Cultural Competency For Health Care Providers
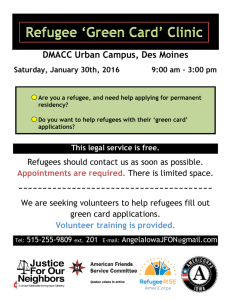
advertisement

Cultural Competency for Health Care Providers January2013 Thispageintentionallyleft blank. i Acknowledgements.............................................................................................................................iv GoalsofThisManual............................................................................................................................1 UnderstandingCulturalCompetency.............................................................................................2 Whatisculturalcompetencyinhealthcare?...........................................................................................2 Whyisculturalcompetencyimportant?...................................................................................................2 WhyisculturallycompetenthealthcareimportantinVermont?..................................................3 BestPracticesforCulturalCompetency........................................................................................5 OfficeofMinorityHealth:CLASStandards...............................................................................................5 Effectivecommunication..................................................................................................................................8 BuildingaCulturallyCompetentPractice–NEW!..................................................................12 Planning,implementing,andevaluatingculturalcompetenceinprimaryhealthcare settings..................................................................................................................................................................13 NationalCenterforCulturalCompetence:GuidelinesfortheFrontDesk..............................17 Toolsforself‐assessmentandimprovement.......................................................................................19 AdditionalResources......................................................................................................................................19 Vermont’sSpecialPopulations.......................................................................................................20 Populationsincludedinthismanual........................................................................................................21 Healthissuescommontopopulationsincludedinthismanual...................................................21 Bhutanese–NEW!...........................................................................................................................................24 BosnianandHerzegovinian.........................................................................................................................34 Burmese–NEW!..............................................................................................................................................43 Burundian............................................................................................................................................................55 Chinese–NEW!................................................................................................................................................63 Congolese.............................................................................................................................................................75 MeskhetianTurks.............................................................................................................................................83 Somali....................................................................................................................................................................87 Sudanese...............................................................................................................................................................93 Vietnamese..........................................................................................................................................................99 AfricanAmericans..........................................................................................................................................105 DeafandHardofHearing............................................................................................................................110 Elderly.................................................................................................................................................................116 LGBTQI(Lesbian,Gay,Bisexual,Transgender,Queer/Questioning,Intersex)..................122 Homeless............................................................................................................................................................130 ii LatinoMigrantFarmWorkers..................................................................................................................143 NativeAmericans............................................................................................................................................147 Women................................................................................................................................................................152 AppendixA.........................................................................................................................................158 iii Acknowledgements ThismanualwasmadepossiblethroughcollaborationbetweenChamplainValleyArea HealthEducationCenter(AHEC),theUniversityofVermont’sCollegeofMedicineAHEC’s SEARCHProgram,andtheFreemanMedicalScholarsProgram. ChamplainValleyAHECgratefullyacknowledgestheVermontCommunityFoundation www.vermontcf.orgforitssupportofourworktoexpandthecontentsofthemanualto includepopulationsnewtoVermontandtorestructurethemanualintoafriendlierand moreaccessibleformat. WethankRobinOrrforhereditorialservicesandoversightoftheserevisions.Wealso wanttothankJudyWechslerofChamplainValleyAHECforherroleincoordinatingthe revisionprocessforthiseditionofthemanual. NumerousSEARCHScholarsandFreemanMedicalStudentshaveconductedresearchand writtensectionsofthismanual;wethankthemfortheircontributions. FreemanMedicalStudents: AlexFolkl,UniversityofVermontCollegeofMedicine,Classof2012 DerekHuang,UniversityofVermontCollegeofMedicine,Classof2012 LauraPiper,UniversityofVermontCollegeofMedicine,Classof2012 LindsayNadeauDuy,UniversityofVermontCollegeofMedicine,Classof2012 SEARCHScholars: PeterB.Cooch,UniversityofVermontCollegeofMedicine,Classof2014 NicoleA.Fossiano,UVM,MastersofSocialWorkcandidate,Classof2013 ChelseaA.Harris,UniversityofVermontCollegeofMedicine,Classof2014 LaurenM.Kreiger,UniversityofVermontCollegeofMedicine,Classof2015 DavidJ.Larsen,UniversityofVermontCollegeofMedicine,Classof2014 Inaddition,wethankthefollowingindividualswhohavegenerouslysharedtheir knowledgeandexpertise: MariaMercedesAvila,MEd,VermontInterdisciplinaryLeadershipEducationfor HealthProfessionals(VT‐ILEHP),UniversityofVermontCollegeofMedicine JonBourgo,TheCommunityHealthCentersofBurlington JacquelineRose,MPH,VermontRefugeeResettlementProgram ThispublicationwasmadepossiblebyGrantNumberU77HP03624fromtheHealth ResourcesandServicesAdministration(HRSA).Itscontentsaresolelytheresponsibilityof theauthorsanddonotnecessarilyrepresenttheofficialviewsoftheUSDepartmentof HealthandHumanServices,HRSA,AreaHealthEducationCenters(AHEC)Program. iv Thispageintentionallyleft blank. v GoalsofThisManual Toprovideacomprehensive,easilyunderstooddefinitionofculturalcompetency. ToraiseawarenessoftheincreasingdiversityinVermontandthenewpopulations joiningourcommunities. Toofferresourcestohelpprovidersbecomebetteracquaintedwithdifferent populations. Tohelpprovidersusetheinformationinthismanualtocomfortablyassesspatients andprovidethebestcarepossible. Toassistproviderswiththeirownsenseofunderstandingbyofferinglinkstoself‐ assessmenttoolsandcontinuingeducationopportunities. Thisresourcewasdesignedforhealthcareproviderstosupportthepromotionofcultural competencyintheirpractice.Itisbynomeansmeanttobecomprehensive,butratherto provideageneraloverviewandtoofferselectresourcesforfurtherstudy. ChamplainValleyAHECrecognizesthatnewpopulationscontinuetosettleinVermontand thatnewdata,resources,andtechnologiestoimproveourunderstandingofhowtobest meetthehealthneedsofadiversepopulationcontinuetobedeveloped.Therefore,our effortstoupdateandrevisetheinformationinthismanualtokeepitcurrentandhelpful forVermontprovidersarealsocontinuous.Asresourcespermit,weintendtoaddsections onnewrefugee,immigrant,andotherspecialpopulationsinVermont.Wealsointendto begintheprocessofsystematicallyupdatingthecontentsofallofthespecificpopulation sections.Wewelcomeyourcommentsandquestionsaswellasanyassistanceorexpertise youcanprovidetoassistusinthisprocess. ThismanualiscopyrightedandprotectedbytheChamplainValleyAreaHealth EducationCenter. Permissionisgrantedtousethismanualfornon‐commercialpurposesifthematerialis notalteredandpropercreditisgiventotheChamplainValleyAreaHealthEducation Center. Permissionisrequiredifthematerialistobemodifiedinanyway,broadlydistributed,or usedinconnectionwithanycommercialactivity. Pleaseusethefollowingcitation: CulturalCompetencyforHealthCareProviders.ChamplainValleyAreaHealthEducation Centerwebsite.http://www.cvahec.org/app/wp‐ content/uploads/2013/10/CulturalCompetencyforHealthcareProviders13.pdf.Revised January,2013.Accessed[insertdate]. Pleasedirectcommentsandquestionsto: JudyWechsler ChamplainValleyAreaHealthEducationCenter 92FairfieldStreet 1 St.Albans,VT05478 T:(802)527‐1474 www.cvahec.org F:(802)527‐1632 UnderstandingCulturalCompetency Whatisculturalcompetencyinhealthcare? Thereisnouniversallyaccepteddefinitionofculturalcompetency.Ingeneral,itisasetof skillsthatallowssomeonetoincreasetheirunderstandingandappreciationofcultural differencesbetweengroups.Therearemanydifferentthingsthatmakeupaperson’s culturalidentity,includingcountryoforigin,language,race,ethnicity,education,family, spiritualtraditions,traditionalmedicalanddietarypractices,andmuchmore. Insimpleterms,culturalcompetencyinhealthcareistheabilitytointeractsuccessfully withpatientsfromvariousethnicand/orculturalgroups.Inpractice,thisinvolves: understandingandrespectingeachpatient’sculturalidentity; effectivecross‐culturalcommunicationbetweenthepatientandthehealthcare provider,includingtheavailabilityofhealth‐relatedlanguageresourcessuchas translatorsandtranslatededucationalmaterial;and theabilityofboththehealthcareproviderandthepatienttoaccessadditional culturalsupportserviceswhenneeded. Thismanualisaresourcedesignedtohelphealthcareprovidersbecomemoreculturally competent.AstheAmericanCollegeHealthAssociationnotes,“culturalcompetencyisan engaging,life‐longjourneyofexpandingyourhorizons,thinkingcriticallyaboutpowerand oppression,andbehavingappropriately.”Inotherwords,culturalcompetencyisnot somethingtobelearnedonceandputonadustyshelfattheoffice.Rather,itisadynamic skillthatmustbecontinuallydevelopedoveralifetime. Whyisculturalcompetencyimportant? TheUnitedStatesisacountryofmanyracesandcultures.Witheachpassingyear,more andmorehealthcareprovidersarerecognizingthechallengeofcaringforpatientswho speakdifferentlanguagesorwhohavedifferentculturalbackgrounds,includingdiverse perspectivesonhealthandwellness.Researchhasshownthateffectivecommunication betweenpatientsandhealthcareprovidersleadstoimprovedtreatmentadherence,higher patientsatisfaction,andbetteroutcomes. Disparitiesinhealthindicatorsandoutcomes In2002,theInstitutesofMedicinepublishedUnequalTreatment,astarkreportthat unmaskedextensivedisparitiesnotonlyintheoverallhealthofminoritypopulationsinthe UnitedStates,butalsointhetypeandqualityofhealthservicesthesegroupsreceived.The resultsofthisreport,thoughhardlyunexpected,nonethelessservedasacatalystforhealth careprovidersandpolicymakersnationwidetoreexaminecaredeliverymodels.1 Interestingly,theauthorsfoundthatneitherdisparitiesinaccesstocare,nordisparitiesin socioeconomicstatuscompletelyaccountedforthedifferenceinhealthoutcomes,so researchersbegantolookforalternativeexplanations.Manyconcludedthatalackof culturalcompetencyonthepartofproviderscouldaccountforatleastpartofthegapin 2 outcomesbetweenminoritypopulationsandnon‐Hispanicwhites,2whichprecipitateda nationalpushtoimprovetheskillset.Currently,mostprofessionalorganizations,fromthe AmericanMedicalAssociationtotheNationalAssociationofSocialWorkers,have publishedstatementsinsupportofculturalcompetency.3 Doesincreasedculturalcompetencyimprovepatienthealth? Formalizedstudyofculturalcompetenceisjustbeginningtoemergefromitsinfancy,so muchoftheexistingscholarlyworkcentersondefiningissuesandidentifyingfuture researchquestions.Intheabsenceofconclusiveresearch,healthprovidersareprobably bestservedbyapproachingtheissuefromBetancourt’sperspective,whoobservedthat “[c]ulturalcompetenceisnotapanaceathatwillsingle‐handedlyimprovehealthoutcomes andeliminatedisparities,butanecessarysetofskillsforphysicianswhowishtodeliver high‐qualitycaretoallpatients.”4 WhyisculturallycompetenthealthcareimportantinVermont? ThemostrecentU.S.Censusdatafrom2010showsthatVermont’spopulationisbecoming increasinglydiverse.Thosewhoidentifythemselvesassomethingotherthannon‐Hispanic whitenowmakeup6%ofourpopulation;amongthoseundertheageof18,thepercentage isnow9%.Inaddition,Vermontregularlywelcomesrefugeesfromtroubledregionsall aroundtheworld:morethan6,000refugeeshavebeenresettledintoVermont communitiessince1989. TheVermontDepartmentofHealth,inits2010reportTheHealthDisparitiesofVermonters, concludesthat“[w]hilethesenumbersarestillproportionatelysmallcomparedtotherest oftheUnitedStates,Vermont’sracialandethnic[minority]populationsaregrowingatafar greaterratethanthepopulationoverall”.Theentirereportcanbefoundat http://healthvermont.gov/research/documents/VTDisparitiesRpt2010.pdf ThesectiononRace,Ethnicity,andCulturalIdentityisattachedasAppendixA. AsVermontbecomesamorediversestate,providerswilltreatpatientsfrommany differentethnicities,cultures,beliefsystems,countries,andbackgrounds.Duetohealth carebarriersresultingfromeducationallevel,language,economicstatus,healthinsurance, culturalbeliefs,andmore,manyhealthissuesarenotaddressedasoftenastheyshouldbe. Often,providersfocusontheirspecialtycareandmaymisswarningsignsofother problemstheyarelessfamiliarwith. 3 ReproducedfromHealth DisparitiesofVermonters2010, publishedbytheVermont DepartmentofHealth. 4 BestPracticesforCulturalCompetency OfficeofMinorityHealth:CLASStandardsa TheOfficeofMinorityHealth,adivisionoftheUnitedStatesDepartmentofHealthand HumanServices,haspublishedasetofnationalstandardsforCulturallyandLinguistically AppropriateServices(CLASstandards).Thesestandardsareprimarilydirectedathealth careorganizations,butcanbeadaptedforusebyindividualhealthcareproviders. Mostofthestandardsarerecommendations,howeverallrecipientsoffederalfunds (includingpaymentsfromMedicaidandMedicare)arerequiredtocomplywithstandards 4through7.Thestandardsarereproducedbelowintheirentirety,withtherequireditems highlightedinyellow. 1. Healthcareorganizationsshouldensurethatpatients/consumersreceivefromall staffeffective,understandable,andrespectfulcarethatisprovidedinamanner compatiblewiththeirculturalhealthbeliefs,practices,andpreferredlanguage. 2. Healthcareorganizationsshouldimplementstrategiestorecruit,retain,andpromote atalllevelsoftheorganizationadiversestaffandleadershipthatarerepresentative ofthedemographiccharacteristicsoftheservicearea. 3. Healthcareorganizationsshouldensurethatstaffatalllevelsandacrossall disciplinesreceiveongoingeducationandtraininginculturallyandlinguistically appropriateservicedelivery. 4. Healthcareorganizationsmustofferandprovidelanguageassistanceservices, includingbilingualstaffandinterpreterservices,atnocosttoeachpatient/consumer withlimitedEnglishproficiency.Theseservicesshouldbeprovidedatallpointsof contactandinatimelymannerduringallhoursofoperation. 5. Healthcareorganizationsmustprovidetopatients/consumersintheirpreferred languagebothverbaloffersandwrittennoticesinformingthemoftheirrightto receivelanguageassistanceservices. 6. Healthcareorganizationsmustassurethecompetenceoflanguageassistance providedtolimitedEnglishproficientpatients/consumersbyinterpretersand bilingualstaff.Familyandfriendsshouldnotbeusedtoprovideinterpretationservices (exceptonrequestbythepatient/consumer). 7. Healthcareorganizationsmustmakeavailableeasilyunderstoodpatient‐related materialsandpostsignageinthelanguagesofthecommonlyencounteredgroups and/orgroupsrepresentedintheservicearea. a Thesearethestandardsineffectasofthismanual’spublicationdate.Themostcurrentversioncanbefound attheOfficeofMinorityHealthwebsite: http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlID=15 5 8. Healthcareorganizationsshoulddevelop,implement,andpromoteawrittenstrategic planthatoutlinescleargoals,policies,operationalplans,andmanagement accountability/oversightmechanismstoprovideculturallyandlinguistically appropriateservices. 9. Healthcareorganizationsshouldconductinitialandongoingorganizationalself‐ assessmentsofCLAS‐relatedactivitiesandareencouragedtointegrateculturaland linguisticcompetence‐relatedmeasuresintotheirinternalaudits,performance improvementprograms,patientsatisfactionassessments,andoutcomes‐based evaluations. 10. Healthcareorganizationsshouldensurethatdataontheindividual patient's/consumer'srace,ethnicity,andspokenandwrittenlanguagearecollectedin healthrecords,integratedintotheorganization'smanagementinformationsystems, andperiodicallyupdated. 11. Healthcareorganizationsshouldmaintainacurrentdemographic,cultural,and epidemiologicalprofileofthecommunityaswellasaneedsassessmenttoaccurately planforandimplementservicesthatrespondtotheculturalandlinguistic characteristicsoftheservicearea. 12. Healthcareorganizationsshoulddevelopparticipatory,collaborativepartnerships withcommunitiesandutilizeavarietyofformalandinformalmechanismstofacilitate communityandpatient/consumerinvolvementindesigningandimplementingCLAS‐ relatedactivities. 13. Healthcareorganizationsshouldensurethatconflictandgrievanceresolution processesareculturallyandlinguisticallysensitiveandcapableofidentifying, preventing,andresolvingcross‐culturalconflictsorcomplaintsby patients/consumers. 14. Healthcareorganizationsareencouragedtomakeavailableregularlytothepublic informationabouttheirprogressandinnovationsinimplementingtheCLAS standards. Legalrequirementsforculturallycompetenthealthcare TheLiaisonCommitteeonMedicalEducationRequirements,whichoversees accreditationforallmedicalschoolsintheUnitedStatesandCanada,requiresthatmedical studentsandfacultymusthaveanunderstandingofthemannerinwhichpeopleofdiverse culturesandbeliefsystemsperceivehealthandillnessandrespondtovarioussymptoms, diseases,andtreatments(StandardED21). TheEmergencyMedicalTreatmentandActiveLaborAct,alsoknownasthePatient Anti‐dumpingAct,requireshospitalsthatparticipateintheMedicareprogramandthat haveemergencydepartmentstotreatallpatients(includingwomeninlabor)inan emergencywithoutregardtotheirabilitytopay.Hospitalsthatfailtoprovidelanguage 6 assistancetopersonsoflimitedEnglishproficiencyarepotentiallyliabletofederal authoritiesforcivilpenalties,aswellasrelieftotheextentdeemedappropriatebyacourt. TheHill‐BurtonAct,enactedbyCongressin1946,encouragedtheconstructionand modernizationofpublicandnonprofitcommunityhospitalsandhealthcenters.Inreturn forreceivingfunds,recipientsagreedtocomplywith"communityserviceobligations,"one ofwhichisageneralprincipleofnon‐discriminationinthedeliveryofservices.TheOffice ofCivilRightshasconsistentlyinterpretedthisasanobligationtoprovidelanguage assistancetothoseinneedofsuchservices. MedicaidregulationsrequireMedicaidprovidersandparticipatingagencies,including long‐termcarefacilities,torenderculturallyandlinguisticallyappropriateservices.The HealthCareFinancingAdministration,thefederalagencythatoverseesMedicaid,requires thatstatescommunicatebothorallyandinwriting"inalanguageunderstoodbythe beneficiary"andprovideinterpretationservicesatMedicaidhearings. Medicareaddresseslinguisticaccessinitsreimbursementandoutreacheducation policies.Medicareprovidersareencouragedtomakebilingualservicesavailableto patientswherevertheservicesarenecessarytoadequatelyserveamultilingualpopulation. Medicarereimburseshospitalsforthecostoftheprovisionofbilingualservicestopatients. TheOfficeofMinorityHealth,adivisionoftheUnitedStatesDepartmentofHealthand HumanServices,haspublishedasetofstandardsforCulturallyandLinguistically AppropriateServices(CLASStandards).Thesestandardsappearinfullunder“Best PracticesforCulturalCompetency”(seepage5).Asnotedabove,allrecipientsoffederal funds(includingpaymentsfromMedicaidandMedicare)arerequiredtocomplywith standards4‐7. TitleVIoftheCivilRightsActof1964providesthat"[n]opersonintheUnitedStates shall,ongroundofrace,colorornationalorigin,beexcludedfromparticipationin,be deniedthebenefitsof,orbesubjectedtodiscriminationunderanyprogramoractivity receivingFederalfinancialassistance." VTStatutesAnnotatedTitle18§1852(a)(15)providesthatpatientswhodonot understandEnglishandpatientswhoarehearingimpairedhavearighttoaninterpreterif thelanguagebarrierorhearingimpairmentpreventsthepatientfromunderstandingthe careandtreatmentprovided. VTStatutesAnnotatedTitle18§8728(a)(5)and(b)(3)providethatpatientswith developmentaldisabilities,andtheirfamilies,havetherighttocommunicateintheir primarylanguageandprimarymodeofcommunication. 7 Effectivecommunication Thebestmedicalcarecomesfromhighqualitycommunicationbetweenthehealthcare teamandpatients.Poorcommunicationcanleadtodelayedcare,inappropriatetreatment, andfrustration.Researchshowsthateffectivecommunicationbuildslastingrelationships betweenprovidersandpatients,whichensuresthatpatientsaremorelikelytodisclose information,returnforfuturevisits,andcomplywithmedicaladvice. Gettoknoweachpatient’ssocialandculturalperspective Todoso,youmaywanttoaskthefollowingquestions. Whatlanguagedoyouspeak? Doyouhavefriendsorrelativeswhomyoucancallforhelp? Areyouinvolvedinareligiousorsocialgroup? Howaremedicaldecisionsmadeinyourfamily? Doyoueverhavetroubleunderstandingyourmedicationbottlesorappointment slips? Ismoneyaproblemforyou?Areyouevershortoffoodorclothing? Takea“cultural”history Thefollowingsimplevariationsonquestionsaskedduringatypicalhistorymayhelpyou gainabetterunderstandingofthepatient’sculturaloutlookondisease. Whatdoyoucallthisillness? Whatdoyouthinkcausedthisproblem? Whydoyouthinkitstartedwhenitdid? Whatdoesyoursicknessdotoyou?Howdoesitwork? Howsevereisyoursickness?Howlongdoyouexpectittolast? Whatproblemshasyoursicknesscausedyou? Whatdoyoufearaboutyoursickness? Whatkindoftreatmentdoyouthinkyoushouldget? Whatarethemostimportantresultsyouhopetogetfromthistreatment? Makeanefforttohireadiversestaff Membersofyourhealthcareteamwhocanspeakmorethanonelanguagecanbe valuableinhelpingthepatientcommunicate,especiallywhenpatientscometoyour officeandinterpreterarrangementshavenotyetbeenmade. Seekingmedicaladviceinanewcountrycanbeintimidating.Havingsomeoneinthe officewhospeaksyourlanguagecanbecomfortingandmaymakethetransitiongo moresmoothly. Havebrochuresandhealthcareinformationavailableinmultiplelanguages Manypamphletshavebeenwrittenindifferentlanguagesforthosewhodonotspeak English.Havingtheseavailablecanensurethatyourpatientsleavetheofficewithwritten informationthattheycanrefertointhefuture. 8 Wheretogetpamphletsinotherlanguages: The24LanguagesProject Electronicaccesstoover200healtheducationbrochuresin24different languages.ThisisaprojectoftheSpencerS.EcclesHealthSciencesLibrary,in partnershipwiththeUtahDepartmentofHealth,theImmunizationAction Coalition,theAssociationofAsianPacificCommunityHealthOrganizations, andmanyothers.http://medlib.med.utah.edu/24languages/ HealthyRoadsMedia Thissitecontainsfreeaudio,writtenandmultimediahealtheducation materialsinanumberoflanguages.ProducedbyaconsortiumofMidwestern organizations.http://www.healthyroadsmedia.org FoundationforHealthyCommunities ANewHampshire‐basedorganizationthathasmedicalformsandhealth informationavailableinseverallanguages. www.healthynh.com/fhc/resources/translateddocuments.php VermontDepartmentofHealthRefugeeHealthProgram http://healthvermont.gov/local/rhealth/rh_fact.aspx Useinterpreterservices Interpretersaretrainedtomakecommunicationeasierandtohelpprovidersrelay importantmedicaladvicetopatients. FamilyandfriendsshouldNOTbeusedtoprovideinterpretationservices(unless requestedbythepatient). Interpretersareavailableinalmosteverylanguageyoumightencounter,bothin Vermontandnationwide.Ifpossible,makearrangementsinadvancesoan interpretercanbeinplaceatthetimeofthevisit. Keepinmindthatyoumayalsoneedinterpretersandhealthcareinformationfor patientswithvisualorhearingimpairments.AmericanSignLanguageinterpreters andhealthinformationinBraillearealsoaccessiblethroughinterpreterservices. FollowtherecommendationsintheVermontRefugeeResettlementProgram’s publicationAQuickGuidetoWorkingWithInterpreters,reproducedonthenext page. 9 AQuickGuidetoWorkingwithInterpretersb Hireatrainedinterpreter;donotasktheclient’s childrentointerpretunlessitisanemergencyandyou havenoimmediatealternative. Ifyouhaveanewinterpreteroradifficultorhighly technicalsituation,scheduleapre‐session.Taketime toexplaintheinformationyouneedtohave communicated. Scheduleenoughtime;workingwithaninterpretertakeslongerthananappointment withoutone. Speakdirectlytotheclient:“Howareyoutoday?”ratherthan,“Askherhowsheis today.” Avoidprofessionaljargon;usetermsalaypersonwouldunderstand. Bepreciseandtrynottostringquestionstogether.Forexample,“Doyousmoke,drink ortakedrugs?”shouldbethreeseparatequestions. Giveyourinterpretertimetoprocessbothyourinformationandtheclient’s. Bepreparedtohavetheinterpreterinterruptwhensomethingneedsclarification. Looktoyourinterpretersasaculturalresource;treatthemwithrespectand consideration. ATipforLocalHealthCareProviders: WhenhiringaninterpreterforaMedicaidpatient,theproviderisexpectedto paytheinterpreter.Thebillingcodeforinterpreterservicesis“T1013”.Aunit ofserviceis15minutesofinterpreting.Providersreceive$15.00foreach15‐ minuteunit. LocalInterpreterServicesandResources TheCommunityHealthCentersofBurlington.TheCommunityHealthCentersof Burlington(CHCB)hasgainedgreatknowledgeaboutinterpreterservicesinitsyears workingwithrefugeeandimmigrantpopulations.ContacttheCHCBforinformationabout whatservicestheyworkwithandrecommend,andtodiscusswhatissueshavecomeupin thepastandhowtheywereabletosolvethem.(802)864‐6309www.chcb.org/ bCourtesyoftheVermontRefugeeResettlementProgram,462HegemanAvenue,Colchester,VT05446;802‐ 654‐1706 10 VermontInterpreterReferralService.TheVermontInterpreterReferralService(VIRS) providesinterpreterservicesfordeafandhardofhearingpatientsinavarietyofsettings, includingmedical.TheyalsoofferComputerAidedRealtimeTranslationservices(CART), whichallowsdeafandhardofhearingpatientstoreaddialoguefromacomputerscreenas theconversationtakesplace.(802)254‐3920ortollfree(800)639‐1519www.virs.org VermontInterpretingandTranslatingServices.TheVermontInterpretingand TranslatingService,locatedinColchester,Vermont,ispartoftheVermontRefugee ResettlementProgram(VRRP)andprovidesprofessionalinterpretationandtranslation. (802)654‐1706or(802)655‐1963http://www.vrrp.org/translation.html AssociationofAfricansLivinginVermont.TheAssociationofAfricansLivinginVermont (AALV),locatedinBurlington,Vermont,providesprofessionalinterpretationand translationaspartofitsAALVInterpretProgram.(802)355‐0795or(802)985‐3106 http://www.africansinvermont.org/interpret/ Otherinterpreterservicesandresources CertifiedLanguagesInternational http://www.certifiedlanguages.com 800‐225‐5254 CyraCom http://www.cyracom.com 520‐745‐9447 NewWorldLanguageServices http://newworldlanguages.com 800‐873‐9865 SpectraCorp CrossCulturalCommunicationServices,Inc. www.embracingculture.com 781‐729‐3736 LanguageLineServices http://languageline.com 800‐752‐6096 PacificInterpreters http://www.pacificinterpreters.com 800‐311‐1232 Telelanguage http://spectracorp.com/services/n_language_services.aspx 877‐695‐7945 http://www.telelanguage.com/interpretation.cfm 888‐983‐5352 Inaddition,TheNationalCouncilonInterpretinginHealthCareoffersavarietyof usefulresourcesontheirwebsite:http://www.ncihc.org.Weparticularlyrecommend theirNationalStandardsofPracticeforInterpretersinHealthCare,whichcanbefoundat http://data.memberclicks.com/site/ncihc/NCIHC%20National%20Standards%20of%20Pr actice.pdf 11 Thispageintentionallyleft blank. 12 BuildingaCulturallyCompetentPractice–NEW! Fundamentally,acceptingtheimportanceofculturalcompetenceinclinicalpracticeis mucheasierthanactuallyestablishingapracticethatincorporatessuchmandates. Howevertherearestepsthatinstitutionsandpracticescantaketofosteranatmosphereof inclusionandtofacilitatethebestoutcomespossiblefortheirpatients.Thefollowing guidelinesandbestpracticesareadaptedfromtheNationalCenterforCultural Competenceandrelatedsources.5‐9_ENREF_5 Planning,implementing,andevaluatingculturalcompetenceinprimary healthcaresettings Createasharedvision Toshapeinitialculturalcompetenceimprovementeffortsandtoevaluatetheeffectofsuch effortsinthefuture,anorganizationmustfirstdefinetheconceptofculturalandlinguistic competenceanditsachievementgoals.Itmaybebeneficialforpracticestotakeaproactive roleindevelopingtheirgoalsbyinvitinglocalfamilies,advocacygroups,orothervested partiestoparticipateinthesediscussions.Thegoalsforsmallorruralpracticesmaybe narrowerthanthoseoflargerpractices;organizersshouldadaptthesuggestionsbelowto meettheiruniquecapabilities. Beinformed.Asahealthcareprofessional,youshoulddevelopasolid understandingoftheculturalgroupsthatyouarelikelytoserve.Understanding eachpatient’sculturalidentityasfullyaspossiblecansignificantlyimprovethe clinicalencounter.Forexample,itmaybeimpossibletoaddresscertainissues,such assexualhistoryordrugandalcoholuse,withoutagooddegreeofcultural sensitivity. Bewareofstereotyping.Whileinformationaboutaspecificculturecanaid understandingofapatient,itisalsoimportanttoremembernoteverypatientfrom aparticularculturewillsharetheexperiencesorholdthebeliefsthatare traditionallyassociatedwiththatculture.Eachpatientisunique,andtherearemany factorsthatalteraperson’sculturalidentity,includingsocioeconomicstatus, education,age,religion,gender,andlifestyle. Respectyourpatients.Strivetoshowrespectforthedignityofeverypatient, regardlessoftheirage,gender,religion,class,sexualorientation,orethnicor culturalbackground.Bewillingtoincorporatetraditionalpracticesreflectingthe healthbeliefsofdifferentculturesintotreatmentplans.It’salsoimportantforyouto accepttherightofpatientstorefusecare. Enlistcommunitysupport.Maintainalistofcommunityresourcestoaddress communicationneeds. 13 Conductaninitialassessment Topinpointareasinneedofimprovement,practicesneedtobewell‐versedintheir strengthsandweaknesses,atboththeadministrativeandcare‐directedlevel.Such assessmentshouldincludemetricsdetailingattitudesandbeliefsandcompliancelevelwith CLASandTitleVIstandards.Pleaseseepage18,“Toolsforself‐assessmentand improvement”,foralistofresourcestohelpevaluateculturalcompetence. Assessthedifferentethnic,cultural,linguistic,andreligiousgroupsthatmaycome incontactwithagivenpracticeinordertodeterminethescopeofthenecessary competencemeasures.Suchassessmentsshouldbeconductedonaregularbasisas demographicsarechangingatanincreasinglyrapidpace. Collectpatientinformationtodeterminecommunicationneeds. Involvepatientsintheprocessofdevisingcommunicationsstrategies. Beawarethatpatientswillhavedifferentlevelsofhealthliteracy,andprovide languageassistancewhenneeded. Assesspatientsatisfactionwiththequalityofculturalservicesrendered. Evaluatecommunicationperformanceovertime. Evaluatecapacity,definegoals Likesomuchelseinmedicine,effortstoimproveculturalcompetencyaresubjectto financialandtemporalconstraints.Assuch,leadersintheseprojectsneedtobehonest aboutthelevelofeffort,amountofresources,andnumberofpartnershipstheirgoalswill requireandusetheseparameterstoinformtheirpriorities.Resourcesdevotedto maintainingordevelopingculturalcompetenceshouldbeidentifiedeachfiscalyearand analyzedovertime.Similarly,prioritiesshouldbeclearlydefined.Thesecouldinclude: raisingawarenessofculturalandlinguisticcompetence; increasingunderstandingandknowledgeofculturalandlinguisticcompetence relatedtothedeliveryofhealthcareservices;and developingskillsetsthatapplyknowledgeofculturalandlinguisticcompetenceto healthdisparities,healthcareaccessandutilization,patientandprovider satisfaction,andparticipatoryresearchmethodologies. Implementchanges Services Offerservicesatflexibletimes,andifpossibleinlocationsthatareeasilyaccessible. Bemindfulofreligiousholidaysandscheduleaccordingly. Makesuremedicalintakeformsareinclusive,withgender‐neutrallanguage (especiallywithregardtogenderidentification). Haveawell‐definedprocedureforidentifyingandaddressingculturally incompetentbehaviorbystaffmembers. Includepolicies,procedures,andfiscalplanningtoensuretheprovisionof translationandinterpretationservices. 14 ‐ ‐ ‐ ‐ ‐ ‐ ‐ Assembleandmaintainalistofinterpretersforbothmanuallycodedand spokencommunication. Includepoliciesandproceduresregardingthetranslationofpatientconsent forms,educationalmaterials,andotherinformationintoformatsthatmeet theliteracyneedsofpatients. Attempttolearnafewcommonphrasesinthedifferentlanguagesspokenby patients. Providesimplevisualaidsandusegesturesorphysicalpromptsforpatients withlimitedEnglishproficiencyorwithlimitedhealthliteracy. Ensurethatprintedinformationdisseminatedbythecliniciswrittenata levelconsistentwiththeaverageliteracylevelofthetargetpopulation. Offerwrittennotificationsinpatients’language(s)oforigin. Somepatientsmayprefertobenotifiedverbally;accountforthis. Humanresourcesandstaffdevelopment Totheextentpossible,hireadiverseandlinguisticallycompetentstaff. Providepre‐serviceandin‐servicetrainingandprofessionaldevelopmentactivities forallstaffandgoverningboardmemberstoensureunderstandingandacceptance ofvalues,principles,andpracticesgoverningculturalandlinguisticcompetence (includingfamilies,youth,peerprofessionals,etc.). Advertisepositionsinpublicationswithdiversereadershipsorinlocationsthat haverobustminoritypopulations. Dedicateresourcestoprovidelanguageaccessservicesfortheorganization. Physicalenvironment Displaypictures,posters,andothermaterialsthatreflecttheculturesandethnic backgroundsofchildren,youth,andfamiliesservedbytheclinic. Ensurethatmagazines,brochures,andotherprintedmaterialsinreceptionareas areofinteresttoandreflectdifferentcultures. Incorporatetoysthatarerepresentativeofdifferentculturalandethnicgroupsinto thereceptionareaandduringanyassessments. Offergender‐neutralbathroomsandotherfacilities. Providesignsthatareinlargeprint,clear,anduseatleasta70%colorcontrastto ensurevisibility. Data Useself‐identificationasanapproachtocollect,report,andevaluatedatafor individualsfromdiverseculturalandlinguisticgroups. Incorporatestrategiestostayinformedaboutmajorhealthandmentalhealth concernsandissuesforethnically/culturallydiverseclientpopulationsresidingin thegeographicregionoftheclinic. ‐ beattunedtodiseaseprevalenceindifferentcommunities 15 ‐ ‐ beawareofandsensitivetodisparitiesamongthesecommunities beawareoftheenvironmentalandsocio‐economicriskfactorsthat contributetohealthdisparitiesamongdifferentcommunities Thefrontdesk Therearemanyaspectsofcarethatextendbeyondpatientinteractionwithagiven provider.Infact,familiesmayhavemorecontactwithsupportstaff—particularly thefrontdesk—thantheydowithhealthcareprofessionals.Giventhisreality, cliniciansmustmakesurethattheymeettheneedsoftheirpatientsinaculturally sensitivemanneratbothaninstitutionalandpersonnel‐basedlevel. SeetheNationalCenterforCulturalCompetence’sGuidelinesfortheFrontDesk, reproducedonthenextpage,foradditionalinformationonthistopic. Elicitregularfeedback Offeropportunitiesforpatientsandfamiliestolodgeanonymouscomplaints regardingtheirexperiencewithclinic,linguistic,oradministrativestaff. Encourageemployeestoregularlycompleteself‐assessmentsandassessmentsof theclinic’sfunctioningasawhole. Identifyandfollowculturalcompetenceparameterstotrackprogressovertime. Supportconcretemechanismstotranslateresultsofqualitysurveysinto improvements. 16 NationalCenterforCulturalCompetence:GuidelinesfortheFrontDesk TheNationalCenterforCulturalCompetence(http://nccc.georgetown.edu/)hasanumber ofusefulresourcesonitswebsite,includingthefollowingrecommendedguidelinesfor addressingculturalandlinguisticcompetenceatthefrontdesk. ThisisanexcerptfromapublicationentitledCulturalCompetence:ItAllStartsattheFront Desk,bySuzanneBronheim,PhD.Theentiredocumentisavailableat: http://nccc.georgetown.edu/documents/FrontDeskArticle.pdf OrganizationalPolicies&Procedures PoliciesandproceduresonhowtoserveindividualswhospeaklittleornoEnglishare writtenandwellknowntostaff.Ataminimum,proceduresshouldaddresswhat resourcesareavailabletostaff,howtheyshoulddetermineafamily’sneedfor languageaccessservices,andhowtheyshouldhandlesituationsinwhich communicationsareproblematic. Policiesandproceduresonhowtoserveindividualswithothercommunicationneeds (e.g.,hearingimpairmentandlimitedliteracylevels)arewrittenandwellknownto staff.Ataminimum,proceduresshouldaddresswhatresourcesareavailabletostaff, howtheyshoulddetermineafamily’sneedforlanguageaccessservices,andhowto handlesituationsinwhichcommunicationsareproblematic. Dedicatedresourcesareallocatedtoprovidelanguageaccessservicesforthe organization. Organizationstaffarewellversedinthepolicies,andknowledgeableofthe procedures,usedtoprovideinformationtofamilies.Suchinformationenablesfamilies toadvocateontheirownbehalfwhentheyexperiencebiasordiscriminationinany aspectofthehealthcareorganization. Organizationalpolicyrequiresperiodicreviewsofthedemographicmakeupofthe communitiesservedtodeterminewhether: ‐ additionalornewlanguageaccessservicesareneeded,or ‐ modificationstopoliciesandpracticesareneededtoaddressnewand emergingpopulations. WorkforceDevelopment Organizationalpoliciesandproceduresincludeeffortstorecruitandretainfrontdesk staffwhoreflecttheculturalandlinguisticdiversityofthecommunitiesserved. Jobdescriptionsandrecruitingnoticesincludeskillsetsandareasofknowledge relatedtoculturalandlinguisticcompetence. 17 Performanceevaluationstandardsincludebehaviors,attitudes,knowledge,andskill setsrelatedtoculturalandlinguisticcompetenceandfamily‐centeredcare. Frontdeskstaffareincludedin professionaldevelopmentandtraining effortsthroughouttheorganizationon culturalandlinguisticcompetenceand family‐centeredcare.Additionally,front deskstaffareprovidedwithnewemployee orientationandongoingprofessional developmentthatincludestraining activitiestailoredtohowculturaland linguisticcompetenceisincorporatedinto theirspecificrolesandfunctionswithinthe organization.Ataminimum,thecontent ofsuchtrainingactivitiesshouldsupport frontdeskstaffin: ‐ ‐ ‐ ‐ Negativeinteractionswith thefrontdeskcanresultin: decreasedormissed appointments reticencetocalltheclinic withquestions lossofreferralsand/or income thefilingofagrievanceor discriminationcomplaint interactingeffectivelywithindividualsfromdifferentculturalandlinguistic groups; workingwellwithtrained/certifiedinterpreters; communicatingsuccessfullyacomplexarrayofinformationtoindividualswho possesslowliteracyskillsorwhoarenotliterate;and confrontingbias,discrimination,andracisminhealth,mentalhealth,and socialservicesystems. QualityImprovement Supervisorsareknowledgeableaboutthebehaviors,attitudes,andskillsetsrequired bythefrontdesktoworkeffectivelywithpatientpopulationsthatareculturallyand linguisticallydiverse.Additionally,supervisorsaretrainedtoconducteffective evaluationsoftheseperformancerequirementsandtosupportstaffinenhancingtheir performance. Informalandformalmechanismsareusedtosolicitinputfromindividualconsumers abouttheirfrontdeskencounters,withspecificqueriesabouttheirexperiencesrelated tothedeliveryofculturallyandlinguisticallycompetentcare.Resultsareusedto informqualityimprovementefforts,includingthemodificationofpoliciesand proceduresand/ortheprovisionoftraining. Mechanismsexistforfamiliestolodgecomplaintsanonymouslysothattheywillnot fearreprisalsforraisingconcerns. Anadvisorycommittee,madeupofdiversefamiliesservedbythepractice,clinic,or hospital,providesinputonoverallorganizationfunctions.Thisinformationshouldbe usedaspartofcontinuousqualityimprovementeffortsoftheorganization. 18 Toolsforself‐assessmentandimprovement InVermont,traininginculturalandlinguisticcompetenceformentalhealthandhealth providersisofferedthroughtheVermontChildMentalHealthInitiativebycontacting MariaMercedesAvilaat(802)999‐4985. TheNationalCenterforCulturalCompetence(NCCC)atGeorgetownUniversityprovides linkstomorethanadozenassessmenttoolsatthefollowingURL: http://nccc.georgetown.edu/resources/assessments.html. TheNCCChasalsodevelopeditsownassessment,theCulturalCompetenceHealth PractitionerAssessment,copyrightedbyGeorgetownUniversity,whichisavailableat: http://nccc.georgetown.edu/features/CCHPA.html. TheCaliforniaAcademyofFamilyPhysicianshasproducedAddressingLanguageAccess IssuesinYourPractice:AToolkitforPhysicians,whichisavailableat: http://www.familydocs.org/assets/Multicultural_Health/Addressing%20Language%20Ac cessToolkit.pdf. AdditionalResources TheEthnoMEDwebsitehttp://ethnomed.org/contains“informationaboutculturalbeliefs, medicalissues,andrelatedtopicspertinenttothehealthcareofimmigrants[…].” TheRefugeeHealthInformationNetworkhttp://rhin.org/“providesmultilingualhealth informationforrefugeesandtheirhealthproviders.” 19 Thispageintentionallyleft blank. 20 Vermont’sSpecialPopulations Populationsincludedinthismanual ThismanualincludesinformationonmajorrefugeeandimmigrantpopulationsinVermont aswellasonthefollowingpopulationsthathaveuniquehealthneeds:AfricanAmerican; NativeAmerican;deafandhard‐of‐hearing;elderly;lesbian,gay,bisexual,transgender, queer/questioningandintersex(LGBTQI);homeless;Latinomigrantfarmworkers;and women. Healthissuescommontopopulationsincludedinthismanual Thefollowingsectionsofthismanualwillhelpyoubecomefamiliarwithhealthcare disparitiesthatarecommonwithincertainspecificpopulations.Inaddition,itshouldbe notedthattherearetwoareasofhealthcaredisparitiesthatarecommontoallofthese groups:mentalhealthandoralhealth. Mentalhealth Mentalhealthisofparticularconcerninrefugeepopulations.Highlevelsofstress,feelings ofdespairandisolation,historiesofviolenceandpersecution,andothercontributing factorscanleadtosevereemotionalproblems.Post‐traumaticstressdisorder(PTSD)and depressionareamongthetwomostcommonmentalillnessesseeninrefugeepopulations. Approachingarefugeepatientaboutmentalillnesscanbecomplicated.Providerswho suspectmentalillnessshouldspeakwiththepatientabouttheirculturalbeliefsregarding mentalillness,asthestigmaisgreaterinsomepopulationsthaninothers.Workingwith thepatienttofindtherightcarefortheirillnessandtounderstandtreatmentoptionscan alsobechallenging.Beingpreparedwiththerightresources,knowingaboutspecific cultures,andbeingsensitivetothewishesofthepatientwillhelpincommunicating concern. MinoritypopulationsintheUnitedStatesarealsoatgreatriskformentalillness.Consider thefollowingfactsfromtheOfficeofMinorityHealth: OneintwoAmericanshasadiagnosablementaldisordereachyear.Thisincludes44 millionadultsand13.7millionchildren. Fewerthanhalfofadultsandonlyone‐thirdofchildrenwithdiagnosablemental disordersseekhelp. Mostmentaldisorders(80‐90%)aretreatableusingmedicationandbehavioral therapies. AfricanAmericansaremorelikelytoexperienceamentaldisorderthanCaucasians. Theyarealsolesslikelytoseektreatment. NativeAmericansandAlaskanNativessufferdisproportionatelyfromdepression andsubstanceabuse. 21 Homelesspeoplehaveoneofthehighestratesofmentalillness. AsianAmericanandPacificIslandersaremorelikelytobemisdiagnosedwhenit comestomentalillness. Oralhealth Therearemanyreasonswhydentalhealthhasbecomeasignificantprobleminhealthcare, particularlyforminoritypopulations.Lackofdentalcareisperhapsthelargest contributingfactortopoororalhealth.Dentalservicesarerarelycoveredundermedical insuranceandwithmorethan40millionuninsuredintheUnitedStates,itiseasytosee whydentalhealthisnotapriorityformany.Dentalworkandmaintenancecanbe expensiveandmanypeoplearemoreconcernedwithday‐to‐daylivingthanwithcavities andtoothdecay. Poororalhealthisextremelycommonamongrefugeepopulations.Manydidnothave accesstocleanwater,toothpaste,toothbrushes,floss,fluoride,oranyothernecessary componentsforhealthyteethandgums.Manyrefugeeshaveneverbeentoadentistorare notawareofthebenefitsoforalhealth. Dentalhealthisextremelybeneficialtothosewhocanaccessitasitcanpreventserious healthcomplications.Poororalhealthcanleadtogumdisease,whichcanresultinlost teethandanincreasedriskforheartdiseaseandstroke.Whenplaquebuildsupand hardensonteethandgums,itcantravelfromthemouthtothebloodstreamwhereitcan clogarteries,damageheartvalves,andcauselungconditions.ResearchattheNational InstitutesofHealth(NIH)hasshownalinkbetweengumdiseaseanddiabetesaswell. Complicationsofdiabetescanbecomemoreseverewithgumdiseaseandconversely, diabetescancausegumdisease,makinggoodoralhygieneparticularlyimportantto diabeticpatients.Finally,oralhealthisextremelyimportantforpregnantwomen.TheCDC statesthatgumdiseaseinpregnantwomenmayputwomenathigherriskofdelivering premature,lowbirthweightbabiesthanwomenwithoutgumdisease. Oralhealthisbestaddressedearly,whenchildrenarefirstbeginningtocareforteethand gums.AccordingtotheVermontDepartmentofHealth,dentaldecayisthesinglemost commonchronicdiseaseofchildhoodandisfivetoeighttimesasprevalentasasthma. Nationally,morethanhalfofallchildrenhavecavitiesbysecondgradeand80%ofchildren havehadcavitiesbythetimetheygraduatehighschool. Providersshouldparticipateinoralhealtheducationasmuchaspossible,andrefer patientstodentalorganizationsthatcanhelp. 22 References 1. FormicolaAJ,StaviskyJ,LewyR.Culturalcompetency:dentistryandmedicine learningfromoneanother.JDentEduc.Aug2003;67(8):869‐875. 2. WhitleyR.Culturalcompetence,evidence‐basedmedicine,andevidence‐based practices.PsychiatrServ.Dec2007;58(12):1588‐1590. 3. EngebretsonJ,MahoneyJ,CarlsonED.Culturalcompetenceintheeraofevidence‐ basedpractice.JProfNurs.May‐Jun2008;24(3):172‐178. 4. BetancourtJ.Culturalcompetency:providingqualitycaretodiversepopulations. TheConsultantpharmacist:thejournaloftheAmericanSocietyofConsultant Pharmacists.2006;21(12):988‐995. 5. GoodeTD.Planning,ImplementingandEvaluatingCulturallyCompetentService DeliverySystemsinPrimaryHealthCareSettings:ImplicationsforPolicyMakers andAdministrators.http://nccc.georgetown.edu/documents/Getting_Started.html. 6. GoodeTD.GettingStarted:Planning,ImplementingandEvaluatingCulturallyand LinguisticallyCompetentServiceDeliverySystemsforChildrenwithSpecialHealth NeedsandtheirFamilies.Washington,DC:NationalCenterforCultural Competence;2003. 7. GoodeTD,JacksonVH.GettingStarted...andMovingOn:Planning,Implementingand EvaluatingCulturalandLinguisticCompetencyforComprehensiveCommunityMental HealthServicesforChildrenandFamilies.Washington,DC:NationalCenterfor CulturalCompetence;2003. 8. GoodeTD,SockalingamS,BronheimS,BrownM,JonesW.APlanner'sGuide:Infusing Principles,ContentandThemesRelatedtoCulturalandLinguisticCompetenceinto MeetingsandConferences.Washington,DC:NationalCenterforCultural Competence;2000. 9. BronheimS.CulturalCompetence:ItAllStartsattheFrontDesk. http://nccc.georgetown.edu/documents/FrontDeskArticle.pdf.AccessedApril, 2012. 23 Thispageintentionallyleft blank. 24 Bhutanese–NEW! CountryInformationa Name: Bhutan(translatesto“LandoftheThunderDragon”inreference totheviolentstormsintheHimalayas) Location: SouthernAsiabetweenChinaandIndia;Southerneastern HimalayaMountains Capital: Thimphu Area: 38,394sq.km.(OnehalfthesizeoftheStateofIndiana) Climate: Variable;tropicalinsouthernplains;coolwintersandhot summersincentralvalley;severewintersandcoolsummersin Himalayas Terrain: Mostlymountainouswithsomefertilevalleysandsavanna;Arable land2.3% Language(s):Sharchhopka28%,Dzongkha(official)24%,Lhotshamkha (Nepalese),other26% EthnicGroups:Bhote50%,ethnicNepalese35%(includingLhotsampas), indigenousormigranttribes15% Population: InBhutan:716,896 RefugeesinNepal:56,710asofJanuary2012b InVT:950c aUnlessotherwisecited,allinformationonthispageisfromtheUnitedStatesofAmerica,CentralIntelligence Agency,TheWorldFactbook.AccessedApril,2012.https://www.cia.gov/library/publications/the‐world‐ factbook/geos/so.html bTheUNRefugeeAgency,2012UNHCRCountryoperationsprolfile‐Nepal.AccessedJune27,2012. http://www.unhcr.org/pages/49e487856.html# cVTRefugeeResettlementProgram,RefugeesinVermontbyCountryofOrigin,FY89‐FY11.Colchester,VT: 2012. 25 26 27 BackgroundandCulture TheNepali‐speakingBhutanese,alsoknownasLhotsampa,areBhutanesecitizensofNepali origin.PeoplefromNepalwereinvitedtopopulatethelowlandsofsouthernBhutaninthe mid‐tolate‐nineteenthandearlytwentiethcenturies.Contactbetweenthenorthern Bhutanese,knownasDruks,andtheNepali‐speakingBhutaneseinthesouthwaslimited. DespitelivinginBhutanforuptofivegenerations,theNepali‐speakingBhutaneseretained theirdistinctiveNepalilanguage,culture,traditions,andreligion.TheNepali‐speaking BhutanesecoexistedpeacefullywithotherethnicgroupsinBhutanuntilthemid1980s, whenBhutan’skingandtherulingDrukmajoritybecameworriedthatthegrowingNepali‐ speakingBhutanesepopulationcouldthreatenthemajoritypositionandthetraditional BuddhistcultureoftheDrukBhutanese.Thegovernmentthereforeinitiatedacampaign, knownas“Onecountry,onepeople,”or“Bhutanization”tostrengthenBhutanesenational identity.ThepoliciesenforcedtheDrukdresscode,religiouspractices,andlanguageuse onallBhutaneseregardlessofpriorpractices.Thesepoliciesnegativelyimpactedthe Nepali‐speakingBhutanesepeople,becausetheydidnotwearthesametraditionaldress, practicethesamereligion,orspeakthesamelanguageasthenorthernBhutanese. Whentheyrefusedtoconformtotherequests,theNepali‐speakingBhutanesewere tortured,raped,andbeaten.Theirhomeswereburnedandtheyweredrivenoutoftheir countrytoNepal.However,Nepalwasunwillingtoacceptthemascitizens,andover 100,000peoplebecamerefugees.TwentyyearslatertheUnitedStateshasagreedto resettle60,000refugeesandasofsummer2012,40,000havebeenresettled. Therearefourmajorcastesystems:Brahmins,Chhetris,Vaishyas,andSudras.The Brahminsaretypicallypriests,scholars,andeducators.Chhetrisarethewarriorsand governors.Vaishyasaremerchantsandfarmers,andtheSudrasarethelaborers.Thecaste systemsarenotasprevalentamongtheyoungergenerationsbutfortheoldergenerations theymaystillholdstrongbeliefsaroundthis. Language.AmongtheNepali‐speakingBhutanese,Nepaliisspokenathome.Themajority oftheyoungergenerationsaremulti‐lingual,speakingNepali,theBhutaneselanguage, DzongkhaandsomeEnglish.EducationinBhutan,aswellastherefugeecampswas instructedinEnglish,withastrongeremphasisplacedonreadingandwritingratherthan thespokenlanguage.TheBritishEnglishdialectwasusedintheschoolssotheNepali‐ speakingBhutanesemayhaveadifficulttimewithAmericanEnglish,especiallywhenit’s spokenfast.TheoldergenerationsofNepali‐speakingBhutanesemaynotbefamiliarwith EnglishandthereforemayfeelisolatedandfeartheywillnotlearnEnglish. Religion.ThemajorityoftheNepali‐speakingBhutaneseareHindu;howeversizable minoritiesalsopracticeBuddhismorChristianity.IntheChittendencountyareathereis notaHinduTemple,whichinhibitstheirabilitytopracticetheirreligion. Family.Historically,membersoftheextendedfamilylivetogether.Grandparentsandthe communityplayamajorroleinchildrearing.Theyoungestsonistypicallyresponsiblefor caringforhisparentsastheyage.Thecommunityisverycloselyknitandeldersarehighly 28 respected.Polygamymaybepracticedbysomebutisnotdiscussedwithinthecommunity. Arrangedmarriagesand“lovematches”arebothcommon.“Lovematches”takeplacewhen ayoungmanisfondofayoungwoman.Theparentsandeldersofthecommunitymust grantpermissionbeforecourtshipcanbegin. Education.In1966Bhutanestablishedapublic schoolsystemwherechildrenbecameeligibleto Itisimportanttocounselpatients, receiveeducationuntilgrade10.Priorto1966 especiallyelders,ongoodoral manyhadlimitededucation,whichiswhymany hygieneincludinghowtobrushand eldersinthecommunityarenotasproficientin floss. English.Nepali‐speakingBhutaneseplaceahigh valueoneducationforbothmalesandfemales,andschoolingcontinuedtobeavailablein therefugeecamps.SomeNepali‐speakingBhutanesecontinuedtheirhighschoolorcollege educationinBhutanandIndia,butthoseawardeddegreeswerenotequivalenttothosein theUnitedStates.ThemajorityofNepali‐speakingBhutaneseintheChittendencountyarea workinfactories,ashousekeepers,andstoreclerks. Theextentofparentalinvolvementintheirchildren’seducationintheUnitedStatesisa newconceptfortheNepali‐speakingBhutanese.Manystudentsstrugglewithtechnologyas theyhavenothadpreviousexposure.Somestudentsalsostrugglewithfriendshipsand feelingsofloneliness. Diet.Riceandlentilsareconsideredstaples.SomeNepali‐speakingBhutanesemaybe vegetarian,manyHinduswhomayeatmeatdonotconsumebeeforpork. Theideaofconsentpriorto HealthCare receivingamedicalprocedure Inthecamps,inpatient,outpatientandhealtheducation andbeinginvolvedinhealth isprovidedbytheAssociationofMedicalDoctorsofAsia caredecisionsmaybeanew (AMDA)‐Nepal.Childhoodvaccinesareroutinely conceptandshouldbe availableandhavehighacceptancerates(measles98%, explained. Diphtheria,Pertussis,TetanusDPT,95%,Polio,94%and BCG94%).However,adolescentboostersarenot routinelygiven.1MostNepali‐speakingBhutanesewillhaveseenpeoplesufferordiefrom preventablecauses,soonceintheUnitedStatesmanyarewillingtoreceiverecommended vaccines(althoughthereisahigherrateofdeclinationoftheHPVvaccine). Historically,theNepali‐speakingBhutanesehaveplacedagreateremphasisonacute healthcare,onlyvisitingadoctoriftheyweresickorhadcomplicationswithpregnancy. Somemaynotbefamiliarwithprimarycare,soprovidersmayhavetoprovideadditional counselingonthebenefitsofpreventivecare.Itisespeciallyimportanttoexplainthat medicationstopreventchronicdiseasessuchasheartdiseaseanddiabetesmayhavetobe takenforyears. Specifichealthconcerns.CommonhealthconcernsamongNepali‐speakingBhutanese refugeesincludemalnutrition,mentalillnesses(includingdepressionandPTSD),poororal 29 health,andlimitedfemalereproductive/gynecologiccare.Intherefugeecamps,food rationsincludedriceandlentils.However,theeffectsofmalnutritionforthispopulation, includingvitaminAdeficiencycausingnightblindness,andvitaminB12deficiencyleading tomacrocyticanemia,arestillprevalent.23 Dentalhealthwaslimitedinthecamps;manyrefugeesmaynothavereceiveddental services. Infectiousdisease.Inthecampsmanyrefugeeswereexposedtotuberculosis.Chronic malnutritionweakenstheimmunesystemsotherearehighratesofrespiratoryillnesses. Poorsanitationinthecampshasincreasedtheratesofdysentery.4 Lifestyleriskfactors.Althoughsmokingratesinthecampswerehigh,newlyresettled refugeesarelesslikelytosmoke,possiblyduetothehighercostofcigarettes.Once resettledintheUnitedStatesthereisahighprevalenceofobesityanddiabetes. Chewingbetelnutwascommonintherefugeecampsanditmaycontinuetobeusedbythe olderBhutaneserefugeepopulation. Betelnutisaseedfromthefruitofapalmfruitthat producesamildlyeuphoricandstimulatingeffect.Itisbelievedtohelpreducetension. However,estimatesofitsuseinVermontarenotavailable.Longtermeffectsofchewing betelnutincludeincreasedriskoforalcancers,pepticulcersandincreasedriskofheart disease. Familyplanningandchildbirth.Moderncontraceptioniswidelyacceptedandused, exceptbyhighlytraditionalindividuals.Mostrefugeesundertheageof35receivedbasic sexeducationintherefugeecamps.Sexualpractices,sexuality,andgynecological conditionsmaybeuncomfortableforNepali‐speakingBhutanesewomentodiscuss, particularlythoseintheoldergenerations.Afemaleprovidermaymakethemmoreatease. Manywomenmayneverhavehadamammogramorpapsmearandcounselingmaybe neededtounderstandtheimportanceofpreventativecare. Childbirth/PostpartumPractices InBhutanwomengavebirthathomewhilebeingoverseenbyadoula,unlesstherewere complications.Whileintherefugeecampswomenreceivedroutineprenatalcareandmany gavebirthinclinics.Anewmothertraditionallyrestsforelevendayspostpartum,only caringforandnursingthebaby,andhasarespitefromcookingandhousework.Onthe eleventhday,thechildisnamedduringapurificationritual,performedbyareligious leader.Infantsaretypicallybreastfedexclusivelyforsixmonths.InBhutanifamotherhad troublebreastfeeding,thebabywouldbefedcow’smilk,howeverformulabecame availableintherefugeecamps.IntheUnitedStates,eldersmayincreasinglytakeon responsibilitiesofchildcarewhilethemotherandfatherworkoutsidethehome. Mentalhealth.ThereisahighprevalenceofmentalillnessincludingPTSD,anxietyand depressionfromforceddisplacement,andhavingwitnessedmurders,torture,physicaland sexualviolence.5,6However,thereisastigmaamongBhutaneserefugeesaboutdiscussing 30 theseexperiencesthatmakeitdifficultforthemtoseekhelpuntilsymptomsbecome severe. Traditionalmedicine.Traditionalhealersmaybeconsultedtosupplementtheuseof modernmedicine.OftenfamiliestryseveralhomeremediesbeforeseekingWestern medicine.Someexamplesoftraditionalmedicineincludeusingbasiltotreatcoughsand thecommoncold;usinggarlic,turmeric,gingerandcardamomforstomachailmentsand massagingwithwarmmustardoiltoreducedmuscleaches. SomeBhutanesemayfollowfoodrestrictionswhentheyaresickorpregnant,asthey believecertainfoodsshouldbeavoided.Thesepracticesmayhavetobeexplicitlyaskedof patientswithadisclaimerofunderstandingandacceptancebeforetheymaybewillingto sharethisinformationtoaprovider. SocialEtiquette PermissionshouldbegrantedbeforecomingtoorenteringBhutanesehomesand prayerareas,whichmaybeinthekitchen. SomeBhutanesecustoms,suchasarrangedmarriage,marryingyoung,andthe occasionalpracticeofpolygamymayconflictwiththeAmericanway,legalsystem andculture. Genderrolesaretraditionallydefined,withfemalesperformingthemajorityofthe householdworkwhilemenaretheprimarydecisionmakersinthefamilyand community. DuetopastexperienceswiththeBhutanesegovernment,Bhutaneserefugeesmay beafraidandfearfulaboutcallingthepoliceforassistance. “Headwiggle”meansyesormaybe. Especiallyforelders,handshakingandeyecontactmaymakethemuncomfortable atfirst.Notmaintainingeyecontactisasignofrespect. Whenfirstofferedfood/drinkitispolitetosayno,willacceptonsecondoffer. Huggingisonlydonebetweenromanticcouples. Traditionally,Nepali‐speakingBhutaneseeatwiththeirhands. 31 Commonlyusedphrases7 English Hello/Goodbye/Iblessthedivinein you Pleasedtomeetyou Thankyou Yes No Idon’tunderstand ExcuseMe/Sorry Getwellsoon Nepali Namaste tapaaiilaaiibhetterakhushii laagyo Dhanyabad Huncha/Ho Hudaina/Haina mailebujhina maaphaganus chadainikohunuhos AdditionalResources TheVermontBhutaneseAssociation:http://vermontbhutaneseassociation.org/ CulturalOrientationResearchCenter.BhutaneserefugeesinNepal.October2007No4. RetrievedJune28,2012from http://www.cal.org/co/pdffiles/backgrounder_bhutanese.pdf Dunkle,S.etal2011.VitaminB12deficiencyinBhutaneserefugees—Nepal.Abstract, EpidemicIntelligenceService. Ellis,H.Suicidesamongresettledrefugees.RetrievedJune20,2012from http://www.refugeehealthta.org InternationalRescueCommittee.ThehealthofrefugeesfromBhutan:February2009. RetrievedJune29,2012from http://www.cal.org/co/email_discussion/Attachments/IRC‐ Bhutanese_Health_FactSheet.pdf MaxymM,etal.Nepali‐speakingBhutanese(Lhotsampa)culturalprofile.2010.Retrieved July1,2012fromhttp//www.ethnomed.org. UnitedNationsHighCommissiononRefugees(UNHCR),HealthInformationSystem (HIS).RetrievedJuly2,2012http://www.unhcr.org/pages/4a30c06f6.html VTRefugeeResettlementProgram,RefugeesinVermontbyCountryofOrigin,FY89‐ FY11.Colchester,VT:2012. TheWorldFactbook.AccessedJune28,2012. https://www.cia.gov/library/publications/the‐world‐factbook/geos/so.html References 1. UnitedNationsHighCommissiononRefugees(UNHCR),HealthInformationSystem (HIS).RetrievedJuly2,2012http://www.unhcr.org/pages/4a30c06f6.html 2. InternationalRescueCommittee.ThehealthofrefugeesfromBhutan:February2009. RetrievedJune29,2012from http://www.cal.org/co/email_discussion/Attachments/IRC‐ Bhutanese_Health_FactSheet.pdf 32 3. Dunkle,S.etal2011.VitaminB12deficiencyinBhutaneserefugees—Nepal.Abstract, EpidemicIntelligenceService 4. InternationalRescueCommittee.ThehealthofrefugeesfromBhutan:February2009. RetrievedJune29,2012from http://www.cal.org/co/email_discussion/Attachments/IRC‐ Bhutanese_Health_FactSheet.pdf 5. Ellis,H.Suicidesamongresettledrefugees.RetrievedJune20,2012from http://www.refugeehealthta.org 6. MaxymM,etal.Nepali‐speakingBhutanese(Lhotsampa)culturalprofile.2010.Retrieved July1,2012fromhttp//www.ethnomed.org. 7. Fromhttp://www.omniglot.com/language/phrases/nepali.php 33 Thispageintentionallyleft blank. 34 BosnianandHerzegovinian CountryInformationa Location: SoutheasternEurope,alongtheAdriaticSea;borderingCroatia, Serbia,andMontenegro Capital: Sarajevo Area: 51,197sq.km.(slightlysmallerthanWestVirginia) Climate: Hotsummersandcoldwinters.Areasofhighelevationhaveshort, coolsummersandlong,severewinters.Mild,rainywintersalong coast. Language: Official:Bosnian,Croatian.Other:Serbian Note:somesourceslistSerbianasanofficiallanguage.Inthis chapterweincludeallthreelanguagestobeasinclusiveas possible. People: Threeethnicgroupspredominate:Bosniak(48%),Serbian(37%), Croat(14%).MostBosniaksself‐identifyasMuslims,Serbsas EasternOrthodox,andCroatsasRomanCatholic. Population:InBosnia‐Herzegovina:4.6million InVT:1710b a Unlessotherwisecited,allinformationonthispageisfromtheUnitedStatesofAmerica,CentralIntelligence Agency,TheWorldFactbook.AccessedApril,2012. https://www.cia.gov/library/publications/the‐world‐factbook/geos/bk.html b VTRefugeeResettlementProgram,RefugeesinVermontbyCountryofOrigin,FY89‐FY11.Colchester,VT: 2012. 35 36 37 Backgroundandculture BosniawasonceapartoftheSocialistFederalRepublicofYugoslavia.However,inthe early1990s,amovementforanindependentBosnianstatetookshape,culminatinginthe declarationofBosnianindependencein1992andformalrecognitionbytheUnitedNations onMay22,1992.1Subsequently,civilwarbrokeoutbetweentheBosniaks,BosnianSerbs, andBosnianCroatsinathree‐waystruggleforpoliticalpower.Asaresultofthewar,more than2millionBosniansfledthecountry.Althoughthewarofficiallyendedin1995withthe signingoftheDaytonPeaceAccords,asof2009anestimated1millionrefugeesremaineda partoftheBosniandiaspora.2 Language.BosniaandHerzegovinahasatleasttwoofficiallanguages—Bosnianand Croation—andsomesourceslistSerbianasathirdofficiallanguage.Themostcommonly spokenlanguageisBosnian.AminorityoftheBosnianpopulationmayalsospeakRomany, Hungarian,Albanian,orSlovene.1 Religion.Religiousaffiliationfallspredominantlyalongethniclines:Bosniakstypically self‐identifyasMuslim,SerbsasEasternOrthodox,andCroatsasCatholic.TheJewishand Protestantfaithsarealsorepresentedinasmallminorityofthepopulation.1 Family.TheBosnianfamilystructurediffersbetweenruralandurbanBosnia.Rural familiesaretypicallypatriarchal,withwomenbearingresponsibilityforthemajorityof domestictasks,andhouseholdsmayincludeseveralmembersoftheextendedfamily(e.g. grandparents.)Inurbansettings,housingdoesnotgenerallyincludeextendedfamily,and responsibilitiesaresharedbetweenhusbandandwife.Inbothruralandurbansettings, childrenareexpectedtocareforelderlyparents.Becauseofthewar,manyrefugeefamilies maybeheadedbywidows.3 Education.Primaryeducationlastsfornineyears,startingatagefiveorsix,andis compulsory.Secondaryeducationmaytakeplaceatathree‐yearvocationalschool,afour‐ yeartechnicalschool,oratafour‐yearuniversity‐preparatoryschoolcalledagimnazia. Post‐secondaryeducationisavailableateightuniversities. Diet.AllthreemealsarerepresentedinaBosniandiet,althoughlunchisthemainmealof theday.Thereisaparticularemphasisonmeatanddairy,especiallybeef,lamb,andpork, althoughstrictMuslimsdonoteatpork.Brandyisapopulardrink,althoughwine,beer, coffee,andsoftdrinksarealsoconsumed.3 HealthCare PrimarycareisfreetothecitizensofBosnia,butpaymentisrequiredforsomemedications andprocedures.Primarycareoccursmainlyincommunity‐basedclinicscalledambulantas; theirprimaryfunctionistriage,withpatientssenttolargersecondary‐carefacilitiesfor diagnosisandtreatmentbyspecialists.Complicatedcasesmaybereferredtotertiarycare facilitiesatuniversityorteachinghospitals.4Ingeneral,hospitalsareunder‐equippedand privatepracticesaretooexpensiveformostcitizens.Overallhealthcareisholistic,with emphasisonvitamins,teas,andotherhomeremedies—oftenduetoalackofaffordable 38 medications.3Thelargestburdenofdiseaseisfromcardiovasculardisease,followedby neuropsychiatricdisease,thenneoplasia.5Depression,anxiety,andPTSDarecommonasa resultofthewar.6HIV/AIDSprevalenceis<.1%.7 UniversalfreehealthcareisavailableinBosnia;asaresult,patientsmaybe concernedabouttheirabilitytopayforcareintheUnitedStates. PrimaryhealthcareplaysasmallerroleinBosniathanitdoesintheUnitedStates, andinpatienthospitalstaysareoftenlonger;asaresult,patientsmaybeconcerned aboutthequalityofprimarycare,andofshort‐durationhospitalstays. SpecialistsplayalargerroleinroutinecareinBosniathanintheUnitedStates,with primarypractitionersservingalargelytriage‐orientedfunction;asaresult,patients maybeconcernedaboutthebroaderscopeofprimarycareintheU.S. ManypatientsmaybeintimidatedbythebureaucracyoftheUShealthcaresystem. Treatmentisoftennotconsideredcompletewithoutmedication,andmanypatients willexpectadetailedexplanationoftheirillnessandcourseofdisease. MentalillnessandphysicaldisabilitycarryastigmaformanyBosnians. DentalcaremaybeavoidedbecauseofinadequatedentalservicesinBosnia. Smokingisverycommon,whileanunderstandingofsecondhandsmokeisnot;in particular,childrenmaybeatriskofexposuretosecondhandsmoke. Althoughspecificexamplesoftheprocessofmedicaldecision‐makinginBosniaare scarce,severalresourcessuggestthatdecision‐makinginvolvestheentirefamily, especiallywhendecisionsconcernend‐of‐lifecare.8,9 SocialEtiquette Whileitisimportanttorealizethatwhatconstitutesacceptablesocialconductinone contextmaybeinappropriateinanother,thefollowinggeneralizationsmaybemadeabout Bosniansocialetiquette10: Eyecontactisconsideredacceptable;lookingstraightintosomeone’seyesisasign ofhonesty. Ahandshakeisthepreferredgreetingbetweenmembersofthesamesexand membersoftheoppositesex. Viewsonpunctualityvary;whileexpectedinbusinesssettings,ininformalmeetings itislessimportant. Itisconsideredgoodmannerstogreettheoldestpersonpresentfirst. 39 CommonlyUsedPhrases English Bosnian Serbian Croatian Hello Dobardan Zdravo Bok Goodbye Dovidjenja Cao Dobidjenja Please Molim Molim Molim Thankyou Hvala Hvala Hvala Goodmorning Dobrojutro Dobrojutro Dobrojutro Goodevening Dobrovec̆ er Dobrovec̆ er Dobrovec̆ er Yes Da Da Da No Ne Ne Ne Tohearsomeofthesephrases(andothers)pronounced,visithttp://www.bbc.co.uk/ languages/european_languages/languages/index.shtmlandselectalanguagefromthe menuontheleft‐handsideofthescreen. AdditionalLanguageResources Bosnian/English,Croatian/English,andSerbian/Englishdictionariesareavailableonlineat http://ba.rjecnik.com/,http://www.rjecnik.com/logindict.cgi,and http://www.recnik.com/,respectively. GoogleTranslatesupportsCroatian/English,Serbian/English,Hungarian/English, Slovene/English,andRomany/Englishtranslations,availableat http://translate.google.com/#. Additionaltranslatedhealthinformationisavailableat: http://healthinfotranslations.com/bosnian.php (Bosnian) http://www.mhcs.health.nsw.gov.au/mhcs/languages/Serbian.html(Serbian) http://www.mhcs.health.nsw.gov.au/mhcs/languages/croatian.html(Croatian) 40 References 1. UnitedStatesDepartmentofState.BackgroundNote:BosniaandHerzegovina. 2012;http://www.state.gov/r/pa/ei/bgn/2868.htm.AccessedApril,2012. 2. BosnianInstitute.AboutBosnia:Diaspora. http://www.bosnia.org.uk/bosnia/viewMetatype.cfm?metatypeID=35.Accessed April,2012. 3. SPIRASI.Bosnia‐Herzegovina.SPIRASICulturalProfilesProject2006; http://cultural.profiles.spirasi.ie/countries/bosnia%20‐h.shtml.AccessedApril, 2012. 4. SearightHR.Bosnianimmigrants'perceptionsoftheUnitedStateshealthcare system:aqualitativeinterviewstudy.JImmigrHealth.Apr2003;5(2):87‐93. 5. WorldHealthOrganization.HighlightsonHealthinBosniaandHerzegovina2005. 2006;http://www.euro.who.int/__data/assets/pdf_file/0014/103208/e88283.pdf. AccessedApril,2012. 6. IowaCenteronHealthDisparities.BosniansandOtherRefugeesFromtheFormer Yugoslavia. http://www.iowahealthdisparities.org/documents/bosniansrefugees.pdf.Accessed April,2012. 7. CentralIntelligenceAgency.TheWorldFactbook:BosniaandHerzegovina. https://www.cia.gov/library/publications/the‐world‐factbook/geos/bk.html. AccessedApril,2012. 8. SearightHR,GaffordJ."It'slikeplayingwithyourdestiny":Bosnianimmigrants' viewsofadvancedirectivesandend‐of‐lifedecision‐making.JImmigrHealth.Jul 2005;7(3):195‐203. 9. WeineSM,WareN,KlebicA.Convertingculturalcapitalamongteenrefugeesand theirfamiliesfromBosnia‐Herzegovina.PsychiatrServ.Aug2004;55(8):923‐927. 10. CultureCrossing.BosniaandHerzegowina. http://www.culturecrossing.net/basics_business_student.php?id=27.Accessed April,2012. 41 Thispageintentionallyleft blank. 42 Burmese–NEW! CountryInformationa Name: UnionofBurma [sometimescalledMyanmar,thename adoptedbytherulingjunta;not recognizedbytheUnitedStates] Location: SoutheasternAsia,betweenBangladesh andThailand;borderstheAndamanSea andtheBayofBengal Capital: Rangoon[junta’sunrecognized administrativecapitalisNayPyiTaw] Area: 676,578sq.km.(slightlysmallerthanTexas) Climate: Tropical.June‐Sept(southwestmonsoon)cloudy,rainy,hot, humid.Dec‐April(northeastmonsoon)lesscloudy,scantrainfall, mildtemperatures,lowerhumidity. Language: Official:Burmese.Other:Karen,Chin People: EthnicitiesincludeBurman(68%),Shan(9%),Karen(7%) Population: InBurma:54million RefugeesinThailand:350,000b InVT:119c a Unlessotherwisecited,allinformationonthispageisfromtheUnitedStatesofAmerica,CentralIntelligence Agency,TheWorldFactbook.AccessedApril,2012. https://www.cia.gov/library/publications/the‐world‐factbook/geos/bm.html bUnitedNationsHighCommissioneronRefugees,ComprehensivePlanAddressingtheNeedsofDisplaced PersonsontheThailand/Myanmar(Burma)Border.AccessedApril,2012.http://www.unhcr.org/cgi‐ bin/texis/vtx/search?page=search&docid=4691eaa82&query=A%20comprehensive%20plan%20addressing %20the%20needs%20of%20displaced%20persons%20on%20the%20Thailand/Myanmar%20%2528Burm a%2529%20border%20in%202007/8 cVTRefugeeResettlementProgram,RefugeesinVermontbyCountryofOrigin,FY89‐FY11.Colchester,VT: 2012. 43 44 45 Backgroundandculture PositionedasamajorcrossroadsinSoutheastAsia,Burmaisoneofthemostdiverse countriesintheworld,witheightmajorethnicpopulationsand130individualsubgroups. Suchdiversitycreatesarichculturallandscape,butitalsosetsthestageforinternal conflict,leavingBurmawiththedubiousdistinctionashomeofoneoftheworld’slongest‐ runningcivilwars.1Until1948,whenBurmeseforcesgainedtheirindependence,Burma wasgovernedbytheBritish:firstasanadministrativeprovinceofIndiaandlaterasaself‐ governingcolony.2Followingindependence,Burmaestablishedaparliamentary government,butpoliticalandethnicconflictcontinued.In1962GeneralNeWinstageda militarycoup,installedaxenophobicauthoritariangovernment,andlaunchedthe “BurmeseWaytoSocialism.”3 ToovercomeresistancefromtheKaren(pronouncedkah‐REN)ethnicgroupthatbeganin 1949andcontinuestoday,NeWinestablishedthe“fourcuts”policytargetingthe insurgents’food,funds,recruits,andinformation.Thestrategyessentiallyamountedto destroyingvillages,whichspawnedamajorrefugeemovementtocampsontheBurmese‐ Thaiborder.4In1988,politicaloppressionandaflaggingeconomyprecipitatedanother rebellion,promptingNeWintostepdown.Theuprisingwasquicklyquashedbysecurity forcesandanewmilitaryjuntaassumedcontrolofthecountry,whichcausedanotherflood ofrefugeestoThailand,andproducedscoresofinternallydisplacedpersons.Themilitary regimeheldfreeelectionsin1990,butitrefusedtostepdownaftertheopposingNational LeagueforDemocracyswept80%oftheseats.Forthenext20years,oppositiongroups continuedtochallengethemilitaryrulewithviolentandnon‐violentprotests;themilitary respondedwithviolentcrackdowns,widespreadarrests,andthekillingofdissidents.This conflictexacerbatedtherefugeecrisis.3 Today,the“StatePeaceandDevelopmentCouncil,”amilitaryjunta,continuestorulethe UnionofBurma.Theregimechangedthecountry’sofficialnametoMyanmarin1989,but manycountriesandinternationalregimes,includingtheUnitedStates,donotrecognizethe namechange. Language.AlthoughBurmeseistheofficiallanguage andisunderstoodbymuchofthepopulation,many Membersofethnic ethnicgroupsspeaktheirowndialect.TheKaren minoritiesmayview dialectfallsintotwomainsubgroupsthatlargelyfollow Burmeseasthe ethniclines:Sgaw‐KarenandPwo‐Karen.Seventy languageof percentofBurmeserefugeesinThaicamps—andthusa oppressionandmay majorityofBurmesenowintheUnitedStates—speak prefertouseastrictly Sgaw‐Karen.Thesedialectsaresimilarinstructure,but Burmesetranslator theirdifferentpronunciationscangreatlyimpede 5 onlyasalastresort. understandingbetweennativespeakers. Religion.ThemajorreligionsinBurmaareBuddhism, Christianity,Animism,andIslam.Asisthecaseinmanycountries,eachfaithdraws membersfrommanydifferentsub‐populationsbuttheretendstobeadominantreligious 46 affiliationamongeachethnicgroup.ThemajorityofBurmansareBuddhistwhiletheChin aremorelikelytobeChristian,particularlyBaptist.6TheKarenalsohaveasizeable Christianpopulation,buttheyaremorecommonlyBuddhist;manypracticingKaren Buddhistsincorporateanimistbeliefs. Animism,whichwasprevalentinBurmabeforemissionariesintroducedChristianity, centersonthebeliefthatalllivingthingshaveaspirit,calledK’la,whichcanbeattackedby dangerousspirits.Manypeoplemayengageinhealingritualsorwearcharmstoprotect theirK’la;additionally,duringsleep,theK’lacandepartthebodysooneshouldtakecare nottowakeapersonbeforetheK’lahasreturned.Someanimistswilltiearedstring aroundtheirwristtohelpretaintheirk’lawhichprovidersshouldremoveonlyif absolutelynecessary. Peopleofallreligionsmayincorporateprinciplesfromayurvedicsystems,alchemyand Chinesemedicine.4 Family.AsinmanyAsiancultures,familyistremendouslyimportantinBurmaandthe broadfeatureshighlightedhereareconsistentacrossthemajorethnicgroups.Historically, membersoftheextendedfamilylivedtogether,andrecentpooreconomicconditions reinforcethistendencybothinBurmaandamongresettledrefugeepopulationsinthe UnitedStates.Itisparticularlycommonfornewly marriedcouplestomoveinwiththeirparents, especiallythewife’s.Withinthefamilystructure, Communalchildrearingin eldersandmenhavethemostauthority,but BurmaandThaiRefugee women’sopinionsarerespectedandwomen campsfacilitateda maintaininheritanceandpropertyrightsupon tendencyforBurmese divorce(exceptChinwhereinheritancefalls parenttoallowtheir exclusivelytomaleheirs).5Pregnantwomen 7 childrentowanderwidely. commandrespectaswell. Careprovidersmayneed towarnparentsaboutthe TheBurmesegenerallyviewchildrearingasa dangersofthispractice, communalresponsibilityandlargefamiliesare 4 especiallyinareaswith common. OnceinAmerica,traditionalBurmese heavytraffic. familystructurecanbecomemorefluid:familiesare oftensmaller,couplesmayoptforengagementsand bigceremoniesratherthansmall,officialweddings, andmenandwomenmaysharehouseholdchores. Education.Burmesesocietyplacesahighvalueoneducationforbothmalesandfemales, howeverconflictoreconomicdemandsoftentruncatethelengthofstudents’schooling.In Burma,governmentalexpenditureoneducationisquitelow(1‐2%ofGDP)butthesystem includesfouryearsofprimaryschool,fouryearsofmiddleschool,andthreeyearsofhigh school.DuetoprotestsamongUniversitystudentsandretaliatorygovernmentaction,the Burmesehighereducationsystemlacksastrongfoundation,particularlyinruralareas wherestudentsareincreasinglylikelytoenrollincorrespondenceorvocationalcourses.5 47 ThereisnoformalaccesstoeducationintheThairefugeecamps.TheRoyalThai Governmentviewstherefugeecampsastemporary,thereforetheydonotallowBurmese refugeesintoThaischools.Withinthecamps,however,thegovernmenthasadopteda laissez‐faireattitude,soeducationisadministeredbytherefugeesthemselves.Withthe assistanceofsomeinternationalnon‐governmentalorganizations(NGOs),schools operatingwithinthecampsprovideeducationfromnurserythroughadultlevels.Since Thailawbarsrefugeesfromholdingjobsoutsidethecamps,thepaucityofjobprospects underminesanyincentiveforstudentstostayinschool.8 Diet.RiceissuchanintegralpartoftheBurmesedietthattheliteraltranslationfor‘how areyou?’is‘haveyoueatenricetoday?’Peopletypicallyeatricewithvegetablecurriesand addmeatorafishpasteasavailable;mostmealsareheavilyspiced.OlderBurmesemay enjoybetelnut,aspiceddishcombiningnuts,lime,andspicesthatismildlysedatingand stainstheteethred.5 Formanyethnicgroups,andespeciallytheKaren,foodisintimatelylinkedtoillness. Burmesetendtocharacterizebothfoodanddiseaseaseither‘hot’or‘cold’andprescribea diettocounteracttheeffectsofsickness—thusifapatienthasahotillness,acareprovider willrecommendacolddiet.Importantly,theclassificationoffoodashotorcolddoesnot necessarilycorrelatetoitsphysicaltemperature.Hotfoodsincludedishesthataresalty, sour,orhighinanimalproteinwhereascolddishesfeaturesweetorbitterflavors.7 Distinctmedicalconditionscanfurtherprecipitatespecificdiets,forexamplepeople diagnosedwithhepatitisareencouragedtoavoidyellowfoods.4 Healthcare Infectiousdisease.IntestinalparasitesareverycommonamongnewlyarrivedBurmese refugees:15%ofthepopulationtestedpositiveforatleastonepathogenicinfectionduring theirdomestichealthexamination,mostcommonlyforgiardiaorstrongyloides.9 MalariaisalsoaseriousconcernforBurmeserefugees,bothbecauseBurmaishometoone ofthemostdrugresistantstrainsandbecausemanyrefugeesspenttimeinthejungle duringperiodsofinternaldisplacement.Malariaissocommonthatrefugeesarelikelyto attributenearlyallfeverstomalaria.Itisimportantforcareproviderstodifferentiate betweenmalariaanddenguefeverwhichisalsoveryprevalent.4 Hepatitisiscommon,butalthoughpeopleareawareofthediseasetheymaynot understandtheimplications.TheKarencommunityinMinnesotareportedthatthey preferredwhendoctorsgavespecificadviceregardingtreatmentandtoldthemexactly whattodo.Diagnosinghepatitiswillalsolikelyinvitequestionsaboutfood,asmany Burmesebelievethatpeoplewithhepatitisshouldn’teatyellowfoodsorfishpaste.Evenin theabsenceofquestions,physiciansshouldexplainthatfoodwillnotalterthecourseofthe disease.4 Burmaranksasoneofthe22high‐burdencountriesfortuberculosis(TB),accordingtothe WHO.TBisstigmatizedinBurmatosuchanextentthatinterpretersmaybereluctantto 48 translateforpatientsduringhomevisitsforfearthattheywillbeassociatedwiththe illness.Alongsimilarlines,patientswithTBoftenexpressgreaterconcernaboutthe disease’simpactontheirplaceinthecommunitythanontheirpersonalhealth.Healthcare providersandBurmesecommunitymembersmayalsohavedifferentdefinitionsof “contacts”,wherepeoplewhocomeandgofrequentlycanbeconsiderednormaland thereforenotconstituteareportableevent.10TBratesarehigheramongtheShan ethnicity.11 Lifestyleriskfactors.Forrecentlyresettledrefugees,malnutritionisamajorhealth concern.Inaddition,thechewingofBetelnutandlimitedaccesstodentalcarecan negativelyimpactoralhealth,leadingtotoothdecayandoralcancers.12Approximately 19%oftheKarenrefugeepopulationsmokes,and80%ofthesmokersaremen.9Ratesof cigaretteandalcoholconsumptionareoftenhigherwithintheChinsubpopulation,where bothpracticesareconsideredtobeastatussymbol.6 AswithmanypopulationsunfamiliarwiththeWesternmodelofcare,Burmeserefugees mayhavetroublewithchronicdiseasemanagement,especiallyiftheirtreatmentplan includestakingmedicineintheabsenceofsymptoms.9 Finally,manyBurmesepeopleareatincreasedriskforleadpoisoning.Althoughsuch contaminationcancomefromfamiliarsourcessuchasoldhomes,theremayalsobe culturalfactorstoconsider.Chiefamongthesearetwofolkdigestiveaids,DawTwayand DawKyin,whichcancontainveryhighlevelsoflead.Inaddition,prolongedexposuretocar batteries—amajorenergysourceforhomesinThaicamps—hasbeenimplicatedinlead poisoning,13andincreasingevidencesuggestsalinkbetweenleadpoisoningandthe practiceofwearingthanaka¸apastemadefromgroundthanakatreeandappliedtothe cheekstoactasacosmetic/sunscreen.14 Familyplanningandchildbirth.Historically,sexeducationinBurmahasbeen nonexistent,buttherehasbeensomemovementtowardHIVeducationinschools. NumerousstudiesconductedinThairefugeecampsindicatethatresidentshavelimited knowledgeaboutreproductivehealth.ThoughsomeBurmesedousecontraception,the socialcapitalofchildrenandabeliefthatcondomsencouragepromiscuitylimitits widespreadadoption.15ProvidersintheUnitedStatesshouldfocusoneducation,andmay findgreatersuccessbycouchingdiscussionsaboutcontraceptionintermsofchildspacing ratherthanpreventingpregnancyaltogether. Asnotedpreviously,pregnantwomenholdaplaceofhonorinBurmeseculture,however pregnancyoutsideofmarriageisasocialtaboo.Duringpregnancy,womenobserveastrict dietaryandbehavioralregimeduetothebeliefthateverysound,touch,taste,smellor actionofthemotherhasaneffectonthefetus.7Womeninrefugeecampsandthose relocatedtoWesternnationsreportpreferringhomebirthstohospitaldeliveries,citing shame(vaginalexams,exposedlegs,thepresenceofmalehospitalstaff)astheirbiggest deterrent. 49 Postpartum,womenaretreatedverydelicately:inthefirstthreedaysthemotherdoesn’t move,relyinginsteadonherhusbandtofeedandbathehertwiceaday,andtotendafire nexttoherbedmeanttoensurewarmth(heatersorhotwaterbottlesmaybeacceptable substitutesinhospitalsettings7).Restrictionscontinueduringthemonthafterdeliveryasa precautionagainst“sickfever.”Althoughmovementisincreasinglyallowed,womenstilldo notgooutside,theymaintainalimiteddietofsoupandrice,andavoidcoldwater completely.AlthoughmanyfamiliesadaptsuchtraditionalpracticesinaWesternsetting, careprovidersshouldstillengagepatientsinconversationsregardingthelengthoftheir hospitalstayandtransportationhome. Mostmothersbreastfeedtheirinfantsforapproximatelyoneandahalfyears,althoughthis periodcanextendtothreeyears.Giventheimportanceofrice,Karenpeopletraditionally feedinfantsafewgrainsbeforecommencingbreastfeeding;accordingly,caregiversshould educatepatientsabouttherisksassociatedwithprelactealfeeds.7 Mentalhealth.Burma’slongstandingcivilwarhasmeantsubjectiontoforcedlabor,rape, violence,andlong‐termfamilialseparationformanyrefugees,withmeasurable consequencesformentalhealth.A2004studybyCardozoetal.foundelevatedlevelsof anxietyanddepressionamongrefugeeslivinginThai‐Burmesebordercampsandlevelsof post‐traumaticstressdisorderwerecomparabletothoseofotherpopulationsthathad experiencedwarandupheaval.16 Treatingmentalillnessinthispopulationcanbeproblematic.Asinmanycultures,the stigmatizationofmentalhealthproblemscanmakepatientsreluctanttoreport symptoms.17Furthermore,manyBuddhistsbelievethattheircurrentcircumstanceisa reflectionoftheiractionsinpastlives,soanydepressedoranxiousfeelingstheymaybe experiencingarejustpunishmentforpriormisdeeds,andthusshouldnotbetreated.Care providersshouldaskquestionstoelicitpatientbeliefsregardingtheoriginoftheir symptoms.18 Traditionalmedicine.TraditionalmedicineinBurmamaydrawonpracticesfrom neighboringAsiancountries,particularlyIndiaandChina.Cupping(seechapteron Vietnam)isnotuncommon.Traditionalbelieftendstoholdthatmalevolentspiritscause illnesssopatientsmaycalluponshamanswhenseekingtreatment.19Mostremediescenter onbalancinghotorcoldillnesswiththeoppositefood(seesectionondiet)oronplant‐ basedmedicines. SocialEtiquette Burma’svastethnicdiversityunderminesanymonolithicnotionofculture.SincetheKaren representthelargestethnicgroupintheU.S.,theyaretheprimaryfocusofthissection, howevertheChinandBurmanpeoplesarealsodiscussed. Aswithanygroup,theapplicabilityoracceptabilityofthesenormsmaydifferbetween ethnicgroupsandindividuals.Itisimportantforproviderstocommunicatewiththeir patientstoachievethehighestlevelofcomfortinthecareprocess. 50 Crossedarmsduringconversationisasignofrespect. Burmeseconsidertheheadtobeboththeliteralandfigurativehighestpartofbody, therefore: ‐ theheadshouldnotbetouchedbyanotherperson,and ‐ objectsshouldneverbepassedoveraperson’shead.19 Thefeetarethelowestpartofthebodyandshouldneverpointdirectlyatsomeone; whenseated,theyshouldbetuckedunderthebody.19 Whenshakinghandsorpassingobjects,oneshouldextendtherighthandwhile supportingtherightelbowwiththelefthand. Nothingshouldbepassedwiththelefthand,whichisusedforpersonalhygiene behaviors.19 Usebothhandstoacceptagift,especiallyfromanelder. Walkingbehindsomeoneismorerespectfulthanwalkinginfront,especiallyifthe bystanderisseated;ifonemustwalkinfrontitiscustomarytoexcuseoneself. Pickingone’snoseiscommonplace,howeverblowingone’snoseintoatissueis considereddisgusting.19 Traditionally,KarenandChinareonlygivenonename,althoughtheymayadopta familynameaftermovingtoWesterncountries;nameordercanleadtocharting confusion. Peopleareaddressedbytheirgivennameandatitle,oftensignifyingthe relationshiptothespeaker(aunt,elder,teacher,etc.).9 AmongtheChinethnicgroup,directeyecontactcanbeinterpretedasachallenge ratherthanasignofcompassion.6 Medicaldecisionsarefrequentlymadebyconsensus.4 Patientsmayanswer“no”toaquestiontobemodest,whenthemoreaccurate answeris“yes.7” Menandwomendon’tusuallytouchinpublic,butaffectionategesturesamong membersofthesamesexarecommon. Patientsreportapreferenceforsamegenderproviders.4 51 References 1. ThorntonP.RestlessSouls:AsiaBooks;2006. 2. CentralIntelligenceAgency.TheWorldFactbook:Burma. https://www.cia.gov/library/publications/the‐world‐factbook/geos/bm.html. AccessedApril,2012. 3. UnitedStatesDepartmentofState.BackgroundNote:Burma.2011; http://www.state.gov/r/pa/ei/bgn/35910.htm#history.AccessedApril,2012. 4. NeimanA,SohE,SutanP.KarenCulturalProfile.2008; http://ethnomed.org/culture/karen/karen‐cultural‐profile.AccessedJuly,2011. 5. BarronS,OkellJ,YinSM,etal.RefugeesfromBurma:TheirBackgroundsandRefugee Experiences.Washington,DC:CenterforAppliedLinguistics;2007. 6. ScarlisCA.ChinCulturalProfile.2010;http://ethnomed.org/culture/chin/chin‐ cultural‐profile.AccessedJuly,2011. 7. StateofQueensland.Burma:Karen,Chin,andRohingyaEthnicities. http://www.health.qld.gov.au/multicultural/health_workers/Burmese‐preg‐ prof.pdf.AccessedJuly,2011. 8. OhS‐A.EducationinRefugeeCampsinThailand:Policy,PracticeandPaucity: CommissionedfortheEFAGlobalMonitoringReport2011:TheHiddenCrisis: ArmedConflictandEducation;2010. 9. PowerDV,MoodyE,TrussellK,etal.CaringfortheKaren.Anewlyarrivedrefugee group.MinnMed.Apr2010;93(4):49‐53. 10. NewJerseyMedicalSchoolGlobalTuberculosisInstitute.ReachingOutToBurmese Refugees.TB&CulturalCompetency:NotesfromtheField,Spring2008.Vol7. Newark,NJ:NewJerseyMedicalSchoolGlobalTuberculosisInstitute;2008. 11. SuwanvanichkijV.Displacementanddisease:TheShanexodusandinfectious diseaseimplicationsforThailand.ConflHealth.2008;2:4. 12. LeeKW,KuoWR,TsaiSM,etal.Differentimpactfrombetelquid,alcoholand cigarette:riskfactorsforpharyngealandlaryngealcancer.IntJCancer.Dec10 2005;117(5):831‐836. 13. NewYorkStateDepartmentofHealth.WorkingWithRefugeesfromBurmato PreventChildhoodLeadPoisoning.2010; http://www.health.ny.gov/environmental/lead/health_care_providers/working_wi th_refugees_from_burma.htm.AccessedApril,2012. 14. RitcheyMD,ScaliaSucoskyM,JefferiesT,etal.LeadpoisoningamongBurmese refugeechildren‐‐Indiana,2009.ClinPediatr(Phila).Jul2011;50(7):648‐656. 15. CentersforDiseaseControlandPreventionDivisionofReproductiveHealth, AmericanRefugeeCommittee.AnAssessmentofReproductiveHealthIssuesAmong KarenandBurmeseRefugeesLivinginThailand.Atlanta,GA2002. 16. LopesCardozoB,TalleyL,BurtonA,CrawfordD.KarenniRefugeesLivinginThai‐ BurmeseBorderCamps:TraumaticExperiences,MentalHealthOutcomes,and SocialFunctioning.SocialScienceandMedicine.2004;58(12):2637‐2644. 17. KniftonL,GervaisM,NewbiggingK,etal.Communityconversation:addressing mentalhealthstigmawithethnicminoritycommunities.SocPsychiatryPsychiatr Epidemiol.Apr2010;45(4):497‐504. 18. LinKM,CheungF.MentalhealthissuesforAsianAmericans.PsychiatrServ.Jun 1999;50(6):774‐780. 52 19. UKCO.BurmeseCulturalProfile:AToolforSettlementWorkers:International OrganizationforMigration;2005. 53 Thispageintentionallyleft blank. 54 Burundian Country Informationa Location: CentralAfrica,Eastofthe DemocraticRepublicofCongo;bordersTanzania, Rwanda,andtheDemocraticRepublicofCongo Capital: Bujumbura Area: 27,830sq.km.(slightlysmallerthanMaryland) Terrain: Hillyandmountainous,droppingtoaplateauintheeast,some plains;considerablealtitudevariation;averagealtitudeis1700m (5600ft) Climate: Equatorial;averageannualtemperaturevarieswithaltitudefrom 17°Cto23°C(63°Fto73°F)butisgenerallymoderate.Twowet seasons(February‐MayandSeptember‐November)andtwodry seasons(June‐AugustandDecember‐January)annually.Average rainfallis150cm(60”). Languages:Kirundi(official)andFrench(official);SwahilispokenalongLake TanganykikaandnearBujumbura. People: Twomajorethnicities:Hutu(85%)andTutsi(14%). Population: InBurundi:10.2million InVT:105b aUnlessotherwisecited,allinformationonthispageisfromtheUnitedStatesofAmerica,CentralIntelligence Agency,TheWorldFactbook.AccessedApril,2012. https://www.cia.gov/library/publications/the‐world‐factbook/geos/by.html bVTRefugeeResettlementProgram,RefugeesinVermontbyCountryofOrigin,FY89‐FY11.Colchester,VT: 2012. 55 56 57 Backgroundandculture BurundigainedindependencefromBelgiumin1962.Thecountry’sindependencebrought ethnictensionsbetweenthemajorityHutuandminorityTutsitotheforefront.In1966,a TutsimilitaryleaderoverthrewtherulinggovernmentandestablishedaTutsijuntaasthe rulingbody.AHutuuprisingwasputdownin1972andalargeportionofthepopulation wasforcedtofleetonearbycountries,withmostsettlinginrefugeecampsinTanzaniaand Rwanda.Instabilityandethnicviolencemarkedthenextseveraldecades,withthedeath tollestimatedbetween90,000and250,000.Apoliticalassassinationin1993ledtothe outbreakofacivilwar.In1994theinterimBurundianpresidentandthepresidentof neighboringRwandawerekilled,whichonlydeepenedtheethnicconflictbetweenthe HutusandTutsis.1 In2005PierreNkurunzizawonpresidentialelectionsandthisendedthe12yearsofcivil war.Infallof2006thegovernmentsignedacease‐firewiththeForcesforNational Liberation,whichwasthelastremainingrebelgroupthathadnotengagedinpeacetalks. Thecease‐firewasnotimplementedfullyandtheFNLhascontinuedtowreakhavoconthe stabilityofthecountry.Todatehowever,conflictbetweentheHutuandTutsiremains problematicandU.S.citizensareencouragednottotraveltoBurundibecauseofthe violence.Thecountryisoneofthetenpoorestcountriesintheworldandtheeconomyis notstableduetothelackofresourcesandyearsofwarthathaveravagedthecountry.1 TheBurundianrefugeeswhohavebeenresettledinVermontareprimarilyfromthegroup ofpeoplewhofledtoTanzaniain1972.PriortobeingresettledintheUnitedStates,many ofthispopulationweredisplacedmultipletimesandspentyearsinexile. ThemajorityofBurundianrefugeesinVermontarrivedherebetween2007and2008,2 howeverinterviewswiththerefugeesrevealthatsomehavebeeninthestatesinceasearly as2004.3Currently113BurundianrefugeeshavebeenresettledinVermont.4Mostofthe VermontBurundianshavecomefromrefugeecampsinTanzania,howeversomearrived fromZambiaandMozambique.3 Language.MostBurundiansspeakKirundiandSwahili.SomeeducatedBurundiansmay alsospeakFrench.Seetheendofthissectionforatranslatedlistofcommonly‐used phrases. Religion.ThemajorityoftheBurundiansareChristian:62%areRomanCatholicand another5%areaffiliatedwithvariousProtestantdenominations.Inaddition,roughly10% ofBurundiansareMuslimand23%followindigenousreligiousbeliefs.1InVermont,about one‐thirdoftheBurundiansareProtestantandtwo‐thirdsareCatholic.3Religionplayeda centralroleintherefugeecampswheretheBurundipeopleweredisplacedandalsoplays animportantroleintheirlifeintheUnitedStates.2,3 Family.Burundiansvaluetheirfamiliesaboveeverything.Assistingandcaringforfamily membersinneedisofutmostimportance.Individualismandplacingone’sownneeds abovethoseoffamilyislookeddownupon.ThefamilysysteminBurundiispatriarchal. 58 Thefatheristheheadofthefamilyandmakesthemajorityofthedecisionsforthefamily. Womenarevaluedfortheirroleinchildbearingbuthavelittledecision‐makingpowerin thesociety.Eldersholdahighroleofrespectinsociety.1,2Achallengeformanyofthe refugeesisthatmanyoftheirfamilymembersremaininrefugeecampsinAfrica.3 Education.TheBurundiangovernmentdidnotpassfreepubliceducationforallchildren until2005.Schoolingisnowrequiredforchildrenagesevento12.Becauseattending schoolrequirespurchasingschoolsuppliesanduniformsmanyfamilieschoosetosend onlytheirsonstoschool.1Intherefugeecampsmostchildrenreceivedfreeprimary education,howeverthecampschoolswereoftenovercrowdedandattendancewas sporadic.Ithasbeenestimatedthat20%oftheadultpopulationisliterate.2 Diet.AtypicalBurundiandietincludesrice,beans,cornmeal,potatoes,fish,meat,and greens.MostBurundiansareopentolearningabouthealthyeating.Mosthavegained weightsincearrivingintheUnitedStates.Typicaldrinksincludewater,milk,tea,juice,and occasionallybeerandsoda.3 Healthcare Mentalhealthissuesarecommonduetothestressfullifeofarefugee.Somerefugeeshave witnessedtraumaticevents,increasingtheirriskforpost‐traumaticstressdisorder(PTSD). ManyBurundiansareanxiousbecausesomeoftheirfamilymemberswereleftbehindat therefugeecamps.Notalltherefugeesknowhowtohandlethesestresses.Highratesof malariaarepresentintherefugeecamps.HIVincidenceislowintherefugeecamps,but highinthecountryofBurundiitself.2WhenBurundiansvisittheirphysician,theyexpectto receivesomesortofmedicationorshot,inadditiontohavingtheirvitalsignstobetakenat everyappointment.Burundianwomenprefer“privatebirths,”meaningnomenintheroom andasfewfemalesaspossible. Languagebarriersareaproblematthedoctor’soffice.SomeBurundiansdonotwantto disclosetheirhealthissuestoatranslator.Thetranslatorisoftenarelativeorfrienddueto thesmallpopulationofBurundianslivinginVermont.Theyonlyvisittheirphysicianwhen theyaresick,andnotforpreventativecareunlessthedoctor’sofficemakesafollow‐up appointmentforthem.InAfricatherewerewalk‐inhealthcarecentersrequiringno appointments.Makinganappointmentatthedoctor’sofficeisoftendifficultduetocultural andlanguagebarriers.Burundiansaresomewhatoffendedwhentheofficeasksfortheir chiefcomplaint.Theyfindthisquestioningrudebecausetheybelievetheirhealthissues aresolelybetweenthemandtheirdoctor.Personalhealthinformationissomethingthey prefernottosharewiththereceptionist.Thesechiefcomplaintquestionsarefrustrating fortheBurundiansbecausetheyinterpretitasaskingthemforadiagnosis,ratherthanthe doctordeterminingthediagnosis.3 Specifichealthconcerns Burundianwomengenerallypreferfemalephysicians,butanygenderisacceptable inanemergency. 59 Burundianwomendonotwantanymenintheroomwhentheygivebirth,even theirhusband.Theyalsoprefertohaveasfewpeopleintheroomaspossible. Whenpossible,avoidusingatranslatorthatisarelativeorfriendofthepatient. Burundiansalsofeeltheirmedicalissuesarenotconfidentialbecausetheyhaveto speakthroughatranslator. InBurundi,peopleonlygotothedoctorwhentheyaresick.Thereisno preventativemedicine.Burundianswillkeepanyappointmentsthedoctor’soffice makesforthem,buttheywillnotmakeanappointmentforthemselvesunless they’resick.Annualphysicalsshouldbescheduledbythedoctor’soffice. MakinganappointmentisstressfulforBurundians. Medicineisexpectedtobeprescribedafteradoctor’svisit. Socialetiquette Burundiansgreateachotherbyshakinghands.Theymayholdhandsforafewminutes afterahandshake.2Theyoftensaymwaramutse,whichmeansgoodmorning.Toshow respect,Burundianswillnotmakeeyecontactandwillbowslightlywithpeopletheyview asabovethem.1Communicationisalsooftenindirectandhighlycontextbased.Thesociety ispatriarchal,sothemanoftenhasthefinalsayonhouseholddecisions.2 CommonlyUsedPhrases English Hello Goodbye Please Thankyou Goodmorning Goodevening Yes No Kirundi Bwakeye N’agasaga Akira Urakoze Mwaramutse Ijororyiza Ego Oya Swahili Hujambo Kwaheri Tafadhali Asante Habariyaasubuhi Habariyajioni Ndiyo Hapanala AdditionalResources AssociationofAfricansLivinginVermont:http://www.africansinvermont.org 60 References 1. RepublicofBurundi.CultureGrams;2008. http://www.culturegrams.com/products/onlineedition.htm. 2. CulturalOrientationResourceCenter.RefugeeBackgrounderNo.2:The1972 Burundians.March2007ed. 3. PiperLE,NadeauLA.BurundianWomenRefugeeNeedsAssessment.St.Albans,VT: ChamplainValleyAHEC;2009. 4. MacQuerrieB.StressesAnewforRefugeesResettledinVT.BostonGlobe.April27, 2009. 61 Thispageintentionallyleft blank. 62 Chinese–NEW! CountryInformationa Location: EasternAsia,betweenNorthKoreaand Vietnam;borderstheEastChinaSea,Korea Bay,YellowSea,andSouthChinaSea Capital: Beijing Area: 9,596,961sq.km.(slightlysmallerthanthe UnitedStates) Climate: extremelydiverse;tropicalinsouthtosubarcticinnorth Languages:S tandardChineseorMandarin(Putonghua,basedonthe Beijingdialect),Yue(Cantonese),Wu(Shanghainese), Minbei(Fuzhou),Minnan(Hokkien‐Taiwanese),Xiang, Gan,Hakkadialects Population: InChina:1.34billion InVermont:1217Chinese(includingTaiwanese)asof2009b a Unlessotherwisecited,allinformationonthispageisfromtheUnitedStatesofAmerica,CentralIntelligence Agency,TheWorldFactbook.AccessedApril,2012. https://www.cia.gov/library/publications/the‐world‐factbook/geos/ch.html bVTRefugeeResettlementProgram,RefugeesinVermontbyCountryofOrigin,FY89‐FY11.Colchester,VT: 2012. 63 64 65 Backgroundandculture Althoughover90%ofMainlandChineseareethnicallyHan,thecountry’simmensesize,a longhistoryofmigrationtotheUnitedStates,andasizeableexpatriatecommunityof ChineseinneighboringAsiancountriesmeanthattheChineseimmigrantscurrentlyliving intheUnitedStatescanbeverydissimilartooneanother.Itcanbemoreusefulfor providerstoexaminethedegreeormannerofacculturation—aconstructdevelopedto describehowindividualsnegotiatetwoculturesusingparameterslikelanguageand practiceofculturalnorms—thantouseethnicidentifiers.Althoughthischapterwillgivea broadoverviewofculturalpracticesandbeliefscommonamongmanyChinesepeoples,it isimportantforhealthcarepractitionerstoseetheirpatientsasindividuals.Factorslike socioeconomicstatus,educationalbackground,orlengthoftimeinAmericamaybemuch biggerforcesinshapingapatient’sculturethantheirethnicheritage. Language.MandarinistheofficiallanguageofthePeople’sRepublicofChinaandTaiwan, buttherearemanydialects,includingShanghainese,Minbei,andMinnan(Hokkien‐ Taiwanese).InHongKong,whichisofficiallyaSpecialAdministrativeRegionofChina,the officiallanguagesareCantoneseandEnglish. LanguageisofparticularconcernfortheelderlyChinese–80% Immigrant ofwhomareforeignborn1–becauseolderfirstgeneration Chinesein immigrantsaremuchlesslikelytounderstandEnglishthan 2 Vermonthave youngerorsecondgenerationimmigrants. Despitetheuseof astrong translatorservices,theliteraturerepeatedlydemonstrates relationship thatlowEnglishproficiencycorrelateswithpoorerhealth withtheir outcomesanddecreasedpatientsatisfaction. translators, oftenviewing TheuseoftranslatorscanbeathornyissueforChinese themassocial immigrants.Somestudiessuggestthatpatientspreferusing advocatesas trainedinterpretersratherthanfamilymembers,citing wellas patientconcernoverdisruptingfamilialpowerdifferentials interpreters. whenusingchildrentotranslate.3However,otherresearch describestheopposite,withpatientschoosingfamily‐based translationbecauseofconcernsoverconfidentialityanda strongculturalpreferencetoshieldtheillfromanydistressing knowledgeregardingtheseverityoftheirdisease.4AccordingtoJonBourgo,Community OutreachManagerattheBurlingtonCommunityHealthCenter,manyoftheChinese ImmigrantsinVermontfeelaverystrongconnectiontotheirtranslators,oftenviewing themasvaluableresourcesandadvocatesbeyondinterpretation. Religion.In2002,ThePeople’sRepublicofChinaofficiallybecameasecularcountry.Yet despiteitsatheiststatus,theregion’slonghistoryofTaoism(Daoism),Buddhism,and Confucianisminformsmanymoderncitizens’philosophical,cultural,andhealthnorms. Taoismemphasizesharmonywithnatureandteachesthatfollowersshouldexercise outside,breathefreshair,andalignthemselveswiththerhythmsoftheuniverse.Taoism furtherincorporatesandexpandsupontheChineseideaofChi(alsocalledQi).5Chicanbe 66 roughlydefinedasthelifeforceanditisabalanceofyinandyang,whereyiniscool, nourishingenergyandyangiswarm,activatingenergy.Food,medicine,andactionsallplay acentralroleinregulatingyinandyang,keepingthebodyinharmonywiththe environment.6Importantlyforhealth,Taoismemphasizespassivity,encouragingfollowers tolookinwardtohealthemselves—aconceptthatcanbefrustratingforWesternhealth professionalswhomaywanttoadoptmoreaggressiveapproachestoagivenillness.7 BuddhismcentersaroundtheprinciplesofInnandKo—causeandeffect—that,coupled withKarma(Fate),arethemaindeterminantsofhealth.5Asmentionedinthechapteron Burma,Buddhistbeliefscanimpacthealthbeliefs,especiallyattitudesregardingmental health,asfollowersmayinterprettheircurrentpoor conditionasjustretributionforthesinsofapastlife, andthusfeellittlecompulsiontotakeactiontoalter Taoism theirlot.8 emphasizes passivity, Finally,Confucianism—abeliefsystemarguably encouraging closertoaphilosophythanareligion9—holdsfive followerstolook tenetsatitscore:benevolence,righteousness,loyalty, inwardtoheal filialpiety,andvirtue.5Thesevaluesgreatlyinform themselves:a familystructure,butalsohaverelevanceincare conceptthatcan provisionastheypredisposepatientstoprefer befrustratingfor familial‐baseddecisionstrategiesandtoputthe Westernhealth welfareofthefamilyunitbeforetheirown. professionalswho Additionally,undercurrentsofstrengthtacitly maywantto runningthrough“righteousness”and“virtue”canlead adoptmore todecreasedhealthseekingbehavior,especially aggressive amongmenwhodon’twanttoappearweak.10Like approachestoa manyotherChinesereligions,Confucianism givenillness. emphasizesharmonywithothersaswellasharmony betweenselfandtheenvironment. Family.FormostChinesepeople,familyisthecornerstoneoftheirlivesandamajor determinantofculture.11AccordingtoConfucianteachings,therearefivemajor relationshipsinalloflife:ruler‐ruled,father‐son,husband‐wife,brother‐brother,and friend‐friend,butallareessentiallymodeledonfamilialrelationships.12Traditionally, powerinthefamilyispredicatedonage,gender,andgeneration,witheldermalesbeing themostrevered,butthefamilyasaunitretainsgreaterimportancethananyindividual member. Theconceptof“face”or“savingface”ishighlyintegratedintofamilydynamics.Filial devotionishugelyimportantinChinesecultureandfailuretodemonstrateabsolute submissionordevotiontoone’sparentscanresultintheentirefamilylosingface,ascan anyotheractsofpoorbehavior,sincefaceisacollectivequalityoftheentirefamily.Fearof bringingshametothefamilycanbeapowerfulmotivatortoconformtosocialandcultural norms.13 67 Intermsofgenderdynamics,traditionalChinesefamiliesvalueandrespectmenmorethan women.Uponmarriage,societyexpectswivestojointheirhusband’shousehold whereupontheyarechargedwithassumingallthechoresofdailylivingandtheprimary caregiverroleforanychildren,elderlyparents,orillmembersofthefamily.Thatbeing said,acrossalldimensionsoffamilyrolesanddynamics,asimmigrantsincreasetheir lengthofstayintheU.S.,theirfamiliesincreasinglycometoresemblethoseofthe dominantculture14—thoughitcanbedifficultforallmemberstonavigatethechanging socialnorms. Education.MostChinesepeople,immigrantorotherwise,valueeducationquitehighly.In theUnitedStates,Chineseteenagersenrollincollegeatmuchhigherlevelsthantheir percentageofthetotalpopulationwouldsuggest,and,evenmorestrikingly,hailfromall pointsonthesocio‐economicspectrum.Inotherwords,itisnotjustthechildrenof educatedimmigrantswhoareenjoyingacademicsuccess,butthosefromworking‐class backgroundsaswell.Differentexplanationsofsuch achievementexist;somecitetheprinciplesofConfucianism, particularlyrespectforauthorityandhardwork,while Valuingstoicism, otherspointtohighparentalinvolvement,andstillothers overtdisplaysof creditethnicsocialstructures.15 affectionare uncommonin Yetdespitesuchwidespreadacademicattainment,health traditional providersmusttakecarenottobeblindedbythe“model Chinesefamilies. minority”paradigmandassumethatallAsianorChinese Membersshow youtharedoingwellinschool,especiallyaseconomic theirlovebythe resourcescanstillplayabigroleineducation,andmany efforttheydevote recentimmigrantsarenotaffluent.16Moreover,although totheirrolesas immigrantyouthmaybequitesuccessful,over50%ofthe providersor ChinesepopulationintheUnitedStatesstillself‐identifiesas caregivers. havinglimitedEnglishproficiency17andliteracyratescan vary.Cliniciansshouldevaluatetheeducationallevelofeach patientindividually. Diet.RiceandnoodlesarethemajorstaplesoftheChinesedietandareusually supplementedwithcookedvegetablesandoccasionallymeat—oftenwelldonebeef.Most Chineseeatthreemealsaday,withdinnerasthelargest,andlistchopsticksastheir preferredutensil.Duetohighlevelsoflactoseintolerance,manyChinesepeoplewillavoid dairy.LikemanySouthAsiancultures(seechapteronBurma),Chinesepeopleclassify foodsashotorcoldaccordingtotheiryinandyangproperties,whichmaynotcorrelateto physicaltemperature.Yin,orcoldfoods,includefruits,vegetables,coldliquidsandbeer, whereasmeat,eggs,hotsoup,andanyfrieditemsconstitutethehot,oryangfoods.Itis importanttomaintainayin‐yangbalanceateverymeal.Additionally,certainillnesslike nosebleedsareconsidered‘hot’illnessessoChinesepeoplemaywanttoincorporate‘cold’ foodstorestorebalanceaspartoftheirtreatmentplan.14 68 Healthcare InfectiousDisease.HepatitisBisendemicinmanyAsiancountries;withinfectionrates10 timesthatofthegeneralpublicintheU.S.,itsdetectionandtreatmentshouldbeamajor concernforcareprovidersseeingChineseImmigrants.Moreover,accordingtoTayloretal., manypatientsmaybeverymisinformedaboutroutesoftransmission,believingthat sharingfoodorutensilswithaninfectedpersonwillleadtoinfection,socliniciansmay needtospendtimeeducatingtheirpatientsregardingpreventivecare.18 AlthoughTuberculosis(TB)testsareaconsistentelementofimmigrants’domestichealth screening,longlatencyperiodsandincreasedundocumentedimmigrationmaymeanthat patientsareharboringundiagnosedTB.Importantly,TBratesamongAsiansandPacific Islandersarealmost10timeshigherthanthatofthegeneralpopulation,1andChinastands asthebiggestsourceofforeign‐bornTBcases.19DensehousinginChinatowns,with extendedfamilieslivingunderthesameroof,canexacerbatetransmission. Cliniciansshouldalsoscreenforparasites,whicharecommoninSouthEastAsia. LifestyleRiskfactors.Consistentwiththe“modelminority”paradigm,smokingand alcoholconsumptionratesareloweramongChineseAmericansthanthegeneralpublic,but increasedacculturationcorrelateswithincreaseduseofbothsubstancesandproviders shouldapproachpatientsonanindividualbasis. Similarly,traditionalChinesedietandanemphasisonoutdoorexercisestemmingfrom TaoismhavelongbeenprotectiveagainstdevelopingcommonWesternlifestyle pathologieslikediabetesandcardiovasculardisease,butuponmovingtotheUnitedStates andadoptingthedominantculture,Chinese‐Americansmaybemoreatrisk.1 Cancerrates,ontheotherhand,remainmuchhigheramongtheChinese.Followinghigh ratesofHepatitisBinfection,hepatocellularcarcinomaisquitecommon.20Prevalenceof nasopharyngealcarcinoma,prostate,andbreastcancersarealsoclimbing,withratesfor bothbreastandprostatecancershigheramongChineseAmericansthanChineselivingin Asia.1Troublingly,evenafteradjustingforaccesstocareandeducationlevel,Chinese immigrantshavemuchlowerratesofcancerscreeningthanNon‐Hispanicwhites.Current reasoningforthisdisparityimplicatesshameandface‐savingasmajorimpedimentsto screeningsincepatientsconsiderthescreeninginvasive.21Otherpatientsmaybefearfulof blooddrawssincetraditionalbelieflinksbloodverycloselywithlifeforce,sopatients worrythatbloodremovalwillweakenthem.14Finally,someChineseAmericans,especially thosewhoareforeign‐born,maynotunderstandthepurposeofscreeningtestsinthe absenceofsymptoms.21 FamilyPlanning/Childbirth.Chineseemphasisonmodestycanclashwitheffortsto discusssexorcontraception,particularlyinthecontextofpremaritalsex,whichmany Chineseconsidertobeshameful.Adolescentsrarelytalktotheirparentsaboutsexual issuesandrelyinsteadonmediasourcesandfriendsforinformation.Sexeducation programsexistinChina,butareoflimitedscope.WhilethemajorityofChineseparents reportcognizanceofchangingsexualnorms(includingpremaritalsex)manystillfeel 69 uncomfortablespeakingwiththeirchildrendirectly.22Chinesecultureremainsstrongly heteronormative:same‐sexrelationshipsoftengounacknowledgedbythefamilyand masculinegirlsorfeminineboysfacepressuretochange.14 Theparamountimportanceoffamilyplacespressureonwomenduringchildbirth. Pregnancyisa“cold”conditionsoexpectantmotherseatyangfoodstomaintainbalance.In asimilarvein,theChinesebelieveparticularactions—whereawomangoesorwhatshe does—hasadirecteffectonthefetus;forexamplevisitingazoowillcausethechildtolook likeananimal.Inthecaseofgeneticdefects,societyblamesthemother’sdietorbehavior. Chinesewomenarelargelyreceptivetoprenatalcare,withuseincreasingbydegreeof acculturationandlengthoftimeintheUnitedStatesanddecreasingwiththeusualbarriers toaccesslikelackofinsurance,loweconomicstandards,andpoorEnglishproficiency.14 Duringchildbirth,malerelativesmaychoosetonotbeintheroom,sincemenstruationand birtharedeemedunclean.ThoughmostChinesepeoplevaluestoicisminthefaceofpain, childbirthisfrequentlyconsideredanexceptionand cliniciansshouldofferpainmedicine,especiallyas manyChinesewomenareafraidofgivingbirth.23 MostChinese Postnatally,mothershaveopenporesandarethusly Immigrantsuseboth vulnerableto“wind”whichcanenterthebodyand Westernand precipitateillness.Womenmaystayindoorsandavoid TraditionalChinese bathingaspreventativemeasures. Medicine,believing WesternMedicineto MentalHealth.ChineseAmericanshavesomeofthe beeffectiveattreating lowestmentalhealthutilizationratesofany acuteillnessand demographicgroupintheU.S.,andalsodemonstrate relyingonChinese highdropoutratesafterseekingtreatment.Many medicineforrecovery barriersexisttohealthseekingbehavior.First, andprevention. religiousandphilosophicaltraditionsinChinafavora holisticviewofthehumanbodyanddon’tmakethe mindbodydistinctionthatissocommonintheWest. Asaresult,Chinesepeoplemaynotthinkofmentalhealthasseparatefromphysicalhealth, whichcanimpedetreatment,ortheymaysomaticizementalsymptomstobodilyones.6 Furthermore,alongingrainedbeliefthatoneshouldlookinsidethefamilyforsupportand dealwithproblemsprivatelymaystigmatizeformalizedphysicianvisits.17 Buddhismcanalsohaveanimpactonmentalhealth.First,becauseBuddhistsmayconsider theircurrentconditionasjustpunishmentforpreviousmisdeedsandconsequentlynot seekcareatall;second,becausetheymaybelievethatiftheyspeakabouttheirconcerns karmawillmakethemreal.1 Traditionalmedicine Chineseuseoftraditionalmedicinecanbeoneofthemoreintimidatingaspectsfor WesternphysicianswhencaringforChinesepatients.Providersmayfeeluncomfortable duetotheirlackoffamiliaritywithtraditionalremedies.Agrowingbodyofliterature indicatesthatmostChineseAmericanswhousetraditionalmedicinesdon’tdosoinplace 70 ofWesterncarebutasacomplement.Ingeneral,Chinesesocietyconsidersmodern biomedicaltreatmenteffectiveforacuteoracute/chronicdiseaseslikefracture,hepatitis, orcancer.TraditionalChineseMedicine(TCM)focusesonalleviatingsymptomsby restoringharmony,takingaholisticapproach.Forthisreason,TCMsplayabiggerrolein preventativecareforChineseAmericans. Practicalconcernsalsoshapepatients’useofTCM.ChineseAmericansfrequently“doctor shop”,soiftheirsymptomsdon’tresolveuponavisittoaWesternprovidertheymay switchtoatraditionalChinesedoctorandviceversa.Alternatively,insurancemayshape careutilizationspatterns:ifcoverageplansdon’treimbursepatientsforTCM,theymay relymoreheavilyontheWesternmedicalsystem,whereasuninsuredpatientswhocan’t affordtoseeabiomedicaldoctormayturntoalternativemedicineinstead.24Finally, ChinesepeoplemayfindWesternmedicinetobetoostrong,withmanyunwantedside effects,andmayuseTCMtoalleviatesucheffects. Cliniciansshouldbeawareofafewcommontraditional medicalpractices.Acupuncture,whichstimulatestheflowof chi,isusedtoalleviatepainandanxiety.Coiningand cupping—theapplicationorhotcoinsorbamboocups— treatscongestionandcoldsbylettingbadenergyoutofthe body.1Thephotoattherightshowsthemarksleftby cuppingapproximatelyonedayfollowingtreatment.24 Ingeneral,Chinesemedicineisnon‐invasiveanddoctors willmakeadiagnosisbytakingthepatient’spulseand askingdetailedquestionsaboutthecontextoftheillness.24 SocialEtiquette Handshakingisanacceptedgreeting,asarenoddingorbowing(slightly). Uponmeetinganewperson,Chinesepeoplelowertheireyesasasignofrespect. Eyecontactbetweenmembersoftheoppositegendermaybeseenasflirtatious. Duringintroductions,oneshouldintroducethejuniorpersontothesenior,orthe familiartotheunfamiliar. Personsshouldbeaddressedbytheirtitle(Mr.orMrs.)orprofessionalqualification (Dr.orEngineer). Personalspaceisimportant,andprovidersshouldavoidphysicalcontactuntilthey haveestablishedarelationshipwiththepatient,andshouldexplainwhytheexamis important. Arespectfuldistanceduringconversationisfour‐fivefeet. 71 Someindividualsmayprefertositsidebysideratherthanfacetoface. Touchinganelder’sheadcanbedisrespectful. Carelesstouchingofachild’sheadisbelievedtoreducedevelopment. Headnoddingcansignaldeferencetoauthorityratherthan“yes”. Chinesepeoplemayavoidsaying“no”tobepolite. Exaggeratedhandgesturesordramaticfacialexpressionarenotcommonamong Chineseandcanbeseenasaggressive. Privacyislinkedto“face”andisveryimportant;practitionersshouldbevery mindfulofconfidentiality. InChina,familynameislistedbeforethegivenname,socareshouldbetakento makesurethatfullnamesarerecordedcorrectlyinhealthrecords. SomeChinesepeoplemayvalueprotectingafamilymemberfromaharshtruth ratherthantellingtheirlovedonetheextentofagivenillnesssoWesterncaregivers shouldbepreparedtonegotiatethissituation. TherearemixedreportsastoChineseattitudestowardstime:someprofilesassert thatpunctualityisveryimportant,whileotherssaythattraditionalChinesepeople placegreaterimportanceonfinishingthetaskathandthanontime.9,14,25 Uponaguest’sdeparture(orpossiblyadoctor’svisit)thehostshouldescortthe guesttoatleastthedoor.Thefartheroneaccompaniesaguestout,thegreaterthe signofrespect. CliniciansshouldaskChinesepatientsforpermissionbeforeaddingicetowater, sincemanybelievecoldbeveragesshockthesystem.Manypreferhotteawhenill. Duringthe10daysofChineseNewYear,oneshouldnotusenegativewordsor phrases;duringthisperiodoneissupposedtoencourageluckandprosperity. CommonlyUsedPhrases Duetothedifficultyexperiencedbynon‐nativespeakersinmasteringpronunciationand tonality,wehavenotincludedaphrase‐list.TheNewYorkUniversitySchoolofMedicine, hasproducedtwoguidesthattranslatecommonly‐usedmedicalphrasesintoMandarinand Cantonese,respectively. http://edinfo.med.nyu.edu/mc/extras/mandarin‐trifold.pdf http://edinfo.med.nyu.edu/mc/extras/cantonese‐trifold.pdf 72 References 1. TomLA.HealthandHealthCareforChinese‐AmericanElders.Curriculumin Ethnogeriatrics:JohnABurnsSchoolofMedicine,UniversityofHawaii;2001. 2. DegniF,KoivusiltaL,OjanlatvaA.Attitudestowardsandperceptionsabout contraceptiveuseamongmarriedrefugeewomenofSomalidescentlivingin Finland.EurJContraceptReprodHealthCare.Sep2006;11(3):190‐196. 3. Ngo‐MetzgerQ,MassagliMP,ClarridgeBR,etal.Linguisticandculturalbarriersto care.JGenInternMed.Jan2003;18(1):44‐52. 4. VoDX,PateOL,ZhaoH,SiuP,GinsburgKR.VoicesofAsianAmericanyouth: importantcharacteristicsofcliniciansandclinicalsites.Pediatrics.Dec 2007;120(6):e1481‐1493. 5. ChenYC.Chinesevalues,healthandnursing.JAdvNurs.Oct2001;36(2):270‐273. 6. GreenG,BradbyH,ChanA,LeeM."WearenotcompletelyWesternised":dual medicalsystemsandpathwaystohealthcareamongChinesemigrantwomenin England.SocSciMed.Mar2006;62(6):1498‐1509. 7. ChenX,SwatzmanLC.HealthBeliefsandExperiencesinAsianCultures.In:Kazarian SS,EvansD,eds.HandbookofCulturalHealthPsychology:AcademicPress;2001. 8. LinKM,CheungF.MentalhealthissuesforAsianAmericans.PsychiatrServ.Jun 1999;50(6):774‐780. 9. QueenslandPartnersinCulturallyAppropriateCare.ChineseCultureProfile: Diversicare;2006. 10. Wei‐ChenT.AsianAmerican'sConfucianism‐basedHealthSeekingBehaviorand Decision‐makingProcess.HomeHealthCareManagement&Practice. 2010;22(7):536‐538. 11. XieX,XiaY,ZhouZ.StrengthsandChallengesinChineseImmigrantFamilies.Great PlainsResearch.2004;14(Fall2004):203‐218. 12. LawP‐l.AnIntroductiontoChineseCultureThroughtheFamily[BookReview]. AsianFolkloreStudies.2005;64(2):327‐329. 13. FangS‐RS,WarkL.DevelopingCross‐CulturalCompetencewithTraditionalChinese AmericansinFamilyTherapy:BackgroundInformationandtheInitialTherapeutic Contact.ContemporaryFamilyTherapy.1998;20(1):59‐77. 14. ChinP.Chinese.In:LipsonJG,DibbleSL,eds.CultureandClinicalCare.San Francisco,CA:UCSFNursingPress;2005. 15. ZhouM,KimSS.CommunityForces,SocialCapital,andEducationalAchievement: TheCaseofSupplementaryEducationintheChineseandKoreanImmigrant Communities.HarvardEducationalReview.2008;76(1):1‐29. 16. LepkowskaD.ModelminoritytaghidesAsiandropoutproblem.TimesEducational Supplement.(May2004). 17. Muse.CulturalCompetencyandChineseMedicine:ImmigrantChineseBeliefsof UtilizationandPluralityinHealthSeekingBehaviorsandHealthCareCoverage. InternationalJournalofTransdisciplinaryResearch.2006;2(1):1‐16. 18. TaylorVM,TuSP,WoodallE,etal.HepatitisBknowledgeandpracticesamong ChineseimmigrantstotheUnitedStates.AsianPacJCancerPrev.Apr‐Jun 2006;7(2):313‐317. 19. HoM‐J.SocioculturalAspectsofTuberculosis:aLiteratureReviewandaCaseStudy ofImmigrantTuberculosis.SocialScienceandMedicine.2004;59:753‐762. 73 20. 21. 22. 23. 24. 25. AuC.Culturalfactorsinpreventivecare:Asian‐Americans.PrimCare.Sep 2002;29(3):495‐502,viii. KandulaNR,WenM,JacobsEA,LauderdaleDS.Lowratesofcolorectal,cervical,and breastcancerscreeninginAsianAmericanscomparedwithnon‐Hispanicwhites: Culturalinfluencesoraccesstocare?Cancer.Jul12006;107(1):184‐192. CuiN,LiM,GaoE.ViewsofChineseparentsontheprovisionofcontraceptionto unmarriedyouth.ReprodHealthMatters.May2001;9(17):137‐145. IpWY,ChienWT,ChanCL.ChildbirthexpectationsofChinesefirst‐timepregnant women.JAdvNurs.Apr2003;42(2):151‐158. MaGX.Betweentwoworlds:theuseoftraditionalandWesternhealthservicesby Chineseimmigrants.JCommunityHealth.Dec1999;24(6):421‐437. YehieliM,GreyMA.EastAsianImmigrants.HealthMatters:APocketGuideto WorkingWithDiverseCulturesandUnderservedPopulations.Yarmouth,ME: InterculturalPress,aNicholasBrealeyPublishingCompany;2005:69‐76. 74 Congolesea RepublicoftheCongo DemocraticRepublicoftheCongo Note:Congoleserefugeescomefromageographicareathatisnowtwocountries:The RepublicoftheCongo(atleft)andtheDemocraticRepublicoftheCongo(atright). WesternAfrica;borderstheSouth AtlanticOcean,Angola,Cameroon, Location CentralAfricanRepublic,Democratic RepublicoftheCongo,andGabon Brazzaville Capital 342,000sq.km.(slightlysmallerthan Area Montana) Tropical;persistenthightemperatures andhumidity;rainyseasonMarch‐ June;dryseasonJune‐October.Coastal Climate/Terrain plain,centralplateau,northernand southernbasins. French(official);54locallanguages,of whichMonokutubaandLingalaarethe mostcommon. 4.2million 41 Language(s) Population Populationin VTb CentralAfrica;bordersAngola, Burundi,CentralAfricanRepublic, RepublicoftheCongo,Rwanda,South Sudan,Tanzania,Uganda,andZambia. Kinshasa 2,344,858sq.km.(slightlylessthan¼ thesizeoftheUnitedStates) Tropical;hotandhumidinequatorial riverbasin,coolerinhighlands;North ofequator,wetseasonApr‐Oct,dry seasonDec‐Feb;southofequator,wet seasonNov‐Mar,dryseasonApr‐Oct. Vastcentralbasinisalow‐lying plateau;mountainsineast. French(official);4mainlocal languages:Lingala,Kingwana, Kikongo,Tshiluba. 71.7million 144 aUnlessotherwisecited,allinformationonthispageisfromtheUnitedStatesofAmerica,CentralIntelligence Agency,TheWorldFactbook.AccessedApril,2012.https://www.cia.gov/library/publications/the‐world‐ factbook/geos/cg.html;https://www.cia.gov/library/publications/the‐world‐factbook/geos/cf.html bVTRefugeeResettlementProgram,RefugeesinVermontbyCountryofOrigin,FY89‐FY11.Colchester,VT: 2012. 75 76 77 78 79 Backgroundandculture Currently,whatmanyrefertoastheCongoconsistsoftwoseparatecountries:theRepublic oftheCongo,withitscapitalinBrazzaville,andtheDemocraticRepublicoftheCongo,with itscapitalinKinshasa. From1970until1997,theDemocraticRepublicoftheCongowasnamedZaire,underthe leadershipofMobutuSeseSeko.WarcametoZairein1994whenthecivilwarinRwanda forcedonemillionrefugeesintoZaire.Someoftheserefugeeswerearmedandbegantokill thepeopleofZaire,leadingtotheformationofmilitiasandinvasionbyforcesfrom Rwanda.ThistensionresultedinthedevelopmentofrebelgroupsintheCongoand eventuallythecountrysawitsowncivilwar.Apeacetreatydrawnupin2002washonored bymostparticipatingparties,buttherewerestillrivalingmilitiasfightingineasternCongo. TheRepublicoftheCongosawitsowncivilwarin1993,whenpoliticalandreligious differencesledtoviolentaltercations.Thefirstcivilwarresultedinthedisplacementof 10,000citizens.In1997theRepublicoftheCongowasfacedwithasecondcivilwar betweenmilitiagroupsandsupportersofthecountry’spresident,PascalLissouba.Apeace agreementwasinstitutedin1999andmanyrefugeesthathadfledreturned. Language.TheofficiallanguageofbothTheRepublicoftheCongo(Brazzaville)andThe DemocraticRepublicoftheCongo(Kinshasa)isFrench,althougheachregionalsohas indigenouslanguages.InTheRepublicoftheCongo(Brazzaville),therearemorethan54 differentlanguages,butMonokutubainthesouthandLingalainthenortharethemost common.InTheDemocraticRepublicoftheCongo(Kinshasa),therearefourmainBantu languages:Lingalainthewest,Kikongointhewestandsouthwest,Tshilubaincentraland southernregions,andSwahiliintheeast. Religion.Inbothcountries,themajorityofcitizensareChristian,mostofwhomareRoman Catholic.AsmallerpercentageisMuslim.InTheRepublicofCongo(Brazzaville),about 50%ofthepopulationholdsindigenousbeliefs. Family.Thereismuchvariationinfamilystructure,dependingontheethnicbackgroundof thefamily.InboththeRepublicofCongo(Brazzaville)andtheDemocraticRepublicof Congo(Kinshasa)thereareextendedfamilieslivingunderonerooforinseveral neighboringhomes.Extendedfamiliestypicallyincludeparents,children,grandparents, cousins,aunts,anduncles.InbothwesternDemocraticRepublicofCongo(Kinshasa)and mostoftheRepublicofCongo(Brazzaville),themother’sbrotherisconsideredthe dominantmale,althoughfamilyitselfismatriarchal.OtherareasoftheCongohavemore patriarchalandpolygamousfamilies. Education.IntheDemocraticRepublicofCongo(Kinshasa),civilwarhasdrastically affectedtheeconomyandeducation.Thereareveryfeweducationalinstitutionsand enrollmentisverylow.Therearethreepublicuniversitiesstillinoperationandseveral privateinstitutions.TheRepublicofCongo(Brazzaville)hasalsobeenseriouslyaffectedby war.Supplyshortageshaveledtothedevelopmentofprivateinstitutions,butmostcannot 80 affordtoutilizethem.Generally,schoolattendanceisrequiredbeginningatagesixand continuinguntil16.Abachelor’sdegreeisgrantedtothosewhocompletesixyearsof primaryschoolingandsevenyearsofsecondaryschooling.MarienNgouabiUniversityis thecountry’sonlypublicuniversity;itoffersdegreesinmedicine,law,andotherfields. Althoughbothcountrieshaveseendamagetotheeducationalinfrastructure,adultliteracy ratesarerelativelygood.IntheRepublicofCongo(Brazzaville)over90%ofmalesand 80%offemalesareliterate.TheDemocraticRepublicofCongo’s(Kinshasa)literacyrateis lower,with81%ofmalesand54%offemaleadultsconsideredliterate. Diet.CongoleseintheDemocraticRepublicofCongo(Kinshasa)experiencehighratesof malnutritionbecausefoodsuppliesaredifficulttoobtain.Staplefoodsarecassava,rice, potatoes,bananas,yams,beans,corn,fish,nuts,fruits,andvegetables.Foodsaresimilarin theRepublicofCongo(Brazzaville),butfishandmeatoftenaccompanystarchierfoods. Healthcare Thetwocountriesfacesimilarhealthaccessproblemsandendemicdiseases.Hospitals, whenavailable,areinpoorconditionandlacknecessaryequipmentandmedications. Underthesecircumstances,mostpeople,especiallythoseinruralareas,turntotraditional healing.Peopleofalllevelsofeducation,socialstatus,andeconomicstatusconsult traditionalhealers,andoftenconsultbothphysiciansandtraditionalhealersconcerning thesameailment.Traditionaltreatmentsincludeherbs,plants,andprayer.Itiscommon forsickpeoplewithoutaccesstohealthfacilitiestositinchurcheswaitingtobecuredby God.Manybelievethatillness,particularlymentalillness,isbroughtonbycursesorby punishmentfromGod.Mentalillnessisofparticularconcernbecausepeoplebelievethat evenwithtreatment,mentalillnesswillneverdisappear. Congolesepeoplehavegreattrustinphysiciansandnurses.Manyareasarestaffedonlyby nurses,whooftenearnhighersalariesthandoctors.Publichealtheducationhasmade greatstridesasamissionoftheMinistryofHealth. Specifichealthconcerns.TheRepublicofCongo(Brazzaville)andtheDemocratic RepublicofCongo(Kinshasa)facesimilarendemicdiseases.Themostcommoninfectious diseasesincludemalaria,tuberculosis,diarrhealdiseases,leprosy,HIV/AIDS,andparasitic infectionslikeschistosomiasis,onchocerciasis,andtrypanosomiasis.Tuberculosisinthe DemocraticRepublicofCongo(Kinshasa)hasahighdetectionrateof70%andatreatment rateof75%.HIV/AIDSratesaresignificantlyhigh,withabout7.5%prevalenceforadults betweenages15and49.Unfortunately,theseriousnessofHIV/AIDSwasdoubtedwhen firstdiscoveredandmostinhabitantsdidnotchangebehavioruntilfamousactorsand musiciansdiedfromcomplicationsofthedisease.Therearenogovernment‐runHIV/AIDS programs,butprivateattemptshavebeenmadetoeducatethepublic.Still,agreatdealof workisneededinthisarea. SocialEtiquette IntheDemocraticRepublicofCongo(Kinshasa),shakinghandsiscommoninurbanareas, whereitisconsideredappropriatetoshakehandswithmembersofoppositeandsamesex, 81 Outsideurbanareas,menandwomendonotshakehands.Verbally,urbanareapopulations greetbysaying,Mbote,whichmeans“hello.”Ineasternandsomesouthernareaswhere Swahiliisspoken,Jambo,meaning“hello”isoftenthegreetingofchoice.Allactivitywhich involveshands(passingobjectstooneanother,shakinghands)isdonewiththerighthand, astheleftisusedforpersonalhygiene. HandshakesarealsousedtogreetoneanotherintheRepublicofCongo(Brazzaville) althoughmanyalsokisseachotheronthecheekwhenmeeting.Verbally,thegreetingis dependentonwhatlanguageisbeingspoken.“Hello”ismostcommonlyMboteorMbotena yo.Inbothcountries,handgesturesandbodylanguagecanbothemphasizeorreplace verballanguage. Eyecontactisacceptedinmostregionsofbothcountries. Planningandconceptionoftimearenotespeciallyvaluedandsomeetingsmaybemissed orpatientsmaybelate. Althoughthetwocountriesaresimilaringeographiclocation,history,andmanycultural practices,itisimportanttoinquireaboutinformationdirectlyrelevanttothepatientbeing seen. WorksConsulted TalleyL,SpiegelPB,GirgisM.AnInvestigationofIncreasingMortalityAmongCongolese RefugeesinLugufuCamp,Tanzania,May‐June1999.JournalofRefugeeStudies. 2001;14(4):412‐427. VanHerpM,ParqueV,RackleyE,FordN.Mortality,ViolenceandLackofAccessto HealthcareintheDemocraticRepublicofCongo.Disasters.2003;27:141‐153. 82 MeskhetianTurks Georgia NOTE:TheMeskhetianTurkshavetheirrootsintheMeskhetianregionofGeorgia.Asa resultofdeportationsanddiscrimination,thepopulationisnowdispersedthroughoutthe region.a DiasporaInformation Location: MeskhetianTurksareknowntoliveinAzerbaijan,Georgia, Kazakhstan,Kyrgizstan,theRussianFederation,Turkey,Ukraine, Uzbekistan Capital: N/A Area: N/A;AncestralregioninsouthernGeorgiais9656sq.km. Climate: AncestralregioninsouthernGeorgiaisdryandrelativelycold;the westernareaiswarmerandhaslushforest. Terrain: AncestralregioninsouthernGeorgiaisinthevalleyoftheMtkvari River,surroundedbymountainsthatare1,000‐2,000mhigh. Language(s):Turkish,Russian Population: Indiaspora:300,000‐400,000livinginninedifferentcountries InVT:difficulttodeterminebecauseimmigrationstatisticsare basedonthecountryofresidenceimmediatelypriorto resettlement,notethnicity;ourbestguessisthat~200 movedtoVTandfewerthan20arestillhere aUnlessotherwisecited,allinformationinthischaptercomesfromapublicationentitledMeskhetianTurks: AnintroductiontoTheirHistory,CultureandResettlementExperiences,byAyşegülAydıngün,ÇigğdemBalım Harding,MatthewHoover,IgorKuznetsov,andSteveSwerdlow.Publishedin2006bytheCenterforApplied Linguistics,itisavailableathttp://www.cal.org/co/pdffiles/mturks.pdf(accessed1/9/11) 83 Backgroundandculture TheMeskhetianTurksareanomadicgroupthathashadarecentincreaseinimmigration totheUnitedStatesandtoVermont.Originally,MeskhetianTurkslivedinMeskhetia,a southernregioninthecountryofGeorgia.Overtime,however,thepopulationwas discriminatedagainstinvariouswaysandforcedintosurroundingcountries.Becauseof thishistory,itisdifficulttoknowhowmanyMeskhetianTurksthereare,butmost estimatesputthepopulationbetween350,000and400,000in2005.TheMeskhetianTurks resideinninedifferentcountries,includingAzerbaijan,Georgia,Kazakhstan,Kyrgyzstan, theRussianFederation,Turkey,Ukraine,Uzbekistan,andtheUnitedStates. TheMeskhetianTurkshaveexperienceddecadesofpersecution,especiallyinregionsof Russia.Becauseoftheirnomadicways,MeskhetianTurkswerenotpermittedtogain permanentresidenceinareasofRussiaandthereforewereunabletoworklegally,own property,haveaccesstohealthandsocialsecuritybenefits,attendhighereducation institutions,registerformarriageandbirthcertificates,orobtaindocumentsof identification.Withoutthesebasicrights,MeskhetianTurksweresubjecttopoverty, deportation,andpersecution,whichledtounbearablelivingconditions.Whereverthey triedtosettle,MeskhetianTurksweresubjecttofurtherdiscriminationanddeportation. Bytheendof2007theUnitedStateshadprovidedrefugeforanestimated12,000 MeskhetianTurks. Language.MostMeskhetianTurksaremultilingual.AnEasternAnatoliandialectof Turkishisspokenbythemajorityofpeople,buttherearecertainwordsinthemain languagethathavebeenadoptedfromseveralothers.MostoftheMeskhetianTurks residingintheUnitedStatesspeakTurkish,Russian,andthelanguageofwhichever countrytheylivedinpriortotheUnitedStates. Religion.MostMeskhetianTurksareSunniMuslim,butmanyofthosewhosettledin RussiaarenotstrictlyobservantduetotheSovietgovernment’sdiscouragementof religion.ThosewhoidentifywithethnicityoriginatinginGeorgiaaregenerallyChristian. Family.MeskhetianTurkfamiliesareextended,includinggrandparents,aunts,uncles,and cousins.Eldersarethemostrespectedandmakealloftheimportantfamilydecisions.Itis commonforMeskhetianTurkstowanttoliveinverycloseproximitytotheirfamily memberswhenresettlingintheUnitedStates. Education.EducationishighlyvaluedbyMeskhetianTurks,howeverdiscriminationwhile livingintheformerSovietUnionmadeeducatingchildrenextremelydifficult.Classrooms wereoftensegregatedandadvancementwasmadepurposefullyunattainableformany. Childrenwerealsotoldthattheywouldneverqualifytofurthertheireducationatthe universitylevelortowork,whichsignificantlydecreasedtheirmotivationtostudy.Itis difficulttoestimateliteracyratesforthispopulationbecausetheyresideinsomany differentcountries. 84 Diet.Dailydietincludespotatoes,rice,vegetables,meat,eggs,cheese,sourcream,and honey.ObservantSunniMuslimsrefrainfromeatingpork. Healthcare BecauseMeskhetianTurkswereunabletoobtainRussiancitizenship,theywerenot qualifiedtoreceivefreehealthcarefromthegovernment.Inaddition,manylivedinrural areasandaccesstohealthcarefromsuchadistancewasextremelylimited.Manyolder MeskhetianTurksareresistanttohealthcareintheUnitedStatesandaskfamilyand friendstosendmedicationsfromRussia.TheCenterforAppliedLinguistics(CAL)points outthatmanyofthesystemsforobtaininghealthcareintheUnitedStatesareunfamiliarto MeskhetianTurks,whichcanbeachallenge.Forexample, makingappointmentsinadvanceandpracticing preventativeratherthancurativemedicinearefrequent obstacles. Special Considerations Commonmedicalproblemsincludedentalproblemsand mentalillness,astheMeskhetianTurkshaveexperienced Thehistoryofthe difficultpastsandhighlevelsofstress.Itisimpossibleto MeskhetianTurks listendemicdiseasesbecausetheMeskhetianTurkscome complicatesthe fromseveraldifferentcountries.Forexample,WHO abilitytopinpoint estimatestheprevalenceofHIV/AIDSinGeorgiatobe acceptedcustoms.It lessthan2%asof2005,butintheFederationofRussia, isrecommendedthat wheremostMeskhetianTurksreside,theprevalenceis providersfamiliarize between0.8%and1.7%.Knowingthecountryoforiginof themselveswiththe thepatientmakesthisknowledgeeasiertoaccess. basichistory,but mostrelevantdetails Socialetiquette shouldcomefromthe “Hello”inTurkishisMerhaba,althoughtheMeskhetian patientsthemselves. TurksspeakaparticulardialectoftheTurkishlanguage andtheremaybevariationsofthisword.Studiesin Georgiahaveshownthathandshakesaregenerally acceptableandeyecontactisvalued.However,SunniMuslimsdonotmakeeyecontact withmembersoftheoppositesex.Checkingwiththepatienttoseewhattheyaremost comfortablewithcanmakefuturegreetingsgomoresmoothly. Worksconsulted AydıngünA,HardingÇB,HooverM,KuznetsovI,SwerdlowS.MeskhetianTurks:An IntroductiontotheirHistory,CultureandResettlementExperiences.CenterforApplied Linguistics,CulturalProfile2006;http://www.cal.org/co/pdffiles/mturks.pdf.Accessed April,2102. MirkhanaovaM.PeopleinExile:TheOralHistoryofMeskhetianTurks.JournalofMuslim MinorityAffairs.2006;26:33‐44. WisconsinDepartmentofHealthandHumanServices.CulturalProfile:MeskhetianTurks 2005.http://dcf.wisconsin.gov/refugee/pdf/mturks_profile.pdf 85 Thispageintentionallyleft blank. 86 Somali CountryInformationa Name: Somalia Location: EasternAfrica,eastofEthiopia;bordersthe IndianOcean,theGulfofAden,Djibouti,Ethiopia, andKenya Capital: Mogadishu Area: 637,657sq.km.(slightlysmallerthanTexas) Climate: principallydesert;duringnortheastmonsoon(Dec‐Feb) temperaturesmoderateinnorth,hotinsouth;duringsouthwest monsoon(May‐Oct)torridinnorth,hotinsouth;irregularrainfall Terrain: primarilyflat,risingtoundulatinghillsinthenorth Language(s):Somali(official),alsoArabic,Italian,English Population: InSomalia:9.9million InVT:573b a Unlessotherwisecited,allinformationonthispageisfromtheUnitedStatesofAmerica,CentralIntelligence Agency,TheWorldFactbook.AccessedApril,2012.https://www.cia.gov/library/publications/the‐world‐ factbook/geos/so.html bVTRefugeeResettlementProgram,RefugeesinVermontbyCountryofOrigin,FY89‐FY11.Colchester,VT: 2012. 87 88 89 BackgroundandCulture Somalia’sestimatedpopulationis9.9millionpeople;theactualpopulation,however,is difficulttoobtainduetothenomadiclifestyleofsomeandthefactthatmorethanone millionhavefledthecountryseekingrefuge.Infact,mostofthechildrenfromSomalia livingintheUnitedStateswereborninKenyainarefugeecampcalledKakuma.Somalia’s locationhasprovenhistoricallyproblematic,asconflictoverbordersandboundarieshas ledtofrequentperiodsofviolence,famine,anddisease.Inaddition,warbetween neighboringEthiopiaandEritrealedtotheformationofmilitiasandtheinvasionof SomaliaastherivalingEthiopiaandEritreafoughtoverSomalia’sallegianceandalliance. EthiopiawithdrewfromSomaliainJanuaryof2007. Ethnically,Somaliais85%Somali,5%Bantu,and10%Arabandsmallerminorities.Inthe pastfiveyears,VermonthasprovidedrefugeforhundredsofcitizensofSomalia,withthe majorityofBantuethnicity. Language.MajorlanguagesincludeSomali,Arabic,English,andItalian.TheSomali languagehasthreedifferentdialectsanduntilrecentlywasunwritten.MostoftheSomalis thathavebeenresettledinVermontareBantuSomalis,whospeakMaiMaiwhichisnota writtenlanguage.VermontisnowalsohometoanincreasingnumberofSomaliSomalis (notofBantuethnicity)whoareliterateinSomali. Religion.Morethan97%ofSomalisareSunniMuslim.AverysmallnumberareChristian. Family.ThepeopleofSomaliaareaffiliatedwithclans.Whilechildrentaketheirfather’s nameandbecomepartofhisclan,motherskeeptheirmaidennamesandtheirpositionin theirownclan. Education.Theformaleducationsystemhasbeensignificantlyimpactedbywar,infact muchofithasbeendestroyed.Literacyandlanguageskillsareofgreatconcernforthis population;roughly50%ofadultmalesand26%ofadultfemalesareliterate. Diet.NomadicandfarminglifestylespredominateinSomalia,leadingtoadietdictatedby locationandavailability.NorthernSomaliaishometomanynomadicpopulations,whoeat plentyofmeatandmilk.SouthernSomaliaandfarmingareaseatlotsofvegetables,millet, andsesame.Dietisalsoinfluencedbyreligionandeconomicstatus.Forexample,strict SomaliMuslimseatgrains,fish,fruit,andvegetablesbutcannoteatanythingfromanimals thathaveeatenotheranimals. HealthCare Healthcareprofessionals,includingnursesandphysicians,arewellrespectedinSomalia, whichdoesnothaveastructuredhealthcaresystemsincemanyhospitalsandclinicswere damagedinwar. AstheUnitedNationsandotherorganizationsworktoprovideaidandsupporttoSomalia, itsresidentsarebeingexposedmoretoprimarycareandWesternmedicine. 90 Infectiousdisease.Waranditsresultingpoverty,lackofeducation,andinsufficienthealth carehaveledtomanyhealthcomplicationsinSomalia.Thoseofmajorconcerninclude tuberculosisandcholera,whichisendemicinmostofthecountry.Respiratoryinfections, malaria,anddiarrhea‐relatedcomplicationscausemostchildhooddeathsandmeasles outbreaksareresponsibleforhighinfantmortality.TheincidenceofHIV/AIDSis significantlylowerthaninotherAfricancountries,howeverthismaynotbereliable becausedatahavebeendifficulttocollect.SincetheWorldHealthOrganizationpredictsa significantincreaseintheincidenceofHIV/AIDS,educationandpreventionprogramsare beingimplemented. Mentalhealth.Mentalhealthispoorlyunderstoodandusuallynotacknowledged. However,post‐traumaticstressdisorder(PTSD)anddepressionareinevitableinacountry withsuchaviolentbackground.PTSDhasalsobeenattributedtochewingkhat,whichisa hallucinogenicleaf. Traditionalmedicine.Traditionalmedicineiswidelypracticed.Illnessesareoftenblamed onangryspiritswithinanillperson.Tohealthepatientinvolvessettlingthesespirits,often byhavinghealingceremonies,eatingspecialfoods,readingtheKoran,andburningincense. Commonhealingpracticesinclude“fireburning”(applyingheatedstickstotheskin), herbalremedies,prayer,andbloodletting.Fireburningisacommontreatmentfor hepatitis,malnutrition,andpneumonia.Bloodletting,similartoextremephlebotomy, consistsoftakingcopiousamountsofbloodfromthepatientinattempttoremovetheir illnesswiththeblood. SocialEtiquette GreetingsvaryinSomalia,dependingontheregion.A Physical commongreetingacceptedinmostregions,however,is contact Nabad,whichmeans“peace.” between membersof Generally,peopleofthesamesexshakehands,butthose theopposite whoareofoppositesexandnotofthesamefamilydonot sex,except touchwhenmeeting. family members,is Directeyecontactisconsideredrudeandistherefore prohibited. unacceptable. Bodylanguageisincorporatedwithspeakinglanguagetomeancertainthingsorto placeemphasisonspeech,makingitmoredramatic. 91 Worksconsulted ComerasamyH,ReadB,FrancisC,CullingsS,GordonH.Theacceptabilityanduseof contraception:aprospectivestudyofSomalianwomen'sattitude.JObstetGynaecol.Jul 2003;23(4):412‐415. DaviesMM,BathPA.ThematernityinformationconcernsofSomaliwomenintheUnited Kingdom.JAdvNurs.Oct2001;36(2):237‐245 DegniF,KoivusiltaL,OjanlatvaA.Attitudestowardsandperceptionsaboutcontraceptive useamongmarriedrefugeewomenofSomalidescentlivinginFinland.EurJContracept ReprodHealthCare.Sep2006;11(3):190‐196. RobertsonCL,HalconL,SavikK,etal.SomaliandOromorefugeewomen:traumaand associatedfactors.JAdvNurs.Dec2006;56(6):577‐587 WissinkL,Jones‐WebbR,DuBoisD,KrinkeB,IbrahimQ.Improvinghealthcareprovision toSomalirefugeewomen.MinnMed.Feb2005;88(2):36‐40. 92 Sudanese CountryInformationa Name: Sudan Location: NorthernAfrica,betweenEgyptandEritrea; borderstheCentralAfricanRepublic,Chad, Egypt,Eritrea,Ethiopia,Libya,andSouthSudan Capital: Khartoum Area: 1,861,484sq.km.(slightlymorethan¼thesize oftheUnitedStates) Climate: ariddesert,hotanddry;rainyseasonvariesbyregion(Apr‐Nov) Terrain: generallyflat,featurelessterrain;desertdominatesnorth Languages:Arabic(official),English(official),Nubian,TaBedawie,Fur Population: InSudan:45million(includesSouthSudan,est.8.3million) InVT:140b a Unlessotherwisecited,allinformationonthispageisfromtheUnitedStatesofAmerica,CentralIntelligence Agency,TheWorldFactbook.AccessedApril,2012.https://www.cia.gov/library/publications/the‐world‐ factbook/geos/su.html bVTRefugeeResettlementProgram,RefugeesinVermontbyCountryofOrigin,FY89‐FY11.Colchester,VT: 2012. 93 94 95 Backgroundandculture Civilwarcamefromirreconcilabledifferencesinreligionandpoliticsinthe1980sandwas followedbyalmosttwentyyearsofhostilityandbloodshed.Hundredsofthousandsof refugeesleftSudaninanattempttoescapeviolenceanddrought,whichcreated uninhabitablelivingconditions.Apeacetreatyin2002wasdraftedinanattempttoend fighting,butconflictinDarfur,aregionofSudan,continued.Itisestimatedthatby2005, morethan2millionpeopleweredisplaced.Inanotherattemptatpeace,acontractwas signedin2006betweenthegovernmentandrebelgroupsinDarfur.However,several otherrebelgroupsdidnotsignthetreaty.Then,inFebruary2011,SouthernSudanseceded fromSudanthroughapublicreferendumsupervisedbytheUnitedNations. Language.TheofficiallanguageisArabic,althoughitissaidthatonlyhalfofthepopulation speaksit.Over100differentlanguagesarespokeninSudan;manyofthemaretribal dialectsandmanyhavenosystematicwrittenform.Englishisspokenbymoreeducated citizenslivinginthesouth. Religion.Morethan70%ofthepopulationisSunniMuslim,concentratedmostlyin northernandcentralSudan.While5%identifyasChristian,theremaining25%areof indigenousreligions. Family.Differentwaysoflifeanddifferentcustomsarepracticedbytheinhabitantsof northernandsouthernSudan.Thesouthallocatesmorerightsandfreedomtowomen, whilemalesaredominantinthenorth.Ingeneral,menworkandleadthefamily,while womentakecareofthehomeandthechildren.Thehouseholditselfisextended,often housingthreegenerations. Education.Childrenaregenerallyrequiredtocompleteatleastnineyearsofeducation, althoughmanydonotbecauseofpoor,overenrolledschoolsystemsandtheneedto providemoreincomeforthefamily.TheUniversityofKhartoumisafour‐yearuniversity withcoursestaughtexclusivelyinArabic.Literacyratesare71%ofadultmalesand52%of adultfemales. Diet.ThetraditionalSudanesedietconsistsofmeatssuchasbeef,chicken,goat,and mutton.Meatisoftenunavailable,however.Someeatfish,millet,vegetables,potatoes, fruits,andbreads.Alcoholhasbeenoutlawed,butbeerisoftendrunkbythoseinthesouth. Malnutritioniscommon. HealthCare DecadesoffightinghaveleftSudanwithfewoperatinghealthclinicsandhospitals. BecauseSudanhasover500tribesand57ethnicgroups,healthdisparitiesdifferbetween groups.Endemictothecountry,however,aremalaria,tuberculosis,leprosy,cutaneousand visceralleishmaniasis,andschistosomiasis.Sicklecellanemiaiscommonamongthe Messeyriatribes.InnorthernSudan,casesofheartdiseaseanddiabetesareincreasing. Approximately260,000peoplearebelievedtobelivingwithHIV/AIDS,anadult 96 prevalencerateof1.1%.Theunmetneedforhealtheducationandawarenesshasbeen recognizedasamajordeficitinSudan.Asaresult,theFederalMinistryofHealthworks closelywithSudanesetelevisionstationstobroadcasthealth‐orientedinformationtothe homesofSudanesefamilies.Programstoeducateaboutdiabetesandbreastcancerarealso beingdeveloped. MentalHealth.Mentalillnessisextremelyfeared,asitisthoughttoresultfromdemonic possession.Treatmentformentalillnessisextremeandcanincludebeingkeptinsolitary confinementwithonlybreadandwater.Whileinconfinement,thepatientisbeaten repeatedlytodrivethedemonicspiritfromthebody.Mentalillnessisthusanimportant healthissuetobeaddressed. TraditionalMedicine.ResearchdonebytheUniversityofKhartoumhasfoundthatmost citizensofSudanconsulttraditionalhealersbeforeseeingadoctor.Healingmethods, dependingontheethnicgroup,mightincludeceremonies,readingsfromtheKoran,dances, ortheuseofrootsorplants.Illnessisoftenthoughttobecausedbypossessionbydemonic spiritsorbysomeonegivingthe“evileye.” SocialEtiquette Acceptedgreetingsvarybyregion.Generally,innorthernareas,Salaamalaykum,or“peace beuponyou”isexchangedwithagentlehandshakebetweenthoseofthesamesex.Inthe south,handshakesarelessfrequentandtheverbalexchangeisoftenGwonada,or“how areyou?” Eyecontactisprohibitedincertainsituations.Women,forexample,arenotpermittedto keepdirecteyecontactwithunknownorholymen. Worksconsulted GeltmanPL,Grant‐KnightW,MehtaSD,etal.The"lostboysofSudan":functionaland behavioralhealthofunaccompaniedrefugeeminorsre‐settledintheUnitedStates.Arch PediatrAdolescMed.Jun2005;159(6):585‐591. KempC,RasbridgeLA.CultureandtheEndofLife:EastAfricanCultures:PartII,Sudanese. JournalofHospiceandPalliativeNursing.2001;3(3):110‐112,120. 97 Thispageintentionallyleft blank. 98 Vietnamese CountryInformationa Name: Vietnam Location: SoutheasternAsia;borderstheGulfof Thailand,GulfofTonkin,andSouth ChinaSea,aswellasChina,Laos,and Cambodia Capital: Hanoi Area: 331,210sq.km.(slightlylargerthanNewMexico) Climate: Tropicalinsouth;monsoonalinnorthwithhot,rainy season(MaytoSeptember)andwarm,dryseason(October toMarch) Terrain: Low,flatdeltainsouthandnorth;centralhighlands;hilly, mountainousinfarnorthandnorthwest Language(s):Vietnamese(official),English(increasinglyfavoredasa secondlanguage),someFrench,Chinese,andKhmer; mountainarealanguages(Mon‐KhmerandMalayo‐ Polynesian) Population: InVietnam:90.1million InVermont:1056b a Unlessotherwisecited,allinformationonthispageisfromtheUnitedStatesofAmerica,CentralIntelligence Agency,TheWorldFactbook.AccessedApril,2012.https://www.cia.gov/library/publications/the‐world‐ factbook/geos/vm.html bVTRefugeeResettlementProgram,RefugeesinVermontbyCountryofOrigin,FY89‐FY11.Colchester,VT: 2012. 99 100 101 Backgroundandculture Vietnamisasocialistrepublicwithapopulationofabout85millionpeople.WorldWarII andtheVietnamWarcreateddifficultconditionsforVietnam,includingatradeembargoby theUnitedStateswhichlastedforover20years,duringwhichtimethepeopleofVietnam experiencedyearsofpoverty,persecution,racism,andisolation.Thousandsoffamilies tookrefugeinothercountries,includingtheUnitedStates,whichhousesseveralrefugee andimmigrantpopulations. Language.MajorlanguagesincludeVietnamese,French,Chinese,English,andKhmer. Religion.ThemajorityofVietnamesepeople(>60%)areBuddhists.Smallerpercentages practiceConfucianism,Taoism,orRomanCatholicism. Family.Householdstypicallyincludeparents,unmarriedchildren,andmarriedsonswith theirfamilies.Malesareconsideredtobethedominantauthority,butbothmalesand femalesworkandshareresponsibilities.Elderlyarecaredforbythefamilyoftheyoungest marriedson,whooftenhasinheritedhisparent’shome. Education.Beginningatagefive,VietnamesechildrenattendschoolMondaythrough Saturday.Schoolisonlyfreeforthefirstsixyears.However,educationisvaluedand childrenareencouragedtofinishhighschool.Sadly,manydropouttobeginworking. Universityeducationisfreeforcertainstudents,butspaceislimited.Currently,private universitiesandsecondaryeducationfacilitiesareincreasing.Literacyestimatesare94% formaleadultsand87%forfemaleadults. Diet.Mostmealsincludewhiterice,meats,saltyfishorpork,vegetables,fruits,orsoups. Foodisplacedatthecenterofthetableandeveryonesharesallofthedishes. HealthCare Thedoctor‐patientrelationshipinVietnamisoftendependentontheageofthedoctor. Youngerphysiciansmightbeconsideredincompetentandaskedabouttheireducationas theyhavenotyetacquiredmuchexperience.Olderphysicians,particularlythosewhohave beenpracticingformorethan20years,areconsideredexperts.Theoldestmaleinthe familymakesallofthehealthcaredecisionsandpatientsareveryrarelyeducatedabout theirconditions.Itisoftenconsideredmoreimportanttospareapatient’sfeelingsthanto tellthemthetruthabouttheirmedicalailment.Informationonmedicationsordiagnostic proceduresisalsonotfrequentlycommunicatedwiththepatientandsoitisnot uncommonforpatientstobeunfamiliarwiththeirmedicalhistories. Specifichealthconcerns.Malnutritionandinadequatehealthcarearecommonin Vietnam.HealthdisparitiesinVietnamaremostlytheresultofpoverty,inadequateaccess tocleanwater,pollution,andwar.BecauseoftheuseofAgentOrangeduringtheVietnam War,birthdefectswerefrequent. 102 Pollutedwater,malnutrition,andpooraccesstomedicationsandhealthcareareonlysome ofthefactorscausinghighratesofdysentery,tuberculosis,choriocarcinoma,hepatitis, typhoid,denguefever,Japaneseencephalitis,cholera,andcholoroquine‐resistantmalaria. HIV/AIDSratesinVietnamareontherise,witharecentWorldHealthOrganization estimateofabout.4%forages15to49. LifestyleRiskfactors.LactoseintoleranceiscommonamongVietnamese.Malnutritionis expectedtoaffectmorethanhalfofthepopulation. MentalHealth.MentalhealthailmentscanbeaparticularconcernintheVietnamese population,astheircountry’sviolenthistoryhasbeendifficulttobear.Thereisastrong stigmaagainstmentalillness,however,andmanytimesemotionaldisturbancesare actuallymanifestedsomatically. TraditionalMedicine.PeoplefromdifferentregionsofVietnamhavedifferentbeliefs abouthealthandsickness.Forexample,manymountainpeoplebelievethatsicknessisa punishmentfromthegodswhilethoseinruralcommunitiesoftenplaceemphasison imbalancedyin‐yangorchi.Treatmentscanincludemagical,religiousandWestern medicine.Herbs,acupuncture,massage,anddermabrasivepracticesarecommon treatments.Cuppingandcoiningarepopularwaystodrawillnessoutofthebody.In coining,acoinisheatedandrubbedalloverthebody.TheVietnamesebelievethatred weltsormarkswillonlyappearonthosewhoaretrulyill.Coiningandotherpractices shouldbekeptinmindformanyAsianculturesandhealthcareprofessionalsshouldnotbe quicktoassumecontusionsresultfromabuseormaltreatment. Above:cuppingmarksroughlyonedayafter treatment.Cuppingusesheatedairinattempt tosuckout“badwinds”orunhealthyair currentsfromthebody. Above:coiningmarksonapatient’sback. Incoining,ahotcoinsometimescovered inboiledoilisrolledalongapatient’s skintobringillnessoutofthebody. 103 SocialEtiquette Thereismoreemphasisonverbalcommunicationandgreetingthanonbody language,whichisoftenconsideredimproper. Thetypicalgreetingmightincludeahandshakeandaverbalchao,whichmeans “greetings.” AlthoughhandshakingisacceptedbymanyVietnamese,physicaltouchingisoften consideredinappropriate. Itisconsideredinappropriatetotouchaperson’sheadasitisconsideredtobethe centerofthesoul.Olderadults,however,arepermittedtotouchtheheadsof youngerchildren. Itisalsoconsideredoffensivetobeckonanotherpersonbyusingonlytheindex finger,asthisgestureisusedtocalladog.Instead,itispreferredtouseallfour fingerswiththepalmfacingdownward. Directeyecontactduringconversationisconsidereddisrespectful. Besensitivetomedicalbeliefsandpractices,assomeAsianculturesdonotadhere toWesternmedicine.Researchingaheadoftimecanprepareyouroffice. AdditionalResources StanfordUniversity:VietnameseHealthCare http://med.stanford.edu/medicalreview/smrvietnam.pdf VietnameseTraditionalMedicinebyLenaLopez www.vietspring.org/custom/trad‐medicine.html Worksconsulted HuntPC.AnIntroductiontoVietnameseCultureforRehabilitationServiceProvidersinthe U.S.Buffalo,NY:CenterforInternationalRehabilitationResearchInformationand Exchange(CIRRIE);2002. LindsayJ,NarayanMC,ReaK.Nursingacrosscultures:theVietnameseclient.HomeHealth Nurse.Oct1998;16(10):693‐700. McKelveyRS,SangDL,BaldassarL,DaviesL,RobertsL,CutlerN.Theprevalenceof psychiatricdisordersamongVietnamesechildrenandadolescents.MedJAust.Oct21 2002;177(8):413‐417. 104 AfricanAmericans Backgroundandculture Definitions.Whenwesay“AfricanAmerican” inthischapter,wearereferringtoAmericans ofAfricanoriginwithmultigenerationaltiesto theUnitedStates.Theinformationthatfollows isspecificforthispopulation.However,itis importanttopointoutthatthereisanother populationofAfricanAmericanslivingin Vermont,andelsewhereintheUnitedStates.TheseareAfricanrefugees.Theyhavebeenin Americaforashorterperiodoftime,andcametothiscountryunderadifferentsetof circumstancesthantheAfricanAmericanswediscusshere.Thatsaid,healthconcerns notedhereandinindividualrefugeechaptersmayoverlapbetweenAfricanpopulations. FordetailedinformationonrefugeeAfricanAmericans,seethecountry‐specificrefugee chaptersinthismanual. History.AfricanAmericanhistoryismarkedbyslavery,discrimination,andthefightfor civilrights.AfricanAmericans’ancestorswereforciblytakenfromAfricaandsoldasslaves intheWest—inCuba,Brazil,andthesouthernUnitedStates.TransportfromAfricatothe Westwassevere,andmanyAfricansdiedenroute.TheAmericanCivilWarwasfoughtin partoverslavery;whenitendedin1865,formerslaveswereostensiblyfree,howevera centurywouldpassbeforesegregationwasendedandtheCivilRightsMovementachieved legislationgraduallyaffordingequalrights.Despitethislegislation,however, discriminationremained(andremains)aproblem;currently,AfricanAmericans experienceasomewhatuneasyandsometimesincompletemeasureofequalitywithin Americansociety1.AdetailedhistoryofAfricanAmericansintheUnitedStatesisbeyond thescopeofthischapter;numerousotherresourcesareavailableforthatpurpose. Demographics.In2010,13%oftheUnitedStatespopulationwasAfricanAmerican2and by2050thisnumberispredictedtogrowto15%.3InVermont,between1990and2007, AfricanAmericanswerethefastestgrowingpopulationinVermont,withtheirnumbers morethantriplingduringthatperiod.4 Culture.AlthoughthetermAfricanAmericanisoftenappliedindiscriminately,“African Americans”areactuallyanextremelyculturallydiversegroup,withancestraltiestostates allovertheCaribbean,SouthAmerica,Africa,Europe,andmanyotherplaces.Becauseof this,manyAfricanAmericanfamiliesareofmixeddescent,havingintermarriedwith Europeans,SouthAmericans,AmericanIndians,orotherethnicgroups.Thiscomplicates anyideaofaunifiedAfricanAmericanculture;indeed,culturalpracticesofonegroupmay notevenberecognizedbyothergroups. PriortoWorldWarII,AfricanAmericanslivedprimarilyarural,Southernlife.AfterWorld WarII,themajorityofAfricanAmericansmigratedtoNorthernurbancenters.Today,the citieswiththehighestpopulationofAfricanAmericansareNewYork,Chicago,Detroit, 105 Philadelphia,LosAngeles,theDistrictofColumbia,Houston,Baltimore,NewOrleans,and Memphis.Ingeneral,religious,family,andcommunitytiesareimportantinAfrican Americanculture.Childrenareoftenraisedinanenvironmentofstrongmoralvaluesand strongincentivetosucceed.However,declininggovernmentaleducationassistanceand decliningjobopportunitiesoftenmakesuccessdifficulttoachieve. Healthcare Severalfactorsconspiretomakethedeliveryofeffectivehealthcaremoredifficultinthe AfricanAmericanpopulationthantheUnitedStatespopulationatlarge:ahistoryofsocial andinstitutionaldiscrimination,overalllowersocioeconomicstatus,decreasedaccessto healthcare,andtheobservationthatmanyAfricanAmericancommunitiesarestruggling withpoverty,substanceabuse,andviolence.1,5 Lowersocioeconomicstatusisapredictorofpoordietarychoices,lowerphysicalactivity, tobaccouse,andalcoholabuse;itisalsoassociatedwithahigherdegreeofchronicstress, whichcorrelatespositivelywithdevelopmentofchronicdisease.5In2005,54%ofnon‐ elderlyAfricanAmericanswerepoorornear‐poor,comparedto26%ofnon‐elderlywhite Americans;intheelderlypopulation,thesefigureswere67%and38%,respectively.6This levelofpovertyleadstodecreasedaccesstohealthcare.5 Communitystructurecanalsoleadtopoorerhealthcare,albeitindirectly.Forexample, propertyvaluestendtobelowerinpredominantlyAfricanAmericancommunities.This leadstolesspropertytaxrevenue,lessbusinessinvestmentinthearea,and,overall,less moneycomingintoinvestinthingslikehealthcareservices.5,7.Thebusinessesthatdo investmaynotbethemosthealthconscious.Forexample,theretendtobemorefast‐food restaurantsandalcoholvendorsinAfricanAmericancommunitiescomparedtowhite Americancommunities,andlessavailabilityofaffordablefreshfruitsandvegetables.7 SpecifichealthconcernsintheAfricanAmericanpopulation6 In2003,theinfantmortalityratewas13.6per1,000birthsintheAfricanAmerican populationversus5.7inthewhiteAmericanpopulation. In2003,AfricanAmericansexperiencedhighermortalityateveryageoflifethan whiteAmericans. In2003,AfricanAmericansdiedfromheartdiseaseatasignificantlyhigherrate thandidwhiteAmericans. In2002,AfricanAmericansdiedatasignificantlygreaterratefrombreast,lung,and colorectalcancerthanwhiteAmericans,despiteroughlyequalratesofscreening. In2004,14.3%ofAfricanAmericanshadtypeIIdiabetes,comparedto8.9%of whiteAmericans. InVermont,between2003and2008,26%ofAfricanAmericanswereuninsured, comparedto13%ofnon‐Hispanicwhites.4 106 In2004,thepercentageofAfricanAmericanswhohadlateornoprenatalcarewas 5.7%,comparedto2.2%forwhiteAmericans. In2004,thepercentageofAfricanAmericanswhohadnotseenadentistinthe previousyearwas43%,comparedto32%ofwhiteAmericans. In2004,17%ofAfricanAmericanchildrenhadasthma,versus12%ofwhite Americanchildren. In2006,therewastentimesasmuchtuberculosisintheAfricanAmerican populationthaninthewhiteAmericanpopulation(CentersforDiseaseControl, 2006). In2004,lifeexpectancywas73yearsforAfricanAmerican,and78yearsforwhite Americans.8 In2008,despiteonlybeing13%ofthepopulation,AfricanAmericansaccountedfor 50%ofnewHIVcases.3 Specificstepsforhealthcareproviders Focusonpreventativehealth,particularlywithrespecttoheartdiseaseand diabetes,bothofwhichoccurathigherrateswithintheAfricanAmerican populationthaninthegeneralpopulation.Screeneverypatient,everytime,forrisk factorssuchasobesity,smoking,diabetes,andhypertension.Lifestylemodifications forheartdiseaseandhypertensionhavebeenshowntobeparticularlyeffectivein thispopulation,9,10ashavecommunityhealthadvisors.11Lifestylemodifications, particularlydietandexercise,areespeciallyimportantinAfricanAmericanteens.12 Screenfordepression.AfricanAmericansaremorelikelytoexperienceamental disorderthanwhiteAmericans.Theyarealsolesslikelytoseektreatment. Sickle‐cellanemiaoccursmorefrequentlyinthispopulation,andalthoughAfrican Americanwomengenerallyunderstandtheseverityofthiscondition,theymay underestimatetheirlikelihoodofgettingit.13 Understandthatthecommunitieswhereyourpatientsliveandworkarediverse, maybedifferentfromoneanother,andwilllikelyhaveamajorimpactontheir healthandhealthcare.Itisimportanttounderstandthesecommunitiesandyour patients’placesinthem. Advisepatientsaboutfactorsthataffectbirthoutcomes,suchasmaternalsmoking, substanceabuse,diet,stress,insufficientprenatalcare,andchronicillness. Providesexualhealthcounseling,especiallywithrespecttoHIV/AIDS. 107 Ensurethatyouarecommunicatingclearlyandcompletelytoyourpatients–oneof theexplanatoryfactorsforpooreroverallhealthinAfricanAmericansislimited accesstohealthinformation.14 Additionalresources VermontDepartmentofHealth,OfficeofMinorityHealthandHealthDisparities: http://healthvermont.gov/local/mhealth/minority.aspx UnitedStatesDepartmentofHealthandHumanServices,OfficeofMinorityHealth: http://minorityhealth.hhs.gov/ 108 References 1. BrisbaneFL,ed.CulturalCompetenceforHealthCareProfessionalsWorkingwith African‐AmericanCommunities:TheoryandPractice.In:CenterforSubstance AbusePrevention,ed.Washington,DC:UnitedStatesDepartmentofHealthand HumanServices;1998. 2. UnitedStatesCensusBureau.StateandCountyQuickFacts.Washington,DC:United StatesCensusBureau;2012. 3. OfficeofMinorityHealthandHealthDisparities.HealthDisparitiesAffecting Minorities:AfricanAmericans.Atlanta,GA:CentersforDiseaseControland Prevention. 4. VermontDepartmentofHealth.TheHealthDisparitiesofVermonters, http://healthvermont.gov/research/documents/VTDisparitiesRpt2010.pdf. Burlington,VT:VermontDepartmentofHealth;2010:50‐63. 5. WilliamsDR,JacksonPB.Socialsourcesofracialdisparitiesinhealth.HealthAff (Millwood).Mar‐Apr2005;24(2):325‐334. 6. JamesC,ThomasM,Lillie‐BlantonM,GarfieldR.KeyFacts:Race,Ethnicity,and MedicalCare,2007Update.Washington,DC:KaiserFamilyFoundation;2007. 7. AirhihenbuwaCO,LiburdL.EliminatinghealthdisparitiesintheAfricanAmerican population:theinterfaceofculture,gender,andpower.HealthEducBehav.Aug 2006;33(4):488‐501. 8. AriasE.UnitedStatesLifeTables,2004.NationalVitalStatisticsReports.Vol56. Hyattsville,MD:NationalCenterforHealthStatistics;2007. 9. StephensT,BraithwaiteH,JohnsonL,HarrisC,KatkowskyS,TroutmanA. CardiovascularRiskReductionforAfrican‐AmericanMenThroughHealth EmpowermentandAngerManagement.HealthEducationJournal.2008;67(3):208‐ 218. 10. RankinsJ,SampsonW,BrownB,Jenkins‐SalleyT.DietaryApproachestoStop Hypertension(DASH)interventionreducesbloodpressureamonghypertensive AfricanAmericanpatientsinaneighborhoodhealthcarecenter.JNutrEducBehav. Sep‐Oct2005;37(5):259‐264. 11. CornellCE,LittletonMA,GreenePG,etal.ACommunityHealthAdvisorProgramto reducecardiovascularriskamongruralAfrican‐Americanwomen.HealthEducRes. Aug2009;24(4):622‐633. 12. Lewis‐MossRK,PaschalA,RedmondM,GreenBL,CarmackC.Healthattitudesand behaviorsofAfricanAmericanadolescents.JCommunityHealth.Oct 2008;33(5):351‐356. 13. GustafsonSL,GettigEA,Watt‐MorseM,KrishnamurtiL.Healthbeliefsamong AfricanAmericanwomenregardinggenetictestingandcounselingforsicklecell disease.GenetMed.May2007;9(5):303‐310. 14. SandersThompsonVL,TalleyM,CaitoN,KreuterM.AfricanAmericanmen's perceptionsoffactorsinfluencinghealth‐informationseeking.AmJMensHealth.Mar 2009;3(1):6‐15. 109 Thispageintentionallyleft blank. 110 DeafandHardofHearing Background Estimatingthesizeofthedeafandhard‐of‐hearing populationintheUnitedStatesisdifficultbecause populationestimateschangedependingonthedefinitions usedtocategorizepeopleasdeaforhard‐of‐hearing.The mostrecentdatasuggeststhatabout0.38%ofthe populationisfunctionallydeaf—thatis,unabletohear anything,evenwiththeassistanceofahearingaid,andthat afurther3.72%ofthepopulationishard‐of‐hearing. However,thesenumbersobscureconsiderableage‐relatedvariation.Infact,the percentageofthepopulationthatisdeaforhard‐of‐hearingbeforeage18islessthan5%, whileafterage65,morethan30%ofthepopulationisdeaforhard‐of‐hearing.Morethan halfofalldeaforhard‐of‐hearingpeoplelosetheirhearinggradually,withtotalloss occurringlaterinlife.1 Causesofhearingloss.Hearinglosscanbehereditaryoracquired,andhereditaryhearing losscanbenon‐syndromicorsyndromic.Innon‐syndromichereditaryhearingloss, hearinglossoccursaloneandistypicallyinheritedmonogenically,althoughpolygenic formsdoexist.Todate,32genesresponsibleformonogenicnon‐syndromichereditary hearinglosshavebeenidentified.2Incontrast,insyndromichereditaryhearingloss, hearinglossoccursalongsideseveralothercomorbiditiescharacteristicofthesyndrome, andisinheritedpolygenically.Todate,396syndromesincludinghearinglossasoneofthe symptomshavebeenidentified.3Someofthemostcommonare4: Hemifacialmicrosomia,characterizedbyfacial,auricular,andcervicalspinal abnormalities Sticklersyndrome,characterizedbyflattenedfacialprofile,cleftpalate,ocular changes,andarthropathy Ushersyndrome,characterizedbyretinitispigmentosa Waardenburgsyndrome,characterizedbypigmentabnormalitiesoftheskinand eyes Branchio‐oto‐renalsyndrome,characterizedbybranchialcleftcystsandrenal abnormalities Pendredsyndrome,characterizedbyahypo–oreu–thyroidgoiter Neurofibromatosis2,characterizedbylate‐onsethearinglosscausedbyvestibular schwannoma;patientsareatalsoatincreasedriskofothertypesofcancer 111 Alportsyndrome,characterizedbyrenalandoculardisease JervellandLange‐Nielsensyndrome,characterizedbyprolongedQ/Tinterval Commoncausesofacquiredhearinglossincludeearinfections,ototoxicdrugs(e.g. streptomycin,aspirin),exposuretohighlevelsofnoise,trauma,otosclerosis (calcificationofthemalleus,incus,orstapes),vestibularschwannomas(atumorof thecellsensheathingtheacousticnerve),Meniere’sdisease(adiseaseofunknown origincharacterizedbyhearingloss,vertigo,andtinnitus),andage‐relatedhearing loss(presbycusis). Culture.Manydeafindividualsidentifythemselvesasmembersofadeafculturewhose elementsinclude,amongothers,asharedlanguagewithdistinctregionalandnational dialects,asharedhistoryandasharedsetofexperiencesresultingfromlivinginahearing world,andadistinctsetofpublicandprivatedeafinstitutions,includingdeafschools, clubs,andsportingevents.Indeed,manydeafpeopledonotregarddeafnessasatrue disability,arguinginsteadthatthedifficultiesdeafpeopleexperienceindailylifearethe resultoflivinginasocietydominatedbythehearing.Forexample,whilecommunication betweendeafandhearingindividualscanbedifficult,adeafindividualmightsuggestthat thisdifficultycouldbealleviatedifhearingindividualslearnedsignlanguage.5Manydeaf organizationsadvocateforequitabletreatmentinareassuchascivilrights,accesstohealth care,accesstofreepubliceducation,thecreationofdeaf‐accessiblemedia,andothers.6 Communication Deafindividualscommunicatewithamixofsignlanguage(AmericanSignLanguage[ASL]) inAmerica,althoughotherdialectsexist),speech,readinglips,andwriting.5,7ASLisnota writtenlanguage,however,andmanydeafindividualsdonothaveahighlevelofEnglish literacy.ThismakescommunicationinwrittenEnglishaproblem.8 Askyourpatienthowtheyprefertocommunicate,andhaveatranslatorpresentifthey prefertocommunicateusingsignlanguage.KeepinmindthatASLisanexpressive language;bodylanguageandfacialexpressionimportmeaningtothesigns(forexample, fear,urgency,orfrustrationcanbeconveyedwithlarger,morerapidsigning).Ifyour patientpreferslipreading,makesureyouhavetheirattentionandthattheycanseeyou clearlybeforebeginningtospeak.Chewinggum,wearingafacemask,orturningyourhead whilespeakingcanimpedeunderstanding.Standinginfrontofabrightlightmayalsomake communicationdifficult.Ifyourpatientpreferswriting,keepinmindthatASLdoesnot followthenormalgrammaticalconventionsofEnglish;diagramsandpicturesmaybe useful.7Inclinicalsettings,makesureyouincludeyourdeafpatientinthediscussionof theirdisease,procedures,andtreatment.Miscommunicationaboutwhat’sgoingtohappen, andwhen,inmedicalprocedurescancausefearandanxietyfordeafpatients,anddeaf peopleconsideritrudetobeexcludedfromanyconversationalinformation.9,10 Whenspeakingwithapatient,rememberthatwhileEnglishcommunicationoftenworksits wayuptothemainpointandthenconcludesabruptly,deafcommunicationoftenbegins abruptlyandthenwindsdownslowly;deafpatientsmaystillbewindingdownwhile 112 healthcareprofessionalsfeelthattheconversationisfinished.10Beawareoflowlevelsof Englishcomprehensionandhealthliteracy,andensurethatyou’veeffectively communicatedallofthenecessaryinformationtoyourpatient(forexample,byhaving themrepeatbacktoyouwhatyou’vesaidtothem).10Finally,ensurethatyourofficeisset uptocommunicateeffectivelywithdeafpatientsforadministrativepurposes.Thisincludes trainingyourstafftocommunicatewithdeafpatients(forexample,instructingoffice assistantstowalkdirectlytoyourpatientinsteadofpagingthemwhenit’stimefortheir appointment)andhavingdeaf‐appropriatetelephoneresourcessuchasTTYathand.See “AdditionalResources”,below,forfurtherinformation. Healthcare Theconceptthatdeafnessisnotadisabilityhasledtohealthcareconflictsbetween membersofthedeafandhearingcommunity.Oneofthemostnotableisthecontroversy surroundingcochlearimplants.Thesearesmalldevicesthataresurgicallyinsertedintoa deafpatient’scochleaandallowthemtohear.5,11Becausemembersofthedeafcommunity donotfeelthatdeafnessisadisability,theyareunderstandablyoffendedbytheprospect ofobtainingamedical“fix”fordeafness.11Additionally,thenormalbiologyofthe developingbrainmakeslanguageacquisitionparticularlydifficultbeyondchildhood;tobe effectiveinrestoringhearingandallowingthedevelopmentofnormalspeech,cochlear implantsmustbeimplantedearly.However,thismeansthatthedecisiontoimplantis oftengreatlyinfluencedbythepatient’sparents.Thepotentialconflictsofinterestbetween thehearingmedicalcommunity,deafchildren,andparentswhomayormaynotbedeaf makesthisaverydifficultissuetoresolve.11,12 Specifichealthconcernsinthedeafandhardofhearingpopulations7‐10,13‐15 Effectivecommunicationwiththehearingworldisoftenthesinglebiggestconcern fordeafindividualswheninteractingwiththehearingworld.Thisisaresultofdeaf individuals’limitedEnglishcapacityaswellasthehearingworld’slimited accommodationfordeafindividuals. Deafindividualsmaynottrusthealthcareprofessionals. Deafindividualsmaybeconcernedaboutbeingperceivedasdumb,aresultofthe historicalclassificationofschoolsforthedeafasschoolsforthe“deafanddumb.” Deafindividualsmayhavelessaccesstohealthservicesasaresultof communicationbarriers,butalsobecausedeafindividualsaremorelikelytobe poorer,unemployed,and/orreceivingfederally‐fundedhealthcare.Inparticular, deafindividualsmayhavelimitedaccesstomentalhealthservicesdespitehigher levelsofanxietyanddepressioninthedeafcommunity. Healthliteracymaybelow;deafpatientsmayhavetroubleunderstandinggeneral topicssuchasdisease,diseaseprevention,andtreatment,andspecifictopicssuchas allergy,bodytemperature,nausea,constipation,andothers.Theymayalsohave 113 troubleunderstandingprescriptionlabels.Thisisaresultofpoorhealtheducation aswellasdifficultyunderstandinginformationpresentedinEnglish. Deafindividualsmayhavelimitedknowledgeofsexualandreproductivehealth, includingknowledgeofHIV/AIDS. Deafindividualsmayhavelimitedknowledgeofpreventativecare,includingcancer prevention. Deafindividualsmayhavelimitedknowledgeofcardiovascularhealth,andmaybe unabletolistthesymptomsofaheartattackorstroke. Deafindividualsmaysufferfromcomorbiditiesassociatedwithsyndromic hereditarydeafness(seeabove). Specificstepsforhealthcareproviders Inadditiontobeingawareofsyndromiccomorbiditiesassociatedwithcongenitaldeafness, healthcareprofessionalsshouldfocusonimprovingcommunicationandeducational outreachtodeafpatients. AdditionalResources AustineSchoolfortheDeaf(Brattleboro,VT): http://www.vcdhh.org/schools/austine‐school‐for‐the‐deaf NationalAssociationoftheDeaf: http://www.nad.org/ UniversityofRochesterMedicalCenter’sDeafWellnessCenter: http://www.urmc.rochester.edu/deaf‐wellness‐center/ VermontCenterfortheDeafandHardofHearing: http://www.vcdhh.org/ VermontCenterforIndependentLiving: http://www.vcil.org/services/peer‐advocacy/deaf‐independence‐program VermontRegistryofInterpretersfortheDeaf: http://www.vtrid.org/ 114 References 1. MitchellRE.HowmanydeafpeoplearethereintheUnitedStates?Estimatesfrom theSurveyofIncomeandProgramParticipation.JDeafStudDeafEduc.Winter 2006;11(1):112‐119. 2. FriedmanTB,GriffithAJ.Humannonsyndromicsensorineuraldeafness.AnnuRev GenomicsHumGenet.2003;4:341‐402. 3. MoodyAntonioSA,StrasnickB.InnerEar,SyndromicSensorineuralHearingLoss. 2009;http://emedicine.medscape.com/article/856116‐overview.AccessedApril, 2012. 4. SmithR,ShearerA,HildebrandM,VanCampG.DeafnessandHereditaryHearing LossOverview.GeneReviews.1993. http://www.ncbi.nlm.nih.gov/pubmed/20301607.AccessedApril,2012. 5. SparrowR.DefendingDeafCulture:TheCaseofCochlearImplants.Journalof PoliticalPhilosophy.2005;13(2):135‐152. 6. NationalAssociationoftheDeaf.AbouttheLawandAdvocacyCenter. http://www.nad.org/issues/about‐law‐and‐advocacy‐center.AccessedApril,2012. 7. UniversityofWashingtonMedicalCenter.CommunicatingWithYourDeafPatient. 2012;http://depts.washington.edu/pfes/PDFs/DeafCultureClue.pdf.Accessed April,2012. 8. McKeeM.BetterHealthThroughAccessibleCommunication.Rochester,NY: NationalCenterforDeafHealthResearch;2009. 9. IezzoniLI,O'DayBL,KilleenM,HarkerH.Communicatingabouthealthcare: observationsfrompersonswhoaredeaforhardofhearing.AnnInternMed.Mar2 2004;140(5):356‐362. 10. MeadorHE,ZazoveP.Healthcareinteractionswithdeafculture.JAmBoardFam Pract.May‐Jun2005;18(3):218‐222. 11. DelostS,LashleyS.TheCochclearImplantControversy. http://www.drury.edu/multinl/story.cfm?id=2442&nlid=166.Interdisciplinary ResearchConference.Springfield,MO:DruryUniversity;2000. 12. GeersAE.Speech,language,andreadingskillsafterearlycochlearimplantation. ArchOtolaryngolHeadNeckSurg.May2004;130(5):634‐638. 13. VernonM,LeighIW.Mentalhealthservicesforpeoplewhoaredeaf.AmAnnDeaf. Fall2007;152(4):374‐381. 14. PollardRQ,BarnettS.Health‐relatedvocabularyknowledgeamongdeafadults. RehabilPsychol.May2009;54(2):182‐185. 15. KvamMH,LoebM,TambsK.Mentalhealthindeafadults:symptomsofanxietyand depressionamonghearinganddeafindividuals.JDeafStudDeafEduc.Winter 2007;12(1):1‐7. 115 Thispageintentionallyleft blank. 116 Elderly Background Demographics.Americansarelivinglongernowthanatanytimein ourhistory.In1900,theaverageAmericanlifeexpectancywas47.3 years;in2000,itwas76.9.In1990,4.1%ofthepopulationwasaged 65orolder;in2003(intheUnitedStates)and2007(inVermont)this numberhadgrownto12%and13.6%,respectively.By2030(inthe UnitedStates),and2020(inVermont),asaresultofagingbaby boomers,those65orolderareexpectedtomakeup20%ofthetotal U.S.population.Thisdemographicshiftispredictedtohave consequencesforthecostofAmericanentitlementprogramssuchasSocialSecurityand Medicare(Medicarecostsarepredictedtorisefrom2.7%ofgrossdomesticproductin 2006to9%in2050.1)Itwillalsoimpactthestructureanddeliveryofhealthcareasmore servicesareadaptedtomeettheneedsofanagingpopulation.2 Normalaging.AccordingtotheWorldHealthOrganization(2008),“agingisnotadisease; agingisadevelopmentalprocess.”Factorsthataffecthowapersonagesincludegenes, lifestyle,diet,co‐morbiddiseases,theenvironment,socialnetworks,andcopingabilities. Commonly,visionandhearingsensitivitydecline.Muscleandbonestrengthlessens.Skin becomeswrinkled,dry,lesselastic,andmorefragile;nailsbecomethickerandbrittle.Lung capacitydecreases.Bladdermusclesweaken,andinmen,theprostatemayenlarge.The speedofdigestionmayslow.Braincellswillbelost,andmemorymaydecline.3These normalchangespredisposetosomecommonhealth‐relatedproblemsofagingofwhich practitionersshouldbeaware. Healthcare Thetop5causesofdeathintheelderlypopulationin1980,1999,and2000,wereheart disease,malignantneoplasm,cerebrovasculardisease,chronicrespiratorydisease,and pneumonia/influenza;thefactthatthesenumbershavenotchangedsignificantlyinthe pastseveraldecadessuggeststhattheywillcontinuetofigureprominentlyinelderly healthcareinthedecadestocome.In2000,otherlikelycausesofdeathinthispopulation includeddiabetes,Alzheimer’sdisease,renaldisease,accidents(includingmotorvehicle accidents)andsepticemia(Heetal.,2005).In2010,accordingtotheCentersforDisease Control,theseleadingcausesofdeathamongtheelderlyremainunchanged. Specifichealthconcernsintheelderlypopulation4,5 visiondisorderssuchasage‐relatedmaculardegeneration,cataracts,diabetic retinopathy,visionloss neurologicaldisorderssuchasAlzheimer’sDiseaseorParkinson’sDisease,balance problems(leadingtofalls),depression boneandjointdisorders,suchasrheumatoid‐andosteoarthritis,gout,osteoporosis 117 cancers,especiallycolorectal,lung,oral,prostate,skin,leukemia chronicobstructivepulmonarydisease diabetes cardiovasculardisorderssuchasmyocardialinfarction,heartfailure,highblood cholesterol,highbloodpressure,stroke mentalhealthissuessuchasworriesaboutdeclininghealthstatus,declining memory,lossofsocialcontact–especiallyinpatientsover85yearsofage dentalconditionssuchastoothdecay,gumdisease,infection,oralcancer digestiveproblemssuchasconstipation,problemswithswallowing,other conditionsassociatedwithslower‐movingdigestivetracts chronicconditions;mostelderlypeoplehaveatleastonechronichealthproblem1 otherconditionssuchashearingloss,kidneydisease,shingles,easybruising Specificstepsforhealthcareproviders Focusonestablishing/maintaininghealthylifestyle.Forexample,promoteage‐ appropriateexerciseregimestohelppreventcardiovascular,metabolic,boneand joint,andotherdisorders;promotemaintenanceofcognitivefunctionby encouragingphysicalactivity,cardiovascularfitness,andabstinencefromtobacco andexcessalcohol(topreventvasculardementia);encouragecontinuouseducation inolderage;providealcoholandtobaccocessationcounseling;andprovide diet/nutritioncounseling. Accountforthepossibilitythatelderlypatientsmighthavepoorvision:makesure lightingisadequate,installhandrailsonstairs. Accountforthepossibilitythatelderlypatientsmighthavehearingloss:sitface‐to‐ facewithpatients,don’tcoveryourmouth,speakslowly,reducebackgroundnoise, speakonthesideofthe“good”ear,etc. Beawarethatdiseaseswithaneurologicalcomponent(e.g.stroke,dementia,or Parkinson’sDisease)canaffectcommunicationbetweenyouandyourelderly patient. Writethingsdownifnecessary. 118 Besensitivetothelifechangesthattheelderlyareexperiencing.Transitionperiods suchasretirement,movingtolongtermcare,orlosingfriendsandspousesareall veryprofoundexperiencesthatshouldbeacknowledged.Educatingthepatient abouthealthylivingandaidingthemastheycopewithlifechangesisimportantto thepatient‐providerrelationship. Beawareof,andscreenfor,memoryloss,urinaryincontinence,depression,andfalls (four“geriatricgiants,”accordingtotheWorldHealthOrganization),hypertension anddiabetes. Conductage‐appropriatepreventativehealthscreeningsasrecommendedbythe WorldHealthOrganizationinthefiguresbelow. Bloodpressure, heightandweight Obesity Cholesterol PapSmear Mammography Colorectalcancer Osteoporosis Alcoholuse YearsofAge 50 55 60 Everyvisit Periodically Everyyear Every1to3years Every1to2years Dependsontests Everyvisit Vision,hearing 119 65 70 75 Routinely Every1to2 years Upperagelimitshouldbeindividualizedforeachpatient Screenings Counseling Every10years Yearly 65 70 75 Onedose Periodically Women:periodically Periodically Upperagelimitshouldbeindividualizedforeachpatient Tetanus‐diphtheria (Td) Pneumococcal Influenza Assesscardiovascular diseaseriskanddiscuss aspirintopreventCVD events Calciumintake Tobaccocessation,drug andalcoholuse,STDs andHIV,nutrition, physicalactivity,sun exposure,oralhealth, injuryprevention,and polypharmacy YearsofAge 50 55 60 Immunizations& Chemoprevention AdditionalResources Age‐friendlyPrimaryHealthCareCentresToolkit,fromtheWorldHealthOrganization. Providesacomprehensiveoverviewofage‐appropriateprimarycare,recommendations fordesigningaprimarycarepracticetomeettheneedsofanelderlypopulation,and sampleformsthatcanbeusedforpreventativehealthscreening. http://www.who.int/ageing/publications/Age‐Friendly‐PHC‐Centre‐toolkitDec08.pdf HealthyAgingforOlderAdults.TheCentersforDiseaseControl’swebsitefocusedon healthyaging.http://www.cdc.gov/aging/ UnitedStatesDepartmentofHealthandHumanServices,AgencyonAging.www.aoa.gov/ 120 References 1. OliverDP,DeCosterVA.Healthcareneedsofagingadults:unprecedented opportunitiesforsocialwork.HealthSocWork.Nov2006;31(4):243‐245. 2. HeW,SenguptaM,VelkoffVA,DeBarrosKA.65+intheUnitedStates:2005Current PopulationReports.Washington,DC:U.S.GovernmentPrintingOffice;2005. 3. WorldHealthOrganization.NormalAgeing‐powerpontpresentation. http://www.who.int/ageing/publications/PPNormalAgeingfortoolkit.pdf.Accessed April,2012. 4. JeonHS,DunkleR,RobertsBL.Worriesoftheoldest‐old.HealthSocWork.Nov 2006;31(4):256‐265. 5. MayoClinicStaff.Aging:WhattoExpectasyouGetOlder. http://www.mayoclinic.com/health/aging/HA00040.AccessedApril,2012. 121 Thispageintentionallyleft blank. 122 LGBTQI(Lesbian,Gay, Bisexual,Transgender, Queer/Questioning,Intersex) Background Definitions1,2: Lesbian:Awomanwhoisemotionally, romantically,and/orsexuallyattractedto otherwomen. Gay:Amanwhoisattractedemotionally,romantically,and/orsexuallytoother men. Bisexual:Apersonwhoisattractedtotwosexesortwogenders,butnotnecessarily simultaneouslyorequally. Transgendered/Transsexual:Individualswhosegenderidentity(i.e.maleorfemale) doesnotmatchtheirbiologicalsex(i.e.XY,XX);transsexualindividualsseekmedical interventiontomorecloselyaligntheirphysicalappearancewiththeirgender identity. Queer:Anumbrellatermforsexualminoritiesthatarenotheterosexual, heteronormative,orgender‐binary.Thistermmaybecontroversial,butitis sometimesusedbyyoungpeopleorforpoliticalpurposes. Questioning:Someonethatisquestioningtheirsexualorientation,unsurewhich gender(s)theyareattractedto. Intersex:Peoplewhoarebornwithphysicalmarkers,sexchromosomes,external genitalia,orinternalreproductivesystems,thatarenotconsideredstandardfor eithermaleorfemale. AlthoughdefiningthesetermsisnecessaryinordertodiscussLGBTQIpopulations,keepin mindthatthesedefinitions,andothers,areimpreciseandoftencontroversialbecauseof thefluidityofhumansexualitywithinandbetweenculturesacrosstime.1,2 Demographics.EstimatesofthesizeoftheLGBTQIpopulationaredifficulttomake.While theUSCensusBureaupublishesstatisticsonthenumberofAmericanslivingassame‐sex couples,nodataiscollectedonbisexual,transgendered,orintersexindividuals.Inaddition, ahistoryofdiscriminationagainstLGBTQIindividualsmakesdatacollectiondifficult.3 Nonetheless,someestimatescanbemade.In2010,thepercentageofVermontersinsame‐ sexcoupleswas1.09%(upfrom0.8%in2000).4Thesizeofthebisexualpopulationis hardertoestimate;inAlfredKinsey’soriginalstudiesonsexualbehavior,46%ofmenand 123 12%ofwomenadmittedtobisexualexperiences(Toufexisetal.,1992),whilestudies conductedinthe1980sand1990sestimatedthesepercentagestobebetween3.3and6% (men)and2.3%(women).5Morerecently,alargesurveyofAmericancollegestudents estimatedthat5%ofwomenand2%ofmenwerebisexual.6Specificdataonthis populationinVermontwasnotavailable.Dataontransgenderedortranssexualindividuals isevensparser,althoughmostestimatessuggestthattheycompriselessthan1%ofthe totalU.S.population.7Finally,estimatessuggestthataboutonein1500‐2000individualsis bornintersex,8,9althoughthisfigureistentativeas“intersex”isdifficulttodefinewith precision,andsome“intersex”conditionsmaygocompletelyunnoticedorunnoticeduntil laterinlife.1 Discrimination.TheLGBTQIcommunityhasbeen,andstillis, subjecttodiscrimination,harassment,andphysicalviolencein boththeUnitedStatesandtheworldwide.WhileU.S.legislation Manyolder hasbeenmovinginrecentdecadestowardsgreaterequalityfor LGBTQIpeople LGBTQIindividuals,itwouldbeprematuretosuggestthattrue feeltheword equalityhasbeenachieved.Acomprehensivediscussionofthe queerhasbeen historyofLGBTQIdiscriminationisbeyondthescopeofthis hatefullyused manual.However,ifyouwouldliketoknowmore,thefollowing againstthemfor organizationsmaybeofinterest:AmericanCivilLibertiesUnion toolongandare Lesbian,Gay,BisexualandTransgenderedProject,GayRightsat reluctantto Change.org,TheIntersexSocietyofNorthAmerica,andThe embraceit. NationalCenterforTransgenderEquality.Pleaserefertothe AdditionalResourceslistedattheendofthechapterforwebsite listingsforeach. Healthcare ManyhealthconcernsoftheLGBTQIcommunityaresharedamongstallitsmembers.For example,discrimination,harassment,andphysicalviolencecancauseanxietyand depressioninLGBTQIindividuals,leadingtolowself‐esteem,feelingsofpowerlessness, substanceabuse,andsuicide.2,10Whilenotconclusive,recent datasuggestthatLGBTQIindividualsmayusetobacco,alcohol, andotherdrugsathigherratesthandoesthegeneral ManyLGBTQI population. individualsdonot telltheirdoctors Furthermore,theperceptionofLGBTQIdiscriminationinthe abouttheirsexual healthcarecommunityhasledtoloweraccessofhealthcare orientation, servicesamongstLGBTQIindividuals.Healthcareaccessisalso becausetheydo threatenedbecauseexistinglegislationoftendoesnotallow notwant LGBTQIpartnerstosharemedicalinsuranceandrestricts discriminationto medicaldecision‐makingrights.Domesticviolencebetween affectthequality LGBTQIpartnersmaygounnoticedbyphysicianswhoassumeit ofhealthcarethey isauniquelyheterosexualissue.Finally,LGBTQIindividualsalso receive. haveuniquehealthneedsasaresultoftheirsexualpractices.11 124 Specifichealthconcernsinthelesbianpopulation13 Breastandgynecologicalcancer:lesbiansmaybeatanincreasedriskofthese cancersduetolowerutilizationofhealthcareservices. Domesticviolence:althoughdomesticviolenceoccursinlesbianhomesathalfthe rateitdoesinheterosexualhomes,itmaygounnoticedbyproviderswhoassumeit isauniquelyheterosexualproblem. Hearthealth:smokingandobesityarethemostprevalentriskfactorsfordisease amonglesbians. Alcohol,tobacco,andsubstanceuse/abuse:seegeneraldiscussionabove. Depression,anxiety:seegeneraldiscussionabove. Specifichealthconcernsinthegaypopulation2,11,12 HIV/AIDSandsafesex:althoughsafe‐sexeducationhasgreatlyreducedthe incidenceofHIV/AIDSinAmerica,gaymenarestillatgreaterriskofcontracting HIVthanthegeneralpopulation,andsafe‐sexpracticeshavebeendecreasingin recentyears. Sexuallytransmitteddiseases(STDs):gaymenareatahigherriskthanthegeneral populationofacquiringSTDs,whichmayincludeHepatitis,thereforeimmunization againstHepatitisisrecommended. Prostate,testicular,andcoloncancer:gaymenmaybeatahigherriskofthese cancersasaresultofdecreasedhealthcareutilization. Bodyimage:gaymenaremorelikelytodevelopanorexiaorbulimia. Analpapilloma:analinfectionwiththehumanpapillomavirusmayberesponsible forincreasedratesofanalcanceramonggaymen. Alcohol,tobacco,andsubstanceuse/abuse:seegeneraldiscussionabove. Depression,anxiety,andsuicide:theseareaconcernforgaymenofallages,but maybeparticularlypronouncedinadolescents. 125 Specifichealthconcernsofthebisexualpopulation11 Sexualhealth:bisexualwomenreporthigher‐risksexual behaviorthanheterosexualwomen,whilebisexualmen Fearof haveahigherriskofcontractingHIVthanheterosexual encountering men. anothernegative experiencewitha Breastcancer(inwomen)andanalcancer(inmen):see healthcareprovider discussionsabove. canleadLGBTQI individualstodelay Hearthealth,nutrition,fitness,andweight. oravoidmedical care. Lackofaccesstosocialsupport,particularlyinbisexual women. Alcohol,tobacco,andsubstanceuse/abuse:seegeneraldiscussionabove. Depression,anxiety,self‐harm,andsuicide:seegeneraldiscussionabove. Specifichealthconcernsofthetransgendered/transsexualpopulation14 Accesstohealthcare:transgendered/transsexualindividualsmaybereluctantto seekcarebecauseoffearofdiscrimination;also,medicalcareforhealthissues specifictotransgenderedindividualsisoftenexpensiveandnotcoveredby insurance. Healthhistory:transsexualindividualsmaybereluctanttosharerelevanthealth history(e.g.gender‐reassignmentsurgery)withhealthcareprofessionalsforfearof discrimination. Hormoneuse:estrogenandtestosteroneusecarriessignificantrisk;hormonesmay alsobeobtainedthroughindirectchannelsoutsidethehealthcaresystem. Cardiovascularhealth:increasedriskbothasaresultofhormoneuseanddecreased utilizationofhealthcareservices. Cancer:hormone‐relatedcancerisrare,butshouldbescreenedfor.Transsexual menwhohavenothadtheirfemalereproductiveorgansremovedruntheriskof gynecologicalcancers,whiletranssexualwomenruntheriskofprostatecancer. Injectablesilicone:sometransgendered/transsexualwomeninjectsiliconetogive them“instantcurves.”Thisisoftenadministeredbynon‐medicalpersonnelandmay migratetounintendedlocations,causingtissuedamage. Fitness:obesityisaconcerninthetransgendered/transsexualpopulation. 126 Alcohol,tobacco,andsubstanceuse/abuse:seegeneraldiscussionabove. Depression,anxiety,self‐harm,andsuicide:seegeneraldiscussionabove. Specifichealthconcernsoftheintersexpopulation Thehealthconcernsofanintersexindividualwilldependonwhythatindividualis intersex.Forexample,congenitaladrenalhyperplasia(CAH)maycauseanintersex conditioninXXindividualsduetoexcesstestosteroneproduction.CAHcausesdecreased levelsofcortisolproduction,leadingtoanimpairedstressresponse,anddecreasedlevels ofaldosteroneproduction,leadingtopotentiallylethalsaltwasting.Thelistofintersex conditionsislong,andeachpatientwillpresentwithauniquesetofhealthconcerns.1 Therefore,adetailedhistoryisthebestwaytodeterminethespecifichealthconcernofa particularpatient.Thatsaid,intersexindividualssufferfromelevatedratesofdepression andanxiety,andpossiblyshame,asaresultofhidingtheirconditionfromsociety.15,16 Specificstepsforhealthcareproviders11,17 Inadditiontobeingawareof,andscreeningfor,theuniquehealthconcernsofLGBTQI individuals,healthcareprofessionalsshouldseektocreateaninclusiveenvironmentin theirpractice. Behonestandawareofyourownbiasesandprejudices. ProvideeducationandtrainingontheLGBTQIcommunityforallstaff. Haveanunisexrestroomavailable. Changethephysicalenvironmentofyourclinic:displaypostersshowingLGBTQI individuals.Postrainbow‐flags,pinktriangles,andotherLGBTQI‐friendlymaterials throughoutofficeandmixedamongsttheothermaterialsintheoffice.Postavisible non‐discriminationstatement.StockLGBTQI‐friendlyliteraturesuchasmagazines andnewslettersinyourwaitingarea. Askpeoplehowtheywouldliketobereferredto,andusepronounsreflectiveofa patient’sgenderidentityratherthanhisorherbiologicalsex. Providerinterviewsandintakeformsshouldbeinclusiveandnon‐judgmental. Ratherthanaskingmaritalstatus,askaboutsignificantsupportsinapatient’slife andleavespaceforsomeonetodescribetheirfamilystructure. Open,non‐judgmentalcommunication,acceptance,andtrustleadtoamoredetailed andaccuratehistory.Thisinturnwillleadtobetterandmoreappropriatecarefor allpatients. 127 ConfidentialityisespeciallyimportanttotheLGBTQIpopulationwhoarestill vulnerabletodiscrimination.Discussconfidentialityissueswithpatientsanddon’t recordsexualorientationinapatient’schartwithoutconsent. Focusonbehaviorratherthansexualorientationwhentreatingallpatients. HeterosexualindividualscanengageinthesamehighriskbehaviorsastheLGBTQI population,andmanyindividualswhodoengageincertainriskybehaviorsdonot self‐identifyasanythingotherthanheterosexual. IncludepartnersofLGBTQIpatientsinhealthcareplanninganddecision‐making. Havehealthpromotioncampaignsthatincludegay,lesbian,bisexual,transgender, queer,andintersexindividualsandtheirfamilies. Additionalresources GayandLesbianMedicalAssociation.AsitewithresourcesforLGBTQIpatientsand practitioners:www.glma.org/ Referto:TopTenThingsLesbians[GayMen,Bisexuals,TransgenderPersons]Should DiscusswithTheirHealthCareProvider: Lesbians:http://www.glma.org/index.cfm?fuseaction=Page.viewPage&pageID=691 GayMen:http://www.glma.org/index.cfm?fuseaction=Page.viewPage&pageID=690 TransgenderedPersons: http://www.glma.org/index.cfm?fuseaction=Page.viewPage&pageID=692 HopeWorks:www.hopeworksvt.org LGBTMentalHealthSyllabus,includesexamplesofhowtoaskinclusive,non‐ heteronormativequestions:www.aglp.org/gap/ OutrightVermont:http://www.outrightvt.org NationalCoalitionforLGBTHealth.http://lgbthealth.webolutionary.com/ RU12?CommunityCenter:www.ru12.org TheIntersexSocietyofNorthAmerica:www.isna.org VermontCares(HIV/AIDSresource):www.vtcares.org VermontDiversityHealthProject:www.vdhp.org VermontersEndingTransgenderOppression:http://vtveto.wordpress.com AmericanCivilLibertiesUnionLesbian,Gay,Bisexual,andTransgenderedProject: http://www.aclu.org/lgbt/index.html GayRightsatChange.org:http://gayrights.change.org/ TheNationalCenterforTransgenderEquality,http://transequality.org/ CDC–Lesbian,Gay,Bisexual,andTransgenderHealthRetrievedJuly20,2012, www.cdc.gov/lgbthealth/ References 1. IntersexSocietyofNorthAmerica.WhatisIntersex? http://www.isna.org/faq/what_is_intersex.AccessedApril,2012. 128 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. JohnsonCV,MimiagaMJ,BradfordJ.Healthcareissuesamonglesbian,gay,bisexual, transgenderandintersex(LGBTI)populationsintheUnitedStates:Introduction.J Homosex.2008;54(3):213‐224. BoslaughS.LocatingDemographicInformationonGLBTPeople:AGuidetothe AvailableReferenceSources.InternationalGLBTArchives,Libraries,Museumsand SpecialCollectionsConference.Minneapolis,MN:GLBTALMS;2006. U.S.CensusBureau.(2010).Same‐sexcouplehouseholdstatisticsfromthe2010 census.RetrievedDecember11,2012from (http://www.census.gov/hhes/samesex/). SmithE,JohnsonS,GuentherS.HealthCareAttitudesandExperiencesDuring GynecologicCareAmongLesbiansandBisexuals.AmericanJournalofPublicHealth. 1985;75(9):1085‐1087. EisenbergM,WechslerH.Substanceusebehaviorsamongcollegestudentswith same‐sexandopposite‐sexexperience:resultsfromanationalstudy.AddictBehav. Jul2003;28(5):899‐913. OlyslagerF,ConwayL.OntheCalculationofthePrevalenceofTransexualism. WPATH20thInternationalSymposium.Chicago,IL:WPATH;2007. MacKenzieD,HuntingtonA,GilmourJA.Theexperiencesofpeoplewithanintersex condition:ajourneyfromsilencetovoice.JClinNurs.Jun2009;18(12):1775‐1783. BlacklessM,CharuvastraA,DerryckA,Fausto‐SterlingA,LauzanneK,LeeE.How SexuallyDimorphicAreWe?ReviewandSynthesis.AmericanJournalofHuman Biology.2000;12:151‐166. PeterkinA,RisdinC.CaringforLesbianandGayPeople:AClinicalGuide.Toronto, ON:UniversityofTorontoPress;2003. BGLAM.CaringforLesbian,Gay,Bisexual,andTransgenderPatients.AnnArbor,MI: UniversityofMichiganMedicalSchool;2005. SilenzioVMB.TopTenThingsGayMenShouldDiscussWithTheirHealthCare Provider.SanFrancisco,CA:Gay&LesbianMedicalAssociation. O'HanlanK.TopTenThingsLesbiansShouldDiscusswiththeirHealthCareProvider. SanFrancisco,CA:Gay&LesbianMedicalAssociation. AllisonR.TopTenThingsTransgenderedPersonsShouldDiscussWithTheir HealthcareCareProvider.SanFrancisco,CA:Gay&LesbianMedicalAssociation. FraderJ,AldersonP,AschA,etal.Healthcareprofessionalsandintersexconditions. ArchPediatrAdolescMed.May2004;158(5):426‐428. LGBTIssuesCommittee,GroupfortheAdvancementofPsychiatry.LGBTMental HealthSyllabus.2011;http://www.aglp.org/gap/.AccessedApril,2012. MineykoA,WilliamsR,AlexanderA,ChanL,Facey‐CrowtherL‐A,WatsonS.Gender andSexualDiversity.GenderandHealthCollaborativeCurriculum http://genderandhealth.ca/en/modules/sexandsexuality/.AccessedApril,2012. 129 Thispageintentionallyleft blank. 130 Homeless Background Definitions.AccordingtotheUnitedStatesDepartment ofHousingandUrbanDevelopment’s2009regulations,a homelessindividuallacksa“fixed,regular,andadequate night‐timeresidence,”andislivinginashelter,an institution,orinanyotherplacenotdesignedor ordinarilyusedforsleepingaccommodation.The McKinney‐VentoHomelessAssistanceAct(2002) broadensthedefinitionofhomelessnessforchildren.For example,childrensharinghousingduetoeconomic hardship,livinginhotels,motels,ortrailerparks, awaitingfostercareplacement,orsimplylivingin substandardhousingareconsideredhomeless. Thesedefinitionsmatterbecausetheyareusedtoincludeandexcludeindividualsfrom governmentsurveysandthereisnofederalhousingassistanceforindividualsnotmeeting theHUDdefinitionofhomelessness,buttheyarenotstatic.Forexample,in2008,certain citiescompletingahomelessnesssurveyforHUDchosetoexcludemultiplefamiliesliving inthesameapartmentandpeoplelivingintrailerparks,althoughthesepeoplewere countedinprevioussurveys.Therefore,althoughhomelessnesshasofficiallydeclinedby 12%inrecentyears,homelessnessadvocatesarguethatthisreductionreflectsanarrowing definitionofwhoishomelessratherthananyrealreductioninhomelessness.1Further confusingcountsistheissueoftheinvisiblehomeless:individualslivinginautomobiles, tents,underbridges,andinotherplaceswheredemographersmightnotfindthem.2 Finally,estimationsofhomelessnessareoftenmadeatasinglepointintime,but homelessnessisanacuteaswellasachronicproblem,andthenumberofhomeless individualsmayfluctuateonashort‐termbasis.Achronically‐homelesspersonisdefined as“anunaccompaniedhomelessindividualwithadisablingconditionwhohaseithera) beencontinuouslyhomelessforayearormoreorb)hashadatleastfourepisodesof homelessnessinthepastthreeyears.3However,TheDepartmentofHealthandHuman Services(2009)estimatesthatoverafive‐yearperiod,2‐3percentoftheU.S.population,or 5‐8millionpeople,willexperienceatleastonenightofhomelessness.Practically,this meansthathomelessnessisdifficulttodefine,difficulttoquantify,andthatcountsmay changewithinorbetweenyearsdependingonwhodoesthecounting,how,where,and when,irrespectiveofanyrealchangesinhomelessness.Theseobservationsshouldbekept inmindwhenreviewingdemographystatisticsbelow. Causesofhomelessness.Povertyandhomelessnessareinextricablylinked.Thisis becausehousingoftenabsorbsasizeable,andgrowing,proportionofafamily’sbudget comparedtofood,childcare,healthcare,andotherexpenditures,andisthereforeoftenthe firstitemcutwhenafamilyisexperiencingfinancialdifficulty.4Whiletherearemany causesofpoverty,twoareespeciallyrelevant.Thefirstofthesehastodowith employment:decliningemploymentopportunities,atrendofreplacingfull‐timewithpart‐ 131 timeortemporaryjobs,andastagnatingminimumwage,makeitdifficultforindividualsto obtainasecure,livablewage.Thesecondofthesehastodowithsocialassistance:stateand federalassistanceprograms—e.g.welfare,subsidizedhousing,andMedicaid/Medicareand otherprograms—aredecreasinginvalueandavailability.Practically,thismeansthat impoverishedindividualsareoftenonelostpaycheckorillnessawayfromhomelessness.4 Otherriskfactorsforhomelessnessincluderelationshipproblems,physicalorsexual abuse,substanceabuse,legaltroubles,and—forchildren—theinstitutionalizationordeath ofaparent.5 Demographics.Accordingtothe2010“PointinTime”reportfromtheVermontCoalition toEndHomelessness,62,782VermonterswerehomelessasofJanuary2010.Ofthese, 1,148weremembersof497families.Thetotalnumberofindividualsthatwere17years oldoryoungerwere766,and317wereover50yearsold.MostlivedinRutland, Chittenden,andBenningtoncounties.Themajorityweremale(andintheUnitedStatesasa whole,40%ofhomelessmenwereveterans).4However,thesenumbersmay underestimatethehomelesspopulationofVermont.Althoughthepopulationofhomeless Vermontershasgonedownsince2000,in2007Vermonthadthehighestrateof homelessnessinNewEngland,andthepercentageofhomelessfamiliesandchildrenhad grown.Additionally,theaveragestayinahomelessshelterisgrowing,from12daysin 2000to26daysin2004.6,7 Healthcare Awidevarietyofhealthproblemsareprevalentinthehomelesspopulation,andtheir morbiditymaybeextremelyhighbecauseofdelaysinseekingcare,non‐adherenceto therapy,andotherfactors.Additionally,middle‐agedindividualsmaydevelopdiseasesthat ordinarilyappearinindividualsmanydecadesolder.8Theseproblemsmaybeexacerbated bylackofhealthinsurance,andlimitedhealthliteracyinhomelessindividualsmaymake treatmentdifficult.9 Mentalhealth.Homelessindividualsaremorelikelythanthegeneralpopulationtosuffer frommentalillness.Thesemayprecede,follow,orbeexacerbatedbyhomelessnessand includeschizophrenia,affectivedisorders,post‐traumaticstressdisorder,depression,low self‐esteem,andhigherratesofsuicidalideationandsuicideattempts.Homeless individualsalsoreportexperiencinggreaterlevelsofstressandarelesslikelytohave adequatecopingstrategiesandsocialsupportnetworksthanthegeneralpopulation. Substanceabuse.Homelessindividualsaremorelikelythanthegeneralpopulationto abusesubstances,includingalcohol,tobacco,marijuana,cocaine(usuallycrackcocaine), heroin,andprescriptiondrugs.Overdosesarecommon.Manyhomelesspeoplemayalso haveaconcurrentsubstanceabuseproblemandmentalillness. Otherhealthconcerns.8,10,11Homelessindividualsarelikelytohaveashorterlifespan thannon‐homelessindividualsandtheyaremorelikelythanthegeneralpopulationto: bephysicallyorsexuallyassaulted 132 develophypothermiaorfrostbiteorfreezetodeath developskindiseasessuchasimpetigo,venousstasisdisease,scabiesandbodylice acquiresexuallytransmitteddiseaseslikeChlamydiaandHIV beunabletocontrolchronicdiseaseslikehypertension,diabetes,andanemia developrespiratorydisordersincludingchronicobstructivepulmonarydiseaseand tuberculosis developmusculoskeletalproblemssuchasosteoarthritis developfootdiseasessuchastineapedis,corns,andcallouses sufferfromunintentionalinjuriessuchasfallsormotorvehiclecollisions Homelesschildrenaremorelikelythannon‐homelesschildrento8,12: becomepregnant developasthma havebehavioraldisorders comedownwithinfectiousdisease,includingupperrespiratorytractinfection, scabies,lice,earinfections,anddiarrhea nothavecompletedtherecommendedscheduleofchildhoodimmunizations sufferfromleadpoisoning bemalnourished(becauseofaninabilitytoaffordnutritiousfood)butobese (becauseofcheaperandeasieraccesstofastfood) havepoordentalhealthandpoorvision sufferfromchildabuse Specificstepsforhealthcareproviders5,9,13 Focusoninfectionpreventionbypromotingvaccinationschedules,facilitating needle‐exchangeandsupervisedinjectionsiteswhereallowedbylaw,provide laundryfacilitieswherepossible,providepodiatryservices,facilitateinsecticide applicationtohomelessshelterbedding. 133 Maintainalistofdrugtherapyprogramsintheareatowhichpatientscanbe referred. Focusonpromotionofsexualhealth. Providecomprehensivecenterswherehomelesspeoplecanaccessmultipleservices inoneplace,astransportationtoandfromhealthcareservicesmaybeanissue. Utilizeamultidisciplinaryteamconsistingofphysicians,socialworkers,mental healthspecialists,andaddictionscounselors. Engageinhealthoutreachtolocalhomelessshelters. Beawarethathomelesspeoplemaybeconcernedaboutprivacyissues,fearfulof largeinstitutionsandthepeoplewhoworkinthem,unawareofservicesavailableto them,andembarrassedaboutdifficultiesmaintainingpersonalhygiene. Beawarethatasaresultofpreviousinteractionswiththepublic,police,family,and healthcareproviders,homelesspeoplemayactinwaysthatseemresistant,bizarre, ordisruptive. AdaptedclinicalguidelinesfromtheHealthCarefortheHomelessClinicians’Network TheHealthCarefortheHomelessClinicians’Network(NHCHC)publishesguidelineson howtoadaptamedicalpracticetoaddressthespecialchallengesfacedbyhomeless patientsthatmaylimittheirabilitytoadheretoaplanofcare.In2010,theyupdatedtheir GeneralPracticesfortheCareofHomelessPatients.9Wehavereproducedthesummaryof recommendationsbelow,initalics.Theentiredocumentisavailableat: http://www.nhchc.org/wp‐content/uploads/2011/09/GenRecsHomeless2010.pdf SummaryofRecommendations: Diagnosisandevaluation History Livingconditions:Askwherepatientisstaying.Exploreaccesstofood,water, restrooms,placetostoremedications;exposuretotoxins,allergens,infection;threats tohealth/safety.Bealerttopossiblehomelessness. Priorhomelessness:Whatprecipitatedit;whetherfirsttime,episodic,chronic;history offostercare. Acute/chronicillness:Askaboutindividual/familialhistoryofasthma,chronicotitis media,anemia,diabetes,CVD,TB,HIV/STIs,hospitalizations. 134 Medications:Askaboutcurrentmedications,includingpsychiatric,contraceptive,and OTCmedications,dietarysupplements,and“borrowed”medicineprescribedforothers. Priorproviders,includingoralhealthproviders:Whatworked/didn’twork,does patienthaveregularsourceofprimarycare. Mentalillness/cognitivedeficit:Problemswithstress,anxiety,appetite,sleep, concentration,mood,speech,memory,thoughtprocessandcontent, suicidal/homicidalideation,insight,judgment,impulsecontrol,socialinteractions; symptomsofbraininjury(headaches,seizures,memoryloss,lability,irritability, dizziness,insomnia,poororganizational/decision‐makingskills). Developmental/behavioralproblems:Adaptive/maladaptive,underlyingpathology. Alcohol/nicotine/otherdruguse:Askaboutuse(amount,frequency,duration);look forsignsofsubstanceabuse/dependence. Healthinsurance:prescriptiondrugcoverage,entitlements(Medicaid/SCHIP, SSI/SSDI),otherassistance. Sexual:Genderidentity,sexualorientation,behaviors,partners,pregnancies, hepatitis/HIV/otherSTIs. Historyandcurrentriskofabuse:Emotional,physical,sexualabuse;knowledgeof crisisresources,patientsafety. Legalproblems/violence:againstpersonsorproperty,historyofarrest/incarceration, treatmentwhileincarcerated. Regular/strenuousactivities:Consistentroutines(treatmentfeasibility);levelof strenuousactivity. Workhistory:Longesttimeheldajob,occupationalinjuries/toxicexposures; vocationalskillsandinterests. Educationlevel,literacy:Everinspecialeducation?If“troublereading,”offerhelpwith intakeform;assessabilitytoreadEnglish. Nutrition/hydration:diet,foodresources,preparationskills,liquidintake. Culturalheritage/affiliation/supports:involvementwithfamily,friends,faith community,othersourcesofsupport. Strengths:Copingskills,resourcefulness,abilities,interests. 135 Physicalexamination Comprehensiveexam‐atfirstencounterifpossible:height,weight,BMI,%bodyfat, abdominalgirth,heart,BP,lungs,thyroid,liverdermatological,oral,fundoscopic, genital,lowerextremities Serial,focusedexams:forpatientsuncomfortablewithfull‐body,unclothedexamat firstvisit Specialpopulations:Victimsofabuse,sexualminorities Dentalassessment:ageappropriateteeth,obviouscaries,dental/referredpain, diabetespatients Diagnostictests Baselinelabs:IncludingEKG,lipidpanel,potassiumandcreatininelevels,HbA1c,liver functiontests,MentalHealthScreening:PatientHealthQuestionnaire(PHQ‐9,PHQ‐2), MHS‐III Asthma:spirometryorpeakflowmonitoring TB:PPDforpatientslivinginsheltersandothersatriskfortuberculosis; QuantiFERON®‐TBGoldtest(QFT‐G),ifavailable STIscreening:Forchlamydia,gonorrhea,syphilis,HIV,HBV,HCV,trichomonas, bacterialvaginosis,monilia Mentalhealth:PatientHealthQuestionnaire(PHQ‐9,PHQ‐2),MHS‐III,MDQ SubstanceAbuseScreening:SSI‐AOD CognitiveAssessment:Mini‐MentalStatusExamination(MMSE),traumaticbrain injuryquestionnaire(TBIQ),RepeatableBatteryfortheAssessmentofNeuro‐ PsychologicalStatus(RBANS) Developmentalassessment:AgesandstagesQuestionnaires,Parents’Evaluationof DevelopmentalStatus(PEDS),DenverII,orotherstandardscreeningtool Interpersonalviolence:PosttraumaticDiagnosisScaleforUsewithExtremelyLow‐ income Women • Forensicevaluation:Ifstrongevidenceofchildabuse • Healthcaremaintenance:Cancerscreeningforadults,EPSDTforchildren 136 Planandmanagement Planofcare Basicneeds:Food,clothing,housingmaybehigherprioritiesthanhealthcare. Patientgoalsandpriorities:Immediate/long‐termhealthneeds,whatpatientwantsto addressfirst. Actionplan:Simplelanguage,portablepocketcard. Afterhours:Extendedclinichours,howtocontactmedicalproviderwhenclinicis closed. Safetyplan:Ifinterpersonalviolence/sexualabusesuspected;mandatoryreporting requirements. Emergencyplan:ContactingPCPbeforegoingtoER,locationofemergencyfacilities, preparationforevacuation. Adherenceplan:Clarificationofcareplan/patientfeedback;useofinterpreter,lay educatorifLEP,identificationofpotentialbarriers. Education,self‐management Patient/parentinstructions:Simplelanguage/illustrations,confirmcomprehension; pocketcardlistingimmunizations,chronicillnesses,medications. Prevention/riskreduction:Protectionfromcommunicablediseases,riskof delayed/interruptedtreatment. Behavioralchange:Individual/smallgroup/communityinterventions,motivational interviewing. Nutritioncounseling:Diet,dietarysupplements,foodchoices,powderedformulafor infants. Peersupport:Supportgroups,consumeradvocates. Educationofshelter/clinicstaff:specialproblems/needsofhomelesspeople. 137 Medications Simpleregimen:Lowpillcount,once‐dailydosingwherepossible;capsules/tabletsfor child>5yrs. Dispensing:Onsite;smallamountsatatimetopromotefollow‐up,decreaseriskof loss/theft/misuse;avoidwrittenprescriptionswhenpossible. Storage/access:Inclinic/shelters;ifnoaccesstorefrigeration,don’tprescribemeds thatrequireit. Patientassistance:Entitlementassistance,free/low‐costdrugsifreadilyavailablefor continueduse. Aidstoadherence:Harmreduction,outreach/casemanagement,directlyobserved therapy. Potentialformisuse:Inhalants,bronchodilators/spacers,painmedications,clonidine, needles. Sideeffects:Primaryreasonfornonadherence(diarrhea,frequenturination,nausea, disorientation). Analgesia/symptomatictreatment:Patientcontract,singleproviderforpain medicationrefills. Immunizations:Perstandardclinicalguidelines;influenza,pneumococcus,HAV,HBV, Tdforadults. Antibiotics:Standardliquidmeasurements,importanceofcompletingregimen,RSV prophylaxis. Dietarysupplements:Multivitaminswithminerals,nutritionalsupplementswithlower resalevalue. Managedcare:Prescribemedicationsthatdon’trequirepre‐authorization,assistance gettingRxfilled. Labmonitoring:Monitorpatientsonantipsychoticmedicationsformetabolic disorders. Associatedproblems,complications Noplacetoheal:Efficacyofmedicalrespite/recuperativecare,supportivehousing. 138 Fragmentedcare:multipleproviders.UseEMR,listprescribedmedsonwallet‐sized card. Maskedsymptoms/misdiagnosis:e.g.,weightloss,dementia,edema,lacticacidosis. Developmentaldiscrepancies:Focusonimmediateconcerns,notpossiblefuture consequences. Functionalimpairments:Documentmedicalandfunctionalimpairments,assistwith SSI/SSDIapplications,tailorplanofcaretopatientneedsandcapacities. Dualdiagnoses:Integratedtreatmentforconcurrentmentalillness/substanceuse disorders. Lossofchildcustody:Supportforparentofchildabusedbyothers,andforabused parent. Follow‐up Contactinformation:Phone,e‐mailforpatient/friend/family/casemanager. Medicalhome:Tocoordinate/promotecontinuityofhealthcare. Frequency:Morefrequentfollow‐up,incentives,nonjudgmentalcareregardlessof adherence. Drop‐insystem:Anticipate/accommodateunscheduledclinicvisits. Transportationassistance:Providecabfare/tokens,helpwithtransportationservices. Outreach/casemanagement:Connectwithcommunityoutreachprograms,HCH providers. Monitorschoolattendance:Addresshealth/developmentalproblemswith family/school. Peersupport:Clientadvocatetoaccompanypatienttoclinicalappointments, ambulatorysurgery. Referrals:Linkagewithspecialists,probonocare,providerssensitivetounderserved populations. 139 Modelofcare Servicedeliverydesign Integrated/interdisciplinary:coordinatedmedical,dental,andpsychosocialservices Multiplepointsofservice:Clinics,drop‐incenters,outreachsites;electronicmedical records,iffeasible. Flexibleservicesystem:Walk‐inspermitted,helpwithresolvingsystemsbarriers. Accesstomainstreamhealthsystem:Readyaccesstosecondary/tertiarycare. Accesstoconvalescentcare/supportedhousing:medical/respitecare,permanent housingwithsupportiveservicesforpatientswithserioushealthconditions. Outreachandengagement Outreachsites:Streets,soupkitchens,shelters,otherhomelessservicesites. Clinicalteam:Useofoutreachworkers,casemanagers,medicalproviderstopromote engagement. Therapeuticrelationship:Person‐centered,trauma‐informed,recovery‐oriented, nonjudgmentalcarebasedontrust,frequentencounters. Incentives:Topromoteengagement:food,drink,vouchers,hygieneproducts, subway/busfare(tokens). Standardofcare Clinicalstandards:scientificevidence,expertopinion,recommendationsof experiencedhomelessservicesproviders.Makeeliminationofhealthdisparitiesa clinicalgoal. Consumerinvolvement:inpeersupport,programgovernance,advocacy,research. Integratedserviceandadvocacy:toimproveserviceaccessforhomelesspeople, addressstructuralcausesofhomelessness,preventstaffburnout,andfacilitateclient recovery. AdditionalResources HomelessnessResourceCenter:http://www.nrchmi.samhsa.gov/default.aspx 140 HomelessinformationVermont(aprojectoftheU.S.DepartmentofHousingandUrban Development,thissitehaslinkstohelpandshelterhotlines,foodbanks,servicegroups, andawidevarietyofotherlocalresources: http://www.hud.gov/local/index.cfm?state=vt&topic=homeless NationalHealthCarefortheHomelessCouncil:http://www.nhchc.org/index.html VermontHousingAwarenessCampaign:http://www.housingawareness.org/index.htm 141 References 1. ThornburghN.Defining'HomelessnessDown'.TimeU.S.A.2008. 2. PeuquetS.ThePersistenceofHomelessnessandtheInvisibleHomeless.2004; http://www.housingforall.org/rop0304%20homelessness.pdf.AccessedApril, 2012. 3. CatonCL,DominguezB,SchanzerB,etal.Riskfactorsforlong‐termhomelessness: findingsfromalongitudinalstudyoffirst‐timehomelesssingleadults.AmJPublic Health.Oct2005;95(10):1753‐1759. 4. NationalCoalitionfortheHomeless.WhyArePeopleHomeless.2009; http://www.nationalhomeless.org/factsheets/why.html.AccessedApril,2012. 5. WrightNM,TompkinsCN.Howcanhealthserviceseffectivelymeetthehealthneeds ofhomelesspeople?BrJGenPract.Apr2006;56(525):286‐293. 6. StatewideHomelessReportJan.27,2010;.http://www.helpingtohouse.org. AccessedJanuary,2013. 7. VermontHousingFinanceAgency.FamilyHomelessnessinVermont.2008; http://www.time.com/time/nation/article/0,8599,1827876,00.html.Accessed April,2012. 8. HwangSW.Homelessnessandhealth.CMAJ.Jan232001;164(2):229‐233. 9. BoninE,BrehoveT,CarlsonC,etal.AdaptingYourPractice:General RecommendationsfortheCareofHomelessPatients.2010; http://www.nhchc.org/wp‐content/uploads/2011/09/GenRecsHomeless2010.pdf. AccessedApril,2012. 10. NationalCoalitionfortheHomeless.HealthCareandHomelessness.2007; http://www.nationalhomeless.org/factsheets/health.html.AccessedApril,2012. 11. HwangSW,TolomiczenkoG,KouyoumdjianFG,GarnerRE.Interventionstoimprove thehealthofthehomeless:asystematicreview.AmJPrevMed.Nov 2005;29(4):311‐319. 12. KarrC,KlineS.Homelesschildren:whateveryclinicianshouldknow.PediatrRev. Jul2004;25(7):235‐241. 13. ShekarS.HomelessandElderly:UnderstandingtheSpecialNeedsofElderlyPersons WhoAreHomeless.Washington,DC:BureauofPrimaryHealthCare,U.S. DepartmentofHealthandHumanServices;2003. 142 LatinoMigrantFarmWorkers Background PopulationinVermont.TheVermontAgencyof Agricultureestimatesthatasmanyas3,000Latino migrantfarmworkers(LMFWs)liveandworkin Vermont.Othergroupsbelievethetruenumberis closerto1,500,perhapsless.Byanyestimate,itis surethatthispopulationhasgrownsignificantly overthelasttenyears.ManyoftheseworkerscomefromsouthernMexico,fromsmall townsintheareasofChiapas,Guerrero,andOaxaca.Therearealsootherswhocomefrom GuatemalaandbiggercitiesinMexico. Language.NearlyalloftheworkersspeakSpanishastheirprimarylanguage.Aportionof theworkers,especiallythosefromruralareasinChiapasorGuatemala,mayspeakanative dialectsuchasMamastheirprimarylanguage.Suchdialectsusuallyderivefromfrom ancientMayanlanguagesandareunwritten.MosthavenothingincommonwithSpanish andareunlikelytobeavailableinanytranslationprogram.LMFWsthatspeakadialectas theirfirstlanguagearelikelytoalsobeproficientinSpanish,butafew,especiallywomen (whoaremuchlesslikelytoreceiveeducationinruralareas),mayonlyspeaklimited Spanish. ApercentageofLMFWswillalsohavesomeabilitytospeakorunderstandEnglish, especiallyiftheyhavebeenintheUnitedStatesforasignificantamountoftime. Religion.Accordingtothemostrecentcensusdata,greaterthan90%oftheMexicanand GuatemalanpopulationsidentifytheirreligionasCatholicorotherChristian.SomeLMFWs fromthemostruralareasmayalsohavearichtapestryofbeliefsthatcombineshamanistic andspiritualisticbeliefswithChristianity.Althoughtheymaynotcomeupnaturallyina history,thesebeliefshavetheabilitytoimpacttheirperceptionofhealthcareandillness. Family.WhilemostLMFWsaremale,therearesomefemaleworkersandsomecouples whocametoVermonttogetherandhaveevenhadchildreninVermont.Manyofthe workershaveaspouseand/orchildreninMexicowhomtheyaresupporting.Some workersarealsosupportingothersinthecommunitybackhome.Generally,theymaintain contactwiththeirfamiliesbackhomethroughcellphonesandcallingcards. Education.TheeducationlevelofLMFWsalsovariesgreatlybyindividual.Thosefrom ruralareasinMexicoandGuatemalaoftenleaveschoolandbeginworkingafterorduring elementaryschool.SomemayevenhavearrivedintheUnitedStatesasteenagers.Many areliterate,butitisnotsafetoassumethatanysingleLMFWwillbeabletoreadand understandmedicalliteraturegiventothem. Diet.Atsomefarms,theworkersareabletodotheirownshopping,butinmanyfarmsthey arecompletelydependentonthefarmownersforanyshoppingneeds,notjustgroceries. 143 Somefactorstoconsiderwhenassessingaspecificworker’sdietcouldincludewhobuys theworker’sgroceries,theworker’scountryoforigin,andhowlongtheworkerhasbeenin theUnitedStates. Legalissues.Immigrationstatusisbasedonacomplexsetoffederalregulations.Asking abouttheimmigrationstatusofapatientshouldbeavoided.Havingdarkerskinand speakingonlySpanishdoesnotmakeanyoneanundocumentedimmigrant.Afewstates haverecentlyintroducedbillsthatmaysubjecthealthcareproviderstoprosecutionfor aidingundocumentedworkers.Vermontisnotoneofthosestates.Additionalquestionson thistopiccanbedirectedtotheVermontHumanRightsCommissionat802‐828‐2482or human.rights@state.vt.us. HealthCare Priorhealthcareexperience.LMFWshavehadvariedexperienceswithhealthcarein theirhomecountries,andinotherpartsoftheUnitedStates.Mexico,Guatemala,andmost otherCentralAmericancountriesofferauniversalhealthcaresystem,wherecareisfree butvariesgreatlyinavailabilitybetweenareas.Themostprevalentmodelforambulatory careinmostpartsofMexicoandGuatemalaarewalk‐inconsultations,wherepatients arrivewithoutanappointmentandwaittobeseen.Thestate‐runsystemiscomplemented byapatchworkofprivatehealthservicesthatcharge.LMFWsfromurbanareasmayhave hadeasyaccesstolow‐costandreliablehealthcareintheirhomecountries,whileothers mayhavelivedaday’sjourneyfromthenearesthospital.Forexample,someworkersare accustomedtohavingtheirchildrendeliveredintheirownhomes,oftenbyfamily members,whileotherswouldneverthinkofhavingababyanywherebutinahospital. Barrierstoseekingcare.LMFWsoftenliveinisolation.Somedonotleavetheirresidence excepttowalktothemilkingbarnforwork.Thisisprimarilybecauseoffearofbeingseen anddeported.Anythingtheyneedisbroughttothematthefarm,usuallybytheir employer.Thisisparticularlytrueclosertothenorthernborderofthestatewhere immigrationofficialshaveamuchstrongerpresence.InsomeareasofFranklinCounty workersseeimmigrationvehiclesdrivebytheirfarmsregularly.Thisclimateoffearisa majorbarriertohealthcareaccess.Othermajorbarriersincludelanguagedifficulties,fear ofhighcosts,andlackoftransportation.Dueinparttothesebarriersmostworkersarenot willingtovisitahealthclinicuntiltheyareinsignificantpainorareunabletowork.Many workerswouldrathercontinueworkingthantaketheneededresttoresolvepain.Other workersstatethatiftheybecameillorinjuredenoughthattheycouldnolongerwork, they’dprefertoreturntotheirhomecountryratherthanseekcareintheUnitedStates; onereasonforthisisthatworkerswouldratherbenearfamilytobenursedtohealthif theywillbeunabletoworkforanextendedperiodoftime. SpecifichealthconcernsintheLMFWpopulation Somecommonproblemsexperiencedarerepetitivemovementinjuries,dentalproblems, dermatologicalconditions,trauma,andgastrointestinalissues. 144 Specificstepsforhealthcareproviders Minimizethenumberofrequiredvisitstotheclinic.Especiallyinthenorthernpart ofthestate,itisariskforLMFWstoleavehomeandgooutintothepublic.In addition,LMFWsareoftendriventoappointmentsbybusyfarmownersor volunteerswhoaregivingfreelyoftheirtime. Ifpossible,inviteLMFWsintoaconsultationroomsoonaftertheyarrive.LMFWs mayfeeluncomfortablesittinginawaitingroomforextendedperiodsoftime, especiallyinareaswhereimmigrationofficialsmakeupasignificantportionofthe localpopulationandmaybeseatedinthesamewaitingroom. DiscusstheextenttowhichanLMFWwishestosharehealthcareinformationwith thefarmowneroremployer.Theprioritymustbetoclearlycommunicateall aspectsofcarewiththepatient,howeveritmaybebeneficialtoaskforpermission tosharesomeinformationwiththeiremployer,whomaybeabletoprovide assistancewithfollow‐upcare,suchasgettingmedications,scheduling appointments,andprovidingtransportation. Ifthecostofmedicalcareiswithintheirmeans,LMFWswillusuallyprefertopayat thetimeofservice,oftenwithcash.Billingforservicescanoftenleadto complications,asworkersmaynotreliablyopenmailormaybelievethattheyhave alreadysettledthecostoftheircare.Ifyoucanapplydiscountsandestablishafinal feeatthetimeofthevisit,itmayreducethesecomplications. Communication.AlthoughthistraitisnotuniquetoLatinculture,manyLMFWshavea strongdesiretopromotepositiveinteractionsandavoiddiscomfortordisharmonyfor anyonetheyinteractwith.Theymayhaveatendencytogivetheanswertheythinkis expectedinsteadoftheirownanswer.Thiscangreatlyaffectcommunicationintheclinic. IfanLMFWisaskeditifisacceptabletouseawrittentranslationservicerather thanavideoorin‐persontranslator,theymayassenteveniftheyarenot comfortablewiththeservice. IfanLMFWgetsthesensethatusinginterpreterservicesisinconvenientforthe clinicorprovider,heorshemaybelesslikelytoutilizetheserviceandleaveout importantinformation. LMFWsmaydiscloseonlyasinglechiefcomplaint,eveniftheyhavemultiple ailments.Direct,sequentialquestioningandcarefulprobingmayberequiredfor themtofullydivulgehealthissuesorpasthistory. Verifyunderstandingusingmorethanyesornoquestions. 145 Interpretationserviceshouldbemadeavailablenotonlyintheconsultation,butat thereceptiondesk,especiallywhendiscussinginstructionsforfillingprescriptions, payment,futureappointments,orpendinglabresults. Anyclinicthatusesphonetranslationservicesshouldbetrainedinusingthe translationservicewhensomeonecallstheclinicdirectlyspeakingSpanish. KnowthelocationoftheSpanishpaperworkinyourofficeanduseitwithSpanish speakers. Usingafamilymember,friend,ornon‐fluentfarmownerasaninterpreterwhen professionalresourcesareavailableshouldbeavoided.Theinformationprovided vianon‐professionaltranslationmaybebiasedorincomplete. EvenifapatientappearsnottospeakEnglish,youshouldneverassumethathe/she cannotunderstandanycommentsyoumakeinEnglish. EvenifaLMWFappearstobeproficientconversinginEnglish,youshouldalways encouragethemtouseaninterpreter,astheystillmaybefarmorecomfortable providingahistoryinSpanish. Additionalresources CommunityHealthPharmacy:ThisisagoodoptionforLMFWswhoarenervousabout leavingthefarmtopickupprescriptions.Itisa340Breduced‐costpharmacythatcanfill prescriptionswrittenbyfederally‐qualifiedhealthcarecenters;theycanmailthe medicationsdirectlytothefarm.1‐888‐669‐9017,158BrentwoodDrive,Suite#7, Colchester,VT05446www.communityhealthpharmacy.com Thepharmacydoesnotofferaphone‐linetranslationservice,butmustcollectbasic informationaboutthepatientinordertofillaprescription.Itmaybemost appropriatetocallthepharmacywhenthepatientandtranslatorarestillpresent. Thepharmacyacceptsbutdoesnotrequireacreditcard;theywillacceptpayment inmoneyorders,checks,orcash. AllthepackageinsertsdistributedwithprescriptionsisavailableinSpanish. Everythingisautomaticallytranslatedexceptforspecificinstructionswrittenin Englishbytheprovider. PriceChoppergrocerystores:Diabetesmedicationsandmanystandardantibioticsare availablefreeofchargeatpharmaciesinPriceChoppergrocerystores. English‐SpanishOccupationalandHealthDictionary: http://www.cbs.state.or.us/osha/pdf/dictionary/english‐spanish.pdf 146 NativeAmericans Background Definition.AmericanIndiansand/orAlaskanNativesare descendantsoftheoriginal,pre‐EuropeaninhabitantsofNorth, Central,andSouthAmericawhomaintainaffiliationswithoneofmanypre‐European tribes.1,2MajorNativeAmericantribesinNorthAmericatodayincludeCherokee,Navajo, Sioux,andEskimo.3 Inthischapter,theterm“NativeAmerican”willbeusedtorefertoallAmericanIndiansor AlaskanNatives,althoughreadersshouldbeawarethatthisisalargeandheterogeneous groupwithsignificantregionaldifferencesinculture,socioeconomicstatus,etc. History.4ThefirstAmericansarrivedintheAmericasfromAsiasome12,000yearsagoby wayofalandbridgethatspannedtheBeringStraitandconnectedpresent‐daySiberiawith Alaska.Overmanythousandsofyears,thesesettlersfannedoutacrossNorthAmerica, shiftedfromalargelynomadictoasettledexistence,learnedtodomesticateplantsand animals,andbuiltupcomplexsocieties. AlthoughEuropeanslikelyhadoccasionalcontactwithNativeAmericanspriorto1492, Columbus’landinginthatyearwasthemosthistorically‐importantfirstpointofcontact betweenthetwogroups.FollowingColumbus’arrival,Europeansspreadoutacrossthe continent;overthenextseveralhundredyears,theyestablisheddominancebyforcein NorthAmerica,therebyendingtheNativeAmericanwayoflife.Diseasewasonemethodby whichEuropeanswereabletoovercomeNativeAmericantribes:smallpox,measles, plague,andotherdiseasesaccompaniedEuropeanstotheNewWorldandkilledscoresof NativeAmericans,whohadnoimmunitytothesediseases.5Someestimatesputthepre‐ EuropeanNativeAmericanpopulationofNorthAmericaat50millionpeople;in2011,it was6.2million.1 InteractionsbetweenNativeAmericansandtheU.S.governmentintheperiodbetweenthe Americanrevolutionarywar(1775‐1783)andtheendofthe19thcenturywere characterizedprimarilybywestwardexpansionofAmericansandforceddisplacementof NativeAmericansontoreservationlandthatwasoftenquitedistantfromancestrallands. Atthistime,threepivotalSupremeCourtdecisionsknownastheMarshallTrilogywere passed.Thefirstoftheseestablishedthat,althoughNativeAmericansweretherightful occupantsoftheirland,theU.S.federalgovernmentheldtitletothatland.Thesecond establishedthattheUnitedStateshasaresponsibilitytoprovidecertainbenefitsforNative Americans.Thethirdestablishedthatthefederalgovernment,andnotthestates,hadfinal legalauthorityoverNativeAmericantribes.6ThesedecisionshaveshapedUnitedStates policytowardsNativeAmericanseversince.TheIndianHealthService,agovernment agencythatprovideshealthcaretoNativeAmericans,isoneresult. Demographics.In2008,4.9millionNativeAmericanslivedintheUnitedStates,makingup about1%ofthetotalAmericanpopulation.Approximately1.9millionofthemlivedon 147 reservations.1AlthoughtheNativeAmericanpopulationincludesmembersof562 federally‐recognizedand100state‐recognizedtribes,thelargesttribesin2000werethe Cherokee,Chippewa,Navajo,Sioux,andEskimo.3 In2010,NativeAmericansmadeup.9%ofVermont’spopulation.ManyofVermont’s NativeAmericansareAbenaki;however,NativeAmericanswithothertribalaffiliationsdo livehere.Whiletherearenofederally‐recognizedNativeAmericantribesinVermont,2in 2012theStateofVermontofficiallyrecognizedfourtribesofAbenaki. Culture.NativeAmericansarealargeandheterogeneousgroupandeachtribehasitsown uniqueculture,thereforeafulldiscussionofNativeAmericancultureisbeyondthescope ofthischapter.However,afewpointsmaybemade.Forexample,manyNativeAmerican traditionsteachthathumansareintimatelyconnectedwitheachother,withnature,and withaCreator.7Patienceandstoicismarevalued.8NativeAmericanmedicineinvolvesa significantspiritualcomponent,andoftentheentirecommunitytakespartinthehealing process.7ManyNativeAmericansmaybe(withgoodreason,giventheirhistoryofbroken treatiesandforceddisplacementatthehandsoftheUnitedStatesgovernment)distrustful ofauthority.NativeAmericansmaybereticentinconversationandslowtosharepersonal information—inparticular,sexualinformation—withoutagooddegreeoftrustestablished withthehealthcarepractitioner.FamilyandextendedfamilyplayalargeroleinNative Americans’lives.Finally,manyNativeAmericantraditionsemphasizelivinginthepresent, withlessfocusonthefuture.ForamorecomprehensiveoverviewofNativeAmerican culture,seeresourcesattheendofthischapter. VermontAbenakiNativeAmericansaredescendentsoftheWesternAbenakitribewhich historicallyoccupiedpartsofVermont,NewYork,Maine,andQuebec.Oraltraditionisvery importantinAbenakiculture.9Decisionsaremadebyconsensus.10 Healthcare Ingeneral,thehealthofNativeAmericanscomparedtothatofthegeneralpopulationis quitepoor.Aswithotherminoritypopulations,NativeAmericanhealthcareismost usefullyframedinthecontextofhealthdisparitiesbetweenNativeAmericanandwhite Americanpopulations. SpecifichealthconcernsintheNativeAmericanpopulation TheUnitedStatesCommissiononCivilRights5statesthatin2002,NativeAmericanswere “770%morelikelytodiefromalcoholism,650%morelikelytodiefromtuberculosis, 420%morelikelytodiefromdiabetes,280%morelikelytodiefromaccidents,and52% morelikelytodiefrompneumoniaorinfluenzathantherestofthe[UnitedStates] population,includingotherminoritypopulations.”NativeAmericanswerealsomorelikely tosufferfrommentalhealthproblems,includingsubstanceabuse(alcohol,marijuana,and cocaine),depression,anxiety,violence,andsuicide,forwhichtherateamongstNative Americansis190%therateoftheUnitedStatespopulation.5Ratesofmetabolicsyndrome andcardiovasculardiseasearealsoextremelyhighinthispopulation,asareHIV,liver disease,teenagepregnancy,andsuddeninfantdeathsyndrome.Overall,theinfant 148 mortalityrateamongNativeAmericansis1.6timesthatofnon‐Hispanicwhite Americans.11 TheUnitedStatesCommissiononCivilRights5determinedthatthesedisparitieshavebeen causedbyseveralintersectingfactors. RacialbiasbyhealthcareworkersleadstosubstandardcareforNativeAmericans. Lackofculturallyandlinguistically‐competentdeliveryofhealthcareservices. Lowsocioeconomicstatusasaresultofdisproportionatelyhighpovertyandlow educationinNativeAmericanpopulations. Poorlifestylechoices‐obesity,substanceabuse,andinactivityarecommoninNative Americanpopulations. AccesstohealthcareispoorforNativeAmericans:healthcarefacilitiestendtobe locatedfarawayfromwhereNativeAmericanslive;waittimesarelong;facilities areoutdated;healthcarepractitionerturnoverishigh(andthereforepatient continuityislow);andNativeAmericanshavelimitedaccesstoMedicareor Medicaid. Specificstepsforhealthcareproviders Appreciateeachpatient’sculturalidentityandallowroomfortraditionalmedical practicestobeincorporatedintothetreatmentplan. AppreciatethatdirectcommunicationisnottypicalofmanyNativeAmerican cultures,butaslowpacetoconversation,andlistening,areveryimportant. Returnpowertoyourpatientbyinvolvingtheminthedecision‐makingprocess wherepossible. FocusoncommunitybyputtingyourpatientintouchwithNativeAmericanhealth supportgroups. Tailoryourdeliveryofinformationtotheeducationallevelofyourpatient. Developanddeliverculturally‐appropriatehealtheducationmaterialsconcerning thingslikesubstanceabuse,exercise,depression,etc. Focusonpreventativecare. Additionalresources AmericanDiabetesAssociation: www.diabetes.org/communityprograms‐and‐localevents/nativeamericans.jsp 149 IndianHealthServices:http://www.ihs.gov/index.cfm OfficeofMinorityHealthAmericanIndian/AlaskanNativeProfile: http://www.omhrc.gov/templates/browse.aspx?lvl=2&lvlID=52 AmericanIndianHealth:http://americanindianhealth.nlm.nih.gov/ AprojectoftheNationalLibraryofMedicine,thissitehascompiledinformationonhealth disparities,statistics,programs,andtraditionalhealthpracticesofNativeAmericans. HealthofAmericanIndianorAlaskaNativePopulation: http://www.cdc.gov/nchs/fastats/indfacts.htm 150 References 1. OfficeofMinorityHealth.AmericanIndian/AlaskaNativeProfile. http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=3&lvlid=26.Accessed April,2012. 2. BureauofIndianAffairs.WhoisanAmericanIndianorAlaskaNative? http://www.bia.gov/FAQs/index.htm.AccessedApril,2021. 3. OgunwoleS.WethePeople:AmericanIndiansandAlaskaNativesintheUnited States:ACensus2000SpecialReport:UnitedStatesCensusBureau;2006. 4. NationalParkService.OtherMigrationTheories. http://www.nps.gov/bela/historyculture/other‐migration‐theories.htm.Accessed April,2012. 5. UnitedStatesCommissiononCivilRights.BrokenPromises:EvaluatingtheNative AmericanHealthCareSystem.Washington,DC:UnitedStatesCommissiononCivil Rights;2004. 6. AmericanIndianPolicyCenter.BriefHistoryofU.S.‐TribalRelations. http://www.americanindianpolicycenter.org/projects/history.html.AccessedApril, 2012. 7. HendrixLR.HealthandHealthCareofAmericanIndianandAlaskaNativeElders. EthnogeriatricCurriculumModule.SanFrancisco,CA:StanfordGeriatricEducation Center. 8. PottsC.CulturallyResponsiveCurriculumforSecondarySchools.Olympia,WA: EvergreenStateCollege;2009. 9. BruchacJ.TheAbenakiPerspectiveonStorytelling. http://www.abenakination.org/stories.html.AccessedApril,2012. 10. COWASSNorthAmericaInc.TheConsensualDecision‐makingProcess. http://www.cowasuck.org/lifestyle/consent2.cfm.AccessedApril,2012. 11. OfficeofMinorityHealth.InfantMortalityandAmericanIndians/AlaskaNatives. http://minorityhealth.hhs.gov/templates/content.aspx?ID=3038.AccessedApril, 2012. 151 Thispageintentionallyleft blank. 152 Women Inthischapterwomenaretreatedasahomogenousgroup; differencesinhealthresultingfromrace,ethnicity,country‐ of‐origin,income,andeducationarelargelyignored. However,practitionersshouldbeawarethatthese differencesexistandthattheymayaffectboththehealthof awomanandthatwoman’sinteractionwiththehealthcare establishment.Practitionersshouldrefertospecific populationchapterstosupplementtheinformationinthis chapterwhenappropriate. Itshouldbenotedthatwomenfarebetterthanmeninsomemeasuresofhealth,suchas longevity(intheUnitedStates,theaveragelifeexpectancyatbirthis5yearslongerfor womenthanitisformen).Thissection,however,focusesonhealthissuesthatare disadvantageousforwomenandonthemanyhealthcareneedsthatareuniquetowomen. Forarecent,comprehensivereviewofwomen’shealthintheUnitedStates,seetheOffice ofWoman’sHealthLiteratureReviewonEffectiveSex‐andGender‐BasedSystems/Models ofCare(2007),fromwhichmuchoftheinformationinthischapteriscompiled: http://www.genderinscience.org/downloads/BM1_references/Brittle%20and%20Bird%2 02007.pdf Background Inrecentdecades,atremendousamountofattentionhasbeenpaidtowomen'shealthby theAmericanmedicalestablishment.Thisisaresultoftherecognitionthatwomenand menhavedifferenthealthcareneedsanddifferentexperiencesofthehealthcaresystem,a recognitionthatwaslackingformuchofthe20thcentury.1Inadditiontothefactthat biologicaldifferencesbetweenwomenandmencontributetouniquediseasesandunique patternsofdiseaseinwomen(OfficeofWomen’sHealth,2007),issuesofgenderinequality havedirectbearingonwomen’saccessto,andexperienceof,thehealthcaresystemaswell astheprevalenceofsomediseasesinwomen.1 Demographics.In2010,womenmadeup50.8%ofthetotalUSpopulation,and50.7%of theVermontpopulation.2 HealthCare Disparities.Althoughthewomen’srightsmovementhasmadegreatstridesinadvancing thecauseofgenderequality,men’sandwomen’sexperienceswiththeAmericanhealth caresystemarenotequal.Inits2007report,1LiteratureReviewonEffectiveSex‐and Gender‐basedSystems/ModelsofCare,theUnitedStatesDepartmentofHealthandHuman Services,OfficeforWomen’sHealthnotedthefollowingdisparities. Availabletimetoaccesshealthcare.Womenaremorelikelythanmentobecaregivers (9%ofwomencomparedto4%ofmen).Thismakeswomenmorelikelytobetheprimary 153 medicaldecision‐makersinthefamily,butitalsoreducestheamountoftimewomenhave availabletoseekhealthcareforthemselves. Costofaccessinghealthcare.Thecostofaccessinghealthcareisasignificantburdenfor manywomencomparedtomen.Forexample,womenoftenearnlessthanmen.Inaddition, ifmarried,womenarelesslikelytohaveinsurancecoverageintheirownnames.This makesthemvulnerabletolossofcoverageduetodeath,divorce,or,iftheyarecoveredby theirhusband'semployer‐sponsoredhealthcareplan,achangeinhisemploymentstatus. Thecostofcaringfordependentchildrenandeldersfurtherexacerbatestheburdenof cost.Costcanalsodecreasethequalityofhealthcarewomenreceive,forexamplewomen aremorelikelythanmentoskipprescribeddosesofnecessarymedicationsduetocost constraints. Continuityofhealthcare.Womenaremorelikelythanmentoreceiveeitherincomplete orfragmentedprimarycare.Thisisaresultofwomen'swidespreaduseofgynecologistsas eithertheirprimarycareproviderorasoneprovideralongsideaninternistorfamily practitioner.Intheformercase,womenwhoseeonlygynecologistsmayreceivebetter specializedcare,butpoorerprimarycare,whileinthelattercase,thefragmentationmay resultinbetterprimarycareservices,butleadtoincreasedcostsintermsoftimeand dollarsspent. Themedicalinterview.Womenexperiencethemedicalinterviewdifferentlythanmen,3 whichcanleadtoinferiormedicalcare.Womenhavefrequentlybeensocializedtobelieve thatcertainbodilyfunctionsshouldbekeptprivate;asaresulttheydonotreportsome symptomsasfrequentlyasmen.Forexample,womenarelesslikelytoreportbowel symptoms,makingtreatmentofirritableboweldiseasedifficult. Otherexamples.Womenmayreceivelesspreventativehealthcounselingthanmen,less accesstohigh‐techtreatments,fewerscreeningsforcoloncancer,andlessaggressiveHIV treatment. Specifichealthconcernsofwomen TheCDCreportsthatin2008,themostrecentyearforwhichdataarecurrentlyavailable, thetoptenleadingcausesofdeathforAmericanfemaleswere: 1. heartdisease 2. cancer 3. stroke 4. chroniclowerrespiratorydisease 5. Alzheimer’sdisease 6. unintentionalinjuries 7. diabetes 8. influenzaandpneumonia 9. kidneydisease 10. septicemia 154 Thefollowingaremorecommoninwomenthaninmen,oroccurexclusivelyinwomen1: urinarytractinfectionsandsexually‐transmitteddiseases(whichmayleadtopelvic inflammatorydiseaseand/orapotentiallyfatalectopicpregnancy) vaginitis,uterinefibroids,ovariancysts,andendometriosis chronicpainand/orchronicfatiguesyndrome adversedrugreactions iron‐deficiencyanemia interstitialcystitis insomnia domesticandsexualviolence migraines incontinence cardiovasculardisease;inaddition,womenmayshowadecreasedawarenessof theirriskforcardiovasculardisease osteoporosis autoimmunediseasessuchaslupus,rheumatoidarthritis,andmultiplesclerosis4 certainkindsofcancer,includingendometrial,uterine,cervical,breast,andthyroid cancer Alzheimer’sdisease(AD): ‐ womenaremorelikelythanmentohaveseverecognitiveimpairment ‐ inthepsychiatricmanifestationofAD,womenaremorelikelytohave depressionandmultiplepsychiatricproblems eatingdisorderssuchasanorexiaorbulimianervosa post‐partumdepressionaftergivingbirth Inaddition,practitionersshouldbeawareofthefollowing: Womenmetabolizedrugsdifferentlythanmen.Forexample,variousisoformsof cytochromeP450s,amajorclassofmetabolically‐activeliverenzymes,are differentiallyexpressedbetweenwomenandmen. Womenalsometabolizedrugsdifferentlyindifferentstagesoftheirlife,forexample dosesofantidepressantmedicationmustoftenbeincreasedtoremaineffectivein pregnantwomen.5 Womenwhoplantohavechildrenshouldbeawareofpossiblemercurytoxicity causedbyeatingmercury‐ladenfish(EPA,2008). 155 Specificstepsforhealthcareproviders1,3 Hireadiversestaff,andensurethatwomenholdpositionsofleadership. Co‐sponsorwomen’shealthinitiativesinyourcommunity. Haveinformationaboutwomen’ssupportorganizationsavailable. Focusonpatienteducation,andspecifically,onheartdisease. Askfemalepatientsiftheyhaveexperienceddomesticorsexualviolence.Ifthey have,makeaccommodationstoincreasethepatient’scomfortindiscussingthese issues,suchasofferingtohaveafemalestaffmemberpresentorhavingafemale staffmembercontinuetheinterview. Taketimetodevelopatrustingrelationshipwithyourpatients;don’tjustrushthem inandoutoftheexamroom. AdditionalResources U.S.DepartmentofHealthandHumanServices:www.4women.gov OurBodies,Ourselves(acomprehensivesitewithlinkstoinformationonmanytopicsin women’shealth):http://www.ourbodiesourselves.org/publications/obos.asp Womenshealth.gov(agovernmentsitewithmanyfactsheets,linkstoclinicaltrials, statistics,healthinitiatives,andothers):http://www.womenshealth.gov/ Women’sHealthattheNationalInstitutesofHealth: http://health.nih.gov/category/WomensHealth VermontNetworkAgainstDomesticandSexualViolence:http://www.vtnetwork.org/ 156 References 1. BrittleC,BirdC.LiteratureReviewonEffectiveSex‐andGender‐based Systems/ModelsofCare.Washington,DC:UnitedStatesDepartmentofHealthand HumanServices,OfficeofWomen'sHealth;January30,2007. 2. UnitedStatesCensusBureau.StateandCountyQuickFacts.Washington,DC:United StatesCensusBureau;2012. 3. HouleC,HarwoodE,WatkinsA,BaumKD.WhatWomenWantFromTheir Physicians:AQualitativeAnalysis.JournalofWomen'sHealth.May23 2007;16(4):543‐550. 4. FairweatherD,RoseNR.Womenandautoimmunediseases.EmergInfectDis.Nov 2004;10(11):2005‐2011. 5. AndersonGD.Pregnancy‐inducedchangesinpharmacokinetics:amechanistic‐ basedapproach.ClinPharmacokinet.2005;44(10):989‐1008. 157 Thispageintentionallyleft blank. 158 AppendixA ExcerptedfromtheVermontDepartmentofHealth’s2010reportTheHealthDisparitiesof Vermonters.Theentirereportcanbefoundat http://healthvermont.gov/research/documents/VTDisparitiesRpt2010.pdf 159 160 161 162 163 164 165 166 167 168 169 170 171 172 173