Ectopic Pancreas in the Ampulla of Vater with Obstructive Jaundice
advertisement

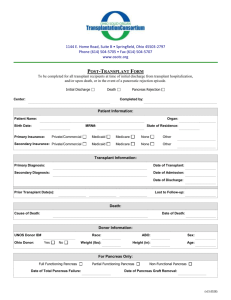
Dig Surg 2006;23:262–264 DOI: 10.1159/000096158 Ectopic Pancreas in the Ampulla of Vater with Obstructive Jaundice A Case Report and Review of Literature Shao-Jiun Chou a, b, Yu-Wei Chou a, Hsiang-Chun Jan a, b, Victor T.K. Chen a, b, Tzu-Hung Chen a, b a Division of General Surgery, Department of Surgery, Cardinal Tien Hospital, College of Medicine, Fu Jen Catholic University, and b Tri-Service General Hospital and National Defense Medical Center, Taipei, Taiwan/ROC Key Words Ectopic pancreas Ampulla of Vater Periampullary tumor Total ampullectomy Sphincterotomy Abstract Ectopic pancreas is an uncommon condition and is usually found in the gastrointestinal tract, such as stomach, duodenum and jejunum. However, ectopic pancreas in the ampulla of Vater is rare and its clinical presentations may be similar to periampullary cancer. It is difficult to diagnose preoperatively. We present such a case where the diagnosis was proven postoperatively. Our patient, a 51-year-old man, presented with epigastric pain, jaundice, weight loss and abnormal laboratory data. Imaging study, including abdominal sonography, abdominal computerized tomography with contrast and endoscopic retrograde cholangiopancreatography, showed a mass protruding into the ampulla of Vater. The mass was resected and histological examination revealed an ectopic pancreas. The patient presented with symptoms of periampullary tumor but the imaging study did not reveal an obvious lesion for us consider the possibility of ectopic pancreas. Surgical excision is indicated for symptomatic Copyright © 2006 S. Karger AG, Basel cases. 1 2 Introduction Ectopic pancreas is defined as pancreatic tissue that lacks direct or vascular connection to normal pancreas [1]. Ectopic pancreas is an uncommon condition. In 70% of the cases it is found in the stomach, duodenum and jejunum [2]. We present a case of ectopic pancreas in the ampulla of Vater (AoV). Only several such cases have been reported in the literature [3–9]. The common presenting symptoms include epigastric pain and jaundice [2]. Our case also had weight loss and abnormal laboratory data, which were not seen in previous reports. Case Report A 51-year-old man presented with epigastric pain for almost 1 year. The pain was dull, intermittent and non-referring. He had a weight loss of 5 kg within 4 months. He consulted a local hospital and was treated for gastritis. Physical examination on admission showed epigastric tenderness, gross jaundice and recent 262 Fig. 1. Marked dilatation of intrahepatic biliary ducts (arrow). Fig. 2. The CBD was dilated in the ampullary region (arrow) and the pancreas was swollen. weight loss. Laboratory data included normal hematocrit and WBC, but elevated serum amylase 806 U/l (normal 20–120 U/l), lipase 1,229 U/l (normal 8–57 U/l), -GT 751 U/l (normal 7– 50 U/l), ALT 195 U/l (normal 10–60 U/l), APT 103 U/l (normal 5–40 U/l), total bilirubin 10.6 mg/dl (normal 0.4–2 mg/dl), direct bilirubin 8.54 mg/dl (normal 0–0.4 mg/dl), and LDH 291 U/l (normal 98–192 U/l). Tumor markers of CA 19-9 was 209.69 U/l (normal 0–37 U/l), CEA was 4.93 ng/ml (normal !5 ng/ml), and AFP was 1.7 ng/ml (normal ! 20 ng/ml). Chest and abdomen Xrays were unremarkable. Abdominal sonography showed a dilated common bile duct (2.0 cm) and dilated intrahepatic ducts. Abdominal computerized tomography (CT) revealed a dilated com- Case Reports 3 5 4 6 Fig. 3. ERCP showed a protruding mass at the AoV. Fig. 4. Distal CBD showed marked narrowing with near total ob- Fig. 5. AoV showed gross hypertrophy without the mass. Fig. 6. Histopathological sections showed pancreatic acini and struction. ducts. mon bile duct extending down to the ampullary region (fig. 1, 2). Endoscopic retrograde cholangiopancreatography (ERCP) showed a dilated common bile duct and a mass protruding into the AoV (fig. 3, 4). A biopsy was done and revealed chronic inflammation. The Whipple procedure was performed due to the suspicion of tumor of AoV. The resected specimen of ampulla showed gross hypertrophy without the mass (fig. 5). Histological evaluation revealed a mixture of pancreatic acini and ducts (fig. 6). The postoperative course was smooth and the patient was discharged on postoperative day 10. During the postoperative follow-up his symptoms were relieved and laboratory data returned to a normal range. Case Reports Discussion The diagnosis of ectopic pancreas is easy if it shows the typical landmark of ‘central dimpling’. However, in our case, such a characteristic sign was not seen. The ectopic pancreatic tissue may be too small and difficult to see near the orifice of the AoV. Ectopic pancreas is usually asymptomatic, but it is capable of producing clinical symptoms, depending on its location and size [10]. In reviewed reports, the most common sites include stomach, duodenum, and jejunum, which account for about 70% of cases [2]. Only a few cases have been reported in the AoV. The sizes reported range from 2.0 to 25 mm [3–9]. The most common 263 presenting symptoms were abdominal pain (45.5%) and epigastric discomfort (12.0%). In our case, ectopic pancreas located in AoV presented with epigastric pain, gross jaundice and weight loss. The symptoms of ectopic pancreas in the AoV are similar to those of periampullary cancer. It is very difficult to differentiate them based on clinical symptoms alone. Useful imaging study of the periampullary region includes abdomen sonography, endoscopic ultrasonography (EUS), abdomen CT, magnetic resonance imaging (MRI), and ERCP. Abdominal sonography may not provide much information in such patients, as in our case, because the ectopic pancreatic tissue is small and located in the submucosal layer of AoV [11]. In EUS the ectopic pancreas in the gastrointestinal tract appears hypoechoic or has mixed echogenic lesions in the submucosa [12]. EUS features of ectopic pancreas in AoV have not been reported. Abdominal CT can evaluate the internal organs near to the periampullary region and rule out any periampullary abnormality. ERCP with biopsy is the most important tool in such cases. Ectopic pancreatic tissue may show the ‘central dimpling’ in ERCP if the tissue is large enough. Endoscopic sphincterotomy may supply larger specimens for diagnosis, however it has more complications, such as hemorrhage, perforation, or pancreatitis. Hayes-Jordan et al. [13] pointed out ectopic pancreas is associated with muscle hypertrophy. Gaspar Fuentes et al. [14] divided ectopic pancreas into four types: type I composed of all cell types (total heterotopia); type II composed of ducts only (canalicular heterotopia); type III composed of acinar cells only (exocrine heterotopia), and type IV composed of islets of Langerhans only (endocrine heterotopia). However, in our case, histological findings revealed a mixture of acini and ducts. The management of ectopic pancreas depends on the presence of symptoms or not. If the patient is asymptomatic, conservative treatment with regular follow-up is recommended. If the patient is symptomatic, as our case, surgical management is indicated. The size and location of ectopic pancreatic tissue determine what kind of procedure should be performed. Tanaka et al. [15] recommended resection of the pancreatic tissue-bearing area, while Jochimen et al. [16] recommended surgical excision of ectopic pancreas if symptoms persisted after supportive treatment failed. If we can localize the ectopic pancreatic tissue preoperatively by imaging study, limited excision is needed. If ectopic pancreatic tissue is not well circumstanced, wide excision is recommended, such as total ampullectomy. However, wide excision may be technically difficult. We suggest biopsy and sphincterotomy to identify the anatomy and histology first, and then excise the area as much as possible without damaging the common bile duct and pancreatic duct. References 1 Barbosa JJ de C, Dockerty MB, Waugh JM: Pancreatic heterotopia: review of the literature and report of 41 authenticated surgical cases of which 25 were clinically significant. Surg Gynecol Obstet 1946;82:527– 542. 2 Kaneda M, Yano T, Yamamoto T, Suzuki T, Fugimori K, Itoh H, Mizumoto R: Ectopic pancreas in the stomach presenting as an inflammatory abdominal mass. Am J Gastroenterol 1989; 84:663–666. 3 Chen CH, Yang CC, Yeh YH, Chou DA, Kuo CL: Ectopic pancreas located in the major duodenal papilla: case report and review. Gastrointest Endosc 2001;53:121–123. 4 Hoelzer H: An occlusion of Vater’s ampulla by accessory pancreas. Zentralbl Chir 1940;67:1715–1717. 5 Varay A: Microscopic epithelioma of Vater’s ampulla. Paris Méd 1946; 1:183–186. 6 Pearson S: Aberrant pancreas. Review of the literature and report of three cases, one of which produced common and pancreatic duct obstruction. Arch Surg 1951;63:168–184. 7 Weber CM, Zito PF, Becker SM: Heterotopic pancreas: an unusual cause of obstruction of the common bile duct. Am J Gastroenterol 1968; 49:153–159. 8 Laughlin EH, Keown ME, Jackson JE: Heterotopic pancreas obstructing the ampulla of Vater. Arch Surg 1983;118:979–980. 9 Kubota K, Bandai Y, Watanabe M, et al: Biliary stricture due to mucosal hyperplasia of the common bile duct: a case report. Hepatogastroenterology 1996;43:14. 10 Armstrong CP, King PM, Dixon JM, Macleod IB: The clinical significance of heterotopic pancreas in the gastrointestinal tract. Br J Surg 1981;68:384–387. 11 Dolan RV, Remine WH, Dockerty MB: The fate of heterotopic pancreatic tissue: a study of 212 cases. Arch Surg 1974;109:762–765. 12 Matsushita M, Hajiro K, Okazaki K, Takakuwa H: Gastric aberrant pancreas: EUS analysis in comparison with the histology. Gastrointest Endosc 1999;49:493–497. 13 Hayes-Jordan A, Idowu O, Cohen R: Ectopic pancreas as the cause of gastric outlet obstruction in a newborn. Pediatr Radiol 1998; 28: 868– 870. 14 Gaspar Fuentes A, Campos Tarrech JM, Fernandez Burgui J: Ectopias pancreaticas. Rev Esp Enferm Apar Dig 1973;39:255–268. 15 Tanaka K, Tsunoda T, Eto T, Yamada M, Jajima Y, Shimogama H, et al: Diagnosis and management of heterotopic pancreas. Int Surg 1993; 78: 32–35. 16 Jochimsen PR, Shirazi SS, Lewis JW: Symptomatic ectopic pancreas relieved by surgical excision. Surg Gynecol Obstet 1981; 153:49–52. Tzu-Hung Chen, MD Division of General Surgery, Department of Surgery Cardinal Tien Hospital 362, Chung Cheng Rd. Hsintien Taipei Hsien 23137 (Taiwan/ROC) Tel. +886 2 2219 3391 66711, Fax +886 2 8665 9727 E-Mail surgery6711@sina.com.tw Acknowledgement We thank Miin-Fu Chen, MD, President of the Taiwan Surgical Association, for his help in revising the manuscript. 264 Case Reports