BLS-CPR HANDBOOK
advertisement

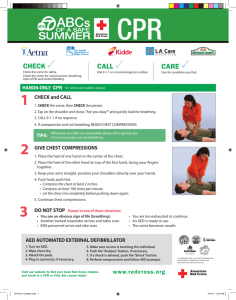
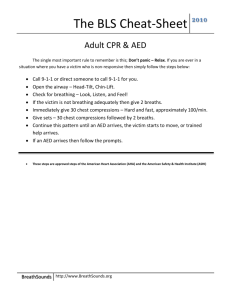
BLS-CPR HANDBOOK BLS-CPR Handbook CPR UPDATES • • • • • • • • • • • • • CPR SEQUENCE Changed from: ABC (airway, breathing, circulation) to CAB (circulation, airway, breathing) The following order is now recommended 1.Check the patient for responsiveness and breathing 2. Call for help and get the AED 3. Check the pulse 4. Give 30 compressions 5. Open the airway and give 2 breaths 6. Resume compressions Rapid circulation of already oxygenated blood is essential to survival. Compressions are the critical element in adult resuscitation. The ABC sequence delays compressions. PULSE CHECK – • • COMPRESSION RATE – • Take no longer than 10 seconds to check for a pulse. If no pulse is detected begin compressions without delay. Compressions should be given at a rate of at least 100 / minute. Each set of compressions should take 18 seconds or less. Faster compressions maintain perfusion pressures required to supply blood to the coronary and cerebral arteries. COMPRESSION DEPTH – – – – New compression depths are as follows: Adult--- at least 2 inches (5 cm) Child--- at least 1/3 the depth of the chest approx. 2 inches (5 cm) Infant—at least 1/3 the depth of the chest approx. 1.5 inches (4 cm) BLS-CPR Handbook CPR UPDATES • AIRWAY AND BREATHING • CRICOID PRESSURE – Cricoid pressure is no longer routinely recommended for use with ventilations. Cricoid pressure still allows aspiration and it is difficult to train providers to perform the maneuver correctly. • LOOK, LISTEN, FEEL – This step has been removed from the sequence entirely. Checking for breathing is done during the responsiveness / signs of cardiac arrest phase. After the first set of 30 compressions, lone rescuers open the airway and give 2 breaths. • • AED USE • CHILDREN 1-8 YEARS OLD – AED with a pediatric dose attenuator is preferred – If a pediatric AED is not available a standard AED may be used. • INFANTS < 1 YEAR OLD – A manual defibrillator is preferred – If a manual unit is not available a pediatric dose attenuator may be used. – If neither of the above units are available a standard AED may be used. BLS-CPR Handbook SCENE SAFETY • SCENE SAFETY • While you may want to rush in and start CPR to save the victim it should not be done with risk to your own safety and possibly your life. The time to check scene safety is before you begin CPR. Some examples of an unsafe scene are: – A vicious dog or dogs – An insane or armed and dangerous person or persons – A room filled with a noxious gas – Motor vehicle accident with an unstable vehicle – Downed electrical lines – Scene involving an industrial accident • If the scene is unsafe call 911 and do nothing until they arrive and secure the scene! BLS-CPR Handbook ONE RESCUER CPR (ADULT) • SEQUENCE – – – – – – – – • Check the patient for responsiveness and breathing Call for help and get the AED. Check the pulse ( < 10 seconds) Give 30 compressions Open the airway and give 2 breaths Resume compressions Repeat for 5 cycles of compressions and breaths and check pulse. If no pulse resume CPR in 5 cycle increments CHECKING RESPONSIVNESS AND BREATHING – Check responsiveness and look for movement or signs of life – Check for breathing (agonal breathing is the same as no breathing) • CALL FOR HELP AND GET THE AED – The earlier the AED is applied the better the chance of survival – The earlier ALS (911) arrives the better the chance of survival – CPR is exhausting. You will need relief in order to do good CPR • CHECK THE PULSE – Check the pulse at the carotid artery for adults – Check 5-10 seconds but not longer than 10 seconds BLS-CPR Handbook ONE RESCUER CPR (ADULT) • • • • COMPRESSIONS COMPRESSION / VENTILATION RATIO 30 compressions to 2 breaths Breaths are 1 second duration • • • • • • COMPRESSION RATE The compression rate is at least 100 / minute COMPRESSION DEPTH The compression depth is at least 2 inches (5 cm) HAND PLACEMENT FOR COMPRESSIONS The hands are placed over the lower half of the sternum • FULL CHEST RECOIL • – • • OPEN THE AIRWAY AND GIVE 2 BREATHS Open the airway by – – – • Head tilt chin lift if there is no evidence of trauma Jaw thrust if there is evidence of trauma If you cannot open the airway with a jaw thrust use head tilt chin lift BREATHING – – – • Always allow the chest to fully expand to allow the vena cava to fill and maximize blood flow to the heart. Give 2 breaths 1 second in duration Breathe just enough to make the chest rise Forceful breaths will fill the stomach with air RESUME COMPRESSIONS AND VENTILATIONS – – – Repeat 5 cycles of 30 compressions and ventilations At the end of 5 cycles check for a pulse If no pulse continue CPR BLS-CPR Handbook ONE RESCUER CPR (ADULT) • • BREATHING RESCUE BREATHING – • BREATHING WITH AN ADVANCED AIRWAY – – – • Completely cover the victim’s mouth with yours Pinch the nostrils shut Open the airway (head tilt chin lift or jaw thrust) Give 1 second breaths just enough to make the chest rise MOUTH TO MASK – – – – • There are 4 methods to apply breaths Mouth to mouth Mouth to mask Ambu bag with mask Ambu bag directly attached to an advanced airway device MOUTH TO MOUTH – – – – • Advanced airways are devices inserted into the trachea, esophagus, or the oropharangeal region to gain control of the airway. They are put in place by doctors, respiratory techs. Paramedics, ore other trained persons. Examples of advanced airways are endotracheal tubes, LMA’s, Combi tubes. When these airways are in place, ventilate the patient at a rate of 6-8 breaths per minute. These breaths are on going and interposed between compressions. BREATHING METHODS – – – – – • If an adult victim has a pulse but is not breathing give rescue breaths at a rate of 12-20 breaths per minute (about 1 breath every 5-6 seconds). Fit the mask to the patient Apply the EC technique to both sides of the mask Open the airway (head tilt chin lift ) Give 1 second breaths just enough to make the chest rise AMBU BAG WITH MASK – – – – – Fit the mask to the patient Grasp the mask using the E C technique Put the head in the head tilt position Give 2 breaths enough to make the chest rise The ambu bag requires 2 rescuers to insure an adequate mask seal BLS-CPR Handbook AUTOMATED EXTERNAL DEFIBRILLATOR • AED • Adult cardiac arrest victims die from either of 2 rhythms – – ventricular tachycardia ventricular fibrillation • Ventricular fibrillation is the most common cause. During ventricular fibrillation the ventricles quiver and do not pump blood due to the random chaotic electrical activity. • The defibrillator produces an electrical charge across the heart that momentarily stops all electrical activity. After defibrillation a meaningful electrical activity or rhythm will occur. • Do not delay defibrillation. Early defibrillation is essential. The earlier defibrillation is performed: – – • The better the chance of survival The less energy is required All new AED units are designed to deliver a single shock and defibrillate only the following rhythms: – – ventricular tachycardia ventricular fibrillation BLS-CPR Handbook AUTOMATED EXTERNAL DEFIBRILLATOR • • • All AED devices operate in basically the same manner. These devices will talk you through the process. The basic sequence is as follows; Power on the AED Attach the pads as shown on pads – – • • Analyze the rhythm (do not touch the patient) The machine will respond with either of 2 responses – – • • • • • • Continue CPR for a full 5 cycles and reanalyze rhythm Proper pad contact is essential for effective defibrillation. To insure good pad contact; Do not apply pads if patient is wet or in a puddle of water Remove patient from water and dry patient of Dry diaphoretic patients before applying pads Wipe off nitroglycerine and other ointments If patient has a hairy chest – – • Charging CLEAR PATIENT Deliver the shock Resume CPR for a full 5 cycles and reanalyze rhythm No shock advised – • Shock advised No shock advised Shock advised – – – – • Anterior / anterior Anterior / posterior Shave the area where pads will be placed Apply pads and pull off hair. Then reinstall pads Do not apply pads near an implanted pacemaker BLS-CPR Handbook TWO RESCUER CPR (ADULT) • SEQUENCE • BOTH RESCUERS ARRIVE AT THE SAME TIME – – – – – – 1. 2. 3. 4. 5. 6. First rescuer confirms arrest and begins CPR and continues CPR Second rescuer calls 911 and gets the AED Second rescuer turns on AED and applies pads Second rescuer sets up on the opposite side from the first rescuer Rescuers switch roles during the analysis phase If a shock is indicated • • a. The AED will charge b. Shock will be advised BOTH RESCUERS MUST BE SURE TO CLEAR THE PATIENT! – – – – • 7. Deliver the shock 8. Immediately resume CPR 9. Second rescuer does compressions 10.First rescuer manages the airway and does ventilations 2 RESCUER PEARLS – – – – – – – – – 1. 2. 3. 4. 5. Communicate Count compressions out loud Locate on opposite sides of the patient Minimize interruptions in CPR to 10 seconds CPR should only be interrupted during analysis and delivery of shock 6. Change rescuers doing compression at the end of every 5 cycles 7. Rescuer doing ventilations should check carotid pulse to evaluate CPR quality BLS-CPR Handbook CHILD CPR • • • • • • CHILD: – is defined as 1 year old to puberty – Puberty is defined as: – Chest or armpit hair on males – Breasts on females OXYGENATION: Oxygen is more important in child CPR Adults arrest due to cardiac failure – (Hemoglobin is fully saturated with oxygen) – Children arrest due to respiratory failure – (Pre-arrest hypoxia does not fully saturate the hemoglobin) As a result: – Children require additional high quality oxygenation – Start 5 cycles of CPR before calling 911 – 2 rescuer CPR ratio (15:2) allows double the number of breaths DIFFERENCES BETWEEN CHILD AND ADULT CPR – When to activate the emergency response system. – If you did not witness the arrest and are alone, provide 2 minutes before leaving the child to activate 911 and get the AED. – If the arrest is sudden and witnessed leave the child, activate 911,get the AED and return to the child. – If the heart rate is less than 60 bpm with poor perfusion begin compressions. BLS-CPR Handbook CHILD CPR • COMPRESSIONS – – – – – – – Compression ratio1 rescuer CPR is 30:2 2 rescuer CPR is 15:2 Compression depth – at least 1/3 the depth of the chest approximately 2 in Compression technique-may use heel of 1 hand or 2 hands if necessary Compression hand location – lower half of the sternum Compression rate – at least 100 per minute • • PULSE CHECK Pulse check – femoral artery • BREATHING – CPR breaths – 2 breaths 1 second duration – Rescue breaths – 1 breath 1 second duration every 3-5 seconds bpm) Advanced airway- 1 breath 1 second duration every 6-8 seconds bpm) Interposed between compressions – • All breaths – Just enough volume to make the chest rise – – – – – – – – – – CASES CASE 1 - Child is pulse less and apnic Start CPR CASE 2 – Child has a pulse < 60 bpm and not breathing Start compressions and ventilations (CPR) CASE 3 – Child has a pulse < 60 bpm and is breathing Start compressions only CASE 4 – Child has a pulse > 60 bpm and is not breathing Give breaths only CASE 5 – Child has a pulse > 60 bpm and is breathing Monitor patient BLS-CPR Handbook (12-20 (8-10 INFANT CPR • INFANT: – is defined as birth through 1 year old • KEY DIFFERENCES IN CPR FOR INFANTS • • Location of pulse check --- Brachial artery Start compressions – – • Compression technique – – • Use 2 finger technique for single rescuers Use 2 thumb encircling technique for 2 rescuer CPR Compression depth – • If there is no pulse If the heart rate is < 60 bpm with poor perfusion At least 1/3 the depth of the chest 11/2 in. 4 cm) Compression: ventilation ratio – – 1 rescuer – 30 compressions to 2 ventilations 2 rescuer - 15 compressions to 2 ventilations • Full chest recoil • When to activate the emergency system – – – – • Non witnessed arrest and alone 2 minutes of CPR before activating 911 and getting AED Sudden witnessed arrest Leave the infant, call 911 and get the AED Breathing – – – CPR – 2 breaths 1 second duration Rescue breaths – 1 second breaths 3-5 times per minute 12-20 bpm) Provide volume just enough to make the chest rise BLS-CPR Handbook INFANT CPR • CASES • CASE 1 Infant is pulse less and apneic Start CPR • CASE 2 Infant has a pulse < 60 bpm and is not breathing – Start compressions and ventilations (CPR) • CASE 3 Infant has a pulse < 60 bpm and is breathing – Start compressions only • CASE 4 Infant has a pulse > 60 bpm and is not breathing – Give rescue breaths only • CASE 5 Infant has a pulse > 60 bpm and is breathing – Monitor patient • 1 RESCUER SEQUENCE (INFANT) – Assess infant for response and breathing – Shout for help • • If someone responds activate 911 and get AED If no one responds continue with CPR protocol – Check brachial pulse ( <10 seconds) – No pulse or pulse <60 bpm and not breathing • Begin CPR at 30:2 – After 5 cycles activate 911 and get AED BLS-CPR Handbook INFANT CPR • 2 RESCUER CPR (INFANT) • Assess responsiveness, breathing and pulse • Rescuer 1 – Does compressions using the 2 thumb hand encircling technique – Compression depth – at least 1/3 depth of the chest – Compression rate at least 100 per minute – Full chest recoil • Rescuer 2 – Calls 911, gets the AED and prepares to ventilate • (compression to ventilation ratio 15:2) – Stops at the end of each 15 compressions to allow 2 ventilations – Breaths - 1 second duration just enough to make the chest rise. BLS-CPR Handbook CHOKING • ADULT AND CHILD VICTIMS • If the patient can cough forcefully, speak, and is able to exchange air let them alone and monitor them. • If the patient cannot breathe or cough, puts their hands to their throat, is having respiratory difficulty, or is turning blue, begin the Heimlich maneuver until the object is dislodged or the patient becomes unconscious. • • • • • • If the victim becomes unconscious: 1. Activate the emergency system 2. Lower patient gently to the ground 3. Begin CPR starting with compressions 4. Do not check for a pulse 5. Every time you give breaths look for object. Remove if visable. • Pregnant women and obese patients go directly to CPR. Chest compressions are used in place of the Heimlich maneuver. • INFANT CHOKING • If the infant is coughing forcefully, has good air exchange, and good color leave them alone and monitor them • If the infant is unable to cough, has poor air exchange, becomes cyanotic,or is making a high pitched noise, give 5 back blows followed by 5 chest thrusts until the infant becomes unconscious. • • • • • • If the infant becomes unconscious or is found unconscious, 1. lay them on a hard flat surface 2. activate the emergency system 3. begin CPR starting with chest compressions 4. when you ventilate look for the object 5. if visible remove it BLS-CPR Handbook