Role of Nurses at OPD for Dengue patients
advertisement

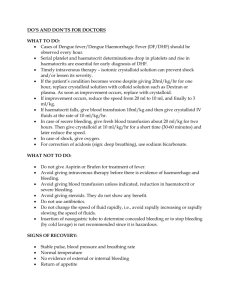
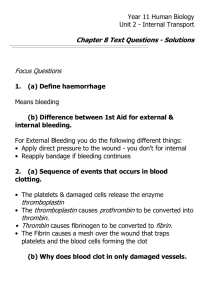
Monitoring for nurses alert in Dengue patients Rasana Waleerattanapa RN. Queen Sirikit National Institute of Child Health Medical Service Department, Ministry of Public Health Bangkok, Thailand Leading factors of the spreading of Dengue Population explosion Migration Increasing urbanization Early rainy season Contents: Transmission Pathophysiology History Screening Equipment Laboratory alert Health education 1.Transmission of Dengue Virus Extrinsic incubation 8-10 days Viremia High fever Intrinsic incubation 5-8 days 2. Pathophysiology Plasma Water Removal: Components of Whole Blood Plasma (55%) •92% water •8% solutes •Albumin •Fibrinogen •immunoglobulin Cellular Components (45 %) •RBC •WBC •Platelets Hallmark Abnormal hemostasis • Increased capillary fragility TT+ petechiae / Bursie •Thrombocytopenia - Platelet drop • Hepatomegaly • If server to be DIC Hypovolemic shock Plasma leakage 24-48 hrs. Into serous spaces Viscosity Hct. rising Hemodynamic change Volume decreased Decreased Cardiac output Circulatory change Pleural peritoneal Principle of treatment for Dengue Volume replacement therapy Effective circulatory Adjust rate IV Transfusion by - Hct. - Clinical - Vital sings - Urine output If the patient had got bleeding should be give blood component How to use electrolyte solution Crystalloid :- Isotonic solution - Osmotic P.= Plasma - 5%D/NSS,5%DLR,5%DAR Colloidal solution:- Plasma expander : - Osmotic Pressure > Plasma 2-3 times, e.g. 10% Dextran-40 - Plasma substitute: Osmotic pressure = plasma, - e.g. plasma, 3.History • Had got high fever T> 39oc • Come from epidemic area • Taken antipyretic –Paradol Temp not decease • No URI symptoms just only new born • Around house – Had people got Dengue • Shopping to see the doctors at clinic,private hospital Who’s screening cases for DHF? Health personnel Screening OPD Ward • Epidemic area • High fever • History Day of Fever • Lab CBC- Hct wbc,Plt. • No fever reduce • Lab CBC Pre sent Tourniquet test .Fragility After take cuff off Don’t count immediately Wait for skin color appear normal Tourniquet Positive test When there is > 10petechii per square inches False negative tourniquet test Obesity Very thin Not good technique During Shock petechiae no appear Good technique – Pressure drop 4.Equipment: Micro- centrifuge Microscope Sphygmomanometer Supplies for using Oral rehydration solution and IV Fluid solution ORS : Na 90 mEq Na 75 mEq Na 45 mEq Kind of solution 5. Laboratory Complete blood count o Hematocrit > base line o White blood cell < 5,000 o Platelet < 100,000 o Lymphocyte + Day of Fever ( D3,D4,D5) CBC เปรียบเทียบผล 18 6.Health Education Explained nature disease Home care: Bed rest, Soft diet, tepid sponging Follow up everyday with CBC Warning signs shock Prevention control -Get rid mosquito Observation another person may be Infected Dengue virus if high fever Screening case by take “ Tourniquet test” Roles of Nurses for caring DF/DHF Patients Natural course of Dengue 1. Febrile Phase - high fever 2- 7 day 2. Critical/ Leakage Phase/ - Plasma leakage - In 24-48 hrs. - Shock 3. Convalescence Phase – - Recovery 2 – 7 days 1. Febrile Phase Problem o High fever/ headache/ retro – orbitalpain o Dry lip, sore throat o arthralgia o Anoxia, nausea, vomiting o Abdominal pain Nursing Care: Vital signs q 4 hrs. – observe signs no fever Force ORS Monitoring rate IV & Care Follow result laboratory and notify Observe signs abnormal and notify Record Intake/Output Education to parent about course of Dengue role of caring and prevention control 2.Leakage phase Major complaints: - Plasma leakage – Hct rising - Plt. drop - Circulatory disturbance CR delay, bleeding - Hepatomagary – Liver enlarge During time leakage 24 – 48 hrs. Principle for nurses monitoring Record Time Start Shock and Temp. Count time after Temp. ( 24- 48 hrs.) - During time leakage 24 -48 hrs. - After Shock then 6 hrs,12 hrs,24 hrs. Record IV Infusion, Type IV Record urine /Shift Notify Dr. Abnormal Signs &symptoms 1.Vital signs alert? Rasana 06/12 Temperature every 4 hrs. Temp.= 37.6 -38.4⁰ C Temp.= 38.5 -39.0⁰ C Temp.= 39.1 – 40.0⁰C Temp.= > 40.1⁰ C Low Fever Middle Fever High Fever Very Fever Pulse Rate = Peripheral pulse. Effective= Heart Pumping and Circulatory Assessment - pulse rate - อัตราการเต้น - rhythm- จังหวะการเต้น -amplitude - คลื่นกระทบ - contour- ลักษณะ Volume: - Full (F) ความแรง - Moderate (MF) - Weak pulse ( W) - Palpable Blood Pressure Blood pressure (Manual/ digital) – circulatory status - Bleeding Assessment – PP < 20 mmHg - Narrow pulse pressure 100/80,90/70, 100/100 - Hypotension – 70/60 - Wide pulse pressure – Recovery - Hypertension – Volume load Respiratory rate Assessment Rate 1 /min Rhythm -regularity, Dyspnea Depth Abnormal RR: > 60/ min Age 0-2 month > 30/min Age 2 month – 1 years > 40/min Age 1 – 5 years > 28/min Age > 5 years Vital Signs Alert • BP PR q 2 hrs. -if no fever or platelet <100,000 • - q 30 – 1 hr. in Shock gr III, IV o Severity 4 grade - Non Shock gr I.II - Shock gr III, IV o Shock gr II- PP narrow Pulse rapid o Shock gr IV – BP , Pulse palpable Early signs and symptoms When there is no fever ( or the peak of fever is lower Not good symptoms Restless, Irritable Drowsy, very weak Refuse to eat and drink Very thirsty Have cool extremities Severe Abdominal pain Persistent vomiting Behavioral change Cold clammy, Mottling skin No urine for 4-6 hrs BP Narrow < 20 mmHg Rapid Pulse increase rate Capillary Refill time > 2 sec. Sings bleeding Bleeding per gum Epitaxis Coffee ground Melena Menstruation Shock 2.Symptoms alert? Problem in Dengue Shock case o Plasma leakage – Hct. rising Hemodynamic change - Narrow Pulse pressure BP 100/80 - Rapid pulse - Delay capillary refill - Cold clammy skin Nursing Diagnosis: o Shock / Impending shock o Abdominal pain - Liver enlarges o Bleeding - Low platelet o Electrolyte imbalance – Ica. Na o Decease urine out - not effective volume Nurses activities: IV •Gr III •rate 10 cc/kg/hr •Gr IV rate Free flow 10 -15 min. •Hct, BS, CBC, LFT,Coag, BG Lab •Group match bleeding O2 Notify Doctor Monitor V/S IV Access Hct. & DTX stat •Via Oxygen •Monitor O2 Sat •Symptoms •Signs •CP >? •Abnormal signs • BP ,PR,RR every 10 15 min .until stable • Control IV •Follow Hct •Record Urine output •Correct complication Oxygen sat Via Oxygen If can’t open IV Transfusion Force ORS immediately but patients good conscious, can talk. ( with syringe) Prepare cut down set during wait the physician Prepare cut down set Prepare set for insert Double Lumen Care IV Transfusion & Record intake Type of IV – 5%D/NSS,5%DAR Control flow rate follow order Dr. Care Position Record total infusion and ORS/shift Care every 2-4 hrs. Management procedure care IV rate Urine output & Content from vomiting, bloody show Record urine output every 8 hrs. ( Febrile phase) Urine 0.5 ml/kg/hr (BW) (Critical phase/Shock) Record urine color To known amount show blood renal effective circulatory Record amount content Calculate of urine output: Volume may be effective circulatory Urine sp.gr < 1.015 mean effective volume. fluid overload > 1.015 mean dehydration/ disturbance volume Volume/shift in 8 hours Step calculation: 1 IBW 2. How many amount urine pass 3. Divide by 8 hours 4. Divide by IBW Hematocrit (Hct.) Febrile -Plt >100,000 - Dehydration Hct. 1-2% Per shift Leakage Plt<100,000 Hct. 4-6 hr Adjust Rate IV - Hct. Rising - leakage - Hct. Drop – bleeding Before & After blood transfusion - Hct. may be 5% compare after Load Dextran-40 complete 1 hr. for Management IV Important Nurse must to know Base line patient Hct. After 24-48 hrs. after plasma leakage Indications in the convalescence phase -Vital signs stable - Wide pulse pressure - Strong and slow pulse - Hct. decrease - Increase urine output - Confluent petechial rash 3.Signs to convalescent phase: A: Appetite B : Base line Pulse rate BP normal ปกติ C: Convalescent Rash-iching D: Diuresis – more frequency Hyper-volemia/ Hypertension/Dyspnea/Tachypnea Nursing care - V/S if High BP notify doctor - Observe signs of fluid overload - Fowler’s position - Oxygen - Discontinue IV fluid - Give medication as in Dr.’s order Convalescence Phase Itching with or without Convalescence rash Nursing care -Explain -Advice not to scratch -Keep clean and dry skin -Use talc powder/ calamine lotion -Antihistamine if indicated List monitoring of DHF patient 1. Vital Signs 2. Signs & Symptoms Notify doctors 3. Care IV Transfusion 4. Hematocrit (Hct.& Lab Test) 5. Urine output 6. Observer signs shock 7. Observe signs bleeding 8. Observe signs fluid overload 9. Observe signs liver failure, Renal failure 10. Notification Cause of death in Dengue: Prolong Shock Fluid overload Massive Bleeding Dead Rasana 06/12 Leakag e Hematolog ic changes Circulatory changes - Platelet drop -BP,Pulse -Hct rising - Bleeding Abnormal symptoms Fluid overload Before Shock • IV before Leakage • Miss diagnosis • N/2,N/3 hypotonic • Hypotonic solution During• Do not calculate IV / Type Shock• Not adjust the Rate Hct./Urine output After Shock Rasana 06/12 • Do not Off IV Convalescent phase • Got Sign Fluid overload Signs & Symptoms Respiratory distress,e.g dyspnea Tachypnea Mark distended abdomen with massive ascites Rapid pulse (usually strong pulse) Narrowing of pulse pressure Crepitation and/or rhonchi Poor tissue perfusion (delayed capillary refill) Symptoms • Puffy eyelid • Ascites • Edema • Restless • Distress Rasana 06/12 Signs 1.Vital signs : -Rapid pulse: Age ,Rhythm -Narrowing of pulse pressure 2.Respiratory distress: -Rapid HR,RR ,Dyspnea, Tachypnea -Poor tissue perfusion CR> 2 S -Oxygen Sat drop>95% Rasana 06/12 Monitoring: Vital signs /.Respiratory distress Measure BP Pulse q 30-1 hr, 1-2 hrs/record Notify Rate Increase - Respiratory - Distress - Restlessness - Ascites - CR delay > 3 sec. - Cool clamp - O2 sat drop< 95% Prepare CPR Rasana 06/12 Treatment monitoring: Furosimide :Lasix -Check V/S every 15 min 4 time -Record urine pass -Observe symptoms - Notify when no urine pass,BP drop,Pulse rapid Colloidal: 10%Dextran-40 - Control rate 10 cc/kg/hr - Ending time charge type IV transfusion - Notify Dr. -Repeat Hct./Notify -Observer symptom, Check V/S Treatment monitoring: Tapping: - Preparing set tapping - Helping doctor tapping - Record amount plural fluid - Observe respiratory rate keep O2 - Observe Bleeding - Follow lab. Electrolyte imbalance Rasana 06/12 Treatment monitoring: Intervention On ET Tube: - Preparing set CPR - Medicine for resuscitation - Equipment - Coordination for move to ICU - Explain family patients Rasana 06/12 Fluid overload: - Pulmonary edema - Respiratory Failure - Pulmonary congestion DEAD shock and Massive bleeding Rasana Waleearattanapa RN. Head of Dengue Ward Queen Sirikit Institute of Child Health Bangkok, Thailand Prolong Shock/ Massive Bleeding Cause of prolong shock - From home - At ER/Ward - Shock not to be improved -Don’t diagnosis shock • Cause of bleeding: - Had got bleeding - Showed external - Internal bleeding - Prolong shock 4 grade Severity in Dengue Non shock - Grade I = TT+ - Grade II = Bleeding Shock grade - Grade III = Narrow pulse pressure - Grade IV= No pulse rate and not measure BP Management for Dengue Shock gr III Signs: Cold clammy. Rapid Pulse ,PP narrow BP 100/80 mmHg, 100/100 mmHg Restless, Weakness, No fever IV resuscitation – Isotonic rate IV 10 cc/kg/hr.Then 7cc/kg/hr Hct.stat,and repeat Hct. Other lab Notify Dr. Monitor BP, PR every 30 min then 1 hr. Management for Dengue Shock gr. IV. Signs: Cold clammy. Can not catch Pulse, BP Restless, weakness. drop fever, CR> 2 sec IV resuscitation – Isotonic free flow 5-10 min follow BP,P if can measure reduce rate IV 10 cc/kg/hr. Hct. And Sugar stat. other lab Notify Dr. Monitor BP, PR every 30 min then 1 hr. Hemorrhagic manifestation: • Tourniquet test positive • Petechiea/Purpura/Ecchymoses • Epistaxis • Gum bleeding • Hematremesis/ Melena • Hypermenorrhea Laboratory : Thrombocytopenia – Platelet decrease 100,000 Prolong PT/APTT – INR Prolong Coagulopathy – Impaired LFT - AST /ALT increase Hematrocrit drop > baseline Severe bleeding: • Gastrointestinal bleeding - Hematemesis - Helena • CNS bleeding • Hypermenorrhea Bleeding :Symptoms History got bleeding from home Epitaxis, Coffee ground, hypermenorrhea Hct. Drop Pulse rapid, Hypotension Prolong shock: Hypoxia Consciousness change: Restless Cold Clammy peripheral CR > 2 sec. O2 situation < 95% Bleeding Activities: - Notify doctor amount of bleeding - Stat Hct. And DTX BG - Preparing blood component - Monitor oxygen saturation - V/S q 1-2 hrs - Control rate blood transfusion - Observe signs blood allergy Rasana 06/12 Observe Bleed in Brain Symptoms - BP drop HR -Tachycadia - Conscious change rapid - Neuro-signs GCS decease - O2 Sat drop < 95% - Bleeding - Coffee ground, Melena - CT Brain-Brain edema, bleed Rasana 06/12 Complications: Bleeding Shock/ Electrolyte imbalanc e Leakage phase Liver failure Renal failure Fluid overloa d Circulator y Change Complication in Dengue severity cases Metabolic Acidosis Electrolyte Imbalance - Hypoglycemia - Hypocalcemia - Hyponatremia - Hypokalemia Hepatic Failure Acute Renal Injury Rasana 06/12 Electrolyte imbalance Hypoglycemia - Follow BS/DTX - Force oral fluid ors/juice - Keep warm - Check V/S q 2 hrs. Electrolyte imbalance Hypocalcemia - Observe convulsion/record duration - Take 10%Ca gluconate dilute 1:1 push slow - Notify Dr, Lab Ca < 8.5 mg% - Monitoring V/S .N/S Electrolyte imbalance (conc.) Hyponatremia & Hypokalemia - Follow lab Na,K and Notify - Change type IV - Take % sodium chloride - Force juice with high Na,K - Monitoring V/S.N/S Rasana Waleerattanapa RN Queen Sirikit National Institute of Child Health 2.Liver loss ability to functions: 80 -90% of liver cell were damaged Causes: Infected Dengue virus –Kuffer cell Impaired Protein Synthesis • Serum Albumin decease • Prothrombin time prolong Coagulopathy: Lab: PT,PTT,INR prolong Coagulation Factor: Factor VII, X ,V Prothrombin time Finding Bleeding Severity of hepatic injury AST/ALT Significant of Platelet dysfunction: THROMBOCYTOPENIA Platelet decrease (loss larger and active) Vitamine K Disseminated Intravascular Coaglulation (DIC) If prolong shock Cause for liver failure in Dengue Prolong shock/ hemorrge Hemoconcentrate plasma leakage Hct rising Blood flow decrease Liver dysfunction Classification of ALF; o Hyperacute -on set 7 days o Acute - onset 8- 20 days o Subacute - 4-12 weeks *Most of DHF on Acute* Laboratory finding: Platelet count- low < 20,000 Prolong- PT,PTT,INR > 1.3 Enzyme increase : - AST/ALT >1,000 - Albumine< 3.5 Clinical features of encephalopathy by grade Grade Clinical Features 1 Confuse, Altered mood, mild or episode drowsiness, impaired intellectual and concentration, decrease psychomotor function, rousable 2 Increased drowsiness with confusion and disorientation, inappropriate behavior, rousable 3 Very drowsy and disorientated, response to simple verbal command, often agitated and aggressive, markedly confused behaviour Response to painful stimuli at best or coma unresponsive, may be complicated by evidence of cerebral edema 4 Symptoms: o High fever o Pain in the upper right area of abdomen o Ascites (build up of fluid in the abdomen) o Nausea, Vomiting o Loss of appetite and weakness o A general sense of not feeling well o Disorientation or confusion o Sleepiness Problem : Fever Symptoms : High Fever > 38⁰ C - 40⁰ C Cause : Liver infection - dysfunction Aim: Prevent convulsion & heat stoke Nursing: -Tepid sponge -Lie on mattress bed for decrease temperature -Check temperature every 2-4 hrs. Problem : Abdominal pain and Ascites Symptoms : Tender and Not comfortable lie Cause : Liver enlarge and build up of fluid in the abdomen Aim: Release pain and support Nursing:- Cold compress - Comfortable position - Observe pain score and notify Problem : Nausea, Vomiting/ Loss of appetite and weakness Symptoms : continue vomiting/ nausea / refuse to eat Cause : liver loss function metabolic Aim: Promotion to eat and drink Nursing: - Special mouth wash - Soft diet and low fat - Follow laboratory electrolyte. etc. Na, K - Observe Neuro-signs Problem : Disorientation or confusion Symptoms : Behavior change, speak bowl Cause : NH3 load in circulation to abrupt brain Aim: Prevent to development hepatic encephalopathy Nursing: - Observe N/S, V/S q 1-2 hrs. - Observe consciousness GCS - Follow laboratory - Notify doctor if the patients abnormal signs Problem : Rick to bleeding Symptoms : bruise or Cause : low platelet Aim: Prevent to bleeding Nursing: - Stop bleed before taken blood test - Observe bleeding - Follow laboratory PT/PTT/INR - Do not invasive procedure - Follow Hct. Management of liver failure in Dengue cases: Control hypoglycemia Given antibiotic - Cefotaxine, Lactulose Severe cases may be blood exchange or hemodialysis Restrict food- low protein Control electrolyte – complication Control blood loss – If the Hct. Drop o o o o o o o o How to detection entering to Liver failure: Prolong Shock with Massive bleeding Severity leakage (Gr III, Gr IV, DSS) Fluid overload Got high fever continuous Lab: SGOT> SGPT = > 1000 Unit Severity bleeding Referral Cases High risk cases Nursing care for acute Kidney injury Dengue hemorrhagic fever Pediatric-modified RIFLE criteria GFR Criteria Urine Output Criteria Risk Increase Cr x1.5 or GFR decrease > 25% UO < 0.5 ml/kg/hr x 8 hrs. Injury Increase Cr x2 or GFR decrease > 50% UO < 0.5 ml/kg/hr x 16hrs. Failure Increase Cr x3 or GFR decrease > 75% Or C rx 4 mg/unit UO < 0.3 ml/kg/hr x 24 hrs. or Anuria for 12 hrs. Loss Persistent acute kidney failure and excretion loss of renal function> 4 weeks End Stage Renal Disease Persistent failure > 3 months ESRD Causes of acute kidney failure 1. Prerenal – Azotenia - Low blood volume - Low blood pressure - Thrombosis - Blood clot - Renal is ischaemia 2. Intrinsic - GFR decrease - Acute interstitial nephritis 3. Postrenal - Urinary tract loss - No urine pass 2 1 3 Renal manifestations in DHF Mild urinary abnormalities include - Proteinuria - Hematuria - Oliguria - Rising of BUN/Cr. Signs and Symptoms: Fatigue Loss Appetite Headache Nausea/Vomiting Urine decease Color of urine change Monitoring : Record urine output Color of urine Volume of urine/shift Force ORS Follow lab: BUN/Cr Natural course of Dengue Febrile – Urine 1.0 cc/kg/hr. Leakage – Urine 0.5 cc/kg/hr. Recovery – Urine > 1.0 cc/kg/hr. Treatment monitoring: Furosimide :Lasix (1mg/kg/dose) - Check V/S every 15 min 4 time - Record urine pass - Observe symptoms - Notify when no urine pass - BP drop,Pulse rapid 08/10/09 Treatment for AKI Peritoneal dialysis Hemo-dialysis CRRT Rasana 06/12 Continuous Renal Replacement Therapy ( CRRT) o SCUF – Slow Continuous Ultrafitration - Ultrafiltration - water o CVVH – Continuous Veno-Venous Hemofiltration - Convection - Water & Solutes o CVVHD -Continuous Veno-Venous Hemodialysis - Diffusion o CVVHDF -Continuous Veno-Venous Hemodiafiltration - Diffusion & Convection ( 3&4 water & Solutes small molecules Control of Uremia) 4’ E Concern for Dengue cases 1.E 2.E 3.E Early Detection Early Notification Early Intervention & Treatment 4. E Early Prevention control