Isolation and Expansion of Adult Cardiac Stem Cells From Human and Murine Heart
Elisa Messina, Luciana De Angelis, Giacomo Frati, Stefania Morrone, Stefano Chimenti, Fabio
Fiordaliso, Monica Salio, Massimo Battaglia, Michael V.G. Latronico, Marcello Coletta,
Elisabetta Vivarelli, Luigi Frati, Giulio Cossu and Alessandro Giacomello
Circ Res. 2004;95:911-921; originally published online October 7, 2004;
doi: 10.1161/01.RES.0000147315.71699.51
Circulation Research is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 2004 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7330. Online ISSN: 1524-4571
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://circres.ahajournals.org/content/95/9/911
Data Supplement (unedited) at:
http://circres.ahajournals.org/content/suppl/2004/11/02/95.9.911.DC1.html
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Circulation Research can be obtained via RightsLink, a service of the Copyright Clearance Center, not the
Editorial Office. Once the online version of the published article for which permission is being requested is
located, click Request Permissions in the middle column of the Web page under Services. Further information
about this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation Research is online at:
http://circres.ahajournals.org//subscriptions/
Downloaded from http://circres.ahajournals.org/ by guest on May 2, 2014
Cellular Biology
Isolation and Expansion of Adult Cardiac Stem Cells From
Human and Murine Heart
Elisa Messina, Luciana De Angelis, Giacomo Frati, Stefania Morrone, Stefano Chimenti,
Fabio Fiordaliso, Monica Salio, Massimo Battaglia, Michael V.G. Latronico, Marcello Coletta,
Elisabetta Vivarelli, Luigi Frati, Giulio Cossu, Alessandro Giacomello
Abstract—Cardiac myocytes have been traditionally regarded as terminally differentiated cells that adapt to increased work
and compensate for disease exclusively through hypertrophy. However, in the past few years, compelling evidence has
accumulated suggesting that the heart has regenerative potential. Recent studies have even surmised the existence of
resident cardiac stem cells, endothelial cells generating cardiomyocytes by cell contact or extracardiac progenitors for
cardiomyocytes, but these findings are still controversial. We describe the isolation of undifferentiated cells that grow
as self-adherent clusters (that we have termed “cardiospheres”) from subcultures of postnatal atrial or ventricular human
biopsy specimens and from murine hearts. These cells are clonogenic, express stem and endothelial progenitor cell
antigens/markers, and appear to have the properties of adult cardiac stem cells. They are capable of long-term
self-renewal and can differentiate in vitro and after ectopic (dorsal subcutaneous connective tissue) or orthotopic
(myocardial infarction) transplantation in SCID beige mouse to yield the major specialized cell types of the heart:
myocytes (ie, cells demonstrating contractile activity and/or showing cardiomyocyte markers) and vascular cells (ie,
cells with endothelial or smooth muscle markers). (Circ Res. 2004;95:911-921.)
Key Words: adult stem cell 䡲 myocardial regeneration and angiogenesis
C
ardiac myocytes have been traditionally regarded as
terminally differentiated cells that adapt to increased
work and compensate for disease exclusively through hypertrophy.1 In the past few years, compelling evidence has
accumulated suggesting that the heart has regenerative potential.2–5 The origin and significance of the subpopulation of
replicating myocytes are unknown; these issues could be
relevant to understand the for mechanisms coaxing endogenous cardiomyocytes to reenter the cell cycle and to the
search for strategies to transplant cardiac progenitor cells.6 In
fact, although embryonic stem cells have an exceptional
capacity for proliferation and differentiation, potential immunogenic, arrhythmogenic, and, particularly, ethical considerations limit their current use. Moreover, autologous transplantation of skeletal myoblasts has been considered because
of their high proliferative potential, their commitment to a
well-differentiated myogenic lineage, their resistance to ischemia, and their origin, which overcomes ethical, immunological, and availability problems. However, even if phase II
clinical trials with autologous skeletal myoblasts are ongoing,
several problems related to potentially life-threatening ar-
rhythmia (perhaps reflecting cellular uncoupling with host
cardiomyocytes7) must be taken into account when this
approach is considered. Furthermore, although cardiomyocytes can be formed, at least ex vivo, from different adult
stem cells, the ability of these cells to cross lineage boundaries is currently causing heated debate in the scientific
community,8 with the majority of reports indicating neoangiogenesis as the predominant in vivo effect of bone marrow
or endothelial progenitor cells.9,10
This report describes the identification and preliminary characterization of cells from the adult human and murine heart,
which have the properties of cardiac stem cells. Because these
cells also have been isolated and expanded from human heart
biopsy specimens, they could have a significant impact on future
clinical strategies to treat patients with heart disease.
Materials and Methods
Tissue Samples
Human tissue was derived from atrial or ventricular biopsy specimens belonging to patients (1 month to 80 years of age) undergoing
heart surgery, in conformation with the guidelines of the Italian
Original received December 5, 2003; first resubmission received June 16, 2004; second resubmission received August 24, 2004; revised resubmission
received September 28, 2004; accepted September 29, 2004.
From the Department of Experimental Medicine and Pathology (E.M., S.M., M.V.G.L., L.F., A.G.), University La Sapienza, Rome; IRCCS “Neuromed (E.M.,
S.M., M.V.G.L., L.F., A.G.),” Pozzilli (IS); Department of Histology and Medical Embriology (L.D.A., M.C., E.V., G.C.), University La Sapienza, Rome;
Campus-Biomedico University (G.F.), Rome; Institute of Neurobiology and Molecular Medicine (M.B.), Consiglio Nazionale delle Ricerche, Rome; Stem Cell
Research Institute (G.S.), Ospedale San Raffaele, Milan; Istituto di Ricerche Farmacologiche “Mario Negri” (S.C., F.F., M.S.), Milan, Italy.
Correspondence to Alessandro Giacomello, Department of Experimental Medicine and Pathology, University La Sapienza, 00161 Rome, Italy; E-mail
alessandro.giacomello@uniroma1.it; and to Giulio Cossu, Department of Histology and Medical Embriology, University La Sapienza, 00161 Rome, Italy.
E-mail giulio.cossu@uniromal.it
© 2004 American Heart Association, Inc.
Circulation Research is available at http://www.circresaha.org
DOI: 10.1161/01.RES.0000147315.71699.51
911
Downloaded from http://circres.ahajournals.org/
by guest on May 2, 2014
912
Circulation Research
October 29, 2004
Department of Health. Murine tissue was derived from the hearts of
previously characterized homozygous MLC1/3F-nlacZ11 and cTnInlacZ12 transgenic mice expressing a nuclear lacZ transgene under
the transcriptional control of the striated muscle myosin light chain
or cTnI promoters, respectively, homozygous B5-eGFP mice,13
homozygous GFP-cKit14 mice, MLC3F-nlacZ/B5-eGFP, MLC3Fnlac-Z/GFP-cKit, and cTnI-nlacZ/B5-eGFP cTnI-nlac-Z/GFP-cKit
crossed mice, SCID mice, and SCID beige mice (Charles River
Italia, Lecco, Italy).
Processing, Isolation, and Cryopreservation of
Sphere-Forming Cells
Isolated myocardial tissue was cut into 1- to 2-mm3 pieces, washed
with Ca2⫹-Mg2⫹–free phosphate-buffered solution (PBS) (Invitrogen), and digested three times for 5 minutes at 37°C with 0.2%
trypsin (Invitrogen) and 0.1% collagenase IV (Sigma, Milan, Italy).
The obtained cells were discarded, and the remaining tissue fragments washed with complete explant medium (CEM) (Iscove’s
Modified Dulbecco’s Medium [IMDM] supplemented with 10%
fetal calf serum, 100 U/mL penicillin G, 100 g/mL streptomycin,
2 mmol/L L-glutamine, and 0.1 mmol/L 2-mercaptoethanol) were
cultured as explants in CEM at 37°C and 5% CO2. After a period
ranging from 1 (embryo) to 3 (adult) weeks, a layer of fibroblast-like
cells was generated from adherent explants over which small,
phase-bright cells migrated. These phase-bright cells were collected
by pooling two washes with Ca2⫹-Mg2⫹–free PBS, one wash with
0.53 mmol/L EDTA (Versene, Invitrogen) (1 to 2 minutes), and one
wash with 0.5 g/L trypsin and 0.53 mmol/L EDTA (Invitrogen) (2 to
3 minutes) at room temperature under visual control. The cells
obtained (from 104 to 4⫻105 cells/explant) were seeded at ⬇0.5 to
2⫻105 cells/mL in poly-D-lysine-coated multiwell plates (BD Bioscences, Milan, Italy) in cardiosphere-growing medium (CGM)
(35% complete IMDM/65% DMEM–Ham F-12 mix containing 2%
B27, 0.1 mmol/L 2-mercaptoethanol, 10 ng/mL epidermal growth
factor [EGF], 20 ng/mL basic fibroblast growth factor [bFGF],
40 nmol/L cardiotrophin-1, 40 nmol/L thrombin, antibiotics, and
L-Glu, as in CEM). Isolation of the cardiosphere-forming cells could
be performed at least 4 times at 6- to 10-day intervals from the same
explant. Cardiospheres (CSs) were passaged every 2 to 3 days by
partial changing of the medium and mechanical trituration of the
larger clusters. Movies of cultured CSs, available in the online data
supplement at http://circres.ahajournals.org, were recorded using a
Nikon-COOLPIX-4500 digital camera connected to a Leitz inverted
microscope. For cryopreservation, we used CEM/DMEM–Ham F12
at 50:50, 5% B27, and 10% DMSO as the freezing medium.
Extensive descriptions of BrdUrd labeling, clonal analysis, differentiation on substrate-coated surface, coculture experiment, immunocytochemistry, flow cytometric analysis, in vivo analysis, and
heterotopic and orthotopic transplantation are provided in the online
data supplement.
Results
Isolation, Expansion, and Features in Culture of
Sphere-Generating Cells
Sphere-generating cells were obtained by mild enzymatic
digestion of explanted human atrial or ventricular biopsy
specimens and embryo, fetal, and postnatal mouse hearts.
Soon after the generation of a layer of fibroblast-like cells
from well-adherent explants, some small, round, phase-bright
cells began to migrate over this coat. These cells could be
harvested periodically by treatment with EDTA and mild
trypsinization and were allowed to grow on poly-D-lysine–
coated culture surfaces in a low-serum (3.5% fetal calf serum)
medium supplemented with a serum substitute (B27), growth
factors (EGF and bFGF), cardiothrophin-1 (CT-1),15 and
thrombin.16 During the first week of culture, the last factor led
to a 7-fold increase in the number of spheres with respect to
that obtained using the medium supplemented with the other
factors, either alone or in combination. Time-course observations of cells derived from human and murine explants
showed that early after their seeding (30 minutes), some of
these cells began to divide while still in suspension. Most
cells became loosely adherent, whereas others remained in
suspension, and some contaminating fibroblast-like cells
attached firmly to the poly-D-lysine coat. Cellular divisions
also were evident from the loosely adherent cell population
and produced clusters of small, round, phase-bright cells (that
we termed CSs) after 10 to 12 hours (Figure 1a). Within 24 to
36 hours of their appearance, CSs increased in size and some
of them detached from the culture surface; after 48 to 72
hours, most CSs were between 20 and 150 m in size, and,
when not subjected to mechanical dissociation, the largest
contained dark zones within the inner mass (Figure 1a).
Murine CSs started beating spontaneously soon after their
generation (Supplementary Movie: mouse CSs movie 1a) and
maintained this function during their life span (Supplementary Movie: mouse CSs movie 1b), whereas human CSs did
so only when cocultured with rat cardiomyocytes (Supplementary Movie: human CSs movie 1a and 1b). To be sure that
contraction was a new trait acquired by the CSs cells,
GFP-labeled human CSs (partially or totally dissociated)
were cocultured with cardiomyocytes prestained (Supplementary Human CSs Movie 2b through 2d) or not prestained
(Supplementary Human CSs Movie 3a through 3d) with Dil.
Contracting GFP-labeled cells were observed after 48 hours
of coculture; furthermore, Cx-43 immunostaining performed
on the cocultures of human GFP-transduced CSs with unlabeled neonatal rat cardiomyocytes showed the typical punctuate fluorescence pattern of the main gap junction protein of
the heart along the cytoplasmatic membrane of the human
cells (Figure 2d and Supplementary Figure VIII), suggesting
that a functional connection is created between the two
cellular populations.
Clonogenesis
CSs were found to be composed of clonally derived cells and
did not simply represent cellular aggregates. In fact, when
human GFP-transduced CSs or murine CSs (derived from
eGFP/MLC3F or eGFP/cTrI mice) were dissociated and
plated as single cells on mitomycin-treated STO fibroblastcoated 96-well plates (or clonally diluted on 10-cm Petri
dishes), fluorescent spheres were generated with a 1% to 10%
efficiency (Figure 2a). These spheres could be subcloned on
poly-D-lysine-coated surfaces, showing the same functional
and phenotypic behavior in culture as the nonclone-derived
CSs. In fact, 3 days after their appearance, some of the
MLC3F-nlacZ/B5-eGFP or cTnI-nlacZ/B5-eGFP mice
clone– derived CSs started to beat (supplementary clone
movie), and, after 48 hours of culture with CEM, the majority
(6 of 7) of these showed expression of the lac-Z transgene
within the nuclei after specific histochemical staining (Figure
2b1 and 2b2 and Supplementary Figure I). Moreover, human
clones derived from a single GFP-labeled cell started a
synchronous beating and expressed cTnI after 48 hours of
coculture with rat cardiomyocytes (Supplementary Movie
human CSs 2a and 2a1 and Supplementary Figure II).
Downloaded from http://circres.ahajournals.org/ by guest on May 2, 2014
Messina et al
Mammalian Adult Cardiac Stem Cells
913
Figure 1. CS proliferation. a, Phase micrograph of floating CSs (cultured from ⬍24 hours to ⬎48 hours) derived from primary culture of a
human atrial biopsy sample. b, Proliferation curves of human and mouse CSs (derived from 8 different subjects [left] and from prenatal and
postnatal hearts [middle and right], respectively) in the presence (middle) and absence (right) of 3.5% serum. Number of spheres refers to the
mean number per well from which 90% of the spheres were withdrawn at each time point for further analysis. Note the different pattern of proliferation between the human and mouse CSs and the rapid rise of the curves, followed by an irreversible decline in the serum-free conditions.
Furthermore, when BrdUrd was added to the culture
medium, virtually all cells in the small CSs and those of the
inner part of the largest CSs were labeled (Figure 3a),
indicating that these cells were newly generated (Supplementary Figures III through Va).
Proliferation
Human CS-generating cells were capable of self-renewal.
With periodical dissociation, together with partial substitution
of CGM every 2 to 3 days, a log-phase expansion of spheres
was obtained (Figure 1b). Mouse CS growth was slower
(probably because of the more differentiated features assumed in culture, such as beating) and serum-dependent as
for the human CSs (Figure 1b).
As shown in Figure 3a and Supplementary Figure V,
confocal immunofluorescence analysis of BrdUrd-labeled
human CSs with anti-BrdUrd (green) and cardiac-troponin I
(cTnI) or atrial natriuretic peptide (ANP) (red) revealed
BrdUrd-positive cells, particularly in the inner of the spheres,
whereas cTnI-positive or ANP-positive cells were mainly
localized in the external layers. Similar features are shown in
Supplementary Figures III and IV. BrdUrd-labeled cells (red)
mostly localized in the center of a CS and colocalize with the
Hoechst-labeled nuclei, whereas cardiac myosin heavy chain
(MHC)-expressing cells (green) were preferentially located in
the boundary layers. Furthermore, several CS cells expressed
cardiac differentiation markers (cTnI, ANP) while still dividing, as indicated by BrdUrd incorporation (Figure 3a and
Supplementary Figure Va), suggesting that early cardiac differentiation already occurred during the proliferation phase of their
growth. Usually within 10 days, some spheres became adherent,
Downloaded from http://circres.ahajournals.org/ by guest on May 2, 2014
914
Circulation Research
October 29, 2004
Figure 2. Clonogenesis and coculture
features. a, Fluorescence analysis of a
single cell (upper right) (obtained from a
dissociated GFP-expressing CS) when
plated by limiting dilution on mitomycintreated STO fibroblast-coated 96-well
plates in CGM over the course of the
generation of the GFP-labeled clone. This
clone could be passaged and expanded
on poly-D-lysine coat (lower left). b, X-Gal
staining of a eGFP/MLC3F clone
(obtained in the same way as were
human clones) after 48 hours of exposure
to growth factor-free medium. In these
conditions, clone cells become more flattened, with many nuclei appearing blue,
demonstrating that a differentiation process occurred (see also Supplementary
Figure I and Supplementary clone movies). c, Fluorescence analysis of partially
dissociated eGFP-labeled human CSs at
96 hours of coculture with rat cardiomyocytes. The same green cells that showed
a synchronous contraction with cardiocytes (see supplementary human CSs
movies) express cTnI. d, Fluorescent
analysis of connexin-43 expression (red)
in eGFP-labeled human CSs cocultured
with rat cardiomyocytes, as in (c). A
punctuate red fluorescence is present in
the cell membrane of human cells (see
Supplementary Figure VIII).
showing a more flattened morphology. Some small cells eventually migrated out from these “sun-like” spheres in the form of
adherent (differentiated) or small, round cells that could generate
new spheres. After thawing from cryopreservation, CSs proliferated again, maintaining their ability to beat (Supplementary
Movie: human CSs movie).
Immunophenotype Characterization and
Fluorescence-Activated Cell Sorting Analysis
Phenotypic analysis of newly developing human and mouse
CSs revealed expression of endothelial (KDR (human)/flk-1
[mouse], CD-31) and stem cell (CD-34, c-kit, sca-1) markers.
As shown in Figure 3b, CSs at the 2- to 10-cell stage strongly
Downloaded from http://circres.ahajournals.org/ by guest on May 2, 2014
Messina et al
Mammalian Adult Cardiac Stem Cells
915
Figure 3. CSs BrdUrd incorporation and CSs characterization. a, Fluorescence confocal analysis of BrdUrd-labeled human CSs for cardiac differentiation markers: 6-m scans (from the periphery to the center of the sphere) and final pictures (small and large images,
respectively) of BrdUrd (green) and cTnI (red) (see Supplementary Figures III through V). b, Confocal analysis of human CSs after 12
hours of culture: CD-34, CD-31, KDR, and c-Kit labeling of CS-generating cells at the beginning of sphere formation. c, fluorescenceactivated cell sorting analysis of postnatal mouse CSs-derived cells. A time course at 0 and 6 days was used, and the phenotype profile for CD34, cKit, Cd31, and sca-1 expression was analyzed and shown as a percentage of positive events. Data are presented as
mean⫾SD (n⫽3). *Statistically significant difference from 0 days. See the graphics in the Table and in Figure 6.
Downloaded from http://circres.ahajournals.org/ by guest on May 2, 2014
916
Circulation Research
October 29, 2004
reacted with antibodies against these antigens. In larger
spheres, the expression pattern of some of these markers
(particularly cKit) was similar to that of the BrdUrd-labeling
(positive staining in the center and in some peripheral zones,
generating satellite spheres; data not shown).
A time course (0 and 6 days) of the quantitative characterization of CS cells with these stem and endothelial markers
was performed by fluorescence-activated cell sorting analysis
(Figure 3c and Supplementary Figure VI). As shown at the
beginning of their formation (0 days), the phenotype of these
cells seems to reflect the epifluorescent microscopy analysis
with ⬇10% of positive staining for all four phenotypes.
However, at 6 days, cKit appears to be the only conserved
marker, suggesting that the cKit⫹ cells could be the main ones
contributing to the maintenance of proliferation. The initial
cell-labeling may reflect an early activation state, as has been
suggested for CD-34 in several systems.17 Fluorescence
microscopy analysis performed on cryosectioned human CSs
revealed expression of cardiac differentiation markers (cTnI,
MHC) and endothelial markers (von Willebrand factor)
(Supplementary Figure Vc1 through Vc3). When totally or
partially dissociated into single cells and cultured on
collagen-coated dishes in the same medium as the explants,
mouse and human CS-derived cells assumed a typical cardiomyocyte morphology, phenotype (Supplementary Figures
Vb1 through Vb2 and VIIc and VIId), and function documented (in the mouse only) by spontaneous contraction
(Supplementary Movie: mouse CSs movie 2a and 2b).
Human CSs did not beat spontaneously; however, these
began to beat within 24 hours when cocultured with postnatal
rat cardiomyocytes, losing their spherical shape and assuming
a “sun-like” appearance. Markers of cardiac differentiation
were coexpressed within GFP in labeled human CSs cells
(Figure 2c).
Transgenic Mice
To follow the differentiation process of CSs during the
prenatal and postnatal age, MLC3F-nlacZ and cTnI-nlacZ
mice were used.11–12 These mice express a form of lacZ
transgene that localizes within the nucleus under the skeletal
and cardiac muscle myosin light chain or cardiac troponin I
promoter, respectively. CSs obtained from embryonic day 9
to 12, fetal day 17 to 18, and from neonatal and adult mice
showed spontaneous expression of the reporter gene in variable
percentages (10% to 60%) of spheres in the different culture
conditions used (Figure 4a1 through 4a4 and Supplementary
Figure VIIa1, VIIa2, VIIb1, and VIIb2). Moreover, regarding the
human ones, CS-generating cells from mice expressed stem
(CD-34, sca-1, cKit) and endothelial cell markers (flk-1, CD-31)
(data not shown).
On this basis, we used transgenic mice expressing GFP
under the control of the c-kit promoter14 to further clarify the
cellular origin of these spheres and to follow the pattern of
their growth process. As shown in Figure 4c1, GFP-positive
cells were present from the beginning of the formation of the
CSs and, albeit with reduced fluorescence intensity, also later
within the mass of cells of the CSs and in cells migrating from
old adherent “sun-like” CSs (Figure 4c2). Moreover, as
suggested by the growth pattern of human CSs, when satellite
secondary CSs appeared to detach from the primary ones,
GFP-positive cells localized on the margins of the latter and
in the inner part of the former.
We studied this process in double-heterozygous mice
obtained from GFP-cKit/MLC3F-nlacZ or GFP-cKit/cTnInLacZ crossings. As shown in Figure 4c3 and 4c4, -Gal
positivity did not colocalize with GFP in cells present within
the growing areas.
In Vivo Survival and Morpho-functional Potential
of the Cardiospheres
To investigate the survival and morpho-functional potential
of the CSs in vivo, two sets of experiments were performed.
In the first, CS cells were injected in the dorsal subcutaneous
region of SCID mice. In the second, they were injected into
the hearts of SCID beige mice, acutely after myocardial
infarction. The objective of ectopic transplantation experiments was to study the pattern and the behavior of growth of
CSs in a neutral milieu (ie, without specific cardiac induction)
to verify their unique potential of generation of the main
cardiac cell types and to exclude the potential of neoplastic
transformation. For these experiments, ⬇60 pooled spheres/
inoculum/mouse from prenatal and postnatal MLC3F-nlacZ/
B5-eGFP mice, TnI-nlacZ/B5-eGFP mice, MLC3F-nlacZ/
CD-1 mice, and cTnI-nlacZ/CD-1 mice were used. During
the first 10 days, beating was appreciable through the skin
over the injection site, distant from large blood vessels. On
day 17, animals were euthanized and the inoculum recognized as a translucent formation, grain-like in size, wrapped
in ramified vessel-like structures. Observation of unfixed
cryosections by fluorescence microscopy (Figure 5a1 through
5a4) revealed the presence of open spheres from which cells
appeared to have migrated. Clusters of “black holes,” particularly in the periphery of the structure, were evident. The
tissue contained tubular formations, surrounded by nuclei
(Hoechst-positive), identified as cardiac sarcomeres by cTnI
and sarcomeric myosin immunostaining (Figure 5b3 through
5b6). ␣-Smooth muscle actin (␣-SMA)-positive structures
(known to be transiently expressed during cardiomyogenesis)2,18 were present in the remainder of the spheres and
associated with the vasculature (the clusters of “black holes”)
(Figure 5a3 through 5a5). This exhibited well-differentiated
structures with a thin endothelium expressing vascular
endothelial–cadherin (Figure 5b1) and a relative large lumen
containing erythrocytes (Figure 5a3), indicating the establishment of successful perfusion by the host. Light microscopic
observation of the inoculum, after X-gal staining, showed
strong nuclear expression of striated muscle-specific lacZ in
the remainder of the spheres and in some cells close to them
(Figure 5b2). No multidifferentiated structures suggesting the
presence of tumor formation were observed.
To test the acquisition of functional competence and the
cardiac regenerative potential of the CSs when challenged
into an infarcted myocardium, orthotopic transplantation
experiments with human CSs were performed. To perform
these, thawed (cryopreserved) adult human CSs from three
atrial (one male and two female) and one ventricular (one
female) biopsy specimens were injected into the viable
myocardium bordering a freshly produced infarct. Each
Downloaded from http://circres.ahajournals.org/ by guest on May 2, 2014
Messina et al
Mammalian Adult Cardiac Stem Cells
917
Figure 4. CSs features in transgenic
mice. a, Phase micrograph of CSs from
MLC3F-nlacZ and cTnI-nlacZ mice.
Nuclear lacZ expression is mainly localized in the external layers of embryo and
adult CSs soon after their formation
(inserts) and after a few days of culture
(right and central panels) (see Supplementary Figure VII). b, Fluorescence
analysis of a spontaneously differentiated
mouse CS. As suggested from the synchronous contraction showen in culture
(supplementary mouse CSs movie), cTnI
(red) is expressed in the sphere and the
migrated cells; in these, last sarcomers
are also evident. c, Fluorescence and
phase analysis of CSs from GFP-cKit,
GFP-cKit/MLC3F-nLacZ, and GFP-cKt/
cTnI-nlacZ mice. GFP-labeled cells were
present a few minutes after their seeding
in culture with CGM, at the beginning of
the generation of the CSs, later in their
inner mass, and after their migration out
from the oldest adherent spheres
(arrows) (upper left, lower left, and central panels). GFP-labeled cells did not
colocalize with the blue-stained ones
(arrows) in CSs from GFP-cKit/MLC3FnLacZ and GFP-cKit/cTnI-nlacZ mice.
Fluorescent cells also were present in
the growth area of the CSs (arrows) (right
upper and right lower panels). Fluorescence, phase (small), and merged (large)
images.
mouse received CSs from a single passage of an explant
(derived from a single subject). Four control infarcted animals were injected with an equal volume of PBS. Eighteen
days after the intervention, the animals were euthanized and
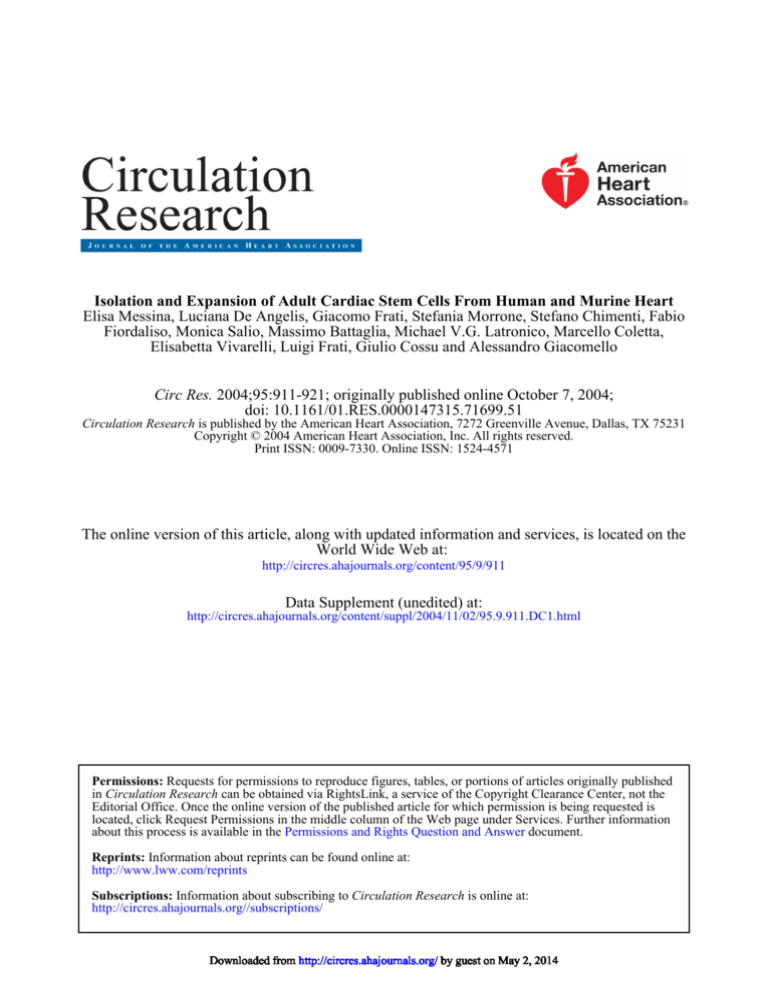
infarct size was determined. Infarct size was 34.9⫾7.1 (SEM,
3.6) and 31.9⫾6.9 (SEM, 3.5) in the CS-treated group and
PBS-injected group, respectively (P⫽NS). However, echocardiography showed better preservation of the infarcted
anterior wall thickness in the CS-treated group compared
with the PBS-injected group (0.80⫾0.29 [SEM, 0.15] versus
0.60⫾0.20 [SEM, 0.08]) (P⫽NS), particularly of percent
fractional shortening (36.85⫾16.43 [SEM, 8.21] versus
17.87⫾5.95 [SEM, 2.43]) (P⬍0.05) (Figure 6 and the Table).
At the time of evaluation, bands of regenerating myocardium were present (with different degrees of organization and
thickness) throughout most of the infarcted areas, as evaluated with hematoxylin– eosin histochemistry (data not shown)
and MHC immunofluorescence (Supplementary Figure IXa1
and IXa2). In the regenerating myocardium, cells expressing
lamin A/C (a specific human nuclear marker) also colocalize
with cardiomyocytes stained positive for MHC (Figure 6a
and 6e and Supplementary Figures IXb1, IXb2, and X), newly
generated capillaries stained for ␣-SMA (Figure 6b1, 6b2, and
6d) and platelet endothelial cell adhesion molecule (Figure
6c), and with connexin-43– expressing cells (data not shown).
Discussion
CSs appear to be a mixture of cardiac stem cells, differentiating progenitors, and even spontaneously differentiated car-
Downloaded from http://circres.ahajournals.org/ by guest on May 2, 2014
918
Circulation Research
October 29, 2004
Figure 5. In vivo analysis (ectopic CSs inoculum). a1 to a5, Ectopic transplantation of CSs from MLC3F-nlacZ/B5-eGFP mouse to SCID
mouse (upper left panels). Fluorescence analysis of unfixed cryosections (a1, a2, and a4) from the subcutaneous dorsal inoculum (day
17). GFP cells seemed to have migrated from the spheres, whereas clusters of vessel-like structures (a2) could be observed mainly in
the external area. Staining for SMA of one of these cryosections showed positive immunoreaction of the sphere and some cells within
the inoculum (a5). b-1 to b6, Fluorescence (b3 to b4) and phase analysis (b5 to b6) of fixed and immunostained cryosections from dorsal
inoculum of CSs from MLC3F-nlacZ/CD-1 and cTnI-lacZ/CD-1 mice. Tubular structures were stained for sarcomeric myosin (b3 to b5)
and cTnI (b4 through b6). X-Gal staining labeled the cells within and those migrating from CS (b2). Endothelial markers (SMA and vascular endothelial– cadherin) stained the vasculature (“black holes”) (a3 and b1).
Downloaded from http://circres.ahajournals.org/ by guest on May 2, 2014
Messina et al
Mammalian Adult Cardiac Stem Cells
919
Figure 6. In vivo analysis (orthotopic transplantation of human
CSs). Orthotopic transplantation performed in a SCID-beige
mouse. Cryopreserved human CSs were transplanted into the
viable myocardium bordering a freshly produced infarct. Confocal analysis of cryosectioned left ventricular heart 18 days
after the coronary ligature shows that (a) cardiomyocytes
expressing MHC (red) in the regenerating myocardium (particularly those indicated by the two central arrows) also stain
positive for lamin A/C (green) (a specific human nuclear
marker). In these cells, MHC expression is evident mainly in
the perinuclear area (see Supplementary Figure X). Lamin A/Clabeled cells (red) are present in newly generated capillaries
staining for ␣-SMA (b1 through d), and platelet endothelial cell
adhesion molecule (c). d, Confocal analysis of colocalization of
lamin A/C-labeled cells (red) with the newly generated capillaries staining for ␣-smooth muscle actin. e, Low-magnification
image shows viable lamin A/C-expressing cells (green) in
regenerating myocardium expressing MHC (red).
Downloaded from http://circres.ahajournals.org/ by guest on May 2, 2014
920
Circulation Research
October 29, 2004
Myocardial Repair (Echocardiography)
CAL⫹CSs
(N⫽4)
LVIDd, mm
AWThd, mm
FS, %
Sham
(N⫽3)
4.10
3.57
SD⫾0.85
SD⫾0.33
SD⫾0.06
SEM⫾0.42
SEM⫾0.13
SEM⫾0.03
0.80
2.13*†
0.60
1.03†
SD⫾0.29
SD⫾0.20
SD⫾0.01
SEM⫾0.15
SEM⫾0.08
SEM⫾0.01
36.85
SD⫾16.43
SEM⫾8.21
Regional wall motion abnormality, %
CAL
(N⫽6)
33.82
SD⫾10.05
SEM⫾6.53
17.87*
59.13*†
SD⫾5.95
SD⫾4.56
SEM⫾2.43
SEM⫾2.63
30.88
SD⫾14.71
SEM⫾7.35
*P⬍0.05 vs CAL⫹CSs.
†P⬍0.05 vs CAL.
Effect of human CSs orthotopic transplantation on echocardiographic index of myocardial
performance. Data are presented as mean⫾SD.
LVIDd indicates left ventricular internal dimension at end diastole; AWThd, anterior wall thickness;
FS, fractional shortening.
diomyocytes. Vascular cells were also present, depending on
the size of the sphere and time in culture. It is possible that,
as for neurospheres,19 differentiating/differentiated cells stop
dividing and/or die, whereas stem cells continue to proliferate
in an apparently asymmetric way, giving rise to many
secondary spheres and to exponential growth in vitro. Mechanical dissociation favors this process. Death, differentiation, and responsiveness to growth factors of the different
cells within the CSs could depend on the three-dimensional
architecture and on localization within the CSs.20 The spontaneous formation of spheres is a known prerogative of neural
stem cells, some tumor cell lines (LIM),21 endothelial cells,22
and fetal chicken cardiomyocytes.23 All these models (ours
included) that mimic the true three-dimensional architecture
of tissues consist of spheroids of aggregated cells that
develop a two-compartment system composed of a surface
layer of differentiated cells and a core of unorganized cells
that first proliferate and then disappear over time (perhaps
through apoptotic cell death). As well-documented in fetal
chick cardiomyocytes and endothelial cell spheroid culture,
three-dimensional structure affects the sensitivity of cells to
survival and growth factors.21,22 In particular, central spheroid
cells do not differentiate and are dependent on survival
factors to prevent apoptosis, whereas the cells of the surface
layer seem to differentiate beyond the degree that can be
obtained in two-dimensional culture and become independent
of the activity of survival factors.23 Furthermore, cell– cell
contact and membrane-associated factors, known to be important for the division of neural precursor cells,24 could be
involved in our system. This is in accordance with the notion
that stem cells (or cells with stem cell function) will only
retain their pluripotency within an appropriate environment,
as suggested by the “niche” hypothesis.25
Thus CSs can be considered clones of adult stem cells,
maintaining their functional properties in vitro and in vivo
after cryopreservation.
While the experiments performed for this article were
ongoing, two articles were published concerning the isolation
of cardiac stem cells or progenitor cells from adult mammalian hearts.26,27 Isolation of these cells was based exclusively
on the expression of a stem cell-related surface antigen: c-kit
in the first article and Sca-1 in the second one. In the first
study,26 freshly isolated c-kit⫹ Lin⫺ cells from rat hearts were
found to be self-renewing, clonogenic, and multi-potent,
exhibiting biochemical differentiation into the myogenic cell,
smooth muscle cell, or endothelial cell lineage but failing to
contract spontaneously. When injected into an ischemic heart,
these cells regenerated functional myocardium. In the second
study,27 Sca-1⫹ cKit⫺ cells from mice hearts were induced in
vitro to differentiate toward the cardiac myogenic lineage in
response to 5⬘-azacytidine. When given intravenously after
ischemia/reperfusion, these cells targeted injured myocardium and differentiated into cardiomyocytes, with and without
fusion with the host cells. Our data obtained on GFP-cKit
transgenic mice also suggest that the adult cardiac stem cell is
cKit⫹. It is possible that CSs enclose a mixed population of
cells that, as in the niche, could promote the viability of cKit
progenitors and contribute to their proliferation. The data
obtained in the present article confirm the existence of adult
cardiac stem cells/progenitor cells. More importantly, they
demonstrate for the first time to our knowledge that it is
possible to isolate cells from very small fragments of human
myocardium and expand these cells in vitro many-fold
(reaching numbers that would be appropriate for in vivo
transplantation in patients) without losing their differentiation
potential. Previously unforeseen opportunities for myocardial
repair could now be identified.
Acknowledgments
This study was supported by Italian Ministery of the University and
of the Scientific and Technological Research (MURST) and by
specific funds of the University of Rome “La Sapienza” from stem
Downloaded from http://circres.ahajournals.org/ by guest on May 2, 2014
Messina et al
cell research. We thank Gianluigi Condorelli for continuous encouragement and valuable discussion. We thank Roberto Latini and Lidia
Staszewsky in particular for their precious contribution in conducting
and analyzing in vivo experiments. We thank Sergio Ottolenghi
(Dipartimento Biotecnologie e Bioscienze, Università MilanoBicocca) for kindly providing transgenic mice. We are also grateful
to Francesco Musumeci and Fabio Miraldi for kindly supplying some
of the heart biopsy specimens. Marta Alessandrini, Dario Sirabella,
Lucia Ricci Vitiani, and Ilaria Falciatori (PhD students), University
la Sapienza of Rome, Italy, are also gratefully acknowledged for
their availability during the course of this work.
References
1. Soonpaa MH, Field LJ. Survey of studies examining mammalian cardiomyocyte DNA synthesis. Circ Res. 1998;83:15–26 .
2. Nadal-Ginard B, Kajstura J, Leri A, Anversa P. Myocyte death, growth,
and regeneration in cardiac hypertrophy and failure. Circ Res. 2003;92:
139 –150.
3. Condorelli G, Borello U, De Angelis L, Latronico M, Sirabella D, Coletta
M, Galli R, Balconi G, Follenzi A, Frati G, Cusella De Angelis MG,
Gioglio L, Amuchastegui S, Adorini L, Naldini L, Vescovi A, Dejana E,
Cossu G. Cardiomyocytes induce endothelial cells to trans-differentiate
into cardiac muscle: implications for myocardium regeneration. Proc Natl
Acad Sci U S A. 2001;98:10733–10738.
4. Laflamme MA, Myerson D, Saffitz JE, Murry CE. Evidence for cardiomyocyte repopulation by extracardiac progenitors in transplanted human
hearts. Circ Res. 2002;90:634 – 640.
5. Glaser R, Lu MM, Narula N, Epstein JA. Smooth muscle cells, but not
myocytes, of host origin in transplanted human hearts. Circulation. 2002;
106:17–19.
6. Hassink RJ, Dowell JD, Brutel de la Riviere A, Doevendans PA, Field LJ.
Stem cell therapy for ischemic heart disease. Trends Mol Med. 2003;9:
436 – 441.
7. Menasche P, Hagege AA, Vilquin JT, Desnos M, Abergel E, Pouzet B,
Bel A, Sarateanu S, Scorsin M, Schwartz K, Bruneval P, Benbunan M,
Marolleau JP, Duboc D. Autologous skeletal myoblast transplantation for
severe postinfarction left ventricular dysfunction. J Am Coll Cardiol.
2003;41:1078 –1083.
8. Preston SL, Alison MR, Forbes SJ, Direkze NC, Poulsom R, Wright NA.
The new stem cell biology: something for everyone. Mol Pathol. 2003;
56:86 –96.
9. Strauer BE, Brehm M, Zeus T, Kostering M, Hernandez A, Sorg RV,
Kogler G, Wernet P. Repair of infarcted myocardium by autologous
intracoronary mononuclear bone marrow cell transplantation in humans.
Circulation. 2002;106:1913–1918.
10. Assmus B, Schachinger V, Teupe C, Britten M, Lehmann R, Dobert N,
Grunwald F, Aicher A, Urbich C, Martin H, Hoelzer D, Dimmeler S,
Zeiher AM. Transplantation of Progenitor Cells and Regeneration
Enhancement in Acute Myocardial Infarction. Transplantation of Progenitor Cells and Regeneration Enhancement in Acute Myocardial
Infarction (TOPCARE-AMI). Circulation. 2002;106:3009 –3017.
Mammalian Adult Cardiac Stem Cells
921
11. Kelly R, Alonso S, Tajbakhsh S, Cossu G, Buckingham M. Myosin light
chain 3F regulatory sequences confer regionalized cardiac and skeletal
muscle expression in transgenic mice. J Cell Biol. 1995;129:383–396.
12. Di Lisi R, Millino C, Calabria E, Altruda F, Schiaffino S, Ausoni S.
Combinatorial cis-acting elements control tissue-specific activation of the
cardiac troponin I gene in vitro and in vivo. J Biol Chem. 1998;273:
25371–25380.
13. Hadjantonakis AK, Gertsenstein M, Ikawa M, Okabe M, Nagy A. Generating green fluorescent mice by germline transmission of green fluorescent ES cells. Mech Dev. 1998;76:79 –90.
14. Cairns LA, Moroni E, Levantini E, Giorgetti A, Klinger FG, Ronzoni S,
Tatangelo L, Tiveron C, De Felici M, Dolci S, Magli MC, Giglioni B,
Ottolenghi S. Kit regulatory elements required for expression in
developing hematopoietic and germ cell lineages. Blood. 2003;102:
3954 –3962.
15. Pennica D, King KL, Shaw KJ, Luis E, Rullamas J, Luoh SM, Darbonne
WC, Knutzon DS, Yen R, Chien KR, et al. Expression cloning of
cardiotrophin 1, a cytokine that induces cardiac myocyte hypertrophy.
Proc Natl Acad Sci U S A. 1995;92:1142–1146.
16. Sabri A, Guo J, Elouardighi H, Darrow AL, Andrade-Gordon P, Steinberg
SF. Mechanisms of protease-activated receptor-4 actions in cardiomyocytes. Role of Src tyrosine kinase. J Biol Chem. 2003;278:11714 –11720.
17. Zammit PS, Beauchamp JR. The skeletal muscle satellite cell.: stem cell
or son o stem cell? Differentiation. 2001;68:193–204.
18. Kruithof BP, Van Den Hoff MJ, Tesink-Taekema S, Moorman AF.
Recruitment of intra- and extracardiac cells into the myocardial lineage
during mouse development. Anat Rec. 2003;271A: 303–314.
19. Galli R, Gritti A, Bonfanti L, Vescovi AL. Neural stem cells: an
overview. Circ Res. 2003;92:598 – 608.
20. Layer PG, Robitzki A, Rothermel A, Willbold E. Of layers and spheres:
the reaggregate approach in tissue engineering. Trends Neurosci. 2002;
25:131–134.
21. Bates RC, Edwards NS, Yates JD. Spheroids and cell survival. Crit Rev
Oncol Hematol. 2000;36:61–74.
22. Korff T, Augustin HG. Integration of endothelial cells in multicellular
spheroids prevents apoptosis and induces differentiation. J Cell Biol.
1998;143:1341–1352.
23. Armstrong MT, Lee DY, Armstrong PB. Regulation of proliferation of
the fetal myocardium. Dev Dyn. 2000;219:226 –236.
24. Svendsen CN, ter Borg MG, Armstrong RJ, Rosser AE, Chandran S,
Ostenfeld T, Caldwell MA. A new method for the rapid and long term
growth of human neural precursor cells. J Neurosci Methods. 1998;85:
141–152.
25. Nilsson SK, Simmons PJ. Transplantable stem cells: home to specific
niches. Curr Opin Hematol. 2004;11:102–106.
26. Beltrami AP, Barlucchi L, Torella D, Baker M, Limana F, Chimenti S,
Kasahara H, Rota M, Musso E, Urbanek K, Leri A, Kajstura J, NadalGinard B, Anversa P. Adult cardiac stem cells are multipotent and support
myocardial regeneration. Cell. 2003;114:763–776.
27. Oh H, Bradfute SB, Gallardo TD, Nakamura T, Gaussin V, Mishina Y,
Pocius J, Michael LH, Behringer RR, Garry DJ, Entman ML, Schneider
MD. Cardiac progenitor cells from adult myocardium: homing, differentiation, and fusion after infarction. Proc Natl Acad Sci U S A. 2003;100:
12313–12318.
Downloaded from http://circres.ahajournals.org/ by guest on May 2, 2014
Isolation and expansion of adult cardiac stem cells from human and murine heart
Supplemental material
Materials and Methods.
Tissue samples. Human tissue was derived from atrial or ventricular biopsies belonging
to patients (aged from 1 month to 80 years) undergoing heart surgery, in conformation
with the guidelines of the Italian Department of Health. Murine tissue (was derived from
the hearts of previously characterized homozygous MLC1/3F-nlacZ (1) and cTnI-nlacZ
(2) transgenic mice (expressing a nuclear lacZ transgene under the transcriptional
control of the striated muscle myosin light chain or of cTnI promoters, respectively),
homozygous B5-eGFP mice (3), homozygous GFP-cKit (4) mice , MLC3F-nlacZ/B5eGFP, MLC3F-nlac-Z/GFP-cKit, cTnI-nlacZ/B5-eGFP cTnI-nlac-Z/GFP-cKit crossed
mice, SCID mice, and SCID beige mice (Charles River Italia., Lecco, Italy). The last two
animals lines were employed as recipient for murine and human cardiospheres because of
their non-inbred background. Samples were stored in ice cold serum-free IMDM
(Invitrogen, , Milan, Italy) and processed within two hours.
Processing, isolation, and cryopreservation of sphere-forming cells. Isolated myocardial
tissue was cut into 1-2 mm3 pieces, washed with Ca++/Mg++-free phosphate buffered
solution (PBS, Invitrogen) and digested trice for 5 min at 37 °C with 0.2% trypsin
(Invitrogen) and 0.1% collagenase IV (Sigma, Milan, Italy). The obtained cells were
discarded and the remaining tissue fragments, washed with complete explant medium
(CEM) [IMDM supplemented with 10% fetal calf serum (FCS) (Hyclone, Logan, UT),
100 Units/ml penicillin G, 100 µg/ml streptomycin, 2 mmol/L L-glutamine (Invitrogen),
0.1 mmol/L 2-Mercaptoethanol (Sigma-Milan, Italy)], were cultured as explants in CEM
at 37°C and 5% CO2. After a period ranging from 1 (embryo) to 3 weeks (adult), a layer
of fibroblast-like cells was generated from adherent explants over which small, phasebright cells migrated. These phase-bright cells were colletted by pooling two washes with
Ca++-Mg++-free/PBS, one wash with 0.53 mmol/L EDTA (Versene, Invitrogen) (1-2
min) and one wash with 0.5 g/L Trypsin- 0.53 mmol/L EDTA (Invitrogen) (2-3 min) at
room temperature, under visual control. The cells thus obtained (from 104 to 4 x 105
cells/explant) were seeded at about 0.5-2 x 105 cells/ml in poly-D-lysine-coated multiwell plates (BD, Bioscences, Milan, Italy), in cardiosphere-growing medium (CGM)
[35% complete-IMDM/65% DMEM-Ham’s F-12 mix containing 2% B27 (Invitrogen)],
0.1 mmol/L 2-mercaptoethanol, 10 ng/ml EGF, 20 ng/ml bFGF (PeproTech, London,
UK), 40 nmol/L Cardiotrophin-1 (RD), 40 nmol/L thrombin (Sigma), antibiotics and LGlu as in CEM]. Isolation of the cardiosphere-forming cells could be performed for at
least 4 times at 6-10 day intervals from the same explant. CSs were passaged every 2-3
days by partially changing of medium and mechanical trituration of the larger clusters.
Movies of cultured CSs were recorded utilizing a Nikon-COOLPIX-4500 digital-camera
connected to a Leitz inverted microscope (Germany). For cryopreservation, we utilized
CEM/DMEM-Ham-F12 (Invitrogen) 50: 50, 5% B27, 10% DMSO (Sigma) as the
freezing-medium.
BrdU labeling. CSs were labeled (0.01 mmol/L BrdU overnight), fixed and screened
according to the kit’s instructions (Roche, IN, USA).
Clonal analysis. Human CSs were transduced with a third-generation lentiviral vector,
pRRLsin.PPT-PGK.GFP expressing green fluorescent protein (GFP), as described
elsewhere (15-5). Murine CSs employed for clonal assay were derived from eGFP- or
eGFP/MLC3F-mice. After washing, GFP-labeled CSs were dissociated into single cells
by trituration in Ca++/Mg++-free PBS, Versene, and 1x trypsin-EDTA solutions in
sequence, resuspended in CGM, and then seeded at a presumed concentration of 1
cell/well in a 96-well plates or 100-500 cells/10 cm Petri dishes coated with a feeder
layer of mitomycin-C (Sigma) (3 µmol/L)-treated STO fibroblasts.
Differentiation on substrate-coated surface. Ca++/Mg++-free PBS-washed and partially
dissociated CSs were seeded in a small volume of CEM (200-300 µl) on type-I collagen(Sigma) or Matrigel- (BD) coated dishes and cultured for 3-6 days.
Co-culture experiment. Isolated primary neonatal rat cardiomyocytes were used as
described (3, 16-6, 7) for co-culture with human CSs. About 10 CSs/1x105
cardiomyocytes were employed (before and after 10 days of culture from thawing),
cultured in CEM, observed at defined times (1, 2, 4, 8 days) for movie recording and then
processed for immunocytochemical analysis. As required, GFP-labeled human CSs were
co-cultured with neonatal rat cardiomyocytes pre-stained with a red fluorescent dye (Dil,
Molecular Probes, Eugene, Oregon USA), according to Serbedzija GN et Al. (17-8) with
slight modifications. Briefly,
washed cardiomyocytes were covered with a diluted
solution (1:80) of Dil (stock of 1mg/ml absolute ethanol) in 0.3 M saccharose (Sigma)
pre-warmed at 37°C, and allowed to incubate for 5 min. at 37°C with 5% CO2. Then,
cells were extensively washed in PBS, re- feuded in their culture medium and re-
incubated at 37°C with 5% CO2. Cardiomyocytes were ready for co-cultures the day
after.
Immunocytochemistry. This was performed as described (18-9) using the following
antibodies: monoclonal (mAb) anti-human-cTnI, anti human-cardiac-MHC, anti-human
connexin-43 (Cx-43) and polyclonal (pAb) anti-human ANP (Chemicon, CA); mAb antiCD-31, CD-34 (BD), mAb anti-Ve-cadherin, anti-sca-1, mAb anti-mouse-cKit
(Pharmigen, BD), mAb anti-human-c-Kit (DAKO, Milan, Italy); pAb anti-human-vonWillebrand-factor and mAb anti-human-KDR (Sigma); mAb and pAb anti-mouse/human
MHC (18-19/9-10), and anti-Smooth-Muscle-Actin (Sigma), mAb anti-human/mousecTnI (20-11), donated by S. Schiaffino (Dep. Of Pathology, Univ. of Padua), pAb antimouse-flk-1 (Santa Cruz, USA).
Light-microscopic analysis of β-Galactosidase activity was performed as described (167).
Confocal analysis was performed with a FV500 Olympus microscope for the mice heart
cryosections, and with a Leica TCS NT for double-fluorescence of human BrdU –labeled
CSs and co-coltures of human GFP-labeled CSs with rat cardiomyocytes.
Immunofluorescence and Flow Cytometric Analysis. The mAbs used were biotinconjugated anti-mouse CD31, FITC- conjugated anti-mouse Sca-1, Biotin-conjugated
anti-mouse CD34, R-PE -conjugated anti-mouse CD117 (c-Kit) from Pharmingen (BD
Biosciences, San Diego, CA); FITC -, R-PE -and PE-Cy5-Streptavidin conjugated were
from Caltag (Burlingame, CA).
Briefly, 5x105 cells were harvested from culture, washed with PBS and stained with the
appropriate dilution of biotin- or fluorescence-conjugated mAb or a negative control for
30 min at 4°C, then washed twice with cold PBS. Then, cells were incubated for an
additional
30 min with fluorescence-conjugated streptavidin or for double
immunofluorescence with a second directly fluorescence-conjugated mAb. Those cells
incubated with biotin-conjugated mAb and fluorescence-conjugated streptavidin were
further incubated with a fluorescence-conjugated mAb and washed with PBS. The
percentage of positive cells determined over 10,000 events acquired, was analyzed by a
FACScalibur cytofluorimeter equipped with a 488-nm argon laser and CellQuest
software (BD Biosciences, San Diego, CA).
In vivo analysis.
Heterotopic transplantation. About 60 washed and pooled cardiospheres, obtained from
pre-
and
post-natal
MLC3F-nlacZ/B5-eGFP,
cTnI-nlacZ/B5-eGFP
or
MLC3F/nLacZ/CD1 and TnI-nLacZ/CD1 mice, were suspended in 100 µl of Matrigel
(BD) and sub-cutaneously injected into the dorsal region of anesthetized (ketamine, 35
mg/kg i.m) adult SCID mice. Transplanted-CSs survival and function were in vivo
monitored by direct palpation of beating through the skin. After three weeks, mice were
sacrificed and the isolated inoculum was embedded in OCT (Miles, IN, USA) for
immunocytochemical analysis.
Orthotopic transplantation. Myocardial Infarction. SCID/beige mice (Taconic Europe,
Denmark) were anesthetized with Avertin (250 mg/kg i.p.), and the trachea intubated with
a 22G venous catheter. Artificial ventilation (stroke volume, 1.0 to 1.5 mL; ventilation
rate, 120 per minute) was initiated, and a left-sided thoracotomy in the fourth intercostal
space was performed. the LAD was ligated immediately distal to the bifurcation of the
left main coronary artery, using an un-traumatic needle and a 7-0 silk thread. After
ligation, successful infarction was immediately evident by a pale discoloration of LV
myocardium due to ischemia. A suspension containing cardiospheres or PBS only was
injected a few minutes after infaction into the LV wall bordering the infarct using a 32G
needle and syringe. Each animal received four 2.5µl injections of the CS suspension (a
mean o 10 spheres/animal) or PBS. At the end of the operation, the thorax was closed,
pneumothorax reduced and tracheal tubes disconnected from the ventilator, thus allowing
free breathing. For sham operation, a control group of mice underwent an identical
surgical procedure with the exception that the LAD was not ligated. Survival rates of
mice after LAD ligation and sham operation were 71% and 100%, respectively. Animals
were sacrificed 18 days post-surgery.
Echocardiography. Two-dimension and M-mode echocardiography was performed on
conscious previously trained mice 18 days after surgery with a 13MHz linear probe
connected to an Aloka 5500 echocardiograph. (34-11).
Infarct size. Infarct size was calculated using computer-based planimetry. OCT
embedded hearts were cut from apex to base in 10 µm thick serial sections. Sections
spacing 500 µm were H&E stained and used for infarct size measurement. Infarct size
was defined as the sum of epicardial and endocardial infarct circumference divided by the
sum of total left ventricular epicardial and endocardial circumferences.
Statistics. Results are mean ± standard deviation. Differences between groups for
functional studies were tested for significance by one-way analysis of variance
(ANOVA) corrected by Bonferroni test. A value of p<0.05 was considered significant.
Refereces
1.
Kelly R, Alonso S, Tajbakhsh S, Cossu G, Buckingham M. Myosin light chain 3F
regulatory sequences confer regionalized cardiac and skeletal muscle expression
in transgenic mice. J. Cell. Biol. 1995;129:383-396.
2.
Di Lisi R, Millino C, Calabria E, Altruda F, Schiaffino S, Ausoni S.
Combinatorial cis-acting elements control tissue-specific activation of the cardiac
troponin I gene in vitro and in vivo. J Biol Chem. 1998;273:25371-25380.
3.
Hadjantonakis AK, Gertsenstein M, Ikawa M, Okabe M, Nagy A. Generating
green fluorescent mice by germline transmission of green fluorescent ES cells.
Mech. Dev. 1998;76:79-90.
4.
Cairns LA, Moroni E, Levantini E, Giorgetti A, Klinger FG, Ronzoni S,
Tatangelo L, Tiveron C, De Felici M, Dolci S, Magli MC, Giglioni B, Ottolenghi
S. Kit regulatory elements required for expression in developing hematopoietic
and germ cell lineages. Blood. 2003;102:3954-62.
5.
Follenzi A, Ailles LE, Bakovic S, Geuna M, Naldini L. Gene transfer by lentiviral
vectors is limited by nuclear translocation and rescued by HIV-1 pol sequences.
Nat. Genet. 2000;25:217-222.
6.
Glaser R, Lu MM, Narula N, Epstein JA. Smooth muscle cells, but not myocytes,
of host origin in transplanted human hearts. Circulation. 2002;106:17-19.
7.
De Luca A, Sargiacomo M, Puca A, Sgaramella G, De Paolis P, Frati G, Morisco
C, Trimarco B, Volpe M, Condorelli G. Characterization of caveolae from rat
heart: localization of postreceptor signal transduction molecules and their
rearrangement after norepinephrine stimulation. J Cell Biochem. 2000;77:529-39.
8.
Serbedzija GN, Fraser SE, Bronner-Fraser M. Pathways of trunk neural crest cell
migration in the mouse embryo as revealed by vital dye labeling. Development.
1990;108(4):605-12.
9.
Tajbakhsh S, Vivarelli E, Cusella-De Angelis G, Rocancourt D, Buckingham M,
Cossu G. A population of myogenic cells derived from the mouse neural tube.
Neuron. 1994;13:813-21
10.
Ferrari S, Molinari S, Melchionna R, Cusella-De Angelis MG, Battini R, De
Angelis L, Kelly R, Cossu G. Absence of MEF2 binding to the A/T-rich element
in the muscle creatine kinase (MCK) enhancer correlates with lack of early
expression of the MCK gene in embryonic mammalian muscle. Cell Growth
Differ. 1997;8:23-34.
11.
Ausoni S, Campione M, Picard A, Moretti P, Vitadello M, De Nardi C, Schiaffino
S. Structure and regulation of the mouse cardiac troponin I gene. J Biol Chem.
1994;269:339-346.
12.
Orlic D, Kajstura J, Chimenti S, Limana F, Jakoniuk I, Quaini F, Nadal-Ginard B,
Bodine M, Leri A, Anversa P. Mobilized bone marrow cells repair the infarcted
heart, improving function and survival. Proc Natl Acad Sci USA. 2001;98:1034410349.
SUPPLEMENTARY MOVIES (1a-b, 2a-b)
1. Mouse CSs. 1a. CSs start to beat at the beginning of their formation (after 24 h
of culture in CGM). 1b. At 10 days of culture most of the CSs continue beating.
2a-b. Spontaneous differentiation of one week old prenatal CS: cells derived from
the sphere show a synchronous contraction and an ordered arrangement.
2. Co-culture of human CSs with neonatal rat cardiomyocytes. 1a. The “sunlike” feature of the CSs evident after 96h of co-culture; beating can be observed
mainly in differentiated cells (external layers), as better
shown at 40x
magnification (1b). 2a-2a1 2a-transmission. Co-culture with GFP-labeled human
single-cell-CSs-derived clone are shown: contraction is mainly present in the
external cells migrating out from the center of the sphere and in those pleated
after dissociation of the clone (2a1). The same features can be observed in the 3a
(transmission)-b (Hoechst labeling)-c (green light and transmission) –d (green
light alone) series of movies, were co-culture of GFP-labeled human CSs with rat
cardiomocytes are shown.. 2b, 2c, 2d. Cells derived from partially dissociated
human GFP-labeled CSs are co-cultured with 6 days old rat cardiomyocytes
labeled with DiL (see methods). Records are performed in green light, so that the
rat cells, red stained, show a brown appearance. In some human cells the dye is
gone through (yellow color) suggesting that a kind of connection has been created
between the two cell populations. In the movie human GFP-labeled cells show a
lined arrangement (as in prenatal mouse CSs in the “mouse CSs movies” 2a-b).
3. Clone movies. In this series of movies, the spontaneous contraction of a clone
generated from the dissociation at single cell level of GFP-labeled mouse CSs and
cultured on growth-arrested STO-fibroblasts (see methods) is shown at different
magnifications, in transmission and green light.
SUPPLEMENTARY FIGURES
Fig. 1. Fluorescent, phase contrast, and merged images of eGFP/MLC3F-CSs-derived
clones: a, a fluorescent clone appears after 48 h of culture in mytomicin-arrested STO
fibroblast (fluorescence, phase, low and high magnification merged images are shown);
b, blue nuclear staining of a spontaneously differentiated clone with clustered, round
shaped cells and, c, same histochemical stain of an other clone grown in growth factorsfree medium, showing a more flattened feature of the cells that seem to migrate from the
center of the cluster toward the feeder layer.
Fig. 2. Fluorescence analysis of partially dissociated eGFP-labeled human CSs-derived
clone at 96 h of co-culture with rat cardiomyocytes: the same green cells that showed a
synchronous contraction with cardiocytes (see also human CSs movies 2a in the
supplementary materials), express cTnI.
Fig. 3. Fluorescence-confocal analysis of BrdU-labeled (red) human CSs for MHC
expression. As in Fig. 2a this high magnification picture shows a preferential localization
of BrdU labeled cells in the central area of the sphere.
Fig. 4. Fluorescent analysis of BrdU-labeled (red) human CSs stained for MHC (green)
and Hoechst (blue). Co-localization of BrdU labeling with the blue staining of the nuclei
is shown in the merged image (4e).
Fig. 5. a, Fluorescence-confocal analysis of BrdU-labeled human CSs for cardiac
differentiation markers: 6 µm scans (from the periphery to the center of the sphere) and
final pictures (small and large images respectively). BrdU (green), cANP (red). b-b1,
Fluorescence phenotype analysis of human partially dissociated-CSs, after four days of
culture on collagen coat in CEM: cTnI (red) and MHC expression appears in the
cytoplasm of the human cells (migrated from the sphere) showing
a triangular or
polygonal shape with a row arrangement. c-1-2, ,Fluorescence phenotype analysis of
human CSs (cryosections): (c) cTnI (red), (c1) sarcomeric myosin and (c2) vWf (green).,
Fig. 6. FACS analysis of post-natal mouse CSs-derived cells. A time course at 0 and 6
days was performed and the phenotype profile for CD34, cKit, Cd31 and sca-1
expression markers was analyzed and showed as percentage of positive events. The table
data are presented as mean + SD (n=3). *Indicates a statistically significant difference
from T 0. Representative graphics for each time points are also shown.
Fig. 7. MLC3F-nLacZ (a-a1) and cTnI-nLcZ (b-b1) mice derived CSs. Most of the cells,
derived from partially dissociated CSs and cultured for 5 days on collagen-coated
surface, show a blue staining both in the adult and embryo mice. c, d, Fluorescence
analysis of differentiating mouse CSs: MHC expression in the cells inside the sphere and
in those starting their migration is shown (c). d, Large version of Fig. 2b.
Fig. 8. Fluorescent analysis of connexin-43 expression (red) in eGFP-labeled human CSs
co-cultured with rat cardiomyocytes (as in fig. 1f): the punctuate red fluorescence in the
cell membrane of human cells is shown at high magnification.
Fig. 9. Orthotopic transplantation on a SCID-bg mouse, of cryopreserved human CSs
into the viable myocardium bordering a freshly produced infarct. a-a1, Fluorescence
analysis of myocardial repair. Images, acquired from the center of the left ventricular
anterior well, show the MHC positive stain (green) in the regeneration area of treated
heart (a), that is absent in the control (a1).Low (b) and high (b1) magnification confocal
analysis of cryosectioned left ventricular heart after 18 days from the coronary ligature,
shows viable lamin A/C expressing cells (green) in regenerating myocardium expressing
MHC (red) (b); b1, a human cell (green nucleus) is migrated and become integrated with
healthy myocardium were the sarcomers red-stained for MHC are evident.
Figure 10. High magnification of manuscript Figure 6a (In vivo analysis (ortotopic
transplantation of human CSs). The thin red stained (MHC) cytoplasmatic rings (more
evident in panels b1-b2), surround the green nuclei (Lamin A/C) of newly generated
myocytes.
a1
a2
20 µm
a4
a3
Transmission
GFP
b1
Merged
b3
b2
25 µm
GFP
c1
Transmission
Fig. 1
GFP
Transmission
25 µm
X-GAL
c2
25 µm
20 µm
c3
X-GAL
Merged
Merged
a
GFP
cTrI/hoechst
b
10 µm
c
Fig. 2
merged
a
b
MHC
BrdU
c
merged
d
MHC
Fig. 3
e
20 µm
f
BrdU
merged
20 µm
a
c
b
BrdU
hoechst
e
d
10 µm
Fig. 4
BrdU/MHC
MHC
f
Brdu/hoechst
MHC/hoechst
a
BrdU/ ANP
20 µm
a1
a2
a3
a4
c1
10 µm
MHC/hoechst
myosin
c2
vWf
vWf
b1
Human
hcTnI/hoechst
b2
MHCI/hoechst
cTnI/hoechst
20 µm
vc
3
Fig. 5
Day 0
labeling (percentage)
CSs-derived cells (FACS analysis)
40
CD 34
*
30
CD 34
20
cKit*
CD 31
10
sca-1
0
-10
cKit
0
6
CD 34
8 + 1,41
12,33333333 + 4,04
cKit*
10,65 + 1,12
29 + 7,81*
CD 31
2,5 + 3,53
sca-1
Day 6
7
*
0
4 + 2,82
time (days)
CD31
Data are expressed as mean+ SD (n=3)
* Indicates a statistically significant difference (cKit: P= 0,015)
sca-1
Fig. 6
Fluorescence inensity
5° day on collagen-coat
Mouse
MLC3F-nlacZ
a1
cTnI-nlacZ
b1
adult
10 µm
adult
b2
a2
embryo
c
20 µm
10 µm
10 µm
mMHC/hoechst
d
embryo
mcTnI/hoechst
Fig. 7
10 µm
5 µm
a
b
GFP
Connexin-43/hoechst
d
e
Figure 8
c
merged
f
Fig.
a 9
b1
b
a1
MHC
100 µm
a2
b2
b1
Lamin A/C
MHC
g
a
Fig. 10
b1
a
Lamin A/C
MHC
b2
f