QUIZ/TEST REVIEW NOTES SECTION 2 RENAL PHYSIOLOGY
advertisement

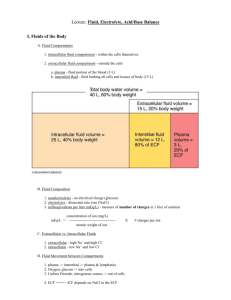
1 QUIZ/TEST REVIEW NOTES SECTION 2 RENAL PHYSIOLOGY FILTRATION [THE KIDNEYS/URINARY SYSTEM] CHAPTER 19 I. REABSROPTION OVERVIEW a. b. c. Learning Objectives: Differentiate the following processes: filtration, reabsorption, secretion, excretion Explain how the structure of the glomerulus promotes and limits filtration Describe the factors that influence GFR and the processes involved in its regulation Explain how creatinine clearance is determined and describe its clinical significance More then 99% of the fluid entering the tubules must be reabsorbed into the blood as filtrate moved through the nephrons Most reabsorption takes place in the proximal tubule, with smaller amounts in the distal segments i. Regulated reabsorption by hormones in the distal nephron allows kidneys to return ions and water to the plasma selectively – as needed to maintain homeostasis Reabsorption may be a Active or Passive i. Water and ions in the proximal tubule have the same solute concentrations as the extracellular fluid, so to move out of tubule cells must use active transport to create concentration or electrochemical gradients ii. DIAGRAM: General Overview of Tubular Reabsorption Active transport of Na+ from tubule men to ECF creates transepithelial electrical gradient in which lumen is more negative than the ECF + Anions then follow the positively charged Na out of the lumen + Net movement of Na and anions from lumen to ECF causes water to follow by osmosis + 2+ Loss of volume from lumen increases the concentration of solutes (K , Ca , Urea) left behind in the filtrate o Unchanged amount of solute in a smaller volume produces an increase concentration Once luminal solute concentrations are higher than solute concentrations in the ECF, the solutes are free to diffuse out of the lumen if the epithelium of the tubule is permeable to them II. PASSIVE FOLLOWED BY ACTIVE; TRANSPORT OF SODIUM a. b. c. Active transport of Na+ is the primary driving force for most renal reabsorption Filtrate entering proximal tubules has a similar ion composition with plasma Filtrate has higher Na+ concentration then proximal tubule cells that separate tubule lumen and interstitial fluid of the peritubular capillaries 2 d. i. Na+ can thus enter tubule cells passively by moving down its electrochemical gradient + + + ii. In proximal tubule Na -H Antiporter players major role in Na reabsorption + One inside tubule cell Na is actively transported out across basolateral membrane by Na+-K+-ATPase III. SECONDARY ACTIVE TRANSPORT: Symport with Sodium a. Sodium-linked secondary active transport i. Sodium binds with other organic metabolite to help transport across tubule into interstitial fluid ii. Responsible for glucose, amino acid, ion, and various organic metabolite reabsorption iii. DIAGRAM: Sodium-linked glucose reabsorption in proximal tubule Na+-dependent glucose reabsorption across proximal tubule epithelium + + Proximal tubule cell apical membrane contains (SGLT) Na -glucose co-transporter that harnesses the energy of Na for use by Glucose to diffuse Na+ is then pumped from proximal tubule cell to interstitial fluid by Na+-K+-ATPase Glucose is then pumped from proximal tubule cell to interstitial fluid by GLUT transporters 3 IV. UREA: PASSIVE REABSORPTION a. b. c. Urea: nitrogenous waste product No active transporters in proximal tubule but will move across epithelium by diffusion if there is a urea + concentration gradient [gradient usually created by active transport of Na and other solutes] Process: i. When Na+ and other solutes are reabsorbed from the proximal tubule the transfer of osmotically active particles makes the ECF more concentrated than the filtrate remaining in the lumen ii. As a response to the osmotic gradient, water moves by osmosis from tubule lumen to ECF iii. When H2O leaves lumen for ECF the filtrate concentration of urea increases because the same amount of urea is contained in a smaller volume iv. Once concentration gradient for urea exists, urea diffuses out of lumen in to ECF V. SATURATION a. Saturation of Renal Transport Plays an Important Role in Kidney Function i. Saturation refers to maximum rate of transport that occurs when all available carriers are occupied by a substrate ii. The transport rate at saturation is the transport maximum (TM) [mg/min] 1. Transport maximum is the maximum rate at which 100% of a substance can be reabsorbed iii. Ex: Glucose Reabsorption 1. Normal plasma glucose concentrations, all glucose that enters the nephron is reabsorbed before it reaches end of proximal tubule 2. If person has diabetes mellitus, or excessive blood glucose concentrations, glucose is filtered faster than the carriers of the peritubular capillaries can reabsorb it a. Result: Glucose escapes reabsorption and is excreted in the urine b. The plasma concentration at which glucose first appears in the urine is called the renal threshold [mg/min] for glucose Calculations a) GFR x plasma concentration = filtration rate b) GFR x renal threshold = TM Transport rate of a substance is proportional to the plasma concentration of the substance up to the point at which transporters become saturated Once saturation occurs transport rate reaches a maximum (T M) The plasma concentration of substrate at which the (TM) occurs is called the renal threshold Excretion = Filtration (increasing) – Reabsorption (constant) VI. PERITUBULAR CAPILLARY PRESSURES FAVORS REABSORPTION a. Drive force for reabsorption from the interstitial fluid into the capillaries is the low hydrostatic pressure that exists along the entire length of the peritubular capillaries i. Peritubular capillaries have hydrostatic pressure [blood pressure; opposes movement of fluid into peritubular capillaries] of 10 mm Hg (in contrast to glomerular capillary hydrostatic pressure which is 55 mm Hg) ii. Colloid osmotic pressure (favors movement of fluid into peritubular capillaries) is 30 mm Hg 1. RESULT: Pressure gradient is 20 mm Hg in favor of absorption of fluid into capillaries a. Fluid that is reabsorbed then passes from capillaries to venous circulation and returns to the heart 4 VII. FLUID/ELECTROLYTE HOMEOSTATIC BALANCE a. b. c. d. e. f. In the coarse of a day we consume roughly 2 liters of food and 6-15 grams of NaCl i. Also bring in various electrolytes including K+, H+, Ca2+, HCO -3 and phosphate (HPO2-4) THIRST: critical because drinking is only normal way to replace lost water SALT APPETITE: critical behavior that leads people to seek and ingest salt (sodium chloride NaCl) Importance of + i. H2O and Na : Associated with ECF volume and osmolarity + ii. K : Inbalances can cause serious problems with cardiac and muscle function 2+ iii. Ca : Variety of body processes, from Exocytosis and muscle contraction to bone formation and blood clotting + iv. H and HCO 3: Ions whose balance determines body pH ECF Osmolarity Affects Cell Volume i. If osmolarity of ECF changes water moves into or out of cells and changes intercellular volume ii. If ECF osmolarity decreases (result of excess water intake) water moves into cells and they swell iii. If ECF osmolarity increases (result of salt intake) water moves into cells and they shrink 1. Shrinking or swelling (changes in cell volume) can impair cell function 2. Ex: Swelling cells ion channels in membrane open disrupts membrane potential and cell signaling Fluid and Electrolyte Balance Requires Integration of Multiple Systems i. Fluid and electrolyte balances is integrative because it involves cardiovascular and respiratory systems, and renal and behavioral responses 1. Rapid Responses performed by: a. Lungs Under Neural Control b. Cardiovascular system 2. Slow Responses performed by: a. Kidneys Under Endocrine and neuroendocrine control CAPATION: The Body’s Integrated Responses to Changes in Blood Volume and Blood Pressure 5 WATER BALANCE OSMOSIS EXPLAINED a. b. c. d. Water Distribution rd a. Plasma: 8% Plasma (effects) 3 space (effects) rd b. Interstitial Tissue: 25% [tissue fluid/external fluid/3 space] intracellular space c. Intracellular Fluid: 67% Tonicity and Cell Volume Osmosis: Water a. Effect of cell in isotonic environment: No Change movement from low b. Effect of cell in hypertonic environment: Cell shrinks/dehydrates gradient to high c. Effect of cell in hypotonic environment: Cell swells/rehydrates gradient IV Fluid Therapy a. Blood volume/pressure therapy i. Isotonic solution b. Rehydration therapy i. Hypotonic solution c. Tonicity d. Salt content determines water movement Volume-Osmolarity Challenges a. Sensors i. Volume receptors = Atria of heart ii. Baroreceptors = Carotid arteries and aortic arch iii. Osmoreceptors = Hypothalamus b. Effectors i. Glomerulus = GFR ii. Hypothalamus = Thirst Fig 20-18 on back of iii. Heart = C.O. (cardiac output) page/overview of system iv. Vasculature = P.R. (peripheral resistance) physiology for dehydration v. DCT = Na Reabsorption compensation vi. Collecting Duct = Water Reabsorption c. Rules i. Body responds to changes in osmolarity before it responds to changes in blood volume/pressure ii. If two efferent pathways have opposite effects on the same effector, assume that negative feedback is dominant; that is, the one that opposes the initial stimulus 6 VIII. URINE CONCENTRATION IS DETERMINED IN THE LOOP OF HENLE AND COLLETING DUCTS a. b. Osmolarity (urine concentration) is a measure of how much water is excreted by the kidneys ↑ (excess) water kidneys excrete copious amounts of dilute urine with osmolarity as low as 50 mOsM i. Removal of excess water in urine is known as dieresis c. ↓ (low) water kidneys conserve water and urine becomes highly concentrated, as high as 1200 mOsM [1200 mOsM is four times as concentrated as blood which is 300 mOsM] + d. Kidneys alter urine concentration by varying the amount of 1) water and 2) Na reabsorbed in distal nephron ((specifically the DCT)) ↑ Osmolarity excess i. Produce Dilute Urine: Non-permeable water membrane (no H2O reabsorption) that allows solute electrolyte solutes such as Na, K, to pass Cl, phosphates ii. Produce Concentrated Urine: Nephron reabsorbs H2O while leaving solute in tubule lumen ↓ Osmolarity decrease of e. Osmosis (diffusion of water from ↓ to ↑ areas) will not take place unless concentration gradient exists electrolyte solutes i. Renal medulla maintains high osmotic concentration in interstitial fluid ii. High Medullary interstitial osmolarity allows urine to be concentrated f. Fluid Movement through the Loop of Henle i. Reabsorption in the proximal tubule is isomotic Loop Diuretics ii. Filtrate entering loop of Henle (descending tubule) has osmolarity of 300 mOsM (isomotic to 1) Furosemide (Lasix) 2) Bumetanide (Bumex) blood) a. Both work on loop of iii. Filtrate leaving loop of Henle (ascending tubule) has osmolarity of 100 mOsM (hyposmotic to Henle blood) b. Block Na-K-Cl (sodium 1. Hyposmotic fluid created by thick portion of ascending limb where Na2+, K+, and Cl- are potassium chloride pumps) transported out of the tubule lumen c. Block reabsorption of 2. These cells apical surface is impermeable to water thus when cells transport solute out sodium (which thus of lumen water cannot follow, creating a hyposmotic solution blocks H2O reabsorption to iv. Hyposmotic fluid leaving the loop of Henle then passing through the distal tubule and into the peritubular collecting duct, its final concentration is determined by the epithelia cells permeability to water in capillaries/interstitial the distal nephron tissue and space) 1. Cells not water permeable water remains in tubule and filtrate remains dilute d. Used to lower fluid volumes (increase 2. Cells water permeable water diffuses out of tubule and into the interstitial fluid excretion) making filtrate becomes concentrated e. Given to patients with v. Kidney’s homeostatic mechanisms can do nothing to restore lost fluid volume; one ingestion or CHF, edema, high blood volume, heart infusion of water (through IV) can replace water that has been lost failure Loop of Henle Volume Concentration Descending Loop Ascending Loop Decreases Unchanged Increases Decreases CAPTION: REFERENCE 7 CAPTION: OSMOLARITY CHANGES AS FILTRATE FLOWS THROUGH THE NEPHRON g. The Loop of Henle Is a Countercurrent Multiplier i. The Renal Countercurrent Multiplier 1. Transfers solutes instead of heat as in a typical countercurrent exchange system 2. Filtrate enters descending limb which is permeable to water and impermeable to ions a. Decreasing Volume b. Increasing Concentration i. Water moving by osmosis into more highly concentrated (bigger gradient) of interstitial fluid of vasa recta 3. Ascending Loop of Henle a. Impermeable to water b. Permeable to ions (Na, K, and Cl) i. Loss of solute (ions) causes filtrate osmolarity to decrease c. 25% of Na and K reabsorption takes place in ascending limb + d. NKCC symporter (Na/K/Cl/Cl) uses energy stored in Na concentration gradient + + to transport Na , K , and 2Cl from lumen of Henle into interstitial fluid i. NKCC symporter inhibited by loop diuretic drugs (Lasix) 8 h. i. The Vasa Recta Removes Water i. Water or solutes that leave the tubule move into the vasa recta if an osmotic or concentration gradient exists between medullary interstitium and blood in vasa recta ii. Blood flowing through the vasa recta removes the water reabsorbed from the loop of Henle Urea Increases the Osmolarity of the Medullary Interstitium IX. HORMONES OF THE FLUID/ELECTROLYTE BALANCE Classification Excrete/Retain Water/Salt Blood Effects Hormones Involved Diuretic Excrete Water Atrial Natriuretic Peptide (ANP) Anti-Diuretic Retain Water Natriuetic Excrete Salt Anti-Natriuetic Retain Salt ↓ volume ↑osmolarity Conserve volume Maintain osmolarity ↓ volume ↓ osmolarity Conserve volume Maintain osmolarity a. Vasopressin (ADH) Angiotensin II Atrial Natriuretic Peptide Angiotensin II Aldosterone Diuretics i. Promote Excretion of or Water ii. Cause decrease in blood volume iii. Cause increase in osmolarity iv. Hormone: 1. Atrial Natriuretic Peptide a. Atrial Natriuretic Peptide (ANP; also known as atriopeptin) b. Peptide hormone produced in specialized myocardial cells in the atria of the heart i. Related hormone [BNP] Brain Natriuretic Peptide is synthesized by ventricular myocardial cells and certain brain neurons c. Released by the heart when myocardial cells stretch more than normal [as would occur with increased blood volume] d. Enhance Na+ and H2O excretion e. Inhibit the release of renin, aldosterone, and vasopressin f. Effects of ANP Inhibits (-) Aldosterone Inhibits (-) Angiotensin Inhibits (-) Vasopressin (ADH) Promotes (+) GFR 2+ Decreases Na reabsorption Prevents thirst and vasoconstriction Decreases water reabsorption Increases urine output Caption: Actions of Natriuretic Peptides 9 b. Anti-Diuretics i. Promote Retention of Water ii. Conserve volume iii. Main osmolarity iv. Hormones: 1. Vasopressin (ADH) a. When acting on target cells water pores are present in the apical membrane that allow water to move out of the lumen (by osmosis) and into interstitial fluid of the renal medulla b. Posterior Pituitary hormone c. Adds water pores (aquaporins) in the apical membrane of the collecting ducts i. Aquaporins activated by arrival of ADH from posterior pituitary gland and bind to designated cells, activating G-protein/cAMP second messenger system ii. Phosphorylation of intracellular proteins causes aquaporin-2 (AQP2) vesicle to move to apical membrane and fuse with it, making the wall permeable to water iii. This process is imitated by Exocytosis and ended by endocytosis is known as membrane recycling 10 d. STIMULI ABBREVIATED Blood osmolarity ↑ Blood volume ↓ Blood pressure ↓ 2. Stimuli for Vasopressin secretion i. Plasma Osmolarity 1. Monitored by Osmoreceptors, which are stretch sensitive cells that active sensory neurons when osmolarity increase above threshold 2. Osmoreceptors found in hypothalamus 3. When plasma osmolarity rises above 280 mOsM Osmoreceptors fire [releasing vasopressin] 4. When plasma osmolarity is below 280 mOsM Osmoreceptors do not fire [no release of vasopressin] ii. Blood volume 1. Stretch sensitive receptors found in the Atria 2. When blood volume is low the receptors signal hypothalamus to secrete vasopressin iii. Blood pressure 1. Monitored by carotid and aortic baroreceptors 2. When blood pressure is low the receptors signal hypothalamus to secrete vasopressin Angiotensin II a. (ANG II) signals aldosterone release from the adrenal cortex b. Tropic hormone; stimulates aldosterone secretion in most situations c. Most potent vasoconstrictor; constricts systemic arteries ↑BP without changing blood volume 11 d. e. Stimulates i. Thirst ii. Aldosterone iii. ADH Is component of the RAAS [Renin-Angiotensin-Aldosterone System] i. A multistep pathway for maintain blood pressure 1. RAAS stimulated by ↓ BP and Blood Volume 2. Juxtaglomerular Granular cells in afferent arterioles of nephron secrete enzyme called renin 3. Renin activates angiotensinogen into angiotensin I 4. Angiotensin I encounters enzyme angiotensin converting enzyme (ACE) and converts ANG I ANG II CAPTION: This map outline the control of aldosterone secretion as well as the blood pressure raising effects of ANG II f. Inhibited by pharmacological drug called ACE Inhibitors i. Antihypertensive drug ii. Drug blocks ACE-mediated conversion of ANG I ANG II; thereby helping to relax blood vessels and lower blood pressure + iii. Less ANG II less aldosterone decrease in Na reabsorption decrease ECF volume 12 c. Natriuetic + i. Cause Na (sodium) loss/excretion ii. Cause H2O loss/excretion iii. Used to lower blood pressure and blood volume iv. Hormone: 1. Atrial Natriuretic Peptide (ANP; also known as atriopeptin) 2. Peptide hormone produced in specialized myocardial cells in the atria of the heart a. Related hormone [BNP] Brain Natriuretic Peptide is synthesized by ventricular myocardial cells and certain brain neurons 3. Released by the heart when myocardial cells stretch more than normal [as would occur with increased blood volume] 4. Enhance Na+ and H2O excretion 5. Inhibit the release of renin, aldosterone, and vasopressin 6. Effects of ANP 2+ Inhibits (-) Aldosterone Decreases Na reabsorption Inhibits (-) Angiotensin Prevents thirst and vasoconstriction Inhibits (-) Vasopressin (ADH) Decreases water reabsorption Promotes (+) GFR Increases urine output d. Anti-Natriuetic i. Promotes Retention of salt ii. Conserves volume iii. Maintains osmolarity iv. Hormones: 1. Angiotensin II 2. Aldosterone a. Steroid hormone synthesized in the adrenal cortex + + b. Increases activity of Na -K -ATPase + + c. Causes Na reabsorption and K secretion d. Maintains blood volume e. Stimulated by i. Low osmolarity ii. Low blood volume 13 f. iii. Hyponatremia (↓ Na2+) iv. Hyperkalemia (↑K) v. Angiotensin II Inhibited by i. High osmolarity CAPTION: Aldosterone action in principal cells LOW BLOOD VOLUME/PRESSURE AND WATER CONSERVATION a. b. Low Blood volume activates RAAS Low blood volume stimulates vasopressin (ADH) secretion HIGH BLOOD VOLUME/PRESSURE AND WATER EXCRETION a. b. X. Atrial baroreceptors respond to high pressure by releasing ANP Pharmacological intervention: ACE inhibitors THE DCT REGULATES THE FINAL SODIUM CONTENT OF URINE a. Effects/mechanism of Na+ reabsorption NOTE: Na reabsorption generally linked to K i. Effect on Water secretion [Na-K exchange] 1. Drives water reabsorption ii. Effect on Potassium NOTE: Na-K exchange can be blocked by 1. Drives potassium reabsorption and secretion aldosterone antagonist Amiloride iii. Is enhanced by aldosterone 1. Aldosterone = Function in Na reabsorption/K secretion [released by adrenal cortex] 14 b. Diuretics Diuretics K Depleting (strong) Loop Diuretics [Na-K-2Cl in ascending limb] Thiazide Diuretics [TSCL in DCT] K Sparing (weak) Amiloride [ENaC in DCT] ARB [Aldosterone Receptor Blocker] ACE inhibitor Thizaides Act on ascending loop of Henle (DCT) Block Na reabsorption blocking water reabsorption increasing urine dilution Block K reabsorption excrete excessive amounts of potassium Giving to people with C.H.F, high BP, edema XI. Acid-Base Balance (pH Homeostasis) a. b. c. d. e. f. Normal pH of body is 7.40 (slightly alkaline) Normal pH range of plasma is 7.38-7.42 i. Acidosis 1. pH is to low 2. Neurons become less excitable and CNS depression results ii. Alkalosis 1. pH is to high 2. Neurons become hyperexcitable firing action potentials at the slightest signal Disturbances of acid-base balance are associated with disturbances in K+ balance Potassium (K+) and (H+) exchangers Compensation of pH leads to K+ imbalances Loop of Henle i. Proximal Tubule 1. Secretes Hydrogen 2. Reabsorbs HCO3ii. Distal Nephron 1. Controls Acid excretion 2. Intercalated cells (I cells) responsible for acid-base regulation 15