open the file... - Excellus BlueCross BlueShield
advertisement

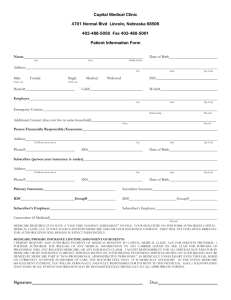
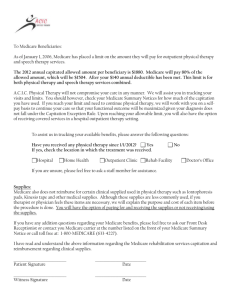
Newsletter for Physicians, Medical Office and Facility Staff Excellus BlueCross BlueShield September 2014 Customer Care Hours of Operation As of August 30, 2014, Customer Care provider phone queues are open: Monday through Thursday from 8 a.m. to 5:30 p.m. Friday from 9 a.m. to 5:30 p.m. As reminder, the regionwide Customer Care phone number is 1-800-920-8889. In this Issue: 3 News You Can Use 5 Coding Update 4 Verifying Provider Demographics 6 Vision Billing Guidelines Effective October 1 Also: ・ Medical Policy Updates ・ News from FLRx ・ Did You Know? ・ Event Calendar A nonprofit independent licensee of the Blue Cross Blue Shield Association September 2014 Table of Contents Tip! Search for article of (click the title to go directly to the article) News You Can Use……p. 3 IMPORTANT CLARIFICATION - Change in Reimbursement Policy for Vaccine Administration Code 90461 Limited to Medicaid Managed Care, Family Health Plus, Child Health Plus and Healthy NY ONLY……p. 4 interest to your practice or facility! P/F Verifying Provider Demographics……p. 4 Preauth for Sleep Management, Cardiac Devices & Radiation Therapy Services……p. 4 Requesting Referrals & Preauthorizations for Outpatient Services? Access Our Clear Coverage™ Electronic Preauthorization System TODAY!……p. 5 Coding Update……p. 5 Drug Screening Billing Guidelines……p. 5 P = Professional F = Facility P/F = Professional & Facility Vision Billing Guidelines Effective October 1……p. 6 Submitting Claims for Sterilization or Hysterectomy Performed on Medicaid Managed Care or Family Health Plus Members……p. 7 Quality Improvement Organization Program Restructuring……p. 8 Talk To Your Patients Age 65 & Older About Exercise & Physical Activity……p. 9 BlueCard® Corner……p. 9-10 Medical Policy Updates……p. 11 News from FLRx……p. 11 We Are Listening! Register Today! P/F Website “Referrals & Auths” Section Revamped Fall Learning Opportunities We listened to your feedback and redesigned our Referrals & Auths page to make it easier for you to: Check out the Education section of our website for information regarding Fall Seminars and Navigating the Blues educational series. Click here to obtain schedules and registration forms. Request authorization Check for approvals View our authorization requirements Attention Plattsburgh Area Providers! All of the other features you currently use are still available. New dates have been added to our Navigating the Blues schedule for seminars in your area! Check it out here. To access the revamped page, visit ExcellusBCBS.com/ProviderReferralsAuths. Physician Satisfaction Survey Coming Soon! P We continually look for ways to improve the quality of our health plan and service to our providers. That’s why we strongly encourage you to complete our 2014 Physician Satisfaction Survey, which will be mailed to your office in the next few weeks. Once completed, simply return the survey in the postagepaid envelope by October 30, 2014. Many of the survey responses from past years have driven positive changes in how we do business, so please share your ideas and feedback with us. A survey will also be forthcoming for office managers. We ask that physicians complete this survey and office managers complete the survey that will arrive later in the month. We look forward to hearing from you! 2 P/F September 2014 News You Can Use P/F Meet Our Medical Directors Our medical director team is made up of physicians who are board-certified in their fields. Every physician on the team has many years of clinical practice experience in upstate New York, and they are proud to live and work in the communities that they serve. Commonly Used Forms - An Many of the forms that you call Customer Care for can be accessed from the Print Forms section of our website. We update our forms periodically so if you make copies of our forms for your office supply, check our website frequently to ensure that you have the most current version. Click here to access the Print Forms section of our website. Our medical directors are committed to working in partnership with you to deliver high-quality, evidence-based and cost-effective health care to our valued members, your patients. Learn more! Click here to access our medical director biographies and code of ethics. Affordable Care Act Update - Preventive Services Coverage Grid - The Health Care Reform section of the Excellus BCBS website contains our most up-to-date Preventive Services Coverage Grid. This grid outlines the mandated preventive services, including Women’s Health Services. Click here to access. Faxing Claims - Unless specifically asked, please do not fax claims to us. Faxed claims frequently arrive with fields missing, faded or blurred, and cannot be processed. The exception would be if you fax a claim to the attention of a particular person. In this scenario, it is important to include a fax cover sheet with the name, department and telephone extension of the employee expecting your fax. We appreciate your cooperation. Authorization Reminder - When a member changes health insurance plans (through a new employer, etc.) he or she will receive a new ID card with a new ID number. If you have an authorization on file for the member, be sure to contact the number on the back of the ID card to request a new authorization. Authorizations under the member’s old ID number will not auto-transfer to the member’s new number. Check ID cards at each visit and make a copy of the card for your file. Also, prior to rendering services, verify benefits and eligibility via at ExcellusBCBS.com/wps/portal/xl/prv/cvg/, or by calling Customer Care at 1-800-920-8889. Preventing Fraud & Abuse - We are dedicated to the prevention of fraud. Click here to visit our website to learn more about types of fraud and learn how to report potential fraud and abuse to our health plan. Clinical Practice Guidelines Update - We have reviewed and updated our Community Principles of Pain Management clinical practice guidelines. To access the updated guidelines, click here. EBS-RMSCO, Inc. Changes Name to “Lifetime Benefit Solutions, Inc.” - EBS-RMSCO, Inc., which provides comprehensive employee benefits administration and innovative risk management solutions to employee benefit programs, has changed its corporate name to “Lifetime Benefit Solutions, Inc.” Beginning this month and through the remainder of 2014, Lifetime Benefit Solutions will change all external branding, including forms and email addresses, to reflect their new name and logo. The ID cards used by their members will change as their groups come up for renewal. This will carry over into 2015. Therefore, it is imperative that you check member ID cards at each visit to verify that you have the current information on file for the member. If you have questions, contact the Lifetime Benefit Solutions Customer Service Center at 1-315-448-9029, or toll-free at 1-877-300-9969. 3 September 2014 IMPORTANT CLARIFICATION - Change in Reimbursement Policy for Vaccine P/F Administration Code 90461 Limited to Medicaid Managed Care, Family Health Plus, Child Health Plus and Healthy NY ONLY As we previously notified you, effective September 1, 2014, reimbursement for vaccine administration will no longer be made if the corresponding vaccine code is not included on the claim. In the past, when providers administered vaccines for which there was no charge for the vaccine serum (e.g., vaccines provided through the Vaccines for Children Program), some practitioners neglected to report the specific vaccine administered with a zero charge. Knowing which vaccines have been administered helps us to collaborate with you to ensure that our members receive all age-recommended vaccines, and it enables us to accurately report quality data to the New York State Department of Health. It is important to note that certain vaccines will continue to be paid at zero charge when provided through the Vaccines for Children Program, and they will be reflected as such on your remittances. Please report the administration of vaccines accordingly using the following vaccine administration codes: 90460, 90471, 90472, 90473, 90474 and G0008-G0010. The multi-component vaccine administration code 90461 will not be reimbursed for Medicaid Managed Care, Family Health Plus, Child Health Plus or Healthy NY. However, code 90461 will continue to be reimbursable for all other lines of business. When this article ran in the July and August issues of this newsletter, we did not indicate which lines of business were impacted by this change. This change only affects our Medicaid Managed Care, Family Health Plus, Child Health Plus and Healthy NY lines of business. We apologize for any confusion. Verifying Provider Demographics P We continue to work with our vendor, Sutherland Global Services, to conduct demographic data verification to ensure that the information we have on file for your practice is current. If our vendor contacts your office, please provide them with the information they request. As a reminder, you can keep your practice information current by making updates via our website. Click here to update the individual or group practice information we have on record for you in our provider database. Please be sure to verify that your office hours and “accepting new patients” status is accurate. This information should be reviewed every 90 days. If your office anticipates challenges meeting New York state visit time frames, you should consider changing your “accepting new patients” status to “closed to new patients” until timely visits are available. It’s also very important that you keep us informed of new provider additions or departures from your practice. We appreciate your cooperation to help ensure that your information is current, which assists our members, your patients. 4 Preauth for Sleep Management, Cardiac Devices & Radiation Therapy Services P/F Our preauthorization program for sleep management, cardiac devices and radiation therapy in partnership with CareCore National, LLC has received New York State Department of Health approval. As of August 25, 2014, CareCore began processing all preauthorization requests as instructed in our bulletin dated June 24, 2014 (access the notice by clicking here). You may contact CareCore by phone at 1-866-889-8056, 7 a.m. to 7 p.m. EST, Monday through Friday, or use our website, ExcellusBCBS.com/Provider, to enter a preauthorization request. Web services are available 24 hours a day, seven days per week. Additionally, as clarification regarding cardiac implantable device preauthorization, Excellus BCBS requires approval for services related to the implantation, upgrade, revision or removal of cardiac devices. Thank you for your patience during our transition to our new preauthorization program. September 2014 Requesting Referrals & Preauthorizations for Outpatient Services? Access Our Clear Coverage™ Electronic Preauthorization System TODAY! P/F We recently introduced our new electronic preauthorization system — Clear Coverage, a Web-based, real-time software developed by McKesson. Clear Coverage is now available for you to use when requesting referrals and preauthorizations for outpatient services, and it is accessible via the Referrals & Auths section of our website, ExcellusBCBS.com/ProviderReferralsAuths. We are excited to offer your office greater self-service options and immediate resolution of preauthorization requests through this new tool. In addition, Clear Coverage offers: ▪ Faster turnaround: 60 percent to 80 percent of requests are answered immediately ▪ Faster pending case resolution: most clinical information is immediately accessible for clinical evaluation ▪ Evidence-based clinical decision support: includes InterQual® criteria for standards of care, as well as regional product specific medical policy criteria, when applicable ▪ Single point-of-access: consolidated workflow for many types of authorizations across multiple payers; allows administration of various payment rules for coordination of benefits For instructions on how to use Clear Coverage, access our resource guide at ExcellusBCBS.com/ProviderEducation. In addition, you may contact your Provider Relations Representative to schedule training. Please direct questions related to Clear Coverage to Customer Care. Stay tuned for details on when Clear Coverage will be available for urgent/emergent preauthorizations! Coding Update P/F Evaluation & Management Codes CMS has identified evaluation and management (E/M) codes as an area having significant error rates. The Recovery Audit Program has started auditing levels of E/M codes. Excellus BCBS has found a high incidence of over-coding for certain E/M services and recommends that physicians carefully document each service provided, according to CMS guidelines. The CMS documentation guidelines for E/M codes may be viewed by clicking here. Drug Screening Tests Billing Guidelines P/F ATTENTION: Physicians, Reference Labs & Hospitals Our billing guidelines for drug screening tests mirror those established by CMS. When submitting claims for drug screening tests, please follow the guidelines outlined in the bulletin issued to your office or facility on July 29, 2014. You can access the notice by clicking here. Note: Billing guidelines pertain to all Excellus BCBS products and lines of business; claims submissions that do not meet our guidelines will be denied. 5 September 2014 Vision Billing Guidelines Effective October 1 P Effective October 1, 2014, Excellus BlueCross BlueShield will require your office to follow the guidelines below when rendering eye exam and eyewear (frames/lenses/contact lenses) services to its members. These guidelines apply to all lines of business. When rendering an eye exam to a member and he or she requires eyewear, bill the exam separately from the claim for eyewear. Both services, even when rendered together, require unique taxonomy codes and therefore require separate claims. The following taxonomy codes should be used: Eye Exam: When billing for an eye exam, use your provider specialty taxonomy code (i.e., 152W00000X). Eyewear (frames/lenses/contact lenses): When billing for eyewear, use taxonomy code 332H00000X. This taxonomy applies only to eyewear. Claim Submission Details Paper - CMS-1500 Claim Form - The taxonomy code should be identified with the qualifier “ZZ” in the shaded portion of Box 24I. If the billing provider is a Group, the taxonomy code should be in the shaded portion of Box 24J. If the billing provider is an Individual, the taxonomy code should be placed in Box 33B. Electronic - For electronic claim submissions with the 837P (ASCX12N/5010X222A1) format, the taxonomy code should be identified as follows: 2000A PRV01 = BI PRV02 = PXC PRV03 = taxonomy code If billing provider is an individual provider, then taxonomy code is reported in Loop 2000A (billing provider loop) 2310B PRV01 = PE PRV02 = PXC PRV03 = taxonomy code If billing provider is a group, then taxonomy code is reported in Loop 2310B (rendering provider loop) 2420A PRV01 = PE PRV02 = PXC PRV03 = taxonomy code Used if a service line rendering provider is different than claim level rendering provider, then the service line taxonomy code is reported in Loop 2420A (service line rendering provider loop) If eye exam and eyewear services are submitted together on the same claim, the claim will deny. If you have billing questions, contact your Provider Relations Representative. For customer care inquiries, please call our dedicated Vision Services line at 1-855-272-6961. 6 September 2014 Submitting Claims for Sterilization or P/F Hysterectomy Performed on Medicaid Managed Care or Family Health Plus Members We remind you of the following special requirements for submitting a claim for sterilization or hysterectomy procedure performed on a member in a Medicaid Managed Care or Family Health Plus program. Sterilization Members must be at least 21 years of age at the time of informed consent and mentally competent, and they must complete and sign the Sterilization Consent Form at least 30 days, but not more than 180 days, prior to a bilateral tubal ligation or vasectomy procedure, or any other medical procedure, treatment or operation for the purpose of rendering an individual permanently incapable of having a child. “Informed consent” means that the member gave consent voluntarily after the provider planning to perform the procedure has: Offered to answer any questions; Told the member that he or she is free to withhold or withdraw consent to the procedure at any time before the sterilization without affecting his or her right to future care or treatment and without loss or withdrawal of any of his or her federally funded benefits; Told the member that there are alternative methods of family planning and birth control; Told the member that the sterilization procedure is considered to be irreversible; Explained the exact procedure to be performed on the member; Described the risks and discomforts the member may experience including effects of any anesthesia; Described the benefits and advantages of sterilization; and Advised the member that the sterilization will not be performed for at least 30 days following the informed consent, and the provider planning to perform the procedure: o Made arrangements so that the above information was effectively communicated to a blind, deaf or otherwise disabled person; o Provided an interpreter if the member did not understand the language on the consent form or the person who obtained informed consent; and o Permitted the member to have a witness present when consent was given. Hysterectomy Hysterectomy is covered only in cases of medical necessity and not solely for the purpose of sterilization. Members must be informed that the procedure will render them permanently incapable of reproducing. A member must complete the Acknowledgement of Receipt of Hysterectomy Information Form, at least 30 days prior to the procedure. Prior acknowledgment may be waived when a woman is sterile prior to the hysterectomy, or in life-threatening emergencies where prior consent is impossible. The performing provider must send a copy of the completed Sterilization Consent Form or Acknowledgement of Receipt of Hysterectomy Information Form to Excellus BCBS either prior to submitting a claim for the procedure or with the claim for the procedure. Providers may obtain these forms via the NYSDOH website at www.health.ny.gov/health_care/medicaid/publications/ldssforms.htm. We will deny payment for sterilization procedures or hysterectomy if the physician fails to submit evidence of informed consent given within the required time frames. 7 September 2014 Quality Improvement Organization Program Restructuring F ATTENTION: Skilled Nursing Facilities, Home Care Providers and Hospitals CMS has notified us of its intent to restructure the Quality Improvement Organization program to improve patient care and health outcomes, as well as to save taxpayer resources. As a result, the Quality Improvement Organization program will be replaced with Beneficiary and Family-Centered Care Quality Improvement Organizations. As of August 1, 2014, Excellus BCBS’s current Quality Improvement Organization program contractor, Island Peer Review Organization, Inc. has been replaced by the new Beneficiary and Family-Centered Care Quality Improvement Organizations contractor, Livanta. Please maintain the following contact information in your records: Address: Livanta BFCC-QIO 9090 Junction Drive, Suite 10 Annapolis Junction, MD 20701 Phone: Toll-free Number: 1-866-815-5440 TTY: 1-866-868-2289 Fax: Appeals: 1-855-236-2423 All other reviews: 1-844-420-6671 Livanta is now responsible for conducting quality of care reviews, discharge and termination of service appeals, and other areas of required review. You must update the notices listed below with the new BFCC-QIO information: The Notice of Medicare Non-Coverage Form (Form CMS 10123-NOMNC); and Important Message from Medicare (IM) (Form CMS-R-193) Need more information or have questions? More information about the Quality Improvement Organization restructuring is detailed in the CMS press release. Click here to access. If you have any questions about the Quality Improvement Organization program, contact the Quality Improvement Organization Program mailbox at QIOProgram@cms.hhs.gov. For questions related to the notices of non-coverage, contact Part_C_Appeals@cms.hhs.gov 8 September 2014 Talk To Your Patients Age 65 & Older About Exercise & Physical Activity Exercise and physical activity are important at every age. However, for your patients who are age 65 and older, it can play a key role in supporting physical and mental health. Exercise and physical activity can make a difference in preventing falls, managing chronic disease and preventing depression. P Be sure to ask your patients about their exercise and physical activity. We realize you have much to accomplish during appointments, so we encourage you to include this topic with annual assessments of chronic health problems (i.e., diabetes, heart disease, osteoarthritis and fall prevention).Keep your conversations focused on the benefits of the exercise and physical activity as it relates to the patient’s overall health and the management of the chronic disease(s). Your promotion and encouragement of healthy changes in your patients can make a difference in keeping patients who are currently exercising engaged, and it can motivate those who are not active to start exercising. The Centers for Medicare & Medicaid Services conducts Health Outcomes Surveys for Medicare enrollees, and one of the areas of inquiry relates to levels of physical activity. Patients are asked if a discussion has taken place with their doctor regarding exercise. These conversations with your patients help to support a quality focus of the Health Outcomes Surveys. We appreciate your attention to this important topic. BlueCard® Corner P/F Medicare Advantage PPO network sharing allows Medicare Advantage PPO members to obtain in-network benefits when traveling or living in a service area of any other BCBS Medicare Advantage PPO plan, as long as the member obtains services from a contracted Medicare Advantage PPO provider. Q. What does this mean for my office? A. If you are a contracted Medicare Advantage PPO provider with us and you render services to Medicare Advantage PPO members from other BCBS plans, these members will be extended the same contractual access to care and will be reimbursed in accordance with your negotiated rate with your Excellus BCBS contract. These members will receive in-network benefits in accordance with their member contract. If you are not a contracted Medicare Advantage PPO provider with us and you provide services for any BCBS Medicare Advantage PPO members, you will receive the Medicare allowed amount for covered services. For urgent or emergency care, you will be reimbursed in accordance with applicable state or federal law. Other services will be reimbursed at the out-of-network benefit level. Q. How will I recognize these members? A. The “MA” suitcase (see example below) on the member’s ID card indicates that he/she is covered under the Medicare Advantage PPO network sharing program. These members have been asked not to show their standard Medicare ID card when receiving services; instead, they should provide their BCBS member ID card. (continued on the following page) 9 September 2014 BlueCard® Corner (con’t) P/F Q. Do I have to provide services to Medicare Advantage PPO members from these other Blue Plans? A. If you are a contracted Medicare Advantage provider with us, you should provide the same access to care as you do for Excellus BCBS Medicare Advantage PPO members. If you are not a Medicare Advantage contracted provider, you may see BCBS Medicare Advantage PPO members; however, you are not required to do so. Should you decide to provide services to these members, you will be reimbursed for covered services at the Medicare-allowed amount, based on where the services were rendered and under the member’s out-of-network benefits. Q. What if my practice is closed to new Medicare Advantage PPO members? A. If your practice is closed to new Medicare Advantage PPO members, you do not have to provide care for out-of-area BCBS members. The same contractual arrangements apply to these members as your local Medicare Advantage PPO members. Q. How do I verify benefits and eligibility? A. Call BlueCard Eligibility at 1-800-676-BLUE (2583) and provide the member’s alpha prefix located on his or her ID card. You may also submit electronic eligibility requests for these members via our website, ExcellusBCBS.com/Provider. If you experience difficulty obtaining eligibility information, please record the alpha prefix and report it to Excellus BCBS. Q. Where do I submit the claim? A. You should submit the claim to Excellus BCBS under your current billing practices. Do not bill Medicare directly for any services rendered. Q. What is the member cost-sharing level and copay? A. Medicare Advantage PPO members who see Medicare Advantage PPO-contracted providers in Excellus BCBS’s service area will pay the same cost-sharing level (in-network cost sharing) they would pay if they received covered benefits from any Medicare Advantage PPO in-network providers. You may collect the copay amounts from the member at the time of service. Q. May I balance-bill the member the difference in my charge and the allowance? A. No, you may not balance-bill the member for this difference. Members may be balance-billed for any deductibles, coinsurance, and/or copays. Q. What if I disagree with the reimbursement amount I received? A. If there is a question concerning the reimbursement amount, contact Customer Care. Q. Who do I contact if I have a question about the Medicare Advantage PPO network? A. If you have any questions regarding the program or products, contact Customer Care. 10 September 2014 Medical Policy Updates P/F Excellus BCBS works to ensure that the development of corporate medical policies occurs through an open, collaborative process. We encourage participating providers to become actively involved in medical policy development. Each month, draft policies are available on our website for review and comment. To access, click here. New! Providers now have the capability of attaching supporting documentation related to their comments. Medical Policy Changes to Align with CareCore Criteria for New UM Programs As a reminder, we collaborated with CareCore National on three new programs: Radiation Therapy, Cardiac Devices and Sleep Services (e.g., sleep studies, PAP devices, supplies). These services have been added to the Utilization Management Standard Clinical Review Preauthorization List, which is available via our website, ExcellusBCBS.com/wps/portal/xl/prv/refauth/guidelines/. Our goal is to work in conjunction with CareCore to create comparable criteria that will allow for consistent decision-making across all lines of business. Please note that the criteria for our Brachytherapy or Radioactive Seed Implants for Prostate Cancer and Positive Airway Pressure Devices medical policies have been revised to be consistent with CareCore’s criteria. When policy criteria change, our requirements related to medical records may also change. Please refer to our website, or call Customer Care, for the most current information. Medical records requirements can also be found on our website. Failure to submit required records with claim submission may delay processing and payment. Although medical policies may be effective on the date they are approved by the Medical Policy Committee, updates to the claims processing systems may not occur for up to 90 days. Questions regarding medical policies should be directed to Customer Care. News from FLRx P/F Wegmans Home Delivery Pharmacy Available to Members Starting August 11, 2014, we began offering an additional pharmacy home delivery option to our members who take prescription maintenance medications and have commercial and Medicare Part D coverage. Wegmans Home Delivery Pharmacy is now an option for members in addition to PrimeMail and Walgreens*. We hope you will encourage your patients to take advantage of one of the pharmacy home delivery options. Home delivery is convenient and can save the member as much as 33 percent on the cost of a three-month supply of their prescription maintenance drugs. Transferring prescriptions is easy! Members simply call one of the following phone numbers: Wegmans Pharmacy 1-800-586-6910 PrimeMail 1-866-260-0487 *ONLY for members with Medicare Part D coverage: Walgreens Mail Service Pharmacy 1-800-999-2655 If you have questions, contact our Pharmacy Help Desk at 1-800-724-5033. (continued on the following page) 11 2014 Stay Current on Important Dates! Post this calendar at your desk! Member Care Management: Together, we’re better. October A nonprofit independent licensee of the Blue Cross Blue Shield Association September Sun Mon Tue Wed Thu Fri Sat 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 September 1st - Office closed for Labor Day Sun Mon Tue Wed Thu Fri Sat 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 October 1st New vision billing guidelines effective October 1. Click here to read the bulletin. - Reimbursement for vaccine administration will no longer be made if the corresponding vaccine code is not included on the claim - applies to 9th Navigating the Blues starts for the month of October Medicaid Managed Care, Family Health Plus, Child Health Plus and 28th Fall Seminars start for the month of October Healthy NY ONLY 11th Navigating the Blues starts for the month of September *Dates subject to change. Help In Managing Your Patients Who Have High Cholesterol Heart disease is the leading cause of death in the United States. High cholesterol levels have been shown to play a major role in the progression of heart disease. September is Cholesterol Education month. With the holiday season only months away, this is a great opportunity to talk to your patients about how to control their cholesterol intake. One way is to encourage them to eat more fruits and vegetables, because there is NO CHOLESTEROL in plant-based foods. Excellus BCBS offers your patients a comprehensive Member Care Management suite of programs to assist them in optimizing their health. If you have patients who are struggling with the management of their heart condition, we can help. We have programs designed specifically for coronary artery disease and congestive heart failure. Our goal is to assist your patients in complying with your treatment plan. You can refer your patients to the programs by calling 1-800-434-9110. Visit us online at ExcellusBCBS.com/Provider. Tried online, but still need help? Contact Customer Care at 1-800-920-8889