Hepatitis A
advertisement

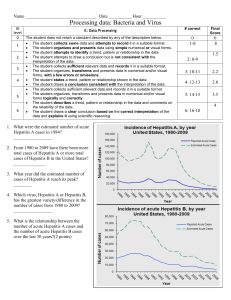
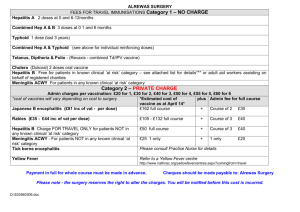
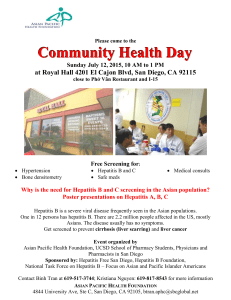
Hepatitis A Studies in Pune (1982-98) Hepatitis A The disease is hyper endemic and the pattern of HAV infection in urban lower middle and rural lower middle classes has remained unchanged. Better hygiene and non-exposure to HAV in higher middle and upper class young population renders them susceptible. Thus the possibility of HAV epidemic amongst them exists. Hepatitis A appears as an emerging infection in adults. Substantial increase in number of hepatitis A cases in higher age group from high socio-economic status has been recorded. ! The causative agent is hepatitis A virus (HAV) ! Earlier referred to as infectious hepatitis. ! Major public health problem, 1.4 The virus million cases each year worldwide. ! ! ! ! ! ! In developing countries, pediatric disease; in developed nations, disease of adults. ! Prevalence of hepatitis A is inversely related to socioeconomic status. Transmission Plus-stranded 7.5 Kb RNA genome. Seven genotypes / Single serotype. HAV grows slowly in cell culture without cytopathic effect. primates. Epidemiology P1 5’ NCR LA LB 1C P3 P2 1D 2A 2B 2C 3A 3B 3C 3D Vpg Laboratory diagnosis Disease ! IgM-anti-HAV is the diagnostic marker Ninety percent infections in children lead to subclinical presentation. Proportion of clinical cases increases with age. Fulminant hepatic failure is a rare serious complication. Does not lead to chronicity. 80 70 60 50 40 30 20 10 0 6-10 SYMPTOMS ! Urine was found to be an alternative IgG ANTI- HAV test specimen for diagnosis of hepatitis A, useful especially in children. ! Blood collection on filter paper disc proved to be satisfactory for anti-HAV detection. 16 WEEKS AFTER EXPOSURE 52 11-15 16-25 1982 AGE GROUP 82% 25+ 1992 1998 Rural lower middle class 110 100 Hep A 90 Non-A 80 Acute viral hepatitis ! ELISA based hepatitis A diagnostic ALT 12 90 % anti-HAV ELISA and Blocking ELISA tests have been developed and are routinely used to provide diagnosis of recent and past infection of hepatitis A virus. technology has been transferred to Hyderabad based industry. This is the first such transfer from NIV, Pune. 8 100 18% ! At NIV, Pune, IgM anti HAV capture JAUNDICE 4 110 for hepatitis A. Markers / symptoms during HAV infection 0 NCR 3’ Poly A Urban Lower-middle class In India, Hepatitis A virus is the main causative agent of acute hepatitis in children. It accounts for significant number of FHF cases in children. % anti-HAV HAV Genome transmission noted in Europe. IgM ANTI- HAV Indigenously developed hepatitis A diagnostic kit 27-30 nm diameter particles. ! Available animal models: Non human ! Fecal-oral route. ! Person-to-person contact. ! Inadequately cooked food. ! Blood-products-associated FECAL HAV Picornaviridae, genus Hepatovirus. 70 60 50 40 30 20 10 0 Non-viral Hepatitis 48% Hep A 40% Viral Hepatitis 52% AGE GROUP Hep B or D 12% Fulminant hepatitis 53 15+ 11-15 6-10 1983 1998 Higher socioeconomic class Year-round PCR-based HAV-RNA positivity %ANTI-HAV % PCR +ve 110 100 90 80 70 60 50 40 30 20 10 0 6-10 11-15 AGE GROUP 16-25 1982 Dendrogram depicting nucleotide sequence identity among HAV strains in VP1/2A region of HAV genome L07730 PANAMA 54 52 IN D 9 4 -2 /V P 1 IIIA 54 54 Effluent L 0 7 7 2 4 Nepal L 0 7 7 2 5 India L 2 0 5 2 8 Japan L 0 7 7 2 9 SierralL e o n e 87 Several animal species shown to be anti-HAV positive. 6 4 Genotyping of HAV strains in sporadic cases from Pune 2 1994-97 Co-circulation of subgenotypes IB and IIIA with predominance of IIIA detected. Mixed infection with IB and IIIA identified in inidividual hepatitis A patients. Multivariate analysis identified lower middle socioeconomic status (22.9 fold), age > 15 years (8.9 fold) and family size > 4 (1.6 fold) as independent risk factors influencing exposure to HAV. Thirty percent HAV RNA positivity in neat sewage samples documents extremely high viral load in the environment. This also represents a potential threat for contamination of drinking water leading to endemicity and extensive outbreaks. 54 GenotypeII GenotypeIA M147 07 98 100 IN D 9 2 - 1 /V P 1 IN D 9 4 - 2 / V P 1 IB GenotypeIB IN D 9 8 - 7 / V P 1 IB L 0 7 7 3 2 Phillipines L 0 7 7 3 1 Indonesia 79 D00924Kenya GenotypeV 0.05 ˜ Isolates indicating mixed genotypes are shown in blue color. Scale indicates genetic distance 0 1978-81 GenotypeVII Ab020564Japan 78 53 8 GenotypeVIIIB L07693France Prolonged fecal excretion and viremia observed in Indian patients and experimental monkey. 10 Genotype IIIA IN D 9 6 - 3 /V P 1 N O R 21 100 99 Sewage plant 12 IN D 9 8 -7 /VP 1 IIIA IN D 0 1 - 10 /VP 1 Affluent 25+ 1998 Hepatitis A in adults % Hep A Cases 35 30 25 20 15 10 5 0 Emergence of epidemic hepatitis A All epidemic HAV isolates from Pune (prefix 03) and around Pune (red) belong to genotype IIIA. 0314456 0313824 12 037108 0313832 26 037082 26 0314447 037107 0314484 IIIA 3 DAUND-B2 DAUND-S1 DAUND-SW 8 9 DAUND-B1 M34084 44 DAUND-S2 037114 49 0313267 AY032861 VII 88 AF268396 88 M14707 IB 77 AF314208 85 M20273 54 AF357222 AF485328 83 K02990 IA 48 AB020565 33 X75215 39 81 X83302 D00924 V M59286 IV An outbreak of hepatitis A in day-care centers for children in Pune emphasizes importance of such centers in the transmission of HAV. From 2003, hepatitis A is assuming epidemic proportions, especially in rural and semi-urban settings. Source remains contaminated water supply. 0.2 Vaccines ! Both killed and attenuated hepatitis A vaccines are available. Most countries do not have definite policies for hepatitis A vaccination. ! NIV studies suggested that 9 months is the appropriate age for hepatitis A vaccination. ! Isolated an Indian strain of HAV in tissue culture and transferred to industry for vaccine preparation. Prevention Ÿ Supply of safe potable water. Ÿ High standards of public and personal hygiene. Ÿ Education of food handlers. Ÿ Vaccination of high-risk individuals: § Children from high socioeconomic status. § Young food handlers. § Siblings of hepatitis A patients. § HBV/HCV carrier children. Patent A patent on Hepatitis B “Novel process of Hepatitis A vaccine preparation” has been filed. 56 The risk factors ! The causative agent is hepatitis B virus ! Transfusion of unscreened blood. ! Improperly sterilized syringes / (HBV). ! Earlier referred as Serum Hepatitis. ! 350 million carriers of the virus needles / dental / other equipments. Based on transmission modes, several high-risk groups have been identified. Mentally compromised children ! Close contact with HBV positive worldwide. individual. ! 34 million HBsAg carriers in India. ! 200-fold higher risk of primary ! Shared razors, toothbrushes with carrier. ! Tattooing. ! Sexual contact with HBV positive hepatocellular carcinoma. ! Wide spectrum of clinical presentations. individual. ! Several transmission modes. ! Efficacious vaccine available since HBV Epidemiology in and around Pune (1982-1998) Orphans Asthamatics Health care personnel Urban Leprosy patients 25 Family contacts of carriers Paid blood donors 20 HBsAg HBsAg+anti-HBc Haemodialysis patients % Positive Hepatitis B Hepatitis B vaccination introduced for tribals of Andaman and Nicobar Islands Prisoners STD patients Dental auxiliary staff Dentists Voluntary blood donors HBsAg 1982. 10 20 30 40 50 60 70 80 90 100 0 Percentage anti-HBc 1982 These high risk individuals must be considered for vaccination 35 1998 1982 Year 1992 1998 Adults HBsAg anti-HBc 25 Cultural practices make tribals a high-risk category Electron micrograph of 42 nm HBV from a blood donor in Pune 1992 Children Rural 30 Percentage Hepadnavirus 10 5 0 ! Multiple sex partners. ! Infected mother to infant. 15 20 15 10 5 Tribal populations and exposure to HBV (%) 0 Infection with HBV may lead to ! Subclinical infection. Children Dhule Maharashtra ! Acute self-resolving hepatitis. ! Fulminant hepatitis. ! Asymptomatic carrier state. ! Chronic hepatitis. ! Cirrhosis. ! Hepatocellular carcinoma. Children Adults 1998 HBV prevalence in Pune was determined according to socio-economic status viz. lower middle class status (LMS) and higher socio-economic status (HS). Bhiwandi Thane Pune 0 10 20 30 58 40 50 60 70 30 anti-HBc Percent Positives Transmission routes Andaman & Nicobar islands HBsAg Ÿ Parenteral Ÿ Inapparent parenteral Ÿ Sexual Ÿ Vertical Ÿ Horizontal Aduilts 1983 Onges Shompens 25 HBV exposure according to socio-economic status, Pune 1998 LMS HS 20 15 10 5 0 6-10 11-15 16-25 Age Groups Nicobarese Andamanese 0 10 20 30 40 HBsAg 50 60 anti-HBc 70 80 90 100 25+ Asymptomatic HBsAg Carriers Chronic Hepatitis B 2% 2% 16% 39% 36% Delta Rn vs Cycle No HBV Standard Diagnostics HBV Pre-Core mutant and clinical presentation As early as 1980, highly sensitive and specific ELISA for the detection of HBsAg was developed at NIV. This represents the first indigenously developed HBsAg ELISA in India. These ELISA reagents were certified by WHO. Delta Rn In 1981, again for the first time, ELISA for the detection of anti-HBs antibodies was developed. 82% 23% Acute Hepatitis B Fulminant Hepatitis B Cycle Number 13% 14% HBV DNA quantitation is a national facility available at NIV Assessment of screening tests / vaccines 86% 87% Negative Mutants Wild ! Evaluation of commercially available Mixture Ÿ Risk of Chronic hepatitis 4.3-fold higher with HBV pre-C wild Ÿ 3.2 fold higher chances of asymptomatic carrier state with pre-C mutants Ÿ Pre-C mutant not associated with fulminant hepatitis assays as part of WHO-SEARO designated national reference center. ! To assess the presence of replicating virus, PCR for the detection of HBV DNA was standardized in 1990. ! From 1985, worked closely with blood banks from Pune in verifying efficiency of the tests used for donor screening. ! An important development was standardization of Quantitative Real Time HBV DNA PCR assay employing primers and probes designed at NIV. ! Immune response to several plasmaderived and recombinant vaccines evaluated in Indian population. HBV Genotypes ! Follow up of vaccinated persons for 14 § Genotype D predominant GNTYP-B GNTYP-C 38 GNTYP-E GNTYP-D 38 60 ASC1027 (19) 99 CLD2235 (25) 56 FHF2376 (5) 65 AVH1164 (8) GNTYP-F 99 GNTYP-H 0.01 60 years. in western India. § Did not influence outcome of HBV infection. § Genotype D highly prevalent in tribes from Andaman and Nicobar islands 61 One orphan selected by needy parents and born to HBsAg carrier mother was vaccinated, followed for seroconversion and finally adopted Creation of awareness about hepatitis B ! Children from several urban and rural schools. ! Family contacts of HBsAg carriers. l Several family contacts immunized l Several HBsAg carriers counselled at a young age l Immunized would-be spouses before marriage l Immunized children at birth, born to HBsAg positive mothers Hepatitis C < Based on NIV results immunization of dental students and dentists was made mandatory in Maharashtra < Orphans screened for HBsAg before adoption 62 ! At present, no confirmatory immuno- ! Earlier known as post-transfusion non A-non B hepatitis (PT-NANB). assays are obligatory. ! Presence of HCV RNA by nested RT ! 170 million hepatitis C virus (HCV) infected individuals worldwide. PCR employing primers from 5'NTR. ! Nested RT-PCR assay (1990) was The disease ! Mostly subclinical. ! High chronicity potential (>70%). ! 50-70% of chronically infected individuals develop chronic liver disease. ! Not a major cause of acute or fulminant hepatitis. standardized at NIV. Screening of clinical samples from all over India for HCV RNA is ongoing. very important parameter in disease staging and response to antiviral therapy. Quantitative real time PCRbased assay was standardized in 2003 on the basis of viral genotypes circulating in India. evaluated in Indian population immediately after availability in the market. hepatocellular carcinoma. The virus ! At present, several host and viral Belongs to family Flaviviridae; positive sense, ssRNA genome (~9.4 kb). Classified into 6 genotypes. ! So far, chimpanzee is the only animal model for HCV. factors are being investigated for chronicity potential and success of interferon therapy. Transmission ! No convenient cell-culture system is ! Parenteral transmission important mode. available. ! At NIV, attempts to infect rhesus ! Quantitation of HCV viral load is a ! First, 2nd and 3rd generation ELISAs ! Important cause for primary Experimental transmission ! ! In dialysis units, a new patient usually gets infected with HCV within six months, mainly through nosocomial spread. Samples from 149 HCV RNA positive patients from different parts of India were genotyped on the basis of phylogenetic analysis. Epidemiology ! Anti-HCV prevalence among age stratified general population is low. 2.82% ! Prevalence was low in rural and 45.07% tribal populations. 52.11% ! Anti-HCV positivity in commercial blood donors was high. NORTH 3.33% ! Dialysis patients and hemophiliacs are at higher risk of getting infection. 33.33% Delta Rn vs Cycle ! Blood donors from a commercial plasmapheresis unit had shown 90% anti-HCV positivity, most antibody positives being HCV RNA positive. 63.33% Delta Rn Electron Micrograph of HCV SOUTH 25.00% 38.89% 14 Diagnosis 12 ! No marker distinguishes between 36.11% acute and chronic infections. Cycle Number ! Detection of anti-HCV antibodies by rd 3 generation screening ELISAs. Blood products being imported in India are screened for HCV RNA at NIV. EAST 25.00% 8 6 4 HCV Genome Organization 5 NTR gp35 gp70 P7 P23 P70 C E1 E2 Ns1 Ns2 Ns3 Structuralprotins P8 P27 P56/58 P68 Ns4A NS4B NS-5A NS-5B 3’ NTR Commercial blood donors 10 75.00% P22 the and intrafamilial are infrequent. Genotypes WEST is ! Other modes like sexual, vertical monkeys and insect cell lines susceptible for other flaviviruses, were not successful. Genotype 1 Genotype 4 Genotype 3 Nontypable 2 Percentage Hepatitis C A new subtype of HCV, 3i, first identified in western India, was later found in other parts of the country. 0 1982 Nonstructural proteins 1983 Year 65 1986 Voluntary Blood Donors 1 / 217 0 / 346 1 / 180 0 / 178 0 / 400 0 / 259 0 / 445 Other studies Association with blood banks As serological tests for HCV were still evolving (1st, 2nd & 3rd generations), the NIV together with local blood banks sorted out the problems of specificity and sensitivity, based on the use of confirmatory Recombinant Immunoblot Assay (RIBA) and PCR tests. Similar trend continues till 2004 25 Anti-HCV positivity in different categories 15 20 Interferon treatment A national facility for the detection of HCV RNA, employing nested RT PCR was set up in July 1995. Samples from different parts of India were screened as a prerequisite for the initiation of interferon therapy as well for the assessment of success of therapy. 5 10 ICMR's multi- centric trial for combination therapy NIV is responsible for all the virological aspects of this trial, including detection and quantitation of HCV RNA and sequencing-based genotyping. Voluntary Blood Donors Patients undergoing Hemodialysis Multiply transfused Patients Chronic Liver Disease Patients Leprosy Patients Acute Viral non-A,non-B Hepatitis Patients Health Care Personnel Patients suffering from Sexually Transmitted Diseases Dentists Institutionalised children with high HBV exposure Normal Pregnant Women 0 Expression of recombinant core antigen Highly immunoreactive recombinant HCV core antigen was expressed in baculovirus system. Prevention In the absence of possibility of vaccine for hepatitis C in the near future, strict adherence to universal precautions in relation to parenteral transmission mode seems the best available choice. 66 Hepatitis E Recognition During 1980, joint efforts of NIV, Pune and NIH, USA led to the recognition of a novel clinical entity, enterically transmitted non-A, non-B or waterborne or epidemic NANB hepatitis, distinctly different from paranterally transmitted non-A, nonB hepatitis identified in the west. Virus-like particles were identified at NIV employing Immune Electron Microscopy in the feces of a NANB patient. Association of this virus with the disease was subsequently confirmed after experimental infection of chimpazees (in collaboration with NIH, USA). In 1990 the virus was named as hepatitis E virus. Electron micrograph of HEV The virus ! Recently classified as a member of a Acute, self-limiting; occasionally leads to fulminant hepatitis. No chronicity recorded. Usually affects young adults; high mortality among pregnant women, especially in the third trimester. The disease was believed to be restricted to developing countries wherein both epidemic as well as sporadic forms exist. However, recent studies have documented hepatitis E among persons from several developed countries without any history of travel to endemic countries. Detection of IgM-anti-HEV by ELISA. In very early acute cases, IgM antibodies may not be detectable, HEV RNA by nested RT PCR may be the method of choice. ! 27-30nm spherical particles. ! The genome is a single-stranded, positive sense RNA of about 7.2 kb. ORF-3: 369 nt Epidemiology Diagnosis newly designated Hepeviridae family. 5’ The disease 3’ Studies conducted at NIV and in different countries have shown that HEV has predilection for young adults. However, an outbreak of hepatitis E among residential school children at Talegaon, India (1988) was recorded. Moreover, ~ 70% anti-HEV positivity among children from Shompen tribe from Andaman and Nicobar Islands was also documented. Diagnostic test development ! ORF-2 ORF-2: 2 kb ORF-1: 5 kb Genotypes HEV strains are classified into 4 79 93 AF103940 52 99 98 98 IND-SW2 IND-SW1 IND-SW3 IND-SW4 98 TAIWAN CH-T11 88 44 AF134812 63 TW6310E TW8E-2 57 100 43 TW6196E TW2494E US2 US-SW 100 US1 68 MEX86 87 99 41 Epidemics of HEV in India be used to detect both type 1 and 4 HEV infections. ! Sporadic HEV cases could be dia- CH-T21 29 hepatitis E. ! Swine and human HEV antigens can 4 HF-030 HF-054 57 100 collected during all HEV epidemics (1976-2004) showed anti-HEV IgM and IgG antibodies. TW74SW 67 Hepatitis E is the major cause of epidemic hepatitis in India. NIV has investigated over 100 outbreaks of ! Sera TW32SW TW5483E 80 protein (both swine and human HEV) expressed in baculovirus system proved to be a highly reactive antigen for ELISA. Based on recombinant ORF-2 antigen, ELISA could efficiently detect both IgM and IgG-anti-HEV antibodies. NAFR83 49 D11092 96 L08816 3 2 gnosed. NIV ELISA was comparable with the commercially available, Genelab ELISA. Maharashtra State 3 L25595 61 87 BUR83 BUR89 45 AKL90 AKL90 76 HYD87 64 TK4-95 49 NEP4-94 2 2 INDFHFL INDFHFL MAD93 70 1 2 PAK87 8 1 5 1 3 8 1 1 1999-2000 2002-03 Indian strains: All human strains - genotype 1 All swine strains - genotype 4 1 69 Goa 45 40 50 40 30 25 the US and strong possibility of zoonotic spread to humans was suspected. Wherever examined, all countries showed anti-HEV positivity in pigs. 10 5 0 6-10 11-15 Age group Affluent Effluent Sewage Plant 30 ! In 1997, swine HEV was discovered in 1998 20 0 35 and bonnet (19.1%) monkeys from India were shown to be anti-HEV positive. 16-25 HSS 25+ LMSS Rural ! In 2001, anti-HEV antibodies were 20 0 Adults ! 2/37 anti-HEV negative transfusion Proportion of sporadic hospitalized hepatitis E cases in Pune recipients sero-converted, 4 and 5 weeks post-transfusion. Though high mortality in pregnant women is the characteristic feature of hepatitis E, in sporadic situation, nonpregnant women as well as men were shown to succumb to fulminant hepatitis E. 100 90 80 70 60 40 30 10 ! Transfusion associated hepatitis E Risk factors Multivariate analysis showed that age > 15 yrs (5.7 fold), lower middle socioeconomic status (2.4 fold) and are well water usage (1.9 fold) important risk factors for contracting infection. Transmission Water contamination Leaky water/drainage pipelines running in close proximity or other means of contamination at the source of water reservoirs results in explosive outbreaks. 200 100 0 0 6-10 11-15 AGE GROUP 16-25 1982 1992 % POSITIVE 0.2 0.4 0.6 0.8 300 200 100 0 0 1 1998 0.2 60 40 20 0 0 0.2 0.4 0.6 0.6 Optcal Density (ELISA) 11-15 AGE GROUP 16-25 1983 0.8 1 25+ Pune HSS urban 110 0 0 0.2 0.4 0.6 Optcal Density (ELISA) In contrast to other countries, different genotypes circulate in humans (genotype-I, 1976-2004) and pigs (genotype IV, 1985-2000) in India. 80 70 60 50 40 30 20 10 0 6-10 11-15 AGE GROUP 70 16-25 1982 The complete genome of Indian swine HEV was sequenced. 25+ 1998 71 1 100 100 90 0.8 200 Anti-HEV positivity documented in pigs from states of Maharashtra, Karnataka and Andaman & Nicobar Islands. Mean age of pigs for seroconversion was 4.8 + 1.6 months. 1998 1 300 Swine HEV 6-10 0.8 Rodents Dogs 110 100 90 80 70 60 50 40 30 20 10 0 0.4 Optical Density (ELISA) Optical Density (ELISA) 25+ Pune didtrict, rural During epidemics, the estimated ratio of clinical:subclinical infections based on serology was shown to be 1:26 in pregnant women. 300 0 may occur in countries endemic for HEV. Intra-familial spread Based on the study of 49 families during an epidemic of hepatitis E, the intra-familial spread was shown to be negligible. Cattle Pigs 50 20 % POSITIVE Children detected in pigs, dogs, cattle, rodents, and chickens from India. Goats were negative. Pune urban LMSS No of Pigs 5 110 No of Dogs 10 % POSITIVE Parenteral transmission ! 1.5% (3/200) voluntary blood donors from Pune positive for HEV RNA. 15 No of Cattle 15 HEV as zoonosis ! In 1994, wild caught rhesus (36.7%) 60 % ANTI-HEV+VE % PCR +ve 20 10 % HEV Cases HEV antibody prevalance in and around Pune About 15% of neat sewage samples collected year round were HEV RNA positive, 7-fold higher risk of infection in sewage workers was documented. No of Rodents Initial studies conducted by NIV showed that ~ 60% of the sporadic hepatitis cases among adults are of NANB type. With the availability of ELISA for IgM-anti-HEV detection, over 40% of sporadic cases among adults were diagnosed as hepatitis E. Delta & other Hepatitis Viruses ! HDV is not an important cause of viral Hepatitis Delta Virus (HDV) hepatitis in western India. ! In 1987, normal immunoglobulin HBsAg preparations were shown to be antidelta positive. d Ag 35 nm TT virus d RNA Hepatitis G Virus (HGV) ! Discovered in 1995. ! Disease potential yet to be confirmed. ! HGV does not contribute to sporadic Ÿ Defective RNA virus. Ÿ Requires HBV multiplication. replication for Non-A, Non-E hepatitis in India. its 72 ! Not an important cause of chronic or fulminant hepatitis. Ÿ Occurs as co- or super-infection with HBV. 62 ! The virus belongs to the family Flaviviridae. Ÿ Leads to severe course of liver disease. ! Discovered in 1997 in Japan. ! Disease potential questionable. ! Parenteral and enteric modes of Phylogenetic analysis of HGV isolates (western India) 91 Ÿ Though HDV replication is HBV dependent, its prevalence is not a simple function of HBV prevalence. Ÿ Parenterally transmitted. IND2 IND5 Peru-72442 IND3 IND4 IND9 IND21 64 Germany-532 87 US7 IND1 69 IND6 94 IND20 HGV-VT58 GHP7 HGV-VT10 88 TH-K10 94 75 HGV-MY67 CHN-NJ1 KR3 TH-T80 III NU60 GHP2 65 Kenya 98 GA9 GA22 IV Zair9 94 Ed3 98 transmission. The virus DNA virus, belong to family Parvoviridae. I II 0.02 Prevalence of anti-delta positivity C2 64 80 Fulminant Hepatitis Prevalence of HGV RNA Sporadic Acute Viral Hepatitis 79 Anti - delta virus antibodies were detected only in blood dooners Rural Area Adults Paid plasma donors NIV-50 NIV-52 64 NIV-49 NIV-53 NIV-74 NIV-51 NIV-69 NIV-70 68 F5 NIV-63 NIV-46 NIV-66 NIV-47 NIV-73 75 NIV-67 54 NIV-75 NIV-68 99 NIV-71 NIV-76 N22 99 NIV-72 93 96 TTVCHN1 TTV33 MONG969 1b 66 TX011 91 99 Be7 BLDN20 A3 3 JaM53 JaM18 JaM28 99 Hemophiliacs Patients suffering from FHF Mentally Compromised Children Voluntary Blood Donors Voluntary Donors Commercial Donors 0 0 1 2 3 4 5 6 7 2 4 6 8 10 12 14 16 18 % HGV RNA Positivity % anti-delta Positivity 76 2 H4 C1 75 NIV-48 0.05 Non-A-E acute viral hepatitis patients Leprosy Patients CK7 JaM21 A4 93 Patients suffering from liver disease(s) Children 5 TS003 53 99 Institutionalised Children 77 1 4 56 Rural Area Children 1a Phylogenetic analysis showed presence of genotypes 1, 1a and 2. 6 TTV DNA positivity ! Though high prevalence of TTV DNA was recorded, no disease association could be shown. ! Ten percent neat sewage samples were TTV DNA positive. ! Sewage treatment did not reduce TTV DNA positivity. HBsAg Carriers HBV-DNA HCV-RNA Negative CLD Patients HBV-DNA Positive CLD Patients CLD Patients Patients undergoing Haemodialysis Hemophiliacs Paid plasma donors Voluntary Blood Donors 0 5 10 15 20 25 30 % TTV DNA Positivity Non-A to E agents ! Despite use of sensitive and specific serological and molecular assays, all acute viral hepatitis cases cannot be diagnosed. ! Non-B, non-C chronic hepatitis cases continue to occur. ! An epidemic of enterically transmitted non-A, non-E hepatitis in a tribe of Andaman and Nicobar islands in December 1987 was investigated by NIV. Subsequently shown to be TTV DNA and HGV RNA negative. So far, no etiologic agent identified. Transmission experiments in rhesus monkeys were unsuccessful. 78