The case - Crain's Detroit Business
advertisement

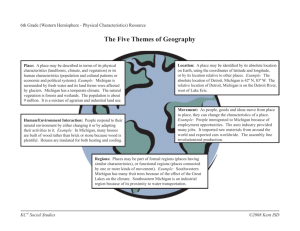
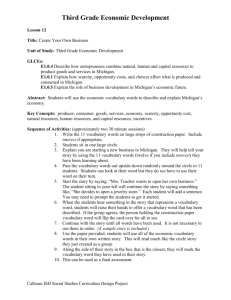
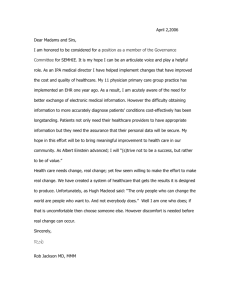
20090302-NEWS--0001-RG1-CCI-CD_-- 2/25/2009 3:32 PM Page 1 CRAIN’S DETROIT BUSINESS March 2, 2009 Page E1 Extra Physician groups split over online information networks, Page E5. Monthly news for health care professionals People Richard Reynolds has been appointed surgeon-in-chief by Children’s Hospital of Michigan. He had been chief of orthopedic surgery. Reynolds joined Children’s in 2006 from Children’s Hospital Los Angeles. Ruben Gomez has joined the staff at Detroit Receiving Hospital as a surgeon. Gomez specializes in burn surgery and will be a member of the hospital’s burn center team. He previously was a civilian burn surgeon, Institute of Surgical Research Burn Unit, at the Brooke Army Medical Center, Fort Sam Houston, in San Antonio, Texas. Andrew Konski has been named chairman of the Department of Radiation Oncology for the Wayne State University School of Medicine and service chief for radiation oncology at the Konski Barbara Ann Karmanos Cancer Center. Konski had been chief medical officer for the partners’ program at Fox Chase Cancer Center, Philadelphia. Alexa Simkow has joined Botsford Hospital, Farmington Hills, as surgical services nursing director. She comes from St. Vincent Medical Center, Toledo, where she was administrative director of Simkow perioperative services. She also was a 17-year employee of Henry Ford Health System. Oakwood Healthcare System has appointed Timothy Sell chief of cardiothoracic surgery. Oakwood also named Eric McBride administrator of its oncology service line; he continues to oversee the Sell cardiovascular service line. Also, Lisa Rutledge, corporate director of community outreach, assumes responsibility for the Center for Exceptional Families and Pediatric Rehab Program. Ambika Mathur, professor in the Wayne State University School of Medicine Department of Pediatrics, has been appointed assistant dean for combined degree programs and postdoctoral affairs. Antoinette Wozniak, president of the medical staff for the Barbara Ann Karmanos Cancer Center, has been named associate center director for education. She will step down as leader of the thoracic multidisciplinary team. She will be replaced in that position by Shirish Gadgeel. Also, Cassann Blake was named team leader of the breast multidisciplinary team and Zeina Naleh was named coleader. The case for reform MICHIGAN PERSPECTIVES Here are two prescriptions for health care reform: Nancy Schlichting: Universal coverage with delivery focused on primary care and incentives aligning health care providers. Michigan’s health care leaders say need is clear, but key questions are how and when Dr. Gregory Forzley: Universal coverage that rewards physicians for quality care, focuses on wellness and expands electronic medical records. NATIONAL PLANS BY JAY GREENE Here’s what major U.S. health care reform proposals would provide: WydenObama Baucus Bennett CRAIN’S DETROIT BUSINESS Most Michigan hospital, physician, insurance Employer “pay or play” mandate Yes Yes No* and business leaders are ready for comprehenExclude small employers Yes Yes NA sive health care delivery and financing reform. A consensus is emerging in Washington and Health insurance pool/exchange Yes Yes Yes among health care practitioners and executives Individual coverage mandate Child Yes Yes in Michigan for universal coverage and the goal Expand Medicaid and SCHIP Yes Yes Yes* that everyone should have a basic set of health benefits. Medicare buy-in at age 55 No Yes No Universal coverage means providing health inUniversal coverage Phased Yes Yes surance — either government sponsored or privateImprove primary care Yes Yes Yes ly purchased — to the 46 million uninsured Americans, including 1.1 million in Michigan. Another 25 Enhance IT, training programs Yes Yes Yes million are underinsured, for a total of 71 million Single-payer No No No people — or 40 percent of adults under age 65 — needRetaining private insurance Yes Yes Yes ing basic or expanded coverage. Prohibit denial of pre-existing conditions Yes Yes Yes More than half of Michigan’s uninsured live in metro Detroit and rely on hospital emergency dePrivate delivery system Yes Yes Yes partments and free clinics for health care services. Cost controls Yes Yes Yes Some of the working uninsured use cash or credit Tax credits Yes NA Yes cards to pay when they need health care. While many are charged higher prices, hospitals and docNOTES: *Employer-based health insurance system eventually phased out under Wyden-Bennett plan. A new, state-based private insurance pool system would be tors write off much of the unpaid cost as bad debt, created. Medicaid and the State Children’s Health Insurance Program (SCHIP) would which ends up as a hidden tax on individuals and be included in the insurance pools that would offer group coverage. companies who pay for insurance. Sources: Web sites for President Barack Obama But the hard part about reforming the health care (www.barackobama.com/issues/healthcare/index.php); Sen. Max Baucus, Dsystem is paying for it. Montana, chairman Senate Finance Committee (finance.senate.gov/healthreform2009/finalwhitepaper.pdf); Rep. Ron Wyden, D-Ore., Estimates range from $100 billion to $150 billion to and Rep. Robert Bennett, R-Utah (www.govtrack.us/congress/bill.xpd?bill=s110-334); provide universal coverage, although some MichiS.B. 334. gan health care leaders believe there is enough money in the system if it were spent more wisely. For the past five years, U.S. Rep. John Conyers, DMore than 100 health care reform plans have been Mich., has sponsored H.R. 676, the United States Naproposed or suggested. Some federal legislation has tional Health Insurance Act, which would create a been introduced for universal government-funded, singlecoverage, including the Healthy payer system that would Americans Act, or S.B. 334, by cover everyone. The proSens. Ron Wyden, D-Ore., and gram would eliminate the Robert Bennett, R-Utah. private health insurance More legislation is expected system. in Washington and at the state Rejected by Michigan level in Michigan this year. leaders also is the idea to Aside from supporting uniprovide tax incentives and versal coverage, Michigan’s health savings accounts to leaders agree on another thing: increase coverage. This A proposal to create a singleconcept was put forth by payer system that would do former President Bush and away with the employer-based most recently by Sen. John and private insurance system, McCain, R-Ariz. similar to government systems On the other hand, in European countries and Michigan leaders like PresDaniel Loepp, Canada, is unworkable in AmerBlue Cross Blue Shield of Michigan See Reform, Page E2 ica. we are doing now “isWhat inefficient, with 46 million uninsured. It is a very poor way to do business. ” 20090302-NEWS--0002-RG1-CCI-CD_-- 2/25/2009 3:30 PM Page 1 Page E2 March 2, 2009 CRAIN’S DETROIT BUSINESS Health Care Extra Reform: State health care leaders say key questions are how, when ■ From Page E1 ident Barack Obama’s goal of universal coverage and preserving the employer-based health insurComparing proposed health care reform plans by industry associations: ance system. AHIP AMA AHA Obama’s plan, which has not Employer “pay or play” mandate No No Yes been formally proposed as legislation, would mandate that large Exclude small employers Yes NA No and medium-sized employers covNational insurance pool/exchange No Yes No er workers. If employers do not ofTax credits to purchase insurance Yes Yes No fer coverage, companies would be required to pay a 4 percent payroll Individual coverage mandate Yes No* Yes tax. Expand Medicaid and SCHIP Yes Yes Yes Obama would then use the payMedicare buy-in at age 55 No No No roll taxes to expand coverage by subsidizing health insurance in a Universal coverage Yes Yes Yes national health insurance exImprove primary care Yes Yes Yes change. People could select private Enhance IT, training programs Yes Yes Yes plans or a new publicly operated Single-payer No No No insurance program. The program could reduce the number of uninRetaining private insurance Yes Yes Yes sured by 25 million people, experts Prohibit denial of pre-existing conditions Yes Yes** Yes say. Private delivery system Yes Yes Yes But Obama’s plan and most other major health care proposals, inCost controls Yes Yes Yes cluding ones presented by nationNOTES: al trade groups such as the * No, but those with means have coverage responsibility. American Hospital Association, the ** Yes, for those continuously (or already) insured. American Medical Association and Sources: America’s Health Insurance Plans, American Medical Association, American America’s Health Insurance Plans, Hospital Association also argue that aggressive efforts need to be made to reduce costs and directing incentives for high- in this country. It was built ham Farms, said physician organier quality. around Medicare and Medicaid 40 zations should be given incentives There is no doubt, however, that years ago and relies on employer- to improve quality and the chance financing this type of health insur- based tax credits,” Schlichting to implement best practices that ance expansion would initially said. “Employers are challenged to will reduce health care costs. cost taxpayers billions of dollars pay for it because costs are up and “I don’t think the status quo is and add to an already off-the-chart we reward the wrong things.” fine,” said Grant. “Everybody federal budget deficit. Schlichting said she favors uni- wants to cover the uninsured. You So how can health care reform versal coverage with a delivery can’t argue with that, but that be achieved, and how soon? system focused on primary care won’t solve the problem.” “What we are doing now is inef- and incentives that align hospiWhile experts talk about imficient, with 46 million unin- tals, physicians and other health proving quality, physicians are on sured. It is a very poor way to do care providers. the front lines trying to deliver business,” said Daniel Loepp, Dr. Gregory Forzley, chairman quality health care everyday, CEO of Blue Cross Blue Shield of of the Michigan State Medical Soci- Grant said. Michigan. ety, also agrees with the premise of “In the back rooms, people are “Hospitals are struggling to take universal coverage, but said com- talking about costs, not quality,” care of the unemployed,” Loepp prehensive reform could take up Grant said. “We have a $2 trillion said. “The whole notion of uncom- to two years. annual health care bill, and it is pensated care is not sustainable In the medical society’s 2006 Fu- going up 10 percent a year. We over the long ture of Medicine have to tackle those costs first, and term. We have report, Forzley physician organizations have the got to find a sussaid reform also ability to root out waste and duplitainable way to must reward cation and drive down costs.” cover everyphysicians for Grant said health care reform body.” providing safe, won’t work unless doctors change Loepp, who quality care; focus their behavior. also chairs the on prevention and “Until we get to the point when health policy wellness; fund an we order fewer (diagnostic tests committee of the expansion of elec- such as magnetic resonance imagChicago-based tronic medical ing), costs will continue to rise,” Blue Cross Blue records; and en- he said. Shield Association, courage coordiGeorge, chairman of the Senate favors preservnated care among Health Policy Committee, said he ing the employerproviders with wants Michigan to move forward based health inmore patient in- with its own health care reform surance system. volvement. plan that focuses on covering the The association “As we reform uninsured and addressing inrepresents 39 the health care equalities of the employer-based Blues’ plans namarket, we want system and individual market. Sen. Tom George, tionally, includto simplify bene“I don’t think we should fall in R-Kalamazoo ing the Michigan fits and product the trap of waiting for the debate Blues. Like the Blues’ and AHIP’s design so it is easier for patients at the federal level,” said George, plans, Loepp believes there should and doctors,” Forzley said. “We who recently announced he will be mandated coverage, but only need a patient-centered medical run for governor. “States can when it is linked to a guaranteed home and reform of the reimburse- make inroads, and Michigan community rating. Under commu- ment system. The incentives are should be discussing it.” George said he will hold a series nity rating, sicker people do not wrong.” At least two other physician of health policy hearings this year pay higher premiums than leaders, Dr. Steven Grant and state to discuss various state approachhealthy people. Nancy Schlichting, CEO of Henry Sen. Tom George, R-Kalamazoo, es to developing a basic set of beneFord Health System and chair of the an anesthesiologist, believe in an fits and coming up with a funding Michigan Hospital & Health Associa- incremental approach to health plan. Work groups will be created to discuss affordability and accestion in Lansing, said the cost of care reform. Grant, chairman of United Physi- sibility of insurance. health care has become unaffordcians, a 2,000-physician indepen“I hope a proposal comes out of able for too many people. “We have a very strange system dent practice association in Bing- that, a Michigan solution,” he said. WHERE THE INDUSTRY STANDS I don’t think we “ should fall in the trap of waiting for the debate at the federal level. ” Gary Faja, Trinity Health’s East proach to coverage,” Halladay Michigan regional executive and said. “We could cover all 160,000 CEO of St. Joseph Mercy Health Sys- uninsured children in Michigan if tem in Ann Arbor, said there is we put the State Children’s Health enough money in the system to Insurance Program funds, Medicaid dollars and (a private insurcover the uninsured. “It is just not allocated with the ance investment) into a pool … right incentives,” Faja said. and have people pay according to “Rather than incent with number their ability.” of procedures, you incent on qualiHalladay said a public-private ty procedures.” partnership to cover the uninIn 2007, Trinity developed a sured is the way to go. health care reform plan with nine In her annual State of the State essential elements for change. Its speech in January, Gov. Jennifer plan matches up best with the Granholm said the federal stimuWyden-Bennett plan, but Faja said lus package approved last month Trinity hasn’t endorsed that plan. by Congress will help Michigan Trinity’s elements include uni- “move further and faster into a versal, continuous coverage; better future.” broad pooling of insurance risk; The National Governors’ Associaaligning payment incentives to co- tion appointed Granholm co-chair ordinate care; use of health infor- of a bipartisan group to make recmation technology; maintaining ommendations to the Obama adhealing relationships with pa- ministration on health care retients; and a special emphasis on form. those at the end of life. “We must have affordable, acOne way to save money is to re- cessible health care for all Ameriduce the variation of care that ex- cans,” she said. ists in different parts of the counFaja predicted that several try, he said. health care bills will be introduced “There is a huge variation. You this year, but the federal govern(smooth things over) with evi- ment will take an incremental apdence-based protocols,” Faja said. proach to reform. Comprehensive Health care researcher Marireform will take several years beanne Udow-Phillips, director of cause of political and economic rethe Center for Healthcare Research alities, he said. and Transformation in Ann Arbor, Schlichting said the stimulus said costs will continue to rise unpackage is the first step toward less the system is overhauled. “The U.S. spends more money health care reform. But how per capita than any other country Michigan uses its estimated $3 bilin the world, but most health sta- lion will determine how many immediate benefits tistics put us just accrue to Michiabove Cuba on gan, she said. critical measures “There are a like life expectannumber of feacy and infant tures in the packmortality,” Udowage for improved Phillips said. “We are paying more access: (expanded and getting less children’s health than many other insurance), Medcountries.” icaid dollars, inAccording to creasing COBRA the Commonwealth benefits, and Fund, the United funds for inforStates is last out mation technoloof 19 industrialgy,” Schlichting ized nations when said. it comes to health Unlike in the Marianne Udow-Phillips, care quality. The Center for Healthcare Research early 1990s, when Congressional Budpowerful specialget Office estiinterest lobbying groups derailed mates that one-third of the $2.3 trilhealth care reform proposed by lion annually spent on health care, then-President Bill Clinton, there or 16 percent of the U.S. economy, does not improve Americans’ is widespread support for massive change. health outcomes. Loepp acknowledged that in the Udow-Phillips said improvements must be made on the deliv- past, the insurance industry has ery side through increased use of been “more obstinate than I would evidence-based guidelines, more like” toward health care reform. involvement of patients in deci- Over the past two years, he said, sion-making, better dissemination there has been a change in attitude of quality measures and more inte- among health insurance executives. gration of care. “There is a conclusion we can’t “We must have improvements to the financing side — funding for sit by the sidelines. We need to be universal coverage, strong incen- reasonable and compromise,” he tives for cost control and con- said. Schlichting said that for the sumer protections,” she said. Doug Halladay, director of Michigan first time, she believes there is Cover the Uninsured Network, said cover- hope for health care reform. “Do I have a crystal ball to know ing the state’s uninsured will require a plan to stabilize rising health care how soon it will happen? The decosts, and to emphasize prevention bate is very important. If we don’t debate, it won’t happen,” she said. and wellness. Jay Greene: (313) 446-0325, “I like Obama’s idea of a blend of options and a sliding scale ap- jgreene@crain.com We are paying “ more and getting less than many other countries. ” 20090302-NEWS--0003-RG1-CCI-CD_-- 2/25/2009 4:27 PM Page 1 March 2, 2009 CRAIN’S DETROIT BUSINESS Page E3 Health Care Extra MSMS priorities for ’09: Smoke-free workplaces, tort reform Julie Novak, 46, was appointed It was when I had to function withexecutive director of the Michigan out his support that I realized how State Medical Society in Lansing in much I had really learned from January after serving 10 months him and from all of my experias acting executive director. She ences. replaced Kevin Kelley, 52, You can never erase who died in January after the loss of someone like a long illness. him, and you feel even Novak joined the state more responsible for carmedical society in 1990 afrying on the mission that ter receiving a bachelor’s he so passionately bedegree in international lieved in: to help doctors relations in 1985 from care for the patients who Michigan State University need them. and a master’s of health What are your priorities services administration for 2009? in 1990 from the University At the end of last year, of Michigan School of Public we were very close to getHealth. Julie Novak, ting legislation to ensure Novak spoke with Jay Michigan State smoke-free workplaces. It Greene, editor of Crain’s Medical Society Health Care Extra. will remain a top legislative priority this year. We What was it like to take over for also will continue work to preKevin Kelly, who worked for the med- serve Michigan’s tort reforms. Acical society for 30 years, the last sev- cess to care for seniors and for the eral as executive director? most vulnerable Michigan citizens I worked with Kevin for 18 must be maintained through apyears, and he was a tremendous propriate funding for Medicare mentor to me and to so many oth- and Medicaid. ers. I’ve said before that if you Fighting inappropriate scope of meet one person like him in your practice expansion will be imporlifetime you are more than lucky. tant again this year. Education remains a core mission for us, offering our physicians courses on everything from practice management to scientific classes, from the autoworkers’ VEBA (Voluntary Employee Benefit Association for health care) to the patient-centered medical home. we seek to reform our health care system. Do Michigan’s doctors stand to gain under President Barack Obama’s health care reform plan? His plan calls for an expansion of Medicaid, Children’s Health Insurance Program and a large employer payor-play mandate to cover their workers What are the or chip into a nabiggest challenges tional insurance exfor Michigan’s docchange. tors? We all stand to Physicians gain if there is a want to provide way for more peoJulie Novak, the very best care ple to have coverMichigan State Medical Society for their patients, age. One of our and they work principles is to hard to stay curensure universal rent on medical treatments, but in coverage for essential benefits and the last two decades many other help make coverage options availrequirements have fallen to physi- able for all residents. There is a cians — understanding complex sense of urgency because employpayment rules, complying with an er-provided coverage is declining increasing number of state and with the poor economy. federal regulations and hiring and Does Blue Cross Blue Shield of managing larger numbers of adMichigan need a legislative fix to help ministrative staff. There is every reason to believe it in the individual market? We did not take a position on the there will be more complexities as We all stand to “gain if there is a way for more people to have coverage. ” individual market reform bills. We are committed to assuring that health insurance is accessible and affordable. While the case for stabilizing the individual insurance market may be compelling, it should not be done in isolation. Considerable attention should be given to the role that Blue Cross and other insurers have in assuring that any reforms have a tangible effect on the ability of individuals to purchase suitable coverage at an affordable price. How goes MSMS Connect, the electronic health information network the medical society launched last year to allow doctors to tap into a variety of health care data to more effectively coordinate patient care? We are in the early stages of describing MSMS Connect to our members and identifying those who are interested in being early adopters. It is clear that health plans and the federal government are increasing the call for information technology in medical practices, and this portal is meant to be an easy entry point for physicians to get started. 20090302-NEWS--0004-RG1-CCI-CD_-- 2/25/2009 Page E4 3:29 PM Page 1 March 2, 2009 CRAIN’S DETROIT BUSINESS Health Care Extra BOYDEN DETROIT ON ATTRACTING TALENT WITH THE HENRY FORD HEALTH SYSTEM “Right from the start the executive candidates Boyden “Our ability to recruit talented and sought-after leaders Detroit brought us were of the highest caliber and MVYV\YJSPLU[ZPZLUOHUJLKI`OH]PUNVMÄJLZ[OYV\NOV\[ L_[YLTLS`X\HSPÄLK¹ [OL<:HUKNSVIHSS`6\YSVJHSRUV^SLKNLVM4PJOPNHU»Z —9VILY[.9PUL`*OPLM6WLYH[PUN6MÄJLY HK]HU[HNLZPZPTWVY[HU[[VH[[YHJ[[VWL_LJ\[P]LZ>L Henry Ford Health System \UKLYZ[HUK`V\YI\ZPULZZHUK^LILSPL]LPU4PJOPNHU¹ /LUY`-VYK/VZWP[HS»Z:[H[LVM[OL(Y[:\YNPJHS:PT\SH[PVU*LU[LY —Jeff Evans, Boyden Detroit Partner Yaremchuk named to panel on ambulatory care practices Kathleen Yaremchuk, chair of otolaryngology-head and neck surgery at Henry Ford Hospital, has been appointed to serve as a member of the National Quality Forum’s steering committee for a project seeking to identify top ambulatory care practices using electronic clinical data. Yaremchuk The project will study quality measures for ambulatory care based on administrative data, enriched by laboratory and pharmacy data and other electronic clinical data. Funding is from Aetna Foundation, United Health Foundation, Cigna Foundation, Wellpoint Foundation and the Pacific Business Group on Health. Winston joins American College of Cardiology board of trustees global executive search. -FBSOIPX #PZEFO%FUSPJUDBOBUUSBDUUPQUBMFOUGPSZPV Call 248.258.0616. %PVH"MMFOt+FGG&WBOTt$ZE,JOOFZt#BSC4XBOt%BNJBO;JLBLJT /0ME8PPEXBSE"WFt#JSNJOHIBNt.*t tboydendetroit.com Stuart Winston, cardiologist at St. Joseph Mercy Health System’s Michigan Heart and Vascular Institute, has been named to the board of trustees of the American College of Cardiology for a five-year term beginning this month. Winston already had served as presiWinston dent of the Michigan chapter and on national committees dealing with quality of care and advocacy. He has been recognized for his work in coordinating Michigan hospitals’ efforts to improve door-to-balloon times for the treatment of myocardial infarction. Cardiac surgery quality project finds improved results A project of the Michigan Society of Thoracic and Cardiovascular Surgeons, Michigan hospitals and Blue Cross Blue Shield of Michigan is starting to facilitate improved outcomes in cardiac surgery and decreasing complications and costs in Michigan. The Cardiac Surgery Quality Collaborative was formed in December 2005 to advance cardiac surgery quality in the state. By collecting, sharing and analyzing patient and hospital outcomes, cardiac surgery team members have implemented process improvement plans based on their best practices to benefit all heart surgery patients in the state. Outcomes to date include: Increased use of the internal mammary artery graft for coronary bypass among seven cardiac surgery programs from 82.1 percent to 91.3 percent. A decrease in the number of patients requiring ventilator support for more than 24 hours postsurgery from 19 percent to 16.8 percent. Health Care Briefs UM Medical School seventh overall in NIH funding for 2008 University of Michigan Medical School doctors and biomedical scientists brought in $301 million in National Institutes of Health research funding in federal fiscal year 2008, ranking the school seventh overall and second among public university medical schools. The awards cover 712 grants to the medical school. Other areas of the university also receive NIH funding totaling $127 million. Nursing mag: Five state hospitals among top hospitals to work for Five Michigan hospitals were named among the “100 Top Hospitals to Work For” by Nursing Professionals, a magazine targeted at nursing students. The five are: William Beaumont Hospital, Royal Oak; Genesys Regional Medical Center, Grand Blanc; Henry Ford Hospital, Detroit; Spectrum Health, Grand Rapids; and University of Michigan Hospitals and Health Centers, Ann Arbor. More than 25,000 randomly selected hospital nurses were surveyed in early 2008 to measure their job satisfaction. Nurses were asked about flexible work arrangements, training and development, diversity and equality, and how strong the nursing voice is within the institution’s workforce. Cleveland Clinic adopts MedHub management system Ann Arbor-based MedHub Inc. has signed a contract with the Cleveland Clinic to deploy its enterprise residency management system across all residency and fellowship programs, graduate medical education and hospital finance. The system is a Web-based group of modules developed to improve communication, information workflow and reporting for physician training and residency program accreditation. The contract, which will involve nearly 5,000 users over 115 residency and fellowship programs, is one of MedHub’s largest installations. Covisint’s data-sharing network picked by Calif.-based initiative Detroit-based Compuware Corp. said its Covisint subsidiary will provide the VIP Health Initiative with a network for the secure sharing of patient information and improved physician collaboration. The Southern California-based initiative was formed by Scripps Mercy Physician Partners, SMPP Services and Physician Partners Management Services. 20090302-NEWS--0005-RG1-CCI-CD_-- 2/25/2009 3:28 PM Page 1 CRAIN’S DETROIT BUSINESS March 2, 2009 Page E5 Health Care Extra Physician groups split over online information networks BY JAY GREENE CRAIN’S DETROIT BUSINESS A rift has developed between the Michigan State Medical Society in Lansing and Bingham Farmsbased United Physicians over competing online health information networks the two organizations are now offering physicians. Last September, United Physicians unveiled its my1HIE information network in a partnership with two other doctor groups. A month later, the medical society announced its MSMS Connect online physician portal. Both systems have contracts with and use technology from Covisint, a subsidiary of Detroit-based Compuware Corp. “We are in competition, and it is confusing physicians,” said Dr. Steven Grant, CEO of United Physicians. But Dr. Gregory Forzley, chair of the medical society, said that while the two online systems — and the nine regional health information networks under development throughout the state — are somewhat different, they are also complementary. “My1HIE has a bigger package they want to offer to physicians,” said Forzley, who also is director of informatics at St. Mary’s Health Care in Grand Rapids. “There is some overlap, but doctors can decide what they want and pick what is best.” United Physicians has partnered with two other physician organizations in Southeast Michigan — Olympia Medical Services and Continuum Management Services, both located in Livonia — to develop my1HIE. Huron Valley Physicians As- are in “ We competition, and it is confusing physicians. ” Dr. Stephen Grant, United Physicians sociation in Ann Arbor joined my1HIE earlier this month. MSMS Connect and my1HIE each will allow participating doctors to use the Internet and their computers to retrieve patient insurance eligibility information, electronically order prescriptions and view lab results. The online health information exchanges are intended to help improve patient care by enhancing communication among doctors, hospitals, health plans and other providers. They also have the potential to save money by reducing duplicative tests and increasing quality. So far, about 700 of 4,000 doctors in the four groups are using Breast cancer linked to gene A specific gene may contribute to the reason Caucasian women have a higher incidence of breast cancer than Asian women, according to research conducted by the Wayne State University School of Medicine. The study, published in the Dec. 15 issue of Cancer Research, provides evidence than an allelic variation in the galectin-e gene may influence a woman’s risk for developing breast cancer. This is a form of the gene that appears more often in Caucasian women than in Asian women that is associated with breast cancer. If further studies support the research, it could lead to the development of drugs that target high-risk genes. Lead researcher: Avraham Raz, professor of pathology and radiation oncology. Additional researchers: Vitaly Balan, research associate; Pratima Nangia-Makker, assistant professor of pathology. UM advances cystic fibrosis fight Researchers at the University of Michigan may have found a way to kill the drug-resistant infections that kill people with cystic fibrosis: a superfine oil-and-water emulsion. The nanoemulsions are nontoxic in people but have successfully killed 150 tested “superbugs.” The results of the study were published in the January issue of Antimicrobial Agents and Chemotherapy. Lead researchers: John LiPuma, professor of pediatrics, University of Michigan Medical School, and James Baker Jr., director, Michigan my1HIE, and another 1,300 have signed licenses to use it, Grant said. About 85 are being added to the system each month. Since January, 100 physicians have signed up to use MSMS Connect, but the medical society may add several thousand doctors this year, said Ben Louagie, director of subsidiary operations for the medical society’s Physician Services Inc., a for-profit subsidiary. Forzley said the purpose of MSMS Connect is to offer a benefit to the association’s 16,000 members and allow them to use the online system on an “a la carte” basis. “We wanted to bring up fairly quickly a tool already developed for doctors by Covisint to give doctors e-mail and other resources (on the Internet),” Forzley said. Forzley said MSMS Connect can be used with physicians’ own practice management systems and other online services they purchase. “We offer (for sale) a number of modules for physicians, like a disease registry tool, quality controls and credentialing services,” Forzley said. “If you have existing services, our way to collaborate is that you don’t have to buy that from us. We can link that in.” But Grant has a few gripes with how the medical society is presenting its network to physicians. “We tried to work with the medical society to partner with them, Research Roundup Nanotechnology Institute for Medicine and Biological Sciences, and the study’s senior author. Additional UM authors: Sivaprakash Rathinavelu, Bridget Foster, Jordan Keoleian, Paul Makidon, and Linda Kalikin. Funding: T. Carroll Haas Research Fund for Cystic Fibrosis, Cystic Fibrosis Foundation, National Institutes of Health, NanoBio Corp. Urinary incontinence treatment William Beaumont Hospital is researching urinary incontinence treatment using the patient’s own stem cells, which are used to strengthen weak muscles that control urination. The hospital said it is the first in the U.S. to conduct this research. The hospital is working with 48 female research participants, whose stem cells will be collected and duplicated. The cells will be injected into the muscles that control urination to strengthen them and prevent leakage. The study will last 12-14 months. Leader researcher: Ken Peters, urology department chair Prostate cancer indicators Researchers from the University of Michigan Comprehensive Cancer Center have identified a panel of small molecules, or metabolites, that appear to indicate aggressive prostate cancer. One metabolite in particular, sarcosine, appeared to be one of the but the meetings didn’t go very far,” Grant said. “Our problem is their promotional literature is strongly implying they are giving (Connect) free to physicians. It is not free. There is a charge for eprescribing and for each additional module.” to “ We wanted bring up fairly quickly a tool already developed. ” Dr. Gregory Forzley, Michigan State Medical Society Grant said my1HIE does not charge doctors to integrate its existing systems into the network. It also offers a significant discount for the first year for additional software applications such as eprescribing and reference laboratory results. Forzley said the medical society has posted additional information on its Web site to more clearly explain the differences between MSMS Connect’s free and paid services. Nonmembers are charged $70 a month for the basic services, he said. One physician leader who has evaluated MSMS Connect and strongest indicators of advanced disease. The finding, if verified by further testing and development, could lead to a simple test that would help doctors determine which prostate cancers are slow-growing and which require aggressive treatment. Results appear in the Feb. 12 issue of Nature. Senior authors: Arul Chinnaiyan, director, Michigan Center for Translational Pathology; Christopher Beecher, professor of pathology. Funding: National Cancer Institute Early Detection Research Network, National Institutes of Health, an MTTC grant, the Burroughs Welcome Foundation, and the Doris Duke Charitable Foundation. Note: Pending patents related to this research have been licensed to Metabalon, a Durham, N.C., company, in which Beecher and Chinnaiyan own equity. my1HIE is Dr. Paul Harkaway, president of Huron Valley. “We had a choice, and we chose my1HIE because they already had done a lot of background work and were ready to take the next step,” Harkaway said. “Our goal is similar to United Physicians’. We need better tools to connect doctors to each other and to other applications to help manage patient care more effectively.” Grant said he is in discussions with physician organizations all over the state about joining my1HIE. “If we can tie up all the physicians in Southeast Michigan, I don’t know what MSMS will do,” Grant said. “Many physicians want to come with us.” Forzley said he expects a number of physicians in individual or small practices to join MSMS Connect. “We are in talks with larger physician organizations,” he said. However, Grant and Forzley agree that information technology subsidies in the recently approved federal economic stimulus package will encourage physicians to buy electronic medical records and join online health information networks. “The stimulus package will help bring down the barrier of using EMRs, and with some doctors saying, ‘I can’t afford that,’ the stimulus dollars will help them pay for it and help doctors with best practices,” Forzley said. Jay Greene: (313) 446-0325, jgreene@crain.com quire them to undergo competency tests or retraining before returning to practice medicine. That could lead to patient safety issues, according to Gary Freed, the lead author of a pair of studies published in Pediatrics. Freed is chief of the division of general pediatrics and director of the Child Health Evaluation and Research Unit at the University of Michigan Health System. Young adults showing signs of a stroke are being misdiagnosed in hospital emergency rooms, according to a study by Wayne State University School of Medicine researchers. Seemant Chaturvedi, professor of neurology and director of the WSU/Detroit Medical Center stroke program, is senior author. Abraham Kuruvilla, the study’s lead author, is a stroke fellow in the Neurology Department. Other research Longtime airline pilots may be in danger of DNA damage from prolonged exposure to cosmic ionizing radiation, according to a study by a 10-person team that included James Tucker, professor and chair of the Department of Biological Sciences in Wayne State University’s College of Liberal Arts and Sciences. The study, which was led by Lee Yong of the National Institute for Occupational Safety and Health, was published in Occupational and Environmental Medicine. One in eight physicians have been inactive in the state where they are licensed for at least a year, and most states do not re- Grants Frank McMaster, a postdoctoral research assistant in the Wayne State University School of Medicine, has been awarded nearly $60,000 for a Young Investigator Award from Narsad to investigate the neurobiology of familial depression in adolescents. The Juvenile Diabetes Research Foundation has awarded nearly $900,000 to Wayne State University faculty to investigate strategies for stopping diabetic retinopathy in its early stages. 20090302-NEWS--0006-RG1-CCI-CD_-- 2/25/2009 4:28 PM Page 1 Page E6 March 2, 2009 CRAIN’S DETROIT BUSINESS Health Care Extra Health care hot seat CON Roundup Report on tax-exempt hospitals finds high salaries, limited benefits to communities BY MELANIE EVANS CRAIN NEWS SERVICE The Internal Revenue Service on Feb. 12 released a long-awaited report on executive pay and community benefits at not-for-profit hospitals. The report, which found six-figure salaries and uneven aid from hospitals to their communities, comes as many tax-exempt hospitals are shedding jobs, squeezing budgets and threatening further cuts to payroll and services in a weak economy. Industry observers say the findings, coupled with public frustration over a painful recession, could fuel calls to replace what are acknowledged to be vague standards for giving tax breaks to hospitals with quantifiable measures — such as spending — of community benefits. “It’s going to seem out of synch with today’s economy,” said Gerald Griffith, a health care lawyer with Jones Day, of the survey’s 2005 executive pay figures. Findings from the 2006 survey of roughly 500 tax-exempt hospitals for the first time reported how much top executives earn in salary and benefits and clarified previously disclosed figures on how hospitals give back to communities in exchange for certain tax breaks. Results are mixed, and industry insiders quickly denounced the survey as unreliable. The recently released report “is NOT-FOR-PROFIT HOSPITALS The Internal Revenue Service released final results from a May 2006 survey of how much roughly 500 tax-exempt hospitals spend on community benefits and executive compensation. Among the key findings: ■14% of hospitals reported 63% of uncompensatedcare spending. ■ 9% of hospitals reported 60% of community benefit costs. ■The aggregate margin was 5%. Roughly one in five hospitals operated at a loss. ■Uncompensated care accounted for the greatest share of community benefit costs, followed by medical education and training, medical research, and community programs. Source: IRS Exempt Organizations Hospital Compliance Project final report a historical compendium — that’s it,” said J. Douglas Clark, vice president of audit compliance and tax at Detroit-based Henry Ford Health System. There were no “aha!” moments in the 200-page report, he said. “Clearly, the data in this compendium is inconsistent and all over the board,” in part because the Clark questions posed to nonprofit hospitals and health care systems to come up with the data were very ambiguous and because there are no clear metrics for quantifying the community benefit a nonprofit health institution or system provides, Clark said. The report is probably the best prima facie evidence that revamp- ing the 990 tax forms and disclosure standards, as was done for filings beginning in 2008, was very much needed, he said. The hope is that once institutions adjust to the new disclosure rules, some of that ambiguity and difficulty in answering questions will be reduced “and comparisons like this will have value,” Clark said. According to the report, not-forprofit CEOs surveyed earned an average of $490,000 in salary and benefits in 2005 and tax officials noted that compensation figures “appear high but also appear supported under current law,” in a summary of the survey’s findings. And among 20 hospitals singled out for unusually high compensation compared with similar hospitals, the average total payout was $1.4 million. The figures exceed 2005 executive payouts reported by compensation consultants Sullivan, Cotter and Associates in Modern Healthcare’s yearly salary sur- vey. Hospital CEOs earned an average total cash compensation in 2005 of $334,000 for system-owned hospitals and $364,500 at free-standing hospitals. Results also found that less than 10 percent of surveyed hospitals accounted for 60 percent of community benefit costs. Care for which hospitals received no payment, including free and discounted care to needy patients, showed a similar concentration, with 14 percent of surveyed hospitals reporting 63 percent of spending. The IRS survey asked hospitals to detail spending for medical research, medical education and training, uncompensated care and programs to deliver health education, screening, immunizations or other initiatives. The American Hospital Association was critical of the survey and dismissed its findings as flawed. Melinda Hatton, general counsel for the group, said the poorly worded questionnaire elicited widely different answers from hospitals on the value and type of community benefits they provide, leaving the results incomplete and misleading. Hatton argued the same ambiguity clouds findings on executive pay. The survey did not require hospitals to separately report bonuses or deferred compensation, which can skew salaries upward from year to year and can vary depending on an executive’s tenure. She lobbied for policymakers to wait for more specific and comprehensive executive pay and community benefit figures that hospitals must begin reporting on yearly tax forms, known as the Form 990, starting in 2009. The IRS last year finished overhauling the Form 990 and added a separate schedule for hospitals to itemize how much and what type of community benefits they provide. The form clearly defines what may be counted as community benefits — Medicare losses and bad debt are excluded from the list — and says all expenses must be reported at cost. The survey is one of many inquiries in recent years by regulators and Congress into the business practices and governance of tax-exempt hospitals. The sector came under scrutiny for aggressive pricing, billing and collection practices that left the uninsured paying rates well above those charged to the insured. Critics, including Sen. Chuck Grassley, R-Iowa, who is the ranking member of the Senate Finance Committee, have pushed for greater transparency and more oversight of tax-exempt health care, with some success. An overhaul of not-for-profits’ yearly tax filings last year included a separate schedule for hospitals to itemize how much and what type of community benefits they provide. Grassley is expected to push for legislation that would tie hospitals’ tax exemptions to quantifiable measures of how much hospitals give back to communities. From Modern Healthcare. Crain’s Detroit Business reporter Sherri Begin Welch contributed to this story. Cancer partners file to move MRT to new center Moving ahead with their joint venture to build a $17 million outpatient radiation cancer center, Crittenton Hospital Medical Center in Rochester Hills and Barbara Ann Karmanos Cancer Institute in Detroit have filed a certificate of need to relocate a $3.4 million megavoltage radiation therapy unit to the new facility under construction in Rochester Hills. “We are proposing to relocate the MRT from Crittenton, where we provide radiation oncology services in a joint venture with Karmanos, to the new outpatient center off M-59 and Crooks Road,” said Michelle Hornberger, Crittenton’s chief strategy officer. Last September, the two hospitals broke ground on the 30,000-square-foot facility, located at 1901 Star Batt Drive. The center, which is expected to open later this year, will include clinical office space, chemotherapy, imaging services and radiation oncology. Hornberger said the hospitals have not made a final decision on the name of the center. It is tentatively named the CrittentonKarmanos Cancer Center. The center will be will be dedicated to the memory of Vivian Stolaruk, the late wife of Steve Stolaruk, who donated the three-acre site. — Jay Greene The following are selected certificate of need filings and decisions from Feb. 1-23. The filings are made with the Michigan Department of Community Health and can be found at www.michigan.gov/mdch by navigating to the “providers” section. Applications received: University of Michigan Health Center, Ann Arbor: Add second fixed CT/PET scanner, $4.5 million. West Winds Medical Center, Commerce Township: Add 15 nursing home beds, $1.2 million. Heartland Health Care, Sterling Heights: New 120-bed nursing home, $15.3 million. Medilodge of Howell: Add 20 nursing home beds, $1.7 million. Livingston Health Campus, Howell: New 56-bed nursing home, $5.3 million. Livingston Care Center L.L.C., Howell: New 56-bed nursing home, $5.5 million. Levan Internists P.C., Livonia: Initiate fixed CT scanner, $1.5 million. Filings not approved: Michigan Institute for Radiation Oncology, Pontiac: Replace CT simulator, $265,000. University of Michigan Health Systems, Ann Arbor: Replace two gamma cameras, $2.1 million. 20090302-NEWS--0007-RG1-CCI-CD_-- 2/25/2009 3:29 PM Page 1 CRAIN’S DETROIT BUSINESS March 2, 2009 Page E7 Health Care Extra Insurers address therapeutic drug-switching concerns BY MIKE SCOTT SPECIAL TO CRAIN’S DETROIT BUSINESS Local health insurers are developing policies to address lingering concerns over therapeutic switching, a practice that has come under fire by physicians, pharmacy groups and consumers. Physicians say they want more authority over whether brandname drugs — such as the sleep-inducing drug Ambien — should be switched for lower-cost generics. They also want compensation for the extra time it takes them to investigate whether such a switch benefits patients. Depending on a patient’s pharmacy benefits, an insurer could save money and the patient could reduce out-of-pocket co-payment costs. Physicians sometimes prescribe a drug because other options haven’t been effective, said Dr. Rose Ramirez, vice speaker of the House for the Lansing-based Michigan State Medical Society, which opposes therapeutic switching. “I write generic prescriptions as much as possible to cut costs, but often as physicians we have specific reasons for selecting the drug that we do,” said Ramirez, a family practitioner at Jupiter Family Medicine in Belmont. Another problem with medication switching is that it could take physicians more time to find the right therapeutic balance for a given condition, said Arlene Gorelick, president of the Epilepsy Foundation of Michigan. Most physicians prescribe medications based on their knowledge of the drug and the paGorelick tient’s needs and condition, Gorelick said. Patients could be adversely affected if generic and brand-name drugs are switched back and forth, she said. “As more generic drugs have come into the marketplace over the past several years, these switches have increased in num- SKEPTICS OF SWITCHING An October 2008 national survey of approximately 1,400 adult users of prescription drugs found that 77 percent of respondents would oppose the practice of therapeutic switching without the consent of the prescribing doctor or patient. Many of the respondents Opposed were unaware that such switching even occurred. The survey also indicated broad opposition to insurance companies offering incentives for physicians who switched from brand-name prescriptions to generics. It was conducted by the Washington-based National Consumers League, a private, nonprofit advocacy group representing consumers on marketplace and workplace issues. 77% Source: National Consumers League, www.nclnet.org bers,” Gorelick said. “There can be significant side effects, and when it happens to an epileptic patient, the results could be catastrophic.” Blue Cross Blue Shield of Michigan began a program in September 2007 that identifies opportunities to promote to physicians cost-effective drug therapies in specific areas. The Blue Cross program notifies physicians of generic drug options without using financial incentives or other tactics to get doctors to prescribe generics, said Laurie Wesolowicz, a certified pharmacist and director of Blue Cross’ clinical pharmacy services. However, earlier in 2007, Blue Care Network, Blue Cross’ health maintenance organization, used an incentive program for three months that compensated physicians up to $100 for each time they prescribed a generic drug instead of a branded drug for certain classes. Helen Stojic, Blue Cross’ director of corporate affairs, said the policy saved members and businesses “several million dollars.” Blue Cross withdrew the program after it experienced backlash from doctors and consumer groups. Wesolowicz said that under the Blues’ current program, a letter is sent to inform a member’s physician when a prescription for a name-brand drug is written that the insurer determines could be replaced by a comparable generic drug at a lesser cost. Wesolowicz said the physician always can agree to or decline the therapeutic switch. If the physician agrees, a second letter will be sent to inform the insured member of the option. The member then also can challenge the medication switch and can contact the physician with concerns, she said. To reduce physician time in the process, Blue Cross does not require the doctor to explain a decision to continue using the higher-cost name-brand drug, Wesolowicz said. Still, Ramirez said physicians spend too much time on the switching requests without being fairly compensated. She said the medical society supports paying physicians more for a therapeutic switch. The use of electronic prescribing may be one way to reduce time and make the process more transparent, Ramirez said. But e-prescribing will work only if insurers make available online their drug formularies and physicians have electronic medical records or other software in place and pharmacies are linked. “My (electronic medical record) will send a message back to me about (the patient’s insurance details) and will walk me through options and suggestions so we don’t have all the headaches when the patient drops off the scrip,” Ramirez said. “E-prescribing doesn’t alleviate all my concerns, but it can save a ton of work and frustration for everyone involved. But you need a lot of pieces in place for it to work,” she said. Blue Cross also does not force pharmacists to switch a member’s medication without approval from both the physician and the member, she said. “Our goal is to let our physicians and members know that there are effective alternatives available for a lesser cost,” Wesolowicz said. “When you look at the rising cost of member co-pays, there is a significant benefit here.” Not all classes of prescriptions are managed under this program. There are about 25 brand-name drugs that would trigger such a physician letter, with the list based largely on FDA approval and guidelines, Wesolowicz said. The classes of prescription drugs that are treated in such a way by Blue Cross tend to be for less serious clinical diagnoses, Wesolowicz said. Examples include sleep drugs, prescription nasal sprays and more. Epileptic drugs, for example, do not generate a physician letter. “We tend not to target drugs where there are therapeutic controversies,” Wesolowicz said. In January, Blue Cross tracked more than 1,100 positive responses in Michigan in which a prescription was switched from a branded drug to a generic, she said. Both physician and member approved of such switches, she said. American Community Mutual Insurance Co., a Livonia insurance company, contracts with a pharmacy benefits manager to administer its prescription drug programs and make care more affordable. “Generic drugs help us do this by providing therapeutically equivalent solutions for consumers as an alternative to more expensive brand drugs,” said Ellen Downey, vice president of corporate communications. “Our (pharmacy benefits manager) has worked with us to implement appropriate generic substiDowney tution and formulary management programs to provide clinically appropriate medications that save consumers money,” she said. If an American Community Mutual Insurance Co. member pre- sents a prescription for a brandname medication at a retail pharmacy or by mail and a generic alternative is available, the insurer’s pharmacy manager or the retail pharmacy may substitute the generic alternative when appropriate, Downey said. Similarly, if a more cost-effective preferred brand alternative is available, the pharmacy manager or retail pharmacy may contact the policyholder’s physician to request a change from the original prescribed brand drug to the preferred brand drug when medically appropriate. Any changes to a patient’s prescription, other than a permitted generic substitution, must be authorized by the patient’s doctor, Downey said. “We do not automatically switch patients from one therapy to another,” she said. To address the medicationswitching policies, the Epilepsy Foundation has been working with state legislators on a bill that would prevent pharmacists from switching unless the change is approved by both the physician and patient, Gorelick said. State Sens. Bruce Patterson, RCanton Township, and Tom George, R-Kalamazoo, an anesthesiologist and chair of the Senate Health Policy committee, introduced Senate Bill 1311 in May 2008. The bill, which wasn’t acted on, would have prevented some therapeutic switching. It also would have eliminated any financial incentives to physicians for prescribing generic drugs. Sue Trussel, Patterson’s media coordinator, said it is possible that a new bill addressing some of the same issues could be introduced this year. Insurers are looking at a variety of ways to manage prescription costs and streamline ordering, Wesolowicz said. “Members have indicated to us that they need help in paying for their prescriptions, and if we can provide such assistance while keeping physicians in the role of the key decision-maker, then it’s a win-win for all parties,” Wesolowicz said. Oakwood CEO: Focus on patients to survive tough times BY JAY GREENE CRAIN’S DETROIT BUSINESS Putting patients, quality and customer service first is a challenge for hospital executives as they seek to cut costs and adjust service mix in the face of a worsening economy and declining profit margins, said Brian Connolly, CEO of Dearborn-based Oakwood Healthcare. Speaking Feb. 16 before fellow health care executives at a breakfast Connolly meeting of the Midwest Healthcare Executives Group and Associates, Connolly said Oakwood is closely evaluat- ing its entire health care operation. MHEGA is an affiliate of the Chicago-based American College of Healthcare Executives. “Many hospitals are at the same place. ... If we focus on patients, we will get through these tough times,” said Connolly. “Everything is on the table now.” Last November, Oakwood announced it would reduce nonclinical employees through attrition by 8 percent to 10 percent. So far, some 35 to 50 employees have been laid off. It also is in the process of cutting costs by $20 million to $30 million. “We continue to hire RNs and clinical occupations,” said Paula Rivera-Kerr, Oakwood’s media relations manager. “We are looking very closely at other nonclinical positions. Any nonclinical position being filled requires review and approval first.” One of the chief drivers of declining profit margins at Southeast Michigan’s 45 hospitals, including Oakwood’s four acute-care facilities, is steadily increasing uncompensated care costs. For example, Oakwood’s uncompensated care, which includes charity care, bad debt and unpaid costs of Medicare and Medicaid, increased 233 percent to $100 million in 2008 from $30 million in 2005, Connolly said. “More Michigan patients have more outof-pocket costs (as insurance co-pays and deductibles rise), and that is increasing uncompensated care,” Connolly said. Another driver of uncompensated care is the growing numbers of the unemployed and uninsured. The state’s 144 hospitals recorded more than $2 billion in uncompensated care in 2008 — a record amount, according to a report this month from the Michigan Health and Hospital Association. In response, Connolly said, Oakwood is reassessing its strategic plan, with an eye on cutting costs. However, the plan will maintain Oakwood’s focus on quality and research, along with building care upward from physicians to primary and specialty services. “We need to demonstrate value — that is, quality, costs and customer service,” Connolly said. “You need all three or the stool will fall over.” This article first appeared on www.crains detroit.com DBpageAD.qxd 2/25/2009 2:55 PM Page 1