Mobile technology takes The Ottawa Hospital further on its journey
advertisement

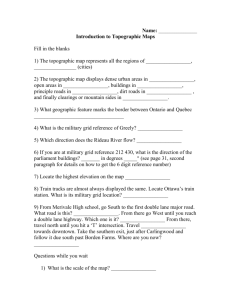
Dr. Glen Geiger, Medical Director & Chief Clinical Information Officer, Information Services, The Ottawa Hospital Feature Mobile technology takes The Ottawa Hospital further on its journey toward excellence T he Ottawa Hospital’s recent foray into mobile computing technology with the Apple iPad® has allowed physicians to revitalize bedside patient rounds and direct care activities. Like other hospitals in the western world, The Ottawa Hospital has seen unprecedented growth in technology over the past four decades; CT and MRI scanners, automated medication infusion pumps, and non-invasive blood pressure cuffs, to name just a few. The paradox of modern healthcare is that despite this proliferation in technology, clinicians across the western world continue to use manual care-delivery processes, largely driven by paper forms, handwritten documentation, FAX machines, and pagers. While other industries have put information technology directly in the hands of frontline workers, healthcare has lagged behind in the transformation of direct patient care, preferring instead to leverage technology only within isolated islands such as medical imaging or the hospital lab. This has resulted in the cumbersome, bureaucratic, unresponsive system with which citizens are very familiar. In a world where your order at Tim Horton’s is entered into a computer to move it to a recipient ten feet away, doctors continue to rely on paper forms and the mail system to request diagnostic testing from remote facilities. The internet allows the average citizen to find services in seconds, while family doctors and other primary care providers have no directory of specialists in their area to help them refer patients for tertiary care. Within hospitals, medication orders and diagnostic testing requests are written on carbon forms and transcribed multiple times before they can be executed, with all the attendant potential for error this entails. At The Ottawa Hospital, computer workstations provide access to patient results at the nursing station and in physician offices but, until recently, access to information at the patient bedside required the medical team to recopy the results or print them from the computer system in order to carry them. Volume 18/Issue 3 Fall 2011 When the Apple iPad® became available last year, The Ottawa Hospital launched an initiative to configure a clinical application that would make patient information available on this mobile platform. By November, the developer’s efforts had borne fruit and the first version of the Clinical Mobile Application was put into production in a pilot project with the Division of General Internal Medicine. The first version allowed Staff Physicians and Residents to review patient lab results, diagnostic imaging reports, and transcribed documents at the patient bedside. ‘handle’ on their care when they received information right at the bedside. The patients felt more in control when they were given the facts directly, rather than filtered by delay and physician recall. Since the initial pilot, the development team has enhanced the Clinical Mobile App with a PACS viewer that allows medical images to be displayed. As the saying goes, “a picture is worth a thousand words”, and for patients and their families, being able to see their own x-ray makes it easier to understand the diagnosis and treatment plan. The paradox of modern healthcare is that despite this proliferation in technology, clinicians across the western world continue to use manual care-delivery processes, largely driven by paper forms, handwritten documentation, FAX machines, and pagers. The application also provided access to information resources such as the hospital formulary, e-CPS, and the hospital’s collection of online journals and e-texts. The results were dramatic. Clinicians recognized the value of the new tool immediately. Having up-to-date patient information available anywhere, anytime, enabled better patient care decisions. Reports began to filter in describing how much easier it was to look after patients. Care teams that had been doing ‘rounds’ from a workstation-equipped conference room began to do bedside rounds again because they could easily carry the information with them. Physicians took to showing results directly to their patients. Anecdotal feedback described how family members of critically ill patients were better able to understand their loved one’s condition when they were shown the information for themselves. At the end of the pilot, the Residents moving out of the pilot area and onto new rotations, refused to give their iPads back and were the envy of their colleagues. Direct interviews with patients confirmed that they, too, felt that the team had a better The privacy of patient information has been of paramount concern throughout this project. Physicians are reminded of the importance of maintaining patient confidentiality during commissioning and a reminder message appears during login. The Clinical Mobile Application is secured by two levels of user passwords and the application does not retain any patient information in its memory. The technical support team also has the ability to erase iPads remotely in the event of loss. Following the success of the pilot, The Ottawa Hospital IS Governance Committee approved the purchase of a further 1,800 iPad 2’s, for deployment to physicians and residents, and clinicians are ‘lining up’ to receive theirs. The next phase of application development will include the ability to order x-rays and lab tests directly from the patient bedside. Physicians and residents have already confirmed that this would enhance their use of the application and would make electronic ordering easier. Feature continued on page 6 5 Karim Bhaloo, BSc, MLT, OSMT District 5 Director Feature Freedom of Information and Ontario hospitals O n October 20, 2010, the Ontario Government introduced the Broader Public Service Accountability Act, 2010 (BPSAA) which received Royal Assent on December 8, 2010. The Act introduced new rules and accountability standards not only for the broader public sector organizations, but also for Local Health Integration Networks (LHINs) and hospitals. Also known as Bill 122, the Act, among other things, brings Ontario hospitals under the umbrella of the Freedom of Information and Protection of Privacy Act (FIPPA). Even though FIPPA will apply to all public or private hospitals effective January 1, 2012, only records that came into the custody or control of the medical facility on or after January 1, 2007 will be subject to the Act. According to the Act, a record means “any record of information however recorded, whether in printed form, on film, by electronic means or otherwise, and includes: a) correspondence, a memorandum, a book, a plan, a map, a drawing, a diagram, a pictorial or graphic work, a photograph, a film, a microfilm, a sound recording, a videotape, a machine readable record, any other documentary material, regardless of physical form or characteristics, and any copy thereof, and b) subject to the regulations, any record that is capable of being produced from a machine readable record under the control of an institution by means of computer hardware Feature continued from page 5 In the long term, The Ottawa Hospital’s mobile strategy includes expanding the use of the device to more clinicians and the use of inter-provider messaging to enhance communication between different members of the care team. The Ottawa Hospital is in discussion with their speech recognition vendor to deliver this technology on iPads. This will complement the current offering of ‘real time’ voice 6 and software or any other information storage equipment and technical expertise normally used by the institution.” public to access them depends on the hospital’s capacity to demonstrate the exemption. Some of the exemptions include: Under FIPPA, citizens of Ontario will have the right to request access to these records unless they are either excluded or exempt. Under the Personal Health Information Protection Act (PHIPA), a citizen can access records about him or herself only. However, under FIPPA anyone can access any records that are under the control of or held by the hospital, public or private, on any issue subject to certain exclusions. Some of these exclusions as set out in the Act include: 1. Proprietary information such as requests for proposals. 2. Employment records. 3. Information prepared by or for in-house legal department. 4. Information produced by the Board or a committee of the Board during a meeting that “a statute authorizes holding the meeting in the absence of the public and the subject-matter of the meeting is a draft of a by-law, resolution or legislation or litigation or possible litigation.” 1. Ecclesiastical records of a church or religious organization that is affiliated with an educational institution or a hospital. 2. Records that relate to the operations of a hospital foundation. 3. Administrative records of a member of a health profession listed in Schedule 1 to the Regulated Health Professions Act, 1991 that relate to the member’s personal practice. 4. Records relating to charitable donations made to a hospital. 5. Records relating to the provision of abortion services. 6. Personal health information as defined in PHIPA. The introduction of FIPPA marks a major change for hospitals in Ontario. In order for these institutions to be compliant with the legislation on January 1, 2012, they must change and or introduce policies and procedures to manage requests made under the legislation. ❖ References: Ministry of Health and Long-Term Care. (2011). The Broader Public Sector Accountability Act, 2010. Accessed on July 6, 2011 at http://www.health.gov.on.ca/en/legislation/ bpsa/fippa.aspx Certain records can be exempt under FIPPA but the public can still request access to such records under FIPPA. The ability of the Pessione, H & Hawkins, P.J. (2011). Application of Freedom of Information to Ontario Hospitals. Hospital News, p.29. recognition, currently available through PC workstations and will allow physicians to create text documents, anywhere, anytime. Electronic medication ordering is a longterm project that will leverage the hospital’s investment in both the PC-based Electronic Medical Record, and its counterpart, the Clinical Mobile Application. Direct entry of medication orders is part of a change in medication workflow, considered essential to preventing medication errors and ensuring patient safety. By the time this functionality becomes available, clinicians will already be very familiar with the use of the mobile device for less critical types of electronic ordering. Speech recognition, electronic ordering, online information resources and mobile access to the Electronic Medical Record, are all part of a cultural shift that is transforming healthcare and TOH is proud to be leading the way. ❖ Photo of Dr. Geiger courtesy of Chrissie DeCurtis Cloutier, The Ottawa Hospital ADVOCATE