Host-parasite relationship Pathogenictiy and virulence
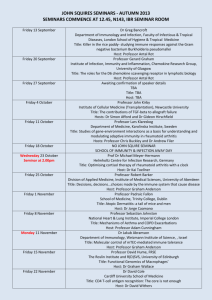
advertisement

Host-parasite relationship Pathogenictiy and virulence Pathomechanism, molecular pathogenesis, virulence factors Infection and diseases, vaccines Dr. Joseph Ongrádi Institute of Medical Microbiology Semmelweis University 2014 1 Definition of the host and the parasite • Host: macroorganism, usually multicellular phylogenetically higher level, eukaryote (animal, plant) (it could be prokaryote) • Parasite: Living on/in the host → damages → can cause disease obtaining necessities of life from the host – – – – non living: unique protein (prion), nucleic acid (viroid) non living/living: virus prokaryote: bacterium microorganism, eukaryote: microscopic fungi, microbes protozoa helmiths – vast majority of microorganisms live in the environment, minor fraction is parasite – biologically there is no sharp distinction between normal and pathogenic 2 Host-parasite relationship • Host: able to exist independently or might depend on microbes • Microorganisms: – saprophytes live in the environment – symbiosis: macro- and microorganism live together (association) • mutualism: advantageous for both (reciprocal benefit) • commensalism: do not damage each other (neutral) • parasitism: advantageous for microorganism (unilateral benefit) damages to macroorganisms → disease 3 Commensalism and mutualism in human as host • Normal microbe flora (bacteria, microscopic fungi) – on skin and mucous membranes, in gut and vagina → colonisation – host cell : microbe cell number = 1:10 – no entry, no penetration, no colonisation inside cells, tissues, organs – (in the blood: occasionally, transiently) • Viruses: no exogenous normal virus flora – (but: latent viruses /episomal, integrated/ can be shed symptomless) – Human endogenous retroviruses (HERV) • 8% of the genome = self • they code for vital functions (e.g. placenta) • Protozoa, helminths: never found in the normal flora 4 Advantages of commensalism/mutualism • For microorganisms – shelter and food – colonisation, but no entry (penetration) into tissues – (through wounds, very rarely → disease) • For the host (human) – to prevent colonisation of harmful microbes (parasites) • Occupying surface and cell receptors • Producing antimicrobial compounds (e.g. lactic acid in vagina, antibiotics) – processing/degrading food components • Producing useful metabolites (vitamin K or B12) 5 Parasite microorganisms • Inducing pathogenic conditions → diseases (>1400 species!) • Damages for human: – – – – entry/penetration from surfaces into tissues → invasivity passively through wounds (damaged tissue integrity) actively (enzymes) multiplication/replication in tissues → pathogenic effects → disease • Types of parasitism (pathogenicity, being pathogenic) – obligate parasites: in defined host (range of hosts) always pathogenic, never found in the normal flora – facultative parasites: depending on the condition of both host and microbe, presence of predisposing /risk factors, members of the normal flora – opportunistic parasites: member of the environment, not pathogenic for healthy people, take advantage in case of host disorders (usually immunosuppression) 6 Predisposing/risk factors enhancing infection I • For facultative pathogens – physical ← mental stress – acute diseases, wounds, burns – chronic debilitating conditions Diabetes, alcoholism, drug abuse, nutritional defects, tumours, leukaemia (combined with immune suppression, see later) – calculi (urinary tract, bile stone) – urinary tract obstruction – certain work conditions • Medical interventions (diagnostic and/or therapeutical) – iatrogenic – changes in the normal microbe flora ← antibiotics, other drugs – surgery, oral surgery (entry of normal, facultative or opportunistic pathogens) – prosthetics, catheters (biofilm!) • Nosocomial infections – in any health care facility, any source of infection, anybody (patients, staff, visitors) 7 Predisposing/risk factors enhancing infection II • For opportunistic microbes – immune deficiencies/defects – physiologically weak (newborns, pregnancy, elderly) immunosenescence determining life expectancy: ≈105 years • Congenital/connatal immune deficiencies – T lymphocytes = cellular immunity ↔ intracellular pathogens, protozoa, helminths – B lymphocytes = humoral immunity ↔ bacteria, fungi, protozoa – complex (T+B cells) – innate immunity (phagocyte functions, interleukin production) – complement system • Acquired immune deficiencies – – – – medication (corticosteroids, cytostatic drugs) radiation (environment, medical) tumours, leukaemia (virus) infections – especially those replicating in immune cells viruses: HHV-6, HHV-7, HIV in CD4+ T cells and macrophages EBV in B cells several bacteria, protozoa in macrophages 8 Specificity of pathogenicity, pathogenic ability • Pathogenicity – ability of the whole population of a given microbe species to elicit disease in a given host or range of hosts – species specific, defined genetically in both host(s) and microbe (yes or no, qualitative) – Koch postulates → molecular Koch postulates (determination at molecular level) • Virulence – in the level of pathogenicity – ability to elicit disease by a smaller population (tribe, strain, type) of the species – genetically determined in the smaller population only (quantitative) • High virulence ↔ low virulence ↔ avirulent (virulence is lost) – increasing virulence: mutations, GMO, bioterrorism – decreasing virulence: mutations, attenuation 9 Quantitation of virulence • Virulence can be measured (number of germs) • How many microbe (or group of microbes) defined among standard circumstances induces pathological conditions (disease, death) = dosis, dose – ID50 = infective dose inducing disease in 50% of hosts (e.g. in susceptible experimental animal) – DL50 = dosis lethalis causing death in 50% of hosts – DL90, DL100, ID100 etc. – TCID50 = tissue culture infecting dose damaging 50% of cultures • Small number of germs (1-102) → disease = high virulence – 1 calicivirus particle → enteritis (resistant to environmental conditions) • Large number of germs (≥ 105) → disease = low virulence – ≥ 105 cholera bacterium → enteritis (extremely sensitive to acidic pH) 10 Factors determining virulence • Constituents or products of microbes – genetically determined (but phenotypically dependent) • Examples of bacterial virulence factors Non-toxic Cell surface constituents • capsule (see later) • flagella, cilia → motility • fimbriae → specific ligands (adhesins) • sex fimbriae (conjugation) • pili → adherence to host cells • invasins → specific ligand to enter cells • glycocalyx/extracellular mucoid substances → biofilm Extracellular enzymes • damaging host cells Toxic • exotoxins • endotoxin (lipopolysaccharide, LPS) 11 Non-toxic virulence factors of bacteria • Capsule – polysaccharide – polypeptide (Bacillus anthracis, D-glutamic acid) • Role of the capsule – protection • mechanical, physico-chemical • biological - anti-phagocytic - masking, hiding other antigens – antigen variations in one species - immune evasion – adhesion to host cells 12 Non-toxic virulence factors of bacteria: extracellular enzymes • Secreted from living bacteria → exert effect on host cells • Examples – Antiphagocytic effect • • • • leukocidines coagulase haemolysins proteases – Facilitating invasion • • • • solubilising cells, tissues of the host streptokinase (fibrinolysin) – (surgery: cleaning wounds) collagenase hyaluronidase 13 Toxic virulence factors: exotoxins Secreted by living bacteria → effect on host cells Major characteristics – polypeptides (mostly A+B subunits), good antigens – well defined structure and effect – some of them are coded by bacteriophages Effect on the host • effect on host surfaces (extracellularly acting) – membrane damage (pore formation → loss of nutrients → cell death – superantigens: APC MHCII + TCR binding → cytokine production → toxic shock (Staphylococcus aureus: toxic shock syndrome toxin, TSST) • intracellularly acting – – – – A+B toxin (A: toxic effect or the opposite, B: cell surface binding) inhibition of protein synthesis (diphtheria) overproduction of mediators, neurotransmitters (acetylcholine → tetanus) hypersecretion (cholera toxin: Na+, Cl-, etc. → diarrhoea Measurement of toxicity – DLM = dosis lethalis minima kills all experimental animals (ng – μg) 14 Superantigens 15 Endotoxin (lipopolysaccharide, LPS) Gram negative bacteria – cell wall Major characteristics • heat stable, conserved in many Gram- bacteria, weakly immunogenic (as antigen) Importance • recognition by innate immunity: • pathogen associated molecular pattern (PAMP) • LPS → LPS binding protein → macrophages, B cells, PMNL, platelets CD14 and TLR4 binding → cell activation → overproduction of inflammatory mediators (IL-1, -8, TNF-α) Biological effects: • beneficial: small amount is immunostimulant (essential for innate immunity) eliciting inflammation → isolation of infective agents • malignant: large amount exerts systemic effects fever, vascular permeability → hypotension, acute phase proteins, hypoglycaemia, cytokine storm, DIC, thrombosis → shock →death 16 Structure of LPS 17 Effects of endotoxin 18 Onset of infection Infection: entry and replication of microorganism in macroorganism Source of infection • Exogenic infected, symptomless human, animal ill carrier environmental vehicles (soil, water, food, etc.) reservoir: animals (rodents and insects) or humans or vehicles carrying pathogenic microbes permanently • Endogenic from the normal flora (skin, mouth, gut, vagina) activation of latent/persistent microbes Contagious infections: from human to human Non-contagious infections: not from human to human 1st infection = primary infection → repeated (secondary) infection 19 Transmission of infection Horizontal spread • Direct contact – human-human, animal-human • Indirect contact – contaminated environment, objects skin, mucous membranes (sexual organs) • Vehicles – air-blow – coughing, sneezing, talking → droplet aerogenic infections – contaminated water, food alimentary/oral infections – blood sucking insects (lice, fleas, ticks, mosquitos) vector (arthropod → host /direct percutan transmission/ → arthropod) • Iatrogenic infections – direct percutaneous infections by contaminated blood/cell/organ donation, equipments Vertical spread • Next generations: transplacental, diaplacental → connatal infection (immediate or late manifestation) 20 Types of transmission 21 Infection process: entry Portals of entry (attachment and penetration) • skin and mucous membranes injuries (damage of integrity) direct penetration (arthropods) • respiratory tract (epithelial or immune cells) • gastrointestinal tract (epithelial or immune cells) • urogenital tract (ascending) Iatrogenic infections • skin, mucous membranes – wounds • implanted cells, tissues, organs • devices – syringes, canules, prosthetics, catheters (urinary tract!) Nosocomial infection • in any healthcare setting, any source, any transmission, any portal of entry, any host (patients, staff, visitor) 22 Microbial infection and shedding 23 Infection process: colonisation, dissemination Colonisation • irreversible, at or near to the site of entry • multiplication of microbes • local infections (tetanus bacterium, wart viruses) Dissemination • spreading in the body – invasion → generalised infection • tissue damage, in the blood (haematogenic), in the lymphatics (lymphogenic), canalicular (respiratory tract), ascending (urogenital tract) Consequence • microbes are found far from the portal of entry • large quantity → several pathogenic effects → disease Incubation time • symptomless period between the moment of infection (frequently unknown) to the onset of symptoms/disease outbreak • few hours – more months (HBV) • several years – decades (protozoa, tumour viruses, prions) 24 Infection process: generalization Dissemination, invasion Extremely harmful if found in the bloodstream: • bacterium – bacteriaemia • virus – viraemia • parasite (protozoon, helmith) – parasitaemia • fungus – fungaemia • toxin – toxaemia Sepsis • Infection → systemic inflammatory response syndrome (SIRS) generalized weakness, malaise, warm skin, rash high (>38°C) or low (<36°C) body temperature tachycardia (>90/min) tachypnoe (>20/min) WBC (10-12x109/L) • Aggravation: organ hypoperfusion • Septic shock: hypotension (systolic BP <90mmHg) resistant to medications • Death: multi organ dysfunction syndrome (MODS) 25 Sepsis 26 Infection process: outcome Symptomless • subclinical, silent, inapparent (or very mild, non-specific symptoms) • quick elimination of the pathogen • very important: symptomless infections in childhood result in lifelong immunity (e.g. toxoplasma) or cross immunity (HSV-1/HSV-2) • Latent – the pathogen remains in the body, activates upon intrinsic/extrinsic factors • Persistent – Viral forms of latency – episomal (herpes) or integrated (retroviruses) The pathogen activated regurarly, shed symptomless (but infects others!) • Carrier state – the pathogen is shed continuously w/o symptoms (source of infection) Manifest infection, manifestation of disease - symptoms are detected • Acute (fulminant = extremely rapid course) • Subacute • Chronic 27 Infection process: outcome Acute Chronic The pathogen disappears from the body → reconvalescence → clinical recovery Times of microbial and clinical recovery are different! Acute (mainly fulminant) Chronic The pathogen remains in the body No pathogen in the body, but irreversible damages death The above courses are natural processes Treatment (medication, antibiotics, vaccination, etc.) profoundly alters disease course! 28 Defence mechanism against pathogenic microbes Unspecific factors Inhibition of attachment, entry and facilitation of removal – skin integrity – upward synchronised movement of cilia in the respiratory tract – pH – skin – organic acids, sebum vagina – lactic acid (Lactobacilli) pH 4-5 stomach – HCl, pH 1-2 – enzymes – tear – lysozyme + blinking mouth, gastrointestinal tract – osmolarity – urine flow – accelerated peristaltic movement, vomiting 29 The role if immune system in the antimicrobial defense Functions of the immune system • recognition of pathogenic microbes (foreign, non-self) • innate immunity – immediate onset of aspecific defense mechanisms • depending on innate immunity: onset of adaptive immunity • recognition of antigens, their presentation • activation of signal transmission among different immune cell subsets (interleukines, chemokines) • mobilisation of the effector cells in the cellular and humoral immune system • destruction of microorganisms and infected cells • elimination of debris produced from microbes, infected cells and unnecessary immune cells • establishment of immune memory Primary infection = first encounter between the macro- and microorganism: above reactions Secondary/repeated infection by the same microbe: activation of immune memory 30 Recognition of pathogenic microbes Monocytes, macrophages, neutrophil phagocytes, dendritic cells • Cell surface receptrors (C-type lectin, TLR1,2,4,5,6) • Endosomal receptors (C-type lectin, TLR3,7,8,9) Recognized molecules • Conserved structures missing in mammalian organisms pathogenic associated molecular pattern (PAMP) LPS, Gram positive bacterial cell wall peptidoglycan, lipoteichoic acid, flagellin, N-formylmethionin, hypomethylated CpG-DNA, ss/dsDNA, ss/dsRNA • Intracellular components of lysed infected (virus, bacteria, protozoa) cells damage associated molecular patterns (DAMP) nuclear polypeptides, mitochondrial DNA, reactive oxygen radicals, matrix proteins, heat shock proteins 31 Activation of the innate immunity Augmented signal transduction from receptors → cascade of events • activation of interferon regulatory factors (IRF) → production of interferons (IFN-α,-β,-γ,-λ) → activation of IFN-stimulated genes (ISG, several hundreds) in immune and adjacent cells, infected cells • formation of intracellular inflammasomes (RIG-I, NLRP3, etc.) and stress granules = protein complexes • protein kinase R (PKR) activation → RNaseL activation →degradation of foreign RNA • caspase activation → programmed cell death of infected cells • release of pro-inflammatory mediators (e.g. IL-1,-2,-8, TNF-α) GM-CSF, G-CSF: phagocyte attraction 32 First signs of manifesting innate immunity • Onset of inflammation – localisation of infecting agents, preventing systemic infection/damage – increased circulation and permeability of capillary membranes → oedema – local and systemic effects of mediators pro-inflammatory cytokines (IL-1,-8,-11, TNF-α, etc.) anti-inflammatory cytokines (TGF-β, IL-4,-6,-10, etc.) attraction of immune cells/phago-, monocytes, macrophages, lymphocytes, etc. – acute phase reaction (systemic effect: fever, malaise) – production of C-reactive protein (CRP): opsonisation and/or aggregation of bacteria 33 Contribution of the complement system to innate immunity Activation and effect through different routes • Bacterial cell wall mannose → mannose binding lectin (MBL) → MASP1/MASP2 protease activation → C4/C2 split → C3 convertase → production of C3a and C3b fragments • C3a and C5a – neutrophil granulocyte chemotaxis • C3b – opsonisation: bacterium + C3b molecule + phagocyte complement receptor enhanced phagocytosis • C5b-C9 - binding Gram negative bacterial lipids → bacteriolysis bacteriocidia 34 Opsonisation 35 The role of phagocytes in the innate immunity Phagocytosis • G-CFS, GM-CSF – augmented production, chemotaxis, tissue entry • main role: kill extracellular pathogens Steps of action • binding (opsonisation +/-) → engulfment and internalisation → phagosome + lysosome fusion → killing in phagolysosome → oxygen dependent (O2-, NO-) oxygen independent (enzymes: lysosyme, lactoferrin, defensins) → digestion of killed microbes → cell death, debris → constituents of pus 36 Natural killer cells Role • to attach and destroy infected cells Natural killer (NK) cells • large, granular lymphocytes • TCR expression + Fc (CD16) receptor+, MHC- Mechanism of killing NK cell receptors + foreign antigen on target cells FasL + Fas Binding → Production of perforin: pore formation in cell membrane of target cells granzyme – intracellular induction of apoptosis 37 Adaptive immune response Role • selective destruction of pathogenic microbes • antigen dependent • different course in primary and secondary infections (immune memory) Course • • • • • • • internalisation of antigens into antigen presenting cell (APC: MØ, DC) proteolysis → peptide subunits carrying epitopes presenting subunits on MHC-I or MHC-II molecules to effector cells activation of effector cells destruction of microorganism: by antibodies ← humoral immunity destruction of infected cells: cellular cytotoxic cells ← destruction of eukaryotic pathogen: immunity 38 Adaptive immune response: activation of effectors cells I Cellular immunity • cytotoxicity: naive CD8+TCR + APC MHC-I antigen peptide → activation → binding infected cells → perforin/granzyme → cell destruction • helper function: naive CD4+TCR + APC MHC-II antigen peptide → activation → cytokine production – Th1 – boosting cellular immunity – Th2 – boosting humoral immunity Humoral immunity • B cells: BCR + Ag (repetitive epitopes) → activation BCR + Th2 cytokines + Ag → activation Plasma cells → antibody = immune globulin (Ig) production + immune memory 39 Adaptive immune response: activation of effectors cells II γ/δ T cells • Phylogenetically early γ and δ TCR + Ag recognition w/o MHC restriction → cytotoxic effects, cytokine production • γ/δ T cells + MHC-like CD1 + Ag → activation of Th1 cells → cytokine production – mucosal immunity Treg (regulatory T cells) • Control of immune reaction to inhibit immune reactions against self Ag • Abnormal functions in the elderly (immunosenescence) 40 Humoral immunity Antibody classes • IgM – produced in primary infection: rapid but transient effect • IgG – later in the course of primary infections, lifelong existence (seroconversion) Rapid production at high level in secondary infections • IgA – dimer, on the surfaces of the mucous membranes → mucosal immunity MALT (BALT, GALT) inhibition of binding of microbes to mucosal cell receptors • IgD – “natural” antibody • IgE – in allergic reactions Functional groups • Anti-adhesive antibodies, IgA – Gram+ bacteria: lipoteichoic acid – Gram- bacteria: pili • Neutralising antibodies – binding microbes (virions), exotoxins, enzymes • Opsonising antibodies – Gram+ bacteria, capsule antigens → promoting phagocytosis 41 Immune reactions against extracellular bacteria I Activation of the innate immunity • Gram- bacterial LPS: macrophage activation → cytokine production • Gram+ bacterial peptidoglycan: complement activation (alternative route) Complement activation → opsonisation • Phagocyte Fc receptor + antibody Fc + complement → rapid, efficient internalisation Major role of antibodies • • • • • IgM/IgG binding → direct bacteriocidia IgM – opsonisation, agglutination, lysis IgG – neutralisation (bacteria, toxins) Polysaccharide antigens → IgM (T independent B cell activation) S. aureus TSST → CD4+ T cell activation → cytokine storm 42 Immune reactions against extracellular bacteria II Immune evasion by bacteria • Defense strategies of microbes to avoid immune reactions – Inhibition of innate immunity weak TLR binding – S. typhi, Y. pestis, Francisella – Capsule – New antigenic variations Masking other antigens (O) – S. aureus – Fibrin cover Protein A: blocks Ig Fc fragment, host cell Ag mimicry Catalase: inactivation of lysosomal enzymes Leukocidin: membrane damage of phagocytes – S. pyogenes – Streptolysin: damages lysosomal membranes M protein: C3 inactivation 43 Immune reactions against intracellular bacteria Infection and survival in phagocytes and macrophages • • • • Immune defense: mostly cellular immunity CD4+ Th1 dominance → IL-12, TNF-α, IFN-γ production → MØ activation MØ MHC-I – Ag-expression: CD8+ T cell and NK cell activation → cytotoxycity APC MHC-II – Ag-expression → B cell activation → antibody production Immune evasion by bacteria • M. tuberculosis: macrophage damage, inhibition of activation by IFN-γ • M. tuberculosis, Legionella, Chlamydia: inhibition of the fusion between phagosome – lysosome • Shigella, Listeria, Rickettsia: damages to lysosomal membrane • Salmonella, Coxiella: inhibition of lysosomal enzymes • Neisseria, enteric bacteria: Inhibition of complement activation (“serum resistance”) Inhibition of opsonisation • Neisseria meningitidis B: self antigen mimicry 44 Immune defense against virus infections Viruses = intracellular parasites! Definitive role of innate immunity • NK cells activated by IL-12 destroy infected cells very early The role of antibodies • unenveloped viruses + Ab → phagocytosis • enveloped viruses + Ab → lysis of virions • neutralising antibodies Destruction of infected cells • phagocyte MHC-II Ag presentation → Activation of B cells → Activation of CD4+ T cells → cytokine production • many types of infected cells: MHC-I Ag presentation → CD8+ T cells activation • cells + Ab + complement → lysis, phagocytosis • ADCC: antibody dependent cellular cytotoxicity (NK Fc receptor + Ab binding) 45 Immune evasion by viruses • Replication in immune cells (HIV, HHV-6, HHV-7 in CD4+ cells) • Persistence: episomal (Herpesviridae), integration (Retroviridae) • Cell-to-cell spread avoiding antibodies (Herpesviridae) • Antigen variations - shift (influenzaviruses, rhinoviruses) • Inhibition of MHC synthesis (adenoviruses, cytomegalovirus U18 gene product) • Interleukin mimicry (Epstein-Barr virus vIL-10) • Complement fragment neutralisation (HSV-1 – C3b) 46 Immune defense against protozoa and helminths I In common speech – parasite = helminths, protozoa, arthropods (known for centuries) – medical parasitology – (microbes = bacteria, viruses, microscopic fungi) Protozoa: single cell eukaryotes (microscopic size) Helmiths: multicellular organisms (microscopic – extremely large size) Immune defense • inefficient, hardly known → chronic debilitating diseases Innate immunity • direct damage – phagocytosis • alternative complement activation – lysis Adaptive immuity • cellular immunity against intracellular parasites – cytotoxic T cells – IFN-γ activated macrophages 47 Immune defense against protozoa and helminths II Adaptive immunity • Humoral immunity against extracellular parasites – Complement activation, antibodies: opsonisation, ADCC, neutralisation – Helminths: Local inflammation, granuloma = localisation → fibrosis IgE and IgE-dependent cytotoxicity, allergy Th2 cytokine dominance (IL-4, IFN-γ, TNF-α) Immune evasion by parasites • Replication inside cells (WBC, liver: malaria, MØ: toxoplasma) • Protecting shell from host polypeptide (Schistosoma in the lung) • Enzyme production (Leishmania: antibody digestion) • Inhibition of phagolysosome fusion (Toxoplasma gondii) • Solubilisation of phagolysosome membrane (Trypanosoma cruzi) • Shift in antigen structure (vegetative forms/cysts) • Generalized immune suppression 48 Immunisation I Aim: Immunisation, vaccination – to protect against invading pathogens Different by historical times, geographical regions, target populations Forms: Active = to mimic primary infection – establishment of adaptive immunity Passive = to substitute antibodies Active immunisation • • • • • • • Introduction of antigen(s) in harmless form → primary infection → immune memory Killed microbes Living, attenuated (avirulent) microbes Attenuated toxins (toxoid) Components of microbes (antigen molecules: capsule polysaccahride, polypeptides) – Artificially produced (HPV L1, HBV surface antigen) – DNA vaccination (future) Adjuvants Slow effect (booster injections), lifelong effect 49 Active immunisation 50 Immunisation II Passive immunisation • Introduction of antibodies • Natural: foetus, breast milk (IgG, IgA) • Artificially: antibodies produced in animals, human (poly-/monovalent), “γ-globulin” • Immediate but transient effect, no immune memory Immunomodulation • Immune therapy (oncology), anti-cytokine MAbs 51 Immunisation III Risks and side effects of immunisation • Reaction (normal) → complication (rare biological effects) → accident (by the product or application) • Active immunisation – Living attenuated microbes: generalization (post-vaccination encephalitis) – (mutants → reversion: e.g. poliomyelitis virus) – Further mutations: loss of antigenicity (BCG) • Passive immunisation – Animal serum → hypersensitivity type I (anaphylaxia) and type III (Arthus reaction, serum sickness) Contraindications • Acute infectious diseases (including incubation time) • Immune system disorders, some forms of allergy • Pregnancy (living attenuated microbes) • Intervals between vaccination (weeks) Controlling • Public health authorities 52 Abnormal immune reactions: hypersensitivity Hypersensitivity reactions Early types • Type I Anaphylaxis – Sensibilisation with Ag (microbes or products, pollen, metals, hay, chemicals, etc. → IgE production → allergy, release of bioactive/vasoactive mediators + Th2 cytokines → shock (death) – Generalized or local (skin) • Type II Cytotoxic – Cell surface Ag + IgM/IgG → complement mediated lysis, NK activity, ADCC – Haptens, drugs, Rh incompatibility • Type III Immune complex (Arthus) reaction, serum sickness – Immune complexes are deposited in tissues → complement activation → chemotaxis of PMNL → local tissue damage, inflammation – (Kidney: glomerulonephritis) Late type • Type IV Cell mediated hypersensitivity – Intrcellular Ag → Th1 cytokine production → local inflammation → macrophage/T cell concentration → granuloma 53 – Tuberculin allergy, Mantoux test 54 Hypersensitivity reactions Autoimmunity and immune tolerance Immune tolerance • No immune response to a particular antigen/antigens • Most important: self antigens • Clonal selection, clonal allergy – established in foetus Automimmunity • Immune reactions to self (own) antigens • Released of sequestered antigens (cell damage) mumps virus → damage of testicular cells → inflammation → infertility • Cross reacting antibodies (microbial antigen ≡ self antigen) Streptococcus M protein – heart muscle adenoviruses – α-gliadin Klebsiella – HLA-B27 Treponema pallidum – cardiolipin Campylobacter jejuni – gangliosides Blocking antibodies, idiotype network • Variable (V) region of antibodies ≈ foreign (?) → anti-idiotypic antibodies → binding → blocking → termination of antibody response 55