1 Chapter 26: Urinary System By: Eddie Tribiana and Piers Frieden
advertisement
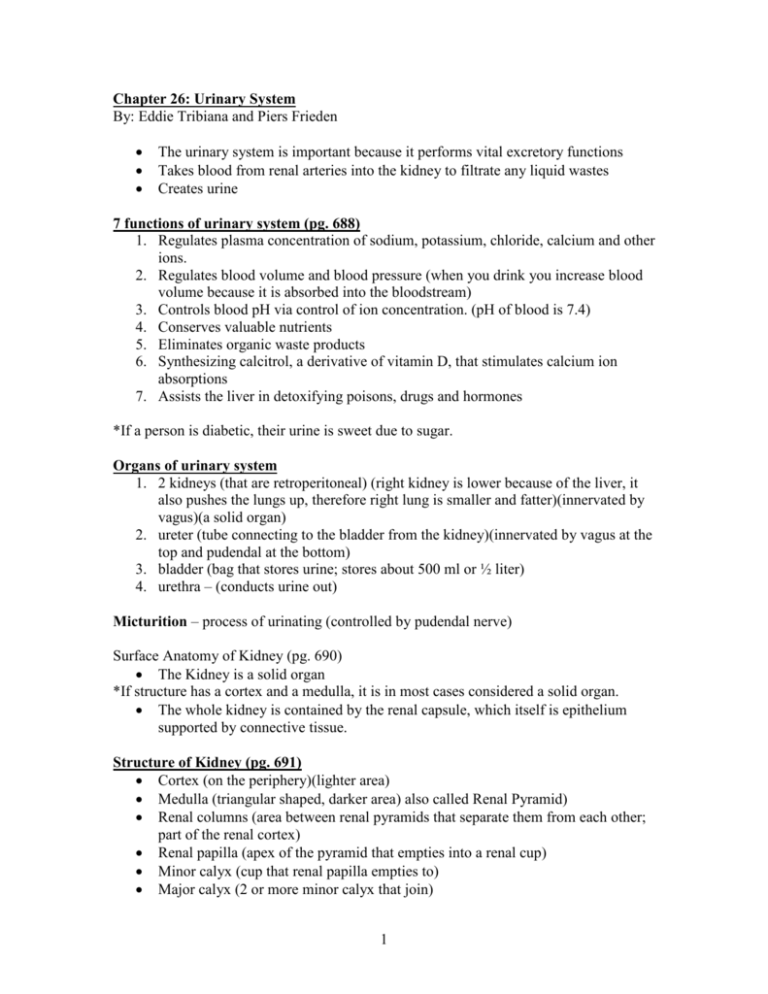
Chapter 26: Urinary System By: Eddie Tribiana and Piers Frieden • • • The urinary system is important because it performs vital excretory functions Takes blood from renal arteries into the kidney to filtrate any liquid wastes Creates urine 7 functions of urinary system (pg. 688) 1. Regulates plasma concentration of sodium, potassium, chloride, calcium and other ions. 2. Regulates blood volume and blood pressure (when you drink you increase blood volume because it is absorbed into the bloodstream) 3. Controls blood pH via control of ion concentration. (pH of blood is 7.4) 4. Conserves valuable nutrients 5. Eliminates organic waste products 6. Synthesizing calcitrol, a derivative of vitamin D, that stimulates calcium ion absorptions 7. Assists the liver in detoxifying poisons, drugs and hormones *If a person is diabetic, their urine is sweet due to sugar. Organs of urinary system 1. 2 kidneys (that are retroperitoneal) (right kidney is lower because of the liver, it also pushes the lungs up, therefore right lung is smaller and fatter)(innervated by vagus)(a solid organ) 2. ureter (tube connecting to the bladder from the kidney)(innervated by vagus at the top and pudendal at the bottom) 3. bladder (bag that stores urine; stores about 500 ml or ½ liter) 4. urethra – (conducts urine out) Micturition – process of urinating (controlled by pudendal nerve) Surface Anatomy of Kidney (pg. 690) • The Kidney is a solid organ *If structure has a cortex and a medulla, it is in most cases considered a solid organ. • The whole kidney is contained by the renal capsule, which itself is epithelium supported by connective tissue. Structure of Kidney (pg. 691) • Cortex (on the periphery)(lighter area) • Medulla (triangular shaped, darker area) also called Renal Pyramid) • Renal columns (area between renal pyramids that separate them from each other; part of the renal cortex) • Renal papilla (apex of the pyramid that empties into a renal cup) • Minor calyx (cup that renal papilla empties to) • Major calyx (2 or more minor calyx that join) 1 • Renal pelvis (2 or more major calyx that join) Pathway of urine urine (formed by kidney)> minor calyx > major calyx > renal pelvis > ureter > urinary bladder > urethra > external urethral sphincter > out Hilus (medially located in the kidney) • Artery (at apex) • Vein (ventrally located) • Renal Pelvis (posteriorly located) Arterial supply (pg. 692) • Receives blood from renal arteries • Kindeys drain to renal veins • Renal veins drain into IVC • Renal arteries are branching off from aorta Renal arteries > Segmental arteries > Interlobar arteries > Arcuate arteries > Interlobular arteries > Afferent arterioles > Glomerulus Glomerulus – a tuft of capillaries Glemerulus is part of the Nephron Nephron – functional unit of the urinary system. Without nephron, we cannot make urine. Nephron (pg.694) Glomerulus is kept in a capsule made up of epithelium called the Glomerular capsule. Glomerular capsule = Bowman’s capsule Glomerulus + Bowman’s capsule = Renal corpuscle Capillaries have simple squamous epithelium for gas exchange to occur. Renal corpuscle is where the first process of urine formation occurs. That process is called filtration. Second part of nephron looks like a corrugated board and is convoluted. It is called the Proximal Convoluted Tubule (PCT). The PCT handles the bulk of the second step in urine formation… Reabsorption PCT has simple cuboidal epithelium necessary for secretion and absorption. 2 Reabsorption occurs along all the tubules but mainly in the PCT (80 –85%) The ascending limb of loop of henle has cuboidal epithelium for absorption The collecting duct also has cuboidal epithelium for absorption Loop of Henle • Thin descending limb – has simple squamous epithelium for secretion and absorption. Water is reabsorbed. • Thick ascending limb – has cuboidal epithelium for absorption. Sodium and cloride ions are reabsorbed. Distal Convoluted Tubule • Secretion of toxins happens at the DCT • The DCT is affected by hormones such as mineralocoriticoids • End of nephron which drops urine off at the collecting duct Part of Nephron Renal Corpuscle Proximal Convoluted Tubule Loop of Henle • Descending limb • Ascending limb Epithelium Simple Squamous Simple Cuboidal with microvilli • • Simple Squamous Simple Cuboidal Function Production of filtrate Reabsorption of water, ions, and all organic nutrients • • Distal Convoluted Tubule Simple Cuboidal Part of Collecting System Collecting Duct Epithelium Simple Cuboidal Papillary Duct Simple Columnar 3 Reabsorption of water Reabsorption of sodium and chloride ions Secretion of ions, acids, drugs and toxins Variable reabsorption of water, sodium ions and calcium ions. Function Variable reabsorption of water and reabsorption or secretion of sodium, potassium, hydrogen and bicarbonate ions Delivery of urine to minor calyx Processes of urine formation 1. Filtration a. Happens at Renal Corpuscle b. Molecules that are big cannot cross cell membrane c. Water, Calcium, Sodium, Potassium, Glucose, and amino acids 2. Re-absorption a. Happens at PCT b. About 85% of water is reabsorbed c. About 55% of ions is reabsorbed 3. Secretion a. Happens at DCT b. Secretes big molecules metabolized from blood through active transport i. Ions, acids, drugs and toxins c. Variable reabsorption of water, sodium and calcium d. Aldosterone controls this portion of the Nephron for salts and minerals. There are about 3 million nephrons per kidney. Nephrons empty into a collecting duct. Collecting duct empties into the renal papilla. It is not part of the nephron Nephron ends at DCT 3 types of Nephrons 1. Cortical nephrons – nephrons in the cortex (most abundant nephrons) 2. Medullary nephrons – nephrons found on the medulla 3. Juxtamedullary nephrons – nephrons found around the borders of the cortex and medulla Urine – fluid that is in the collecting duct ADH (anti-diuretic hormone) controls collecting duct. If there is a lot of water in urine and blood volume is very low, pituitary gland will secrete ADH and go to the collecting duct to reabsorb more water until blood volume is at a homeostatic level. Peritubular capillaries – capillaries around the loop of henle. Venous Capillaries (pg. 692) Efferent Arterioles > Peritubular capillaries > Venules > Interlobular veins > Arcuate veins > Interlobar veins > Renal veins *Reabsorption involves peritubular capillaries because reabsorption happens all along the tube. 4 Urinary bladder (pg. 699) Rugae – folds of mucosa found in the bladder. Center of Trigone – a triangle within the bladder that lacks the rugae, that is formed between the openings of the 2 ureters and the neck of the urinary bladder. It does not distend. Bladder has transitional epithelium (when bladder is full, it looks like squamous epithelium and when it is empty it looks like cuboidal) The posterior wall of urinary bladder has the urethral openings. Detrusor muscle – muscle of the bladder (smooth muscle) At the neck of the urinary bladder, there is a sphincter called the internal urethral sphincter that is made up of smooth muscle (involuntary control of internal urethral sphincter). The internal urethral sphincters is stimulated by stretch receptors in the wall of bladder which tell the brain when the bladder is full. Pudendal nerve has parasympathetic involuntary function and somatic voluntary functions. Urogenital diaphragm is made of skeletal muscle. Male urethera: ~7” – 8” long 1. Prostatic urethra 2. Membranous urethra (~3”) (pierces urogenital diaphragm) 3. Penile urethra or Bulbo urethra Female urethra: ~1” – 1 ½” long 1. Membranous urethra Micturition reflex – the peristaltic movement of the urinary bladder. The detrusor muscle has stretch receptors that send message to brain that bladder is full. Brain sends message back to bladder to external sphincter to hold it (ability to hold for half an hour before next message.) Sending message between brain and bladder. Micturition reflex (pg. 705) – The process of urination that is initiated by stretch receptors in the bladder wall. If you can’t void urine, external urethral sphincter is spasming 5 Aging and the Urinary System Incontinence – Lack of ability to hold urine. Men can have problems due to an enlarged prostate. 6