Standard and active preventive care
advertisement

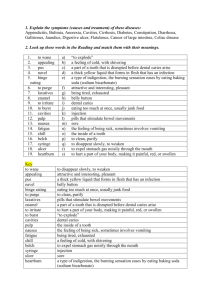
Journal of Minimum Intervention in Dentistry J Minim Interv Dent 2011; 4 (2) According to the patient susceptibility, two types of preventive care are available: standard and active preventive care. Preventive standard care is indicated for patient with low susceptibility for caries occurrence, in order to reduce the risk for recurrence of caries. Standard preventive care includes daily oral hygiene (tooth brushing, the use of fluoride toothpaste and flossing), dietary advice and patient motivation. The patient is instructed to brush at least twice a day with fluoride toothpaste and clean between teeth once a day with floss or another interdental cleaner. Low sugar diet has to be advised without frequent snacks between meals. Regular dental visits are recommended to the patient as well. This type of care can be compared to conventional maintenance therapy for patients who have not developed any new caries lesions in the past 2 or 3 years. For individuals highly susceptible to caries, active care is recommended. Active preventive care includes the standard care regime with addition of professional decontamination, remineralisation, management of aetiological factors and the use of fissure sealants. Standard and active preventive care 1 1 Miletic I , Baraba A . 1 Department of Endodontics and Restorative Dentistry, School of Dental Medicine, University of Zagreb, Gunduliceva 5, 10 000 Zagreb, Croatia According to the patient susceptibility, two types of preventive care are available: standard and active preventive care. Preventive standard care is indicated for patient with low susceptibility for caries occurrence, in order to reduce the risk for recurrence of caries. This type of care could be compared to conventional maintenance therapy for patients who have not developed any new caries lesions in the past 2 or 3 years. For individuals highly susceptible to caries, active care is recommended. Active preventive care includes the standard care regime with addition of professional decontamination, remineralisation, management of aetiological factors and the use of fissure sealants. Decontamination is used to rebalance the oral microflora. Few actions of decontamination are available: professional mechanical tooth cleaning (PMTC), Chlorhexidine and stabilizing restorations. Remineralisation is indicated for incipient, non-cavitated lesions with a use of fluorides or more recently introduced casein derivates. When Casein PhosphopeptideAmorphous Calcium Phosphate (CPP-ACP) or Casein Phosphopeptide-Amorphous Calcium Fluoride Phosphate (CPP-ACFP) is applied in Decontamination is used to rebalance the oral microflora. Few actions of decontamination are available: professional mechanical tooth cleaning (PMTC), Chlorhexidine and stabilizing restorations. PMTC involves the removal of dental plaque using an ultrasonic scaler and a fluoride prophypaste with a polishing brush. PMTC is the most effective method for plaque removal; it suppresses dental caries and reduces salivary levels of mutans streptococci. Chlorhexidine is a topical antimicrobial agent, effective in the elimination of mutans streptococci in the oral cavity [1,2]. Periodic use of Chlorhexidine is helpful for patients with Periodontitis or those with high salivary levels of cariogenic bacteria. Application of Chlorhexidine is recommended if the test for S. mutans (e.g. GC Saliva-Check SM) is found positive, indicating high number of bacteria in saliva. Decontamination is performed with 0.12% Chlorhexidine mouthwash or by professional application of chlorhexidine gel directly into the pockets, providing a high concentration of the agent. the oral environment, it will bind to biofilms, plaque, bacteria, hydroxylapatite (tooth structure) and soft tissue localising bioavailable calcium, phosphate and fluoride ions. Therapy of aetiological factors can also be Stabilizing restorations are indicated for patients highly susceptible to caries and are placed after excavation of caries using Atraumatic Restorative Treatment (ART) (Figure 1). . Figure 1. 17-year-old female patient with extensive caries lesions, highly susceptible to caries (Image: Ivana Miletic). managed by some simple advice on oral hygiene, diet or saliva flow stimulation, to help rebalance the oral environment. Since dental caries is a bacteria-dependent, multifactorial disease, preventive measures such as sealants, can be implemented once patients susceptible to caries are identified. Sealants act as a barrier, protecting tooth enamel from plaque, bacteria and acid and preventing pit and fissure caries. Correspondence address: Professor Ivana Miletic DDS, PhD Department of Endodontics and Dentistry, School of Dental Medicine, University of Zagreb, Gunduliceva 5, 10 000 Zagreb, Croatia Restorative 20 Journal of Minimum Intervention in Dentistry J Minim Interv Dent 2011; 4 (2) This technique is based on the partial removal of caries tissue, using only manual cutting instruments (Figure 2). Remineralisation is indicated for incipient, noncavitated lesions with a use of fluorides or more recently introduced casein derivates. Casein Phosphopeptide-Amorphous Calcium Phosphate TM (CPP-ACP, Recladent ), (e.g. GC Tooth Mousse) has a capacity to deliver higher amounts of phosphate and calcium ions on the tooth surface. Casein Phosphopeptide-Amorphous Calcium Fluoride Phosphate (CPP-ACFP), (e.g. GC MI Plus Paste) contains fluoride ions beside calcium and phosphate. When placed on the tooth surface, TM Recladent interacts with hydrogen ions and forms the neutral ion species calcium hydrogen phosphate, which can enter the tooth and produce the enamel mineral. When CPP-ACP or CPP-ACFP is applied in the oral environment, it will bind to biofilms, plaque, bacteria, hydroxylapatite (tooth structure) and soft tissue providing bio-available calcium, phosphate and fluoride ions [7]. CPP-ACFP is contraindicated for children under six, because of high amount of fluoride ions and risk of fluoride ingestion. Figure 2. Caries is excavated using hand instruments (ART technique) (Image: Ivana Miletic). Therapy of aetiological factors can also be managed by some simple advice on oral hygiene, diet or saliva flow stimulation, to help rebalance the oral environment. The use of chewing gums, especially with xylitol and CPP-ACP, can promote remineralisation, saliva stimulation, increasing flow output and buffering capacity. For dry mouth conditions, different products can be advised to the patient to decrease discomfort or increase salivary flow rate (e.g. GC Dry Mouth Gel), (Figure 4). The material used for stabilizing restorations is glassionomer cement (GIC), (e.g. GC Fuji IX, Fuji Triage), (Figure 3). Figure 3. After caries removal, stabilizing restorations, using GIC (GC Fuji Triage) are placed (Image: Ivana Miletic). Figure 4. GC Dry Mouth Gel (Image: Anja Baraba). High-viscosity GICs have higher compression strength, wear resistance and material surface hardness values when compared to the conventional GICs and some of the resin modified GICs [3-5]. High-viscosity GICs are capable to form satisfactory bonds with enamel and dentin. Furthermore, they release fluoride ions over a prolonged period, promote good biological response (biocompatibility) and have a coefficient of thermal expansion close to that of tooth structures [6]. Setting of these materials is rapid and early moisture sensitivity is reduced. With stabilizing restorations the reservoir of bacteria is removed and the remaining tooth structure is protected. Stabilizing restorations help in maintenance of oral hygiene by decreasing the discomfort caused by brushing on exposed dentine. Final restorations are not indicated until the patient's susceptibility to caries is under control. Since dental caries is a bacteria-dependent, multifactorial disease, preventive measures such as sealants, can be implemented once patients susceptible to caries are identified. Daily brushing and flossing help remove food particles and bacteria from the smooth surfaces. However, pits and fissures are more difficult to keep clean. Toothbrush cannot reach into the microscopic grooves to remove tiny particles of food or plaque. 21 Journal of Minimum Intervention in Dentistry J Minim Interv Dent 2011; 4 (2) Sealants are indicated [8]: On pits and fissures of children’s primary teeth when it is determined that the tooth, or the patient, is susceptible to caries; On pits and fissures of children’s, adolescents’ and adults’ permanent teeth when it is determined that the tooth, or the patient, is susceptible to caries; On early (non-cavitated) carious lesions, in children, adolescents and adults to reduce the percentage of lesions that progress. References: 1. 2. 3. Sealants act as a barrier, protecting tooth enamel from plaque, bacteria and acid and preventing pit and fissure caries. Sealants should be placed as soon as possible in highly susceptible patients (Figures 5 and 6) [8]. When sealants are applied to incipient lesions, bacteria become nonviable and caries does not progress. Sealant material effectively eliminates the nutrient source for S. mutans, thus changing a lesion from caries-active to caries-inactive [9]. To ensure an effective seal, sealants must remain in place and completely cover pits and fissures. As long as the sealant remains intact, the occlusal surface will be protected from decay. Regular dental visits are important so that the sealants could be checked and reapplied when needed. GIC and flowable resin composites are materials used for fissure sealing. GIC are less sensitive to moisture control with the ability to release fluoride ions, which may contribute to caries prevention. 4. 5. 6. 7. 8. Figure 5. Tooth 36, in an 8-year-old female patient, highly susceptible to caries (Image: Ivana Miletic). . 9. Figure 6. GIC fissure sealant (GC Fuji Triage) placed on tooth 36 (Image: Ivana Miletic). . 22 Emilson CG. Susceptibility of various microorganisms to chlorhexidine. Scand J Dent Res 1977; 85: 255–65. Maltz-Turkienicz M, Krasse B, Emilson CG. Effects of chlorhexidine and iodine on in vitro plaques of Streptococcus mutans and Streptococcus sanguis. Scand J Dent Res 1980; 88: 28–33. Peutzfeldt A, García-Godoy F, Asmussen E. Surface hardness and wear of glass ionomers and compomers. Am J Dent 1997; 10: 15-7. Guggenberger R, May R, Stefan KP. New trends in glassionomer chemistry. Biomaterials 1998; 19: 479-83. Yap AUJ, Cheang PHN, Chay PL. Mechanical properties of two restorative reinforced glass-ionomer cements. J Oral Rehabil 2002; 29: 682-8. da Silva RC, Zuanon AC. Surface roughness of glass ionomer cements indicated for atraumatic restorative treatment (ART). Braz Dent J 2006; 17: 106-9. Cross KJ, Huq NL, Reynolds EC. Casein phospopeptides in oral health- chemistry and clinical applications. Curr Pharm Des 2007; 13: 793-800. Rethman J. Trends in preventive care: caries risk assessment and indications for sealants. J Am Dent Assoc 2000; 131(Suppl): 8S-12S. Mertz-Fairhurst EJ, Schuster GS, Fairhurst CW. Arresting caries by sealants: results of a clinical study. J Am Dent Assoc 1986; 112: 194–7.