File - Dr. Jerry Cronin
advertisement

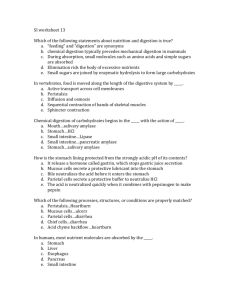
Chapter 24 The Digestive System The Digestive System Gastroenterology is the study of the gastrointestinal system. The digestive system functions are ingestion, secretion, digestion (chemical and mechanical), mixing and propulsion, absorption and defecation. The Digestive System The digestive system, also called the gastrointestinal system, is composed of the alimentary canal (GI tract), and the accessory organs. The alimentary canal extends from the mouth to the anus through the ventral body cavity (approximately 9 m, or 30 ft.). The accessory organs include the teeth, tongue, salivary glands, liver, gallbladder, and pancreas. The Digestive System The GI tract, and accessory organs like the liver and pancreas, are responsible for facilitating the body’s metabolic processes. Catabolism: Larger molecules are broken into smaller molecules (mouth, stomach, duodenum). • In the GI tract, this is called digestion and can occur by either mechanical or chemical means. Anabolism: Smaller molecules are used as building blocks for larger molecules (liver). The Digestive System Mechanical digestion includes all movements that facilitate catabolic processes: Mastication Swallowing Mixing • Increase contact of food with digestive chemicals Peristalsis • Movement of muscles within the GI tract that facilitates movement of food The Digestive System Chemical digestion is mainly accomplished by using water to break chemical bonds (hydrolysis). Fats are broken down into fatty acids and glycerol. Carbohydrates are broken down from polysaccharides into monosaccharides. Proteins are broken down into polypeptides and amino acids. The Digestive System (Interactions Animation) Enzyme mediated hydrolysis You must be connected to the internet to run this animation Anatomy Overview The wall of the GI tract from the lower esophagus to the anal canal has the same basic, four-layered arrangement of tissues. The four layers of the tract, from deep to superficial, are the mucosa, submucosa, muscularis, and serosa/adventitia. The lumen is the inside of the tube. Anatomy Overview The mucosa is a mucous membrane made of various types of epithelium sitting on a loose connective tissue called the lamina propria. Nonkeratinized stratified squamous epithelium (for protection) lines the pharynx, esophagus, and anus. Simple columnar epithelium (for secretion/absorption) lines the stomach and intestines. • Located among the epithelial cells are various glandular cells that secrete mucus and fluid into the lumen of the tract (exocrine). Anatomy Overview The lamina propria contains a prominent lymphoid tissue (mucosa-associated lymphatic tissue or “MALT”) that protect against disease. Underneath it is the muscularis mucosae, a thin layer of smooth muscle that throws the lining of the stomach and small intestines into tiny folds (increases surface area to aid digestion/absorption). Anatomy Overview The submucosa is composed of loose connective tissue that binds the mucosa to the muscularis. It contains blood and lymphatic vessels (to receive absorbed substances) and an extensive network of neurons known as the submucosal plexus. Anatomy Overview The muscularis of the mouth, pharynx, superior and middle parts of the esophagus, and anal sphincter contains skeletal muscle that allows for voluntary swallowing and control of defecation. Throughout the rest of the tract, it is smooth muscle, arranged in inner circular and outer longitudinal sheets, with the myenteric nerve plexus continuing between them. Anatomy Overview The serosa/adventitia is the outermost layer. If attached to surrounding tissues (e.g. around the esophagus), it is called adventitia - a fibrous connective tissue arranged around the organ which it supports. If contained in the peritoneal cavity, it is called serosa , which has a slippery mesothelium surface layer. • Serosa covers the intra-abdominal organs as the visceral peritoneum. Anatomy Overview Anatomy Overview The peritoneum is the body’s largest serous membrane, and it wraps around most abdominopelvic organs. The visceral peritoneum forms the “serosa” of the alimentary canal and covers other intra-abdominal organs. It then continues around the abdominal wall as the parietal peritoneum. Anatomy Overview Unlike the pericardium and pleurae, which smoothly cover the heart and lungs, the peritoneum contains large folds that bind the organs to one another and to the cavity walls. There are five major peritoneal folds: • • • • • greater omentum falciform ligament lesser omentum mesentery mesocolon Anatomy Overview The greater omentum is the largest peritoneal fold. It drapes over the transverse colon and the anterior coils of the small intestine like a “fatty apron”. • It contains many lymph nodes that help combat and contain infections of the GI tract. • The large amount of adipose tissue can greatly expand (as seen in people with “beer bellies”). Anatomy Overview The falciform ligament attaches the liver to the anterior abdominal wall and diaphragm. Anatomy Overview • The lesser omentum is a peritoneal fold that suspends the stomach and duodenum from the inferior edge of the liver. – It forms a pathway for blood vessels (hepatic portal vein and common hepatic artery) to enter the liver, and it contains the common bile duct. Anatomy Overview Together, the mesentery (of the small intestine) and mesocolon (of the large intestine) attach the bowel to the posterior abdominal wall, holding the intestines loosely in place as muscular contractions mix and move the luminal contents along the GI tract. Anatomy Overview Some abdominopelvic organs are covered by visceral peritoneum only on their anterior surfaces. The portion of the organ that lies behind the peritoneum is said to be “retroperitoneal”. Organs in the retroperitoneal space include: The kidneys and ureters Most of the pancreas The adrenal glands The aorta and inferior vena cava Physiology Overview Digestive activities of the gastrointestinal tract occur in three overlapping phases: 1. The cephalic phase 2. The gastric phase 3. The intestinal phase As we study the glands of the mouth, stomach, and small intestine – as well as the secretions of the accessory organs the liver and pancreas – we will learn about the specifics of all 3 phases. Physiology Overview During the cephalic phase of digestion, the smell, sight, thought, or initial taste of food activates neural centers in the cerebral cortex, hypothalamus, and brain stem to prepare for digestion. The brain stem activates the facial (CN VII) and glossopharyngeal (CN IX) nerves to stimulate secretion of saliva, while the vagus nerves (CN X) stimulate secretion of gastric juice. Physiology Overview Once food reaches the stomach, the gastric phase of digestion begins. Neural and hormonal mechanisms (the hormone gastrin is a key player) promote secretion of gastric juice and increase gastric motility. The intestinal phase of digestion begins once food enters the small intestine. Neural and hormonal responses promote the continued digestion of foods that have reached the small intestine. The Mouth The oral or buccal cavity, is formed by the cheeks, hard and soft palates, and the tongue. Mechanical digestion of food through mastication (chewing) enables it to be mixed with saliva to form a soft flexible bolus that can be easily swallowed. Saliva starts the process of chemical digestion of food • Saliva is 99.5% water, with tiny amounts of dissolved ions, IgA, lysozyme (a bacteriolytic enzyme), and salivary amylase (a digestive enzyme that acts on starch). The Mouth Three large salivary glands secrete most of the saliva: the parotid, submandibular, and sublingual glands. The smaller glands are found on the lips (labial), cheeks (buccal), palate (palatal), and tongue (lingual). Daily salivary secretions average 1–1½ liters. The Mouth Salivary regulation is under the control of the ANS Parasympathetic stimulation promotes secretion of a moderate amount of saliva. Salivary centers are located in the brain stem and efferent nerve impulses are transmitted by the facial (VII) and glossopharyngeal (IX) nerves. • Touch (pressoreceptors), smell, taste (taste buds), and psychological factors are also salivary stimulators. Sympathetic stimulation decreases saliva secretions. The Mouth (Interactions Animation) Carbohydrate Digestion in the Mouth You must be connected to the internet to run this animation The Mouth (Interactions Animation) Lipid Digestion in the Mouth You must be connected to the internet to run this animation The Mouth The tongue is composed of skeletal muscle under voluntary somatic motor control - it forces the moistened food bolus into position for swallowing (deglutition) and places the bolus into contact with the teeth for chewing. The extrinsic muscles of the tongue attach to bones in the area and move the tongue from side to side. Intrinsic muscles originate within the tongue and alter its shape and size for speech and swallowing The Mouth The Mouth The teeth or dentes are located in sockets of the alveolar processes of the mandible and maxillae. The sockets are lined by the periodontal ligament a dense fibrous connective tissue that anchors the teeth to the socket walls and acts as a shock absorber during chewing. A typical tooth has three major external regions: the crown, root, and neck. • The neck of each tooth is covered by the gingivae , or gums, which extend slightly into each socket. The Mouth Dentin is a calcified connective tissue that forms most of the tooth. The dentin of the crown is covered by enamel, a harder-than-bone calcified material and encloses the pulp cavity, a space filled with pulp (a connective tissue containing blood vessels, nerves, and lymphatic vessels). The Mouth Humans have two dentitions or sets of teeth. There are 20 deciduous or “baby teeth” which begin to erupt around 6 months of age. • All are lost between 6–12 yrs. of ages There are 32 permanent teeth numbered from right to left, top (1–16) to bottom (17–32). • The third molars (teeth 1, 16, 17, and 32) are the wisdom teeth. The Mouth (Interactions Animation) Mastication You must be connected to the internet to run this animation Deglutition Deglutition is the act of swallowing food. The oropharynx and laryngopharynx have digestive as well as respiratory functions, and swallowed food must transit them both on the way to the esophagus – and it must do so while not going into the nasal cavity or the airway. This complex process involves many muscles subject to a number of voluntary and involuntary controls. • Deglutition has 3 stages: voluntary, pharyngeal, and esophageal. Deglutition The first stage is the voluntary act of the tongue forcing the bolus to the back of the oral cavity and into the oropharynx. The involuntary pharyngeal stage begins as the bolus passes into the oropharynx - receptors send impulses to the deglutition center in the medulla and pons. Returning impulses cause the soft palate to move superiorly and posteriorly to close the nasopharynx. The epiglottis moves slightly inferiorly to close the glottis. Deglutition The esophageal stage of swallowing begins once the bolus enters the esophagus. Peristalsis, a progression of coordinated contractions and relaxations of the circular and longitudinal layers of the muscularis, push the bolus onward. Deglutition (Interactions Animation) Deglutition You must be connected to the internet to run this animation The Esophagus The only digestive system function that occurs in the esophagus is propulsion (moving food into the stomach). The esophagus is a muscular tube that begins inferior to the laryngopharynx, and positioned posterior to the trachea. Leaving the neck, it traverses the thoracic cavity down the posterior mediastinum before piercing the diaphragm through the esophageal hiatus. The Esophagus The mucosa of the esophagus is nonkeratinzed stratified squamous epithelium The type of muscle in the muscularis of the esophagus varies by region • the superior 1/3 is skeletal muscle • the intermediate 1/3 is skeletal and smooth muscle • the inferior 1/3 is smooth muscle The Esophagus Upper and lower esophageal sphincters (UES and LES) are situated at each end of the tube. The LES regulates the movement of food from the esophagus into the stomach. • Incompetence of the LES results in Gastroesophageal Reflux Disease (GERD), which manifests as “heart burn”. The Stomach The stomach is a J-shaped enlargement of the GI tract situated between the esophagus and the first part of the small intestine (the duodenum). The position and size of the stomach varies continually - the diaphragm pushes it inferiorly with each inhalation and pulls it superiorly with each exhalation. Rugae are large folds in the mucosa of the empty stomach which enable gastric distension, depending on the amount of stomach contents. The Stomach Empty, the stomach is about the size of a large sausage, but it is the most distensible part of the GI tract and can expand to accommodate a large quantity of food. Because a meal can be eaten much more quickly than the intestines can digest and absorb it, one of the functions of the stomach is to serve as a mixing chamber and holding reservoir. As a functional adaptation, the gastric muscularis The Stomach The stomach has four main regions: the cardia the fundus the body the pylorus Note the additional oblique layer of smooth muscle in the gastric muscularis, which is limited primarily to the body of the stomach The Stomach Simple columnar epithelial cells (surface mucous cells) line the mucosal surface and secrete a protective mucous. Columns of secretory cells extend down into the lamina propria forming gastric glands. Several gastric glands open into the bottom of narrow The Stomach A variety of specialized exocrine and endocrine cell types populate the gastric glands and pits. Exocrine gland cells include: • mucous neck cells which produce mucus • parietal cells which produce intrinsic factor and HCl • chief cells which secrete the protease pepsinogen and gastric lipase Enteroendocrine G cells, located mainly in the pyloric antrum, secrete the hormone gastrin into the bloodstream. The Stomach The secretions of the mucous, parietal, and chief cells form gastric juice, which totals 2–3 l/d. The stomach is protected from its own gastric juice by a 1–3 mm thick layer of alkaline mucus secreted by surface mucous cells and mucous neck cells. The Stomach The strongly acidic nature of gastric juice kills many microbes, partially denatures proteins in food, and converts pepsinogen into pepsin. Pepsin is the only proteolytic enzyme in the stomach. Gastric lipase splits triglycerides. Intrinsic factor (IF) is needed for absorption of vitamin B12 in the terminal ileum. • Vitamin B12 is needed for RBC production. The Stomach Disturbing the balance between hydrochloric acid production, pepsin secretion, and mucosal defenses can lead to erosion of the stomach's epithelial lining. This graphic shows an endoscopic view of a gastric erosion, possibly caused by consumption of too much alcohol or use of an NSAID drug such as aspirin or ibuprofen. The Stomach • Gentle, rippling, peristaltic movements called mixing waves pass over the stomach every 15 to 25 seconds. – These waves macerate food, mix it with secretions of the gastric glands, and reduce it to a soupy liquid called chyme. The Stomach (Interactions Animation) Stomach Peristalsis You must be connected to the internet to run this animation The Stomach (Interactions Animation) Chemical Digestion - Gastric Acid You must be connected to the internet to run this animation The Stomach (Interactions Animation) Protein Digestion in the Stomach You must be connected to the internet to run this animation