Case Studies in Family Planning
advertisement
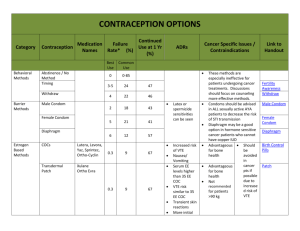
Case Studies in Family Planning Jennifer McCaul MD Family Medicine Refresher Course March 6, 2015 Unintended Pregnancy Of 3.2million pregnancies per year in US- 49% are unintended. › 43% of unintended pregnancies end in termination. › Highest rate in teens and young adults.- almost 10% 18-24 year olds yearly. › Obese women are at higher risk of unintended pregnancy. › Women > 40 have the second highest rate of unintended pregnancy. › Patient Driven Contraception Selection › › Selection of best family planning method for your patient requires working together. Questions to ask: › › › › › › › › › › › › › › › › › pMHx? Smoker? Male or female partners? FHx stroke or blood clots? Age? Frequency of intercourse? Need for STD protection? Are you good at taking meds? Need for non-contraceptive benefits? Cost? Desired degree of permanence? Comfort with insertion/vaginal? Tolerance of irregular bleeding? Weight? Breastfeeding? Baseline menstrual characteristics? What has worked/not worked in past? What are the options? › › › › › › › › › Combined oral contraceptives (COCs) Natural family planning/fertility awareness Withdrawal Progestin-only pill Depo-Provera Copper IUD (Paragard) Levonorgestrel IUD (Mirena, Skyla) Emergency contraception Spermicides Progestin Implant (Nexplanon) › Nuva Ring › Evra Patch › Diaphragm › Male Condoms › Female condoms › Tubal ligation › Essure › Lactational Amenorrhea › Vasectomy › Effectiveness of Family Planning Methods › Effectiveness ranges › Most effective with <1 pregnancy/100 women/ 1year › Implant, › More effective › Depo, › IUD, vasectomy, Tubal, essure LAM, pills, patch, ring Less effective › Condoms, › diaphragm, FAM Least effective with approx 30 pregnancies/100 women/1year › Withdrawal, spermicides Choosing the right method › If difficulties arise: › WHO and CDC both have published, easily accessible guidelines regarding elegibility for contraception and recommended methods for comorbid diseases. Nexplanon Etonorgestrel implant Good for 3 years 0.05% failure rate Implanted into biceps groove in office visit Removed through sm incision Manufacturer training mandatory Menstrual irregularities common Acne/wt gain less common Likely less effect on BMD then depo Paragard Copper IUD Effective for 10 years Menses are heavier NSAIDs effective to decrease No hormone side effects >99% Effective – typical use Mirena Levonorgestrel releasing IUS Local progestin Effective for 5 years Menses Lighten- approved for treatment of menorrhagia Hormone side effects are rare >99% effective -typical use Skyla Low dose LNG-IUS Good for 3 years Less progestin side effect Radio-opaque ring to allow x-ray visualization Depot Medroxyprogesterone Acetate Every 3 mo intramuscular inj Can initiate any time if preg (-) Back up for 7 days if not within 5 days of start of menses Highly effective 96% Wt gain- worse in obese women Bleeding irregularly Decrease BMD-returns after stopping DEXA not recommended Delayed fertility return Combined Oral Contraceptive Pills (COCs) Safe for most young women Typical use effectiveness 92% Benefit – acne treatment and regulated cycles Many contraindicationsparticularly in older women with comorbid conditions May be less effective in obese women Also 3 mo- Seasonale, Seasonique 12 mo- lybrel Contraceptive Patch (Evra) Weekly transdermal patch Estrogen and progesterone Continuous delivery Less effective in wt > 90 kg Higher risk of VTE Vaginal Contraceptive Ring (Nuva) 3 wks in, 1 wk out Lowest estrogen dose- continuous Use back up if out > 3 hrs And now for the Cases…. Mary is a 46 year old who has been on the pill for many years and still does not want to become pregnant. She is a non-smoker, nl BMI and otherwise healthy. Which of the following could be a good option for her? › A. Continue the OCP › B. Place a paragard › C. Refer for Tubal › D. Place a Nexplanon › E. Tell her to stop pill and not to worry, she probably can’t get pregnant › F. All of the above › G. A, B, C and D When to stop the Pill? In a non-smoker, in absence of other adverse clinical conditions, the pill can generally be safely continued to menopause. › Check FSH annually on day 6-7 of the placebo pills to decide if the pill can be discontinued. › There may be a small increased risk of breast cancer in pill users. › There is probably a decreased risk of ovarian and endometrial cancer with pill usage. › There is an increased incidence of VTE and risk factors should be re-evaluated often. › How to start the Pills….. › If a new start or has been off pill for a while Quick start- if pregnancy test negative and > 5 days since LMP then barrier for 5-7 days › BP should always be checked › Jill is a 25 yo G1P1, in a monogamous relationship, wishes to space her pregnancies. She is 64”, 225 lbs. and still trying to lose her baby weight. She wonders what the best method for her is. Which is the least appropriate method for her? A. LNG-IUS › B. Depo › C. OCP › D. Copper IUD › Best options for the Obese patient Depo-provera causes up to 20 lb wt gain › OCP associated VTE risk increases in obese patients, use particular care in smokers › › WHO identifies BMI >25 as an independent risk factor for VTE with OCP use. Obese OCP users are 2X as likely to have arterial embolic disease or MI as non-obese › Contraceptive patches are less effective in obese women and recommended to be used only with caution in women >90kg. › Vaginal ring contraception is not thought to be affected by weight. › Kari is a 16 yo G0P0 who presents for her initial gyn visit and asks for contraception, she has recently become sexually active with her first partner. Non-smoker. Regular menses. › You first appropriately recommend: A. A pap smear › B. A complete gyn exam › C. Screening for Chlamydia › D. Telling her mother › You ask Kari a number of questions and find out she has a hard time keeping to a regular schedule and does not think she will remember pills. › Turns out she is not alone: OCP Adherence in Adolescents 45% at 3 mos 33% at 12 mos › › Options you offer her include: Patch › Ring › IUD › Implant › Condoms (for STD protection alone) › Which of the following is true about intrauterine contraceptive use in adolescents? A. If the patient is found to have STD at the time of insertion, the IUD should be removed › B. IUDs are no more likely to be expelled when inserted in nulliparous patients than in their parous counterparts. › C. Unintended pregnancy is up to 22X more frequent in short acting contraceptive users than in adolescents using LARC. › D. Adolescents who use LARC are more likely to be infertile later in life. › The “Active” Adolescent › › › › › › › 42 percent of US teens aged 15-19 have had sexual intercourse. 82 percent of adolescent pregnancies are unplanned. Short acting methods have higher discontinuation rates and higher pregnancy rates than LARCsand are chosen by a majority of teens. Intrauterine device usage is safe in adolescents, does not increase infertility, does not increase risk of PID after 20 days after insertion. If STD+ at time of insertion, leave in place and treat. Although IUDs can be inserted relatively easily in nulliparous patients there may be a higher risk of expulsion in these patients. No benefit from misoprostol. Be sure to counsel about cost, confidentiality and expected changes in menstrual cycle. Tina is a 20 year old university student who presents to your clinic 8 hours after an episode of intercourse with her boyfriend during which they noticed that the condom “broke.” She is worried about preventing pregnancy. With perfect use of condoms the failure rate is 14% at one year. › FYI…..NO ONE has perfect use of condoms › Tina has never used another method of contraception. After counseling Tina about her options at this stage, she opts for emergency contraception. Which of the following is true? A. She should not have any side effects at all from use of emergency contraception. › B. Emergency contraception requires a prescription. › C. Patients taking emergency contraception may not get their next menses for months. › D. It may be worthwhile to give a second dose on the prescription in case of vomiting within ½ hr of use. › E. EC must be taken within 12 hours of unprotected intercourse. › Emergency Contraception › Options include: › › › › › › › High dose Levonorgestrel (plan B, next choice) High dose COC (Yuzpe method- two-six tabs taken twice, 12 hr apart) Ullipristal (Ella) Copper IUD Placement All should be done within 5 days of intercourse Next menses generally within 1 wk of nl schedule. Progestin only typically more effective and with less side effects but all should be given with anti-emetics. Janet is a 36 year old G3P3 whose history includes a DVT in her last pregnancy. She has stopped her coumadin and is worried about unintended pregnancy, she asks you what she can do to prevent it, knowing hormones are risky. Your advice would be: A. Tubal ligation › B. Copper IUD › C. Natural family planning › D. Essure › E. Barrier methods › F. All of the above › G. None of the above › The patient who cannot tolerate hormones…. There are multiple non-hormonal methods available to this patient population. › Important questions to ask: › › When (if ever) do you want to become pregnant? › <5y- IUD (probably both fine), NFP, barrier methods › >5y- copper iud › How imperative is it that you avoid pregnancy? › Very- IUD › Not- NFP, barrier, withdrawal › Are you done with your childbearing? › Yes-Essure, tubal, vasectomy The patient with prior VTE The mechanism of increased risk of VTE is increased liver production of clotting factors. › In theory progestin only contraceptives (implant, IUD, Depo, mini-pill) should not increase risk of VTE. › Remember to inquire about menorrhagiacopper IUD can worsen this. › NFP/Fertility Awareness/Withdrawal › › › Effectiveness ranging from 3% annual pregnancy rate to 27%. Best for couples that are monogamous, mutually dedicated to avoiding contraception and for whom unplanned pregnancy is acceptable due to high failure rate. For more information including provider education courses http://www.usccb.org/issues-andaction/marriage-and-family/natural-familyplanning/what-is-nfp/science/nfp-education-forhealthcare-professionals.cfm Essure- An alternative to BTL Permanent › Non-hormonal › Office-Based hysteroscopy › Well-tolerated › Needs test for confirmation › Gwen is a 28 year old presenting to your office requesting contraception. PMHx of SLE and depression. Smokes 1ppd. BMI 32. BP 138/72. Which of the following is a contraindication to COCs? A. Borderline BP › B. SLE › C. Depression › D. Smoker › E. Obesity › Contraindications to COCs › Absolute VTE hx › SLE › Smoker >35 › Liver disease › Estrogen responsive tumor › Uncontrolled HTN › › Relative Smoker <35 › Depression › Migraine › Obesity › Family/personal history of Breast Cancer › Non-contraceptive benefits to OCPs Cycle regulation › Treatment dysmenorrhea/menorrhagia › Treatment of acne › Hormonal HA may improve with extended cycle › Decreased risk of endometrial and ovarian cancer. › Cindy is 22, nulliparous, has been on depo for 2 cycles. She is having irregular bleeding and is frustrated. She wants to know how long should she try to wait it out? › Amenorrhea with Depo › Month 1 › 50% have < 8 days monthly › 40% have 11-30 days › Month 3 › 30% amenorrhea › 35% 11-30 days › Month 12 › 60% amenorrhea › 80% 1-7 days spotting Treatment of Progestin only bleeding Can occur with mini-pill, IUD, implant and Depo › Can be treated with: › Estrogen alone- 21 days then 7 days break › COC- 21 days then 7 day break › NSAIDS- 5-7 days › › Levonorgestrel IUS- Average at 1year 10% bleed monthly › 20% amenorrhea › Sarah is a 31yo G4P4 who has had a Paragard IUD in for the last 4 years. She is generally happy with it but she could not feel the strings on her check this month. On exam you can not feel the strings. What is your next step? A. Quantitative HCG › B. Ultrasound › C. add COCs › D. reassure her- its probably still in there… › E. A and B › F. all of the above › Management of Missing IUD strings- Is it in the Abdomen, Uterus or Sewer? Managing Missing IUD strings You must find the IUD- Can’t assume it fell out, you must check KUB (if pregnancy is negative). › If b-HCG >1500- IUP should be visible- if not r/o ectopic › › › IUDs reduce total risk and number of ectopic and intrauterine pregnancies. However, the ratio of ectopic/intrauterine pregnancies is increased when an IUD is in place. If pregnancy on US, and the IUD is below it, pregnancy outcomes improve with removal. › If in place on TVUS and strings are not visible can leave in place until removal necessary, remove with removal device, remove with hysteroscopy. › Amy is a 24 yo G1P1 who is 3 months postpartum. She inquires about breastfeeding safe contraception that won’t affect her milk supply. Which of the following options is the least appropriate? A. Mirena IUD › B. COCs › C. Skyla IUD › D. Progestin only pill › E. Paragard IUD › F. Nexplanon implant › The Breastfeeding Mom Lactational amenorrhea method is a highly effective temporary method of contraception. › Another method of contraception must be used as soon as any of the following occurs: › › › › › menstruation resumes the frequency or duration of breastfeeding is reduced bottle feeds are introduced the baby reaches 6 months of age. Progestin only, copper IUD, and barrier contraceptive methods are all safe in the breastfeeding mom and will not affect her milk supply. › Progestin only minipill may be less effective at prevention of pregnancy than other methods. › Conclusion Successful initiation and maintenance of effective family planning requires collaboration between physician and patient and may prevent millions of unintended pregnancies yearly. › Talk with your patients and take time to explain side effects. It will result in better continuation rates and longer term success. › Questions????? Thank you References available on request.