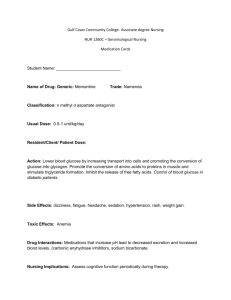
The effects of hyperglycemia on glucose metabolism in
advertisement

The effects of hyperglycemia on glucose metabolism in epithelial ovarian cancer by Lisa Danielle Kellenberger A Thesis presented to The University of Guelph In partial fulfillment of the requirements for the degree of Doctor of Philosophy in Biomedical Science Guelph, Ontario, Canada © Lisa Kellenberger, February, 2016 ABSTRACT THE EFFECTS OF HYPERGLYCEMIA ON GLUCOSE METABOLISM IN EPITHELIAL OVARIAN CANCER Lisa Danielle Kellenberger University of Guelph, 2016 Advisor: Dr. Jim Petrik Glucose metabolism in cancer cells is uniquely adapted to maximize the production of both ATP and the precursors needed to support cell proliferation and tissue growth. Glycolysis, an anaerobic process normally limited by the presence of oxygen, proceeds at an elevated rate in both aerobic and anaerobic conditions. Glycolysis consumes large quantities of glucose while producing relatively small amounts of energy. The inefficiency of this process is not detrimental to the cell when glucose is abundant. However, evidence suggests that in cancer the normal concentration of circulating glucose does not meet the energy demands of the tumour and is therefore a limiting factor in cancer cell metabolism. Hyperglycemic conditions such as diabetes are becoming common comorbidities in cancer patients and are associated with increased risk and poorer prognosis of epithelial ovarian cancer (EOC). We hypothesise that elevated blood glucose permits tumour metabolism to function at maximal capacity thereby facilitating tumour growth and metastasis. The goal of this thesis was to examine the metabolic response and glucose transport kinetics of EOC in hyperglycemic environments. By inducing ovarian tumour growth in mouse models of Type 1 and Type 2 diabetes, we found that accelerated disease progression occurs in a glucose concentration-dependent manner. In addition, for the first time we show that EOC cells express not only the passive glucose transporters (GLUTs), but also a class of active glucose transporters, the sodium-glucose symporters (SGLTs). Glucose uptake into EOC cells in hyperglycemia is mediated by this sodium-dependent glucose transport. Surprisingly, SGLT2 appears to be a tumour suppressor: knockdown of SGLT2 in ovarian cancer cells increases the relative risk of death in tumour-bearing mice by more than 50 times. PET scans measuring accumulation of the glucose analogue fluoro-deoxyglucose (FDG) are a vital component of EOC treatment. However, FDG is a poor substrate for SGLTs, suggesting that current imaging fails to detect a large fraction of glucose transport into tumours. The use of SGLT-specific glucose analogues, particularly in patients with metabolic dysfunction, presents an opportunity to enhance the power of PET imaging and provide a more complete picture of tumour metabolism which may have therapeutic benefits. Acknowledgements Dr. Jim Petrik, Esteemed Professor, who always puts things in perspective. Thank you. It’s been righteous. Dr. Alison Holloway, a mentor, advocate, and voice of reason for me since I was 17. My advisory committee: Dr. Jon Lamarre, Dr. Roger Moorehead and Dr. Lindsay Robinson. Maka Natsvlishvili, an expert and a wonderful teacher. Everyone at the Central Animal Facility for their help, support and genuine interest in these projects. Michelle Ross, who always listened and commiserated. Dr. Jim Greenaway, the ultimate scientist, cynic, and skeptic. Amanda Kerr, who shared the science happy-dance. Sam Russell, Jackie Dynes, and Funk Nights. Simone ten Kortenaar, the dancer, whistler, and optimist. Kata Osz, an artist, technician and general badass. Josh Antunes, for the techno and the drifting. Dr. Jenny Bruin, who trusted me with her work. Dr. Amy McPhedran, who always did more than her job. Mom, Dad, Nonnie and Grandpa for their unconditional support. Mark and Kevin who have been friends, foes, defenders, and great little brothers. Kelsey, who promised to read my “book”. Labmates, officemates, roommates. The pool, the road, the gym. The Science Gods (sometimes). Generous funding from a CIHR Vanier Canada Graduate Scholarship. Those damned mice. iv Declaration of work performed I declare that with the exception of the items listed below, all work reported in this thesis was performed by me. All tumour induction surgeries were performed with the assistance of Dr. Jim Petrik. Dr. Jim Petrik and Dr. Jim Greenaway assisted with some of the tissue collection. Insulin staining on pancreas sections in Figure 2A was done by Michelle Ross and serum insulin quantification in Figure 8A was done by Nicole DeLong in the lab of Dr. Alison Holloway at McMaster University. Intravenous injections of radiolabelled glucose analogues (Chapter 3) were performed by Jennifer Randall of the University of Guelph Central Animal Facility. Statistical analyses of mouse data in Chapter 3 were performed with the help of Dr. Cate Dewey. Kata Osz stained the tumour tissue slides shown in Figure 21B and C. The human ovarian tumour tissue microarray (Chapter 3) was imaged at the Advanced Optical Microscopy Facility (AOMF) at the University Health Network in Toronto. v TABLE OF CONTENTS Declaration of work performed .................................................................................... v LIST OF TABLES ...........................................................................................................ix LIST OF FIGURES.......................................................................................................... x LIST OF ABBREVIATIONS .......................................................................................... xiii CHAPTER 1: INTRODUCTION AND LITERATURE REVIEW ....................................... 1 Ovarian cancer ........................................................................................................... 1 Histological classifications ........................................................................................ 1 Screening and prevention ......................................................................................... 2 Tumour development ................................................................................................ 3 Diagnosis and clinical staging ................................................................................... 4 Treatment and disease management ....................................................................... 6 Current challenges.................................................................................................... 6 Glucose metabolism .................................................................................................. 7 Glycolysis ................................................................................................................. 7 Cellular Respiration .................................................................................................. 8 The citric acid cycle ............................................................................................... 8 The electron transport chain and oxidative phosphorylation.................................. 8 Anaerobic glycolysis (fermentation) .......................................................................... 9 Glucose metabolism in cancer ................................................................................. 9 The Warburg Effect............................................................................................... 10 Mitochondria ........................................................................................................ 11 Hypoxia ............................................................................................................... 12 Tumour acidification ............................................................................................ 13 Speed of metabolism ........................................................................................... 13 vi Metabolic intermediates....................................................................................... 14 Primary genetic changes ..................................................................................... 15 Hexokinase 2 (HK2) ............................................................................................ 16 High interstitial fluid pressure .............................................................................. 16 Metabolic flexibility............................................................................................... 17 Contributions of the tumour microenvironment ................................................ 18 The Crabtree Effect ............................................................................................. 18 Glucose transport .................................................................................................... 19 GLUTs .................................................................................................................... 19 SGLTs .................................................................................................................... 21 Positron emission tomography (PET) .................................................................... 24 Principle .................................................................................................................. 25 Limitations .............................................................................................................. 25 Use in gynecological cancers ................................................................................. 27 RATIONALE ................................................................................................................. 28 Hypothesis and objectives ...................................................................................... 28 CHAPTER 2: SYSTEMIC HYPERGLYCEMIA AND EOC PROGRESSION ................ 29 Introduction .............................................................................................................. 29 Materials and Methods ............................................................................................ 31 Results ...................................................................................................................... 39 Discussion ................................................................................................................ 58 CHAPTER 3: GLUCOSE TRANSPORT IN HYPERGLYCEMIC EOC ......................... 65 Introduction .............................................................................................................. 65 Materials and Methods ............................................................................................ 67 Discussion .............................................................................................................. 106 vii CHAPTER 4: ANTIDIABETIC EFFECTS OF METFORMIN AS EOC THERAPY ...... 114 Introduction ............................................................................................................ 114 Materials and Methods .......................................................................................... 117 Results .................................................................................................................... 123 Discussion .............................................................................................................. 143 CHAPTER 5: GENERAL DISCUSSION ..................................................................... 149 Overview ................................................................................................................. 149 The metabolic syndrome, diabetes, and EOC ..................................................... 151 Coordinated metabolism in the tumour microenvironment ............................... 154 Intersection of tumour metabolism and systemic metabolism.......................... 155 Glucose transport and diagnostic potential ........................................................ 157 Study Limitations ................................................................................................... 158 Conclusions ........................................................................................................... 160 REFERENCES ............................................................................................................ 161 Appendix I: Supplementary figures ......................................................................... 184 Appendix II: Source of supplies and materials ....................................................... 188 Appendix III: Recipes for solutions ......................................................................... 192 Appendix IV: RT-PCR primer sets............................................................................ 196 viii LIST OF TABLES Table 1: Prevalence of ovarian tumours by histology ...................................................... 2 Table 2: Frequency of EOC diagnoses by FIGO stage ................................................... 5 Table 3: SGLT protein expression in human ovarian cancer ......................................... 81 Table 4: Cox proportional hazard regression model for ovarian cancer survival ......... 102 Table 5: Median survival times of mice with SGLT2 KD tumours ................................ 103 ix LIST OF FIGURES Figure 1: SGLT secondary active symporters ............................................................... 22 Figure 2: Streptozotocin treatment models Type 1 diabetes ......................................... 41 Figure 3: Type 1 diabetes promotes tumour growth in proportion to blood glucose ...... 42 Figure 4: Chronic hyperglycemia limits ovarian tumour growth ..................................... 44 Figure 5: Acute and chronic hyperglycemia decrease survival in mice with EOC ......... 45 Figure 6: Tumour induction improves glucose tolerance in chronically diabetic mice ... 47 Figure 7: High blood glucose in Type 2 diabetic mice predicts larger tumours .............. 50 Figure 8: Tumours improve insulin sensitivity in Type 2 diabetic mice .......................... 51 Figure 9: EOC cells conditioned to hyperglycemic media accelerate scratch wound closing .......................................................................................................... 54 Figure 10: Cells conditioned to hyperglycemia are sensitive to glucose deprivation ..... 55 Figure 11: ID8-25 cells, but not ID8-6 cells, increase glucose consumption in hyperglycemia. ............................................................................................. 56 Figure 12: In high glucose media, cells conditioned to hyperglycemia have lower metabolic viability than cells conditioned to physiological glucose ............... 57 Figure 13: GLUT and SGLT transporters are expressed in ID8 cells ............................ 79 Figure 14: SGLT2 is overexpressed in human serous ovarian cancer .......................... 80 Figure 15: SGLTs affect glucose transport in hyperglycemia in cells conditioned to normal physiological glucose concentrations (ID8-6) ................................... 83 Figure 16: SGLTs affect glucose transport in hyperglycemia in cells conditioned to high glucose concentrations (ID8-25)................................................................... 84 Figure 17: SGLT inhibition does not affect cell metabolic viability ................................. 86 x Figure 18: Phlorizin and phloretin inhibit scratch wound healing in ID8-6 cells ............. 88 Figure 19: SGLT glucose transporters limit cell invasion in ID8-6 cells ......................... 90 Figure 20: Knockdown of SGLT2 in ID8 cells changes proliferative behaviour in culture ..................................................................................................................... 92 Figure 21: GLUT1 protein expression is higher the tumours of diabetic mice than in those of WT mice ......................................................................................... 94 Figure 22: Both GLUT and SGLT transporters are responsible for functional glucose uptake into tumours ...................................................................................... 96 Figure 23: SGLT2 KD impairs glucose uptake through active transport, but total glucose uptake is maintained through compensation by GLUTs ............................... 97 Figure 24: Expression of GLUT1 is highly upregulated in tumours with reduced SGLT2 expression at 45 days PTI ............................................................................ 99 Figure 25: SGLT2 knockdown leads to significantly larger primary tumours at death . 101 Figure 26: SGLT2 KD in tumours significantly decreases overall survival................... 102 Figure 27: Secondary disease is much more severe in mice with SGLT2 KD tumours ................................................................................................................... 104 Figure 28: Poor overall survival is associated with severe secondary disease, regardless of primary tumour weight, in mice bearing SGLT2 KD tumours 105 Figure 29: Cellular effects of metformin....................................................................... 116 Figure 30: Metformin inhibits EOC cell viability in high glucose .................................. 125 Figure 31: Metformin reduces cell number in glucose-deprived cultures .................... 127 Figure 32: Metformin increases cellular glucose consumption .................................... 129 xi Figure 33: Metformin-mediated increase in glucose consumption is independent of glucose transporter expression .................................................................. 130 Figure 34: Small tumours normalize blood glucose in diabetic mice ........................... 133 Figure 35: Daily metformin treatment does not affect EOC outcomes in WT mice ...... 135 Figure 36: Metformin treatment in WT mice with tumours impairs glucose tolerance over time. ........................................................................................................... 136 Figure 37: Daily metformin treatment does not affect EOC outcomes in Type 2 diabetic mice ............................................................................................................ 139 Figure 38: The presence of a tumour or treatment with metformin both improve glucose tolerance in diabetic mice ........................................................................... 140 Figure 39: Metformin treatment does not reduce the weight of established tumours .. 142 Figure 40: EOC metabolism is a product of cell genotype, the tumour microenvironment, and systemic glucose conditions ................................................................ 151 Figure 41: Positive SGLT1 staining on human ovarian tumour tissue ......................... 184 Figure 42: Dapagliflozin treatment does not affect tumour weight ............................... 186 xii LIST OF ABBREVIATIONS ABAM antibiotic/antimycotic AGE-RAGE advanced glycation end product receptor complex AMG 14C-α-methyl-d-glucopyranoside ANOVA analysis of variance ATP adenosine triphosphate BRCA breast cancer CB cytochalasin B DAB 3,3’-diaminobenzidine DAPI 4’,6-diamidino-2-phenylindole DMEM Dulbecco’s Modified Eagle Medium DNA deoxyribonucleic acid EOC epithelial ovarian cancer ETC electron transport chain FBG fasting blood glucose FBS fetal bovine serum FDG fluoro-deoxyglucose FIGO International Federation of Gynecology and Obstetrics G6P glucose-6-phosphate GLOX glucose oxidase GLUT facilitative glucose transporter IPGTT intraperitoneal glucose tolerance test HIF-1α hypoxia inducible factor alpha HK hexokinase HRP horseradish peroxidase ID8 mouse surface epithelial ovarian cancer cells IGF insulin-like growth factor IHC immunohistochemistry LDH lactate dehydrogenase KD knockdown xiii KO genetic knockout MTT 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide MRI magnetic resonance imaging OXPHOS oxidative phosphorylation PBS phosphate buffered saline PET positron emission tomography PFK phosphofructokinase PK pyruvate kinase PPP pentose phosphate pathway PT phloretin PTI post tumour induction PZ phlorizin RIPA radioimmunoprecipitation assay RT-PCR polymerase chain reaction SDS PAGE sodium dodecyl sulfate polyacrylamide gel electrophoresis SEER Surveillance Epidemiology and End Results (National Cancer Institute) SGLT sodium-glucose transporter STIC serous tubal intraepithelial carcinoma STZ streptozotocin T1DM Type one diabetes mellitus T2DM Type two diabetes mellitus TBST Tris-buffered saline with tween20 TCA the citric acid cycle TZD thiazolidinedione VDAC voltage-dependent anion channel WB Western blot WHO World Health Organization WST-1 water-soluble tetrazolium salt 1 WT wild type xiv CHAPTER 1: INTRODUCTION AND LITERATURE REVIEW Ovarian cancer Currently there are approximately 17,000 Canadian women living with ovarian cancer. Each year nearly 2,800 new cases are diagnosed and the disease claims the lives of 1,750 women, making it the most deadly gynecologic cancer and the fifth leading cause of all cancer deaths in women.1,2 Ovarian cancer most commonly affects postmenopausal women (median age at diagnosis is 62) and both incidence and mortality increase with age. In the general population the lifetime risk of developing ovarian cancer is 1.4% (1 in 71).2 BRCA gene mutation carriers are at a significantly increased risk (BRCA1: 30-60%, BRCA2: 15-30%)3 and cases in these women appear ten years earlier on average.4 Histological classifications Ovarian tumours can have stromal, germinal, or epithelial origins. Epithelial tumours are by far the most prevalent and make up close to 90% of ovarian cancers. The World Health Organization (WHO) has identified eight histologic subtypes of epithelial ovarian cancer (EOC): serous, endometrioid, mucinous, clear cell, transitional cell, squamous cell, mixed epithelial and undifferentiated.5 Table 1 indicates the prevalence of ovarian tumours based on histopathology.6 1 Table 1: Prevalence of ovarian tumours by histology Origin* Tumour Malignancy* Histology Benign 60% Borderline 10% High-grade serous 70% Epithelial 60% Low-grade serous <5% Malignant 30% 85-90% Mucinous 3% Endometrioid 10% Clear cell 5-10% Germ cell 30% Malignant <5% Sex-cord 8% stromal Malignant <5% * Remaining percentages of disease have undefined pathologies It is becoming clear that the histopathological subtypes of ovarian cancer are also associated with particular mutations.7 One of the most significant advances in the past decade has been the development of more descriptive classifications of ovarian cancer subtypes that also include cells of origin and genetic signatures (reviewed in 6). Screening and prevention Disease screening and prevention have been extremely challenging in EOC. Up to 90% of EOCs do not have an identified genetic component and there are no easily identifiable precursor lesions. Traditionally, the most successful clinical tools have been 2 transvaginal ultrasound and identification of elevated levels of the serum marker CA125, however neither is sensitive or specific enough for screening.7 In women at high risk for the disease, primarily BRCA mutation carriers, risk-reducing salpingooophorectomy is the most protective strategy.8 Tumour development For many years, epithelial ovarian cancer was suspected to arise from the continual disruption of the ovarian surface epithelium during ovulation. According to this “incessant ovulation” hypothesis, repeated post-ovulatory follicle repair9–12 and its associated inflammation13 enhance the possibility of mutagenesis. Continual follicle repair also increases the frequency of cortical inclusion cysts which are invaginations of the surface epithelium that expose naïve epithelial cells to the hormone-rich, thus potentially tumourigenic, ovarian stroma.14 This hypothesis supports many of the clinical observations related to disease risk factors: in general, circumstances that increase the number of ovulatory events are associated with increased risk of ovarian cancer, such as nulliparity, history of pelvic inflammatory disease and endometriosis. Conversely, fewer ovulatory events are generally associated with decreased risk of the disease, including oral contraceptive use and multiple pregnancies.15 The understanding of ovarian tumour development has been complicated by the fact that “epithelial ovarian cancer” has historically encompassed a histologically diverse group of pelvic tumours.16 As a way to reconcile this diversity of tumours Kurman and others used an integrated analysis of clinical, pathological and molecular genetics to 3 propose a two-pathway model that divides ovarian cancers into Type I, low-grade and borderline lesions; and Type II, high-grade aggressive tumours.17 Characterization of these pathways continues to improve as new genomic and microenvironmental data become available.9 The past decade has seen a substantial paradigm shift in the understanding of the cellular origins of EOC. Despite the fact that tumours were thought to arise from the ovarian epithelium, both tubal ligation and hysterectomy were found to provide a 67% reduction in the risk of developing ovarian cancer.15 In 2001, Piek and others noticed that the fallopian tubes of women carrying BRCA mutations often had dysplastic regions and occult cancers18 and shortly after, Medeiros and others implicated the fimbriae of the fallopian tubes as sites development of early serous tumours.19 In one study 71% of cases diagnosed as “serous ovarian carcinoma” showed lesions in the tubal epithelium known as serous tubal intraepithelial carcinomas (STICs).20 It is now accepted that many serous tumours originally considered as ovarian in origin actually arise from the fimbriated ends of the fallopian tubes.21 Current mouse models provide direct evidence that metastatic serous “ovarian” cancer can develop from primary fallopian tube tumours that grow to the engulf the ovary.22 Diagnosis and clinical staging Diagnosis of ovarian cancer is complicated by the fact that its symptoms are ambiguous and often resemble gastrointestinal problems.23,24 The most significant barrier to improving ovarian cancer outcomes is the inability to effectively identify the disease in 4 its early stages. The five-year survival rate drops precipitously once the disease has spread beyond the ovary, yet the majority of cases are not detected until after this point. At diagnosis, EOC is most commonly characterized as Stage III or IV using the International Federation of Gynecology and Obstetrics (FIGO) staging system (Table 2).25 The most current FIGO staging criteria reflect the importance of histological type/grading at the time of staging and the identification of STICs at the primary site. 26 Table 2: Frequency of EOC diagnoses by FIGO stage FIGO Stage Description Percent at diagnosis* 5-year survival I Confined to ovary/fallopian tube and peritoneal fluid 15% 90% II Extension/metastasis to other pelvic organs or peritoneum 19% 70% III Spread along both pelvic and abdominal peritoneal surfaces IV 39% 60% Distant metastases 17% * Remaining percentages of disease have undefined stages The spread of EOC is facilitated by the circulation of peritoneal fluid that carries particularly aggressive cells from the primary tumour to other pelvic and abdominal surfaces.10,27 Close to 40% of EOC patients present with malignant abdominal ascites that plays a critical part in chemoresistant and recurrent disease.28 5 Treatment and disease management Despite the fact that EOCs are so histologically diverse, the same treatment regime is generally used on tumours of all subtypes: cytoreductive surgery followed by several cycles of carboplatin and paclitaxel chemotherapy.29 The goal of the initial surgery is histopathological diagnosis, staging, and maximum removal of tumour tissue. 29 Minimum residual disease is associated with longer survival30 and it has been suggested that a low volume of disease after surgery may be a more important prognostic factor than an initial low stage.17,31 Recommended surgery may include total hysterectomy, bilateral salpingo-oophorectomy, tumour debulking, and omentectomy.32 Because ovarian cancer usually presents as peritoneal disease, surgery often examines structures adjacent to the ovaries including the fallopian tubes.33 Following surgery and chemotherapy, the disease is monitored using medical imaging and/or serum markers such as CA-125.7 Most women who succumb to the disease die of malignant bowel obstruction from widespread metastatic disease and limited mortality is associated with the primary ovarian tumour.29 Current challenges Despite advances in treatment over the past forty years, death rates from ovarian cancer have not changed appreciably between 2001 and 2012.25 In addition to late detection and disease spread within the peritoneal cavity, treatment challenges include drug resistance and cancer recurrence even after initial response to treatment. On average, advanced disease recurs within 18 months of treatment.29 Patients are given platinum-based chemotherapies until their tumours become resistant, at which point 6 doxorubicin or topotecan is recommended.34 The median survival of patients with platinum-resistant, recurrent disease is about three years, and just one year from the onset of platinum resistance.35 According to a recent international consortium, improving patient outcomes will come from using distinct histological and genetic subtypes to: stratify clinical trial design; identify new therapeutic targets; develop better experimental models; and design tools for prevention and early detection.36 Glucose metabolism In order to survive and replicate, the cells in ovarian tumours rely on the oxidation of glucose as their primary source of ATP energy, using metabolic processes that can occur both aerobically (oxidative phosphorylation, oxphos) and anaerobically (glucose fermentation). Glycolysis The anaerobic process of glycolysis in the cell cytoplasm initiates both oxphos and fermentation by metabolising a glucose molecule into two 3-carbon pyruvate molecules and two molecules of ATP. The net result of glycolysis can be represented as the following equation: Glucose + 2 NAD+ + 2 ADP + 2 Pi 2 NADH + 2 pyruvate + 2 ATP + 2 H2O + 4 H+ The rate of pyruvate production is controlled at the levels of the regulatory enzymes hexokinase (HK), phosphofructokinase (PFK), and pyruvate kinase (PK) in reactions that are virtually irreversible and are allosterically regulated by their products. While the 7 efficiency of ATP formation in glycolysis is only about 3%, the glycolytic reactions also supply the cell with various anabolic precursors. For example, in addition to continuing through the glycolytic cycle the first product of glycolysis, glucose-6-phosphate (G6P), can be further metabolised by G6P dehydrogenase to enter the pentose phosphate pathway (PPP) and synthesize ribose-5-phosphate required for nucleotide biosynthesis.37,38 Cellular Respiration The citric acid cycle When oxygen is present, pyruvate (the end product of glycolysis) is converted to acetyl coenzyme A which is further metabolized through the enzymes of the citric acid cycle (TCA), a series of reactions that take place in the mitochondria. The net reaction of the TCA can be summarized as: 2 acetyl-CoA + 6 H2O + 2 ADP 4 CO2 + 16 H+ + 2 CoA + 2 ATP + 2 FADH2 + 6 NADH While the TCA itself only produces two molecules of ATP, there are four dehydrogenase enzymes in the cycle that reduce the electron carriers NAD+ to NADH and FAD+ to FADH2. For every two electrons subsequently released from these carriers, up to three molecules of ATP can be synthesized through the electron transport chain (ETC). The electron transport chain and oxidative phosphorylation Oxidative phosphorylation (oxphos) refers to the generation of ATP energy in the mitochondria through the electron transport chain and the ATP synthetase enzyme. The 8 ETC is a series of four protein complexes located in the mitochondrial membrane, where each consecutive protein has a higher affinity for electrons. As electrons are released from the carriers NADH and FADH2 and move down the chain, the resulting release of energy is used to create a proton gradient across the mitochondrial membranes. When H+ ions are pumped from the inner mitochondrion to the outer chamber of mitochondrion, they create a strong negative electrical potential in inner mitochondrial matrix. Hydrogen atoms flow with this concentration gradient through ATP synthetase to form ATP from ADP. The newly synthesized ATP diffuses through the mitochondrial membranes to cytoplasm. In aerobic conditions, cells can produce up to 36 molecules of ATP per molecule of glucose from glycolysis and cellular respiration. Anaerobic glycolysis (fermentation) In the absence of oxygen, cells undergo lactic acid fermentation to regenerate the NAD+ required for glycolysis. Glucose2 lactate + 2 H+ When oxygen becomes available again, this reaction is reversed and pyruvate + NADH + H+ are regenerated. Glucose metabolism in cancer Normal cell metabolism is under the influence of the “Pasteur effect” where oxygen inhibits glycolysis through phosphofructokinase (PFK) regulation to facilitate the mitochondrial oxidation of glucose. However, glucose metabolism in cancer cells does 9 not adhere to these same patterns of regulation. In 1924 the German researcher Otto Warburg made a seminal observation of cancer cell metabolism: tumours produce significantly more lactate than normal tissue, indicating an abnormally active glycolytic pathway.39 The glycolytic rate in tumour cells can be more than 30 times higher than in normal cells.40 Curiously, Warburg’s tumours appeared to have uncoupled glycolysis from oxygen levels to maintain their highly glycolytic phenotype even in the presence of adequate oxygen, thus demonstrating “aerobic glycolysis.”41 Although not all cancerous cells have the same abnormalities in metabolism,42 the Warburg phenotype is so well preserved across diverse malignancies that it is now considered an independent hallmark of cancer.43 The Warburg Effect Understanding the significance of the Warburg phenotype remains a challenge and it is still not clear whether the effect is a “cause, correlate or facilitator” of a progressing malignancy.44 Warburg originally postulated that the abnormal metabolism of cancer cells is a result of defective mitochondria, writing that “the respiration of all cancer cells is damaged”41 – despite the fact that many investigators, including Warburg himself, found that cancer tissues maintain normal levels of respiration in addition to generating high levels of lactic acid.39,45–47 Warburg believed that impaired respiration was the ultimate cause of cancer, thus only cancer cells would show this property, even though significant evidence showed that aerobic glycolysis is common to many rapidly proliferating cell populations.48 Rather than damage to respiration, the Warburg effect more accurately reflects an impairment of glycolytic control.49 10 The diversity of factors associated with the development of the Warburg effect suggests that there is no single cause or consequence of abnormal metabolism in tumours. Parallel, reciprocal changes to genetic and environmental factors drive the evolution of the glycolytic switch.50,51 The structure and function of cancer cell mitochondria, the hypoxic nature of tumours, lactate-driven acidification of the tumour microenvironment, the capacity for metabolic turnover, production of biosynthetic intermediates, primary genetic changes, and the interstitial fluid pressure of tumours are all associated with the metabolic profile of cancer. Mitochondria Both structural and functional impairment of mitochondria are significant factors in the altered metabolism of cancer cells.52,53 Although damages to cellular respiration are not as complete or as universal as Warburg predicted, there is evidence that mitochondria in some highly glycolytic tumour cells have an impaired ability to transport electrons from pyruvate to molecular oxygen.54,55 While the mitochondria are not inactive, they may act at a low capacity56 and cancerous cells often have fewer organelles and reduced mitochondrial DNA (mtDNA) content.57 There are mutations and copy number changes to the mtDNA of many cancers53 in addition to nuclear DNA mutations in proteins involved in respiration.49 The function of TCA proteins located in the mitochondria including succinate dehydrogenase, fumarate dehydrogenase, and isocitrate dehydrogenase are also impaired in some cancers.49,58–60 Furthermore, inhibition of the respiratory enzyme citrate synthase can activate an epithelialmesenchymal transition that increases metastasis and proliferation.61 Taken together, 11 mitochondrial dysfunction leads to a more highly glycolytic phenotype that has been directly linked to tumourigenicity, while increasing oxidative phosphorylation can reduce the growth of cancer in vivo and in vitro.62 Hypoxia The Warburg Effect is often thought to arise as an adaptation to environmental pressures. In this case, cancer cells are not believed to be inherently glycolytic, but rather that the phenotype of aerobic glycolysis is secondary to intermittent hypoxia.63,64 Oxygen levels in the tumour microenvironment are significantly reduced as a result of pathologic tumour vasculature. Solid tumours inefficiently and chaotically develop new blood vessels to support their growing mass and consequently develop large areas of poorly perfused tissue.43 In these areas a steep oxygen gradient develops between the vasculature and the diffusion limit of oxygen, exposing many tumour cells to hypoxic conditions.65 A cell with an increased capacity for glycolytic metabolism would have a survival advantage in these transient hypoxic conditions. In support of this hypothesis, short-term hypoxia has been found to lead to the irreversible oncogenic transformation of embryonic mouse cells by promoting aerobic glycolysis that remains and supports growth even once normal oxygen pressure is restored.41 The cellular response to low oxygen is mediated primarily through the hypoxia-inducible factor (HIF) signaling cascade which regulates processes including glucose metabolism, angiogenesis, apoptosis, proliferation and survival and pH regulation. Gregg Semenza’s group in particular has made significant contributions to the understanding of HIF’s 12 effects on metabolism.66 Oncogenic stabilization of HIF1α induces the glycolytic proteins HK2, PFK-1, aldolase, enolase, and PKM2.40,66 Thus, hypoxia leads to the Warburg phenotype because glycolytic products build up and exceed the capacity of aerobic respiration, the production of lactate acid increases as Warburg observed. Tumour acidification A number of studies have shown that the lactate produced by increased glycolysis contributes to the aggressiveness of tumours. In order to prevent cellular acidification, lactate is shuttled out of the cell leading to the acidification of the tumour microenvironment.40 Acidity has been shown to promote proliferation,63 signal67 and facilitate68 tumour angiogenesis, suppress the immune response to a developing tumour,69 and increase mutation rate70,71 and resistance to chemotherapy.72 The pH of tumour tissue is around 0.5 units lower than normal, so H+ ions from the tumour diffuse and cause damage to surrounding normal tissue, thus facilitating invasion.73–75 Mathematical modeling shows that tumour acid production alone can explain both benign (a result of autotoxicity) and invasive tumour growth76, though the Warburg effect is not necessarily associated with metastatic potential.77 Speed of metabolism Cancer cells produce about 10% more total ATP than normal cells to support their rapid proliferation.49 When tissues are rapidly consuming energy, most of it is regenerated by the high turnover of anaerobic glycolysis.38 Although this is a relatively inefficient 13 process, if the cell is not limited by glucose availability aerobic glycolysis can supply ATP up to 100 times faster than oxphos.40 The production of lactate is necessary to sustain a high rate of glycolysis. The coenzyme NAD+ is required for the GAPDH reaction in the fifth glycolytic reaction. In oxphos NAD+ is regenerated by the electron transport chain, a process that is too slow to sustain cancer cell metabolism. As a consequence, tumour cells must regenerate NAD+ by converting pyruvate into lactate through lactate dehydrogenase (LDH). Metabolic intermediates In order to proliferate, the cell not only requires ATP energy, but also sufficient macromolecule biosynthesis and maintenance of redox balance.51 High rates of glycolysis have been shown to increase the production of biosynthetic building blocks including proteins, phospholipids, fat and nucleic acids.78,79 The ability of cells to produce these precursors allows them to become autonomous for their ability to take up nutrients, and thus reduce their dependence on the extracellular environment. Pyruvate kinase activity in glycolysis appears to be central to the production of anabolic precursors. Blocking the PKM2 isoform in cancer cells from converting phosphoenolpyruvate to pyruvate causes accumulation of upstream products which are then available substrates for the PPP and thus cell precursors for biosynthesis.80 Other secreted molecules from glucose metabolism, like lactate and alanine, can be used as precursors for hepatic gluconeogenesis which may provide further fuel for the tumour.81 14 Primary genetic changes While the Warburg effect may arise secondary to factors in the tumour microenvironment, there is also substantial evidence to suggest that it is a result of mutations in non-metabolic tumour suppressors or oncogenes.50,82,83 As early as the 1960s, it was noticed that the treatment of cells with an oncolytic virus increases glucose transport beyond what is expected for rapid growth alone, suggesting a switch to a less efficient metabolic process.84,85 More recently, a study showed that a glycolytic phenotype emerged from progressive transformation of primary human fibroblast cells with different oncogenes.86 The p53 tumour suppressor, which is mutated in 60-80% of all EOC cases,3 stimulates respiration and suppresses glycolysis. Loss of p53 function induces a Warburg phenotype through elevated activity of the glycolytic enzyme phosphofructokinase49 and enhanced flux through the pentose phosphate pathway. 87,88 Several papers have implicated the Akt kinase pathway in cancer cells as the main driver of Warburg effects as Akt oncogenes activate HK2 and PFK1/2, and promote GLUT recruitment to the plasma membrane.89,90 Expression of the M2 fetal isoform of pyruvate kinase (PK) rather than the PKM1 splice variant also plays an important role in the glycolytic switch and results in tumorigenesis.91 Most of the research on cancer cell metabolism and the Warburg effect has been done in solid tumours where the microenvironment is thought to largely mediate the Warburg effect. However, the effect also appears in hematologic malignancies: acute leukemia is dependent on glycolysis for survival and abnormally high glucose uptake visualized by FdG-PET is used to detect and stage Hodgkin’s disease, non-Hodgkin’s lymphomas and multiple myeloma.92 Because the “metabolic switch” can occur independently of tumour stromal 15 tissue, it may be an inherent property of malignant cells rather than exclusively a consequence of the microenvironment. Hexokinase 2 (HK2) Hexokinase 2 catalyses the formation of glucose to G6P, the first step of metabolism through both PPP and glycolysis. HK2 has emerged as an essential mediator of the Warburg Effect and, as the slowest step in the glycolytic pathway in some cancers,93 it may be the most important step in determining glycolytic flux.94–96 HK2 expression has been correlated with poor overall survival and its inhibition can restore oxidative metabolism and reduce proliferation.97 The Pederson group has contributed much of the research on the role of HK2 in cancer metabolism and describe hexokinase 2 as a “facilitator and gatekeeper of malignancy.” 98,99 HK2 can translocate between the mitochondria and cytosol in response to glucose. When it is bound to the mitochondrial membrane by the voltage dependent anion channel (VDAC), it promotes glycolysis by escaping allosteric inhibition by G6P.100 Pederson has proposed that the Warburg effect results from overexpressed HK2, VDAC binding HK2 to the mitochondria, and upregulation of the HK2 gene.99 High interstitial fluid pressure Tumours have been described as “biological pressure pumps” due to their high interstitial fluid pressure and microvascular pressure.101,102 This characteristic provides a major challenge to the delivery of therapeutic agents and immune cells, while 16 simultaneously helping to propel potentially metastatic cells out of the tumour. 103 The Van’t Hoff equation predicts that CO2 from the aerobic metabolism of glucose lowers intracellular osmotic pressure, while lactate produced from glycolysis increases intracellular osmotic pressure. A “Warburg ratio” (lactate:CO2) of greater than 1.0 indicates that there is relatively more glycolysis than oxphos, and osmotic pressure will rise, driving outward currents of interstitial fluid.103 Therefore the high interstitial fluid pressure common to solid tumours may be a direct consequence of tumour metabolism. Metabolic flexibility Although tumours have been described as “glucose addicted” they are in fact quite flexible in their fuel use and metabolize amino acids, fatty acids,104 lactate,51 ketones105 and particularly glutamine.106,107 Moreover, they are not committed to glycolysis. The Warburg effect is often misunderstood as a preference for glycolysis over respiration despite the fact that even in the most aggressive tumour cells tested, Warburg found almost an equal contribution of fermentation and respiration.41 In some tumour cells mitochondria are responsible for most of the ATP production.108 This flexibility means that for cancer cells to “starve” both respiration and fermentation must be compromised. In normal cells, impairing only one pathway is sufficient to kill.109 Cancer cells display different balances of glycolysis, oxidative phosphorylation and glutaminolysis depending on glucose availability and other environmental conditions.110–113 17 Contributions of the tumour microenvironment In solid tumours, intercellular interactions are crucial for cancer progression. Stromal cells including fibroblasts, immune cells and vascular endothelial cells make up the heterogeneous tumour tissue and contribute to tumour growth and resistance to therapeutics.114 Intratumoral heterogeneity of metabolism is emerging as an essential determinant of carcinogenesis.115 Michael Lisanti’s group has described a “reverse Warburg effect” in which cancer-associated fibroblasts (CAFs) are metabolically reprogrammed to perform aerobic glycolysis. This transformation allows the fibroblasts to enrich the microenvironment with lactate, pyruvate and ketone bodies which epithelial cancer cells then take up and metabolise through oxidative phosphorylation to synthesize high volumes of ATP.105,116,117 To facilitate this, cancer cells also induce increased expression of the H+-coupled lactate export protein monocarboxylate transporter 4 (MCT4) in stromal cells.117,118 Others have shown that a metabolic symbiosis exists between cancer cells in oxygenated and hypoxic environments within the tumour. The expression of the MCT1 importer in oxidative cancer cells allows them to use lactate exported by glycolytic cancer cells as a primary fuel.119,120 The Crabtree Effect Herbert Crabtree was a contemporary of Warburg who described a local, reversible adaptation in tumours where high levels of glucose suppress oxygen consumption and respiration and accelerate glycolysis. Crabtree confirmed Warburg’s observation that tumours showed abnormally high levels of glycolysis and oxygen is ineffective at 18 reducing glycolysis. However, he also observed that glycolytic activity in vitro limited respiration on average 12% in glucose vs non-glucose solution.121 Recent studies in Barrett’s esophagus confirm that the Crabtree effect is important to tumour development and is related advancement of pre-malignant lesions overt cancer.122 Glucose transport A primary consequence of the Warburg Effect is that cells have abnormally high glucose requirements. Glucose is a large, hydrophilic molecule that requires specific transmembrane proteins to cross the cell’s lipid bilayer, and so the expression of glucose transporters is a key mediator of aerobic glycolysis.123 There are two classes of transporters: facilitative glucose transporters (GLUTs) and sodium/glucose cotransporters (SGLTs). GLUTs The thirteen identified mammalian GLUT isoforms are grouped into three classes based on sequence similarities. Class I GLUTS (1,2,3,4) have been well characterized and are the most important in human disease.123 The GLUT proteins rely on a downhill concentration gradient to move glucose and other hexoses across the lipid bilayer. The magnitude and direction of glucose transport is dependent on both the number of glucose transporters and the steepness of the gradient.123 The expression of transporter isoforms is highly tissue specific. GLUT1 is expressed in erythrocytes but is also widely distributed in tissues throughout the body. GLUT2 is specific to the liver, pancreas and 19 small intestine; GLUT3 to the brain; and GLUT4 to insulin-responsive tissues including skeletal muscle, cardiac and adipose tissue. GLUT expression is integral to many metabolic and energy-sensing pathways including HIF, c-myc, Akt and AMPK. A pool of GLUTs is stored in vesicles in the cytoplasm and are translocated to the cell membrane as needed, most notably through insulin signaling pathways. GLUT transport works through a model of alternate conformation. Glucose binds to sites either on inside or outside of cell and this binding changes the protein conformation to open to the other side of membrane.38 GLUTs in cancer. GLUTs are essential to cancer metabolism (reviewed in 124) and their function is well documented in the literature. Experiments that oncogenically transform fibroblasts show that oncogenic transformation itself may trigger GLUT1 activity,40 one of the main determinants of the Warburg effect.125 GLUT1 is highly expressed in ovarian cancer, where tumour status (benign, borderline, or malignant) is correlated with the level of GLUT1 expression.126,127 Almost all invasive epithelial carcinomas are positive for GLUT1, independent of stage, grade, or histological subtype.126,128 Expression of GLUT-1 correlates with tumour proliferation and microvessel density in EOC. In addition, patients with rapidly proliferating advanced stage tumours overexpressing GLUT-1 have a lesser chance for optimal cytoreduction.127 Antibodies to GLUT1 decrease proliferation, induce apoptosis in nonsmall cell lung cancer and breast cancer cell lines, and appear to synergize with a 20 number of chemotherapeutics to enhance their apoptotic effects.79 Likewise, antisense GLUT1 mRNA inhibits tumour growth.129 SGLTs The sodium/glucose cotransporters work against the glucose concentration gradient and are required to establish and maintain higher intracellular glucose concentrations.130 The main actions of the SGLTs are in glucose reabsorption from the proximal tubule of the kidney (primarily SGLT2) and the brush border of the small intestine (primarily SGLT1). In the enterocyte, after being pumped into the cell, glucose flows with its concentration gradient through GLUT2 on the basolateral side of the enterocyte, thus moving glucose back into the blood stream (Figure 1).130 SGLTs are also expressed in the heart, brain, liver, thyroid and skeletal muscle.131 21 Figure 1: SGLT secondary active symporters SGLT in pathology. While there is a large body of research on the role of GLUTs in cancer, the contributions of the second class of glucose transporters is virtually unknown. Most of the research on SGLTs comes from outside of the cancer literature. In the last decade, the action of SGLT2 has garnered attention as a therapeutic target in Type II diabetes (reviewed in 132) as it increases renal glucosuria and adds to the effects of other antidiabetic drugs to improve glucose tolerance.133 SGLTs also play essential roles in mediating ischemic stress in the brain,134 protecting against the LPS-induced 22 apoptosis implicated in inflammatory bowel diseases (IBD) and bacterial enteritis,135 and defending against cardiac disease.136 Isoforms and structure. SGLTs belong to the 12-member SLC5 gene family of hexose transporters. SGLT1 and SGLT2 import sodium and glucose with 2:1 and 1:1 stoichiometry respectively and differ in the substrates they transport. SGLT1 is a high affinity transporter that moves both glucose and galactose while SGLT2, specific for glucose, transports at a high capacity but has a glucose affinity that is about four times lower. SGLT3 appears to act as a glucose sensor rather than a functional transporter; glucose binds similarly and produces an inward current of Na+, but no glucose molecules are transported across the cell membrane.137–140 Regulation. SGLT1 upregulation is mediated by the cAMP-PKA signaling pathway and takes several days to act.141 Over minutes, activation of cAMP pathway results in recruitment of an intracellular reserve pool of transporters to the plasma membrane where the number of cotransporters in the plasma membrane regulated by endo- and exo- cytosis of vesicles.130 In cardiac tissue, SGLT1 expression and function are regulated by insulin and leptin.136 SGLT expression and translocation to the cell membrane is also regulated through AMPK activation.142–144 Protein-protein interaction with extracellular domain of EGFR stabilizes SGLT-1 to prevent proteasomal degradation.145 Because SGLT1 expression is dependent on EGFR expression, it has been suggested that EGFR has a role in maintaining basal intracellular glucose level by this mechanism.40,145 23 Mechanism of action. Using the electrochemical gradient maintained by the Na+/K+ ATPase pump, SGLTs are secondary active symporters that transport glucose into the cell coupled with Na+. Glucose/sodium symport is followed by anions and water to maintain electroneutral isotonic fluid absorption.146 In addition to Na+ driven cotransport, glucose can enter the cell with protons although the affinity for sugar becomes orders of magnitude lower. The SGLT protein transports with a 6-step model of internalization. External Na+ binds, increasing transporter’s affinity for glucose. Glucose then binds, creating a conformational change that expose Na+ and glucose to the inside of the cell. Glucose and then sodium are released and the protein returns to its original conformation. Transport is reversible depending on the concentration gradient of Na+, but it is asymmetrical and favours the internalization of glucose.146 Actions other than glucose transport SGLTs can act as uniporters to move sodium into the cell in the absence of glucose131 or glucose transport.147 In certain protein conformations, SGLT1 is also a water cotransporter with an osmotic permeability similar to AQP0130,148,149 which has therapeutic applications in oral rehydration therapy.150 These glucose-independent roles may contribute to cancer cell function, particularly in maintaining osmotic balance and cell membrane potential, both of which are altered in cancer cells.151 Positron emission tomography (PET) Both glucose metabolism and transporter expression in cancer cells are clinically useful. Positron emission tomography (PET) is an imaging technique that has become standard 24 in cancer diagnostics. PET takes advantage of the cancer cell’s metabolic requirements by visualizing tumours based on their abnormally high uptake of glucose which may be 20-30 times higher than in normal cells.40 However, this imaging is not consistently useful across a wide variety of tumours. In current practice only glucose taken up through the GLUT transport channels is detectable130, suggesting that there is potential to increase the strength of this imaging if SGLT-mediated transport is also visualized. Principle Patients are fasted overnight and given an intravenous injection of the radiolabelled glucose analogue 18F-2-deoxy-D-glucose (FDG). FDG is taken up into cells through GLUT transporters with similar kinetics as glucose and is phosphorylated by hexokinase (HK) to FDG-6-phosphate, but no further.152 This property allows its accumulation in tissue as a function of time and can be used to calculate transport and HK activity.130 Gamma rays emitted from the fluorine molecule are used to visualize the accumulation of glucose in tissues on a PET scan.153 Tissues with high glucose transport and hexokinase activity, like tumour cells, appear brighter on the scan. This technique is usually combined with other imaging techniques like computerized tomography (CT) or magnetic resonance imaging (MRI), to achieve better spatial resolution that improves the power and utility of the technique.149,154 FDG-PET can be used as a quantitative measurement using standardized uptake value (SUV) or ratio (SUR; uptake per dose). Limitations 1. Tumour biology. Not all tumours have the same level of metabolic activity and up to 30% of tumours are FDG-PET-negative.155 Even within tumours up to a quarter of 25 FDG in a tumour can be from non-tumour tissue.156 Furthermore, while PET is good at differentiating between live and dead cells, it cannot distinguish live cells with lowered metabolism (quiescent cells).155 The technique requires that FDG accumulates in tissues, so it is not useful in malignancies in tissues where dephosphorylation of FDG-6-phosphate allows glucose to diffuse out of cell.157 FDG uptake is also at least partially dependent on blood flow which is often severely compromised in tumours.158 In addition, the phase of menstrual cycle also affects level of uptake in ovaries.159 2. Signal interference. Although patients are fasted to decrease circulating insulin before a scan, insulin levels can affect FDG distribution, as can insulin-sensitizing drugs such metformin.160 Chemotherapy or its associated inflammation can result in false positive FDG uptake.161,162 Hyperglycemia can affect FDG uptake as normal glucose provides greater competition for labelled glucose to enter the tumour.163 The timing of imaging can have an effect as tissues have varying FDG uptake on delayed images which can alter background levels of uptake.164 High glucose uptake in pelvic organs, particularly the bladder, can obscure tumour metabolism in these tissues.159 3. Sensitivity and resolution. The resolution of PET, even when combined with other imaging modalities like CT, is poor below 0.8 cm3 and thus too low to detect early tumours.165 It is especially poor at finding new, previously unknown metastases.166 26 There are numerous causes of false-negatives and false-positives that can make it difficult to interpret scans.167 Use in gynecological cancers Despite these limitations, FDG uptake is increased in both ovarian cell lines168 and ovarian tumours,169 and FDG-PET reportedly has high specificity for ovarian lesions larger than 5mm.159 Tumour morphology, background activity, limited spatial resolution have been implicated where FDG-PET has performed poorly in clinical use.168 A 2009 report from Cancer Care Ontario concluded that PET adds limited value to diagnosis of pelvic masses and does not recommend its use in the diagnosis of ovarian cancer170,171, though in some cases the SUVmax of FDG-PET/CT can be useful for differentiating benign or borderline from malignant tumours.170,172 FDG-PET can help clinicians decide for or against surgery based on whether there is a localized mass or widespread disease171 and it can help reduce the need for second-look surgeries following first-line treatment.161 It is most useful in monitoring the response to treatment, residual/refractory disease, and recurrence.161,166,173,174 In combination with rising serum CA-125, FDG-PET/CT can also be sensitive and specific for early diagnosis of relapse in otherwise asymptomatic patients.175 27 RATIONALE Most tumours undergo a “glycolytic shift” as they become more aggressive. In contrast to glucose metabolism through oxidative phosphorylation, glycolysis provides the cell with rapid but inefficient ATP production. As a result, tumours consume exponentially more glucose than normal tissue. Since circulating glucose is the primary source of fuel for transformed cells, systemic metabolic control may be an important mediator of epithelial ovarian cancer (EOC). As the prevalence of diabetes continues to rise, it will be important to understand the effects of long-term comorbidities like hyperglycemia. Hypothesis and objectives We hypothesize that chronic hyperglycemia will accelerate the growth of ovarian tumours by providing an abundance of fuel needed for rapid proliferation, and that tumour metabolism may be mitigated by normalization of systemic blood glucose. The following objectives were designed to test this hypothesis: Objective 1. Determine the effects of hyperglycemia on EOC metabolism, growth and survival in vitro and in a diabetic mouse model of EOC. Objective 2. Examine the mechanisms of glucose uptake in physiologic and hyperglycemic environments. Objective 3. Assess the treatment potential of systemic glucose control to prolong disease-free survival in vivo. 28 CHAPTER 2: SYSTEMIC HYPERGLYCEMIA AND EOC PROGRESSION Introduction Epithelial ovarian cancer (EOC) is the deadliest gynecologic cancer2 and despite advances in treatment over the past thirty years, the overall survival rate remains below 40%.9 In the majority of cases, a diagnosis is not made until after the disease has spread beyond the ovary and is much more challenging to treat. Although first-line surgery and platinum-based chemotherapy can be effective, most late-stage cancers recur within 16 to 18 months.29,176 There are limited options for second-line therapy and most cancers will eventually become chemo-resistant.7 In addition to these challenges, comorbid diabetes affects 8-18% of cancer patients.177 Women with type 2 diabetes (T2DM) are at an increased risk of developing ovarian cancer178 and EOC patients with pre-existing diabetes have a much poorer overall survival rate than non-diabetic patients.179–182 T2DM is characterized by hyperglycemia and hyperinsulinemia and is often related to obesity, which carries its own risk factors including high body mass index (BMI), sex steroid metabolism, and inflammation.183,184 Despite substantial epidemiological evidence, the underlying mechanisms of the cancer-diabetes association are still poorly understood. Insulin increases the circulating, local and bioavailable growth factors including insulinlike growth factor 1, leading many to believe that hyperinsulinemia is the primary influence on cancer risk and progression in type 2 diabetics.181,185 The role of 29 hyperglycemia has been largely overlooked, despite its significant pro-tumorigenic potential.186 Like most malignancies, EOC cells metabolize considerably more glucose than their normal counterparts.187 Abnormally elevated glycolytic activity, even in aerobic conditions, is characteristic of the glucose metabolism in most cancer cells, accompanied by the conversion of pyruvate to lactate in large amounts (the Warburg Effect).41,43 Evidence suggests that the quantity of glucose required to maintain this metabolic phenotype can exceed the normal glucose content of blood.188 The rate of glucose uptake also increases with increasing extracellular glucose,123 suggesting that its supply is a rate-limiting factor for metabolism in cancerous cells.189 Increased glucose uptake has been shown to coincide with the transition from premalignant lesions to invasive cancer and has been linked with overall tumour aggressiveness.63,190 We hypothesized that the hyperglycemic conditions of diabetes can remove growth restrictions imposed by limited glucose availability and lead to more aggressive progression of epithelial ovarian cancer. In this study we investigated the in vivo and in vitro effects of hyperglycemia on epithelial ovarian cancer cell growth. 30 Materials and Methods Animals Wildtype (WT) C57bl/6 mice were purchased from Charles River Laboratories (Wilmington, MA, USA), and Akt2 null C57bl/6 mice (https://www.jax.org/strain/006966) were purchased from Jackson Laboratories (Bar Harbour, ME, USA). An Akt2 null mouse colony was established from breeder mice and animals were genotyped prior to beginning experiments. Animals were housed at the Central Animal Facility at the University of Guelph and all experiments were conducted according to Canadian Council on Animal Care guidelines. Mice were kept on a 12h light:dark cycle and had free access to food and water. For all experiments, adult mice were between 12 and 24 weeks old at the time of surgery. Mouse model of epithelial ovarian cancer Spontaneously transformed murine epithelial cells from C57Bl/6 mice (ID8) were diluted in 5µl phosphate buffered saline (PBS) and injected under the ovarian bursa of WT or Akt2 null mice. This orthotopic, syngeneic mouse model of EOC closely replicates ovarian serous adenocarcinoma in women. By 90 days post-tumour induction, mice develop large primary tumours, secondary peritoneal lesions, and significant abdominal ascites.10 In survival experiments, mice were sacrificed when they became moribund due to the accumulation of ascites fluid. 31 Type 1 Diabetes Mellitus (T1DM) Streptozotocin ([2-deoxy-2-(3-(methyl-3-nitrosoureido)-D- glucopyranose]; STZ) is a pancreatic β-cell toxin commonly used to model T1DM.191,192 Mice were treated with a standard streptozotocin dosing schedule (Animal Models of Diabetic Complications Consortium; AMDCC) two weeks prior to tumour induction surgery. Briefly, STZ (Sigma, Oakville, ON) was dissolved in 50mM sodium citrate buffer (pH 4.5) made up fresh daily. Mice received 200µl IP injections of 50mg/kg STZ or vehicle control for six consecutive days. Blood glucose was measured ten days following the last injection and mice were considered hyperglycemic if non-fasted glucose was above 300mg/dl (16.7mM). Type 2 Diabetes Mellitus (T2DM) C57BL/6 mice homozygous for a mutant Akt2 allele have poor glucose tolerance and reduced insulin sensitivity that result in hyperglycemia and hyperinsulinemia but are not obese.193,194 Obesity often accompanies T2DM and is independently associated with diabetes and cancer so this model allowed us to isolate the contributions of high glucose and high insulin. Mice were genotyped using the following primers designed by Jackson Laboratories: Akt2 wildtype reverse: TGCACAATCTGTCTTCATGCCAC; Akt2 common forward: ACCAACCCCCTTTCAGCACTTG; Akt2 mutant reverse: TACACTTCATTCTCAGTATTGTTTTGC. Products are 110bp (wildtype), 277bp (mutant), or 110bp and 277bp (heterozygote). 32 Food Consumption Food consumption at three weeks post tumour induction (PTI) was calculated by taking the initial weight of dry food and subtracting food weight after five days. This value was divided by the number of mice in the cage and the number of days in the measurement period to determine food consumed per mouse per day. Intraperitoneal glucose tolerance tests Mice were fasted for four hours prior to intraperitoneal glucose tolerance tests (IPGTT). After recording baseline blood glucose, mice were given an intraperitoneal injection of glucose (1 mg/g body weight in saline solution at a volume of 10µl/g body weight). Blood glucose measurements were taken at 15, 30, 60, and 120 minutes after glucose challenge using a handheld glucose monitor (Freestyle Lite, Abbott Laboratories). Values that exceeded the measurement range of the glucose monitor were considered 27.8mM (maximum reading). Insulin levels were measured in trunk blood from fasted animals at sacrifice using an ultra-sensitive mouse insulin ELISA kit (Crystal Chem, Downers Grove, IL). Data are presented as the average integrated area under the curve (iAUC) ± SEM where iAUC is the area under the curve relative to fasting blood glucose (FBG) at time 0 (just before glucose injection). iAUC was calculated using the trapezoidal method. The glucose:insulin ratio was used as an indication of insulin sensitivity.195 33 Tissue collection and preparation Mice were fasted for 4-6 hours prior to sacrifice by cervical dislocation. Following euthanasia, trunk blood was collected and fasting blood glucose was measured immediately using a handheld glucose monitor. The remaining blood was allowed to clot then centrifuged to obtain serum samples and stored at -80oC. Ovarian tumours were removed, weighed, and divided into sections for subsequent analysis. Sections were either fixed in 10% neutral buffered formalin (Fisher Scientific, Whitby, ON) for wax embedding and tissue sectioning, or flash frozen in liquid nitrogen and stored at -80oC for protein extraction. Secondary disease was evaluated at time of sacrifice by aspirating ascites and by visual assessment of the number of secondary lesions. Both ascites volume and secondary lesions were scored qualitatively on a relative 4-point scale with 0 indicating absence of secondary disease and 3 indicating the most widespread disease. Mice with scores of 0 and 1 were considered “low” and scores of 2 and 3 were considered “high”. Immunohistochemistry In order to confirm the effects of streptozotocin, immunohistochemical detection of insulin was performed on 5µm paraffin-embedded sections of pancreatic tissue from STZ-treated mice. Sections were deparaffinized in xylene and rehydrated in graded alcohol solutions. Endogenous peroxidase activity was quenched using 1% (vol/vol) hydrogen peroxide and antigen retrieval was performed by immersing slides in 10mM citrate buffer at 90°C for 12 minutes. Tissues were blocked in 5% (wt/vol) bovine serum 34 albumin in PBS for 10 minutes and slides were then incubated overnight with antiinsulin primary antibody (Cell Signal Technologies, Danvers, MA) diluted in 0.01M PBS (pH 7.5) containing 2% (wt/vol) BSA and 0.01% (wt/vol) sodium azide at 4°C in a humidity chamber. All subsequent incubations were performed at room temperature. Anti-rabbit biotinylated secondary antibody (Sigma, Oakville, ON) was diluted in the same buffer and incubated for 2 hours. Tissues were then washed in PBS and incubated with avidin and biotinylated horseradish peroxidase (ExtrAvidin, Sigma, Oakville, ON) for 1 hour. Antibodies were visualized using 3’ 3’-diaminobenzidine tetrahydrochloride (DAB) (Sigma, Oakville, ON) and tissue was counterstained with Carazzi’s Hematoxylin, dehydrated, and mounted with Permount (Fisher Scientific, Whitby, ON). Cell Culture Mouse-derived epithelial ovarian cancer cells (ID8; kindly donated by Drs. Paul Terranova and Kathy Roby, Kansas State University, Kansas, USA), human ovarian cancer cells (SKOV-3; ATCC, Manassas, VA, USA), and human normal ovarian surface epithelium (NOSE; generously donated by Dr. Jinsong Liu, MD Anderson Cancer Center, Houston, TX) were maintained in DMEM supplemented with 10% fetal bovine serum (FBS), 1% antibiotic/antimycotic (Gibco BRL, Burlington, ON) and 2% Lglutamine (Life Technologies, Burlington ON). All experimental treatments were performed in serum-free DMEM. 35 ID8 and SKOV3 cells are typically cultured in DMEM that contains supra-physiological amounts of glucose (25mM). We refer to these “diabetic” cells as ID8-25 and SKOV325. To test the effects of hyperglycemia, we created a parallel line of “normal” cells chronically cultured in physiological glucose (6mM) that we named ID8-6 and SKOV3-6. The -6 lines were created by passaging the -25 cells in gradually reduced concentrations of glucose over a period of three weeks. These lines were then maintained in 6mM glucose. To account for any differences caused by higher passage numbers during the glucose reduction, ID8-6 and ID8-25 cells were passage-matched in all experiments. Viability assay The MTT assay measures cellular reduction of a tetrazolium salt to a coloured formazan product in an NADH- and NADPH-dependent manner and reflects primarily glycolytic activity.196 Cells were seeded at a density of 1500 cells/well (ID8), 3000 cells/well (SKOV3), or 4000 cells/well (NOSE) in triplicate in 96 well plates and allowed to attach overnight. Cells were then serum starved for 6 hours and treated with different concentrations of glucose for 48 hours. Following treatment, cells were incubated with MTT (5mg/ml; Sigma, Oakville, ON) for one hour at 37°C and lysed with MTT lysis buffer overnight at 37°C. Absorbance was quantified in a microplate reader at 570nm. 36 Scratch wound assay To examine the motility of cells in different concentrations of glucose, ID8-6 and ID8-25 cells were grown to confluency in 24 well plates and serum starved for 6 hours. A plastic pipette tip was used to remove an area of cells down the centre of the dish. Wells were gently washed with PBS to remove detached cells before treatment. Phase contrast images were taken at three marked points along the scratch at t=0 and t=24 hours. Wound sizes were determined using ImageScope software and are presented as the fraction of the original scratch covered by cells. Glucose consumption and cell number Glucose concentration in the cell media was measured using the glucose oxidase method and reagents from Pointe Scientific (Canton MI, USA). After 24 hours of treatment, glucose concentration in the sample wells was subtracted from the glucose concentration in blank wells to determine the amount of glucose consumed. Relative cell number was approximated by the absorbance of the crystal violet nuclear stain; to account for any differences in the rate of cell proliferation, glucose consumption was divided by relative crystal violet absorbance (590nm) to determine per-cell glucose uptake. 37 Statistical Analysis Data were analyzed using GraphPad Prism statistical analysis software. Results are reported as mean ± standard error of the mean (SEM). Significance threshold was set at 0.05 and p values are listed in the figure legends. Comparisons between means were measured by two-way ANOVA followed by a Bonferroni correction, or by unpaired twotailed Student’s t-test. The relationship between tumour weight and FBG or insulin was considered significant if the slope of a linear regression was significantly different from zero. Overall survival data are plotted on a Kaplan-Meier survival curve and differences were determined by a log-rank (Mantel-Cox) test. 38 Results Mice with higher systemic glucose develop more severe disease in a model of epithelial ovarian cancer. Fasting blood glucose is normally maintained within a narrow physiological range through a highly dependent relationship with insulin. To determine the insulinindependent effects of glucose on tumour growth, we used the beta-cell toxin streptozotocin (STZ) to inhibit pancreatic insulin production and model Type 1 diabetes (T1DM). Without the production of insulin, Type 1 diabetic mice are unable to import glucose into cells and thus have significantly elevated fasting blood glucose (18.81 ± 1.93 mM vs 6.41 ± 0.27 mM in controls). As in T1DM, STZ-treated animals also have lower body weights despite consuming more food than their untreated counterparts (Figure 2C). We treated mice with STZ two weeks prior to inducing ovarian tumours by sub-bursal injection of syngeneic malignant cells (ID8). Blood glucose levels remained significantly elevated until the end of the study at 90 days post-tumour induction (PTI) (Figure 3A). Although diabetic patients are reported to have higher operative morbidity,197 we did not find that STZ-treated mice suffered any adverse events related to hyperglycemia either at surgery or during subsequent incision healing. Mice were sacrificed at 30, 60 and 90 days after tumour initiation. STZ-treated animals developed significantly larger tumours than control mice as early as 30 days PTI (Figure 3B) and tumour size was proportional to fasting blood glucose (Figure 3C). Furthermore, STZ-treated hyperglycemic mice had a greater burden of secondary 39 disease than normoglycemic mice as measured by the number of secondary tumour lesions disseminated throughout the peritoneal cavity (Figure 3E). The accumulation of abdominal ascites (Figure 3D), another indicator of secondary disease, was unchanged with STZ treatment. 40 Figure 2: Streptozotocin treatment models Type 1 diabetes A) Representative insulin staining (brown) of pancreas sections from mice four weeks after STZ treatment (two weeks post-tumour induction). Arrows in STZ image indicate pancreatic islets. 100x magnification. B) Fasting blood glucose prior to tumour-induction surgery. Bars are mean + SEM, n=8. ***p<0.001 vs mice without STZ treatment (control). C) Food consumption at 3 weeks post tumour induction (PTI). Bars are mean + SEM, n≥3. ***p<0.0001 vs mice without STZ treatment (control). D) Body weights of control and STZ treated animals. Values are mean ± SEM, n=4-16. *p<0.05. 41 Figure 3: Type 1 diabetes promotes tumour growth in proportion to blood glucose A) Fasting blood glucose in tumour-bearing mice with or without STZ-induced hyperglycemia. Values are mean ± SEM, n=4-16. *p<0.05. B) Mean tumour weights at 30, 60 and 90 days post tumour induction (PTI). Bars are mean + SEM n≥4. *p<0.05. C) Relationship between fasting blood glucose and tumour weight at 60 days PTI. Each point represents a single animal. Open circles represent control mice, closed circles represent STZ-treated mice. n≥6. Slope is significantly non-zero by linear regression (p<0.0001). D) Qualitatively assessed ascites volume and E) secondary lesions. Values are proportion of mice with relatively “high” or “low” ascites volume or number of secondary lesions. n=4. 42 Chronic glucose deficiency in mice interferes with ovarian tumour growth. Type 1 Diabetes, formerly known as juvenile-onset diabetes, is commonly diagnosed in youth and adolescents and leads to glucose-related tissue damage in patients as young as eight years old.198 In addition to the acute hyperglycemia modeled by STZ treatment two weeks prior to tumour induction, we wanted to assess the impact of type 1 diabetic tissue damage on tumour development. To investigate the effects of long-term (chronic) hyperglycemia, we treated mice with STZ 15 weeks before introducing ovarian tumours. These mice had significantly higher fasting blood glucose (10.58 ± 0.59 mM vs 5.03 ± 0.29 mM in control mice) at surgery and the hyperglycemia was maintained until mice became moribund (Figure 4D). Six mice were excluded from the study due to complications of diabetes. Surprisingly, we found that at death, hyperglycemic mice had smaller tumours (Figure 4A) than normoglycemic mice, in addition to more ascites (Figure 4B) and fewer secondary lesions (Figure 4C). Furthermore, in four of the nine STZ-treated mice that developed ascites, the abdominal fluid was pale and watery (not shown) unlike the hemorrhagic ascites typical to this mouse model. In contrast to the effects of short-term STZ treatment, there was an inverse relationship between fasting blood glucose at surgery and tumour weight at death (Figure 4E). Fasting blood glucose at death was unrelated to tumour weight (Figure 4F). Despite the development of smaller primary tumours and fewer secondary lesions in these mice, both long-term and short-term hyperglycemia led to decreased survival times compared to control mice (Figure 5). 43 Figure 4: Chronic hyperglycemia limits ovarian tumour growth Mice were treated with STZ or vehicle control 15 weeks prior to tumour induction surgery to model chronic Type 1 diabetes. A) Tumours were removed and weighed when mice became moribund. Values are mean + SEM, n≥9. ***p<0.001 vs control. Secondary disease was evaluated at time of death by B) ascites volume and C) number of secondary lesions. Values are proportion of mice with “high” or “low” scores. n≥9. D) Fasting blood glucose at time of surgery and when mice became moribund. Bars are mean + SEM, n=9 control, n=19 STZ. Different letters indicate significant (p<0.05) differences between bars. E) Relationship between fasting blood glucose at tumour induction surgery and tumour weight at death. n=7 control, n=15 STZ. Each point represents a single animal. Slope is significantly non-zero by linear regression (p<0.001). F) Relationship between fasting blood glucose and tumour weight at death. n=9 control, n=10 STZ. Slope is not significantly different from zero. 44 Percent survival 100 Acute control Acute STZ Chronic control Chronic STZ 50 0 0 20 40 60 80 100 Days PTI Figure 5: Acute and chronic hyperglycemia decrease survival in mice with EOC Kaplan-Meier survival curve of acutely (dashed lines) and chronically (solid lines) diabetic mice (Type 1 diabetes). There is no statistical difference in survival between mice in acute or chronic groups. STZ-treated mice had a significantly poorer overall survival than control (nondiabetic) mice. Log-rank (Mantel-Cox) between STZ and controls, p<0.05. n≥8. 45 The development of ovarian tumours improves impaired glucose tolerance in chronically hyperglycemic mice. In addition to elevated fasting blood glucose, diabetes is associated with glucose intolerance, or an impaired ability to clear glucose from the blood in response to a glucose challenge. To better characterize the effects of systemic hyperglycemia on EOC, we performed intraperitoneal glucose tolerance tests (IPGTT). After a period of fasting, mice were injected with 1 mg/g body weight glucose in saline. Blood glucose was then measured at 15, 30, 60 and 120 minutes after injection and the integrated area under the plot of blood glucose was calculated in relation to the baseline glucose level (integrated area under the curve, iAUC). One week after tumour induction, STZtreated mice had a significantly higher iAUC of blood glucose (Figure 6A and B) than normoglycemic mice, indicating poorer glycemic control. Interestingly, by 55 days PTI STZ-treated mice showed significant improvements in glucose tolerance that had reduced iAUC values to normal (Figure 6C). 46 Figure 6: Tumour induction improves glucose tolerance in chronically diabetic mice A) and B) Blood glucose is higher in STZ-treated mice (closed circles) than in control mice (closed circles) at all timepoints (p<0.05) following an intraperitoneal glucose challenge. Values are mean ± SEM, n≥9. C) Integrated area under the curve (iAUC) of glucose tolerance graphs in A) and B). Different letters indicate significant differences between bars (p<0.05). 47 Mice with Type 2 diabetes grow larger tumours and die earlier in a model of epithelial ovarian cancer. T2DM is a prevalent health concern that has been correlated with many cancers. 199 In contrast to T1DM which is a condition of insulin deficiency, Type 2 diabetes mellitus (T2DM) is characterized by an impaired insulin response that promotes a compensatory increase in production and leads to hyperinsulinemia. In the STZ model we demonstrated the glucose alone can affect tumour size, but others have predicted that the hyperinsulinemia, rather than hyperglycemia, drives cancer development. 181,185 To investigate the combined effects of insulin and glucose on EOC tumour growth, we used a non-obese Akt2-/- (KO) mouse model of hyperglycemia (Figure 7C) and hyperinsulinemia (Figure 8A). Sixty days after initiating ovarian tumours, KO mice had larger tumours than Akt2+/+ (WT) mice, and mice heterozygous for Akt (+/-) had an intermediate tumour weight (Figure 7A). A survival study also indicated more aggressive cancer associated with T2DM as KO mice died significantly earlier than WT mice (Figure 7B). Interestingly, growing tumours were associated with a drop in insulin concentration in the blood (Figure 8C) and a lower glucose:insulin ratio which indicated better insulin sensitivity. Higher fasting blood glucose predicts larger tumours in Akt2 KO mice. There was a significant positive correlation between the level of fasting blood glucose (FBG) at 30 days post tumour induction (PTI) and tumour weight at 90 days PTI (Figure 7C). Blood glucose levels at the time of tumour collection had no correlation to tumour weight (Figure 7D). Most surprisingly, we found that insulin levels were not associated 48 with tumour weight as many have predicted (Figure 8C). Furthermore, in contrast to the normal relationship between insulin and glucose, we found no correlation of insulin with fasting blood glucose at any experimental timepoint (Figure 8D). 49 Figure 7: High blood glucose in Type 2 diabetic mice predicts larger tumours Ovarian tumours were induced in wildtype mice (WT) and mice homozygous (Akt2-/-) or heterozygous (Akt2+/-) for Akt2. A) Mean tumour weight at 30, 60 and 90 days post tumour induction (PTI). Bars are mean + SEM, n≥5. *p<0.05. B) Percent survival of wildtype (solid line) and Akt2-/- (dashed line) tumour bearing mice. Time to death is significantly shorter in Akt2-/- mice than in WT controls. p=0.0193, n=6. C) Mean fasting blood glucose (FBG) measured at tumour induction surgery. Bars are mean + SEM, n≥62. ***p<0.001. D) Relationship between FBG at 30 days PTI and tumour weight at 90 days PTI. Slope is significantly non-zero by linear regression (p=0.0093). E) Relationship between FBG at 90 days and tumour weight at 90 days PTI. Linear regression slope not significantly different from zero (p=0.067). Each point represents a single animal. n=7 WT, n=6 Akt2-/-. 50 Figure 8: Tumours improve insulin sensitivity in Type 2 diabetic mice A) Fasting blood insulin and B) glucose:insulin ratio at 30, 60 and 90 days post tumour induction (PTI). Bars are mean + SEM, n≥6. Bars sharing the same letter are not significantly different (p<0.05). C) Relationship between tumour weight and insulin concentration at 90 days PTI and D) relationship between fasting blood glucose and insulin concentration at 90 days PTI. Slope is not significantly different from zero. Each point represents a single animal. n≥5. 51 Cells conditioned to high glucose media have altered glucose-dependent growth kinetics. In normal homeostatic conditions, fasting blood glucose in humans falls in the range of 3.9 - 5.5mM, while random (unfasted) samples are typically 4.4 - 6.6mM and under 7.8mM two hours after a meal.200 Many cancerous cell lines are cultured in media with supra-physiological concentrations of glucose, including ID8 cells which are normally grown in high glucose (25mM) DMEM. From these “diabetic” or “hyperglycemic” cells, we derived a “normoglycemic” cell line, ID8-6, by reducing glucose concentrations in the media over a period of three weeks and maintaining the cells in DMEM with 6mM glucose. The chronic culture conditions of ID8 cells significantly altered their growth kinetics. Although ID8-25 cells were more successful at closing a scratch wound than ID8-6 cells (Figure 9) they also appeared to be more sensitive to glucose deprivation (Figure 10) based on measurements of cell number. We predicted that environmental glucose was a rate limiting factor in glucose metabolism and that when more glucose was available, cells would respond by increasing glucose uptake. We found that although this was true of ID8-25 cells, ID8-6 cells did not show the same response (Figure 11). Based on our hypothesis, we predicted that cells would increase uptake in direct proportion to the total glucose available. However, we found that all cells consumed proportionally less glucose in hyperglycemic conditions (Figure 11A). One of the hallmarks of cancer cells that drives their glucose consumption is the rate of metabolism through the glycolytic and oxidative phosphorylation pathways. We 52 measured the metabolic viability of cells using the MTT assay and again found differences between cells cultured in 6mM and those cultured in 25mM glucose. While ID8-6 cell viability increased in a glucose-dependent fashion from 0mM to 25mM, ID825 cell viability plateaued at physiological glucose levels (Figure 12A). To evaluate whether these results were specific to our murine cell line, we established normal- and high- glucose variants of the human ovarian cancer cell line SKOV3 (SKOV3-6 and SKOV3-25). As in ID8 cells, SKOV3-6 cells were more metabolically active than SKOV3-25 cells in hyperglycemia (Figure 12B). 53 Figure 9: EOC cells conditioned to hyperglycemic media accelerate scratch wound closing A) Images were analyzed to determine the fraction of the scratches covered by cells after 24 hours. B) Representative images of cells after 24 hours at 10x magnification. Dashed lines indicate the width of the initial scratch. Bars are mean + SEM, n=3. **p<0.01, ***p<0.001. 54 Cells relative to normoglycemic control 2.5 ID8-6 ID8-25 2.0 1.5 1.0 b * * a a a 0.5 0.0 2mM 6mM 16.7mM 25mM Glucose in media Figure 10: Cells conditioned to hyperglycemia are sensitive to glucose deprivation Cells were cultured in different glucose concentrations for 24 hours. Crystal violet absorbance at 590 nm was used as a cell number proxy. Bars are mean + SEM relative to normoglycemic (6mM glucose) conditions. Different letters represent significant differences between ID8-25 cells (black bars) by one-way ANOVA (p<0.05). ID8-6 cells (white bars) are not significantly different across glucose concentrations. Brackets indicate differences between cell lines at the same glucose concentration. ID8-6 n=4; ID8-25 n=9 *p<0.05. 55 Figure 11: ID8-25 cells, but not ID8-6 cells, increase glucose consumption in hyperglycemia. A) Fraction of glucose consumed relative to the initial glucose concentration in the cell media. B) Total glucose consumed in mg/dL. C) Relative glucose consumption per cell. Bars are mean + SEM, n≥5. Different letters represent significant differences between bars (p<0.05). 56 Figure 12: In high glucose media, cells conditioned to hyperglycemia have lower metabolic viability than cells conditioned to physiological glucose MTT absorbance was used to determine the metabolic viability of cells. A) Viability of mouse epithelial ovarian cells acclimatized to physiological (ID8-6, white bars) or hyperglycemic (ID8-25, black bars) conditions. ID8-6, n≥8; ID8-25, n=13. B) Viability of human ovarian cancer cells acclimatized to physiological (SKOV3-6, white bars) or hyperglycemic (SKOV3-25, black bars) conditions. SKOV3-6, n=4; SKOV3-25, n=11. Values are mean + SEM. Stars indicate differences vs 6mM (normoglycemic control). Brackets indicate differences between cell lines at a single glucose concentration. *p<0.05, **p<0.01, ***p<0.001. 57 Discussion Type 2 diabetes (T2DM) is a large and growing health burden worldwide. In population studies it is consistently associated with increased incidence and mortality in multiple cancers.199 T2DM is characterized by insulin insensitivity which leads to a combination of hyperglycemia and hyperinsulinemia. In this study we showed that high systemic glucose, with or without insulin, accelerates ovarian tumour progression. Tumour growth and survival in Type 1 diabetes Insulin is a powerful mitogen and pro-tumorigenic factor and is generally considered a driving force for cancer development in diabetics.201,202 Type 1 diabetes is characterized by hyperglycemia but a deficiency in insulin which makes it a good model for isolating the effects of high blood glucose from hyperinsulinemia. Type 1 diabetes (T1DM) is an autoimmune disorder that results in the destruction of insulin-producing beta cells in the pancreas. We induced T1DM in vivo by using the beta-cell toxin streptozotocin (STZ). Two weeks after STZ treatment, we injected transformed epithelial ovarian (ID8) cells under the ovarian bursa in c57bl/6 mice in an orthotopic, syngeneic model of EOC developed in our lab. In this model, tumour development at 30 days post-tumour induction (PTI) models Stage I human disease and EOC progression at 60 and 90 days PTI are representative of Stages II and III. We found that as early as 30 days PTI, STZ-treated mice had significantly larger tumours than normoglycemic controls. By 60 days, STZ-treated mice showed more aggressive 58 secondary disease. Moreover, we found that the degree of dysglycemia directly influenced the size of the primary tumour (Figure 3C). This is in agreement with the glucose concentration-dependent increase in proliferation that has been shown in cancer cells in vitro203 and human studies that have shown that there are proportional increases in the risk of overall cancer mortality with concurrent increases in plasma glucose.204 There are currently no other studies that have used a T1DM model of diabetes to evaluate cancer progression. Based on these intriguing results, we anticipate that a short-term STZ model will be a powerful tool for investigating tumour cell metabolism. However, such an acute and short-term hyperglycemia is probably not representative of a human diabetic condition. In reality, diabetes is a chronic disease that causes significant damage to normal cells, particularly those of the endothelium. It is reasonable to expect that these changes will impact the development of a tumour, which relies on interactions with its local environment. In order to more accurately model the physiological effects of chronic hyperglycemia, we also treated mice with STZ 15 weeks prior to tumour induction. These mice had milder, but still significant, hyperglycemia (10.58 ± 0.59 mM) at tumour induction surgery than the mice with “acute” diabetes (18.81 ± 1.93 mM). We suspect that this difference reflects a partial recovery of the beta-cell population in the time between STZ treatment and tumour induction.205 Chronically elevated blood glucose interfered with the growth of ovarian tumours, which were significantly smaller than those in normoglycemic mice (Figure 4A). Because cancer cells rely on the recruitment of other cell types to populate a tumour and facilitate its growth, these unanticipated results could be a reflection of irreversible cellular damage caused by chronic 59 hyperglycemia which prevented somatic cells from interacting with cancer cells. Cancer associated fibroblasts (CAF) in particular make up a large portion of tumour mass and are significant contributors to cancer progression.206 Diabetes, however, is associated with low numbers of fibroblasts and fibroblasts with impaired motility.207 If local fibroblasts have sustained cellular damage due to hyperglycemia, it is possible that cancer cells will be unable to efficiently recruit them into tumours. Similarly, vascular damage in diabetes may inhibit the tumour’s ability to recruit new vessels which would limit tumour growth and metastasis.43,208 In addition to metabolic influences of blood glucose on tumour growth, the pathological stress of diabetes itself contributes to long-term mortality in cancer patients,209 affecting overall survival even if disease-free survival is not significantly worse.179 Adding to this evidence, we found that despite the differences in tumour size, STZ treatments at 2 and 15 weeks prior to surgery both similarly decreased survival compared to nondiabetic mice. Comorbid hyperglycemia can accelerate time to death in cancer patients, and may do so independently of primary tumour size. The discrepancy between survival and tumour size in the T1DM STZ mice may also reflect differences in secondary disease that our scoring system does not take into account, in particular immune response and the tumour-promoting effects of chronic systemic inflammation.210 The ascites in the 15week STZ animals was less hemorrhagic than that in the control animals (data not shown), which might indicate differences in composition or malignant potential which could affect tumour spread within the peritoneal cavity. 60 Tumour growth and survival in Type 2 diabetes In women, the hyperinsulinemia and hyperglycemia of T2DM is often associated with obesity. Models of diet-induced T2DM have shown increased primary tumour growth and more metastatic disease in orthotopic ovarian211 and breast201 cancers. However, obesity can independently contribute to tumour growth. To separate the effects of obesity from the influence of insulin and glucose in T2DM, we used non-obese Akt2 knockout mice on a c57bl/6 background that have an impaired ability to translocate glucose transport proteins to the cell surface in response to insulin. As in the short-term STZ-treated animals, we found that these mice grew larger primary tumours in proportion to higher fasting blood glucose and died earlier than their wildtype counterparts (Figure 7A and B). Systemic glucose Tumours have been shown to act as glucose sinks, inducing host hypoglycemia in a tumour mass-dependent fashion,212,213 particularly in the areas closest to the tumour.212,214 In some cancer patients with epithelial-derived malignancies, this property of tumours leads a condition called non-islet cell tumour-induced hypoglycemia (NICTH).215 In addition to testing whether circulating glucose can affect tumour growth, we were interested in the reciprocal effect of the tumour on systemic glucose. We showed that the growth of ovarian tumours improved glycemic control in T2DM by both normalizing the fasting insulin level and by improving insulin sensitivity (Figure 8). Intraperitoneal glucose tolerance tests in STZ-treated mice demonstrated that growing 61 tumours also improved glucose tolerance in T1DM (Figure 6), suggesting that the tumour-mediated reduction in hyperglycemia is not entirely insulin-mediated. Surprisingly, we found that many of our mice had substantial abdominal fat (data not shown), despite the fact that Akt2 KO results in an 80-90% reduction of fat depots.194 We interpret this as further evidence that tumours caused significant disturbances in global metabolic maintenance. In vitro ID8 cells are normally maintained in high glucose DMEM media (25mM glucose, ID825). In order to compare EOC cell growth in normal and hyperglycemic conditions, we created a parallel line of ID8 cells that were passaged in progressively lower concentrations of glucose and eventually maintained at a physiological level (6mM, ID86). These cells allowed us to model the effects of both glucose addition and glucose deprivation. ID8-6 and ID8-25 cells showed markedly different responses to environmental glucose. Subsequently, another group showed that breast cancer cells in glucose concentrations above 5mM have significantly higher rates of proliferation, clonogenicity, motility, upregulation/activation of pro-oncogenic signaling, and reductions in apoptosis.216 In order to measure metabolic viability, we used the MTT assay which is sensitive to NADH produced primarily through glycolysis. Although MTT activity is generally thought to reflect mitochondrial succinate activity, only a small proportion of tetrazolium reduction occurs this way.196 62 Although ID8-25 cells consumed more glucose in response to substrate availability, the MTT assay showed no increase glycolysis compared to control (Figure 12). This suggests that glycolytic metabolism may be saturated at normal glucose concentrations. However, because the glucose uptake increases, the saturation point must occur downstream of hexokinase (HK) which is necessary to keep glucose from diffusing back out of the cell. An increase in glucose uptake with no change in glycolysis could suggest less efficient metabolism. This observation could be an indication of the Crabtree Effect, in which high glucose saturates enzymes responsible for oxidative phosphorylation.121 It may also be reflective of a defect in oxidative phosphorylation in the ID8-25 cells that could necessitate an increase in glycolysis, representative of the Warburg Effect. Both the Crabtree and Warburg effects are associated with increased malignancy.217 Conversely, ID8-6 cells did not increase glucose uptake in response to substrate availability, but they did show a relative increase in glycolytic flux in 25mM glucose compared to 6mM glucose. These cells may have limited capacity to upregulate glucose transporters, or HK could potentially be saturated in these conditions and prevent further glucose uptake. However, the increase in glycolytic activity indicates that enzymes lower down the glycolytic cascade (phosphofructokinase, pyruvate kinase) are not saturated at normal glucose concentrations and are therefore able to increase energy production. Although we did not see higher glucose consumption over 24 hours, it is possible that over a longer period this increased glycolytic activity would result in increased glucose uptake. As mouse epithelial ovarian cells become more glycolytic they also become malignant and aggressive218 which would suggest that in ID8-6 cells, a high glucose environment 63 would be associated with more aggressive disease than a lower glucose environment. Glucose starvation, which we modeled in ID8-25 cells in 6mM glucose, has been shown to induce a caspase-independent cell death similar to autophagy.219 Consequently, we would expect that ID8-25 cells in 6mM would be susceptible to death. We found that there were fewer ID8-25 cells in total in conditions of glucose deprivation (Figure 10), but environmental glucose did not influence their ability to close a scratch wound (Figure 9). Neither of these assays shows what processes are responsible for changes in cell number, so it is unclear whether these data indicate differences in cell proliferation or cell death. Also, although treating ID8-25 cells in 6mM glucose represents glucose deprivation, the cells are not in hypoglycemic media and so may not be under enough metabolic stress to induce cell death. Both ovarian cancer and T2DM are insidious diseases that are often diagnosed well after pathological changes have occurred.25,220 In patients presenting with both illnesses, the combined systemic metabolic defects in diabetes and the cellular metabolic transformations in ovarian cancer cells have had a long window of interaction. The in vitro results from this study show that cancer cells developed in hyperglycemic environments are metabolically distinct from those in normoglycemic environments. These differences could indicate that certain cancer treatments will have different outcomes in diabetic compared to nondiabetic patients. Hyperglycemia is a potentially modifiable risk factor for poor overall survival in women with EOC and the results of this study support the possibility that anti-hyperglycemic drugs would be a beneficial adjuvant cancer therapy. 64 CHAPTER 3: GLUCOSE TRANSPORT IN HYPERGLYCEMIC EOC Introduction Epithelial ovarian cancer (EOC) is the fifth leading cause of cancer death among women.1,2 EOC is a challenge both to detect and to treat, resulting in a survival rate that has been virtually unchanged in the last 30 years. In large population studies, T2DM has been associated with the risk and prognosis of many different cancers.199 Previous studies in our lab have shown that ovarian tumour growth is more aggressive in diabetic environments independent of insulin levels (Chapter 2). Hyperglycemia also increases the ability of EOC cells to take up glucose, but the expression, regulation and uptake kinetics of glucose transporters in these conditions are unknown. Glucose primarily enters cells by facilitated diffusion through glucose transporters (GLUTs). The activation of GLUT genes is one of the earliest events in oncogenesis 221 and high GLUT1 expression is often associated with poor prognosis and more aggressive disease.222 Almost all invasive epithelial carcinomas are positive for GLUT1, independent of stage, grade, or histological subtype.126,127 As a passive transporter, GLUT activity is dependent on the direction and magnitude of the glucose concentration gradient across the cell membrane. Glucose can also enter the cell against its concentration gradient through a class of sodium-dependent secondary active symporters (SGLTs). The most well studied isoforms, SGLT1 and SGLT2, are normally expressed in the small intestine and kidney proximal tubule respectively. Few papers 65 have looked at SGLT expression in malignancies and only one published study has demonstrated functional glucose uptake through the SGLTs in tumours.223 One of the hallmark characteristics of cancer is a glycolytic phenotype that necessitates high glucose uptake to produce ATP and the biosynthetic precursors required for proliferation. This elevated glucose uptake has been exploited in clinical imaging. Using positron emission tomography (PET), the accumulation of the glucose analogue 18fluoro-deoxy-glucose (FDG) can differentiate tumour tissue from normal tissue. In EOC, FGD-PET can be useful in monitoring response to treatment but it has poor utility as a diagnostic tool. FDG is efficiently transported through GLUT transporters, but it is a poor substrate for SGLTs.224 FDG is the only oncolytic tracer currently in clinical use. If sodium-glucose transport is functionally important in glucose uptake into ovarian tumour tissue, the use of an SGLT-transportable glucose analogue could substantially increase the power of imaging. Glucose transport through SGLTs has the potential to release cancer cells from the constraints of extracellular glucose concentration and thus provide a level of selfsufficiency for energy production. The goal of this study was to characterize the expression and relative contributions of the GLUT and SGLT transporter families in the glucose uptake and tumour growth of epithelial ovarian cancer, in both normoglycemic and hyperglycemic environments. 66 Materials and Methods Reverse transcription PCR Reverse transcription (RT)-PCR was used to determine the mRNA expression of glucose transporters SGLT1-3 and GLUT1-4 in ID8-25 cells. Total RNA was extracted from cell lysates of serum-starved ID8-25 cells using the Qiagen RNA Extraction Kit (RNeasy Mini kit, Qiagen, Mississauga, ON) and stored at -80°C prior to use. RNA samples were reverse transcribed to cDNA using in 50µl reactions with 1µl Oligo(dT) 12-18 primer, 1µl 10mM dNTP, 10µl of each RNA sample (65ºC for 5 minutes in an MJ Research PTC-200 Thermo Cycler); four parts 5X First-Strand buffer, 2 parts 0.1M DTT (supplied with SuperScript II Reverse Transcriptase kit, Life Technologies Inc., Burlington, ON) and one part RNasin in 7µl (42ºC for 2 minutes); 1µl of SuperScript II Reverse Transcriptase. The reverse transcription reaction was then carried out at 42ºC for 50 minutes. Inactivation was induced by incubating the tubes at 70ºC for 15 minutes. Final cDNA products were stored at -20ºC. Primer sequences were determined by Mus musculus gene sequences using NCBI Primer-Blast. These primers, generated from Laboratory Services Molecular Biology Lab (Guelph, ON), were stored at -20ºC. Sequences are provided in Appendix IV. The cDNA was amplified in 50 µl reactions containing one part 10mM dNTP mix, five parts 10x buffer and one part 1x Taq (New England BioLabs Ltd., Pickering, ON), forward and reverse primers, 1µl of cDNA and nuclease-free water. The PCR reaction 95ºC for 30 seconds; appropriate annealing temperature (previously determined) for 30 67 seconds; 72ºC for 1 minute; for 35 cycles. PCR products were then incubated at 72ºC for 10 minutes and stored at 4ºC until they were separated on a 1% agarose gel and visualized with ethidium bromide using the FluorChem8800 gel documentation imaging system. Immunohistochemistry In order to determine the protein expression of SGLT transporters in human EOC, immunohistochemical detection of SGLT1 and SGLT2 was performed on a microarray that included normal ovarian tissue, serous adenocarcinomas and metastatic tissue cores (OV208 microarray; US Biomax, Rockville, MD). Sections were deparaffinized in xylene and rehydrated in graded alcohol solutions. Endogenous peroxidase activity was quenched using 1% (vol/vol) hydrogen peroxide and antigen retrieval was performed by immersing slides in 10mM citrate buffer at 90°C for 12 minutes. Tissues were blocked in 5% (wt/vol) bovine serum albumin in PBS for 10 minutes and slides were then incubated overnight with anti-SGLT1 or -SGLT2 primary antibody (Abcam, Cambridge Science Park, Cambridge, MA) diluted in 0.01M PBS (pH 7.5) containing 2% (wt/vol) BSA and 0.01% (wt/vol) sodium azide at 4°C in a humidity chamber. All subsequent incubations were performed at room temperature. Anti-rabbit biotinylated secondary antibody (Sigma, Oakville, ON) was diluted in the same buffer and incubated for 2 hours. Tissues were then washed in PBS and incubated with avidin and biotinylated horseradish peroxidase (ExtrAvidin, Sigma, Oakville, ON) for 1 hour. Antibodies were visualized using 3’ 3’-diaminobenzidine tetrahydrochloride (DAB) (Sigma, Oakville, ON), tissue was counterstained with Carazzi’s Hematoxylin then dehydrated and mounted 68 with Permount (Fisher Scientific, Whitby, ON). Tissue cores were considered to have no SGLT protein expression if total positive pixel counts were less than 2%. Immunohistochemistry of SGLT2 (Abcam, Cambridge Science Park, Cambridge, MA) and GLUT1 (Santa Cruz Biotechnologies, Santa Cruz, CA) in mouse tissue sections was performed identically. Cell Culture Mouse-derived epithelial ovarian cancer cells (ID8; kindly donated by Drs. Paul Terranova and Kathy Roby, Kansas State University, Kansas, USA), human ovarian cancer cells (SKOV-3; ATCC, Manassas, VA, USA), and human normal ovarian surface epithelium (NOSE; generously donated by Dr. Jinsong Liu, MD Anderson Cancer Center, Houston, TX) were maintained in DMEM supplemented with 10% fetal bovine serum (FBS), 1% antibiotic/antimycotic (Gibco BRL, Burlington, ON) and 2% Lglutamine (Life Technologies, Burlington ON). All experimental treatments were performed in serum-free DMEM. ID8 and SKOV3 cells are typically cultured in DMEM that contains supra-physiological amounts of glucose (25mM). These “diabetic” cells were referred to as ID8-25 and SKOV3-25. To test the effects of hyperglycemia, we created a parallel line of “normal” cells chronically cultured in physiological glucose (6mM) that we named ID8-6 and SKOV3-6. The -6 lines were created by passaging the -25 cells in reducing concentrations of glucose over a period of three weeks. These lines were then maintained in 6mM glucose. To account for any differences caused by higher passage 69 numbers during the glucose reduction, ID8-6 and ID8-25 cells were passage-matched in all experiments. Drugs Phlorizin (PZ; Sigma, Oakville, ON) competitively inhibits glucose transport through sodium/glucose cotransporters (SGLTs). Cytochalasin B (CB; Sigma, Oakville, ON) and phloretin (PT; Santa Cruz Biotechnologies, Santa Cruz, CA) inhibit glucose transport through the passive glucose transporters (GLUTs). Cytochalasin B is a more potent GLUT inhibitor than phloretin, however it has two binding sites, one of which affects cell cytoskeleton by interfering with actin assembly. Thus, CB was not appropriate for motility studies and was replaced by PT.225 Viability assay The WST-1 assay measures extracellular reduction of a tetrazolium salt to a coloured formazan product dependent on the net rate of NADH reduction. NADH produced in the mitochondrial TCA cycle is the primary reductant for extracellular WST-1 reduction via transmembrane electron transport.226 ID8 cells were seeded at a density of 1500 cells/well in triplicate in 96 well plates and allowed to attach overnight. Cells were then serum starved for 6 hours and treated for 48 hours in serum-free conditions. Following treatment, cells were incubated with treatment media containing water-soluble tetrazolium salt (WST)-1 reagent (Roche Applied Science, Laval, QC) at a 1:10 dilution 70 at 37ºC for one hour. Absorbance was quantified 450nm with 630nm correction on a microplate reader. Scratch wound assay To examine the motility of cells in different concentrations of glucose, ID8-6 and ID8-25 cells were grown to confluency in 24 well plates and serum starved for 6 hours. A plastic pipette tip was used to remove an area of cells down the centre of the dish. Wells were gently washed with PBS to remove detached cells before treatment. Phase contrast images were taken at three marked points along the scratch at t=0 and t=24 hours. Wound sizes were determined using ImageScope software and are presented as the fraction of the original scratch covered by cells. Glucose consumption and cell number Glucose concentration in the cell media was measured using the glucose oxidase method and reagents from Pointe Scientific (Canton MI, USA). After 24 hours of treatment, glucose concentration in the sample wells was subtracted from the glucose concentration in blank wells to determine the amount of glucose consumed. Relative cell number was approximated by the absorbance of the crystal violet nuclear stain. To account for any differences in the rate of cell proliferation, glucose consumption was divided by relative crystal violet absorbance (590nm) to determine a per-cell uptake comparison. 71 Invasion Assay (Boyden chamber) In vitro cell invasive/migratory capacity was measured using a Boyden chamber assay (Biocoat Matrigel invasion chambers; BD Biosciences, Franklin Lakes, NJ). ID8-6 and ID8-25 cells were grown on a Matrigel-coated upper membrane (10,000 cells per well) and treated with 100µM phlorizin or DMSO vehicle control, in serum-free DMEM containing 6mM or 25mM glucose. The lower chamber contained drug-free media with 10% FBS to act as a chemoattractant. Cells were incubated at 37°C and allowed to migrate for 20 hours. Cells were removed from the upper chamber using cotton swabs. 500µl of 5% glutaraldehyde PBS was added to the lower chamber and incubated for 10 minutes at room temperature. Migrated cells were stained by adding 500µl 0.5% toluidine blue staining solution in the lower chamber and incubating for 15 minutes. Manual counting of cells in three fields of view per membrane was used to quantify number of invaded cells. shRNA SGLT2 knockdown ID8-6 and ID8-25 cells were cultured in 12-well plates in complete medium (6mM glucose or 25mM glucose DMEM containing FBS). At 40% confluence, cells were treated with 5µg/ml Polybrene (Santa Cruz Biotechnologies, Santa Cruz, CA) and infected with either: a pool of three shRNA constructs, each encoding SGLT2-specific 19-25 nt (plus hairpin loop) shRNA; or with control shRNA particles (scrambled sequence) (Santa Cruz Biotechnologies, Santa Cruz, CA) overnight. Polybrene media was then replaced with normal media and incubated overnight. After 48 hours, cells 72 were selected with puromycin dihydrochloride (Santa Cruz Biotechnologies, Santa Cruz, CA) for 12 weeks. Clonal knockdown colonies were grown from single puromycinresistant cells. Western blot analysis was used to evaluate SGLT2 protein knockdown. Animals Wildtype c57bl/6 mice were purchased from Charles River Laboratories (Wilmington, MA, USA), c57bl/6 Akt2 null mice (https://www.jax.org/strain/006966) were purchased from Jackson Laboratories (Bar Harbour, ME, USA). An Akt2 null mouse colony was established from breeder mice and animals were genotyped prior to beginning experiments. Animals were housed at the Central Animal Facility at the University of Guelph and all experiments were conducted according to Canadian Council on Animal Care guidelines. Mice were kept on a 12h light:dark cycle and had free access to food and water. For all experiments, adult mice were between 12 and 24 weeks old at time of surgery. Mouse model of epithelial ovarian cancer Spontaneously transformed murine epithelial cells from C57Bl/6 mice (ID8) were diluted in 5µl phosphate buffered saline (PBS) and injected under the ovarian bursa of WT or Akt2 null mice. This orthotopic, syngeneic mouse model of EOC closely replicates ovarian serous adenocarcinoma in women. By 90 days post-tumour induction, mice develop large primary tumours, secondary peritoneal lesions, and significant abdominal ascites.10 In survival experiments, mice were sacrificed when they became moribund due to the accumulation of ascites fluid. 73 Type 2 Diabetes Mellitus (T2DM) C57BL/6 mice homozygous for a mutant Akt2 allele are non-obese animals with poor glucose tolerance and reduced insulin sensitivity that result in hyperglycemia and hyperinsulinemia.193,194 Mice were genotyped using the following primers designed by Jackson Laboratories: Akt2 wildtype reverse: TGCACAATCTGTCTTCATGCCAC; Akt2 common forward: ACCAACCCCCTTTCAGCACTTG; Akt2 mutant reverse: TACACTTCATTCTCAGTATTGTTTTGC. Products are 110bp (wildtype), 277bp (mutant), or 110bp and 277bp (heterozygote). Intraperitoneal glucose tolerance tests Mice were fasted for four hours prior to intraperitoneal glucose tolerance tests (IPGTT). After recording baseline blood glucose, mice were given an intraperitoneal injection of glucose (1 mg/g body weight in saline solution at a volume of 10µl/g body weight). Blood glucose measurements were taken at 15, 30, 60, and 120 minutes after glucose challenge using a handheld glucose monitor (Freestyle Lite, Abbott Laboratories, Abbott Park, IL). Values that exceeded the measurement range of the glucose monitor were considered 27.8mM (maximum reading). Plasma for insulin quantification was collected in heparinized capillary tubes during the IPGTT or from trunk blood from fasted animals at sacrifice using an ultra-sensitive mouse insulin ELISA kit (Crystal Chem, Downers Grove, IL). Data are presented as the average integrated area under the curve (iAUC) ± SEM where iAUC is the area under the curve relative to fasting blood glucose (FBG) at time 0 (immediately before glucose 74 injection). iAUC was calculated using the trapezoidal method. The glucose:insulin ratio was used as an indication of insulin sensitivity.195 Tissue collection and preparation Mice were fasted for 6 hours prior to sacrifice by cervical dislocation. Following euthanasia, trunk blood was collected and fasting blood glucose was measured immediately using a handheld glucometer. The remaining blood was allowed to clot then centrifuged to obtain serum samples and stored at -80oC. Ovarian tumours were removed, weighed, and divided into sections for subsequent analysis. Sections were either fixed in 10% neutral buffered formalin (Fisher Scientific, Whitby, ON) for wax embedding and tissue sectioning or flash frozen in liquid nitrogen and stored at -80oC for protein extraction. Secondary disease was evaluated at time of sacrifice by ascites volume and number of secondary lesions. Mice were scored on a 4-point scale with 0 indicating absence of secondary disease. Mice with scores of 0 and 1 were considered “low” and scores of 2 and 3 were considered “high”. Radioisotope uptake Alpha-methyl-glucopyranoside (AMG) and 2-Deoxy-D-glucose (2-DG) are glucose analogues that are preferentially transported by SGLTs and GLUTs respectively.224 Transporter-specific glucose uptake was determined using [3H] 2-DG and [14C] AMG (Moravek Biochemicals, Brea, CA). Mice were given a single tail vein injection of 25µCi 75 of [3H]2-DG and 5µCi of [14C]AMG 1.5 hours before sacrifice. Volumes of blood and ascites and sections of tumour, skeletal muscle, liver and ovary were collected. The samples were incubated at 55°C in ScintiGest solubilisation fluid (Fisher Scientific, Whitby, ON) until the tissue dissolved. Thirty percent H2O2 was added to decolorize samples. An aliquot of scintillation cocktail (CytoScint; MP Biomedicals, Santa Ana, CA) was added to each sample and the total radioactive disintegrations per minute (dpm) were determined using a Beckman LS 6500 liquid scintillation counter (Beckman Coulter, Fullerton, CA). Western Blots Protein was collected from tumour tissue or SGLT2 knockdown cells using RIPA lysis buffer and quantified using the DC Protein Quantification kit (Bio-Rad, Mississauga, ON). Total protein lysates (20-40 µg) were used for immunoblot analysis. Lysates were separated by SDS-PAGE on 10% gels. Proteins were electro-transferred onto nitrocellulose membranes (Amersham, Piscataway, NJ) then blocked for 1 hour at room temperature in 5% (wt/vol) skim milk in TBS-T (TBS with 1%(vol/vol) Tween 20). Primary antibodies (SGLT1 (1:500, Abcam, Cambridge Science Park, Cambridge, MA), SGLT2 (1:500, Abcam, Cambridge Science Park, Cambridge, MA), GLUT1 (1:200, Santa Cruz) and β-actin (1:8000, Cell Signal Technologies, Danvers, MA) were diluted in TBS-T skim milk and incubated overnight at 4°C on a rocking platform. After washing with TBS-T blots were incubated with peroxidase-conjugated anti-rabbit secondary antibody (1:1000 dilution; Cell Signal Technologies, Danvers, MA) or anti-mouse IgG (1:1000 dilution, Cell Signal Technologies, Danvers, MA) for one hour at room 76 temperature on a rocking platform. Reactive protein was detected with ECL chemiluminescence (Perkin Elmer, Waltham, MA). Membranes were imaged on the BioRad ChemiDoc XRS+ and densitometry was performed using Bio-Rad Image Lab 5.1. Protein values were expressed as a ratio with β-actin. Statistical Analysis In vivo data were analyzed using Statistix 7 analytical software. Results are reported as mean ± standard error of the mean (SEM). Significance threshold was set at 0.05 and p values are listed in the figure legends. Tumour weight at survival was analyzed using a one-way ANOVA followed by Tukey’s post-hoc. The significance of metastastic secondary disease was measured using a Wilcox Rank Sum test for metastasis by knockdown (ID8-6 and genotype were not significant in this model). Differences in ascites volume by group were significant (chi squared approximation p=0.0025) but there were no differences in pairwise comparisons. Differences in ascites volume were therefore determined using a Kruskal-Wallis one-way nonparametric ANOVA by knockdown. Overall survival data are plotted on a Kaplan-Meier survival curve and differences were determined by a proportional hazards regression. All other data were analyzed using GraphPad Prism statistical analysis software. Comparisons between means were measured by two-way ANOVA followed by a Bonferroni correction, or by unpaired two-tailed Student’s t-test. 77 Results Both passive and active glucose transporters are expressed in EOC Using reverse transcription PCR we showed the expression of both passive (GLUT1, GLUT3) and active (SGLT2) glucose transporters in ID8 murine epithelial ovarian cancer (EOC) cells (Figure 13). This is the first demonstration that sodium-glucose transporters are expressed in ovarian cancer. To further characterize the expression of SGLT transporters, we immunostained human tissue microarrays containing tissue samples from serous ovarian adenocarcinomas, metastases, and normal ovarian tissue (Figure 14). Using Imagescope software to quantify protein expression, we found that both SGLT1 and SGLT2 were present in normal ovaries at low levels (3.1 ± 0.2 % and 23.8 ± 2.8 % respectively). In tumours, SGLT1 was only expressed in about a third of samples, in which staining density was only about 16%. SGLT2, however, was expressed in all samples with high density (67.5 ± 2.9 % positive pixels). Both isoforms were overexpressed in tumours, though expression in metastases was no different than in normal tissue. Expression did not differ by stage, but low grade tumours were associated with higher SGLT expression. Staining was diffuse throughout the cytoplasm and there was no clearly defined expression at the cell membrane. Positive staining for SGLT1 is shown in the supplementary figures (Figure 41, Appendix I). 78 Figure 13: GLUT and SGLT transporters are expressed in ID8 cells Reverse transcription PCR for glucose transporters in mouse epithelial ovarian cancer cells (ID8-25). A) Secondary active sodium glucose transporter 2 (SGLT-2) expressed. Positive controls: mouse kidney. B) Facilitative glucose transporters (GLUT) GLUT-1 and GLUT-3 are expressed. Positive controls: GLUT-2, mouse liver and GLUT-4, mouse skeletal muscle. NTC, no-template control. 79 Figure 14: SGLT2 is overexpressed in human serous ovarian cancer Immunostaining for SGLT1 and SGLT2 on tissue microarrays of human serous epithelial ovarian cancers. Staining was quantified using Imagescope software to determine the number of positive and negative pixels within a tissue section. A) Representative tissue cores of normal and malignant (FIGO Stage 3c, Grade 3) ovarian 80 tissue. Pixels intensity was categorized as negative, weak positive, positive, or strong positive. Normal tissue (n=26), carcinomas (n=48), metastases (n=18). B) Staining by tissue type C) Staining of serous adenocarcinomas by FIGO stage D) Staining of serous adenocarcinomas by histological grade *p<0.05, **p<0.01, ***p<0.001 between total positive pixel counts. Table 3: SGLT protein expression in human ovarian cancer SGLT1 Tissue expression SGLT2 Positive pixel density Mean ± SEM (%) N Percent Normal 18 100.0 3.1 ± Tumours 15 31.3 15.8 Grade 2 9 56.3 Grade 3 6 6 Tissue expression Positive pixel density Mean ± SEM (%) N Percent 0.2 16 100.0 23.8 ± 3.8 ± 4.0 48 100.0 67.5 ± 2.9 20.9 ± 5.9 16 100.0 78.4 ± 3.6 18.8 8.3 ± 2.4 32 100.0 62.1 ± 3.7 15 100.0 68.4 ± 3.9 28.6 19.4 ± 8.4 6 100.0 48.2 ± 11.9 Stage 1 Stage 2 Stage 3 8 33.3 13.1 ± 4.3 20 100.0 69.0 ± 4.5 Metastases 7 38.9 3.7 ± 0.6 18 100.0 37.2 ± 5.3 81 GLUT transporters are active in physiological glucose concentrations (6mM) and SGLT transporters are active in hyperglycemic conditions (25mM) In order to evaluate the relative contributions of GLUT and SGLT transporters, we used class-specific glucose transport inhibitors. Phlorizin (PZ) selectively inhibits glucose transport through the SGLTs, while phloretin (PT) and cytochalasin B (CB) inhibitor only GLUT-mediated glucose transport. Based on the mRNA expression in ID8 cells, we can infer that in ID8 cells, PZ is acting on SGLT2 and PT/CB are acting on GLUT1 and GLUT3. ID8 cells were differentiated into two subtypes through serial passaging. ID8-6 cells are conditioned to normal physiological concentrations of glucose (6mM) and ID8-25 cells are conditioned to supra-physiological glucose (25mM). In both cell lines, PZ inhibited glucose consumption in high-glucose media compared to cells treated with a vehicle control (Figures 15 and 16). PZ had no significant inhibitory effect on glucose uptake in normal glucose concentrations. PT, on the other hand, significantly reduced glucose uptake in 6mM but not 25mM glucose. In ID8-25 cells the combination treatment with PZ and CB did not have additive inhibitory effects on glucose uptake in either normal or high glucose (Figure 16). Regardless of transporter inhibition, these cells consumed more glucose in high-glucose media than in physiological glucose, even though glucose was plentiful. Even in 6mM glucose media, the total consumption represented less than a third of the total glucose available. 82 Figure 15: SGLTs affect glucose transport in hyperglycemia in cells conditioned to normal physiological glucose concentrations (ID8-6) Glucose consumption by ID8-6 cells in normoglycemic and hyperglycemic culture conditions. Cells were treated with 50µM PT or 200µM PZ in 0.01% DMSO. A) Total glucose consumed in mg/dL. B) Fraction of glucose consumed relative to the initial glucose concentration. C) Relative glucose consumption per cell. Bars are mean + SEM, n≥3. Bars sharing the same letter are not significantly different (p<0.05). 83 Figure 16: SGLTs affect glucose transport in hyperglycemia in cells conditioned to high glucose concentrations (ID8-25) A) Total glucose consumed in mg/dL. B) Fraction of glucose consumed relative to the initial glucose concentration. C) Relative glucose consumption per cell. Drugs were dissolved in 0.01% DMSO. Combination treatment was 50µM PZ and 0.5µM CB. Bars are mean + SEM, n≥3. Different letters indicate significant differences between bars (p<0.05) 84 Glucose concentration does not alter the effect of glucose inhibitors on viability. The metabolic viability of cells was measured using the WST-1 assay (Figure 17). Phlorizin (PZ, SGLT inhibitor) had no effect on cell viability, while phloretin (PT, GLUT inhibitor) potently decreased viability in a concentration-dependent manner in both ID86 and ID8-25 cells. The combination of PZ and CB on ID8-25 cells had no effect on cell viability. 85 Figure 17: SGLT inhibition does not affect cell metabolic viability A) and B) Viability of mouse epithelial ovarian cells acclimatized to physiological conditions. ID8-6, n≥3; C)-E) Viability of mouse epithelial ovarian cells acclimatized to hyperglycemic conditions. Combination treatment (PZ+CB) is 50uM PZ and 0.5uM CB. ID8-25, n=3. *p<0.05, **p<0.01, ***p<0.001. Bars are mean + SEM. Different letters, or brackets with stars, indicate significant differences between bars (p<0.05) 86 Inhibition of the SGLTs does not affect wound healing in hyperglycemia In “non-diabetic” ID8-6 cells, the GLUT inhibitor phloretin (PT) inhibited wound healing a scratch assay in both normal- and high-glucose media (Figure 18). The SGLT inhibitor phlorizin (PZ), however, only inhibited wound healing in 6mM glucose. The combination of phlorizin and phloretin did not have an additive effect on the fraction of the scratch wound that was filled in over 24 hours. 87 Figure 18: Phlorizin and phloretin inhibit scratch wound healing in ID8-6 cells Images were analyzed to determine the fraction of the scratches covered by cells after 24 hours. Representative images of cells after 24 hours at 4x magnification. Dashed lines indicate the width of the initial scratch. A) ID8-6 cells in 6mM glucose. B) ID8-6 cells in 25mM glucose. Combo is 100µM PZ + 100µM PT. Bars are mean + SEM, n=3. **p<0.01, ***p<0.001. 88 Phlorizin increases the invasive capacity of ID8-6 but not ID8-25 cells Cells conditioned to high glucose (ID8-25) were more invasive than ID8-6 cells regardless of available glucose (Figure 19A, a vs b). However, SGLT channel inhibition with PZ equalized the number of migrated cells across all experimental groups by increasing ID8-6 cell invasiveness and decreasing (6mM) or maintaining (25mM) ID8-25 invasiveness (Figure 19A, black bars). Relative to cells treated with DMSO vehicle control, ID8-6 cells treated with PZ were significantly more invasive than ID8-25 cells (Figure 19B). 89 Figure 19: SGLT glucose transporters limit cell invasion in ID8-6 cells Cells were cultured in the upper chamber of trans-wells coated with Matrigel and allowed to migrate towards the lower chamber using FBS as a chemoattractant. Purple staining indicates cells that have migrated through the Matrigel membrane. Bars are mean + SEM. Different letters indicate significant differences within DMSO control treatments (white bars) p<0.05. Phlorizin treatments (black bars) were not significantly 90 different from one another. (p<0.05). Stars indicate significant differences between DMSO and PZ treatments within each cell line/glucose condition. *p<0.05, ***p<0.001. A) Number of cells migrated through Matrigel, with representative images. B) Migration of PZ-treated cells relative to DMSO control. Knockdown of SGLT2 opposes contact-dependent growth inhibition The SGLT2, the sodium-glucose transporter isoform present in our cells, was stably knocked down using shRNA (Figure 20A). Cells with lowered SGLT2 expression had an altered pattern of growth in culture where individual cells appeared to migrate away from a group of cells, rather than multiplying to expand an existing group of cells (Figure 20B). KD cells were also resistant to contact-dependent growth inhibition and continued to grow on top of a fully confluent monolayer of cells, forming three-dimensional foci with cords of stacked cells projecting outward (Figure 20C). 91 Figure 20: Knockdown of SGLT2 in ID8 cells changes proliferative behaviour in culture SGLT2 expression in ID8-6 and ID8-25 cells was knocked down using shRNA packaged in lentiviral particles. A) Representative Western blots showing protein expression of SGLT2 in cells treated with empty vectors (left) and shRNA constructs (KD, right). Protein knockdown was evaluated by densitometry. ID8-6 cells had an apparently complete SGLT2 knockdown by this technique and ID8-25 cells protein expression was reduced by 65%. B) Representative images of cell migration in cultures of KD clones at 4x magnification. C) Representative images of cell foci formed at high confluency by KD clones. 92 GLUT1 protein expression appears greater in diabetic mice than in WT mice In both tumours with and without SGLT2 expression (ID8-25), GLUT1 expression appears qualitatively greater in Akt2 KO mice than in normoglycemic WT mice (Figure 21A and B). In mice whose ovaries were injected with SGLT2 KD cells, SGLT2 expression did not differ by genotype, but in WT mice appeared considerably higher than GLUT1 expression (Figure 21C). 93 Figure 21: GLUT1 protein expression is higher the tumours of diabetic mice than in those of WT mice Representative images of tumour tissue stained by immunohistochemistry. A) GLUT1 expression in from Akt2 KO mice appears higher than in WT mice. B) In mice whose tumours were initiated with ID8-25 SGLT2 knockdown cells, GLUT1 expression appears higher in Akt2 KO than in WT mice. C) SGLT2 expression in mice with SGLT2 knockdown cells does not appear to differ between genotypes. (Not quantified). 94 Glucose is transported into orthotopic ovarian tumours by both GLUT and SGLT. In order to determine the functional expression of GLUT and SGLT transporters in murine EOC tumours, we injected radioisotope-tagged glucose analogues into the tail veins of wildtype (WT) and Akt2 -/- (KO) mice four months PTI. Alpha-methylglucopyranoside (14C-AMG) is specifically transported through the SGLT transporter family and deoxyglucose (3H-DG) is specifically transported through the GLUT transporter family. Both GLUT and SGLT transporter families contribute to glucose uptake in tumours in approximately equal amounts (Figure 22). All tissues took up the same total glucose per gram (data not shown). Total glucose uptake per gram was unchanged in SGLT2 KD cells and a significant increase in the amount of GLUTmediated transport completely compensated for the loss of SGLT2 expression (Figure 23). 95 Figure 22: Both GLUT and SGLT transporters are responsible for functional glucose uptake into tumours Bars show the relative uptake of each isotope. Stars indicate significant differences in the fractions of 3H-DG (transported by GLUTs) and 14C-AMG (transported by SGLTs). Different letters indicate differences in uptake between tissues. (p<0.05). N=4. 96 Figure 23: SGLT2 KD impairs glucose uptake through active transport, but total glucose uptake is maintained through compensation by GLUTs A) A 3H-DG : 14C-AMG ratio above 1.0 indicates that there was more GLUT-mediated glucose transport than SGLT-mediated transport. There were no significant differences between control WT and Akt2 KO ratios in SGLT2 control mice. B) Total glucose uptake per gram of tissue (sum of disintegrations per minute of 3H-DG + 14C-AMG divided by tissue weight). Control n=4; KD n=1. Bars represent mean + SEM (control) or values from the single animal with an SGLT2 KD tumour. 97 45 days after tumour induction, GLUT1 protein expression is upregulated in diabetic mice with SGLT2 KD tumours. At 45 days PTI we found no significant differences in the weights of tumours in any experimental condition (Figure 24A). Western blot analysis showed that in Akt2 KO mice, GLUT1 expression was upregulated beyond accurate quantification. Tumours from mice that were injected with SGLT2 KD ID8 cells had the same SGLT2 protein expression as those injected with control ID8 cells (Figure 24B and C). 98 Figure 24: Expression of GLUT1 is highly upregulated in tumours with reduced SGLT2 expression at 45 days PTI Transformed mouse ovarian epithelial cells (ID8-25) were injected under the ovarian bursa of wildtype (WT) and Akt2-/- (KO) mice. Injected cells had normal (control) or knocked down (SGLT2 KD) expression of SGLT2. A) Mean tumour weight at 45 days 99 post tumour induction (PTI). Bars are mean + SEM n=4. Differences in tumour weights were non-significant. p=0.065 between control and SGLT2 KD in WT mice. B) Protein expression of glucose transporters in 45-day tumours. Each lane represents protein from an individual animal. C) Densitometry of Western blots relative to β-actin loading control. Bars are mean + SEM n≥3. ***p<0.001. SGLT2 KD increases tumour weight and decreases overall survival SGLT knockdown significantly increased tumour weight at the time of death in a cell line-dependent manner (Figure 25). Tumours initiated with ID8-6 cells were associated with decreased tumour weight after controlling for the variation due to the SGLT2 KD. In a univariate analysis, however, cell type (ID8-6 / ID8-25) had no effect. Knockdown of SGLT2 in ID8-25 cells increased tumour weight in WT mice, while SGLT2 KD in ID8-6 cells caused significantly larger tumours in the diabetic Akt2 KO mice. Mice whose tumours had knocked-down SGLT2 expression had a relative risk of dying of nearly 25 times. When considered in a multivariate model, after controlling for variation in ID8-6 and WT the relative risk of dying was more than 57 times higher in mice with SGLT2-deficient tumours (Figure 26). ID8-6 cells or a WT genotype also increased the relative risk of death by 5 and 3.5 times respectively, although their effects were non-significant if SGLT2 KD mice were removed from the model. 100 Figure 25: SGLT2 knockdown leads to significantly larger primary tumours at death Tumours were removed and weighed when mice became moribund. Representative images of A) wildtype mice and B) Akt2-/- mice and tumours. (ID8-25 cells, SGLT2 control and SGLT2 KD.) Bars represent mean + SEM. Different letters represent significant differences between all groups (p<0.05). n=5 per group. SGLT2 KD (p<0.0001) increases tumour weight. ID8-6 decreases (p=0.0364) tumour weight after controlling for the variation due to KD, but without KD its effects are not significant. 101 Control, WT SGLT2 KD, WT Percent survival 100 Control, KO SGLT2 KD, KO 50 0 0 50 100 150 Days PTI Figure 26: SGLT2 KD in tumours significantly decreases overall survival Solid lines indicate tumours developed from ID8-25 cells, dashed lines indicate those from ID8-6 cells. The experiment was terminated at 126 days and mice that were sacrificed at 126 days were considered to have lived. N=5 per group. Survival of ID8-25 control mice overlaps survival of ID8-6 control mice. Table 4: Cox proportional hazard regression model for ovarian cancer survival Variable RR p 95% CI lower 95% CI upper SGLT2 knockdown 24.48 0.0019 - - Univariate SGLT2 knockdown 57.26 0.0002 79.628 103.3 Multivariate ID8-6 (vs ID8-25) 5.29 0.0053 66.946 95.498 Multivariate Akt2 WT (vs KO) 3.45 0.0319 74.61 103.79 Multivariate 102 Table 5: Median survival times of mice with SGLT2 KD tumours Experimental Group Median survival (days PTI) WT KD ID8-6 69 Akt2 KO KD ID8-6 86 WT KD ID8-25 111 WT Control ID8-25 112 Akt2 KO KD ID8-25 115.5 Akt2 KO Control ID8-6 126 Akt2 KO Control ID8-25 126 WT Control ID8-6 126 Tumours deficient in SGLT2 have more severe secondary disease The number and dispersal of secondary lesions plus the volume of ascites in tumourbearing mice constitute our assessment of secondary disease. Knockdown mice had higher rates of metastasis (p>0.00001), but differences were not significant by ID8-6 or genotype (Figure 27). The severity of secondary disease is associated with overall survival. Widespread metastatic lesions are more consistently associated with morbidity than tumour size (Figure 28). 103 Figure 27: Secondary disease is much more severe in mice with SGLT2 KD tumours A) Representative images of advanced peritoneal disease. Secondary lesions (B, C) were scored on a 4-point scale with 0 indicating absence of secondary disease and 4 indicating more than 10 lesions spread throughout the peritoneal cavity. Tumours with SGLT2 knockdown have higher rates of metastasis (p>0.00001). Neither cell type (ID86/ID8-25) nor genotype (WT/Akt2-/-) significantly affected number of secondary lesions. 104 4 400 300 3 200 2 100 1 Secondary score Tumour weight (mg) Primary tumours ID8-6 KO ID8-25 KO ID8-6 WT ID8-25 WT Secondary lesions 0 0 60 75 90 105 120 135 Days PTI Figure 28: Poor overall survival is associated with severe secondary disease, regardless of primary tumour weight, in mice bearing SGLT2 KD tumours Data represent the cohort of mice (WT or Akt2 KO) injected with ID8-6 or ID8-25 SGLT2 KD cells. Coloured circles represent primary tumour weights at death. The secondary lesion scores for animals that died on a particular day are marked by blue squares. Shorter survival times were generally associated with small primary tumours but high secondary scores which indicate multiple metastatic lesions spread throughout the peritoneal cavity. In mice that survived longer, there appears to be more variability in both tumour weight and secondary scores. 105 Discussion Glucose uptake in epithelial ovarian tumours occurs through the coordinated actions of active (SGLT) and passive (GLUT) transporters Glucose can enter cells through two classes of transporters. The GLUT proteins facilitate transmembrane diffusion and are upregulated in most cancers.227 The sodiumglucose transporters (SGLT) can move glucose against its concentration gradient by using the inward sodium concentration gradient maintained by the Na+/K+ pump. Here we demonstrated for the first time that members of both transporter families are expressed in epithelial ovarian cancer (EOC). ID8 murine EOC cells express the mRNA of SGLT2, GLUT1 and GLUT3, all of which are high capacity glucose transporters. GLUT1 and GLUT3 have previously been reported in EOC, however in our subsequent experiments we decided to focus on the contributions of the GLUT1 isoform because of its stronger association with tumour development.126 Very few data exist on the expression of the SGLTs in human cancers. Where it has been examined, SGLT isoforms vary among tumour types: preliminary studies have shown that SGLT1 is expressed in breast145,228, prostate145,228, head and neck229, colon230, laryngeal231, pancreatic232, oral233, and ovarian cancers234 while SGLT2 expression has been noted in lung,235 pancreatic223, and prostate223 cancers. We used a tissue microarray of serous ovarian adenocarcinomas from women to examine the protein expression of SGLT1 and SGLT2. SGLT1 protein was expressed at low levels in about 30% of serous adenocarcinoma samples, while SGLT2 was strongly expressed in all samples (Figure 14). Neither isoform was correlated with tumour stage, but lower 106 expression was associated with more poorly differentiated tumours. Subsequent to these experiments, another group investigated SGLT expression in ovarian cancer. Contrary to our findings, this large study found that SGLT1 was overexpressed and was an independent biomarker for poor prognosis. The reason for the differences in SGLT1 expression in the two sets of samples is puzzling considering that the histochemical methodology and antibody used were the same.234 It is unclear whether or not they looked for SGLT2 expression. In order to determine the relative contributions of each class of transporters, we used class-specific inhibitors of GLUTs and SGLTs. Inhibition of the GLUT transporters with cytochalasin B or phloretin reduced glucose uptake in cells cultured in a physiological glucose concentration (6mM), but was ineffective in hyperglycemic conditions (25mM glucose). Conversely, inhibition of the SGLT transporters with phlorizin had greater effects in high glucose than in normal glucose. Rather surprisingly, the combination of SGLT and GLUT inhibitors did not have an additive effect on glucose uptake. We hypothesize that this is a result of their reciprocal effects in high and low glucose: because the GLUT transporters had low activity in high glucose, competitively inhibiting them in these conditions would have had little additional effect on overall glucose consumption. The same would be true of inhibiting SGLT transporters physiological concentrations of glucose. In vivo, GLUT-mediated uptake compensated for a lack of SGLT2. Mice whose tumours had reduced expression of SGLT2 took up relatively less of the SGLT-specific glucose analogue 14C-AMG than those with SGLT2. However, compensation from the GLUT transporters maintained similar total glucose uptake (Figure 23). Expression of the two 107 families of transporters appears to be inversely associated. In colon cancer cells SGLT1 is downregulated following oncogenic transformation while GLUT1 is upregulated.230 Similarly, in renal epithelial cells hypoxia increases GLUT1 expression but concurrently decreases SGLT1 and SGLT2.236 The influence of oxygen levels on SGLT expression suggests that they may be regulated by HIF-1α expression, whose pro-tumourigenic effects could explain the increased SGLT expression after oncogenic transformation. In tumours from diabetic mice at 45 days PTI, we saw significant upregulation of GLUT1 protein in the SGLT2 KD group which matched the pattern of radioactive glucose uptake observed at 120 days (Figure 24). However, despite confirmation of SGLT2 knockdown in the tumour-initiating cells, we did not see a decrease in SGLT2 protein expression in tumours at 45 days by Western blot. In WT animals, tumours initiated with SGLT2 deficient cells did not show changes in the expression of either SGLT2 or GLUT1, although again there was an increase functional activity of GLUT transporters at 120 days PTI. In addition, although GLUT1 appeared to be significantly upregulated in SGLT2 KD cells by Western blot at 45 days PTI, immunohistochemical analysis showed the opposite pattern in tumour samples taken at morbidity (Figure 21). This may be due to the relatively small size of these tumours, as well as the fact that they were taken at animal death. We were unable to collect enough sample to stain for SGLT2 expression in tumours initiated with SGLT2-competent cells. These results indicate that transporter expression is not directly associated with uptake kinetics, and suggest that SGLT2 expression in non-cancerous cells in the tumour may obscure the knockdown that was clearly seen in isolated cells in vitro. 108 The active sodium-glucose symporter SGLT2 is protective against cancer death, primary tumour growth, and metastatic secondary disease in an orthotopic mouse model of EOC The uptake and phosphorylation of glucose are the most important steps in determining glycolytic flux.94–96 Hypothesising that inhibited SGLT transport would slow tumour growth, we stably knocked down the expression of the SGLT2 isoform in ID8 cells using shRNA. Although SGLT1 has the capacity to take up glucose when SGLT2 activity is compromised,237 Western blot analysis suggested that this isoform had limited expression in the ID8-cell tumours. Although there was efficient uptake of the lentiviral particles containing the shRNA against SGLT2, achieving knockdown was very difficult particularly in ID8-25 (cells conditioned to hyperglycemia). If SGLT2 is more important in cells in high glucose (ID8-25), then KD cells would be less likely to survive even if they are puromycin resistant. Because we selected single cells that appeared most active in the presence of puromycin, it is possible that we selected for cells that had lesser knockdown due to the random integration of the lentiviral construct into the genome of the cell. The results of this study strongly opposed our hypothesis and rather than improving the outcome of EOC in a mouse model, SGLT2 KD actually increased the relative risk of dying by 57 times. We can only speculate on the mechanism behind these surprising results. Interestingly, SGLTs appear to be protective in many cases: increasing overall survival231 or disease free survival232, and higher expression in better differentiated tissues.229,230 We expected that the ability for SGLT2 to take up glucose independently of its extracellular concentration would lead to more aggressive disease. However, it 109 could instead have relieved some of the selective pressure for mutations or non-genetic actions that would facilitate metastasis. If SGLT2 KD provides a strong impetus for cells to move away from the primary tumour to gain access to resources in a more abundant and less competitive environment, we would expect to see more cell motility and a greater spread of secondary disease. Results from the mouse model (Figure 27), cell invasion assay (Figure 19) and the movement of individual cells in culture (Figure 20B) all seem to support this premise. Secondary disease is a better predictor of death than primary tumour weight. The impact of SGLT KD in EOC may also be related to its role as an ion transporter. Transport through SGLTs can be driven by protons as well as sodium.130 The dysregulated metabolism of cancer cells results in high extracellular H+ concentrations that may favour SGLT-mediated glucose uptake. There is an extensive body of evidence indicating that GLUT1 overexpression is associated with aggressive disease. Overexpression of GLUT1 in EOC predicts response to chemotherapy and shorter disease-free survival238 and expression progressively increases with stage and grade suggesting it may be related to malignant transformation.239,240 These data indicate that SGLT2 knockdown may be promoting EOC growth indirectly by increasing GLUT1, which would suggest that SGLT somehow limits GLUT upregulation. In our experiments GLUT1 compensation did not increase overall glucose uptake, but simply maintained the levels seen in tumours with SGLT2-competent cells. However, we saw profound effects on EOC outcome, so the contribution of SGLT2 is not necessarily a glucose-related phenomenon. A similar situation has been noted in neurons, where SGLT1 expression appears to be important even in cells that have an 110 abundance of GLUT3 and more than sufficient glucose uptake capacity.130 The glucosesensing or water- and ion- transporting roles of SGLT could be the significant effectors preventing oncogenesis. In the mouse model, the level of systemic glucose played a limited role in the impact of SGLT2 KD on cancer progression. Neither genotype nor cell type had significant effects on their own, which highlights the dominant effect of SGLT2 KD, but they did influence survival in multivariate analyses. After controlling for SGLT2 KD and cell type, normoglycemic (wildtype) mice were more 3.5 times more likely to die than hyperglycemic and hyperinsulinemic (Akt2 KO) mice. This could be an indication that diabetic conditions support tumour growth, particularly when glucose transport is dysregulated. Mice whose tumours were induced by injection of ID8-6 cells were more than five times more likely to die than those with ID8-25 tumours after controlling for SGLT2 KD and genotype. Part of the effect of ID8-6 over ID8-25 could be attributed to the difference in amount of SGLT knockdown (Figure 20A). The studies presented here show compelling data that SGLT2 acts as a tumour suppressor. Knockdown of SGLT2 in tumour cells increased tumour size, severity of secondary disease, and substantially reduced survival times. In vitro observations complemented this finding and collectively indicated a protective role for SGLT2 in cell proliferation and migration, particularly in hyperglycemic conditions. Taken together, SGLT2 appears to be most powerful on cell motility/invasion. There are several examples of things that have limited effect on primary tumour growth but that promote migration and increase the formation of metastases, including L-lactate.105 111 The overexpression of SGLT2 in the tissue microarray and the ability of its inhibition to promote tumour growth seem at odds with one another. However, protein expression does not necessarily reflect membrane expression or the kinetics of glucose uptake. As yet there have been no functional studies of SGLT-mediated glucose uptake in human ovarian tumours. Moreover, the ability of GLUTs to compensate for reductions in SGLTmediated glucose uptake make these results hard to interpret. Based on these findings, we would expect the use of SGLT2 inhibitors to be associated with an increase cancer or cancer-related death. Safety studies of SGLT2-inhibiting diabetes drugs have not shown prohibitively high incidences of cancer, although it is acknowledged that these data are not conclusive.241 FDG may underrepresent the total amount of glucose uptake into cancer cells The high accumulation of the glucose analogue FDG is used to differentiate highly glycolytic tumour tissue from normal tissue. Currently, FDG is the only FDA approved oncolytic tracer and more than 90% of oncological PET imaging uses FDG. 161 However, FDG is a poor substrate for SGLTs. Because FDG is not transported through the SGLT transporters, this suggests that tumours fulfilling metabolic needs through SGLTs will have weaker PET results that may contribute to a false-negative diagnosis. Moreover, the results of this study suggest that low or falling SGLT transport may indicate more aggressive disease. 112 GLUTs and SGLTs appear to coordinate glucose transport into cancer cells and have differential importance in normal and high glucose environments. GLUT was able to compensate for the decreased 14C-AMG uptake in SGLT KD tumours by raising its uptake of 3H-DG. It would be interesting to see if SGLT transport could compensate in the same way if the GLUTs were compromised. Conclusions GLUT1 expression is historically considered the most important glucose transporter in cancer cells and is correlated with many markers of advanced disease. For the first time, we show that a second class of transporter, SGLT, is not only expressed, but also makes significant functional contributions to EOC progression. 113 CHAPTER 4: ANTIDIABETIC EFFECTS OF METFORMIN AS EOC THERAPY Introduction Metformin is a commonly prescribed and inexpensive first-line diabetes treatment that has shown promise as a novel cancer therapeutic. In epithelial ovarian cancer (EOC), however, its antineoplastic effects are inconsistent across different study populations and are confounded by the underlying interaction between cancer and diabetes.242 Some studies have shown that metformin decreases cancer risk in patients with T2DM,243,244 while others have found no association with the risk of ovarian cancer.245 Similarly, some studies have shown that metformin improves the survival for ovarian cancer patients with concurrent diabetes181,246,247 while others have found that metformin use among diabetic EOC patients does not affect progression-free survival or overall survival.180,248 Metformin lowers glucose in an insulin-independent manner by inhibiting hepatic gluconeogenesis, increasing peripheral glucose uptake in skeletal muscle and decreasing renal and intestinal glucose reabsorption (reviewed in 249). These effects are primarily mediated through the AMPK energy sensing pathway and its downstream inhibition of mTOR.250,251 Increases in AMPK activation in response to a high AMP:ATP ratio signal an energy deficit and promote a catabolic state through mechanisms such as autophagy and the inhibition of anabolic proteins. Pre-clinical studies have shown that the AMPK pathway also mediates anti-proliferative effect of metformin in EOC.252 Metformin has a further range of effects on cancer cells through AMPK-independent 114 mechanisms that inhibit mTOR signaling253 and cell proliferation, and promote apoptosis and cell cycle arrest.254,255 Figure 29 illustrates some of metformin’s cellular effects. Metformin appears to be particularly toxic to p53 negative cells in colon cancer256 and can selectively kill cancer stem cells in breast cancer.257 However, the greatest potential of metformin as a cancer treatment may be its synergistic effect with various chemotherapeutics.258 Metformin potentiates the effects of doxorubicin,257 paclitaxel259,260 and cisplatin261–264 and can resensitize previously chemo-resistant cells. Authors have postulated that the mechanisms behind this cooperation include the additive affects of chemotherapy on activation of AMPK259,262, the ability of metformin to selectively target cancer stem cells that are not affected by chemotherapy alone 257, further cytotoxicity261, or though inhibition of the MAPK/ERK pathway, leading to apoptosis.264 Combination with chemotherapy may allow therapeutic effects to be reached at much lower concentrations than required by chemotherapy as a single agent.265 The NIH clinical trials database lists three phase II and III trials recruiting to look at ovarian cancer and metformin + paclitaxel and/or carboplatin. Although metformin is an antidiabetic drug and diabetes is related to poor cancer outcomes,199 very little research has examined metformin’s antineoplastic effects through this mechanism. We hypothesized that despite metformin’s direct cellular effects on EOC, its primary action in diabetic cancer patients is through the reduction of systemic fuel availability. The goals of this study were to investigate both the effects of metformin on diabetic vs nondiabetic populations in a mouse model of EOC, and the effects of hyperglycemia on metformin action in vitro. 115 Figure 29: Cellular effects of metformin 116 Materials and Methods Cell Culture Mouse-derived epithelial ovarian cancer cells (ID8; kindly donated by Drs. Paul Terranova and Kathy Roby, Kansas State University, Kansas, USA) were maintained in DMEM supplemented with 10% fetal bovine serum (FBS), 1% antibiotic/antimycotic (Gibco BRL, Burlington, ON) and 2% L-glutamine (Life Technologies, Burlington ON). All experimental treatments were performed in serum-free DMEM. Drugs Phlorizin (PZ; Sigma, Oakville, ON) competitively inhibits glucose transport through sodium/glucose cotransporters (SGLTs). Cytochalasin B (CB; Sigma, Oakville, ON) inhibits glucose transport through the passive glucose transporters (GLUTs). Metformin hydrochloride was purchased from Sigma (Oakville, ON). Viability assay The MTT assay measures cellular reduction of a tetrazolium salt to a coloured formazan product in an NADH- and NADPH-dependent manner and reflects primarily glycolytic activity. Cells were seeded at a density of 1500 cells/well in triplicate in 96 well plates and allowed to attach overnight. Cells were then serum starved for 6 hours and treated for 48 h in serum-free conditions. Following treatment, cells were incubated with MTT 117 (5mg/ml; Sigma, Oakville, ON) for one hour at 37°C and lysed with MTT lysis buffer overnight at 37°C. Absorbance was quantified in a microplate reader at 570nm. Scratch wound assay To examine the motility of cells in different concentrations of glucose, ID8-6 and ID8-25 cells were grown to confluency in 24 well plates and serum starved for 6 hours. A plastic pipette tip was used to remove an area of cells down the centre of the dish. Wells were gently washed with PBS to remove detached cells before treatment. Phase contrast images were taken at three marked points along the scratch at t=0 and t=24 hours. Wound sizes were determined using ImageScope software and are presented as the fraction of the original scratch covered by cells. Glucose consumption and cell number Glucose concentration in the cell media was measured using the glucose oxidase method and reagents from Pointe Scientific (Canton MI, USA). After 24 hours of treatment, glucose concentration in the sample wells was subtracted from the glucose concentration in blank wells to determine the amount of glucose consumed. Relative cell number was approximated by the absorbance of the crystal violet nuclear stain. To account for any differences in the rate of cell proliferation, glucose consumption was divided by relative crystal violet absorbance (590nm) to determine a per-cell uptake comparison. 118 Animals Wildtype c57bl/6 mice were purchased from Charles River Laboratories (Wilmington, MA, USA), and c57bl/6 Akt2 null mice (https://www.jax.org/strain/006966) were purchased from Jackson Laboratories (Bar Harbour, ME, USA). An Akt2 null mouse colony was established from breeder mice and animals were genotyped prior to beginning experiments. Animals were housed at the Central Animal Facility at the University of Guelph and all experiments were conducted according to Canadian Council on Animal Care guidelines. Mice were kept on a 12h light:dark cycle and had free access to food and water. For all experiments, adult mice were between 12 and 24 weeks old at time of surgery. Metformin hydrochloride (Sigma, Oakville, ON) was dissolved in sterile PBS and administered as a daily IP injection at either 50mg/kg/day or 150mg/kg/day. Mouse model of epithelial ovarian cancer Spontaneously transformed murine epithelial cells from C57Bl/6 mice (ID8) were diluted in 5µl phosphate buffered saline (PBS) and injected under the ovarian bursa of WT or Akt2 null mice. This orthotopic, syngeneic mouse model of EOC closely replicates ovarian serous adenocarcinoma in women. By 90 days post-tumour induction, mice develop large primary tumours, secondary peritoneal lesions, and significant abdominal ascites.10 In survival experiments, mice were sacrificed when they became moribund due to the accumulation of ascites fluid. 119 Type 2 Diabetes Mellitus (T2DM) C57BL/6 mice homozygous for a mutant Akt2 allele have poor glucose tolerance and reduced insulin sensitivity that result in hyperglycemia and hyperinsulinemia.193,194 Obesity often accompanies T2DM and is independently associated with diabetes and cancer. Akt2-/- mice are not obese so this model isolates the contributions of high glucose and high insulin. Mice were genotyped using the following primers designed by Jackson Laboratories: Akt2 wildtype reverse: TGCACAATCTGTCTTCATGCCAC; Akt2 common forward: ACCAACCCCCTTTCAGCACTTG; Akt2 mutant reverse: TACACTTCATTCTCAGTATTGTTTTGC. Products are 110bp (wildtype), 277bp (mutant), or 110bp and 277bp (heterozygote). Food Consumption Weekly food consumption was calculated by taking the initial weight of dry food and subtracting food weight after 5 days. This value was divided by the number of mice in the cage and the number of days in the measurement period to determine food consumed per mouse per day. Intraperitoneal glucose tolerance tests Mice were fasted for four hours prior to intraperitoneal glucose tolerance tests (IPGTT). After recording baseline blood glucose, mice were given an intraperitoneal injection of glucose (1 mg/g body weight in saline solution at a volume of 10µl/g body weight). Blood glucose measurements were taken at 15, 30, 60, and 120 minutes after glucose 120 challenge using a handheld glucose monitor (Freestyle Lite, Abbott Laboratories, Abbott Park, IL). Values that exceeded the measurement range of the glucose monitor were considered 27.8mM (maximum reading possible). Data are presented as the average integrated area under the curve (iAUC) ± SEM. The iAUC is the area under the curve relative to FBG at time 0 and was calculated using the trapezoidal method. Tissue collection and preparation Mice were fasted for 6 hours prior to sacrifice by cervical dislocation. Following euthanasia, trunk blood was collected and fasting blood glucose was measured immediately using a handheld glucometer. The remaining blood was allowed to clot then centrifuged to obtain serum samples and stored at -80oC. Ovarian tumours were removed, weighed, and divided into sections for subsequent analysis. Sections were either fixed in 10% neutral buffered formalin (Fisher Scientific, Whitby, ON) for wax embedding and tissue sectioning or flash frozen in liquid nitrogen and stored at -80oC for protein extraction. Secondary disease was evaluated at time of sacrifice by ascites volume and number of secondary lesions. Mice were scored on a 4-point scale with 0 indicating absence of secondary disease. Mice with scores of 0 and 1 were considered “low” and scores of 2 and 3 were considered “high”. Statistical Analysis Data were analyzed using GraphPad Prism statistical analysis software. Results are reported as mean ± standard error of the mean (SEM). Significance threshold was set 121 at 0.05 and p values are listed in the figure legends. Comparisons between means were measured by two-way ANOVA followed by a Bonferroni correction, or by unpaired twotailed Student’s t-test, unless otherwise noted. Overall survival data are plotted on a Kaplan-Meier survival curve and differences were determined by a log-rank (MantelCox) test. 122 Results In vitro Metformin affects systemic metabolism in diabetic patients but has little risk of hypoglycemia in nondiabetics. To determine if there were also differential effects at a cellular level in EOC cells, we tested the effects of metformin in physiological glucose concentrations (6mM) and hyperglycemic concentrations (25mM). The MTT assay was used to measure the metabolic viability of ID8, SKOV3, and normal human ovarian epithelium (NOSE) treated with metformin. The concentration of glucose did not affect the metabolic response to metformin (Figure 29A). In previous experiments we have found that the chronic culture conditions of cells can affect their response to treatment media with different concentrations of glucose. We compared the effects of metformin in 6mM glucose media on cells chronically cultured in normoglycemic conditions (-6 cell lines) and those cultured in diabetic conditions (-25 cell lines). The metabolic viability of cells acclimatized to hyperglycemic conditions was significantly more sensitive to the effects of metformin. ID8-6 cells showed no significant response to metformin until 80mM and SKOV3-6 were unaffected until 40mM. Interestingly, the metabolic response of SKOV3-6 cells was identical to that of normal ovarian epithelium (Figure 29B). In ovarian cancer cells acclimatized to hyperglycemia (ID8-25, SKOV3-25; Figure 31, part A) there were dose-responsive declines in viability that were significant after 5mM and 2.5mM metformin respectively. These findings are in line with other studies which have also found no direct toxicity (necrosis, apoptosis) in this dose range indicating that 123 it is at a therapeutic level.266 The viability of NOSE cells was only reduced at metformin concentrations greater than 40mM. The MTT assay measures NADH formed primarily through glycolysis compared to oxidative phosphorylation. These results imply that the glycolytic flux in “diabetic” cancer cells is more sensitive to inhibition by metformin. 124 Figure 30: Metformin inhibits EOC cell viability in high glucose MTT absorbance was used to determine cell viability. A) Viability of mouse epithelial ovarian cancer, human ovarian cancer, and normal human ovarian epithelial cells (ID8, SKOV3, NOSE) in media containing physiological glucose (6mM) or high glucose (25mM). B) Viability of cells chronically cultured in physiological (red, 6mM glucose) or hyperglycemic (blue, 25mM glucose) conditions. Left: murine, right: human. Black dashed line indicates cells derived from normal epithelial and cultured in physiological glucose. n=3. Values are mean ± SEM. Stars indicate differences between cell lines at a single metformin concentration. *p<0.05, **p<0.01, ***p<0.001. 125 Although metformin had a greater effect on metabolic viability in high glucose, cell number appeared to be more affected in conditions of glucose deprivation (Figure 30A). Consistent with this, the ability of metformin-treated cells to heal a scratch wound was impaired in low but not high glucose (Figure 30B). 126 Figure 31: Metformin reduces cell number in glucose-deprived cultures A) ID8-25 cells were cultured in different glucose concentrations for 48 hours with or without 50mM metformin. Crystal violet absorbance at 590 nm was used as an indicator of cell number. Bars are mean + SEM. Stars indicate significant differences from crystal violet absorbance in 6mM glucose. Brackets indicate differences between treatments at the same glucose concentration. n=2; **p<0.01, ***p<0.001. B) Scratch wounds were made by clearing an area of cells with a pipette tip. Images were analyzed to determine the fraction of the scratches covered by cells after 48 hours of treatment with 5mM metformin. Bars are mean + SEM, n=4. **p<0.01, ***p<0.001. 127 Metformin significantly increased cellular glucose consumption regardless of environmental glucose availability (Figure 31). To determine whether glucose uptake capacity contributed to this increase in glucose uptake, we used glucose transport inhibitors to both the passive (GLUT; cytochalasin B) and active (SGLT; phlorizin) glucose transporters. In low glucose, total glucose uptake was still enhanced compared to control in the presence of glucose transport inhibitors. In high glucose, GLUT inhibition abrogated this effect and glucose uptake was unchanged with cytochalasin B treatment (Figure 32A). On a per-cell basis the increases in glucose consumption were reduced, however a statistical trend remained (p<0.09) (Figure 32B). 128 Figure 32: Metformin increases cellular glucose consumption Cells were treated with 5mM metformin in media containing normal (6mM) and high (25mM) concentrations of glucose. A) Total glucose consumed in mg/dL B) Relative glucose consumption per cell. C) Fraction of glucose consumed relative to the initial glucose concentration in the cell media. Bars are mean + SEM, n≥5. Different letters represent significant differences between bars (p<0.05). 129 Figure 33: Metformin-mediated increase in glucose consumption is independent of glucose transporter expression Cells were treated with 5mM metformin dissolved directly into culture medium, 50µM phlorizin (PZ in 0.01% DMSO; SGLT inhibitor), or 0.5µM cytochalasin B (CB in 0.01% DMSO; GLUT inhibitor) in media containing normal and high concentrations of glucose. A) Total glucose consumed in mg/dL. B) Relative glucose consumption per cell. Bars are mean + SEM, n≥4. *p<0.05, **p<0.01, ***p<0.001 between metformin and vehicle control. 130 In previous work we have shown that EOC progresses faster in both type 1 and type 2 diabetic mice than in nondiabetic animals. We predicted that normalizing blood glucose in diabetic animals would improve EOC outcome by reducing the amount of systemic glucose available for the tumour to consume. Metformin has also been shown to have beneficial effects in normoglycemic preclinical models through direct effects on cellular signalling pathways. In order to assess the effects of metformin on EOC tumour growth we used induced tumours in both wildtype (WT) mice and a genetic model of non-obese mice with a T2DM hyperglycemic, hyperinsulinemic phenotype (Akt2 KO). Three in vivo studies were performed using a mouse model of ovarian cancer developed in our lab. Briefly, syngeneic ID8 cells were injected orthotopically beneath the ovarian bursa of C57bl/6 mice. These cells develop into disease that closely replicates human serous ovarian cancer. Tumour development over 30, 60 and 90 days is representative of EOC Stages 1, 2 and 3 respectively. In population studies, the use of metformin has been correlated with a lower risk of developing cancer. The first study was designed to evaluate the ability of chronic metformin administration to prevent tumour growth. WT and Akt2 KO mice received daily IP injections of either metformin or PBS control at 50 mg/kg body weight between two weeks after surgery until 90 days PTI. Metformin had no effect on fasting blood glucose in WT mice. In KO mice, although FBG dropped significantly over time posttumour induction, the effects of metformin and PBS were identical (Figure 33B). At 90 days PTI, the weight of tumours in the metformin treated mice was no different than those in PBS treated mice within each genotype (Figure 33A). In contrast to previous experiments which showed that Akt2 KO mice grew significantly larger tumours than 131 WT mice 90 days PTI (Figure 7A), a one-way ANOVA of control and metformin in both genotypes (comparison between Figure 33As) in this trial showed no significant differences in tumour weight. Tumour initiation in this trial was weak and the lack of a genotype-related effect was probably due to the very small size of these tumours. 132 Figure 34: Small tumours normalize blood glucose in diabetic mice Tumours in wildtype and diabetic (Akt2 -/-) mice were treated with daily IP injections of 50mg/kg/day metformin (2 weeks PTI to 60 days PTI) then 150mg/kg/day (60 until 90 days PTI). A) Metformin treatment did not affect tumour. B) Fasting blood glucose. Bars are mean + SEM, n=5. *p<0.05, **p<0.01, ***p<0.001. 133 The human dose is of metformin is approximately 35mg/kg/day orally.267 In our experiments, the original dose of 50 mg/kg/day IP was chosen based on literature at the time which used this dose in chronic administration.268 However, because this dose did not affect the blood glucose in the Akt2 KO mice as we had expected, we increased the daily dose of metformin to 150 mg/kg/day in a second study.263 In this second study, we again began metformin treatment at two weeks PTI in order to evaluate the effects of metformin on tumour growth prevention. Mice were sacrificed when they became moribund. We found no differences in the length of survival or tumour weight at survival in WT mice treated with either metformin or PBS control (Figure 34A and B). Qualitatively there was a slight reduction in the number of secondary lesions, but our scoring system for evaluating secondary disease did not allow us to determine statistical significance from these data (Figure 34C). We measured food consumption to determine whether the drug was affecting total glucose intake and found that metformin had no effect (Figure 35A). In PBS treated mice, the presence of the developing disease resulted in significant fluctuations in fasting blood glucose. Metformin appeared to protect against this variability (Figure 35B). We performed IPGTTs in mice with and without tumours to determine whether metformin alone could affect glucose tolerance. Metformin had no effect on the glucose tolerance of mice with tumours, but surprisingly it significantly worsened glucose tolerance in mice without tumours (Figure 35C and D). 134 Figure 35: Daily metformin treatment does not affect EOC outcomes in WT mice A) Tumours were removed and weighed when mice became moribund. Values are mean + SEM, control: n=9, metformin: n=6. There was no significant difference in tumour weight at death between metformin- or control-treated mice. B) Kaplan-Meier survival curve of WT mice with ovarian cancer that received 150mg/kg daily metformin in PBS IP treatment from two weeks PTI until death. There is no statistical difference in survival between groups by log-rank (Mantel-Cox) test. C) Secondary lesions and ascites volume. Values are proportion of mice with “high” or “low” scores. 135 Figure 36: Metformin treatment in WT mice with tumours impairs glucose tolerance over time. WT mice bearing tumours were treated with daily metformin injections (150mg/kg) beginning two weeks PTI. A) Food consumption at 2, 7 and 10 weeks PTI (0, 5 and 8 weeks of metformin treatment). Bars are mean + SEM, n=5. B) Fasting blood glucose 136 between surgery (0 weeks) and death (†). Bars are mean + SEM, n=5; *p<0.05 vs baseline. Comparison of FBG from baseline is by two-way ANOVA with Dunnett’s posthoc test. C) Results of intraperitoneal glucose tolerance tests (IPGTT). ***p<0.001 vs control at a specific time point. D) Integrated area under the curve (iAUC) of IPGTTs. Glucose tolerance was impaired at 90 days PTI vs 60 days PTI in metformin-treated mice with tumours. *p<0.05. Control: n=9, metformin: n=6. 137 In diabetic mice (Akt2 KO), there were no differences in tumour weight, length of survival or severity of secondary disease (Figure 36). Mice in this trial died earlier than expected (Figure 36B), likely due to tumour initiation with high passage cells that accelerated disease progression. Food consumption decreased over time as EOC progressed, but there were no differences between PBS and metformin treatments (Figure 37A). In IPGTTs, metformin had no effect on glucose tolerance regardless of the presence of a tumour. However, in all Akt2 KO groups, glucose tolerance improved with time and the addition of metformin did not add to these effects (Figure 37D). Mice without tumours that were treated with metformin showed the same improvement in glucose tolerance as untreated mice with tumours. As in the wildtype mice, although there were clear differences in glucose tolerance between groups, FBG was more variable (Figure 37B). 138 Figure 37: Daily metformin treatment does not affect EOC outcomes in Type 2 diabetic mice Tumours were removed and weighed when mice became moribund. Values are mean + SEM, control: n=14. There was no significant difference in tumour weight at death between metformin- or control-treated mice. B) Kaplan-Meier survival curve of WT mice with ovarian cancer that received 150mg/kg daily metformin in PBS IP treatment from two weeks PTI until death. There is no statistical difference in survival between groups by log-rank (Mantel-Cox) test. C) Secondary lesions and ascites volume. Values are proportion of mice with “high” or “low” scores. 139 Figure 38: The presence of a tumour or treatment with metformin both improve glucose tolerance in diabetic mice Akt2 KO mice bearing tumours were treated with daily metformin injections (150mg/kg) beginning two weeks PTI. A) Food consumption at 2, 4 and 7 weeks PTI (0, 2 and 5 weeks of metformin treatment). Bars are mean + SEM, n=5. B) Fasting blood glucose 140 between 3 weeks PTI (1 week of metformin treatment) and 8 weeks PTI (six weeks of metformin treatment. Bars are mean + SEM, n=5; Brackets indicate significant differences between bars. *p<0.05. C) Results of intraperitoneal glucose tolerance tests (IPGTT). D) Integrated area under the curve (iAUC) of IPGTTs. In Akt2 KO diabetic mice, glucose tolerance between 30 and 60 days PTI was improved by the presence of tumours. Mice that underwent a sham surgery showed improved glucose tolerance with metformin treatment *p<0.05. Control: n=9, metformin: n=6. 141 In the third study, we investigated whether metformin administered to WT mice with established tumours (from 60d PTI to 90d PTI), could have an effect on disease progression/regression. There were no differences in tumour size. Figure 39: Metformin treatment does not reduce the weight of established tumours Wildtype mice were allowed to grow tumours for 60 days before 30 days of daily treatment with 150mg/kg/day metformin IP. Bars are mean tumour weight at 90 days PTI + SEM, n=5. 142 Discussion Preclinical evidence suggests that the glucose-lowering drug metformin is effective in limiting EOC growth in vitro. The OCT1 transporter is necessary for metformin entry into cells and is expressed in the human ovarian cancer cells lines SKOV3 and OVCAR3, as well as in malignant cells in ovarian tumours.269 Metformin can inhibit proliferation, migration, invasion, and adhesion in EOC monolayer culture as well as inhibit the formation of tumour spheres, induce cell cycle arrest and increase apoptosis.260–263,270 We have previously shown that both Type 1 and Type 2 diabetes significantly accelerate the growth of ovarian tumours in a mouse model of EOC. The goal of this study was to determine if EOC progression can be prevented or reversed by lowering blood glucose. Metformin is a widely prescribed antidiabetic drug which has recently been shown to improve both the risk and outcome of a number of cancers. By inducing ovarian cancer in both WT and diabetic (Akt2 KO) animals, we hoped to identify any protective effects of metformin through its action in lowering systemic hyperglycemia as well direct its effects on EOC cells. Cellular effects in different glucose levels The effects of metformin appear to be dependent on the level of environmental glucose. Metformin reduced cell number in restricted glucose but not hyperglycemia (Figure 30A) and it inhibited wound healing in normal but not high glucose (Figure 30B). These findings are consistent with other studies that have shown high glucose impairs or even reverses the anti-cancer effects of metformin.271,272 When treated with metformin, cells 143 in 5mM glucose show gene expression changes in pro-tumorigenic pathways; this effect is abolished cells in high glucose (10mM or above).216 This is perhaps not surprising because many of metformin’s effects are dependent on AMPK activation, which also responds to the AMP:ATP ratio. A low AMP:ATP ratio indicates high energy availability and would oppose the effects of metformin, meaning that the same drug dose in high glucose would be less effective at promoting AMPK-mediated anti-neoplastic effects. Several studies have suggested that increased metformin efficacy in low glucose is due partly to downregulation of the glycolytic enzyme pyruvate kinase M2 (PKM2) in these conditions.271,273,274 The effects of metformin on a systemic level are mostly concentrated in the liver and skeletal muscle where AMPK activation increases glucose uptake and decreases gluconeogenesis to reduce blood glucose. In vivo, we evaluated metformin’s effect on tumour weight and overall survival. Although metformin has direct effects on cells, we anticipated that when given systemically in hyperglycemic mice, metformin’s anti-cancer effects would be mediated primarily through its ability to reduce blood glucose. In our model, metformin was unable to oppose tumour growth in either normal or hyperglycemic mice. The doses of metformin that we used (50mg/kg/day and 150mg/kg/day) did not reduce blood glucose and so we cannot draw conclusions on the effect of lowering glucose on the progression of EOC. In a pilot study, we administered up to 250 mg/kg/day IP in an effort to reduce blood glucose, however within four days of this dosing three mice had died and we reduced the dose to 150mg/kg/day. However, the lack of effect of metformin on tumour growth in normoglycemic mice suggests that it has limited influence directly on cancer cells. This finding is in disagreement with a 144 number of studies of EOC that demonstrate metformin can reduce primary tumour growth and proliferation, and the formation of metastases.260,262,263,266 Although the metformin doses in these studies were similar to what we used, these studies were all performed with subcutaneous xenografts in immunocompromised mice. Both the ovarian microenvironment10 and immune-related inflammation43 significantly impact tumour biology, which could explain why metformin treatments were ineffective in our orthotopic model. Litchfield and others used a similar ID8 orthotopic model and found that metformin inhibited tumour growth in normoglycemic mice but not diet-induced hyperglycemic mice.272 In their study, metformin treatment began three weeks prior to tumour induction and the tumours that developed were much smaller than what we typically see (~40mg in untreated normoglycemic mice and ~90mg in untreated hyperglycemic mice vs ~150mg and ~350mg in our mice). Taken together with our findings, these data suggest that metformin’s effects against EOC are primarily preventative rather than reductive. These same conclusions have been drawn in colorectal cancer where metformin has been found to limit tumour initiation but have no effects on existing tumours.275 Alterations in angiogenesis may provide the mechanism for this limited tumour growth. Metformin can decrease VEGF and/or microvessel density262,276 and in a breast cancer model it has been shown to reduce tumour angiogenesis, but not affect tumour volume.270 145 Metformin and reprogramming of cellular metabolism Several studies contend that metformin's inhibitory effects on cancer progression are cancer cell autonomous and AMPK-independent, instead acting through inhibition of mitochondrial enzymes to decrease cellular respiration and promote a compensatory increase in glucose uptake and glycolytic flux.277–280 We found that although short-term changes in environmental glucose did not affect viability with metformin treatment (Figure 29A), chronic culture in high glucose was associated with reduced viability, i.e. a decrease in glycolytic flux (Figure 29B). A highly glycolytic phenotype is generally related to more aggressively malignant cells, but forcing glycolysis also increases the tumour’s demand for glucose and can make cells acutely sensitive to glucose deprivation. The sensitivity of cells to metformin is dependent on their ability to cope with energetic stress.280 In the presence of glucose, metformin can suppress the overall efficiency of metabolism to inhibit the proliferation of human colon and thyroid cancers.271 When glucose becomes a limiting factor for metabolism, this metformininduced metabolic inefficiency induces cell death.271,277,279 The higher rate of glucose consumption we demonstrated with metformin treatment (Figure 31B) may suggest that metformin increased glycolytic activity. Dosing Drug repositioning often means using different concentrations to elicit different physiological responses. In diabetes, the effective dose for metformin has maximal pharmacological effect on tissue-specific metabolism in the liver and skeletal muscle, but minimal systemic toxicity. Using metformin in cancer treatment may require a 146 different dose and different dosing schedule that induces both pharmacological and toxic effects.281 For example, metformin at a concentration that effectively upregulates pAMPK may have no influence on decreasing mammary cancer severity in nondiabetic rats and mice.282 There are also large differences in the drug concentrations that are effective over different time periods. One group refers to the “metformin paradox” where long term metformin treatment over weeks or months requires only micromolar concentrations of metformin to elicit anti-cancer effects, whereas short term (12-48 hour) experiments need higher drug concentrations far beyond the human therapeutic dose of 15-17 µM.216 It is possible that rather than having a dose-responsive effect against cancer, there is a threshold concentration for drug effect that 150mg/kg/day did not reach which could partially explain the lack of effect that we saw in our in vivo models. Conclusion This study does not support a role for single-agent metformin treatment of EOC in either physiological or diabetic environments. We were unable to evaluate its effect on tumour growth through reduction in blood glucose, however others have shown that in diabetic animals, combined treatment of both anti-tumour and anti-hyperglycemia therapies give the best tumour-reductive outcome.213 Our in vitro findings support reports that high environmental glucose inhibits metformin’s anti-cancer effects. Taken together with our previous work that showed markedly worse EOC outcomes in diabetic mice, we conclude that glycemic control is an important consideration in EOC management. In diabetic mice the lower cell-level efficacy of metformin in hyperglycemia could be offset 147 by the fact that it reduces this hyperglycemia through actions on the liver and skeletal muscle. If there is a role for metformin in the treatment of EOC, the variability of its effects in preclinical models has shown that it will be essential to identify the subset of patients likely to respond, which could include evaluation of systemic glucose homeostasis, concurrent therapies, OCT1 transporter expression283 and oncogenic mutations.284 148 CHAPTER 5: GENERAL DISCUSSION Overview Glucose is an important energy substrate, survival factor, and pro-angiogenic molecule. This thesis examines the influence of high glucose availability on the growth of epithelial ovarian tumours, and attempts to the regulation of systemic glucose can be exploited therapeutically in cancer treatment. Since beginning this work, a number of significant discoveries have altered our understanding of cancer cell metabolism and tumour metabolism. In 2011, Hanahan and Weinberg updated their seminal “Hallmarks of Cancer” to include “reprogramming energy metabolism.”43 Hexokinase52,98,99 and the PKM2 fetal isoform of pyruvate kinase91 have emerged as key drivers of the Warburg effect. The sodium glucose transporter 1 (SGLT1) was found to be expressed in cancer cells and physically stabilized by EGFR, suggesting a role for EGFR in glucose balance.145,228 Perhaps most significantly, the meaning of abnormal “cancer metabolism” has expanded to include both cellular and intercellular characteristics. A metabolic symbiosis has been discovered between oxygenated and hypoxic cancer cells as they share lactate to maximize energy production.119 In addition, observation of a “Reverse Warburg” effect demonstrated an essential role for metabolically reprogrammed cancer-associated fibroblasts.116 Disrupting the unique energy balance of both cancer cells and tumours have direct anti-cancer consequences. Advances in the efficacy of EOC treatment have come from stratifying patients by disease type on histological and genetic levels. However, neither of these takes into 149 account the functional bioenergetic heterogeneity inherent at the levels of the cell, tumour and body. As the results presented here demonstrate, tumours with the same histologic and genetic characteristics can behave differently in different glucose conditions. As studies move toward the development of clinical applications, research will need to consider another level of complexity—interaction with the systemic environment. The results of this thesis demonstrate pro-tumorigenic roles for both long-term and shortterm exposure to systemic hyperglycemia and implicate common metabolic comorbidities of EOC, particularly diabetes, as significant challenges to address. Can systemic metabolic dysfunction mask cancer diagnosis or monitoring, particularly using FDG-PET? Can it increase cancer aggressiveness and lead to poorer prognoses by providing an unlimited fuel supply? Do standard treatments for diabetes, like insulin or lactate infusions, have detrimental effects by enhancing tumour growth or interfering with cancer treatments? The key findings of this thesis are that: 1. Hyperglycemia promotes EOC independent of insulin; 2. Tumour development ameliorates dysfunctional systemic metabolism; 3. Knockdown of the active glucose transporter SGLT2 promotes EOC spread; 4. Secondary disease predicts death independent of primary tumour size; and 5. Anti-neoplastic effects of metformin are highly glucose-specific. 150 Figure 40: EOC metabolism is a product of cell genotype, the tumour microenvironment, and systemic glucose conditions The metabolic syndrome, diabetes, and EOC The metabolic syndrome is defined by the pathologic triad of hyperglycemia and hyperinsulinemia (T2DM), and obesity. It is a significant and growing population health concern with as much as one third of the population affected. The syndrome has health 151 effects on multiple organs and is related to various vascular and microvascular diseases.198 Its effect as both a risk factor and poor prognostic factor in cancers is undeniable but poorly understood.199 In some studies, ovarian cancer has been linked to the metabolic syndrome and each of its three conditions independently. 178,179 The effects of mitogenic insulin signalling are thought to be the primary drivers of this association. However, insulin-independent mechanisms may also contribute, particularly through energy-sensing pathways and glucotoxic damage. Toxicities of excess glucose could benefit tumour progression by facilitating cellular and genetic damage through the development of an acidic environment, transient hypoxia, oxidative stress, and glycation including the development of advanced glycation end products and their receptors (AGE/RAGE).186,285 Taken together hyperglycemia provides ongoing genomic instability, one of the hallmarks of cancer.43 Dysregulated systemic metabolism can also affect cancer cell metabolism. The aerobic glycolysis in many cancer cells is associated with more aggressive malignancies in vitro.48,121 Highly glycolytic cells demonstrate the Crabtree effect where glucose induces a further shift away from oxidative energy production. Diabetes, particularly T1DM, is associated with a “thrifty” genotype where cells are genetically or epigenetically reprogrammed take up more glucose.286 It is possible that this is a risk factor for cellular transformation or a promotional influence on tumour development. The metabolic syndrome is primarily a consequence of lifestyle and thus understanding its connections to cancer can potentially indicate modifiable risk factors. In ovarian cancer, where the etiology is still poorly understood and treatment of advanced disease 152 is still largely ineffective over the long term, this would be a significant finding. Moreover, researchers have suggested that the effects of diabetes can be extrapolated to all cancer patients as the associated risks may occur within the normoglycemic and insulinemic ranges.184 Diabetes treatment and cancer Treatments for diabetes and cancer can interact in detrimental ways. Antihyperglycemic treatments inducing elevated plasma insulin (sulfonylureas) seem to increase cancer risk but insulin-sensitizers (metformin, thiazolidinediones) seem to reduce cancer risk.242,287,288 Some groups have proposed that the increased risk of cancer in diabetics is not attributable to insulin itself, but rather to the effects of insulin insensitivity on the dysregulation of AMPK signalling or the action of insulin-like growth factor-1 (IGF-1)-cholesterol synthesis pathway.202 On the other hand, patients with diabetes tend to receive less aggressive cancer treatment.289 Diabetes is associated with higher infection rates177 and compared with their nondiabetic counterparts, cancer patients with pre-existing diabetes are approximately 50% more likely to die after surgery.290 This high operative morbidity may limit the number of diabetic patients having comprehensive surgical staging179 and explain why diabetic patients are more often diagnosed with higher tumour stages. 289 153 Coordinated metabolism in the tumour microenvironment Transformed cells are one part of a complex and heterogeneous tumour microenvironment that plays an essential role in cancer progression.114 Our lab has shown that the interaction of transformed ovarian epithelial cells with the ovarian stroma is crucial to the development of highly aggressive tumours in the mouse model described in this thesis.10 The microenvironment, particularly its oxygen levels, also influences metabolism.121 While the Warburg effect describes genetic adaptations of tumour cells, the Crabtree effect (inhibition of oxphos and promotion of glycolysis in high glucose) describes reversible, short term adaptations to changes in energy and oxygen balance which may occur at protein or epigenetic levels. In the 1960s, the Crabtree effect was considered characteristic of cancer cells and part of the malignant transformation.291 Although the Crabtree effect is not often mentioned in contemporary literature, in addition to the Warburg effect it is important to consider this as part of the microenvironment-metabolism interaction.217,292 The reverse Warburg effect demonstrates a central role of reprogrammed cancerassociated fibroblasts (CAFs) in tumour metabolism.116 Similarly, lactate is shared in a metabolic symbiosis between oxic and hypoxic cancer cells within a tumour. 119 The in vitro studies in this thesis show that increased environmental glucose can influence cells to increase their glucose uptake. However, in vivo tumours are poorly perfused tissues. Interestingly, the reverse Warburg effect shows that tumours can enrich their own microenvironment and thus gain some autonomy from systemic circulation and the need for tumour vascularization or angiogenesis.105 This could have implications for the effectiveness of antiangiogenic therapies or chemotherapy delivery to the tumour. In 154 hyperglycemic conditions, tumours are also able to increase glucose uptake by promoting glucose transfer across the capillary walls into the IF, which occurs without the need for glucose transport proteins.214 Glucose can accumulate within the tumour tissue to potentially create a locally hyperglycemic environment, which could explain the ability of passive GLUTs to compensate for lack of active SGLT2-mediated glucose transport (Chapter 3). Intersection of tumour metabolism and systemic metabolism Just as cellular growth occurs within the tumour microenvironment, tumour growth occurs within the larger ecosystem of the host which varies in its own systemic metabolism. In this thesis we hypothesized that high blood glucose levels would promote tumour growth by providing an abundance of energetic fuel. However, the relationship between systemic and tumour glucose control is reciprocal and cancer itself can drive changes in systemic metabolism. We saw that tumours in our animal model actually improved the diabetes of both STZ and Akt2 KO mice. In T1DM mice lacking insulin, the presence of a tumour improved glucose tolerance (Figure 6). In hyperinsulinemic Akt2 KO mice, tumours improved insulin sensitivity (Figure 8A and B). In fact, tumours appeared to be as effective as metformin at normalizing glucose tolerance in T2DM mice (Figure 37D). The high glucose demands of tumour tissue might suggest that it acts as a glucose sink and improvements in systemic glucose would be due to a large tumour mass. However, the tumours in the chronically diabetic STZ mice with improved glucose tolerance were 155 smaller than tumours in control mice (Figure 4A). This could indicate that the tumour is influencing systemic glucose indirectly through secreted factors in the blood. Hypoglycemia has been noted in many cancer patients and is thought to be due to a combination of cachexia, renal and hepatic impairment, excessive glucose consumption or decreased glucose production293 which can be resolved with removal of the tumour.294 However, the body is able to compensate for much of the tumour’s effect, in some cases overcompensating,295–297 by increasing glycogenolysis and gluconeogenesis from non-carbohydrate sources212,298 This compensation at the site of the liver could lead to relative hyperglycemia in the hepatic veins and might contribute to the fact that the liver is such a common site of metastasis (Figure 27A). Similarly, we saw that the intestines were a major site of metastasis. Aside from being well perfused, metastatic cells in this location may co-opt dietary glucose as it is absorbed. High blood glucose, or an associated hyperglycemic peritoneal fluid, could promote the survival of circulating tumour cells with metastatic potential. If high blood glucose is cancer-promoting, then it might be expected that haematological malignancies would be most acutely accelerated in diabetic conditions, however there is no published data looking at these effects. Diabetes has similar influences on the body as cancer: cachexia, heightened gluconeogenesis concomitant with an increase in liver mass, and dysregulation of insulin and glucagon levels. At a cellular level diabetes induces similar host compensation: impaired oxphos leads to increased glucose tolerance, reduced fat mass, and increased insulin sensitivity, which oppose the progression of the metabolic 156 syndrome.299 As a comorbidity with EOC, diabetes may accelerate these cancer-driven changes in the host ecosystem. Glucose transport and diagnostic potential These studies demonstrated that glucose enters cancer cells through both GLUT and SGLT. It is possible that PET scans using FDG are only accounting for a portion of glucose uptake, underestimating the number and metabolic activity of malignant lesions. A first generation SGLT-specific tracer, alpha-methyl-4-deoxy-4-[18F]fluoro-Dglucopyranoside (Me4FDG) has been developed.130 Because SGLT-mediated glucose transport is reliant on the extracellular sodium concentration, using multi-modal uptake imaging combining FDG + Me4FDG + Na+ could add power to PET scanning in diagnosis and treatment monitoring.300–303 Implications for EOC treatment The best available treatment tools against ovarian cancer are surgery304, imaging and monitoring blood levels of CA-125305–309, and platinum-based chemotherapies310, all of which are confounded by hyperglycemia. In addition to the dysregulation of systemic metabolism caused by the tumour itself, many standard cancer treatments induce hyperglycemia. Total parenteral nutrition, tube feeding, steroids and glucocorticoids are often used in oncology and have been shown to result in hyperglycemia.177,311 Intravenous solutions that contain lactate (Ringer’s, 157 Hartmann’s) are also often given to cancer patients and, given the tumour’s ability to use lactate as a fuel, may in fact be detrimental.105 Even in previously diabetic patients, hyperglycemic treatment varies widely. In many cases, comprehensive glucose management may not be included as part of an overall treatment plan for the cancer,312 partly because it can be particularly difficult to both aggressively monitor blood glucose and maintain quality of life during cancer treatment.313 Since blood glucose can often be managed effectively through diet, nutrition could become an important part of EOC treatment. Specific low-carbohydrate diets have been suggested as a means to starve cancer cells of glucose, and studies using ketogenic diets have shown potential anticancer benefits.314 However, ketones have recently been shown to actually fuel cancer in part because of their contributions to the “reverse Warburg” effect. The ability of tumours to use ketones as fuel has even been suggested to partly explain the diabetescancer connection.105 Taken together, any modifications to systemic fuel availability should be taken into consideration as potentially confounding factors when treating ovarian cancer patients. Study Limitations One of the most significant limitations of cancer metabolic research in vitro is that cell culture conditions are hyperglycemic and hyperoxic,64 both of which directly oppose the usual conditions of the tumour microenvironment. The phenotypic differences between ID8-6 and ID8-25 cells clearly demonstrated that high glucose medium influences cell robustness and metabolism. 158 Through the use of both Type 1 and Type 2 diabetic animal models, we were able to separate some of the effects of insulin from those of glucose. However, the reductive approach we took did not consider other contributors to glucose regulation, particularly other hormonal factors.315 Furthermore, we did not consider the effects of inflammation, immunity and angiogenesis which are inextricably linked to both metabolism and tumour growth. Limitations of animal models The Akt2 KO model was originally used because of its non-obese type 2 diabetic phenotype, however it appears that under some conditions, Akt2 KO can also influence tumour development, potentially confounding our results.316 In addition, we were unable to reduce systemic blood glucose with metformin in these mice and therefore could not directly test the hypothesis that normalizing blood glucose could reduce tumour growth in diabetic environments. This lack of impact on blood glucose could be due to opposing effects of the Akt2 KO and metformin. Akt2 plays an important role in the exocytosis of intracellular GLUT4 to the cell membrane to facilitate insulin-dependent glucose uptake.317 Eliminating Akt2 expression in mice results in insulin insensitivity and consequently hyperglycemia. On the other hand, metformin achieves most of its antidiabetic effects by increasing glucose uptake into skeletal muscle. Metformin decreases the endocytosis of GLUT4 transporters from the cell membrane back into the cytosol.318 The inactivation of Akt2-mediated GLUT4 trafficking antagonizes metformin’s ability to maintain transporter expression and increase glucose consumption in cells, which would limit its ability to reduce blood glucose in Akt2 KO mice. 159 Another limitation related to in vivo work was the difficulty in characterizing secondary disease, which we found to be an essential measure of morbidity. In chronically diabetic mice, we saw significant reductions in overall survival compared to normoglycemic animals together with significantly smaller tumours which suggested a large contribution of secondary disease. In addition, mice with SGLT2-deficient tumours presented with many metastatic lesions that were strongly associated with poor survival. In women metastases lead to death because of their physical affect vital organs, but the secondary lesions in our model were too small to have this same influence. “Secondary disease” includes humoral and intraperitoneal factors that are not accounted for in our scoring method. Conclusions Collectively, the data presented in this thesis indicate that altered tumour metabolism is much broader than the Warburg effect. The effects of systemic metabolic comorbidities such as diabetes can confound EOC diagnosis, treatment and overall survival through fundamental changes in tumour biology.209 Antidiabetic pharmaceuticals have great potential as adjuvants to cancer treatment and because altered glucose homeostasis is common in cancer patients, these therapies have wide applicability to normoglycemic patients. Moreover, the identification of SGLT2 as a powerful tumour suppressor opens exciting possibilities for improved screening and drug targeting. 160 REFERENCES 1. Navaneelan, T. Trends in the incidence and mortality of female reproductive system cancers. Statistics Canada, catalogue no. 82–624–X (2015). 2. Canadian Cancer Society. Canadian Cancer Statistics Special topic : Predictions of the future burden of cancer in Canada. 1–151 (2015). 3. Bast, R. C., Hennessy, B. & Mills, G. B. The biology of ovarian cancer: new opportunities for translation. Nat. Rev. Cancer 9, 415–28 (2009). 4. Boyd, J. & Rubin, S. C. Hereditary ovarian cancer: molecular genetics and clinical implications. Gynecol. Oncol. 64, 196–206 (1997). 5. Kurman, R. J., Carcangiu, M. & Herrington, C. World Health Organisation Classification of Tumours of the Female Reproductive Organs. International Agency for Research on Cancer 4th ed., (2014). 6. Devouassoux-Shisheboran, M. & Genestie, C. Pathobiology of ovarian carcinomas. Chin. J. Cancer 34, 50–5 (2015). 7. Karst, A. M. & Drapkin, R. Ovarian cancer pathogenesis: a model in evolution. J. Oncol. 2010, 932371 (2010). 8. Kauff, N. D. et al. Risk-reducing salpingo-oophorectomy in women with a BRCA1 or BRCA2 mutation. N. Engl. J. Med. 346, 1609–15 (2002). 9. Landen, C. N., Birrer, M. J. & Sood, A. K. Early events in the pathogenesis of epithelial ovarian cancer. J. Clin. Oncol. 26, 995–1005 (2008). 10. Greenaway, J., Moorehead, R., Shaw, P. & Petrik, J. Epithelial-stromal interaction increases cell proliferation, survival and tumorigenicity in a mouse model of human epithelial ovarian cancer. Gynecol. Oncol. 108, 385–94 (2008). 11. Risch, H. A. Hormonal etiology of epithelial ovarian cancer, with a hypothesis concerning the role of androgens and progesterone. J. Natl. Cancer Inst. 90, 1774–86 (1998). 12. Choi, J.-H., Wong, A. S. T., Huang, H.-F. & Leung, P. C. K. Gonadotropins and ovarian cancer. Endocr. Rev. 28, 440–61 (2007). 13. Ness, R. B. & Cottreau, C. Possible role of ovarian epithelial inflammation in ovarian cancer. J. Natl. Cancer Inst. 91, 1459–67 (1999). 14. Auersperg, N., Wong, a S., Choi, K. C., Kang, S. K. & Leung, P. C. Ovarian surface epithelium: biology, endocrinology, and pathology. Endocr. Rev. 22, 255– 88 (2001). 161 15. Holschneider, C. H. & Berek, J. S. Ovarian cancer: epidemiology, biology, and prognostic factors. Semin. Surg. Oncol. 19, 3–10 (2000). 16. Dubeau, L. & Drapkin, R. Coming into focus: the nonovarian origins of ovarian cancer. Ann. Oncol. 24, viii28–viii35 (2013). 17. Kurman, R. J. & Shih, I.-M. Pathogenesis of ovarian cancer: lessons from morphology and molecular biology and their clinical implications. Int. J. Gynecol. Pathol. 27, 151–60 (2008). 18. Piek, J. M. et al. Dysplastic changes in prophylactically removed Fallopian tubes of women predisposed to developing ovarian cancer. J. Pathol. 195, 451–6 (2001). 19. Medeiros, F. et al. The tubal fimbria is a preferred site for early adenocarcinoma in women with familial ovarian cancer syndrome. Am. J. Surg. Pathol. 30, 230–6 (2006). 20. Kindelberger, D. W. et al. Intraepithelial Carcinoma of the Fimbria and Pelvic Serous Carcinoma: Evidence for a Causal Relationship. Am. J. Surg. Pathol. 31, 161–169 (2007). 21. Dubeau, L. The cell of origin of ovarian epithelial tumours. Lancet Oncol. 9, 1191– 1197 (2008). 22. Kim, J. et al. High-grade serous ovarian cancer arises from fallopian tube in a mouse model. Proceedings of the National Academy of Sciences 109, 3921–3926 (2012). 23. Bankhead, C. R. et al. Identifying symptoms of ovarian cancer: a qualitative and quantitative study. BJOG 115, 1008–14 (2008). 24. Goff, B. A., Mandel, L. S., Melancon, C. H. & Muntz, H. G. Frequency of symptoms of ovarian cancer in women presenting to primary care clinics. JAMA 291, 2705–12 (2004). 25. National Cancer Institute. Surveillance Epidemiology and End Results (SEER). (2012). 26. Prat, J. FIGO Committee on Gynecologic Oncology. Staging classification for cancer of the ovary, fallopian tube, and peritoneum. Int. J. Gynecol. Obstet. 124, 1–5 (2014). 27. Hynninen, J. et al. FDG PET/CT in staging of advanced epithelial ovarian cancer: Frequency of supradiaphragmatic lymph node metastasis challenges the traditional pattern of disease spread. Gynecol. Oncol. 126, 64–68 (2012). 28. Ahmed, N. & Stenvers, K. L. Getting to know ovarian cancer ascites: opportunities 162 for targeted therapy-based translational research. Front. Oncol. 3, 256 (2013). 29. Jayson, G. C., Kohn, E. C., Kitchener, H. C. & Ledermann, J. A. Ovarian cancer. Lancet 384, 1376–1388 (2014). 30. du Bois, A. et al. Role of surgical outcome as prognostic factor in advanced epithelial ovarian cancer: a combined exploratory analysis of 3 prospectively randomized phase 3 multicenter trials: by the Arbeitsgemeinschaft Gynaekologische Onkologie Studiengruppe Ovarialkarzin. Cancer 115, 1234–44 (2009). 31. Kurman, R. J., Visvanathan, K., Roden, R., Wu, T. C. & Shih, I.-M. Early detection and treatment of ovarian cancer: shifting from early stage to minimal volume of disease based on a new model of carcinogenesis. Am. J. Obstet. Gynecol. 198, 351–6 (2008). 32. King, M.-C., Marks, J. H. & Mandell, J. B. Breast and ovarian cancer risks due to inherited mutations in BRCA1 and BRCA2. Science 302, 643–6 (2003). 33. Kyriazi, S., Kaye, S. B. & deSouza, N. M. Imaging ovarian cancer and peritoneal metastases--current and emerging techniques. Nat. Rev. Clin. Oncol. 7, 381–93 (2010). 34. Gordon, A. N. et al. Recurrent epithelial ovarian carcinoma: a randomized phase III study of pegylated liposomal doxorubicin versus topotecan. J. Clin. Oncol. 19, 3312–22 (2001). 35. Griffiths, R. W. et al. Outcomes After Multiple Lines of Chemotherapy for Platinum-Resistant Epithelial Cancers of the Ovary, Peritoneum, and Fallopian Tube. Int. J. Gynecol. Cancer 21, 58–65 (2011). 36. Vaughan, S. et al. Rethinking ovarian cancer: recommendations for improving outcomes. Nat. Rev. Cancer 11, 719–25 (2011). 37. Guyton, A. C. & Hall, J. E. Guyton and Hall Textbook of Medical Physiology. (Saunders Elsevier, 2011). 38. Voet, D. & Voet, J. G. Biochemistry. (John Wiley & Sons, Inc, 2004). 39. Warburg, O., K, P. & E, N. Ueber den stoffwechsel der tumoren. Biochem Z 152, 319–344 (1924). 40. Ganapathy, V., Thangaraju, M. & Prasad, P. D. Nutrient transporters in cancer: Relevance to Warburg hypothesis and beyond. Pharmacol. Ther. 121, 29–40 (2009). 41. Warburg, O. On the Origin of Cancer Cells. Science (80-. ). 123, 309–314 (1956). 163 42. Funes, J. M. et al. Transformation of human mesenchymal stem cells increases their dependency on oxidative phosphorylation for energy production. Proc. Natl. Acad. Sci. U. S. A. 104, 6223–8 (2007). 43. Hanahan, D. & Weinberg, R. A. Hallmarks of cancer: the next generation. Cell 144, 646–74 (2011). 44. Kim, J. & Dang, C. V. Cancer’s molecular sweet tooth and the Warburg effect. Cancer Res. 66, 8927–30 (2006). 45. Chance, B. & Hess, B. On the control of metabolism in ascites tumor cell suspensions. Ann. N. Y. Acad. Sci. 63, 1008–16 (1956). 46. Chance, B. & Castor, L. N. Some Patterns of the Respiratory Pigments of Ascites Tumors of Mice. Science 116, 200–2 (1952). 47. Weinhouse, S. On respiratory impairment in cancer cells. Science 124, 267–9 (1956). 48. Greiner, E. F., Guppy, M. & Brand, K. Glucose is essential for proliferation and the glycolytic enzyme induction that provokes a transition to glycolytic energy production. J. Biol. Chem. 269, 31484–90 (1994). 49. Koppenol, W. H., Bounds, P. L. & Dang, C. V. Otto Warburg’s contributions to current concepts of cancer metabolism. Nat. Rev. Cancer 11, 325–337 (2011). 50. Kroemer, G. & Pouyssegur, J. Tumor cell metabolism: cancer’s Achilles' heel. Cancer Cell 13, 472–82 (2008). 51. Cairns, R. A., Harris, I. S. & Mak, T. W. Regulation of cancer cell metabolism. Nature reviews. Cancer 11, 85–95 (2011). 52. Pedersen, P. L. The cancer cell’s ‘power plants’ as promising therapeutic targets: an overview. J. Bioenerg. Biomembr. 39, 1–12 (2007). 53. Modica-Napolitano, J. S., Kulawiec, M. & Singh, K. K. Mitochondria and human cancer. Curr. Mol. Med. 7, 121–31 (2007). 54. Eboli, M. L., Paradies, G., Galeotti, T. & Papa, S. Pyruvate transport in tumourcell mitochondria. Biochim. Biophys. Acta 460, 183–7 (1977). 55. Pelicano, H. et al. Mitochondrial respiration defects in cancer cells cause activation of Akt survival pathway through a redox-mediated mechanism. J. Cell Biol. 175, 913–23 (2006). 56. Bellance, N. et al. Bioenergetics of lung tumors: Alteration of mitochondrial biogenesis and respiratory capacity. Int. J. Biochem. Cell Biol. 41, 2566–2577 (2009). 164 57. Desouki, M. M., Kulawiec, M., Bansal, S., Das, G. M. & Singh, K. K. Cross talk between mitochondria and superoxide generating NADPH oxidase in breast and ovarian tumors. Cancer Biol. Ther. 4, 1367–73 (2005). 58. Pollard, P. J. Accumulation of Krebs cycle intermediates and over-expression of HIF1 in tumours which result from germline FH and SDH mutations. Hum. Mol. Genet. 14, 2231–2239 (2005). 59. Dang, L. et al. Cancer-associated IDH1 mutations produce 2-hydroxyglutarate. Nature 465, 966 (2010). 60. Gottlieb, E. & Tomlinson, I. P. M. Mitochondrial tumour suppressors: a genetic and biochemical update. Nat. Rev. Cancer 5, 857–66 (2005). 61. Lin, C.-C. et al. Loss of the respiratory enzyme citrate synthase directly links the Warburg effect to tumor malignancy. Sci. Rep. 2, 785 (2012). 62. Schulz, T. J. et al. Induction of oxidative metabolism by mitochondrial frataxin inhibits cancer growth: Otto Warburg revisited. J. Biol. Chem. 281, 977–81 (2006). 63. Gatenby, R. a & Gillies, R. J. Why do cancers have high aerobic glycolysis? Nat. Rev. Cancer 4, 891–9 (2004). 64. Zu, X. L. & Guppy, M. Cancer metabolism: facts, fantasy, and fiction☆. Biochem. Biophys. Res. Commun. 313, 459–465 (2004). 65. Hockel, M. & Vaupel, P. Tumor Hypoxia: Definitions and Current Clinical, Biologic, and Molecular Aspects. JNCI J. Natl. Cancer Inst. 93, 266–276 (2001). 66. Semenza, G. L. Targeting HIF-1 for cancer therapy. Nat. Rev. Cancer 3, 721–732 (2003). 67. Goodwin, M. L., Gladden, L. B., Nijsten, M. W. N. & Jones, K. B. Lactate and Cancer: Revisiting the Warburg Effect in an Era of Lactate Shuttling. Front. Nutr. 1, 2014–2016 (2015). 68. Walenta, S. & Mueller-Klieser, W. F. Lactate: mirror and motor of tumor malignancy. Semin. Radiat. Oncol. 14, 267–74 (2004). 69. Choi, S. Y. C., Collins, C. C., Gout, P. W. & Wang, Y. Cancer-generated lactic acid: a regulatory, immunosuppressive metabolite? J. Pathol. 230, 350–5 (2013). 70. Morita, T., Nagaki, T., Fukuda, I. & Okumura, K. Clastogenicity of low pH to various cultured mammalian cells. Mutat. Res. 268, 297–305 (1992). 71. Yuan, J., Narayanan, L., Rockwell, S. & Glazer, P. M. Diminished DNA repair and elevated mutagenesis in mammalian cells exposed to hypoxia and low pH. Cancer Res. 60, 4372–6 (2000). 165 72. Raghunand, N., Mahoney, B., van Sluis, R., Baggett, B. & Gillies, R. J. Acute metabolic alkalosis enhances response of C3H mouse mammary tumors to the weak base mitoxantrone. Neoplasia 3, 227–35 73. Martínez-Zaguilán, R. et al. Acidic pH enhances the invasive behavior of human melanoma cells. Clin. Exp. Metastasis 14, 176–86 (1996). 74. Gatenby, R. A. & Gawlinski, E. T. The glycolytic phenotype in carcinogenesis and tumor invasion: insights through mathematical models. Cancer Res. 63, 3847–54 (2003). 75. Gatenby, R. A. & Gawlinski, E. T. A reaction-diffusion model of cancer invasion. Cancer Res. 56, 5745–53 (1996). 76. Smallbone, K., Gavaghan, D. J., Gatenby, R. A. & Maini, P. K. The role of acidity in solid tumour growth and invasion. J. Theor. Biol. 235, 476–84 (2005). 77. Xu, H. N. et al. Is Higher Lactate an Indicator of Tumor Metastatic Risk? A Pilot MRS Study Using Hyperpolarized (13)C-Pyruvate. Acad. Radiol. 21, 223–31 (2014). 78. Arora, K. K. & Pedersen, P. L. Functional significance of mitochondrial bound hexokinase in tumor cell metabolism. Evidence for preferential phosphorylation of glucose by intramitochondrially generated ATP. J. Biol. Chem. 263, 17422–8 (1988). 79. Rastogi, S., Banerjee, S., Chellappan, S. & Simon, G. R. Glut-1 antibodies induce growth arrest and apoptosis in human cancer cell lines. Cancer Lett. 257, 244– 251 (2007). 80. Friedrich, M. J. Researchers aim to stop tumor growth by shutting off cancer’s fuel supply. JAMA 303, 1021–2 (2010). 81. Deberardinis, R. J., Sayed, N., Ditsworth, D. & Thompson, C. B. Brick by brick: metabolism and tumor cell growth. Curr. Opin. Genet. Dev. 18, 54–61 (2008). 82. Jang, M., Kim, S. S. & Lee, J. Cancer cell metabolism: implications for therapeutic targets. Exp. Mol. Med. 45, e45 (2013). 83. Ward, P. S. & Thompson, C. B. Metabolic reprogramming: a cancer hallmark even warburg did not anticipate. Cancer Cell 21, 297–308 (2012). 84. Venuta, S. & Rubin, H. Effects of glucose starvation on normal and rous sarcoma virus-transformed chick cells. J. Natl. Cancer Inst. 54, 395–400 (1975). 85. Hatanaka, M., Huebner, R. J. & Gilden, R. V. Alterations in the characteristics of sugar uptake by mouse cells transformed by murine sarcoma viruses. J. Natl. Cancer Inst. 43, 1091–6 (1969). 166 86. Ramanathan, A., Wang, C. & Schreiber, S. L. Perturbational profiling of a cell-line model of tumorigenesis by using metabolic measurements. Proc. Natl. Acad. Sci. U. S. A. 102, 5992–7 (2005). 87. Jiang, P. et al. p53 regulates biosynthesis through direct inactivation of glucose-6phosphate dehydrogenase. Nat. Cell Biol. 13, 310–6 (2011). 88. Goldstein, I. et al. P53 Promotes the Expression of Gluconeogenesis-Related Genes and Enhances Hepatic Glucose Production. Cancer Metab. 1, 9 (2013). 89. Elstrom, R. L. et al. Akt stimulates aerobic glycolysis in cancer cells. Cancer Res. 64, 3892–9 (2004). 90. Robey, R. B. & Hay, N. Is Akt the ‘Warburg kinase’?-Akt-energy metabolism interactions and oncogenesis. Semin. Cancer Biol. 19, 25–31 (2009). 91. Christofk, H. R. et al. The M2 splice isoform of pyruvate kinase is important for cancer metabolism and tumour growth. Nature 452, 230–3 (2008). 92. Shanmugam, M., McBrayer, S. K. & Rosen, S. T. Targeting the Warburg effect in hematological malignancies: from PET to therapy. Curr. Opin. Oncol. 21, 531–6 (2009). 93. Schulz, J. et al. Regulation of anaerobic glycolysis in Ehrlich ascites tumour cells. Acta Biol. Med. Ger. 36, 1379–91 (1977). 94. Mathupala, S. P., Rempel, A. & Pedersen, P. L. Aberrant glycolytic metabolism of cancer cells: a remarkable coordination of genetic, transcriptional, posttranslational, and mutational events that lead to a critical role for type II hexokinase. J. Bioenerg. Biomembr. 29, 339–43 (1997). 95. Rivenzon-Segal, D., Boldin-Adamsky, S., Seger, D., Seger, R. & Degani, H. Glycolysis and glucose transporter 1 as markers of response to hormonal therapy in breast cancer. Int. J. Cancer 107, 177–82 (2003). 96. Artemov, D., Bhujwalla, Z. M., Pilatus, U. & Glickson, J. D. Two-compartment model for determination of glycolytic rates of solid tumors by in vivo 13C NMR spectroscopy. NMR Biomed. 11, 395–404 (1998). 97. Wolf, A. et al. Hexokinase 2 is a key mediator of aerobic glycolysis and promotes tumor growth in human glioblastoma multiforme. J. Exp. Med. 208, 313–26 (2011). 98. Mathupala, S. P., Ko, Y. H. & Pedersen, P. L. Hexokinase-2 bound to mitochondria: cancer’s stygian link to the ‘Warburg Effect’ and a pivotal target for effective therapy. Semin. Cancer Biol. 19, 17–24 (2009). 99. Pedersen, P. L. Warburg, me and Hexokinase 2: Multiple discoveries of key 167 molecular events underlying one of cancers’ most common phenotypes, the ‘Warburg Effect’, i.e., elevated glycolysis in the presence of oxygen. J. Bioenerg. Biomembr. 39, 211–22 (2007). 100. John, S., Weiss, J. N. & Ribalet, B. Subcellular localization of hexokinases I and II directs the metabolic fate of glucose. PLoS One 6, e17674 (2011). 101. Netti, P. A., Baxter, L. T., Boucher, Y., Skalak, R. & Jain, R. K. Time-dependent behavior of interstitial fluid pressure in solid tumors: implications for drug delivery. Cancer Res. 55, 5451–8 (1995). 102. Boucher, Y. & Jain, R. K. Microvascular pressure is the principal driving force for interstitial hypertension in solid tumors: implications for vascular collapse. Cancer Res. 52, 5110–4 (1992). 103. Rutz, H. P. A biophysical basis of enhanced interstitial fluid pressure in tumors. Med. Hypotheses 53, 526–529 (1999). 104. Samudio, I. et al. Pharmacologic inhibition of fatty acid oxidation sensitizes human leukemia cells to apoptosis induction. J. Clin. Invest. 120, 142–56 (2010). 105. Bonuccelli, G. et al. Ketones and lactate ‘fuel’ tumor growth and metastasis: Evidence that epithelial cancer cells use oxidative mitochondrial metabolism. Cell Cycle 9, 3506–3514 (2010). 106. Wise, D. R. & Thompson, C. B. Glutamine addiction: a new therapeutic target in cancer. Trends Biochem. Sci. 35, 427–33 (2010). 107. Buzzai, M. et al. The glucose dependence of Akt-transformed cells can be reversed by pharmacologic activation of fatty acid beta-oxidation. Oncogene 24, 4165–73 (2005). 108. Rodríguez-Enríquez, S. et al. Oxidative phosphorylation is impaired by prolonged hypoxia in breast and possibly in cervix carcinoma. Int. J. Biochem. Cell Biol. 42, 1744–1751 (2010). 109. Warburg, O., Wind, F. & Negelein, E. THE METABOLISM OF TUMORS IN THE BODY. J. Gen. Physiol. 8, 519–30 (1927). 110. Jose, C., Bellance, N. & Rossignol, R. Choosing between glycolysis and oxidative phosphorylation: A tumor’s dilemma? Biochim. Biophys. Acta 1807, 552–61 (2011). 111. Anderson, A. S., Roberts, P. C., Frisard, M. I., Hulver, M. W. & Schmelz, E. M. Ovarian tumor-initiating cells display a flexible metabolism. Exp. Cell Res. 328, 44–57 (2014). 112. Griguer, C. E., Oliva, C. R. & Gillespie, G. Y. Glucose metabolism heterogeneity 168 in human and mouse malignant glioma cell lines. J. Neurooncol. 74, 123–33 (2005). 113. Berridge, M. V, Herst, P. M. & Tan, A. S. Metabolic flexibility and cell hierarchy in metastatic cancer. Mitochondrion 10, 584–8 (2010). 114. Bissell, M. J. & Radisky, D. Putting tumours in context. Nat. Rev. Cancer 1, 46–54 (2001). 115. Yoshida, G. J. Metabolic reprogramming: the emerging concept and associated therapeutic strategies. J. Exp. Clin. Cancer Res. 34, 111 (2015). 116. Pavlides, S. et al. The reverse Warburg effect: Aerobic glycolysis in cancer associated fibroblasts and the tumor stroma. Cell Cycle 8, 3984–4001 (2009). 117. Martinez-Outschoorn, U. E., Lisanti, M. P. & Sotgia, F. Catabolic CancerAssociated Fibroblasts (CAFs) Transfer Energy and Biomass to Anabolic Cancer Cells, Fueling Tumor Growth. Semin. Cancer Biol. (2014). 118. Fiaschi, T. et al. Reciprocal metabolic reprogramming through lactate shuttle coordinately influences tumor-stroma interplay. Cancer Res. 72, 5130–40 (2012). 119. Sonveaux, P. et al. Targeting lactate-fueled respiration selectively kills hypoxic tumor cells in mice. J. Clin. Invest. 118, 3930–42 (2008). 120. Semenza, G. L. Tumor metabolism: cancer cells give and take lactate. J. Clin. Invest. 118, 3835–7 (2008). 121. Crabtree, H. G. Observations on the carbohydrate metabolism of tumours. Biochem. J. 23, 536–45 (1929). 122. Suchorolski, M. T., Paulson, T. G., Sanchez, C. A., Hockenbery, D. & Reid, B. J. Warburg and Crabtree effects in premalignant Barrett’s esophagus cell lines with active mitochondria. PLoS One 8, e56884 (2013). 123. Bouché, C., Serdy, S., Kahn, C. R. & Goldfine, A. B. The cellular fate of glucose and its relevance in type 2 diabetes. Endocr. Rev. 25, 807–830 (2004). 124. Szablewski, L. Expression of glucose transporters in cancers. Biochim. Biophys. Acta 1835, 164–9 (2013). 125. Yamamoto, T. et al. Over-expression of facilitative glucose transporter genes in human cancer. Biochem. Biophys. Res. Commun. 170, 223–30 (1990). 126. Rudlowski, C. et al. GLUT1 mRNA and protein expression in ovarian borderline tumors and cancer. Oncology 66, 404–410 (2004). 127. Semaan, A. et al. Expression of GLUT-1 in epithelial ovarian carcinoma: 169 correlation with tumor cell proliferation, angiogenesis, survival and ability to predict optimal cytoreduction. Gynecol. Oncol. 121, 181–6 (2011). 128. Kalir, T. et al. Immunohistochemical staining of GLUT1 in benign, borderline, and malignant ovarian epithelia. Cancer 94, 1078–1082 (2002). 129. Noguchi, Y. et al. Suppression of facilitative glucose transporter 1 mRNA can suppress tumor growth. Cancer Lett. 154, 175–82 (2000). 130. Wright, E. M., Loo, D. D. F. & Hirayama, B. A. Biology of human sodium glucose transporters. Physiol. Rev. 91, 733–794 (2011). 131. Wright, E. M., Loo, D. D. F., Hirayama, B. a & Turk, E. Surprising versatility of Na+-glucose cotransporters: SLC5. Physiology (Bethesda). 19, 370–376 (2004). 132. Narendran, P. & Saeed, M. Dapagliflozin for the treatment of type 2 diabetes: a review of the literature. Drug Des. Devel. Ther. 8, 2493 (2014). 133. Tahara, A., Takasu, T., Yokono, M., Imamura, M. & Kurosaki, E. Effects of the combination of SGLT2 selective inhibitor ipragliflozin and various antidiabetic drugs in type 2 diabetic mice. Arch. Pharm. Res. (2015). doi:10.1007/s12272-0150621-8 134. Yu, A. S. et al. Regional distribution of SGLT activity in rat brain in vivo. Am. J. Physiol. Cell Physiol. 304, C240–7 (2013). 135. Yu, L. C. H., Flynn, A. N., Turner, J. R. & Buret, A. G. SGLT-1-mediated glucose uptake protects intestinal epithelial cells against LPS-induced apoptosis and barrier defects: a novel cellular rescue mechanism? FASEB J. 19, 1822–35 (2005). 136. Banerjee, S. K., McGaffin, K. R., Pastor-Soler, N. M. & Ahmad, F. SGLT1 is a novel cardiac glucose transporter that is perturbed in disease states. Cardiovasc. Res. 84, 111–118 (2009). 137. Barcelona, S., Menegaz, D. & Diez-Sampedro, A. Mouse SGLT3a generates proton-activated currents but does not transport sugar. AJP Cell Physiol. 302, C1073–C1082 (2012). 138. Balon, T. W. SGLT and GLUT: are they teammates? Focus on ‘Mouse SGLT3a generates proton-activated currents but does not transport sugar’. Am. J. Physiol. Cell Physiol. 302, C1071–2 (2012). 139. Diez-Sampedro, A. et al. A glucose sensor hiding in a family of transporters. Proc. Natl. Acad. Sci. 100, 11753–11758 (2003). 140. Bianchi, L. & Díez-Sampedro, A. A single amino acid change converts the sugar sensor SGLT3 into a sugar transporter. PLoS One 5, (2010). 170 141. Wright, E. M., Hirsch, J. R., Loo, D. D. & Zampighi, G. a. Regulation of Na+/glucose cotransporters. J. Exp. Biol. 200, 287–93 (1997). 142. Sakar, Y. et al. Metformin-induced regulation of the intestinal d-glucose transporters. J. Physiol. Pharmacol. 61, 301–307 (2010). 143. Sopjani, M. et al. Regulation of Na+-coupled glucose carrier SGLT1 by AMPactivated protein kinase. Mol. Membr. Biol. 27, 137–44 (2010). 144. Yamazaki, Y., Ogihara, S., Harada, S. & Tokuyama, S. Activation of cerebral sodium-glucose transporter type 1 function mediated by post-ischemic hyperglycemia exacerbates the development of cerebral ischemia. Neuroscience 310, 674–85 (2015). 145. Weihua, Z. et al. Survival of cancer cells is maintained by EGFR independent of its kinase activity. Cancer Cell 13, 385–93 (2008). 146. Wright, E. M., Hirayama, B. A. & Loo, D. F. Active sugar transport in health and disease. J. Intern. Med. 261, 32–43 (2007). 147. Kothinti, R. K., Blodgett, A. B., North, P. E., Roman, R. J. & Tabatabai, N. M. A novel SGLT is expressed in the human kidney. Eur. J. Pharmacol. 690, 77–83 (2012). 148. Sasseville, L. J., Cuervo, J. E., Lapointe, J.-Y. & Noskov, S. Y. The structural pathway for water permeation through sodium-glucose cotransporters. Biophys. J. 101, 1887–95 (2011). 149. Panayotova-Heiermann, M. & Wright, E. M. Mapping the urea channel through the rabbit Na(+)-glucose cotransporter SGLT1. J. Physiol. 535, 419–25 (2001). 150. Hirschhorn, N. & Greenough, W. B. Progress in oral rehydration therapy. Sci. Am. 264, 50–6 (1991). 151. Yang, M. & Brackenbury, W. J. Membrane potential and cancer progression. Front. Physiol. 4, 185 (2013). 152. Blodgett, T. M., Meltzer, C. C. & Townsend, D. W. PET/CT: form and function. Radiology 242, 360–85 (2007). 153. Pimlott, S. L. & Sutherland, A. Molecular tracers for the PET and SPECT imaging of disease. Chem. Soc. Rev. 40, 149–162 (2011). 154. Kitajima, K., Ebina, Y. & Sugimura, K. Present and future role of FDG-PET/CT imaging in the management of gynecologic malignancies. Jpn J Radiol 32, 313– 323 (2014). 155. Gambhir, S. S. Molecular imaging of cancer with positron emission tomography. 171 Nat. Rev. Cancer 2, 683–93 (2002). 156. Kubota, R. et al. Intratumoral distribution of fluorine-18-fluorodeoxyglucose in vivo: high accumulation in macrophages and granulation tissues studied by microautoradiography. J. Nucl. Med. 33, 1972–80 (1992). 157. Som, P. et al. A fluorinated glucose analog, 2-fluoro-2-deoxy-D-glucose (F-18): nontoxic tracer for rapid tumor detection. J. Nucl. Med. 21, 670–675 (1980). 158. Smith, T. a. The rate-limiting step for tumor [18F]fluoro-2-deoxy-D-glucose (FDG) incorporation. Nucl. Med. Biol. 28, 1–4 (2001). 159. Prakash, P., Cronin, C. G. & Blake, M. A. Role of PET/CT in Ovarian Cancer. American Roentgen Ray Society W464–W470 (2009). at <http://www.ajronline.org/doi/pdf/10.2214/AJR.09.3843> 160. Steenkamp, D. W., McDonnell, M. E. & Meibom, S. Metformin may be associated with false-negative cancer detection in the gastrointestinal tract on PET/CT. Endocr. Pract. 20, 1079–83 (2014). 161. Zhu, A., Lee, D. & Shim, H. Metabolic positron emission tomography imaging in cancer detection and therapy response. Semin. Oncol. 38, 55–69 (2011). 162. Ryu, J. S., Choi, N. C., Fischman, A. J., Lynch, T. J. & Mathisen, D. J. FDG-PET in staging and restaging non-small cell lung cancer after neoadjuvant chemoradiotherapy: correlation with histopathology. Lung Cancer 35, 179–87 (2002). 163. Alavi, A. et al. Positron emission tomography imaging in nonmalignant thoracic disorders. Semin. Nucl. Med. 32, 293–321 (2002). 164. Cheng, G. et al. Dynamic changes of FDG uptake and clearance in normal tissues. Mol. Imaging Biol. 15, 345–52 (2013). 165. Kostakoglu, L., Agress, H. & Goldsmith, S. J. Clinical role of FDG PET in evaluation of cancer patients. Radiographics 23, 315–40; quiz 533 (2003). 166. Gaeta, C. M., Sher, A. C., Kohan, A., Rubbert, C. & Avril, N. Recurrent and metastatic breast cancer PET, PET/CT, PET/MRI: FDG and new biomarkers. Q J Nucl Med Mol Imaging (2013). 167. Chang, J. M. et al. False positive and false negative FDG-PET scans in various thoracic diseases. Korean J. Radiol. 7, 57–69 168. Lutz, a M., Ray, P., Willmann, J. K., Drescher, C. & Gambhir, S. S. 2-deoxy-2-[F18]fluoro-D-glucose accumulation in ovarian carcinoma cell lines. Mol. Imaging Biol. 9, 260–6 (2007). 172 169. Rohren, E. M., Turkington, T. G. & Coleman, R. E. Clinical applications of PET in oncology. Radiology 231, 305–32 (2004). 170. Schwarz, J. K., Grigsby, P. W., Dehdashti, F. & Delbeke, D. The role of 18F-FDG PET in assessing therapy response in cancer of the cervix and ovaries. J. Nucl. Med. 50 Suppl 1, 64S–73S (2009). 171. Prefontaine, M. & Walker-Dilks, C. PET Recommendation Report 7 IN REVIEW PET Imaging in Ovarian Cancer PET Imaging in Ovarian Cancer : Recommendations. (2009). 172. Tanizaki, Y. et al. Diagnostic Value of Preoperative SUVmax on FDG-PET/CT for the Detection of Ovarian Cancer. Int. J. Gynecol. Cancer (2014). 173. Son, H. et al. Role of FDG PET/CT in staging of recurrent ovarian cancer. Radiographics 31, 569–83 (2011). 174. Gouhar, G. K., Siam, S., Sadek, S. M. & Ahmed, R. A. Prospective assessment of 18F-FDG PET/CT in detection of recurrent ovarian cancer. Egypt. J. Radiol. Nucl. Med. 44, 913–922 (2013). 175. Ghosh, J. et al. Role of FDG PET-CT in asymptomatic epithelial ovarian cancer with rising serum CA-125: a pilot study. Natl. Med. J. India 26, 327–31 (2013). 176. Berek, J. S., Crum, C. & Friedlander, M. Cancer of the ovary, fallopian tube, and peritoneum. Int. J. Gynecol. Obstet. 119, S118–S129 (2012). 177. Psarakis, H. M. Clinical Challenges in Caring for Patients With Diabetes and Cancer. Diabetes Spectr. 19, 157–162 (2006). 178. Lee, J.-Y. et al. Diabetes mellitus and ovarian cancer risk: a systematic review and meta-analysis of observational studies. Int. J. Gynecol. Cancer 23, 402–12 (2013). 179. Bakhru, A., Buckanovich, R. J. & Griggs, J. J. The impact of diabetes on survival in women with ovarian cancer. Gynecol. Oncol. 121, 106–11 (2011). 180. Shah, M. M. et al. Diabetes mellitus and ovarian cancer: More complex than just increasing risk. Gynecol. Oncol. 135, 273–277 (2014). 181. Gallagher, E. J. & LeRoith, D. Diabetes, antihyperglycemic medications and cancer risk: smoke or fire? Curr. Opin. Endocrinol. Diabetes. Obes. 20, 485–94 (2013). 182. Lamkin, D. M. et al. Glucose as a prognostic factor in ovarian carcinoma. Cancer 115, 1021–7 (2009). 183. Leitzmann, M. F. et al. Body mass index and risk of ovarian cancer. Cancer 115, 173 812–22 (2009). 184. Grote, V. A., Becker, S. & Kaaks, R. Diabetes mellitus type 2 - an independent risk factor for cancer? Exp. Clin. Endocrinol. diabetes Off. J. Ger. Soc. Endocrinol. Ger. Diabetes Assoc. 118, 4–8 (2010). 185. Giovannucci, E. et al. Diabetes and cancer: a consensus report. in Diabetes care 33, 1674–1685 (2010). 186. Kellenberger, L. D. et al. The role of dysregulated glucose metabolism in epithelial ovarian cancer. J. Oncol. 2010, 514310 (2010). 187. Zhang, X. D. et al. Effect of 2-deoxy-D-glucose on various malignant cell lines in vitro. Anticancer Res. 26, 3561–6 188. Tayek, J. A. A review of cancer cachexia and abnormal glucose metabolism in humans with cancer. J. Am. Coll. Nutr. 11, 445–56 (1992). 189. Rodríguez-Enríquez, S., Marín-Hernández, A., Gallardo-Pérez, J. C. & MorenoSánchez, R. Kinetics of transport and phosphorylation of glucose in cancer cells. J. Cell. Physiol. 221, 552–559 (2009). 190. Younes, M., Lechago, L. V, Somoano, J. R., Mosharaf, M. & Lechago, J. Wide expression of the human erythrocyte glucose transporter Glut1 in human cancers. Cancer Res. 56, 1164–7 (1996). 191. Van Belle, T. L. L., Taylor, P. & von Herrath, M. G. G. Mouse Models for Type 1 Diabetes. Drug Discov. Today Dis. Model. 6, 41–45 (2009). 192. King, A. J. F. The use of animal models in diabetes research. Br. J. Pharmacol. 166, 877–894 (2012). 193. Dummler, B. et al. Life with a single isoform of Akt: mice lacking Akt2 and Akt3 are viable but display impaired glucose homeostasis and growth deficiencies. Mol. Cell. Biol. 26, 8042–51 (2006). 194. Garofalo, R. S. et al. Severe diabetes, age-dependent loss of adipose tissue, and mild growth deficiency in mice lacking Akt2/PKB beta. J. Clin. Invest. 112, 197– 208 (2003). 195. Vuguin, P., Saenger, P. & Dimartino-Nardi, J. Fasting Glucose Insulin Ratio: A Useful Measure of Insulin Resistance in Girls with Premature Adrenarche. J. Clin. Endocrinol. Metab. 86, 4618–4621 (2001). 196. Berridge, M. V, Tan, A. N. S., Mccoy, K. D. & Wang, R. U. I. The Biochemical and Cellular Basis of Cell Proliferation Assays That Use Tetrazolium Salts. 4–9 (1996). 174 197. Bower, W. F. et al. Overt diabetes mellitus adversely affects surgical outcomes of noncardiovascular patients. Surgery 147, 670–5 (2010). 198. White, N. H. Long-term Outcomes in Youths with Diabetes Mellitus. Pediatr. Clin. North Am. 62, 889–909 (2015). 199. Zelenko, Z. & Gallagher, E. J. Diabetes and cancer. Endocrinology and Metabolism Clinics of North America 43, 167–185 (2014). 200. American Diabetes Association. Standards of medical care in diabetes. Diabetes Care 37, (Suppl 1): S14–S80 (2014). 201. Phoenix, K. N., Vumbaca, F., Fox, M. M., Evans, R. & Claffey, K. P. Dietary energy availability affects primary and metastatic breast cancer and metformin efficacy. Breast Cancer Res. Treat. 123, 333–44 (2010). 202. Yang, X.-L. & Chan, J. C. Diabetes, insulin and cancer risk. World J. Diabetes 3, 60–4 (2012). 203. Han, L. et al. High Glucose Promotes Pancreatic Cancer Cell Proliferation via the Induction of EGF Expression and Transactivation of EGFR. PLoS One 6, e27074 (2011). 204. Parekh, N., Lin, Y., Hayes, R. B., Albu, J. B. & Lu-Yao, G. L. Longitudinal associations of blood markers of insulin and glucose metabolism and cancer mortality in the third National Health and Nutrition Examination Survey. Cancer Causes Control 21, 631–42 (2010). 205. Plesner, A., Ten Holder, J. T. & Verchere, C. B. Islet remodeling in female mice with spontaneous autoimmune and streptozotocin-induced diabetes. PLoS One 9, (2014). 206. Karagiannis, G. S. et al. Cancer-associated fibroblasts drive the progression of metastasis through both paracrine and mechanical pressure on cancer tissue. Mol. Cancer Res. 10, 1403–18 (2012). 207. Lerman, O. Z., Galiano, R. D., Armour, M., Levine, J. P. & Gurtner, G. C. Cellular dysfunction in the diabetic fibroblast: impairment in migration, vascular endothelial growth factor production, and response to hypoxia. Am. J. Pathol. 162, 303–12 (2003). 208. Nerlich, A. G., Hagedorn, H. G., Böheim, M. & Schleicher, E. D. Patients with diabetes-induced microangiopathy show a reduced frequency of carcinomas. In Vivo 12, 667–70 209. Renehan, A. G. et al. Diabetes and cancer (2): Evaluating the impact of diabetes on mortality In patients with cancer. Diabetologia 55, 1619–1632 (2012). 175 210. Kerr, A. D. The Role of Chronic , Systemic Inflammation in the Progression of Epithelial Ovarian Cancer. (2012). 211. Al-Wahab, Z. et al. Metformin prevents aggressive ovarian cancer growth driven by high-energy diet: similarity with calorie restriction. Oncotarget 6, 10908–10923 (2015). 212. Shapot, V. S. & Blinov, V. a. Blood glucose levels and gluconeogenesis in animals bearing transplantable tumors. Cancer Res. 34, 1827–32 (1974). 213. Pavelić, K. et al. Growth and treatment of Ehrlich tumor in mice with alloxaninduced diabetes. Cancer Res. 39, 1807–13 (1979). 214. Gullino, P. M., Grantham, F. H. & Courtney, a H. Glucose consumption by transplanted tumors in vivo. Cancer Res. 27, 1031–40 (1967). 215. de Groot, J. W. B. et al. Non-islet cell tumour-induced hypoglycaemia: a review of the literature including two new cases. Endocr. Relat. Cancer 14, 979–93 (2007). 216. Wahdan-Alaswad, R. et al. Glucose promotes breast cancer aggression and reduces metformin efficacy. Cell Cycle 12, 3759–69 (2013). 217. Diaz-Ruiz, R., Rigoulet, M. & Devin, A. The Warburg and Crabtree effects: On the origin of cancer cell energy metabolism and of yeast glucose repression. Biochim. Biophys. Acta 1807, 568–76 (2011). 218. Anderson, A. S. et al. Metabolic changes during ovarian cancer progression as targets for sphingosine treatment. Exp. Cell Res. 319, 1431–42 (2013). 219. Kueck, A. et al. Resveratrol inhibits glucose metabolism in human ovarian cancer cells. Gynecol. Oncol. 107, 450–7 (2007). 220. Harris, M. I., Klein, R., Welborn, T. A. & Knuiman, M. W. Onset of NIDDM occurs at least 4-7 yr before clinical diagnosis. Diabetes Care 15, 815–9 (1992). 221. Shibata, K. et al. Placental leucine aminopeptidase (P-LAP) and glucose transporter 4 (GLUT4) expression in benign, borderline, and malignant ovarian epithelia. Gynecol. Oncol. 98, 11–8 (2005). 222. Cho, H., Lee, Y. S., Kim, J., Chung, J.-Y. & Kim, J.-H. Overexpression of Glucose Transporter-1 (GLUT-1) Predicts Poor Prognosis in Epithelial Ovarian Cancer. Cancer Invest. 31, 607–15 (2013). 223. Scafoglio, C. et al. Functional expression of sodium-glucose transporters in cancer. Proc. Natl. Acad. Sci. 112, E4111–E4119 (2015). 224. Bormans, G. M. et al. Synthesis and biologic evaluation of (11)c-methyl-dglucoside, a tracer of the sodium-dependent glucose transporters. J. Nucl. Med. 176 44, 1075–1081 (2003). 225. Lin, S., Lin, D. C. & Flanagan, M. D. Specificity of the effects of cytochalasin B on transport and motile processes. Proc. Natl. Acad. Sci. U. S. A. 75, 329–33 (1978). 226. Berridge, M. V, Herst, P. M. & Tan, A. S. Tetrazolium dyes as tools in cell biology: new insights into their cellular reduction. Biotechnol. Annu. Rev. 11, 127–52 (2005). 227. Macheda, M. L., Rogers, S. & Best, J. D. Molecular and cellular regulation of glucose transporter (GLUT) proteins in cancer. J. Cell. Physiol. 202, 654–662 (2005). 228. Blessing, A. et al. Sodium/Glucose Co-transporter 1 Expression Increases in Human Diseased Prostate. J. Cancer Sci. Ther. 4(9), 302–312 (2012). 229. Helmke, B. M. et al. Expression of SGLT-1 in preneoplastic and neoplastic lesions of the head and neck. Oral Oncol. 40, 28–35 (2004). 230. Baron-Delage, S. et al. Deregulation of hexose transporter expression in Caco-2 cells by ras and polyoma middle T oncogenes. Am. J. Physiol. 270, G314–23 (1996). 231. de Miguel-Luken, M.-J. et al. MAP17 (PDZKIP1) as a novel prognostic biomarker for laryngeal cancer. Oncotarget 6, 12625–36 (2015). 232. Casneuf, V. F. et al. Expression of SGLT1, Bcl-2 and p53 in primary pancreatic cancer related to survival. Cancer Invest. 26, 852–859 (2008). 233. Hanabata, Y., Nakajima, Y., Morita, K.-I., Kayamori, K. & Omura, K. Coexpression of SGLT1 and EGFR is associated with tumor differentiation in oral squamous cell carcinoma. Odontology 100, 1–8 (2011). 234. Lai, B. et al. Overexpression of SGLT1 is correlated with tumor development and poor prognosis of ovarian carcinoma. Arch. Gynecol. Obstet. 285, 1455–61 (2012). 235. Ishikawa, N., Oguri, T., Isobe, T., Fujitaka, K. & Kohno, N. SGLT gene expression in primary lung cancers and their metastatic lesions. Jpn. J. Cancer Res. 92, 874– 9 (2001). 236. Zapata-Morales, J. R., Galicia-Cruz, O. G., Franco, M. & Morales, F. M. Hypoxiainducible factor-1α(HIF-1α) protein diminishes sodium glucose transport 1 (SGLT1) and SGLT2 protein expression In renal epithelial tubular cells (LLC-PK1) under hypoxia. J. Biol. Chem. 289, 346–357 (2014). 237. Vallon, V. et al. Knockout of Na-glucose transporter SGLT2 attenuates hyperglycemia and glomerular hyperfiltration but not kidney growth or injury in 177 diabetes mellitus. Am. J. Physiol. Renal Physiol. 304, F156–67 (2013). 238. Cantuaria, G. et al. GLUT-1 expression in ovarian carcinoma: association with survival and response to chemotherapy. Cancer 92, 1144–50 (2001). 239. Cantuaria, G. et al. Expression of GLUT-1 glucose transporter in borderline and malignant epithelial tumors of the ovary. Gynecol. Oncol. 79, 33–7 (2000). 240. Shin, S. J. et al. Ciglitazone enhances ovarian cancer cell death via inhibition of glucose transporter-1. Eur. J. Pharmacol. 743, 17–23 (2014). 241. Lin, H.-W. & Tseng, C.-H. A Review on the Relationship between SGLT2 Inhibitors and Cancer. Int. J. Endocrinol. 2014, 719578 (2014). 242. Bowker, S. L., Yasui, Y., Veugelers, P. & Johnson, J. a. Glucose-lowering agents and cancer mortality rates in type 2 diabetes: assessing effects of time-varying exposure. Diabetologia 53, 1631–7 (2010). 243. Evans, J. M. M., Donnelly, L. a, Emslie-Smith, A. M., Alessi, D. R. & Morris, A. D. Metformin and reduced risk of cancer in diabetic patients. BMJ 330, 1304–5 (2005). 244. Dilokthornsakul, P. et al. The effects of metformin on ovarian cancer: a systematic review. Int. J. Gynecol. Cancer 23, 1544–51 (2013). 245. Franciosi, M. et al. Metformin therapy and risk of cancer in patients with type 2 diabetes: systematic review. PLoS One 8, e71583 (2013). 246. Zhang, Z.-J. & Li, S. The prognostic value of metformin for cancer patients with concurrent diabetes: a systematic review and meta-analysis. Diabetes. Obes. Metab. 16(8), 707–710 (2014). 247. Kumar, S. et al. Metformin intake is associated with better survival in ovarian cancer: a case-control study. Cancer 119, 555–62 (2013). 248. Romero, I. L. et al. Relationship of type II diabetes and metformin use to ovarian cancer progression, survival, and chemosensitivity. Obstet. Gynecol. 119, 61–7 (2012). 249. Hur, K. Y. & Lee, M.-S. New mechanisms of metformin action: Focusing on mitochondria and the gut. J. Diabetes Investig. 6, 600–9 (2015). 250. Zakikhani, M., Dowling, R., Fantus, I. G., Sonenberg, N. & Pollak, M. Metformin is an AMP kinase-dependent growth inhibitor for breast cancer cells. Cancer Res. 66, 10269–73 (2006). 251. Dowling, R. J. O., Zakikhani, M., Fantus, I. G., Pollak, M. & Sonenberg, N. Metformin inhibits mammalian target of rapamycin-dependent translation initiation 178 in breast cancer cells. Cancer Res. 67, 10804–12 (2007). 252. Rattan, R., Giri, S., Hartmann, L. C. & Shridhar, V. Metformin attenuates ovarian cancer cell growth in an AMP-kinase dispensable manner. J. Cell. Mol. Med. 15, 166–78 (2011). 253. Kalender, A. et al. Metformin, independent of AMPK, inhibits mTORC1 in a rag GTPase-dependent manner. Cell Metab. 11, 390–401 (2010). 254. Ben Sahra, I. et al. The antidiabetic drug metformin exerts an antitumoral effect in vitro and in vivo through a decrease of cyclin D1 level. Oncogene 27, 3576–86 (2008). 255. Yasmeen, A. et al. Induction of apoptosis by metformin in epithelial ovarian cancer: involvement of the Bcl-2 family proteins. Gynecol. Oncol. 121, 492–8 (2011). 256. Buzzai, M. et al. Systemic treatment with the antidiabetic drug metformin selectively impairs p53-deficient tumor cell growth. Cancer Res. 67, 6745–52 (2007). 257. Hirsch, H. a., Iliopoulos, D., Tsichlis, P. N. & Struhl, K. Metformin selectively targets cancer stem cells, and acts together with chemotherapy to block tumor growth and prolong remission. Cancer Res. 69, 8832–8833 (2009). 258. Patel, S., Kumar, L. & Singh, N. Metformin and epithelial ovarian cancer therapeutics. Cell. Oncol. (Dordr). 38, 365–75 (2015). 259. Rocha, G. Z. et al. Metformin Amplifies Chemotherapy-Induced AMPK Activation and Antitumoral Growth. Clin. Cancer Res. 17, 3993–4005 (2011). 260. Lengyel, E. et al. Metformin inhibits ovarian cancer growth and increases sensitivity to paclitaxel in mouse models. Am. J. Obstet. Gynecol. 212, 479.e1– 479.e10 (2015). 261. Gotlieb, W. H. et al. In vitro metformin anti-neoplastic activity in epithelial ovarian cancer. Gynecol. Oncol. 110, 246–50 (2008). 262. Rattan, R., Graham, R. P., Maguire, J. L., Giri, S. & Shridhar, V. Metformin suppresses ovarian cancer growth and metastasis with enhancement of cisplatin cytotoxicity in vivo. Neoplasia 13, 483–491 (2011). 263. Shank, J. J. et al. Metformin targets ovarian cancer stem cells in vitro and in vivo. Gynecol. Oncol. 127, 390–7 (2012). 264. Xie, Y. et al. Metformin combined with p38 MAPK inhibitor improves cisplatin sensitivity in cisplatin‑resistant ovarian cancer. Mol. Med. Rep. 10, 2346–50 (2014). 179 265. Iliopoulos, D., Hirsch, H. A. & Struhl, K. Metformin decreases the dose of chemotherapy for prolonging tumor remission in mouse xenografts involving multiple cancer cell types. Cancer Res. 71, 3196–201 (2011). 266. Wu, B. et al. Metformin inhibits the development and metastasis of ovarian cancer. Oncol. Rep. 28, 903–8 (2012). 267. Kinaan, M., Ding, H. & Triggle, C. R. Metformin: An Old Drug for the Treatment of Diabetes but a New Drug for the Protection of the Endothelium. Med. Princ. Pract. 24, 401–15 (2015). 268. Hawley, S. A., Gadalla, A. E., Olsen, G. S. & Hardie, D. G. The antidiabetic drug metformin activates the AMP-activated protein kinase cascade via an adenine nucleotide-independent mechanism. Diabetes 51, 2420–5 (2002). 269. Segal, E. D. et al. Relevance of the OCT1 transporter to the antineoplastic effect of biguanides. Biochem. Biophys. Res. Commun. 414, 694–9 (2011). 270. Gao, S. et al. Attenuating tumour angiogenesis: a preventive role of metformin against breast cancer. Biomed Res. Int. 2015, 592523 (2015). 271. Bikas, A. D. et al. Glucose-deprivation increases thyroid cancer cell sensitivity to metformin. Endocr. Relat. Cancer 22, 919–32 (2015). 272. Litchfield, L. M. et al. Hyperglycemia-induced metabolic compensation inhibits metformin sensitivity in ovarian cancer. Oncotarget 6, 23548–23560 (2015). 273. Silvestri, A. et al. Metformin Induces Apoptosis and Downregulates Pyruvate Kinase M2 in Breast Cancer Cells Only When Grown in Nutrient-Poor Conditions. PLoS One 10, e0136250 (2015). 274. Birsoy, K. et al. Metabolic determinants of cancer cell sensitivity to glucose limitation and biguanides. Nature 508, 108–112 (2014). 275. Sui, X. et al. Use of metformin alone is not associated with survival outcomes of colorectal cancer cell but AMPK activator AICAR sensitizes anticancer effect of 5fluorouracil through AMPK activation. PLoS One 9, e97781 (2014). 276. Yilmaz, B. et al. Metformin regresses endometriotic implants in rats by improving implant levels of superoxide dismutase, vascular endothelial growth factor, tissue inhibitor of metalloproteinase-2, and matrix metalloproteinase-9. Am. J. Obstet. Gynecol. 202, 368.e1–8 (2010). 277. Scotland, S. et al. Mitochondrial energetic and AKT status mediate metabolic effects and apoptosis of metformin in human leukemic cells. Leukemia 27, 2129– 38 (2013). 278. Dykens, J. a et al. Biguanide-induced mitochondrial dysfunction yields increased 180 lactate production and cytotoxicity of aerobically-poised HepG2 cells and human hepatocytes in vitro. Toxicol. Appl. Pharmacol. 233, 203–10 (2008). 279. Wheaton, W. W. et al. Metformin inhibits mitochondrial complex I of cancer cells to reduce tumorigenesis. Elife 3, e02242 (2014). 280. Andrzejewski, S., Gravel, S.-P., Pollak, M. & St-Pierre, J. Metformin directly acts on mitochondria to alter cellular bioenergetics. Cancer Metab. 2, 12 (2014). 281. Menendez, J. A. et al. Oncobiguanides: Paracelsus’ law and nonconventional routes for administering diabetobiguanides for cancer treatment. Oncotarget 5, 2344–8 (2014). 282. Thompson, M. D. et al. Lack of effect of metformin on mammary carcinogenesis in nondiabetic rat and mouse models. Cancer Prev. Res. (Phila). 8, 231–9 (2015). 283. Shu, Y. et al. Effect of genetic variation in the organic cation transporter 1 (OCT1) on metformin action. J. Clin. … 117, 1422–31 (2007). 284. Ma, Y. et al. K‑ras gene mutation as a predictor of cancer cell responsiveness to metformin. Mol. Med. Rep. 8, 763–768 (2013). 285. Aleksandrovski, Y. A. Molecular mechanisms of the cross-impact of pathological processes in combined diabetes and cancer. Research and clinical aspects. Biochem. Biokhimiia 67, 1329–1346 (2002). 286. Ross, S. a & Milner, J. a. Epigenetic modulation and cancer: effect of metabolic syndrome? Am. J. Clin. Nutr. 86, s872–7 (2007). 287. Simon, D. & Balkau, B. Diabetes mellitus, hyperglycaemia and cancer. Diabetes Metab. 36, 182–191 (2010). 288. Bodmer, M., Becker, C., Meier, C., Jick, S. S. & Meier, C. R. Use of metformin and the risk of ovarian cancer: a case-control analysis. Gynecol. Oncol. 123, 200– 4 (2011). 289. Van De Poll-Franse, L. V et al. Less aggressive treatment and worse overall survival in cancer patients with diabetes: a large population based analysis. Int. J. cancer 120, 1986–1992 (2007). 290. Barone, B. B. et al. Postoperative mortality in cancer patients with preexisting diabetes: systematic review and meta-analysis. Diabetes Care 33, 931–9 (2010). 291. Rogozan, I. O. N. Relations Between Tumor and Metastasis. 978–984 (1965). 292. Vadlakonda, L., Dash, A., Pasupuleti, M., Anil Kumar, K. & Reddanna, P. Did we get pasteur, warburg, and crabtree on a right note? Front. Oncol. 3, 186 (2013). 181 293. Singh, R. et al. Non-hyperinsulinemic hypoglycemia in a patient with a gastrointestinal stromal tumor. Eur. J. Intern. Med. 17, 127–9 (2006). 294. Marks, L. J., Steinke, J., Podolsky, S. & Egdahl, R. H. Hypoglycemia associated with neoplasia. Ann. N. Y. Acad. Sci. 230, 147–60 (1974). 295. Bishop, J. S. & Marks, P. A. Studies on carbohydrate metabolism in patients with neoplastic disease. II. Response to insulin administration. J. Clin. Invest. 38, 668– 72 (1959). 296. Jasani, B., Donaldson, L. J., Ratcliffe, J. G. & Sokhi, G. S. Mechanism of impaired glucose tolerance in patients with neoplasia. Br. J. Cancer 38, 287–92 (1978). 297. Norton, J. A., Maher, M., Wesley, R., White, D. & Brennan, M. F. Glucose intolerance in sarcoma patients. Cancer 54, 3022–3027 (1984). 298. Denton, I. C., Kerlan, R. A. & McGraw, R. Brain tumor with hyperosmolar hyperglycemic nonketotic diabetic coma. JAMA 218, 256–7 (1971). 299. Pospisilik, J. A. et al. Targeted deletion of AIF decreases mitochondrial oxidative phosphorylation and protects from obesity and diabetes. Cell 131, 476–91 (2007). 300. Jacobs, M. A. et al. Multiparametric magnetic resonance imaging, spectroscopy and multinuclear (23Na) imaging monitoring of preoperative chemotherapy for locally advanced breast cancer. Acad. Radiol. 17, 1477–85 (2010). 301. Ouwerkerk, R. Sodium magnetic resonance imaging: from research to clinical use. J. Am. Coll. Radiol. 4, 739–41 (2007). 302. Ouwerkerk, R. et al. Elevated tissue sodium concentration in malignant breast lesions detected with non-invasive 23Na MRI. Breast Cancer Res. Treat. 106, 151–160 (2007). 303. Jacobs, M. A. et al. Monitoring of neoadjuvant chemotherapy using multiparametric, 23Na sodium MR, and multimodality (PET/CT/MRI) imaging in locally advanced breast cancer. Breast Cancer Res. Treat. 128, 119–126 (2011). 304. Ferriss, J. S. et al. Does significant medical comorbidity negate the benefit of upfront cytoreduction in advanced ovarian cancer? Int. J. Gynecol. Cancer 22, 762– 9 (2012). 305. Menzin, A. W., Kobrin, S., Pollak, E., Goodman, D. B. & Rubin, S. C. The effect of renal function on serum levels of CA 125. Gynecol. Oncol. 58, 375–7 (1995). 306. Turgutalp, K. et al. Serum levels of cancer biomarkers in diabetic and non-diabetic proteinuric patients: a preliminary study. Clin. Chem. Lab. Med. 51, 889–95 (2013). 182 307. Esteghamati, A. et al. The inverse relation of CA-125 to diabetes, metabolic syndrome, and associated clinical variables. Metab. Syndr. Relat. Disord. 11, 256–61 (2013). 308. Breborowicz, A., Breborowicz, M., Pyda, M., Połubinska, A. & Oreopoulos, D. Limitations of CA125 as an index of peritoneal mesothelial cell mass. Nephron. Clin. Pract. 100, c46–51 (2005). 309. Joo, N.-S., Kim, K.-N. & Kim, K. S. Serum CA125 concentration has inverse correlation with metabolic syndrome. J. Korean Med. Sci. 26, 1328–32 (2011). 310. da Silva Faria, M. C. et al. Effect of diabetes on biodistribution, nephrotoxicity and antitumor activity of cisplatin in mice. Chem. Biol. Interact. 229, 119–31 (2015). 311. Harris, D. et al. Glucocorticoid-induced hyperglycemia is prevalent and unpredictable for patients undergoing cancer therapy: an observational cohort study. Current Oncology 20, e532–e538 (2013). 312. Balding, L., Philips, T. M. & Fleming, J. S. The management of diabetes in cancer patients receiving palliative care in a hospital setting. Palliat. Med. 24, S129 (2010). 313. Poulson, J. The management of diabetes in patients with advanced cancer. J. Pain Symptom Manage. 13, 339–46 (1997). 314. Stanley, I. a, Ribeiro, S. M., Giménez-Cassina, A., Norberg, E. & Danial, N. N. Changing appetites: the adaptive advantages of fuel choice. Trends Cell Biol. 24, 118–27 (2014). 315. Aronoff, S. L., Berkowitz, K., Shreiner, B. & Want, L. Glucose Metabolism and Regulation: Beyond Insulin and Glucagon. Diabetes Spectr. 17, 183–190 (2004). 316. Linnerth-Petrik, N. M., Santry, L. A., Petrik, J. J. & Wootton, S. K. Opposing functions of Akt isoforms in lung tumor initiation and progression. PLoS One 9, e94595 (2014). 317. Cho, H. et al. Insulin resistance and a diabetes mellitus-like syndrome in mice lacking the protein kinase Akt2 (PKB beta). Science 292, 1728–31 (2001). 318. Yang, J. & Holman, G. D. Long-term metformin treatment stimulates cardiomyocyte glucose transport through an AMP-activated protein kinasedependent reduction in GLUT4 endocytosis. Endocrinology 147, 2728–36 (2006). 319. Cefalu, W. T. Paradoxical insights into whole body metabolic adaptations following SGLT2 inhibition. J. Clin. Invest. 124, 485–7 (2014). 320. Merovci, A. et al. Dapagliflozin improves muscle insulin sensitivity but enhances endogenous glucose production. J. Clin. Invest. 124, 509–14 (2014). 183 Appendix I: Supplementary figures Figure 41: Positive SGLT1 staining on human ovarian tumour tissue 184 Dapagliflozin treatment does not affect the weight of established tumours We hypothesized that reducing systemic blood glucose in diabetic mice would moderate the growth of epithelial ovarian tumours by limiting fuel availability. We were unable to reduce fasting blood glucose in metformin-treated mice (Chapter 4), so we attempted to do so using the SGLT2 inhibitor dapagliflozin, a member of the thiazolidinedione (TZD) class of drugs that is based on the structure of phlorizin (PZ). TZDs have recently been developed as a promising new treatment in Type 2 diabetes (T2DM): SGLT2 increases glucose reuptake into the renal circulation, and blocking this reuptake significantly reduces blood glucose in an insulin-independent manner. Dapagliflozin (Cayman Chemical, Ann Arbor, MI) was formulated in polyethylene glycol/water/ethanol (45:45:10, v/v/v) at a concentration of 5 mg/ml. Mice received a daily dose of 1 mg/kg dapagliflozin by oral gavage for 45 days (80 days PTI to 125 days PTI). 185 Figure 42: Dapagliflozin treatment does not affect tumour weight A) Fasting blood glucose after two weeks (PTI day 95) and six weeks (PTI day 125) of dapagliflozin treatment. B) Tumour weights from mice sacrificed at PTI day 125. Bars are mean + SEM. Brackets with stars indicate differences between bars by two-way ANOVA with Bonferroni corrections. N=5 mice per group. *p<0.05, **p<0.01. 186 In mice 125 days post-tumour induction, daily dapagliflozin treatment for approximately six weeks (45 days) did not result in a reduction in blood glucose. After two weeks of treatment, WT animals had a paradoxical increase in blood glucose that may represent a systemic compensation for dapagliflozin-induced glucosuria (Figure 41A). Dapagliflozin has been associated with an increase in endogenous glucose production that is independent of the decrease in plasma glucose concentration319 and can reduce the glucose-lowering effects by half.320 When mice were sacrificed at 125 days PTI, the differences in FBG were abrogated. It is possible that by this point in EOC development, tumours had already altered glucose metabolism (Figures 6 and 8), reducing the efficacy of dapagliflozin to reduce systemic glucose. Dapagliflozin treatment was also unable to affect tumour weight (Figure 41B), although the small size of the tumours may have masked any statistical differences. These data indicate that dapagliflozin cannot reduce the weight of established tumours, however they do not address whether or not glucose reduction at tumour initiation can limit tumour growth. 187 Appendix II: Source of supplies and materials [14C] α-methyl-D-glucopyranoside Moravek Biochemicals, Brea, CA [3H] 2-deoxy-D-glucose Moravek Biochemicals, Brea, CA Acrylamide Bio-Rad Laboratories, Mississauga, ON Agarose Life Technologies Inc., Burlington, ON Ammonium persulfate (APS) Fisher Scientific, Whitby, ON Antibiotic-antimycotic (ABAM) Life Technologies Inc., Burlington, ON Anti-GLUT1 antibody Santa Cruz Biotechnologies, Santa Cruz, CA Anti-mouse secondary antibody Cell Signal Technologies, Danvers, MA Anti-rabbit secondary antibody Cell Signal Technologies, Danvers, MA Anti-SGLT1 antibody Abcam, Cambridge, MA Anti-SGLT2 antibody Abcam, Cambridge, MA Anti-β-actin antibody Cell Signal Technologies, Danvers, MA Aprotinin Sigma, Oakville, ON Biocoat Matrigel invasion chambers BD Biosciences, Franklin Lakes, NJ Biotinylated anti-rabbit secondary antibody Sigma, Oakville, ON Bovine serum albumin (BSA) Sigma, Oakville, ON Buffered formalin (10%) Fisher Scientific, Whitby, ON Citric acid Sigma, Oakville, ON Corning cryovials Fisher Scientific, Whitby, ON Costar culture dishes Corning Life Sciences, Lowell, MA Crystal Violet Sigma, Oakville, ON Cytochalasin B Sigma, Oakville, ON CytoScint liquid scintillation cocktail MP Biomedicals, Santa Ana, CA Dapagliflozin Cayman Chemical, Ann Arbor, MI DC Protein Quantification kit Bio-Rad Laboratories, Mississauga, ON Deoxyribonucleoside triphosphate (dNTP) Life Technologies Inc., Burlington, ON Diaminobenzidine tetrahydrochloride (DAB) Sigma, Oakville, ON Dithiothreitol (DTT) Life Technologies Inc., Burlington, ON 188 DMSO Sigma, Oakville, ON DNA ladder (100bp) Life Technologies Inc., Burlington, ON Dulbecco's Modified Eagle Medium (DMEM) Life Technologies Inc., Burlington, ON Enhanced chemiluminescence (ECL) Perkin Elmer, Waltham, MA Ethanol Greenfield Ethanol Inc., Brampton, ON Ethidium Bromide Bio-Rad Laboratories, Mississauga, ON Ethylenediaminetetraacetic acid (EDTA) Fisher Scientific, Whitby, ON Extravidin peroxidase Sigma, Oakville, ON Fetal bovine serum (FBS) Life Technologies Inc., Burlington, ON Glass coverslips Fisher Scientific, Whitby, ON Glucose Fisher Scientific, Whitby, ON Glycerol Fisher Scientific, Whitby, ON Hematoxylin Fisher Scientific, Whitby, ON Hydrogen peroxide Sigma, Oakville, ON Leupeptin Sigma, Oakville, ON L-glutamine Life Technologies Inc., Burlington, ON Metformin hydrochloride Sigma, Oakville, ON Methanol Fisher Scientific, Whitby, ON MTT Sigma, Oakville, ON Nitrocellulose membranes Amersham, Piscataway, NJ Nuclease-free water Applied Biosystems, Foster City, CA Pepstatin A Sigma, Oakville, ON Permount Fisher Scientific, Whitby, ON Phenylmethanesulfony fluoride (PMSF) Roche Applied Science, Laval, QC Phloretin Santa Cruz Biotechnologies, Santa Cruz, CA Phlorizin Sigma, Oakville, ON Phosphate buffered saline Life Technologies Inc., Burlington, ON Polybrene Santa Cruz Biotechnologies, Santa Cruz, CA Potassium chloride Fisher Scientific, Whitby, ON 189 Potassium iodide Fisher Scientific, Whitby, ON Potassium phosphate monobasic Fisher Scientific, Whitby, ON puromycin dihydrochloride Santa Cruz Biotechnologies, Santa Cruz, CA Rnasin Fisher Scientific, Whitby, ON Rneasy Mini Kit Qiagen, Toronto, ON ScintiGest tissue solubilizer Fisher Scientific, Whitby, ON SGLT2 shRNA lentiviral particles Santa Cruz Biotechnologies, Santa Cruz, CA Skim milk powder Fisher Scientific, Whitby, ON SKOV-3 cell line ATCC, Manassas, VA Sodium azide Fisher Scientific, Whitby, ON Sodium chloride Fisher Scientific, Whitby, ON Sodium citrate dihydrate Fisher Scientific, Whitby, ON Sodium dodecyl sulfate (SDS) Sigma, Oakville, ON Sodium fluoride (NaF) Fisher Scientific, Whitby, ON Sodium orthovanadate (NaV) Sigma, Oakville, ON Streptozotocin Sigma, Oakville, ON Sucrose Sigma, Oakville, ON Superfrost Plus glass slides Fisher Scientific, Whitby, ON SuperScript II Reverse Transcriptase kit Life Technologies Inc., Burlington, ON Taq DNA polymerase New England BioLabs, Pickering, ON Tetramethylethylenediamine (TEMED) Sigma, Oakville, ON Tissue microarray (human ovarian cancer) US Biomax, Rockville, MD Tris base Fisher Scientific, Whitby, ON Tris Hydrochloride Fisher Scientific, Whitby, ON Triton X-100 Sigma, Oakville, ON Trypsin-EDTA (10x) Invitrogen (Life Technologies) Turbo DNA-free kit Applied Biosystems, Foster City, CA Tween-20 Fisher Scientific, Whitby, ON Vacutainer Serum Separator Tube Fisher Scientific, Whitby, ON 190 Western Blot apparatus Bio-Rad WST-1 Roche Applied Science, Laval, QC Xylene Fisher Scientific, Whitby, ON 191 Appendix III: Recipes for solutions 50 mM sodium citrate buffer (pH 4.5 for streptozotocin) Sodium citrate 0.441 g in RO H2O up to 15mL 20x Phosphate Buffered Saline (Stock PBS for IHC) Sodium chloride 16.0g or Potassium chloride 0.4g Sodium potassium dibasic anhydrous 2.3g Potassium phosphate monobasic (pH 7.4) 0.4g Immunohistochemistry Blocking Solution 5% BSA 10g Sodium azide 0.2g 1x PBS 200mL Citrate Buffer Stock A – Citrate Buffer Citric Acid 2.1g RO H2O 100mL Stock B – Citrate Buffer Sodium citrate dihydrate 14.7g RO H2O 500mL 192 Working Citrate Buffer (pH 6.0) Stock A 18mL Stock B 82mL RO H2O up to 1L Sodium Citrate with Tween 20 (pH 6.0) Sodium citrate dihydrate 2.94g RO H2O up to 1L Tween 20 0.5mL Carazzi’s Hematoxylin Hematoxylin 0.25g Glycerol 50mL Aluminum potassium sulfate (APS) 12.5g Potassium iodide 0.05g RO H2O 200mL RIPA Lysis Buffer 10mM Tris HCl 0.788g RO H2O (pH adjusted to 7.6) up to 495mL 5mM Ethylenediaminetetraacetic acid (EDTA) 0.7306g 50mM Sodium chloride 1.461g 30mM Tetrasodium pyrophosphate 3.988g 1% Triton X-100 5mL 193 Protease inhibitors per mL RIPA (added fresh before each use) Aprotinin (2.5mg/mL) 2µL Phenylmethanesulfonyl fluoride (PMSF; 0.871g/mL) 20µL Sodium Orthovanadate (NaV; 0.1mM) 2µL Sodium fluoride (NaF; 50mM) 50µL Pepstatin A (1mg/mL) 1µL Leupeptin (2mg/mL) 1µL Reducing Buffer (3x) (Western blot) 10% SDS 2mL Glycerol 1mL 1M Tris HCl 0.5mL pH adjusted to 6.8 Bromeophenol Blue 10mg RO H2O up to 9mL DTT 1:7 ratio 5x Running Buffer (Tris-Glycine Buffer; Western blot) Tris base 15.1g Glycine 72.1g 10% SDS 10mL RO H2O up to 1L Transfer Buffer (Western blot) Tris base 7.0g Glycine 3.02g Methanol (added fresh before use) 200mL RO H2O up to 1L 194 10x Tris buffered saline (TBS; pH 7.6) Tris base 24.2g Sodium chloride 80.0g RO H2O up to 1L Tween 20 1 ml 50x Tris-acetate-EDTA (TAE) Buffer (PCR) Tris base 121g Glacial acetic acid 28.6g 0.5M EDTA 50mL RO H2O up to 500mL 195 Appendix IV: RT-PCR primer sets Primer set and accession number Annealing temperature Product size (bp) 55°C 191 55°C 156 SGLT3 Forward TGAGAGACCCAACAGATGAAGA (slc5a3) nm_017391 Reverse TCAAGAAGCCAGCCATTAGAG 55°C 165 GLUT1 Forward (slc2a1) nm_011400 Reverse CAGATGATGCGGGAGAAGAA 60°C 236 GLUT2 Forward (slc2a2) nm_031197 Reverse TCCTGGTCTTCACCCTGTTT 60°C 189 60°C 209 60°C 171 SGLT1 Forward (slc5a1) nm_019810 Reverse SGLT2 Forward (slc5a2) nm_133254 Reverse Sequence (3’-5’) TCTTCGTCATCAGCGTCATC GGGGGCTTCTGTGTCCATTTC ATGATGACCGTGGCTGTGT TTCCTGCCCTGTTCCTTTTC ACAACAAACAGCGACACCAC GGTCGGTTCCTCGGTTTTAG GLUT3 Forward (slc2a3) nm_011401 Reverse GAACAAAAGACCCCCTCCTC GLUT4 Forward (slc2a4) nm_009204 Reverse CCTGCTTGGCTTCTTCATCT AACCTCTCTCCAGCACCAAA TTTGCCCCTCAGTCATTCTC 196