Rubella Clinical Information - Minnesota Department of Health
advertisement

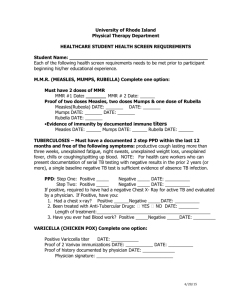
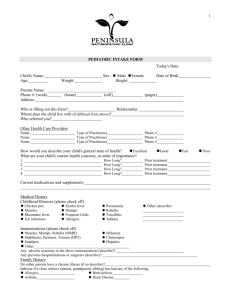
For healthcare providers Minnesota Department of Health Rubella Clinical Information Epidemiology of rubella Rubella is no longer considered endemic in the United States. However, continued success depends upon maintaining high vaccination rates, because cases of rubella continue to be imported into the United States. Rubella disease can occur anytime of the year, but is most frequently seen during late winter and spring. • Rubella is characterized by a mild, maculopapular rash. The rubella rash occurs in 50– 80% of rubella-infected persons. • Children usually develop few or no constitutional symptoms. Adults, however, may experience a 1–5 day prodrome of low-grade fever, headache, malaise, mild coryza, and conjunctivitis. • Postauricular occipital and posterior cervical lymphadenopathy is characteristic and precedes the rash by 5-10 days. • Arthralgia or arthritis may occur in up to 70% of adult women with rubella. • Rare complications include thrombocytopenic purpura and encephalitis. Prevention of congenital rubella syndrome (CRS) is the focus of rubella outbreak control and vaccination efforts. When infection occurs during pregnancy, especially during the first trimester, the risk of fetal infection may be as high as 90%. The virus may affect all organs of the fetus and cause a variety of congenital defects. Infection may lead to fetal death, spontaneous abortion, or premature delivery. While fetal infection may occur throughout pregnancy, CRS is rare when infection occurs after the 20th week of gestation. Diagnosing rubella Many rash illnesses, especially measles and scarlet fever, mimic rubella infection. Up to 50% of rubella infections may be subclinical. In diagnosing rubella, clinicians should consider: • Including both rubella and measles in the differential diagnosis of patients presenting with an acute generalized rash and fever. • Ordering serology tests only if the clinical case definition is met; otherwise, false positive results may be detected. • Collecting specimens for both culture and serology. Acute rubella infection is lab confirmed by the presence of one or more of the following: • a positive rubella-specific IgM antibody, • a significant rise in IgG antibody from paired acute and convalescent sera, • a positive viral culture for rubella, or • detection of the virus by reverse transcriptionpolymerase chain reaction (RT-PCR). Refer to MDH “Lab Testing for Rubella” fact sheet. Rubella is characterized by the following: • Acute onset of a maculopapular rash lasting < 3 days • Fever > 99°F (>37.2°C) • Arthralgia, arthritis, lymphadenopathy, or conjunctivitis Measles is characterized by the following: • A generalized maculopapular rash lasting ≥3 days • Fever ≥ 101oF (38.3°C) • Cough, coryza, or conjunctivitis Treating rubella Treatment is supportive. Rubella disease is normally mild and self-limited. Communicability of rubella • Persons with rubella are infectious from 7 days before rash onset to 5 to 7 days after rash onset. • The disease is most contagious when the rash is erupting. • The virus is shed in nasopharyngeal secretions and spreads when secretions get into mucous membranes such as the mouth, nose, eyes, or nonintact skin. • The virus is also spread when nasopharyngeal secretions (droplets) are sprayed during coughing and sneezing. • Prolonged and intimate contact are key variables for transmission. • The incubation period for rubella is usually 16 to 18 days but can range from 14 to 21 days. Preventing transmission of rubella Vaccination is the primary means to prevent disease. To prevent transmission of rubella in healthcare settings: • Patients suspected to have rubella should be placed in private rooms. In addition to Standard Precautions, Droplet Precautions should be followed until 7 days after rash onset. • Room doors can remain open and special ventilation is not required. • If measles is suspected, the patient should be placed in a negative pressure room. Airborne Precautions should be followed until 4 days after rash onset. Reporting: Rubella is a reportable disease. Report suspect cases of rubella immediately to the Minnesota Department of Health. MDH can facilitate testing and exposure follow-up. Call 612-676-5414 or toll-free 877-676-5414. (6/2008) Page 1 of 2 Rubella Clinical Information – page 2 To prevent the transmission of rubella in school and work settings: • Exclude persons suspected to have rubella from school or work until 7 days after onset of the rash, or until rubella has been ruled out. Handling exposure to rubella Neither rubella vaccine nor immune globulin (IG) is effective for post-exposure prophylaxis of rubella. Vaccination recommendations • All persons born in 1957 or later should have at least one dose of MMR vaccine, or documented serologic evidence of immunity. • Children should receive two doses of rubella vaccine, given as MMR. • Give the first dose at 12 to 15 months of age and the second dose at school entry (4 to 6 years of age) or, if not given at school entry, by age 12. • Persons born outside the U.S. are especially unlikely to be vaccinated. • Women should be vaccinated at least 4 weeks before becoming pregnant. Exposure to rubella during pregnancy If a pregnant woman is exposed to rubella and her immune status is unknown, test a blood specimen for rubella IgG antibody to determine immunity. If not detectable, collect a second specimen 2 to 3 weeks later and run concurrently with the first (paired sera). If negative, collect a third specimen 6 weeks after exposure and test concurrently with the first specimen. Negative tests indicate that no infection occurred.1 Immune globulin (IG) is not routinely recommended for post-exposure prophylaxis of rubella in early pregnancy or in any other circumstances; [however, disease may be modified or suppressed] IG does not prevent rubella infection or viremia. Administering IG may provide an unwarranted sense of security, as infants with congenital rubella have been born to women who received IG shortly after exposure. Regardless of these limitations, administration of IG may be considered if the pregnancy is not terminated. In such cases, intramuscular administration of 20 ml of immune globulin within 72 hours of rubella exposure may reduce—but will not eliminate—the risk for rubella.2 Vaccination and pregnancy Women who are pregnant or intend to become pregnant within 4 weeks should not receive rubella vaccine. Prior to administering rubella or MMR vaccine, the Immunization Program P.O. Box 9441 Minneapolis, MN 55440-9441 612-676-5414, 1-877-676-5414 www.health.state.mn.us/immunize Advisory Committee on Immunization Practices (ACIP) recommends that vaccine providers ask females of childbearing age if they are pregnant or likely to become pregnant in the next 4 weeks. Women who are pregnant or intend to become pregnant should be counseled about the potential risk for CRS and the importance of being vaccinated as soon as they are no longer pregnant.2 If a pregnant woman is inadvertently vaccinated or if she becomes pregnant within 4 weeks after vaccination, counsel her about the concern for the fetus. MMR vaccination during pregnancy should not ordinarily be a reason to consider termination of the pregnancy. Vaccinate females of childbearing age who are not pregnant after advising them of the theoretical risks of vaccination during pregnancy and the importance of not becoming pregnant during the 4 weeks following vaccination. Outcomes after vaccination during pregnancy Subclinical fetal infection has been detected serologically in approximately 1%-2% of infants born to susceptible vaccinees, regardless of the vaccine strain. Data collected by the CDC in the Vaccine in Pregnancy (VIP) Registry from 1971 to 1989 found no evidence that CRS occurred in offspring of the 321 susceptible women who received rubella vaccine and who continued pregnancy to term. The observed risk of vaccine-induced malformation was 0%, with a maximum theoretical risk of 1.6%, based on 95% confidence limits (1.2% for all types of rubella vaccine). Since the risk of the vaccine to the fetus appears to be extremely low, if it exists at all, routine termination of pregnancy is not recommended.3 The Vaccine in Pregnancy Registry maintained by the Centers for Disease Control and Prevention for rubella was discontinued in 1989. 1. Red Book: 2003 Report of the Committee on Infectious Diseases 26th edition. 26 ed. Elk Grove Village, IL: American Academy of Pediatrics; 2003. 2. Watson JC, Hadler SC, Dykewicz CA, Reef S, Phillips L. Measles, mumps, and rubella--vaccine use and strategies for elimination of measles, rubella, and congenital rubella syndrome and control of mumps: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. May 22 1998; 47(RR-8): 1-57. 3. Epidemiology and prevention of vaccine-preventable diseases. 8th ed. Atlanta, Ga.: Dept. of Health & Human Services, Centers for Disease Control and Prevention; Washington DC: printed and distributed by the Public Health Foundation; 2004. (6/2008) Page 2 of 2