SAXE-Restrepo Webinar #1
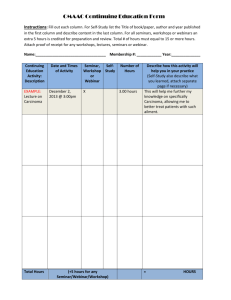
advertisement

Common, Costly, Deadly: Postoperative Respiratory Compromise Ruben D Restrepo, MD, RRT, FAARC INITIATIVES Webinar Series Show Your Control Panel Open Control Panel Closed Control Panel INITIATIVES Webinar Series Continuing Education • This activity has approved this program for 1.0 contact hour of CRCE and CNE. • At the end of this webinar, you can obtain those continuing education credits by logging on to www.saxetesting.com/init Complete the post-test and evaluation form. • Upon successful submission, you will be able to print your certificate of completion. Accreditation Statement American Association for Respiratory Care, 9425 N. MacArthur Blvd., Suite 100, Irving, TX 75063. Saxe Communications is an accredited provider of continuing education by the American Nurses Credentialing Center (ANCC) Provider (Saxe Communications) is approved by the California Board of Registered Nursing. Provider # 14477 INITIATIVES Webinar Series Commercial Disclosure This educational module was made possible through an unrestricted educational grant provided by Covidien. Unless cited, the contents and conclusions of this course are solely those of the course provider. INITIATIVES Webinar Series Our Speaker Ruben Restrepo, MD, RRT, FAARC INITIATIVES Webinar Series Disclosures Planner and Speaker: Ruben D. Restrepo, MD, RRT, FAARC Medical Advisory Board and Speaker — Teleflex Medical Investigator and Speaker – Covidien Advisory Board - Salter Labs Investigator - Fisher & Paykel Investigator – Hill Rom Nurse Planner: Lisa Caffery, RN, MSN, CIC Disclosures: No conflicts. No off-label use of products are discussed in this webinar. INITIATIVES Webinar Series Common, Costly, Deadly: Postoperative Respiratory Compromise Ruben D Restrepo, MD, RRT, FAARC Ruben D Restrepo, MD, RRT, FAARC INITIATIVES Webinar Series Learning Objectives • Define postoperative respiratory compromise (PRC). • Describe the overall impact of PRC. • Review the current recommendations to prevent PRC. INITIATIVES Webinar Series Outline • Incidence of postoperative respiratory complications • Overall impact • Risk factors • Current guidelines on respiratory monitoring • How to reduce PRC INITIATIVES Webinar Series Postoperative Complications • Postoperative Pulmonary Complications (PPCs) • Preoperative • Intraoperative • Postoperative • Postoperative Respiratory Compromise (PRC) • Respiratory insufficiency • Respiratory failure • Respiratory arrest INITIATIVES Webinar Series Postoperative Pulmonary Complications Symptoms • Fever (> 38oC) • New-onset productive cough • Change in breath sounds (rales or rhonchi) • Tachypnea • Dyspnea • Altered mental status Radiologic • Atelectasis • New infiltrates Outcomes • Prolonged postoperative mechanical ventilation (> 48 hr) • Pneumonia • Unplanned reintubation Laboratory Values • Hypoxemia (PaO2 < 60 mm Hg on RA) • Leukocytosis • Microbiology of sputum Branson RD. Respir Care. 2013;58:1974-1984. INITIATIVES Webinar Series Incidence of PPCs • PPCs = 12.5% of all surgical proceduresatients1 • Annual incidence (2–40%)1 • Twice as common as postop cardiac complications • Respiratory depression = 1.5% to 7%2-4 • By 2019, anticipate a 31.6% increase (1.3 million cases)5 1. 2. 3. 4. 5. Branson RD, Respir Care. 2013;58:1974-1984. Smetana GW, Cleve Clin J Med. 2009;76:S60-5. Dimick JB, J Am Coll Surg. 2004;199:531-537. Hall RE, Am J Cardiol. 1997;79:1680-1682. Agarwal SJ, Academy Health Congress, June 2011. INITIATIVES Webinar Series Incidence of and Risk Factors for Pulmonary Complications after Nonthoracic Surgery • 1,055 June 2001 – October 2003 • 321 inguinal hernia repairs • 238 orthopedic limb surgeries • 92 upper abdominal surgeries • 28 suffered a PPC within 7 days of surgery • 13 developed respiratory failure • 9 contracted postoperative pneumonia (1 died) • 5 cases of atelectasis • 1 pneumothorax • LOS 27.9 days vs. 4.5 days (p = 0.006) McAlister FA, et al. AJRCCM. 2005;171:514-517. INITIATIVES Webinar Series Association between Preoperative/Operative Variables and the Occurrence of Postoperative Pulmonary Complications Variable n OR (95% CI) p Value Age > 65 years 332 5.73 (2.49-13.15) < 0.001 Sx > 2.5 hours 321 5.07 (2.27-11.33) < 0.001 Perioperative NG tube 66 13.50 (6.08-29.96) < 0.001 Upper abdominal incision 92 4.49 (1.92-10.50) < 0.002 Positive cough test, smoked >40 pack-years, hx of COPD, FEV > 9 sec, daily productive cough 353 2.71–4.28 0.01–0.04 McAlister FA, et al. AJRCCM. 2005;171:514-517. INITIATIVES Webinar Series ACP systematic review of Postoperative Pulmonary Complications after Noncardiothoracic Surgery PPCs Level of Evidence PPCs Reintubation Prolonged intubation Pneumonia I; good Results 20% vs. 17% 0-2.9% 7-22% 0-2.8% Respiratory failure Overall infection I; fair 30% in IV group; 23% epidural 47% in IV group; 43% epidural Death Respiratory failure Pneumonia I; fair 4% vs. 3% 10% epidural vs. 14% IV 5% epidural vs. 8% IV Pneumonia Lobar atelectasis Respiratory failure I; fair Overall PPCs: 16% epidural; 23% IV Atelectasis Pneumonia Respiratory failure I; poor 23% epidural vs. 18% 3% vs. 3% I; poor 20% epidural vs. 28% IV; 40% IM morphine 4% epidural vs. 20% IV; 24% IM morphine Lung expansion therapy: IS; deep-breathing exercises; CPAP Lawrence VA, et al. Ann Intern Med. 2006;144:596-608. INITIATIVES Webinar Series Overall Impact of PPCs • Increased morbidity and mortality • Increased length of stay • Lack of rapid identification INITIATIVES Webinar Series Clinical Burden • Increased mortality • 300-fold increase in 30-day mortality1 • 147-fold increase in abdominal reconstruction2 • Failure to wean vs. complication-free patients3 • 30-day mortality = 29% vs. 2% • 1-year mortality = 56% vs. 9% • 5-year mortality = 78% vs. 42% 1. Gupta PK, et al. Head Neck. 2012;34:321-327. 2. Fischer JP. Plastic Reconstr Surg. 2013;132:826e-5e. 3. Khuri SF, Ann Surg. 2005;242:326-341. INITIATIVES Webinar Series Clinical Burden • Twice the number of readmissions within 30 days1 • 87% reduction in median survival in patients with PPC2 • Precipitating cause of cardiac arrest 1. Sigl JC, et al. Annual Meeting of the ASA 2010:A859. 2. Khuri SF, et al. Ann Surg. 2005;242:326-341. INITIATIVES Webinar Series Clinical Burden of Respiratory Insufficiency • 2010 AHRQ statistical brief • Respiratory insufficiency, arrest and failure (RIAF) is one of the five conditions resulting in the most rapidly increasing hospital costs for Medicare-covered stays in the U.S.1 • Inpatients with RIAF originate on the general care floor. • Higher mortality rates (34.6%) than non-RIAF cases (1.2%) 2 • Postoperative respiratory failure has become a hospital focus under Medicare’s Inpatient Quality Reporting Program (Patient Safety Indicator #11).1 1. Wier LM, Healthcare Cost and Utilization 2010. 2. Zhan C, Miller MR. JAMA. 2003;290:1868-1874:764. INITIATIVES Webinar Series Cost of Care • PPC case attributable cost = $52,0001 • $1.05 billion to $23.5 billion2-3 • In 2007, RIAF were related to 385,800 inpatient stays costing $7.7 billion.3 • Significantly longer LOS (2 days longer than cardiac complications)2 • Inpatients with RIAF originate on the general care floor • Longer lengths of hospital and ICU stays than non-RIAF cases (11.5 vs. 5.8 days and 4.1 vs. 2.9 days, respectively).5 1. 2. 3. 4. 5. Dimick JB, et al. J Am Coll Surg 2004;199(4):531-537. Wier LM, et al. AHRQ Brief #91. June 2010. Reed K, May R. 7th Annual HealthGrades Patient Safety in US Hospitals. June 2010. Lawrence VA, et al. J Gen Intern Med. 1995;10:671-678. Wi Kelley SA, Crit Care Med 2012;40:764. INITIATIVES Webinar Series Risk Factors Preoperative • Age > 50 years • ASA class > 2 • Liver disease • Congestive heart failure • Cancer • COPD • Cigarette use • Obesity • OSA • Impaired sensorium • Corticosteroid use • Alcohol use Intraoperative • Surgery longer than 3 hr • Emergency surgery • Perioperative blood transfusion • General anesthesia • Use of NMB agents • Type of surgery • • • • • • Open aortic resection Head and neck surgery Upper abdominal surgery Thoracic surgery Neurosurgery High tidal volume Branson RD. Respir Care. 2013;58:1974-1984. INITIATIVES Webinar Series Patients at Risk for Respiratory Compromise • Postoperative Patients (includes all high-risk patients) Advanced age • Organ system dysfunction • Concurrent CNS depressant use • Preoperative chronic opioid tolerance • Obesity • • Body needs more oxygen Increased weight = increased work of breathing Weinger M, Lee L. APSF Newsletter. 2011;26(2):21-40. INITIATIVES Webinar Series Patients at Risk for Respiratory Compromise (cont’d) • Obstructive sleep apnea (OSA) • 2% in women and 4% in men; majority are undiagnosed1 • High prevalence of OSA patterns after surgery, usually due to narcotics2 • Increased risk on days 2-3 (less monitoring, less pain, increased sleep)3 • Opioid usage • Directly depresses the central respiratory drive • Fear of respiratory depression is one of the major barriers to effective use of opioids to manage post-op pain4 1.Mirrakhimov AE, et al. BMC Pulm Med. 2013;13:10. 2.Blake DW, et al. Anaesth Intensive Care. 2009;37:720-725. 3.Parikh SN, et al. J Arthroplasty. 2002;17(5):635-642. 4.Brockopp D, et al. Int J Nurs Stud. 1998;35:226-232. INITIATIVES Webinar Series Intraoperative Factors Anesthesia Decreased cortical response – lower drive Loss of muscle tone Loss of airway patency Suppression of neural and muscular activity Reduced response to asphyxia Branson RD. Respir Care. 2013;58:1974-1984. INITIATIVES Webinar Series How to Reduce PPC? INITIATIVES Webinar Series Meta-Analyses and RCT of Lung Expansion Interventions to Prevent PPCs Author, Year Type of Sx Intervention Studies/RCT Thomas and McIntosh, 1994 Upper abdominal IS, IPPB, DBEs 116/14 Overend, 2001 Upper and lower abdominal IS, IPPB, DBEs, CPAP, PEP, or CPAP with PT 85/4 Chumillas et al, 1998 Upper abdominal DBEs vs. no prophylaxis Fagevik Olsen et al, 1997 abdominal DBEs vs. no prophylaxis DBEs + PEP vs. no p. Hall et al, 1991 abdominal IS, CPT Hall et al, 1996 abdominal IS v. DBEs IS vs. IS + CPT Intra-abdominal vascular NCPAP 12h vs. NC Bonner et al, 2002 Lawrence VA, et al. Ann Intern Med. 2006;144:596-608. INITIATIVES Webinar Series Meta-Analyses and RCT of Lung Expansion Interventions to Prevent PPCs n PPCs/Outcomes Level of Evidence Intervention (n of studies) Results 1337 Atelectasis or infiltrate I; poor Is vs. no Tx (2) OR 0.44; 95% CI .18-.99 IS vs. IPPB (3) OR 0.73; 95% CI .39-1.36 IS vs. DBE (4) OR 0.91; 95% CI .57-1.4 IPPB vs. DBE (2) OR 0.94; 95% CI .28-3.17 81 Bronchitis, atelectasis, pneumonia I; poor DBE Fewer CXR abnormalities (15% vs. 39%; p=0.02) Fewer PPCs (8% vs. 20%; p=0.11) 368 Pneumonia I; poor DBE 0.6% vs. 7% no Tx; p<0.05 876 Abnormal CXR and microbiology sputum I; poor IS vs. CPT (NSD) CXR (16% vs. 15%); PPCs (22% both) 456 Abnormal CXR and microbiology sputum I; poor IS vs. CPT PPCs (8% vs. 11%); p=0.50 I; good NCPAP vs. conventional Hypoxemia 5% vs. 16%; p=0.01 Pneumonia 2% vs. 5%; p=0.45 Reintubation 1% vs. 5%; p=0.21 204 Pneumonia, severe hypoxemia Lawrence VA, et al. Ann Intern Med. 2006;144:596-608. INITIATIVES Webinar Series Strength of Evidence for Specific Interventions to Reduce Risk of PPCs Strategy Strength of Evidence Type of Complication Studied Lund expansion modalities A Atelectasis, pneumonia, bronchitis, severe hypoxemia Postoperative NG decompression B Atelectasis, pneumonia, aspiration Short-acting NMB B Atelectasis, pneumonia Laparoscopic vs. open operation C Spirometry, atelectasis, pneumonia Smoking cessation I Postoperative ventilatory support Routine parenteral/enteral nutrition D Atelectasis, pneumonia, empyema, RF Lawrence VA, et al. Ann Intern Med. 2006;144:596-608. INITIATIVES Webinar Series I COUGH: a Multidisciplinary Patient Care Program to Reduce PPCs 1. Incentive spirometry 2. Coughing and deep breathing 3. Oral care (brushing teeth and using mouthwash daily) 4. Understanding (patient and family education) 5. Getting out of bed frequently (3 times daily) 6. Head-of-bed elevation Cassidy MR, et al. JAMA Surg. 2013;148:740-745. INITIATIVES Webinar Series Before and After I COUGH: Pneumonia Risk Pneumonia raw data from BMC % Pneumonia raw data from comparable hospitals % Pneumonia risk-adjusted BMC (CE ratio or CR) I COUGH Transition After I COUGH 3.0 3.0 2.5 2.5 2.0 2.0 1.5 1.5 2.0 2.0 0.5 0.5 July 2008 to June 2009 CY 2009 July 2009 to June 2010 CY 2010 Risk-Adjusted Ratio (OE Ratio or OR) Raw Data % Before I COUGH July 2010 to June 2011 Cassidy MR, et al. JAMA Surg. 2013;148:740-745. INITIATIVES Webinar Series Before and After I COUGH: Risk of Unplanned Intubation Unplanned intubation raw data from BMC % Unplanned intubation raw data from comparable hospitals % Unplanned intubation risk-adjusted BMC (OE ratio or OR) I COUGH Transition After I COUGH 2.3 2.3 2.0 2.0 1.7 1.7 1.4 1.4 1.1 1.1 0.8 0.8 0.5 0.5 July 2008 to June 2009 CY 2009 July 2009 to June 2010 CY 2010 Risk-Adjusted Ratio (OE Ratio or OR) Raw Data % Before I COUGH July 2010 to June 2011 Cassidy MR, et al. JAMA Surg. 2013;148:740-745. INITIATIVES Webinar Series How to Reduce PRC? • Comprehensive and rigorous monitoring strategy • 77% records missing a vital sign11 • Respiratory rate — least documented VS • Delayed interventions occur in 50% of patients with respiratory distress, with a median duration of delay of 12 hr.2 • Early detection of RC determines success of interventions32 • Reduces rescue calls • Reduces ICU admissions • Higher risk for PRC in first 24 hours4 1. 2. 3. 4. Chen J, et al. Resuscitation. 2009;80:35-43. Quach JL, et al. J Crit Care. 2008;23:325-331. Taenzer AH, Anesthesiology. 2010;112:282-287. Taylor S, et al. Am J Surg. 2005;190:752-756. INITIATIVES Webinar Series Continuous Monitoring of Respiratory Function Purpose: Notifies medical professionals of conditions which may, if unaddressed, lead to adverse events. • The Anesthesia Patient Safety Foundation recommends that health care professionals “consider the potential safety value of continuous monitoring of oxygenation and ventilation in patients receiving PCA or neuraxial opioids in the postoperative period.”1 • In patients undergoing PCA, continuous oximetry and capnography monitoring reveal frequent desaturation and bradypnea.2 • Continuous monitoring with pulse oximetry provides early detection of physiological decline, reducing rescue events & ICU transfers.3 1. Weinggarten TN, et al. Curr Opin Anaesthesiol. 2013;26:116-125. 2. Overdyk FJ, et al. Anesth Analg. 2007;105(2):412-418. 3. Taenzer AH, Anesthesiology. 2010;20-28. INITIATIVES Webinar Series Monitoring Guidelines Organization Continuous SpO2 for patient at risk for RC ASA APSF ASPMN JC X X X X X X X Continuous capnography for patients at risk for RC Continuous monitoring by telemetry may be used X X ASA = American Society of Anesthesiologists APSF = Anesthesia Patient Safety Foundation ASPMN = American Society for Pain Management Nursing JC= Joint Commission INITIATIVES Webinar Series Respiratory Rate (RR) • Respiratory abnormalities are the most common prior to ICU admission1 • Abnormal RR = strong predictor of in-hospital mortality2 1. Peberdy MA, et al. JAMA. 2008;299:785-792. 2. Buist M, et al. Resuscitations 2004;62:137-141. INITIATIVES Webinar Series Association Between Clinically Abnormal Observations and Subsequent In-hospital Mortality: a Prospective Study RR<6 / min M.Buist et al./ Resuscitation 62 (2004) 137-141 Decrease of consciousness Loss of consciousness Fitting Tachypnea Bradycardia Hypertension Tachycardia Hypotension SaO2<90% 0 10 20 30 40 50 60 Percent of Total Buist M, et al. Resuscitations 2004;62:137-141. INITIATIVES Webinar Series Association Between Clinically Abnormal Observations and Subsequent In-hospital Mortality: A Prospective Study 40 30 20 10 0 Independent Predictors of Mortality Buist M, Resuscitation 2004;62(2):137-141 . Event Odds Ratio (95% CI) Bradypnea (RR < 6) 14.4 (2.6 - 80.0) Tachypnea (RR > 30) 7.2 (3.9 - 13.2) Loss of consciousness 6.4 (2.9 - 13.6) Decrease of consciousness 6.4 (2.6 - 15.7) Hypotension 2.5 (1.6 - 4.1) Hypoxemia (SpO2 < 90%) 1 2 2.4 (1.6 - 4.1) 3 4 100 80 60 40 20 0 Number of abnormal observations Extremes of respiration rate are strong predictors of in-hospital mortality on the general ward. Buist M, et al. Resuscitations 2004;62:137-141. INITIATIVES Webinar Series Percent of mortality Prevalence (%) 50 Respiratory Rate (RR) • Respiratory abnormalities are the most common prior to ICU admission1 • Abnormal RR = strong predictor of inhospital mortality2 • Strongest predictor of ICU admission (> 35 bpm)3 • OR 9.1 (95% CI, 3.5–23.8)2 1. Peberdy MA, et al. JAMA. 2008;299:785-792. 2. Buist M, et al. Resuscitation. 2004;62:137-141. 3. Barford C, et al. Scand J Trauma Resusc Emerg Med. 2012;20-28. INITIATIVES Webinar Series Monitoring Devices • Oxygenation • Ventilation INITIATIVES Webinar Series Pulse Oximetry Image provided by R. Restrepo INITIATIVES Webinar Series Continuous SpO2 • Reduces ICU stay and estimated cost of ICU care • Postoperative hypoxemia • SpO2 < 90% for at least 30 seconds • SpO2 alarms (90% and 10 sec) wireless pager violations1,2 • ≈ 75% reduction of rescue events • ≈ 50% reduction in ICU transfers 1. Ochroch EA, et al. Anesth Analg. 2006;102:868-875. 2. Taenzer AH, et al. Anesthesiology. 2010;112:282-287. INITIATIVES Webinar Series Pulse Oximetry for Perioperative Monitoring Hypotheses tested: • Use of pulse oximetry is associated with improvement in detecting and treating hypoxemia. • Early detection and treatment of hypoxemia reduces morbidity and mortality in the perioperative period. • Use of pulse oximetry per se reduces morbidity and mortality in the perioperative period. • Use of pulse oximetry reduces unplanned respiratory admissions to the ICU, decreases the length of ICU readmission, or both. Pedersen T, et al. Cochrane Database Syst Rev. 2014;3:CD002013. INITIATIVES Webinar Series Pulse Oximetry for Perioperative Monitoring Implications for practice: • The proliferation of monitors in anesthesia is obvious. • The goal of monitoring as an adjunct to clinical decision making is to directly reduce the incidence of complications. • Unambiguous, accurate information helps clinicians choose and initiate correct therapeutic interventions. • The human factor—the individual clinician’s action—is perhaps far more important than implementing new monitoring equipment or other new safety initiatives in situations where we wish to reduce the rate of postoperative complications. • Can pulse oximetry protect against the human factor? Pedersen T, et al. Cochrane Database Syst Rev. 2014;3:CD002013. INITIATIVES Webinar Series Pulse Oximetry for Perioperative Monitoring Implications for practice: • SpO2 monitoring substantially reduced the extent of perioperative hypoxemia. • SpO2 enabled the detection and treatment of hypoxemia and related respiratory events and promoted several changes in patient care. • The implementation of perioperative pulse oximetry monitoring was not, however, the breakthrough that could reduce the number of postoperative complications. • The data suggest that there may be a benefit for a population at high risk of postoperative pulmonary complications. Pedersen T, et al. Cochrane Database Syst Rev. 2014;3:CD002013 INITIATIVES Webinar Series Why Capnography? Because ventilation and oxygenation are VERY different concepts. Image provided by R. Restrepo Image INITIATIVES Webinar Series Oxygenation and Ventilation The process of getting O2 into the body Ventilation Oxygenation 2-separate physiologic processes Provided by permission from Covidien The process of eliminating CO2 from the body INITIATIVES Webinar Series Important but Different Measurements etCO2 • Reflects ventilation • AH and apnea detected immediately SpO2 • Reflects oxygenation • Values lag with AH and apnea “Cases of respiratory depression were 28 times as likely to be detected, if they were monitored by capnography, as those who were not monitored.” “… end tidal carbon dioxide monitoring is an important addition to oximetry for detecting respiratory depression.” Waugh J, et al. Respir Care. 2007;52(11) INITIATIVES Webinar Series Oxygenation vs. Ventilation Now hold your breath... Note what happens to the 2 waveforms How long did it take the EtCO2 waveform to go flat line? How long did it take the SpO2 to drop below 90%? INITIATIVES Webinar Series Continuous EtCO2 • May provide earliest indicator of RC • Hypercapnia can occur with normal SpO2 • ASA recommends capnography for deeply sedated patients • Overdyk (2007) • 178 patients received PCA • SpO2 < 90% = 12% • RR < 10 x 3 min (41%) and x 2 min (58%) Overdyk FJ, et al. Anesth Analg. 2007;105(2):412-418. INITIATIVES Webinar Series Capnography CO2 (mmHg) Slow respirations – opioid/ sedative effect 40 0 Time CO2 (mmHg) Shallow, irregular breathing – partial airway obstr. (OSA 40 0 Time CO2 (mmHg) 40 Rebreathing 0 Time CO2 (mmHg) 40 Apnea, agonal breathing 0 Time Graphs provided by R. Restrepo INITIATIVES Webinar Series SpO2 plus EtCO2 • PCA patients • 65% reduction in overall adverse effects and cost • Obstacles to implementation • Alarm fatigue (95% of hospitals surveyed) • Single monitor preferred (71%) Wong M, et al. Physician-Patient Alliance for Health and Safety. 2013. INITIATIVES Webinar Series Image provided courtesy of Covidien 1. Linde-Zwirble WL, Bloom JD, Mecca RS, Hansell DM. Postoperative pulmonary complications in adult elective surgery patients in the US: severity, outcome and resources use. Crit Care Med. 2010;14: P210. 2. Agarwal SJ, Erslon MG, Bloom JD. Projected incidence and cost of respiratory failure, insufficiency and arrest in Medicare population, 2019. Abstract presented at Academy Health Congress, June 2011. 3. Wier LM, Henke R, Friedman B. Diagnostic Groups with Rapidly Increasing Costs, by Payer, 2001 -2007. Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality. Statistical Brief #91. June 2010. Available at: http://ww.hcupus.ahrq.gov/reports/statbriefs/sb91.pdf 4. Kelley SD, Agarwal S, Parikh N, Erslon M, Morris P. Respiratory insufficiency, arrest and failure among medical patients on the general care floor. Crit Care Med. 2012;40(12):764. INITIATIVES Webinar Series Conclusion 1. Respiratory compromise is common, costly, and deadly. 2. Current monitoring regimens may be inadequate for preventing respiratory compromise and other adverse events. 3. Current monitoring practices are inconsistent and suboptimal. 4. Adverse events are frequently preceded by respiratory abnormalities. 5. Continuous monitoring of respiratory function provides notification to the medical professional of conditions which may, if unaddressed, lead to adverse events. INITIATIVES Webinar Series Continuing Education • This activity has been approved for 1.0 contact hour of CRCE and CNE. • At the end of this webinar, you can obtain those continuing education credits by logging on to www.saxetesting.com/init • Complete the post-test and evaluation form. • Upon successful submission, you will be able to print your certificate of completion. Accreditation American Association for Respiratory Care, 9425 N. MacArthur Blvd., Suite 100, Irving, TX 75063. Saxe Communications is an accredited provider of continuing education by the American Nurses Credentialing Center (ANCC) Provider (Saxe Communications) is approved by the California Board of Registered Nursing. Provider # 14477 INITIATIVES Webinar Series This webinar has been recorded and will be archived on www.initiatives-patientsafety.org for on-demand viewing. You can also obtain CE/CRCEs for viewing and completing the on-demand webinar. INITIATIVES Webinar Series Questions & Answers INITIATIVES Webinar Series