general characteristics of the endocrine system
advertisement

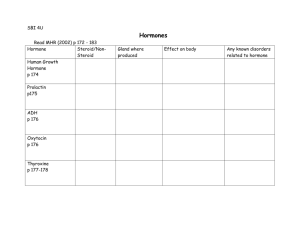
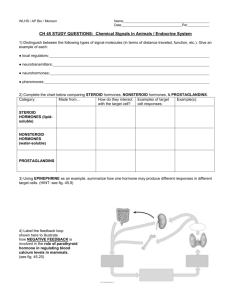
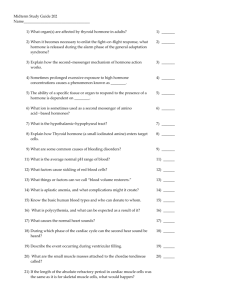
GENERAL CHARACTERISTICS OF THE ENDOCRINE SYSTEM FIGURE 17.1 1. The endocrine system consists of glands that secrete chemical signals, called hormones, into the blood. In addition, other organs and cells beside the glands seen in figure 17.1 secrete hormones. For example, organs of the digestive system secrete hormones that function to regulate the digestive process. 2. Endocrine (G. endo, within; crino, separate). A tissue that secretes internally a product called a hormone. The hormone has its effect on another tissue separated by some distance from the tissue producing the hormone. 3. Hormone (G. hormon, to set into motion). The secretory product of an endocrine tissue that causes a response in another tissue. A. Hormones are usually produced in small quantities. B. Hormones are secreted into the interstitial space (the area around cells). C. Hormones enter the circulatory system and are transported to other tissues. D. Hormones act on their "target tissue" which produces a response. Endocrine tissue Endocrine cell Hormone Blood Interstitial space Target tissue What causes the hormone to move from the endocrine cell to the blood and from the blood into the target tissue? 17-1 E. Hormones function as amplitude-modulated signals, i.e., the response produced by the target tissue is proportional to the amount of the hormone reaching the target tissue. In contrast, the nervous system is frequency-modulated, i.e., the response of the target tissue is proportional to the number of all-or-none action potentials reaching the target tissue. FIGURE 17.2 3. Intercellular chemical signals allow one group of cells (e.g., endocrine cells) to control the activity of other cells (e.g., target tissues). Examples are TABLE 17.1 A. Autocrine chemical signals have a local effect on a cell type that is the same as the cell type releasing the signal. B. Paracrine chemical signals have a local effect on a cell type that is different from the cell type releasing the signal. C. Hormones usually effect target tissues distant from the cells releasing the hormone. D. Neurohormones are hormones secreted by neurons. E. Neurotransmitters are released by neurons and stimulate or inhibit postsynaptic terminals. A neurotransmitter can be an autocrine signal (between neurons) or a paracrine signal (between a neuron and a muscle cell). F. Neuromodulators are released by neurons and can modify the release of neurotransmitters from axons (presynaptic facilitation or inhibition) or the sensitivity of the postsynaptic terminal to the neurotransmitter. Thus, neuromodulators can be autocrine or paracrine signals. G. Pheromones are released into the environment and alter the physiology and behavior of other individuals. Example: sex pheromones in the urine of dogs and cats. 17-2 CHEMICAL STRUCTURE OF HORMONES Hormones can be classified into a "protein" group and a lipid group. The chemical characteristics of each group determines how the hormones affect the body. Category Examples PROTEIN GROUP Proteins Growth hormone, insulin, parathyroid hormone, and prolactin Glycoprotein (protein + carbohydrate) Follicle-stimulating hormone (FSH), luteinizing hormone (LH), and thyroid-stimulating hormone (TSH) Polypeptides (two or more amino acids) Adrenocorticotropic hormone (ACTH), antidiuretic hormone (ADH), calcitonin, endorphins, glucagon, hypothalamic hormones, melanocyte-stimulating hormone (MSH), oxytocin, thyrotropin-releasing hormone (TRH), and thymosin Amino Acid Derivatives Epinephrine, melatonin, norepinephrine, and thyroid hormones (T3 and T4) LIPID GROUP Steroids (cholesterol is a precursor for all the steroid hormones) Estrogens, glucocorticoids (cortisol), mineralocorticoids (aldosterone), progestins (progesterone), and testosterone Fatty Acids Leukotrienes, prostacyclins, prostaglandins, and thromboxanes CONTROL OF SECRETION RATE 1. Regulation by a nonhormone substance. FIGURE 17.4 A. Action. An increase of a nonhormone substance stimulates or inhibits hormone production. The change in hormone levels causes a decrease in the substance, i.e. negative feedback. Given that the pancreas secretes insulin in response to an increase in blood glucose levels, and that insulin increases the uptake of glucose by most tissues, As blood glucose levels increase, The pancreas is ____________________ (inhibited or stimulated) Insulin secretion ____________________ (increases or decreases) Blood glucose levels ____________________ (decrease or increase) B. Examples: 1) Glucose - insulin 2) Calcium - calcitonin and parathyroid hormone 3) Potassium and sodium - aldosterone 17-3 2. Regulation by the nervous system. FIGURE 17.5 A. Action. Neurotransmitter released by a neuron stimulates or inhibits hormone production. B. Examples: 1) Hypothalamic hormones 2) ADH and oxytocin from the posterior pituitary 3) Epinephrine and norepinephrine from the adrenal gland 3. Regulation by hormones. FIGURE 17.6 A. Action E1 H1 E2 Response Target tissue Negative feedback H2 1) Endocrine gland E1 produces hormone H1 which stimulates endocrine gland E2 to produce hormone H2. 2) H2 can act on the target tissue. 3) H2 can inhibit E1 which then produces less H1. Therefore production of H2 by E2 decreases. This is a negative-feedback mechanism. 4) When H2 decreases E1 is no longer inhibited. Therefore H1 increases which stimulates E2 to produce more H2. 17-4 ☞As H2 levels increase, E1 is ____________________ (inhibited or stimulated) H1 levels ____________________ (decrease or increase) E2 is ____________________ (inhibited or stimulated) H2 levels ____________________ (decrease or increase) ☞As H2 levels decrease, E1 is ____________________ (inhibited or stimulated) H1 levels ____________________ (decrease or increase) E2 is ____________________ (inhibited or stimulated) H2 levels ____________________ (decrease or increase) 5) Note that the response by the target tissue could result in movement away from homeostasis. That is, the response can be too large or two small. The amount of H2 regulates the response because hormones are amplitude modulated signals. That is, a large amount of H2 increases the response and a small amount of H2 decreases the response. Thus, by controlling the amount of H2, the response is controlled and homeostasis is maintained. B. Examples: 1) Thyroid hormones 2) Estrogen 3) Progesterone 4) Testosterone 4. Patterns of secretion. FIGURE 17.8 A. A relatively constant secretion rate is important in long term maintenance. For example, thyroid hormones maintain a constant basal metabolic rate. B. An increase or decrease in response to a stimulus allows the organism to respond to different conditions. For example, epinephrine secretion increases in response to exercise or stress. C. Cyclic patterns allow periodic change. For example, hormones involved with reproductive readiness change on a monthly basis. 17-5 TRANSPORTATION AND DISTRIBUTION IN THE BODY 1. Hormones are transported dissolved in blood plasma (liquid part of blood). 2. Hormones are transported bound to plasma proteins. The plasma proteins prevent the metabolism and excretion of the hormones. This means the hormone is present for a longer time. METABOLISM AND EXCRETION 1. Hormones are broken down by enzymes in the blood and/or are excreted into the urine or into bile. 2. Half-life is the amount of time it takes to remove or inactivate half of the hormone initially present. For example, suppose a hormone has a half-life of one minute. Time 0 1 2 3 Amount 16 8 4 2 How much of the hormone is left at four minutes? 3. The half-life of a hormone is related to its solubility. A. Hormones with a short half-life (seconds or minutes) are water soluble. Generally, this is the "protein" group of hormones. B. Hormones with a long half-life (hours or days) are lipid soluble. This includes the lipid group of hormones and the thyroid hormones (amino acid derivative). ☞Given the following patterns of secretion: Hormone B secretion rate Hormone A secretion rate Time Time Hormone A probably has a ____________________ (short or long) half life? Hormone B probably has a ____________________ (short or long) half life? 17-6 Explain: INTERACTION OF HORMONES WITH THEIR TARGET TISSUES 1. When the hormone combines with the receptor the result is: A. Activation of, or increased activity of, something the cell can already do. B. Inhibition of a cell activity. 2. Hormone receptors are proteins or glycoproteins. Their three-dimensional shape allows them to be specific for a single hormone. FIGURE 17.11 What other examples have we seen in this course that depend upon the three-dimensional shape between reacting molecules? 3. Different tissues have different receptors. Thus, a hormone can affect only tissues that have a receptor for that hormone. Receptors 1 2 1 Tissue A 3 Tissue B Hormone H1 can affect tissues A and B. Hormone H2 can affect only tissue A, and hormone H3 can affect only tissue B. 17-7 4. Different tissues can produce different responses to the same hormone. The binding of the hormone to its receptor is a signal. The response to that signal depends upon the type of cell. 1 2 1 Tissue A 3 Tissue B Hormone H1 can stimulate tissue A, but inhibits tissue B. 5. The number of receptors in a give tissue can decrease or increase. FIGURE 17.13 A. Down regulation. The number of receptors decreases due to decreased synthesis of receptors or increased breakdown of receptors. B. Up regulation. The number of receptors increases due to increased synthesis of receptors. Predict the effect of down and up regulation on the response of the target tissue to a hormone. Explain Down regulation ___________________ (increases or decreases) the response. Up regulation ___________________ (increases or decreases) the response. CLASSES OF HORMONE RECEPTORS 1. Membrane-bound receptors are proteins found within the plasma membrane. Intracellular receptors are proteins found inside cells, within the cytoplasm or the nucleus. 2. The hormone binding to membrane-bound receptors or intracellular receptors functions as a signal that causes a response from the cell. FIGURE 17.14 17-8 Which type of hormone, the “protein” group or the “lipid” group is most likely to activate intracellular receptors? Explain. Overview of Responses to Hormones Binding to Their Receptors Hormone Hormone Membrane-Bound Receptor Receptor linked to ion channel Opens or closes ion channels Receptor linked to G protein Intracellular Receptor Receptor linked to enzyme Activates genes Activates already existing enzymes Synthesizes new enzymes Cell response Membrane-Bound Hormone Receptors At least three major mechanisms exist by which the binding of chemical signals to membranebound receptors result in responses from cells: 1) directly alter membrane permeability, 2) activate G proteins, or 3) directly alter enzyme activity. Receptors That Directly Alter Membrane Permeability FIGURE 17.15 1. The receptor is part of an ion channel. When a hormone binds to the receptor/ion channel, the channel changes shape, opening or closing depending on the type of ion channel. The resulting increase (channel opens) or decrease (channel closes) in ion movement leads to the cell’s response. 2. For example, serotonin can combine to its receptor on a Na+ channel, resulting in the movement of Na+ into a cell, producing depolarization. See table 17.5 for other examples. 17-9 Receptors That Activate G Proteins FIGURE 17.16 1. G proteins consist of three subunits, which from largest to smallest, are called alpha (α), beta (β), and gamma (γ). The G proteins are so named because they bind to guanine nucleotides (see chapter 3). A. G proteins are associated with receptor molecules within the plasma membrane. In the inactive state, guanine diphosphate (GDP) is bound to the alpha subunit of the G protein. B. When a hormone binds to the receptor, the receptor changes shape. 1) GDP is released from the alpha subunit. Guanine triphosphate (GTP), which is more abundant than GDP, binds to the alpha subunit activating it. 2) The G protein separates from the receptor and the activated alpha subunit separates from the beta and gamma subunits. 3) The activated alpha subunit can cause a variety of effects, which are responsible for producing cellular responses. C. After a few seconds, the activated alpha subunit turns itself off by converting GTP to GDP. D. The alpha subunit then recombines with the beta and gamma subunits (go back to step A). 2. G proteins regulate membrane ion channels. FIGURE 17.17 A. The activated alpha subunit can combine with an ion channel, causing the ion channel to open or close. B. For example, epinephrine can combine with its receptor on smooth muscle cells. The activated alpha subunit cause a Ca2+ channel to open and Ca2+ move into the cell. C. Ca2+ can act as intracellular mediators, which are ions or molecules that stimulate or inhibit cell activities (see table 17.7 for other examples). Ca2+ bind to calmodulin, and together they activate enzymes that result in smooth muscle contraction. FIGURE 9.24 17-10 3. G proteins regulate the activity of enzymes. The increased or decreased enzyme activity produces the cell’s response. FIGURE 17.18 A. For example, glucagon can combine with its receptor in the plasma membranes of liver cells, resulting in the formation of activated alpha subunits. B. The activated alpha subunit activates the enzyme adenylate [a-den′i-lat] cyclase. C. Adenylate cyclase promotes the conversion of ATP to cyclic adenosine monophosphate (cAMP). ATP Adenylate cyclase cAMP D. cAMP is an intracellular mediator that activates protein kinases. cAMP + Protein kinase (inactive) Protein kinase (active) E. Protein kinases are enzymes that affect the activity of other enzyme through phosphorylation, which is the addition of a phosphate group to a molecule. 1) Phosphorylation increases the activity of some enzymes and decreases the activity of other enzymes. 2) For example, cAMP activates protein kinases that cause the activation of enzymes that break down glycogen to glucose, which is then released from liver cells. F. The activity of cAMP is limited by phosphodiesterase, which converts cAMP to adenosine 5' monophosphate (AMP). 4. See Table 17.6 for examples of hormones that bind to membrane-bound receptors and activate G proteins. 17-11 Receptors That Directly Alter the Activity of Intracellular Enzymes 1. The receptor is either associated with enzymes inside the cell or the intracellular portion of the receptor can function as an enzyme. 2. When the hormone binds to the receptor, enzymes within the cell are activated. A. The receptor is directly associated with enzymes. FIGURE 17.20 1) Guanylate [gwahn′i-lil] cyclase is an enzyme associated with certain membranebound receptors. For example, when atrial natriuretic hormone binds to receptors on kidney cells, the enzyme guanylate cyclase is activated. The activated guanylate cyclase causes the conversion of guanosine triphosphate (GTP) to cyclic guanosine monophosphate (cGMP). 2) cGMP is an intracellular mediator that can stimulate kidney cells to increase secretion of Na+. B. The intracellular portion of the receptor functions as an enzyme. FIGURE 17.21 1) For example, when insulin binds to the insulin receptor, the inner part of the receptor adds a phosphate group from ATP to itself and other proteins. 2) The phosphorylated receptor (or other proteins) activates intracellular mediators, which stimulate the cell to increase glucose uptake. See table 17.8 for other examples. Cascade Effect FIGURE 17.22 1. Hormones that activate intracellular mediators often produce a cascade effect in which a few molecules activate several molecules, each of which activates several molecules, and so on. 2. Thus, the cascade effect is an amplification system in which the activation of a few molecules results in the activation of the many, many molecules that are responsible for the cell’s response. 17-12 Intracellular Receptors FIGURE 17.23 1. A hormone, such as aldosterone, diffuses through the plasma membrane and binds to the intracellular receptor. 2. The receptor/hormone combination activates a segment of DNA (a gene). 3. Messenger RNA is synthesized (transcription) and moves to ribosomes where an enzyme is synthesized (translation). 4. The enzyme produces the cell’s response. For example, aldosterone increases Na+ transport in the kidneys. See table 17.9 for other examples. Of membrane-bound receptors and intracellular receptors, which produces the more rapid response from a cell? Explain. 17-13