Down Syndrome: A Multidisciplinary Perspective
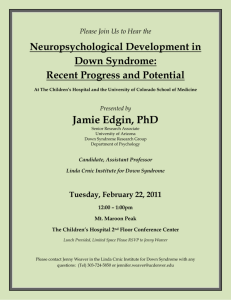
advertisement

J Am Acad Audiol 6 : 39-46 (1995) Down Syndrome : A Multidisciplinary Perspective Allan O. Diefendorf* Marilyn J. Bull* Debbie Casey-Harvey* Richard T. Miyamoto* Molly L. Pope* Julia J. Renshaw* Richard L. Schreiner* Michelle Wagner-Escobar* Abstract Trisomy 21, a genetic disorder resulting from a chromosomal abnormality, is one of the most common forms of mental disability in the United States . Individuals with Down syndrome frequently present with a constellation of medical problems including conductive hearing loss and, to a lesser degree, sensorineural hearing loss . As part of a health care team, audiologists must be sensitive to and aware of medical conditions prior to establishing intervention strategies . Medical conditions, by necessity, precede audiologic interventions and, therefore, a close working relationship among team members is critical . Yet, audiologic and communication interventions should be established at the earliest possible time for maximizing an individual's development potential . This article stresses the importance of a multidisciplinary team in the provision of services so that prevention of further disabilities, improved outcomes of medical interventions, and appropriate habilitative and educational planning may ensue. Key Words: Amplification, audiologic intervention, Down syndrome, hearing impairment risomy 21, a genetic disorder resulting from a chromosomal abnormality, is one T of the common forms of mental disability in the United States, with an incidence of approximately 1/700 live births . In 1866, Langdon Down prepared the first adequate description of this syndrome - hence, the name, Down syndrome . The correct diagnosis of Down syndrome can often be made at birth, fostering early identification and immediate habilitative planning . Otolaryngologic and audiologic problems are common in Down syndrome and constitute potential additional disability. These topics are the focus of this paper and emphasize the importance of early and regular re-evaluation of the audiologic status of every child with Down syn'Indiana University School of Medicine, James Whitcomb Riley Hospital for Children, Indianapolis, Indiana Reprint requests : Allan O . Diefendorf, Indiana University School of Medicine, James Whitcomb Riley Hospital for Children, Indianapolis, IN 46202 drome. Skilled pediatric audiologic and otolaryngologic management in association with appropriate communication intervention can greatly enhance the social and cognitive function of children with Down syndrome . GENETIC CONSIDERATIONS he genetic imbalance leading to Down synT drome can be represented by either Full 21 trisomy (nondisjunction), Partial 21 trisomy (translocation), or mosaicism (postfertilization nondisjunction) . When nondisjunction occurs during the first meiotic division of reproductive cells, both #21 chromosomes end up in one cell. Instead of both cells having 23 chromosomes, one cell has 24 chromosomes, and the other has 22 . The loss of a #21 chromosome makes it highly unlikely for an egg containing 22 chromosomes to survive. However, the egg with 24 chromosomes can survive. Union with a cell containing 23 chromosomes results in a child with 47 chromosomes who has Down syndrome or trisomy 21 . Journal of the American Academy of Audiology/ Volume 6, Number 1, January 1995 Paternal origin of the extra chromosome is estimated to occur in less than 5 percent of cases of trisomy 21, with the remaining 95 percent to 97 percent being maternal in origin . In over 94 percent of the cases, Down syndrome is due to nondisjunction (Cooley and Graham, 1991). Translocation (approximately 4%) involves the transfer of one portion of a chromosome to a completely different chromosome . During meiosis, the chromosomes are close together for extended periods of time . They may touch, stick to each other, and then separate . When they separate, a segment of a chromosome might be pulled off and lost (deletion) or attach itself to another chromosome (translocation). As an example, a part of the #21 chromosome might attach itself to the #14 chromosome . If this occurs during meiosis, one cell will then have 23 chromosomes, with one 21 and one #14/21 chromosome . Fertilization of the egg or sperm containing the #14/21 translocated chromosome will result in a child with 46 chromosomes, including two #21 chromosomes and one #14/21 chromosome . This child, too, will have Down syndrome because of the partial trisomy 21 caused by the translocation . If nondisjunction happens after fertilization, mosaicism results. For example, nondisjunction may take place just after fertilization when four cells are dividing to form eight cells. If one of the four cells divides unevenly, this leads to 47 chromosomes on one daughter cell, 45 in another, and 46 in the remaining six cells. The cell containing 45 chromosomes will die. If the 47-chromosome cell contains a third #21 chromosome, all subsequent daughter cells of this cell will also have 47 chromosomes, or trisomy 21 . The end result will be a child who will have about 80 percent normal cells and 20 percent trisomic cells. The child may look as though he has Down syndrome. However, the physical abnormalities can be less obvious, and the mental disability may be less severe . Mosaicism is rare and accounts for fewer than 3 percent of all children with Down syndrome . Although the clinical diagnosis of Down syndrome can often be made readily, diagnosis in each child should be confirmed by chromosome analysis . Chromosomal studies are useful in the prenatal detection of the syndrome and for recognizing women who may have an increased risk of having a child with Down syndrome (i .e ., those over 35 years or having previously borne a child with Down syndrome). However, this "at-risk" group accounts for only about one-third of Down syndrome births . 40 OUTER AND MIDDLE EAR. ANOMALIES T he communication handicap of Down syndrome children is well documented . However, the causative factors (see Table 1) underlying that problem are not well understood . It is known that these children demonstrate a substantially higher prevalence of hearing impairment than the general population and that hearing loss is usually present in early infancy. Otologic findings and coexisting hearing losses are, therefore, suspect in hindering their acquisition of language skills . The craniofacial configuration of children with Down syndrome is a contributory factor to many of the otolaryngologic problems that occur. Anatomically, diminished dimensions of the external ear structures are characteristic of this population . Aase et al (1973) have documented that the longitudinal dimension of the pinna of newborns with Down syndrome is more than two standard deviations below that of normal newborns. Moreover, the pinna is usually low set. The external auditory meatus is frequently narrow or stenotic (1/z to ~/s the size of age-matched controls), predisposing to occlusion by even minimal quantities of cerumen. Anomalies of the middle ear that have been noted (Harada and Sando, Table 1 Factors that Impact Language and Speech Development Medical Complications Heart problems Failure to thrive Seizures Frequent URls Cognitive/Language-Speech Deficits Language deficits Speech production deficits Memory and attention deficits Hypotonia Delayed acquisition of coordination movement (sitting, crawling, standing, ambulating) Poor oral motor skill development (feeding, swallowing, tongue coordination, jaw stability) Reduced speech production Sensory Deficits Hearing loss/auditory perceptual dysfunction Visual deficits Sensory integration deficits Social Communication Difficulties Complicated nurturing/lack of bonding Stressed relationships Reduced interaction patterns Down Syndrome/Diefendorf et al 1981) include hypoplasia of the epitympanum, varying amounts of mesenchymal tissue in the middle ear including the round window niche, a poorly developed and narrow round window niche, ossicular abnormalities, and wide angle of the facial genu . Congenital eustachian tube abnormalities have been documented by Sando and Haruo (1990) in a study of temporal bone histopathology. Structural anomalies of the eustachian tube exist, including a far more acute angle of entry into the nasopharynx. This, coupled with diminished tube size, predisposes these children to stasis of secretions, ascending infection, and recurrent otitis media. It has been suggested that the child with Down syndrome may be more susceptible to upper respiratory tract infection than the normal child because of peculiar nasopharynx development . In addition to an increase in the prevalence of otitis media with effusion, anatomic considerations in nasopharyngeal development are likely responsible for nasal obstructions and subsequent rhinorrhea . Obstructive apnea is a problem recently recognized to occur with significant frequency in persons with Down syndrome. Failure to treat in severe conditions may result in failure to thrive, hypoxemia, and suboptimal mental function and progress to heart disease secondary to disease of the lung . Generalized muscular hypotonia is also characteristic of Down syndrome . It is postulated that this hypotonia might extend to the tensor veli palatini muscle causing eustachian tube dysfunction. This would result in poor middle ear aeration and subsequent middle ear effusions and infections . Moreover, the epithelium of the middle ear may be roughened due to vitamin A deficiency, increasing the chance of effusion (Coleman et al, 1979). Ossicular abnormalities include congenital malformation and bony erosion from inflammation . It is difficult, if not impossible, to determine whether deformed ossicles represent congenital malformation or osseous remodeling by chronic infection. Ossicular fixation also occurs in Down syndrome and may result in a potentially correctable conductive hearing loss . INNER EAR AND RETROCOCHLEAR ANOMALIES nner ear abnormalities are reported for both cochlear and vestibular structures . Cochlear abnormalities are more prevalent than vestibular abnormalities. When present, inner ear abnormalities are generally mild . Igarashi et al (1977) and Harada and Sando (1981) reported that the length of the cochlear spirals are shorter than that of normal controls . In a series of 12 temporal bones studied by Harada and Sando (1981), the most frequently observed abnormality of the inner ear was endolymphatic hydrops confined to the apical turn of the cochlea. Although there are no reports of specific abnormalities of the VIIIth nerve in Down syndrome, central nervous system abnormalities are likely to be seen. Crome et al (1966) and Crome and Stern (1972) reported that the weight of the cerebellum and brain stem is reduced when compared with normal subjects and may be consistent with the lack of development in these structures . In addition, Palo and Savolainen (1973) suggested that there is a deficiency of the specific myelin basic protein in Down syndrome . Banik et al (1975) reported evidence of abnormal or incomplete myelination, which may reflect general structural changes affecting neuronal growth and synaptogenesis . HEARING LOSS T he reported prevalence of hearing loss in Down syndrome varies, depending on the study population, age of the study group, criteria used to specify hearing loss, and procedural variables, including the type of test administered. Strome (1981) noted a prevalence of 42 percent to 78 percent, verifying that the occurrence of hearing loss is much more frequent in the Down syndrome population than in the population at large. Gerber (1977) has indicated that deafness is rare in this group. On the other hand, studies utilizing developmentally appropriate test techniques report that the majority of hearing impairments are mild to moderate in severity, varying 15 to 40 dB above normal threshold (Greenberg et al, 1978 ; Balkany et al, 1979). Glovski (1966), describing audiometric evaluation by air conduction of 38 children with Down syndrome, found decreased hearing sensitivity in over 70 percent. The type of hearing loss was not reported since sensorineural integrity was not evaluated via boneconduction audiometry. Brooks et al (1972) found 77 percent of their subjects with Down syndrome to have decreased hearing. Middle ear pathologic conditions were reported in 60 percent of the patients, despite a mean age of 26 years for men and 24 years for women. Schwartz and Schwartz (1978) reported that 67 percent of their sample (39 children with a mean age of Journal of the American Academy of Audiology/Volume 6, Number 1, January 1995 3 years) demonstrated otoscopic evidence of pathologic ear conditions . Balkany et al (1979) examined 107 patients with Down syndrome (mean age of 12 years). Hearing loss was identified in 78 percent of their population . Additionally, among the 64 percent of ears identified with binaural losses, 54 percent were of a conductive nature, 16 percent had sensorineural loss, and 8 percent had mixed-type hearing loss . According to Balkany et al (1979), about 40 percent of the children with conductive hearing loss could not be explained by middle ear effusion or chronic otitis media. These patients had normal-appearing otoscopic examinations, suggesting the presence of middle ear anomalies. Surgical procedures on selected Down syndrome patients revealed ossicular malformations and destruction caused by inflammation due to chronic infection. These studies, coupled with surgical and histopathologic findings, confirm that the majority of hearing losses appear to be conductive in nature . Furthermore, in contrast to the natural history of middle ear effusion in the normal pediatric population, the prevalence of this condition tends to remain high in the Down syndrome population, regardless of age. It is recommended that individuals with Down syndrome and persistent conductive hearing loss be treated aggressively from five perspectives : to normalize hearing, to break the cycle of recurrent suppurative otitis media, to prevent chronic ear disease, for early identification of longstanding hearing loss, and for provision of appropriate amplification. Once the child who is at risk for longstanding hearing loss is identified, the nature of the long-standing loss must be assessed . For the Down syndrome population with stenotic ear canals, wax accumulation, otitis media, ossicular malformation, or adhesions, the audiology-otology team is critical . Even for the child identified with a moderate sensorineural hearing loss, the potential of a conductive overlay complicating the habilitation process is great. A close working relationship with the otologist is essential for the audiologist to know when the timing is right to plan appropriate intervention with amplification. For many children, medical and surgical management of a conductive hearing loss may continue for months or years without complete resolution of the hearing loss . This delay in identification of a potentially unresolvable conductive hearing loss can be reduced by routine postoperative audiograms and/or air- and bone42 conducted auditory evoked response testing as well . Conversely, successful resolution and hearing improvement following medical management of a conductive hearing loss can camouflage an underlying mild sensorineural hearing loss for years. Although hearing sensitivity and responsiveness may be somewhat or even greatly improved following medical management, a significant hearing loss may still exist. Clearly, accurate post-treatment hearing assessment is critical in the early identification of the child with Down syndrome with permanent hearing impairment . AUDIOLOGIC CONSIDERATIONS A udiometric evaluation of the Down syndrome population is an essential part of their habilitative management . While conductive pathology is high, underlying sensorineural hearing loss may be present. Therefore, the first objective of audiologic testing is to obtain reliable auditory responses. Visual reinforcement audiometry (VRA), conditioned play audiometry, or conventional test procedures must be selected based on the child's developmental age. Greenberg et al (1978) reported the use of VRA(Wilson et a1,1976; Wilson and Moore, 1978 ; Thompson and Wilson, 1984; Wilson and Thompson, 1984) on 41 subjects with Down syndrome between the ages of 6 months and 6 years. Thresholds, or minimum response levels, were obtained on 81 percent of these subjects . Consistent with other reports, there was higher than normal incidence of hearing loss among these children . Thompson et al (1979) also found that subjects with Down syndrome needed to be functioning above a 10- to 12-month developmental age level to be successfully tested using the VRAprocedure. If clinicians are interested in predicting potential success with the VRAprocedure for children with Down syndrome, the Bayley Scales of Infant Development (BSID) (Bayley, 1969) mental age equivalent score provides the most distinct distribution between successful and unsuccessful tests with the dividing point being a BSID mental age equivalent of at least 10 months . In early studies, reliable hearing tests were felt to be difficult to obtain due to the mental disability associated with Down syndrome . However, if clinicians consider test procedures suited to the patient's mental age and developmental level, audiometric data can be more easily acquired . Play audiometry is usually very successful with older individuals with Down syndrome, even at full adult chronological age. The Down Syndrome/Diefendorf et al "eager to please" nature of children with Down syndrome can lead to frequent false responses when testing this population . Therefore, regardless of behavioral approach, stringent criteria must be established and met to ensure conditioned responses to sound. Additionally, the use of control trials must be implemented to monitor false responding behavior . Speech audiometry is a very important tool for the audiologist . Speech is familiar to young children and will hold their attention. Beginning measures may need to be completed in the sound field due to typically poor headphone acceptance and potential for collapsed ear canals . Obtaining a soundfield speech reception threshold (SRT) followed by a bone-conducted SRT as an indicator of conductive involvement may initially be of most diagnostic value. Individual ear SRTs can also be obtained with insert phones to minimize the complications of collapsed ear canals . Audiologic testing of a child with Down syndrome can be influenced by many variables . Use of familiar items, toys, or spondees may often yield more reliable results. Establishing accurate audiometric results on a young child with Down syndrome frequently requires multiple test sessions . Therefore, keeping things the same, or routine, will often help . Consistent use of the same examiner, sound suite, and toys and effective and consistent praise and reinforcement can often facilitate testing. Once children are comfortable and in a "routine," progress can be made toward obtaining reliable measures . The high incidence of conductive hearing loss makes acoustic immittance an essential part of each hearing evaluation . For younger children, the effectiveness of tympanometry may be compromised by narrow and stenotic ear canals, wax accumulation, and patient cooperation. However, Schwartz and Schwartz (1978) demonstrated the differential diagnostic value of tympanometry for children ages 2 weeks to 11 years with Down syndrome by reporting: (1) the ability to complete tympanograms on 100 percent of their sample ; and (2) the ability to differentiate normal ears from ears with middle ear effusion or suspected ossicular fixation . Of additional significance was the high percentage of absent or elevated acoustic stapedial reflex thresholds found in their sample of children with Down syndrome . Schwartz and Schwartz (1978) speculated that the absent acoustic reflexes may be related to the generalized hypotonia that is common to children with Down syndrome . Loss of tonicity may reduce the tension of the stapedius muscle . Subsequently, greater sound intensity may be necessary to achieve sufficient muscular contraction . In addition, it is also possible that there may be certain subtle changes in the neuronal organization of the reflex arc in these children ; thus, these changes might preclude contraction of the stapedius muscle to acoustic stimulation. Each of these findings is potentially relevant to understanding how children with Down syndrome process auditory information. Interpretation of patent pressure-equalization tubes can be difficult due to the unusually small volume of the ear canal and middle ear space in Down syndrome children . It is helpful and recommended to compare pre- and postoperative volume readings to aid in the interpretation of tube patency. To encourage early identification of hearing loss, the utilization of the auditory brainstem response (ABR) in the newborn nursery or in early infancy for children with Down syndrome is an accepted practice. Squires et al (1980) published one of the first comparative studies of the ABR in individuals with Down syndrome . As a group, the subjects showed shorter central conduction times than a normal comparison group. Additionally, absolute wave V latencies for the subjects with Down syndrome tended to be shorter, despite the fact that the investigators did not control for hearing loss . Folsom et al (1983) also reported shorter wave V latencies for their study group of children (12 months and younger) with Down syndrome . The infants with Down syndrome also showed a steeper latency-intensity slope. Taken together, these studies point out the necessity of establishing latency curves across intensity that are specific to children with Down syndrome . The reported abnormalities in the cochlear and/or neural structures in Down syndrome appear to be reflected in their ABR latencies and, as such, compromise the use of normal latency curves, across intensity, as indices of hearing level. Hearing levels in infants with Down syndrome, particularly older than 6 months, that are determined solely by using the expected latency curves for normal infants, rather than completing a threshold search at decreasing intensity levels, may underestimate the degree of hearing loss and result in false negative findings . Children with Down syndrome should be given every opportunity to improve their hearing by appropriate amplification strategies . The presence of any hearing loss may further complicate the known speech and language delays Journal of the American Academy of Audiology/ Volume 6, Number 1, January 1995 and cognitive limitations that characterize these children . Therefore, children with even minimal hearing loss should be considered candidates for amplification in an attempt to maximize opportunities for advancement. Although an aggressive approach to fitting amplification is stressed, the timing of this intervention must be viewed from a wide perspective . Frequently, the recommendation for amplification will be delayed due to a history of fluctuating conductive hearing loss . Further, many infants and children with Down syndrome will experience prolonged hospitalizations, multiple surgeries, and other medical complications so that hearing loss may not become a priority until they become stable medically. It is appropriate in these circumstances for the audiologist to serve as a resource for the child and his family, communicating with otologists, pediatricians, and speech/language pathologists to ensure eventual intervention with amplification as soon as it is feasible . As with all populations, it is essential to consider the child's family agenda in terms of their readiness and commitment to proceed with amplification. In general, the earlier amplification can be introduced, the more easily it may be incorporated into the child's daily routine and the better the prognosis for long-term acceptance. Adjustment to and successful use of amplification is often more challenging when introduced to the older child with Down syndrome because the child may resist the implementation of a new routine. Regardless of the child's age, ongoing and collaborative consultation with the family is essential in determining the most appropriate timing for intervention with amplification . Once a collaborative relationship with the family is established, the audiologist may also comfortably address important issues such as anticipated benefits and limitations, concerns of family members and others working with the amplification system, and special management considerations . For example, most children are initially amused and entertained by the fact that they can make the hearing aid squeal by putting their hand over the microphone . In most cases, this behavior will last a few days and then lose its charm and disappear. In the child with Down syndrome, the ability to make the hearing aid squeal may not extinguish quickly and may become a behavior that continues long after the fitting. "Feedback is fun" may become a behavioral issue that is annoying to parents. Another common behavioral complaint by parents is that they frequently find the hearing 44 aid turned off. It may be necessary to allow periods of time at home when the child doesn't wear his hearing aids, in order to keep them on at school. There are no easy answers in dealing with these behavioral issues either for the parents or the audiologist . Although reduced wearing time may not be the best answer audiologically, it may be the only solution to keep the family working toward success. The use of loaner amplification will not only facilitate rapid delivery after a long-standing hearing impairment is identified but will also allow the audiologist to meet the demands of changing circumstances such as fluctuant and/or progressive hearing loss . For children with small or stenotic ear canals, use of a bone-conduction hearing aid with a stretch headband to hold the bone oscillator in place may be the most effective amplification option until the child's ear canals grow or can be surgically altered. If the size of the child's ears are adequate to allow the use of effective earmolds, conventional air-conduction hearing aids would be the instruments of choice . Due to the power limitations of the bone oscillator, effective amplification with boneconduction instruments is limited to those patients with mild to moderate conductive impairment. Although it is common practice to fit children with bilateral hearing loss with binaural amplification, initially fitting one hearing aid and later adding the second may often increase the potential for eventual long-term acceptance in this population . Given the high incidence of chronic middle ear effusions, an earmold for each ear is provided so the hearing aid can be alternated between ears if necessary during periods when one ear is draining . This strategy promotes gradual and eventual adjustment to amplification and reduces the possibility of the child having to readjust to amplification after long periods of time without it . LANGUAGE AND SPEECH PLANNING C hildren with Down syndrome are predisposed for language learning deficits . The profile of language learning is quite different when compared to the "normal developmental profile" and when compared to the profiles of other children with mental disability. The child with Down syndrome demonstrates a decrease in the rate of acquiring speech and language as other cognitive skills increase with age (StoelGammon, 1990). Additionally, research has indicated that speech and language development for Down Syndrome/Diefendorf et al children with Down syndrome progresses in an uneven pattern characterized by rapid spurts and changes with long periods of plateau (Miller, 1987). Moreover, Miller and his colleagues (1989, 1990) have described various language learning profiles that have been noted with Down syndrome children . Three profiles have been described: (1) production and comprehension skills that are commensurate with mental age; (2) production skills that lag substantially behind comprehension skills and mental age; and (3) production and comprehension skills that are behind. Table 2 Goals for Enhancing Speech and Language Learning Medical Complications It is important to have a pediatrician that leads a multidisciplinary team and supports early intervention for communication . Cognitive/Language-Speech Deficits Developing joint attention Developing cognitive language skills (object permanence, cause-effect, object concept) Increasing initiated communication Improving imitation skills Expanding turn taking Increasing functional interaction with objects Developing vocabulary/concepts Increasing mean length of utterance Enhancing processing of language Increasing flexible use of vocabulary Developing pragmatic skills Utilizing augmentative communication (i .e ., sign language) Expanding consonant/vowel variety Increasing sequencing of syllable structures (CV, VC CVC) Improving phonologic skills Decreasing rate of speech Monitoring fluency Motor Skill Deficits Cotreatment with occupational and physical therapy Movement and exploration of environment Oral motor stimulation and feeding Sensory Deficits Otologic intervention Audiologic intervention Ophthalmologic intervention Sensory integration programming Enhancing visual/auditory attention Social Communication Limitations Parent education Increasing initiated communication attempts Increasing parent identification of communication attempts Following child's lead Turn taking Developing conversational formats Developing repair strategies The complexity of language development patterns described demonstrates that children with Down syndrome represent a heterogeneous population . As such, factors that influence language development must be viewed carefully for each child. From this analysis, goals (see Table 2) to enhance language learning can be developed. Given that Down syndrome will most likely continue to be a leading cause of mental disability, the challenge is to continue to improve early intervention strategies . Goals for the future should include close otologic management, improved identification of the long-standing hearing loss, earlier intervention with amplification, aggressive speech/language programming, and continued empowerment of the family striving to meet the needs of a child with Down syndrome . REFERENCES Aase JM, Wilson AC, Smith DW (1973). Small ears in Down's syndrome : a helpful diagnostic aid. J Pediatr 82 :845-847 . Balkany T, Downs MP, Jafek BW, Krajicek MJ. (1979) . Hearing loss in Down's syndrome . Clin Pediatr 18 :116-188 . Balkany TJ, Mischke RE, Downs MP, Jafek BW. (1979) . Ossicular abnormalities in Down's syndrome . Otolaryngol Head Neck Surg 87 :372-384 . Banik NL, Davison AN, Palo J, Savolainen H. (1975) . Biochemical studies of myeline isolated from the brains of patients with Down's syndrome . Brain 98 :213-218 . Bayley N. (1969) . Bayley Scales of Infant Development. New York : Psychological Corp . Brooks DN, Wolley H, Kanjilal GC . (1972). Hearing loss and middle ear disorders in patients with Down's syndrome (mongolism) . J Ment Defic Res 16:21-29 . Coleman M, Schwartz RH, Schwartz DM . (1979) . Otologic manifestations in Down's syndrome . Down's Syndrome Papers and Abstracts for Professionals 2:1 . Cooley WC, Graham JM . (1991) . Down syndrome - an update and review for the primary pediatrician . Clin Pediatr 30 :233-253 . Crome L, Cowie W, Slater E . (1966) . A statistical note on cerebellar and brainstem weight in mongolism . J Ment Defic Res 10 :69-72 . Crome L, Stern J. (1972) . Pathology ofMental Retardation . Baltimore : Williams and Wilkins . Down JL. (1866) . Observations on ethnic classifications. London Hospital Reports 3 :259-262 . Folsom RC, Widen JE, Wilson WR. (1983) . Auditory brainstem responses in Down's syndrome infants . Arch Otolaryngol 109:607-610 . 45 Journal of the American Academy of Audiology/ Volume 6, Number 1, January 1995 Gerber SE . (1977) . High risk conditions . In : Gerber SE, ed . Audiometry in Infancy. New York: Grime & Stratton. Glovski L . (1966) . Audiological assessment of a mongoloid population . D-aining School Bull 63 :27-36 . Greenberg DB, Wilson WR, Moore JM, Thompson G. (1978) . Visual reinforcement audiometry (VRA) with young Down's syndrome children . J Speech Hear Disord 43 :448-458. Harada T, Sando I. (1981). Temporal bone histopathologic findings in Down's syndrome . Arch Otolaryngol 107 :96-103. Igarashi M, Takahashi M, Alford BR, Johnson PE . (1977). Inner ear morphology in Down's syndrome . Acta Otolaryngol 83 :175-181 . Miller J. (1987). Language and communication characteristics of children with Down syndrome . In : Pueschel S, Tingey C, Rynders J, Crocker A, Crutcher D, eds. New Perspectives on Down Syndrome . Baltimore : Paul H. Brookes, 233-261. Miller J, Miolo G, Sedey A, Rosin M . (1990, April) . Productive Language Deficits in Children with Down Syndrome . Paper presented at the 23rd Annual Gatlinburg Conference on Research and Theory in Mental Retardation, Brainerd, MN . Miller J, Rosin M, Pierce K, Miolo G, Sedey A. (1989, Nov.) . Language Profile Stability in Children with Down Syndrome . Presented at the American Speech-LanguageHearing Association Convention, St . Louis, MI . Palo J, Savolainen H. (1973) . The proteins of human myelin in inborn errors of metabolism and in chromosomal anomalies . Acta Neuropathol 24 :56-61 . Sando I, Haruo T. (1990) . Otitis media in association with various congenital diseases. Ann Otol Rhinol Laryngol Suppl 148 :13-16 . Schwartz DM, Schwartz RH . (1978) . Acoustic impedance and otoscopic findings in your children with Down's syndrome. Arch Otolaryngol 104:652-656 . Squires N, Aine C, Buchwald J, Norman R, Galbraith G. (1980). Auditory brain stem response abnormalities in severely and profoundly retarded adults . Electroencephalogr Clin Neurophysiol 50:172-185 . Stoel-Gammon C. (1990) . Down syndrome : effects of language development . ASHA 42-44. Strome M. (1981) . Down's syndrome : a modern otorhinolaryngological perspective. Laryngoscope 91 :1581-1594. Thompson G, Wilson WR . (1984) . Clinical application of visual reinforcement audiometry. Semin Hear 5:88-99 . Thompson G, Wilson WR, Moore JM . (1979). Application of visual reinforcement audiometry (VRA) to low-functioning children . J Speech Hear Disord 44 :80-90. Wilson WR, Moore JM, Thompson G. (1976) . Sound-Field Auditory Thresholds of Infants Utilizing Visual Reinforcement Audiometry (VRA) . Paper presented at the American Speech and Hearing Association Convention, Houston, TX . Wilson WR, Moore JM. (1978). Pure Tone Earphone Thresholds ofInfants Utilizing Visual Reinforcement Audiometry (VRA). Paper presented at the American Speech and Hearing Association Convention, San Francisco, CA. Wilson WR, Thompson G. (1984) . Behavioral audiometry. In : Jerger J, ed . Pediatric Audiology. San Diego: College-Hill Press, 1-44 .