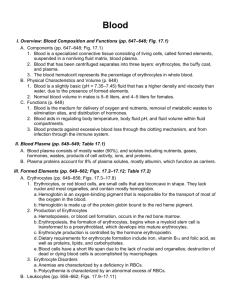
CARDIOVASCULAR SYSTEM: Blood: Chapter 19 Cardiovascular System Consists of: 1. a pump 2. a transport system 3. a fluid medium Components of Blood: specialized fluid of connective tissue Plasma Formed Elements Erythrocytes, leukocytes, platelets buffy coat Functions of Blood 1. Delivery of from the lungs & from the digestive tract to 2. Transport of wastes (CO2 & metabolic wastes) to 3. Transport of . from the endocrine organs to their target organs. 4. Maintenance of body temperature 5. Maintenance of normal pH in body tissues 6. Maintenance of blood volume 7. Prevention of blood loss 8. Prevention of infection Characteristics of Blood: 1. color: 2. pH 3. temperature 4. volume: normovolemic (7% of body weight) hypovolemic: Hypervolemic How does blood volume effect blood pressure (BP)? PLASMA: makes up 50-60% of blood volume •clear, pale yellow •90% water ↑ water = ↑ plasma volume (clinically plasma volume expanders) 1 •also contains: a. proteins (plasma proteins): synthesized in -albumin: carrier protein, buffer, maintains osmotic pressure -globulins immunoglobulins: IgG, IgA, IgM transport globulins hormone binding proteins: TBG metalloproteins: transferrin apolipoproteins - (lipoprotein) -fibrinogen -other plasma proteins: hormones, enzymes b. other: dissolved gasses, nutrients •serum: plasma without clotting proteins Key Differences between Plasma and IF 1.) Levels of O2 and CO2 2.) Concentrations & types of dissolved proteins Plasma contains more protein Plasma proteins do not pass through capillary walls FORMED ELEMENTS: (p. 658 table 19-3) Formation of Formed Elements •hemopoiesis (hematopoiesis) hemocytoblast: 3 Types of Formed Elements: 1.) RBC or Erythrocytes 2.) WBC or Leukocytes 3.) Platelets 2 1. Erythrocytes: •anucleate – can’t undergo mitosis – continuously formed in bone marrow live for aprx. 3-4 months • also lack mitochondria – rely on anaerobic metabolism packets of hemoglobin (Hb) • disc shaped, flexible Importance of RBC Shape and Size High surface-to-volume ratio ▪ Quickly absorbs and releases oxygen ▪ Discs form stacks called rouleaux ▪ Smooth the flow through narrow blood vessels ▪ Discs bend and flex entering small capillaries: ▪ 7.8 µm RBC passes through 4 µm capillary • most numerous of the formed elements: 1 mm3 (µl) contains aprx. 5 million RBCs • hematocrit (VPRC or PCV): Normally - females 36-42%, males 44-50% Hct increases during dehydration Hct decreases if internal bleeding or RBC formation problems Viscosity: • each RBC contains hemoglobin: Globin Heme pigment Fe -expressed as grams/100 ml of whole blood, normal 12 - 18g/dl -oxyhemoglobin (HbO2) -reduced or deoxyhemoglobin (HHb) - carbaminohemoglobin (HbCO2) - release nitric oxide to dilate blood vessels Fetal Hemoglobin: Storage form of Hb found in embryos 3 Formation of Erythrocytes: erythropoiesis: 3 million/second As cells differentiate, accumulate hemoglobin then lose organelles and nucleus Reticulocyte released from bone marrow, matures into erythrocyte in blood Reticulocyte count shows erythropoietin (EPO) – from kidneys released during hypoxia- stimulates hemopoiesis renal failure reduces EPO production (note testosterone also increases EPO production) Blood Doping: artificially boosting Hct to increase O2 delivery to cells & aerobic performance Dietary requirements: Carbohydrates /Fat intake Folic Acid: necessary for protein synthesis B12 & intrinsic factor – Destruction of Erythrocytes RBC phagocytized (hemolysis) by macrophages in the liver, spleen and bone marrow (some RBC hemolyze in the bloodstream & Hb excreted by kidneys in urine, if excessive= hemoglobinuria) RBC - Hb split off and broken down into heme and globin globin portion: iron: stored or transported via transferrin heme portion → Fe stripped and remainder is biliverdin → bilirubin →bloodstream to liver for excretion in bile→ large intestine jaundice: bilirubin diffuses into skin/sclera urobilin — yellow stercobilin: brown 4 Transfusion and Blood Replacement Blood Groups or Types are genetically determined ABO Blood Groups Antigen (termed agglutinogens): antigen A or B cell membrane surface proteins – cellular “ID” cards Antibody (agglutinins): found in plasma, Anti-A or Anti-B Identify and attack foreign antigens: form antigen-antibody complex (agglutination) or clumping & hemolyze Called a cross (transfusion) reaction: ABO Blood Typing: Named for presence/absence of RBC antigen Blood Group RBC antigens Plasma antibodies Blood that can be received A B AB O AB is universal recipient: O is universal donor: Rh (D) Blood Groups: Rh antigen either (+) or (-) Rh + is dominant: R RR or Rr are: rr is: Normally Rh- does not have Rh antibodies Only forms them if sensitized (exposed): concern if Rh- mother (Rh+ father) has Rh+ fetus Hemolytic Disease of the Newborn Mom type O blood & baby A or B Mom’s anti-A and Anti-B antibodies can cross placenta Mom Rh- & baby Rh+ 5 2. Leukocytes: aprx. 5000 – 10000 per mm3 • circulate for short periods • have nuclei • Functions: 1.) defend against pathogens\ 2.) remove toxins and wastes 3.) attack • capable of amoeboid movement and can migrate from the blood vessel and travel to the injury site diapedesis (emigration): • find infections/damaged tissues via positive chemotaxis • neutrophils, eosinophils and monocytes capable of phagocytosis Granulocytes and Agranulocytes: under control of colony-stimulating factors & cytokines Granulocytes: (derived from myeloblast) stimulated by G-CSF & GM-CSF 1. Neutrophil (polymorphonuclear leukocytes PMNs): 1st on site Pale cytoplasm with granules attack bacteria marked by antibodies or complement engulf bacteria/pathogens - metabolism increases (respiratory burst) results in H2O2 and superoxide anions which kill bacteria secrete defensins to kill pathogen (bacteria, fungi, viruses) release prostaglandins and leukotrienes 2. Eosinophils: attack anything coated with antibodies use phagocytosis and exocytosis (nitric oxide & cytotoxic enzymes) sensitive to allergens also moderate inflammation from mast cells & neutrophils 3. Basophils: rarest of the leukocytes important for triggering the inflammatory response release histamine and heparin 6 Agranulocytes: 1. Lymphocytes (derived from lymphoblast) Second most numerous some circulate/migrate mostly found in Part of the body’s specific defense system Three Classes of Lymphocytes: 1.) T Cells: cell-mediated immunity 2.) B Cells: humoral immunity 3.) NK (natural killer) cells: immune surveillance Destroy and kill abnormal cells 2. Monocytes (derived from monoblast) stimulated by M-CSF and GM-CSF tissue macrophages Differential Count: detects changes in WBC populations Leucopenia (leukopenia): Leukocytosis Leukemia Regulation of WBC Production Colony-stimulating factors = CSFs : Hormones that regulate blood cell populations: 1. M-CSF stimulates monocyte production 2. G-CSF stimulates granulocyte (neutrophils, eosinophils, and basophils) production 3. GM-CSF stimulates granulocyte and monocyte production 4. Multi-CSF accelerates production of granulocytes, monocytes, platelets, and RBCs 3. Platelets (megakaryocytes) or thrombocytes (derived from progenitor cells) • 150,000 – 400,000 per mm3 of blood • not typical cell – more like cell fragment with chemicals • megakaryocyte can form aprx. 4000 platelets • only live for • stored in • functions: release chemicals for clotting, form platelet plug, clot retraction thrombocytopoiesis: in bone marrow TPO (thrombopoietin), IL-6 stimulate platelet formation 7 thrombocytopenia: thrombocytosis HEMOSTASIS 1. Vascular phase 2. Platelet phase 3. Coagulation phase Step 1: Vascular Phase: immediate response • Vascular Spasm• Endothelial cells release chemicals & hormones (ADP, prostacyclin, endothelians) • Endothelial cell membranes become sticky Step 2: Platelet Phase: begins within 15 seconds • Platelets become sticky - platelet adhesion & aggregation forms platelet plug Platelets stick to •Normally platelets don't cling to each other or the smooth lining of blood vessels. injury causes platelets to become activated: release chemicals 1.) ADP (adenosine diphosphate) – 2.) thromboxane A2 – 3.) serotonin – 4.) platelet-derived growth factor (PDGF) – 5.) calcium ions – 6.) prostacyclin – 7.) protein C or S • positive feedback of activation & attraction of platelets to the area. Step 3: Coagulation Phase (Blood Clotting): begins 30 seconds or more after the injury • Requires clotting factors (procoagulants): proteins or ions in plasma • Extrinsic pathway begins in vessel wall (outside of bloodstream) – TF (Factor III) “short-cut” to final steps • Intrinsic pathway– begins in bloodstream – PF-3 8 • Common pathway – begins when enzymes from either activate Factor X forming prothrombinase 1.) Prothrombinase is formed 2.) Converts proenzyme prothrombin into enzyme thrombin 3.) Finally thrombin catalyzes the joining of the protein fibrinogen molecules present in the plasma into a fibrin mesh Procoagulants: enhance clot formation Anticoagulants: inhibit clot formation heparin, prostacyclin, protein C, antithrombin-III, aspirin Normally anticoagulants dominate & clotting is prevented, but when a vessel is ruptured procoagulant activity increases Clot formation normally complete w/i 3-6 min. Clotting process needs Ca++ and vitamin K After clot is formed, clot retraction occurs. ruptured vessel edges are drawn together – easier for repair by fibroblasts, smooth muscle cells, endothelial cells When healing is complete, clot digestion (fibrinolysis) occurs. t-PA activates plasminogen into plasmin "Clinically Speaking" (see applications manual) 1. Anemia: decreased ability to carry/deliver oxygen A. Insufficient numbers of RBC: -hemorrhagic anemia: due to internal or external bleeding -hemolytic anemia: RBC are prematurely lysed 9 -aplastic anemia- caused by destruction of the bone marrow Can be hereditary or caused by drugs -pernicious anemia: lack of vitamin B12 B. Decreased ability of Hb to carry O2: -iron deficiency anemia: more common in women C. Abnormal Hb -sickle cell anemia: hypoxia caused hemoglobin to change shape which changes shape of RBC 2. Polycythemia: -blood doping 3. Leukemias: Bone marrow cancer that results in large numbers of abnormal WBCs These cells “crowds out” the RBC and platelets Abnormal WBCs can migrate 4. Infectious Mononucleosis: Caused by Epstein-Barr virus Flu-like symptoms 5. Thromboembolytic conditions: thrombus: abnormal stationary blood clot caused by: genetics, lack of anti-coagulants embolism: travelling blood clot dangerous if becomes stuck in smaller blood vessel Tx: heparin, coumadin (warfarin), dicumarol, TPA, streptokinase, aspirin 10 6. Hemophilias: x-linked genetic disorder problems with clotting 7. Impaired liver function: liver unable to synthesize procoagulants Liver also needs vitamin K to make clotting factors Common hematology diagnostics: see pages 123-126 in Applications Manual Other: Synthetic Blood Genetically engineered Platelet Rich Plasma Therapy Speeds recovery from damaged ligaments & tendons (may regenerate fibers) 11