tremor - DFCM Open
advertisement
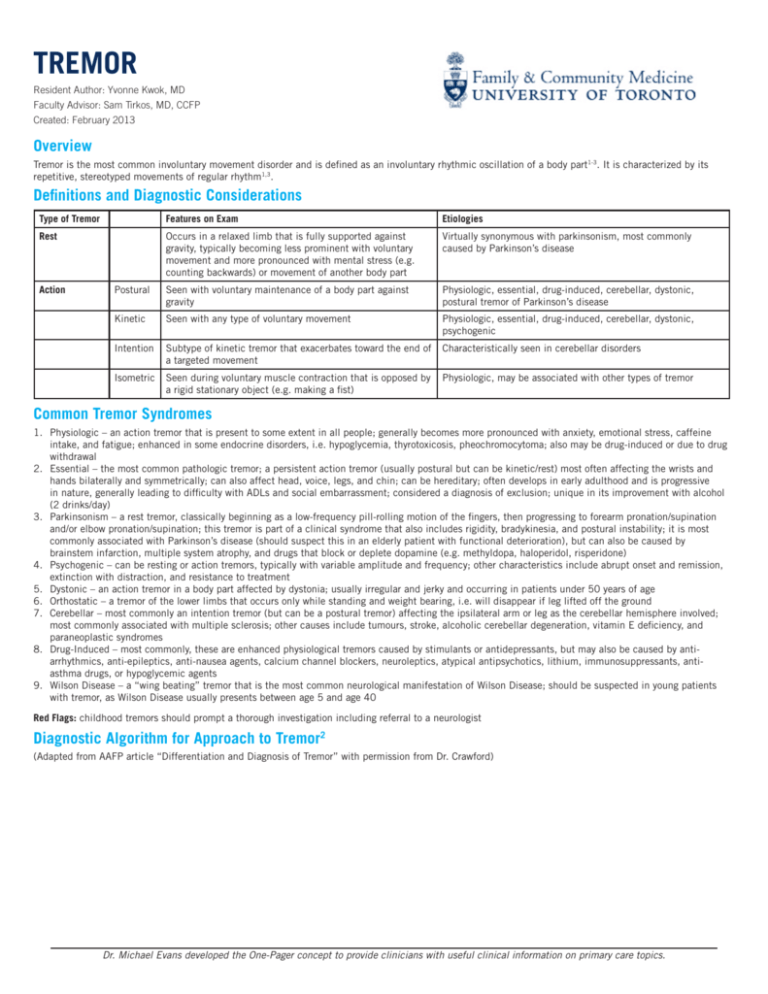
TREMOR Resident Author: Yvonne Kwok, MD Faculty Advisor: Sam Tirkos, MD, CCFP Created: February 2013 Overview Tremor is the most common involuntary movement disorder and is defined as an involuntary rhythmic oscillation of a body part1-3. It is characterized by its repetitive, stereotyped movements of regular rhythm1,3. Definitions and Diagnostic Considerations Type of Tremor Features on Exam Etiologies Rest Occurs in a relaxed limb that is fully supported against gravity, typically becoming less prominent with voluntary movement and more pronounced with mental stress (e.g. counting backwards) or movement of another body part Virtually synonymous with parkinsonism, most commonly caused by Parkinson’s disease Postural Seen with voluntary maintenance of a body part against gravity Physiologic, essential, drug-induced, cerebellar, dystonic, postural tremor of Parkinson’s disease Kinetic Seen with any type of voluntary movement Physiologic, essential, drug-induced, cerebellar, dystonic, psychogenic Intention Subtype of kinetic tremor that exacerbates toward the end of a targeted movement Characteristically seen in cerebellar disorders Isometric Seen during voluntary muscle contraction that is opposed by a rigid stationary object (e.g. making a fist) Physiologic, may be associated with other types of tremor Action Common Tremor Syndromes 1. Physiologic – an action tremor that is present to some extent in all people; generally becomes more pronounced with anxiety, emotional stress, caffeine intake, and fatigue; enhanced in some endocrine disorders, i.e. hypoglycemia, thyrotoxicosis, pheochromocytoma; also may be drug-induced or due to drug withdrawal 2. Essential – the most common pathologic tremor; a persistent action tremor (usually postural but can be kinetic/rest) most often affecting the wrists and hands bilaterally and symmetrically; can also affect head, voice, legs, and chin; can be hereditary; often develops in early adulthood and is progressive in nature, generally leading to difficulty with ADLs and social embarrassment; considered a diagnosis of exclusion; unique in its improvement with alcohol (2 drinks/day) 3. Parkinsonism – a rest tremor, classically beginning as a low-frequency pill-rolling motion of the fingers, then progressing to forearm pronation/supination and/or elbow pronation/supination; this tremor is part of a clinical syndrome that also includes rigidity, bradykinesia, and postural instability; it is most commonly associated with Parkinson’s disease (should suspect this in an elderly patient with functional deterioration), but can also be caused by brainstem infarction, multiple system atrophy, and drugs that block or deplete dopamine (e.g. methyldopa, haloperidol, risperidone) 4. Psychogenic – can be resting or action tremors, typically with variable amplitude and frequency; other characteristics include abrupt onset and remission, extinction with distraction, and resistance to treatment 5. Dystonic – an action tremor in a body part affected by dystonia; usually irregular and jerky and occurring in patients under 50 years of age 6. Orthostatic – a tremor of the lower limbs that occurs only while standing and weight bearing, i.e. will disappear if leg lifted off the ground 7. Cerebellar – most commonly an intention tremor (but can be a postural tremor) affecting the ipsilateral arm or leg as the cerebellar hemisphere involved; most commonly associated with multiple sclerosis; other causes include tumours, stroke, alcoholic cerebellar degeneration, vitamin E deficiency, and paraneoplastic syndromes 8. Drug-Induced – most commonly, these are enhanced physiological tremors caused by stimulants or antidepressants, but may also be caused by anti- arrhythmics, anti-epileptics, anti-nausea agents, calcium channel blockers, neuroleptics, atypical antipsychotics, lithium, immunosuppressants, anti- asthma drugs, or hypoglycemic agents 9. Wilson Disease – a “wing beating” tremor that is the most common neurological manifestation of Wilson Disease; should be suspected in young patients with tremor, as Wilson Disease usually presents between age 5 and age 40 Red Flags: childhood tremors should prompt a thorough investigation including referral to a neurologist Diagnostic Algorithm for Approach to Tremor2 (Adapted from AAFP article “Differentiation and Diagnosis of Tremor” with permission from Dr. Crawford) Dr. Michael Evans developed the One-Pager concept to provide clinicians with useful clinical information on primary care topics. TREMOR Investigations1,4 Management Type of Tremor Treatment Physiologic Identify and remove/treat the precipitating cause, +/- propranolol Essential Propranolol – starting dose of 30mg BID, can titrate up to 320mg BID as needed Primidone – starting dose of 25mg QHS, gradual titration by 25mg increments to max of 750mg QHS. *Could consider combo therapy of propranolol + primidone for resistant tremors Gabapentin – target dose of 400mg TID Other therapies with less evidence for routine use: other beta blockers, EtOH (rebound tremor seen), benzodiazepines, botulinum toxin, surgery Parkinsonism Remove dopamine antagonists (e.g. antipsychotics) and cholinergic drugs (e.g. cholinesterase inhibitors). Treat with Levodopa (+carbidopa) or dopamine agonists Other: anticholinergics (trihexyphenidyl hydrochloride, benztropine), amantadine, MAO B inhibitors, COMT inhibitors (used as an adjunct to extend the action of levodopa), deep brain stimulation – DBS) Cerebellar Identify and treat underlying cause; no medications have been shown to be helpful; consider Deep Brain Stimulation (DBS) Psychogenic Psychotherapy Dystonic Pharmacotherapy not proven to be useful – can try clonazepam or antipsychotics; treatment of underlying dystonia with botulinum toxin may be helpful Drug-Induced Discontinue or reduce the dose of the medication causing tremor. Orthostatic Clonazepam – 0.5mg QHS, with gradual titration by 0.5mg increments to max of 6mg/day Gabapentin Wilson’s disease Chelation therapy, dietary restriction – only curative therapy is liver transplantation Bottom Line: Tremor is a symptom of many disorders and diagnosis is based on a thorough history and physical exam, which includes careful characterization of the activation condition, location, and frequency of the tremor. It is important to differentiate physiologic tremors from pathologic tremors. References can be found online at http://www.dfcm.utoronto.ca/programs/postgraduateprograme/One_Pager_Project_References.htm