Detection of choledocholithiasis by EUS in acute pancreatitis: a
advertisement
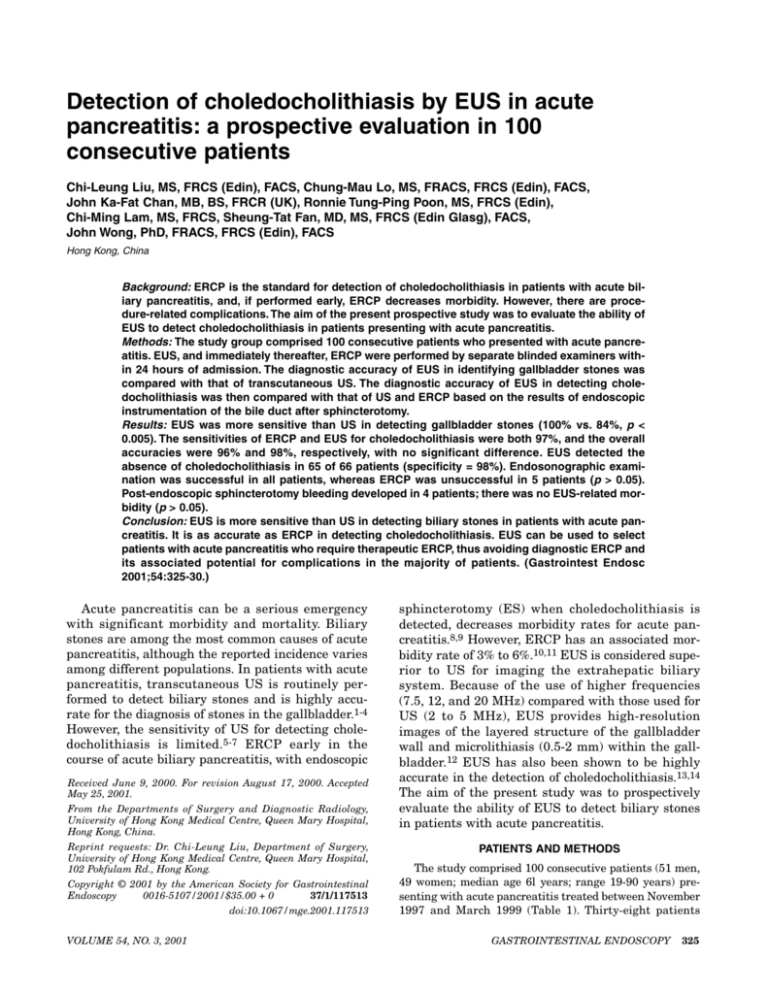
Detection of choledocholithiasis by EUS in acute pancreatitis: a prospective evaluation in 100 consecutive patients Chi-Leung Liu, MS, FRCS (Edin), FACS, Chung-Mau Lo, MS, FRACS, FRCS (Edin), FACS, John Ka-Fat Chan, MB, BS, FRCR (UK), Ronnie Tung-Ping Poon, MS, FRCS (Edin), Chi-Ming Lam, MS, FRCS, Sheung-Tat Fan, MD, MS, FRCS (Edin Glasg), FACS, John Wong, PhD, FRACS, FRCS (Edin), FACS Hong Kong, China Background: ERCP is the standard for detection of choledocholithiasis in patients with acute biliary pancreatitis, and, if performed early, ERCP decreases morbidity. However, there are procedure-related complications. The aim of the present prospective study was to evaluate the ability of EUS to detect choledocholithiasis in patients presenting with acute pancreatitis. Methods: The study group comprised 100 consecutive patients who presented with acute pancreatitis. EUS, and immediately thereafter, ERCP were performed by separate blinded examiners within 24 hours of admission. The diagnostic accuracy of EUS in identifying gallbladder stones was compared with that of transcutaneous US. The diagnostic accuracy of EUS in detecting choledocholithiasis was then compared with that of US and ERCP based on the results of endoscopic instrumentation of the bile duct after sphincterotomy. Results: EUS was more sensitive than US in detecting gallbladder stones (100% vs. 84%, p < 0.005). The sensitivities of ERCP and EUS for choledocholithiasis were both 97%, and the overall accuracies were 96% and 98%, respectively, with no significant difference. EUS detected the absence of choledocholithiasis in 65 of 66 patients (specificity = 98%). Endosonographic examination was successful in all patients, whereas ERCP was unsuccessful in 5 patients (p > 0.05). Post-endoscopic sphincterotomy bleeding developed in 4 patients; there was no EUS-related morbidity (p > 0.05). Conclusion: EUS is more sensitive than US in detecting biliary stones in patients with acute pancreatitis. It is as accurate as ERCP in detecting choledocholithiasis. EUS can be used to select patients with acute pancreatitis who require therapeutic ERCP, thus avoiding diagnostic ERCP and its associated potential for complications in the majority of patients. (Gastrointest Endosc 2001;54:325-30.) Acute pancreatitis can be a serious emergency with significant morbidity and mortality. Biliary stones are among the most common causes of acute pancreatitis, although the reported incidence varies among different populations. In patients with acute pancreatitis, transcutaneous US is routinely performed to detect biliary stones and is highly accurate for the diagnosis of stones in the gallbladder.1-4 However, the sensitivity of US for detecting choledocholithiasis is limited.5-7 ERCP early in the course of acute biliary pancreatitis, with endoscopic Received June 9, 2000. For revision August 17, 2000. Accepted May 25, 2001. From the Departments of Surgery and Diagnostic Radiology, University of Hong Kong Medical Centre, Queen Mary Hospital, Hong Kong, China. Reprint requests: Dr. Chi-Leung Liu, Department of Surgery, University of Hong Kong Medical Centre, Queen Mary Hospital, 102 Pokfulam Rd., Hong Kong. Copyright © 2001 by the American Society for Gastrointestinal Endoscopy 0016-5107/2001/$35.00 + 0 37/1/117513 doi:10.1067/mge.2001.117513 VOLUME 54, NO. 3, 2001 sphincterotomy (ES) when choledocholithiasis is detected, decreases morbidity rates for acute pancreatitis.8,9 However, ERCP has an associated morbidity rate of 3% to 6%.10,11 EUS is considered superior to US for imaging the extrahepatic biliary system. Because of the use of higher frequencies (7.5, 12, and 20 MHz) compared with those used for US (2 to 5 MHz), EUS provides high-resolution images of the layered structure of the gallbladder wall and microlithiasis (0.5-2 mm) within the gallbladder.12 EUS has also been shown to be highly accurate in the detection of choledocholithiasis.13,14 The aim of the present study was to prospectively evaluate the ability of EUS to detect biliary stones in patients with acute pancreatitis. PATIENTS AND METHODS The study comprised 100 consecutive patients (51 men, 49 women; median age 6l years; range 19-90 years) presenting with acute pancreatitis treated between November 1997 and March 1999 (Table 1). Thirty-eight patients GASTROINTESTINAL ENDOSCOPY 325 C-L Liu, C-M Lo, J K-F Chan, et al. EUS in acute pancreatitis Table 1. Clinical characteristics of 100 patients who presented with acute pancreatitis Clinical factor Age (y) Gender ratio (male:female) Duration of symptom (days) Febrile on presentation Clinical jaundice Serum amylase on admission (U/L) Alkaline phosphatase on admission (U/L) Lactate dehydrogenase on admission (U/L) Total serum bilirubin on admission (µmol/L) Ranson’s score15 ≥3 A Normal range 61 (19-90)* 51:49 1 (0-5)* 16 (16%)† 14 (14%)† 1630 (355-2600)* – – – – – 30-110 109 (30-813)* 49-138 488 (245-3070)* 197-401 29 (6-177)* 7-19 38 (38%)† – *Values expressed in median with range in parentheses. †Number of patients with percentage in parentheses. B C Figure 1. A, EUS image showing elongated stone in common bile duct. B, Endoscopic retrograde cholangiogram showing stone in common bile duct. C, Endoscopic view showing stone being removed from common bile duct with basket after endoscopic sphincterotomy. S, Stone; CBD, common bile duct; GB, gallbladder. 326 Value GASTROINTESTINAL ENDOSCOPY (38%) were diagnosed to have a severe attack of acute pancreatitis with a Ranson’s score of ≥3.15 Exclusion criteria included a known diagnosis of recurrent pancreatitis related to chronic alcoholism or hyperlipidemia and post-ERCP pancreatitis when that procedure was performed for reasons other than suspected biliary stones. Of the 100 patients, 15 had a previous diagnosis of gallstone disease and 8 had undergone cholecystectomy. The diagnosis of acute pancreatitis was based on acute abdominal pain and a serum amylase level greater than 3 times the upper limit of normal (normal <110 U/L). Biochemical analyses of blood samples for liver and renal function, arterial blood gases, calcium level, and lipid profiles, were performed after admission. US was performed in all patients shortly after admission; CT of the abdomen with contrast was performed on 27 patients. All US examinations were performed by expert radiologists with 2- to 4-MHz transcutaneous US probes (XP 10, Acuson, Mountain View, Calif.). EUS and ERCP were both performed within 24 hours of admission on all patients by endoscopists blinded to the results of US. For EUS, patients were placed in the left lateral position, an anesthetic spray was applied to the pharynx, and sedation was obtained by intravenous administration of diazepam and pethidine hydrochloride. By using a 7.5-MHz echoendoscope (GF-UM20 or JFUM20, Olympus Optical Co., Ltd., Tokyo, Japan), US images of the gallbladder and bile duct were obtained with the instrument placed in the first and second parts of duodenum and at the level of the distal antrum and pylorus. Biliary tract images were obtained at different angles by adjusting the position of the probe to minimize examination “blind spots.” A persistent echogenic focus with or without posterior acoustic shadowing was considered a biliary stone, microlithiasis, or sludge. ERCP was performed immediately after EUS by a second endoscopist blinded to the EUS findings with the patient still under conscious sedation. Once the ERCP findings were reported by the second endoscopist, the EUS findings were disclosed. If either test disclosed choVOLUME 54, NO. 3, 2001 EUS in acute pancreatitis C-L Liu, C-M Lo, J K-F Chan, et al. Table 2. Etiology of acute pancreatitis Etiology No. of patients (%) Biliary Gallstone present Previous cholecystectomy Hepatolithiasis without gallstones Alcoholism Hyperlipidemia Idiopathic Carcinoma of head of pancreas Total 67 8 2 8 7 6 2 100 (67) (8) (2) (8) (7) (6) (2) (100) Table 4. Detection of choledocholithiasis in 100 patients with acute pancreatitis by ERCP ERCP diagnosis of choledocholithiasis Final diagnosis of choledocholithiasis (No. of patients) Positive Negative Positive Negative 31 1 3 60 ERCP was unsuccessful in 5 patients. Table 5. Detection of choledocholithiasis in 100 patients with acute pancreatitis by EUS Table 3. Sensitivity of transcutaneous US and EUS in detection of cholelithiasis in 100 patients with acute pancreatitis Sensitivity Cholecystolithiasis Choledocholithiasis US EUS p Value 56/67 (84%) 9/34 (26%) 67/67 (100%) 33/34 (97%) <0.005 <0.001 ledocholithiasis, ES was performed (Fig. 1). By using endoscopic instrumentation of the bile duct after ES as the standard for the presence of choledocholithiasis, the diagnostic accuracy of EUS was compared with that of US and ERCP. If US, ERCP, and EUS did not detect choledocholithiasis, a presumptive diagnosis of no ductal stones was made because it was considered to be ethically unacceptable to perform ES and instrumentation of the bile duct to confirm the absence of stones. Direct inspection of gallbladder content after cholecystectomy was used as the standard for the presence of gallstones. However, in a few patients who refused or were considered unsuitable for cholecystectomy, a presumptive diagnosis of gallstones was made when both US and EUS showed one or more to be present. When US and EUS both indicated the absence of gallstones, a presumptive diagnosis of no gallstones was made. All patients were closely followed for recurrence of symptoms after endoscopic clearance of choledocholithiasis with or without definitive surgery for biliary stones (gallstones and hepatolithiasis). Informed consents for the study and the endoscopic procedures were obtained from all patients. The study protocol was approved by the ethics committee of our hospital. Sensitivity, specificity, and overall accuracy of US, EUS, and ERCP in the detection of biliary stones were compared with the McNemar test. Statistical analysis was performed with SPSS for Windows computer software (SPSS Inc., Chicago, Ill.). A p value of < 0.05 was considered statistically significant. RESULTS The etiology of acute pancreatitis in the 100 patients is summarized in Table 2. Acute pancreatitis was biliary in origin in 77 patients; in 67 a diagnosis of gallstones was made. The presence of gallstones was confirmed by a direct inspection of the VOLUME 54, NO. 3, 2001 EUS diagnosis of choledocholithiasis Final diagnosis of choledocholithiasis (No. of patients) Positive Negative Positive Negative 33 1 1 65 Table 6. Comparison of transcutaneous US, ERCP, and EUS in detection of choledocholithiasis in 100 patients with acute pancreatitis Sensitivity* Specificity† Overall accuracy* Successful examination† Procedure-related morbidity† US ERCP EUS 26% 100% 75% 100% 0% 97% 95% 96% 95% 4% 97% 98% 98% 100% 0% *p < 0.001 comparing US vs. ERCP or EUS. †p > 0.05 comparing all 3 diagnostic modalities. gallbladder contents after cholecystectomy in 59 of these patients. A presumptive diagnosis of gallstones was made based on US and EUS in the remaining 8 patients; 5 refused cholecystectomy and 3 were considered unfit for surgery. US detected gallstones in 56 patients but missed them in 11 patients. Small gallstones in these 11 patients were subsequently detected by EUS and confirmed by cholecystectomy. The median size of gallstones missed by US was 3 mm (range 1-6 mm). Thus, the sensitivity of US in the detection of gallstones was 84%, significantly less than that of EUS (100%, p < 0.005) (Table 3). Examination of the distal common duct by US was unsatisfactory in many cases because the duct was frequently obscured by bowel distended with gas. US detected ductal stones in 9 of the 34 patients with a final diagnosis of choledocholithiasis, yielding a sensitivity of 26%, which was significantly less than that of EUS (97%, p < 0.001) (Table 3). The detection of choledocholithiasis by ERCP and EUS is summarized in Tables 4 and 5. The sensitivity, specificity, and overall accuracy of ERCP and EUS in detecting choledocholithiasis were 97%, 95%, and GASTROINTESTINAL ENDOSCOPY 327 C-L Liu, C-M Lo, J K-F Chan, et al. Figure 2. Endoscopic view of major duodenal papilla showing impacted small pigmented stone (S) that escaped detection by EUS. 96% versus 97%, 98%, and 98%, respectively, with no significant difference (Table 6). EUS examination was successful in all patients, whereas ERCP was unsuccessful in 5 patients (p > 0.05). In 2 of these 5 patients, EUS indicated the presence of choledocholithiasis. Repeat ERCPs were successful, and stones were retrieved after ES. The remaining 3 patients underwent operative cholangiography during subsequent cholecystectomy, and the absence of ductal stones was confirmed. In 3 patients, ERCP was falsely positive for choledocholithiasis. This was probably related to small air bubbles introduced during cannulation and injection of contrast. EUS and ERCP both missed the diagnosis of choledocholithiasis in 1 patient, resulting in a sensitivity of 97% for both. A small stone impacted in the papilla of 1 patient escaped detection by EUS (Fig. 2), the findings being misinterpreted as an edematous papilla. Except for this patient, EUS accurately detected stones within the papilla in 6 other patients. EUS detected hepatolithiasis in the left lobe of the liver in 2 patients but missed hepatolithiasis in the right posterior segment in 1 patient. All 3 patients with hepatolithiasis had concomitant choledocholithiasis that was detected by EUS. Hepatolithiasis was correctly diagnosed by ERCP in all of these patients. ERCP-related complications occurred in 4 patients (4%). All 4 had post-ES bleeding that required a therapeutic endoscopic procedure during the same endoscopy session (3 patients) or the next day (1 patient). Among these patients, ERCP resulted in a false positive diagnosis of choledocholithiasis in 1 patient. None of the patients required blood transfusion. No EUS-related complication was 328 GASTROINTESTINAL ENDOSCOPY EUS in acute pancreatitis observed. The median duration of EUS was 14 minutes (range 8-23 minutes). Although it was not possible to validate the presumptive absence of choledocholithiasis when both ERCP and EUS were negative (false negativity by both investigations), no patient in whom both studies were negative subsequently had symptoms develop suggestive of retained stones after a median follow-up of 22 months (range 12-29 months). Similarly, although it was not possible to validate the presumptive absence of gallstones because cholecystectomy was not performed when both US and EUS were negative for gallstones, no patient with negative findings by both studies had clinical evidence of gallstones after a median follow-up of 20 months (range 11-28 months). In addition to the detection of biliary stones, EUS was also helpful in determining the etiology of pancreatitis in 2 patients with carcinoma of the head of pancreas (Table 2). These diagnoses were subsequently confirmed by histologic examination of surgical resection specimens. DISCUSSION The accuracy of US in detecting gallbladder stones is high, with reported sensitivities ranging from 92% to 96%.1-4 Traditionally, detection of gallstones in patients with acute pancreatitis has been based primarily on US, but small gallstones are frequently encountered. Theoretically, small stones pass more readily into the common duct and through the papilla to cause acute pancreatitis. It has been reported that when stones are less than 3 mm in diameter or are located in the gallbladder infundibulum, the sensitivity of US is only 65%.16 A recent study of the accuracy of US in detecting gallstones in 946 patients also found a false negative rate of 1.3%.4 Although accuracy in gallstone detection in patients with acute pancreatitis can be improved by repeating US at a later time, gallstones can still elude detection in a sizable number of patients.17 EUS, with its high-image resolution and close proximity to the biliary system during examination, is considered superior to US for gallbladder imaging. A study of 45 patients with clinically suspected biliary stones but with at least 2 normal US examinations found that EUS detected evidence of stones in the gallbladder of 26 patients.18 In the present study, the sensitivity of US in detecting cholelithiasis was only 84% and was inferior to that of EUS (100%, p < 0.005). However, a limitation of the present study was that the standard for absence of gallstone included the EUS examination. Nevertheless, none of the patients evaluated in this way had clinical evidence of gallstones on follow-up. VOLUME 54, NO. 3, 2001 EUS in acute pancreatitis With its high accuracy for detection of microlithiasis within the gallbladder, EUS can play a role in the identification of biliary causes of “idiopathic” pancreatitis. In a recent study of 89 patients presenting with acute pancreatitis, EUS detected occult biliary stones in 14 (78%) of 18 patients with a diagnosis of idiopathic pancreatitis by conventional radiologic methods; 18% of all cases of biliary pancreatitis were diagnosed by EUS alone.19 When a biliary cause is identified, treatment can be initiated early, thereby reducing the risk of recurrent pancreatitis and its associated morbidity and mortality. In addition to its sensitivity for detection of occult cholelithiasis, EUS can also accurately detect choledocholithiasis.13,14 EUS is reported to have a significantly higher sensitivity (96%) than US (63%) or CT (71%) in detecting choledocholithiasis with sensitivity unaffected by stone size or bile duct diameter.20 In addition, EUS performed before cholecystectomy can aid in the accurate selection of patients with choledocholithiasis for surgical exploration of the duct.21 In patients with acute biliary pancreatitis, EUS performed just before ERCP can aid in the selection of patients for therapeutic endoscopic intervention, thereby obviating the need for diagnostic ERCP with its potential risks in at least 50% of patients. In the present study, EUS demonstrated the absence of choledocholithiasis in 65 of 66 patients with a specificity of 98% (Table 5). In fact, in one patient with post-ES bleeding, ERCP resulted in a false positive diagnosis of choledocholithiasis. Thus, this complication could potentially have been avoided by EUS. EUS is less invasive and its use can prevent repeated unsuccessful attempts at cannulation during ERCP, which can potentially worsen acute pancreatitis. Despite the advantages of EUS in relation to ERCP, EUS has limitations when investigating the possibility of choledocholithiasis in patients presenting with acute pancreatitis. In our area of the world, the bile duct in these patients frequently harbors small, soft, pigmented stones that may not cast an echogenic shadow. Thus, detection by EUS of such a stone impacted at the papilla can be difficult. In the present study, the correct diagnosis in 1 of the 7 patients who had an impacted stone was missed by EUS. Later in the course of the study our technique was modified to include a side-view echoendoscope (JF-UM20, Olympus) instead of an oblique-viewing instrument. This allowed direct inspection of the papilla. Another drawback of EUS is that it is difficult to examine the intrahepatic biliary tree. In our geographic region, hepatolithiasis accounts for acute pancreatitis in a small number of patients (3 patients in the present study).22 VOLUME 54, NO. 3, 2001 C-L Liu, C-M Lo, J K-F Chan, et al. Intrahepatic ductal stones can easily be missed in this group of patients; EUS failed to show such stones in 1 patient in the present study. Thus, other imaging modalities (US, CT, or ERCP) may be required for the diagnosis of hepatolithiasis in patients with acute pancreatitis. EUS could potentially provide prognostic information in patients with acute pancreatitis. Schoefer et al.23 preliminarily reported data from a prospective study of the prognostic value of EUS in 31 patients with acute pancreatitis. A numerical EUS score was developed based on EUS findings (organ size, aspect of the outer margin of pancreas, echogenicity, location, and the extent of peripancreatic fluid). The EUS score correlated significantly with the duration of hospital stay, duration of fever, length of intensive care, and CT prognostic index. In another prospective study,24 there appeared to be a relationship between EUS findings of peripancreatic fluid and echogenicity of the pancreas and mean hospital stay. However, the timing of EUS for documentation of pancreatic lesions in this study is unclear. Although these data are intriguing, further studies are required to evaluate the prognostic role of EUS in patients with acute pancreatitis. Magnetic resonance imaging (MRI) has been shown to be highly accurate in detecting choledocholithiasis (sensitivity 85% to 100%).25-27 MRI has also been reported as useful in patients with acute pancreatitis by providing a severity index and because it is helpful in differentiating interstitial pancreatitis from necrotizing pancreatitis.28 Like EUS, MRI could in theory detect choledocholithiasis in patients presenting with acute pancreatitis and thereby aid in the selection of patients for therapeutic ERCP. However, the accuracy of MRI in the detection of choledocholithiasis in the setting of acute pancreatitis has not been fully documented. Compared with MRI, EUS is more readily available in our hospital, especially within the first 24 hours after admission. Moreover, if choledocholithiasis is detected by EUS, ERCP with ES can be performed immediately while the patient is still sedated. Further study of the cost-effectiveness of these 2 modalities in the detection of choledocholithiasis in patients with acute pancreatitis is needed. The present study was performed in a region where the incidence of pigmented stones is high. Over 70% of our patients presenting with acute pancreatitis have biliary stones. This figure is much higher than that for Western countries. Therefore, the results of the present study may not be generally applicable to other regions. However, because the frequency of choledocholithiasis is lower among Western populations, an accurate but less invasive GASTROINTESTINAL ENDOSCOPY 329 C-L Liu, C-M Lo, J K-F Chan, et al. diagnostic modality for confirmation of the presence of bile duct stones prior to therapeutic ERCP would be of even greater value. Whether EUS or MRI will become the investigation of choice may depend on the local availability of expertise and facilities. In summary, EUS is more sensitive than US in detecting cholelithiasis and choledocholithiasis in patients with acute pancreatitis. Moreover, EUS is as accurate as ERCP in detecting choledocholithiasis. EUS can be used to select patients with acute pancreatitis for therapeutic ERCP, thus avoiding diagnostic ERCP with its greater potential for morbidity in a majority of patients. The potential benefit and the cost-effectiveness of this new endoscopic approach require further investigation. REFERENCES 1. Lee CL, Wu CH, Chen TK, Lai YC, Yang SS, Huang CS, et al. Prospective study of abdominal ultrasonography before laparoscopic cholecystectomy. J Clin Gastroenterol 1993;16:113-6. 2. Shea JA, Berlin JA, Escarce JJ, Clarke JR, Kinosian BP, Cabana MD, et al. Revised estimates of diagnostic test sensitivity and specificity in suspected biliary tract disease. Arch Intern Med 1994;154:2573-81. 3. Weltman DI, Zeman RK. Acute diseases of the gallbladder and biliary ducts. Radiol Clin North Am 1994;32:933-50. 4. Chintapalli KN, Ghiatas AN, Chopra S, Escobar B, Esola CC, Dodd GD. Sonographic findings in cases of missed gallstones. J Clin Ultrasound 1999;27:117-21. 5. Neoptolemos JP, Hall AW, Finlay DF, Berry JM, Carr-Locke DL, Fossard DP. The urgent diagnosis of gallstones in acute pancreatitis: a prospective study of three methods. Br J Surg 1984;71:230-3. 6. Pasanen PA, Partanen KP, Pikkarainen PH, Alhava EM, Janatuinen EK, Pirinen AE. A comparison of ultrasound, computed tomography and endoscopic retrograde cholangiopancreatography in the differential diagnosis of benign and malignant jaundice and cholestasis. Euro J Surg 1993; 159:23-9. 7. Varghese JC, Liddell RP, Farrel MA, Murray FE, Osborne H, Lee MJ. The diagnostic accuracy of magnetic resonance cholangiopancreatography and ultrasound compared with direct cholangiography in the detection of choledocholithiasis. Clin Radiol 1999;54:604-14. 8. Neoptolemos JP, Carr-Locke DL, London NJ, Bailey IA, James D, Fossard DP. Controlled trial of urgent endoscopic retrograde cholangiopancreatography and endoscopic sphincterotomy versus conservative treatment for acute pancreatitis due to gallstones. Lancet 1988;2:979-83. 9. Fan ST, Lai ECS, Mok FPT, Lo CM, Zheng SS, Wong J. Early treatment of acute biliary pancreatitis by endoscopic papillotomy. N Engl J Med 1993;328:228-32. 10. Shields SJ, Carr-Locke DL. Sphincterotomy techniques and risks. Gastrointest Endosc Clin N Am 1996;6:17-42. 11. Cotton PB. Outcomes of endoscopic procedures: struggling towards definitions. Gastrointest Endosc 1994;40:514-8. 330 GASTROINTESTINAL ENDOSCOPY EUS in acute pancreatitis 12. Dill JE, Hill S, Callis J, Berkhouse L, Evans P, Martin D, et al. Combined endoscopic ultrasound and stimulated biliary drainage in cholecystitis and microlithiasis—diagnoses and outcomes. Endoscopy 1995;27:424-7. 13. Amouyal P, Amouyal G, Levy P, Tuzet S, Palazzo L, Vilgrain V, et al. Diagnosis of choledocholithiasis by endoscopic ultrasonography. Gastroenterology 1994;106:1062-7. 14. Prat F, Amouyal G, Amouyal P, Pelletier G, Fritsch J, Choury AD, et al. Prospective controlled study of endoscopic ultrasonography and endoscopic retrograde cholangiography in patients with suspected common-bile duct lithiasis. Lancet 1996;347:75-9. 15. Ranson JHC, Rifkind KM, Roses DF, Fink SD, Eng K, Spencer EC. Prognostic signs and the role of operative management in acute pancreatitis. Surg Gynecol Obstet 1974;139:69-81. 16. Kurol M, Forsberg L. Ultrasonography in the diagnosis of acute cholecystitis. Acta Radiol Diagn Stockh 1984;25:379-83. 17. Goodman AJ, Neoptolemos JP, Carr-Locke DL, Finlay DBL, Fossard DP. Detection of gallstones after acute pancreatitis. Gut 1985;26:125-32. 18. Dahan P, Andant C, Levy P, Amouyal P, Amouyal G, Dumont M, et al. Prospective evaluation of endoscopic ultrasonography and microscopic examination of duodenal bile in the diagnosis of cholecystolithiasis in 45 patients with normal conventional ultrasonography. Gut 1996;38:277-81. 19. Liu CL, Lo CM, Chan JKF, Poon RTP, Fan ST. EUS for detection of occult cholelithiasis in patients with idiopathic pancreatitis. Gastrointest Endosc 2000;51:28-32. 20. Sugiyama M, Atomi Y. Endoscopic ultrasonography for diagnosing choledocholithiasis: a prospective comparative study with ultrasonography and computed tomography. Gastrointest Endosc 1997;45:143-6. 21. Aubertin JM, Levoir D, Bouillot JL, Becheur H, Bloch F, Aouad K, et al. Endoscopic ultrasonography immediately prior to laparoscopic cholecystectomy: a prospective evaluation. Endoscopy 1996;28:667-73. 22. Liu CL, Fan ST, Wong J. Primary biliary stones: Diagnosis and management. World J Surg 1998;22:1162-6. 23. Schoefer M, Rathgeber A, Lang J, Nagell W, Dancygier H. Prognostic value of endoscopic ultrasound in acute pancreatitis [abstract]. Gastroenterology 1998;114:A495. 24. Chak A, Hawes RH, Cooper GS, Hoffman B, Catalano MF, Wong RC, et al. Prospective assessment of the utility of EUS in the evaluation of gallstone pancreatitis. Gastrointest Endosc 1999;49:599-604. 25. Reinhold C, Taourel P, Bret PM, Cortas GA, Mehta SN, Barkun AN, et al. Choledocholithiasis: evaluation of MR cholangiography for diagnosis. Radiology 1998;209:435-42. 26. Liu TH, Consorti ET, Kawashima A, Ernst RD, Black CT, Greger PH, et al. The efficacy of magnetic resonance cholangiography for the evaluation of patients with suspected choledocholithiasis before laparoscopic cholecystectomy. Am J Surg 1999;178:480-4. 27. Demartines N, Eisner L, Schnabel K, Fried R, Zuber M, Harder F. Evaluation of magnetic resonance cholangiography in the management of bile duct stones. Arch Surg 2000;135:148-52. 28. Lecesne R, Taourel P, Bret PM, Atri ML, Reinhold C. Acute pancreatitis: interobserver agreement and correlation of CT and MR cholangiopancreatography with outcome. Radiology 1999;211:727-35. VOLUME 54, NO. 3, 2001