Malignant Hyperthermia
advertisement

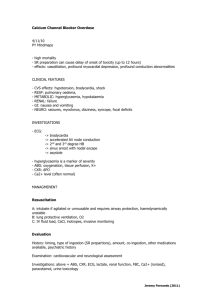
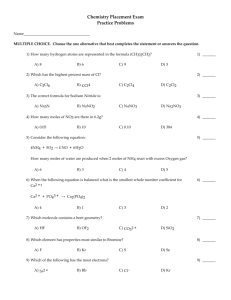
Jennifer Chen Cluster 8 Malignant Hyperthermia Abstract A patient, waiting to undergo his cardiac surgery, is lying on a surgical platform. An anesthesiologist enters the surgical room and injects some general anesthetics into the patient’s bloodstream. The patient appears normal until after a few minutes, the patient suddenly experiences increasing body temperatures leading to a high fever, muscle rigidity, and increased heart rate. The anesthesiologist is perturbed, runs out of the surgery room, and alerts the surgical staff of the patient’s alarming symptoms. The surgical staff identifies the symptoms as Malignant Hyperthermia. What exactly is Malignant Hyperthermia and how is it caused? Malignant Hyperthermia, a rare skeletal muscular disease found in humans, pigs, horses, and many other animals, is a channelopathy caused by abnormal calcium channels. This paper serves to investigate the problems within the specific ion channels known to cause the disease. The goal of the paper is to understand more about Malignant Hyperthermia and about how particular ion channels associated with the disease operate. Learning about the chemistry behind the disease is crucial in order to prevent future occurrences of Malignant Hyperthermia and to design new treatments. Introduction Malignant hyperthermia is a fatal, inherited disorder that affects less than 200,000 people in the United States. [1] As mentioned in the abstract, Malignant Hyperthermia is channelopathy, or a disease caused by mutations in channel protein genes. Malignant Hyperthermia is triggered by anesthetics, which includes common inhalants, and by medication containing succinylcholine, a substance often used as a muscle relaxant in emergency medicines. [2] After the initial trigger, life-threatening symptoms ensue. These symptoms include overly active metabolism in skeletal muscles, muscle contraction and rigidness, rising body temperature, and difficulty removing carbon dioxide from the body. [2] Temperature can rise 1 C for every 5 minutes; hence, the word hyperthermia is included in disease’s name. [3] If not treated immediately, death is a possible consequence. Before we discuss the causes of malignant hyperthermia, we must first understand some background information about calcium ion channels and the path the calcium ions involved travel during muscle contraction. For this process, refer to figure 1. First, an action potential (nerve impulse) from a sodium/potassium channel is triggered. [4] The action potential reaches the T-tubule. [4]. The T tubule (traverse tubule) is a deep fold of the cell Figure 1 [9] membrane that contains many L-type calcium channels (also known as Dihydropyridine receptors). [6] L-type calcium channels are voltage-gate channels that regulate the flow of Ca2+. [6] The action potential causes an electrical difference near the L-type calcium channels and activates them. [3] As a result, the L-type calcium channels open and allow Ca2+ ions to flow into the cell. Notice from figure 1, there is a gap between the T tubule and the sarcoplasmic reticulum, a type of smooth endoplastic reticulum organelle involved in pumping calcium ions and is a storage room for the Ca2+ ions. [4] How can Ca2+ ions cross this gap? Studies show that the L-type calcium channel contains many subunits, as seen in figure 2. One particular subunit, the α1, is very close to the sarcoplasmic reticulum membrane at various areas, known as triads, where there is only Figure 2 [10] a gap of approximately 120 A. [3] These triad regions contain “foot processes” that joins the T tubule to the sarcoplasmic reticulum. [3] The foot processes are composed of 4 Ltype calcium channels (or dihydropyridine receptors) paired with 1 Ryanodine receptor (RYR1). [3] (refer to figure 3 to see the foot processes; only 2 dihydropyridine receptors instead of 4 are shown for more clarity) Figure 3 [3] Through these foot processes, the Ca2+ ions reaches the Ryanodine Receptor, causes the RYR1 to activate and release the Ca2+ stored inside the sarcoplasmic reticulum. From there, the calcium ions continue to proteins such as actin and myosin, which interact to ultimately allow muscle contraction. Results One cause of Malignant Hyperthermia has been linked to a mutation in the RYR1 gene. [3] The RYR1 is a ligand-gated calcium channel located in the membrane of the sarcoplasmic reticulum. Ryanodine receptors, like other known ion channels, are gates, controlling the movement of Ca2+ ions across the membrane. The ligand for RYR1 is cytosolic (meaning inside the cell) Ca2+. [3] Scientists believe there are two binding sites on the RYR1, one that is a “high-affinity site that induces channel opening and a lowaffinity site which inhibits the channel.” [3] The high-affinity site is know as the activation site and the low-affinity site is known as the inhibit ion site. [4] The exact location of these sites is undetermined. There are two sides to the ryanodine receptor: a cytoplasmic side and a luminal side. (Refer to figure 4) The structure of RyR1 is similar to a clover with four repeating parts. (Figure 4). [3] Figure 4 [6] provided by Terrence Wagenknecht, from Wadsworth Center, NY State Dept. of Health Scientists are able to study the disease through pigs, which have been found to also have malignant hyperthermia. The disorder in pigs is called porcine stress syndrome (PSS). [3] Because human research is difficult to undertake, many researchers are looking at PSS pigs. Evidence from experiments show that PSS is a result of a mutation that involves a substitution of arginine to cysteine at point 615 on the RYR1 gene. [3] In humans, there are approximately 30 mutations, including the Arg615Cys substitution, that can occur on the RYR1 gene. [5] However, how these mutations alter the ryanodine channel is unknown. We do know that the symptoms of the disease are due to excess levels of Ca2+ ions released from the sarcoplasmic reticulum inside skeletal muscle cells. [4] When a person with Malignant Hyperthermia receives general anesthetics, a sudden and great amount of Ca2+ ions is released. Ca2+ ions are involved in both metabolism ad muscle contraction. [3] As a result, an overflow of Ca2+ ions would cause muscle contraction and increased body metabolism. We now face a more difficult question: How do mutations in the ryanodine channel cause it to release so much excess Ca2+? From more recent studies, scientists have found that in PSS pigs, the “rate and extent” [3] of Ca2+ released by ryanodine receptors is higher than compared to pigs that do not have PSS. In addition, the channels open longer and close shorter, thus causing a large amount Ca2+ ions being released. [3] In mutant RYR1, general anesthetics can increase the affinity for cytosolic Ca2+ to bind onto A- sites more, while at the same time decrease the affinity for cytosolic Ca2+ to bind onto I- sites even more. Figure 5 (Refer to figure 5) [4] Some studies propose that cytosolic Mg2+ is a factor in the whole process. Cytosolic Mg2+ ions are believed to be able to bind onto either the A-site or the I-site to inhibit the RYR1. [4] By binding onto the A-site, the cytosolic Mg2+ blocks cytosolic Ca2+ ions from binding onto the A-site. By binding onto the I-site, the cytosolic Mg2+ can inhibit the ryanodine receptor directly. A mutated RYR1 channel seems to have lower attraction for the cytosolic Mg2+. [4][7] Refer to figure 5 for an illustration of differences between affinities of cytosolic Ca2+ cytosolic Mg2+ in normal and mutant RYR1. Therefore, there may possibly be some sort of chemical structure change in the channel to cause such a reduced attraction. As a result, the mutant RYR1 is less inhibited and more than normal amounts of Ca2+ ions can be released. However, this explanation is contradictory because several studies have shown that there is no decreased attraction with Mg2+ – that mutated RYR1 and normal RYR1 have similar affinities. Another study proposed that Malignant Hyperthermia is a result of a process that the researches called “store overload-induced Ca2+ release”. [8] This phrase basically describes the process of when the sarcoplasmic reticulum contains an overload of Ca2+ ions, Ca2+ ions will be spontaneously released. [8] While previous studies mentioned before focused on cytosolic Ca 2+ ions, this study focused on luminal Ca2+ ions. The researchers discovered that in mutated Arg615Cys ryanodine receptors, the threshold needed for luminal Ca2+ ions to activate the ryanodine receptor is lower. [8] The activation of the ryanodine receptors leads to the “store overload-induced Ca2+ release” process. [8] Therefore, in RYR mutated receptors, the “store overload-induced Ca2+ release” [8] process would be more likely to occur compared to normal RYR1. [8] The study furthermore found that general anesthetic further reduced the threshold needed for luminal Ca2+ ions to activate the ryanodine receptors even more. [8] Thus, the “store overload-induced Ca2+ release” process is even more likely to occur and in turn, more Ca2+ ions are released. [8] Conclusion Malignant Hyperthermia is a complicated disease that even today, scientists cannot understand the complete molecular processes behind the ryanodine receptor. So far, we know that the disease is caused by mutations in the RYR1 gene that cause the receptor to release more than normal amounts of Ca2+ ions. However, we still face countless other questions such as exactly how is the ryanodine receptor altered by such a mutation and how do general anesthetics trigger the symptoms. Scientists must answer these pivotal questions necessary for the understanding of the disease first. Once we have answered these questions, we will have more hope of generating a better treatment or even cure for Malignant Hyperthermia. Acknowledgements I would like to thank my chemistry professor, Toby Allen, for providing me the inspiration to research about ion channels. I also thank chemistry professors Dean Tantillo and Tim Patten for channeling your chemistry knowledge to me. I want to also thank teacher fellow, Matt Peck, for providing advice and editing my paper. Also, I would like to thank Clarabelle Cheng-Yue for proofreading my research paper. Bibliography [1] "Prevalence and Incidence of Malignant hyperthermia." Wrong Diagnosis. 2008. Adviware Pty Ltd. 27 Jul 2008 <http://www.wrongdiagnosis.com/m/malignant_hyperthermia/prevalence.htm>. [2] "Malignant hyperthermia." Wikipedia. 12 July 2008 . Wikimedia Foundation, Inc., . 27 Jul 2008 <http://en.wikipedia.org/wiki/Malignant_hyperthermia>. [3] Ashcroft, Frances. Ion Channels and Disease . San Diego: Academic Press, 2000. [4] "Muscle Contraction" Wikipedia. 12 July 2008 . Wikimedia Foundation, Inc., . 27 Jul 2008 <http://en.wikipedia.org/wiki/Muscle_contraction>. [5] “López, José, Nancy Linares, Isaac N. Pessah, and Paul D. Allen. "Enhanced response to caffeine and 4-chloro-m-cresol in malignant hyperthermia-susceptible muscle is related in part to chronically elevated resting [Ca2+]i ." MUSCLE CELL BIOLOGY AND CELL MOTILITY 28810 Nov 2004. 27 Jul 2008 <http://ajpcell.physiology.org/cgi/content/abstract/288/3/C606>. [6] Diwan, Joyce J. "Biochemistry of Metabolism." Ca++ Signals. 2007. 29 Jul 2008 <http://www.rpi.edu/dept/bcbp/molbiochem/MBWeb/mb1/part2/casignal.htm>. [7] Laver, D R, V J Owen, P R Junankar, N L Taske, A F Dulhunty, and G D Lamb. "Reduced inhibitory effect of Mg2+ on ryanodine receptor-Ca2+ release channels in malignant hyperthermia." Biophys J. 73(4) Oct 1997 29. Jul 2008 <http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=1181092>. [8] Jiang, Dawei, Wenqian Chen1, Jianmin Xiao, Ruiwu Wang, Huihui Kong, Peter P. Jones, Lin Zhang, Bradley Fruen, and S. R. Wayne Chen. "Reduced Threshold for Luminal Ca2+ Activation of RyR1 Underlies a Causal Mechanism of Porcine Malignant Hyperthermia." J. Biol. Chem. Vol. 283, Issue 3025 July 2008. 29 Jul 2008 <http://www.jbc.org/cgi/content/full/283/30/20813#SEC3>. [9] Korf, Bruce R. "Korf Genetics." Human Genetics and Genomics . Blackwell Publishing. 29 Jul 2008 <http://www.blackwellpublishing.com/korfgenetics/figure.asp?chap=16&fig=Fig16-2>. [10] Millar, 2007. Cerebrospinal Fluid Research. 29 Jul 2008 <http://www.cerebrospinalfluidresearch.com/content/4/1/8/figure/F2?highres=y>.