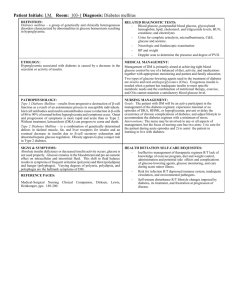
diabetes mellitus type diabetes mellitus type 1 diabetes mellitus type
advertisement

PATHOPHISIOLOGY OF DIABETES MELLITUS R. Mohammadi Biochemist (Ph.D.) Faculty member of Medical Faculty BLOOD GLUCOSE REGULATION METABOLIC FUELS Glucose F tt Acids Fatty A id Ketone Bodies Aminoacids ECONOMIC OF FUELS Cellular Capacity C ll Needs Cell N d Fuel Availability Hormonal Condition ROLE OF TISSUES Liver F tt Tissue Fatty Ti Muscle ROLE OF HORMONES Insulin Glucagon E i Epinephrine hi Cortisol Thyroid Hormone Growth Hormone GLUCOSE TRANSPORTERS GLUT1 GLUT1 GLUT2 GLUT 2 GLUT3 GLUT3 GLUT4 GLUT 4 GLUT5 GLUT 5 GLUT7 GLUT 7 All tissues Liver, β-cell, I t ti Intestine, kid kidney All Tissues Fatty Tissue, Muscle Intestine kidney Intestine, Endoplasmic Reticulum BLOOD GLUCOSE REGULATION G O FEEDING STATE NONFEEDING STATE FEEDING STATE ABSORPTION OF MONOSACCHARIDES O OS CC S ب درر دوو م رـرحله ور مكانيسممها ين ي كليه ازز همين تليالل ي سلولهايي اپپيـي ي ون .ول ش خون گردش ل ر تليالل ببهداخل ول اپپيـي ي تليالل و ) (۲انتقالل ازز سلول پي ي ول اپـي ل سلول جري روروده ببهداخل پذيرد (۱) :انتقالل ازز مجراي صورت مييپ ير ين ججذب منوساكاريدها ازز روروده .اين ب و ري ل ۲۵ -۳ججذب شكل بـراي بازجذب گلوكز و گاال كـتوز استفاده ميكنند. HEXOKINASE & GLUCOKINASE Glc + ATP Glc 6-p + ADP PATHWAYS OF G COS METABOLISM GLUCOSE O S Triacylglcerol Glycogen Glc 6-p Glcolysis Pentose Phosphate Uronic Acid INSULIN Prepro Pre proinsulin insulin (100 aa) Signal Peptide Proinsulin Pro insulin (86 aa) Peptide C I Insulin li (A Chain with 21 aa & B Chain 30 aa) مكانيسم ٓازا ازي فعاليت ت واسطه ف ال گلوكز هبه ا طه انكرااس ميششود .گل كز هاي پانك سلوللهاي طريق GLUT2اوارد ل ايش مي ايابد ،از ط ق گردش خخون افزا ش گلوكز در گ ش وقتي گل كز گلوكز (۱) .قت توسط گل كز انسولين ت ط ادسازي ان ل احل كان شكل ۳۹-۸مرا ل ٓ ٓ گلوكوكيناز وارد مسير گليكوليز شده كه نتيجه ان افزايش غلظت ATPميباشد ) ATP .(۲كانال پتاسيمي وابسته بـه ATPرا ميبندد كه نتيجه ان دپوالريزاسيون غشاء و بازشدن كانال كلسيمي وابسته به ولتاژ ميباشد ) .(۳با افزايش غلظت كلسيم داخلسلولي ) ،(۴اگزوسيتوز گرانولهاي ترشحي حاوي انسولين تحريك ميشود ).(۵ NONFEEDING STATE GLUCAGON Synthesis as Proglucagon 29 Amino Acids Act on Liver & Fatty Tissue Increased Glycogenolysis Glycogenolysis, Gluconeogenesis, Lipolysis, β-Oxidation EPINEPHRINE Synthesis from Tyrosine A t on Li Act Liver & Muscle M l Increased Glycogenolysis & Gluconeogenesis CORTISOL Synthesis from Cholesterol I Increased d Gluconeogenesis Gl i Increased Proteolysis Increasesd or Decreased Lipolysis THYROID HORMONE Sythesis from Tyrosine I Increased d Glycogenolysis Gl l i Increased Glucose Absorption GROWTH HORMONE 191 Amino Acids I Increased d Gluconeogenesis Gl i Inhibition of Glc Uptake Increased Lipolysis DIABETES MELLITUS (DM) DEFINITION Of DM Clinical DM Is A Syndrome of Disordered Metabolism with Inappropriate Hyperglycemia Due to an Absolute or Relative Deficiency of Insulin It May Be Due to Deficiency of Insulin Secretion Defect in Insulin Action or Secretion, Both Clinical Presentation of DM DM Is Clinically Presented by Three Polys which Are Due to Glycosuria Polyuria Polydipsia Polyphagia yp g COMPLICATIONS OF DM Acute Chronic ACUTE COMPLICATIONS OF DM Are Due to Reduced Insulin Activity and Increased Counter Regulatory Hormenes, Hormenes, specially glucagon Severity of Complications Are Dependent on Glucagon / Insulin Ration Acute Complications Are 1) Hyperglycemia 2) Diabetic Ketoacidosis (DKA) yp Coma 3) Hyperosmolar 4) Hypoglycemia HYPERGLYCEMIA Postprandial Hyperglycemia Fasting Hyperglycemia Glucosuria which results in Three Polys which are first presentations of overt DM: 1) Polyuria (and Nocturia Nocturia)) 2) Polydipsia 3) Polyphagia (and weight loss) loss) DIABETIC KETOACIDOSIS (DKA) Is duo to increased lipolysis due to absence of insulin activity, so it is more common in type 1 DM and is uncommon in type 2 DM May results in Coma due to hyperosmolality and acidosis Electrolyte imbalance may occurs: 1) Hyponatremia occurs due to sodium excretion in urine and i increased d plasma l water t because b off increased i d osmolality l lit 2) In spite of potassium excretion, plasma potassium level remains normal because of a shift of K+ out of cells. But during insulin therapy,, K+ move back into cells and hypokalamia results. therapy HYPEOSMOLAR COMA Is More Common in type 2 DM Results from Sever hyperosmolality due to sever hyperglycemia yp g y ( >800 >800 mg/ mg/dL g dL)) and severe dehyratation HYPOGLYCEMIA Is complication of insulin treatment in both type 1 DM and type 2 DM, but may also occur with oral oral hypoglycemic drugs, such as sulfonyureas Acute response is mediated by counter regulatory hormones Common symptoms are night sweats, nightmares, morning headaches CHRONIC COMPLICATIONS OF DM Microvascular Macrovascular M l Others CHRONIC COMPLICATIONS OF DM Microvascular Eye Disease R ti Retinopathy, th Macular M l Edema Ed Neuropathy Sensory & Motor, Autonomic Nephropathy CHRONIC COMPLICATIONS OF DM Macrovascular Coronary Artery Diseases P i h l Vascular Peripheral V l diseases di Cerebrovascular Diseases CHRONIC COMPLICATIONS OF DM Others Gastrointestinal p Diarrhea,, Gastroparesia Genitourinary Uropathy, Sexual Dysfunction Dermatology Infections Eyes Glucoma, Cataract CLASSIFICATION OF DIABETES MELLITUS American Diabetes Association (ADA) Classify DM into Four Calss Calss:: Type 1 Type 2 Other Specific p Types yp GDM DM Type ype 1 5% - 10% 10% Frequency Previoysly Named Juvenile-onset DM JuvenileInsulin--dependent DM Insulin Abruptt Onset Ab O t Normal Body Weight Family History Is Less Common Autoimmune Often Ketones Present Total Insulin Deficiency DM Type 2 90% - 95 90% 95% % Frequency Previoysly y y Named Adult-onset DM AdultNoninsulin--dependent DM Noninsulin GraduaI Onset Obesity Family History Is Common No Autoimmune No Ketones Partial Insulin D fi i Deficiency / Resistance R i t DIABETES MELLITUS TYPE 1 Is an autoimmune disease caused by selective destruction of pancreatic beta cells Genetic susceptibility p y is related,, at leaset in p part,, to the inheritance of specific immune response genes associated with HLA HLA--DR/DQ on chromosome 6, as well as other genes and genetic markers I hypothesized Is h h i d that h a precipitating i i i events occurs, such as viral infection, infection, toxin exposure, exposure, or other environmental influence, influence, which trigers the autoimmune destruction of beta cells. DIABETES MELLITUS TYPE 1 Have 2 subtypes 1) Ia including 95 95% % 0f patients who have autoantibodies 2) Ib including 5% of patients who have not autoantibodies Autoantibodies includes Islet cell antibodies (ICA) glutamic acid decarboxylase (GAD) tyrosine phosphatasephosphatase-2 protein (IA2 (IA2) Insulin Autoantibodies (IAA) DIABETES MELLITUS TYPE 1 Is More common in Children Whom have rapid onset Also, may be seen in adults who often have slow progression which may results in Wrong Diagnosis as type 2 , so they are called Latent Autoimmune Diabetes of Adulthood (LADA) OBESITY , METABOLIC SYNDROME & TYPE 2 DIABETES OBESITY IS LIFE THREATENING Obesity Increases the Chance of Developing Type T pe II Diabetes Atherosclerosis Cancers of Colon, Breast, Prostate & Endometrium BODY MASS INDEX (BMI) Obesity y Is Defined in Terms of BMI Weight in Kg BMI = (Height in m)2 BMI BMI BMI BMI BMI < 18. 18.5 = 18. 18.5 – 24 24..9 = 25 – 29 29..9 = 30 – 40 > 40 Underweight Normal Overweight Obese Morbidly Obese FATTY TISSUE IS AN ENDOCRINE OC ORGAN O G Adipocytes Secrets Different Adipokins Adipokins:: Leptin Adiponectin Resistin Cytokines such as TNFH TNFH TNF H INCDUCES DYSLIPIDEMIA TNFH Hormone-sensitve Lipase Lipoprtein Lipase Clearance of VLDL from Circulation Hepatic Synthesis of TAGs Release of FFAs Into Circulation Hepatic Uptake off FFAs Blood VLDL Hepatic Synthesis of VLDL TNFH TNF H INDUCES DYSLIPIDEMIA TNFH Expression & Activity of LCAT Expression of ABC Transporters Blood HDL Expression of APo A-I A I & Apo Apo-A-IV A IV FFAs INDUCE HYPERGLYCEMIA FFAs Competitive Inhibition of GLUT2 & GLUT4 Activation of PKC Phosphorylation of IRS-1 IRS 1 & IRS-2 IRS 2 GLUT4 Translocation In Muscle Blood Glucose Interfering with Down-Regulation of Gluconeogenesis In Liver PANCREATIC COMPENSATION Hyperinsulinemia yp Increased Cell Proliferation Stimulation of Sympatthetic Nervous System Normal or Near Normal Blood Glucose Increased Risk of Different Types Of Cancers Na & Water Retention Vasoconstriction Hypertension DECOMPENSATION PROCESS Increased FFAs and/or Cytokines Gradual Loss of the Ability of the Pancreas to Overproduce Insulin Increased Blood Glucose Type 2 Diabetes Begins MTABOLIC SYNDROME The insulin resistance associated with obesityy increases the risk of developing type 2 diabetes, diabetes, heart disease, disease, hypertension hypertension,, and several types of cancers cancers.. Increased risk of some of these diseases may occur long before the patient becomes diabetic, so the condition between the onset of insulin resistance and development of type 2 diabetes is referred as metabolic syndrome METABOLIC SYNDROME WHO Defines Metabolic Syndrome as Two or More of the Following Conditions: Abdominal Abd i l obesity b it Dyslipidemia (Increased VLDL and Decreased HDL) Hypertenstion Insulin Resistant (Modest increase in FBS) METABOLIC SYNDROME Defining criteria according to the Third Report of NCEP Expert panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults i l d the include th presence off Three Th or More M off the th following conditions: Impaired p Fasting g Glucose Blood Pressure ≥ 135 / 85 mmHg Waist circumference > 102 cm in men and > >88 88 cm in women Serum TG ≥ 150 mg/dL mg/dL HDL--C < 40 mg/ HDL mg/dL dL in men and < 50 mg/ mg/dL dL in women RISK FACTORS OF TYPE 2 DM Family y History y Of Diabetes Obesity Inactivity Hi h Blood High Bl d Pressure P Low HDL or High TG History of GDM or Child Birth > 4 kg History of Impaired GTT Race : Americans, Africans Polycystic Ovary Syndrome or Acanthosis Nigricans History of Vascular Diseases OTHER SPECIFIC TYPES 1) Genetic Defects of Beta Cell Function M t it -onsett diabetes MaturityMaturity di b t off the th young (MODY) 2) Genetic Defects in Insulin Action Leperchaunism syndrome 3) Pacntreatic Diseases Pancreatitis, Cystic Fibrosis, Hemochromatosis, Neoplasms 4) Endocrinopathies Hyperthyroidism, Cushing, Pheochromocytoma, Pheochromocytoma, Glucagonoma, Glucagonoma, Aldostronoma 5) Drugs Glucocorticoides,, Nicotinic Acid, Thyroid Hormones, Phenytoein, Glucocorticoides Phenytoein, Thiazides, α-Interferon, Beta Beta--Blockers 4) Infections Congenital Rubella, Coxsakie Coxsakie,, CMV 5) Genetic Defect of B Cell Function 6) Other Genetic Syndromes Down, Klinfelter, Klinfelter, Turner, Chorea, Porphyria GESTATIONAL DIABETES S (G MELLITUS (GDM)) Is defined as glucose intolerance that develops p or is first recognized g during pregnancy Develops during approximately 7% of all pregnancies There is both insulin insensitivity and failure to increase insulin secretion Low-Risk Women LowLess than 25 years Normal weight before pregnancy Race Race Absence of DM in first related Absence of abnormal glucose intolerance Absence of complicated pregnancy High-Risk Women HighMore than 37 years Pregnancy weight > 80 kg Race Race Family y history y of DM Polycystic ovary syndrome Previous macrosomia Previous unexplained stillbirth