the significance of spasticity in the upper and lower
advertisement

THE
UPPER
SIGNIFICANCE
AND
OF
LOWER
JOHN
M.
LIMBS
MAZUR,
Front
SPASTICITY
ANNE
ChilcIi’en’s
the thoracic
level, 26% at the upper lumbar level,
Fifty-four
per cent of these patients
demonstrated
upper
limbs;
limbs;
9%
were
flaccid
in the lower
casts, and were less likely
less likely to be independent
to walk than
in activities
patients
with normal
upper
important
in the evaluation,
The
purpose
of
this
paper
neurological
involvement
bifida
cystica,
the
paralysis.
the various
is to
level
of
goals
types
in
of
which
and
The
may
spastic
patterns
has
with
with
time
because
system
anomalies
lesions
no previous
versus
flaccid
and the effect
activities
of daily
involvement
of
is often
complex
and
been thought
to be of
and the
1963a,b;
J. M. Mazur.
MD. Associate
Southern
Illinois
University
62708,
USA.
A. Stillwell.
B App Sci (Phty).
M. B. Menelaus.
MD. FRCS.
Royal
Children’s
Australia.
Requests
Hospital.
for reprints
No.
the
as
resultant
Smith
para1965).
should
2. MARCH
associated
central
the Arnold-Chiari
syri ngomyelia,
of the cord.
of the degree
Professor
School
Deputy
FRACS,
Flemington
be sent
1986 British
Editorial
Society
0301
620X/86/2038
S2.00
68-B,
of
such
hydrocephalus.
and tethering
reports
1986
in the upper;
orthopaedic
of
to Mr
M. B. Menelaus.
and
Joint
spacecould
in late
Springfield.
Chief
Physiotherapist
ChiefOrthopaedic
Road.
Parkville.
of Bone
We
of spasticity
Medicine.
Surgery
24%
procedures,
were
more
at the sacral level.
limbs with normal
spastic
days
in the lower
in hospital
and
with spastic
upper limbs
to require
special
schools
of the lesion,
patients.
childhood
or
logical
pattern
to the level
paralysed
at
the degree
of spasticity
adolescence,
and the effect
upon function
and prognosis,
of
in
were
than
is
the
neuro-
spina
present
paper
(MBM)
recognised
that either
a
or a flaccid
paralysis
could
be present
(Menelaus
Moreover,
the
neurological
involvement
can
malformation,
occupying
VOL.
occur
and Drummond
believed
that the lesion
was frean upper
motor
neurone
condition,
basing
this
on electrical
stimulation
studies
of the neural
(Stark
and Drummond
1971). The senior
author
change
nervous
find
correlate
to perform
neurological
with
myelomeningocele
The principal
lesion
of this
spastic
1980).
spastic
lumbar level and 13%
paralysis
in the lower
those with flaccid
paralysis.
Patients
of daily living and were more likely
the
the lower
motor
neurone
type.
paresis
to be flaccid
(Sharrard
Stark
quently
belief
plaque
but were
with functional
patients.
The
incidence
of
neurological
on the ability
to walk
living
are described.
were evaluated
and classified
according
Thirty-one
per cent of the patients
were
30% at the lower
the classic
flaccid
limbs.
more
MENELAUS
!vh’Ihow’ne
limbs. In addition
to the spinal cord level
treatment
and prognosis
of myelodysplastic
lesion
and degree
of spasticity
the treatment
of myelodysplastic
children
confusing.
limbs,
13% were spastic
in the upper and lower
Patients
with spastic
lower limbs required
MALCOLM
Ho.s1ntal,
One hundred
and nine children
with myelodysplasia
and type of paralysis
and its effect on functional
ability.
THE
MYELOMENINGOCELE
STILLWELL.
Rota!
i/it’
IN
IN
Surgeon
Victoria
Illinois
3052,
MATERIAL
AND
METHODS
This study
consisted
of a functional
analysis
of children
with spina bifida cystica.
All children
aged 8 to 18 years.
inclusive,
who lived close enough
to the Royal
Children’s
Hospital,
Melbourne,
to be recalled
and
personally
examined
were
were asked
and
logically
disturbed
children
were
included.
The
parents
I I 2 agreed
to participate.
adolescent
excluded
with
the examiner.
The
All examinations
patients’
histories
might
affect
the
two
they
left
109 children
were
were
performed
obtained
This
and hospital
records.
operative
procedures
was directed
toward
and
because
All diagnoses.
were recorded,
those diagnoses
neurological
of
125
One
mentally
could
children
psychoretarded
not
co-operate
for the project.
by
from
the authors.
the parents
hospitalisations.
and
Particular
attention
and operations
that
involvement.
The
physical
examination
included:
measuring
the head
circumference;
examining
voluntary
muscle
power
by a manual
muscle
test; assessing
sensation
with
reference
to pain
and light
reflexes,
touch;
examining
Babinski’s
sign,
position
sense.
deep tendon
clonus
and rapid
alternating
movement;
and the assessment
ofintention
tremor.
All abnormalities
were recorded,
and the patients
were grouped
according
to the neurological
level and
degree
of spasticity.
There
were
two
main
groups
depending
on the presence
or absence
of spasticity
in the
lower extremities.
Each group
was then divided
into two
subgroups
depending
upon
whether
or not the upper
limbs were normal.
213
214
J, M. MAZUR,
Classification.
limbs)
included
the
spinal
to the
Group
cord,
level
no motor,
ties were
IA
lesions
(flaccid
involving
Neurological
of the
sensory
normal.
but
or reflex
Group
the
of the long
area
of interruption
paralysis
activity.
central
nervous
there
manifested
by
or pain-withdrawal
was
down
there
was
IA except
that spastiThis group
contained
system
abnormalineurone
signs in the
paralysis
of the lower
segment
ofthe
cord
above
with interrup-
system
an
intact
lesion
The upper
extremilower
limbs,
spastic
upper
limbs)
was similar
to Group
city was present
in the upper
limbs.
those with associated
central
nervous
ties responsible
for the upper
motor
upper
limbs,
In Group
hA
(spastic
limbs).
the lesion spared
the terminal
which
was, however,
cut off from
tion
was
below
activity.
(flaccid
lB
tracts.
upper
spasticity.
reflex.
Below
motor
was well below
The neurological
exaggerated
It was believed
the cervical
spine.
level of the lesion
was
the
reflex
that
as deteralso was
recorded
pin-prick
by the
most
caudal
dermatome
with
The percentages
to determine
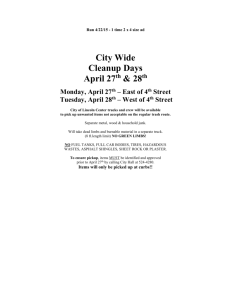
Fig.
Distribution
of patients
within
ofthe
spinal cord lesion.
Group
flaccid
paralysis
in lower
limbs.
limbs:
IIB. spastic
I
neurological
groups.
showing
the level
IA. flaccid
paralysis
in lower
limbs:
lB.
spastic
upper limbs:
lIA. spastic
lower
upper
and lower limbs.
classified
according
to the most caudal
intact
nerve
root
mined
by motor
function.
The sensory
function
and light-touch
sensation.
each group
were calculated
I
neurone
the spasticity
was caused
by an isolated
segment
of spinal
cord
functioning
below
the myelomeningocele
plaque.
Group
JIB (spasticity
in upper
and lower limbs)
was similar to Group
IIA with the addition
of spasticity
being
present
in the upper
limbs
even though
the spina
bifida
defect
M. MENELAUS
paralysis
of the lower
the terminal
portion
of
function
lesion,
A. STILLWELL,
ofpatients
the prevalence
the lower
sensory
the non-dominant
Group
in
cord
IA
lesion
level
side.
on
the
(complete
flaccid
and normal
upper
of 59 patients
30 girls
(54%),
dominant
side,
paralysis
limbs).
and
and
5 on
below
the spinal
There
were a total
29 boys,
in this
group.
ofeach
type oflesion.
Any asymmetry
between
the sides
of the body was recorded
for both the motor
and sensory
examination.
Functional
ability.
Intellectual
ability
was assumed
to be
normal
if the child
attended
a normal
school
and was
within
two grades
of that expected
for the chronological
The ages ranged
from
8 years
I month
to I 8 years
II
months
(average
14 years
3 months).
The level of the
motor
lesion was thoracic
in 13 patients,
upper
lumbar
in
12. lower
lumbar
in 20 and sacral
in 14 (Fig.
I). Within
Group
IA there
were 51 (86%)
community
walkers,
I
household
walker
and
7 non-walkers
(Table
I). The
age.
patients
in this
perform
themselves
daily activity
skills, all but one
and maintain
their personal
Independence
in
feeding,
personal
hygiene
and
dressing
was assessed
to determine
the functional
level in
activities
of daily living.
Patients
were classified
according to their mobility.
as community
walkers,
household
walkers
and
non-walkers.
Independence
and
walking
were
compared
between
patients
in the four
group
scored
very
well
in their
abilities
groups.
1OC
a
ae
C
0
RESULTS
The age range
months
(average
was from
14 years
8 years
I month
2 months).
There
and 54 boys. The level of the motor
lesion
(31%)
was thoracic,
in 28 (26#{176}/o)upper
(30%)
lower
and sensory
patients
(58%);
motor
(4%).
level
There
in 10 patients:
lumbar,
and
in 14 (13%)
to 18 years 7
were 55 girls
in 34 patients
lumbar,
in 33
sacral.
lesions
were at corresponding
the sensory
level was
in 42 patients
was right-left
The
right
side
levels
in 63
lower
than
the
was
70
0
ec
C
0
40
70
50
!
at a lower
level than the non-dominant
left; in the other
2 patients,
the lower motor
level was on the non-dominant
left side.
There
were 20 patients
with sensory
asymmetry:
I 5 had
112929
S
a.
20
Hflfl
motor
(38%),
and higher
in 4 patients
side asymmetry
in motor
level
in 8 the dominant
ec
0
F
H
IA
0
F
H
D
H
0
F
hA
lB
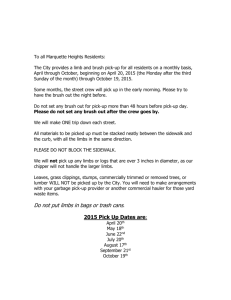
Fig.
F
HO
PB
2
Relationship
between
independence
in skills
of
daily
living
(F, feeding:
H. hygiene:
D. dressing)
and
neurological
group.
Patients
with
normal
upper
limbs (Groups
IA and IlA) were more
likely
to be independent
than
those
with
spastic
upper
limbs (Groups
lB and IIB).
THE
JOURNAL
OF BONE
to
being able to feed
hygiene
(Fig. 2).
AND
JOINT
SURGERY
THE
(flaccid
Group
lB
pnised
only
SIGNIFICANCE
lower
OF SPASTLCITY
limbs,
spastic
(9%
of the
10 patients
were 6 boys and 4 girls. The
months
to 18 years 7 months
All the
pin-prick
patients
and
in this
position
upper
total
limbs)
series).
ages ranged
from
(average
14 years
group
sensation
patients
had an intention
strated
abnormal
rapid
the spasticity.
The level
IN THE
had
UPPER
ing,
com-
feed
sonal
hygiene
Group
JIB
9 years
I month).
6
normal
light
touch,
in the upper
limbs;
6
tremor,
and 7 patients
demonalternating
movement
as well as
of the motor
lesion was thoracic
Table
I.
and
Summary
dressing
ofall
(Fig.
2).
CW
HW
NW
Total
CW
HW
NW
6
1
6
13
1
1
Upperlumbar
11
0
1
12
0
Lowerlumbar
20
0
0
20
Sacral
14
0
0
51
1
7
Thoracic
Total
=
CW
HW
NW
Community
= Household
= Non-walker
Group
ankle
knee
reflexes,
and
lower
reflex,
reflexes,
8 patients
Although
there
sony awareness
Total
CW
HW
in
10, and
Group
walkers,
Group
limbs
daily
VOL.
5
7
0
1
0
1
2
0
0
14
0
0
59
3
2
limbs).
This
group
of
4
3
had
had
had
a positive
was no voluntary
below
the spinal
contractures
were thoracic
lower
Babinski’s
movement
cord lesion,
lumbar
in two or more
in 7 patients,
in 9 (Fig.
IA, patients
in Group
IIA
and demonstrated
good
skills
living
(Fig.
2). All the patients
No.
per-
in all four
total
series)
limbs).
There
in this group,
were
14
6 boys
Group
IhB
CW
HW
NW
Total
1
6
7
0
0
7
7
3
3
4
10
1
2
2
5
2
7
2
0
9
0
2
0
2
0
0
0
0
0
0
0
0
0
0
5
10
10
6
10
26
4
9
14
26
alternating
movements
as well as spasticity.
In this group
only one patient
was a community
walker,
4 were household walkers
and 9 could
not walk at all. They had poor
daily activity
skills, only 7 being able to feed themselves
ankle
clonus,
4 had
abnormal
hamstring
reflex.
and no senstimulation
I).
muscles.
The
upper
lumbar
Ten
patients
IIA were community
walkers,
6 were household
and 10 were non-walkers
(Table
I). Like those
6k-B.
own
NW
muscles
in 12, in the tibialis
anterior
in 5, in the gastrocnemius
and soleus
in 12, in the tibialis
posterior
in 6,
and in the long
toe flexor
muscles
in 5 patients.
Ten
had
lesions
their
reflexes,
and 8 had a positive
Babinski’s
reflex.
All 14
patients
showed
spasticity
or hyper-reflexia
in the upper
limbs.
All the patients
had normal
light touch,
pin-prick
and position
sensation
in the upper
limbs.
Eight patients
had an intention
tremor,
and
10 had abnormal
rapid
hA
ofthe
leg evoked
a flexion
withdrawal
reflex in 8 ofthe
26
patients.
Because
of the spasticity,
contractures
developed
in the hamstrings
in 8 patients,
in the peroneal
patients
motor
after
themselves.
upper
lumbar
in 5, and lower
lumbar
in 2. Six patients
had increased
ankle
reflexes,
4 had ankle
clonus,
3 had
increased
knee
reflexes,
3 had pathological
hamstring
Group
patients
(24%
of the total series) comprised
I 3 boys and
13 girls. The ages ranged
from
8 years
9 months
to 18
years
6 months
(average
14 years 4 months).
All of the
patients
in this group
demonstrated
increased
deep tendon reflexes
indicating
an upper
motor
neurone
paralysis
below
the spinal
cord
lesion.
Twelve
patients
had an
increased
increased
(spasticity
(13%
of the
look
dress
Total
walker
walker
(spastic
hA
18 could
and 8 girls. The ages ranged
from 8 years 6 months
to I 7
years
I 1 months
(average
14 years
I month).
The motor
lesions
within
Group
IIB were
thoracic
in 7 patients,
GrouplB
IA
lesion
21 could
and
215
IN MYELOMENINGOCELE
the patients
Group
Spinal
LIMBS
independently,
patients
lB did not perform
as well as Group
IA in daily
functions
but 6 were independent
regarding
eat-
hygiene
LOWER
There
in 7 patients,
upper
lumbar
in I, and lower
lumbar
in 2
(Fig.
I); three patients
were community
walkers,
2 were
household
walkers
and 5 were
non-walkers
(Table
I).
Group
activity
AND
2. MARCH
1986
in
(Fig. 2).
Walking
ability.
The relationship
between
spasticity
and
walking
was carefully
analysed.
In the patients
with thoracic lesions,
the number
ofcommunity
walkers
decreased
from 6 out of 13 in Group
IA to I out of7 in Group
lB
(both
groups
having
flaccid
lower
limbs),
to none
in
Group
upper
walkers
hA and none
lumbar
lesions,
in Group
IA,
Group
hA and I out of5 in Group
IIB. Similarly,
in the
patients
with lower
lumbar
lesions,
all were community
walkers
in Groups
IA and lB. 7 out of 9 in Group
IIA
and none
in Group
JIB. All of the patients
with sacral
motor
lesions
were in Group
IA and all were community
walkers.
Hydrocephalus.
Spasticity
in the upper
limbs was related
to the number
lus. Patients
in
had normal
upper
in the activities
of
except
one could
in Group
IIB. In patients
with
I I out of 12 were
community
none in Group
lB. 3 out of 10 in
of shunt
in Groups
operations
IA and
shunt
procedures
each while
IIB had an average
of four
each respectively.
shunts;
both were
Two patients
patients
with
done
hA
had
for
hydrocepha-
an average
of two
patients
in Groups
lB and
and five shunt
procedures
in the series had infected
thoracic
lesions
in Group
216
J. M. MAZUR.
IIB.
Only
one
patient
had
a head
A. STILLWELL,
circumference
greater
than two standard
deviations
from normal
and she was
also a Group
[lB patient
with a thoracic
lesion.
Orthopaedic
admissions.
Patients
in Group
IA required
fewer
shorter
in
orthopaedic
admissions
periods
of immobilisation
Groups
lB.
IIA,
or
and
than
IIB.
The
operations
did the
number
of
who
had
spasticity
more
dren
likely to require
in Group
lB and
special
schools
In the
past.
in their
upper
limbs,
bifida
is equally
important.
were
the
cord
below
and
were
I) had complete
the myelomeningocele
loss
were
spinal
cord
of paralysis,
Group
a flaccid
paraparesis
below
the spinal
II patients
have a spastic
paraparesis.
(Group
below
however,
cystica
I patients
cord
The
lesion,
largest
of sensation
and
plaque.
Presumably
only
lesion.
spashave
Group
group
reflexes
there
no functioning
neural
elements
below the plaque,
or
lesion
involved
the terminal
portion
of the spinal
so that function
was intact
down
to a certain
level,
which
there
was impairment
of motor,
sensory,
reflex activity.
Group
II patients
had a “gap”
in cord
function
with loss of motor,
sensory,
distal
to which
was an intact
but
cord.
In the isolated
cord,
spasticity
and reflex activity,
isolated
segment
of
and stretch
reflexes
may
be striking.
Tonic
reflexes
could
be elicited:
for
example.
stroking
the dorsum
of the foot evoked
foot or
toe extension,
Although
there
was no voluntary
movement of the legs and no central
response
to pin-prick,
the
slightest
stimulation
at any point
of the leg generally
evoked
a fiexion-withdrawal
reflex.
Theoretically,
there
would
be a third
group
in which
patients
would
have a
“skip
long
normal
lesion”.
descending
cord
In these
tracts
showing
and then linking
would
then expect
area
there
and
the
of lower
patients
running
no lower
up with
to find
motor
there
would
through
an
motor
an intact
voluntary
neurone
neurone
segment
movement
denervation.
infants
and
we studied
and adolescence;
the type
change
with
age because
be normal
area of abfunctions,
below.
One
below the
In our
series
were no patients
with a “skip lesion”.
Stark
and Baker
(1967)
examined
newborn
infants
presented
a study similar
to ours. They found
3% of
spina
bifida
patients
to be neurologically
normal;
patients
in
of neurological
of associated
as a spacecord. (2) All
care
of the
senior
author
(MBM);
this would
exclude
neurologically
normal
or near normal
children
as they would
not have
been referred
for orthopaedic
care.
In the present
study.
each group
was divided
into
subgroup
A, those
with normal
upper
limbs,
and subgroup
B, those
with spasticity
in the upper
limbs.
Spasticity
shunts
in the upper
limbs
required
to control
B subgroups
those
had
pendence
and 70%
activities.
schooling:
limb
as
many
spasticity
to the number
of
Patients
in the
shunt
operations
adversely
as
affected
inde-
in activities
of daily living:
8 1 % of Group
ofGroup
IIA were independent
in feeding,
and dressing
Group
IIB
Upper
only 4 of 10 children
IIB attended
normal
and were within
their
chronological
lB and
lB
three
related
Group
two
3 of
thoracic
and
lumbar
All patients
with sacral
IA. One would
not
II as the plaque
would
functioning
spinal
cord
IA
per-
ofGroup
in all
also seemed
and 77%
of
in Group
schools.
Patients
with
in all groups.
were in Group
lesions
in Group
there to be any
while only 60%
were independent
limb spasticity
of Group
IA
85%
attended
normal
school
their
expected
level for
found
ever,
was related
hydrocephalus.
twice
in A. Upper
sonal hygiene
and 29%
of
classified
according
to the level of the
This study
demonstrates
that the type
tic or flaccid,
two grades
of
age. Patients
special
schools.
Six of the 10 chilI I ofthe
18 in Group
[lB attended
DISCUSSION
with spina
newborn
central
nervous
system
abnormalities
such
occupying
lesion or tethering
ofthe
terminal
our patients
were
under
the orthopaedic
for the disabled.
patients
studied
hospital
Scholastic
ability
was correlated
with
the
the upper
limbs.
Eighty-five
per cent
of
in Group
IA and 77% ofpatients
in Group
hA
school
and were within
for their
chronological
They
late childhood
lesion
might
of
attended
a normal
the expected
level
43% similar
to our Group
I; 50%
similar
to our Group
II; and 3% had “skip lesions”.
The differences
between
our series and theirs
may be related
to the following.
( I)
and
patients
admissions
for orthopaedic
procedures
averaged
3, 5, 4
and 5 per patient
respectively
for Groups
IA, lB. IIA and
IIB. and the number
oforthopaedic
operations
averaged
4, 7, 6 and 7 per patient
respectively.
Periods
in plaster
casts
averaged
17, 30, 27 and 30 weeks
per patient
for
Groups
IA, lB. IIA and IIB respectively.
Schooling.
function
patients
M. MENELAUS
to
hA
grades
of
age. while
14 in Group
lesions
lesions,
expect
were
howsacral
be too caudal
for
below
the level of
the lesion.
One would
expect
sacral
lesions
in Group
lB
as it would
be possible
to have a sacral
plaque
and an
associated
cerebral
anomaly
creating
spasticity
above
the
plaque;
there were, however,
no such cases in the series.
more
Orthopaedically,
patients
with spasticity
difficult
to manage.
Patients
in Groups
IIB required
60% more orthopaedic
more operations
and longer
in casts
were much
lB. hA and
hospital
admissions,
than did patients
in
Group
IA.
Literature
in the past has related
walking
ability
to
the level
of the motor
lesion.
Our
patients’
walking
ability
compares
favourably
with those reports
(Hoffer
et
a!. 1973; De Souza
and Carroll
1976; Feiwell,
Sakai
and
Blatt
1978; Stillwell
and Menelaus
1983).
Figures
comparing
walking
abilityto
neurosegmental
meaning.
however,
unless
the presence
spasticity
that
is taken
into
account,
Our
level have
or absence
data
clearly
little
of
shows
the presence
ofspasticity
adversely
affects
walking.
Patients
in Groups
lB and IIB were handicapped
abnormal
not only
upper
weaker
of crutches
Groups
IIA
limb functions;
these spastic
but less coordinated,
making
difficult.
and IIB,
THE
Spasticity
caused
JOURNAL
in the lower
impaired
overall
OF
BONE
AND
by
limbs were
the control
JOINT
limbs,
in
function;
SURGERY
THE
these
patients
had
SIGNIFICANCE
persistent
OF SPASTICITY
contractures
IN THE
and
lower
UPPER
limb
deformities
which hampered
orthotic
fitting and eventual
walking.
Patients
in Group
IA (flaccid
lower limbs,
with
normal
upper
limbs)
had the best prognosis,
functioned
best in activities
ofdaily
living and were the best walkers.
The observation
and documentation
of the precise
neurological
is important
child’s
status
for
potential
activities;
ofeach
child
three
reasons:
ability
(2) to give
to
realistic
with
(I)
walk
and
expectations
myelomeningocele
to determine
perform
AND
LOWER
LIMBS
created
one contracture
important.
therefore,
fled according
cid in addition
the motor
that
to whether
to grouping
their limbs arc
them according
wish
to thank
ofthe
manuscript.
Vicki
De Souza U, Carroll
N. Ambulation
patient.
J Bone
Joint
Surg
(Am]
altered
if spasticity
nise the difference
voluntary
voluntary
VOL.
68--B.
into
control
control.
No.
account
of patients
management
is present.
between
1986
evaluation,
with
may
myelomenneed
to
be
The surgeon
must
recoga spastic
muscle
under
no
and an overpowering
Transferring
a spastic
2. MARCH
in the
Ann
Jones
for
the
muscle
under
muscle
that had
of the braced
mvelomeningocele
1976:58
A: I I I 2 8.
E, Sakai I), Blatt T. The effect of hip reduction
patients
with
myelomeningocele:
potential
gains
surgical
treatment.
J BoneJoint
Su[Ain]
1978:60
Hoffer
MM,
Feiwell
lation
in patients
1973:55
A:137
Menelaus
MB. T/zt’ orthopat’du
ed. Edinburgh
etc: Churchill
WJW.
Spina
Smith
ED. Spina
Springfield,
Stark
GD, Baker GC.
in myelomeningocele.
Stark
GD,
Des
in
of
on function
and hazards
A: 169 73.
F, Perry R, Perry J, Bonnett C. Functional
ambuwith myelomeningocele.
J Bone Joint .Surg [.4i;z]
48.
Sharrard
taken
and
Feiwell
cance
be
Morris
REFERENCES
to the parents;
Sharrard
WJW.
Meningomyelocele:
closure ofthe sac. Proc Soc
and prognosis
Orthopaedic
spastic
or flacto the level of
the
normal
pniate surgery.
The orthopaedic
surgeon.
more
than any
other
clinician
managing
these patients.
has the greatest
opportunity
to observe
neurological
deterioration.
Spasticity
is clearly
an important
factor.
Its signifishould
may simply
lead to another.
It is
these patients
should
be classi-
lesion.
The
authors
preparation
and (3) to decide
on the appropriate
management.
In
addition,
it is important
to observe
any deterioration
in
the neurological
status
which
may, ifdue
to syningomyeha or cord tethering.
be stabilised
or improved
by appro-
treatment,
ingocele.
217
IN MYELOMENINGOCELE
hifida
Illinois:
hifida.
0/
Livingstone.
hifida
S1fl(1
prognosis
i/ic total
Thomas,
neurological
Lb’s Med
of immediate
1963h:
involvement
.Veurol
Drummond
M. The spinal cord
itled Child A/euro!
197 I : 13 suppl
operative
12.
I : 190
care Of s,;iiial
1965.
Child
2nd
(v.stica.
1980.
i%-Ied 1963a:56:5l()
Paraplegia
and
CC
The
?;lciFzag(’nle?lt
9.
I?1v(’lolnc!un,gocelc.
of the lower limbs
1967:9:
732 44.
lesion in myelomeningocele.
25: 1 15.
Stillwell
A. Menelaus
MB.
Walking
ability
in mature
spina
hifida.
.1 Pediatr
On/sop
1983:3:
184 90.
patients
with