BAPTIST HEALTH Schools Little Rock School of Practical Nursing

BAPTIST HEALTH Schools Little Rock
School of Practical Nursing
PSNG 2016 Medical Surgical II
Clinical Paperwork Requirements/Guidelines
Concept Mapping
Complete the following per guidelines and return the forms in a folder. Be prepared for clinical, making copies of forms at the clinical site will result in a UP for this requirement.
1.
Data Collection Tool
2.
Nurses Notes
3.
Clinical Medication Forms
4.
Application/Description of Disease Tool (to be completed on day 2 of clinical)
Guidelines: a.
Why did your patient seek healthcare? ( This information can be found on your completed
Data Collection Tool – Section I) b.
Medical Diagnosis: Specific to this admission (This information can be found on your completed Data Collection Tool – Section I). c.
Description of Disease Process: Give a brief description of the medical diagnosis or disease process that brought the patient to the hospital. List sources where the information was obtained. d.
Signs and Symptoms: List the signs and symptoms most common for this disease process.
List the sources where the information was obtained.
5.
Concept Mapping
Guidelines: a.
Admitting Complaint: As stated on the Application/Description of Disease form. b.
Medical Diagnosis: As stated on the Application/Description of Disease form. c.
Medical Interventions your patient is receiving related to their medical diagnosis. d.
Priority Assessment: From knowledge gained through theory and observation, what needs to be assessed on this client? e.
Problems: Based on your assessment and data collection
• Identify four patient problems that are the most important.
• Problems need to be related to the reason for admission
• Place each problem in a separate box on the Basic Tool for Concept Mapping. f.
Supporting Data - any abnormal data associated with the problem including physical assessment information, medications, lab results, x-ray results etc. g.
Prioritize problems and draw a line linking the problems associated with each other.
6.
Problem Intervention Flow sheet - For each of the four problems noted on the concept map identify 4 interventions and evaluate patient’s response to each intervention. a.
State Patient problem (from Concept Map)
b.
Desired Outcome: Define the expected behavior are assessment findings you want the patient to achieve that demonstrates the problem is resolved or progress has been made towards resolving the problem.
• Example: Patient will maintain a level of pain less than 4. c.
Intervention: those things that the nurse does to assist patient in reaching the desired outcome.
• Example: Medicate PRN for LOP > 4.
• Example: Reposition every 2 hours. d.
Rational and or evaluation of your patient’s response to the intervention
• Example: Medication – LOP 2 States, “My leg feels much better.”
7. Concept Map Grading Guide : Concept Maps will be graded using the Concept Map Grading Guide.
A copy of this guide will be submitted with paperwork in a folder.
Resources:
Schuster, P. M. (2002). Concept mapping: a critical-thinking approach to care planning. Philadelphia: F.
A. Davis Company.
Timby, B. K. & Smith, N. E. (2007)/ Introductory Medical-Surgical Nursing (9 th
ed.). Philadelphia:
Lippincott Williams & Wilkins.
Texas Collaborative for Teaching Excellence. Clinical thinking strategies: concept mapping. Retrieved
December 19, 2006, from http://cord.org/txcollabnursing/onsite_conceptmap.htm
Roach, S. S. (2004). Introductory Clinical Pharmacology. (7 th
ed.). Philadelphia: Lippincott Williams &
Wilkins.
Originated: January 2007 (BHSPN CC)
Revised July 2007
PNSG 2016 Medical Surgical Nursing II
Concept Map Grading Guide
Presentation Criteria/Grading Sheet
STUDENT NAME___________________ ID#_________ DATE__________
REQUIREMENT
Nurses Notes
POINTS
POSSIBLE
5
POINTS
EARNED
Completed Data Collection Tool
Application Form
Clinical Medication Form Completed per guidelines
Concept Map: Admitting complaint, Medical diagnosis, and Priority Assessment
5
10
10
10
Concept Map: Identifies 4 key problems, prioritize the problem, and lines drawn to indicate relationships (red ink for lines)
Supporting data listed for each problem
Intervention flow sheet (each problem has four interventions and rational & patient response to intervention)
Intervention flow sheet (each problem has an appropriate desired outcome))
Submitted completed assignment at the time determined by the instructor
(If turned in late 15 points will be subtracted from total points)
20
5
15
5
15
SP=77-100 point
UP=less than 77 points
Comments:_____________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
______________________________________________________________________________________
Revised: 2/2008
BAPTIST HEALTH Schools Little Rock
School of Practical Nursing
PSNG 2016 Medical Surgical II
Data Collection Tool Guidelines
The Data Collection Tool is to be turned in with the Concept Mapping Tool in a notebook.
Forms are to be handwritten. Photocopying is not allowed.
Sources of information: patient, family or chart (physician orders, progress notes, history and physical, radiology, lab). If you can’t find it in the chart ask the patient.
Data Collection Tool Guidelines:
Section I
Complete section 1 of data collection tool in the following manner:
1. Include patient age, sex, admit date, allergies, and code status.
Infection control: standard precautions unless they are in isolation. List if on contact, airborne or droplet precautions.
2. Admitting complaint-what brought patient to the hospital or to seek health services.
Example: chest pain, abdominal pain, headaches, heart surgery, fever etc.
Admitting VS-can be found on the graphic sheet.
3.
A medical diagnosis would be more specific than the admitting complaint. This information may be found in the physician’s orders, progress notes or in the history and physical.
Example: chest pain may be revised to pneumonia or anterior myocardial infarction. Abdominal pain may be revised to pancreatitis or bowel obstruction.
There may not be a revised diagnosis. The admitting complaint may be the medical diagnosis.
4. Medical interventions-what was done to treat or diagnose the admitting complaint or medical diagnosis.
5.
Example: surgical/diagnostic procedures related to the stated diagnosis.
Admitting physician-usually the physician who wrote admit order.
Physician consults-explain why a consult was needed.
You should be able to find this in the physician’s order.
6. Medical History- what illness or disease process do they have or have been treated for in the past.
Examples: Heart disease, hypertension, cancer, malaria.
7.
8.
9.
Surgical history- Any surgeries they have had and the dates.
Examples: CABG X5 1998, right hip replacement 1997, appendectomy 1952.
Allergies-list all allergies including food and drug.
Example: latex, tape, dye, chocolate, and red dye.
Psycho-social history includes if they are married, single, widowed. Who do they reside with. Where do they reside. May also include occupation, financial restraints, and education.
Cultural history includes ethnic groups, religious groups, or anything that might make their plan of care more unique.
Current emotional status- is the patient happy, sad, crying, angry, ect.
10. Current weight-found on the graphic
History of weight gain/loss.
Diet order/restrictions-found in the physician’s orders
Examples: Soft with 1000 mL fluid restriction in 24 hours. TF- Glucerna at 50 mL/hour with 100 mL water flush every 6 hours.
10.
Activity level: should find in the physician’s order.
Example: Up ad lib. BRP
11.
Miscellaneous equipment: any equipment the patient has on their bed, body, or needed for ambulation.
Example: specialty beds, walker’s, plexi- pulse boots, IV pump, PCA.
13. Dressing change orders: Be specific: where, when, with what. The information should be found in the physician’s orders.
14 Vital Signs: Document the most current and go forward from there. These are the vital signs that you obtain.
Section II
List ABNORMAL findings only from your physical assessment, If the assessment is within normal limits write WNL. Be prepared to discuss both normal and abnormal finding with your instructor.
Be sure to cover the following assessments:
1.
HEENT
2.
Neurological assessment
3.
Heart
4.
Lung/Respiratory assessment
5.
GI assessment
6.
GU assessment
7.
Musculoskeletal assessment
8.
Peripheral Vascular assessment
9.
Skin assessment
10.
IV assessment
11.
Safety assessment and safety precautions
Section III
Lab Orders: List all lab ordered in the past 72 hours. This information is in the physician orders. In addition the physician orders for FSBS need to be listed is this section (this order may have been ordered anytime during the hospital stay).
Lab Results: Found under the “lab” tab. Record the lab listed for your patient for the past
72 hours. Your patient may have a lot of lab or very little. Place NA in areas where there is no lab.
*FSBS should be listed for the days you are at the clinical site, starting with your day one and progress forward.
Section IV
Special tests and Procedures:
1.
Review the physician orders for when the test was ordered.
2.
Put the type of procedure/test ordered.
3.
Look up the procedure/test then describe, using your own words. The description should be how you would explain the procedure to the patient and their family. Also describe any special considerations associated with the procedure or test. Be sure to reference your resource you used.
For example: NPO, contraindicated if pregnant, or not Glucophage within 48 hours of procedure.
4.
To find the results you will need to locate the report regarding the procedure/test.
You will usually find these reports under the “radiology” tab in the chart. Look under
“impression” at the end of the document for results.
Originated 10/2005
Revised 1/2007
Revised 7/2007
Section V
Medication orders:
1.
Look in the physician orders for the medications that have ordered. Order sheets are placed with the most recent orders on top.
2.
Review and compare MAR with the physician’s orders.
3.
List all scheduled medications patient is currently receiving and all PRN medications that the patient has received in the last 24 hours. Include the trade name and generic name of medication and the dose, frequency and route.
4.
For additional information see assigned clinical instructor.
BAPTIST HEALTH Schools Little Rock
School of Practical Nursing
PNSG 2016 Medical Surgical II
Student Name: _____________________________ ID # ____________________ Date: _____________________
SECTION I: Patient Information
Age: ____ Sex: ___ Admit Date: __________ Code Status: __________ Infection Control: _________________
Admitting Complaint: ___________________________________________________________________________
Admitting Vital Signs:___________________________________________________________________________
Medical Diagnosis: ____________________________________________________________________________
Medical Interventions: __________________________________________________________________________
Admitting Physician: ___________________________________________________________________________
Physician Consults/ why: ________________________________________________________________________
_____________________________________________________________________________________________
Medical History: ______________________________________________________________________________
_____________________________________________________________________________________________
Surgical History: ______________________________________________________________________________
_____________________________________________________________________________________________
Allergies: _____________________________________________________________________________________
Psycho-social/cultural history: ____________________________________________________________________
_____________________________________________________________________________________________
Current Emotional Status: _______________________________________________________________________
Current Weight: ______________ History of Gain/Loss_______________________________________________
Diet Orders (restrictions/TF included): _____________________________________________________________
_____________________________________________________________________________________________
Activity Level: _______________________ Miscellaneous Equipment: __________________________________
Dressing Change Order: _________________________________________________________________________
Indicate normal versus abnormal by putting ↑ or ↓ by abnormal readings!!!!
Time/Date TEMP PULSE RESP B/P PAIN PULSE OX INTERVENTION FOR ABNORMAL
RESULT
SECTION II: Abnormal findings from physical assessment:
HEENT: __________ __________________________________________________________________________
_____________________________________________________________________________________________
Neurological Assessment : ______________________________________________________________________
_____________________________________________________________________________________________
Heart Assessment/Cardiac Monitor: ______________________________________________________________
_____________________________________________________________________________________________
_____________________________________________________________________________________________
Lung/Respiratory Assessment: __________________________________________________________________
_____________________________________________________________________________________________
_____________________________________________________________________________________________
GI Assessment: ___________________ ____________________________________________________________
_____________________________________________________________________________________________
GU Assessment: _______________________________________________________________________________
_____________________________________________________________________________________________
_____________________________________________________________________________________________
I & O: Yes/No (record the intake and output for your shift)
Date Shift Intake Output
Musculoskeletal: _______________________________________________________________________________
_____________________________________________________________________________________________
Peripheral Vascular: __________________ _________________________________________________________
_____________________________________________________________________________________________
Skin Assessment: _____________________________ _________________________________________________
_____________________________________________________________________________________________
IV Assessment : _______________________________________________________________________________
_____________________________________________________________________________________________
Safety Assessment/Safety Precautions: ____________________________________________________________
_____________________________________________________________________________________________
OTHER: ____________________________________________________________________________________
_____________________________________________________________________________________________
SECTION III: Lab Orders (INCLUDE FINGERSTICK BLOOD SUGARS):
LAB NORMAL
VALUES
RESULT
DATE
WBC
ADMISSION LAB
DATE:
RBC
HGB
HCT
Platelets
Na+
K+
Cl
Serum Glucose
BUN
Creatinine
PT
PTT
INR
FSBS (Blood Sugar)
FSBS (Blood Sugar)
FSBS (Blood Sugar)
OTHER:
RESULT
DATE
SECTION IV: Special Procedures/Test: (List Date, Type, Results) # them.
Type of Procedure: Date: Description of Procedure and document resources used: ordered completed
Results of Procedure: ___________________________________________________________________________
_____________________________________________________________________________________________
Type of Procedure: Date: Description of Procedure and document resources used: ordered completed
Results of Procedure: ___________________________________________________________________________
Type of Procedure: Date: Description of Procedure and document resources used: ordered completed
Results of Procedure: ___________________________________________________________________________
_____________________________________________________________________________________________
_____________________________________________________________________________________________
Type of Procedure: Date: Description of Procedure and document resources used: ordered completed
Results of Procedure: ___________________________________________________________________________
_____________________________________________________________________________________________
_____________________________________________________________________________________________
SECTION V: Medication List:
Med
#
11
12
13
14
7
8
9
10
6
4
5
2
3
1
Medication Order:
Generic and Trade Name
Dosage, Frequency, and Route
revised: 7/2007
BAPTIST HEALTH Little Rock
School of Practical Nursing
PNSG 2016 Medical Surgical II
Clinical Medication Form
Guidelines
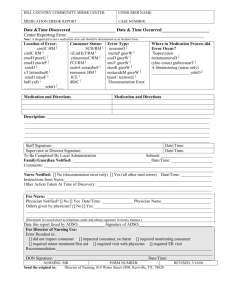
Directions: Complete the Clinical Medication Form for all scheduled medications your patient is receiving and for any PRN’s received in the past 24 hours. The forms will need to be completed prior to medication administration and will be submitted with your concept map. Include all of the following required information; be brief.
1.
Date ordered a.
Review the physician’s orders for the original date medication ordered.
2.
Generic Name a.
Not capitalized
3.
Trade name a.
Capitalized
4.
Dose a.
What is the dose ordered? b.
Is this dose within the normal range? (Circle yes or no. If the answer is no be prepared to discuss with Instructor why.)
5.
Route a.
How is the medication ordered?
6.
Frequency a.
How often is the medication ordered? (Define any abbreviations used)
7.
Time Due a.
What are the specific times the medication is to be given?
8.
Classification a.
Many drugs have multiple classifications; what is the classification related to your patient?
9.
Pharmacokinetics a.
Where is the medication metabolized? b.
How is the medication excreted?
10.
Desired actions a.
Why is your patient receiving the medication? b.
What does the doctor want to happen with this medication?
11.
Side effects a.
Adverse effects (if underlined it is most frequent side effect, if it is Capitalized and in Red it is life threatening side effect) b.
Has to be specific for the route given
12.
Nursing interventions a.
What will you monitor for your patient? (if desired actions are occurring, side effects) b.
Look under Nursing Implications for additional information; has to be specific for the route given.
Originated 1/2007
BAPTIST HEALTH Schools Little Rock
School of Practical Nursing
PNSG 2016 Medical Surgical Nursing II
Clinical Medication Form
Name of Drug (generic and trade name)
Dose/Route/Frequency
Date ordered
Classification
Is dose within normal range?
Desired action (for your patient)
Pharmacokinetics (metabolized and excreted)
Nursing Interventions
Name of Drug (generic and trade name)
Date ordered
Classification
Pharmacokinetics (metabolized and excreted)
Dose/Route/Frequency
Is dose within normal range?
Desired action (for your patient)
Nursing Interventions
Revised: 7/2007
BAPTIST HEALTH Schools Little Rock
School of Practical Nursing
Application/Description of Disease
PNSG 2016 Medical Surgical Nursing II
Reason patient needed Healthcare:
Medical Diagnosis or Disease:
Description of Disease Process:
---------------------------------------
Signs and Symptoms:
1.
---------------------
Medical Management:
------------------------------------
---------------------------------------
2.
---------------------
------------------------------------
--------------------------------------------------------------------------
3.
---------------------
--------------------------------------------------------------------------
--------------------------------------4.
--------------------- ------------------------------------
---------------------------------------
5.
---------------------
------------------------------------
--------------------------------------------------------------------------
6.
---------------------
--------------------------------------------------------------------------
--------------------------------------7.
--------------------- ------------------------------------
---------------------------------------
8.
---------------------
------------------------------------
--------------------------------------------------------------------------
9.
---------------------
--------------------------------------------------------------------------
---------------------------------------
---------------------------------------
---------------------------------------
---------------------------------------
------------------------------------
------------------------------------
------------------------------------
--------------------
*Description of disease process, signs and symptoms, and medical management is to be retrieved from your text book, Introductory Medical-Surgical Nursing or other educational resources.
Medical management includes medication and any interventions such as surgery or interventional procedures.
Revised: 7/2007
#
Problem:
Supporting data:
#
Problem:
Supporting data:
Originated: 1/2007 Revised 7/2007
BAPTIST HEALTH Schools Little Rock
School of Practical Nursing
PNSG 2016 Medical Surgical Nursing II
Concept Mapping
Admitting complaint:
___________________________
___________________________
Medical diagnosis
___________________________
___________________________
Medical intervention and treatment:
___________________________
___________________________
___________________________
___________________________
___________________________
Priority Assessment
___________________________
___________________________
___________________________
___________________________
___________________________
#
Problem:
Supporting data:
#
Problem:
Supporting data:
BAPTIST HEALTH Little Schools Little Rock
School of Practical Nursing
PNSG 2016 Medical Surgical Nursing II
Problem Intervention Flow Sheet
Problem number:____________________________________________________
#
____________________________________________________
Intervention
Desired Outcomes: The patient will ____________________________________
___________________________________________________________________
___________________________________________________________________
Rational and patient’s response to intervention
1.___________________________________________
___________________________________________
2. __________________________________________
__________________________________________
3. __________________________________________
___________________________________________
4. __________________________________________
__________________________________________
1. _______________________________________
_________________________________________
2. _______________________________________
________________________________________
3. _______________________________________
________________________________________
4. _______________________________________
________________________________________
Originated: 1/2007
Revised: 2/2008