Urinalysis in the diagnosis of renal disease
advertisement

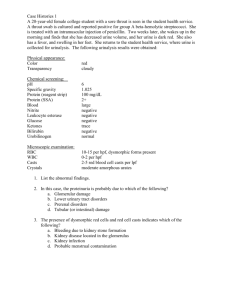
Urinalysis in the diagnosis of renal disease Theodore W Post, MD Burton D Rose, MD UpToDate performs a continuous review of over 270 journals and other resources. Updates are added as important new information is published. The literature review for version 10.2 is current through April 2002; this topic was last changed on June 26, 2000. Patients with renal disease may have a variety of different clinical presentations. Some have symptoms that are directly referable to the kidney (gross hematuria, flank pain) or to extrarenal sites of involvement (edema, hypertensive, signs of uremia). Many patients, however, are asymptomatic and are noted on routine examination to have an elevated plasma creatinine concentration or an abnormal urinalysis. Once renal disease is discovered, the presence or degree of renal dysfunction is assessed and the underlying disorder is diagnosed. Although the history and physical examination can be helpful, the most useful information is initially obtained from estimation of the glomerular filtration rate (GFR) and examination of the urinary sediment. Estimation of the glomerular filtration rate (GFR) is used clinically to assess the degree of renal impairment and to follow the course of the disease. (See "Assessment of renal function: Plasma creatinine; BUN; and GFR"). However, the GFR provides no information on the cause of the renal disease. This is achieved by the the urinalysis and, if necessary, radiologic studies and/or renal biopsy. This card will provide an overview of the interpretation of the urinalysis in the patient with renal disease. A general approach to the patient with renal disease, including the utility of radiologic studies and renal biopsy are discussed separately. (See "Approach to the patient with renal disease including acute renal failure"). URINALYSIS – The major noninvasive diagnostic tool available to the clinician is the urinalysis. Although examination of the urine can also provide some information about disease severity, such a direct relationship between the urinalysis and severity is not always present. In a patient with acute glomerulonephritis, for example, normalization of the urinalysis represents resolution of the active inflammatory process. However, this can reflect either recovery or healing with irreversible glomerular scarring and nephron loss. In this setting, repeat renal biopsy may be required to accurately estimate the status of the renal disease [1]. Despite these potential limitations, a complete urinalysis should be performed in all patients with renal disease. The specimen should be examined within 30 to 60 minutes of voiding; a midstream specimen is adequate in men, but the external genitalia should first be cleaned in women to avoid contamination with vaginal secretions. The urine should be centrifuged at 3000 rpm for three to five minutes, and the supernatant then poured into a separate tube. A small amount of sediment should be placed on a slide, while the supernatant should be tested for color (particularly for color suggesting the presence of heme pigments), protein, pH, concentration, and glucose. Color – Normal urine is clear and light yellow in color; it is lighter when dilute and darker when concentrated, such as after an overnight water restriction. The urine may also be white (eg, due to pyuria or phosphate crystals), green (eg, due to the administration of methylene blue, amitriptyline, or propofol [2]), black (eg, due to malignancy or ochronosis), or shades of red or brown [3]. Although urine that is white, green, and black is extremely uncommon, the intermittent excretion of red to brown urine is observed in a variety of clinical settings [3,4]. The initial step in the evaluation of this problem is centrifugation of the urine to see if the red color is in the urine sediment or the supernatant (show figure 1). • Hematuria is responsible if the red color is seen only in the urine sediment, with the supernatant being clear. If, on the other hand, it is the supernatant that is red, then the supernatant should be tested for heme with a urine dipstick. (See "Red urine: Hematuria; hemoglobinuria; myoglobinuria"). • A red supernatant that is negative for heme is a rare finding that can be seen in several conditions, including porphyria, the use of the bladder analgesic phenazopyridine, and the ingestion of beets in susceptible subjects. • A red supernatant that is positive for heme is due to myoglobinuria or hemoglobinuria. Hemoglobinuria and myoglobinuria can be usually be distinguished by looking at the plasma which is red with hemoglobinuria and its normal color with myoglobinuria. Protein – The urine dipstick primarily detects albumin but not other proteins, such as immunoglobulin light chains. This test is highly specific, but not very sensitive for the detection of proteinuria; it becomes positive only when protein excretion exceeds 300 to 500 mg/day. Thus, the urine dipstick is an insensitive method to detect microalbuminuria, the earliest clinical manifestation of diabetic nephropathy. In this setting, the development of a positive dipstick for albumin is a relatively late event, occurring at a time when there is already marked structural injury. (See "Microalbuminuria in diabetic nephropathy and as risk factor for cardiovascular disease"). The semiquantitative categories on the dipstick should be used with caution and only as a rough guide since urine concentration will affect the measurement. A dilute urine, for example, will underestimate the degree of proteinuria. False-positive results are common with many iodinated radiocontrast agents [5]. Thus, the urine should not be tested for protein with the dipstick for at least 24 hours after a contrast study. Sulfosalicylic acid test – In contrast to the urine dipstick, SSA detects all proteins in the urine [6]. This characteristic makes the SSA test particularly useful in older patients who present with acute renal failure, a benign urinalysis, and a negative or trace dipstick. In this setting, myeloma kidney, in which immunoglobulin light chains form casts that obstruct the tubules, must be excluded. A significantly positive SSA test in conjunction with a negative dipstick usually indicates the presence of nonalbumin proteins in the urine, most often immunoglobulin light chains. (See "Pathogenesis of myeloma kidney"). Similar to the urine dipstick, radiocontrast agents can cause false positive SSA results [4]. The sulfosalicylic acid (SSA) test is performed by mixing one part urine supernatant (eg, 2.5 mL) with three parts 3 percent sulfosalicylic acid, and grading the resultant turbidity according to the following schema (the numbers in parentheses represent the approximate protein concentration) [3]: 0 = no turbidity (0 mg/dL) trace = slight turbidity (1 to 10 mg/dL) 1+ = turbidity through which print can be read (15 to 30 mg/dL) 2+ = white cloud without precipitate through which heavy black lines on a white background can be seen (40 to 100 mg/dL) 3+ = white cloud with fine precipitate through which heavy black lines cannot be seen (150 to 350 mg/dL) 4+ = flocculent precipitate (>500 mg/dL) Measurement of quantitative urinary protein excretion – Most patients with persistent proteinuria should undergo a quantitative measurement of protein excretion. This can be accomplished by a 24-hour urine measurement; however, collecting these specimens may be cumbersome in ambulatory care settings. An alternative method using a random urine specimen has been described [79]. This test calculates the total protein-to-creatinine ratio (mg/mg). This ratio correlates closely with daily protein excretion in g/1.73m2 of body surface area (show figure 2). Thus, a ratio of 4.9 (as with respective urinary protein and creatinine concentrations of 210 and 43 mg/dL) represents a daily protein excretion of approximately 4.9 g/1.73 m2. It is important to note the units of measurement in your laboratory. If the urinary creatinine concentration is measured in mmol/L, the formula must be amended as follows since 1 mg/dL equals 0.088 mmol/L (see "Measurement of urinary protein excretion"): Protein excretion @ (Urine [protein] x 0.088) ÷ Urine [creatinine] (See "Estimation of protein excretion" for automatic calculation of protein excretion using this method). Normal urinary protein excretion should be less than 150 mg per day. Levels above this (proteinuria) that persist beyond a single measurement should not be ignored since it implies an abnormality in glomerular permeability. In this circumstance, it is important to understand how to differentiate between relatively benign (eg, orthostatic proteinuria) or common causes of proteinuria (eg, diabetic proteinuria) and uncommon causes that require nephrology consultation. The approach to this problem is discussed in detail elsewhere. (See "Proteinuria: The primary care approach", see "Evaluation of isolated proteinuria" and see "Overview of heavy proteinuria and the nephrotic syndrome"). Hydrogen ion concentration – The urine hydrogen ion concentration, measured as the pH, reflects the degree of acidification of the urine. The urine pH ranges from 4.5 to 8.0, depending upon the systemic acid-base balance. The major clinical use of the urine pH occurs in patients with metabolic acidosis. The appropriate response to this disorder is to increase urinary acid excretion, with the urine pH falling below 5.3 and usually below 5.0. A higher value may indicate the presence of one of the forms of renal tubular acidosis. Distinction between the various types of RTA can be made by measurement of the urine pH and the fractional excretion of bicarbonate at different plasma bicarbonate concentrations. (See "Overview of renal tubular acidosis"). The diagnostic use of the urine pH requires that the urine be sterile. Infection with any pathogen that produces urease, such as Proteus mirabilis, can result in a urine pH above 7.0 to 7.5. (See "Chapter 13B: Meaning of urine osmolality and pH"). Osmolality and specific gravity – The solute concentration of the urine (or other solution) is a function of the number of solute particles per unit volume; it is most accurately measured by the osmolality of the solution. The plasma osmolality is maintained within a very narrow range (approximately 285 mosmol/kg), principally because the kidney is able to excrete urine with an osmolality markedly different from that of plasma. (See "Chapter 6B: Antidiuretic hormone and water balance" and see "Chapter 9A: Water balance and regulation of plasma osmolality"). Since the urinary concentration varies markedly based upon volume status, the urine osmolality is useful only when correlated with the clinical state. This measurement is most useful in the diagnosis of patients with hyponatremia, hypernatremia, and polyuria. (See "Diagnosis of hyponatremia", see "Diagnosis of hypernatremia", and see "Diagnosis of polyuria and diabetes insipidus"). If an osmometer is unavailable, the concentration of the urine can be assessed by measuring the specific gravity, which is defined as the weight of the solution compared with that of an equal volume of distilled water. The specific gravity generally varies with the osmolality. However, the presence of large molecules in the urine, such as glucose or radiocontrast media, can produce large changes in specific gravity with relatively little change in osmolality. (See "Urine osmolality vs specific gravity"). Glucose – The presence of glucose in the urine as detected semiquantitatively with a dipstick may be due to either the inability of the kidney to reabsorb filtered glucose in the proximal tubule despite normal plasma levels (renal glucosuria) or urinary spillage because of abnormally high plasma concentrations. In patients with normal renal function, significant glucosuria does not generally occur until the plasma glucose concentration is above 180 mg/dL (10 mmol/L). Renal glucosuria can occur as an isolated defect but is more commonly observed in association with additional manifestations of proximal dysfunction, including hypophosphatemia, hypouricemia, renal tubular acidosis, and aminoaciduria. This constellation is called the Fanconi syndrome and may result from a variety of disorders, particularly multiple myeloma. (See "Types of renal disease in multiple myeloma" and see "Etiology and diagnosis of type 1 and type 2 renal tubular acidosis"). The use of urinary glucose levels to screen for and monitor diabetes mellitus is limited for a number of reasons. These include the relative insensitivity of the measurement (since moderate hyperglycemia is required before a positive test is obtained); its dependence upon the urine volume; and its value which reflects the mean plasma glucose concentration and not the level at the time of measurement. (See "Screening for diabetes mellitus" and see "Blood glucose monitoring in management of diabetes mellitus"). Dipstick detection of hematuria and pyuria – Microscopic hematuria may be discovered incidentally when heme (either red blood cells or hemoglobin) is detected on a dipstick. Dipsticks for heme detect 1 to 2 red blood cells per high power field and are therefore at least as sensitive as urine sediment examination, but result in more false positive tests. By comparison, false negative tests are unusual; as a result, a negative dipstick reliably excludes abnormal hematuria [10]. Although red cells may be lysed in dilute urine, the hemoglobin that is released will be detected by the dipstick. (See "Evaluation of hematuria"). Dipsticks may also detect leukocyte esterase and nitrite, the former corresponding to pyuria and the latter to Enterobacteriaceae which convert urinary nitrate to nitrite. Although this test is a simple and inexpensive screen for urinary tract infection, it may also detect pyuria not associated with infection. (See "Urine sampling and culture in the diagnosis of urinary tract infection"). Significant causes of sterile pyuria include interstitial nephritis, renal tuberculosis, and nephrolithiasis. Although the detection of hematuria and pyuria by dipstick may be useful as a screening test, they cannot replace microscopic examination of the urine sediment in patients with renal disease. Such examination permits the detection of elements, such as red and white blood cell casts and epithelial cells and/or casts, which cannot be found by dipstick alone. URINE SEDIMENT – Although microscopic examination of the urine sediment in the patient with renal disease may reveal crystals, bacteria, cells, or casts, the presence of small amounts of one or more of these elements may be observed in healthy individuals. In a normal patient, for example, one high power field may contain 0 to 4 white blood cells and 0 to 2 red blood cells, and one cast may be observed in 10 to 20 low powered fields [11]. In addition, crystals of uric acid, calcium oxalate, or phosphate may occasionally be seen. Crystals – Whether crystals form in the urine depends upon a variety of factors, including the degree of supersaturation of constituent molecules, the urine pH, and the presence of inhibitors of crystallization. Many different forms may be observed in normal patients and in those with defined disorders: • Uric acid crystals – Uric acid crystals as well as amorphous urates are observed in acid urine, a milieu which favors the conversion of the relatively soluble urate salt into the insoluble uric acid (show sediment 1A-1B). (See "Uric acid renal diseases"). • Calcium phosphate or calcium oxalate crystals – The formation of calcium oxalate crystals is not dependent upon the urine pH, while calcium phosphate crystals only form in a relatively alkaline urine (show sediment 2A-2B). (See "Risk factors for idiopathic calcium stones"). • Cystine crystals – Cystine crystals, with their characteristic hexagonal shape, are diagnostic of cystinuria (show sediment 3). (See "Cystine stones"). • Magnesium ammonium phosphate crystals – Magnesium ammonium phosphate (struvite) and calcium carbonate-apatite are the constituents of struvite stones (show sediment 4). (See "Pathogenesis and clinical manifestations of struvite stones"). Normal urine is undersaturated with ammonium phosphate and struvite stone formation occurs only when ammonia production is increased and the urine pH is elevated to decrease the solubility of phosphate. Both of these requirements may be met when urinary tract infection occurs with a urease-producing organism, such as Proteus or Klebsiella. Although the observation of crystals in the urine is most frequently of little diagnostic importance, there are several notable exceptions. These include the presence of cystine or ammonium magnesium phosphate crystals (as mentioned above), the combination of acute renal failure and calcium oxalate crystals (a setting consistent with ethylene glycol ingestion), and the presence of a larger number of uric acid crystals occurring in association with acute renal failure (consistent with tumor lysis syndrome). (See "Management of methanol and ethylene glycol intoxication" and see "Tumor lysis syndrome"). Bacteria – The presence of bacteria in a urine sediment is most frequently due to contamination of the specimen upon collection. (See "Urine sampling and culture in the diagnosis of urinary tract infection"). Although normal urine is sterile, asymptomatic bacteriuria is increasingly recognized but is usually not treated. (See "Approach to the patient with asymptomatic bacteriuria"). Cells – The cellular elements found in the urinary sediment include red blood cells, white blood cells, and epithelial cells. Infrequently, tumor cells may also be observed, thereby suggesting the diagnosis of genitourinary malignancy (eg, bladder cancer) and/or infiltration of the renal parenchyma with malignant cells (eg, lymphoma). Hematuria – Transient hematuria is relatively common in young subjects and is not indicative of disease. As an example, one study evaluated 1000 young men who had yearly urinalyses between the ages of 18 and 33; hematuria was seen in 39 percent on at least one occasion and 16 percent on two or more occasions [12]. In another series of men over the age of 50 who were tested weekly for three months, hematuria was present in 10 percent [13]. In this age group, however, even transient hematuria may be important since it may reflect a serious underlying condition, such as bladder cancer. (See "Evaluation of hematuria"). Transient hematuria can also occur with urinary tract infection (eg, cystitis or prostatitis. This is typically accompanied by pyuria and bacteriuria and patients may often complain of dysuria. Hematuria may be grossly visible or microscopic. The color change does not necessarily reflect the degree of blood loss since as little as 1 mL of blood per liter of urine can induce a visible color change. As previously mentioned, the intermittent excretion of red to brown urine can be observed without red blood cells. (See "Red urine: Hematuria; hemoglobinuria; myoglobinuria"). Microscopic hematuria is commonly defined as the presence of more than 2 red blood cells per high powered field in a spun urine sediment (show sediment 5) [6]. Evaluation of red cell morphology also may be helpful in the patient with hematuria. The red cells are typically uniform and round (as in a peripheral blood smear) with extrarenal bleeding, but usually have a dysmorphic appearance with renal lesions [14,15], particularly glomerular diseases [15]. This change in morphology is manifested by blebs, budding, and segmental loss of membrane, resulting in marked variability in red cell shape and a reduction in mean red cell size (show sediment 6A-6B). Persistent hematuria should be evaluated. Among the more common causes are kidney stones, malignancy, and glomerular diseases (show figure 3). (See "Evaluation of hematuria"). Pyuria – White cells are slightly larger than red cells and can be identified by their characteristic granular cytoplasm and multilobed nuclei (since most are neutrophils) (show sediment 7). Infection is the most common cause of pyuria alone; the routine urine culture may be negative with tuberculous infection. (See "Urine sampling and culture in the diagnosis of urinary tract infection" and see "Renal disease in tuberculosis"). Pyuria has less diagnostic value if it occurs in association with other cellular casts, additional cellular elements, and/or proteinuria (see below). In addition to neutrophils, eosinophils and lymphocytes may also be seen in the urine. These cells can be identified by a Wright's stain of the sediment. Although it has been proposed that the finding of eosinophiluria is relatively specific and might be diagnostic of acute interstitial nephritis, the diagnostic accuracy of urinary eosinophils is uncertain. (See "The significance of urinary eosinophils"). Urinary lymphocytes may be observed in disorders associated with infiltration of the kidney by lymphocytes, such as chronic tubulointerstitial disease. (See "Renal disease in sarcoidosis"). Epithelial cells – Epithelial cells may appear in the urine after being shed from anywhere within the genitourinary tract. However, only renal tubular cells are diagnostically significant. Renal tubular cells are 1.5 to 3 times larger than white cells and contain a round, large nucleus. Since it is difficult to distinguish renal tubular cells from lower urinary tract cells, the presence of epithelial cells in casts is the only reliable finding to indicate a renal origin of the cell. Although an occasional finding of an epithelial cell cast is normal, increased numbers suggest a number of disorders, including acute tubular necrosis, pyelonephritis, and the nephrotic syndrome. Casts – Casts conform to the shape of the renal tubule in which they formed and are therefore cylindrical with regular margins. All casts have an organic matrix composed primarily of Tamm-Horsfall mucoprotein. Many different types of casts may be observed. Some can be found in normal individuals, while others are diagnostic of significant renal disease [16]. The observation of cells within a cast is highly significant since their presence is diagnostic of an intrarenal origin. Hyaline casts – Hyaline casts, which are only slightly more refractile than water, are not indicative of disease and are primarily observed with small volumes of concentrated urine or with diuretic therapy; they may occur at a frequency of 10 casts per high powered field. Red cell casts – The finding of red cell casts, even if only one is seen, is virtually diagnostic of glomerulonephritis or vasculitis (show sediment 8). (See "Hematuria: Glomerular versus extraglomerular bleeding"). White cell casts – The presence of white cell casts and pyuria alone is most consistent with a tubulointerstitial disease or acute pyelonephritis (show sediment 9A-9B). They may also be observed with many glomerular disorders. Epithelial cell casts – Acute tubular necrosis and acute glomerulonephritis, disorders in which epithelial cells are desquamated, may be associated with epithelial cell casts (show sediment 10A-10B). Fatty casts – Among patients with significant proteinuria, the degeneration of cells within epithelial casts may result in a characteristic "Maltese cross" appearance and a fatty cast (show sediment 11A-11B). These droplets are composed of cholesterol esters and cholesterol, which may also be observed free in the urine. (See "Significance of lipiduria"). Granular casts – Granular casts, which are observed in numerous disorders, represent degenerating cellular casts or aggregated proteins (show sediment 12). Waxy casts – Waxy casts are thought to be the last stage of the degeneration of a granular cast (show sediment 13). Since this degenerative process is probably slow, it is most likely observed in nephrons with very diminished flow. Waxy casts are therefore most consistent with the presence of advanced renal failure. Broad casts – As with waxy casts, broad casts, which are wider than other casts and tend to have a granular or waxy appearance, are thought to form in the large tubules of nephrons with little flow. They are most often observed in patients with advanced renal failure. PATTERNS – The diagnostic value of the urinalysis in the patient with renal disease lies in the association between different patterns of urinary findings and different renal diseases. In many cases, the urinary findings point toward one or only a few disorders (show table 1). Hematuria with red cell casts, dysmorphic red cells, heavy proteinuria (greater than 3.5 g/day), or lipiduria – Any of these findings, singly or in combination, is virtually diagnostic of glomerular disease or vasculitis (show sediment 14A14D). The absence of these pathognomonic changes, however, does not exclude these diagnoses. (See "Differential diagnosis of glomerular disease" and see "Significance of lipiduria"). Multiple granular and epithelial cell casts with free epithelial cells – These findings are strongly suggestive of acute tubular necrosis in a patient with acute renal failure, although their absence does not exclude this diagnosis (show sediment 15A-15C). In this setting, ischemic or toxic injury to the tubular epithelial cells can lead to cell sloughing into the tubular lumen due either to cell death or to defective cell-to-cell or cell-to-basement membrane adhesion [17]. In addition to acute tubular necrosis, similar urinary abnormalities can also be induced by marked hyperbilirubinemia alone (plasma bilirubin concentration usually above 8 to 10 mg/dL or 136 to 170 µmol/L); how this occurs is not clear [18]. Pyuria with white cell and granular or waxy casts and no or mild proteinuria – This constellation is suggestive of tubular or interstitial disease or urinary tract obstruction (show sediment 16A-16E). White cells and white cell casts can also be seen in acute glomerulonephritis, particularly postinfectious glomerulonephritis; in this setting, however, there are also other signs of glomerular disease, such as hematuria, red cell casts, and proteinuria. Hematuria and pyuria with no or variable casts (excluding red cell casts) – These findings may be seen in acute interstitial nephritis, glomerular disease, vasculitis, obstruction, and renal infarction. Eosinophiluria may also be seen with acute interstitial nephritis, but the absence of this finding does not exclude the diagnosis. (See "The significance of urinary eosinophils"). Hematuria alone – The significance of isolated hematuria (ie, without other cellular elements or casts, including red cell casts) varies with the clinical setting. It is suggestive of vasculitis or obstruction In the patient with acute renal failure, and of urolithiasis in the patient with flank pain. It can also be found with mild glomerular disease (particularly postinfectious glomerulonephritis, IgA nephropathy, thin basement membrane disease, and hereditary nephritis), polycystic kidney disease, and with extrarenal disorders such as tumors, and prostatic disease. (See "Evaluation of hematuria" and see "Glomerular hematuria: IgA; Alport; thin basement membrane disease"). Pyuria alone – Assuming no contamination with vaginal secretions (which is unlikely if there are no large vaginal epithelial cells in the sediment), pyuria alone is usually indicative of urinary tract infection (including tuberculosis). Sterile pyuria suggests some form of tubulointerstitial disease, such as analgesic nephropathy. Normal or near-normal (few cells with little or no casts or proteinuria; hyaline casts are not an abnormal finding) – In patients with acute renal failure, a relatively normal urinalysis suggests prerenal disease, urinary tract obstruction, hypercalcemia, myeloma kidney (although the SSA test should be markedly positive), some cases of acute tubular necrosis, or a vascular disease with glomerular ischemia but not infarction (scleroderma, atheroemboli [which are irregularly shaped and do not completely occlude vessels], and rare cases of polyarteritis nodosa affecting the renal arteries but not the glomeruli). With chronic renal disease, disorders that should be considered include prerenal disease (as with congestive heart failure), urinary tract obstruction, benign nephrosclerosis, and tubular or interstitial diseases. References 1. Chagnac, A, Kiberd, BA, Farinas, MC, et al. Outcome of the acute glomerular injury in proliferative lupus nephritis. J Clin Invest 1989; 84:922. 2. Lepenies, J, Toubekis, E, Frei, U, Schindler, R. Green urine after motorcycle accident. Nephrol Dial Transplant 2000; 15:725. 3. Rose, BD. Pathophysiology of Renal Disease, 2d ed, McGraw-Hill, New York, 1987, pp. 10-16. 4. Baran, RB, Rowles, E. Factors affecting coloration of urine and feces. J Am Pharm Assoc 1973; 13:139. 5. Morcos, SK, El-Nahas, AM, Brown, P, Haylor, J. Effect of iodinated water soluble contrast media on urinary protein assays. BMJ 1992; 305:29. 6. Doolan, PD, Alpen, EL, Theil, GB. A clinical appraisal of the plasma concentration and endogenous clearance of creatinine. Am J Med 1962; 32:65. 7. Schwab, SJ, Christensen, RL, Dougherty, K, Klahr, S. Quantitation of proteinuria by the use of protein-to-creatinine ratios in single urine samples. Arch Intern Med 1987; 147:943. 8. Abitbol, C, Zilleruelo, G, Freundlich, M, Strauss, J. Quantitation of proteinuria with urine protein/creatinine ratios and random testing with dipsticks in children. J Pediatr 1990; 116:243. 9. Steinhauslin, F, Wauters, JP. Quantification of proteinuria in kidney transplant recipients: Accuracy of the urine protein/creatinine ratio. Clin Nephrol 1995; 43:110. 10. Schroder, FH. Microscopic hematuria. Requires investigation. BMJ 1994; 309:70. 11. Wright, WT. Cell counts in urine. Arch Intern Med 1959; 103:76. 12. Froom, P, Ribak, J, Benbassat, J. Significance of microhaematuria in young adults. Br Med J 1984; 288:20. 13. Messing, EM, Young, TB, Hunt, VB, et al. The significance of asymptomatic microhematuria in men 50 or more years old: Findings of a home screening study using urinary dipsticks. J Urol 1987; 137:919. 14. Fairley, KF, Birch, DF. Hematuria: A simple method for identifying glomerular bleeding. Kidney Int 1982; 21:105. 15. Pollock, C, Pei-Ling, L, GØory, AZ, et al. Dysmorphism of urinary red blood cells – value in diagnosis. Kidney Int 1989; 36:1045. 16. Rose, BD. Pathophysiology of Renal Disease, 2d ed, McGraw-Hill, New York, 1987, pp. 68-69. 17. Racussen, LC, Fivush, BA, Li, Y-L, et al. Dissociation of tubular cell detachment and tubular cell death in clinical and experimental "acute tubular necrosis". Lab Invest 1991; 64:546. 18. Eknoyan, G. Renal disorders in hepatic failure (letter). Br Med J 1974; 2:670.