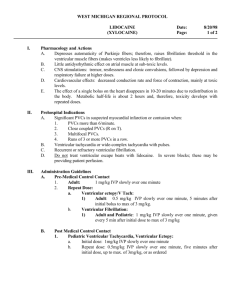
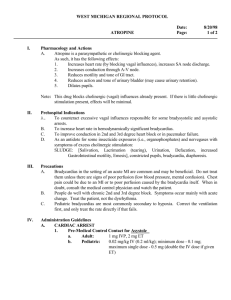
TABLE OF CONTENTS - Emergency Medical Services
advertisement

Medication Card Guidelines – New by Vicki Updated 10.2012 Medication Cards are part of the overall grade for EMSP 2348 Pharmacology Section. Keep in mind that the student is preparing the cards to take into the clinical setting where they MUST know the drugs completely before being allowed to administer them to a patient. The guidelines needed to successfully complete this assignment are as follows: 1. The cards need to be done on Index cards in a spiral notebook; the other alternative is to do them on index cards and then place them in a binder of some sorts so the cards do not “fall out” after completing them. I will NOT take them LOOSE or held together with a binder clip since they can come loose easily. 2. The size of the cards is up to the student in what you are willing to carry but keep in mind that the smaller they are makes it easier to place them in your lab coat. 3. The following information must be on EVERY card. a. Class b. Mechanism of Action c. Indications d. Contradictions e. Side Effects f. Precautions g. How Supplied h. Administration/Dosage 4. THEY MUST BE LEGIBLE IN YOUR HANDWRITING –not anyone’s else’s. 5. Supplied in this packet is some information to help. You will be responsible to complete the medications in this packet, but as health care evolves very rapidly, more medications may need to be added before Paramedic School is completed. A good example is frequently cardiac medications may be added or deleted due to new research. There will be adequate time to add these drugs if it is deemed necessary. 6. The Packet will NOT be scanned into computers and made into drug cards. Commercial Drug Cards are also NOT acceptable either. 7. CARDS MUST BE HANDWRITTEN 8. Cards are due the 1st day of class, graded and then returned to the student. Keep in mind that this assignment will help prepare you for the EMSP 2348 Pharmacology Final exam which has ¾ of the questions on the medications themselves. 9. Under Side Effects Charts, the Key is the following: When it is underlined and has a “C”=COMMON; When it is Bolded and has italics= LT-Life Threatening TABLE OF CONTENTS PAGE NUMBER I. ALL EMERGENCIES A. OXYGEN 1 II. CARDIOVASCULAR EMERGENCIES VASOPRESSORS A. EPINEPHRINE (1:10,000) B. DOPAMINE C. NOREPINEPHRINE D. VASOPRESSIN 2/3 4/5 6/7 8/9 BETA BLOCKERS A. PROPRANOLOL B. METOPROLOL C.ATENOLOL 10/11 12/13 14/15 ANTIDYSHYTHMICS A LIDOCAINE B. PROCAINAMIDE C. AMIODARONE D. MAGNESIUM SULFATE (CARDIAC) E. ADENOSINE F. CALCIUM CHLORIDE 16/17 18/19 20/21 22/23 24/25 26/27 CALCIUM CHANNEL BLOCKERS A. VERAPAMIL B. DILTIAZEM 28/29 30/31 IV. PARASYMATHOLYTICS A. ATROPINE 32/33 V. CARDIAC GLYCOSIDES A. DIGITALIS 34 VI. THROMBOLYTICS (FIBRINOLYTICS) A. ASPIRIN B. RETAPLASE 35/36 37/38 VII. ALKALINIZING AGENTS A. SODIUM BICARBONATE 39/40 TABLE OF CONTENTS (CONT.) PAGE NUMBERS VIII. ANALGESICS A. MORPHINE B. FENTANYL C. NITROUS OXIDE:OXYGEN (50:50) – NITRONOX 41/42 43 44 IX. DIURETICS A. LASIX 45 X. ANTIANGINAL AGENTS A. NITROGLYCERIN 46/47 XI. ANTIHYPERTENSIVES A. LABETALOL 48/49 XII. RESPIRATORY EMERGENCIES A. ALBUTEROL B. EPINEPHRINE (1:1.000) C. METHYPREDNISOLONE (SOLU-MEDROL) D. DEXAMETHASONE (DECADRON) E. RACEMIC EPINEPHRINE (MicroNefrin) 50/51 52/53 54 55 56 XIII. METABOLIC-ENDOCRINE EMERGENCIES A. 50% DEXTROSE B. THIAMIN C. GLUCAGON 57 58 59 XIV. NONTRAUMATIC NEUROLOGICAL EMERGENCIES A. DIAZEPAM 60/61 XV. HYPERTENSIVE DISORDERS OF PREGNANCY A. MAGNESIUM SULFATE (NONCARDIAC) 62/63 XVI. TOXICOLOGICAL EMERGENCIES A. ACTIVATED CHARCOAL B. BENADRYL C. EPINEPHRINE (1:1,000) D. NARCAN E. PROMETHAZINE (PHENERGAN) 64 65/66 67/68 69/70 71 CATIONS / ANIONS Sodium + (Na ) Calcium ++ (Ca ) ++ Mg K + Information on Cations Hypo- causes Hypo- signs / symptoms Hyper - causes Hyper – signs / symptoms 90% of extracellular ions; needed for depolarization; maintains fluid / electrolyte balance; kidneys excrete and conserve, prn; excreted mostly in feces Most abundant ion in the body – predominately extracellular; combines with HPO4 in teeth and bone; involved in blood coagulation; depolarization & contraction; excreted mostly in feces – sm. amt. In urine 50% found in bone; 45% found in intracellular + space (with K ); 5% found in extracellular + + space; triggers Na /K pump; nerve transmission; neuromuscular activity; heart functions; excreted in urine / feces Most abundant intracellular ion; needed for nerve / muscle tissue electrical trans-mission; repolarization; most excreted in urine - Excessive perspiration - vomiting / diarrhea - diuretics - burns - muscle weakness - dizziness - headache - decreased B/P - increased pulse - abdominal cramping - seizures - water loss without salt loss - too much salt intake - profuse watery diarrhea Hypopara-thyroidism; kidney failure; acute pancreatitis; vitamin D deficiency; inadequate ++ Mg & protein; increased HPO4 levels Numbness / tingling in fingers; increased reflexes; muscle / abdominal cramping; seizures; laryngeal spasms (asphyxia); dysrhythmias Parathyroid / thyroid dysfunction; diuretics; too much vitamin D (Fish, liver oil,egg yolk,fortified milk) - thirst - fatigue - restless / agitation - coma - hyper-thermia - oliguria / anuria - dry, sticky, mucus membranes Lethargy; weakness; anorexia; nausea / vomiting; polyuria; itching; bone pain; depression; renal stones; confusion, stupor, coma Diarrhea; nasogastric ++ suctioning with a Mg free fluid; alcoholism; malnutrition; diabetes; diuretics Weakness; irritability; decreased LOC; seizures; arrhythmias Renal failure; meds. (cathartics/antacids) = too ++ much Mg ; severe Dehydration; hypothermia Low B/P; weakness; paralysis; nausea; vomiting; altered LOC Vomiting / diarrhea; poor absorption by the body; kidney disease; diuretics, steroids, theophylline; increased + Na intake (too many + + charges = body dumps K in urine) Hypo - causes Cramps / fatigue; paralysis; nausea / vomiting; confusion; polyuria; shallow respirations; dysrhythmias Acute renal failure; burns; crush injuries; infections; All cause large shift from intracellular to extracellular Rx: Insulin, D50W, HCO3 = + shifts K intracellular Irritability; anxiety; abdominal cramping; diarrhea; weakness; paresthesia; V-fib. Excessive vomiting; dehydration; certain diuretics Muscle spasms; alkalosis; hypoventilation; coma Intracellular shifts; polyuria; alcoholism Decreased LOC; seizures; more susceptible to infections; muscle pain Information on Anions Chloride (Cl ) - HCO3 - HPO4 Major extracellular anion; diffuses easily between extra- / intracellular space; regulates osmotic pressure; follows sodium; combines with + H to form HCL; most excreted in urine Weak base in buffer system; combines with + H in metabolic acidosis; 20 bicarbonate ions for every 1 carbonic acid (normal body process cause blood to be more acidotic) Principle intracellular buffer; in bone and teeth ++ with Ca ; component of cell membranes Hypo – signs / symptoms Hyper – causes Hyper – signs / symptoms Renal insufficiency (not excreted); extracellular shifts Anorexia; nausea / vomiting; muscle weakness; hyperreflexes; tachycardia OXYGEN Mechanism of action - Increases arterial oxygen tension (PaO2) and hemoglobin saturation - Transported by hemoglobin - Enables cells to break down glucose into a usable form Indications - Chest pain - Ischemia - Hypoxemia - Cardiac arrest Contraindications - None Precautions / side effects - Low flow with COPD patients not oxygen starved - Mucous membrane irritation Administration / dosage - Nasal cannula, face masks, Venturi masks - Nasal cannula 1-6 liters/minute delivers 24-44% oxygen - Face mask - nonrebreather 10-15 liters/minute delivers 90-100% oxygen - Venturi mask delivers various % of oxygen Paramedic implications - Use humidified when possible - Use cautiously in nonhypoxic COPD patients NEVER WITHHOLD OXYGEN IF PATIENT’S ARE HYPOXIC!!!!! 1 EPINEPHRINE (1:10,000) Class: Sympathomimetic, vasopressor, bronchodilator Mechanism of Action - Catecholamine that stimulates alpha- and beta- adrenergic receptors 1. Beta1 stimulation leads to: - positive inotropic effects (↑ force of cardiac contraction) - positive chronotropic effects (↑ rate of cardiac contraction) - positive dromotropic effects (↑ conduction velocity) - 3 above help with rate post-arrest - increased cardiac output (CO) - increased myocardial oxygen requirements 2. Beta2 stimulation leads to: - peripheral vasodilation and bronchodilation 3. Alpha1 stimulation leads to peripheral vasoconstriction: - arterial / venous vasoconstriction (vasopressor) = increased SVR (perfusion pressure) - constriction to renal, mesenteric, coronary, pulmonary and cerebral vessels - makes the heart more susceptible to direct countershock in cardiac arrest (Ventricular fibrillation) (due to increased hydrostatic pressure) = reason it is given during cardiac arrest 4. Inhibits histamine release (stops degranulation) during anaphylactic reaction (Effects start within 90 seconds and are short lived) Indications 1. Asystole 2. Ventricular-Fibrillation/pulseless Ventricular-Tachycardia 3. Pulseless electrical activity (PEA) 4. Severe anaphylaxis Contraindications 1. Hypersensitvity 2. Patients with underlying cardiovascular disease 3. Tachyarrhythmias 5. Hypovolemic shock 6. Not with alkaline drugs Side Effects CNS Cardiovascular GI / GU Anxiety Anginal pain Nausea Dizziness Vomiting Dysrhythmias- LT Headache Hypertension Urinary retention Restlessness Palpitations Ischemia Subarachnoid Hemorrhage- LT Tremors Weakness Bold italics = LT = life-threatening reactions Respiratory Dyspnea 2 Skin Pallor Coldness Necrosis Urticaria Eyes Pupil dilation EPINEPHRINE (1:10,000) Precautions: 1. increased myocardial workload may lead to ischemia, infarction 2. hypersensitivity (may have increased airway resistance due to sulfites in the preparation) 3. use cautiously in patients with: - Heart disease - Diabetes - Hypertension - Given along with other sympathomimetics or with phosphodiesterase inhibitors (caffeine, amiophylline, Dipyridamole, Erectile dysfunction meds) may exacerbate dysrhythmia response 4. Deactivated with sodium bicarbonate / lasix (alkaline solutions) 5. Patients on MAO inhibitors (Marplan, Nardil, Parnate) ← (Anti-depressant drugs) – potentiates the effects How Supplied - 1mg/10ml = 1:10,000 (prefilled syringe) Administration/Dosage Administered by: - IVP, IO, ET Cardiac Arrest 1mg (1:10,000) IVP or IO Followed by a 20cc flush and raising the patients arm Repeat every 3-5 minutes Endotracheal dose 2-2.5 times the IVP dose Use 1:1,000 and place in 10cc of fluid Use ONLY if IV or IO site cannot be established May produce transient β effects = vasodilation = ↓ Coronary perfusion pressure Severe Anaphylaxis: 1.0mg SIVP (1:10,000) over 5 minutes - Repeat in 5-15 minutes PRN (as needed)) Pediatric dose: Cardiac arrest - 0.01mg/kg IVP (0.1 mL/kg) 3 DOPAMINE (INTROPIN) Class: Sympathomimetic, vasopressor Mechanism of Action Catecholamine that stimulates dopaminergic, beta and alpha adrenergic receptors (dose dependent) Naturally occurring precursor of norepinephrine 1. Low doses (dopaminergic stimulation) leads to: (0.5 to 2 µg/kg/min) – NOT used in the field - Renal, mesenteric, cerebral, coronary vasodilation - Increased urinary output 2. Intermediate doses (Beta1 stimulation) leads to: (2 to 10 µg/kg/min) - Positive inotropic response (↑ force of cardiac contractions) (β1) - Positive chronotropic response (↑ rate of cardiac contractions) (β1) - Positive dromotropic effects (↑ conduction velocity) - Increased cardiac output (CO) (β1) - Increased myocardial oxygen requirements (β1) 3. High doses (Alpha1 stimulation) leads to peripheral vasoconstriction: (10 to 20 µg/kg/min) - Arterial and venous vasoconstriction (vasopressor) - Increased SVR - Vasoconstriction to renal, mesenteric, and coronary vessels Indications 1. Cardiogenic shock 2. Neurogenic shock 3. Septic shock 4. Hypotension that occurs after return of spontaneous circulation (post-arrest) 4. Symptomatic bradycardia (refractory, not responding, to oxygen, and atropine) 5. Symptomatic heart blocks (second type II and third degree) 6. Severe CHF Contraindications 1. Not used first line for hypovolemic shock 2. Tachyarrhythmias or Ventricular-Fibrillation 3. Patients with pheochromocytoma (catecholamine producing tumor on adrenal gland) 4. Known hypersensitivity 5. Not with alkaline solutions 4 DOPAMINE (INTROPIN) Side Effects CNS Headache - C Cardiovascular Anginal pain- C Eyes Dilated pupils (high doses) Anxiety Tachycardia-C Ectopic beats, palpitations-C VasoconstrictionC Aberrant conduction Hypertension (rise in diastolic pressure) Italic = C = common side effects GI Nausea - C Vomiting- C Respiratory Dyspnea- C Skin Gangrene (high doses for a long time) Necrosis Tissue sloughing with extravasation Precautions 1. May cause increased workload on the heart 2. Hypoxia, hypercarbia, acidosis reduce drug effectiveness 3. Tissue necrosis if it infiltrates 4. High doses may cause paradoxical hypotension because the increased SVR = decrease in stroke volume (SV) and cardiac output (CO) 5. Discontinue use gradually 6. Deactivated with sodium bicarbonate / lasix (alkaline solutions) 7. Patients on MAO inhibitors (Marplan, Nardil, Parnate) ← (Anti-depressant drugs) – potentiates the effects 8. Beta blockers may blunt the inotropic effects 9. When given with phenytoin (dilantin) - hypotension, bradycardia and seizures may develop 10. Given along with other sympathomimetics or with phosphodiesterase inhibitors (caffeine, amiophylline, Dipyridamole, Erectile dysfunction meds) may exacerbate dysrhythmia response How Supplied - 200mg/5ml - 400mg/5ml - 800mg/5ml READ LABEL CAREFULLY Administration/Dosage Administered: titrate intravenous infusion (IV infusion, Piggyback) Infusion preparation 200, 400, 800mg in 250-500cc Beta Dose range 2 - 10µg/kg/minute Start at 2 – 5 µg/kg/minute Alpha Dose range 10 - 20µg/kg/minute Start at 10 -15µg/kg/minute Pediatric dose 2-20ug/kg/min IV infusion 5 NOREPINEPHRINE (LEVOPHED) Class: sympathomimetic, agonist, vasopressor Mechanism of action - Alpha1 stimulation leads to peripheral vasoconstriction: - Arterial / venous vasoconstriction (vasopressor) - Increased SVR - Vasoconstriction to renal, mesenteric, and coronary vessels - Pulmonary vasoconstriction - Beta1 stimulation leads to: - Positive inotropic response (↑ force of cardiac contractions) (β1) - Positive chronotropic response (↑ rate of cardiac contractions) (β1) - Positive dromotropic effects (↑ conduction velocity) - Increased myocardial oxygen requirements - Increased cardiac output (due to ↑ inotropic + chronotropic + dromotropic effects) PREDOMINATELY ALPHA1 STIMULATING DRUG Indications - use if other vasopressors are not working – severe hypotension SBP < 70mmHg – drug of last resort 1. Cardiogenic shock 2. Neurogenic shock 3. Septic shock 4. Poison / Drug induced hypotension 5. Blood pressure support after resuscitation from cardiac arrest - if B/P is low due to ↓ PVR Not used to treat hypovolemia Contraindications 1. Hypotension due to hypovolemia (need appropriate fluid replacement first) 2. Profound hypoxia 3. Profound hypercarbia 4. Hypertension 5. Hypersensitivity Side effects CNS Cardiovascular Headache- C Reflex bradycardia Restlessness Dysrhythmias - LT Tremor Chest pain LT Dizziness Hypertension Anxiety Palpitations Tachycardia Decreased CO Italic = C = common side effects GI GU Respiratory Eyes Skin Nausea - C Oliguria Distress Photophobia Diaphoresis Vomiting- C Renal failure Dyspnea Gangrene Organ ischemia Organ ischemia Apnea Necrosis (with infiltration) Bold italic = LT = life-threatening reaction 6 NOREPINEPHRINE (LEVOPHED) Precautions 1. Increases myocardial workload and oxygen consumption 2. If it infiltrates it can cause tissue necrosis 3. May contribute to hypoxia due to pulmonary vasoconstriction 4. Use cautiously with: - Cardiogenic shock - Acute MI - CHF - In the presence of hypoxia, hypercarbia, acidosis - MAO inhibitor therapy within 14 days (Marplan, Nardil, Parnate) ← (Anti-depressant drugs) - Beta adrenergic antagonists blunt the Beta1 effects How supplied - 4mg / 4ml Administration / dosage Administered – IV infusion (piggyback) Infusion preparation Mix: 4mg / 250cc D5NS Dosage range 0.5 to 30µg / minute Start infusion at 0.5 to 1µg / minute Titrate to a B/P of 90-110 mmHg Higher doses may be needed for Poison / Drug induced hypotension CONSTANTLY ASSESS HEMODYNAMIC STATUS 7 VASOPRESSIN Class: Hormone, Vasopressor, Antidiuretic Mechanism of Action 1. 2. - Non-adrenergic vasoconstrictor stimulates smooth muscle (V1 receptors) Increases: coronary perfusion pressure (hydrostatic pressure) vital organ blood flow ventricular fibrillation frequency (amplitude of the waves – may turn fine VF into coarse VF) cerebral oxygen delivery Vasoconstricts better than epinephrine with hypoxia and acidosis present – effects last longer Produces greater arteriole tone than epinephrine Does not increase myocardial O2 consumption like epinephrine (post-arrest) Indications Prehospital: - Ventricular fibrillation / Pulseless ventricular tachycardia (may replace 1st or 2nd dose of Epinephrine) (one dose) - May be useful alternative to epinephrine in Asystole / PEA (may replace 1st or 2nd dose of epinephrine) (one dose) Other Uses: - Control bleeding with esophageal varicies - Distributive shock (high-space) →Septic shock Contraindications - ischemic heart disease PVCs = ischemia or necrosis Advanced arteriosclerosis During 1st stage of labor Side effects CNS Drowsiness Cardiovascular Angina GI Cramps Flushing Headache Lethargy Arrest = LT ↓ CO Dysrhythmias = LT Heartburn Nausea Vomiting GU Uterine cramping Respiratory Bronchial constriction Skin Sweating Urticaria Gangrene Tremors Vertigo Gangrene ↑ BP MI = LT Peripheral vasoconstriction Italic = C = common side Bold italic = LT = life-threatening reactions 8 VASOPRESSIN Precautions - - Use cautiously in patients with: - Epilepsy - Migraine - Asthma - Heart failure - Angina - Vascular disease - Renal disease The young and old How supplied - 20 Units / ml Administration / Dosage Administered – IVP; IO; ET Dose: Cardiac arrest – 40 U - IVP / IO (only give one dose) ET dose: 2 – 2.5 x IV dose in 10 cc of fluid 9 PROPRANOLOL (INDERAL) Class: Non-selective beta-adrenergic blocker (β1and β2), sympatholytic, antihypertensive, antianginal Mechanism of Action 1. Blocks Beta1 receptors leading to: - depressed automaticity at the SA node - decreased AV node and intraventricular conduction - decreased heart rate and force of contraction - decreased myocardial O2 consumption - decreased blood pressure 2. Blocks Beta2 receptors leading to: - possible bronchoconstriction 3. Decreases renin release from the kidneys (Blocks Beta1 receptors in kidneys) - vasodilation Indications 1. Supraventricular Tachyarrhythmias (refractory to other therapies – vagal maneuver, and adenosine) 2. To prevent recurrent Ventricular Tachycardia 3. Atrial-Fibrillation/Atrial-Flutter with a rapid ventricular response 4. MAT – Multifocal Atrial Tachycardia 5. To prevent angina 6. To treat hypertension Contraindications 1. Asthma / COPD 2. Bradycardia / heart blocks (second and third degree) 3. CHF patients 4. Cardiogenic shock 5. Any patient with depressed cardiac function 6. Cocaine intoxication Side Effects CNS Depression Cardiovascular Bradycardia GI Diarrhea Dizziness- C CHF- LT Dry mouth Drowsiness Fatigue - C Cold extremities Postural Hypotension Hallucinations Profound hypotension Insomnia 2nd or 3rd heart block - LT Lethary - C Vasodilation Italic = C = common side effects Eyes / Ears Dry, burning eyes Visual disturbances Metabolic Hypoglycemia Nausea - C Vomiting Respiratory Bronchospasms Dyspnea Wheezing Bold italic = LT = life-threatening reactions 10 PROPRANOLOL (INDERAL) Precautions - diabetes mellitus renal / hepatic disease peripheral vascular disease history of systemic insect sting reaction (anaphylactic reactions) may mask the symptoms of hypoglycemia (except sweating) in the diabetic patient myasthenia gravis How Supplied - 1mg/1ml Administration/Dosage Administered - Slow IVP Initial Dose 1-3 mg Slow IVP (over 2-5 minutes) May dilute in 9ml to deliver easier Subsequent Dose May repeat dose in 2 minutes Total Dose 0.1 mg/kg 11 Metoprolol (Lopressor) Class: Beta Blocker: Selective beta adrenegeric (β1) mainly in the cardiac muscle, sympatholytic, antihypertensive, antianginal; Does not usually affect β2 receptors; Mechanism of Action 1. Beta-blocking activity of metoprolol as shown by - HR and CO at rest and upon exercise - SBP upon exercise - Inhibition of isoproterenol-induced tachycardia -reflex orthostatic tachycardia. 2. For Antihypertensive effects - Antagonizes catecholamines at peripheral adrenergic receptors leading to cardiac output - Central effect leading to sympathetic outflow to the periphery - Suppression of renin activity – at higher doses - Blocking catacholamine-induced HR and velocity = decreased myocardial contraction and BP - O2 requirements of heart - making it useful for angina pectoris 4. At higher dosages, will inhibit B2 in bronchial and vascular musculature. Indications 1. Hypertension 2. Angina pectoris 3. Prevention of MI 4. Decreased Mortality of Recent MI 5. CHF 6. Stable Narrow complex tachycardia – second line after vagal maneuver and Adenosine 7. Rate control in atrial fibrillation and atrial flutter and MAT Contraindications 1. Uncompensated CHF 2. Pulmonary Edema 3. Cardiogenic Shock 4. Bradycardia or heart block 5. hypersensitivity to B-Blockers 6. Lung disease with bronchospasm 12 Metoprolol (Lopressor) (con’t) Side Effects CNS Fatigue - C Weakness Cardiovac. Bradycardia=LT CHF = LT GI / GU Nausea=C Vomiting=C Eyes/Ears Blurred vision Stuffy nose Depression Insomnia Nightmare Pulm Edema Diarrhea=C Hypotension Constipation Vasoconstriction in Dry mouth extremities Dizziness - C Cardiac Arrest=LT Impotence Common side effect =C bold italics = LT = life-threatening reactions Precautions Renal impairment Diabetes Mellitus COPD/ Asthma Heart failure CAD Well compensated CHF Hepatic disease How Supplied 5mg/5cc ampule Administration/Dosage Administered: Slow IVP over 1 minute Initial Dose 5mg IVP Subsequent Dose Repeat in 5min x 3 doses Total Dose 15mg 13 Metabolic Hyperglycemia Masked hypoglycemia response Respiratory Bronchospasm=LT Wheezing dyspnea Atenolol (Tenormin) Class: Beta Blocker, selective B1, B2 only at high doses Mechanism of Action 1. Blocks stimulation of beta1 receptors 2. doesn’t affect B2 3. negative chronotropic and inotropic (increases rate of SA node, increases recovery time) 4. slows AV conduction time 5. HR 6. O2 consumption 7. renin-aldosterone, angiotension system at high doses Indications Hypertension, Angina Prevention of MI Stable Narrow complex tachycardias - second line after vagal maneuver and Adenosine Rate control in atrial fibrillation and atrial flutter and MAT Contraindications Hypersensitivity to B-Blockers Uncompensated CHF Pulm edema Cardiogenic shock Bradycardia or heart block, 2nd/3rd Side Effects CNS Fatigue=C Weakness=C Cardiovac. Bradycardia / Heart block =LT CHF=LT GI / GU Nausea=C Eyes/Ears Blurred vision Metabolic Hyperglycemia Respiratory Bronchospasms Vomiting Stuffy nose Masked hypoglycemic response Wheezing Depression=C Insomnia=C Nightmare Pulm Edema=LT Diarrhea=C Hypotension=LT Constipation Vasoconstriction Dry mouth Cardiac Arrest Impotence Common side effect =C bold italics = LT = life-threatening reactions Precautions Renal impairment Geriatric (reduce dose) Pulm Disease,-COPD/Asthma Diabetes Mellitus Thyroid disease Well compensated CHF 14 Dyspnea Atenolol (Tenormin) How Supplied 500mcg/cc (0.5mg) Administration/Dosage Administered: Slow IVP over 5 minutes Initial Dose 5mg over 5min Subsequent Dose Repeat in 5mg in 10 min; give over 5min 15 Total dose 10 mg LIDOCAINE (XYLOCAINE) Class: Class I-B Antidysrhythmic, local amide-type anesthetic Mechanism of Action 1. Blocks fast sodium channels leading to decreased automaticity in the bundle of His and purkinje system - During pathological states – keeps Na++ from entering cells during Phase 4 2. Shortens repolarization times (refractory period) (does not block K+ = refractory period is NOT slowed) 3. Anesthetic properties help to suppress ventricular ectopy after MI 4. Decreases conduction velocity through ischemic zones in the ventricles 5. May terminate reentry ventricular arrhythmias 6. Raises the ventricular fibrillation threshold Indications 1.Ventricular-Fibrillation / Pulseless Ventricular-Tachycardia (IF amiodarone is NOT available) 2. Stable Ventricular-Tachycardia of unknown origin 3. Post Arrest Ventricular irritability (if rate and rhythm support lidocaine) (ensure oxygenation first) Contraindications 1. Bradycardia with PVC’s 2. Heart blocks (second or third degree) (Stokes-Adams syndrome) 3. Idioventricular rhythms 4. Wolff-Parkinson-White syndrome / Supraventricular Tachycardia 5. Hypersensitivity to amide anesthetics Do not use prophylactically Side Effects CNS 1. paresthesia 2. Dizziness = C 3. Slurred speech 4. Drowsiness Cardiovascular Bradycardia = LT Collapse Edema Heart Block = LT Hypotension = C 5. Altered LOC 7. Muscle twitching 8. Seizures = LT Italic = C = common side effects Eyes / Ears 6. Tinnitus 6. Blurred vision GI Nausea Vomiting Respiratory 9. Depression = LT 9. Arrest = LT Bold italic = LT = life-threatening reactions (Numbers indicate signs of increasing toxicity) IF USED IN THERAPEUTIC DOSES THESE PROBLEMS USUALLY DON’T OCCUR 16 Skin Rash Edema Urticaria LIDOCAINE (XYLOCAINE) Precautions 1. May cause (or worsen) ventricular dysrhythmias or cause asystole when administered to patients with: - Sinus bradycardia - Heart blocks - Atrial fibrillation or atrial flutter with accelerated ventricular response - Junctional rhythm 2. Effectiveness is reduced in the presence of: - hypoxia - electrolyte imbalances - acid-base disturbances 3. Use cautiously on: - patients with respiratory depression, hypovolemia - Elderly patients and patients with liver problems, CHF, or cardiogenic shock - patients taking beta blockers How supplied - Ampule and prefilled syringes for IVP - Vials of 1-2gm for IV infusions READ LABEL CAREFULLY SO YOU ADMINISTER THE PROPER AMOUNT Administration/Dosage Administered by – IVP / IO, ET or IV Infusion (piggyback) IVP / IO dose Initial (loading) dose – 1-1.5mg/kg Subsequent dose – 0.5-0.75mg/kg ET dose 2-2.5 times the IVP dose in 10cc Use ONLY if IV site is unavailable IV infusion Infusion preparation – 1-2gm / 250 or 500cc Dose range – 1-4mg / minute Total dose - 3mg/kg - Repeat IVP dose every 3-5 minutes - Elderly patients and patients with liver problems, CHF, or cardiogenic shock – deliver initial loading dose (1-1.5mg/kg) - deliver infusion at ½ the normal range - BOLUS PRIOR TO INFUSION INFUSIONS ARE ONLY USED ON PULSING PATIENTS Pediatric dose: 1mg/kg IVP, IO, ET 17 PROCAINAMIDE (PRONESTYL) Class: Class I-A antidysrhythmic, ester-type local anesthetic Mechanism of Action 1. Blocks slow sodium channels (SA and AV nodes) leading to decreased automaticity (atrial) 2. Blocks fast sodium channels (muscle cells and ventricular conduction system) to decrease muscle depolarization (ventricular) 3. Prolongs repolarization time in the conduction system (blocks K+ = slows repolarization) 4. Conduction velocity is decreased in the atrium, bundle of his and purkinje fibers - 3 and 4 lead to prolonged QT intervals 5. Contractility may be decreased in a damaged myocardium = decreased delivery of stroke volume 6. Produces peripheral vasodilation - with rapid IVP or toxic levels drug blocks Na+ and ACh decreasing smooth muscle depolarization 7. Increase the Ventricular fibrillation threshold Indications 1. Stable pulsing ventricular tachycardia (monomorphic / polymorphic – unknown origin) (class IIb) 2. Stable Supraventricular dysrhythmias (not controlled by vagal maneuvers and adenosine) 3. Pharmacological conversion of Atrial fibrillation (with rapid ventricular response in WPW syndrome) 4. Ventricular irritability post arrest (if rate and rhythm support the drug) (if not controlled by Lidocaine) Contraindications 1. Bradycardia with PVC’s 2. Heart blocks (second and third degree) 3. Idioventricular rhythms 4. Torsades de pointes (due to QT prolongation) 5. Digitalis toxicity (may further depress conduction) 6. Tricyclic Antidepressant toxicity 7. Hypersensitvity Side effects CNS Depression Cardiovascular Hypotension GI Abdominal pain Dizziness = C Heart blocks = LT Anorexia Giddiness Hallucinations Headache Q-T Prolongation Torsades de points Ventricular arrhythmias = LT Bitter taste Diarrhea Hepatomegaly Psychosis Weakness Italic = C = common side effects Blood Reduction in: neutrophils, basophils, eosinophils = LT ThromboCytopenia = LT Nausea Vomiting Bold Italic = LT = life-threatening reaction 18 Respiratory Dyspnea Skin Angioneurotic edema = LT Depression = LT Flushing Arrest = LT Pruritis Rash Urticaria PROCAINAMIDE (PRONESTYL) Precautions 1. May precipitate / worsen AV heart block 2. May cause ventricular arrhythmias 3. May cause hypotension (due to Na+ and ACh blocking with rapid IVP or toxic levels in the system) 4. Effectiveness is reduced in the presence of: - hypoxia - electrolyte imbalance - acid-base disturbances 5. Use cautiously with: - liver / kidney impairment - acute MI - CHF - digitalis toxicity - asthma – due to anticholinergic effect (inhibits secretions = thickens mucus secretions (plugs)) 6. Conversion of atrial fibrillation may lead to clot dislodgement and PE developing How supplied - 1000mg/10ml (for IVP) - 1gm/2ml (for infusion) Administration / dosage Administered - Slow IVP and IV infusion Slow IVP 20-50mg SIVP (over 1 minute) May dilute in 10cc to facilitate delivery Total dose: 17 mg/kg - SIVP until: IV Infusion Infusion preparation – 1-2gm / 250 or 500cc Dose range – 1-4mg / minute 1. dysrhythmia is suppressed 2. hypotension develops 3. QRS widens more than 50% 4. 17mg/kg have been given If any of the above 4 occurs – discontinue temporarily – contact physician BOLUS PRIOR TO THE INFUSION IV INFUSION USED AFTER CONVERSION OR MALIGNANCY HAS CLEARED INFUSIONS ONLY USED ON PULSING PATIENTS REDUCE MAINTENANCE INFUSION RATE WITH LIVER AND KIDNEY DYSFUNCTION Pediatric dose: - 15mg/kg slow IVP / IO (over 30 to 60 minutes) 19 AMIODARONE (CORDARONE) Class: Antidysrhythmic Mechanism of Action 1. Acts directly on all cardiac tissue. 2. Blocks Na+, Ca++, K+ and alpha and beta receptors - Prolongs duration of action potential and refractory period = QT prolongation - Decreases - automaticity, conductivity, contractility - Relaxes coronary and vascular smooth muscle = - Decreases peripheral vascular resistance - Increases coronary blood flow 3. Useful for the treatment of atrial and ventricular arrhythmias Indications for Use 1. Ventricular fibrillation / Pulseless ventricular tachycardia (class IIb) 2. Stable ventricular tachycardia (monomorphic) 2. Stable recurrent ventricular tachycardia (polymonorphoric) with normal QT segment (MAY be effective) 3. Rate control for atrial fibrillation / atrial flutter in patients with CHF (potential risk of conversion to sinus rhythm should be considered) Contraindications 1. Hypersensitivity 2. Bradycardia 3. High degree heart blocks (second and third degree) 4. Cardiogenic shock 5. Pulmonary congestion Side Effects CNS Cardiovascular Respiratory GI Musculoskeletal Skin Fatigue Conduction abnormalities = LT Dysrhythmias = LT Bradycardia - C Cough Nausea Pain in extremities Slate-blue pigmentation Eyes, Ears, Nose, Throat Blurred vision Dyspnea Vomiting Weakness Rash Dry eyes Pulmonary fibrosis - LT Inflammation Diarrhea Photosensitivity Halos HeadacheC Dizziness C Insomnia Ataxia Paresthesia Hypotension SA node dysfunction = LT Sinus arrest = LT Malaise CHF Italics = C = common side effect Abdominal pain Anorexia Loss of vision Photophobia Hepatoxicity Corneal / macular degeneration Constipation Bold Italics = LT = life-threatening reactions 20 AMIODARONE Precautions 1. Thyroid disease (can cause hypo- or hyperthyroidism) 2. 2nd or 3rd degree heart block (slow or stop infusion if seen) 3. Electrolyte imbalances (↓K+ and ↓Mg++ - may predispose to arrhythmias) 4. Bradycardia (slow or stop infusion if seen) 5. Pulmonary disease 6. May produce vasodilation and hypotension 7. May have (-) inotropic effects 8. May prolong QT interval = possible development of Torsades de Pointes How supplied - 150mg / 3cc (50mg / ml) Administration/Dosage Administered: slow IVP and IV infusion Initial (loading) dose CARDIAC ARREST 300 mg slow IVP over 3-5 minutes Dilute in 20-30cc NS Subsequent doses CARDIAC ARREST 150 mg slow IVP in 3-5 minutes PULSING TACHYCARDIAS 150 mg / 100cc over 10 minutes PULSING TACHYCARDIAS May repeat in 10 minutes, PRN Dilute in 20-30cc NS Pediatric dose: - Cardiac arrest: 5mg/kg rapid IVP - Perfusing tachycadias: 5mg/kg over 20-60 minutes - Maximum dose – 15 mg/kg 21 Total Dose CARDIAC ARREST 2.2 gm IV / 24 hours MAGNESIUM SULFATE (CARDIAC) Class: Electrolyte, Anticonvulsant Mechanism of Action 1. CNS depressant 2. Believed to reduce the release of ACh by motor nerves so seizure activity is decreased (↓ grand mal activity) 3. Slows HR at the SA node, prolongs AV node conduction time = ↓ dromotropy 4. Causes peripheral vasodilation (Ca++ channel blocking properties) 5. Stabilize cell membranes (__↓__ Mg++ levels = ___↓__ membrane threshold potentials = ___↑___ cellular & Purkinje fiber excitability = ___↑___ chance for arrhythmia development) 6. Necessary for Na+ / K+ pump function Indications 1. Hypomagnesemia 2. Torsades de pointes 3. Hypokalemia - Needed to replenish intracellular K+ 4. Ventricular fibrillation / Pulseless VT – associated with torsades de pointes or hypomagnesemia 5. Severe asthma attack (Phase II / Status asthmaticus) Contraindications 1. Renal disease 2. Shock 3. Heart block 4. Hypocalcemia 5. Hypermagnesemia Side effects CNS Cardiovascular GI Metabolic Decreased B/P - C Belching Hypermagnesemia Coma = LT Depressed deep Cramps Heart block - LT tendon reflexes - C Depression - C Bradycardia - C Lethargy - C Increased pulse - C Weakness - C Decreased SVR - C Italic = C = common side effects Bold italic = LT = life-threatening reactions Respiratory Depression – LT Arrest - LT Paralysis - LT CALCIUM CHLORIDE / CALCIUM GLUCONATE ANTAGONIZES = HAVE AVAILABLE Precautions 1. May cause CNS depression and hypocalcemia 2. Rapid IV injection may cause hypotension, heart block, cardiac and/or respiratory arrest 3. Renal impairment may increase chance of toxicity How Supplied - 10%, 12.5%, 50 % solution in 40, 80, 100, and 125 mg/mL 22 MAGNESIUM SULFATE (CARDIAC) Administration/Dosage Adult: - Ventricular Fibrillation / pulseless Ventricular Tachycardia = 1-2gm (2-4 mL) / 10ml D5W slow IVP / IO (over 1-2 min.) (50% solution) - Torsades de Pointes (with a pulse) = 1-2 grams in 50 to 100 cc D5W slow IVP over 5 to 60 minutes Pediatric: - 25 – 50 mg/kg over 10-20 minutes - Max. dose = 2 grams 23 ADENOSINE (ADENOCARD) Classification: antidysrhythmic Mechanism of Action 1. Decreases conduction of electrical impulse through the AV. node. (keeps K+ in and Ca++ out in SA & AV nodes leads to hyperpolarization of the SA / AV nodes = ↓ SVT rates) 2. Interrupts AV re-entry pathways (causing paroxysmal supraventricular tachycardia (PSVT)) 3. Slows sinus rate 4. Only works on tachycardias produced by re-entry pathways (PSVT / Wolfe-Parkinson White (WPW)) 5. Found naturally in all body cells 6. Rapidly metabolized in the blood vessels (endothelium and RBCs) Indications 1. Convert stable PSVT to NSR (if oxygen and vagal maneuvers do not work) 2. Convert Wolff-Parkinson-White (WPW) to NSR • Have defibrillator available – could convert to Atrial Fibrillation with rapid ventricular response – may need to cardiovertConvert Stable 3. Junctional tachycardia (if oxygen and vagal maneuvers do not work) 4. May consider for unstable narrow-complex tachycardias while preparing for cardioversion (ONE dose) 5. Stable Monomorphic wide-complex tachycardias (could be SVT with aberrancy) (2 doses) Contraindications 1. Patients who are hypersensitive 2. Second or third degree heart block 3. Sick sinus syndrome 4. Atrial fibrillation 5. Atrial flutter 6. Ventricular Tachycardia (unstable) 7. Tachycardia associated with asthma attack 8. Poison / drug induced tachycardia Side Effects (self limiting due to short half-life) CNS Apprehension Cardiovascular GI Metallic taste Atrial tachydysrhythmiaLT Arm tingling Chest pain Nausea Blurred vision Facial flushing- C Throat tightness Dizziness, lightheaded Hypotension Numbness Palpitations Sweating Italics = C - common side effect Bold Italics = LT - life-threatening reactions Respiratory Dyspnea- C Bronchoconstriction Hyperventilation - HALF-LIFE IS 5 – 10 SECONDS Precautions 1. May produce brief periods of heart blocks, asystole (up to 15 seconds), PVC's, PAC's, bradycardia or tachycardia. 2. Arrhythmias only last a few seconds due to the short half-life 3. Patients on theophylline (xanthine bronchodilator) / caffeine – require higher doses 4. Patients with transplanted hearts – require smaller doses (3mg – ½ dose) 5. Patients on dipyridamole and carbamazepine (inhibits thromboxane A2 = antiplatelet drug) – require smaller doses (3mg = ½ dose) 24 ADENOSINE (ADENOCARD) How supplied - 6mg in 2ml Administration/dosage Administered: RAPID IV push – Elevate legs post delivery. Draw up adenosine dose and flush in 2 separate syringes Attach both syringes to IV port closest to patient – clamp IV tubing Push IV Adenosine as quickly as possible – keep pressure on Adenosine plunger – push NS flush as rapidly as possible Initial Dose 6mg rapid IV push (1-3 seconds) Subsequent Doses – (1-2 minutes later) 12mg rapid IV push (1-3 seconds) FOLLOW EACH DOSE WITH A 20 CC BOLUS Doses are delivered 1-2 minutes after each other, if the patient does not convert Maximum single dose – 12 mg Pediatric dose - Initial dose: 0.1mg/kg IVP followed by 5ml flush - Second dose: 0.2mg/kg IVP followed by 5ml flush Maximum 1st dose – 6 mg 25 Total Dose 18mg CALCIUM CHLORIDE Class: Electrolyte Mechanism of Action 1. Necessary for: - transmission of nerve impulses - contraction of cardiac muscle, smooth muscle, skeletal muscle - renal function - blood clotting - regulation of neurotransmitter and hormones storage and release - maintaining structural and functional integrity of cell membranes and capillary beds 2. Causes significant increase in myocardial contractility and ventricular automaticity 3. IVP administration improves vascular tone and myocardial contractility in hypocalcemic states 4. May increase or decrease peripheral vascular resistance (PVR) Indications 1. Hyperkalemia (except when associated with digitalis toxicity) 2. Hypocalcemia 3. Hypermagnesemia 4. Calcium channel blocker overdose 5. Cardiac arrest resulting from: hypocalcemia, hyperkalemia, or overdose on calcium channel blocking drugs 6. Antidote for toxic effects from beta-blocking toxicity 7. To prevent hypotensive effects of calcium channel blocking agents (verapamil and diltiazem) Contraindications 1. Cardiac arrest (not caused by hypocalcemia, hyperkalemia, or overdose on calcium channel blocking drugs) 2. Hypercalcemia 3. Not with sodium bicarbonate 4. Digitalis toxicity (calcium concentrations will be elevated due to toxicity) 5. Renal or cardiac disease Side effects Cardiovascular Bradycardia GI Gastric irritation GU Renal dysfunction Cardiac Arrest - LT Anorexia Renal Failure- LT Constipation Dysrhythmias - LT Heart block Flatulence Hypotension Nausea / Vomiting Rebound Diarrhea Hypertension Shortened Q-T Bold Italics – LT = life-threatening reactions Metabolic Hypercalcemia (coma) - LT Metabolic Alkalosis Renal stones 26 Skin Burning at the IV site Tissue necrosis (if it infiltrates) Pain CALCIUM CHLORIDE Precautions 1. Rapid injection may cause: hypertension, dysrhythmias, bradycardia, cardiac arrest 2. Coronary and cerebral vasospasms 3. Use cautiously on patients: - with renal disease - with cardiac disease - with COPD - on digitalis - with GI obstruction or decreased motility 4. Flush line between calcium and sodium bicarb to avoid precipitation How Supplied - 1gm/10ml (10ml of 10% solution) Administration/Dosage Administered: slow IVP - 8-16 mg/kg (usually 5-10 cc) slow IVP - repeat the dose in 10 minutes, prn Pediatric dose: - 20 mg/kg (0.2 cc/kg) slow IVP of a 10% solution – repeat once in 10 minutes for documented conditions 27 VERAPAMIL (ISOPTIN, CALAN) Class: Ca++ channel blocker, antidysrhythmic, antihypertensive, antianginal Mechanism of action 1. Inhibits movement of calcium ions across cell membranes during depolarization - Decreases afterload – dilation of arterioles - Dilates coronary arteries - Depresses myocardial contractility 2. Inhibits coronary vasospasm 3. Slows SA and AV node conduction - Decreases atrial automaticity / AV conduction and prolongs AV node refractory period (will prolong PR interval) - May cause high degree heart blocks (second and third degree) 4. Decreases myocardial oxygen requirements Drug has greater effect on conduction system than the smooth muscle Indications 1. 2. 3. SVT / Junctional Tachycardia - after adenosine Atrial-fibrillation or atrial-flutter with rapid ventricular response / Mulitfocal Atrial Tachycardia Angina - Prinzmetal’s angina - Chronic stable angina - Preinfarction angina (make sure patient is hemodynamically stable) Hypertension 4. Contraindications 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. Hypersensitivity Cardiogenic shock Severe CHF Sick sinus syndrome Bradycardia Heart blocks (second and third degree) Severe hypotension (< 90 mmHg) Acute myocardial infarction (unless associated with SVT) Wolff-parkinson-white syndrome (WPW) with atrial fibrillation or flutter Ventricular tachycardia (all-wide complex tachycardias) Side effects CNS Dizziness Headache Lightheadedness Blurred vision Cardiovascular GI Constipation AV block = LT Bradycardia Nausea CHF= LT Edema Hypotension Palpitations Italic = C - common side Bold italic = LT = life-threatening reactions 28 GU Nocturia Polyuria Respiratory Dyspnea Shortness of breath VERAPAMIL (ISOPTIN, CALAN) Precautions 1. Run a 12-lead EKG prior to administration 2. Use cautiously with: - Liver impairment - Older adults - Patients on digitalis or beta blocker - CHF - Cirrhosis - Duchenne’s muscular dystrophy 3. Concurrent with IV Beta blocker may produce severe hypotension - Use with extreme caution in patients receiving oral β-blockers How supplied - 5mg / 2ml Administration / dosage Administered - Slow IVP (over 1-2 minutes) Initial dose 2.5 to 5mg SIVP Subsequent dose – 15 to 30 minutes after initial dose 5 to 10mg SIVP - PRN Total dose 20mg Within 30 minutes - MAKE SURE SYSTOLIC PRESSURE IS AT 100 mmHg OR HIGHER PRIOR TO ADMINISTRATION - CONSTANTLY REASSESS HEMODYNAMIC STATUS - IV calcium may restore blood pressure in toxic cases (some may give calcium prior to avoid ↓ BP and HR) Pediatric dose: - 0-1 year: 0.1-0.2mg / kg slow IVP (max. dose 2mg) - 1-15 years: 0.1-0.3mg / kg slow IVP (max. dose 5mg) 29 Diltiazem (Cardiazem) (dil-tye-a-zem) Class: Calcium Channel Blocker Mechanism of Action 1. Inhibits calcium ion influx across the cell membranes during depolarization -Systemic vasodilation resulting in BP -Coronary vasodilation resulting in frequency and severity of attacks of angina -Suppression of arrhythmias -Relaxes coronary vascular smooth muscles -Slows SA/AV conduction times; dilates peripheral arteries Indications Stable Supraventricular Dysrhythmia – after adenosine Rapid Ventricular rates in: - Atrial fibrillation - Atrial flutter - Multifocal Atrial Tachycardia Contraindications Hypersensitivity Sick Sinus Syndrome 2nd/3rd degree Block BP < 100 mmHg Recent MI or pulmonary congestion WPW – with atrial fib or flutter Cardiogenic shock Concomitant use of IV β-blockers Wide complex tachycardias Poison or drug induced tachyarrhythimas Side Effects CNS Dizzy Drowsiness=C Headache=C Nervousness Abnormal dreams Cardiovac. Arrhythmias=LT CHF=LT Peripheral edema=C Bradycardia=LT Hypotension Palpitations common side effect = C GI Nausea=C Vomiting Diarrhea Constipation=C GU Nocturia Acute renal failure=LT Sexual dysfunction polyuria bold italics = LT - life-threatening reactions 30 Respiratory Cough Dyspnea Diltiazem (Cardiazem) Precautions: Severe hepatic dysfunction/injury Geriatric patients (reduced dose) Severe renal insufficiency History of serious ventricular dysrhythmias CHF Hypotension How Supplied 25mg / 5cc vial / 50mg / 10cc vial Administration/Dosage Administered: slow IVP over 2 minutes Initial Dose 0.25mg/kg SIVP - over 2 mintues Subsequent Dose Repeat in 15 minutes 0.35mg/kg - over 2 minutes 15-20 mg for average patient 20-25 mg for average patient Maintenance Dose Maintenance Dose: 125mg (25cc) / 100cc Infuse at: 5-15 mg/hour Titrate to HR Diltiazem is incompatible with Lasix – don’t administer simultaneously MAKE SURE SYSTOLIC PRESSURE IS AT 100 mmHg OR HIGHER PRIOR TO ADMINISTRATION - CONSTANTLY REASSESS HEMODYNAMIC STATUS 3 ATROPINE SULFATE Class: Anticholinergic (parasympatholytic); GI antispasmodic Mechanism of Action - Inhibits action of acetylcholine at the muscarinic receptors located within the myocardium, smooth muscle, and glands causing: 1. Increased SA node automaticity + Enhanced AV node conduction = Accelerated heart rate = Improved cardiac output (chronotropic / dromotropic effects) – (affects rate NOT force of contraction) 2. Will reduce SLUDGE effects of Organophosphate overdose: decreases body secretions - S = excessive salivation (drug will stop this) - L = excessive lacrimation (drug will stop this) - U = excessive urination (drug will stop this) - D = excessive defecation (drug will stop this) - G = increased gut motility (drug will stop this) - E = emesis (drug will stop this) 3. Decreased GI / GU motility 4. Relaxes bronchial smooth muscles (bronchodilation) 4. Dilated pupils Indications 1. Symptomatic bradycardia 2. Symptomatic heart blocks (first degree and second type I) **** 3. Organophosphate poisoning – Large doses may be needed 4. Nerve gas poisoning (sarin, soman) – Large doses may be needed *****2nd type II and 3rd degree HB = Transcutaneous pacing (TCP) or sympathetic infusion is best for these patients******* Contraindications 1. Hypersensitivity 2. Narrow angle acute glaucoma 3. GI obstruction 4. Tachycardia 5. Prostatic enlargement 6. Myocardial ischemia 7. Thyrotoxicosis Side effects CNS Anxiety Confusion Dizziness Drowsiness, Coma Cardiovascular Angina PVC’s Tachycardia = LT Hyper - or Hypotension Eyes Blurred vision Eye pain Glaucoma Photophobia Psychosis / Hallucinations Paradoxical Bradycardia Pupil dilation Weakness Headache Bold italics = LT = Life threatening Eye dryness 32 GI Anorexia Constipation Dry mouth Abdominal distention / pain Decreased gut motility – Paralytic Ileus LT Nausea Vomiting GU Dysuria Impotence Retention Skin Flushing Dry skin Rash Decreased or absent sweating Urticaria ATROPINE SULFATE Precautions: 1. Hypersensitivity 2. Use cautiously in patients with: - Coronary artery disease (CAD) - Congestive heart failure (CHF) - COPD (due to decreased bronchiole secretions = increased mucus plugging) - Patients with fever or exposed to high temperatures 3. Large doses: - Decrease GI motility - Inhibit gastric acid secretion - May block nicotinic receptors at the neuromuscular junctions = possible respiratory depression How supplied - Prefilled syringes containing 1mg/10ml (0.1mg/ml) CHECK THE CONTAINER FOR CONCENTRATION Administration/dosage Administered: IVP = IV push / IO Symptomatic Bradycardia 0.5 IVP Repeat the dose every 3-5 minutes Total dose: 3mg Organophosphate Poisoning 1-2 mg IVP IVP dose repeated every 5 -15 minutes until secretions are decreased IM dose may be given if IV site is not available Large doses 2-4 mg or more may be needed E.T. Dose 2 to 2.5 times the IVP dose Repeat every 3-5 minutes Total dose: 3mg (2-3 doses 1-1.5 mg each time) ONLY USED IF YOU CAN’T START AN IV. NEVER GIVE TOO SLOWLY OR LESS THAN 0.5MG IN A SINGLE BOLUS TO THE ADULT PATIENT Pediatric doses: - Bradycardia: 0.02mg/kg (0.2cc/kg) IVP / IO - maximum single dose (bolus): 0.5mg (child) and 1.0mg (adolescent) - maximum total dose: 1mg (child) and 2mg (adolescent) vm - Organophosphate Poisoning < 12 years old - 0.02 - 0.05mg/kg IV / IO every 20-30 minutes – until symptoms reverse > 12 years old – 2 mg IV / IO then 1-2 mg IV / IO every 20-30 minutes – until symptoms reverse NEVER GIVE LESS THAN 0.1MG IN A SINGLE BOLUS IN THE PEDIATRIC PATIENT 33 CARDIAC GLYCOSIDES ONE OF THE OLDEST MEDICATIONS KNOW TO HUMANS. THEY INCREASE FORCE (INOTROPIC) OF CONTACTIONS. WHEN USED FOR CHF THEY INCREAS CARDIAC OUTPUT BY REDUCING LEFT VENTRICULAR DIAMETER AND DECREASE VENOUS PRESSURE. THESE EVENTS HASTEN THE REDUCTION OF PERIPHERAL AND PULMONARY EDEMA. THE THERAPEUTIC INDEX (THERAPEUTIC DOSE / TOXIC DOSE) OF DIGITALIS IS LOW, SO THE POSSIBILITY OF DIGITALIS TOXICITY SHOULD ALWAYS BE CONSIDERED WITH PEOPLE ON THIS DRUG. DIGITALIS IS A POTENT AND POTENTIALLY TOXIC DRUG. DIGOXIN (LANOXIN) Class: Cardiac glycoside, antidysrhythmic Mechanism of Action 1. Inhibits sodium / potassium pump = Increases influx of sodium and calcium ions into the intracellular space = increased cardiac contractility (+ inotropic effect) 2. Increases vagal tone = - Decreases SA node firing, prolongs conduction through the AV node (- chronotropic effect) 3. In atrial fibrillation or flutter it decreases number of atrial impulses reaching the ventricles (- chronotropic effect) 4. Improves cardiac output (CO) (↓ baroreceptor response = ↓ SNS discharge = ↓ BP) - Due to (+) inotropic effects Indications 1. Control ventricular rate with Atrial-Fibrillation 2. Control ventricular rate with Atrial-Flutter 3. Paroxysmal supraventricular tachycardia (PSVT) 4. CHF 5. Cardiogenic shock Contraindications 1. Hypersensitivity 2. Ventricular fibrillation 3. Ventricular Tachycardia 4. 2nd (type II) or 3rd AV block (in the absence of a pacemaker) 5. Digitalis toxicity (low therapeutic index) Side effects – usually due to toxicity CNS Cardiovascular Eyes GI Blood Anorexia = C Diarrhea = C Atrial fibrillation Blurred vision = C = LT Apathy, Yellow or green Ventricular – Hemorrhagic Thrombocytopenia = LT confusion, vision fibrillation or necrosis of the delirium tachycardia = LT intestines = LT Hallucinations Halo effect Nausea = C AV block = LT Headache Bradycardia Vomiting = C Depression PVC’s Anorexia Hypotension Seizures = LT Restlessness Weakness Italic = C = common side effects Bold Italic = LT = life-threatening reactions Skin Rash Precautions 1. Use with caution when administered to patients: - with heart blocks (1st and 2nd type I) - with WPW - with liver or kidney disease - on beta blockers - with severe pulmonary disease 2. Toxicity is potentiated in patients with: hypokalemia, hypomagnesemia, and hypercalcemia (make heart more sensitive to digitalis) 3. Crosses the placenta and can effect fetal heart rate as it effects mother 4. Has a low therapeutic index Supplied Administration/dosage – Administered Slow IVP - 0.25mg – 1mg / 1 - 2ml Administered: slow IVP Dose: Initial – 4-6mcg /kg (over 5 minutes) / 2nd and 3rd dose 2-3 mcg /kg 34 ASPIRIN Class: Nonsteroidal Anti-inflammatory Drug (NSAID), antipyretic, platelet inhibitor, nonnarcotic analgesic Mechanism of Action 1. 2. 3. 4. - Inhibits prostaglandin synthesis and release (from mast cells). This action: decreases pain and fever produced Antipyretic agent by: inhibition of prostaglandins action on hypothalamus heat-regulating center vasodilation and sweating Analgesic agent acts on peripheral nervous system Platelet inhibitor = prevents formation of thromboxane A2 Post-plaque rupture in vessels → “sticky” platelets adhere to damaged vessel (within 1-5 seconds) → platelets release thromboxane A2 (chemical causes → platelet aggregation and vasoconstriciton) Aspirin delivery leads to: - Vasodilation (platelet inhibitor / thromboxane A2 inhibitor) - Decreased clot formation (platelet inhibitor / thromboxane A2 inhibitor) - Reduces inflammation (inhibition of prostaglandin synthesis) - Reduces fever (inhibition of prostaglandin synthesis and antipyretic properties) - Pain reduction (analgesic property) IF STARTED WITHIN 24 HOURS OF ONSET OF ACUTE MI – IT REDUCES MORTALITY ALMOST TO THE SAME DEGREE OF THROMBOLYTIC THERAPY Indications 1. 2. 3. 4. 5. Mild to moderate pain and fever Reducing the risk of recurrent transient ischemic attacks (TIA) Chest pain or other signs/symptoms of acute MI EKG changes suggestive of acute MI To reduce inflammation Contraindications 1. 2. 3. 4. 5. Active ulcer disease Hemophilia Hemorrhagic states - Active GI bleeding - Hemorrhagic stroke Known hypersensitivity to NSAIDs or salicylates Children or adolescents with flu-like symptoms / chickenpox (Varicella) 35 ASPIRIN Side effects CNS Confusion Eyes / Ears Dim vision Dizziness Reversible hearing loss Tinnitus Drowsiness Headache Blood ↓ plasma iron concentration Leukopenia = LT GI Reversible hepatotoxicity Anorexia Metabolic Hypoglycemia Respiratory Hypernea Skin Angioedema Hypokalemia Wheezing Bruising Prolonged bleeding Diarrhea Hyponatremia Bronchospasms Laryngeal edema Hives Shortened erythrocyte survival time Thrombocytopenia= LT Italic = C = common side effects Dyspepsia (inhibits pepsin) = GI discomfort = C Peptic ulcer formation Bleeding Heartburn Nausea = C Bold Italic = LT = life-threatening reactions Precautions 1. Chronic use may lead to GI ulcerations, bleeding, or perforation 2. Alcohol may increase the risk of GI bleeding 3. Allergic reactions are more likely if the patient has a history of asthma (hypersensitivity) 4. Use cautiously with: - GI disorders - Asthma - Impaired renal / liver function - Dehydrated children - Histories of coagulation defects - Bleeding disorders Administration / Dosage Administered - PO (orally) – Mild pain and fever 325-650mg - PO Myocardial Infarction 160-325mg / day - PO NON-ENTERIC – chewing is preferred 36 Rash Urticaria RETEPLASE (RETAVASE) Class: Inhibitor of platelets Mechanism of Action: 1. 2. Converts endogenous plasminogen (plasma protein) to plasmin Plasmin then degrades the fibrin matrix of the thrombus = clot breaks up Indications: 1. 2. Acute MI (to improve ventricular function) Reduce mortality associated with AMI Contraindications: 1. 2. 3. 4. 5. 6. Active internal bleeding History of stroke Recent intracranial or intra-spinal surgery or trauma Intracranial neoplasm, arteriovenous malformations, or aneurysm Known bleeding diathesis (inherited physical condition predisposing to diseases or conditions) Severe uncontrolled hypertension Side effects: Bleeding Disorders Hemorrhage may occur in the: Intracranial or retroperitoneal spaces GI, GU, or Respiratory systems Venous cutdowns, arterial punctures, or sites of recent surgery Cardiovascular Cholesterol embolus - LT Arrhythmias from reperfusion Heart failure - LT Cardiac arrest - LT Cardiac tamponade - LT Recurrent ischemia - LT Dysrhythmias: Ventricular fibrillation - LT Sinus bradycardia Accelerated idioventricular PVC’s SVT Ventricular tachycardia Many of these effects may be due to to the MI and may or may not be due to the medication Hypersensitivity Serious allergic reaction Bold italics – LT = Life threats Precautions: 1. 2. 3. 4. IM injections and nonessential handling of the patient should be avioided during treatment Monitor for bleeding complications Perform venipunctures carefully and only when necessary (watch the sites once medication is delivered) If arterial puncture is necessary, use an upper extremity that can be manually compressed 37 RETEPLASE (RETAVASE) How supplied: In a kit with components for reconstitution: 1. 2. 3. 4. 5. Single use reteplase vials – 10.8 units each Single use diluent vials of sterile water – 10 cc each Sterile 10cc syringe with 20 gauge needle Sterile dispensing pins Sterile 20 gauge needle Administration and dosage: 1. 2. Reconstitute the retavase Swirl (not shake) the vial gently to dissolve the retavase Deliver the 10 units – slow IVP over 2 minutes Deliver the second 10 units after 30 minutes Heparin and aspirin should be administered concomitantly (simultaneously) – Heparin should NOT be delivered through the same IV line 38 SODIUM BICARBONATE Class: electrolyte replacement, alkalinizing agent Mechanism of action 1. Neutralizes excess acid - Helps blood and body fluid return to a normal physiological pH - Improves metabolic processes - Allows sympathomimetic agents to work more effectively 2. Raises the pH in serum and urine so drugs can be excreted from the body more rapidly by the kidneys 3. Encourages redistribution of K+ ions from extracellular to intracellular fluid - ↑ H+ causes K+ to move out and H+ moves into the intracellular space 4. Electrolyte replacement (diarrhea) H+ + HCO3- ↔ H2CO3 ↔ H2O + CO2 Indications 1. Metabolic acidosis 2. Certain poisonings (methanol / ethylene glycol) 3. Rhabdomyolysis 4. Hyperkalemia 5. Overdoses with: - barbiturates - tricyclic antidepressants - aspirin - lithium - cocaine - diphenhydramine 6. DKA 7. Prolonged resuscitation with effective ventilation 8. Return of spontaneous circulation after long arrest interval Contraindications 1. Hypokalemia / hypocalcemia / hypernatremia 2. CHF 3. Metabolic / Respiratory alkalosis 4. Renal failure 5. Abdominal pain of unknown origin (due to distention side effect) 6. Hypertension Side effects CNS Confusion Headache Hyperreflexia - C Cardiovascular Cardiac arrest - LT Edema Irregular pulse GI Belching - C Cramps Distention - C Metabolic Alkalosis -C Hypocalcemia Hypokalemia Irritability Water retention Flatulence Intracellular acidosis (if not ventilated) Respiratory Apnea - LT Cyanosis Shallow, slow respirations Induces left shift in oxy-dissociation curve Seizures (caused Weight gain Increased thirst by alkalosis) = LT Tetany Tremors Twitching = C Weakness Italic = C = common side effects Bold italic = LT = life-threatening reaction AFTER ADMINISTRATION REASSESS VENTILATIONS OFTEN (H+ + HCO3- ↔ H2CO3 ↔ H2O + CO2) 39 SODIUM BICARBONATE Precautions 1. Temporary therapy in metabolic acidosis (best to give according to blood gases) 2. Rapid or excessive administration may cause - alkalosis, hypokalemia, hypocalcemia or dysrhythmias 3. Alkalosis leads to – hypoxia (left shift of oxyhemoglobin dissociation curve) + cerebral vasoconstriction 4. IV use may cause - fluid/electrolyte disturbances, fluid overload, and pulmonary edema 5. Can cause intracellular acidosis - H+ + HCO3- ↔ H2CO3 ↔ H2O + CO2 6. Do not give simultaneously with catecholamines – will reduce effectiveness 7. Precipitates with calcium chloride, atropine, morphine, magnesium sulfate (don’t give simultaneously) 8. Use cautiously with: - CHF - Cirrhosis - Hypertension - Toxemia – Pregnancy induced hypertension - Renal disease 9. Infiltration can lead to severe tissue damage How supplied - 50 meq / 50ml Administration / dosage Administered - IVP Initial dose 1mEq / kg - IVP Repeat in 10 minutes using subsequent dose Subsequent dose 0.5mEq / kg - IVP Should be delivered according to blood gas analysis REASSES VENTILATIONS OFTEN AFTER ADMINISTRATION!!!! SUBSEQUENT DOSES SHOULD BE BASED ON - BLOOD GAS ANALYSIS ADEQUATE VENTILATION AND CPR ARE MAJOR “BUFFER AGENTS” IN CARDIAC ARREST Pediatric dose: 1mEq/kg IVP / IO 40 MORPHINE SULFATE Class: narcotic analgesic Mechanism of action 1. CNS depressant - Inhibits pain perception - Decreases emotional response to pain (SNS response) - Causes sedation - Depresses respiratory centers in the brainstem 2. Decreases preload (venous dilation) 3. Decreases afterload (arteriole dilation) - #2 and #3 occur due to ↓ SNS response (↓ responsiveness of alpha receptors) /stimulate histamine release from Mast cells / baroreceptor inhibition - More venous dilation than arteriole Pain inhibition = ↓ SNS response = ↓ preload and afterload = reduction in myocardial O2 requirements Indications 1. To relieve pain and anxiety with: - myocardial infarction - unstable angina / non-STEMI – use ONLY if not responding to nitrates - traumatic injury - malignancy 2. To treat pulmonary edema (with or without chest pain and BP >100mmHg) Contraindications 1. Significant hypotension 2. Respiratory depression (unless caused by pulmonary edema and BP isadequate) 3. Acute asthma attack 4. CNS depression due to: - Head injuries - Drug overdose (CNS depressants) - Poisoning 5. Undiagnosed abdominal pain 6. Hypersensitivity Side effects CNS Addiction Confusion Dizziness - C Cardio-vascular Bradycardia Eyes / Ears Blurred vision GI Anorexia Reflex tachycardia Miosis (pupil constriction) C Constipation - C Diplopia Cramps Tinnitus Nausea - C Hypotension LT Palpitations Drowsiness C Euphoria Headache Sedation - C Italic = C = common side effects GU Urinary retention Reduced libido (with prolonged use) Vomiting Bold italic = LT = life-threatening reaction 41 Respiratory Depression - LT Other Histamine release = Decreased cough reflex ↓ B/P; ↑ HR; ↑sweating; flushing of the face; wheezing; dyspnea C MORPHINE SULFATE Precautions 1. May cause severe respiratory depression and / or hypotension with rapid injection 2. Commercial preparations may contain sulfites causing allergic reactions = - Hypersensitivity 3. Use cautiously with: - Liver / kidney disease - Head injury - COPD, asthma, pulmonary disease - Child < 18 years old - Prostatic hypertrophy = decreased urination 4. May worsen bradycardia or HB with inferior MI or Right Ventricular infarct How supplied 2mg / ml or 10mg / ml Administration / dosage Administered - slow IVP or IM Relief of moderate to severe pain Unstable Angina / Non-STEMI 1-5 mg SIVP – ONLY if not responding to nitrates 5-20 mg IM Ensure systolic BP (SBP) remains ≥ 100 mmHg - Antagonized by Narcan (for respiratory depression) - Have atropine available in case bradycardia develops To reduce preload (CHF / STEMI) 2 - 4mg SIVP Repeat in 5-15 minutes until desired response is obtained Ensure systolic BP (SBP) remains ≥ 100 mmHg - MONITOR VITALS FREQUENTLY - DISCONTINUE IF HYPOTENSION (BP less than 100 mmHg) or RESPRIATORY DEPRESSION DEVELOPS Pediatric doses: - slow IVP: 0.1 / 0.2mg/kg - up to 15mg 42 Fentanyl (Sublimaze) Class: narcotic analgesic Mechanism of action 1. Inhibits ascending (sensory) pain pathways in CNS, increases pain threshold, and alters pain perception by binding to opiate receptors. Indications 1. Pain control 2. Sedation for invasive airway procedures (rapid sequence induction) – conscious sedation Contraindications 1. 2. 3. 4. 5. 6. Hypersensitivity Myasthenia gravis Respiratory depression Head injury Cardiac dysrhythmia Hypotension Side effects CNS Dizziness Delirium Cardio-vascular Bradycardia=LT Arrest=LT Eyes / ears Blurred vision Miosis (pupil constriction)=C GI Nausea=C Vomiting Sedation=C Hypotension=C Euphoria Hypertension common side effects=C bold italic = life-threatening reaction GU Respiratory Depression=LT Arrest=LT Laryngospasm=LT Precautions 1. elderly 2. respiratory depression 3. increased intracranial pressures 4. seizure disorders 5. severe respiratory disorders 6. dysrhythmias How supplied 0.05 mg/ml Administration / dosage Administered – IM - slowly Dosage: Pain relief/anesthesia: 0.05-0.1 mg q 1-2 hours as needed to control pain – resuscitative equip available Dilute above amt in 5 cc NS Narcan should be available to reverse respiratory depression 43 Other Nitrous oxide:Oxygen (50/50) Nitronox Class: gaseous analgesic/anesthetic Mechanism of action A blend of 50% O2 and nitrous oxide. When inhaled, depresses the CNS causing anesthesia; In addition, the high concentration of oxygen delivered along with the nitrous oxide increases oxygen tension in the blood, thereby reducing hypoxia. It is self administered Indications Moderate to severe pain Anxiety Apprehension Contraindications 1. Impaired LOC 2. Head injury 3. Chest trauma (pnemothorax) 4. Inability to comply with instructions 5. Decompression sickness (nitrogen narcosis, air transport, air embolus) 6. Undiagnosed abdominal pain or marked distention 7. Bowel obstruction 8. Hypotention 9. Shock 10. COPD Side effects CNS Dizzy Cardiovascular GI GU Malignant Nausea/vomiting hypertention **Rare but dangerous common side effect=C bold italic = LT = life-threatening reaction Respiratory Apnea (LT) Skin Cyanosis How supplied - D or E cylinders - blue and green in USA; blue and white in Canada Administration / dosage – start an IVP prior to administration Adult: ENSURE enough O2 is in the tank to ensure oxygenation - invert cylinder several times before use – this mixes O2 and nitrous oxide Instruct the patient to inhale deeply through a patient held mask or mouthpiece Pediatric: Same Special Consideration: Pregnancy: Nitrous oxide has been shown to increase the incident of spontaneious abortion Nitrous oxide - is 34 times more soluble than nitrogen and will diffuse into pockets of trapped gas in the patient (intestinal obstruction, pneumothorax, blocked middle ear. As nitrogen leaves and is replaced by larger amts of nitrous oxide, increase pressures or volumes may cause serious damage, for example, intestinal rupture Nitrous oxide is non-explosive gas Patient must hold mask and self administer 44 FUROSEMIDE (LASIX) Class: Sulfonamide-type loop diuretic Mechanism of Action 1. Inhibits reabsorption of sodium and chloride in the proximal tubule and loop of Henle 2. Causes rapid diuresis (within 15-20 minutes) 3. Causes venodilation (within 5 minutes) = reduced preload 4. Decreases renal vascular resistance = increased renal blood flow 5. Results in excretion of Na+, Cl-, K+, H+, Ca++, Mg++, HCO-3, HPO46. May cause electrolyte imbalances Indications 1. Edema associated with: (BP needs to be greater than 100 mmHg – no signs of shock) - CHF - Cirrhosis of the liver - Renal disease 2. Cerebral edema 3. Hypertensive emergencies Contraindications 1. Pregnancy 2. Hypotension 3. Electrolyte depletion 4. Hypovolemia / dehydration 5. Hypersensitivity to Sulfa drugs 6. Anuria Side Effects CNS Dizziness Headache Cardiovascular Collapse - LT Chest pain GI Anorexia Constipation Fluids / Electrolytes Electrolyte depletion - LT Metabolic alkalosis - C Weakness Vertigo EKG changes Orthostatic hypotension Diarrhea Nausea - C Hypovolemia - LT Restlessness Common side effect=C Eyes / Ears Blurred vision Ototoxic – Given too quickly = tinnitis and deafness Vomiting bold italic = LT = life-threatening reaction Precautions 1. Excessive diuresis may cause: hypovolemia, electrolyte depletion 2. Use cautiously with: sulfonamide sensitivity, renal impairment, digitalized patients, cirrhosis or liver failure 3. May precipitate with all catecholamines and deactivate Epinephrine 4. May develop transient deafness with rapid administration How Supplied - 10mg / mL in 2-, 4-, 8mL ampules or 10mg / mL in 10-mL vial Administration and Dosage - Slow IV Push - 20-40 mg – (0.5 to 1mg/kg) IVP slowly (over 1-2 minutes) - if no response to initial dose – give 2mg/kg (double dose) - Start with low dose if patient not on Lasix - Repeat in 1-2 hours Pediatric dose: 1mg/kg slow IVP – Total dose 6mg/kg 45 NITROGLYCERIN (NITROSTAT) Class: antianginal, vasodilator, and nitrate Mechanism of action 1. Relaxes vascular smooth muscle - promoting vasodilation 2. Decreases preload (predominately) - venous dilation = ↓ preload = ↓ heart size - ↓ heart size = ↑ blood flow to coronary and collateral vessels = myocardial perfusion is improved 3. Decreases afterload - ↓ arteriole pressure = ↓ aortic pressure = left ventricle works better 4. Decreases myocardial O2 consumption / workload 5. Improves collateral flow to ischemic regions 6. Dilates pulmonary capillary beds - fluid in alveoli and interstitial space are pulled back into the vessels Pain relief occurs within 2 minutes & therapeutic effects observed up to 30 minutes. Indications – systolic pressure ≥ 100 mmHg 1. Angina 2. Chest pain with myocardial infarction 3. Pulmonary edema associated with CHF or MI 4. Hypertensive emergencies with Acute Coronay Syndromes or acute CHF Contraindications 1. Increased ICP 2. Hypotension 3. Hypovolemia 4. Viagra use within 24 hours 5. Right ventricular infarct 6. Severe bradycardia or tachycardia 7. Hypersensitivity Side effects CNS Anxiety Confusion Dizziness - C Cardiovascular Atrial fibrillation Collapse - LT Increase in angina GI Abdominal pain Diarrhea Dyspepsia GU Dysuria Impotence Urinary frequency Uncoordination Nausea Dysrhythmias LT Headache - C Palpitations Vomiting Nervousness Postural hypotension - C Vertigo PVC’s Weakness Reflex Tachycardia Syncope Italic = C = common side effects Bold italic = LT = life-threatening reaction 46 Eyes Blurred vision Skin Flushing - C Pallor Burning sensation in contact area - C Sweating Pallor NITROGLYCERIN (NITROSTAT) Precautions 1. The drop in B/P may lead to decreased cerebral perfusion 2. Patient may develop tolerance to the drug 3. A reduction in the diastolic pressure may lead to ischemia and angina developing 4. Use cautiously with: - the patient having an inferior wall MI with possible RV involvement - severe renal / hepatic impairment - glaucoma Administration / dosage – ESTABLISH AN IV PRIOR TO ADMINISTRATION (on borderline patients- pressure close to 100mmHg) Administered: - pills, spray, patches, ointments, IV infusion - Prehospital - administer nitro. sublingually through pills or spray Dose: - 1 - 0.3 - 0.4mg tablet sublingual - repeated every 5 minutes (give up to 3 tablets) Sit or lie patient down – instruct not to swallow until tablet is entirely dissolved Dose: - 1-2 sprays - 0.4mg per spray sublingual - every 5 minutes (up to 3 sprays in 15 minutes) Spray for 0.5 to 1.0 seconds – Do not shake canister (may produce bubbles and alter medication delivery) MONITOR VITALS AFTER EACH DOSE PRIOR TO ADMINISTERING MORE DRUG SYSTOLIC BLOOD PRESSURE SHOULD NOT BE LESS THAN 100 mmHg PRIOR TO ADMINISTRATION. When administering to patients with: 1. Acute MI – don’t let systolic pressure drop more than 10% 2. Hypertension – don’t let systolic pressure drop more than 30% 47 ANTIHYPERTENSIVES HYPERTENSIVE TREATMENTS HYPERTENISVE URGENCY HYPERTENSIVE EMERGENCY DIASTOLIC PRESSURE EXCEEDS 130 mmHg B/P NEEDS TO BE LOWERED WITHIN 24 HOURS B/P NEEDS TO BE LOWERED WITHIN 30-60 MINUTES HOURS FUNCTIONAL DISTURBANCES OF CNS, HEART, KIDNEYS FUNCTIONAL DISTURBANCES OF – CNS, HEART, KIDNEYS HYPERTENSIVE ENCEPHALOPATHY LABETALOL (TRANDATE NORMODYNE) (done) Class: Beta blocker Mechanism of Action: 1. Alpha 1 blocking agent - vasodilation, decreased peripheral vascular resistance, orthostatic hypotension 2. Nonselective beta blocking agent - effects the SA, AV, ventricular muscle = - bradycardia, delay in AV conduction, depressed cardiac contractility More potent Beta blocker than Alpha blocker = BP reduces without reflex tachycardia Indications: - Hypertensive Emergencies All patients with suspected MI and unstable angina (if not contraindicated) Useful as adjunctive agent with fibrinolytic therapy (may reduce nonfatal reinfarction and recurrent ischemia) To convert SVT (reentry SVT, A-fib or A-flutter with rapid ventricular response) to NRS or to slow ventricular response To reduce myocardial ischemia in AMI patients with elevated HR, BP or both ENSURE BP is over 100 mmHg Contraindications: - Bronchial Asthma Uncompensated CHF High Degree Heart Blocks (2nd and 3rd degree) Cardiogenic Shock Severe Bradycardia Pulmonary edema Hypersensitivity Side effects: CNS Anxiety CV AV block = LT EENT Double vision GI Diarrhea = C GU Dysuria Dizziness Bradycardia Nausea = C Ejaculatory failure Fatigue / Malaise Headache Tremors Chest pain Dry burning eyes Sore throat Tinnitus Visual changes Vomiting Impotence HEME Agranulocytosis = LT RESP Bronchospasms = LT Dyspnea Wheezing Constipation CHF= LT Orthostatic Taste Hypotension disturbances Mental Ventricular depression Dysrhythmia = LT Drowsiness Palpatations Nightmares Peripheral edema Scalp Pulmonary tingling edema Cold extremities Italic = C = common side Bold italic = LT = life-threatening reactions MS Muscle cramps SKIN Fever Pruritus Rash Urticaria 48 LABETALOL (TRANDATE NORMODYNE) (done) Precautions: - Use with caution in: - COPD patients (nonallergic bronchospastic disease) - Well-compensated patients with history of heart failure - Pheochromocytoma - Impaired hepatic function - Impaired renal function - Jaundice - Diabetes mellitus - Peripheral vascular disease - Thyroid disease - Nitroglycerin may augment hypotensive effects How Supplied: - 5mg / ml (4, 8, 20, 40 ml vials) Administration / Dosage: - Delivered Slow IVP and IV infusion Slow IVP Dose: Initial Dose 10 mg Slow IVP (over 1-2 minutes) Subsequent doses 10 to 20 mg every 10 minutes, prn IV infusion dose: - Mix: 200 mg / 250 cc Infuse at – 2 to 8mg / minute (titrate to supine blood pressure) 49 Total dose 150 mg ALBUTEROL (PROVENTIL) Class: Beta2 adrenergic agonist Mechanism of Action 1. Predominately stimulates β2 receptors 2. Minimal β1 stimulation 3. May cause reflex tachycardia (with high doses) 4. Promotes intracellular shift of K+ from serum 5. Inhibits histamine release from Mast cells 6. Increased diuresis Indications 1. Relief of bronchospasms associated with asthma, chronic bronchitis, emphysema - Reduces mucus secretions, capillary leaking, mucosal edema (by blocking histamine release) 2. Prevention of exercise-induced asthma and bronchospasms Contraindication 1. Hypersensitivity 2. Tachydysrhythmias 3. Severe cardiac disease Side Effects CNS Anxiety Dizziness - C Flushing Hallucinations Headache - C Irritability Stimulation - C Tremors - C Italic = C = common side Cardiovascular Angina GI Heartburn Dysrhythmias Hypertension Palpitations - C Tachycardia - C Nausea - C Vomiting Musculoskeletal Inhibition of uterine contractions Muscle cramps Precautions 1. May develop tolerance with prolonged use (vm) 2. Repeated or excessive use may lead to paradoxical bronchoconstriction 3. Use cautiously with: - cardiac disorders - hypertension - diabetes - prostatic hypertrophy 50 Respiratory Cough ALBUTEROL (PROVENTIL) How Supplied - 2.5mg/ 2.5ml Administration/Dosage Two ways to administer: 1. Metered dose inhaler: - 1- 2 sprays (90 - 180µg is delivered) q 4-6 hours – Max.: 12 inhalations / day 2. Nebulizer: - Adults and children over 12: Dilute 2.5mg in 3.0 ml of NS - Nebulizer should deliver 3.0 ml over 5 to 15 minutes – 3-4 times / day Pediatric dose: 0.05 - 0.15mg / kg (0.01 - 0.03ml / kg) in 2ml NS via nebulizer – may be repeated q 20 minutes – 3 times 51 EPINEPHRINE (1:1,000) Class: Sympathomimetic, vasopressor, bronchodilator Mechanism of Action - Catecholamine that stimulates alpha- and beta- adrenergic receptors 1. Beta1 stimulation leads to: - positive inotropic effects (↑ force of cardiac contraction) - positive chronotropic effects (↑ rate of cardiac contraction) - positive dromotropic effects (↑ conduction velocity) - increased cardiac output (CO) - increased myocardial oxygen requirements 2. Beta2 stimulation leads to: - peripheral vasodilation and bronchodilation 3. Alpha1 stimulation leads to peripheral vasoconstriction: - arterial / venous vasoconstriction (vasopressor) = increased SVR - constriction to renal, mesenteric, coronary, and cerebral vessels - pulmonary vasoconstriction - making the heart more susceptible to direct countershock in cardiac arrest (Ventricular fibrillation) = reason it is given during cardiac arrest 4. Inhibits histamine release (stops degranulation) during anaphylactic reaction (Effects start within 90 seconds and are short lived) Indications 1. Acute asthma attacks 2. Exacerbation of some forms of COPD 3. Mild anaphylaxis 4. Symptomatic Bradycardia (refractory, not responding, to oxygen and atropine) Contraindications 1. Hypersensitvity 2. Patients with underlying cardiovascular disease 3. Tachyarrhythmias 4. Not with alkaline drugs 5. Shock 6. Patients with hypertension 52 EPINEPHRINE (1:1,000) Side Effects CNS Anxiety Dizziness Cardiovascular Anginal pain Dysrhythmias LT Hypertension Palpitations - LT Ischemia Headache Restlessness Subarachnoid Hemorrhage = LT Tremors Weakness Italic = C = common side GI / GU Nausea - C Vomiting-C Respiratory Dyspnea Skin Pallor Coldness Urinary retention Necrosis Urticaria Bold italics = LT = life-threatening reactions Precautions 1. Increased myocardial workload may lead to ischemia, infarction 2. May have increased airway resistance due to sulfites in the preparation = hypersensitivity 3. Use cautiously with: - Heart disease - Diabetes - Hypertension 4. Excreted into breast milk – use cautiously on nursing mothers How supplied - Ampules and prefilled syringes containing - 1mg/1ml - Vials containing: - 30mg/30cc Administration / dosage Administered – SQ / IM / IV infusion Mild Anaphylaxis or Acute Asthma Attack 0.3 to 0.5mg - IM / SQ Mix infusion: Refractory Bradycardia Every 15 – 20 minutes, PRN Dosage range: 1-2mg / 250 or 500cc 2-10µg / minute Low doses – 2-5µg / minute = β effects High doses – 5-10µg / minute = α effects Pediatric dose: 0.01mg/kg up to 0.3mg IVP, IO 53 Eyes Pupil dilation Methylprednisolone (Solu-Medrol) Class: Anti-inflammatory glucocorticoid Mechanism of action: suppresses acute and chronic inflammation potentiates vascular smooth muscle relation by beta-adrenergic agonist. Indications: Acute Spinal cord trauma Anaphylaxis Bronchodilator for unresponsive asthma Septic shock (controversial) Adrenal insufficiency (SoluCortef) Contraindications: Psychosis;hypersensitivity Idiopathic thrombocytopenia Acute glomerulonephritis Fungal infections Nonasthmatic bronchial disease Diabetes (causes hyperglycemia) Side effects CNS Depression Sweating Headache Cardiovascular GI Hypertension Circulatory collapse Embolism Diarrhea=C Nausea GI hemorrhage=LT common side -C GU Respiratory EENT Fungal infection Blurred vision Cataracts tachycardia bold italic = LT - life-threatening reactions How supplied Injectable; acetate; 20 mg, 40mg , 80mg; succinate: 40mg; 125mg, 500mg 100mg Administration / dosage Adult:40-125 IM/IV Onset of action: 1-2 hrs; duration 8-24 hrs Administered – IM/IV 54 DEXAMETHASONE (DECADRON) Class : Glucocorticoid Mechanism of action: 1. 2. 3. Synthetic steroid related chemically to the natural hormones secreted by the adrenal cortex Suppress acute and chronic inflammation Potentiates the relaxation of vascular and bronchial smooth muscles by beta-adrenergic agonistst Indications: 1. 2. 3. 4. 5. 6. Allergic reactions Asthma Reduce swelling in the CNS Endocrine, rheumatic, hematological disorders Septic shock Chronic inflammation Slow onset (4-8 hrs) not considered a first-line medication for allergic reactions. Contraindications: 1. 2. Hypersensitivity to the product Active untreated infections Side effects: 1. 2. 3. 4. Decreased wound healing Hypertension GI bleeding Hyperglycemia Precautions: Barbiturates and phenytoin (Dilantin) can decrease effects How supplied: 1. 2. 3. 4. 4mg / mL in 1-, 5-, 10-, 25-, 30 mL vials 10 mg / mL in 10 mL vials, 1mL syringe, 1mL ampule 20 mg / mL in 5mL vials, 5mL syringe 24mg / mL (IV only) in 5- and 10mL vials Administration / dose: Adult: 4-24 mg IV Pediatric: 0.25-0.5 mg/kg IV / IO 55 RACEMIC EPINEPHRINE (MicroNefrin) Class : Sympathomimetic Mechanism of action: 1. 2. 3. Bronchodilator that stimulates B2 receptors in lungs = relaxation of bronchial smooth muscles a. Alleviates bronchospasm b. Increases vital capacity c. Reduces airway resistance Useful in treating laryngeal edema Inhibits the release of histamine Indications: 1. 2. 3. 4. Bronchial asthma Treatment of bronchospasm Croup (laryngotracheobronchitis) Laryngeal edema Monitor vital signs closely Contraindications: 1. 2. 3. Hypertension Underlying cardiovascular disease Epiglottitis Side effects: 1. 2. Tachycardia Dysrhythmias Precautions: 1. 2. 3. 4. 5. May produce tachycardia and other dysrhythmias Excessive use may cause bronchospasm Rebound exacerbation of severe croup may occur following during administration MAO inhibitors may potentiate the effects Beta antagonists may blunt the bronchodilating response How supplied: Meter dose inhaler: 0.16 – 0.25 mg / spray Solution: 7.5, 15, 30 mL in 1% or 2.25% solution Administration / dose: - Metered dose inhaler Adult: 1. 2. 2-3 inhalations – repeat once in 5 minutes, prn Dilute 5mL (1%) in 5mL saline – administer over 15 minutes Pediatric: Administer by aerosolization 1. 2. 3. Less than 20 kg - Dilute 0.25mL (0.1%) in 2.5cc saline 20-40kg – Dilute 0.5mL in 2.5mL saline Over 40 kg – Dilute 0.75mL in 2.5mL saline 56 50% DEXTROSE (D50W) Class: carbohydrate, caloric agent Mechanism of action 1. Increases blood glucose concentrations 2. Provides calories 3. Decreases rate of ketone production 4. Osmotic diuretic Indications 1. Acute alcoholism with coma (deliver thiamine prior to D50W) 2. Hypoglycemia 3. Coma of unknown cause (NEED TO CHECK BG) 4. Status epilepticus of uncertain cause 5. Hyperkalemia – with insulin may shift K+ back to the intracellular space Contraindications 1. Hypersensitivity to corn or corn products 2. Thiamine deficient patients (may cause Korsakoff’s psychosis or Wernicke’s encephalopathy) 3. Intracranial hemorrhage (unless patient is hypoglycemic) Side effects Cardiovascular Hypertension CHF - LT Pulmonary edema - LT GU Osmotic diuresis Metabolic ↓ K+ and Mg++ Fluid overload bold italic = LT - life-threatening reactions Precautions 1. Excessive IV administration may cause fluid volume or solute overload 2. Use cautiously with: - Carbohydrate intolerance; renal insufficiency; chronic alcoholism (give Thiamine first); diabetes How supplied - 25gm / 50ml (50% solution) Administration / dosage Administration - Slow IVP (in a large vein) Dose – 12.5 to 25 grams (25 to 50 cc) - Perform a D-stick prior to administration if possible - Give Thiamine prior if alcohol use is suspected Pediatric dose: 2 - 4ml / kg slow IVP - dilute 1:1 with sterile water to form a 25% solution (D25) 57 Skin Irritation Necrosis THIAMINE Class: vitamin B1 Mechanism of action 1. 2. Required for metabolic processes Co-enzyme important in carbohydrate metabolism - helps the breakdown of glucose in the Kreb Cycle - Thiamine is consumed in the process Thiamine deficiency results in accumulation of pyruvic acid with subsequent conversion to lactic acid Indications 1. 2. 3. Coma of unknown origin Alcoholic patients with altered sensorium and / or delirium tremens Thiamine deficiency - due to: - fasting or anorexia - alcoholism - cirrhosis - prolonged vomiting Thiamine is not produced by body – it must be obtained by diet (the above patients don’t take in, absorb, and utilize thiamine effectively) Contraindications 1. Hypersensitivity (rare) Side effects CNS Restlessness Weakness Cardiovascular Collapse Hypotension Pulmonary edema LT GI Diarrhea - C Hemorrhage Nausea - C Respiratory Throat tightness Dyspnea Skin Angioneurotic edema Cyanosis Pruritis Sweating Urticaria Italic = C = common side effects Bold italic = LT = life-threatening reaction Precautions 1. Severe hypersensitivity 2. Cardiovascular collapse 3. Death Usually occurs after repeated IV administration How supplied - 100mg / 1ml or 2 ml Administration / dosage Administered – Slow IVP or IM Dose: - 100mg IVP or - 50mg IM and 50mg IVP Pediatric dose: 10-25mg IVP (for critically ill children) – not usually recommended 58 Glucagon Class: Hyperglycemic agent; pancreatic hormone, insulin antagonist Mechanism of action: 1. Protein secreted by alpha cells of the pancreas. When released results in blood glucose elevation by increasing the breakdown of glycogen to glucose (glycogenolysis) and stimulating glucose synthesis (gluconeogenesis). 2. Only effective in treating hypoglycemia if liver glycogen is available and therefore may be ineffective in chronic states of: a. Hypoglycemia b. Starvation c. Adrenal insufficiency 3. Exerts (+) inotropic action on the heart and decreases renal vascular resistance a. Why used to manage patient with beta-blocker and calcium-channel blocker cardiotoxicity (that do not respond to other conventional therapy) Indications: 1. Altered LOC when hypoglycemia is suspected 2. Beta-blocker and calcium channel blocker toxicity. Contraindications: 1. Hyperglycemia 2. Hypersensitivity to proteins Side effects CNS Cardiovascular GI tachycardia Hypotension Vomiting=C GU Respiratory Skin Urticaria common side effects=C How supplied 1unit (1mg) white powder with 1 mL of diluting solution (supplied) Reconstitute the powder with the diluent DO NOT MIX WITH NORMAL SALINE Administration / dosage - IM Adult - 0.5mg-1mg IM - repeat in 7-10 min Calcium Channel OD/Beta blocker OD: 3mg to 10 mg SIVP (over 3-5 minutes) – followed by infusion at 3 - 5mg / hour 59 DIAZEPAM (VALIUM) Class: Sedative / hypnotic, antianxiety agent, anticonvulsant, skeletal muscle relaxant Mechanism of Action 1. CNS depressant - Reduces anxiety - Causes sedation - Induces amnesia 2. Relaxes skeletal and/or smooth muscle 3. Anticonvulsant (acts on the limbic, thalamic and hypothalamaic regions of the CNS) - ↑ the chance of gammaaminobutyric acid (GABA) combing with receptors that make up Cl- channels on cell membranes =↑ Cl- movement into the cells (intracellular space become negative) = ↓ cell depolarization 4. Decreases agitation, tremors, hallucinations associated with alcohol withdrawal Indications 1. Status epilepticus 2. Pre – Cardioversion and / or Transcutaneous Pacing 3. Severe anxiety 4. Skeletal muscle spasm relaxation 5. Acute alcohol withdrawal PREDOMINATELY USED FOR STATUS EPILEPTICUS AND PRECARDIOVERSION / TCP IN THE PREHOSPITAL SETTING. Contraindications 1. Pregnancy 2. Alcohol or other sedative drugs with depressed vital signs 3. Respiratory depression 4. Hypotension 5. Hypersensitivity Side Effects CNS Anxiety Cardiovascular EKG changes Eyes / Ears Blurred vision - C GI Anorexia GU Urine retention Confusion Depression Hypotension Orthostatic hypotension - C Constipation Diarrhea Incontinence Dizziness - C Drowsiness C Fatigue Tachycardia Phlebitis Tinnitus Mydriasis (pupil dilation) Nystagmus Diplopia Vascular impairment (if IVP into sm. hand vein) Hallucinations Headache Insomnia Tremors Italic = c = common Dry mouth Nausea Vomiting Bold Italic = LT - life-threatening reactions 60 Respiratory Respiratory depression LT Laryngospasm Decreased gag reflex Skin Dermatitis Itching Rash DIAZEPAM (VALIUM) Precaution 1. Rapid IV therapy can cause profound hypotension, and respiratory depression 2. Use cautiously with: - COPD patients - Hepatic / renal disease - older adults - children - Myasthenia gravis patients 3. Precipitates with most fluids (don’t administer with other drugs) - Administer through an IV of NS How Supplied - Prefilled syringe and ampule - 10mg / 2ml Administration/Dosage Administered - Slow IVP, IM, Rectally (usually for pediatric patients) Status Epilepticus 5-10mg - Slow IVP (over 2 minutes) Pre-cardioversion 5-10mg - Slow IVP (5-10 minutes prior to procedure) Eclampsia 5-10 mg - Slow IVP Anxiety 2-5mg - IM - REPEAT DRUG AS NEEDED IF HEMODYNAMIC STATUS ALLOWS - MONITOR VITALS FREQUENTLY - Do not mix with other medications or fluids - may precipitate - ANTAGONIZED BY FLUMAZENIL (Romazicon): DOSE – 0.2 mg (2 mL) over 15 seconds – TOTAL DOSE – 3mg - Reverses the effects in 1-2 minutes Pediatric dose: - 1 month to 5 years: 0.2-0.5mg slow IVP every 2-5 minutes up to 5mg. - 5 years and older: 1mg slow IVP every 2-5 minutes up to 10 mg Rectal dose: 0.5-0.7 mg/kg in a 1cc syringe - place the patient in a prone position - KY the syringe - Insert the syringe 4-5 cm into the rectum ELDERLY – Reduce dose by 50% After rectal administration hold the buttocks together to prevent leakage 61 MAGNESIUM SULFATE (NON-CARDIAC) Class: Electrolyte Mechanism of Action 1. CNS depressant 2. Believed to reduce the release of ACh by motor nerves so seizure activity is decreased (↓ grand mal activity) 3. Slows HR at the SA node, prolongs AV node conduction time = ↓ dromotropy 4. Causes peripheral vasodilation (Ca++ channel blocking properties) 5. Stabilize cell membranes (__↓__ Mg++ levels = ___↓__ membrane threshold potentials = ___↑___ cellular & Purkinje fiber excitability = ___↑___ chance for arrhythmia development) 6. Necessary for Na+ / K+ pump function Indications 1. 2. 3. Eclampsia (seizures) Preterm labor (labor prior to 36 weeks) – uterine relaxation Bronchodilator – after B2 agonist and anticholinergic agents have been used (Status Asthmaticus) Contraindications 1. Renal disease 2. Shock 3. Heart block 4. Hypocalcemia 5. Hypermagnesemia 6. Last 2 hours of labor Side effects CNS Cardiovascular GI Metabolic Decreased B/P - C Belching Hypermagnesemia Coma - LT Depressed deep Cramps Heart block - LT tendon reflexes - C Depression - C Bradycardia - C Lethargy - C Increased pulse - C Weakness - C Decreased SVR - C Italic = C = common side effects Bold italic = LT - ife-threatening reactions Respiratory Depression - LT Arrest - LT Paralysis - LT CALCIUM CHLORIDE / CALCIUM GLUCONATE ANTAGONIZES = HAVE AVAILABLE Precautions 1. May cause CNS depression and hypocalcemia 2. Rapid IV injection may cause hypotension, heart block, cardiac and/or respiratory arrest 3. Renal impairment may increase chance of toxicity How Supplied - 10%, 12.5%, 50 % solution in 40, 80, 100, and 125 mg/mL 62 MAGNESIUM SULFATE (NON-CARDIAC) Administration/Dosage (vm) Administered - slow IVP, IV infusion, IM Slow IVP dose 1-4gm / 10cc (10% solution) – IVP over 3 minutes IV infusion: IM dose 1-4gm / 10ml (50% solution) – use if IV cannot be started Split the dose in half and deliver in 2 different muscles Mix: 4-5gm / 250cc Infusion should not exceed 3ml / min. 63 ACTIVATED CHARCOAL Mechanism of Action 1. Binds to and absorbs ingested poisons thereby inhibiting their G.I. absorption 2. Effective with aspirin, amphetamines, strychnine, Dilantin, theophylline, and phenobarbital. 3. Absorbs enzymes, vitamins, minerals, and nutrients from G.I. tract Most effective if given within 30 minutes of ingestion Indications 1. Poisoning 2. Overdose 3. Following emesis 4. When emesis is contraindicated Contraindications 1. Not with: cyanide, mineral acids, strong bases, methanol, ethanol, iron tablets, lithium, phenobarbital, ASA, lead, arsenic 2. Patients with decreased LOC if airway is not controlled (may cause vomiting) 3. Not with milk, ice cream, sherbet 4. Hypersensitivity Side Effects GI Nausea / Vomiting; Black stools; Constipation; Diarrhea (with sorbitol); Abdominal cramping; Bloating Precautions 1. 2. Not with altered mental status unless ET and NG tubes are in place Absence of bowel sounds How supplied Bottles containing 25 and 50 grams of drug – mixed with water or sorbitol (a cathartic) Route and Dose Administered: Orally or NG tube Adult dose 1-2 gram/kg or: Approximately 10x the amount of poison ingested Pediatric dose <1 year old – 1 gm/kg 1-12 years old – 15 – 30 grams 64 DIPHENHYDRAMINE (BENADRYL) Class: antihistamine Mechanism of Action 1. Competes with H1 receptor sites found on the lungs, adrenal glands, veins, arterioles, capillaries, heart, gastrointestinal muscles. 2. Histamine-mediated effects are blocked by diphenhydramine: Effects of Histamine are as follows: - bronchial constriction - small vessel vasodilation - excessive capillary permeability Drug aids in reducing the effects of histamine - hypotension - edema - pruritis (hives) 3. Reverses effects of phenothiazine tranquilizers (dystonic reactions)* 4. Causes CNS depression 5. Anticholinergic properties (blocks ACh) 6. Antiemetic Indications 1. Anaphylactic shock (after administration of O2 and Epinephrine) 2. Allergic reactions 3. Acute dystonic (extrapyramidal) reactions* 4. Motion sickness *Dystonic reaction signs /symptoms - unusual posture, change in muscle tone, drooling, uncontrolled movements all do to antipsychotic drugs (Haldol, Thorazine, Mellaril) or certain antiemetics (Phenergan, Compazine, Reglan)). Contraindications 1. Narrow angle acute glaucoma 2. Patients taking MAO inhibitors 3. Newborns and nursing mothers 4. Hypersensitivity Side Effects CNS Cardiovascular GI GU Anxiety Confusion Palpitations Tachycardia Dysuria Urinary retention Dizziness - C Drowsiness C Euphoria Hypertension Hypotension Anorexia Constipation -C Diarrhea Dry mouth C Nausea Fatigue Paresthesia Poor coordination Italic = C = common side effects Vomiting Eyes, Nose, Throat Blurred vision Dilated pupils Dry nose - C Dry throat - C Nasal Stuffiness Tinnitus 65 Respiratory Skin Chest tightness Increased thick secretions Wheezing Rash Photosensitivity Urticaria DIPHENHYDRAMINE (BENADRYL) Precautions 1. Use cautiously with (due to anticholinergic effects of the drug): - COPD - Narrow angle glaucoma - Prostatic enlargement - G.I. obstruction 2. Cardiovascular disease 3. Hypertension 4. Liver disease 5. Elderly 6. Patient’s with CNS depression 7. Patient’s with asthma How supplied - Ampules and prefilled syringes - 50mg/1ml Administration / Dosage Administered - Slow IVP or IM Allergic reaction or Mild Anaphylaxis 25-50mg - IM Severe Anaphylaxis 25mg-50mg - Slow IVP Pediatric dose: Kids > 10kg Allergic reaction or Mild Anaphylaxis 1.25 mg/kg - IM Severe Anaphylaxis 1.25 mg/kg - Slow IVP 66 EPINEPHRINE (1:1,000) Class: Sympathomimetic, vasopressor, bronchodilator Mechanism of Action - Catecholamine that stimulates alpha- and beta- adrenergic receptors 1. Beta1 stimulation leads to: - positive inotropic effects (↑ force of cardiac contraction) - positive chronotropic effects (↑ rate of cardiac contraction) - positive dromotropic effects (↑ conduction velocity) - increased cardiac output (CO) - increased myocardial oxygen requirements 2. Beta2 stimulation leads to: - peripheral vasodilation and bronchodilation 3. Alpha1 stimulation leads to peripheral vasoconstriction: - arterial / venous vasoconstriction (vasopressor) = increased SVR - constriction to renal, mesenteric, coronary, and cerebral vessels - pulmonary vasoconstriction - making the heart more susceptible to direct countershock in cardiac arrest (Ventricular fibrillation) = reason it is given during cardiac arrest 4. Inhibits histamine release (stops degranulation) during anaphylactic reaction (Effects start within 90 seconds and are short lived) Indications 1. Acute asthma attacks 2. Exacerbation of some forms of COPD 3. Mild anaphylaxis 4. Symptomatic Bradycardia (refractory, not responding, to oxygen and atropine) (infusion) 5. Symptomatic heart blocks (second type II and third degree) (infusion) Contraindications 1. Hypersensitvity 2. Patients with underlying cardiovascular disease 3. Tachyarrhythmias 4. Not with alkaline drugs 5. Shock 6. Patients with hypertension 67 EPINEPHRINE (1:1,000) Side Effects CNS Anxiety Dizziness Cardiovascular Anginal pain Dysrhythmias LT Hypertension Palpitations - LT Ischemia Headache Restlessness Subarachnoid Hemorrhage = LT Tremors Weakness Italic = C = common side GI / GU Nausea - C Vomiting-C Respiratory Dyspnea Skin Pallor Coldness Urinary retention Necrosis Urticaria Bold italics = LT = life-threatening reactions Precautions 1. Increased myocardial workload may lead to ischemia, infarction 2. May have increased airway resistance due to sulfites in the preparation = hypersensitivity 3. Use cautiously with: - Heart disease - Diabetes - Hypertension 4. Excreted into breast milk – use cautiously on nursing mothers How supplied - Ampules and prefilled syringes containing - 1mg/1ml - Vials containing: - 30mg/30cc Administration / dosage Administered – SQ / IM / IV infusion Mild Anaphylaxis or Acute Asthma Attack 0.3 to 0.5mg - IM / SQ Mix infusion: Refractory Bradycardia Every 15 – 20 minutes, PRN Dosage range: 1-2mg / 250 or 500cc 2-10µg / minute Low doses – 2-5µg / minute = β effects High doses – 5-10µg / minute = α effects Pediatric dose: 0.01mg/kg up to 0.3mg IVP, IO 68 Eyes Pupil dilation NALOXONE (NARCAN) Class: Opiate antagonist Mechanism of Action 1. Reverses effects of narcotics or synthetic narcotics - Competes for and displaces narcotic molecules from opiate receptors in the brain - Reverses stupor, coma, respiratory depression caused by opiates - Duration of action is shorter than opiates Indications - Narcotic / synthetic narcotic overdose - Coma of unknown cause - Coma from alcohol Narcotics - heroin, morphine, methadone, codeine, Demerol, Dilaudid, Paregoric, fentanyl, Percodan, hydromorphone, meperidine, oxycodone, propoxyphene Synthetic narcotics (narcotic agonists / antagonist) - Talwin, Darvon, Nubain, Stadol Contraindications - Hypersensitivity to the drug Respiratory depression is due to nonopiate drugs Side effects CNS Seizures - LT Tremors Cardiovascular Hypertension Hypotension Ventricular Dysrhythmias - LT Cardiac arrest - LT Bold italic = LT - life-threatening GI Nausea Respiratory Pulmonary edema LT Hyperventilation Vomiting Skin Sweating Side effects usually occur due to rapid IVP causing withdrawal to occur = deliver slow IVP to increase respirations Precautions - May need to repeat the dose (effects of Narcan may wear off before narcotic) - May cause excitement, hypertension, tachycardia (due to rapid IVP) - May cause hypertension or hypotension, pulmonary edema, ventricular fibrillation if given to patients with cardiovascular disorders. How supplied - Ampoules or prefilled syringes containing - 2 mg / 2ml or 0.4mg / 1mL or 10mL - Vials containing 10mg / 10ml 69 NALOXONE (NARCAN) Administration and dosage: Administered - Slow IVP, IM, SQ, ET (diluted) , Infusion Slow IVP 0.4-2mg SIVP Repeat at 2-3 minute intervals ET 2-2.5 times the SIVP dose Dilute in 10cc of fluid After 10mg have been given, with no response, reevaluate diagnosis Repeat S/A IVP route Darvon / Alcohol 2-5mg SIVP Infusion 8mg / 1000cc of D5W Infuse at 2/3 of the initial reversal dose – titrated to desired effect *** GIVE THE DRUG SLOWLY TO INCREASE THE PATIENTS MINUTE VOLUME *** If GIVEN RAPIDLY IT CAN CAUSE WITHDRAWAL LEADING TO ADVERSE SIDE EFFECTS Pediatric dosage: - Less than 5 years old or less than 20kg - 0.1mg/kg – up to 10mg - Over 5 years old or over 20kg - 2mg – up to 10mg Titrate to effect Incompatible with bisulfate (is an additive in epinephrine ) and alkaline solutions. 70 PROMETHAZINE (PHENERGAN) Class : Phenothiazine, antihistamine Mechanism of action: 1. 2. 3. H1 receptor antagonist that blocks the actions of histamine at the H1 receptors Also possesses sedative, anti-motion, antiemetic and considerable anticholinergic activity. Often administered with analgesics, particularly narcotics, to potentiate their effects Indications: 1. 2. 3. 4. 5. Nausea and vomiting Motion sickness Preoperative and postoperative, obstetric (during labor) sedation To potentiate the effects of analgesics Allergic reactions Contraindications: 1. 2. 3. 4. Hypersensitivity Comatose states CNS depression from alcohol, barbiturates, or narcotics Signs associated with Reye’s syndrome Side effects: 1. 2. 3. 4. 5. 6. 7. Sedation Dizziness Allergic reactions Dysrhythmias Nausea and vomiting Hyperexcitability Dystonias when given with some MAO inhibitors Precautions: 1. 2. 3. 4. 5. May impair mental and physical ability Use in children may cause hallucinations, convulsions, and sudden death Used with epinephrine may decrease BP further Used with other CNS depressants may have an additive sedative effect Use with caution in patients with asthma, peptic ulcer and bone marrow depression. How supplied: 25, 50 mg / mL in 1mL ampoules and Tubex syringes Administration / dose: IV / IM Adult: 12.5 – 25 mg IV or deep IM Pediatric: Not indicated in pre-hospital setting 71