A Wisp of Air: Review of Respiratory Medication
advertisement

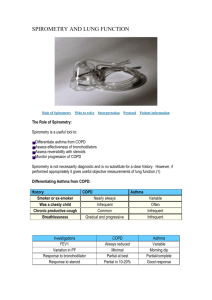
Disney wikia art A Wisp of Air: Review of Respiratory Medication Kathy Tripepi-Bova MSN, RN, CCRN, CCNS Keith Anderson PharmD Functions • provide oxygen to the blood stream and remove carbon dioxide • enable sound production or vocalization as expired air passes over the vocal chords • enable protective and reflexive non-breathing air movements such as coughing and sneezing, to keep the air passages clear • control of Acid-Base balance in the blood and thus control the blood pH One breath • Normal respiratory rate is 10- 15 breaths per minute. • For inspiration, the inspiratory center sends nerve impulses along the phrenic nerve to the diaphragm and along the intercostal nerves to the external intercostal muscles to stimulate inspiration (2 seconds) • For expiration the inspiratory center stop firing for about 3 seconds which allows the muscle to relax and the lungs to recoil Lower airways •www.aduk.org.uk/ gfx/lungs.jpg http://histology.med.umich.edu/medical/respiratorysystem&docid=JPBVlGa23XXLpM&w=850&h=562&ei=OhSCTv 3yHqP-sQKQxuSbDw&zoom=1 Respiratory System – alveoli http://www.livinghe althfully.com/201202/ Lining of the alveoli • Type I cells or Type I alveolar cells – Make up 97% of the alveolar surface – Very thin components of the blood air barrier – Coated by a thin layer of water • Surfactant: a lipoprotein that is produced in the lungs Produced by Type II cells Cover the remaining 3% of the alveolar surface reduces the surface tension of fluid in the lungs and prevents the alveoli from collapsing Production begins in utero at about 20 weeks gestation • Macrophages – important in removing any debris that escapes the mucus and cilia in the conducting portion of the system – Also known as dust cells http://quizlet.com/15237551/respirator y-system-flash-cards/ http://www.studydroid.c om/index.php?page=vie wPack&packId=539058 COPD and Asthma AIRWAY DISEASES Bronchitis • Airway changes lead to hypersecretion of mucus and impaired cilia which lead to a chronic productive cough • Bronchial wall thickening leads to progressive obstruction to air flow “Blue bloater” COPD-Emphysema • A loss of elasticity in the walls of the small air sacs in your lungs. – Eventually, the walls stretch and break, creating larger, less efficient air sacs that aren't able to handle the normal exchange of oxygen and carbon dioxide. • When emphysema is advanced, the patient must work hard to expel air from their lungs • Breathing can consume up to 20 percent of the resting energy. Altered dynamics of breathing • • • • Diaphragm is pushed down Intercostal space enlarges as lung expands Must use neck muscles to aid in respiration “Purse lip breathing” on exhalation Pink puffer COPD-Emphysema • Primary signs and symptoms – shortness of breath – or the feeling of not being able to get enough air • Treatments focus on relieving symptoms and avoiding complications. Asthma Definition of asthma • a chronic inflammatory disorder of the airways that involves many different cells, including mast cells, eosinophils, and T lymphocytes • inflammation causes recurrent episodes of wheezing, dyspnea, and cough Pathogenesis • Airway inflammation with airway reactivity – contraction of the airway smooth muscles – microvascular leakage – bronchial hyper-responsiveness • Asthma differs from other airway diseases because of – absence of bronchiolitis – lack of fibrosis – absence of granulation tissue Early asthma response (EAR) • With exposure to a trigger, there mobilization of histamines, prostaglandin and leukotrienes. • This causes – Airway smooth muscle constriction – Mucous hypersecretion – Mucosal edema Late asthma response (LAR) • Includes mobilization of lymphokines and other chemotactic compounds that may cause lymphocytes, neutrophils and eosinophils to migrate to the site of airway hyperreactivity LAR results in • Damage to the respiratory epithelium • Amplification of the inflammatory process • Propagation of the inflammatory response along other airways Goals of Asthma Therapy • • • • • Prevent chronic symptoms such as cough and wheezing maintain near normal pulmonary function maintain normal activity levels-this includes exercise Prevent recurrent exacerbation Provide optimal pharmacotherapy with minimal side effects • Meet patients and families expectations of satisfaction with asthma care Prevent and decrease symptoms Improve health status Reduce frequency and severity of exacerbations Improve exercise capacity Global strategy for the diagnosis, management, and prevention of COPD: Revised 2014. Global initiative for Chronic obstructive lung disease (GOLD). http://www.goldcopd.org (Accessed October 25, 2014) In Patients with FEV1/FVC < 70% Stage Characteristics I: Mild COPD FEV1 ≥ 80% predicted II: Moderate COPD 50% ≤ FEV1 < 80% predicted III: Severe COPD 30% ≤ FEV1 < 50% IV: Very Severe COPD FEV1 < 30% predicted Global strategy for the diagnosis, management, and prevention of COPD: Revised 2014. Global initiative for Chronic obstructive lung disease (GOLD). http://www.goldcopd.org (Accessed October 25, 2014) Patient Characteristic Spirometric Classification Exacerbations per year CAT mMRC A Low Risk Less Symptoms GOLD 1-2 ≤1 <10 0-1 B Low Risk More Symptoms GOLD 1-2 ≤1 ≥10 ≥2 C High Risk Less Symptoms GOLD 3-4 ≥2 <10 0-1 D High Risk More Symptoms GOLD 3-4 ≥2 ≥10 ≥2 Global strategy for the diagnosis, management, and prevention of COPD: Revised 2014. Global initiative for Chronic obstructive lung disease (GOLD). http://www.goldcopd.org (Accessed October 25, 2014) Patient Group Recommended 1st Choice Alternative Choice Other Possible Treatments A • SA anticholinergic prn or • SA β2-agonist prn • LA anticholinergic or • LA β2-agonist or • SA anticholinergic and SA β2-agonist • Theophylline • B • LA anticholinergic or • LA β2-agonist • SA anticholinergic and/or SA β2-agonist Theophylline • ICS + LA β2-agonist or • LA anticholinergic • LA β2-agonist and LA anticholinergic or • LA anticholinergic and PDE-4 Inhibitor or • LA β2-agonist and PDE-4 Inhibitor C • D ICS + LA β2-agonist and/or LA anticholinergic SA=short acting LA=long acting ICS=inhaled corticosteroid PDE=phophodiesterase inhibitor LA anticholinergic and LA β2-agonist • ICS + LA β2-agonist and PDE-4 Inhibitors or • LA anticholinergic and LA β2-agonist or • LA anticholinergic and PDE-4 Inhibitor • • • • • • SA anticholinergic and/or SA β2-agonist Theophylline Carbocysteine SA anticholinergic and/or SA β2-agonist Theophylline Global strategy for the diagnosis, management, and prevention of COPD: Revised 2014. Global initiative for Chronic obstructive lung disease (GOLD). http://www.goldcopd.org (Accessed October 25, 2014) Short acting β2 agonists Medication Usual dose Duration Albuterol MDI: 2 puffs q4-6 hours Nebulization: 2.5mg q6-8 hours 4-6 hours Levalbuterol MDI: 2 puffs q4-6 hours Nebulization: 0.63-1.25mg TID 6-8 hours Long acting β2 agonists Formoterol Foradil Aerolizer: 12mcg q12 hours Perforomist: 20mcg BID 12 hours Arformoterol 15mcg BID 12 hours Indacaterol 75-300mcg daily 24 hours Olodaterol 5mcg daily 24 hours Salmeterol 50mcg q12 hours 12 hours Short acting anticholinergics Medication Usual dose Duration Ipratropium MDI: 2 puffs 4-6X daily Nebulization: 2.5mL 3-4X daily 6-8 hours Long acting anticholinergics Tiotropium Handihaler: 18mcg daily Respimat*: 5mcg daily 24 hours Aclidinium 400mcg BID 12 hours *Available 1/15 ICS + LA β2 agonists Medication Usual Dose Budesonide/salmeterol 160/4.5mcg BID Fluticasone/salmeterol* 250/50mcg BID Fluticasone/vilanterol 100/25mcg daily Mometasone/formoterol** 10/200mcg-10/400mcg BID *DPI dose (MDI not approved for COPD) **Not FDA approved for COPD SA anticholinergic + SA β2 agonists Ipratropium/albuterol Respimat: 1 inhalation 4-6X daily Nebulization: 3mL 4-6X daily LA anticholinergic + LA β2 agonists Umeclidinium/vilanterol 62.5/25mcg daily Global strategy for the diagnosis, management, and prevention of COPD: Revised 2014. Global initiative for Chronic obstructive lung disease (GOLD). http://www.goldcopd.org (Accessed October 25, 2014) N Engl J Med. 2011; 365(8): 689–698 Global strategy for the diagnosis, management, and prevention of COPD: Revised 2014. Global initiative for Chronic obstructive lung disease (GOLD). http://www.goldcopd.org (Accessed October 25, 2014) Ann Pharmacother. 2012 Dec;46(12):1717-21 Global strategy for the diagnosis, management, and prevention of COPD: Revised 2014. Global initiative for Chronic obstructive lung disease (GOLD). http://www.goldcopd.org (Accessed October 25, 2014) N Engl J Med. 1999;340(25):1941-7 Chest. 2007;132(6):1741-7 JAMA. 2010 Jun 16;303(23):2359-67 Am J Respir Crit Care Med. 2014;189(9):1052-64 JAMA. 2013;309(21):2223-31 Reduce impairment Reducing Risk • • • • • Prevent chronic and troublesome symptoms Require infrequent use of SA β2 agonists Maintain normal lung function Maintain normal activity levels • • • Prevent recurrent exacerbations Minimize need for ED visits/hospitalizations Prevent progressive loss of lung function Provide optimal therapy with minimal or no adverse effects Components of severity Intermittent Symptoms Persistent Mild Moderate Severe ≤2 days/week >2 days/week but not daily Daily Throughout the day Nighttime awakenings ≤2x/month 3-4x/month 1x/week but not nightly Often 7x/week SA β2 agonist use ≤2 days/week >2 days/week, but not daily or >1x/day Daily Several times per day Interference with normal activity None Minor limitation Some limitation Extremely limited • • • • FEV1 > 80% predicted FEV1 /FVC normal Lung function • Exacerbations requiring systemic corticosteroids 0-1/year Recommended step for initiating treatment • FEV1 > 80% predicted FEV1 /FVC normal • FEV1 > 60% but <80% predicted FEV1 /FVC reduced 5% ≥2/year Step 3 Step 1 • FEV1 > 60% predicted FEV1 /FVC reduced >5% Step 2 Step 4 or 5 And consider short course of oral systemic corticosteroids National Heart, Lung, and Blood Institute, National Asthma Education and Prevention Program. Expert panel report 3: guidelines for the diagnosis and management of asthma. Bethesda, Md.: National Heart, Lung, and Blood Institute; Revised August 2007. http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.pdf. Accessed October 25, 2014 National Heart, Lung, and Blood Institute, National Asthma Education and Prevention Program. Expert panel report 3: guidelines for the diagnosis and management of asthma. Bethesda, Md.: National Heart, Lung, and Blood Institute; Revised August 2007. http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.pdf. Accessed October 25, 2014 Drug Low Daily Dose Medium Daily Dose High Daily Dose Beclomethasone HFA 80-240mcg >240-480mcg >480mcg Budesonide DPI 180-600mcg >600-1200mcg >1200mcg Fluticasone HFA: 88-264mcg DPI: 100-300mcg HFA: >264-440mcg DPI: >300-500mcg HFA: >400mcg DPI: >500mcg Mometasone DPI 200mcg 400mcg >400mcg • Clinical effects – – – – – – Decreased severity of symptoms Improved asthma control and quality of life Improved PEF and spirometry Diminished airway hyper-responsiveness Prevention of exacerbations Reduction in systemic corticosteroid courses, ED care, hospitalizations, and deaths due to asthma Medication Fluticasone/salmeterol DPI Fluticasone/salmeterol HFA Budesonide/formoterol Mometasone/formoterol ICS dose Usual dose Low-medium dose 100/50mcg BID Medium-high dose 250/50-500/50mcg BID Low-medium dose 45/21mcg BID Medium-high dose 115/21-230/21mcg BID Low-medium dose 160/9mcg BID Medium-high dose 320/9mcg BID Medium dose 200/10mcg BID High dose 400/10mcg BID *LA β2 agonists should not be used as monotherapy Medication Dose Albuterol MDI: 4-8 puffs every 20 minutes up to 4 hours, then every 1-4 hours prn Nebulizer: 2.5-5mg every 20 minutes X3 doses, then 2.5mg every 1-4 hours prn, or 10-15mg/hr continuously Levalbuterol 1.25-2.5mg every 20 minutes X3 doses, then 1.25-5mg every 1-4 hours prn Ipratropium+albuterol 3mL every 20 minutes X3 doses, then as needed Corticosteroids (methylprednisolone, prednisolone, prednisone) 40-80mg daily until PEF ≥70% of predicted personal best • SA β2 agonists recommended for all patients – Mild-moderate exacerbations may use MDI or nebulizer – Nebulizer for severe exacerbations • Ipratropium – Recommended in ED for up to 3 hours for severe exacerbations – Not recommended for hospitalized patients