From www.bloodjournal.org by guest on March 6, 2016. For personal use only.
CLINICAL OBSERVATIONS, INTERVENTIONS, AND THERAPEUTIC TRIALS
Clinical description of 44 patients with acute promyelocytic leukemia who
developed the retinoic acid syndrome
Martin S. Tallman, Janet W. Andersen, Charles A. Schiffer, Frederick R. Appelbaum, James H. Feusner, Angela Ogden, Lois Shepherd,
Jacob M. Rowe, Christopher François, Richard S. Larson, and Peter H. Wiernik
We examined the incidence, clinical
course, and outcome of patients with
newly diagnosed acute promyelocytic
leukemia (APL) who developed the retinoic acid syndrome (RAS) treated on
the Intergroup Protocol 0129, which prospectively evaluated the role of alltrans retinoic acid (ATRA) alone during
induction and as maintenance therapy.
Forty-four of 167 (26%) patients receiving
ATRA for induction developed the syndrome at a median of 11 days of ATRA
(range, 2-47). The median white blood cell
(WBC) count was 1450/L at diagnosis
and was 31 000/L (range, 6800-72 000/
L) at the time the syndrome developed.
ATRA was discontinued in 36 of the 44
patients (82%) and continued in 8 patients (18%), with subsequent resolution
of the syndrome in 7 of the 8. ATRA was
resumed in 19 of the 36 patients (53%) in
whom ATRA was stopped and not in 17
(47%). The syndrome recurred in 3 of
those 19 patients, with 1 death attributable to resumption of the drug. Ten of
these 36 patients received chemotherapy
without further ATRA, and 8 achieved
complete remission (CR). Among 7 patients in whom ATRA was not restarted
and were not treated with chemotherapy,
5 achieved CR and 2 died. Two deaths
were definitely attributable to the syndrome. No patient receiving ATRA as
maintenance developed the syndrome.
(Blood. 2000;95:90-95)
r 2000 by The American Society of Hematology
Introduction
Randomized clinical trials have shown that the vitamin A derivative all-trans retinoic acid (ATRA) significantly improves the
outcome of patients with acute promyelocytic leukemia (APL).1,2
Although ATRA is generally well tolerated, some patients develop the retinoic acid syndrome (RAS), manifested by unexplained fever, weight gain, respiratory distress, interstitial pulmonary infiltrates, pleural and pericardial effusions, episodic
hypotension, and acute renal failure.3 This syndrome is the most
serious toxicity of ATRA and is often, but not always, associated
with the development of hyperleukocytosis.4-6 It has been suggested that patients who have a white blood cell count (WBC) that
exceeds 5000/µL on day 1, 6000/µL on day 5, 10 000/µL on day 10,
or 15 000/µL on day 15 are at high risk for the development of
RAS.1
The pathogenesis of the syndrome is not completely understood. However, several possible mediators have been identified,
including cathepsin G, a serine protease that enhances capillary
permeability7; cell adhesion molecules on APL cells such as
CD15s(Lex) and integrins CD11a and CD11b, which interact
with the endothelial cell receptor ICAM (intercellular adhesion molecule)-1; and hematopoietic growth factors such as
interleukin (IL)-1, tumor necrosis factor (TNF)␣ and IL-6, which
promote leukocyte activation.8-10 Increased expression of IL-1 in
leukemic promyelocytes may induce endothelial cell expression
of ICAM-1 and vascular cell adhesion molecule (VCAM)-1, which
may allow for leukemic cell binding to endothelium.11 Finally,
exposure of the promyelocytic leukemia cell line NB4 to ATRA
promotes formation of leukoaggregates via LFA-1/ICAM-2 interaction, providing another potential mechanism contributing to the
syndrome.12
The best approach to predict, prevent, or treat the syndrome
has not been established. To further characterize this complication,
we examined the incidence, clinical manifestations, lung pathology, clinical course, and outcome of patients with newly diagnosed APL who developed RAS treated on the National Cancer
Institute Intergroup Protocol 0129, which prospectively evaluated
the role of ATRA alone during induction and as maintenance
therapy.2
From Eastern Cooperative Oncology Group, Northwestern University Medical
School, Robert H. Lurie Comprehensive Cancer Center, Chicago IL; Eastern
Cooperative Oncology Group, Harvard School of Public Health, Division of
Biostatistics, Boston MA; Cancer & Leukemia Group B, Wayne State University, Barbara Ann Karmanos Cancer Center, Detroit, MI; Southwest Oncology
Group, University of Washington, Fred Hutchinson Cancer Research Center,
Seattle WA; Children’s Cancer Group, Children’s Hospital Oakland, Oakland,
CA; Pediatric Oncology Group, Texas Children’s Hospital, Houston TX;
National Cancer Institute of Canada Clinical Trials Group, Kingston, Ontario;
Eastern Cooperative Oncology Group, University of Rochester, Rambam
Medical Center, Haifa, Israel; Southwestern Oncology Group, University of
New Mexico, Department of Pathology, Albuquerque, NM; Eastern Cooperative Oncology Group, Our Lady of Mercy Cancer Center, New York Medical
College, Bronx NY.
CA17145, CA23318, CA31983, CA20319, CA03161, CA11083, CA32102,
CA14958, CA66636, and CA21115 from the National Cancer Institute, National
Institutes of Health, Bethesda, MD, and the US Department of Health and
Human Services. Its contents are solely the responsibility of the authors and do
not necessarily represent the official views of the National Cancer Institute.
Submitted March 29, 1999; accepted September 1, 1999.
Study was coordinated by the Eastern Cooperative Oncology Group (Robert L.
Comis, Chair) and supported in part by US Public Health Service grants
90
Presented in part at the meeting of the American Society of Hematology, San
Diego, CA, December 1997.
Reprints: Martin S. Tallman, Northwestern University Medical School, Division
of Hematology/Oncology, Department of Medicine, Robert H. Lurie Comprehensive Cancer Center, 233 East Erie St, #700, Chicago, IL 60611; e-mail:
m-tallman@nwu.edu.
The publication costs of this article were defrayed in part by page charge
payment. Therefore, and solely to indicate this fact, this article is hereby
marked ‘‘advertisement’’ in accordance with 18 U.S.C. section 1734.
r 2000 by The American Society of Hematology
BLOOD, 1 JANUARY 2000 • VOLUME 95, NUMBER 1
From www.bloodjournal.org by guest on March 6, 2016. For personal use only.
BLOOD, 1 JANUARY 2000 • VOLUME 95, NUMBER 1
APL PATIENTS WITH THE RETINOIC ACID SYNDROME
91
Treatment of the retinoic acid syndrome
Materials and methods
Treatment with ATRA
Intergroup Protocol 0129 was a prospective trial conducted between April
1992 and February 1995 in which patients with newly diagnosed APL
established by morphology were randomized to either ATRA 45 mg/m2/d
divided into 2 daily doses orally or daunorubicin 45mg/m2 by intravenous
(IV) bolus on days 1 to 3 and cytosine arabinoside 100 mg/m2 by
continuous IV infusion on days 1 to 7 for induction.2 Patients who achieved
a complete remission (CR) received 2 cycles of consolidation chemotherapy. They were then randomized to either maintenance therapy with daily
ATRA 45 mg/m2/d for 1 year or observation. Patients ⬍ 3 years of age were
randomized to receive ATRA as just described or daunorubicin 1.5 mg/kg/d
by IV bolus on days 1 to 3 plus cytosine arabinoside 3.3 mg/kg/d by
continuous IV infusion on days 1 to 7. All patients on the ATRA induction
arm were required to have a WBC ⱕ10 000/µL either at presentation, or
after hydroxyurea, prior to initiating ATRA. Hydroxyurea was given any
time the WBC increased to ⱖ 30 000/µL. Patients failing to respond to
ATRA for induction after a maximum of 90 days, or failing before 90 days
of ATRA because of toxicity or progressive disease, were allowed to cross
over to the chemotherapy arm. Patients randomized to induction chemotherapy who did not achieve CR after 2 cycles did not cross over to the ATRA
arm but were removed from the study and treated at the physician’s
discretion.
At the earliest sign or symptom of the syndrome, ATRA was to be
discontinued and dexamethasone initiated at 10 mg IV twice daily. If the
syndrome resolved, ATRA was to be reinstituted at 75% of the initial dose
and then escalated to the full dose after 3 to 5 days if the syndrome did not
recur. All but 3 patients were given 10 mg per day of dexamethasone. Two
patients were given 20 mg per day, and 1 was given 1 mg per day. Among
the patients receiving 10 mg per day, the mean duration of dexamethasone
was 9 days (range, 1-49 days). One of the 2 patients given 20 mg per day of
dexamethasone received 1 day of the drug; the other received 7 days of the
drug; and the single patient treated with 1 mg per day received 17 days of
the drug.
Statistical methods
Univariate analyses of the association between ever-developing RAS and
dichotomous predictors were conducted with Fisher’s exact test. Evaluations of the association of continuous predictors and of multicovariate
models were performed with logistic regression (SAS V6.12). P values
⬍.05 were considered to be significant.
Results
Clinical characteristics of patients with
the retinoic acid syndrome
A total of 172 patients were evaluable for analysis on the ATRA arm. Details
of the patient characteristics and outcome have been previously reported.2
Five of these patients never received ATRA (2 patients crossed over before
any treatment, 2 patients were randomized to ATRA but received chemotherapy, and 1 patient died of intracerebral hemorrhage after the first dose) and
are excluded from this analysis. Forty-four of the remaining 167 (26%; 95%
CI, 20%-34%) patients developed definite RAS during induction therapy
with ATRA.
Table 1 presents the initial characteristics of the patients with and
without RAS. Briefly, the median age was 42 years among patients
who developed RAS and 35 years among those who did not. The
WBC at diagnosis was slightly lower among those who developed
RAS than those who did not, with medians of 1450/µL and
2000/µL, respectively. One patient (2%) among those who developed RAS was reported to have the microgranular variant M3v of
APL in the original data set.2 However, more detailed review for
this analysis indicated that another patient had M3v. Twenty-one
(17%) of the cases who did not develop RAS had M3v. Among
Diagnosis of the retinoic acid syndrome
Table 1. Initial characteristics and clinical outcome
Patients
The diagnosis of RAS was made clinically by the presence of otherwise
unexplained fever, weight gain, respiratory distress, interstitial pulmonary
infiltrates, and pleural or pericardial effusions during treatment with ATRA.
No single sign or symptom itself was considered diagnostic of the
syndrome.3 Cases were identified by reviewing records of patients reported
to have a grade 2 or higher pulmonary or cardiac toxicity as well as by
reviewing cases identified by the institution as having the syndrome from
adverse drug reporting. Seven other patients had signs or symptoms
consistent with the syndrome, but all had concurrent medical problems,
such as bacteremia, sepsis, or congestive heart failure, making accurate
diagnosis of RAS impossible. Therefore, these 7 patients were indeterminate3 and are not included in the cohort of patients categorized as definitely
having the syndrome.
Forty-eight patients treated with chemotherapy who developed grade 2
or worse pulmonary or cardiac toxicity were analyzed for the presence of a
cardiorespiratory distress syndrome similar to that associated with ATRA,
which has been reported rarely.13 One patient developed Streptococcal
mitus bacteremia with adult respiratory distress syndrome, 1 had an
arrhythmia, 8 sustained substantial declines in the left ventricular ejection
fraction, 4 had fungal pneumonia, 1 had sternal heaviness, and the
remainder had either pneumonia, pulmonary infiltrates of undetermined
etiology, fluid overload, or pleural effusion. One patient had pulmonary
infiltrates 2 days prior to study entry with a WBC 34 600/µL and an oxygen
saturation of 85%. On day 1 of chemotherapy, the patient underwent
leukapheresis for a WBC of 42 500/µL and the pulmonary symptoms
resolved, reflecting disease-related pulmonary symptoms.
Characteristic
RAS* (n ⫽ 44)
Non-RAS (n ⫽ 123)
Age, y
Median (Range)
42 (4-81)
35 (1-76)
⬎55
11 (25%)
21 (17%)
23 (52%)
57 (46%)
54 (43%)
Gender
Male
Performance status
0
17 (39%)
1
17 (39%)
51 (41%)
⬎1
10 (22%)
18 (16%)
White blood cell count at diagnosis
(per µL)
Median (Range)
⬎10 000
1450 (400-35 900)
2000 (300-64 800)
3 (7%)
20 (17%)
2 (4%)
21 (17%)
BCR1 (L)
16 (59%)
43 (53%)
BCR2 (V)
0
7 (9%)
BCR3 (S)
10 (37%)
27 (33%)
M3v
PML-RAR␣
True negative
Hydroxyurea at entry
1 (4%)
4 (5%)
3 (4%)
19 (15%)
Outcome
Complete response
3-y disease-free survival
28 (64%)
74%
93 (76%)
66%
RAS indicates the retinoic acid syndrome; BCR, breakpoint cluster region; L, long
form; V, variable form; S, short form.
From www.bloodjournal.org by guest on March 6, 2016. For personal use only.
92
BLOOD, 1 JANUARY 2000 • VOLUME 95, NUMBER 1
TALLMAN et al
those who were evaluated, slightly more than 50% in each group
had the long form of the PML/RAR␣ fusion protein. Three (7%)
patients received hydroxyurea prior to ATRA among those who
developed RAS, compared to 19 (15%) among those who did not.
No patients receiving ATRA for maintenance developed the
syndrome.
There was no significant difference in the CR rate between those
who developed RAS (64%) and those who did not (76%), and there
was no difference in disease-free survival between the 2 groups
among those who did achieve a CR (74% and 66% at 3 years,
respectively).
Timing of the retinoic acid syndrome
RAS developed after a median of 11 days of ATRA (range, 2-47
days).
White blood cell count at the time of the retinoic acid syndrome
The maximum WBC count among the 44 patients who developed
the syndrome ranged from 6800/µL to 72 000/µL (median,
31 000/µL).
Major manifestations of the retinoic acid syndrome
The major manifestations (ⱖ10% incidence) of RAS included
respiratory distress, fever, pulmonary edema, pulmonary infiltrates,
pleural or pericardial effusions, hypotension, bone pain, headache,
congestive heart failure, and acute renal failure. (Table 2). Mechanical ventilation was required in 26% of patients with the syndrome.
Outcome of the retinoic acid syndrome
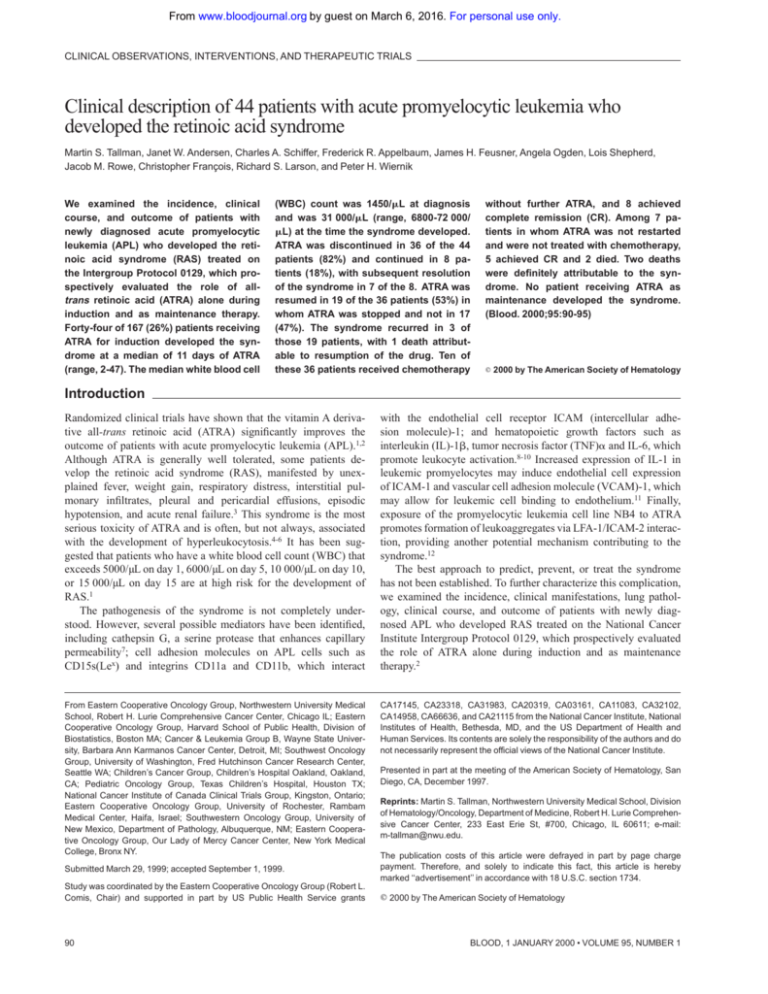
All but 2 of the 44 patients were treated with dexamethasone.
ATRA was discontinued when the syndrome developed in 36 of the
44 patients (82%) and was continued in 8 patients (18%) (Figure 1).
The syndrome resolved in all 8 patients in whom ATRA was
continued, but 1 patient died of intracerebral hemorrhage attributable to the underlying disease. Among the 36 patients in whom
ATRA was stopped, it was resumed in 19 (53%), 11 (58%) under
coverage of steroids. Ten of these 36 patients crossed over to
chemotherapy without restarting ATRA, and 8 achieved CR. The
syndrome recurred in 3 of 19 patients after reinstitution of ATRA
(2 under coverage of steroids), with 1 death attributable to
recurrence of the syndrome, 1 death due to cardiorespiratory arrest
and sepsis, and 17 CRs. Among the 7 patients in whom ATRA was
not resumed and who were not crossed over to chemotherapy, 5
achieved CR after having received 14, 16, 19, 24, and 26 days of
ATRA, and 2 patients died, 1 of intracerebral hemorrhage due to
progressive disease and 1 of multiorgan failure attributable to the
syndrome.
Table 2. Major manifestations of the retinoic acid syndrome
Manifestation
% of Patients
Respiratory distress
84
Fever
81
Pulmonary edema
54
Pulmonary infiltrates
52
Pleural/pericardial effusion
36
Hypotension
18
Bone pain
14
Headache
14
Congestive heart failure
11
Acute renal failure
11
Figure 1. Outcome of 44 patients with retinoic acid syndrome. *Retinoic acid
syndrome, 1 each.
Deaths due to the retinoic acid syndrome
There were 2 deaths definitely attributed to RAS. A 52-year-old
man presented with a WBC count of 3100/µL and developed patchy
bilateral pulmonary infiltrates, fever, and pleural effusions on day 4
of ATRA, with a peak WBC count of 56 100/µL on day 6. ATRA
was discontinued on day 4, and dexamethasone was administered.
ATRA was resumed on day 12 at 75% dose after the syndrome
resolved, and the WBC had decreased to 11 700/µL while he was
still receiving tapering doses of dexamethasone (⬍10 mg every 12
hours), but ATRA was discontinued again on day 18 because the
syndrome recurred. The WBC had increased in 24 hours from
8800/µL to 21 300/µL when ATRA was discontinued the second
time and to 55 800/µL on the day of death. He sustained a
myocardial infarction and died on day 20. The second patient was a
4-year-old girl who presented with a WBC count of 6000/µL and
developed a peak WBC count of 58 100/µL on day 10, when
hydroxyurea was begun. RAS developed on day 29. Despite 17
days of dexamethasone (initially started on day 13 for increased
intracranial pressure due to pseudotumor cerebri and tapered
beginning on day 27), she died on day 30 with pulmonary infiltrates
and hypotension.14
Histologic findings in cases with fatal retinoic acid syndrome
We obtained formalin-fixed postmortem lung tissue for histologic
evaluation from the 2 patients who died. The histologic findings in
the lungs of these 2 patients were consistent with the concept that
ATRA therapy led to differentiation, endothelial cell damage, and
leukocyte infiltration into the lung (Figure 2). ATRA promotes in
vitro differentiation of APL cells over a period of days and, indeed,
circulating myeloid precursors at various stages of differentiation
were present in the microvasculature of both cases. An intraalveolar myeloid infiltrate was prominent in 1 case and mild in the
other, consistent with the hypothesis that ATRA exposure alters
adhesive properties of differentiating APL cells that may lead to
interaction with the endothelium and extravasation from the
blood.11,12 In the case with a prominent intra-alveolar infiltrate,
additional findings indicative of endothelial cell damage were
present and included intra-alveolar edema, interalveolar hemorrhage, and fibrinous exudates.
Prognostic factors for the development of RAS
It has been suggested that patients with a WBC that exceeds
5000/µL on day 1, 6000/µL on day 5, 10 000/µL on day 10, or
15 000/µL on day 15 are at increased risk for RAS.2 Table 3
presents the number of patients who met these criteria and whether
they ever developed RAS.
From www.bloodjournal.org by guest on March 6, 2016. For personal use only.
BLOOD, 1 JANUARY 2000 • VOLUME 95, NUMBER 1
APL PATIENTS WITH THE RETINOIC ACID SYNDROME
93
subsequent 5-day period also showed no discrimination between
patients who developed RAS and those who did not.
The on-study characteristics listed in Table 1 were analyzed for
their predictive value for the development of RAS. As noted above,
only 1 of 44 patients who developed RAS was confirmed to have
M3v at the time the original manuscript was prepared. However,
the subsequent detailed review for this analysis identified a second
patient who had M3v. In multicovariate logistic regression models,
only M3v status was significantly associated with protection from
developing RAS whether considering 1 of 44 (P ⫽ .01) or 2 of 44
(P ⫽ .042). Age (P ⫽ .27), gender (P ⫽ .60), performance status
(P ⫽ .60), molecular break point (P ⫽ .82), and receipt of
hydroxyurea prior to ATRA (P ⫽ .20) were not associated with the
development of RAS in this population. There was no association
of WBC at diagnosis with duration of the syndrome.
Discussion
Figure 2. Histologic findings in cases with fatal retinoic acid syndrome. (A)
Histologic appearance of normal lung tissue. L shows lung alveolae in normal lung;
* indicates normal neutrophil in microvasculature. (B) Lung tissue showing infiltration
of alveolae with leukocytes from a patient who succumbed to the retinoic acid
syndrome. W shows myeloid cells in the airspace (most leukocytes to left of ‘‘w’’); the
lobated nuclei of myeloid cells is prominently seen. Arrows indicate fibrinous exudate
due to vascular leak of serum fibrin.
A total of 110 of 167 patients (66%) met at least 1 of the criteria,
only 31 of whom ever developed RAS. Thus, the sensitivity
(probability of meeting the criteria given that a patient ever
developed RAS) is 31/44, or 70% (95% CI, 55%-83%), and the
specificity (probability of not meeting the criteria given that a
patient never developed RAS) is only 44/123, or 36% (95% CI,
27%-45%). The overall false-positive rate is 64%, and a number of
patients met 2 or more criteria without ever developing RAS. There
is no discrimination between those who developed RAS and those
who did not with these criteria in this large population. In addition,
a time-varying model that considered the predictive value of WBC
at entry and days 5, 10, and 15 for development of RAS in a
All-trans retinoic acid represents a major advance that has made
APL the most curable subtype of acute myeloid leukemia (AML) in
adults.1,2 However, a major toxicity of ATRA has been RAS.3
Neither the pathogenesis nor the optimal way to prevent or treat the
syndrome has been established.
Among 167 patients with newly diagnosed APL treated with
ATRA alone for induction, RAS developed in 26%. An additional 7
patients may have had RAS, but this could not be determined
because of concurrent medical problems. None of these indeterminate cases were treated with corticosteroids. Although the syndrome usually resolved rapidly with the early administration of
dexamethasone even among patients who continued ATRA, the
deaths of 2 patients (5%) were definitely attributable to the
syndrome. The incidence of the syndrome has varied in other
reports from 5% to 27% and the mortality from 5% to 29%.6,13-19
(Table 4). A cohort of patients similar to that reported here, treated
with ATRA alone, had a similar incidence of 27%.6 However, the
mortality rate of patients with the syndrome in the present report is
substantially lower (5% vs 29%), likely reflecting the earlier
recognition and institution of dexamethasone, as experience with
ATRA has accumulated.
The concurrent administration of chemotherapy with ATRA
may decrease the incidence of the syndrome. However, this has not
clearly been established. In the first report of the AIDA (all-trans
retinoic acid plus idarubicin) trial, in which all patients receive
idarubicin concurrently with ATRA, the incidence of the syndrome
was 10%.17 As the experience with concurrent ATRA plus idarubicin expanded, the incidence of the syndrome decreased.18 Among
Table 4. Comparison of the incidence and outcome of the retinoic acid
syndrome (RAS) in other reports
Table 3. Number of patients whose white blood cell count met criteria
predicting the development of the retinoic acid syndrome (RAS)
Study
No. of Patients Meeting Criteria* (%)
None
Any
Total
1
2
3
4
No RAS
44
79
123
30 (24%)
28 (23%)
16 (13%)
5 (4%)
RAS
13
31
44
18 (41%)
10 (23%)
1 (2%)
2 (5%)
Total
57
110
167
48 (29%)
38 (23%)
17 (10%)
7 (4%)
*One criterion equals one of the following; 2 criteria equal any two of the
following; 3 criteria, 3 of the following; 4 criteria, 4 of the following: white blood cell
(WBC) count higher than 5000/µL on day 1, WBC count higher than 6000/µL on day 6,
WBC count higher than 10 000/µL on day 10, WBC count equal to or higher than
15 000/µL on day 15.
No. of
Patients
Induction
Incidence
(%)
Mortality (%)* Mortality (%)†
of Patients
of All Treated
With RAS
Patients
Vahdat6
78
ATRA
27
29
Wiley15
22
ATRA ⫹ steroids
9
50
5
Avvisati17
20
ATRA ⫹ chemo
10
0
0
Mandelli18
240
ATRA ⫹ chemo
3
17
0.4
Asou19
196
ATRA ⫾ chemo
6
9
0.5
De Botton13
413
ATRA ⫾ chemo
15
8
1
Tallman2
167
ATRA
26
5
1
*Percentage of patients with RAS with death attributable to RAS.
†Percentage of all treated patients with death attributable to RAS.
8
From www.bloodjournal.org by guest on March 6, 2016. For personal use only.
94
BLOOD, 1 JANUARY 2000 • VOLUME 95, NUMBER 1
TALLMAN et al
240 patients treated with the AIDA regimen in the most recent
trials, only 6 (3%) patients developed the syndrome and 1 patient
died. An additional 11 patients had a constellations of signs and
symptoms that led to an ‘‘indeterminate’’ classification. The
incidence of the syndrome in the Japanese Adult Leukemia Study
Group (JALSG) trial, in which chemotherapy was introduced early
for the prevention of hyperleukocytosis, was 11 of 196 patients
(6%) with 1 death, which occurred early in the trial when there was
less experience with the syndrome.19 An overall incidence of 15%
was reported by the European APL group, with a mortality rate of
8% of patients with the syndrome.13 No difference in the incidence
of the syndrome was observed among patients treated with
concurrent versus sequential ATRA and chemotherapy. In this trial,
some patients received concurrent chemotherapy for a rapidly
rising WBC count. These series suggest that although the incidence
of RAS may be reduced, the mortality rate due to the syndrome is
low and is not different than the mortality in our series when the
syndrome is recognized and treated early.
There were no pretreatment variables predictive of the syndrome, including median age, gender, WBC count, or breakpoint
location20 except for M3v. Patients with M3v appear to be protected
from the syndrome, but the reason(s) is not clear. Furthermore, we
did not find a WBC count above 5000/µL on day 1, or above
6000/µL, 10 000/µL, or 15 000/µL on days 5, 10, or 15 of ATRA,
respectively, predictive for the development of the syndrome, as
was observed by Fenaux and colleagues.21 Similarly, Vahdat and
colleagues found that the initial WBC count as well as the rate of
rise was not statistically correlated with the development of the
syndrome.6
The pathogenesis of the syndrome has not been completely
determined. However, the autopsy findings reported here provide
insight. The constellation of histologic findings (edema, hemorrhage, fibrinous exudates, and leukocyte infiltration) likely results
from microvasculature damage, because similar histologic findings
are seen in a variety of diseases, including trauma, sepsis, and the
adult respiratory distress syndrome.22-27 The final common pathway is an insult to the endothelium followed by a predictable series
of events, including edema, hemorrhage, fibrinous exudates, neutrophilic infiltration, and respiratory failure.
Patients with AML and hyperleukocytosis with pulmonary
compromise may have indistinguishable clinical presentations
from patients with APL who develop RAS. However, in cases of
AML with hyperleukocytosis, pulmonary compromise appears to
result primarily from formation of leukoaggregates in the circulation.28 In contrast, Frankel et al reported leukocytic infiltration
without leukoaggregate formation in 2 cases of RAS.3 The
histologic findings in the 2 fatal cases of RAS reported here were
identical to those described by Frankel et al.3 Taken together, these
observations indicate that different cellular and molecular mechanisms cause RAS in contrast to leukostasis in AML, although the
clinical scenario is similar. Migration of leukocytes into tissue such
as lung is important in the pathogenesis of RAS, but leukemic cell
adhesion to each other and the formation of leukoaggregates may
be important in leukostasis in AML.
Strategies to prevent the syndrome have been explored. Wiley
and Firkin tested the prophylactic administration of corticosteroids
in 12 patients whose WBC rose above 10 000/µL on ATRA.15 None
of these 12 patients developed any pulmonary toxicity despite a
peak WBC count of up to 112 000/µL. Although this decreased
incidence compared to other trials suggests a benefit, the number of
patients studied was small, and no prospective randomized trial has
been conducted.16-18 Two groups of investigators have reported the
use of a lower dose of ATRA. Castaigne and colleagues showed
that the administration of a lower dose of ATRA of 25 mg/m2/d
resulted in a similar CR rate and similar toxicity profile, including a
similar incidence of RAS as the standard dose.29 However, an even
lower dose of 15-20 mg/m2/d appeared to result in less frequent
development of the syndrome.30 Whether novel retinoids such as
9-cis retinoic acid and AM-80 will be associated with a decreased
incidence of the syndrome is not known.31,32
Several observations regarding the clinical course of patients
with the syndrome can be made. First, ATRA need not necessarily
be discontinued if RAS develops, providing that dexamethasone is
instituted at the earliest sign or symptom. ATRA was continued in 8
patients and, in 7 of the 8 patients, the syndrome resolved and CR
was achieved uneventfully. However, the success of that approach
may depend on the severity of the syndrome and the rapidity of
institution of dexamethasone. Second, ATRA can be successfully
reintroduced following resolution of the syndrome without concomitant steroids. The ability to resume ATRA may be attributable to
suppression of cytokines by corticosteroids together with a continuous reduction in the cell burden. However, the syndrome can recur
despite prophylactic steroids, and it led to the death of 1 patient in
this series. Third, there does not appear to be a risk of the syndrome
when ATRA is given as maintenance therapy to patients in CR. This
issue is important because recent data suggest the value of
maintenance ATRA, even in patients who present with WBC
counts ⱕ5000/µL.2,16 Finally, mortality from the syndrome is now
very low.
What, then, is the recommended approach to prevent and treat
the syndrome? Because recent data suggest that concurrent ATRA
plus chemotherapy may prevent relapse, and because the incidence of the syndrome may be lower, this approach is emerging as a routine strategy for all patients.16 Prophylactic corticosteroids cannot be recommended for routine use at the present
time. Studies evaluating the role of corticosteroid prophylaxis are
underway. If moderate or severe RAS develops, it is prudent to
discontinue ATRA. Prompt administration of dexamethasone is
critical, not only when the diagnosis is definitively established, but
also at the first sign of unexplained dyspnea, fever, weight gain, or
pulmonary infiltrate. When the syndrome resolves, ATRA can
safely be restarted in most patients; however, continued close
observation is warranted. Further studies of growth factor expression and modulation of adhesion molecules may provide further
insights into the pathogenesis of the syndrome and lead to its
prevention.
References
1.
Fenaux P, Le Deley MC, Castaigne S, et al. Effect
of all-trans retinoic acid in newly diagnosed acute
promyelocytic leukemia: results of a multicenter
randomized trial. Blood. 1993;82:3241-3249.
2.
Tallman MS, Andersen JW, Schiffer CA, et al. Alltrans retinoic acid in acute promyelocytic leukemia. N Engl J Med. 1997;337:1021-1028.
3.
Frankel SR, Eardley A, Lawers G, Weiss M, Warrell RP. The ‘‘retinoic acid syndrome’’ in acute promyelocytic leukemia. Ann Intern Med. 1992;117:
292-296.
5.
Warrell RP, Frankel SR, Miller WH Jr, et al. Differentiation therapy of acute promyelocytic leukemia
with tretinoin (all-trans-retinoic acid). N Engl J
Med. 1991;324:1385-1393.
4.
Castaigne S, Chomienne C, Daniel MT, et al. Alltrans retinoic acid as a differentiation therapy for
acute promyelocytic leukemia. I. Clinical results.
Blood. 1990;76:1704-1709.
6.
Vahdat L, Maslak P, Miller WH Jr, et al. Early mortality and the retinoic acid syndrome in acute promyelocytic leukemia: impact of leukocytosis, lowdose chemotherapy, PML-RAR␣ isoform, and
From www.bloodjournal.org by guest on March 6, 2016. For personal use only.
BLOOD, 1 JANUARY 2000 • VOLUME 95, NUMBER 1
7.
8.
9.
CD13 expression in patients with all-trans retinoic
acid. Blood. 1994;84:3843-3849.
Seale J, Delva L, Renesto P, et al. All-trans retinoic acid rapidly decreases cathepsin G synthesis and mRNA expression in acute promyelocytic
leukemia. Leukemia. 1996;10:95-101.
Di Noto R, Schiavone EM, Ferrara F, Manzo C,
Lo Pardo C, Del Vecchio L. All-trans retinoic acid
promotes a differential regulation of adhesion
molecules on acute myeloid blast cells. Br J Haematol. 1996;88:247-255.
Di Noto R, Schiavone EM, Ferrara F, Manzo C,
Lo Pardo C, Del Vecchio L. Expression and
ATRA-driven modulation of adhesion molecules
in acute promyelocytic leukemia. Leukemia.
1994;8(suppl 2):S71-S76.
10. Dubois C, Schlageter MH, de Gentile A, et al.
Modulation of IL-8, IL-1, and G-CSF secretion
by all-trans retinoic acid in acute promyelocytic
leukemia. Leukemia. 1994;8:1750-1757.
11. Marchetti M, Falanga A, Giovanelli S, Oldani E,
Barbui T. All-trans retinoic acid increases adhesion to endothelium of the human APML cell line
NB4. Br J Haematol. 1996;93:360-366.
12. Larson RS, Brown DC, Sklar LA. Retinoic acid
induces aggregation of the acute promyelocytic
leukemia cell line NB4 by utilization of LFA-1 and
ICAM-2. Blood. 1997;90:2747-2756.
13. De Botton S, Dombret H, Sanz M, et al. Incidence, clinical features, and outcome of all-transretinoic acid syndrome in 413 cases of newly diagnosed acute promyelocytic leukemia. Blood.
1998;92:2712-2718.
14. Smith-Whitley K, Lange B. Fatal all-trans retinoic
acid pneumonitis [letter]. Ann Intern Med. 1993;
118:472.
15. Wiley JS, Firkin FC. Reduction of pulmonary tox-
APL PATIENTS WITH THE RETINOIC ACID SYNDROME
icity by prednisolone prophylaxis during all-trans
retinoic acid treatment of acute promyelocytic leukemia. Leukemia. 1995;9:774-778.
16. Fenaux P, Chastang C, Sanz M, et al. A randomized comparison of all transretinoic acid (ATRA)
followed by chemotherapy and ATRA plus
chemotherapy and the role of maintenance
therapy in newly diagnosed APL. Blood. 1999;94:
1192-1200.
17. Avvisati G, Lo Coco F, Diverio D, et al. AIDA (Alltrans retinoic acid plus idarubicin) in newly diagnosed acute promyelocytifc leukemia: a GIMEMA
pilot study. Blood. 1996;88:1390-1398.
18. Mandelli F, Diverio D, Avvisati G, et al. Molecular
remission in PML/RAR␣-positive acute promyelocytic leukemia by combined all-trans retinoic acid
and idarubicin (AIDA) therapy. Blood. 1997;90:
1014-1021.
19. Asou N, Adachi K, Tamura J, et al. Analysis of
prognostic factors in newly diagnosed acute promyelocytic leukemia treated with all-trans retinoic
acid and chemotherapy. J Clin Oncol. 1997;16:
78-85.
20. Gallagher RE, Willman CL, Slack JL, et al. Association of PML/RAR␣ fusion mRNA type with pretreatment hematologic characteristics, but not
treatment outcome in acute promyelocytic leukemia. An intergroup molecular study. Blood. 1997;
90:1656-1663.
21. Fenaux P, Castaigne S, Chomienne C, Dombret
H, Degos L. All-trans retinoic acid treatment for
patient with acute promyelocytic leukemia. Leukemia. 1992;6(suppl 1):64-66.
22. Silberschmid M, Lund C. Lung fraction and morphology after hemorrhagic shock, soft tissue
trauma and regional ischemia in dogs. Eur Surg
Res. 1978;10:404-414.
95
23. McLaughlin JD, Leellacer R, Attar S, Cowley RA.
The lung in trauma. Amer Surg. 1970;36:157-162.
24. Clowes G, Hirsch E, Williams L, et al. Septic lung
and shock in man. Ann Surg. 1975;181:681-692.
25. Corrin B . Lung pathology in septic shock. J Clin
Pathol. 1980;33:891-894.
26. Fallat R, Mielke C, Rodvien R. Adult respiratory
distress syndrome and gram-negative sepsis: a
deadly duo. Arch Intern Med. 1980;140:612-613.
27. Feng D, Nagy JA, Pyne K, Dvorak HF, Dvorak
AM. Neutrophils emigrate from venules by a
transendothelial cell pathway in response to
fMLP. J Exp Med. 1998;189:903-915.
28. McKee LC, Collins RD. Intravascular leukocyte
thrombi and aggregates as a cause of morbidity
and mortality in leukemia. Medicine.
1994;53:463-478.
29. Castaigne S, Lefebvre P, Chomienne C, et al. Effectiveness and pharmacokinetics of low-dose
all-trans retinoic and (25 mg/m2) in acute promyelocytic leukemia. Blood. 1993;82:3560-3563.
30. Chen GQ, Shen ZX, Wu F, et al. Pharmacokinetics and efficacy of low-dose all-trans retinoic acid
in the treatment of acute promyelocytic leukemia.
Leukemia. 1996;10:825-828.
31. Miller VA, Rigas JR, Benedetti FM, et al. Initial
clinical trials of the retinoid receptor panagonist
9-cis retinoic acid. Clin Cancer Res. 1996;2:471475.
32. Tobita T, Takeshita A, Kitamura K, et al. Treatment
with a new synthetic retinoid, Am80, of acute promyelocytic leukemia relapsed from complete remission induced by all-trans retinoic acid. Blood.
1997;90:967-973.
From www.bloodjournal.org by guest on March 6, 2016. For personal use only.
2000 95: 90-95
Clinical description of 44 patients with acute promyelocytic leukemia who
developed the retinoic acid syndrome: Presented in part at the meeting of
the American Society of Hematology, San Diego, CA, December 1997.
Martin S. Tallman, Janet W. Andersen, Charles A. Schiffer, Frederick R. Appelbaum, James H. Feusner,
Angela Ogden, Lois Shepherd, Jacob M. Rowe, Christopher François, Richard S. Larson and Peter H.
Wiernik
Updated information and services can be found at:
http://www.bloodjournal.org/content/95/1/90.full.html
Articles on similar topics can be found in the following Blood collections
Clinical Trials and Observations (4268 articles)
Information about reproducing this article in parts or in its entirety may be found online at:
http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests
Information about ordering reprints may be found online at:
http://www.bloodjournal.org/site/misc/rights.xhtml#reprints
Information about subscriptions and ASH membership may be found online at:
http://www.bloodjournal.org/site/subscriptions/index.xhtml
Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American Society of
Hematology, 2021 L St, NW, Suite 900, Washington DC 20036.
Copyright 2011 by The American Society of Hematology; all rights reserved.