1
2
3
4
American Nurses Association
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
NURSING INFORMATICS: SCOPE AND STANDARDS OF
PRACTICE
September 13, 2007
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
Draft for Review by
Congress on Nursing Practice and Economics
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
1
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
Acknowledgements
Workgroup Members (2007)
Nancy Staggers, PhD, RN, FAAN, Chairperson
Michele Calogero, MSN, RN
Margaret F. Budnik, DM, RN
Diane Castelli, RN
Melissa Christensen
Mary F. Clarke, PhD, RN, BC
Tina Dieckhaus, BSN, RN-BC, Leader, Integration and Tenets
Paulette Fraser, MS, RN-BC, Co-leader Metastructures
Josette Jones, PhD, RN-BC, Co-leader Competencies
Sally Kellum, MSN, RN-C
Rosemary Kennedy, MBA, RN, Co-leader NI Standards
Kathleen Krichbaum, RN, PhD
Sheryl LaCoursiere, PhD, RN-BC, Leader, Functional Areas
Angela Lewis, BSN, RN-BC
Teresa McCasky, MBA, BSN, RN-BC
Ramona Nelson, PhD, RN, FAAN, Co-leader, Metastructures
Agnes Padernal, PhD, RN
Amy Peck, RN
Mollie R. Poynton PhD, APRN
Loretta Schlachta-Fairchild, PhD, RN, CHE
Norma Street, MSN, RN
Sharon Sweeney Fee, PhD, RN, Leader, Ethics section
Dawn Weathersby, MS, RN, Co-leader NI Standards
Jill Winters, PhD, RN
Seth Wolpin PhD MPH RN, Co-leader Competencies
Lisa Wynn, MA, RN-BC
ANA Staff
Carol J. Bickford, PhD, RN-BC, Content Editor
Yvonne D. Humes, MSA
Therese Myers, JD
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
2
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
51
52
53
54
55
Table of Contents
Acknowledgments ......................................................................................................................... 2
Introduction .................................................................................................................................... 5
Metastructure, Concepts, and Tools of Nursing Informatics .................................................... 6
Metastructures: Data, Information, and Knowledge......................................................................... 6
Sciences Underpinning Nursing Informatics .................................................................................. 10
Language as a Tool for Nursing Informatics .................................................................................. 10
Concepts and Tools from Information Science and Computer Science ........................................ 10
Human—Computer Interaction and Related Concepts ................................................................. 10
Phenomena of Nursing .................................................................................................................. 14
Functional Areas for Nursing Informatics ................................................................................. 15
Administration, Leadership, and Management ............................................................................. 18
Analysis .......................................................................................................................................... 19
Compliance and Integrity Management ......................................................................................... 21
Consultation .................................................................................................................................. 22
Coordination, Facilitation and Integration ...................................................................................... 23
Development .................................................................................................................................. 24
Education and Professional Development ..................................................................................... 25
Policy Development and Advocacy................................................................................................ 26
Research and Evaluation ............................................................................................................... 27
Integrated Areas............................................................................................................................. 28
Functions Areas Conclusion .......................................................................................................... 29
Informatics Competencies .......................................................................................................... 30
The Intersection of Informatics Competencies and NI Functional Areas....................................... 30
Developing a New Competencies Matrix ....................................................................................... 37
Competencies and Metastructures ................................................................................................ 37
Work in Progress............................................................................................................................ 37
NI Competencies Conclusion......................................................................................................... 37
The Integration of Nursing Informatics...................................................................................... 38
Tenets of Nursing Informatics .................................................................................................... 41
Ethics in Nursing Informatics ..................................................................................................... 41
The Future of Nursing Informatics ............................................................................................. 44
Standards of Nursing Informatics Practice ............................................................................... 56
Overarching Principles for Nursing Informatics Practice................................................................57
Standards of Practice ....................................................................................................................58
Standard 1 Assessment................................................................................................................ 58
Standard 2 Problem or Issues ...................................................................................................... 58
Standard 3 Outcomes Identification...............................................................................................58
Standard 4 Planning....................................................................................................................... 59
Standard 5 Implementation ............................................................................................................ 59
Standard 5A Coordination of Activities...........................................................................................61
Standard 5B Health Teaching, Health Promotion, and Education for Informatics Solutions..........61
Standard 5C Consultation..............................................................................................................62
Standard 6 Evaluation....................................................................................................................62
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
3
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
Standards of Professional Performance ................................................................................... 63
Standard 7 Education..................................................................................................................... 64
Standard 8 Professional Practice Evaluation................................................................................. 64
Standard 9 Quality of Nursing Informatics Practice ....................................................................... 65
Standard 10 Collegiality ................................................................................................................. 66
Standard 11 Collaboration ............................................................................................................. 66
Standard 12 Ethics......................................................................................................................... 67
Standard 13 Research ................................................................................................................... 68
Standard 14 Resource Utilization .................................................................................................. 68
Standard 15 Advocacy ................................................................................................................... 69
Standard 16 Leadership................................................................................................................. 70
Glossary ........................................................................................................................................ 72
References....................................................................................................................................74
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
4
1
2
3
THE SCOPE OF NURSING INFORMATICS PRACTICE
Introduction
4
Nursing informatics (NI) is a specialty that integrates nursing science, computer science, and
5
information science to manage and communicate data, information, knowledge and wisdom in
6
nursing practice. NI supports consumers, patients, nurses, and other providers in their decision-
7
making in all roles and settings. This support is accomplished through the use of information
8
structures, information processes, and information technology.
9
The goal of NI is to improve the health of populations, communities, families, and individuals
10
by optimizing information management and communication. These activities include the design
11
and use of informatics solutions and/or technology to support all areas of nursing, including, but
12
not limited to, the direct provision of care, establishing effective administrative systems,
13
designing useful decision support systems, managing and delivering educational experiences,
14
enhancing life long learning, and supporting nursing research.
15
The NI definition remains essentially synonymous with that found in the 2001 Scope and
16
Standards of Nursing Informatics but now includes the additional concept of wisdom. The term
17
individuals refers to patients, healthcare consumers and any other recipient of nursing care or
18
informatics solutions. The term patient refers to consumers in both a wellness and illness model.
19
The discussion of the definition and goal of nursing informatics evolved from work by Staggers
20
and Thompson (2002).
21
NI is one example of a discipline-specific informatics practice within the broader category of
22
health informatics. NI has become well established within nursing since its recognition as a
23
specialty for registered nurses by the American Nurses Association (ANA) in 1992. It focuses on
24
the representation of nursing data, information, knowledge (Graves and Corcoran, 1989) and
25
wisdom (Nelson, 1989; Nelson, 2002) as well as the management and communication of
26
nursing information within the broader context of health informatics. Nursing informatics (1)
27
provides a nursing perspective, (2) illuminates nursing values and beliefs, (3) denotes a practice
28
base for nurses in NI, (4) produces unique knowledge, (5) distinguishes groups of practitioners,
29
(6) focuses on the phenomena of interest for nursing, and (7) provides needed nursing
30
language and word context to health informatics (Brennan, 2003).
31
The scope and standards of practice address both informatics nurse specialists (INSs), those
32
formally prepared at the graduate level in informatics or a related field, as well as informatics
33
nurses (INs), those generalists who have gained experience in the field but do not have
34
educational preparation at the graduate level in an informatics-related area. NI is at the end of a
35
transition period between these two title distinctions and function distinctions. Informatics
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
5
1
practice is complex and requires graduate educational preparation for all nurses working in the
2
specialty going forward.
3
Nursing Informatics: Scope and Standards of Practice expands upon earlier work within NI,
4
building upon historical knowledge (ANA, 1994, 1995, 2001) and includes new, state-of-the-
5
science material for the specialty. Because of the rapid changes in related sciences, NI roles,
6
and advances in the science of informatics, a new document was needed. This revision
7
provides new material including: a) adding the concept of wisdom to NI metastructures, b)
8
transitioning the roles section away from job titles to role functions that may be integrated within
9
various NI roles and subspecializations, c) identifying commonalities between INSs and other
10
informatics specialists d) providing a distinction between INs and INSs, e) expanding the work
11
on NI competencies to describe typical NI competencies for typical NI functional areas, f)
12
expanding the discussions in ethics, human-computer interaction and the future of NI, g)
13
integrating new functions across clinical practice and NI and h) changing the section previously
14
titled “Boundaries of Nursing Informatics” to a discussion about the cross-disciplinary nature of
15
NI acknowledging the blurring of boundaries among other informatics and nursing specialties.
16
This revised scope and standards document can be useful in several ways. First, the
17
document outlines the attributes and definition of the specialty. Second, the document can be
18
useful to educational programs and NI practitioners as a reference and guide. Third, this work
19
can serve as a reference for employers and regulatory agencies to assist with developing
20
position descriptions, determining required informatics competencies, and initiating NI positions
21
in health organizations. Last, the material can serve as a source document for legal opinions,
22
funding agencies, and others seeking to improve health through NI.
23
Metastructures, Concepts, and Tools of Nursing Informatics
24
To understand NI, its metastructures, sciences, concepts and tools are first explained.
25
Metastructures are overarching concepts used in theory and science. Also of interest are the
26
sciences underpinning NI, concepts and tools from information science and computer science,
27
human–computer interaction and ergonomics concepts, and the phenomena of nursing.
28
Metastructures: Data, Information, Knowledge, and Wisdom
29
In the mid 1980’s Blum (1986) introduced the concepts of data, information and knowledge as a
30
framework for understanding clinical information systems and their impact on health care. He
31
did this by classifying the then current clinical information systems by the three types of objects
32
that these systems processed. These were data, information and knowledge. He noted that the
33
classification was artificial with no clear boundaries; however, increasing complexity between
34
the concepts existed. In 1989, Graves and Corcoran built on this work when they published
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
6
1
their seminal work that described the study of nursing informatics using the concepts of data,
2
information and knowledge. The article contributed two broad principles to NI that will be
3
acknowledged here. The first contribution was a definition of nursing informatics (NI) that was
4
widely accepted in the field.
5
The second contribution of Graves and Corcoran (1989) was an information model that
6
identified data, information, and knowledge as key components of NI practice. The Graves
7
model is presented in Figure 1.
Management
Processing
Data
8
9
Information
Knowledge
Figure 1. Conceptual Framework for the Study of Nursing Knowledge.
10
Reprint permission has been requested.
11
Graves and Corcoran (1989) drew from Blum (1986) to define the three concepts as follows:
12
•
Data are discrete entities that are described objectively without interpretation,
13
•
Information is data that are interpreted, organized, or structured, and
14
•
Knowledge is information that is synthesized so that relationships are identified and
15
formalized.
16
Data, which are processed to information and then knowledge, may be obtained from
17
individuals, families, communities, and populations. Data, information, and knowledge are of
18
concern to nurses in all areas of practice. For example, data derived from direct care of an
19
individual may then be compiled across persons and aggregated for decision-making by nurses,
20
nurse administrators, or other health professionals. Further aggregation may address
21
communities and populations. Nurse-educators may create case studies using these data, and
22
nurse-researchers may access aggregated data for systematic study
23
As an example, an instance of vital signs for an individual—heart rate, respiration,
24
temperature, and blood pressure—can be considered (a set of) data. A serial set of vital signs
25
taken over time, placed into a context, and used for longitudinal comparisons is considered
26
information. That is, a dropping blood pressure, increasing heart rate, respiratory rate, and fever
27
in an elderly, catheterized person are recognized as being abnormal for this person. The
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
7
1
recognition that the person may be septic and, therefore may need certain nursing interventions
2
reflects information synthesis (knowledge) based on nursing knowledge and experience.
3
Figure 2 builds on the work of Graves and Corcoran by providing a depiction of the
4
relationship of data, information, and knowledge. As data are transformed into information and
5
information into knowledge, each level increases in complexity and requires greater application
6
of human intellect. The X-axis in Figure 2 represents interactions within and between the
7
concepts as one moves from data to wisdom; the Y-axis represents the increasing complexity of
8
the concepts and interrelationships.
Wisdom
Understanding,
applying,
applying with
compassion
Constant Flux
Knowledge
Interpreting,
Integrating
and understanding
Increasing
Complexity
Information
Organizing and
interpreting
Data
Naming,
Collecting
And organizing
9
10
.
11
Figure 2. The Relationship of Data, Information, Knowledge and Wisdom
12
13
*Reprinted with modification from Englebardt, S. & Nelson, R. Health Care Informatics: An
Interdisciplinary Approach, Copyright (2002), Figure 1-4, page 13 with permission from Elsevier.
Increasing Interactions and Inter-relationships
14
Wisdom is defined as the appropriate use of knowledge to manage and solve human
15
problems. It is knowing when and how to apply knowledge to deal with complex problems or
16
specific human need (Nelson, 1989; Nelson, 2002). While knowledge focuses on what is known,
17
wisdom focuses on the appropriate application of that knowledge. For example, a knowledge
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
8
1
base may include several options for managing an anxious family, while wisdom would guide
2
the decisions about which of these options are most appropriate with a specific family. As this
3
example demonstrates, the scope of NI is based on the scope of nursing practice and nursing
4
science with a concentration on data, information and knowledge. It is not limited by the current
5
technologies. If the study of NI was limited to what the computer can process, the study of
6
informatics could not fully appreciate the interrelationships that exist between nursing
7
science/practice and information science/technology. NI must consider how nurses have an
8
impact on the technology and how the technology has an impact on nursing. An understanding
9
of this interaction makes it possible to understand how nurses create knowledge and how they
10
11
make use of that knowledge in their practices.
The appropriate use of knowledge involves the integration of empirical, ethical, personal and
12
aesthetic knowledge in the process of implementing actions. The individual must apply a high
13
level of empirical knowledge in understanding the current situation, apply a professional value
14
system in considering possible actions, be able to predict the potential outcome of these actions
15
with a high level of accuracy, and then to have the will power to carry out the selected action in
16
the current environment. An example of applied wisdom demonstrating this integration in NI is
17
the appropriate use of information management and technological tools to support effective
18
nursing practice.
19
The addition of wisdom raises new and important research questions. This challenges the
20
discipline to develop tools and processes for classifying, measuring and coding wisdom as it
21
relates to nursing, NI, and informatics education. These research avenues will help clarify the
22
relationships between wisdom and the intuitive thinking of expert nurses. Such research will be
23
invaluable in building information systems to support expert healthcare practitioners as well
24
support the decision process of more novice nurses and others.
25
Two interrelated forces have encouraged the expansion of the NI model to include wisdom.
26
First, the initial work was limited to the types of objects processed by automated systems in the
27
mid 1980’s. However, NI is now concerned with the use of information technology to improve
28
the access and quality of health care that is delivered to individuals, families and communities.
29
The addition of the concept of wisdom expands the focus of the model from the technology and
30
the processing of objects to include the interaction of the human with the technology and
31
resultant outcome(s).
32
Nurses have been recognized as primary users and processors of information for over 40
33
years (Jydstrup and Gross, 1966; Zielstroff, 1981). Other authors have focused on the amount
34
of time nurses actually spend administering direct care to patients or the time involved in
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
9
1
documentation (Norrie, 1999; Jinks, 2000; Harrison, 2002). In fact, Jydstrup and Gross (1966)
2
estimated in the 1960s that nurses in acute care spent 30% to 40% of their time in information
3
processing activities. In her frequently cited article, titled, “How do nurses spend their time?”
4
Hendrickson (1990) determined that nurses spend only 31% of their time with patients. Other
5
aspects of the nursing role included information management with ancillary services.
6
Sciences Underpinning Nursing Informatics
7
A significant contribution of Graves and Corcoran (1989) was a description and definition of
8
nursing informatics (NI) that was widely accepted in the field in the 1990s. It stated that NI is a
9
combination of nursing science, information science, and computer science to manage and
10
process nursing data, information, and knowledge to facilitate the delivery of health care. The
11
central notion was that the application of these three core sciences was what made NI unique
12
and differentiated it from other informatics specialties.
13
In addition to these three core sciences, other sciences may be required to solve informatics
14
issues. James Turley expanded the model of NI to include cognitive science (1996). Certainly
15
the cognitive aspect of humans is a critical piece for INSs and for INs to understand. However,
16
other sciences may be equally as critical depending upon the issue at hand. For example, if the
17
INS is dealing with a system’s implementation in an institution, an understanding of
18
organizational theory may be germane to successful implementation (Staggers & Thompson,
19
2002). As science evolves, other core sciences may need to be included in future nursing
20
informatics models.
21
Although the core sciences are foundational to the work in NI, the practice of the specialty
22
can be considered an applied science rather than a basic science. The combination of sciences
23
creates a unique blend that is greater than the sum of its parts, a unique combination that
24
creates the definitive specialty of NI. Further, informatics realizes its full potential within health
25
care when it is grounded within a discipline, in this case, the discipline is nursing. Computer and
26
information science applied in isolation will have less impact if not applied within a disciplinary
27
framework. Through application, the science of informatics can solve critical healthcare issues
28
of concern to a particular discipline.
29
Language as a Tool for Nursing Informatics
30
Many of the tools used by the informatics nurse and informatics nurse specialist are based on
31
metastructures and concepts that incorporate knowledge from nursing and other health and
32
information sciences. Nursing knowledge is developed through the ability to extract, synthesize,
33
and analyze data that specifically defines nursing phenomena. Many different languages and
34
ways of organizing data, information, and knowledge exist based on different concepts.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
10
1
The creation of nursing taxonomies and nomenclatures has occurred over the past years
2
allowing these iterations to occur. The ANA has formalized the recognition of these
3
languages/vocabularies through a review process of the Committee on Nursing Practice
4
Information Infrastructure (CNPII). For more information, see Table 1 and
5
http://nursingworld.org/npii/terminologies.htm. To promote the integration of standardized
6
terminologies within information technology solutions, the ANA’s Nursing Information and Data
7
Set Evaluation Center (NIDSEC) conducts the following activities:
8
•
9
10
11
Develops and disseminates standards pertaining to information systems that support the
documentation of nursing practice, and
•
Evaluates voluntarily submitted information systems against these standards.
Table 1. ANA Recognized Terminologies and Data Element Sets
Setting Where Developed
Content
1. NMDS
Nursing Minimum Data Set
Currently Recognized
All Nursing
Clinical Data Elements
2. NMMDS
Nursing Management Minimum Data
Set
Currently Recognized
All Settings
Nursing Administrative Data
Elements
All Nursing Care
Diagnoses, Interventions, and
Outcomes
4. ICNP®
International Classification of Nursing
Practice
Currently Recognized
All Nursing
Diagnoses, Interventions, and
Outcomes
5. NANDA
NANDA International
Currently Recognized
All Nursing
Diagnoses
6.NIC
Nursing Interventions Classification
Currently Recognized
All Nursing
Interventions
7. NOC
Nursing Outcomes Classification
Currently Recognized
All Nursing
Outcomes
Home Care, Public Health, and
Community
Diagnoses, Interventions, and
Outcomes
Data Element Sets
Nursing Developed Terminologies
3. CCC
Clinical Care Classification
Currently Recognized
8. OMAHA SYSTEM
Omaha System
Currently Recognized
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
11
9. PCDS
Patient Care Data Set
Retired
Acute Care
Diagnoses, Interventions, and
Outcomes
Perioperative
Diagnoses, Interventions and
Outcomes
11. ABC
ABC Codes
Currently Recognized
Nursing and Other
Interventions
12. LOINC®
Logical Observation Identifiers
Names and Codes
Currently Recognized
Nursing and Other
Outcomes and Assessments
13. SNOMED CT
Systematic Nomenclature of Medicine
Clinical Terms
Currently Recognized
Nursing and Other
Diagnoses, Interventions, and
Outcomes
10. PNDS
Perioperative Nursing Data Set
Currently Recognized
Multidisciplinary Terminologies
1
At a higher level of structure, several resources have developed to facilitate interoperability
2
between different types of systems of concepts and nomenclature. For instance, the Systemized
3
Nomenclature of Medicine (SNOMED-CT; http://www.snomed.org) is considered a universal
4
healthcare reference terminology and messaging structure. For nursing, SNOMED CT enables
5
terminology from one system to be mapped to concepts from another, e.g., Omaha System with
6
North American Nursing Diagnosis Association (NANDA), Nursing Interventions Classification
7
(NIC) and Nursing Outcomes Classification (NOC). On a larger scale, the Unified Medical
8
Language System of the National Library of Medicine (UMLS;
9
http://www.nlm.nih.gov/research/umls) incorporates the work of over one hundred vocabularies,
10
including SNOMED CT (http://www.nlm.nih.gov/research/umls/metaa1.html). The informatics
11
nurse and informatics nurse specialist must be aware of these tools, and may be called upon to
12
understand the concepts of one or more languages, the relationships between related concepts,
13
and integration into existing vocabularies for a given organization.
14
The importance of languages and vocabularies cannot be understated. Informatics nurses
15
must seek a broader picture of the implications of their work, and the uses and outcomes of
16
languages and vocabularies for end users. For instance, nurses working in mapping a home
17
care vocabulary with an intervention vocabulary must see beyond the technical aspect of the
18
work. They must understand that there may be a case manager for a multi-system health
19
organization or a home care agency who will be developing knowledge of nursing acuity and
20
case mix based on the differing vocabularies that they have integrated. The INS must attempt to
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
12
1
envision the differing functions that may be used with the data, information and knowledge that
2
have been created.
3
Concepts and Tools from Information Science and Computer Science
4
Informatics tools and methods from computer and information sciences are considered
5
fundamental elements of NI, including:
6
•
Information technology
7
•
Information structures
8
•
Information management
9
•
Information communication
10
Information technology includes computer hardware, software, communication, and network
11
technologies, derived primarily from computer science. The other three elements are derived
12
primarily from information science; a) Information structures organize data, information, and
13
knowledge for processing by computers, b) Information management is an elemental process
14
within informatics in which one is able to file, store, and manipulate data for various uses, and c)
15
Information communication processes enable systems to send data, and to present information
16
in a format that improves understanding. The use of information technology distinguishes
17
informatics from more traditional methods of information management. Thus, NI incorporates
18
the above four additional elements from computer and information science. Underlying all of
19
these are human–computer interaction concepts discussed in the next section.
20
Human–Computer Interaction and Related Concepts
21
Human–computer interaction (HCI), usability and ergonomics concepts are of fundamental
22
interest to the INS. Essentially, HCI deals with people, software applications, computer technology
23
and the ways they influence each other (Dix, Finlay, Abowd, & Beale et al., 2004). Elements of
24
HCI are rooted in psychology, social psychology and/or cognitive science. However, the design,
25
development, implementation, and evaluation of applications derive from applied work in
26
computer science, the specific discipline at hand (in this case nursing), and information science.
27
For example, an INS would assess an application before purchase to determine whether the
28
application design complements the way nurses cognitively process medication orders.
29
A related concept is usability which deals with specific issues of human performance during
30
computer interactions for specific tasks within a particular context (Dix, et al., 2004). Usability
31
issues address the efficiency and effectiveness of an application. For example, an INS might
32
study the ease of learning an application, the ease of using an application, or the speed of task
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
13
1
completion and errors that occurred during application use when determining which system or
2
application would be best utilized on a nursing unit.
3
The term ergonomics typically is used in the United States to describe the design and
4
implementation of equipment, tools, and machines related to human safety, comfort, and
5
convenience. Commonly, the term ergonomics refers to attributes of physical equipment or to
6
principles of arrangement of equipment in the work environment. For instance, an INS may
7
have a role in ensuring that good ergonomics principles are used in an intensive care unit to
8
select and arrange various devices to support workflow for cross-disciplinary providers as well
9
as patients’ families.
10
HCI, usability, and ergonomics are related concepts typically subsumed under the rubric of
11
human factors or how humans and technology relate to each other. The overall goal is better
12
design for software, devices and equipment to promote optimal task completion in various
13
contexts or environments. Optimal task completion includes the concepts of efficiency and
14
effectiveness, including considerations about the safety of the user. These concepts are
15
essential for the INS and IN to understand for effective strategies to develop, select, implement,
16
and evaluate information structures and informatics solutions.
17
The importance of human factors in healthcare was elevated with the Institute of Medicine’s
18
2001 report (IOM, 2001). Before this, HCI and usability assessments and methods were being
19
incorporated into health at a glacial speed. In the past 5 years the number of HCI and usability
20
publications in healthcare has increased substantially. Vendors have installed usability
21
laboratories and incorporated usability testing of their products into their systems lifecycles. The
22
FDA has mandated usability testing as part of their approval process for any new devices (FDA,
23
2007). Thus, HCI and usability are critical concepts for INs and INSs to understand. Numerous
24
usability methods and tools are available, e.g., heuristics (rules of thumb), naturalistic
25
observation and think aloud protocols. Readers are referred to HCI references to learn these
26
methods.
27
Phenomena of Nursing
28
The metaparadigm of nursing comprises four key concepts: nurse, person, health, and
29
environment. Nursing actions are based upon the inter-relationships between the concepts and
30
are related to the values nurses hold relative to them. Nurses make decisions about
31
interventions from their unique perspectives. Decision-making is the process of choosing among
32
alternatives. The decisions that nurses make can be characterized by both the quality of
33
decisions and the impact of the actions resulting from those decisions. As knowledge workers,
34
nurses make numerous decisions that affect the life and well-being of individuals, families, and
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
14
1
communities. The process of decision-making in nursing is guided by the concept of critical
2
thinking. Critical thinking is the intellectually disciplined process of actively and skillfully using
3
knowledge to conceptualize, apply, analyze, synthesize, and/or evaluate data and information
4
as a guide to belief and action (Scriven and Paul, 1997).
5
Clinical wisdom is the ability of the nurse to add experience and intuition to a situation
6
involving the care of a person (Benner, 1999). Wisdom in informatics is the ability of the
7
informatics nurse specialist to evaluate the documentation drawn from a Health Information
8
System (HIS) and the ability to adapt or change the system settings or parameters to improve
9
the workflow of the clinical nurse.
10
Nurses’ decision-making is described as an array of decisions that include specific
11
behaviors, as well as cognitive processes surrounding a cluster of issues. For example, nurses
12
use data transformed into information to determine interventions for persons, families, and
13
communities. Nurses make decisions about potential problems presented by an individual and
14
about appropriate recommendations for addressing those problems. They also make decisions
15
in collaboration with other health care professionals such as physicians, pharmacists or social
16
workers. Decisions also may occur within specific environments, such as executive offices,
17
classrooms, and research laboratories.
18
An information system collects and processes data and information. Decision support
19
systems are computer applications designed to facilitate human decision making processes.
20
Decision support systems are typically rule-based, using a specified knowledge base and a set
21
of rules to analyze data and information and provide recommendations. Other decision support
22
systems are based upon knowledge models induced directly from data, regression or
23
classification models that predict characteristics or outcomes.
24
An expert system is a type of decision support system that implements the knowledge of
25
one or more human experts. Recommendations take the form of alerts (for instance, calling user
26
attention to abnormal lab results, potential adverse drug events) or suggestions, e.g.,
27
appropriate medications, therapies or other actions (Haug, Gardner & Evans, 1999). Whereas
28
control systems implement decisions without involvement of a user, decision support systems
29
merely provide recommendations and rely upon the wisdom of the user for appropriate
30
application of these provided recommendations. As Blum demonstrated in the mid-1980s, the
31
concepts of data, information, knowledge and wisdom to exemplify different levels of automated
32
systems. The relationships among these concepts and information, decision support, and expert
33
systems are represented in Figure 4.
34
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
15
1
Wisdom
2
Expert
System
3
4
Knowledge
5
Decision
Support
System
6
Information
7
8
Information
System
9
Data
10
11
12
Figure 4. Levels and Types of Automated Systems
13
14
Reprinted from Englebardt, S. Nelson, R. Health Care Informatics: An Interdisciplinary
Approach, Copyright (2002), Figure 1-5, page 14 with permission from Elsevier.
15
16
In summary, the INS must be able to navigate the complexity of the relationships between
the following elements and understand how they facilitate decision-making:
17
•
Data, information, knowledge and wisdom
18
•
Nursing science, information science, computer science and other sciences of interest to
19
the issue at hand (e.g., cognitive science),
20
•
Nurse, person, health, environment, and decision-making
21
•
Information structures, information technology, managing and communicating
22
information
23
Functional Areas for Nursing Informatics
24
To describe the current work of INs, two relevant sources were reviewed. First, Newbold (2006)
25
created a database of job titles for nurses working in informatics beginning in the early 1980s.
26
As of early 2006, the database included titles for 6338 members of nursing and informatics
27
organizations, conference attendees and participants on NI electronic discussion lists. However,
28
the top 50 job titles did not translate into consistent responsibilities and job activities. INs with
29
different titles may actually be performing the same functions. Or INs with the same titles may,
30
in fact, perform very different functions.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
16
1
Second, a 2007 Health Information Management and Systems Society (HIMSS) survey of
2
776 informatics nurses categorized NI work into job responsibilities as opposed to job titles
3
(HIMSS, 2007). The top job responsibility of respondents was systems implementation (45%),
4
down from 67% in 2004. The second and third top job responsibilities reported by HIMSS
5
respondents were system development (41%) and liaison (35%).
6
Not only are there varied titles and activities within nursing informatics, the environments in
7
which INSs and INs practice are many and evolving. Initially, NI focused nearly exclusively in
8
the hospital setting. Now INs work in such diverse settings as home health and hospice
9
agencies, nursing homes, public and community health agencies, physician offices and
10
ambulatory care centers. They are employed by medical device vendors, large and small
11
software companies, web content providers, disease management companies, government
12
agencies and a host of other settings (Sensmeier, West & Horowicz, 2004). Across
13
environments, INSs and INs commonly practice in interdisciplinary healthcare environments. In
14
many settings, INSs and INs are expected to interact with information technology (IT)
15
professionals during all phases of the systems lifecycle. And more commonly than in the past,
16
INs may be the IT professionals themselves.
17
Nursing informatics supports multiple constituencies and stakeholders such as cross-
18
disciplinary team members, health care consumers, information technology professionals,
19
health care agencies and organizations. INSs are particularly well suited to work in
20
multidisciplinary and interdisciplinary environments. After all, nurses plan, implement and
21
coordinate activities involving multiple constituencies in a consumer-centered fashion from their
22
earliest days.
23
INSs use scientific and informatics principles. More importantly, they employ creative
24
strategies for meaningful informatics solutions. INSs also bring unique perspectives of cross-
25
disciplinary work, solid understanding of operational processes and the value of consumer
26
advocacy to informatics functions. INs and INSs may find that they need varying kinds of
27
advanced preparation to match the informatics project at hand. For instance, an INS
28
coordinating the implementation of an informatics solution such as a learning management
29
system may benefit from advanced preparation in adult education.
30
Many registered nurses have worked on informatics initiatives for many years and have built
31
their knowledge base and expertise from on-the-job experiences. The evolving mandate for
32
electronic information systems and the increasing complexity of healthcare services and
33
practice have raised the bar for the nursing professional. Select informatics competencies are
34
now becoming requirements for inclusion in all undergraduate and graduate nursing curricula.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
17
1
Accredited graduate level educational programs for this specialty nursing practice first were first
2
offered in 1989 and now are more commonly available, especially through distance education
3
and on-line programs. Rather than offer discipline specific informatics programs, some
4
universities have elected to embrace an interdisciplinary approach by offering graduate studies
5
in health informatics or bioinformatics. Completion of a graduate level informatics degree
6
program is now becoming the standard.
7
Professional certification as an informatics nurse became a reality in late 1995 when the
8
American Nurses Credentialing Center (ANCC) offered the nursing informatics certification
9
exam as its first computer-based examination. Informatics nurses and informatics nurse
10
specialists may elect to pursue other pertinent certifications in areas such as project
11
management, security and privacy, Six Sigma, network management, knowledge management,
12
A+ certification. Employers are beginning to use certification as a preferred characteristic during
13
the hiring process.
14
Because of the tendency to confuse roles with titles and the vast number of position titles
15
and lack of standardization among them, this section describes the functional areas for INSs
16
and INs. The following present overall functional areas of Nursing Informatics:
17
•
Administration, Leadership and Management
18
•
Analysis
19
•
Compliance and integrity management
20
•
Consultation
21
•
Coordination, facilitation and integration
22
•
Development
23
•
Educational and professional development
24
•
Policy development and advocacy
25
•
Research and evaluation
26
The last discussion in this section describes integrated functions, especially those crossing
27
clinical practice and informatics. INSs may be in positions that focus primarily in one functional
28
area, or, more frequently, several functional areas are combined within a particular NI position.
29
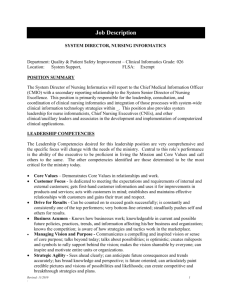
Administration, Leadership, and Management
30
As is true in administration in general, leadership and management functions in nursing
31
informatics consist of both higher-level and mid-level administrative functions (ANA, 2004b).
32
Increasingly, INSs are attaining senior leadership positions. Positions may be titled President,
33
Director, Chief Information Officer (CIO), or another similar leadership titles (AMIA NI Working
34
Group, 2006; Staggers and Lasome, 2005; Greene, 2004). In this functional capacity, nursing
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
18
1
informatics leaders are expected to be visionary and establish the direction of large-scale
2
informatics solutions. The nursing informatics leader often serves as a catalyst for developing
3
strategic plans, creating national or system policies and procedures, and serving as champion
4
for complex projects and disparate system users.
5
In mid-level management, INSs may supervise resources and activities for all components of
6
the organization’s systems life cycle. These activities may include needs analysis, requirements
7
development, design, development, selection and purchase, testing, implementation, and
8
evaluation of systems to support all facets of nursing and healthcare delivery. In all levels,
9
leadership functions combine the skills of superb communication, change management, risk
10
assessment and coalition building with political finesse, business acumen and strategic
11
application knowledge.
12
INSs serving in this functional area may focus most of their energies on leadership and
13
management. In other positions, administration may be a component of a position merged with
14
other functional areas. Examples might include:
15
•
INS at a large hospital system, supervising an implementation and education team,
16
representing nursing interests on various IT committees, performing project
17
management for multiple documentation projects and having oversight of nursing
18
standards and vocabularies utilized within applications.
19
•
Project Director for a clinical software company, managing implementation teams for
20
various client projects (hospitals to ambulatory facilities) and consulting with clients on all
21
aspects of systems selection, customization, adoption and use of software.
22
•
Grants Administrator for an information science research agency seeking and writing
23
grants that would fund Nursing Informatics (NI) related projects, designing budgets and
24
ensuring optimal allocation of resources.
25
Analysis
26
Data can be aggregated and analyzed in an infinite number of ways to synthesize knowledge,
27
inform decision support and outcomes management activities, and advance the science of
28
nursing informatics. The INS may use a number of tools to accomplish these activities. For
29
instance, taxonomies and clinical vocabularies may be used to tag consumer data to perform
30
higher level analyses. Using groups of data, meta-analyses may be employed to identify large
31
scale trends. Systems and requirements analysis may track the flow of data within a system,
32
customized to end-user needs. Workflow analysis may detail steps taken for a number of
33
different tasks.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
19
1
A major responsibility of the INS is to understand work process flows, the particular
2
informatics solution, and how these impact each other. Processes must be designed so that
3
interactions between users and computers are successful. Competency in formal systems
4
analysis techniques and use of statistical software may be required. These techniques compare
5
the capabilities and limitations of systems to be installed, and where changes must be designed.
6
Discrepancies between the current and ideal systems must be identified and redundancies
7
removed. The clinical analysis process also may include tools and systematic methods, such as
8
process redesign, to enhance safety and reduce inefficiencies.
9
INSs also may engage in the process of knowledge discovery in databases (KDD). Using
10
sound methodologies and practical evidence-based recommendations, the INS can discover
11
information and knowledge related to diverse areas of nursing practice. Knowledge discovery
12
methods, including data mining and machine learning methods, can be applied along with
13
statistical analysis and data visualization techniques, to identify and understand patterns in very
14
large data stores, such as enterprise data warehouses (Fayyad, 1996).
15
Analysis also is required with languages and taxonomies. Nursing languages such as
16
Nursing Interventions Classification (NIC), Nursing Outcomes Classification (NOC) and medical
17
vocabularies must be periodically re-evaluated for their applicability and currency (Center for
18
Nursing Classification and Clinical Effectiveness, 2004). Analysis of a meta-database such as
19
the Unified Medical Language System (UMLS; National Library of Medicine, 2006) requires
20
knowledge of nursing as well as medical vocabularies in order to analyze groups of taxonomies,
21
a perfect blend of needs for the expertise of an INS.
22
Analysis outcomes may be related to any domain of nursing practice—clinical, education,
23
research or administration – and the complexity and levels of outcomes must be determined for
24
health care consumers, populations and institutions. Analysis can include the use of Human-
25
Computer Interaction (HCI) principles and methods, discussed earlier. In that domain, INSs use
26
HCI tools and methods such as heuristics and cognitive walk-through to analyze the fit of users,
27
tasks, and contexts. Many other tools are available. Analysts use system tools to maintain data
28
integrity and reliability, facilitate data aggregation and analysis, identify outcomes and develop
29
performance measurements. These techniques allow nurses to contribute to the development of
30
a knowledge base consisting of the data, information, theories and models that are used by
31
nurses and other stakeholder in decision-making and support of healthcare processes. Analysis
32
activities may include:
33
34
•
Nursing analyst in a hospice setting who tracks health consumer data to establish a
case mix weight to determine nursing personnel allocations.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
20
1
•
2
3
research data related to diagnosis and nursing procedures
•
4
5
6
Quality improvement (QI) Specialist in a hospital system aggregating multi-site
Quality Assurance (QA) Analyst who works with nurse managers to retool current
work processes after examining existing system data in customized QA reports
•
An analyst who applies knowledge discovery methods to warehoused electronic data
to build a predictive model of patient falls.
7
8
Compliance and Integrity Management
With the emergence of national laws advocating for the protection of health information, INSs
9
are responsible for ensuring the ethical use of data, as well as data integrity, security and
10
confidentiality of protected health information. Part of the function of the INS is knowledge and
11
application of ethical standards. The advent of the Health Insurance Portability and
12
Accountability Act (HIPAA) of 1996 (U.S. Congress, 1996) regulations has required that
13
healthcare organizations revise operational procedures for staff, as well as technical processes,
14
to maintain compliance. INSs must be fluent in these new requirements, and are involved in
15
creating, implementing and assuring organizational change to meet new legislative mandates in
16
this area. Compliance also includes adherence to national and international standards. These
17
standards may include those from government agencies, for instance the Food and Drug
18
Administration (FDA) and National Institutes of Health (NIH), as well as accreditation
19
organizations such as The Joint Commission.
20
Ethical issues related to consumer privacy abound. One such issue occurs with knowledge
21
discovery in databases, where in some cases, prediction of outcomes based on individual
22
characteristics and past behavior or usage may be used to stratify groups of persons. Although
23
used in a variety of industries, the process of knowledge discovery in databases remains
24
controversial in health care. Adequate HIPAA protections must be in place, and relevant ethical
25
issues must be considered in all phases of data retrieval and analysis. For example, analysis of
26
genomic data may result in sensitive predictions of disease susceptibility. Given the explosive
27
growth of large data stores and enterprise data warehouses, knowledge discovery in databases
28
is a process important for extraction of useful information and knowledge while considering and
29
protecting consumer privacy. The INS can help ensure a balanced view of data access and
30
information privacy.
31
In health care, the emerging sciences of genomics and bioinformatics could be used to
32
predict risk for certain diseases, and thus insurability risk. Ethical issues surround the use of
33
new products, such as embedded technologies and radio-frequency identification (RFID), for
34
instance, and their application in caring for persons with Alzheimer’s Disease and other
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
21
1
dementias. As the profession matures, some of these issues will be resolved and associated
2
standards will be established. Upcoming requirements will continue to evolve, some of which
3
are mentioned in the scope of practice Future of NI section. Examples of compliance and
4
integrity management activities might include:
5
•
Security Officer for a hospital, ensuring that HIPAA standards are met by software
6
vendors within the organization, periodically monitoring software audit logs for breaches;
7
ensuring that passwords are not shared and backup and disaster procedures are in
8
place and operational.
9
•
10
11
Compliance Officer for a state health agency writing and enforcing policies that conform
to state and national laws as they relate to records retention.
•
12
Care Coordinator Administrator for a hospital system who ensures the confidentiality of
data transmitted via telehealth and telemedicine devices
13
Consultation
14
Informatics nurses and informatics nurse specialists apply informatics knowledge and skills to
15
serve as a resource to clients, both formally and informally, in external and internal settings.
16
Consultants are experts in the areas of process redesign, strategic/IT planning, system
17
implementation, writing informatics publications, evaluating clinical software products, working
18
with clients to write requests for proposals, performing market research, assisting in the
19
planning of conferences, academic courses, and/or professional development programs. These
20
expert INSs may work for a consulting firm, be employed as staff of the organization where they
21
consult, own an independent practice, or be identified as an expert by writing about nursing
22
informatics subjects and speaking at nursing informatics-related events. Flexibility, good
23
communication skills, breadth and depth of clinical and informatics knowledge, and excellent
24
interpersonal skills are needed to respond to what can be rapidly changing projects and
25
demands. Examples might include:
26
•
Consultant with individuals and groups in defining health care information problems and
27
identifying methods for implementing, utilizing and modifying IT solutions and data
28
structures that support health care access, delivery and evaluation.
29
•
30
31
32
Consulting as the Project Manager, ensuring that team members are performing duties
as assigned and the project is completed within budget.
•
Consulting with clients in writing requests for proposals to elicit vendor bids for
informatics solutions and in evaluating vendor responses.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
22
1
2
Coordination, Facilitation and Integration
One of the most common NI job functions is implementing informatics solutions. Nurses are
3
particularly well suited for IT implementation, as it essentially follows the nursing process of
4
assessment, planning, implementation and evaluation (ANA, 2004a). Also, the INS frequently
5
serves as a bridge between informatics solution users and IT experts. The IN or INS serves as
6
project coordinator, facilitating change management and integrating the information and
7
technology to transform processes during the project lifecycle. In this job function, project
8
management knowledge and skills are core to the successful outcome of the project. Project
9
coordination can span small, departmentally-centered applications to electronic health record
10
(EHR) enterprise-wide installations, from coordinating a rehabilitation module in the
11
rehabilitation unit to installing a full-EHR in 42 hospitals.
12
Of particular note, effective communication is an inherent part of many NI job functions, but
13
especially related to coordination, facilitation and integration activities. The IN and INS are at the
14
hub of cross-disciplinary communication among professional disciplines and IT, serving as
15
translators and integrators for system requirements and impacts.
16
In another instance, informatics nurses serve as the liaison between software engineers and
17
the end-users. In this capacity, the informatics nurse would ensure that the necessary testing or
18
research was performed to determine the end-user’s needs, and this information is conveyed to
19
the software engineer in terms the engineer could understand. Once the engineer has created a
20
product, the INS would then evaluate the utility of the product from the viewpoint of the end-
21
user. This liaison type of facilitation and coordination occurs in multiple environments. Ensuring
22
the integration of nursing vocabularies and standardized nomenclatures within applications is
23
another example. INSs in this functional capacity are also acting as usability experts and
24
making recommendations on ideal formats for the utilization of technology. Examples of
25
coordination, facilitation and integration might include:
26
•
Project Coordinator for a statewide electronic medical record implementation
27
coordinating all aspects of the project and supervising a cross-disciplinary team to train
28
public health personnel to use the application.
29
•
Project manager for a clinical software company managing the resources and activities
30
using tools such as project management software and project plans for clients whose
31
responsibilities cross inpatient and ambulatory areas
32
•
Clinical Liaison for a telehealth software vendor communicating with providers and
33
consumers to ensure that all parties are agreeable to development and implementation
34
plans and assure that providers using the system receive adequate technical education.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
23
1
•
Usability Expert on a software development team advising software engineers on screen
2
design from the standpoint of clinical documentation needs, performing and/or
3
coordinating testing of iterative designs and validating clinical requirements with the
4
users.
5
Development
6
Development was listed as the second most common job responsibility of HIMSS NI
7
respondents in 2007 (HIMSS, 2007). A developer is responsible for translating user
8
requirements into effective informatics solutions. INSs are involved in a vast array of
9
development activities, from conceptualizing models for applications, to software and hardware
10
design, to the design of education manuals to the design of complex technology networks. As
11
part of this function, INSs and INs participate in the process of designing, iterative development,
12
testing, and dissemination of quality informatics solutions for nurses, interdisciplinary providers,
13
and consumers. Understanding the information needs of nurses and the nursing profession,
14
consumers and consumer care processes, as well as knowledge of business, client services,
15
projected market directions, product design, product development methods, market research,
16
contemporary programming, systems design, and modeling language are essential for
17
practicing in a development environment.
18
Adherence to national standards and regulatory requirements are also essential to any
19
development work. In order to ensure interoperability between systems, INSs and INs involved
20
in system development must be knowledgeable about international standards requirements. For
21
instance, existing standards such as Health Level Seven (HL-7), International Organization for
22
Standardization (ISO), Current, Procedural Terminology (CPT), International Classification of
23
Disease (ICD), and Digital Image Communication (DICOM) group standards as well as Section
24
508 accessibility standards (Hammond, 1995; U.S. General Services Administration, 2006) may
25
be of importance. An understanding of the current work on standards is mandatory. Examples
26
of development responsibilities might include:
27
•
Developer with a personal health record software vendor creating user-friendly screens
28
for consumers to enter information as well as screens for nurses to use to display and
29
interpret the consumer data.
30
•
Database administrator with a large multi-site teaching organization managing an
31
expanded nursing vocabulary set for inpatient, ambulatory and home health nursing
32
documentation needs.
33
34
•
Nurse web-content developer for a consortium creating and validating content for
educational handouts, help and tool tips for user interfaces that display national
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
24
1
guidelines and educational tools. This would include new an innovative tools for
2
knowledge dissemination.
3
4
•
Programmer in a hospital IT Department coding software for documenting diabetic
education.
5
Education and Professional Development
6
Education is a critical component of many NI functions and may directly impact the success or
7
failure of any new/modified IT solution. Vendors of information systems frequently use the term
8
training when referring to client education; however in nursing, the broader concept of education
9
is used. Adherence to solid educational principles is a component of education and professional
10
development (American Nurses’ Association, 2000). Teaching nurses and nursing students,
11
healthcare consumers, and other interdisciplinary health team members about the effective and
12
ethical uses of information technology, as well as NI concepts and theories, is essential for
13
encouraging the optimal use of informatics solutions in nursing practice. Because of ever-
14
changing requirements in health information technology, continuing education is also essential.
15
INSs and INs in this functional capacity develop, implement and evaluate educational curricula
16
and educational technologies that meet the educational needs of learners.
17
In this role, educators and trainers assess and evaluate informatics skills and competencies
18
while providing feedback to learners regarding the effectiveness of the learning activity and the
19
learner’s ability to demonstrate newly acquired skills. Educators and trainers manage, evaluate,
20
report and utilize data and information related to learners and the educational delivery system.
21
These INSs are innovators in defining and developing educational technologies, integrating the
22
solutions into the educational and practice environments, and challenging the systems and
23
organizations to consider and embrace innovative informatics processes and solutions.
24
The INS must also consider information competency as well as literacy issues. Computer
25
literacy is a core competency needed in health care, and should be taught in nursing curricula at
26
all levels. In addition, information literacy must be integrated into practice and used to support
27
knowledge management. These are the foundation of informatics competencies.
28
Education and professional development includes not only INSs and INs as well as end-
29
users, but also consumers. With the advent of distance technologies such as telehealth and
30
internet-based consumer-accessible applications, new competencies are needed to ensure that
31
the delivery of health information to consumers is displayed at an appropriate level of
32
understanding, since there may not be face-to-face feedback associated with encounters where
33
the consumer is physically present. Cultural issues, language considerations and literacy level
34
of consumers may not be apparent, and materials may need to be more fully assessed for
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
25
1
appropriate presentation and understanding. INSs may need to ensure presentation of content
2
for web-based knowledge portals of private and government health organizations that may exist
3
in multiple locations, or only virtually. Health information many need to be distilled for consumer
4
consumption. Thus, the education and professional development function involves not only
5
educating informatics nurses and informatics nurse specialists, but also developing interfaces
6
that are appropriate to the consumer. Examples of education and professional development
7
activities might include:
8
•
9
a nursing informatics degree program and/or teaching nursing students at all levels the
10
11
Professor of Nursing at a major university teaching graduate nursing students enrolled in
basic principles and foundations of NI.
•
Clinical Preceptor for newly hired nurses and students providing orientation about the
12
telehealth program, engaging the learners in using the telehealth technology, and role
13
modeling various telehealth nurse responsibilities with regard to monitoring of
14
physiologic parameters and provision of consumer education through the telephone or
15
video.
16
•
17
18
operations, capabilities, troubleshooting, limitations and benefits.
•
19
20
Educator for a vendor traveling internationally to train nurses on the product’s
Staff Development liaison for a large hospital educating nurses and other end users
about how to integrate clinical applications into their work processes.
•
Help Desk team member for a large oncology center working with users as product
21
upgrades are released, answering clinical user questions on the phone or in person and
22
trouble-shooting user problems.
23
•
Patient Education Coordinator facilitating electronic consumer health resources.
24
•
Web developer, responsible for development, maintenance and presentation of disease
25
content for a hospital web portal
26
Policy Development and Advocacy
27
INSs play a key role in development of health policy, particularly bringing expertise regarding
28
the data and information content, the structure of data, and the IT solutions with those attributes.
29
Policy development may be at any level — international, national, state, professional specialty,
30
institution or a work unit. INSs are experts in defining the data needed and the structure,
31
management, and availability of those data for decision-making. As such they advocate for
32
consumers, providers, and the enterprise, and articulate relevant issues from a nursing
33
perspective. Policy-related activities may include developing, writing, implementing and
34
evaluating guidance. Regardless of the level or activity, INSs are active partners in the
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
26
1
development of health policy, particularly related to information management and
2
communication, infrastructure development, and economics.
3
The advocacy function of the INS or IN also encompasses consumer health. INs may be part
4
of initiatives such as promoting the adoption of technology for rural health programs to increase
5
access to health services. Advocacy may include educating legislators about increasing
6
telecommunication access, expanding reimbursement for technology-enabled consumer
7
services, or educating the public on ways to access health-related materials via the Internet.
8
Examples of policy development and advocacy function of the INS or IN might include:
9
•
10
11
national information standards task force.
•
12
13
President of a health information management organization, representing nursing on a
A lobbyist participating in advocacy efforts on behalf of consumers for increased
government funding for demonstration or pilot informatics projects
•
A President of a nursing informatics organization writing letters to elected officials to
14
obtain their support for reimbursement of services by remote, technology-enabled
15
providers.
16
Research and Evaluation
17
INSs conduct research about the design, development, implementation and impact of
18
informatics solutions on users, such as healthcare organizations, providers, consumers and
19
payers. INS nurse researchers use systematic methods of inquiry, including traditional and
20
newer techniques to identify and evaluate data, information, knowledge and wisdom in
21
informatics solutions and data repositories. Research and evaluation functions include, but are
22
not limited to:
23
•
Research related to concept or symbolic representation of nursing phenomena
24
•
Evaluation of clinical decision-making in nursing
25
•
Applied research in development, implementation, usability and outcome impacts of
26
27
solutions
•
28
29
resources
•
30
31
34
Evaluation of effective methods for information systems implementation, acceptance and
utilization
•
32
33
Consumers’ and interdisciplinary providers’ use of health information tools and
Human factors or ergonomics research about the design and impact of systems on
interdisciplinary providers, consumers, nurses, and their interactions
•
Evaluation research on the effects of systems on the processes and outcomes of
consumer care
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
27
1
•
Usability testing of nursing and consumer applications
2
•
Evaluating how consumers utilize computerized health care products
3
•
Research in clinical vocabularies
4
•
Interaction of consumers, providers and technology
5
•
Consumer communication and usage of technology-based support groups
6
Research in nursing informatics can span a range of activities, from experimental research to
7
process improvement and informal evaluation to evidence-based practice. Much of the work is
8
innovative and may be initiated by INSs, or conducted at the request of an organization or
9
agency. INSs working in this functional area might conduct research projects to develop and
10
refine standardized nursing vocabularies, or link nursing interventions to outcomes in large data
11
sets. This work is essential in defining, describing and evaluating data, information and
12
knowledge and wisdom. It might include the evaluation of organizational attributes for
13
successful adoption of documentation systems or the impact and efficacy of hardware and
14
software solutions.
15
Nursing informatics research may also include a consumer orientation. It could include the
16
elements of effective nurse-consumer interactions in web-based interactions with older
17
consumers or it may include the impact of new applications on nurses’ workflow. Patient
18
reactions to instant messaging from providers might be studied. Examples of the research
19
function of the INS might include:
20
•
21
22
The Chief for Nursing Research for a large software company overseeing projects to
evaluate the impact of enterprise electronic health records on patient care outcomes.
•
Nursing Informatics Analyst in a hospital IT department aggregating data about the
23
incidence of decubiti, creating trend reports and predictive models for nurse managers
24
and analyzing outcomes against quality indicators.
25
26
•
Nurse Researcher conducting a usability study related to consumer entry of information
at a clinic-based kiosk versus in-person interview.
27
Integrated Functional Areas
28
Informatics solutions are foundational support for healthcare delivery. In some cases, however,
29
informatics solutions are more tightly integrated with care delivery. For instance, clinical care
30
and informatics intersect in areas such as telehealth and radiation oncology and serve as
31
examples of integrated functional areas. Telehealth serves as the exemplar.
32
Telehealth, as defined by the U.S. Office for the Advancement of Telehealth, is “the use
33
electronic information and telecommunications technologies to support long-distance clinical
34
health care, patient and professional health-related education, public health and health
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
28
1
administration” (U.S. Office for the Advancement of Telehealth, 2003). Telenursing is the use of
2
distance or telecommunications technologies by nurses (Milholland, 2000; National Council of
3
State Boards of Nursing, 2003) or nursing personnel to monitor consumer and public health and
4
administrative functions, as well as deliver healthcare education. Because of the widespread
5
expansion of telehealth technologies, standards have been developed that take into account
6
differing countries’ cultures and governance standards (Milholland-Hunter, 2001). Standards
7
may relate to the transmission of data and information as well as protocols for providing care.
8
Nursing informatics primarily fulfills a clinical support role, as opposed to a direct clinical
9
practice role. Telehealth is primarily a clinical practice role, with technical aspects required to
10
execute delivery of care, but not as its focus. The 2004 International Telenursing Survey (Grady,
11
Schlachta-Fairchild and Elfrink, 2005) surveyed international telenurses worldwide. Of the 719
12
participants, only 18 telenurses have informatics in their job titles. Within this group, over half of
13
telenurses were advanced practice clinicians. Ten of the clinicians have the term informatics in
14
their titles. Thus, the interface between nursing informatics and telehealth nursing primarily
15
occurs at the technical aspects or technical support level currently. In the future, telehealth may
16
evolve to toward an emphasis on information (versus technology) and informatics principles,
17
methods and tools may expand in the future.
18
Standards for telehealth nursing clinical practice are outlined in the ANA Core Principles on
19
Telehealth (1998) and ANA Competencies for Telehealth Technologies in Nursing (1999)
20
documents. These documents describe the interface between telehealth and informatics,
21
referring to the technical aspects of telehealth as clinical support and telehealth as clinical
22
practice. Examples of the telehealth function of the IN or INS might be:
23
•
24
25
Telehealth Network Coordinator for a rural telehealth program, assuring the appropriate
deployment of technology, and customization for distance-related needs.
•
Program Manager for Telehealth in a home health agency, organizing the integration of
26
telehealth into the agency’s operations, supporting the alignment of telehealth
27
technology with the overall technology strategy of the agency, assuming leadership in
28
the adoption and implementation of the program, and evaluating and maintaining
29
telehealth outcomes and accountability for those outcomes (Starren et al., 2005)
30
•
Nurse Researcher conducting a program evaluation comparing the impact of an online,
31
telehealth cardiac education program versus an in person support group on level of
32
depression and adherence to diet.
33
Functional Areas Conclusion
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
29
1
With the continued miniaturization of technology, developments in information science and
2
nursing science, NI functions will continue to expand into the future, evolving into functions not
3
yet envisioned. INSs and INs will need to continually assess and incorporate new knowledge
4
management and technology trends into their own practices. Integrated functional areas will
5
continue to grow. The functional areas listed here will be combined with new areas to create
6
innovative positions of the future.
7
Informatics Competencies
8
Because of the increased visibility of information and technology within healthcare settings and
9
complementary educational programs, many stakeholders are being faced with a need to define
10
informatics competencies for nurses. Human resource managers and educational planners are
11
just two examples of stakeholders who have an interest in competencies for nursing informatics.
12
Since the year 2000, researchers and professional organizations have completed
13
substantial work toward defining nursing informatics competencies (Androwich et al., 2003;
14
Curran, 2003; Desjardins, et al., 2003; HIMSS, 2005; Jiang, Chen & Chen, 2004; Staggers,
15
Gassert & Curran, 2000, 2001, 2002). Various lists of informatics competencies are available,
16
especially those geared toward nurses’ educational levels (see references).
17
A keen interest has emerged for identifying informatics competencies for various nursing
18
roles. Stakeholders, such as employers and educators, are requesting clarification about these
19
competencies. For the discussion here, competencies for typical nursing informatics roles are
20
especially pertinent. To this end, a matrix has been developed, based upon a thorough
21
literature review and the work from a consensus panel. This text and accompanying matrix
22
suggests competencies for typical nursing informatics functional areas discussed in the previous
23
section.
24
The Intersection of Informatics Competencies and NI Functional Areas
25
A review of the literature was conducted to examine work on informatics competencies,
26
concentrating on the inter-relationship of nursing roles and informatics competencies. Staggers,
27
Gassert and Curran (2000, 2001, 2002) published initial work in this area, defining and
28
validating informatics competencies for nurses at these four levels of practice: beginning,
29
experienced, INS, and informatics innovator. This research and framework more closely aligns
30
to educational requirements for all nursing specialties at the beginning and experienced levels,
31
and then identifies specific competencies for the specialty roles of INS and the informatics
32
innovator. The above mentioned work by Staggers et al (2001, 2002) not only promoted the integration of
33
informatics competencies into educational curricula but also impacted policy documents.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
30
1
To date, the majority of authors have focused on the competencies needed for nursing
2
curricula. For example, Curran (2003) and faculty colleagues identified informatics
3
competencies for nurse practitioners at Columbia University School of Nursing. Desjardins,
4
Cook, Jenkins and Bakken (2005) focused on beginning nurse competencies, expanding them
5
to include the knowledge and skills for information literacy to support evidenced-based practice.
6
Similar to Staggers et al. (2002), this study also categorized competencies into four levels of
7
nursing practice. Barton (2005) echoed a similar view of informatics competencies for the
8
beginning nurse, identifying a need for competencies in both technology or computer literacy as
9
well as information literacy for undergraduate nursing programs.
10
Educational content areas for required informatics competencies have been examined by
11
several authors. McNeil, Elfrink, Pierce, Beyea, Bickford, and Averill (2005) asked the Deans
12
and directors of 672 Baccalaureate and above education programs to identify informatics
13
content taught in their undergraduate and graduate programs. Twenty-five unique content areas
14
were identified for undergraduate (i.e., beginning nurse) and graduate (i.e., experienced nurse)
15
levels of practice. Among the top-ranked competencies for both programs were: a) accessing
16
electronic resources, b) ethical use of information systems, c) evidence based practice skills
17
and d) skills for computer-based patient records. The undergraduate program respondents more
18
often identified basic hardware and software skills while the graduate program respondents
19
included competencies related to innovation and change theory, national health database
20
knowledge and general systems theory.
21
Jiang, Chen and Chen (2004) surveyed Taiwanese nursing education programs ranging from
22
non-vocational and vocational nursing programs to collegiate programs for 2-, 4-, 5-year and
23
graduate-level programs. The authors identified seven domains of competencies and linked
24
them to differing levels of nursing education in Taiwan. In contrast to work in the US, these
25
authors identified domains mostly related to computer versus information literacy, including
26
hardware, software and network concepts; principles of computer application; skills in computer
27
usage; program design; limitations of the computer; personal and social issues; and attitudes
28
toward the computer.
29
New categories and concomitant competencies for education, as well as practice, are also
30
available. Androwich, I. M., Bickford, C. J., Button, P. J., Hunter, K. M., Murphy, J., &
31
Sensmeier, J. (2003) described NI competencies needed to improve patient safety and expand
32
nursing practice. Garde, Harrison, and Hovenga, (2005) reported specific competencies for:
33
34
•
Nursing informatics knowledge and skills (e.g., Health Information Systems,
Electronic Patient records, Telehealth)
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
31
1
•
Information technology knowledge and skills (e.g., programming principles, software
2
development, methodologies and processes, system analysis and design, database
3
design and management)
4
•
Knowledge and skills in organizational and human behavior (e.g., project
5
management, inter-professional communication, risk management, policies and
6
procedures).
7
8
9
•
Clinical and health-related knowledge and skills (e.g., evidence based practice,
clinical guidelines, care pathways).
The Healthcare Leadership Alliance (HLA), announced the creation of the HLA Competency
10
Directory in the fall of 2005. This directory identifies 300 competencies across multiple
11
healthcare management roles categorized in five domains: a) leadership: b) communications
12
and relationship management, c) professionalism; d) business knowledge and skills, and e)
13
knowledge of the healthcare environment. This comprehensive list of competencies can be
14
retrieved from the HLA site at http://www.healthcareleadershipalliance.org/directory.cfm. This
15
directory may be especially pertinent for those working in interdisciplinary settings.
16
Developing a New Competencies Matrix
17
A competencies matrix was derived from the initial work of Staggers, Gassert and Curran
18
(2002). Evidence was also found in the review of literature and the content areas described in
19
the ANCC NI Certification exam located at
20
http://www.nursingworld.org/ancc/cert/eligibility/informatics.html. Unique competencies were
21
abstracted from each of the references and included into a comprehensive list. These
22
competencies were subsequently categorized by a panel of reviewers into three overall areas:
23
Computer Literacy, Information Literacy, and Professional Development/Leadership. These
24
categories may be found on the vertical axis of the matrix. Computer literacy competencies
25
relate to the psychomotor use of computers and other technological equipment (Barton, 2005).
26
Information literacy competencies deal with information retrieval knowledge and skills: knowing
27
when there is a need for information; identifying the information needed to address a given
28
problem or issue; finding the needed information and evaluating the information; organizing the
29
information; and using the information effectively to address the problem or issue at hand.
30
(American Library Association, 2006). Professional development and leadership competencies
31
refer to the ethical, procedural, safety and management issues for informatics solutions in
32
nursing practice, education, research and administration.
33
34
The horizontal section of the matrix was based upon the four educational levels from the
literature as well as the NI functional areas defined earlier in this document. It is important to
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
32
1
recognize that informatics competencies need to be integrated in all educational levels. The
2
panel identified competency foci for each particular functional area indicated by an “X.” As seen
3
in the matrix, competencies cross the different Nursing Informatics functional areas. Although
4
each sub-heading includes more granular competencies beneath it, nurses would not
5
necessarily be expected to achieve every competency within a sub-heading. The areas
6
identified by the “X” merely indicate an area of emphasis.
7
The lack of an “X” does not mean that the skill is completely absent for that given role, nor
8
does it mean that someone in that role is required to have every skill indicated in the matrix;
9
rather it means that the skill may not be emphasized in a particular functional area or NI role.
10
For example, a quality improvement (QI) specialist is used as an example of a NI role that would
11
emphasize the analysis functional area. An Informatics Nurse Specialist working in a quality
12
improvement area would require competency in many of the indicated computer literacy skills
13
including administration, communication, desktop, systems, and quality improvement, but would
14
not likely need the simulation skills identified in the matrix. A quality assurance specialist, listed
15
in the same functional area, would, however, need knowledge and skills about simulations,
16
especially if the NI in this role works in an institution using simulation for staff development or for
17
a vendor using this product.
18
The Functional Area-Competency Framework provides an example of the nursing informatics
19
competencies for different functional areas within NI roles. Telehealth, which may be seen as
20
more of an integrative area rather than a stand-alone functional role is presented in the matrix to
21
reflect intersections with various competencies. The list is not exhaustive, but presents
22
beginning guidance for the essential NI competencies across computer literacy, information
23
literacy, and professional development skills and knowledge. Currently the identified
24
competencies are at different levels. In the future they may be re-evaluated, expanded or
25
collapsed.
26
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
33
1
Integrated Areas
Research and Evaluation
X
X
Policy Development and Advocacy
Consultation
X
X
Education and Professional Development
Compliance and Integrity Management
X
X
Development
Analysis
X
X
Coordination, Facilitation, and Integration
Administration
Informatics Innovator
Informatics Specialist
Experienced Nurse
Beginning Nurse
Knowledge and Skills
Competency Categories
Table 2. Informatics Competencies by NI Functional Areas
Computer
Literacy
Computer Skills - Administration
Computer Skills - Communication
Computer Skills - Data Access
Computer Skills - Documentation
Computer Skills - Education
Computer Skills - Monitoring
Computer Skills - Basic Desktop Software
Computer Skills - Systems
Computer Skills - Quality Improvement
Computer Skills - Research
Computer Skills - Project Management
Computer Skills - Simulation
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
34
Information
Literacy
Informatics Skills – Evaluation
Informatics Skills – Role
Informatics Skills - System Maintenance
Informatics Skills - Analysis
Informatics Skills - Data/Data Structure
Informatics Skills - Design and Development
Informatics Skills - Fiscal Management
Informatics Skills - Implementation
Informatics Skills - Management
Informatics Skills - Programming
Informatics Skills - Requirements
Informatics Skills - System Selection
Informatics Skills - Testing
Informatics Skills - Training
Informatics Knowledge - Impact
Informatics Knowledge - Privacy/security
Informatics Knowledge - Systems
Informatics Knowledge - Research
Informatics Knowledge - Regulations
Informatics Knowledge - Usability/Human
Factors
Informatics Knowledge - Education
Informatics Knowledge - Models and Theories
Informatics Knowledge - Nursing
Classification, Taxonomies and Nomenclature
System Lifecycle
Organization Change Management
Systems Theory
Management Science
Standards for Privacy and Security
Human Computer Interaction
Computer Assisted Instruction
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
35
Statistical Analysis
Adapting information technology as a primary
means of patient safety
Openness to disruptive innovation
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
Professional
Development
Integration of a reference terminology for
nursing in nursing practice
Integration of multidisciplinary language
infrastructure and standards in practice
Recognize the role on informatics in nursing
Knowledge representation methodologies for
evidenced based practice
Incorporation of technology and software for
the development of clinical information
systems
Reinforce conceptual framework
Applying newfound skills in modeling and
designing systems
Combining design processes with engineering
Consider object-oriented modeling
Support by providing data for decision making
-Demand evidence based databases
Use of information technology to support
clinical and admin processes
Promote openness in knowledge to innovate
technology in health care
Adopting computerized patient records
Promoting the need for yielding integrated,
scalable applications
Use of information technology to support
patient safety initiatives
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
X
1
2
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
36
1
2
Competencies and Metastructures
The components of metastructures - data, information, knowledge and wisdom - can be
3
compared and contrasted with the elements in the competencies matrix. Using a patient care
4
example, the Beginning Nurse uses skills that rely on the ability of obtaining data. Computer
5
skills, data entry, and the use of the patient’s electronic medical record are the major focus of
6
their practice. The Experienced Nurse builds upon this and applies the basic computer skills into
7
information regarding the patient.
8
The INS has obtained expertise in nursing, as well as higher levels of computer literacy,
9
information literacy and professional development/leadership. This increased level represents
10
knowledge within nursing informatics. For example, the ability to analyze systems and
11
processes is evident. This leads to the use of knowledge for patient care, administration,
12
research or educational activities. Last, the Informatics Innovator has achieved a level of
13
knowledge coupled with experience. Thus, the innovator exemplifies wisdom. Wisdom in
14
informatics might be the creation of unique methods for system design or evaluation, or the
15
political finesse to justify system purchase.
16
Work in Progress
17
Work in NI competencies is an area in evolution. There is not yet one consolidated list of
18
competencies across educational levels, or a reference list of competencies for employers.
19
Perhaps it is premature to close the innovation demonstrated to date. Yet the proliferation of
20
lists can be confusing to the uninitiated.
21
In addition to numerous researchers, academics and employers, many professional
22
organizations are actively working toward identifying competencies for nursing informatics, such
23
as:
24
•
25
The American Medical Informatics Association (AMIA)’s 10x10 program (Oregon
Health & Science University Biomedical Informatics, 2006).
26
•
AMIA Educational Workgroup.
27
•
The HIMSS nursing informatics working group.
28
•
An NLN Task Group on Informatics Competencies and subsequent initiatives.
29
•
Technology Informatics Guiding Education Reform (TIGER).
30
NI Competencies Conclusion
31
The work on informatics competencies has expanded greatly in the last five years. After the
32
initial work of Staggers, et al (2001, 2002), numerous authors and agencies have now
33
developed informatics competencies. The new Informatics Competencies by NI Functional
34
Areas matrix (Table 2) marries competencies with typical NI functional areas. In the future, the
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
37
1
rapid pace of technological change and generation of information and knowledge will present
2
challenges for maintaining current and accurate competencies for nursing informatics. Faculty
3
must have an understanding of competencies for nursing informatics so that NI becomes an
4
integral part of curricula and also to stimulate research. While interest in competencies in the
5
educational arena continues to develop, there is a growing interest by employers. More
6
important, within the next few years, the myriad efforts and lists of NI competencies could
7
benefit from consensus and consolidation.
8
9
The Integration of Nursing Informatics
As the use of technology increasingly becomes integrated into nursing and every nursing role,
10
the boundaries between the roles of nurses and informatics nurses are even more blurred. It
11
becomes important to identify those items that would be common along a continuum for nurses
12
in all levels and specialties, and also the functions that make the practice of nursing informatics
13
unique from other nursing specialties. Information is central to healthcare delivery. All nurses
14
must be skilled in managing and communicating information and are primarily concerned with
15
the content of that information, while nursing informatics is concerned with the creation,
16
structure and delivery of that information. Information needs are facilitated from the simple use
17
of technology at the bedside to provide direct care, to providing access to healthcare information
18
at the healthcare consumer’s point of need, through managing the data from this information to
19
develop new nursing knowledge. This range in the use of information and technology can be
20
visualized on a continuum as seen in Figure 5.
21
22
Nurse using information
and technology to
support their specific
domain of practice
Informatics Nurse support,
change, expand, transform
practice by the design and/or
implementation of information
technology
23
Figure 5
24
A Continuum of Information and Technology Integration into Nursing Practice
25
26
NI is also integrated into other healthcare informatics specialties. The INS is often
27
responsible for implementing or coordinating projects involving multiple disciplines. The INS is
28
expected to interact with professionals involved in all phases of the information systems lifecycle
29
and with professionals in all aspects of system utilization. NI can be conceptualized either as an
30
integral part of healthcare informatics or as an overlapping specialty within healthcare
31
informatics. In many cases, core concepts that are common to many informatics disciplines are
32
identified and underpin each specialty. There are also individualized concepts and methods that
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
38
1
are unique to each discipline. Two concept diagrams presented by Englebardt and Nelson
2
(2002) demonstrate the different approaches to the role of NI in relation to other healthcare
3
informatics specialties. (see Figure 6 and Figure 7)
4
5
Figure 6
Health Care Informatics
Specialist: Umbrella Model
Figure 7
Health Care Informatics Specialist:
Overlapping Model
6
Reprinted with permission
7
NI is also integrated into all aspects of the healthcare continuum. This integration allows for
8
access of healthcare information at the point of need, such as at the bedside in acute healthcare
9
settings, ambulatory care settings, at home or even when traveling locally or globally.
10
The Boundaries of Nursing Informatics
11
This section summarizes the differences between NI and other specialties in nursing, and
12
reviews the differences between NI and other informatics specialties. To reiterate, NI is a
13
specialty that integrates nursing science, computer science, and information science to manage
14
and communicate data, information, knowledge and wisdom in nursing practice. Although
15
critical thinking is a requirement of nursing practice, NI facilitates this critical thinking through the
16
integration of data, information, knowledge and wisdom to support patients, nurses, and other
17
practitioners in their decision-making in all roles and settings. The difference between NI and
18
other nursing specialties is the emphasis on informatics concepts, tools, and methods to
19
facilitate nursing practice.
20
Although some outside the specialty might consider NI synonymous with information
21
technology, focusing on technology alone does not define NI; it is merely supportive of the work
22
of NI. Facilitating the synthesis of data and information into knowledge and wisdom is central to
23
NI; information technology assists in this process. INSs have moved toward the behaviors that
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
39
1
Hannah, Ball and Edwards described in 1994 and have adopted an anticipatory proactive
2
stance and are continuously striving to exploit technology in the design, structure, and
3
presentation of information, as well the impact this has on healthcare delivery in general, and
4
the nursing process specifically. Figure 8 demonstrates the connection between the different
5
foci of nursing and NI. These are represented along a continuum versus having distinct
6
boundaries.
7
Figure 8. Nursing and Nursing Informatics Foci
8
9
10
Nursing Focus
Nurses, patients, health, environment
11
Nursing Informatics Focus
Information user, information recipients,
information exchange
12
13
Content of information, support for
Design, structure and representation of
14
evidence based practice changes
data as information
16
Using information applications and
Develop, implement and evaluate
17
technology
applications and technology, insuring the
15
18
quality, effectiveness, efficiency and usability
19
of applications and technology
20
21
NI is also differentiated from other informatics specialties. The roles of healthcare providers
22
overlap, but each has a distinct emphasis making them different. Each informatics specialty is
23
aligned uniquely with their primary role, requiring that INSs build on their base nursing
24
knowledge with unique informatics skills. Nursing informatics exists as a recognized component
25
of both the broad field of healthcare informatics and as a specialty within nursing (Brennen,
26
2003). This results in a unique body of knowledge and demonstrates the need for advanced
27
preparation unique to nursing. NI incorporates informatics concepts used by others, but applies
28
them to a foundation of nursing. What differentiates an INS and IN from others in this area is the
29
knowledge of nursing content and process. The synthesis of informatics and nursing results in a
30
whole that is greater than the parts. An understanding of how informatics can support patient
31
care within the context of the nursing process is a foundation for NI. Core components of
32
informatics knowledge and skills underpin all informatics specialties, such as the use of
33
technology, computer literacy and data management structures. There are also components
34
unique to each discipline such as their taxonomy.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
40
1
2
Tenets of Nursing Informatics
•
3
4
Nursing informatics has a unique body of knowledge, preparation and experience within the
specialty, and identifiable techniques and methods.
•
Nursing informatics supports the clinical and non-clinical efforts of nurses, and other
5
providers to improve the quality of care and the welfare of health care consumer.
6
Information or informatics methods alone do not improve patient care; rather, this
7
information is used by clinicians and managers to effect improvements in care, information
8
management and patient outcomes.
9
•
10
11
Nursing informatics collaborates with and is closely linked to other health-related informatics
specialties.
•
Although concerned with information technology, nursing informatics focuses on efficient
12
and effective delivery of complete and accurate information in order to achieve quality
13
outcomes.
14
•
15
16
interwoven throughout the practice of NI.
•
17
18
19
Human factors, human–computer interaction, ergonomics, and usability concepts are
Nursing informatics promotes established, emerging, and innovative information
technologies.
•
Nursing informatics’ key concerns include ensuring the confidentiality and security of health
care data and information and advocating privacy.
20
Ethics in Nursing Informatics
21
Nursing has a long history of applying ethical principles to nursing practice, with a primary
22
concern for the patient and a commitment to the professional code of ethics for nurses. Thus,
23
the Code of Ethics for Nurses with Interpretive Statements (ANA, 2001) serves as a guidepost
24
for the informatics nurse facing ethical issues, dilemmas and decisions. The ANA policy on
25
privacy and confidentiality addresses the impact of HIPAA legislation and the ethics of
26
protecting information in a changing healthcare environment. Additionally, with the increase in
27
Electronic Health Records (EHR) across multiple systems, decisions related to the use of
28
information in the EHR must strike a balance between "ethically justified ends and otherwise
29
appropriate means" (IMIA, 2006, p.1). The primacy of concern for patients and the commitment
30
to the Code of Ethics for Nurses form a foundation for considering ethical issues in nursing,
31
including nursing informatics. However, the practice of nursing informatics, a highly specialized
32
and non-traditional nursing practice, begs consideration of specialty-specific ethical guidelines.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
41
1
Ethical questions or issues often arise when common corporate business practices run
2
counter to the ethical mandates of health care professionals. The INS brings an integrated,
3
systems perspective to discussions of ethical issues, such as:
4
•
5
6
health information and healthcare service delivery?
•
7
8
9
10
Is a code of ethics integrated into the expanding distributed environment of electronic
Is the individual responding to a healthcare related e-mail or web site inquiry
appropriately licensed and qualified?
•
In health care related electronic communication, are appropriate safeguards in place to
protect the sender’s identity and privacy, the content and integrity of messages, and the
respondent’s identity?
11
The International Medical Informatics Association (IMIA) has developed a detailed code of
12
ethics for health information professionals. The IMIA Code of Ethics is meant to guide decision-
13
making for “gathering, processing, storing, communicating, using, manipulating and accessing
14
health information” (IMIA, 2006, p. 2). As such, it offers specialty-specific ethical guidance
15
applicable to nursing informatics. The IMIA code describes general principles of informatics
16
ethics and two are of special interest to nursing informatics: information privacy and disposition,
17
and legitimate infringement. The information privacy and disposition principle states that all
18
persons have a fundamental right to privacy, and hence control over the collection, storage,
19
access, use, communication, manipulation and disposition of data about themselves (IMIA,
20
2006, p3). However, this principle must be balanced with the principle of legitimate
21
infringement, which states that this fundamental right is tempered by the legitimate, appropriate
22
and relevant data needs of a free, responsible and democratic society, and by the equal and
23
competing rights of other persons (IMIA, 2006, p. 4).
24
Further, INSs should understand and apply the basic principles of autonomy, beneficence,
25
non-malfeasance and justice as they relate to the practice of informatics (ANA, 2001). The INS
26
encounters questions of biomedical ethics throughout systems development, implementation,
27
and administration. For example, informatics professionals including nurse specialists must
28
determine whether patients have the ability to see all of their lab results online, perhaps before a
29
clinician has seen them. This decision may not be so much a technical question as an ethical
30
question, concerning the principle of patient autonomy. Security standards respond to the
31
principles of autonomy and non-malfeasance. In the United States, decisions concerning the
32
appropriate access and use of data may be guided by both HIPAA rules and the ethical principle
33
of justice.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
42
1
The general principles described by IMIA and the ANA Code of Ethics provide a solid
2
foundation for INSs as they apply ethical principles in their practice. The INS has a responsibility
3
to advocate for data confidentiality, integrity and security, quality management of information,
4
and legitimate data use. These needs must be balanced with users’ timely access to accurate
5
data for decision-making in all settings. The role of ethics in Informatics practice is increasing
6
and INSs are in a unique position to make or aid decision-making for informatics policy and
7
operations. INSs can harmonize organizational risk with users’ needs for timely data access.
8
INS, in particular, can serve as the voice of wisdom in all settings – as translators and
9
advocates for users who also understand the relevant ethical, political, and technological
10
11
considerations.
New computing approaches such as knowledge discovery, clinical data repositories (CDR)
12
and data warehouses have already created new opportunities for the INS to apply ethical
13
principles. Vast data stores of personal data currently exist in the electronic realm.
14
Contemporary organizations are grappling with complex issues, for example regulation of data
15
access such that only appropriate data is accessed by appropriate users. As technologies
16
evolve and data stores increase, the ethics of data use and protection will become increasingly
17
intricate, requiring continual evaluation and monitoring. Pertinent considerations for all health
18
informatics professionals include the following ethical responsibilities:
19
•
20
21
To ensure personal competence, integrity, diligence and responsibility for all actions
performed (IMIA, 2006).
•
To ensure that an electronic record, or the data contained in it, are used only for the
22
stated purposes for which the data was collected or for the purposes that are otherwise
23
ethically defensible (IMIA, 2006, p 6)
24
•
To ensure that appropriate structures are in place to evaluate the technical, legal and
25
ethical acceptability of the data collection, storage, retrieval, processing, accessing,
26
communication and utilization of data in the settings in which they carry out their work
27
(IMIA, 2006, p 7).
28
•
To ensure that healthcare professionals are informed about the status of the information
29
services upon which users rely and must immediately advise users of any problems or
30
difficulties that might be associated or could reasonably be expected to arise in
31
connection with these informatics services (IMIA 2006, p 6). For example, processes
32
such as phone trees for notification of system difficulties need to be addressed in both
33
the planning and implementation of those services.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
43
1
In conclusion, the INS has the opportunity and responsibility to address ethical concerns
2
related to design, implementation and utilization of health care information systems and data
3
obtained through reporting mechanisms. The INS is challenged to balance the improvement of
4
health care with individual privacy, security and safety concerns. Balancing the autonomy of
5
patients and their health information along with the just use of health information to benefit
6
others requires thoughtful consideration across multiple levels. Given the complexity and
7
challenge of making ethical decisions related to health care information systems, the INS must
8
contribute to and act in accordance with a broad-based understanding of the applicable ethical
9
principles.
10
The Future of Nursing Informatics
11
The rate of change in our discipline is rapid and the state of NI will change even shortly after this
12
document is in print. Three of the current trends will likely influence the direction of this change
13
in nursing informatics: the positions and competencies for nurses and informatics, technological
14
aspects of the field, and changes in healthcare delivery and regulatory requirements.
15
Trends in Positions and Competencies for Nurses and Informatics
16
The boundaries are blurring for INSs, other nurses, and associated health informatics
17
disciplines. As information and technology are more highly integrated into the workplace, nurses
18
in all settings will gain informatics knowledge and skills. The number and complexity of
19
informatics competencies for nurses will continue to escalate. Some informatics competencies
20
ascribed to informatics specialists will likely transition to mainstream nurses, and the level of
21
competencies required for INSs will continue to expand. Thus, the baseline set of NI
22
competencies required of nurses at all levels will rise in the future.
23
In the last few years, new areas of nursing have been incorporated into nursing informatics.
24
For example, nurses who heavily use information and technology, such as telehealth nurses,
25
may be considered one type of IN. As others in nursing design, implement and evaluate
26
informatics solutions, the scope of nursing informatics may continue to expand. The
27
globalization of informatics and nursing informatics is apparent. Nursing informatics is
28
becoming a world community with less distinction and more commonalities among INSs
29
everywhere.
30
Last, the role boundaries between other health informatics colleagues and NI are less
31
conspicuous than in the past. One of the centerpieces of NI practice is its cross-disciplinary
32
nature, with INSs often leading cross-disciplinary projects to craft usable informatics solutions
33
for use by many disciplines. INSs have assumed executive positions in the health informatics
34
arena. NI and other health informatics colleagues also function in many of the same positions,
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
44
1
blurring boundaries while sharing a common set of functions, skills and knowledge. This trend
2
will likely continue as professional informatics organizations define a shared, core set of
3
knowledge and skills required by all informatics specialties. Probably the clearest trend is
4
evolving change in the functional areas for INSs, a state of continual change away from a more
5
generic set of skills for any one discipline and toward a shared set of competencies based upon
6
functional areas required to enact a particular position (i.e., clinical analyst, informatics
7
executive, futurist, KDD researcher or database developer)
8
Trends in Technology
9
Information technology is becoming commonplace in our lives as well as in health care. For the
10
first time in history, a generation exists never having known a world without the internet, cell
11
phones, online social networks, blogs, and other technology-influenced media. These techno-
12
influenced individuals will be entering the healthcare field as knowledge workers as well as
13
consumers of healthcare delivery. Implications for NI are:
14
•
15
Creating new models for work and education for superbly techno-savvy users, who have
less resistance to technology. In fact, they will demand it.
16
•
Adapting to users with less skill in face-to-face communications,
17
•
Having consumers with even greater expectations for accelerated information and
18
19
technology implementations.
Several advances in technology will likely impact nursing informatics in the future. A number
20
of these are outlined in the following sections.
21
Nanotechnology
22
Nanotechnology is expected to more heavily impact health care in the next 2-5 years.
23
Nanotechnology refers to microscopic technology on the order of one-billionth of a meter. This
24
technology will likely impact the diagnosis and treatment of many diseases and conditions
25
(Gordon, Boniger & Cooper, 2007). Some of the pending technologies that will impact the INS,
26
clinicians and patients may include:
27
•
28
New methods for medication administration
o
29
tools circulating within patients’ bloodstreams.
30
31
32
33
Sensing patient’s internal drug levels by having miniature medical diagnostic
o
•
Chemotherapy delivered directly to a tumor site, reducing systemic side-effects
New monitoring devices for the home:
o
A talking pill bottle that enables patients to push a button to hear prescription
information
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
45
1
o
Bathroom counters that announce whether it is safe to mix two medications
2
o
A shower with built-in scales to calculate body mass index (Hong Kong
3
4
Polytechnic University)
o
5
6
Measuring devices in the bathroom to track urine frequency and output and
upload these data to a system or care manager
o
Non-invasive Blood Glucose Monitors to eliminate sticks, sensors to compute
7
blood sugar levels using a multi-wavelength reflective dispersion photometer
8
(Hong Kong Polytechnic University )
9
New Technology Tools for Managing Public Health Concerns and Information about
10
Populations
11
The threat of terrorism, bioterrorism, and the need for improved disease management across
12
traditional boundaries drives the demand for new tools and solutions that will concern the INS.
13
A partnership with public health professionals and the emergence of public health informatics is
14
a response to the need for population management tools and early disease detection.
15
Devices and Hardware
16
The increased miniaturization of devices will change where and how IT solutions will be
17
deployed and adopted. No perfect hardware solution exists in the market today to address all
18
diverse nursing workflows and mobile caregiver demands. An emphasis on ergonomics and
19
human-computer interaction will lead to new solutions to support diverse workflow requirements.
20
New integrated technologies will increase common access to health information, e.g., cell
21
phones, smart phones, PDA’s, and multi-functional devices. These solutions are becoming
22
ubiquitous in daily lives. They will change how clinicians and patients expectations and
23
interactions with various technology solutions. In particular, providers will continue to be
24
challenged to be as knowledgeable about new disease treatments and research findings as
25
patients with accessible devices are.
26
Wearable Computing
27
Wearable computing is a revolutionary paradigm shattering myths about what computers are
28
and how they should be used. A computer can be worn, much as eyeglasses or clothing are
29
worn, and interactions with the user are based on the context of the situation. With heads-up
30
displays, embedded sensors in fabrics, unobtrusive input devices, personal wireless local area
31
networks, and a host of other context sensing and communication tools, wearable computers
32
can act as an intelligent assistant and/or a data collection and analysis device.
33
34
Many of these devices are available now. Smart fabrics with embedded sensors have been
on the commercial market since 2000 and are being used in shirts, gloves and other clothing.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
46
1
These wearable computer and remote monitoring systems are intertwined with the user’s
2
activity so that the technology becomes transparent. Sensors and devices can gather data
3
during the patient’s daily routine, providing researchers and/or healthcare providers/significant
4
others a periodic or continuous data feed of the subject's health at work, school, exercise, sleep,
5
rather than the current "snapshot" generated during a typical hospital or clinic visits. A partial
6
list of applications for wearable computing includes (Wearable Computing, 2007a):
7
•
Sudden Infant Death Syndrome monitoring for infants
8
•
Ambulatory cardiac and respiratory monitoring
9
•
Ambulatory monitoring of neuromuscular disease
10
•
Monitoring of Ventilation During Exercise
11
•
Monitoring Rescue Workers Vital Signs
12
•
Activity Level of Post-Stroke Patients
13
•
Patterns of Breathing in Asthma
14
•
Assessment of Stress in Individuals
15
•
Arrhythmia Detection and Control of Selected Cardiac Conditions
16
•
Daily Activity Monitors
17
•
Monitoring heat stress and dehydration
18
19
20
Wearable computing is applicable to workers as well as consumers or patients. Examples
here may include:
•
21
22
workflow or allowing logon to systems
•
23
24
25
Proximity badges and RFID (radio frequency Identification) allow tracking of providers for
Wearable glasses allow a heads-up display of vital signs or images while also focusing
on the patient. (Wearable computing, 2007b)
•
Bar code scanners that fit on a finger or wrist- activated input devices
Future developments for input methods may also be applicable in the healthcare market. For
26
example, an "interface-free," touch-driven computer screen, manipulated intuitively with the
27
fingertips, responds to varying levels of pressure. Another example is virtual keyboards using
28
Bluetooth technology. A keyboard can be displayed and used on any surface (Keyboard, 2007).
29
Robotics
30
The use of robotics will expand more broadly into patient care areas. Robots have been used
31
for many years to deliver supplies to patient care areas. Robotics enable remote surgeries and
32
virtual reality surgical procedures. At Johns Hopkins, robots are being used to provide language
33
translation to patients (Greenback, 2007). Hand-assist devices have helped patients regain
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
47
1
strength after a stroke (Device, 2007). Robots are providing a remote presence for physicians to
2
be able to virtually examine patients by manipulating remote cameras (Remote Presence,
3
2007). In the future, robots may also be used in direct patient care, for instance, to help lift
4
morbidly obese patients.
5
Knowledge Representation
6
As more and more electronic data become available for and about patients over their life time,
7
clinicians will need advanced tools to help locate, synthesize and even cope with this vast
8
volume of data. New research areas will expand regarding advances in displaying vast amounts
9
of data to clinicians to optimize patient care, patient and clinician efficiencies while avoiding
10
medical errors. NI may need more nurses trained in knowledge representation, semantic
11
representation and other knowledge areas. This also has implications for knowledge discovery
12
in databases, data quality and a continued emphasis on data standards and data quality
13
Nurses make numerous, complex, and diverse decisions in their daily practice. Decision
14
making for nursing practice must consider relevant evidence-based and patient-specific
15
information. As nurse decision-making grows increasingly complex, the need for computerized
16
clinical decision support will increase. In the absence of adequately explicit evidence-based
17
guidelines for nursing decisions, novel technologies will be necessary to synthesize evidence
18
from the literature and/ or induce models from clinical data. Knowledge discovery in databases
19
could play an important role in the induction of clinical knowledge models.
20
Genomics
21
The advances in the human genome and understanding of individual DNA will have a dramatic
22
impact on what we know about patients. These data, especially once they are integrated into an
23
EHR or Personal Health Records (PHRs), will lead to advances in customized patient care, and
24
customized medications targeted to individuals’ responses to medications. Care processes and
25
medications can be very specifically customized to patients based on their unique DNA profile
26
and how they have responded to specific medications and other interventions in the past. This
27
will dramatically change how patients are managed for specific diseases and conditions,
28
extending into the prevention of some diseases.
29
The inherent complexity of customized patient care will demand computerized clinical
30
decision support. Predictive disease models based upon patients’ specific DNA profiles will
31
emerge as clinicians better understand DNA mapping. These advances have implications for a
32
new model of care and for INSs’ participation in the development of genomic-IT solutions. More
33
than ever, patients will need to be partners in this development. Genomics will lead to many
34
specialized advances in care delivery and be linked to exact, individualized data within a
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
48
1
Personal Health Record (PHR). Subsequently, advanced disease management with the goal
2
aimed at disease prevention will be possible. This change has many implications for ethics as
3
well as informatics. In fact, genomics competencies and curricular guidelines are available at
4
http://nursingworld.org/ethics/genetics.
5
New Educational Technologies
6
Evolving teaching technologies are changing the education stratagems used in the classroom,
7
the lab, and the clinical setting. For example, patient care simulators allow students to run
8
programmed care scenarios in a safe environment and provide innovative options for teaching
9
critical thinking skills. Group learning tools such as clickers, used in interactive teaching, can
10
change how students engage with class content as well as how they learn to function as
11
members of a team (Michaelsen, Fink, Knight, 2007). Distance education technologies such as
12
web-based course management systems and the related student support services are
13
challenging basic education concepts such as what academic resources must be included in a
14
library collection or how a university defines a credit hour of education. Administrative
15
information systems are now automating basic university functions such as admissions,
16
registration, student record management, grant management and financial aid for example
17
(Nelson, et. al., 2006). This automation is forcing institutions to review and in many cases to
18
redesign their educational policies and procedures. These technologies require a paradigmatic
19
shift in knowledge delivery, impacting students, instructors and course content.
20
Within these modern educational settings, faculty, with little more than office applications for
21
support, continue to manage large amounts of educational data about individual students,
22
curricula and accreditation. Comprehensive, enterprise-wide educational information systems
23
that integrate administrative and academic functions are just beginning to provide educators
24
with applications to manage all aspects of the educator role. As nursing informatics faculty
25
become actively involved in the design, monitoring and evaluation of these comprehensive
26
systems, they will create the healthcare educational institutions of the future.
27
Traditional tuition models are a barrier to the globalization of education, but they are being
28
slowly eroded. New educational models are already being created as universities educate
29
beyond their walls or create virtual educational experiences, e.g., partnering with other
30
institutions to deliver classes for students across a region. Perhaps in the future, universities will
31
partner with business entities and vendors to create innovative models of education.
32
33
34
Curriculum design will change. Information is now generated and made available so quickly
that baseline knowledge for students will evolve away from specific content to methods of
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
49
1
finding accurate, current information and knowledge. In the future, students may not be
2
evaluated on specific knowledge for one area or course, but instead be evaluated on their
3
growth over time. The INS will be core in pushing this marriage of informatics and new
4
educational models because of the focus on managing information.
5
New Tools for Patients and Continued Access to Health Information
6
Patients will continue to become stronger partners with providers, with increased accountability
7
for their own care. This type of model will require solutions and patient education by clinical
8
nurses and INSs to devise the best methods of care as well as solutions to monitor and
9
maintain patients’ health.
10
Expanded Use of IT in Nursing
11
The earlier discussions imply that technology use will increase everywhere in our work and
12
home settings, even constantly traveling with us as wearable devices. Two implications are
13
outlined here. One is a current concern about students relying on available, structured
14
information, computerized alerts and reminders in systems such as EHRs and DSSs. Some
15
educators and administrators now are concerned that students’ critical thinking skills may
16
diminish. This concern may mean that INS and educators of the future will determine and test
17
new, effective academic and practice models. Perhaps academic applications will be designed
18
differently than practice applications to encourage questioning and active cognitive
19
engagement. Or system designers may need to rethink systems to promote a different cognitive
20
engagement by practitioners. Or educators might teach a new level of human information
21
processing to maximize human capabilities, one beyond students needing to memorize
22
structures for a physical examination and similar static information stored in an EHR. In this
23
model, information technology serves as support and not a replacement for human thinking and
24
judgment.
25
Second, as applications are increasingly integrated into healthcare, the impact of downtime
26
becomes more severe and quick recovery methods imperative. Especially with orders
27
management in place, institutions must ensure continual uptimes. Stratagems and technologies
28
are available to support continual uptime and the INS is typically involved in defining, designing
29
and installing them. Pervasive computing creates a new standard for information access – even
30
when there is no power supply, e.g., a laptop was developed using a hand crank to generate
31
power (MIT, 2007). Thus, INSs must be strong advocates for systems to be continuously
32
available. Likewise, they can be intimately involved in disaster recovery, including being an
33
advocate for funding allocations for recovery methods.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
50
1
In 2005, the Hurricane Katrina incident emphasized the importance of having redundant
2
systems and effective disaster recovery procedures. Requirements for current and future
3
systems will include:
4
•
5
6
24X7 operation and performance with redundancies throughout the system, failovers
and tested high reliability
•
Tools to assist with monitoring and managing the IT environment. Tools set up to
7
monitor system use and catch technology issues before system failure occurs, more
8
preventative than reacting to an issue later.
9
•
Scalable IT solutions as more clinical applications come on-line
10
•
Solutions that IT departments can manage without in-depth technology expertise
11
Implications for INSs
12
There are a number of implications for INSs. INSs will need to have a systematic method for
13
becoming aware of emerging technologies and their projected impact(s) to healthcare and
14
informatics. INSs can be essential leaders and partners for the safe and smart incorporation of
15
new technology and techniques into health informatics solutions. The content or information on
16
devices is still the most critical component of the technology and INSs can serve as content
17
designers in this capacity. Areas such as genomics may have ethical considerations that INSs
18
may need to voice and champion. The continued sub-specialization within NI will continue to
19
expand and INSs may find themselves specializing in the safe use of particular technologies.
20
All of these areas have implications for curricular design and education in the future. The
21
expansion of technology emphasizes the need for continuous availability of systems. On the
22
other hand, the digital divide is still apparent, with some having little access to information
23
technology. INSs can be leaders in eliminating the digital divide. In all examples, INSs can
24
advocate and apply methods for users to learn and use new technologies effectively and safely.
25
Trends in Health Delivery and Regulatory Initiatives
26
Current driving forces have greatly increased the pace of information technology and EHR
27
installations in the US. These forces include a national emphasis on patient safety, including
28
technology installation as a focal point for reducing for errors in healthcare. A second driving
29
force is that both health organizations, such as AHRQ and IHI, as well as non-health
30
organizations, such as Leapfrog, are impatient with slow progress to the point that they are
31
providing incentives for health institutions to implement informatics solutions. Other forces will
32
likely escalate the pace of adoption. Organizations are using value versus return on investment
33
models to justify health IT and pay for performance models will likely accelerate EHR
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
51
1
installations. Data are becoming more visible to consumers and hospital boards. Organizations
2
will continue to expand the transparency of data and, more importantly, the quality of care being
3
delivered.
4
Regulatory requirements and standards will shape the future. INSs will be at the table
5
defining these and future standards, designing, building, implementing, using and certifying
6
products that comply with the standards. A number of projects are underway with a sample
7
including:
8
•
CCHIT- Certification Commission for Healthcare Information Technology.
9
“CCHIT is a recognized certification body for electronic health records and their
10
networks, and an independent, voluntary, private-sector initiative. Their mission
11
is “to accelerate the adoption of health information technology by creating an
12
efficient, credible and sustainable product certification program” (CCHIT, 2007).
13
•
HL7 is defining interoperability standards for systems.
14
•
The IEEEP2407 working group is focusing on developing standards for
15
16
Personalized Health Informatics.
•
The Joint Commission continues to expand regulatory compliance for patient
17
safety, e.g., National Patient Safety Goals, medication reconciliation and other
18
requirements with implications for the INS.
19
•
20
21
The Health Information Technology Standards Panel (HITSP) is harmonizing
industry-wide health IT standards
•
Nationwide Health Information Network (NHIN) initiative is creating prototype
22
architectures for widespread health information exchange
23
The FDA (Food and Drug Administration) has several initiatives underway:
24
•
25
Bar Code Label Requirements for Human Drug Products and Biological
Products (FDA, 2007)
26
•
Draft guidelines for the safe and effective use of radio frequency devices
27
•
Nanotechnology development (FDA Nanotechnology, 2007) and an potential
28
expansion of products covered, e.g., advanced decision support tools and similar
29
informatics applications.
30
New Care Delivery models
31
Care is no longer a local phenomenon. Patients in rural ICUs can be monitored remotely by
32
intensivists and ICU nurses. Pharmacists are providing remote pharmacological assistance to
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
52
1
rural areas. Radiologists can read images in realtime from anywhere in the world. Physicians
2
are assisted by robots while examining patients in distant locations.
3
Care is no longer limited to traditional healthcare settings, even when it is delivered locally.
4
Clinicians are now available in retail stores, work settings and other non-traditional places.
5
These new settings will require new designs, deployment and support models that will challenge
6
the NI specialist. INSs involvement in the development of the robust health information
7
infrastructure includes but is not limited to:
8
•
9
10
Continued innovation of systems and expansion into less traditional settings such as
Long Term Care and rural communities
•
Personal Health Records – INSs will assist with development of and encourage
11
individuals to maintain an electronic vaccination history, their past medical history,
12
medications, allergies, condition/status, visit history in an easily accessible online format.
13
As well, patients online communications with healthcare providers will continue to
14
increase
15
•
Clinical Data Repositories and Regional Health Information Organizations will support
16
accurate, timely and secure transfer of patient data across care settings within a
17
community (ultimately across hospitals, clinics, pharmacies, laboratories, clinician office,
18
long term care facilities and others)
19
Consumer Informatics
20
Patients will become stronger partners with providers, having increased accountability and
21
interest in access to their own EMR data, and for their own care. As consumers become more
22
technically savvy, they will consider their electronic healthcare data as necessary and
23
accessible as their banking information or stock transactions online. Likewise, consumers will
24
being monitoring and managing the health of their younger AND older family members for whom
25
they are responsible.
26
External Partnerships
27
Healthcare will likely see non-traditional organizations entering the healthcare arena. For
28
example, one company with an online application for individual, secure, financials is now
29
investigating expansion into personal health records. Likewise, healthcare should create new,
30
non-traditional partnerships. For instance, perhaps a partnership with the video-gaming industry
31
would also be fruitful for interactive EHRs and provide ideas for optimal user interfaces.
32
Implications for INSs
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
53
1
New care models have vast implications for informatics nurses. These new delivery models will
2
require INSs to continue to develop informatics solutions for care in multiple, remote locations.
3
INSs should have a key role in informatics solutions that emphasize quality care (McCormick, et
4
al., 2007). We need new models to speed the design to use portions of the systems life cycle.
5
An 18 – 24 month build and implementation cycle is not tenable in an era of rapidly changing
6
technology, care delivery and expanding information access. Because of the increasing the
7
number information technology installations and the need to respond to increasing regulatory
8
requirements, INSs will be at centerstage for all phases of the systems lifecycle. They will be
9
developing and implementing new informatics solutions, ensuring that data quality exists for
10
implemented solutions and evaluating the impact of solutions. The new model of consumer
11
informatics will require technical solutions and patient education jointly from clinical nurses and
12
INSs. INSs will need to devise the best methods of care as well as designing solutions to enable
13
patients to monitor and maintain their own health. INSs will play a key role in designing new
14
tools for data capture and analyses to comply with regulatory guidelines.
15
Futures Conclusion
16
The positions and competencies of nurses, changes in technology and new trends in health
17
delivery and regulation will impact the future of Nursing Informatics. Important concepts
18
underpinning the above themes include:
19
•
Preparing for and evolving with new information and technology changes,
20
•
Inventing and delivering new educational models to teach both new and existing nursing
21
22
professionals,
•
23
24
technologies across all areas of nursing and health settings
•
25
26
29
Incorporating newer technologies and methods to redesign care, research and
administrative processes,
•
27
28
Designing, developing, implementing and evaluating solutions for new information and
Pioneering, designing and facilitating the changes in care models as they evolve away
from episodic care toward more predictive and preventative models.
•
Focusing on usability – designing and evaluating how information is presented to
promote ease of use and adoption (human computer interaction).
30
The global nature of informatics is already apparent. In the future, care models and data will
31
be shared even more widely. New technologies will create wider access to information and the
32
need for a new generation of data and information management skills, analytic tools, new
33
educational models and different cognitive skills. Traditional boundaries of institutions, care
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
54
1
delivery and education will continue to erode. New positions and functional areas are emerging.
2
Increased collaboration among NI colleagues and a shared scope and standard of NI practice
3
will be the hallmark of the future.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
55
1
STANDARDS OF NURSING INFORMATICS PRACTICE
2
3
Nursing informatics (NI) is the specialty that integrates nursing science, computer science,
4
and information science to manage and communicate data, information, knowledge, and
5
wisdom in nursing practice. Nursing informatics facilitates the integration of data, information,
6
knowledge, and wisdom to support patients, nurses, and other providers in their decision-
7
making in all roles and settings. This support is accomplished through the use of information
8
structures, information processes, and information technology.
9
The goal of nursing informatics is to improve the health of populations, communities,
10
families, and individuals by optimizing information management and communication. These
11
activities include the design and use of informatics solutions and/or technology to support all
12
areas of nursing, including, but not limited to, the direct provision of care, establishing effective
13
administrative systems, managing and delivering educational experiences, enhancing life long
14
learning, and supporting nursing research.
15
The standards of nursing informatics practice include two components: the standards of
16
practice and the standards of professional performance. Each standard includes accompanying
17
measurement criteria that provide more detail about the expected knowledge, skills, and abilities
18
necessary to meet that standard. Some standards include additional measurement criteria
19
specific to informatics nurse specialists and their role and practice.
20
The standards of practice are organized using a general problem-solving framework that
21
closely models the language provided in Nursing: Scope and Standards of Practice (ANA, 2004)
22
describing the familiar nursing process of assessment, diagnosis, identification of outcomes,
23
planning, implementation, and evaluation. The problem-solving framework supports all facets of
24
informatics practice, helps to identify and clarify issues, and aids in the selection, development,
25
implementation, and evaluation of informatics solutions. These steps are not mutually exclusive
26
and may often overlap.
27
Informatics solution is a generic term used in this document to describe an application,
28
product, method, tool, workflow change or other recommendation an informatics nurse makes
29
after identifying and analyzing a need or an issue. An informatics solution may encompass
30
technology and non-technology products such as developing a database, purchasing a new
31
computer application, creating a standardized nursing vocabulary, designing informatics
32
curricula, creating a spreadsheet, tailoring an application to a particular environment, designing
33
a research study to describe required informatics competencies, describing information flow in a
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
56
1
process redesign, creating newly re-engineered processes or creating a structure for
2
information presentation.
3
The standards of professional performance also reflect the model language provided in
4
Nursing: Scope and Standards of Practice (ANA, 2004), have been re-ordered, and include an
5
additional standard and accompanying measurement criteria addressing advocacy.
6
These standards of nursing informatics practice and the identified measurement criteria
7
apply to all informatics nurses and their practices. The measurement criteria for the informatics
8
nurse specialist reflect the additional expectations for this role and advanced level of practice.
9
Overarching Principles for Nursing Informatics Practice
10
Three overarching principles are inherent in every aspect of nursing informatics practice and
11
should be considered by informatics nurses and informatics nurse specialists when addressing
12
the standards of practice.
13
The informatics nurse:
14
1. Incorporates theories, principles, and concepts from appropriate sciences into informatics
15
practice. Examples of theories could include information, systems, and change theories.
16
Principles and concepts could include project management, implementation methods,
17
workflow analyses, with process redesigns, organizational culture, or database structures.
18
2. Integrates ergonomics and human–computer interaction (HCI) principles into informatics
19
solution design, development, selection, implementation, and evaluation.
20
3. Systematically determines the social, legal, regulatory and ethical impact of an informatics
21
solution within nursing and health care.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
57
1
STANDARDS OF NURSING INFORMATICS PRACTICE
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
Standards of Practice
STANDARD 1. ASSESSMENT
The informatics nurse collects comprehensive data, information, and knowledge
pertinent to the situation.
Measurement Criteria:
The informatics nurse:
Collects data, information, and knowledge in a systematic and ongoing process, such as
with a needs assessment to refine the issue or problem, or with workflow analyses to
examine current practice, workflow, and the potential impact of an informatics solution
on that workflow.
Involves the patient, family, nurse, other healthcare providers, and key stakeholders, as
appropriate, in holistic data collection.
Prioritizes data collection activities based on the immediate or anticipated needs of the
situation.
Uses appropriate evidence-based assessment techniques and instruments in collecting
pertinent data to define the issue or problem.
Uses analytical models and assessment tools that facilitate problem solving.
Synthesizes available data, information, and knowledge relevant to the situation to
identify patterns and variances.
Documents relevant data in a retrievable format.
STANDARD 2. PROBLEMS OR ISSUES
The informatics nurse analyzes the assessment data to determine the problems or
issues.
Measurement Criteria:
The informatics nurse:
Derives the problems, needs, or issues based on assessment data.
Validates the problems, needs, or issues with the patient, family, nurse, other healthcare
providers, and key stakeholders when possible and appropriate.
Documents problems, needs, or issues in a manner that facilitates the determination of
the expected outcomes and plan.
STANDARD 3. OUTCOMES IDENTIFICATION
The informatics nurse identifies expected outcomes for a plan individualized to the
situation.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
58
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
Measurement Criteria:
The informatics nurse:
Involves the patient, family, nurses, other healthcare providers, and key stakeholders in
formulating expected outcomes when possible and appropriate.
Considers associated risks, benefits, costs, current scientific evidence, environmental
factors, and expertise when formulating expected outcomes.
Defines expected outcomes in terms of the patient, patient values, ethical
considerations, environment, organization, or situation with such consideration as
associated risks, benefits and costs, and current evidence-based knowledge.
Includes a time estimate for attainment of expected outcomes.
Develops expected outcomes that provide direction for all key stakeholders.
Modifies expected outcomes based on changes in the status or evaluation of the
situation.
Documents expected outcomes as measurable goals.
Additional Measurement Criteria for the Informatics Nurse Specialist:
The informatics nurse specialist:
Identifies expected outcomes that incorporate scientific evidence and are achievable
through implementation of evidence-based practices.
Identifies expected outcomes that maximize quality, efficiency, and effectiveness
balanced with economy.
Supports the use of clinical guidelines, such as, but not limited to the integration of
clinical guidelines into practice, information system and informatics solutions, and
knowledge bases.
STANDARD 4. PLANNING
The informatics nurse develops a plan that prescribes strategies, alternatives, and
recommendations to attain expected outcomes.
Measurement Criteria:
The informatics nurse:
Develops a customized plan considering clinical and business characteristics and the
environmental situation.
Develops the plan in conjunction with the patient, family, nurse, other healthcare
providers, key stakeholders, and others, as appropriate.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
59
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
Includes strategies within the plan that address each of the identified problems and
issues, which may include strategies for the synthesis of data, information, and
knowledge to enhance healthcare delivery.
Provides for continuity within the plan.
Incorporates an implementation pathway or timeline within the plan.
Establishes the plan priorities with the key stakeholders and others as appropriate.
Utilizes the plan to provide direction to healthcare team members and other stakeholders.
Defines the plan to reflect current statutes, rules and regulations, and quality standards
Integrates current research and trends in the planning process.
Considers the clinical, financial, and social impact of the plan.
Uses standardized language, tools, and methodologies to document the plan.
Participates in the design and development of interdisciplinary processes and
informatics principles to address the situation or issue.
Contributes to the development and continuous improvement of organizational systems
that support the planning process.
Supports the integration of clinical, human, financial, and technical resources to enhance
and complete the decision-making processes.
STANDARD 5. IMPLEMENTATION
The informatics nurse implements the identified plan.
Measurement Criteria:
The informatics nurse:
Implements the plan in a safe and timely manner.
36
Documents implementation and any modifications, including changes or omissions, of
37
the identified plan.
38
Utilizes specific evidence-based actions and steps specific to the problem or issues to
39
achieve the defined outcomes.
40
Utilizes clinical, financial, technical, and community resources and systems to implement
41
the plan.
42
Collaborates with colleagues and other stakeholders to implement the plan.
43
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
60
1
2
Implements the plan using principles and concepts of quality, project, or systems
management.
3
4
5
6
Fosters organizational systems that support implementation of the plan.
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
Incorporates new knowledge and strategies to initiate change in informatics and nursing
practices if desired outcomes are not achieved.
STANDARD 5A: COORDINATION OF ACTIVITIES
The informatics nurse coordinates activities.
Measurement Criteria:
The informatics nurse:
Coordinates implementation of the plan, including activities and resources necessary to
achieve desired outcomes.
Synthesizes data and information to prescribe necessary system and environmental
support measures.
Documents the coordination of the activities.
Measurement Criteria for the Informatics Nurse Specialist:
The informatics nurse specialist:
Provides leadership in the coordination of interdisciplinary informatics activities.
Coordinates system and community resources that enhance delivery of care across
continuums.
STANDARD 5B: HEALTH TEACHING, HEALTH PROMOTION, AND EDUCATION FOR INFORMATICS
SOLUTIONS
The informatics nurse employs strategies to promote health teaching, health promotion,
and education for informatics solutions.
Measurement Criteria:
The informatics nurse:
Identifies the need to integrate health content and learning resources into healthcare
systems that address such topics as healthy lifestyles, risk-reducing behaviors,
developmental needs, activities of daily living, and preventive self-care.
Participates in the design, development, implementation, and evaluation of health
promotion materials and health teaching methods appropriate to the situation and the
patient’s developmental level, learning needs, readiness, ability to learn, language
preference, and culture. The informatics nurse focuses on the integration of these into
informatics solutions
Contributes to the design, development, implementation, and evaluation of the
educational content, materials, and teaching strategies in a wholistic manner
(psychosocial, cognitive, affective) needed for the continuing education and professional
development programs necessary to implement the plan.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
61
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
Additional Measurement Criteria for the Informatics Nurses Specialist:
The informatics nurse specialist:
Synthesizes empirical evidence on risk behaviors, learning theories, behavioral change
theories, motivational theories, epidemiology, and other related theories and frameworks
when designing health information and patient education materials and programs.
Designs health information and patient education appropriate to the patient’s
developmental level, learning needs, readiness to learn, and cultural values and beliefs.
Evaluates health information resources, such as the Internet, within the area of practice
for accuracy, readability, and comprehensibility to help patients, family, healthcare
providers, and others access quality health information.
Creates opportunities for feedback and evaluation of the effectiveness of the educational
content and teaching strategies used for the continuing education and professional
development programs necessary to implement the plan.
STANDARD 5C: CONSULTATION
The informatics nurse provides consultation to influence the identified plan, enhance the
abilities of others, and effect change.
Measurement Criteria for the Informatics Nurse
The informatics nurse:
Synthesizes data, information, theoretical frameworks and evidence when providing
consultation.
Facilitates the effectiveness of a consultation by involving the stakeholders in the
decision-making process.
Communicates consultation recommendations that influence the identified plan, facilitate
understanding by involved stakeholders, enhance the work of others, and effect change.
The informatics nurse specialist:
Develops recommendations and strategies to address and resolve complex issues and
problems.
Establishes formal and informal consultative relationships that can also provide
professional development and mentorship opportunities.
STANDARD 6. EVALUATION
The informatics nurse evaluates progress towards attainment of outcomes.
Measurement Criteria:
The informatics nurse:
Conducts a systematic, ongoing, and criterion-based evaluation of the outcomes in
relation to the structures and processes prescribed by the plan and the indicated
timeline.
Includes key stakeholders and others involved in the plan or situation in the evaluative
process.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
62
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
Supports the integration and use of evidence-based methods, tools and guidelines
linked to effective outcomes.
Evaluates the effectiveness of the planned strategies in relation to the attainment of the
expected outcomes.
Uses ongoing assessment data to revise the problems and issues, the outcomes, the
plan, and the implementation and evaluative processes as needed.
Disseminates the results to key stakeholders and others involved in the plan or situation
as appropriate.
Documents the results of the evaluation.
Additional Measurement Criteria for the Informatics Nurse Specialist:
The informatics nurse specialist:
Uses the results of the evaluation analyses to make or recommend process or structural
changes including policy, procedure or protocol documentation, as appropriate.
Synthesizes the results of the evaluation analyses to determine the impact of the plan on
the affected patients, families, groups, communities, and institutions, networks, and
organizations.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
63
1
2
3
4
5
6
7
8
9
10
STANDARDS OF PROFESSIONAL PERFORMANCE
STANDARD 7. EDUCATION
The informatics nurse attains knowledge and competency that reflects current nursing
and informatics practice.
Measurement Criteria:
The informatics nurse:
Participates in ongoing educational activities related to appropriate knowledge bases
and professional issues.
11
12
Demonstrates a commitment to lifelong learning through self-reflection and inquiry to
identify learning needs.
13
14
Seeks experiences that reflect current practice in order to maintain skills and
competence in informatics practice and role performance.
15
16
Acquires knowledge and skills appropriate to the specialty area, practice setting, role, or
situation.
17
18
Maintains professional records that provide evidence of competency and life long
learning.
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
Seeks experiences and formal and independent learning activities to maintain and
develop clinical and professional skills and knowledge.
Additional Measurement Criteria for the Informatics Nurse Specialist:
The informatics nurse specialist:
Uses current research findings and other evidence to expand knowledge, enhance role
performance, and increase knowledge of professional issues.
STANDARD 8. PROFESSIONAL PRACTICE EVALUATION
The informatics nurse evaluates one’s own nursing and informatics practice in relation to
professional practice standards and guidelines, relevant statutes, rules, and regulations.
Measurement Criteria:
The informatics nurse’s practice reflects the application of knowledge of current practice
standards, guidelines, statutes, rules, and regulations.
The informatics nurse:
Engages in self-evaluation of practice on a regular basis, identifying areas of strength as
well as areas in which professional development would be beneficial.
38
39
Obtains informal feedback regarding one’s own practice from peers, professional
colleagues, key stakeholders, and others.
40
Participates in systematic peer review as appropriate.
41
Takes action to achieve goals identified during the evaluation process.
42
43
Provides rationales for practice beliefs, decisions, and actions as part of the informal and
formal evaluation processes.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
64
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
STANDARD 9. QUALITY OF PRACTICE
The informatics nurse systematically enhances the quality and effectiveness of nursing
and informatics practice.
Measurement Criteria:
The informatics nurse:
Demonstrates quality by documenting the application of the nursing process in a
responsible, accountable, and ethical manner.
Uses the results of quality improvement activities to initiate changes in nursing and
informatics practice and in the healthcare delivery system.
Uses creativity and innovation in nursing and informatics practice to improve care
delivery.
Incorporates new knowledge to initiate changes in nursing and informatics practice if
desired outcomes are not achieved.
Participates in quality improvement activities. Such activities may include:
Identifying aspects of practice important for quality monitoring.
Using indicators developed to monitor quality and effectiveness of nursing
and informatics practice.
Collecting data to monitor quality and effectiveness of nursing and
informatics practice.
Analyzing quality data to identify opportunities for improving nursing and
informatics practice.
Formulating recommendations to improve nursing and informatics
practice or outcomes.
Implementing activities to enhance the quality of nursing and informatics
practice.
Engaging in the development, implementation, and evaluation of policies,
procedures and/or guidelines to improve the quality of practice.
Participating on interdisciplinary teams to evaluate clinical care or delivery
of health services.
Participating in efforts to minimize costs and unnecessary duplication.
Analyzing factors related to safety, satisfaction, effectiveness, and
cost/benefit options.
Analyzing organizational systems for barriers
Implementing processes to remove or decrease barriers within
organizational systems.
Obtains and maintains professional certification if available in the area of expertise.
Designs quality improvement initiatives.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
65
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
Implements initiatives to evaluate the need for change.
Evaluates the practice environment in relation to existing evidence, identifying
opportunities for the generation and use of research.
STANDARD 10. COLLEGIALITY
The informatics nurse interacts with and contributes to the professional development of
peers and colleagues.
Measurement Criteria:
The informatics nurse:
Shares knowledge and skills with peers and colleagues as evidenced by such activities
as presentations at formal or informal meetings and professional conferences.
Provides peers with feedback regarding their practice and/or role performance.
17
Interacts with peers and colleagues to enhance one’s own professional nursing practice
18
and/or role performance.
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
Maintains compassionate and caring relationships with peers and colleagues.
Contributes to an environment that is conducive to the education of healthcare
professionals.
Contributes to a supportive and healthy work environment.
Additional Measurement Criteria for the Informatics Nurse Specialist:
The informatics nurse specialist:
Participates on interdisciplinary professional teams that contribute to role development
and, directly or indirectly, advance nursing, informatics practice, and health services.
Mentors other registered nurses and colleagues as appropriate.
STANDARD 11. COLLABORATION
The informatics nurse collaborates with key stakeholders and others in the conduct of
nursing and informatics practice.
Measurement Criteria:
The informatics nurse:
Communicates with key stakeholders regarding the practice of nursing and informatics.
Communicates with key stakeholders regarding the role of nurses and nursing within the
domain of healthcare informatics and patient care delivery.
Collaborates in creating a documented plan focused on outcomes and decisions related
to the management of data, information, and knowledge for the delivery of healthcare
services.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
66
1
2
Partners with others to effect change and generate positive outcomes through
knowledge of the plan and situation.
3
4
Documents plans, communications, rationales for plan changes, and collaborative
discussions.
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
Additional Measurement Criteria for Informatics Nurse Specialist:
The informatics nurse specialist:
Partners with others to enhance health care, and ultimately patient care, through
interdisciplinary activities such as education, consultation, management, technological
development, or research opportunities.
STANDARD 12. ETHICS
The informatics nurse integrates ethical provisions in all areas of practice.
Measurement Criteria:
The informatics nurse:
Uses the Code of Ethics for Nurses with Interpretive Statements (ANA, 2001) to guide
practice.
Uses nursing and informatics principles and methodologies in a manner that preserves
and protects patient autonomy, dignity and rights.
Employs informatics principles, standards, and methodologies to establish and maintain
patient confidentiality within legal and regulatory parameters.
Evaluates factors related to privacy, security, and confidentiality in the use and handling
of data, information, and knowledge.
Promotes active engagement of community members in the oversight and management
of the exchange of health information.
Serves as a patient advocate assisting patients in developing skills for self advocacy.
Contributes to resolving ethical issues of patients, colleagues, or systems as evidenced
in such activities as participating on ethics committees.
Reports illegal, incompetent, or impaired practices.
Seeks available resources as needed when formulating ethical decisions.
Demonstrates a commitment to practicing self-care, managing stress, and connecting
with self and others.
Additional Measurement Criteria for the Informatics Nurse Specialist:
The informatics nurse specialist
Participates on multidisciplinary and interdisciplinary teams that address ethical risks,
benefits, and outcomes.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
67
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
Informs administrators or others of the risks, benefits, and outcomes of programs and
decisions that affect healthcare delivery.
STANDARD 13. RESEARCH
The informatics nurse integrates research findings into practice.
Measurement Criteria:
The informatics nurse:
Utilizes the best available evidence, including research findings, to guide practice
decisions.
Actively participates in research activities at various levels appropriate to the nurse’s
level of education and position. Such activities may include:
Identifying clinical, nursing, and informatics problems or issues specific to
nursing research
Participating in data collection such as surveys, pilot projects, and formal
studies.
Participating in a formal committee or program.
Sharing research activities and/or findings with peers and others
Conducting research.
Critically analyzing and interpreting research for application to practice.
Using research findings in the development of policies, procedures, and
standards of practice in patient care.
Incorporating research as a basis for learning.
Additional Measurement Criteria for the Informatics Nurse Specialist:
The informatics nurse specialist:
Contributes to nursing knowledge by conducting or synthesizing research that discovers,
examines and evaluates knowledge, theories, criteria, and creative approaches to
improve health care.
Formally disseminates research findings through activities such as presentations,
publications, consultation, and journal clubs.
STANDARD 14. RESOURCE UTILIZATION
The informatics nurse considers factors related to safety, effectiveness, cost, and impact
on practice in the planning and delivery of services to achieve expected outcomes.
Measurement Criteria:
The informatics nurse:
Evaluates factors such as safety, effectiveness, availability, cost and benefits,
efficiencies, and impact on practice, when choosing practice options that would result in
the same expected outcome.
Assists stakeholders in identifying and securing appropriate and available services to
address identified needs and implement and complete the plan or other activity.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
68
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
Assigns or delegates tasks based on the knowledge, skills and abilities of the individual,
complexity of the task, and predictability of the outcome.
Assists stakeholders in becoming informed consumers about the options, costs, risks,
and benefits of the plan and its associated activities.
Additional Measurement Criteria for the Informatics Nurse Specialist:
The informatics nurse specialist:
Develops innovative solutions and applies strategies to obtain appropriate resources for
nursing initiatives.
Secures organizational resources to ensure a work environment conducive to
completing the identified plan and outcomes.
Develops evaluation methods to measure safety and effectiveness for interventions and
outcomes.
Promotes activities that assist stakeholders, as appropriate, in becoming informed about
costs, risks, and benefits of care or of the plan and solution.
Standard 15. Advocacy
The informatics nurse advocates for the protections and rights of patients, healthcare
providers, institutions and organizations, and for issues related to data, information,
knowledge and health care.
Measurement Criteria:
The informatics nurse:
Supports patient access to their own personal health information within a reasonable
timeframe.
Promotes patient awareness of how their personal health data and information may be
used and who has access to it.
Supports the individual’s right and ability to supplement, request correction of, and share
their personal health data and information.
Evaluates factors related to privacy, security, and confidentiality in the use and handling
of health information.
Promotes awareness and education of the healthcare consumer with regard to
appropriate data collection, information sharing, information access, and associated
issues.
Supports patient involvement in their own care, facilitated by access to personal
healthcare data.
Promotes active engagement of community members in the development, oversight, and
management of health information exchange.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
69
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
35
36
37
38
39
40
41
42
43
44
45
46
47
48
49
50
Educates clinicians, patients and communities about the rights, responsibilities, and
accountability involved in the collection, use, and exchange of healthcare data and
information.
Incorporates the identified needs of the patient, family, healthcare provider, organization,
and key stakeholders in policy development, program and services planning, and
systems design.
Integrates advocacy into the implementation of policies, programs and services, and
systems for the patient.
Evaluates the effectiveness of advocating for the patient, family, healthcare provider,
organization, and key stakeholders when assessing the expected outcomes.
Demonstrates skill in advocating before providers and stakeholders on behalf of the
patient, community, or population.
Strives to resolve conflicting expectations from patients, families, communities,
populations, healthcare providers, and other stakeholders.
Additional Measurement Criteria for the Informatics Nurse Specialist:
The informatics nurse specialist:
Demonstrates skill in advocating on behalf of the patient, key stakeholders, programs,
and services before public representatives and decision-makers.
Exhibits fiscal responsibility and integrity in policy development and advocacy activities
and processes.
Serves as an expert for patients, peers, other healthcare providers, and other
stakeholders in promoting and implementing policies related to the management of data
information, and knowledge.
STANDARD 16. LEADERSHIP
The informatics nurse provides leadership in the professional practice setting and the
profession.
Measurement Criteria:
The informatics nurse:
Engages in teamwork as a team player and a team builder.
Works to create and maintain healthy work environments in local, regional, national, or
international communities.
Displays the ability to define a clear vision, the associated goals, and a plan to
implement and measure progress.
Demonstrates a commitment to continuous, life long learning for self and others.
Teaches others to succeed by mentoring and other strategies.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
70
1
Exhibits creativity and flexibility through times of change.
2
Demonstrates energy, excitement, and a passion for quality work.
3
4
Willingly accepts mistakes by self and others thereby creating a culture in which risktaking is not only safe, but expected.
5
Inspires loyalty through valuing of people as the most precious asset in an organization.
6
7
Directs the coordination of the plan across settings and among caregivers and other
stakeholders.
8
9
Serves in key roles in the work setting by participating on committees, councils, and
administrative teams.
10
11
12
13
14
15
16
17
18
19
20
21
22
Promotes advancement of the profession through participation in professional
organizations.
Assumes leadership roles within organizations representing nursing informatics
professional practice within the healthcare domain.
Additional Measurement Criteria for the Informatics Nurse Specialist:
The informatics nurse specialist:
Serves in key leadership roles defining the vision, strategy and tactical plans related to
the management of data, information, and knowledge.
Works to influence decision-making bodies to improve patient care, health services, and
policies through such things as the adoption of data standards.
23
24
Promotes communication of information and advancement of the profession through
writing, publishing, and presentations for professional or lay audiences.
25
Designs innovations to effect change in practice and outcomes.
26
27
Provides direction to enhance the effectiveness of the interdisciplinary team and key
stakeholders.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
71
1
GLOSSARY
2
Beginning nurse – A nurse preparing for initial entry into nursing practice or who has just
3
begun a nursing career.
4
5
Computer literacy – the knowledge and skills to use basic computer applications and computer
6
technology
7
8
Data – Discrete entities that are described objectively without interpretation.
9
10
Decision support system – computer applications designed to facilitate human decision
11
making processes. Usually DSS are rule-based, using a specified knowledge base and a set of
12
rules to analyze data and information and provide recommendations typically through the use of
13
a knowledge base and rules to make recommendations to users
14
15
Experienced nurse – A nurse with proficiency in one or more domains of interest.
16
17
Expert system – A type of decision support system that implements the knowledge of one or
18
more human experts
19
20
Human-Computer Interaction – HCI deals with people, software applications, computer
21
technology and the ways they influence each other.
22
23
Informatics Nurse Specialist – the INS is a RN with formal, graduate education in the field of
24
informatics or a related field. A specialist in the field of informatics in nursing.
25
26
Informatics Nurse – The IN is a RN with an interest or experience working in an informatics
27
field. A generalist in the field of informatics in nursing.
28
29
Informatics solution – A generic term used to describe the product an IN specialist
30
recommends after identifying and analyzing an issue. Informatics solutions may encompass
31
technology and non-technology products such as information systems, new applications,
32
nursing vocabulary, or informatics curricula.
33
34
Information – Data that are interpreted, organized, or structured.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
72
1
Information Literacy – Recognizing when information is needed and having the ability to
2
locate, evaluate, and effectively use the needed information
3
4
Interdisciplinary – Reliant on the overlapping skills and knowledge of each team member and
5
discipline, resulting in synergistic effects where outcomes are enhanced and more
6
comprehensive than the simple aggregation of any team member’s individual efforts.
7
8
Knowledge – Information that is synthesized so that relationships are identified and formalized.
9
10
Nursing informatics (NI) – A specialty that integrates nursing science, computer science, and
11
information science to manage and communicate data, information, knowledge and wisdom in
12
nursing practice. Nursing informatics facilitates the integration of data, information, and
13
knowledge to support patients, nurses, and other providers in their decision-making in all roles
14
and settings. This support is accomplished through the use of information structures,
15
information processes, and information technology.
16
17
Wisdom – the appropriate use of knowledge to solve human problems. It is knowing when and
18
how to apply knowledge.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
73
1
2
References
Alliance for Nursing Informatics Member Organization Report (2005). AMIA NIWG Activities for
3
2006. Retrieved on December 8, 2006 from
4
http://www.allianceni.org/doc/ANI_MemberOrgReport2005-06.pdf
5
American Library Association. (2006). Information Literacy Competency Standards for Higher
6
Education. [Electronic Version]. Retrieved September 15, 2006 from
7
http://www.ala.org/acrl/ilcomstan.html
8
American Medical Informatics Association Nursing Informatics Working Group. (2006). Roles in
9
Nursing Informatics. URL http://www.amia.org/mbrcenter/wg/ni/roles/inf_nrs.asp [accessed
10
11
12
13
14
15
16
17
18
19
20
21
22
23
24
25
2006 February 28]
American Nurses’ Association. (1998). Core Principles on Telehealth. Washington DC:
American Nurses Publishing.
American Nurses’ Association. (1999). Competencies for Telehealth Technologies in Nursing
Washington, DC: American Nurses Publishing.
American Nurses’ Association. (2000). Scope and Standards of Practice for Nursing
Professional Development. Silver Spring, MD: American Nurses’ Association.
American Nurses Association (2001). Code of Ethics for Nurses. Retrieved on October 17, 2006
from www.nursingworld.org/ethics
American Nurses’ Association. (2004a). Nursing Scope and Standards of Practice. Silver
Spring, MD: American Nurses’ Association.
American Nurses’ Association. (2004b). Scope and Standards for Nurse Administrators. Second
Edition. Silver Spring, MD: American Nurses’ Association.
American Nurses Association (2006) Privacy and Confidentiality Position Statement. Retrieved
on January 3, 2007 from http://www.nursingworld.org/readroom/position/ethics/
Androwich, I. M., Bickford, C. J., Button, P.J., Hunter, K. M., Murphy, J., Sensmeier, J. (2003)
26
Clinical information systems: A framework for reaching the vision. Washington DC:
27
American Nurses Publishing.
28
29
30
31
32
33
Barton, A. J. (2005). Cultivating informatics competencies in a community of practice. Nursing
Administration Quarterly, 29(4), 323-328.
Bellinger, G., Castro, D., & Mills, A. (2004). Data, Information, Knowledge, and Wisdom. URL
http://www.systems-thinking.org/dikw/dikw.htm [accessed 2006 February 28]
Benner, P. E., Hooper-Kyriakidis, P. L., Stannard, D. (1999). Clinical wisdom and interventions
in critical care: A thinking-in-action approach. Saunders Pub.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
74
1
Blum, B. (1986). Clinical information systems. New York: Springer-Verlag.
2
Brennen, P.F. A discipline by any other name. Journal of the American Medical Informatics
3
Association. 2002;9:306-307.
4
CCHIT. (2007). URL: http://www.cchit.org/, accessed 1/15/07.
5
Center for Nursing Classification and Clinical Effectiveness, University of Iowa. (2004).
6
Overview of NIC/NOC. URL http://www.nursing.uiowa.edu/centers/cncce [accessed 2006
7
February 28]
8
9
10
11
12
Clark, Donald, (2004) Understanding: The Continuum of Understanding retrieved March 21,
2007 from http://www.nwlink.com/~donclark/performance/understanding.html.
Curran, C. R. (2003). Informatics competencies for nurse practitioners. American Association of
Critical Care Nurses Clinical Issues, 14(3), 320-330.
Dejardins, K. S., Cook, S. S., Jenkins, M., Bakken, S. (2005). Effect of an informatics for
13
evidence-based practice curriculum on nursing informatics competencies. International
14
Journal of Medical Informatics, 74, 1012-1020.
15
Device (2007). http://www.sciencedaily.com. Accessed 2/14/07.
16
Dix, A., Finlay, J., Abowd, G., & Beale, R. (2004). Human-computer interaction. Harlow,
17
18
19
England: Pearson, Prentice Hall.
Englebardt, S. & Nelson, R. (2002) Health care informatics: An interdisciplinary approach. St.
Louis: Mosby-Year Book, Inc.
20
FDA, (2007). URL: http://www.fda.gov/oc/initiatives/barcode-sadr/. Accessed 1/22/07.
21
FDA Nanotechnology, (2007). URL: www.fda/nanotechnology. Accessed 1/5/07.
22
Garde, S., Harrison, D., & Hovenga, E. (2005). Skill needs for nurses in their role as health
23
informatics professionals: A survey in the context of global health informatics education.
24
International Journal of Medical Informatics, 74(11-12), 899-907.
25
Gordon, A.T., Lutz, G.E., Boninger, M. L., & Cooper, R. A. (2007). Introduction to
26
nanotechnology: potential applications in physical medicine and rehabilitation. American
27
Journal of Physical Medicine & Rehabilitation. 86(3), 225- 241.
28
29
30
31
32
33
34
Grady, J., L. Schlachta-Fairchild, and V. Elfrink. (2005). Results of the 2004 International
Telenursing Survey. Telemedicine and e-Health, 11(2), 197.
Graves, J. & Corcoran, S. (1989) The study of nursing informatics. Image, 21(4) Winter, 227230.
Greenback, L. (2007). Robot aids John Hopkins patients. The Baltimore Examiner. URL:
http://www.examiner.com/a-498079. Robot_aids_Johns_Hopkins_patients.htm Accessed
1/9/07.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
75
1
2
3
4
5
6
7
8
9
Greene, J. (2004). RN to CIO: High-tech nurses bridge hospitals’ cultural divide. Hospitals and
Health Networks 78(2):40-6, 2.
Hammond, W. E. (1995). Glossary for Healthcare Standards. URL http://dmiwww.mc.duke.edu/dukemi/acronyms.htm [accessed 2006 February 28]
Hannah, K. J., Ball, M. J., & Edwards, M. J. (Eds.) (1994). Introduction to Nursing Informatics.
New York: Springer-Verlag.
Harrison, L. (200) Nursing activity in general intensive care. Journal Clinical Nursing, 11(2), 15867.
Haug, P., Gardner, R., & Evans, S. (1999). “Hospital-Based Decision Support”. In E.S. Berner
10
(Ed.), Clinical Decision Support Systems: Theory and Practice (pp.77-104). New York:
11
Springer-Verlag.
12
Health Information Management Systems Society (HIMSS). (2005, September 8). HLA
13
Competency Directory: Ensuring Future Leaders Meet the Challenges of Managing the
14
Nation's Healthcare Organizations. Retrieved November 22, 2006, from Health Information
15
Management Systems Society Web Site:
16
http://www.himss.org/asp/ContentRedirector.asp?ContentId=65250
17
Healthcare Information and Management Systems Society (HIMSS). (2007). 2007 HIMSS
18
Nursing Informatics Survey. Accessed at
19
http://www.himss.org/content.files.surveyesults/2007Nursing informatics.pdf., July 9,
20
2007Milholland, K. (2000). Telenursing, telehealth, nursing and technology advance
21
together. Geneva, Switzerland: International Council of Nurses.
22
23
24
Hendrickson, G. (1990) How do nurses use their time? Journal of Nursing Administration Mar;
20(3): 31-8.
International Medical Informatics Association (2006). IMIA Code of Ethics for Health
25
Information Professionals. Retrieved on October 17, 2006 from
26
www.imia.org/English_code_of_ethics.html
27
28
29
30
31
32
33
34
IOM (2001). Crossing the Quality Chasm: A New Health System for the 21st Century.
Washington, D.C.: National Academies Press.
IOM (2004). Health Professions Education: A Bridge to Quality. (report -descriptive).
Washington, DC.
Jiang, W., Chen, W., & Chen, Y. (2004). Important computer competencies for the nursing
profession. Journal of Nursing Research, 12(3), 213-225.
Jinks, AM. (2000) What do nurses do? An observational survey of the activities of nurses on
acute surgical and rehabilitative wards. Journal Nursing Manage 2000 Sep;8(5); 273-9
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
76
1
2
Jydstrup, R.A., & J.J.Gross. (1966) Cost of information handling in hospitals. Health Services
Research 1(3): 235-271.
3
Keyboard (2007). URL: (http://www.thinkgeek.com/computing/input/8193/). Accessed 2/14/07.
4
Marin, H. F. (2005). Nursing informatics: Current issues around the world. International Journal
5
6
7
8
9
of Medical Informatics, 74, 857-860.
McCormick, K. et al., (2007). Guideposts to the future – An agenda for Nursing Informatics.
JAMIA, 14(1), 19-24.
McNeil, B. J., Elfrink, V. L., Pierce, S. T., Beyea, S. C., Bickford, C. J., & Averill, C. (2005).
Nursing informatics knowledge and competencies: A national survey of nursing
10
education programs in the United States. International Journal of Medical Informatics,
11
74(11-12), 1021-1030.
12
McNeil, B. J., & Odom, S. K. (2000). Nursing informatics education in the United States:
13
proposed undergraduate curriculum. Health Informatics Journal, 6, 32-38.
14
Michaelsen, M., Fink, L, Knight, A. (2007) Team Based Learning: the Power of Teams for
15
Powerful Learning. URL: http://www.ou.edu/idp/teamlearning/. Accessed February 14,
16
2007.
17
18
Milholland-Hunter, K. (2001). International professional standards for telenursing programmes.
Geneva, Switzerland: International Council of Nurses.
19
MIT, (2007). One laptop per child. URL: http://www.laptop.org/. Accessed January 22, 2007.
20
National Council of State Boards of Nursing. (2003). The National Council of State Boards of
21
Nursing Position Paper on Telenursing: A Challenge to Regulation. URL
22
http://www.ncsbn.org/pdfs/TelenursingPaper.pdf [accessed 2006 February 28]
23
National League for Nursing. (2005). Core Competencies of Nurse Educators© With
24
Task Statements. Retrieved December 4, 2006 from
25
http://www.nln.org/profdev/corecompetencies.pdf
26
National League for Nursing. (2005). Task Group on Informatics Competencies.
27
Retrieved December 4, 2006 from
28
http://www.nln.org/aboutnln/AdvisoryCouncils_TaskGroups/informatics.htm
29
National Library of Medicine. (2006). Unified Medical Language System. URL
30
http://www.nlm.nih.gov/research/umls [accessed 2006 February 28]
31
32
Nelson, R. & Ball, M. Eds. (2004) Consumer Informatics: Applications and Strategies in Cyber
Healthcare (pp. 151). New York: Springer Verlag
33
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
77
1
2
3
Nelson, R. & Joos, I. (1989, Fall). On language in nursing: From data to wisdom. PLN Vision.
p. 6.
Nelson, R., Meyer, L., Rizzolo, M.A., Rutar, P., Proto, M.B., & Newbold, S. (2006). The evolution
4
of educational information systems and nurse faculty roles. Nursing Education Perspectives.
5
September/October 2006 27(5), 189-195.
6
7
8
9
10
11
12
Newbold, Susan K. (2006). Nursing Informatics Database- Job Titles as of January 17, 2006.
Electronic correspondence. Email to snewbold@umaryland.edu.
Norrie, P. (1999) The parameters that cardiothoracic intensive care nurses use to assess the
progress or deterioration of their patients. Nursing Critical Care ; 4(3): 133-7.
Norrie, P. (1997). Nurses' time management in intensive care. Nursing Critical Care May-Jun;
2(3): 121-5.
Oregon Health & Science University Biomedical Informatics Distance Learning Course
13
(2006). Retrieved December 1, 2006 from
14
http://www.amia.org/10x10/partners/ohsu
15
Remote Presence, (2007). URL:
16
http://www.cisco.com/application/pdf/en/us/guest/netsol/ns554/c647/cdccont_0900aecd8040
17
73a3.pdf. Accessed 2/14/07
18
Saranto, K. & Leino-Kilpi, H. (1997). Computer literacy in nursing; developing the information
19
technology syllabus in nursing education. Journal of Advanced Nursing, 25, 377-385.
20
21
22
23
24
25
26
27
28
29
30
31
32
33
34
Sensmeier, J, West, L., & Horowicz, J. K. (2004). Survey reveals, role, compensation of nurse
informaticists. Computers, Informatics, Nursing 22(3): 171, 178-81.
Staggers, N., & Gassert, C. (2000). Competencies for nursing informatics. In B. Carty (Ed.),
Nursing informatics: Education for practice (pp. 17-34). New York: Springer-Verlag.
Staggers, N., Gassert, C. A., & Curran, C. (2001). Informatics competencies for nurses at four
levels of practice. Journal of Nursing Education, 4(7), 303-316.
Staggers, N., Gassert, C., & Curran, C. (2002). A Delphi study to determine informatics
competencies for nurses at four levels of practice. Nursing Research, 51(6), 383-390.
Staggers, N, & Lasome, C. F. (2005). RN, CIO: An executive informatics career. Computer,
Informatics, Nursing 23(4): 201-6.
Staggers, N., & Thompson, C. B. (2002). The evolution of definitions for Nursing Informatics: A
critical analysis and revised definition. JAMIA, 33(1), 75-81.
Stanford University Graduate School of Business. (2005). Moore’s Law. Commentary by H.
Mendelson. URL http://www.thocp.net/biographies/papers/moores_law.htm [accessed 2006
February 28]
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
78
1
2
Starren, J., C. Tsai et al. (2005). The role of nurses installing telehealth technology in the home.
Computers, Informatics, Nursing 23(4): 181-9.
3
TIGER (2006). TIGER- Technology Informatics Guiding Educational Reform summit: Evidence
4
and Informatics Transforming Nursing. Bethesda, MD. Web site accessed September
5
13, 2007 from http://www.tigersummit.com/.
6
7
8
9
10
11
Turley (1996). Toward a model for nursing informatics. Image: Journal of Nursing Scholarship
Winter; 28(4): 309-13.
U.S. Congress. (1996). Health Insurance Portability and Accountability Act of 1996. Public Law
No. 104-191:Washington, D.C.: United States Congress; 1996.
URL http://thomas.loc.gov/cgi-bin/bdquery/z?d104:HR03103:|TOM:/bss/d104query.html
[accessed 2006 February 28]
12
U.S. General Services Administration Office of Governmentwide Policy, IT Accessibility &
13
Workforce Division (ITAW). (2006). Section 508. URL http://www.section508.gov
14
[accessed 2006 February 28]
15
U.S. Office for the Advancement of Telehealth. (2003). 2001 Report to Congress on
16
Telemedicine. URL http://telehealth.hrsa.gov/pubs/report2001/intro.htm [accessed 2006
17
February 28]
18
19
20
21
Wearable Computing, (2007a). URL’s http://www.osnf.com/p_smart.html;
http://www.media.mit.edu/wearables. Accessed 24 Jan 2007.
Wearable Computing (2007b). URL: http://www.microoptical.net/Products/medical.html.
Accessed 2/14/07.
22
Willson, D., Bjornstad, G., Lussier, J., Matney, S., Miller, S., Nelson, N., Neiswanger, M., Pinto,
23
K., & Thompson,C. (2000). Nursing informatics career opportunities. In Carty, B. (ed).
24
Nursing Informatics: Education for Practice. NewYork: Springer.
DRAFT Nursing Informatics: Scope and Standards of Practice-9-13-07
©American Nurses Association
79