Muscle Excitability-
advertisement

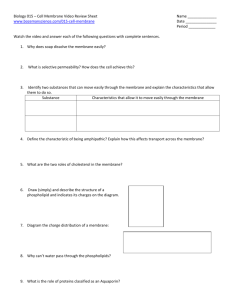
PSIO 603/BME 511 February 19, 2007 1 Dr. Janis Burt MRB 422; 626-6833 jburt@u.arizona.edu MUSCLE EXCITABILITY - Ventricle READING: Boron & Boulpaep pages: 483-507 OBJECTIVES: 1. Draw a picture of the heart in vertical (frontal plane) section. Include the elements of the conduction system in your drawing. 2. Describe the sequence of activation of the heart. List the three benefits of the sequence in optimizing cardiac function. 3. Draw an action potential characteristic of ventricular cells, label its phases, describe the membrane's relative ion permeabilities for each phase, and compare these relative permeabilities to those of skeletal muscle and nerve. 4. Discuss the significance for cardiac function of the high resting potassium permeability. 5. Relative to an action potential, illustrate the timing of the three refractory periods observed in a cardiac myocyte. Provide a definition for each refractory period. State which channel’s activation/inactivation characteristics determine the refractory state of the heart. Graph the relationship between that channel’s availability and membrane potential. State the significance of refractory periods to normal pulsatile function of the heart. LECTURE OUTLINE I. Sequence of Activation – Overview (Objectives 1, 2) A. Normal Sequence of Activation: Sinoatrial node → right atrium, interatrial tracts, and internodal tracts → atrioventricular node and left atria → atrioventricular node → Bundle of HIS → bundle branches → Purkinje fibers → ventricle (apex to base, endocardial surface to epicardial surface) B. Benefits of normal activation sequence 1. Maximizes ventricular filling 2. Optimizes ventricular contraction by stabilizing valve leaflets and septum early in contraction 3. Maximizes ejection by synchronizing contractile activation in the ventricular wall II. Excitability of Ventricular Cells: A. The Action potential - Figure 1&2 (Objectives 3 & 4) 1. Action potential duration is 100x longer than in SKM or nerve with 4 distinct phases. 2. During Phase 4 the membrane potential is dominated by PK (IK1 channels), which are ~10x more numerous than in SKM or nerve. a) High resting PK: stabilizes the resting membrane potential; minimizes arrhythmias by necessitating a large stimulus (depolarization of neighboring cells) to result in successful activation (ventricles are slaves to the pacemaker cells). b) The resting permeabilities for PK :PNa :PCl are: 1 : 0.05 : 0.1 (note: PNa is 10-50x higher than in nerve or SKM; PCl is comparable to nerve, 100x less than SKM. c) The density of Na,K-ATPase enzymes in heart membrane is greater than SKM or nerve. 3. During phase 0, the action potential upstroke, PNa increases resulting in an influx of Na+ (Na-channel comparable to nerve and SKM but with slower kinetics). 4. Phase 1, the early repolarization phase, involves a transient increase in PK (resulting in efflux of K+) and Na-channel inactivation. PSIO 603/BME 511 February 19, 2007 2 Dr. Janis Burt MRB 422; 626-6833 jburt@u.arizona.edu 5. Phase 2, the plateau phase, requires an increase in PCa and a decrease in PK (decrease in IK1 activity). a) The calcium channel is voltage activated, dihydropyridine sensitive, and regulated by cAMP-dependent protein kinase. b) PK decreases as Mg2+ blocks the IK1 channels. 6. Phase 3, repolarization, voltage activated K channels open (IK - delayed rectifiers) and Ca channels close. As the membrane repolarizes Mg2+ block of IK1 channels is relieved and resting membrane permeabilities are restored. 7. As heart rate increases action potential duration decreases; however time between action potentials shortens to a greater extent than the action potential. B. Refractory periods – Figures 1,3,4 (Objective 5) 1. absolute refractory period - the period of time during which no action potential can be initiated, regardless of stimulus strength (ARP in Figure 1) and is considerably longer in duration than observed in skeletal muscle. 2. effective refractory period, the period of time during which no propagated action potentials can be elicited regardless of stimulus strength. 3. relative refractory period (RRP) the period of time in which a response can be elicited but the stimulus required is larger than normal and the amplitude of the action potential is abnormally small. 4. supranormal period (SNP) the period during which a slightly smaller than normal stimulus elicits a propagated response, although the amplitude of the action potential is reduced compared to normal. 5. Full recovery time (FRT) represents the time before a normal action potential can be elicited with a normal stimulus. 6. Refractory properties reflect the recovery of Na-channels to a state from which they can be activated. 7. The long duration of the action potential and the refractory characteristics of the cell insure that cardiac cells are nearly completely relaxed by the time they are repolarized. Cardiac muscle cannot be tetanized because of these membrane properties. LECTURE NOTES I. Sequence of Activation (Objectives 1 & 2) The normally functioning heart follows a specific pattern of activation every time it contracts. This pattern optimizes function by maximizing ventricular filling, contraction and ejection. The activation sequence begins with an action potential at the sinoatrial node, the pacemaker of the heart. The electrical event spreads via gap junctions to the surrounding atria and along specialized interatrial and internodal conduction pathways to the left atrium and atrioventricular node (AV node), respectively. The AV node represents the only point of electrical continuity between the atrium and ventricle. When the excitatory event leaves the AV node, it passes rapidly along the Bundle of HIS, the bundle branches and the purkinje network to the ventricles. Activation of the ventricles occurs initially at the septum and apex of the heart and progresses towards the base of the heart, and from the endocardial surfaces towards the epicardial surfaces. Activation of the ventricles begins ~ 0.15 sec after the atria. This delay between atrial and ventricular activation assures maximal ventricular filling. The sequence of activation within the ventricle insures efficient contraction and ejection by: i) stabilizing the septum and valve leaflets early in the contraction, and ii) activating from apex-to-base and endocardium-to-epicardium. The latter results in pushing the blood towards the aortic valve and PSIO 603/BME 511 February 19, 2007 3 Dr. Janis Burt MRB 422; 626-6833 jburt@u.arizona.edu prevents cells located at the epicardial surface from having to contract against "flacid" cells near the endocardial surface. How do the electrical properties of the cells of the heart insure that this sequence occurs beat after beat? When this pathway of normal activation fails, what properties insure a “back-up” strategy for activation of the heart? What circumstances predispose the heart to arrhythmias? These are the questions we will address over the next week or two. II. Excitability in Ventricular, Atrial and Non-nodal Conducting Cells (Objectives 3 & 4) A. The Action potential: The action potentials of ventricular and non-nodal conduction system cells last for ~250-300 msec; atrial cell action potentials last ~150 msec. These long duration potentials are characterized by several phases (0-4) as shown in Figure 1. Phase 4 -- diastole or rest. The resting permeability of the ventricular cell membrane is dominated by potassium. Ventricular cells have an approximate ten fold higher resting permeability to potassium than do skeletal muscle or nerve cells. This high resting potassium permeability (like the high chloride permeability in skeletal muscle) stabilizes the resting membrane potential reducing the risk of arrhythmias by necessitating a large stimulus to excite the cells. The ventricles are thereby rendered slaves to the pacemaker cells of the heart. The permeabilities of Na and Cl (relative to potassium) are (PK : PCl : PNa) 1 : 0.1 : 0.05. Note that the ventricular cell is more permeable to Na+ at rest than other excitable cells. As a consequence of the high Na+ permeability, the density of Na,K-ATPase enzymes in the membrane is high. Since this pump is electrogenic, its activity contributes several millivolts to the resting membrane potential. Phase 0 -- action potential upstroke. As in skeletal muscle and nerve the upstroke results from an increase in PNa. The voltage gated Na channel Figure 1 Action potential and expressed in the heart is a different gene product than underlying permeability changes for that expressed by skeletal muscle or neural tissues. ventricular and purkinje cells. (modified from reference 2) Phase 1 -- early repolarization. The ionic basis of this phase is a transient increase in potassium permeability (IK-to) and Na-channel inactivation. Phase 2 -- plateau. This is the most distinctive feature of the cardiac action potential. The plateau requires two changes in membrane permeability: 1) an increase in calcium permeability through voltage-activated, L-type Ca channels that are dihydrophyridine sensitive; and 2) a decrease in potassium permeability. During the plateau phase potassium permeability is ~ 1/10 the resting potassium permeability. This decrease in PK is indirectly voltage dependent – at depolarized potentials Mg2+ enters and blocks the IK1 channels. 1 2 3 0 4 P 0 P 0 2+ Phase 3 -- repolarization. Repolarization occurs as Ca channels inactivate and voltage activated K channels open (delayed rectifiers - IK). As repolarization proceeds the IK channels deactivate and the Mg2+ block of the IK1 channels is relieved, which restores the resting permeabilities of the membrane. P 10 0 * PSIO 603/BME 511 February 19, 2007 4 It is interesting to note that the permeability of most excitable cells is lowest when the membrane potential is at the resting level. This conserves energy by reducing the number of Na+ and K+ ions that need to be pumped. Cardiac tissue is the exception to the rule. The cardiac cell’s overall membrane permeability is actually less during the active phase (dominated by the plateau) than during the rest phase. In large part, this difference reflects high resting permeability to K+ and the block of the underlying potassium channels (IK1) that occurs with depolarization. Lower permeability during activation is advantageous to the heart during high heart rates because K+ efflux is spared and the energy required to restore that K+ to the intracellular space (via the Na,K-ATPase) conserved for contraction. Dr. Janis Burt MRB 422; 626-6833 jburt@u.arizona.edu Figure 2 - Epinephrine (black vs. grey curves) shortens the ventricular action potential by enhancing ICa-L and IK. (modified from reference 2) P 0 10 Sympathetic and Parasympathetic Control P The ventricles are well innervated by 0 sympathetic fibers that release norepinephrine. This transmitter binds to β-adrenergic receptors, which transduce the activation of protein kinase A. This kinase enhances the activity of ICa-L and IK channels (see figure 2). In addition to delivering more calcium to the contractile apparatus (stronger contractions), these changes in channel activity cause a shortening of the action potential’s duration. ARP RRP FRT SNP % Na Channels Available B. Refractory Periods (Objective 5) Due to the activation/inactivation characteristics of the voltage-gated Na+ channel underlying phase 0, cardiac muscle is refractory to stimulation until it is repolarized. At the cellular level, the period of time during which no action potential can be initiated, regardless of stimulus strength, is called the absolute refractory period (ARP - Figure 1). At the tissue level, the absolute refractory period translates into the effective refractory period, which is defined as the period of time during which no propagated action potentials can be elicited. The ARP lasts until the membrane potential repolarizes to levels more negative than -65 mV. The ARP is followed by a period in which an action potential can be elicited but the stimulus required is larger than normal and the Figure 3 - Na-channel availability amplitude of the elicited action potential is abnormally determines the refractory properties of small. This period is the relative refractory period the heart. (modified from reference 2) Repolarize (RRP). As the membrane potential repolarizes an + increasing fraction of the total Na channels becomes available for activation (Figure 3). Thus, a stimulus delivered at the beginning of the RRP will elicit an action potential of small amplitude, and one delivered towards the end of the RRP will elicit an action potential of larger amplitude. The RRP is followed by the supranormal period (SNP) during which a slightly smaller than normal stimulus elicits a normal propagated response. Full recovery time (FRT) represents the time after which a normal action potential Membrane can be elicited with a normal stimulus. Potential (mV) 5 Figure 4 - Cardiac contraction is nearly complete with the onset of phase 4 (top panel). Consequently, tetanus is not possible in this muscle type. In skeletal muscle, repolarization occurs early in contraction, making summation and tetanus possible. 2 0 3 4 Tension 1 +50 Membrane Potential (mV) The refractory properties of the cardiac cell are suited to the function of the organ. The timing of the electrical and contractile events is such that the heart relaxes before it can contract again (Figure 4). At a heart rate of 72 beats/min (bpm) and action potential duration of ~300 msec, the time between beats (referred to as electrical diastole) is around 530 msec. At a heart rate of 200 bpm and an action potential duration of 300 msec the interval between beats would be 0 msec. Since it is during diastole that the heart has time to fill with blood, it is clear that in order to be an effective pump at fast heart rates the duration of the action potential must decrease. In general, the duration of the action potential varies inversely with the frequency. Shortening of the action potential reflects the effects of sympathetic drive on Ca and K channel function. Dr. Janis Burt MRB 422; 626-6833 jburt@u.arizona.edu Membrane Potential (mV) PSIO 603/BME 511 February 19, 2007 References Cited in Figures: 1. Physiology by L.S. Costanzo. W.B. Saunders Co., Philadelphia, 1998. 2. Physiology of the Heart (2nd ed.) by A.M. Katz, Raven Press, N.Y. 1992. 3. Ionic Channels of Excitable Membranes by Bertil Hille. Tension C. Action Potential Duration 0 Action potential duration, even within the ventricle, varies. The purkinje fibers have the longest duration (~300 or longer msec at resting heart rates), atrial cells the shortest (150-200msec -85 at resting heart rates); within the ventricle cells 3 msec closest to the chamber have longer duration action potentials than the those at the epicardial surface. This latter comparison is worth remembering – the ramifications of this are that despite depolarizing after ventricular cells near the endocardium, the epicardial cells repolarize first. How can so many different durations result from the same types of channels? Although all these cells have the same array of channel types, their relative numbers differ considerably. You might expect that delayed rectifiers would be more numerous in cells with shorter duration action potentials, if so, you would be correct. You might also expect that Ca-channel density is lower in regions with short action potentials, this too is true.