BIOPAC STUDENT LAB: LESSON#5
advertisement

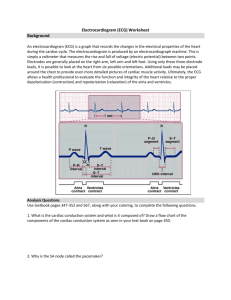
1 Biology 220, Lab Exercise 10 & 11 LABORATORY EXERCISE 10 (BIOPAC STUDENT LAB: LESSON#5) Introduction to the Electrocardiogram (ECG): Effects of Exercise OBJECTIVES: 1. Describe the normal pattern of impulse production and conduction in the tissues of the heart. 2. Describe the normal ECG and explain how it is produced. 3. Obtain an ECG prior to physical exercise, immediately postexercise and 2-minutes post-exercise. Evaluate the cardiac rate, P-R segment, ST segment and TP segment of each. Be able to explain the changes that occur. 4. Describe the effects of sympathetic and parasympathetic innervation upon the heart. 5. Correlate the ECG waves and intervals with the (a) phases of the cardiac cycle, (b) heart sounds, (c) aortic pressure, (d) position of AV valves & aortic & pulmonary valves, (e) left ventricular volume, and (f) left ventricular pressure INTRODUCTION In previous lab exercises, you observed the electrical activity that was produced by contracting skeletal muscles. The recording was called an electromyogram or EMG. In today’s exercise you will be recording the electrical events of the heart muscle. Because the cardiac muscle cells have such a long action potential, the electrical events create a consistent, reproduceable sequence of waves in a recording called an ELECTROCARDIOGRAM OR ECG (EKG). Furthermore, there are no motor units in the heart, and all cardiac muscle cells in the atria or ventricles contract fully and simultaneously; therefore, the amplitude of the electrical waves should not change. Before going any further, let’s review the association between the electrical events of the heart and the mechanical events. Electrical events include depolarization and repolarization of the cardiac muscle tissue. Remember that all atrial cells will depolarize first; then the ventricular cells will depolarize. Answer the following 3 questions before proceeding: (refer to Chapter 9 in your textbook if necessary) Q1. What characteristic of cardiac muscle fibers enables the cells to depolarize simultaneously? ____________ ________________ Q2. Why is there a delay between atrial depolarization and ventricular depolarization? Q3. How long does an action potential last in a cardiac muscle cell? _________________ rd Note in figure 14-27 in your textbook (Silverthorn, 3 ed.), that the electrical events of a cardiac muscle cell precedes the contraction by a few milliseconds. This is an important point to keep in mind when analyzing an ECG. The electrical events of the heart are controlled by the heart’s internal cardiac conduction system during normal heart rhythm. In vivo, the rhythmic beating of the human heart will occur at a rate of approximately 70-80 beats/ minute in the complete absence of any nervous or hormonal rd influences on the SA node (pacemaker- refer to page 470, Silverthorn, 3 ed.). The mechanical events of the heart are divided into contraction and relaxation. This is called the cardiac cycle. One cardiac cycle consists of atrial contraction and relaxation followed by ventricular contraction and relaxation. The contraction phase is called SYSTOLE, and the relaxation phase is called DIASTOLE. When you take your pulse rate, you are actually measuring the number of ventricular systoles in a given period of time. Before coming to lab, Msword doc=220\labmanual\F2004\Ex10&11-ECG&Rx JT 10/03 2 Biology 220, Lab Exercise 10 & 11 answer the following questions and label Figure 1 below: • What is your resting heart rate? ______________________bpm (beats per minute) • Name 2 places on your body where the pulse is normally taken: ____________________________________________ • Why is the SA node considered to be the pacemaker of the heart? Most likely your heart rate was not 70-80 bpm. It was probably lower if you are resting. Therefore, nervous and/or hormonal factors must be regulating the heart rate in vivo. As you know, a large number of sympathetic and parasympathetic axons terminate on the SA node rd (refer to p.480, Silverthorn, 3 ed.). Activity in the parasympathetic (vagus) nerves which release acetylcholine (ACh) causes the heart rate to decrease, whereas activity in the sympathetic nerves which release the neurotransmitter norepinephrine (NE), increases the heart rate. Furthermore, sympathetic nerve fibers also innervate the cardiac muscle and will stimulate an increase in strength of contraction. Parasympathetic neurons (from the Vagus N.) have very little effect on the force of contraction. In the resting state, there is considerably more parasympathetic activity to the heart than sympathetic, and so the normal resting heart rate of about 60-70 bpm is below the inherent rate of 70-80 bpm. Parasympathetic stimulation of the SA node causes the pacemaker cells to take longer to reach threshold while sympathetic stimulation causes the cells to reach threshold at a faster rate (reference: Fig. 9-24, textbook). Today we will see how resting and exercising have an effect on the autonomic nervous system, in turn, influencing the heart rate. The electrocardiogram (ECG or EKG) is primarily a tool for evaluating the electrical events within the heart. The action potentials of cardiac muscle cells can be viewed as batteries that cause electrical charge to move throughout the body fluids. These fluctuations of electrical charges or currents can be detected by electrodes at the surface of the skin. Before proceeding any further, READ pp.471474"The Electrocardiogram", IN YOUR TEXTBOOK (by Silverthorn, 3rd ed.). Figure 1. Label the waves in the simulation of the normal ECG above (2 cardiac cycles). The ECG line looks a little like an action potential but actually each wave represents a different part of the action potentials that are generated in different regions of the myocardium. In the ECG, the P wave represents depolarization of the atria; the QRS complex reflects the depolarization of the ventricles. The T wave represents repolarization of the ventricles at the beginning of diastole. There are 3 times when no current is flowing in the heart musculature and the ECG remains at baseline: 1. 2. 3. during AV nodal delay (from end of P to beginning of QRS complex), and known as the PR segment (because sometimes the Q wave is too small to detect), resting value= 0.16 seconds th (Guyton, Medical Physiology 10 ed.) ; during the plateau phase of ventricular depolarization prior to repolarization, visible as the ST segment (end of S to beginning of T wave) resting value=0.12 seconds; and during isovolumetric ventricular relaxation and initial filling of the ventricles prior to atrial Msword doc=220\labmanual\F2004\Ex10&11-ECG&Rx JT 10/03 3 Biology 220, Lab Exercise 10 & 11 depolarization - TP segment (end of T to beginning of P wave) . During periods of strenuous exercise it is these 3 phases of the cardiac cycle that exhibit the most change in duration. We will be examining this in today’s lab experiment. · Now label the PR, ST, and TP segments in Figure 1 on the previous page. You should learn the significance of each segment as described above (refer to Fig 14-21 in your text book if you need assistance). Although atrial depolarization is represented by the P wave of the ECG, atrial contraction (atrial systole) is delayed (about 10 msec) as a result of the latent period during which time calcium ions enter the cytosol from the ECF. Maximal atrial contraction actually occurs between the P & Q waves of the ECG. And although the QRS complex represents ventricular depolarization, maximal ventricular systole actually occurs between the S & T waves, for the same reasons. Ventricular diastole begins at the middle of the T wave and ends at the R peak of the next QRS complex on the ECG. • Label atrial & ventricular systole in Figure 1 on the preceeding page. In this experiment, you will be using the Biopac Student Lab to visualize your ECG, electrocardiogram. You should understand how to calculate heart rate, determine interval times and wave lengths by hand from a paper copy. You will also calculate these values on the Computerized Biopac Lab using the tools from the tool bar. Your instructor will show you how to calculate the heart rate by hand on paper and from the Biopac. Figure 2 . Set up for the ECG, Biopac Lesson 5. Msword doc=220\labmanual\F2004\Ex10&11-ECG&Rx JT 10/03 4 Biology 220, Lab Exercise 10 & 11 PROCEDURE: to be tested on each person, time permitting. Note that we will NOT be following the directions on the computer screen after the calibration step is completed. · · · · · 1. Set up the electrodes as shown in figure 2. Open Lesson 5 (L05-ECG.1)using your test subject’s first name or i.d. number for the folder title. Click OK. 2. Make sure that the electrodes adhere securely to the skin. If they are being pulled up, you will not get a good ECG signal. Plug the SS2L lead into Channel 2 on the acquisition unit. Perform the calibration step. 3. After the reading stops, obtain a resting ECG by clicking on Record. The subject must be sitting and not moving or talking!! Record the resting ECG for about 20 seconds, then click on Suspend. Take your pulse rate and record in table 10.1 (to verify the accuracy of the Biopac recording). The ECG recording should look typical of that in Figure 1 with discernable waves. If it looks abnormal, check the placement of the electrodes and repeat the recording. 4. Unclip the lead wires from the electrodes. Have the test subject jog on the treadmill or perform jumping jacks for two minutes at a pace that will significantly raise the heart rate. DO NOT ALLOW THE SUBJECT’S HEART RATE TO INCREASE >80% ABOVE NORMAL RESTING VALUES. NOTE: If you are in poor physical shape or sick, you should not perform this exercise as the test subject- have someone else in your group do it. 5. After exercising, re-attach the lead wires to the electrodes and immediately click on Resume. Record the post-exercise ECG for about 20 seconds and click on Suspend. Take your pulse rate and record in Table 10.1. 6. Wait 2 minutes and click on Resume to get the 2-minute postexercise ECG. Record for 20 seconds. Click Suspend and take your pulse rate (record in table 10.1). Now click on Done to exit the ECG reading for this student. Note: Biopac data is not automatically saved. After each student is done, click on "copy to floppy or network". Save in \biology on al\Student Data\ student data storage Bio 220 7. Re-open Lesson L05 from the lessons menu and hook the next person up to the Biopac unit. Repeat steps 1-7 for 2 people in your group. If time allows you can test all members or your group. DATA ANALYSIS: 1. Enter the Review Saved Data mode. 2. Magnify 4-6 cardiac cycles in the resting segment and print in landscape format. Save printout for future reference. 3. Analyze your data: Set up the measurement boxes at the top of the screen as follows: CH 2 delta T (delta time / change in time; this is an ‘x’ axis measurement) CH 2 BPM (beats per min) CH 2 delta [difference in AMPLITUDE (y-axis) between the first point and last point that is highlighted] The delta time measurement is the difference in time between the end and beginning of an area highlighted by the I-beam tool on the graph in seconds or milliseconds (ms). The BPM measurement first calculates the difference in time between the end and beginning of the area selected by the Ibeam tool, and then divides this value by 60 seconds/minute, which gives you beats per minute. Delta tool will measure the difference in amplitude (millivolts – mv) between the first point and last point that is highlighted.. 4. Using the I-beam cursor, select the area between two successive RESTING R waves. Read the BPM measurement and record it: ________. Record the BPM for the next 2 heartbeats and record: ________, _______. Now determine the mean of the 3 BPMs and record in Table 10.1. 5. Determine the amplitude (milliVolts) of the P wave and R wave. To do this, use the I-beam Msword doc=220\labmanual\F2004\Ex10&11-ECG&Rx JT 10/03 5 Biology 220, Lab Exercise 10 & 11 cursor to highlight 3 different P waves from beginning to the highest point in the P wave, in each segment of the experiment. The amplitude of the wave (mV) will appear in the “delta” measurement window. Write these values down and calculate the mean (___________, __________, __________mV). Record the MEAN in Table 1. To find the max amplitude of the R wave, highlight from the end of the P wave to the top of the R wave. Do this in 3 consecutive cardiac cycles and calculate the mean. (You may need to magnify the area to get an accurate measurement. Use the delta value to record the amplitude of 3 consecutive R waves (___________, __________, __________mV), determine the mean and record the MEAN for each segment of the experiment in Table 10.1. 6. Determine the duration of a PR segment (highlight from the peak of the "P" wave to the top of the R wave), an ST segment (bottom of "S" to top of "T" wave), and the TP segment (top of "T" to peak of "P" wave of next cardiac cycle). To do this, MAGNIFY A SMALL SECTION IN EACH SEGMENT OF THE EXPERIMENT. Then highlight each interval with the I-beam cursor and read the Delta T measurement window. Record your data in Table 1. 7. Repeat steps #1-6 on the other 2 segments of the lesson (immediately post-exercise and 2 minutes later). Table 1. ECG data*** of test subject:____________________________________ Mean Mean (top of P to (bottom of S (top of T to top Mean amplitude of amplitude of top of R) to top of T) of P) heart rate P wave R wave P-R interval* ST interval* T-P interval* Pulse ECG (bpm) (mv) @ (mv)@ (seconds)_____(seconds)_____(seconds)_______rate**__ Resting (1st segment) ________________________________________________________________________________________________ Immediately post-exercise (2nd segment) % change between 1st & 2nd segment ________________________________________________________________________________________________ 2 min post-exercise (3rd segment) % change between 2nd & 3rd segment _____________________________________________________________________________ @use the delta tool to determine these values * use the "delta T" tool to determine these values. ** pulse rate is taken by hand after each segment of the test *** use a maximum of 2 numbers to the right of the decimal point in each of your data recordings, if applicable Msword doc=220\labmanual\F2004\Ex10&11-ECG&Rx JT 10/03 6 Biology 220, Lab Exercise 10 & 11 10 pt assignment (turn these 2 pages in before leaving lab today) Name: _____________________________ · DATA ANALYSIS QUESTIONS: · Where did you see the greatest change in the duration of each segment of the cardiac cycle (PR, ST or TP) immediately post-exercise compared to the resting ECG? Why did these changes occur? · Did the 2 minute post exercise heart rate (bpm) return to resting values? If not, why ? Should you expect to see significant changes in the duration of the P wave, QRS complex or T wave when comparing resting to immediate-post-exercise ECG’s? Why or why not? • Was there a large difference between the amplitude of the P waves when comparing the first and second segments of the test? The R waves? If so, what is the reason for the big difference? REVIEW QUESTIONS 1. Think of the placement of the electrodes in an EMG vs. an ECG. Why don’t the electrodes have to be placed directly over the heart for an ECG recording to be made? 2. Why do the mechanical events of the cardiac cycle occur a fraction of a second later than the electrical events? 3. Explain how and why the heart rhythm would change if the cells of the SA node stopped functioning. Msword doc=220\labmanual\F2004\Ex10&11-ECG&Rx JT 10/03 7 Biology 220, Lab Exercise 10 & 11 4. What things would you look for, in an ECG, to determine abnormal rhythms (arrhythmias) in the heart? (refer to your textbook) 5. What is the calculation for cardiac output? 6. Describe how venous return, parasympathetic stimulus, and sympathetic stimuli affect cardiac output. Msword doc=220\labmanual\F2004\Ex10&11-ECG&Rx JT 10/03 8 Biology 220, Lab Exercise 10 & 11 LABORATORY EXERCISE 11 VIRTUAL PHYSIOLOGY - EFFECTS OF DRUGS ON THE FROG HEART We have already learned that the organ systems that coordinate all of the bodily functions are the nervous and endocrine systems. They do this by secreting chemicals, endogenous secretions, which act upon target cells that exhibit specific receptors for the chemicals. The chemicals reach their target by traveling in the blood and ISF. The endogenous secretions are so named because they are produced by the body and act internally. However, we can also regulate many of the bodily functions by taking drugs into our body. Many drugs simulate the actions of endogenous secretions while others act uniquely. A drug is therefore, considered to be exogenous and exhibits pharmacological effects upon the body. The exogenous, pharmacological effects of drugs may be the same as the endogenous physiological effects of natural secretions. We will see examples of this in the Virtual Physiology Frog lab today. Open the Virtual Physiology Frog CD to the lab that deals with Frog Heart. You will be instructed to dispense various drugs onto an exposed frog heart in this virtual lab. After the application of each drug, the heart rate will be displayed and a myogram of the atrial and ventricular contractions will be shown to you on an oscilloscope screen. Ventricular contraction Atrial contraction You should read through the information in the virtual exercise after running the lab experiment in order to help you answer the questions. Record the Frog heart rate and amplitude (force) of contraction in the table below : Drug Heart Rate (bpm) NORMAL CALCIUM DIGITALIS PILOCARPINE ATROPINE POTASSIUM EPINEPHRINE CAFFEINE Msword doc=220\labmanual\F2004\Ex10&11-ECG&Rx JT 10/03 Ventricular Amplitude (# of squares) Other Observations: e.g. atrial fluctuations, etc. 9 Biology 220, Lab Exercise 10 & 11 NICOTINE (topical) (systemic) Data Review: You should be able to explain and describe the effects of the following drugs on heart rate and strength of contraction: 1) pilocarpine, 2) epinephrine, 3) atropine, 4) caffeine, 5) potassium and 6) nicotine. Questions for further Review: 1. Which of the drugs exhibited sympathomimetic activity and what does this term mean? 2. Which of the drugs exhibited parasympathomimetic activity and what does this term mean? 3. What are the molecular mechanisms that cause K+ (potassium) to affect the heart rhythm? Why would excessive K+ in the blood stream cause death? 4. Describe the molecular effects of Atropine on the nervous system. 5. Ground troops in the Iraqi war were issued injectable atropine. Can you explain why this may be useful? 6. Why do the effects of nicotine that is delivered topically or systemically differ? Msword doc=220\labmanual\F2004\Ex10&11-ECG&Rx JT 10/03