ICD-10 FAQs – Forms - indianamedicaid.com
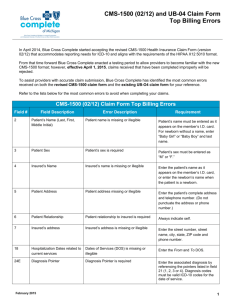
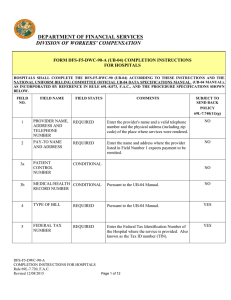
advertisement

ICD-10 FAQs – Forms Questions Click on the question to link to the answer. Once you have viewed the answer, use the page arrow key in the top toolbar to navigate back to this list of questions. Q: Are all claim forms ready for the ICD-10 transition? ...................................................................................................... 1 Q: Where do I find the ICD indicator for the UB-04 claims? ............................................................................................... 1 Q: Can you tell me what values go in fields 17 and 21 (the one-digit ICD Ind qualifier) of the new HCFA (CMS-1500) form? What are the options? ............................................................................................................................................... 1 Q. What has changed on the CMS-1500 claim form as a result of ICD-10? When will the form be published and available for use? ................................................................................................................................................................ 2 Q: Are all claim forms ready for the ICD-10 transition? A: The Uniform Billing (UB-04) Form does not change for ICD-10; however, some of the valid field entries do. See Indiana Health Coverage Programs (IHCP) Provider Bulletin BT201352 for details. The revised 1500 Health Insurance Claim Form (version 02/12) (CMS-1500) includes additional diagnosis fields and an ICD version indicator. Effective April 1, 2014, the Indiana Health Coverage Programs (IHCP) began accepting only the revised version of the CMS-1500 (02/12) paper claim form. See IHCP Provider Bulletin BT201353 for more information. Web interChange was also updated to incorporate ICD-10-related changes for electronic claim submissions. Q: Where do I find the ICD indicator for the UB-04 claims? A: The ICD indicator for the Uniform Billing Form (UB-04) paper claim form will be the same indicator used on the revised 1500 Health Insurance Claim Form (version 02/12), the CMS-1500. The indicator will be a “9” for ICD-9 diagnosis codes or a “0” for ICD-10 diagnosis codes. The IHCP has required this indicator on the UB-04 since January 6, 2014. Q: Can you tell me what values go in fields 17 and 21 (the one-digit ICD Ind qualifier) of the new HCFA (CMS1500) form? What are the options? A: At this time, the new qualifier section in field 17 is not required for the IHCP. However, you may continue to enter the name of the referring physician that is required, if applicable. For waiver-related services, enter the provider name of the case manager. Note: The term “referring provider” includes physicians primarily responsible for the authorization of treatment for lock-in or Right Choices Program members. No changes have been made to fields 17a and 17b. For field 21 ICD Ind, the indicator will be a “9” for ICD-9 diagnosis codes or a “0” for ICD-10 diagnosis codes. © 2015 Hewlett-Packard Development Company, LP 1 Q. What has changed on the CMS-1500 claim form as a result of ICD-10? When will the form be published and available for use? A. For information about the revised 1500 Health Insurance Claim Form (version 02/12) draft form, see IHCP Provider Bulletin BT201353. © 2015 Hewlett-Packard Development Company, LP 2