Canadian Journal of Cardiology 27 (2011) 27–30
Society Guidelines
Canadian Cardiovascular Society Atrial Fibrillation
Guidelines 2010: Implementing GRADE and Achieving
Consensus
Anne M. Gillis, MD, FRCPC,a Allan C. Skanes, MD, FRCPC,b and the CCS Atrial Fibrillation
Guidelines Committeec
Department of Cardiac Sciences, University of Calgary and Libin Cardiovascular Institute of Alberta, Calgary, Alberta, Canada
b
Division of Cardiology, University Hospital, University of Western Ontario, London, Ontario, Canada
c
For a complete listing of committee members, see page 30.
ABSTRACT
O
ED
a
RÉSUMÉ
Dans cet article, nous décrivons le processus de mise à jour des lignes
directrices de 2010 en matière de fibrillation auriculaire (FA) de la Société
Canadienne de Cardiologie. L’élaboration des lignes directrices repose sur
le système d’évaluation Grading of Recommandations Assessment, Development and Evaluation (GRADE). Le système d’évaluation GRADE distingue la qualité de la preuve (très faible, faible, moyenne ou élevée) de la
force des recommandations (forte ou conditionnelle, i.e. faible). Le système d’évaluation GRADE permet de reconnaître les valeurs et les préférences en ce qui a trait à la prestation des soins cliniques, ainsi que les
coûts des interventions, pour déterminer la force des recommandations.
Les relations du groupe d’experts avec l’industrie ou autres conflits
d’intérêts potentiels ont été divulguées initialement et annuellement.
Chaque recommandation a été approuvée par au moins les deux tiers du
groupe d’experts (ceux qui étaient en conflit d’intérêt se sont abstenus de
voter sur certaines recommandations).
EM
BA
R
G
This article describes the process of the Canadian Cardiovascular Society
2010 atrial fibrillation (AF) guidelines update. Guideline development was
based on the GRADE (Grading of Recommendations Assessment, Development and Evaluation) system of evaluation. GRADE separates the quality of evidence (very low, low, moderate, or high quality) from the strength
of recommendations (strong or conditional, ie, weak). GRADE allows acknowledgement of values and preferences in the provision of clinical care
as well as costs of interventions in determining the strength of recommendations. Disclosures of relationships with industry or other potential
conflicts of interest were reported at the outset and annually. Each recommendation was approved by at least a two-thirds majority of the voting
panel (those with a significant conflict recusing themselves from voting on
those specific recommendations).
Atrial fibrillation (AF) is the most common sustained arrhythmia treated in clinical practice and is associated with
substantial morbidity. Indeed, the lifetime risk of developing AF in individuals older than 40 years is 1 in 4.1 The
Canadian Cardiovascular Society (CCS) last published a set
of recommendations on the diagnosis and management of
AF in 2005.2 Since then, major advances in the management
of AF have occurred, including the results of clinical trials
providing guidance on pharmacologic therapies for management of AF,3-5 antithrombotic therapies for prevention of
systemic thromboembolism,6,7 the continuing evolution of
catheter ablation for treatment of AF,8-10 and the development of a simple semiquantitative scale that closely approximates patient-reported subjective measures of quality of life
Received for publication November 4, 2010. Accepted November 11, 2010.
Corresponding author: Dr Anne M. Gillis, Department of Cardiac Sciences, The University of Calgary, 3280 Hospital Dr NW, Calgary, Alberta,
Canada T2N 4N1. Tel: 403-220-6841; fax: 403-270-0313.
E-mail: mgillis@ucalgary.ca
The disclosure information of the authors and reviewers are available
from the CCS on the following Web sites: www.ccs.ca and www.
ccsguidelineprograms.ca.
This statement was developed following a thorough consideration of medical literature and the best available evidence and clinical experience. It
represents the consensus of a Canadian panel comprised of multidisciplinary experts on this topic with a mandate to formulate disease-specific
recommendations. These recommendations are aimed to provide a reasonable and practical approach to care for specialists and allied health professionals obliged with the duty of bestowing optimal care to patients and
families, and can be subject to change as scientific knowledge and technology advance and as practice patterns evolve. The statement is not intended
to be a substitute for physicians using their individual judgment in managing clinical care in consultation with the patient, with appropriate regard
to all the individual circumstances of the patient, diagnostic and treatment
options available and available resources. Adherence to these recommendations will not necessarily produce successful outcomes in every case.
A complete list of the Primary and Secondary Panel Members are listed
in the Appendix on page 30.
0828-282X/$ – see front matter © 2011 Canadian Cardiovascular Society. Published by Elsevier Inc. All rights reserved.
doi:10.1016/j.cjca.2010.11.003
28
Canadian Journal of Cardiology
Volume 27 2011
Table 1. GRADE: Rating quality of evidence
Quality
Comments
High
Future research unlikely to change confidence in estimate of
effect; eg, multiple well-designed, well-conducted clinical
trials
Further research likely to have an important impact on
confidence in estimate of effect and may change the estimate;
eg, limited clinical trials, inconsistency of results or study
limitations
Further research very likely to have a significant impact on
the estimate of effect and is likely to change the estimate; eg,
small number of clinical studies or cohort observations
The estimate of effect is very uncertain; eg, case studies,
consensus opinion
Moderate
Low
Very low
Modified and reprinted with permission from Guyatt, et al.17
GRADE, Grading of Recommendations Assessment, Development, and
Evaluation.
O
ED
guage literature, using MEDLINE or Cochrane library
searches and a critical appraisal of the evidence focusing predominantly on the results of randomized clinical trials and
systematic reviews. In the absence of such data, recommendations were based on the results of large cohort studies or smaller
clinical studies. The recommendations were finalized by informed consensus through one face-to-face meeting, conference calls, e-mail correspondence, and final review by all members of the primary panel. Specifically, the writing group
presented each preliminary recommendation with its attendant
supportive evidence in summary form. Following discussion,
an anonymous vote was obtained in which a two-thirds majority was considered consensus. Failing consensus, further discussion was directed at areas of divergence of opinion until either
consensus was reached or it was deemed by the chair(s) that
consensus would not be reached and a recommendation could
not be made. A two-thirds majority was achieved in all cases.
The primary panelists were principally responsible for the document, but an independent secondary panel reviewed the recommendations and provided feedback. All members of the
primary panel formally approved the final document prior to
submission to the Guidelines Committee and CCS Executive
for review and approval.
As outlined in a separate communication, this is the first
CCS Guidelines Panel to use the GRADE (Grading of Recommendations Assessment, Development and Evaluation) system
of evaluation,13,14 replacing the American College of Cardiology and American Heart Association scale for level of evidence
that was used previously.15 In the past, guidelines have been
criticized as being inconsistent in how they rate quality of evidence and strength of recommendations, which may lead to
confusion in interpretation of the recommendations and failure to adhere to the guidelines.16 GRADE (www.gradeworkinggroup.org) was created by a group of international guideline
developers, including a large Canadian representation to address the shortcomings of other rating systems.17-21 The approach separates the quality of evidence (very low, low, moderate, or high quality; see Table 1), from the strength of
recommendations (strong or conditional, ie, weak; see Table
2). GRADE allows acknowledgment of values and preferences
in the provision of clinical care, as well as of the cost of therapies, in determining the strength of recommendations.
GRADE has already been adopted by more than 45 international organizations, including the World Health Organiza-
EM
BA
R
G
in AF.11 In 2009, the CCS convened a primary panel of
experts to undertake a comprehensive review of current
knowledge and management strategies in the field of AF and
to develop an up-to-date evidence-based set of recommendations, easily available to primary care physicians, emergency room physicians, internists, and cardiologists, on the
diagnosis and management of patients with AF. The guidelines are broadly applicable across a spectrum of practice
environments. It is expected that optimized management of
AF may improve quality of life and reduce rates of stroke
and hospitalization for AF-related causes across all levels of
care in a large population of patients.
Simultaneous with the evolution in treatments for AF, the
CCS has been implementing a unique Canadian knowledge
translation (KT) model for disseminating guidelines.12,13
Known as the CCS closed-loop model for KT, it has the aim of
improving the uptake and integration of guidelines into clinical practice. The model involves assembling a multidisciplinary
primary panel to draft guidelines and then using a multipronged, multimedia approach to dissemination. Dissemination strategies involve regional and national face-to-face, interactive, case-based workshops and a dedicated Web site
featuring practical tools and tips for end users as well as synchronous and asynchronous e-learning programs. Feedback
from KT program participants and guideline end users drives
the selection and development of new content for subsequent
annual guideline updates, which are then disseminated and
evaluated as part of a regular annual cycle. This cyclical approach to guideline development, dissemination, and evaluation results in a powerful compendium of guidelines that address a specific topic and are highly relevant to and highly
valued by care providers. The CCS experienced success with
this model through applying it to heart failure beginning in
2005. As AF emerged as a major topic requiring updated, comprehensive, multidisciplinary guidelines, the CCS has embarked on this second closed-loop KT program.
A primary working group was formed and met face-toface in October 2009 to agree on the process of achieving
consensus, to address issues related to real or perceived conflict of interest related to specific recommendations, to discuss the process of weighing the strength of a recommendation and the quality of evidence supporting the recommendation, to identify the full membership of the primary
panel, to finalize topics for guideline development, and to
develop writing groups for each topic. Conflicts were disclosed prior to forming the writing groups. The Appraisal of
Guidelines for Research and Evaluation instrument was
used to guide primary panel structure and guideline development.14 Membership of the primary panel was expanded
to include wide representation (from primary care, internal
medicine, emergency medicine, and general cardiology, in
addition to cardiac electrophysiology) and to increase the
proportion of panel members having no conflict of interest
or relationships with industry to 5 of 19 members (26%).
Writing groups were developed with specific attention to
content expertise and conflict of interest. It was decided that
each recommendation must be approved by a two-thirds
majority of the voting panel (those with a significant conflict
recusing themselves from voting on those specific recommendations).
The working groups undertook a review of the English lan-
Gillis et al.
Implementing GRADE
29
Table 2. Factors determining the strength of the recommendation
Factor
Comment
Quality of evidence
The higher the quality of evidence, the greater the probability that a strong recommendation is indicated; eg, strong
recommendation that patients with AF at moderate to high risk of stroke be treated with oral anticoagulants.
The greater the difference between desirable and undesirable effects, the greater the probability that a strong recommendation is
indicated; eg, strong recommendation that patients with AF ⱖ 48-h duration receive oral anticoagulation therapy for at least 3
wk prior to planned cardioversion and 4 wk following.
The greater the variation or uncertainty in values and preferences, the higher the probability that a conditional
recommendation is indicated; eg, aspirin may be a reasonable alternative to oral anticoagulant therapy in patients at low risk of
stroke.
The higher the cost, the lower the likelihood that a strong recommendation is indicated; eg, conditional recommendation for
catheter ablation as first-line therapy for AF.
Difference between desirable
and undesirable effects
Values and preferences
Cost
AF, atrial fibrillation.
Modified and reprinted with permission from Guyatt, et al.17
10. Wilber DJ, Pappone C, Neuzil P, et al. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA 2010;303:333-40.
11. Dorian P, Guerra PG, Kerr CR, et al. Validation of a new simple scale to
measure symptoms in atrial fibrillation: the Canadian Cardiovascular Society Severity in Atrial Fibrillation scale. Circ Arrhythm Electrophysiol
2009;2:218-24.
12. Graham MM, Pullen C. Renovating CCS guidelines and position statements: a new foundation. Can J Cardiol 2010;26:233-5.
R
G
1. Etiology and Initial Investigations
2. Management of Recent-Onset Atrial Fibrillation and
Flutter in the Emergency Department
3. Rate and Rhythm Management
4. Catheter Ablation for Atrial Fibrillation/Atrial Flutter
5. Surgical Therapy
6. Prevention of Stroke and Systemic Thromboembolism
in Atrial Fibrillation and Flutter
7. Prevention and Treatment of Atrial Fibrillation Following Cardiac Surgery
9. Cappato R, Calkins H, Chen SA, et al. Updated worldwide survey on the
methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol 2010;3:32-8.
O
ED
tion, the American College of Physicians, the Cochrane Collaboration, the American College of Chest Physicians, and
many others.
The updated guidelines are published in 7 articles:
EM
References
BA
A specific chapter on atrial tachyarrhythmias in the congenital heart disease population was not undertaken at this time
but is planned for a future update.
1. Lloyd-Jones DM, Wang TJ, Leip EP, et al. Lifetime risk for development
of atrial fibrillation: the Framingham Heart Study. Circulation 2004;110:
1042-6.
2. Kerr C, Roy D. Canadian Cardiovascular Society Consensus Conference:
Atrial fibrillation 2004 executive summary. Available at: http://
www.ccs.ca/download/consensus_conference/consensus_conference_
archives/2004_Atrial_Fib_ES.pdf. Accessed November 11, 2010.
3. Roy D, Talajic M, Nattel S, et al. Rhythm control versus rate control for
atrial fibrillation and heart failure. N Engl J Med 2008;358:2667-77.
4. Van Gelder IC, Groenveld HF, Crijns HJ, et al. Lenient versus strict rate
control in patients with atrial fibrillation. N Engl J Med 2010;362:1363-73.
5. Hohnloser SH, Crijns HJ, van Eickels M, et al. Effect of dronedarone on
cardiovascular events in atrial fibrillation. N Engl J Med 2009;360:668-78.
6. Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in
patients with atrial fibrillation. N Engl J Med 2009;361:1139-51.
7. Connolly SJ, Pogue J, Hart RG, et al. Effect of clopidogrel added to aspirin
in patients with atrial fibrillation. N Engl J Med 2009;360:2066-78.
8. Nair GM, Nery PB, Diwakaramenon S, et al. A systematic review of
randomized trials comparing radiofrequency ablation with antiarrhythmic
medications in patients with atrial fibrillation. J Cardiovasc Electrophysiol
2009;20:138-44.
13. Kerr CR. CCS guidelines and position statements are important, but do
they make the GRADE? Can J Cardiol 2010;26:177-8.
14. The AGREE Collaboration. Development and validation of an international appraisal instrument for assessing the quality of clinical practice
guidelines: the AGREE project. Qual Saf Health Care 2003;12:18-23.
15. Fuster V, Rydén LE, Cannom DS, et al. ACC/AHA/ESC 2006 guidelines for
the management of patients with atrial fibrillation: full text: a report of the
American College of Cardiology/American Heart Association Task Force on
practice guidelines and the European Society of Cardiology Committee for
Practice Guidelines (Writing Committee to Revise the 2001 guidelines for the
management of patients with atrial fibrillation) developed in collaboration
with the European Heart Rhythm Association and the Heart Rhythm Society.
Circulation 2006;114:e257-354.
16. Sniderman AD, Furberg CD. Why guideline-making requires reform.
JAMA 2009;301:429-31.
17. Guyatt GH, Oxman AD, Vist G, et al. GRADE: an emerging consensus
on rating quality of evidence and strength of recommendations. BMJ
2008;336:924-6.
18. Guyatt GH, Oxman AD, Kunz R, et al. GRADE Working Group. Rating
quality of evidence and strength of recommendations: what is “quality of
evidence” and why is it important to clinicians? BMJ 2008;336:995-8.
19. Schünemann HJ, Oxman AD, Brozek J, et al. Grading quality of evidence
and strength of recommendations for diagnostic tests and strategies. BMJ
2008;336:1106-10.
20. Guyatt GH, Oxman AD, Kunz R, et al. Rating quality of evidence and
strength of recommendations: incorporating considerations of resources
use into grading recommendations. BMJ 2008;336:1170-3.
21. Guyatt GH, Oxman AD, Kunz R, et al. Rating quality of evidence and
strength of recommendations: going from evidence to recommendations.
BMJ 2008;336:1049-51.
30
Canadian Journal of Cardiology
Volume 27 2011
Appendix 1. Primary and secondary panel members
Primary panel members
Cochair
Cochair
Member
Member
Member
Member
Member
Member
Member
Member
Member
Member
Member
Member
Member
Member
Mario Talajic, MD, FRCP(C)
Teresa Tsang, MD, FRCP(C)
Atul Verma, MD, FRCP(C)
Jan Brozek, MD, PhD
Grant Stotts, MD, FRCP(C)
Member
Member
Member
Special Collaborator
Special Collaborator
Dept of Cardiac Sciences, University of Calgary, Libin Cardiovascular Institute of Alberta
Division of Cardiology, University of Western Ontario
Division of Cardiology, Department of Medicine, McMaster University
Faculty of Medicine, University of British Columbia
Division of Cardiology, Dalhousie University
Division of Cardiology, University of Toronto
Division of Cardiology, Medicine Department, McMaster University
Electrophysiology Service, Montreal Heart Institute, Université de Montréal
Division of Cardiology, University of Alberta
University of Calgary, Libin Cardiovascular Institute of Alberta
Montreal Heart Institute, Université de Montréal
Montreal Heart Institute, Université de Montréal
Division of Cardiology, Dalhousie University
Department of Cardiac Sciences, and Physiology & Pharmacology, University of Calgary
Representative of The College of Family Physicians of Canada, Ancaster, Ontario
Department of Emergency Medicine, Ottawa Hospital Research Institute, University of
Ottawa
Montreal Heart Institute, Université de Montréal
Division of Cardiology, University of British Columbia
Heart Rhythm Program, Southlake Regional Health Centre
Departments of Clinical Epidemiology & Biostatistics and Medicine. McMaster University
University of Ottawa, The Ottawa Hospital. Representative of the Canadian Stroke Network
Secondary panel members
Division of Cardiology, University of Western Ontario,
St. John’s, New Brunswick
Department of Cardiology, McGill University Health Center
Division of Cardiology, Brampton Civic Hospital
St. Paul’s Hospital Heart Centre, University of British Columbia
St. Paul’s Hospital Heart Centre, University of British Columbia
Division of Cardiac Surgery, University of Western Ontario
Department of Medicine, Langley Memorial Hospital, Langley, BC
Department of Cardiac Sciences, University of Calgary, Libin Cardiovascular Institute of
Alberta
R
G
Member
Member
Member
Member
Member
Member
Member
Member
Member
EM
BA
Malcolm Arnold, MD, FRCP(C)
David Bewick, MD, FRCP(C)
Vidal Essebag, MD, MSc, FRCP(C)
Milan Gupta, MD, FRCP(C)
Brett Heilbron, MBChB, FRCP(C)
Charles Kerr, MD, FRCP(C),
Bob Kiaii, MD, FRCS(C)
Jan Surkes, BA (hon) MD FRCP(C)
George Wyse, MD, PhD, FRCP(C)
O
ED
Anne M. Gillis, MD, FRCP(C)
Allan Skanes, MD, FRCP(C)
Stuart Connolly, MD, FRCP(C)
John Cairns, MD, FRCP(C),
Jafna Cox, BA, MD, FRCP(C), FACC
Paul Dorian, MD, MSc. FRCP(C)
Jeff Healey, MD, FRCP(C)
Laurent Macle, MD, FRCP(C)
Sean McMurty, MD, PhD, FRCP(C)
Brent Mitchell, MD, FRCP(C)
Stanley Nattel, MD, FRCP(C)
Pierre Page, MD, FRCPS
Ratika Parkash, MD, MSc, FRCP(C)
P. Timothy Pollak, MD, PhD FRCP(C)
Michael Stephenson, MD, CCFP, FCFP
Ian Stiell, MD, MSc, FRCP(C)
Canadian Journal of Cardiology 27 (2011) 31–37
Society Guidelines
Canadian Cardiovascular Society Atrial Fibrillation
Guidelines 2010: Etiology and Initial Investigations
Jeff S. Healey, MD, MSc,a Ratika Parkash, MD, MSc,b Tim Pollak, MD,c Teresa Tsang, MD,d
Paul Dorian, MD, FRCPC,e and the CCS Atrial Fibrillation Guidelines Committeef
Population Health Research Institute, McMaster University, Hamilton, Ontario, Canada
b
Dalhousie University, Halifax, Nova Scotia, Canada
c
d
e
f
University of Calgary, Calgary, Alberta, Canada
University of British Columbia, Vancouver, British Columbia, Canada
St. Michael’s Hospital and University of Toronto, Toronto, Ontario, Canada
O
ED
a
For a complete listing of committee members, see Gillis AM, Skanes AC. Canadian Cardiovascular Society Atrial Fibrillation Guidelines
2010: Implementing GRADE and achieving consensus. Can J Cardiol 2011;27:27-30.
ABSTRACT
RÉSUMÉ
L’évaluation initiale des patients présentant une fibrillation auriculaire (FA) devrait comprendre un questionnaire détaillé, un examen
physique et un bilan sanguin de base. Cette première évaluation a
pour but d’identifier l’étiologie (et particulièrement les causes réversibles) de la FA, de décrire le type de FA (paroxystique, persistante ou permanente), d’évaluer le degré de symptomatologie du
patient, d’identifier ses co-morbidités et d’évaluer son risque tromboembolique. L’indication d’investigations supplémentaires et le
plan de traitement spécifique au patient dépendent de cette évaluation initiale qui doit être complète et systématique.
EM
BA
R
G
The initial evaluation of patients with atrial fibrillation (AF) should
include a comprehensive history, physical examination, and initial investigations. The initial evaluation of patients with AF has several
important purposes, including the identification of the etiology of AF,
particularly the identification of reversible causes of AF; the description of the pattern of AF; the assessment of the degree of symptomatic
impairment due to AF; the assessment of the thromboembolic risk of
the patient; and the identification of common comorbidities. Additional investigations may then be undertaken, with the decision guided
by the initial evaluation. A comprehensive and systematic initial evaluation forms the foundation for a patient-specific plan for the management of AF.
Initial Evaluation of AF
The initial evaluation of a patient with atrial fibrillation
(AF) should consist of a comprehensive history (including social, drug, and family history), physical examination, and initial investigations (Table 1). This evaluation has many important purposes, including assessing the degree of symptomatic
impairment due to AF, developing a therapeutic strategy for
symptom relief, assessing and managing thromboembolic risk,
establishing prognosis, and, where possible, identifying the underlying etiology of AF. The identification of the etiology of AF
during the initial investigation is particularly important for
several reasons:
Received for publication November 9, 2010. Accepted November 9, 2010.
on this topic with a mandate to formulate disease-specific recommendations.
These recommendations are aimed to provide a reasonable and practical approach to care for specialists and allied health professionals obliged with the
duty of bestowing optimal care to patients and families, and can be subject to
change as scientific knowledge and technology advance and as practice patterns
evolve. The statement is not intended to be a substitute for physicians using
their individual judgment in managing clinical care in consultation with the
patient, with appropriate regard to all the individual circumstances of the
patient, diagnostic and treatment options available and available resources.
Adherence to these recommendations will not necessarily produce successful
outcomes in every case.
Corresponding author: Jeff S. Healey, Population Health Research Institute, McMaster University, DBCVSRI Building, Hamilton Health SciencesGeneral Site, 237 Barton St E, Room C3-121, Hamilton, Ontario, L8L 2X2
Canada. Tel.: 905-527-0271, ext 40319; fax: 905-523-9165.
Email address: Jeff.Healey@phri.ca
The disclosure information of the authors and reviewers is available from the
CCS on the following Web sites: www.ccs.ca and www.ccsguidelineprograms.ca.
This statement was developed following a thorough consideration of medical literature and the best available evidence and clinical experience. It represents the consensus of a Canadian panel comprised of multidisciplinary experts
0828-282X/$ – see front matter © 2011 Canadian Cardiovascular Society. Published by Elsevier Inc. All rights reserved.
doi:10.1016/j.cjca.2010.11.015
32
Canadian Journal of Cardiology
Volume 27 2011
Values and preferences. This recommendation places a
high value on a comprehensive evaluation of patients with
AF and a lower value on initial costs to the health care
system.
Documentation of AF and Its Characteristics
It is incumbent upon the physician to document AF in at
least one electrocardiogram lead, as the perception of “irregularly irregular” palpitations may be the result of a variety of
arrhythmias, including atrial tachycardia, atrial flutter, premature atrial and/or ventricular contractions, or nonarrhythmic
causes.
The predominant pattern of AF should be determined, as
this is helpful for directing therapy:1
1. First detected AF
2. Paroxysmal: AF is self-terminating within 7 days of recognized onset
3. Persistent: AF is not self-terminating within 7 days or is
terminated electrically or pharmacologically or
4. Permanent: AF in which cardioversion has failed or in
which clinical judgment has led to a decision not to
pursue cardioversion
One may not be able to identify the pattern of AF at the
time of initial presentation, and the pattern may change over
time. An assessment of the nature and severity of symptoms
and their impact on quality of life should also be performed.
Symptoms associated with AF are highly variable and may include palpitations, dyspnea, dizziness, weakness, or chest pain.2
The frequency and duration of symptoms vary, as can the severity, with some patients being truly asymptomatic and others
having debilitating symptoms.2 The impact of these symptoms
on lifestyle as well as a record of emergency department visits,
hospital admissions, and cardioversions should be made, along
with a record of all prior interventions (eg, drug therapy, catheter ablation, etc) for AF.
Symptoms at the termination of paroxysms should be
sought and if present, symptom–rhythm correlation can be
made using an ambulatory electrocardiogram (Holter monitor,
event monitor, or loop recorder). Patients with sick sinus syndrome often have sinus pauses, particularly following the termination of AF, which may limit the use of rate- or rhythmcontrolling medications and may require the use of permanent
pacing. Any supraventricular tachycardia (SVT), including
atrial tachycardia and atrial flutter, can lead to the development
of AF, and successful ablation of the underlying SVT may
eliminate the associated AF.3,4 Therefore, it is important to
elicit and investigate any history of regular palpitations. This
can be further explored using ambulatory electrocardiographic
monitoring.
EM
BA
R
G
History and physical examination
Establish pattern (new onset, paroxysmal, persistent, or
permanent)
Establish severity (including impact on quality of life)
Identify etiology
Identify reversible causes (hyperthyroidism, ventricular pacing,
supraventricular tachycardia, exercise, etc)
Identify risk factors whose treatment could reduce recurrent AF or
improve overall prognosis (ie, hypertension, sleep apnea, left
ventricular dysfunction, etc)
Take social history to identify potential triggers (ie, alcohol, intensive
aerobic training, etc)
Elicit family history to identify potentially heritable causes of AF
(particularly in lone AF)
Determine thromboembolic risk
Determine bleeding risk to guide appropriate antiplatelet or
antithrombotic therapy
Review prior pharmacologic therapy for AF, both for efficacy and for
adverse effects
Measure blood pressure and heart rate
Determine patient height and weight
Comprehensive precordial cardiac examination and assessment of
jugular venous pressure and carotid and peripheral pulses to
detect evidence of structural heart disease
12-Lead electrocardiogram
Document presence of AF by electrocardiography
Assess for structural heart disease (myocardial infarction, ventricular
hypertrophy, atrial enlargement, congenital heart disease) or
electrical heart disease (ventricular preexcitation, Brugada
syndrome)
Identify risk factors for complications of therapy for AF (conduction
disturbance, sinus node dysfunction, or repolarization);
document baseline PR, QT, or QRS intervals
Echocardiogram
Document ventricular size, wall thickness, and function
Evaluate left atrial size (if possible, left atrial volume)
Exclude significant valvular or congenital heart disease
(particularly atrial septal defects)
Estimate ventricular filling pressures and pulmonary arterial
pressure
Complete blood count, coagulation profile, renal, thyroid, and liver
function
Fasting lipid profile, fasting glucose
O
ED
Table 1. Baseline evaluation of atrial fibrillation for all patients
1. To identify risk factors for AF, which, if treated, could
reduce or eliminate the occurrence of further AF
2. To identify important risk factors, which, if treated,
could improve the overall outcome of the patient, independent of AF
3. To aid in assessing the prognosis of AF in the individual
patient
4. To assist in the selection of optimal AF therapy in the
individual patient
RECOMMENDATION
All patients with AF should undergo a complete history
and physical examination, electrocardiogram, echocardiogram, and basic laboratory investigations. Details are highlighted in Table 1 (Strong Recommendation, Low-Quality
Evidence).
Other ancillary tests should be considered under specific
circumstances. Details included in Table 2 (Strong Recommendation, Low-Quality Evidence).
Evaluation of the Impact of AF on Quality of Life
AF causes a greater degree of impairment of quality of life
in most patients than is generally appreciated. Although
rarely life threatening, AF can cause moderate and sometimes severe distress and substantially alter everyday functioning. In a referral practice, a majority of patients have a
quality of life that is similar to that of patients following
Healey et al.
CCS Atrial Fibrillation Etiology and Initial Investigations
33
Table 2. Evaluation of quality of life (QOL) using the CCS SAF scale*
Impact on quality of life
Class 0
Class 1
Class 2
Class 3
Class 4
Asymptomatic
Minimal effect on QOL
Minor effect on QOL
Moderate effect on QOL
Severe effect on QOL
* The intent of the CCS SAF scale is to capture AF-related symptoms and
QOL. However, the scale evaluates not only symptoms that occur during
episodes of AF but also the consequences of ongoing treatment for AF (ie,
medication-related side effects).
We recommend that the assessment of patient well-being, symptoms, and quality of life be part of the evaluation
of every patient with AF (Strong Recommendation, LowQuality Evidence).
We suggest that the quality of life of the AF patient be
assessed in routine care using the CCS SAF scale (Conditional Recommendation, Low-Quality Evidence).
Table 3. Additional investigations useful in selected cases
Investigation
Chest radiography
Ambulatory electrocardiography
(Holter monitor, event monitor,
loop monitor)
Treadmill exercise test
EM
BA
R
G
myocardial infarction. Impaired quality of life is primarily
the result of symptoms from AF but is also influenced by
side effects from the AF therapies, illness perceptions, and
patient factors such as depression. In the absence of a gold
standard method to treat AF patients, improving quality of
life and relieving symptoms are often the primary goals in
the management of AF patients.
Making treatment plans and assessing treatment effectiveness require a consistent and standardized approach to
measuring the impact of overall quality of life of the AF
syndrome. In 2005, the Canadian Cardiovascular Society
Atrial Fibrillation Guidelines Committee set out to create
and validate a standard approach to assessing overall quality
of life in AF patients, by developing the Severity in Atrial
Fibrillation (SAF) scale (Table 2). This semiquantitative
scale ranges from 0 (no impact of AF or its treatment on
overall quality of life and patient functioning) to SAF 4
(resulting in a severe impairment of functioning and overall
quality of life). A multicentre Canadian study has shown
that the results of this scale correlate well with previously
validated symptom scores and generic measures of quality of
life and that it can be easily applied by a variety of caregivers
at the beside with minimal training.2,5,6
An increasing recognition that the presence of AF on an
electrocardiogram or the frequency and duration of episodes of
AF (“the AF burden”) are poorly correlated with long-term
morbidity and overall quality of life has led to an increasing
emphasis on subjective patient-defined outcomes to most effectively assess the usefulness of overall management and specific treatments in AF. An explicit assessment of the effect of AF
on QOL, preferably using a scale such as the SAF scale in every
patient seen with AF, is recommended and can be used as a
baseline to assess the effects of new or changed therapy in individual patients (Table 3). Patients vary widely with respect to
severity of symptoms and overall quality of life related to AF. It
is difficult to give appropriate counsel and weigh risks and
benefits of therapy without an explicit understanding of the
consequences of AF and its treatment on the patient’s wellbeing.
Such an approach serves to emphasize that simply slowing
the ventricular rate under the strategy of rate control or restoring and maintaining sinus rhythm using a strategy of rhythm
control may not necessarily improve patient well-being and
quality of life. Careful evaluation and ongoing reevaluation of
the impact of the disorder and its treatment on overall patient
well-being are required.2
RECOMMENDATION
O
ED
SAF score
Transesophageal echocardiography
Electrophysiological study
Serum calcium and magnesium
Sleep study (ambulatory oximetry
or polysomnography)
Ambulatory blood pressure
monitoring
Genetic testing
Potential role
Exclude concomitant lung
disease, heart failure,
baseline in patients
receiving amiodarone
Document AF, exclude
alternative diagnosis (atrial
tachycardia, atrial flutter,
AVNRT/AVRT,
ventricular tachycardia),
symptom–rhythm
correlation, assess
ventricular rate control
Investigation of patients with
symptoms of coronary
artery disease, assessment
of rate control
Rule out left atrial appendage
thrombus, facilitate
cardioversion in patients
not receiving oral
anticoagulation, more
precise characterization of
structural heart disease
(mitral valve disease, atrial
septal defects, cor
triatriatum, etc)
Patients with documented
regular supraventricular
tachycardia (ie, atrial
tachycardia, AVNRT/
AVRT, atrial flutter) that
is amenable to catheter
ablation
In cases of suspected
deficiency (ie, diuretic use,
gastrointestinal losses),
which could influence
therapy (ie, sotalol)
In patients with symptoms of
obstructive sleep apnea or
in select patients with
advanced symptomatic
heart failure
In cases of borderline
hypertension
In rare cases of apparent
familial AF (particularly
with onset at a young age)
with additional features of
conduction disease,
Brugada syndrome, or
cardiomyopathy
AVNRT/AVRT, atrioventricular nodal reentrant tachycardia/atrioventricular reentrant tachycardia.
34
Canadian Journal of Cardiology
Volume 27 2011
Cardiac causes
Hypertension
Heart failure*
Coronary artery disease with prior myocardial infarction
Left ventricular dysfunction (systolic and diastolic)*
Including hypertrophic, dilated, and restrictive cardiomyopathies
Valvular heart disease
Congenital heart disease* (early repair of atrial septal defect)
Pericardial disease
Postsurgical (particularly cardiac surgery)
Sick sinus syndrome
AF as a result of ventricular pacing*
Supraventricular tachycardia (including Wolff-Parkinson-White
syndrome, atrial tachycardia, atrial flutter, or other)*
Genetic/familial
Noncardiac causes
Obstructive sleep apnea*
Obesity*
Excessive alcohol ingestion (acute or chronic)*
Hyperthyroidism*
Vagally mediated (ie, habitual aerobic training)*
Pulmonary disease (pneumonia, chronic obstructive pulmonary
disease, pulmonary embolism, pulmonary hypertension)
Lone (idiopathic) AF
* Denotes cause for which treatment may prevent the development or
recurrence of AF.
nosis of AF and may influence choices of therapy for both rate
and rhythm control.
Screening history and physical evaluation for obstructive
and nonobstructive sleep apnea should be performed in all
patients, and further testing, such as ambulatory oximetry
or polysomnography, or appropriate referral to a specialist
in sleep medicine should be considered if the history is suggestive of sleep apnea.
EM
BA
R
G
Identification of the Etiology of AF
AF is a disease of advancing age, whose prevalence increases
from 0.1% in patients under age 50 to 10%-15% in those ⬎80
years old.7 This has important public health implications for
the aging Canadian population. In most cases, AF is associated
with underlying heart disease–most commonly, hypertension,
heart failure, left ventricular systolic dysfunction, and valvular
heart disease.8-11 Although these conventional risk factors are
present in ⬎70% of North American patients,12,13 there are
important additional considerations.
First, additional risk factors such as hyperthyroidism,14
Wolff-Parkinson-White syndrome,3,15 and unnecessary ventricular pacing,16-19 although much less prevalent, are important to identify as they have additional deleterious effects and
their treatment could eliminate further AF in affected patients.
Second, because Canada is a country with a significant immigrant population, it is important to remember that in many
patients, AF may be the result of conditions that are much less
common among individuals born in North America, such as
rheumatic heart disease, complicated hypertension, and pericarditis.20 Third, there are emerging data identifying additional conditions such as obesity, sleep apnea. and alcohol intake as risk factors for the development of AF and its
complications.21-23 Finally, there are still approximately 15%20% of AF patients who do not have identifiable comorbidities.24 While these patients would be classified as having “lone”
(idiopathic) AF, some may have a genetic predisposition to AF,
an SVT that leads to the development of AF or have AF as a
result of high vagal tone, such as secondary to intensive aerobic
exercise.25
The underlying etiologic conditions associated with AF
should be determined. In Canada, the most important of
these risk factors is hypertension.11,13 Careful blood pressure measurement should be conducted, as outlined by the
Canadian Hypertension Education Program guidelines for
the diagnosis of hypertension.26,27 Clinicians should pursue
a diagnosis of hypertension in patients with frequent borderline office readings, particularly those with significant
left atrial enlargement or left ventricular hypertrophy. Ambulatory blood pressure monitoring may facilitate this in
patients with paroxysmal AF; however, these devices are
greatly influenced by the variable heart rate during AF, limiting their sensitivity and specificity in patients with persistent or permanent AF.
Particular effort should also be given to identify potentially
reversible causes of AF (Table 4), such as hyperthyroidism and
excessive alcohol. Although only 3.1% of AF patients have
hyperthyroidism, it is still an important example of a treatable
cause.28 Identification of both of these disorders on the patient
history may be particularly difficult in the elderly. Other common, conventional risk factors include coronary artery disease
with prior myocardial infarction, left ventricular systolic dysfunction, and valvular heart disease. Identification of such
structural heart disease is important, as it influences the prog-
Table 4. Potential causes of atrial fibrillation
O
ED
Values and preferences. These recommendations recognize that improvement in quality of life is a high priority
for therapeutic decision making.
RECOMMENDATION
Underlying causes or precipitating factors for AF including hypertension should be identified and treated. Details
are highlighted in Table 3 (Strong Recommendation, HighQuality Evidence).
Values and preferences. This recommendation recognizes that therapy of underlying etiology can improve management of AF and that failure to recognize underlying factors may result in deleterious effects.
Determination of Cardiovascular Risk in AF
AF is associated with a 3- to 6-fold increased risk of stroke or
non– central nervous system (CNS) systemic embolism.10,29-34.
It is thought that ⬇15% of all strokes are due to AF and that
this increases to 25% for patients ⬎80 years old.10 Both oral
anticoagulation and antiplatelet medication reduce the risk of
stroke in patients with AF but are associated with an increased
risk of bleeding.33,35,36 For this reason, several risk stratification schemes have been developed to identify patients with the
highest risk of stroke, in whom the benefit of oral anticoagulant
therapy outweighs the risk of bleeding.37,38 Initial investigation of patients with AF should identify risk factors for stroke,
as this is necessary to help guide the appropriate use of antico-
Healey et al.
CCS Atrial Fibrillation Etiology and Initial Investigations
O
ED
and should be performed in all patients with AF. This will
identify left ventricular hypertrophy or systolic dysfunction,
significant valvular or congenital heart disease, and, rarely,
complications such as left atrial appendage thrombus. All of
these are necessary for making appropriate decisions regarding
the use of rate- and rhythm-controlling agents and anticoagulant medications. An evaluation of left atrial size should also be
conducted, as this provides important information about the
likelihood of AF recurrence or the development of persistent or
permanent AF, which can help guide optimal therapy for
symptom improvement. In certain cases, such as the assessment
of valvular or congenital heart disease or the exclusion of left
atrial appendage thrombus, transesophageal echocardiography
may be required.
Routine blood work should be performed at the time of the
initial evaluation of patients with AF. A complete blood count
and coagulation studies should be performed as they will inform decisions about the use of anticoagulant and antiplatelet
medications. Serum electrolytes and creatinine should also be
determined because antiarrhythmic and newer anticoagulant
medications may be more likely to cause adverse effects in those
with electrolyte disorders or renal insufficiency. Serum creatinine and a urinalysis may also identify chronic kidney disease,
another common complication of hypertension, the most prevalent risk factor for AF. Liver function tests should also be
performed at baseline, both to aid in the identification of excessive alcohol intake and as a baseline for potentially hepatotoxic medications, such as amiodarone, that are frequently administered in the treatment of AF. A lipid profile is
recommended in most patients as part of an overall assessment
of cardiovascular risk.
Ambulatory electrocardiography monitoring is not routinely required but has a number of important purposes, such
as initial documentation of AF, identification of other forms of
SCT, assessment of ventricular rate control, and the correlation
of patient’s symptoms with both rhythm and heart rate. Although not routinely recommended, exercise testing may supplement ambulatory monitoring in certain patients with exercise-related symptoms. Invasive electrophysiological studies
should be considered in those patients with idiopathic AF at a
young age, particularly in those with documented SVT other
than AF or symptoms suggestive of such arrhythmias.
EM
BA
R
G
agulant and antiplatelet medication. Risk factors include a history of stroke, transient ischemic attack, or non-CNS systemic
embolism; hypertension; heart failure; left ventricular ejection
fraction ⱕ35%; increasing age; and diabetes mellitus. Other
moderate risk factors include female gender and peripheral vascular disease.37 Many of these same conditions are also associated with an increased risk of bleeding. The initial evaluation of
patients with AF should also elicit a bleeding history, prior
antiplatelet and anticoagulant use, and degree of INR control39
to aid in the determination of the ideal strategy for stroke prevention. For a full discussion, see Cairns et al.40
The use of stroke risk stratification schemes is undergoing a
period of reevaluation. First, there is increasing appreciation
that the same clinical characteristics that predict stroke also
predict bleeding;41 thus patients with a lower risk of stroke are
also less likely to have bleeding complications of therapy. Second, there are 2 new therapies that have been shown to prevent
stroke in patients with AF: clopidogrel (added to acetylsalicyclic acid [ASA])34 and dabigatran.42 These 2 agents have different bleeding profiles and are substantially easier for patients
to take and have far fewer food and drug interactions than
warfarin, thus changing the risk/benefit equation for stroke
prevention in AF. Regardless of the specific agents used to
prevent stroke and the threshold for their use, the identification
of stroke risk factors remains vital to properly inform therapy.
In contrast, it should be noted the pattern of AF (paroxysmal vs
persistent or permanent) does not influence these decisions.43
Furthermore, the AFFIRM trial strongly suggests that the apparent suppression of AF with antiarrhythmic medications
does not obviate the need for oral anticoagulation in patients
with AF and additional risk factors for stroke.44
Traditionally, the prevention of cardiovascular events in patients with AF has focused on the prevention of stroke and
non-CNS systemic embolism. It should be noted, however,
that in recent clinical trials, the most common adverse cardiovascular event in patients with AF is now the development of
heart failure.34,41,42 Patients with AF also frequently require
hospitalization, and these patients have a particularly high subsequent mortality.45 Thus, the appropriate identification and
treatment of hypertension and asymptomatic left ventricular
systolic dysfunction, as well as the appropriate evidence-based
management of heart failure, are also important in the management of patients with AF.
35
References
The Physical Examination and Initial
Investigations for AF
The physical findings suggestive of AF include an irregular
pulse (that may not be rapid), an irregular jugular venous pulse
with loss of a-wave, and variation in the intensity of the first
heart sound. The physical examination may also uncover
causes of AF, including hypertension, left ventricular systolic
dysfunction, heart failure, valvular heart disease, congenital
heart disease (ie, fixed-split S2 in patient with an atrial septal
defect), or hyperthyroidism.
A number of routine investigations are warranted in all patients presenting with a history of AF (see Table 1). An electrocardiogram is useful both in AF and sinus rhythm. Evidence
of left atrial enlargement, left ventricular hypertrophy, preexcitation, conduction disease, or myocardial infarction should
be sought. A transthoracic echocardiogram is also invaluable
1. Fuster V, Ryden LE, Cannom DS, et al. ACC/AHA/ESC 2006 guidelines
for the management of patients with atrial fibrillation-executive summary:
a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines. J Am Coll Cardiol 2006;48:
854-906.
2. Dorian P, Guerra PG, Kerr CR, et al. Validation of a new simple scale to
measure symptoms in atrial fibrillation: the Canadian Cardiovascular Society Severity in Atrial Fibrillation scale. Circ Arrhythm Electrophsiol
2009;2:213-4.
3. Chen PS, Pressley JC, Tang AS, et al. New observations on atrial fibrillation
before and after surgical treatment in patients with the Wolff-ParkinsonWhite syndrome. J Am Coll Cardiol 1992;19:974-81.
4. Haissaguerre M, Fischer B, Labbe T, et al. Frequency of recurrent atrial
fibrillation after catheter ablation of overt accessory pathways. Am J Cardiol 1992;69:493-7.
36
Canadian Journal of Cardiology
Volume 27 2011
5. Paquette M, Roy D, Talajic MM, et al. Role of gender and personality on
quality-of-life impairment in intermittent atrial fibrillation. Am J Cardiol
2000;86:764-8.
24. Heuzey JY, Breithardt G, Camm AJ, et al. The RECORDAF study: design, baseline data and profile of patients according to chosen treatment
strategy for atrial fibrillation. Am J Cardiol 2010;105:687-93.
6. Reynolds MR, Ellis E, Zimetbaum P. Quality of life in atrial fibrillation:
measurement tools and impact of interventions. J Cardiovasc Electrophysiol 2006;19:762-8.
25. Molina L, Mont L, Marrugat J, et al. Long-term endurance sport practice
increases the incidence of lone atrial fibrillation in men: a follow-up study.
Europace 2008;10:618-23.
7. Kannel WB, Wolf PA, Benjamin EJ. Prevalence, incidence, prognosis,
and predisposing conditions for atrial fibrillation: population-based estimates. Am J Cardiol 1998;82:2N-9N.
26. Hackman DG, Khan NA, Hemmelgarn BR, et al. The 2010 Canadian
Hypertension Education Program recommendations for the management
of hypertension: part 2 - therapy. Can J Cardiol 2010;26:249-58.
8. Benjamin EJ, Levy D, Vaziri SM, et al. Independent risk factors for atrial
fibrillation in a population-based cohort. The Framingham Heart Study.
JAMA 1994;271:840-4.
27. Quinn RR, Hemmelgarn BR, Padwal RS, et al. The 2010 Canadian Hypertension Education Program recommendations for the management of
hypertension: part 1 - blood pressure measurement, diagnosis and assessment of risk. Can J Cardiol 2010;26:241-8.
10. Wolf PA, Dawber TR, Thomas HE Jr, et al. Epidemiologic assessment of
chronic atrial fibrillation and risk of stroke: the Framingham Study. Neurology 1978;28:973-7.
11. Krahn AD. The natural history of atrial fibrillation: incidence, risk factors
and prognosis in the Manitoba Follow-up Study. Am J Med 1995;98:47684.
12. Verdecchia P, Reboldi GP, Gattobigio R, et al. Atrial fibrillation in hypertension. Hypertension 2003;41:218-23.
29. Atrial Fibrillation Investigators. Risk factors for stroke and efficacy of antithrombotic therapy in atrial fibrillation. Arch Intern Med 1994;154:1449-57.
30. Wolf PA, Abbot RD, Kannel WB. Atrial fibrillation as an independent
risk factor for stroke: the Framingham Study. Stroke 1991;22:983-8.
31. Wolf PA, Abbot RD, Kannel WB. Atrial fibrillation: a major contributor
to stroke in the elderly. Arch Intern Med 1987;147:1561-4.
32. Hart RG, Halperin JL. Atrial fibrillation and stroke. Revisiting the dilemmas. Stroke 1994;25:1337-41.
33. Poli D, Antonucci E, Grifoni E, et al. Stroke risk in atrial fibrillation patients
on warfarin: predictive ability of risk stratification schemes for primary and
secondary prevention. Thrombo Haemost 2009;101:367-72.
R
G
13. Healey JS, Connolly SJ. Atrial Fibrillation: hypertension as a causative
agent, risk factor for complications and potential therapeutic target. Am
Heart J 2003;91:9G-14G.
28. Kim DD, Young S, Cutfield R, et al. A survey of thyroid function test
abnormalities in patients presenting with atrial fibrillation and atrial flutter to a New Zealand district hospital. N Z Med J 2008;121:82-6.
O
ED
9. Kannell WB, Abbot RD, Savage DD, et al. Epidemiologic features of
chronic atrial fibrillation. The Framingham Study. N Engl J Med 1982;
306:1018-22.
BA
14. Krahn AD, Klein GJ, Kerr C, et al. How useful is thyroid function testing
in patients with recent-onset atrial fibrillation? The Canadian Registry of
Atrial Fibrillation Investigators. Arch Intern Med 1996;156:2221-4.
15. Sharma AD, Klein GJ, Guiradon GM, et al. Atrial fibrillation in patients
with Wolff-Parkinson-White syndrome: incidence after surgical ablation
of the accessory pathway. Circulation 1985;72:161-9.
EM
16. Skanes AC, Krahn AD, Yee R, et al. Progression to chronic atrial fibrillation after pacing: The Canadian Trial of Physiologic Pacing. J Am Coll
Cardiol 2001;38:167-72.
34. Hart RG, Pearce LA, Aquilar MI. Meta-analysis: anti-thrombotic therapy
to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann
Intern Med 2007;146:857-67.
35. ACTIVE Investigators, Connolly SJ, Pogue J, Hart RG, et al. Effect of
clopidogrel added to aspirin in patients with atrial fibrillation. N Engl
J Med 2009;30:2066-78.
36. Hart RG. Antithrombotic therapy to prevent stroke in patients with atrial
fibrillation: a meta-analysis. Ann Intern Med 1999;131:492-501.
17. Sweeney MO, Bank AJ, Nsah E, et al. Minimizing ventricular pacing to
reduce atrial fibrillation in sinus-node disease. N Engl J Med 2007;357:
1000-8.
37. Hughes M, Lip GYH. Stroke and thromboembolism in atrial fibrillation:
a systematic review of stroke risk factors, risk stratification schema and
cost-effectiveness data. Thrombo Haemost 2009;99:295-304.
18. Healey JS, Toff WD, Lamas GA, et al. Cardiovascular outcomes with atrialbased pacing compared with ventricular pacing: meta-analysis of randomized
trials, using individual patient data. Circulation 2006;114:11-7.
38. Stroke Risk in Atrial Fibrillation Working Group. Comparison of 12 risk
stratification schemes to predict stroke in patients with nonvalvular atrial
fibrillation. Stroke 2008;39:1901-10.
19. Sweeny MO, Hellkamp AS, Ellenbogen KA, et al. Adverse effect of ventricular pacing on heart failure and atrial fibrillation among patients with
normal baseline QRS duration in a clinical trial of pacemaker therapy for
sinus node dysfunction. Circulation 2003;107:2932-7.
39. Connolly SJ, Pogue J, Eikelboom J, et al. Benefit of oral anticoagulant over
antiplatelet therapy in atrial fibrillation depends on the quality of international normalized ratio control achieved by centres and countries as measured by time in therapeutic range. Circulation 2008;118:2029-37.
20. Ntep-Gweth M, Zimmermann M, Meiltz A, et al. Atrial fibrillation in
Africa: clinical characteristics, prognosis and adherence to guidelines in
Cameroon. Europace 2010;12:482-7.
40. Cairns JA, Connolly S, McMurtry S, Stephenson M, Talajic M, CCS
Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: prevention of stroke and systemic
thromboembolism in atrial fibrillation and flutter. Can J Cardiol 2011;
27:74-90.
21. Kanagala R, Murali NS, Friedman PA, et al. Obstructive sleep apnea and
the recurrence of atrial fibrillation. Circulation 2003;107:2589-94.
22. Wang TJ, Parise H, Levy D, et al. Obesity and the risk of new-onset atrial
fibrillation. JAMA 2004;292:2471-7.
23. Conen D, Tedrow UB, Cook NR, et al. Alcohol consumption and risk of
incident atrial fibrillation in women. JAMA 2008;300:2489-96.
41. Healey JS, Hart RG, Pogue J, et al. Risks and benefits of oral anticoagulation compared with clopidogrel plus aspirin in patients with atrial fibrillation according to stroke risk: the Atrial Fibrillation Clopidogrel Trial
with Irbesartan for Prevention of Vascular Events (ACTIVE-W). Stroke
2008;39:1482-6.
Healey et al.
CCS Atrial Fibrillation Etiology and Initial Investigations
37
44. The AFFIRM Investigators. A comparison of rate control and rhythm control
in patients with atrial fibrillation. N Engl J Med 2002;347:1825-33.
43. Hart RG, Pearce LA, Rothbart RM, et al. Stroke with intermittent atrial
fibrillation: incidence and predictors during aspirin therapy. Stroke
Prevention in Atrial Fibrillation Investigators. J Am Coll Cardiol 2000;35:
183-7.
45. Rivero-Ayerza M, Scholte Op Reimer W, Lenzen M, et al. New-onset atrial
fibrillation is an independent predictor of in-hospital mortality in hospitalized
heart failure patients: results of the EuroHeart Failure Survey. Eur Heart J
2008 Jul;29(13):1618-24. Epub 2008 May 31.
EM
BA
R
G
O
ED
42. Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in
patients with atrial fibrillation. N Engl J Med 2009;361:1139-51.
Canadian Journal of Cardiology 27 (2011) 38 – 46
Society Guidelines
Canadian Cardiovascular Society Atrial Fibrillation
Guidelines 2010: Management of Recent-Onset Atrial
Fibrillation and Flutter in the Emergency Department
Ian G. Stiell, MD, MSc,a Laurent Macle, MD, FRCPC,b and the CCS Atrial Fibrillation
Guidelines Committeec
a
b
For a complete listing of committee members, see Gillis AM, Skanes AC. Canadian Cardiovascular Society Atrial Fibrillation Guidelines
2010: Implementing GRADE and achieving consensus. Can J Cardiol 2011;27:27-30.
ABSTRACT
O
ED
c
Department of Emergency Medicine, Ottawa Hospital Research Institute, University of Ottawa, Ottawa, Ontario, Canada
Department of Medicine, Electrophysiology Service, Montreal Heart Institute, Université de Montréal, Montreal, Québec, Canada
RÉSUMÉ
La fibrillation auriculaire (FA) est la forme d’arythmie la plus fréquemment rencontrée à la salle d’urgence. La plupart des patients présentant une FA ou un flutter auriculaire d’apparition récente peuvent être
traités en toute sécurité au service des urgences sans nécessiter
d’hospitalisation. Les priorités du traitement à l’urgence incluent une évaluation rapide de l’état hémodynamique ainsi que
l’identification et le traitement de la cause sous-jacente et/ou des
facteurs précipitants. Le patient doit être soigneusement questionné
sur ses symptômes, pour tenter de déterminer le début d’apparition de
l’arythmie. Le risque d’accident vasculaire cérébral (AVC) doit être
déterminé dans tous les cas, en utilisant, par exemple, le score de
CHADS2. Chez les patients hémodynamiquement stables et présentant une FA ou un flutter auriculaire d’apparition récente, une stratégie
soit de contrôle de la fréquence ventriculaire soit de conversion et
maintien du rythme sinusal doit être adoptée, en tenant compte de
nombreux éléments comme la durée de la FA et la sévérité des
symptômes. Si l’on retient une stratégie de conversion et maintien du
rythme sinusal, la cardioversion pourra être électrique ou pharmacologique. Avant cardioversion chez les patients non anticoagulés, il
faudra être certain que la durée de l’épisode de FA ou de flutter
EM
BA
R
G
Atrial fibrillation (AF) is the most common arrhythmia managed by
emergency physicians. There is increasing evidence that most patients
with recent-onset AF or atrial flutter (AFL) can be safely managed in
the emergency department (ED) without the need for hospital admission. The priorities for ED management of recent-onset AF/AFL include
rapid assessment of potential hemodynamic instability and identification and treatment of the underlying or precipitating cause. A careful
evaluation of the patient’s history should be performed to determine
the time of onset of the arrhythmia. All patients should be stratified
using a predictive index for the risk of stroke (eg, CHADS2). For stable
patients with recent-onset AF/AFL, a strategy of either rate control or
rhythm control could be selected based on multiple factors including
the duration of AF and the severity of symptoms. If a strategy of rhythm
control has been selected, either electrical or pharmacologic cardioversion may be used. Before proceeding to cardioversion in the absence of systemic anticoagulation, physicians must be confident that
the duration of AF/AFL is clearly ⬍48 hours and that the patient is not
at a particularly high risk of stroke. When the duration of AF/AFL is
⬎48 hours or uncertain, rate control should be optimized first and
Atrial fibrillation (AF) is the most common arrhythmia managed by emergency physicians and accounts for approximately
one-third of hospitalizations for cardiac rhythm disturbances.1
In Canada, the estimated overall rate of hospitalization with AF
is 583 per 100,000 population.2 Hospital admissions for AF
have increased by 66% over the past 20 years due to an aging
Received for publication November 9, 2010. Accepted November 10, 2010.
specific recommendations. These recommendations are aimed to provide a
reasonable and practical approach to care for specialists and allied health
professionals obliged with the duty of bestowing optimal care to patients
and families, and can be subject to change as scientific knowledge and
technology advance and as practice patterns evolve. The statement is not
intended to be a substitute for physicians using their individual judgment
in managing clinical care in consultation with the patient, with appropriate
regard to all the individual circumstances of the patient, diagnostic and
treatment options available and available resources. Adherence to these
recommendations will not necessarily produce successful outcomes in every
case.
Corresponding author: Ian G. Stiell, MD, MSc, Clinical Epidemiology
Unit, F657, Ottawa Hospital, 1053 Carling Ave, Ottawa, Ontario, Canada
K1Y 4E9. Tel.: ⫹1-613-798-5555, ext.: 18683; fax: ⫹1-613-761-5351.
E-mail: istiell@ohri.ca
The disclosure information of the authors and reviewers is available from the
CCS on the following websites: www.ccs.ca and www.ccsguidelineprograms.ca.
This statement was developed following a thorough consideration of
medical literature and the best available evidence and clinical experience. It
represents the consensus of a Canadian panel comprised of multidisciplinary experts on this topic with a mandate to formulate disease-
0828-282X/$ – see front matter © 2011 Canadian Cardiovascular Society. Published by Elsevier Inc. All rights reserved.
doi:10.1016/j.cjca.2010.11.014
Stiell et al.
Atrial Fibrillation and Flutter in the ED
39
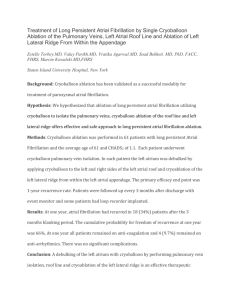
Emergency Department Management of RecentOnset AF/AFL
Overall approach
The priorities for ED management of recent-onset AF/AFL
(Fig. 1) include rapid assessment of potential hemodynamic
instability, the identification and treatment of the underlying
or precipitating cause, and a careful assessment of the patient’s
history with particular attention to the risk of thromboembolism. At this time, evidence equally supports a strategy of rate
control or rhythm control for stable patients with known onset
of AF/AFL within 48 hours. Both approaches are presented here.
The decision regarding the initial strategy of rate versus rhythm
control depends upon multiple factors including patient and physician preference, clarity of the history of onset of symptoms, type
and duration of AF, severity of symptoms, associated cardiovascular disease and medical conditions, and age.
EM
BA
R
G
population and a rising prevalence of chronic heart disease.3,4
The overall mortality rate for patients with AF is approximately
double that for patients in normal sinus rhythm.5 The rate of
ischemic stroke among patients with nonvalvular AF averages 5% per year, 2 to 7 times that of the population without
AF.5-7 Atrial flutter (AFL) may also occur in the patient with
AF or may present as an isolated arrhythmia. The goals of
therapy and management approaches for AFL are similar to
those for AF.
In the emergency department (ED), physicians often
manage patients with either recent-onset (first detected or
recurrent) or those with permanent AF/AFL.8 In the case of
permanent AF/AFL, cardioversion has previously failed or
clinical judgment has led to a decision not to pursue cardioversion, and ED care focuses on rate control and treatment
of underlying conditions.9 When AF terminates spontaneously within 7 days of recognized onset, it is designated
paroxysmal; when sustained beyond 7 days, AF is designated
persistent. This chapter will focus on those with symptomatic, recent-onset episodes of AF/AFL (either newly detected, recurrent paroxysmal, or recurrent persistent episodes), the most common arrhythmia managed in the
ED.10,11 There are 2 competing strategies for management:
rate-control and rhythm-control treatment.1,12-14 The ratecontrol approach consists of ventricular rate control, oral
anticoagulation, no attempt to return the patient to sinus
rhythm in the ED, and delayed cardioversion after 4 weeks,
if indicated. With the rhythm-control approach, attempts
are made to cardiovert patients to sinus rhythm in the ED,
either pharmacologically or electrically, and then discharge
them home in sinus rhythm.15-17
auriculaire est inférieure à 48 heures et que le patient ne présente pas
un risque particulièrement élevé d’AVC. Lorsque la durée de l’épisode
de FA ou de flutter auriculaire est incertaine ou supérieure à 48 heures, la fréquence cardiaque sera optimisée et les patients seront anticoagulés pour 3 semaines précédant et 4 semaines suivant la cardioversion. Au départ de la salle d’urgence, tous les patients avec FA
ou flutter auriculaire d’apparition récente devront faire l’objet d’un
suivi rapproché pour déterminer la présence de cardiopathie sousjacente et évaluer la nécessité d’un traitement antithrombotique ou
antiarythmique au long cours.
O
ED
the patients should receive therapeutic anticoagulation for 3 weeks
before and 4 weeks after planned cardioversion. Adequate follow-up of
patients with recent-onset AF/AFL is recommended to identify structural heart disease and evaluate the need for long-term antithrombotic
or antiarrhythmic therapy.
Evidence for Emergency Department
Management
Variation in practice within Canadian EDs has been observed, and this variation likely reflects a lack of high-quality
evidence to guide the acute management of recent-onset AF
patients.18,19 Standard guidelines and textbooks are unable
to offer clear evidence-based direction for emergency
physicians.1,20 Particularly controversial is the issue of using
rhythm control or rate control.1,12-14 The very large AFFIRM and AF-CHF clinical trials compared rate and
rhythm control but did not explore the optimal management for recent-onset AF/AFL patients presenting to the
ED with ⬍48 hours of symptoms.21,22 In the United States,
patients are often admitted to hospital under the cardiology
service or discharged home after rate-control therapy only.23-25 One Canadian site has described 2 cohorts of patients successfully treated with rhythm control with good
results.11,26 Other studies of rhythm control in the ED have
been small or did not include both pharmacologic and electrical cardioversion as an option.15,17,23,27,28
RECOMMENDATION
We recommend that in stable patients with recent-onset
AF/AFL, a strategy of rate control or rhythm control could
be selected (Strong Recommendation, High-Quality Evidence).
Values and preferences. This recommendation places a
high value on the randomized controlled trials investigating
rate control as an alternative to rhythm control for AF/AFL,
recognizing that these trials did not specifically address the
ED environment.
Assessment
Uncommonly, patients with recent-onset AF/AFL will
present with hemodynamic instability and must be immediately cardioverted as described later. Most patients are stable,
presenting with palpitations, chest tightness, or weakness, although some patients, especially the elderly, are often unaware
that they have a tachyarrhythmia or when it started. A careful
history should be taken to determine the time of onset, if
known, and particularly to determine if it was within the past
48 hours. Other important points to determine include previous episodes and treatment, associated cardiac conditions, current antiarrhythmic agents, anticoagulation and current INR
level, rhythm on most recent ECG, and risk of thromboembolism per the CHADS2 [Congestive Heart Failure, Hypertension, Age, Diabetes, Stroke/Transient Ischemic Attack] score
(see Table 1 and Therapies for Prevention of Stroke and Vas-
40
Canadian Journal of Cardiology
Volume 27 2011
Strategy of rhythm-control for recent-onset AF/AFL
Known duraon < 48 h
(and not high-risk paents1)
Duraon > 48 h or unknown
or high-risk paents1
Failed CV
Hemodynamically
unstable
Urgent electrical
cardioversion2
Rate-control
Hemodynamically
stable
Therapeuc OAC for
3 weeks before
cardioversion
Pharmacological
or electrical
cardioversion2
TEE-guided cardioversion
(OAC iniated with
heparin bridging)3
Successful CV
Anthromboc therapy
Anthromboc therapy
1Paents
at parcularly high risk of stroke (e.g. mechanical valve, rheumac heart disease, recent stroke/TIA)
biphasic waveform preferred
must be iniated and connued unl a therapeuc level of oral ancoagulaon has been established.
2150-200J
3Heparin
-OAC connued for 4 consecuve weeks.
-If AF/AFL persists or recurs or if AF/AFL has been recurrent,
anthromboc therapy as appropriate (per CHADS2 score) should
be connued indefinitely.
-Early follow-up should be arrange to review ongoing
anthromboc strategy.
O
ED
-In general, no prior or subsequent ancoagulaon is
required.
-If AF/AFL persists or recurs or if AF/AFL has been recurrent,
anthromboc therapy as appropriate (CHADS2 score) should
be iniated and connued indefinitely.
-Early follow-up should be arranged to review anthromboc
strategy.
R
G
Figure 1. A management strategy for patients with recent-onset AF/AFL.
Unstable patients
EM
BA
cular Events). AF may be related to acute, temporary causes
including alcohol use (eg, “holiday heart syndrome”), myocardial ischemia or infarction, myocarditis or pericarditis, pulmonary embolism or other pulmonary diseases, hyperthyroidism,
and other metabolic disorders. In such cases, successful treatment of the underlying condition may promote the resolution
of AF. Routine chemistry and hematology are indicated as well
as, in some cases, troponin and thyroid-stimulating hormone
levels. Transesophageal echocardiography, if available, is useful
to exclude the presence of left atrial clot in patients in whom
the onset of arrhythmia is unclear and cardioversion is desired.
If recent-onset AF/AFL has caused hemodynamic instability with hypotension, acute coronary syndrome, or florid pulmonary edema, then patients must undergo immediate electrical cardioversion. This is a relatively uncommon presentation
of recent-onset AF/AFL, and physicians must ensure that the
patient is not in long-standing persistent AF/AFL, as attempts
to cardiovert such patients are likely to fail and may increase
morbidity. In this case, the rapid AF may be secondary to an
Table 1. CHADS2 risk criteria for stroke in patients with nonvalvular
atrial fibrillation if not treated with anticoagulation
Risk criteria
Prior stroke or TIA
Age ⬎75
Hypertension
Diabetes mellitus
Congestive heart failure
Data from Gage BF, et al54 and Wang TJ, et al.55
Score
2
1
1
1
1
acute decompensation of an underlying condition such as sepsis or hypovolemia. Generally, unstable patients need not be
given an anticoagulant either before or following cardioversion
if the duration of AF/AFL is known to have occurred ⬍48
hours. However, if the duration of AF/AFL is ⱖ48 hours or
unknown or the patient is at particularly high risk of stroke (eg,
mechanical valve, rheumatic valve disease, recent stroke, or
transient ischemic attack), we suggest administering the patient
intravenous unfractionated heparin or low-molecular-weight
heparin before cardioversion if possible or immediately thereafter if even a brief delay is unacceptable. Such a patient should
then be bridged with heparin and started on a course of oral
anticoagulants for ⱖ4 weeks postcardioversion.
RECOMMENDATION
We recommend for patients with acute hemodynamic
instability secondary to rapid recent-onset AF/AFL, immediate electrical conversion to sinus rhythm (Strong Recommendation, Low-Quality Evidence).
Values and preferences. This recommendation places a
high value on the immediate management of hemodynamic instability and a lower value on anticoagulation status under these
circumstances. It is also recognized that this is a relatively rare circumstance and that, in most cases, stroke risk and anticoagulation
status can be considered prior to immediate cardioversion.
Rate control
Criteria for adequate rate control vary. A sustained, uncontrolled tachycardia over weeks may lead to deterioration of left
Stiell et al.
Atrial Fibrillation and Flutter in the ED
41
Drug
Diltiazem*
Metoprolol
Verapamil*
Digoxin
Dose
Risks
0.25 mg/kg IV bolus over
10 min; repeat at 0.35
mg/kg IV
2.5-5 mg IV bolus over
2 min; up to 3 doses
0.075-0.15 mg/kg over
2 min
0.25 mg IV each 2 h;
up to 1.5 mg
Hypotension, bradycardia
Hypotension, bradycardia
Hypotension, bradycardia
Bradycardia, digitalis
toxicity
* Calcium-channel blockers should not be used in patients with heart failure or left ventricular dysfunction.
RECOMMENDATION
In hemodynamically stable patients with AF/AFL of
known duration ⬍48 hours in whom a strategy of rhythm
control has been selected:
We recommend that rate-slowing agents alone are acceptable while awaiting spontaneous conversion (Strong
Recommendation, Moderate-Quality Evidence).
We recommend that synchronized electrical cardioversion or pharmacologic cardioversion may be used when a
decision is made to cardiovert patients in the emergency
department. See Table 2 for drug recommendations (Strong
Recommendation, Moderate-Quality Evidence).
We suggest that antiarrhythmic drugs may be used to
pretreat patients before electrical cardioversion in ED in
order to decrease early recurrence of AF and to enhance
cardioversion efficacy (Conditional Recommendation,
Low-Quality Evidence).
R
G
ventricular function, a condition called tachycardia-related cardiomyopathy, so it is important that adequate rate control be
achieved.29 Physicians should attempt to reduce the heart rate
prior to discharge from the ED to target rates of ⬍100 beats per
minute (bpm) at rest and ⬍110 bpm during moderate exercise
(such as a walk test). The most commonly used drugs are intravenous diltiazem, verapamil, and metoprolol (Table 2).
Digoxin is not considered a first-line agent for rate control
because of slow onset of action and it affects only resting heart
rate. It may be useful in patients with heart failure and left
ventricular systolic dysfunction or as an adjunctive agent, allowing lower doses of beta-blockers or calcium channel blockers to be used. At discharge from the ED, physicians should
ensure the patient is placed on oral rate-control medications
and the appropriate prophylaxis for stroke.
capability. Prevention of thromboembolism for patients managed
with rhythm control is discussed later.
Spontaneous conversion of recent-onset AF to sinus rhythm
within 24 hours is common. Some emergency physicians have
the patients return the following day for cardioversion at that
time if spontaneous conversion has not occurred.5,35 In this
scenario, after documentation of appropriate rate control, patients at low risk of stroke can be discharged on rate control
alone to return the following day for reevaluation. Patients who
remain in AF can then undergo DC cardioversion at this time
as long as the total duration of AF remains ⬍48 hours.
O
ED
Table 2. Recommended intravenous drugs for heart rate control in
the ED
BA
Rhythm control
EM
Cardioversion in the absence of systemic anticoagulation
carries a risk of thromboembolism when AF/AFL has been
present for ⬎48 hours. When the duration of AF/AFL has been
⬍48 hours, cardioversion appears to have an acceptably low
risk of thromboembolism except in particularly high-risk
groups.30,31 Such high-risk situations include the presence of a
mechanical valve, rheumatic valve disease, or recent stroke or
transient ischemic attack unless the patient is already on oral
anticoagulation with a therapeutic INR. There is no evidence
that the risk of thromboembolism or stroke differs between
pharmacologic and electrical cardioversion. Before proceeding
to immediate cardioversion in the absence of systemic anticoagulation, physicians must be confident that the onset of AF/
AFL is clearly ⬍48 hours and that the patient is not at a particularly high risk of stroke. Most patients in the ED are acutely
aware of the time of onset of symptoms but some are not. In
such situations, a transesophageal echocardiogram may be used
to establish the safety of immediate cardioversion. If patients
are on warfarin, it is important to ensure that their INR has
been therapeutic for ⱖ3 consecutive weeks.1,32
Rate-control drugs have not been shown to enhance the rate
of conversion when a rhythm-control approach is used. Physician and patient preferences dictate whether to start rhythmcontrol treatment with drugs or with electrical cardioversion.
Initial use of antiarrhythmic agents may also prevent immediate
recurrence of AF after electrical cardioversion.33,34 All patients
undergoing pharmacologic or electrical cardioversion require continuous electrocardiographic monitoring and temporary pacing
Values and preferences. These recommendations place
a high value on determination of the duration of AF/AFL as
a determinant of stroke risk with cardioversion. Also, individual considerations of the patient and treating physician
are recognized in making specific decisions about method of
cardioversion.
Pharmacologic cardioversion
Physicians may consider several drugs for the pharmacologic cardioversion of recent-onset AF/AFL in the
ED13,15,16,36,37 (Table 3). Procainamide is administered intravenously over 60 minutes at a dose of 15-17 mg/kg and occasionally is accompanied by transient hypotension. A recent report described the successful use of procainamide in the ED,
where this drug was 60% effective for conversion of recentonset AF.38 This study showed procainamide to have an excellent safety profile, even for patients already taking oral antiarrhythmic agents. Oral propafenone or flecainide, both Class IC
agents, can be safely administered in the ED but can be expected to have slower onset of action than intravenous
drugs.39-41 The Class III agent ibutilide is administered intravenously and has been shown to effectively and quickly terminate AF and AFL of recent onset.42 Ibutilide is associated with
a 2%-3% risk of torsades de pointes but this risk can be mitigated by pretreatment with intravenous magnesium sulphate.43 Amiodarone and sotalol are not recommended for
recent-onset AF as they are no more effective than placebo in
the initial 6-8 hours and are associated with adverse reac-
42
Canadian Journal of Cardiology
Volume 27 2011
Drug
Class IA
Procainamide
Dose
Efficacy
Risks
15-17 mg/kg IV
over 60 min
⫹⫹
5% Hypotension
Class IC*
Propafenone
450-600 mg PO
⫹⫹⫹
Flecainide
300-400 mg PO
⫹⫹⫹
Hypotension,
1:1 flutter,
bradycardia
Hypotension,
1:1 flutter,
bradycardia
1-2 mg IV over
10-20 min
Pretreat with
MgSO4 1-2
mg IV
⫹⫹
Class III
Ibutilide
2-3% Torsades
de pointes
* Class IC drugs should be used in combination with AV nodal blocking
agents (beta-blockers or calcium channel inhibitors). Class IC agents should
also be avoided in patients with structural heart disease.
RECOMMENDATION
We recommend that electrical cardioversion may be conducted in the ED with 150-200 joules biphasic waveform as
the initial energy setting (Strong Recommendation, LowQuality Evidence).
Values and preferences. This recommendation places a
high value on the avoidance of repeated shocks and the
avoidance of ventricular fibrillation that can occur with synchronized cardioversion of AF at lower energy levels. It is
recognized that the induction of VF is a rare but easily
avoidable event.
R
G
tions.44-49 Adenosine transiently slows heart rate, does not cardiovert AF, and is associated with a significant risk of ventricular arrhythmias in Wolff-Parkinson-White syndrome with AF
(see Rapid Preexcitation later). Recent trials of vernakalant
have demonstrated high clinical efficacy of this intravenous
agent for conversion of recent-onset AF.50,51 This atrial selective antiarrhythmic drug was recently approved for use in the
European Union, but in North America it is currently available
only for investigational use.
successful electrical cardioversion in the ED, after pretreatment with intravenous procainamide. Patients had no serious adverse events and their ED lengths of stay averaged
only 4-6 hours.26 Current guidelines recommend starting
with a higher energy level, such as 150-200 joules for biphasic waveform devices in order to increase the likelihood of
initial success and thus limit the cumulative energy dose
with multiple attempts at cardioversion.1,52 Likewise, an
anterior-posterior pad positioning may be more effective
than an anterior-lateral approach.1,53 Sedation typically involves rapid acting agents such as intravenous fentanyl,
propofol, and midazolam.
O
ED
Table 3. Recommended drugs for pharmacologic conversion in
the ED
Electrical cardioversion
AF occurring in the setting of Wolff-Parkinson-White
syndrome (Fig. 2) is a precarious situation because rapid
atrioventricular conduction through the accessory pathway
may precipitate ventricular fibrillation. In these patients,
drugs that block atrioventricular conduction (digoxin, calcium channel blockers, beta-blockers, and adenosine) are
contraindicated because they do not slow conduction
EM
BA
Synchronized electrical cardioversion is highly effective
and physicians have the option of pretreating with antiarrhythmic drugs or proceeding directly to electrical shock. In
a series of 660 patients, one Canadian site described 91.0%
Rapid preexcitation during AF
Figure 2. Electrocardiogram of rapid ventricular preexcitation (Wolff-Parkinson-White syndrome) during atrial fibrillation. Note very rapid (up to 300
bpm) irregular wide QRS complexes.
Stiell et al.
Atrial Fibrillation and Flutter in the ED
43
RECOMMENDATION
We recommend, in patients with rapid ventricular preexcitation during AF (Wolff-Parkinson-White syndrome):
Urgent electrical cardioversion if the patient is hemodynamically unstable (Strong Recommendation, Low-Quality Evidence).
Intravenous antiarrhythmic agents procainamide or
ibutilide in stable patients (Strong Recommendation, LowQuality Evidence).
AV nodal blocking agents (digoxin, calcium channel
blockers, beta-blockers, adenosine) are contraindicated
(Strong Recommendation, Low-Quality Evidence).
RECOMMENDATION
We recommend that hemodynamically stable patients
with AF/AFL of ⱖ48 hours’ or uncertain duration for
whom a strategy of rhythm control has been selected
should have rate control optimized and receive therapeutic oral anticoagulants (OAC) therapy (warfarin [INR
2-3] or dabigatran) for 3 weeks before and at least 4
weeks postcardioversion.
Following attempted cardioversion:
If AF/AFL persists or recurs or if symptoms suggest that
the presenting AF/AFL has been recurrent, the patient
should have antithrombotic therapy continued indefinitely
(using either OAC or aspirin as appropriate).
If sinus rhythm is achieved and sustained for 4 weeks, the
need for ongoing antithrombotic therapy should be determined based on the risk of stroke, and in selected cases,
expert consultation may be required (Strong Recommendation, Moderate-Quality Evidence).
R
G
Values and preferences. These recommendations place
a high value on avoidance of the degeneration of preexcited
AF to ventricular fibrillation. It is recognized that degeneration can occur spontaneously or it can be facilitated by the
administration of specific agents that in the absence of ventricular preexcitation would be the appropriate therapy for
rate control of AF.
or oral anticoagulants as appropriate based on the patient’s
risk of thromboembolism. If sinus rhythm is achieved and
sustained for 4 weeks, the need for ongoing antithrombotic
therapy should be based on the risk of stroke. If rhythm
control is not anticipated, aspirin is sufficient for those with
a CHADS2 score of 0, whereas oral anticoagulants are preferred if the CHADS2 score is 1 and strongly recommended
if the CHADS2 score is ⱖ2 (see Prevention of Stroke and
Systemic Thromboembolism in Atrial Fibrillation and Flutter).60 If the patient is at particularly high risk of stroke (eg,
mechanical valve, rheumatic valve disease, recent stroke or
transient ischemic attack), even when the duration of newonset AF/AFL is ⬍48 hours, we recommend that cardioversion be delayed and that oral anticoagulants be prescribed
for 3 weeks before and at least 4 weeks postcardioversion.
Subsequent antithrombotic therapy should be based on balancing the risks of stroke and bleeding.
O
ED
through the accessory pathway and, therefore, may precipitate VF. We recommend urgent electrical cardioversion if
the patient is hemodynamically unstable or intravenous antiarrhythmic agents procainamide or ibutilide in stable patients. Amiodarone should be used with caution in the case
of preexcited AF as several case reports have described the
occurrence of VF after intravenous administration.45
EM
BA
Practical tip. Identification of preexcited AF can be challenging
and should be considered with any very rapid (240-300 bpm)
sustained, highly irregular wide complex tachycardia (Fig. 2).
Spontaneous degeneration of preexcited AF to VF can occur in the
absence of administration of medication. As such, DC cardioversion is most often the preferred option when preexcited AF is very
rapid.
Prevention of thromboembolism
Perhaps the most important and controversial aspect of ED
management for recent-onset AF/AFL is ensuring that patients
do not sustain a stroke. Physicians should be familiar with the
CHADS2 risk scoring system54,55 (Table 1). If warfarin is prescribed, patients need careful follow-up to minimize the risk of
bleeding.56,57 Dabigatran is a promising new oral anticoagulant that reversibly inhibits thrombin and can be used with a
fixed-dose regimen without the need for routine coagulation
monitoring.58,59
a. Duration of AF/AFL 48 hours or high-risk patient. In
stable patients with AF/AFL ⬎48 hours or of uncertain
duration in which a strategy of rhythm control has been
selected, rate control should first be optimized. The patient
should also receive therapeutic warfarin (INR 2-3) or dabigatran for 3 weeks before and at least 4 weeks after attempted cardioversion.1,32 Antithrombotic therapy should
be continued indefinitely if symptoms suggest that AF/AFL
has been recurrent or if AF/AFL persists, using either aspirin
Values and preferences. These recommendations place
a high value on minimizing stroke risk by rate control, appropriate anticoagulation and delayed cardioversion, and a
lower value on symptomatic improvement associated with
immediate cardioversion.
b. Duration of AF/AFL 48 hours and not high risk. In stable
patients with AF of known duration ⬍48 hours in whom a
strategy of rhythm control has been selected, we recommend
that they may generally be cardioverted without prior or subsequent anticoagulation or use of heparin. If symptoms suggest
that AF/AFL has been recurrent or if AF/AFL persists, then
antithrombotic therapy should be commenced and continued
indefinitely as the risk of stroke with paroxysmal AF is equivalent to that of permanent AF.61,62 Aspirin is sufficient for those
with a CHADS2 score of 0, whereas oral anticoagulants are
preferred for patients with a CHADS2 score of 1 and strongly
recommended if the CHADS2 score is ⱖ2 (see Prevention of
Stroke and Systemic Thromboembolism in Atrial Fibrillation
and Flutter).60
44
Canadian Journal of Cardiology
Volume 27 2011
We recommend that hemodynamically stable patients
with AF/AFL of known duration ⬍48 hours for whom a
strategy of rhythm control has been selected may generally undergo cardioversion without prior or subsequent
anticoagulation. However, if the patient is at particularly
high risk of stroke (eg, mechanical valve, rheumatic heart
disease, recent stroke, or transient ischemic attack), cardioversion should be delayed and the patient should receive OAC for 3 weeks before and at least 4 weeks postcardioversion.
Following attempted cardioversion:
If AF or AFL persists, recurs, or if symptoms suggest that
the presenting AF/AFL has been recurrent, antithrombotic
therapy (OAC or aspirin as appropriate) should be commenced and continued indefinitely.
If NSR is achieved, the need for ongoing antithrombotic
therapy should be determined based on the risk of stroke
according to CHADS2 score and early consultant follow-up
should be arranged (Strong Recommendation, Low-Quality Evidence).
Disposition and follow-up
Most patients with recent-onset AF/AFL may be discharged
home from the ED within a period of 6-12 hours, once adequate rate or rhythm control has been achieved. We recommend hospital admission of symptomatic patients with decompensated heart failure or myocardial ischemia. Occasionally,
admission may be required for highly symptomatic patients in
whom adequate rate or rhythm control cannot be achieved.
RECOMMENDATION
We recommend hospital admission for highly symptomatic patients with decompensated heart failure or myocardial ischemia (Strong Recommendation, Low-Quality Evidence).
We suggest limiting hospital admission to highly symptomatic patients in whom adequate rate control cannot be
achieved (Conditional Recommendation, Low-Quality Evidence).
BA
R
G
Values and preferences. These recommendations place
a high value on minimizing stroke risk by appropriate anticoagulation prior to cardioversion in all patients except
those at very low risk of stroke due to a short duration of
AF/AFL. A lower value is placed on symptomatic improvement associated with immediate cardioversion in patients
who are deemed not to be at very low risk of stroke despite
an apparent short duration of AF/AFL.
Values and preferences. This recommendation places a
higher value on the symptomatic improvement with immediate cardioversion as well as avoidance of precardioversion
anticoagulation. A lower value is placed on the small risks
associated with transesophageal echocardiography.
O
ED
RECOMMENDATION
EM
c. Transesophageal echocardiography. If the onset of
symptoms is not clearly ⬍48 hours or there is a particularly
high risk of stroke, we suggest that patients may undergo
cardioversion guided by transesophageal echocardiography,
as an alternative to anticoagulation prior to cardioversion.63,64 Patients with no identifiable left atrial thombus
may undergo immediate cardioversion. Prior to cardioversion, pretreatment with heparin must be initiated and continued until a therapeutic level of oral anticoagulation has
been established. Oral anticoagulation must be continued
for a minimum of 4 weeks (as discussed). For patients in
whom thrombus is identified by transesophageal echocardiography, oral anticoagulation should be prescribed for ⱖ3
weeks and transesophageal echocardiography repeated to
confirm the resolution of thrombus before proceeding to
cardioversion.
Values and preferences. This recommendation places a
high value on the need for monitoring of the response to
therapy and its reassessment, as well as ancillary investigation and treatment not available in the ED in patients with
complex medical conditions associated with AF/AFL. A
lower value is placed on the attendant costs of admission to
hospital in patients with complex medical conditions associated with AF/AFL.
Adequate follow-up is recommended to identify structural
heart disease and the possible need for long-term anticoagulation or antiarrhythmic therapy. Patients with newly detected
AF/AFL should have outpatient echocardiography and referral
to a cardiologist or internist. Adequate and early follow-up are
necessary to safely monitor the INR of patients discharged on
warfarin. The need for long-term antithrombotic therapy may
be reviewed by the appropriate consultant, weighing the risks
and benefits. Long-term rhythm management should also be
reviewed by a consultant, based on the estimated probability of
recurrence, the symptoms during AF, and other factors.
RECOMMENDATION
RECOMMENDATION
When the duration of an episode of AF/AFL is uncertain, we suggest that patients may undergo cardioversion
guided by transesophageal echocardiography, as an alternative to anticoagulation prior to cardioversion. However, anticoagulation needs to be simultaneously started and maintained for ⱖ4 weeks postcardioversion (Conditional
Recommendation, High-Quality Evidence).
We suggest that after conversion to sinus rhythm has
been achieved, whether antiarrhythmic drug therapy is indicated should be based on the estimated probability of
recurrence and the symptoms during AF. Long-term therapy will need to be determined by an appropriate outpatient
consultation (Conditional Recommendation, Low-Quality
Evidence).
Stiell et al.
Atrial Fibrillation and Flutter in the ED
45
Conclusion
Physicians frequently encounter ED patients with recentonset AF/AFL and may safely manage these patients with either
a rate-control or rhythm-control strategy. Immediate specialist
consultation or admission to hospital is not often necessary.
Careful consideration of the risks of thromboembolism is a
priority and appropriate follow-up is important. There is a
need for more evidence to specifically guide the unique management of patients in the ED with recent-onset AF.
13. Page RL. Newly diagnosed atrial fibrillation. N Engl J Med 2004;351:
2408-16.
14. Hiatt WR, Lincoff M, Harrington RA. Acute pharmacological conversion
of atrial fibrillation to sinus rhythm. Is short-term symptomatic therapy
worth it? A report from the December 2007 Meeting of the Cardiovascular and Renal Drugs Advisory Committee of the Food and Drug Administration. Circulation 2008;117:2956-7.
15. Taylor DM, Aggarwall A, Carter M, Garewal D, Hunt D. Management of
new onset atrial fibrillation in previously well patients less than 60 years of
age. Emerg Med Austral 2005;17:4-10.
16. Raghavan AV, Decker WW, Meloy TD. Management of atrial fibrillation
in the emergency department. Emerg Med Clin N Am 2005;23:1127-39.
17. Burton JH, Vinson DR, Drummond K, et al. Electrical cardioversion of
emergency department patients with atrial fibrillation. Ann Emerg Med
2004;44:20-30.
18. Stiell IG, Clement CM, Brison RJ, et al. Variation in management of
recent-onset atrial fibrillation and flutter (RAFF) among academic hospital emergency departments. Ann Emerg Med 2010;57:13-21.
19. Borgundvaag B, Ovens H. Cardioversion of uncomplicated paroxysmal
atrial fibrillation: a survey of practice by Canadian emergency physicians.
Can J Emerg Med 2004;6:155-60.
O
ED
Values and preferences. This recommendation places a
high value on minimizing the risk of infrequent but serious
side effects associated with long-term antiarrhythmic drugs.
A high value is also placed on the appropriate use of specialty care to make patient-specific decisions to minimize
these risks. A lower value is placed on the avoidance of
symptoms associated with subsequent episodes of AF/AFL
if antiarrhythmic drugs cannot be avoided.
20. Marx JA, Hockberger RS, Walls RW. Rosen’s Emergency Medicine: concepts and clinical practice. 6th ed. St Louis: Mosby, 2006.
References
21. Wyse DG, Waldo AL, DiMarco JP, et al, for the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) Investigators. A
comparison of rate control and rhythm control in patients with atrial
fibrillation. N Engl J Med 2002;347:1825-33.
R
G
1. Fuster V, Ryden LE, Cannom DS, et al. ACC/AHA/ESC 2006 guidelines
for the management of patients with atrial fibrillation. J Am Coll Card
2006;48:149-246.
2. Humphries KH, Jackevicius C, Gong Y, et al. Population rates of hospitalization for atrial fibrillation/flutter in Canada. Can J Cardiol 2004;20:
869-76.
22. Roy D, Talajic M, Nattel S, et al. Rhythm control versus rate control for
atrial fibrillation and heart failure. N Engl J Med 2008;358:2667-77.
23. Decker WW, Smars PA, Vaidyanathan L, et al. A prospective, randomized
trial of an emergency department observation unit for acute onset atrial
fibrillation. Ann Emerg Med 2008;52:322-8.
4. Friberg J, Buch P, Scharling H, Gadsbphioll N, Jensen GB. Rising rates of
hospital admissions for atrial fibrillation. Epidemiology 2003;14:666-72.
24. Santini M, De Ferrari GM, Pandozi C, et al. Atrial fibrillation requiring
urgent medical care. Approach and outcome in various departments of
admission. Data from the Atrial Fibrillation/Flutter Italian Registry
(FIRE). Ital Heart J 2004;5:205-13.
BA
3. Wattigney WA, Mensah GA, Croft JB. Increasing trends in hospitalization for atrial fibrillation in the United States, 1985 through 1999: implications for primary prevention. Circulation 2003;108:711-6.
EM
5. Krahn AD, Manfreda J, Tate RB, Mathewson FA, Cuddy TE. The natural
history of atrial fibrillation: incidence, risk factors, and prognosis in the
Manitoba Follow-Up Study. Am J Med 1995;98:476-84.
6. Flegel KM, Shipley MJ, Rose G. Risk of stroke in non-rheumatic atrial
fibrillation. Lancet 1987;1:526-9.
7. Wolf PA, Abbott RD, Kannel WB. Atrial fibrillation as an independent
risk factor for stroke: The Framingham Study. Stroke 1991;22:983-8.
8. Heilbron B, Klein GJ, Talajic M, Guerra PG. 2004 Canadian Cardiovascular Society Consensus Conference: atrial fibrillation–management of
atrial fibrillation in the emergency department and following acute myocardial infarction. Can J Cardiol 2005;21(Suppl B):61B-6B.
9. Skanes AC, Dorian P. 2004 Canadian Cardiovascular Society Consensus
Conference: atrial fibrillation– etiology and initial investigation of atrial
fibrillation. Can J Cardiol 2005;21(Suppl B):11B-4B.
10. Connors S, Dorian P. Management of supraventricular tachycardia in the
emergency department. Can J Cardiol 1997;13 (Suppl A):19A-24A.
11. Michael JA, Stiell IG, Agarwal S, Mandavia DP. Cardioversion of paroxysmal atrial fibrillation in the emergency department. Ann Emerg Med
1999;33:379-87.
12. Wyse DG, Simpson CS. 2004 Canadian Cardiovascular Society Consensus Conference: atrial fibrillation–rate control versus rhythm control: decision making. Can J Cardiol 2005;21(Suppl B):15B-8B.
25. del Arco C, Martin A, Laguna P, Gargantilla P, for the Spanish Atrial
Fibrillation in Emergency Medicince Study Group. Analysis of current
management of atrial fibrillation in the acute setting: GEFAUR-1 study.
Ann Emerg Med 2005;46:424-30.
26. Stiell IG, Clement CM, Perry JJ, et al. An aggressive protocol for rapid
management and discharge of emergency department patients with recent-onset episodes of atrial fibrillation and flutter. Can J Emerg Med
2010;12:181-91.
27. Joseph AP, Ward MR. A prospective, randomized controlled trial comparing the efficacy and safety of sotalol, amiodarone and digoxin for the
reversion of new-onset atrial fibrillation. Ann Emerg Med 2000;36:1-9.
28. Domanovits H, Schillinger M, Thoennissen J, et al. Termination of recent-onset atrial fibrillation/flutter in the emergency department: a sequential approach with intravenous ibutilide and external electrical cardioversion. Resuscitation 2000;45:181-7.
29. Lemery R, Brugada P, Cheriex E, Wellens HJ. Reversibility of tachycardia-induced left ventricular dysfunction after closed-chest catheter ablation of the atrioventricular junction for intractable atrial fibrillation. Am J
Cardiol 1987;60:1406-8.
30. Lown B. Electrical reversion of cardiac arrhythmias. Br Heart J 1967;29:
469-89.
46
Canadian Journal of Cardiology
Volume 27 2011
31. Goldman M. The management of chronic atrial fibrillation: indications
and method of conversion to sinus rhythm. Prof Cardiovasc Dis 1959;2:
465-79.
48. Letelier LM, Udol K, Ena J, Weaver B, Guyatt GH. Effectiveness of
amiodarone for conversion of atrial fibrillation to sinus rhythm: a metaanalysis. Arch Intern Med 2003;163:777-85.
32. Singer DE, Albers GW, Dalen JE, et al. Antithrombotic therapy in atrial
fibrillation: American College of Chest Physicians Evidence-Based Clinical
Practice Guidelines (8th Edition). Chest 2008;133(6 Suppl):546S-52S.
49. Miller MR, McNamara RL, Segal JB, et al. Efficacy of agents for pharmacologic conversion of atrial fibrillation and subsequent maintenance of
sinus rhythm: a meta-analysis of clinical trials. J Fam Pract 2000;49:103346.
34. Schwartzman D, Musley S, Koehler J, Warman E. Impact of atrial fibrillation duration on postcardioversion recurrence. Heart Rhythm 2005;2:
1324-9.
35. Roden DM. Risks and benefits of antiarrhythmic therapy. N Engl J Med
1994;331:785-91.
36. ACLS Guidelines: Part 7.3: Management of symptomatic bradycardia and
tachycardia. Circulation 2005;112:IV-67-IV-77.
37. Nichol G, McAlister FA, Pham B, et al. Meta-analysis of randomised
controlled trials of the effectiveness of antiarrhythmic agents at promoting
sinus rhythm in patients with atrial fibrillation. Heart 2002;87:535-43.
38. Stiell IG, Clement C, Symington C, et al. Emergency department use of
intravenous procainamide for patients with acute atrial fibrillation or flutter. Acad Emerg Med 2007;14:1158-64.
51. Roy D, Pratt CM, Torp-Pedersen C, et al. Vernakalant hydrochloride for
rapid conversion of atrial fibrillation. A phase 3, randomized, placebocontrolled trial. Circulation 2008;117:1518-25.
52. Wyse DG. Initial energy for electrical cardioversion of atrial fibrillation: is
more better? Am J Cardiol 2000;86:324-5.
53. de la Morandiere KP, Morriss H. Paddle position in emergency cardioversion of atrial fibrillation. Emerg Med J 2005;22:44-6.
54. Gage BF, Waterman AD, Shannon W, et al. Validation of clinical classification schemes for predicting stroke: results from the National Registry
of Atrial Fibrillation. JAMA 2001;285:2864-70.
55. Wang TJ, Massaro JM, Levy D, et al. A risk score for predicting stroke or
death in individuals with new-onset atrial fibrillation in the community:
The Framingham Heart Study. JAMA 2003;290:1049-56.
56. Hylek EM, Evans-Molina C, Shea C, et al. Major hemorrhage and tolerability of warfarin in the first year of therapy among elderly patients with
atrial fibrillation. Circulation 2007;115:2689-96.
R
G
39. Blanc JF, De Ledinghen V, Trimoulet P, et al. Premalignant lesions and
hepatocellular carcinoma in a non-cirrhotic alcoholic patient with iron
overload and normal transferrin saturation. J Hepatol 1999;30:325-9.
50. Roy D, Rowe BH, Stiell IG, et al. A randomized, controlled trial of
RSD1235, a novel anti-arrhythmic agent, in the treatment of recent onset
atrial fibrillation. J Am Coll Cardiol 2004;44:2355-61.
O
ED
33. Oral H, Ozaydin M, Sticherling C, et al. Effect of atrial fibrillation duration on probability of immediate recurrence after transthoracic cardioversion. J Cardiovasc Electrophysiol 2003;14:182-5.
40. Khan IA. Single oral loading dose of propafenone for pharmacological
cardioversion of recent-onset atrial fibrillation. J Am Coll Cardiol 2001;
37:542-7.
57. Wyse DG. Bleeding while starting anticoagulation for thromboembolism
prophylaxis in elderly patients with atrial fibrillation: from bad to worse.
Circulation 2007;115:2684-6.
58. Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in
patients with atrial fibrillation. N Engl J Med 2009;361:1139-51.
42. Hongo RH, Themistoclakis S, Raviele A, et al. Use of ibutilide in cardioversion of patients with atrial fibrillation or atrial flutter treated with class
IC agents. J Am Coll Cardiol 2004;44:864-8.
59. van Ryn J, Stangier J, Haertter S, et al. Dabigatran etexilate: a novel,
reversible, oral direct thrombin inhibitor: interpretation of coagulation
assays and reversal of anticoagulant activity. Thromb Haemost 2010;103:
1116-27.
EM
BA
41. Alboni P, Botto GL, Baldi N, et al. Outpatient treatment of recent-onset
atrial fibrillation with the “pill-in-the-pocket” approach. N Engl J Med
2004;351:2384-91.
43. Gowda RM, Khan IA, Wilbur SL, Vasavada BC, Sacchi TJ. Torsade de
pointes: the clinical considerations. Int J Cardiol 2004;96:1-6.
44. Martinez-Marcos FJ, Garcia-Garmendia JL, Ortega-Carpio A, et al. Comparison of intravenous flecainide, propafenone and amiodarone for conversion of acute atrial fibrillation to sinus rhythm. Am J Cardiol 2000;86:
950-3.
45. Tijunelis MA, Herbert ME. Myth: intravenous amiodarone is safe in
patients with atrial fibrillation and Wolff-Parkinson-White syndrome in
the emergency department. Can J Emerg Med 2005;7:262-5.
46. Hilleman DE, Spinler SA. Conversion of recent-onset atrial fibrillation
with intravenous amiodarone: a meta-analysis of randomized controlled
trials. Pharmacotherapy 2002;22:66-74.
47. Chevalier P, Durand-Dubief A, Burri H, et al. Amiodarone versus placebo
and classic drugs for cardioversion of recent-onset atrial fibrillation: a
meta-analysis. J Am Coll Card 2003;41:255-62.
60. Cairns JA, Connolly S, McMurtry S, Stephenson M, Talajic M, CCS
Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: prevention of stroke and systemic
thromboembolism in atrial fibrillation and flutter. Can J Cardiol 2011;
27:74-90.
61. Nieuwlaat R, Dinh T, Olsson SB, et al. Should we abandon the common
practice of withholding oral anticoagulation in paroxysmal atrial fibrillation? Eur Heart J 2008;29:915-22.
62. Stramba-Badiale M. Atrial fibrillation subtypes, risk of stroke, and antithrombotic therapy. Eur Heart J 2008;29:840-2.
63. Klein AL, Grimm RA, Murray D, et al. Use of transesophageal echocardiography to guide cardioversion in patients with atrial fibrillation. N Engl
J Med 2001;344:1411-20.
64. Manning WJ. Strategies for cardioversion of atrial fibrillation: time for a
change? (Editorial). N Engl J Med 2001;344:1468-70.
Canadian Journal of Cardiology 27 (2011) 47–59
Society Guidelines
Canadian Cardiovascular Society Atrial Fibrillation
Guidelines 2010: Rate and Rhythm Management
Anne M. Gillis, MD, FRCPC,a Atul Verma, MD, FRCPC,b Mario Talajic, MD, FRCPC,c
Stanley Nattel, MD, FRCPC,c Paul Dorian, MD, FRCPC,d and the CCS Atrial Fibrillation
Guidelines Committeee
a
University of Calgary/Libin Cardiovascular Institute of Alberta, Calgary, Alberta, Canada
b
Montreal Heart Institute, Université de Montréal and McGill University, Montreal, Québec, Canada
d
e
Southlake Regional Health Centre, Newmarket, Ontario, Canada
St Michael’s Hospital and University of Toronto, Toronto, Ontario, Canada
O
ED
c
For a complete listing of committee members, see Gillis AM, Skanes AC. Canadian Cardiovascular Society Atrial Fibrillation Guidelines
2010: Implementing GRADE and Achieving Consensus. Can J Cardiol 2011;27:27-30.
ABSTRACT
RÉSUMÉ
Les principaux objectifs du traitement de la fibrillation auriculaire (FA) et
du flutter auriculaire sont d’atténuer les symptômes des patients,
d’améliorer leur qualité de vie et de réduire au minimum la morbidité
associée à la FA et au flutter auriculaire. Le traitement de l’arythmie
consiste d’abord à ralentir la fréquence ventriculaire. La décision d’un
traitement avec antiarythmiques de classe I ou III pour la conversion
et/ou le maintien du rythme sinusal repose sur la présence de
symptômes et les préférences du patient. L’objectif du contrôle de la
fréquence ventriculaire pour la FA ou le flutter auriculaire persistant ou
permanent est une fréquence cardiaque inférieure à 100/min au repos.
Les béta-bloquants ou les inhibiteurs calciques (non-dihydropyridine) sont
les médicaments de premier choix pour le contrôle de la fréquence ventriculaire de la FA et du flutter auriculaire chez la plupart des patients sans
antécédent d’infarctus du myocarde ou dysfonction ventriculaire gauche.
La digoxine n’est pas recommandée en monothérapie pour le contrôle de
la fréquence ventriculaire chez les patients actifs. L’ajout de digoxine ou
de dronédarone en combinaison avec d’autres agents peut être considéré
pour optimiser le traitement. Chez les patients dont la fonction ventriculaire
EM
BA
R
G
The goals of atrial fibrillation (AF) and atrial flutter (AFL) arrhythmia management are to alleviate patient symptoms, improve patient quality of
life, and minimize the morbidity associated with AF and AFL. Arrhythmia
management usually commences with drugs to slow the ventricular rate.
The addition of class I or class III antiarrhythmic drugs for restoration or
maintenance of sinus rhythm is largely determined by patient symptoms
and preferences. For rate control, treatment of persistent or permanent
AF and AFL should aim for a resting heart rate of ⬍100 beats per minute.
Beta-blockers or nondihydropyridine calcium channel blockers are the
initial therapy for rate control of AF and AFL in most patients without a
history of myocardial infarction or left ventricular dysfunction. Digoxin is
not recommended as monotherapy for rate control in active patients.
Digoxin and dronedarone may be used in combination with other agents
to optimize rate control. The first-choice antiarrhythmic drug for maintenance of sinus rhythm in patients with non structural heart disease can be
any one of dronedarone, flecainide, propafenone, or sotalol. In patients
with abnormal ventricular function but left ventricular ejection fraction
Atrial fibrillation (AF) and atrial flutter (AFL) are often associated with rapid and irregular ventricular rates causing palpitations, dyspnea, fatigue, reduced exercise tolerance, other symp-
toms, and in some cases, left ventricular dysfunction and
congestive heart failure. The approach to the management of
AF and AFL includes, in parallel, identification and treatment
Received for publication November 4, 2010. Accepted December 3, 2010.
with a mandate to formulate disease-specific recommendations. These recommendations are aimed to provide a reasonable and practical approach to care for specialists and allied health professionals obliged with the duty of bestowing optimal
care to patients and families, and can be subject to change as scientific knowledge
and technology advance and as practice patterns evolve. The statement is not
intended to be a substitute for physicians using their individual judgment in managing clinical care in consultation with the patient, with appropriate regard to all
the individual circumstances of the patient, diagnostic and treatment options available and available resources. Adherence to these recommendations will not necessarily produce successful outcomes in every case.
Corresponding author: Dr Anne M. Gillis, University of Calgary, Cardiac
Sciences, 3280 Hospital Drive N.W., Calgary, Alberta, Canada T2N 4Z6.
Tel: ⫹1-403-220-6841, fax: ⫹1-403-270-0313.
E-mail: amgillis@ucalgary.ca
The disclosure information of the authors and reviewers is available from the
CCS on the following Web sites: www.ccs.ca and www.ccsguidelineprograms.ca.
This statement was developed following a thorough consideration of medical
literature and the best available evidence and clinical experience. It represents the
consensus of a Canadian panel comprised of multidisciplinary experts on this topic
0828-282X/$ – see front matter © 2011 Canadian Cardiovascular Society. Published by Elsevier Inc. All rights reserved.
doi:10.1016/j.cjca.2010.11.001
48
Canadian Journal of Cardiology
Volume 27 2011
Goals of AF Arrhythmia Management
The major goals of AF and AFL arrhythmia management
are to
● Identify and treat underlying structural heart disease and
other predisposing conditions
● Relieve symptoms
● Improve functional capacity and quality of life (QOL)
● Reduce morbidity and mortality associated with AF and
AFL, that is,
● Prevent tachycardia-induced cardiomyopathy
● Reduce or prevent emergency room visits or hospitalizations secondary to AF and AFL
● Prevent stroke or systemic thromboembolism
EM
BA
R
G
of precipitating causes, antithrombotic therapy based on risk
factors for stroke, drug therapy to control ventricular rates, and
antiarrhythmic therapy as required to restore and/or maintain
sinus rhythm with the major goal of alleviating patient symptoms and minimizing the morbidity associated with AF (Fig.
1).1,2 Arrhythmia management usually commences with drugs
to slow the ventricular rate. The addition of class I or class III
antiarrhythmic drugs for restoration or maintenance of sinus
rhythm is largely determined by patient symptoms and preferences as, to date, none of the large randomized trials has demonstrated that pharmacologic therapy to maintain sinus
rhythm has improved survival or reduced the risk of stroke.3-7
AF may be classified as newly detected, paroxysmal (self-terminating episodes lasting ⬍7 days), persistent (non–self-terminating
episodes lasting ⬎7 days), or permanent (no further attempts or
no initial attempt to restore sinus rhythm to be undertaken).8-9
The nature of AF is recurrent and frequently progressive (Fig. 2).
Although a treatment strategy of rate control or rhythm control
may be selected initially, the treatment strategy may change over
time if the selected treatment strategy has been unsuccessful, as the
arrhythmia progresses, or as the patient’s condition changes (Fig.
1).10 Thus, treatment strategies and their effectiveness, safety, and
acceptability must be constantly reevaluated. Factors that might
influence a decision for rate control versus rhythm control are
summarized in Table 1.
AFL may also occur in the patient with AF or may present as
an isolated arrhythmia. The goals of therapy and management
approaches for AFL are similar to those for AF.
est normale, les anti-arythmiques de premier choix pour le maintien du
rythme sinusal incluent la dronédarone, la flécaïnide, la propafénone ou
le sotalol. Chez les patients dont la fonction ventriculaire est anormale
mais avec fraction d’éjection ventriculaire gauche supérieure à 35 %, on
recommande la dronédarone, le sotalol ou l’amiodarone. Chez les patients dont la fraction d’éjection ventriculaire gauche est inférieure à 35
%, seule l’amiodarone est recommandée. Un traitement anti-arythmique
occasionnel (“pill-in-the-pocket”) peut-être considéré comme alternative
au traitement antiarythmique quotidien chez les patients symptomatiques qui présentent des épisodes de FA ou de flutter auriculaire infréquents mais de longue durée. L’ablation par cathéter doit être considérée chez les patients symptomatiques après échec du traitement
antiarythmique et pour lesquels une stratégie de maintien du rythme
sinusal demeure indiquée.
O
ED
⬎35%, dronedarone, sotalol, or amiodarone is recommended. In patients with left ventricular ejection fraction ⬍35%, amiodarone is the
only drug usually recommended. Intermittent antiarrhythmic drug
therapy (“pill in the pocket”) may be considered in symptomatic patients with infrequent, longer-lasting episodes of AF or AFL as an
alternative to daily antiarrhythmic therapy. Referral for ablation of AF
may be considered for patients who remain symptomatic after adequate trials of antiarrhythmic drug therapy and in whom a rhythm
control strategy remains desired.
RECOMMENDATION
We recommend that the goals of ventricular rate control
should be to improve symptoms and clinical outcomes
which are attributable to excessive ventricular rates (Strong
Recommendation, Low-Quality Evidence).
We recommend that the goals of rhythm control therapy
should be to improve patient symptoms and clinical outcomes and that these goals do not necessarily imply the
elimination of all AF (Strong Recommendation, ModerateQuality Evidence).
Overview of AF Management
Detecon and
Treatment of
Precipitang Causes
AF Detected
Patterns of AF
Newly Diagnosed AF
Managementt off
M
Arrhythmia
A
Assessment
t off
Thromboembolic Risk
(CHADS2 )
P
Paroxysmal
l
OAC
Aspirin
Rate
Control
P i
Persistent
Rhythm
Control
No anthromboc may be
appropriate in selected young
paents with no stroke risk factors
Figure 1. Overview of AF management. If a strategy of rate or rhythm
control is not successful, crossover to the alternate strategy may be
required. AF, atrial fibrillation; OAC, oral anticoagulation.
Permanent
Figure 2. Interrelationships among categories of AF. Arrows indicate
most common forms of progression. AF, atrial fibrillation. Adapted
and reprinted with permission from Fuster V, et al.8 Circulation 2006;
114(7):e257-e354. ©2006 American Heart Association, Inc.
Gillis et al.
Rate and Rhythm Management
49
Favours rate control
Favours rhythm control
Persistent AF
Paroxysmal AF
Newly detected AF
More symptomatic
Aged ⬍65 years
No hypertension
Congestive heart failure clearly
exacerbated by AF
No previous antiarrhythmic
drug failure
Patient preference
Less symptomatic
Aged ⱖ65 years
Hypertension
No history of congestive
heart failure
Previous antiarrhythmic
drug failure
Patient preference
AF, atrial fibrillation.
Values and preferences. These recommendations place
a high value on the decision of individual patients to balance
relief of symptoms and improvement in QOL and other
clinical outcomes with the potentially greater adverse effects
of class I or class III antiarrhythmic drugs compared with
rate-control therapy.
EM
BA
R
G
Referral for Specialty Care
Most patients with a history of AF or AFL should be considered for referral to a cardiologist or an internist with an interest in
cardiovascular disease for an expert opinion on management of AF
or AFL, as well as any underlying cardiovascular conditions. Patients aged ⱕ35 years with symptomatic AF should be referred to
an arrhythmia specialist to rule out other forms of supraventricular
tachycardia that may trigger AF (so-called “tachycardia-induced
tachycardia”) and that would be best treated by radiofrequency
ablation. Patients with isolated AFL may also be considered for
referral for curative ablation therapy.11 Patients who remain
highly symptomatic despite multiple trials of antiarrhythmic drug
therapy or who remain unresponsive to or intolerant of rate-controlling therapies should be referred to an arrhythmia specialist for
an expert opinion on management alternatives.
rate-control strategies.15 No difference in the primary outcome
(composite of cardiovascular death, heart failure hospitalization,
stroke, systemic embolism, bleeding, and arrhythmic events) was
found, and the lenient strategy rate goal was achieved in a larger
proportion of patients, with lower drug doses and fewer combinations of drugs, resulting in far fewer visits to achieve the intended
target.15 Relatively few patients randomized to lenient rate control
had resting heart rates ⬎ 100 to 110 bpm. Furthermore, at the end
of the first year, average resting heart rates were 86 ⫾ 15 and 75 ⫾
12 bpm in the lenient and strict rate-control arms, respectively,
and the difference of 10 to 11 bpm remained through the remainder of the trial. Thus, although the definition of lenient seems
quite liberal, in the trial itself the difference in heart rates in the 2
groups was quite small. Since few patients had resting heart rates
⬎100 bpm and previous studies cannot conclusively show the
safety of resting heart rates ⬎100 bpm, we recommend that a
heart rate target of ⬍100 bpm at rest be used for most patients. In
all cases, the heart rate target may need modification based on
patient symptoms and preferences. Patients with persistent or permanent AF or AFL who have exertional symptoms possibly due to
excessive heart rates should have an assessment of rate response to
exercise. Activity heart rate assessment can be achieved in a variety
of ways, including recording heart rate after brisk hall walking or
stair climbing, 24-hour ambulatory monitoring, or formal exercise
testing. Correlation of symptoms and heart rate may also be
achieved by patient-activated electrocardiogram (ECG) rhythm
strips (“event recorders”). In all patients, it is reasonable to verify
that symptoms are caused by rapid ventricular rates. Finally, it
should be noted that rate control in paroxysmal AF is empirical,
and heart rate targets are impractical for these briefer episodes of
AF.
O
ED
Table 1. Factors favouring rate versus rhythm control
Rate Control of AF and AFL
Rate control is an important part of therapy for all patients with AF or AFL. The primary goal of rate control is to
improve symptoms and prevent deterioration of cardiac
function associated with excessively rapid ventricular rates
during AF or AFL. In addition, therapy for rate control
should aim to improve exercise tolerance, QOL, and to
avoid hospitalization. Tachycardia-induced cardiomyopathy refers to a condition characterized by reversible left ventricular systolic dysfunction occurring in patients with
chronic rapid heart rates. This complication can occur in
some patients with AF or AFL and very rapid ventricular
rates (eg, ⬎120/min for most or all of the time) and is totally
or partially reversible and preventable with adequate rate
control.12
Heart rate targets
In the past, adequate heart rate control had been empirically
defined as ⱕ80 beats per minute (bpm) at rest.3-6,8,13,14 A recent
study randomized patients to strict (ⱕ80 bpm at rest and ⱕ110
bpm during moderate exercise) or lenient (⬍110 bpm at rest)
RECOMMENDATION
We recommend that ventricular rate be assessed at rest in
all patients with persistent and permanent AF or AFL
(Strong Recommendation, Moderate-Quality Evidence).
We recommend that heart rate during exercise be assessed in patients with persistent or permanent AF or AFL
and associated exertional symptoms (Strong Recommendation, Moderate-Quality Evidence).
We recommend that treatment for rate control of persistent or permanent AF or AFL should aim for a resting heart
rate of ⬍100 bpm (Strong Recommendation, High-Quality Evidence).
Values and preferences. These recommendations place a
high value on the randomized clinical trials and other clinical
studies demonstrating that ventricular rate control of AF is an
effective treatment approach for many patients with AF.
Heart rate control agents
Beta-blockers, nondihydropyridine calcium channel
blockers (diltiazem, verapamil), and digitalis are the primary
drugs used for ventricular rate control during AF or AFL.
The approach to selection of rate-control agents is shown in
Figure 3. The doses, adverse effects, and practical tips about
the different rate-control agents are summarized in Table 2.
All these drugs act by slowing atrioventricular (AV) nodal
conduction and prolonging AV nodal refractoriness. Many
50
Canadian Journal of Cardiology
Volume 27 2011
Rate-control Drug Choices
No Heart
Disease
Hypertension
CAD
Heart Failure
β-blocker
Dilazem
Verapamil
Combinaon Rx
Digitalis†
Di
it li †
β-blocker*
Dilazem
Verapamil
β -blocker
bl k
± digitalis
*β-blockers preferred in CAD
†Digitalis may be considered as
monotherapy in sedentary individuals
beta-adrenoceptor blockers or calcium channel blockers
during exercise. Digitalis should thus be avoided as the sole
agent in active patients.21,22 On its own, digoxin does not
routinely control the heart rate and frequently has to be
combined with another rate-slowing drug. Drug combinations are frequently effective when treatment with a single
agent fails. Dronedarone is a newly released analogue of
amiodarone with significant rate-controlling properties23
which may also be useful in selected patients. Amiodarone
has significant rate-controlling properties in addition to its
antiarrhythmic actions and may be used in refractory patients. However, because of the risk of toxicity associated
with long-term use, it should be used only when other ratecontrol strategies are not feasible or are insufficient.
RECOMMENDATION
Figure 3. Selection of rate-control drug therapy is based on the
presence or absence of underlying heart disease and other comorbidities. Combination therapy (Rx) may be required. CAD, coronary
artery disease.
EM
BA
R
G
small comparative drug trials have been performed but have
not shown major advantages of one agent over another.13-19
In small, mostly blinded randomized trials, beta-adrenoceptor blockers led to lower heart rates at rest and exercise but
no change or a decrease in exercise capacity.14 Calcium
channel blockers were less effective at heart rate lowering on
exercise but led to an increase or no change in exercise capacity. In one study, beta-adrenoceptor blockers added to
digoxin did not result in improved QOL, whereas calcium
blockers resulted in small improvements in physical and
emotional function.20
Digitalis prolongs AV nodal refractoriness by enhancing
vagal tone. During exercise, vagal tone is withdrawn, and
therefore digitalis controls the heart rate less effectively than
We recommend beta-blockers or nondihydropyridine
calcium channel blockers as initial therapy for rate control
of AF or AFL in most patients without a past history of
myocardial infarction or left ventricular dysfunction
(Strong Recommendation, Moderate-Quality Evidence).
We suggest that digoxin not be used as initial therapy for
active patients and be reserved for rate control in patients
who are sedentary or who have left ventricular systolic dysfunction (Conditional Recommendation, Moderate-Quality Evidence).
We suggest that digoxin be added to therapy with betablockers or calcium channel blockers in patients whose
heart rate remains uncontrolled (Conditional Recommendation, Moderate-Quality Evidence).
We suggest that dronedarone may be added for additional rate control in patients with uncontrolled ventricular
rates despite therapy with beta-blockers, calcium channel
blockers, or digoxin (Conditional Recommendation, Moderate-Quality Evidence).
We suggest that amiodarone for rate control should be
reserved for exceptional cases in which other means are not
feasible or are insufficient (Conditional Recommendation,
Low-Quality Evidence).
O
ED
Dronedarone
Table 2. Drugs for heart rate control
Class
Dose
Adverse effects
Beta-blockers
Atenolol
50-150 mg orally daily
Bradycardia, hypotension,
fatigue, depression
As per atenolol
As per atenolol
Bisoprolol
Metoprolol
Nadolol
Propranolol*
Calcium channel
blockers
Verapamil*
Diltiazem*
Digoxin
2.5-10 mg orally daily
25-200 mg orally twice a
day
20-160 mg orally daily to
twice a day
80-240 mg orally 3 times
a day
120 mg orally daily to
240 mg orally twice a
day
120-480 mg orally daily
0.125-0.25 mg orally
daily
Values and preferences. These recommendations recognize that selection of rate-control therapy needs to be
individualized on the basis of the presence or absence of
underlying structural heart disease, the activity level of the
patient, and other individual considerations.
As per atenolol
As per atenolol
Bradycardia, hypotension,
constipation
Bradycardia, hypotension,
ankle swelling
Bradycardia, nausea,
vomiting, visual
disturbances
* Sustained release preparations are available and generally preferred to
prolong the dose interval and improve patient convenience or compliance.
Rate control in specific patient populations
Beta-blockers are preferred as a rate-control agent in patients after myocardial infarction and in patients with congestive heart failure.24 Calcium channel blockers should be
avoided in these populations but may be preferred in patients
with chronic pulmonary disease and at risk of bronchoconstriction.14,19 Digitalis may be useful as monotherapy in sedentary
patients and is often useful in combination with beta-blockers
or calcium channel blockers.
Practical tip. Carvedilol is a less-potent -adrenergic
blocking agent compared to metoprolol. Carvedilol is less effective for rate control of AF compared to metoprolol.25
Gillis et al.
Rate and Rhythm Management
51
We recommend beta-blockers as initial therapy for rate
control of AF or AFL in patients with myocardial infarction
or left ventricular systolic dysfunction (Strong Recommendation, High-Quality Evidence).
Values and preferences. This recommendation places a
high value on the results of multiple randomized clinical
trials reporting the benefit of beta-blockers to improve survival and decrease the risk of recurrent myocardial infarction
and prevent new-onset heart failure following myocardial
infarction, as well as the adverse effects of calcium channel
blockers in the setting of heart failure.
RECOMMENDATION
We recommend the optimal treatment of precipitating
or reversible predisposing conditions of AF prior to attempts to restore or maintain sinus rhythm (Strong Recommendation, Low-Quality Evidence).
We recommend a rhythm-control strategy for patients
with AF or AFL who remain symptomatic with rate-control
therapy or in whom rate-control therapy is unlikely to control symptoms (Strong Recommendation, Moderate-Quality Evidence).
We recommend that the goal of rhythm-control therapy
should be improvement in patient symptoms and clinical
outcomes, and not necessarily the elimination of all AF
(Strong Recommendation, Moderate-Quality Evidence).
EM
BA
R
G
Nonpharmacologic Treatment
Some patients may require the implantation of a permanent pacemaker to manage drug-exacerbated symptomatic bradycardia, particularly in patients with paroxysmal AF and sinus node disease associated with symptomatic sinus pauses, and thus safely allow adequate
pharmacologic control of rapid ventricular rates. Isolated nocturnal
pauses are often observed in asymptomatic patients with persistent or
permanent AF and do not constitute an indication for pacing.
AV junction ablation requiring the implantation of a permanent pacemaker should be considered in patients with refractory
symptoms associated with excessive heart rates despite adequate
trials of rate-control drugs, including combination drug therapy.
This procedure results in adequate rate control in virtually all patients and has been associated with improvements in clinical
symptoms, exercise tolerance, QOL, and ventricular function.26
Biventricular pacing should be considered after AV junction ablation in patients with left ventricular systolic dysfunction.27 In selected patients, control of AF by left atrial or pulmonary vein
catheter ablation to restore sinus rhythm can be considered as an
alternative to AV nodal ablation requiring permanent pacing.9,11
Practical tip. As an alternative to AV junction ablation, an
attempt at restoration of sinus rhythm via electrical or pharmacologic cardioversion may be warranted to control heart rate in
cases in which this can be achieved, such as in the setting of
persistent AF or AFL.
shown to decrease mortality or reduce the incidence of thromboembolic complications in AF patients compared to rate control
alone.3-7 Thus, the decision to pursue sinus rhythm maintenance
should be directed to patients who remain symptomatic with AF
or AFL despite adequate rate control (Table 1). Symptoms may
include palpitations, fatigue, exercise intolerance, or symptoms of
heart failure. In these patients, restoration and maintenance of
sinus rhythm can alleviate these symptoms and improve QOL.
Improvement in patient QOL and function, and not the total
elimination of AF, should always be the focus of rhythm control.
The benefits of any antiarrhythmic drug therapy must also be
balanced against the side effects and toxicities of such therapy. If
drug therapy fails to achieve a meaningful improvement in patient
QOL, then alternatives to the strategy of pharmacologic rhythm
control should be considered, including catheter ablation of AF or
rate control alone.
Practical tip. When pursuing a rhythm-control strategy for
AF, there needs to be a reasonable expectation of maintenance
of sinus rhythm.
O
ED
RECOMMENDATION
Values and preferences. These recommendations place
a high value on the decision of individual patients to balance
relief of symptoms and improvement in QOL and other
clinical outcomes with the potentially greater adverse effects
of the addition of class I or class III antiarrhythmic drugs to
rate-control therapy.
RECOMMENDATION
We recommend AV junction ablation and implantation
of a permanent pacemaker in symptomatic patients with
uncontrolled ventricular rates during AF despite maximally
tolerated combination pharmacologic therapy (Strong Recommendation, Moderate-Quality Evidence).
Values and preferences. This recommendation places a
high value on the results of many small randomized trials and
one systematic review reporting significant improvements in
QOL and functional capacity as well as a decrease in hospitalizations for AF following AV junction ablation in highly symptomatic patients.
Rhythm Control of AF and AFL
It is important to emphasize that compared with rate control
alone, the strategy of maintaining sinus rhythm has never been
Mechanism of action of antiarrhythmic drugs
The mechanisms underlying AF are complex, likely differing among patients and even within individual patients as a
function of the evolution of their cardiac condition.28 It has
been hypothesized that AF is initiated by arrhythmogenic foci,
often originating in the pulmonary veins.29 However, AF is
maintained by multiple small reentrant wavelets, sometimes
described as “rotors.”30 Formation and persistence of these
wavelets is favoured by a shortened atrial refractory period and
action potential duration, which occur during AF.31 The primary action of many antiarrhythmic medications is to lengthen
refractory periods by prolonging action potential duration, to
inhibit the formation of wavelets responsible for AF maintenance,32 or to reduce the phase-0 sodium current to destabilize
AF-maintaining rotors.33-35
52
Canadian Journal of Cardiology
Volume 27 2011
Table 3. Antiarrhythmic drugs for rhythm control
I
Dosage
Efficacy at 1 Year
Toxicity
Comments
Flecainide
50-150 mg twice/d
30%-50%
Propafenone
150-300 mg 3 times/d
30%-50%
Contraindicated in patients with CAD or LV
dysfunction
Should be combined with an AV nodal
blocking agent
Contraindicated in patients with CAD or LV
dysfunction
Should be combined with an AV nodal
blocking agent
Amiodarone
100-200 mg OD (after 10 g
loading)
60%-70%
Dronedarone
400 mg twice/d
40%
Ventricular tachycardia
Bradycardia
Rapid ventricular response to AF or
atrial flutter (1:1 conduction)
Ventricular tachycardia
Bradycardia
Rapid ventricular response to AF or
atrial flutter (1:1 conduction)
Abnormal taste
Photosensitivity
Bradycardia
GI upset
Thyroid dysfunction
Hepatic toxicity
Neuropathy, tremor
Pulmonary toxicity
Torsades de pointes (rare)
GI upset
Bradycardia
Sotalol
40-160 mg twice/d
30%-50%
Torsades de pointes
Bradycardia
Beta-blocker side effects
R
G
III
Drug
Low risk of proarrhythmia in a wide range of
populations
Limited by systemic side effects
Most side effects are dose and duration
related
Very effective for rate control
Only antiarrhythmic shown to reduce
hospitalizations and cardiovascular
mortality in ATHENA trial
May increase mortality in patients with
recently decompensated heart failure, EF
⬍35% (ANDROMEDA trial)
Effective rate-control agent
New drug – limited experience outside trials
Should be avoided in patients at high risk of
torsades de pointes VT - especially women
aged ⬎65 y taking diuretics or those with
renal insufficiency
QT interval should be monitored 1 wk after
starting
Use cautiously when EF ⬍40%
Heart rhythm specialists may use with lower
EFs if patient has ICD
O
ED
Class
BA
ANDROMEDA, Antiarrhythmic Trial With Dronedarone in Moderate to Severe Congestive Heart Failure Evaluating Morbidity Decrease; ATHENA, A
Placebo-Controlled Double-Blind, Parallel Arm Trial to Assess the Efficacy of Dronedarone 400 Mg Bid for the Prevention of Hospitalization or Death From Any
Cause in Patients With Atrial Fibrillation/Flutter; AV, atrioventricular; CAD, coronary artery disease; EF, ejection fraction; ICD, implantable cardioverter defibrillator; LV, left ventricular; VT, ventricular tachycardia.
EM
Class I drugs, such as flecainide and propafenone, block
sodium channels.35 This slows atrial conduction, lengthens
atrial refractoriness, and suppresses automaticity.36 By destabilizing AF-maintaining rotors, this class of drugs can
prevent the persistence of AF.33-35 Class III drugs such as
sotalol or dofetilide block potassium channels and thus prolong action potential duration.37 With sufficient action potential prolongation, class III drugs prevent AF recurrence.
Drugs such as amiodarone and dronedarone have multiple
effects, including both class I and class III mechanisms of action.38 Both drugs also have noncompetitive beta-blocking and
calcium channel blocking effects. Thus, both not only are capable of maintaining sinus rhythm but can be effective ratecontrol agents as well.23,39
Antiarrhythmic drug therapy to maintain sinus rhythm
In the absence of an antiarrhythmic drug, the recurrence rate of
AF is about 75% over 1 year.8 Thus, recurrences are very likely
once the AF process starts. If a decision is made to pursue a longterm strategy of rhythm control, patients will often require maintenance oral antiarrhythmic drug therapy. While antiarrhythmic
drugs will not completely eliminate AF, they can substantially
reduce AF burden and improve QOL. Reduction of AF burden by
itself without demonstration of alleviated symptoms or reduced
morbidity is insufficient to recommend the routine use of class I or
class III antiarrhythmic drugs. Ideally, such therapy should also
reduce other, more quantitative outcomes such as hospitalization
or even mortality, but to date, only limited data exist to support
the notion that rhythm-control therapy can accomplish such
goals.39-41
The dosages, efficacy, side effects, and some practical tips
about the various antiarrhythmic drugs are summarized in
Table 3. The choice of drugs to use depends on an individual
patient’s profile and the presence or absence of underlying structural heart disease, as summarized in Figures 4 and 5. Of all the
currently available antiarrhythmic drugs, amiodarone has
been demonstrated to have the highest efficacy in reducing
AF burden.42,43 Unfortunately, it also has numerous important noncardiac side effects, which prevent it from being
used as an agent of first choice.44 Other antiarrhythmic
drugs are less efficacious but have fewer side effects compared with amiodarone.42 These drugs still carry some risk
however, particularly in patients with underlying heart disease.45 Thus, the choice of which antiarrhythmic agent to
use long-term should be guided by evidence-based outcomes (where available) and the safety and efficacy profile of
each agent in the context of the specific clinical profile of the
patient (see Table 3 and Figs. 4 and 5).
In patients with normal ventricular function, the firstchoice antiarrhythmic drug can be either dronedarone, flecai-
Gillis et al.
Rate and Rhythm Management
53
Dronedarone
Flecainide*
Propafenone*
Propafenone
Sotalol
Catheter Ablation
Amiodarone
* Class I agents should be AVOIDED in CAD
They should be combined with AV-nodal blocking agents
Figure 4. Antiarrhythmic drug choices for prevention of atrial fibrillation in patients without structural heart disease. Antiarrhythmic drugs
are presented in alphabetical order. Given the side effect profile of
amiodarone, its use is generally reserved for occasions when other
drug choices have been demonstrated to be ineffective, contraindicated, or not well-tolerated. CAD, coronary artery disease; AV,
atrioventricular.
EM
BA
R
G
nide, propafenone, or sotalol. These drugs are less effective
(with respect to reducing the number and duration of recurrences) than amiodarone42,43 but also have fewer side effects.
Flecainide, propafenone, sotalol, and dronedarone likely have
similar efficacy in maintaining sinus rhythm, based on their
efficacies.39,42,43,46-48 However, direct comparisons of these
drugs for suppression of AF have not been made. Propafenone
and flecainide must be combined with an AV nodal blocking
agent in order to avoid paradoxically increasing the ventricular
rate during AF or AFL (see below).45 Furthermore, a specific
effort (eg, stress test) should be made to exclude ischemic heart
disease in those ⬎50 years of age or anyone with symptoms
suggestive of ischemic heart disease, or Framingham high-risk
patients when propafenone and flecainide drugs are to be used.
Sotalol carries a higher risk of torsades de pointes, particularly
in women or those with renal insufficiency.48-50 Dronedarone
has a structure similar to amiodarone, although dronedarone is
known to be less effective in maintaining sinus rhythm.51,52
Dronedarone is generally well-tolerated, with a relatively
low incidence of side effects or proarrhythmia. In the
ATHENA (A Placebo-Controlled, Double-Blind, Parallel
Arm Trial to Assess the Efficacy of Dronedarone 400 Mg bid
for the Prevention of Cardiovascular Hospitalization or
Death From Any Cause in Patients With Atrial Fibrillation/
Flutter) trial, dronedarone was shown to reduce hospitalization and cardiovascular mortality in AF patients.39 The
panel chose not to make a specific recommendation that
dronedarone should be the first antiarrhythmic drug considered for prevention of AF since dronedarone’s efficacy for
maintenance of sinus rhythm is comparable to other modestly effective rhythm-control agents (flecainide, propafenone,
and sotalol). Also, dronedarone has been shown to be harmful in
patients with decompensated heart failure (see below).53 It is possible that the rate-control effects of dronedarone contributed to
the reduction in hospitalizations for AF reported in ATHENA.
In patients with abnormal ventricular function but left
ventricular ejection fraction ⬎35%, dronedarone, sotalol,
and amiodarone are all reasonable choices (Fig. 5). However, in patients with left ventricular ejection fraction
⬍35%, amiodarone, is the only drug usually recommended
because of its low risk of proarrhythmia in heart failure.4,54
Sotalol or dronedarone could be considered for treatment of
AF in dronedarone patients with a left ventricular ejection
fraction ⬍35% and in the absence of symptoms of severe
heart failure, particularly if they have an implantable cardioverter defibrillator. There is an increased risk of proarrhythmia in heart failure patients taking sotalol,45 likely because
of downregulation of potassium currents and loss of repolarization reserve with heart failure.55 However, sotalol is
used selectively by heart rhythm specialists in patients protected by an implantable defibrillator. The ANDROMEDA
(Antiarrhythmic Trial With Dronedarone in Moderate to
Severe Congestive Heart Failure Evaluating Morbidity Decrease) trial found that dronedarone may increase the risk of
mortality in recently decompensated heart failure patients
in recently decompensated individuals (New York Heart
Association classes III and IV) who were hospitalized.53
Although the American College of Cardiology, American
Heart Association, and European Society of Cardiology 2006
AF guidelines do not recommend the use of propafenone, flecainide, or sotalol in the setting of hypertension and documented left ventricular hypertrophy,8 the writing group felt
that the scientific data supporting this recommendation is
weak. Certainly, concern about the use of these drugs due to
increased risk of proarrhythmia is warranted if abnormalities of
repolarization are noted in the ECG. However, in this setting
the choice of antiarrhythmic drug should be individualized on
the basis of the patient profile and consideration of the risks
and benefits of each drug.8
O
ED
Antiarrhythmic Drug Choices
N
l Ventricular
V t i l Function
F
ti
Normal
Antiarrhythmic Drug Choices
Abnormal Left Ventricular Function
EF > 35%
EF ≤ 35%
Amiodarone
Dronedarone
Sotalol*
Amiodarone
Catheter Ablation
* Sotalol should be used with caution with EF 35-40%
Contraindicated in women >65 yrs taking diuretics
Figure 5. Antiarrhythmic drug choices for prevention of AF in patients
with depressed left ventricular systolic function. Dronedarone is contraindicated in patients with acutely decompensated heart failure. Sotalol
may be used with caution in selected patients with mild to moderate
reduction in left ventricular ejection fraction. EF, ejection fraction.
54
Canadian Journal of Cardiology
Volume 27 2011
RECOMMENDATION
R
G
We recommend use of maintenance oral antiarrhythmic
therapy as first-line therapy for patients with recurrent AF in
whom long-term rhythm control is desired (see Figs. 4 and 5)
(Strong Recommendation, Moderate-Quality Evidence).
We recommend that oral antiarrhythmic drug therapy
should be avoided in patients with AF or AFL and advanced
sinus or AV nodal disease unless the patient has a pacemaker
or implantable defibrillator (Strong Recommendation,
Low-Quality Evidence).
We recommend that an AV blocking agent should be
used in patients with AF or AFL being treated with a class I
antiarrhythmic drug (eg, propafenone or flecainide) in the
absence of advanced AV node disease (Strong Recommendation, Low-Quality Evidence).
therefore cause an increased ventricular response due to a
reduction in the number of concealed activations in the AV
node. In the most extreme cases with very slow organized
atrial activation, conversion of AF to AFL and subsequent
1:1 conduction of AFL can ensue, causing a very high ventricular rate and risk of ventricular tachyarrhythmia.
Practical tip. Class I agents should be combined with an
AV nodal blocking agent (beta-blocker, verapamil, diltiazem,
or digoxin) to avoid this risk.
Certain class III agents, such as sotalol, lengthen the QT
interval and carry a risk of torsades de pointes polymorphic
ventricular tachycardia (VT) (1%-3%). Any additional risk
factor that prolongs the QT interval increases the likelihood
of torsades de pointes VT. This includes female sex, left
ventricular dysfunction, significant left ventricular hypertrophy, bradycardia, or hypokalemia or hypomagnesemia
(often resulting from diuretic use). By reducing net repolarizing current,45,55,58 these factors can individually or collectively reduce “repolarization reserve” and increase the risk of
drug-induced torsades de pointes. Advanced age reduces the
efficiency of drug-eliminating systems (renal function, biotransforming capacity), as well as the volume of distribution
for many drugs, and is therefore also a risk factor for druginduced torsades de pointes. Since sotalol is cleared via the
kidneys, any renal dysfunction also increases the proarrhythmic risk. Periodic ECG monitoring of the QT interval
should be performed and the drug should be reassessed if the
QT is longer than 500 ms or the QTc exceeds 480 ms. Other
drugs that increase the QT interval (erythromycin, clarithromycin, antipsychotics) should be avoided by a patient
while on sotalol (a full list is available at www.torsades.org).
Amiodarone and dronedarone both carry a low risk of
proarrhythmia because of their multiple class effects. Dronedarone is generally safe and well-tolerated. In patients with decompensated heart failure, however, it has been shown to increase mortality (Table 3).53 Amiodarone rarely causes torsades
de pointes VT, but has numerous noncardiac toxicities.44 Patients should avoid direct sun exposure to avoid photosensitivity. A clinical exam, with careful history to elicit symptoms of
toxicity (eg, sleep disturbance, tremor, gait instability, constipation), and pulmonary assessment should be performed periodically to check for toxicity. Hepatic enzymes and thyrotropin
should be measured every 6 months in all patients on amiodarone, regardless of symptoms.
Bradycardia can be exacerbated by any antiarrhythmic
agent, whether because of sinus node or AV node dysfunction.
If bradycardia results in symptoms, the drug should be discontinued, or consideration should be given to implantation of a
permanent pacemaker.
Generally, class I or class III antiarrhythmic drugs may be
initiated as an outpatient, in spite of the risk of proarrhythmia. Particularly in patients with no underlying heart disease, the risk of proarrhythmia is quite low. If a conduction
disturbance (such as sinus or AV node dysfunction) is present or if a patient has risk factors for torsades de pointes VT
or significant underlying heart disease, then consideration
should be given to drug initiation in hospital. Amiodarone is
the only medication that has been shown to be safe when
initiated as an outpatient in patients with heart failure and
left ventricular dysfunction.4,5
O
ED
As previously discussed, the goal of antiarrhythmic drug
therapy should be reduction (not necessarily elimination) of
AF burden with concomitant improvement in QOL. If a
patient has occasional breakthroughs of AF, but few symptoms, therapy may be considered successful. Antiarrhythmic
drug therapy should be reassessed periodically based on both
efficacy and side effects. If patients fail to respond to or
cannot tolerate a particular drug, an alternative drug may be
tried after an appropriate washout period. If a patient fails
multiple medications, then alternatives to consider include
catheter ablation of AF to maintain sinus rhythm (SR) or
abandonment of rhythm control in favour of rate control
alone (Fig. 1).
EM
BA
Values and preferences. These recommendations place
a high value on the decision of individual patients to balance
relief of symptoms and improvement in QOL and other
clinical outcomes with the potentially greater adverse effects
of class I and class III antiarrhythmic drugs compared with
rate-control therapy.
Risks of antiarrhythmic drug therapy
Risks of the various antiarrhythmic drugs are listed in
Table 3. All antiarrhythmic drugs carry the potential of
proarrhythmia, so that treatment of AF or AFL may increase
the risk of other, more malignant arrhythmias (often ventricular in origin).45 The class I agents (flecainide and
propafenone) can increase the risk of ventricular arrhythmias in patients with coronary artery disease or left ventricular dysfunction, so these agents should be avoided in these
populations.56,57 Class I agents slow the atrial rate in AF by
slowing conduction in reentrant rotors or wavelets. The
ventricular response to AF is determined by complex interactions between the rate and pattern of activation of the
proximal AV node from the atrium on one hand and the
refractory properties of the AV node on the other. Because
of the decremental conduction properties of AV nodal tissue
(involving Ca2⫹-current– dependent action potentials and
zones of poor cell-to-cell coupling), atrial impulses that fail
to conduct through the AV node leave the node partially
refractory to the next impulse, a phenomenon called concealed conduction. Paradoxically, a slowing in atrial rate can
Gillis et al.
Rate and Rhythm Management
55
Pretreatment with antiarrhythmic drugs for 1 to 4 weeks
prior to cardioversion can improve the acute efficacy of cardioversion and reduce the chance of early recurrence of AF postcardioversion, particularly in patients with prior recurrence
postcardioversion.60-62
Cardioversion may need to be repeated if antiarrhythmic drug
therapy is changed because of recurrent persistent AF. Even when
a patient is doing well on maintenance antiarrhythmic therapy,
occasional recurrences of persistent AF can occur and may require
a change in the antiarrhythmic drug regimen. In such patients,
intermittent cardioversion to restore sinus rhythm may be an integral part of the long-term rhythm-control strategy.
RECOMMENDATION
O
ED
We recommend electrical or pharmacologic cardioversion for restoration of sinus rhythm in patients with AF or
AFL who are selected for rhythm-control therapy and are
unlikely to convert spontaneously (Strong Recommendation, Low-Quality Evidence).
We recommend pretreatment with antiarrhythmic
drugs prior to electrical cardioversion in patients who have
had AF recurrence postcardioversion without antiarrhythmic drug pretreatment (Strong Recommendation, Moderate-Quality Evidence).
Values and preferences. These recommendations place
a high value on the decision of individual patients to pursue
a rhythm-control strategy for improvement in QOL and
functional capacity.
RECOMMENDATION
BA
R
G
Intermittent Antiarrhythmic Drug Therapy (“Pill
in the Pocket”)
Some patients with symptomatic AF have relatively long-lasting episodes (eg, ⬎4 hours) but with long intercurrent periods of
sinus rhythm between episodes (eg, ⬍2-6/y). In these patients, a
strategy of daily maintenance antiarrhythmic drug therapy may be
unnecessary. An alternative possibility is to prescribe oral antiarrhythmic drugs that can be taken at the time of an episode for
acute termination of AF. Clinical trial data have shown this “pill in
the pocket” strategy to be both safe and effective.59 The drugs
most commonly used for this purpose are class I agents given as
a single dose at the onset of AF. Flecainide is given as a single
or cumulative 200 to 300-mg dose, and propafenone is given as a
single 450 to 600-mg dose. Both these agents have a 50% to 80%
efficacy in acutely terminating AF. Some physicians also prescribe
a rapidly acting beta-blocker (eg, metoprolol 50 to 100 mg), to be
taken at the same time as the class I antiarrhythmic agent in order
to minimize the risk of accelerating the ventricular response. In
patients taking daily medication, an additional dose of the drug
can be used in this manner.
Practical tip. Because of the risk of 1:1 AV conduction of AFL
or the risk of bradycardia, an initial trial of this strategy may be performed in a monitored setting to verify safety and efficacy of this
approach in a given patient. Combination with a rapidly acting betablocker or calcium blocker is recommended (for patients not already
on AV nodal blocking medication or known significant AV nodal
dysfunction), particularly in patients in whom this approach has been
verified in a monitored setting or in patients with little risk of bradycardia or hypotension associated with this therapy.
Patients should ensure their drugs have not expired if the
time between episodes is very long.
EM
We recommend intermittent antiarrhythmic drug
therapy (“pill in the pocket”) in symptomatic patients
with infrequent, longer-lasting episodes of AF or AFL as
an alternative to daily antiarrhythmic therapy (Strong
Recommendation, Moderate-Quality Evidence).
Values and preferences. This recommendation places a
high value on the results of clinical studies demonstrating
the efficacy and safety of intermittent antiarrhythmic drug
therapy in selected patients.
Cardioversion as part of the rhythm-control strategy
Maintenance antiarrhythmic drug therapy can be very effective
at preventing AF recurrences. However, these drugs, given at
maintenance doses, are unlikely to convert patients to sinus
rhythm if AF is already present. Longer durations of AF (⬎48
hours) are particularly less likely to convert to sinus rhythm in
response to antiarrhythmic drugs. Thus, patients in AF for whom
rhythm control is desired should be considered for electrical cardioversion prior to initiation of maintenance antiarrhythmic therapy. Pharmacologic cardioversion is much less effective than electrical cardioversion. If the patient has never had an attempt at
restoration of sinus rhythm, it may be appropriate to observe the
patient postcardioversion without antiarrhythmic therapy.
Drug conversion of AF
Acute restoration of sinus rhythm from recent onset AF is most
commonly performed using electrical cardioversion. Drug conversion
may, however, be an effective alternative. While less effective than the
electrical method, pharmacologic conversion avoids the need for general anaesthesia and may reduce the risk of early recurrence of AF. Oral
antiarrhythmic agents such as flecainide and propafenone may be
given as single doses (see discussion of “pill in the pocket,” above).59
Ibutilide is an intravenous class III medication that is typically given as
a single dose of 1 mg, which may be repeated once. It is superior to
intravenous procainamide, but its use is limited by a 2% to 3% risk of
torsades de pointes VT.63,64 Ibutilide is more effective for AFL than
for AF. The risk of torsades de pointes VT associated with ibutilide
can be reduced by pretreatment with 1 to 2 g magnesium sulphate
administered intravenously.65 Intravenous procainamide can also be
used as a single dose of 15 to 17 mg/kg over 20 to 30 minutes but is
associated with a 5% risk of hypotension and is less effective than
ibutilide.63,64 Intravenous and oral amiodarone are not effective for
acute conversion (conversion in ⬍6-8 hours) of AF and therefore
should not be used routinely for this purpose.66,67
Need for anticoagulation
When considering either electrical or pharmacologic cardioversion
of AF, patients should be adequately anticoagulated to prevent postconversion thromboembolic complications.2,8,68 The risk of thromboembolism is the same whether conversion is achieved electrically or
with drugs.2-8 Although oral antiarrhythmic drug therapy given in
maintenance doses is less likely to acutely convert AF to sinus rhythm,
56
Canadian Journal of Cardiology
Volume 27 2011
Table 4. Randomized trials of pacing modes and impact on AF occurrence
Number
Age (y)
Pacing indication
Follow-up (y)
Pacing modes
AF occurrence (%/y)
Risk reduction (%)
P value
Danish80 AAI vs VVI
CTOPP81
Extended82 CTOPP
MOST83
Danish87 AAI vs DDD
225
71 ⫾ 17
SND
5.5
AAI vs VVI
4.1 vs 6.6
46
.012
2568
73 ⫾ 10
All pacemaker patients
3.1
AAI/R or DDD/R vs VVI/R
5.3 vs 6.3
18
.05
2568
73 ⫾ 10
All pacemaker patients
6.4
AAI/R or DDD/R vs VVI/R
4.5 vs 5.7
20
.009
2050
74 (67-80)
SND
2.7
DDDR vs VVIR
7.9 vs 10.0
21
.008
177
74 ⫾ 9
SND
2.9
AAI vs DDDR-s vs DDDR-l
2.4 vs 8.3 vs 6.2
73
.02
AF, atrial fibrillation; AAI, atrial pacing; AAAIR, atrial rate adaptive pacing; CTOPP, Canadian Trial of Physiologic Pacing; DDDR, dual chamber rate adaptive
pacing; DDDR-l, long atrioventricular delay; DDDR-s, short atrioventricular delay; SND, sinus node disease; VVI, ventricular pacing; VVIR, ventricular rate
adaptive pacing.
O
ED
trophysiologic parameters important for AF which might provide
novel therapeutic targets for therapy of AF.9,70,71 Candidates for upstream therapy include statins (3 hydroxy-3-methyl-glutaryl-CoA reductase inhibitors), drugs that suppress the renin-angiotensin-aldosterone system, and omega-3 fatty acids. Statins may prevent adverse
atrial electrical remodelling associated with AF by anti-inflammatory
antioxidant, anti-proliferatory, or antiapoptotic effects.70-74 Blockers
of the renin angiotensin system may prevent myocyte hypertrophy,
apoptosis, and intercellular fibrosis, as well as exerting indirect effects
on atrial myocyte electrophysiology.70,75 Clinical studies have reported that statin therapy may prevent AF, particularly in patients
following cardiac surgery.76 However, a consistent benefit has not
been observed in all patient groups evaluated.77 Drugs which inhibit
the renin angiotensin system have been reported to be effective for
primary and secondary prevention of AF, with the greatest benefit
observed in patients with left ventricular hypertrophy and/or heart
failure.78 However, valsartan did not prevent AF recurrence in the
largest randomized prospective trial to date, testing the hypothesis that
angiotensin receptor blockade might be an effective therapy for AF.79
At present, studies are underway evaluating the role of omega-3 fatty
acids for prevention of AF.71,73,74 The evidence to date, however theoretically appealing, does not support specific recommendations directed at upstream molecular targets as part of the management strategy for AF.
BA
R
G
one should consider appropriate anticoagulation prior to starting any
antiarrhythmic drug therapy in patients who are in persistent AF. This
applies even to patients who have low risk of stroke and may not
require long-term systemic anticoagulation.2,68
Although the objective of the rhythm-control strategy is to
reduce the burden of AF, there is no evidence that AF reduction
reduces the risk of stroke or systemic embolism.68 Many patients
may have ongoing episodes of asymptomatic AF despite elimination of symptomatic episodes.69 In the AFFIRM (Atrial Fibrillation Follow-up Investigation of Rhythm Management) trial, the
risk of stroke was the same in both groups for most of the trial, but
in the fifth year, a nonsignificant trend toward increased risk of
stroke was observed in patients assigned to rhythm control. In
both arms of the AFFIRM trial, many of the strokes occurred after
anticoagulation was stopped or when the international normalized
ratio was subtherapeutic, which happened more often in the
rhythm-control arm because of inappropriate withdrawal of oral
anticoagulation with restoration of sinus rhythm, one of the presumed advantages of rhythm control in that era.68 Thus, patients
should continue on appropriate anticoagulation or antiplatelet
therapy or a combination, according to their individual embolic
risk as determined by the CHADS2 score.2
Nonpharmacologic therapy for rhythm control
EM
If antiarrhythmic drug therapy is ineffective at reducing symptoms or not well-tolerated, consideration of AF ablation may be
desirable.11 If AF ablation is a serious option, the patient should be
referred to an arrhythmia expert for further discussion.
RECOMMENDATION
We recommend radiofrequency ablation of AF in patients who remain symptomatic following adequate trials of
antiarrhythmic drug therapy and in whom a rhythm-control strategy remains desired (Strong Recommendation,
Moderate-Quality Evidence).
Values and preferences. This recommendation places a
high value on the decision of individual patients to balance
relief of symptoms and improvement in QOL with the
small but measurable risk of serious complication with catheter ablation.
Novel therapeutic targets
Experimental research into the substrates that initiate and maintain AF have identified some molecular targets upstream of the elec-
Prevention of AF in the pacemaker population
A number of prospective, randomized clinical trials have reported
that atrial- or dual-chamber pacing reduces the risk of paroxysmal and
permanent AF in patients with symptomatic bradycardia as the primary indication for cardiac pacing.80-84 The data from these trials are
summarized in Table 4. In contrast, the United Kingdom Pacing and
Cardiovascular Events Trial Investigators did not observe a benefit of
dual-chamber pacing over ventricular for prevention of AF in patients
with AV block as the indication for pacing.85 Thus, these data suggest
that the primary benefit of dual-chamber pacing for reducing the risk
of AF is observed in patients with sinus node disease and intact AV
node conduction.
The Mode Selection Trial Investigators reported that patients who were more frequently paced in the ventricle were
more likely to develop AF.86 The risk of developing AF increased approximately 1% for each 1% increase in ventricular
pacing. Nielsen et al87 also reported that patients with sick
sinus syndrome randomized to atrial rate adaptive pacing pacing were less likely to develop AF during follow-up (7.4%)
compared with patients randomized to dual-chamber rate
adaptive pacing with a short (ⱕ150 ms) or long (300 ms) AV
intervals (23.3% and 17.5%, respectively). There are no data to
Gillis et al.
Rate and Rhythm Management
57
RECOMMENDATION
We suggest that patients requiring pacing for the treatment of symptomatic bradycardia secondary to sinus node
dysfunction, atrial or dual-chamber pacing be generally
used for the prevention of AF (Conditional Recommendation, High-Quality Evidence).
We suggest that, in patients with intact AV conduction,
pacemakers be programmed to minimize ventricular pacing
for prevention of AF (Conditional Recommendation, Moderate-Quality Evidence).
Values and preferences. These recommendations recognize a potential benefit of atrial or dual-chamber pacing
programmed to minimize ventricular pacing to reduce the
probability of AF development following pacemaker
implantation.
5. Van Gelder IC, Hagens VE, Bosker HA, et al. A comparison of rate
control and rhythm control in patients with recurrent persistent atrial
fibrillation. N Engl J Med 2002;347:1834-40.
6. Testa L, Biondi-Zoccai GG, Dello Russo A, et al. Rate-control vs. rhythmcontrol in patients with atrial fibrillation: a meta-analysis. Eur Heart J
2005;26:2000-6.
7. Ogawa S, Yamashita T, Yamazaki T, et al. Optimal treatment strategy for
patients with paroxysmal atrial fibrillation: J-RHYTHM study. Circ J
2009;73:242-8.
8. Fuster V, Rydén LE, Cannom DS, et al. ACC/AHA/ESC 2006 guidelines
for the management of patients with atrial fibrillation: full text: a report of
the American College of Cardiology/American Heart Association Task
Force on Practice Guidelines and the European Society of Cardiology
Committee for Practice Guidelines (Writing Committee to Revise the
2001 guidelines for the management of patients with atrial fibrillation)
developed in collaboration with the European Heart Rhythm Association
and the Heart Rhythm Society. Circulation 2006;114:e257-354.
9. Camm AJ, Kirchhof P, Lip GY, et al. Guidelines for the management of
atrial fibrillation: the Task Force for the Management of Atrial Fibrillation
of the European Society of Cardiology (ESC). Eur Heart J 2010;31:2369429.
O
ED
suggest that atrial overdrive pacing substantially reduces AF.88
Recently, algorithms designed to minimize ventricular pacing
have been shown to reduce the risk of persistent AF following
pacemaker implantation in patients with sinus node disease.89
10. Wyse DG, Simpson CS. Rate control versus rhythm control— decision
making. Can J Cardiol 2005;21(suppl B):15B-18B.
11. Verma A, Macle L, Cox JL, Skanes AC, CCS Atrial Fibrillation Guidelines
Committee. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: catheter ablation for atrial fibrillation/atrial flutter. Can J Cardiol 2011;27:60-6.
EM
BA
R
G
Management of AF: Chronic Disease
Management Principles
Chronic disease management principles dictate that the primary
care physician is central to coordination of patient care. Ideally, support for the primary care physician should facilitate delivery of care,
with specialty clinics providing care to more complex cases and tertiary
care specialists reserved for the most challenging cases. To facilitate
management of AF patients, specialty clinics have been formed in
some regions, and others are in planning stages.90 Participation of the
referring physicians is essential to the success of AF clinics, in which
nurse clinicians or nurse practitioners play a key role in patient education and reassurance about both AF and the treatment plan. Direct
contact with an AF physician specialist may not be required in all
cases. In some instances, recommendations about urgent intervention
to control the ventricular rate and initiate anticoagulation to prevent
stroke are provided by the AF physician specialist, with reassessment at
a later date. Some data suggest that patient education and continuity
of care provided by AF clinics may reduce emergency room visits.90
References
1. Healey JS, Parkash R, Pollak T, Tsang T, Dorian P, CCS Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: etiology and initial investigations. Can J Cardiol 2011;27:31-7.
2. Cairns JA, Connolly S, McMurtry S, Stephenson M, Talajic M, CCS
Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: prevention of stroke and systemic
thromboembolism in atrial fibrillation and flutter. Can J Cardiol 2011;
27:74-90.
3. Wyse DG, Waldo AL, DiMarco JP, et al; Atrial Fibrillation Follow-up
Investigation of Rhythm Management (AFFIRM) Investigators. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med 2002;347:1825-33.
4. Roy D, Talajic M, Nattel S, et al. Rhythm control versus rate control for
atrial fibrillation and heart failure. N Engl J Med 2008;358:2667-77.
12. Grogan M, Smith HC, Gersh BJ, et al. Left ventricular dysfunction due to
atrial fibrillation in patients initially believed to have idiopathic dilated
cardiomyopathy. Am J Cardiol 1992;69:1570-3.
13. Rawles JM. What is meant by a controlled ventricular rate in atrial fibrillation? Br Heart J 1990;63:157-61.
14. Dorian P, Connors P. Pharmacological and non pharmacological methods for rate control. Can J Cardiol 2005;21(suppl B):11B-14B.
15. Van Gelder IC, Groenveld HF, Crijns HJ, et al. Lenient vs strict rate
control in patients with atrial fibrillation. N Engl J Med 2010;362:136373.
16. Nikolaidou T, Channer KS. Chronic atrial fibrillation: a systematic review
of medical heart rate control management. Postgrad Med J 2009;85:30312.
17. Bjerregaard P, Bailey WB, Robinson SE. Rate control in patients with
chronic atrial fibrillation. Am J Cardiol 2004;93:329-32.
18. Segal JB, McNamara RL, Miller MR, et al. The evidence regarding the
drugs used for ventricular rate control. J Fam Pract 2000;49:47-59.
19. Boriani G, Biffi M, Diemberger I, Martignani C, Branzi A. Rate control in
atrial fibrillation: choice of treatment and assessment of efficacy. Drugs
2003;63:1489-509.
20. Tsuneda T, Yamashita T, Fukunami M, et al. Rate control and quality of
life in patients with permanent atrial fibrillation: the Quality of Life and
Atrial Fibrillation (QOLAF) Study. Circ J 2006;70:965-70.
21. Farshi R, Kistner D, Sarma JS, et al. Ventricular rate control in chronic
atrial fibrillation during daily activity and programmed exercise: a crossover open-label study of five drug regimens. J Am Coll Cardiol 1999;33:
304-10.
22. David D, Segni ED, Klein HO, et al. Inefficacy of digitalis in the control
of heart rate in patients with chronic atrial fibrillation: beneficial effect of
an added beta adrenergic blocking agent. Am J Cardiol 1979;44:1378-82.
58
Canadian Journal of Cardiology
Volume 27 2011
24. Goldstein RE, Boccuzzi SJ, Cruess D, Nattel S; The Adverse Experience
Committee and the Multicentre Diltiazem Postinfarction Research
Group. Diltiazem increases late-onset congestive heart failure in postinfarction patients with early reduction in ejection fraction. Circulation
1991;83:52-60.
25. Vittorio TJ, Zolty R, Kasper ME, et al. Differential effects of carvedilol
and metoprolol succinate on plasma norepinephrine release and peak exercise heart rate in subjects with chronic heart failure. J Cardiovasc Pharmacol Ther 2008;13:51-7.
26. Wood MA, Brown-Mahoney C, Kay GN, et al. Clinical outcomes after
ablation and pacing therapy for atrial fibrillation: a meta-analysis. Circulation 2000;101:1138-44.
27. Doshi RN, Daoud EG, Fellows C, et al. Left ventricular-based cardiac
stimulation post AV nodal ablation evaluation (the PAVE study). J Cardiovasc Electrophysiol 2005;16:1160-5.
28. Nattel S. New ideas about atrial fibrillation 50 years on. Nature 2002;415:
219-26.
29. Haïssaguerre M, Jaïs P, Shah DC, et al. Spontaneous initiation of atrial
fibrillation by ectopic beats originating in the pulmonary veins. N Engl
J Med 1998;339:659-66.
41. Corley SD, Epstein AE, DiMarco JP, et al. Relationships between sinus
rhythm, treatment, and survival in the Atrial Fibrillation Follow-Up Investigation of Rhythm Management (AFFIRM) Study. Circulation 2004;
109:1509-13.
42. Roy D, Talajic M, Dorian P, et al; Canadian Trial of Atrial Fibrillation
Investigators. Amiodarone to prevent recurrence of atrial fibrillation.
N Engl J Med 2000;342:913-20.
43. Singh BN, Singh SN, Reda DJ, et al; Sotalol Amiodarone Atrial Fibrillation Efficacy Trial (SAFE-T) Investigators. Amiodarone versus sotalol for
atrial fibrillation. N Engl J Med 2005;352:1861-72.
44. Doyle JF, Ho KM. Benefits and risks of long-term amiodarone therapy for
persistent atrial fibrillation: a meta-analysis. Mayo Clin Proc 2009;84:
234-42.
45. Roden, DM. Mechanisms and management of proarrhythmia. Am J Cardiol 1998;82:491-571.
46. UK Propafenone PSVT Study Group. A randomized, placebo-controlled
trial of propafenone in the prophylaxis of paroxysmal supraventricular
tachycardia and paroxysmal atrial fibrillation. Circulation 1995;92:2550-7.
47. Naccarelli GV, Dorian P, Hohnloser SH, Coumel P; Flecainide Multicenter Atrial Fibrillation Study Group. Prospective comparison of flecainide versus quinidine for the treatment of paroxysmal atrial fibrillation/
flutter. Am J Cardiol 1996;77:53A-59A.
R
G
30. Jalife J, Berenfeld O, Mansour M. Mother rotors and fibrillatory conduction: a mechanism of atrial fibrillation. Cardiovasc Res 2002;54:204-16.
40. Connolly SJ, Crijns HJ, Torp-Pedersen C, et al. Analysis of stroke in
ATHENA: a placebo-controlled, double-blind, parallel-arm trial to assess
the efficacy of dronedarone 400 mg BID for the prevention of cardiovascular hospitalization or death from any cause in patients with atrial fibrillation/atrial flutter. Circulation 2009;120:1174-80.
O
ED
23. Davy JM, Herold M, Hoglund C, et al. Dronedarone for the control of
ventricular rate in permanent atrial fibrillation: the Efficacy and safety of
dRonedArone for The cOntrol of ventricular rate during atrial fibrillation
(ERATO) study. Am Heart J 2008;156:527e1-e9.
31. Allessie M, Ausma J, Schotten U. Electrical, contractile and structural
remodelling during atrial fibrillation. Cardiovasc Res 2002;54:230-46.
BA
32. Wang J, Bourne GW, Wang Z, et al. Comparative mechanisms of
antiarrhythmic drug action in experimental atrial fibrillation: importance of use-dependent effects on refractoriness. Circulation 1993;88:
1030-44.
EM
33. Comtois P, Kneller J, Nattel S. Of circles and spirals: bridging the gap
between the leading circle and spiral wave concepts of cardiac reentry.
Europace 2005;7(suppl 2):10-20.
34. Kneller J, Kalifa J, Zou R, et al. Mechanisms of atrial fibrillation termination by pure sodium channel blockade in an ionically-realistic mathematical model. Circ Res 2005;96:e35-47.
35. Kawase A, Ikeda T, Nakazawa K, et al. Widening of the excitable gap
and enlargement of the core of reentry during atrial fibrillation with a
pure sodium channel blocker in canine atria. Circulation 2003;107:
905-10.
36. Danse PW, Garratt CJ, Allessie MA. Flecainide widens the excitable gap at
pivot points of premature turning wavefronts in rabbit ventricular myocardium. J Cardiovasc Electrophysiol 2001;12:1010-7.
37. Derakhchan K, Villemaire C, Talajic M, Nattel S. The class III antiarrhythmic drugs dofetilide and sotalol prevent AF induction by atrial premature complexes at doses that fail to terminate AF. Cardiovasc Res 2001;
50:75-84.
48. Benditt DG, Williams JH, Jin J, et al; d,l-Sotalol Atrial Fibrillation/Flutter Study Group. Maintenance of sinus rhythm with oral d,l-sotalol therapy in patients with symptomatic atrial fibrillation and/or atrial flutter.
Am J Cardiol 1999;84:270-7.
49. Lehmann MH, Hardy S, Archibald D, Quart B, MacNeil DJ. Sex difference in risk of torsade de pointes with d,l-sotalol. Circulation 1996;94:
2535-41.
50. Wanless RS, Anderson K, Joy M, Joseph SP. Multicenter comparative
study of the efficacy and safety of sotalol in the prophylactic treatment of
patients with paroxysmal supraventricular tachyarrhythmias. Am Heart J
1997;133:441-6.
51. Singh BN, Connolly SJ, Crijns HJ, et al. Dronedarone for maintenance of
sinus rhythm in atrial fibrillation or flutter. N Engl J Med 2007;357:98799.
52. Heuzey JY, Ferrari GM, Radzik D, et al. A short-term, randomized, double-blind, parallel-group study to evaluate the efficacy and safety of dronedarone versus amiodarone in patients with persistent atrial fibrillation: the
DIONYSOS study. J Cardiovasc Electrophysiol 2010;21:597-605.
53. Køber L, Torp-Pedersen C, McMurray JJ, et al. Increased mortality after
dronedarone therapy for severe heart failure. N Engl J Med 2008;358:
2678-87.
38. Shinagawa K, Shiroshita-Takeshita A, Schram G, Nattel S. Effects of
antiarrhythmic drugs on fibrillation in the remodeled atrium: insights into
the mechanism of the superior efficacy of amiodarone. Circulation 2003;
107:1440-6.
54. Deedwania PC, Singh BN, Ellenbogen K, et al; Department of Veterans
Affairs CHF-STAT Investigators. Spontaneous conversion and maintenance of sinus rhythm by amiodarone in patients with heart failure and
atrial fibrillation: observations from the veterans affairs congestive heart
failure survival trial of antiarrhythmic therapy (CHF-STAT). Circulation
1998;98:2574-9.
39. Hohnloser SH, Crijns HJ, van Eickels M, et al. Effect of dronedarone on
cardiovascular events in atrial fibrillation. N Engl J Med 2009;360:66878.
55. Nattel S, Maguy A, Le Bouter S, Yeh YH. Arrhythmogenic ion-channel
remodeling in the heart: heart failure, myocardial infarction, and atrial
fibrillation. Physiol Rev 2007;87:425-56.
Gillis et al.
Rate and Rhythm Management
59
57. Boriani G, Biffi M, Capucci A, et al. Oral propafenone to convert recentonset atrial fibrillation in patients with and without underlying heart disease: a randomized, controlled trial. Ann Intern Med 1997;126:621-5.
58. Kannankeril PJ, Roden DM. Drug-induced long QT and torsade de
pointes: recent advances. Curr Opin Cardiol 2007;22:39-43.
59. Alboni P, Botto GL, Baldi N, et al. Outpatient treatment of recent-onset
atrial fibrillation with the “pill-in-the-pocket” approach. N Engl J Med
2004;351:2384-91.
60. Brodsky MA, Allen BJ, Walker CJ III, et al. Amiodarone for maintenance
of sinus rhythm after conversion of atrial fibrillation in the setting of a
dilated left atrium. Am J Cardiol 1987;6:572-5.
61. Van Gelder IC, Crijns HJ, Van Gilst WH, et al. Efficacy and safety of
flecainide acetate in the maintenance of sinus rhythm after electrical cardioversion of chronic atrial fibrillation or atrial flutter. Am J Cardiol 1989;
64:1317-21.
62. Plewan A, Lehmann G, Ndrepepa G, et al. Maintenance of sinus rhythm
after electrical cardioversion of persistent atrial fibrillation: sotalol vs bisoprolol. Eur Heart J 2001;22:1504-10.
63. Volgman AS, Carberry PA, Stambler B, et al. Conversion efficacy and
safety of intravenous ibutilide compared with intravenous procainamide
in patients with atrial flutter or fibrillation. Am Coll Cardiol 1998;31:
1414-9.
75. Kuzniatsova N, Shantsila E, Lip GY. Atrial fibrillation: blockade of the
renin-angiotensin system in atrial fibrillation. Nat Rev Cardiol 2010;7:
428-30.
76. Fauchier L, Pierre B, de Labriolle A, Grimard C, Zannad N, Babuty D.
Antiarrhythmic effect of statin therapy and atrial fibrillation: a meta-analysis of randomized controlled trials. J Am Coll Cardiol 2008;51:828-35.
77. Negi S, Shukrullah I, Veledar E, Bloom HL, Jones DP, Dudley SC. Statin
Therapy for the Prevention of Atrial Fibrillation Trial (SToP AF trial)
[published online ahead of print October 13, 2010]. J Cardiovasc Electrophysiol doi: 10.1111/j.1540-8167.2010.01925.x.
78. Schneider MP, Hua TA, Böhm M, Wachtell K, Kjeldsen SE, Schmieder
RE. Prevention of atrial fibrillation by renin-angiotensin system inhibition: a meta-analysis. J Am Coll Cardiol 2010;55:2299-307.
79. GISSI-AF Investigators, Disertori M, Latini R, Barlera S, et al. Valsartan
for prevention of recurrent atrial fibrillation. N Engl J Med. 2009;360:
1606-17.
80. Andersen HR, Nielsen JC, Thomsen PE, et al. Long-term follow-up of
patients from a randomised trial of atrial versus ventricular pacing for
sick-sinus syndrome. Lancet 1997;350:1210-6.
81. Connolly SJ, Kerr CR, Gent M, et al. Effects of physiologic pacing versus
ventricular pacing on the risk of stroke and death due to cardiovascular
causes. N Engl J Med 2000;342:1385-91.
82. Kerr CR, Connolly SJ, Abdollah H, et al. Canadian Trial of Physiological
Pacing: effects of physiological pacing during long-term follow-up. Circulation 2004;109:357-62.
R
G
64. Slavik RS, Tisdale JE, Borzak S. Pharmacologic conversion of atrial fibrillation: a systematic review of available evidence. Prog Cardiovasc Dis
2001;44:121-52.
74. Savelieva I, Camm J, Statins and polyunsaturated fatty acids for treatment
of atrial fibrillation. Nat Clin Pract Cardiovasc Med 2008;5:30-41.
O
ED
56. Teo KK, Yusuf S, Furberg CD. Effects of prophylactic antiarrhythmic
drug therapy in acute myocardial infarction: an overview of results from
randomized controlled trials. JAMA 1993;270:1589-95.
BA
65. Tercius AJ, Kluger J, Coleman CI, White CM. Intravenous magnesium
sulfate enhances the ability of intravenous ibutilide to successfully convert
atrial fibrillation or flutter. Pacing Clin Electrophysiol 2007;30:1331-5.
EM
66. Siu CW, Lau CP, Lee WL, Lam KF, Tse HF. Intravenous diltiazem is
superior to intravenous amiodarone or digoxin for achieving ventricular
rate control in patients with acute uncomplicated atrial fibrillation. Crit
Care Med 2009;37:2174-9 [quiz: 2180].
67. Galve E, Rius T, Ballester R, et al. Intravenous amiodarone in treatment of
recent-onset atrial fibrillation: results of a randomized, controlled study.
J Am Coll Cardiol 1996;27:1079-82.
68. Sherman DG, Kim SG, Boop BS, et al. Occurrence and characteristics
of stroke events in the Atrial Fibrillation Follow-up Investigation of
Sinus Rhythm Management (AFFIRM) study. Arch Intern Med 2005;
165:1185-91.
69. Flaker GC, Belew K, Beckman K, et al. Asymptomatic atrial fibrillation:
demographic features and prognostic information from the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM)
study. Am Heart J 2005;149:657-63.
70. Dobrey D, Nattel S. New antiarrhythmic drugs for treatment of atrial
fibrillation. Lancet 2010;375:1212-23.
71. Raven U. Antiarrhythmic therapy in atrial fibrillation. Pharmacol Ther
2010;128:129-45.
72. Smit MD, Van Gelder IC, Upstream therapy of atrial fibrillation. Expert
Rev Cardiovasc Ther 2009;7:763-78.
73. Savelieva I, Kourliouros A, Camm J. Primary and secondary prevention of
atrial fibrillation with statins and polyunsaturated fatty acids: review of
evidence and clinical relevance. Naunyn Schmiedebergs Arch Pharmacol
2010;381:1-13.
83. Lamas GA, Lee KL, Sweeney MO, et al. Mode selection trial in sinus-node
dysfunction: ventricular pacing or dual-chamber pacing for sinus-node
dysfunction. N Engl J Med 2002;346:1854-62.
84. Skanes AC, Krahn AD, Yee R, et al; CTOPP Investigators. Progression to
chronic atrial fibrillation after pacing: the Canadian Trial of Physiologic
Pacing. J Am Coll Cardiol 2001;38:167-72.
85. Toff WD, Camm AJ, Skehan JD; United Kingdom Pacing and Cardiovascular Events Trial Investigators. Single-chamber versus dualchamber pacing for high-grade atrioventricular block. N Engl J Med
2005;353:145-55.
86. Sweeney MO, Hellkamp AS, Ellenbogen KA, et al; Mode Selection Trial
Investigators. Adverse effect of ventricular pacing on heart failure and
atrial fibrillation among patients with normal baseline QRS duration in a
clinical trial of pacemaker therapy for sinus node dysfunction. Circulation
2003;107:2932-7.
87. Nielsen JC, Kristensen L, Andersen HR, et al. A randomized comparison
of atrial and dual-chamber pacing in 177 consecutive patients with sick
sinus syndrome: echocardiographic and clinical outcome. J Am Coll Cardiol 2003;42:614-23.
88. Gillis AM. Selective pacing algorithms for prevention of atrial fibrillation:
the final chapter? Heart Rhythm 2009;6:295-301.
89. Sweeney MO, Bank AJ, Nsah E, et al. Search AV Extension and Managed Ventricular Pacing for Promoting Atrioventricular Conduction
(SAVE PACe) Trial: minimizing ventricular pacing to reduce atrial
fibrillation in sinus-node disease. N Engl J Med 2007;357:1000-8.
90. Gillis AM, Burland L, Arnburg B, et al. Treating the right patient at the
right time: an innovative approach to the management of atrial fibrillation. Can J Cardiol 2008;24:195-8.
Canadian Journal of Cardiology 27 (2011) 60 – 66
Society Guidelines
Canadian Cardiovascular Society Atrial Fibrillation
Guidelines 2010: Catheter Ablation for Atrial
Fibrillation/Atrial Flutter
Atul Verma, MD, FRCPC,a Laurent Macle, MD, FRCPC,b Jafna Cox, MD, FRCPC,c
Allan C. Skanes, MD, FRCPC,d and the CCS Atrial Fibrillation Guidelines Committeee
a
Southlake Regional Health Centre, Newmarket, Ontario, Canada
b
Queen Elizabeth II Health Sciences Centre, Halifax, Nova Scotia, Canada
d
e
Montreal Heart Institute, Montreal, Québec, Canada
London Health Sciences Centre, London, Ontario, Canada
O
ED
c
For a complete listing of committee members, see Gillis AM, Skanes AC. Canadian Cardiovascular Society Atrial Fibrillation Guidelines
2010: Implementing GRADE and achieving consensus. Can J Cardiol 2011;27:27-30.
ABSTRACT
RÉSUMÉ
L’ablation par cathéter est un traitement reconnu visant le maintien du
rythme sinusal chez les patients atteints de fibrillation auriculaire (FA)
ou de flutter auriculaire. Il a été démontré que dans la majorité des cas
de FA (et particulièrement sa forme paroxystique), cette arythmie est
déclenchée par des salves d’extrasystoles qui prennent origine dans
les veines pulmonaires. L’ablation par cathéter, réalisée par cautérisations à la jonction des veines pulmonaires et de l’oreillette gauche,
isole les foyers initiateurs de l’arythmie. Lors de l’intervention, d’autres
cautérisations peuvent être effectuées dans les oreillettes, pour tenter
d’éliminer le substrat de l’arythmie, notamment dans les cas de FA
persistante. Il n’est pas encore démontré que cette procédure est
associée à une réduction de la mortalité ou du risque thrombo-embolique. Son indication actuelle est essentiellement d’améliorer les
symptômes de la FA. L’ablation par cathéter est plus efficace que les
médicaments antiarythmiques pour le maintien du rythme sinusal
chez les patients avec FA. Son taux de succès (absence de récidive
d’arythmie) est de 75-90 % après 1-2 procédures. Par contre, le taux
EM
BA
R
G
Catheter ablation of atrial fibrillation (AF) offers a promising treatment
for the maintenance of sinus rhythm in patients for whom a rhythm
control strategy is desired. While the precise mechanisms of AF are
incompletely understood, there is substantial evidence that in many
cases (particularly for paroxysmal AF), ectopic activity most commonly
located in and around the pulmonary veins of the left atrium plays a
central role in triggering and/or maintaining arrhythmic episodes.
Catheter ablation involves electrically disconnecting the pulmonary
veins from the rest of the left atrium to prevent AF from being triggered. Further substrate modification may be required in patients with
more persistent AF. Successful ablation of AF has never been shown to
alter mortality or obviate the need for oral anticoagulation; thus, the
primary indication for this procedure should be improvement of symptoms caused by AF. The success rate of catheter ablation for AF is
superior to the efficacy of antiarrhythmic drugs, but success is still in
the range of 75%-90% after 2 procedures. Ablation is also associated
As discussed in detail by Gillis et al,1 studies have failed to show
that a rhythm control strategy improves mortality or reduces
the incidence of thromboembolic complications in atrial fibril-
lation (AF) compared to the use of rate control alone. Thus, the
decision to pursue rhythm control should be directed to patients who are symptomatic with their AF despite rate control,
Received for publication November 5, 2010. Accepted November 16, 2010.
specific recommendations. These recommendations are aimed to provide a
reasonable and practical approach to care for specialists and allied health
professionals obliged with the duty of bestowing optimal care to patients
and families, and can be subject to change as scientific knowledge and
technology advance and as practice patterns evolve. The statement is not
intended to be a substitute for physicians using their individual judgment
in managing clinical care in consultation with the patient, with appropriate
regard to all the individual circumstances of the patient, diagnostic and
treatment options available and available resources. Adherence to these
recommendations will not necessarily produce successful outcomes in every
case.
Corresponding author: Atul Verma, MD, FRCPC, Southlake Regional
Health Centre, 712 Davis Dr, Suite 105, Newmarket, Ontario, L3Y 8C3
Canada. Tel.: 905-953-7917; fax: 905-953-0046.
E-mail: atul.verma@utoronto.ca
The disclosure information of the authors and reviewers is available from the
CCS on the following websites: www.ccs.ca and www.ccsguidelineprograms.ca.
This statement was developed following a thorough consideration of
medical literature and the best available evidence and clinical experience. It
represents the consensus of a Canadian panel comprised of multidisciplinary experts on this topic with a mandate to formulate disease-
0828-282X/$ – see front matter © 2011 Canadian Cardiovascular Society. Published by Elsevier Inc. All rights reserved.
doi:10.1016/j.cjca.2010.11.011
Verma et al.
Catheter Ablation for Atrial Fibrillation/Atrial Flutter
61
In patients with more persistent AF, electrical and structural
remodelling of the atria occur, creating an abnormal atrial substrate that tends to perpetuate AF.6 Changes include a decrease
in atrial refractoriness, atrial fibrosis, and atrial stretch.7 Thus,
while PV isolation remains the primary AF ablation approach
in persistent AF, it is believed that further ablation of the substrate is required to treat AF in this population. The most
common forms of substrate modification are linear ablation
and electrogram-guided ablation. Linear ablation involves creating lines of block along the LA roof and the mitral annulus
and occasionally in the RA, mimicking the original surgical
maze procedure.8 Electrogram-guided ablation involves targeting specific electrical signals (eg, complex “fractionated” signals) that may represent critical areas of AF perpetuation.9 The
optimal strategy of substrate modification remains an area of
active investigation.
Procedural Considerations
AF ablation is a complex procedure, requiring a high degree
of operator expertise and advanced technological support.
R
G
with the aim of improving quality of life. Many of these symptomatic patients, such as younger patients with “lone” AF, were
underrepresented in trials comparing rate and rhythm control.
Furthermore, in all of these trials, antiarrhythmic drug therapy was
used for the rhythm control strategy. Antiarrhythmic drugs remain “first-line” therapy for the maintenance of sinus rhythm, but
these medications have only modest efficacy at maintaining sinus
rhythm over the long term. They are also associated with side
effects, in particular proarrhythmia, which limit their long-term
use, especially in younger patients. Catheter ablation offers an alternative to maintaining sinus rhythm when drugs have been ineffective or cannot be tolerated. Data have shown that the success
rate of catheter ablation in maintaining sinus rhythm is superior to
that of drug therapy and is associated with improved quality of life
(see later). While there are clearly upfront risks associated with this
invasive procedure, the risks have decreased substantially over time
and, if successful, the procedure obviates the long-term risks of
antiarrhythmic drugs. Thus, for many highly symptomatic patients who cannot be pharmacologically controlled, catheter ablation offers a promising alternative.
de complications majeures est important, de l’ordre de 2-3 %. Aussi,
l’ablation par cathéter ne doit elle être considérée que chez les patients avec FA symptomatique et qui ne répondent pas au traitement
pharmacologique. L’ablation par cathéter du flutter auriculaire est
encore plus efficace et comporte moins de risques. Elle peut donc être
considérée en première intention, comme alternative aux médicaments antiarythmiques.
O
ED
with a complication rate of 2%-3%. Thus, ablation should primarily be
used as a second-line therapy after failure of antiarrhythmic drugs. In
contrast to AF, catheter ablation of atrial flutter has a higher success
rate with a smaller incidence of complications. Thus, catheter ablation
for atrial flutter may be considered a first-line alternative to antiarrhythmic drugs.
EM
BA
Mechanism of Action of Catheter Ablation of AF
Catheter ablation for AF should be distinguished from atrioventricular (AV) junction ablation and pacemaker implantation,
which is used for rate control but for not maintenance of sinus
rhythm. It should also be distinguished from catheter ablation of
typical right atrial flutter, which is a distinct procedure (described
later in this article). Catheter ablation of AF aims to eliminate both
the triggers of AF and the substrate that maintains AF, to achieve
long-term sinus rhythm.
While the mechanism of AF is very complex, rapid ectopic
activity from the pulmonary veins (PVs) may be responsible for
both triggering and maintaining AF, in particular paroxysmal
AF.2 Scherf and colleagues3 first described how rapidly firing
ectopic foci within the atria could degenerate the atria into a
fibrillatory rhythm. It was the seminal report by Haissaguerre
and colleagues,4 however, that first applied this principle in
clinical practice. In their report, they described how most of the
triggering foci for AF in the human originated in or around the
PVs of the left atrium (LA). More than 90% of the foci originate in this region, with 10% originating in other areas such as
the LA posterior wall, interatrial septum, coronary sinus, superior vena cava, and crista terminalis in the right atrium (RA).4
By ablating around the PVs and electrically isolating them
from the rest of the atria, the triggering foci can be eliminated
and AF prevented (Fig. 1). The procedure is sometimes referred to as a “pulmonary vein isolation” procedure for this
reason. Over time, this technique has proved to be widely effective at maintaining sinus rhythm, particularly in patients
with paroxysmal AF, and has evolved to become the cornerstone of AF catheter ablation procedures.5
Figure 1. Ablation lesion set for pulmonary vein isolation. Computed
tomography scan of the posterior view of the left atrium including the
pulmonary veins. Veins are labelled as follows: LSPV, left superior;
LIPV, left inferior; RSPV, right superior; RIPV, right inferior pulmonary
vein. The red dots represent point-by-point ablation lesions created by
radiofrequency energy in the left atrium surrounding the pulmonary
veins, thus electrically disconnecting them from the rest of the
atrium. The darker dots represent lesions on the posterior wall of the
left atrium, and the lighter dots represent circumferential lesions
along the anterior aspect of the left atrium.
62
Canadian Journal of Cardiology
Volume 27 2011
O
ED
therapy alone.18 Ablation also resulted in a significant improvement in quality of life. Another trial has demonstrated similar
results.19 Failures most commonly occur as a result of electrical
reconnection between the PVs and the LA due to recovery of
previous ablation sites.20 Improved outcomes have been demonstrated with repeat procedures to isolate electrically reconnected PVs. Technologies that will help create more permanent lesions during the first ablation may improve long-term
success rates and decrease the need for repeat procedures.
In patients with persistent AF, the success rates are 10%15% lower than those described for paroxysmal AF with a
higher need for repeat procedures.21 This lower success rate
is predominantly due to the fact that the substrate has to be
targeted and ablated in addition to PV isolation, meaning
more complex and lengthy procedures. Furthermore, the
optimal lesion set to target the substrate has yet to be fully
determined, although there are data to suggest that hybrid
techniques targeting more than just PV isolation may be
required.22 With 2 procedures, the success rate of ablation
for persistent AF may approach the success rates for paroxysmal AF.21 Lower success rates (by 5%-10% compared
with paroxysmal AF) have also been reported in patients
with structural heart disease, such as cardiomyopathy,23 although the benefit in this population may still be significant.
The PABA-CHF trial, for example, reported improvements
in ejection fraction in patients with congestive heart failure
despite the lower overall procedural success rate.24
In patients who do not have a successful outcome postablation,
some may become responsive to antiarrhythmic drug therapy that
was previously ineffective. While many patients undergoing ablation wish to discontinue antiarrhythmic drugs, those who cannot
maintain sinus rhythm postablation may achieve good rhythm
control with adjuvant antiarrhythmic drug therapy.
Most studies have looked at 1-year outcomes for AF ablation. Very few longer-term data are available. It appears that
after 12-18 months, most patients will continue to do well, but
5%-10% of patients will have late recurrences beyond that time
period.25-28 Further data are required to understand better the
long-term durability of the results of AF ablation.
EM
BA
R
G
While AF ablation is performed as an outpatient, day procedure, the intervention often takes about 3-5 hours or longer to
complete. Patients need to be orally anticoagulated with warfarin for at least 1-2 months prior to the procedure and at least
3-6 months postablation to minimize the risk of a thromboembolic complication. Some centres will routinely perform
preprocedural transesophageal echocardiography to rule out
atrial thrombus prior to performing the ablation.10
The procedure itself may be performed under general anaesthesia or heavy conscious sedation using benzodiazepines and/or
opiates.11,12 The entire procedure is performed through systemic
venous access via the femoral and/or subclavian or internal jugular
veins. Access to the LA is achieved by performing a transseptal
puncture across the interatrial septum to cross from the RA to the
LA. Because the major focus for ablation is in the LA, the patient
is systemically anticoagulated to minimize thromboemboic
events. In general, the procedure is performed with the patient
adequately anticoagulated, either by sustaining the preprocedure
warfarin (usually allowing the INR to fall to the lower end of the
therapeutic range) or with use of bridging low-molecular-weight
heparin both before and after the procedure. In the latter case,
unfractionated heparin is administered with access to the LA.
Likewise, bridging low-molecular-weight heparin is reinitiated
within hours of the sheath removal and continued until a therapeutic INR is reestablished with oral anticoagulant therapy. The
anatomy and electrical activity of the LA are often reconstructed
using a 3-dimensional mapping system that then guides the rest of
the procedure. Ablation is most commonly performed with radiofrequency energy delivered from a catheter tip. Technologies are
evolving, however, to use different catheter designs and energy
sources to maximize energy delivery while minimizing the risks,
such as perforation.
Following ablation, patients are evaluated at regular intervals with electrocardiograms and Holter monitoring to determine the success of the procedure. Early recurrences of AF may
occur within the first 3 months postablation due to acute inflammation in the LA but do not necessarily indicate long-term
failure of the procedure; at least 50% of these recurrences will
resolve spontaneously after 3 months.13,14
Efficacy of Catheter Ablation for AF
Since AF ablation was first described ⬎10 years ago, the
technique and technology have evolved such that fairly consistent success rates can be achieved for patients with paroxysmal
AF and minimal associated structural heart disease.15 In these
patients, the success rate of maintaining sinus rhythm off antiarrhythmic drug therapy is 60%-75% after 1 procedure and
75%-90% after 2 procedures.12 In a recent meta-analysis of 6
clinical trials that compared ablation with antiarrhythmic drug
therapy in a total of 693 patients, ablation was associated with
a significantly increased odds of freedom from AF at 12 months
(odds ratio [OR] 9.74; 95% confidence interval [CI] 3.9823.87).16 Ablation was also associated with a decreased rate of
cardiovascular hospitalization (OR 0.15; 95% CI 0.10-0.23).
These results were achieved with a repeat ablation rate of 17%.
The results were also quite consistent between trials.17 In a
recent multicenter, randomized trial comparing catheter ablation with antiarrhythmic drug therapy, 66% of patients maintained sinus rhythm off drugs after a single ablation of paroxysmal AF compared with only 16% with antiarrhythmic drug
Risks of Catheter Ablation of AF
As with any invasive procedure, catheter ablation of AF is
associated with procedural risk. While the risk of any complication was reported to be 6%-8% in early experiences,29 these
risks have decreased appreciably in the past 5 years30 and are
currently in the range of 2%-3%. The most common risk is a
vascular access complication such as hematoma, pseudoaneurysm, and AV fistula, occurring in 1%-2% of cases. Less common but more serious risks include those of cardiac perforation
(0.5%-1%) and thromboembolism (0.5%-1%). Cardiac perforation can often be managed by percutaneous drainage (pericardiocentesis), although surgical repair is rarely required.
Acute thromboembolic stroke results in transient deficits in
most affected patients. Pulmonary vein stenosis used to be a
more common complication when ablation was initially performed by ablation within the PVs. However, current ablation
techniques deliver energy outside of the PVs within the LA,
thus avoiding the stenosis hazard and making this complication
quite uncommon today (⬍0.5%).
Verma et al.
Catheter Ablation for Atrial Fibrillation/Atrial Flutter
63
First-line
Failed first-line drug
Failed second-line drug
Failed multiple drugs
Longstanding*
Persistent
Paroxysmal
––
––
⫹
⫹⫹
–
⫹
⫹⫹
⫹⫹⫹
⫹
⫹⫹
⫹⫹⫹
⫹⫹⫹
⫹, Balance of risk and benefit in favour of catheter ablation.
* Ongoing symptomatic AF for ⱖ1 year.
Values and preferences. This recommendation recognizes that the balance of risk with ablation and benefit in
symptom relief and improvement in quality of life must be
individualized. It also recognizes that patients may have relative or absolute cardiac or noncardiac contraindications to
specific medications.
Because most of the patients included in clinical trials to date
have been with paroxysmal AF and because the success rate is
higher in this population, these patients are favoured for ablation
therapy. However, patients with symptomatic persistent AF are
increasingly undergoing ablation. The risk/benefit ratio of performing catheter ablation for AF in various subtypes of AF is detailed in Table 1.
EM
BA
R
G
Candidates for Catheter Ablation of AF
The decision to pursue a strategy of maintaining sinus rhythm
should be aimed at reduction of patient symptoms.1 To date, there
are no clinical trial data available demonstrating a reduction in
mortality or stroke through maintenance of sinus rhythm, including through the use of catheter ablation. Thus, the primary indication for catheter ablation is in patients with symptomatic AF for
whom the symptoms are adversely affecting quality of life. Patients
with totally asymptomatic AF are not candidates for ablation, with
the possible exception of patients in whom AF is thought to be
adversely affecting left ventricular function (such as with tachycardia-induced cardiomyopathy). Antiarrhythmic drug therapy is
still considered first-line therapy for maintenance of sinus
rhythm,5 while catheter ablation should only be considered for
patients for whom adequate trials of drug therapy fail. This hierarchy generally means a trial of ⱖ2 drugs in most patients. More
recent clinical trials have demonstrated superiority of ablation in
patients for whom ⱖ1 antiarrhythmic drugs have failed, and these
trials form the basis for a conditional recommendation for select
patients to be considered for catheter ablation as the initial treatment of AF. Younger patients, for example, may want to avoid
long-term amiodarone treatment use given the drug’s accompanying (or cumulative) risks. Patients may also have cardiac or noncardiac absolute or relative contraindications to certain drugs1 (see
Table 3 in Gillis et al1 in this issue). Also, patients are unlikely to
benefit from specific medications if 1 medication in the same class
has already failed.
Table 1. Risk/benefit ratio for ablation in patients with
symptomatic AF
O
ED
Fatal complications are quite rare, occurring in approximately
1:1000 cases. However, because of the proximity of the esophagus
to the posterior LA wall, the esophagus may be damaged as a result
of ablation in the LA. Rarely, this damage can result in a fistula
forming between the LA and esophagus, which most often presents 2-4 weeks postablation as an unexplained fever with or without chest pain and unexplained neurologic events.31 Because this
complication often goes unrecognized, it leads to sepsis and death.
Use of lower power outputs during ablation, esophageal monitoring, and postprocedural proton pump inhibition may all reduce
the already small risk of this complication.
RECOMMENDATION
We recommend catheter ablation of AF in patients who
remain symptomatic following adequate trials of anti-arrhythmic drug therapy and in whom a rhythm control strategy remains desired (Strong Recommendation, ModerateQuality Evidence).
Values and preferences. This recommendation recognizes that failure of multiple antiarrhythmic drugs results in
few alternative strategies if maintenance of sinus rhythm is
preferred based on symptom burden reduction and quality
of life improvement.
We suggest catheter ablation to maintain sinus rhythm
in select patients with symptomatic atrial fibrillation and
mild-moderate structural heart disease who are refractory or
intolerant to ⱖ1 antiarrhythmic medication (Conditional
Recommendation, Moderate-Quality Evidence).
Practical tip. There is no formal definition for “adequate trials of
anti-arrhythmic drug therapy” mentioned in the first recommendation. Early studies assessing AF ablation required that patients have
failed therapeutic doses of ⱖ2 different antiarrhythmics.
This “strong” recommendation stems from both the data and
the belief of the consensus committee that AF ablation be reserved
for patients who have had trials of therapeutic doses of ⱖ2 different antiarrhythmics drugs prior to being considered for catheter
ablation. Electing to perform ablation after a trial of ⬍2 drugs may
be appropriate in carefully selected patients but meets only a “conditional” recommendation based on the more limited availability
of data to support this approach.
In highly selected patients, AF ablation may be offered as firstline therapy. Data from 1 small pilot study of 70 patients showed
a 63% recurrence rate in the antiarrhythmic arm versus only 13%
in the ablation arm (P ⬍ .001) with a significant reduction in
hospitalization and improvement in quality of life.32 In addition,
although this has not been studied in detail, some patients with
tachybrady syndrome are unable to tolerate drug therapy because
of bradyarrhythmic complications in the absence of a permanent
pacemaker. If the AF can be successfully ablated, then antiarrhythmic therapy and the need for permanent pacing may be avoided,
especially in younger patients.33
RECOMMENDATION
We suggest catheter ablation to maintain sinus rhythm
as first-line therapy for relief of symptoms in highly selected
patients with symptomatic, paroxysmal atrial fibrillation
(Conditional Recommendation, Low-Quality Evidence).
64
Canadian Journal of Cardiology
Volume 27 2011
While there is no absolute age limit for ablation, most clinical experiences have included few patients ⱖ75 years old and
almost no patients ⱖ80 years old due to concern of increased
complication rates.
Finally, if the LA size is too enlarged (typically ⬎55-mm diameter in the parasternal long-axis view on standard echo), the success
rate of catheter ablation is poor. Thus, if ablation is to be considered, it should be done prior to severe LA enlargement.
Practical tip. The following represents a typical, but not exclusive, profile of a patient who is referred for consideration of
AF ablation today:
Age ⬍80 years
Patients who are symptomatic with their AF
Patients who have tried but failed or are intolerant of antiarrhythmic drug therapy
Paroxysmal AF or short-standing persistent AF
Minimal to moderate structural heart disease (eg, LV dysfunction or valvular disease).
RECOMMENDATION
We recommend curative catheter ablation for symptomatic patients with typical atrial flutter as first line therapy
or as a reasonable alternative to pharmacologic rhythm or
rate control therapy (Strong Recommendation, ModerateQuality Evidence).
EM
BA
R
G
Need for Anticoagulation With Catheter Ablation
of AF
To date, there is no clinical evidence to suggest that successful catheter ablation of AF affects long-term stroke risk. One
major reason is that some asymptomatic AF may continue to
occur postablation undetected by intermittent monitoring.
Data show that more intensive or continuous monitoring may
detect episodes of asymptomatic AF in patients who have had a
“successful” outcome,34 and this AF may contribute to ongoing thromboembolic risk. Even in patients in whom AF is
eliminated, there is a lack of data to support anticoagulation
withdrawal in patients with other risk factors for stroke. Trials
to evaluate this question are currently under way, including the
large-scale CABANA study. At present, if a patient has sufficient risk to warrant oral anticoagulation for their AF preablation (eg, a CHADS2 [Congestive Heart Failure, Hypertension,
Age, Diabetes, Stroke/Transient Ischemic Attack] risk score of
ⱖ2), then it is recommended that oral anticoagulation be continued indefinitely postablation regardless of apparent procedural success.35,36 Furthermore, because the very long-term
results of ablation have not been fully elucidated beyond 2-5
years, the very late recurrence rate may also warrant ongoing
anticoagulation. Avoidance of oral anticoagulation is not an
indication for catheter ablation of AF at present.
Catheter Ablation of Atrial Flutter
Typical right atrial flutter is a distinct arrhythmia from AF,
although the 2 often coexist, occurring together in up to 40%50% of patients with atrial flutter. Typical flutter is characterized
by the classic “sawtooth” pattern on the electrocardiogram and
often conducts 2:1 with a ventricular response of 150 beats per
minute. Atrial flutter carries the same thromboembolic risk as AF
and should be anticoagulated according to the same guidelines as
AF. In contrast to AF, however, typical right atrial flutter involves
a single reentrant circuit around the tricuspid annulus. By ablating
a line along the isthmus that extends from the tricuspid annulus to
the inferior vena cava, flutter can easily be eliminated in a single
procedure with a success rate of ⬎85%-90%.37 Given the simplicity of this procedure (in contrast to AF ablation) with its accompanying low risk and given that atrial flutter is very hard to
control pharmacologically, flutter ablation is recommended as an
alternative first-line therapy to drugs. This has been supported by
a number of clinical trials comparing atrial flutter ablation to drug
therapy.15,38 However, after elimination of AFL, over the next 5
years, approximately 60%-65% of patients will develop AF as a
stand-alone problem.39
O
ED
Values and preferences. This recommendation recognizes that individual patients may have a strong intolerance
or aversion to antiarrhythmic drugs such that the risk of
ablation is deemed warranted.
Practical tip. AF ablation should not be considered as an alternative to oral anticoagulation. If a patient has a high thromboembolic risk profile (eg, CHADS2 risk score of ⱖ2), then the
patient should continue oral anticoagulation even after successful AF ablation. Studies of long-term monitoring have consistently shown asymptomatic episodes of AF both prior to and
following ablation. Initiation of oral anticoagulation should
also not be delayed when indicated in patients pending referral
for AF ablation.
Values and preferences. This recommendation recognizes the high efficacy, low complication rate of catheter
ablation and low efficacy of pharmacologic therapy,
whether rate or rhythm control.
Practical tip. Typical atrial flutter is more challenging to control medically with antiarrhythmic drugs than is AF and adequate rate control is more difficult to achieve. Given the high
success rate and low complication rate of atrial flutter ablation,
it is a strongly recommended as a first-line therapy in comparison to AF ablation.
Ablation of Accessory Pathways and Other
Arrhythmias in AF
The presence of an accessory pathway (eg, Wolff-Parkinson-White syndrome) with evidence of preexcitation (delta
wave) during AF presents a rare but potentially life-threatening
situation.40 If the pathway has a short refractory period, it may
allow AF to conduct to the ventricles with a very high ventricular rate response. High ventricular rates can occasionally lead
to degeneration into ventricular tachycardia or fibrillation, resulting in a cardiac arrest. Administration of an AV nodal
blocking agent during preexcited AF can exacerbate this problem and should be avoided. In these cases, especially if the
patient has a history of syncope or rapid AF, catheter ablation
of the accessory pathway is strongly recommended to avoid any
possibility of cardiac arrest.
Verma et al.
Catheter Ablation for Atrial Fibrillation/Atrial Flutter
65
6. Nattel S, Burstein B, Dobrev D: Atrial remodeling and atrial fibrillation:
mechanisms and implications. Circ Arrhythm Electrophysiol 2008;1:62-73.
In patients with evidence of ventricular preexcitation
during AF, we recommend catheter ablation of the accessory pathway, especially if AF is associated with rapid ventricular rates, syncope, or a pathway with a short refractory
period (Strong Recommendation, Low-Quality Evidence).
Values and preferences. This recommendation places a
high value on the prevention of sudden cardiac death in
patients at high risk and a low value on the small complication rate of catheter ablation of the accessory pathway.
RECOMMENDATION
In young patients with lone, paroxysmal AF, we suggest
an electrophysiological study to exclude a reentrant tachycardia as a cause of AF; if present, we suggest curative ablation of the tachycardia (Conditional Recommendation,
Very Low-Quality Evidence).
Values and preferences. This recommendation recognizes that supraventricular tachycardia can initiate AF when
the substrate for AF is present and can be ablated with a high
success rate and minimal risk.
8. Willems S, Klemm H, Rostock T, et al. Substrate modification combined
with pulmonary vein isolation improves outcome of catheter ablation in
patients with persistent atrial fibrillation: a prospective randomized comparison. Eur Heart J 2006;27:2871-8.
9. Nademanee K, McKenzie J, Kosar E, et al. A new approach for catheter
ablation of atrial fibrillation: mapping of the electrophysiologic substrate.
J Am Coll Cardiol 2004;43:2044-53.
10. Michael KA, Redfearn DP, Baranchuk A, et al. Transesophageal echocardiography for the prevention of embolic complications after catheter ablation for atrial fibrillation. J Cardiovasc Electrophysiol 2009;20:
1217-22.
11. Verma A, Marrouche NF, Natale A: Pulmonary vein antrum isolation:
intracardiac echocardiography-guided technique. J Cardiovasc Electrophysiol 2004;15:1335-40.
12. Finta B, Haines DE: Catheter ablation therapy for atrial fibrillation. Cardiol Clin 2004;22:127-45, ix.
13. Themistoclakis S, Schweikert RA, Saliba WI, et al. Clinical predictors and
relationship between early and late atrial tachyarrhythmias after pulmonary vein antrum isolation. Heart Rhythm 2008;5:679-85.
14. Koyama T, Sekiguchi Y, Tada H, et al. Comparison of characteristics and
significance of immediate versus early versus no recurrence of atrial fibrillation after catheter ablation. Am J Cardiol 2009;103:1249-54.
References
EM
BA
R
G
In younger patients, other reentrant supraventricular tachycardias, such as AV nodal reentry or AV reentrant tachycardia
using an accessory pathway, can degenerate into AF. Elimination of the reentrant tachycardia can therefore prevent episodes
of AF. Thus, clear onset of AF resulting from another supraventricular tachycardia is an indication for seeking and eliminating
the underlying tachycardia by ablation, if possible. If no such
onset is clearly demonstrable, in younger patients it may be
warranted to perform a general electrophysiological study prior
to AF ablation, to look for and eliminate other underlying
tachyarrhythmias, and assess the outcome prior to performing
AF ablation.
7. Allessie M, Ausma J, Schotten U: Electrical, contractile and structural
remodeling during atrial fibrillation. Cardiovasc Res 2002;54:230-46.
O
ED
RECOMMENDATION
1. Gillis AM, Verma A, Talajic M, Nattel S, Dorian P, CCS Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: rate and rhythm management. Can J Cardiol
2011;27:47-59.
2. Nattel S, Opie LH: Controversies in atrial fibrillation. Lancet 2006;367:
262-72.
3. Scherf D, Schaffer AI, Blumenfeld S: Mechanism of flutter and fibrillation. AMA Arch Intern Med 1953;91:333-52.
4. Haissaguerre M, Jais P, Shah DC, et al. Spontaneous initiation of atrial
fibrillation by ectopic beats originating in the pulmonary veins. N Engl
J Med 1998;339:659-66.
5. Calkins H, Brugada J, Packer DL, et al. HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation:
recommendations for personnel, policy, procedures and follow-up. A report of the Heart Rhythm Society (HRS) Task Force on catheter and
surgical ablation of atrial fibrillation. Heart Rhythm 2007;4:816-61.
15. Verma A, Natale A: Should atrial fibrillation ablation be considered firstline therapy for some patients? Why atrial fibrillation ablation should be
considered first-line therapy for some patients. Circulation 2005;112:121422; discussion 1231.
16. Piccini JP, Lopes RD, Kong MH, et al. Pulmonary vein isolation for the
maintenance of sinus rhythm in patients with atrial fibrillation: a metaanalysis of randomized, controlled trials. Circ Arrhythm Electrophysiol
2009;2:626-33.
17. Calkins H, Reynolds MR, Spector P, et al. Treatment of atrial fibrillation with
antiarrhythmic drugs or radiofrequency ablation: two systematic literature reviews
and meta-analyses. Circ Arrhythm Electrophysiol 2009;2:349-61.
18. Wilber DJ, Pappone C, Neuzil P, et al. Comparison of antiarrhythmic drug
therapy and radiofrequency catheter ablation in patients with paroxysmal
atrial fibrillation: a randomized controlled trial. JAMA 2010;303:333-40.
19. Jais P, Cauchemez B, Macle L, et al. Catheter ablation versus antiarrhythmic
drugs for atrial fibrillation: the A4 study. Circulation 2008;118:2498-505.
20. Verma A, Kilicaslan F, Pisano E, et al. Response of atrial fibrillation to pulmonary vein antrum isolation is directly related to resumption and delay of
pulmonary vein conduction. Circulation 2005;112:627-35.
21. Bhargava M, Di Biase L, Mohanty P, et al. Impact of type of atrial fibrillation
and repeat catheter ablation on long-term freedom from atrial fibrillation:
results from a multicenter study. Heart Rhythm 2009;6:1403-12.
22. Verma A, Mantovan R, Macle L, et al. Substrate and Trigger Ablation for
Reduction of Atrial Fibrillation (STAR AF): a randomized, multicentre,
international trial. Eur Heart J 2010;31:1344-56.
23. Chen MS, Marrouche NF, Khaykin Y, et al. Pulmonary vein isolation for
the treatment of atrial fibrillation in patients with impaired systolic function. J Am Coll Cardiol 2004;43:1004-9.
24. Khan MN, Jais P, Cummings J, et al. Pulmonary-vein isolation for atrial
fibrillation in patients with heart failure. N Engl J Med 2008;359:1778-5.
66
Canadian Journal of Cardiology
Volume 27 2011
25. Sawhney N, Anousheh R, Chen WC, Narayan S, Feld GK: Five-year
outcomes after segmental pulmonary vein isolation for paroxysmal atrial
fibrillation. Am J Cardiol 2009;104:366-72.
33. Khaykin Y, Marrouche NF, Martin DO, et al. Pulmonary vein isolation
for atrial fibrillation in patients with symptomatic sinus bradycardia or
pauses. J Cardiovasc Electrophysiol 2004;15:784-9.
26. Wokhlu A, Hodge DO, Monahan KH, et al. Long-term outcome of atrial
fibrillation ablation: impact and predictors of very late recurrence. J Cardiovasc Electrophysiol 2010;21:1071-8.
34. Hindricks G, Piorkowski C, Tanner H, et al. Perception of atrial
fibrillation before and after radiofrequency catheter ablation: relevance
of asymptomatic arrhythmia recurrence. Circulation 2005;112:30713.
28. Hunter RJ, Berriman TJ, Diab I, et al. Long-term efficacy of catheter
ablation for atrial fibrillation: impact of additional targeting of fractionated electrograms. Heart 2010;96:1372-8.
29. Cappato R, Calkins H, Chen SA, et al. Worldwide survey on the methods,
efficacy, and safety of catheter ablation for human atrial fibrillation. Circulation 2005;111:1100-5.
30. Cappato R, Calkins H, Chen SA, et al. Updated worldwide survey on the
methods, efficacy, and safety of catheter ablation for human atrial fibrillation. Circ Arrhythm Electrophysiol 2010;3:32-8.
31. Cummings JE, Schweikert RA, Saliba WI, et al. Brief communication:
atrial-esophageal fistulas after radiofrequency ablation. Ann Intern Med
2006;144:572-4.
36. Themistoclakis S, Corrado A, Marchlinski FE, et al. The risk of thromboembolism and need for oral anticoagulation after successful atrial fibrillation ablation. J Am Coll Cardiol 2010;55:735-43.
37. Spector P, Reynolds MR, Calkins H, et al. Meta-analysis of ablation of
atrial flutter and supraventricular tachycardia. Am J Cardiol 2009;104:
671-7.
38. Da Costa A, Cucherat M, Pichon N, et al. Comparison of the efficacy of
cooled-tip and 8-mm-tip catheters for radiofrequency catheter ablation of
the cavotricuspid isthmus: a meta-analysis. Pacing Clin Electrophysiol
2005;28:1081-7.
39. Perez FJ, Schubert CM, Parvez B, et al. Long-term outcomes after catheter
ablation of cavo-tricuspid isthmus dependent atrial flutter: a meta-analysis. Circ Arrhythm Electrophysiol 2009;2:393-401.
40. Berry VA: Wolff-Parkinson-White syndrome and the use of radiofrequency catheter ablation. Heart Lung 1993;22:15-25.
EM
BA
R
G
32. Wazni OM, Marrouche NF, Martin DO, et al. Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of symptomatic atrial fibrillation: a randomized trial. JAMA 2005;293:
2634-40.
35. Oral H, Chugh A, Ozaydin M, et al. Risk of thromboembolic events after
percutaneous left atrial radiofrequency ablation of atrial fibrillation. Circulation 2006;114:759-65.
O
ED
27. Lo LW, Tai CT, Lin YJ, et al. Predicting factors for atrial fibrillation acute
termination during catheter ablation procedures: implications for catheter
ablation strategy and long-term outcome. Heart Rhythm 2009;6:311-8.
Canadian Journal of Cardiology 27 (2011) 67–73
Society Guidelines
Canadian Cardiovascular Society Atrial Fibrillation
Guidelines 2010: Surgical Therapy
Pierre Pagé, MD,a and the CCS Atrial Fibrillation Guidelines Committeeb
a
b
From the Research Center, Hôpital du Sacré-Coeur de Montréal, Montreal, Québec, Canada
For a complete listing of committee members, see Gillis AM, Skanes AC. Canadian Cardiovascular Society Atrial Fibrillation Guidelines
2010: Implementing GRADE and Achieving Consensus. Can J Cardiol 2011;27:27-30.
RÉSUMÉ
Surgery for atrial fibrillation (AF) has been demonstrated as an effective
treatment to restore and maintain sinus rhythm in patients for whom a
rhythm control strategy is desired. It is usually offered to patients undergoing other types of cardiac surgery (eg, mitral valve repair or replacement, coronary artery bypass grafting, aortic valve surgery, intracardiac
defects, ascending aortic surgery). It is also feasible as a stand-alone
procedure, bearing a high success rate. In the past few years, less-invasive
procedures have been described. AF is a triggered arrhythmia, resulting
from ectopic activity most commonly located in and around the pulmonary veins of the left atrium. Therefore, electrical isolation of the pulmonary veins from the rest of the left atrium in order to prevent AF from being
triggered is the rationale common to all surgical techniques. Further substrate modification may be required in patients with more persistent AF.
This is done by adding ablation of the posterior left atrium with connecting
lines of block between pulmonary veins, to the mitral valve annulus, as
well as in specific sites in the right atrium. The left atrial appendage is
resected or occluded at the same time. Despite patients’ high rate of
freedom from AF after surgery (70%– 85% at 1 year), surgical ablation of
AF has never been clearly shown to alter long-term mortality. The available literature supports the recommendation to stop oral anticoagulation
therapy 6 months after surgery when sinus rhythm can be documented,
because a very low rate of thromboembolic events is reported. However,
Il est démontré que la chirurgie de fibrillation auriculaire (FA) est un
traitement efficace pour restaurer et maintenir le rythme sinusal chez les
patients pour qui une stratégie de contrôle du rythme est indiquée. On
l’offre habituellement aux patients qui doivent subir d’autres types de
chirurgie cardiaque (par exemple réparation ou remplacement d’une valvule mitrale, pontage coronarien, chirurgie de la valvule aortique). Cette
chirurgie est également possible en tant qu’intervention primaire et isolée
et présente un taux de succès élevé. Au cours des dernières années, des
interventions moins effractives ont été décrites. La FA étant une arythmie
déclenchée par l’activité ectopique localisée le plus souvent dans les
veines pulmonaires, l’isolation électrique des veines pulmonaires demeure le fondement habituel de toutes les techniques chirurgicales.
D’autres modifications du substrat peuvent être nécessaires chez les
patients présentant une FA plus persistante. Cela est fait par l’ajout de
lignes d’ablation dans l’oreillette gauche postérieure entre les veines pulmonaires, vers l’anneau valvule mitrale, ainsi que dans des sites
spécifiques dans l’oreillette droite. L’oblitération ou la résectionde
concomitantel’appendice auriculaire gauche est fortement recommandée. Malgré le taux élevé de patients qui sont épargnés d’une FA après la
chirurgie (70 %– 85 % à 1 an), il n’a jamais été clairement démontré que
l’ablation chirurgicale d’une FA pouvait modifier la mortalité à long terme.
Selon la littérature chirurgicale, l’arrêt du traitement par anticoagulants
EM
BA
R
G
O
ED
ABSTRACT
It appears essential to evaluate the surgical approaches to atrial
fibrillation (AF) in view of the following clinical objectives: (1) to
avoid symptoms associated with rapid and irregular heart beat; (2)
to avoid blood stasis in the atrium and the attendant risk of throm-
boembolic events; and (3) to preserve atrial function, which ensures optimal cardiac performance. There is a need to balance the
priority given to each of these objectives in relation to the clinical
condition associated with the arrhythmia, as one objective may
Received for publication November 13, 2010. Accepted November 19,
2010.
on this topic with a mandate to formulate disease-specific recommendations.
These recommendations are aimed to provide a reasonable and practical approach to care for specialists and allied health professionals obliged with the
duty of bestowing optimal care to patients and families, and can be subject to
change as scientific knowledge and technology advance and as practice patterns
evolve. The statement is not intended to be a substitute for physicians using
their individual judgment in managing clinical care in consultation with the
patient, with appropriate regard to all the individual circumstances of the
patient, diagnostic and treatment options available and available resources.
Adherence to these recommendations will not necessarily produce successful
outcomes in every case.
Corresponding author: Pierre Pagé, MD, Research Center, Hôpital du
Sacré-Coeur de Montréal, 5400, Gouin B. West, Montreal, Québec, H4J 1C5,
Canada.
E-mail: pierre.page@umontreal.ca
The disclosure information of the authors and reviewers is available from the
CCS on the following Web sites: www.ccs.ca and www.ccsguidelineprograms.ca.
This statement was developed following a thorough consideration of medical literature and the best available evidence and clinical experience. It represents the consensus of a Canadian panel comprised of multidisciplinary experts
0828-282X/$ – see front matter © 2011 Canadian Cardiovascular Society. Published by Elsevier Inc. All rights reserved.
doi:10.1016/j.cjca.2010.11.008
68
Canadian Journal of Cardiology
Volume 27 2011
dominate, depending on the clinical presentation of AF and the
associated cardiac pathology. For instance, symptoms may be the
main target in the case of occasional paroxysmal “lone” AF, prevention of thromboembolism may be the major motivation to
terminate permanent or persistent AF, and improvement of cardiac performance may be the main objective in treating AF associated with congestive heart failure or valvular disease.
The maze procedure, designed and first reported by Cox et
al,1 was based on the assumption that many electrophysiological mechanisms coexist in the atrium, thus necessitating a standardized procedure that would address each of them. These
assumptions were as follows:
tion of preoperative AF exceeds 6 months, 70% to 80% of patients
remain in AF if they do not undergo a specific AF procedure.31,37
Therefore, ablation has been recommended concomitant with a mitral valve procedure in any patient who has had AF for more than 6
months.29 Meta-analyses including prospective randomized trials have documented a high success rate of AF surgery (typically
the Cox Maze procedure or several of its later modifications) in
terms of restoration of sinus rhythm.38-54 In the Mayo Clinic
experience, there was a significant difference in freedom from
AF 2 years after a concomitant maze operation (74% ⫾ 8%)
compared with 27% ⫾ 7% for a control group with mitral
valve surgery alone.55 One of the largest series of patients undergoing the maze surgery associated with other primary cardiac operations was published by Beukema et al in 2008.54
They performed surgery concomitant with a radiofrequencymodified maze procedure in 258 patients (updated to 700 in
2010)56 with permanent AF. Sustained sinus rhythm, including an atrial rhythm or an atrial-based paced rhythm, was present in 69% of their patients at 1 year, in 56% at 3 years, and in
52% at 5 years.54,56 In a recent study by Kim et al including
540 patients undergoing mitral valve repair or replacement, the
maze procedure was also performed in 36% of this group.57 After
5 years, the incidence of sinus rhythm was 86% in the patients
who had undergone the maze procedure but only 24% in patients
who did not undergo the procedure. Therefore, there is moderately high-quality evidence to demonstrate the 1-year efficacy of
concomitant AF surgery to eliminate AF in patients undergoing
cardiac surgical interventions.
R
G
1. According to the conceptual notion of Garrey,2 fractionation of the atrial tissue into smaller segments would not
allow multiple reentrant wavelets to be maintained.
2. To preserve atrial contraction, mandatory for the transport
function and for eliminating the risk of thromboembolic
events, all these segments should be linked to each other.
Impulse propagation into dead-end pathways would not
allow reentry to occur but would allow depolarization of
sufficient atrial myocardium to ensure contraction.
3. The numerous atrial incisions required to address the
first 2 assumptions would interrupt any possible macroreentrant pathway.
oraux 6 mois après la chirurgie est recommandé lorsque le rythme
sinusal peut être documenté de façon certaine et puisqu’il y a un taux
très faible de thromboembolies. Par ailleurs, peu de données probantes sont disponible pour appuyer l’innocuité de l’omission d’un traitement anticoagulant à prise orale à long terme. C’est donc dire que la
chirurgie devra surtout être utilisée comme procédure concomitante
pendant la chirurgie cardiaque pour d’autres maladies ou comme
procédure distincte après l’échec de tentatives précédentes d’ablation
par cathéter et de médicaments antiarythmiques.
O
ED
there is no evidence-based data to support the safety of omitting
long-term oral anticoagulation. Thus, surgery should be used primarily
as a concomitant procedure during cardiac surgery for other diseased
states or as a stand-alone procedure after failure of prior attempts of
catheter ablation and antiarrhythmic drugs.
EM
BA
This procedure has been applied clinically since 1987 and
has proven extremely effective.3-12 However, despite this success, the maze procedure was perceived as difficult and associated with significant morbidity,13 leading several authors to
develop novel strategies aimed at simplifying the procedure
without compromising the results. Less-invasive approaches
have been designed to avoid sternotomy by accessing the left
atrium through minimal incisions and to avoid cardiopulmonary bypass by accessing atrial tissue from the epicardium.14-26
Furthermore, new information regarding the role of the pulmonary vein–left atrial junction, drivers and rotors occurring
in the posterior left atrium, and the role of the intrinsic cardiac
nervous system has been incorporated into the evolving surgical rationale.27,28 In addition, it has been recognized that the
underlying cardiac disorders might alter treatment outcomes.
A number of factors, therefore, need to be considered when
reengineering the surgical algorithm for AF management.29,30
Elimination of AF
A number of studies have shown that preoperative AF in patients undergoing cardiac surgical interventions is an independent
factor for late major adverse cardiac events and poorer survival.31-36 The literature also indicates that once AF appears in patients with mitral valve disease, it is uncommon for mitral valve
surgery alone to restore sinus rhythm.31,34,36,37 In this context, the
duration of AF is a critical factor in predicting the return of sinus
rhythm. When AF has been present for 3 months or less, sinus
rhythm may resume in up to 80% of patients, but when the dura-
Outcome Benefit: Cardiac Events and Survival
Whether AF surgery affords improved clinical outcome to patients with preoperative AF remains controversial.13,52,54-58 Although it is generally accepted that preoperative AF is predictive of
cardiac mortality and morbidity, it is unclear whether direct surgical correction of AF restores the survival curves of AF patients to
the same level as those of patients without preoperative AF. Shortterm and intermediate-term rates of sinus rhythm after classical
maze or its variant procedures differ widely: between 44% and
95%.4-13,38-61 However, none of the 6 randomized trials comparing outcomes in patients undergoing surgery with and without
concomitant maze procedures has shown a clear benefit on mortality or stroke.56 Nevertheless, many observational reports suggest
that concomitant AF correction has the potential to improve longterm survival. In the study by Kim et al, a multivariate analysis
indicated that the absence of a maze procedure in the presence of
AF during mitral valve replacement or repair was an independent
predictor of cardiac death and major adverse events.57 Overall, the
maze procedure was associated with better event-free survival.
Bando et al also reported better survival in mitral valve patients who
Pagé et al.
Surgical Therapy
69
RECOMMENDATION
We recommend that a surgical AF ablation procedure be
undertaken in association with mitral valve surgery in patients
with AF when there is a strong desire to maintain sinus rhythm,
the likelihood of success of the procedure is deemed to be high,
and the additional risk is low (Strong Recommendation, Moderate-Quality Evidence).
RECOMMENDATION
We recommend that closure (excision or obliteration) of
the left atrial appendage be undertaken as part of the surgical
ablation of AF associated with mitral valve surgery (Strong
Recommendation, Low-Quality Evidence).
We suggest that closure of the left atrial appendage be undertaken as part of the surgical ablation of persistent AF in
patients undergoing aortic valve surgery or coronary artery bypass surgery if this does not increase the risk of the surgery
(Conditional Recommendation, Low-Quality Evidence).
Values and preferences. These recommendations place
a high value on stroke reduction and a lower value on any
concomitant loss of atrial transport with left atrial appendage closure.
R
G
Values and preferences. This recommendation recognizes that individual institutional experience and patient
considerations best determine for whom the surgical procedure is performed.
tion of sinus rhythm not only improves survival in this
group but also reduces the risks for stroke, other thromboembolism, and anticoagulant-related hemorrhage.58,59,62,63
Furthermore, one study reported that the absence of a maze
procedure was the only risk factor for late stroke in patients
undergoing mechanical mitral valve replacement.62 This
high freedom from late stroke likely is attributable to excision or obliteration of the left atrial appendage—an integral
component of the maze procedure—in addition to restoration of sinus rhythm in the majority of patients.
O
ED
underwent the maze procedure in the presence of preoperative AF,
compared with patients who underwent mitral valve surgery alone.58
On the other hand, there was no significant difference in survival data
in the Mayo Clinic experience,55 whereas Bando et al have, in a retrospective study, reported that patients with the adjunct of a maze
procedure showed a similar high degree of freedom from cardiovascular-related death (96.9%) and stroke (98.2%), compared with a
group of patients without preoperative AF.58,59,62 Although these reports constitute low-quality evidence because of their retrospective
design, they suggest that the maze procedure may improve survival
when combined with mitral valve repair. In addition, other reports
have failed to demonstrate a difference in mortality and morbidity
early after surgery, whether the maze procedure is carried out concomitantly with mitral valve surgery or not.41,54,58-61
RECOMMENDATION
BA
We recommend that patients with asymptomatic lone
AF, in whom AF is not expected to affect cardiac outcome,
should not be considered for surgical therapy for AF (Strong
Recommendation, Low-Quality Evidence).
EM
Values and preferences. This recommendation recognizes that patients with lone AF are at low risk for stroke or
other adverse cardiovascular outcomes. Thus, elimination
of AF in the absence of a high number of symptoms is
unlikely to result in an improvement in quality of life.
RECOMMENDATION
In patients with AF who are undergoing aortic valve
surgery or coronary artery bypass surgery, we suggest that a
surgical AF ablation procedure be undertaken when there is
a strong desire to maintain sinus rhythm, the success of the
procedure is deemed to be high, and the additional risk low
(Conditional Recommendation, Low-Quality Evidence).
Values and preferences. This recommendation recognizes that left atrial endocardial access is not routinely required for aortic or coronary surgery. This limits ablation to
newer epicardial approaches.
Stroke
The risk for late stroke after a maze procedure remains remarkably low throughout the surgical literature.4-7,9,13,36,46,52,54-63 Recent data suggest that restora-
Lesion Set
The original cut-and-sew Cox Maze III procedure has been
modified in 2 main ways: (1) the use of ablative energy sources
deployed with new devices and (2) the elimination of some
lines of block. The latter changes consisted of limiting the lesions to electrically isolating the pulmonary veins (PVs) from
the rest of the left atrium (Fig. 1), avoiding connecting lines to
the base of the left atrial appendage and to the mitral isthmus,
and also avoiding ablation in the right atrium. According to the
Heart Rhythm Society recommendation document, the term
maze should apply only to the lesion sets mimicking that of the
Cox Maze III procedure.30 Modifications allowed to this terminology include the replacement of most of the Cox Maze III
incisions with bipolar radiofrequency (Fig. 2, often referred to
as the “Cox Maze IV procedure”)13,41,44,45,47-50,54,64 or with
cryothermic devices.60 Less extensive lesion patterns should
not be referred to as a maze. Although new technologies such as
bipolar radiofrequency may reliably produce transmural lines
of block and can be applied minimally invasively for PVs, they
do not allow secure performance of connecting lines in the left
atrial isthmus or inside the right atrium.13,25,26 Thus, they
cannot allow the complete performance of the original lesion
pattern of the Cox Maze III procedure necessary for optimal
results in cases of persistent or permanent AF. On the other
hand, recent studies have begun to explore the role of isolation
of the PVs for paroxysmal AF.14-26 These studies usually report
small sample sizes and limited follow-up. In a series of minimally invasive bilateral PVs, Edgerton et al reported that at
6-month follow-up, 86% of patients with paroxysmal AF were
in normal sinus rhythm as evaluated by Holter monitor, pacemaker interrogation, or event monitor.15 Unfortunately, the
70
Canadian Journal of Cardiology
Volume 27 2011
Ao
LAA exclusion
PA
LAA
PV isolation
lesions
PV
PV
PV
PV
LV
IVC
R
G
Figure 1. Isolation of the left- and right-sided pulmonary veins performed with the use of an irrigated bipolar radiofrequency probe (fat
dotted lines). Pattern referred to the PVI procedure in Table 1. The
site of exclusion of the left atrial appendage is indicated by the sharp
dotted lines. Ao, ascending aorta; IVC, projection of the inferior vena
cava; LAA, left atrial appendage; LV, left ventricle; PA, pulmonary
artery; PV, pulmonary veins.
Postoperative Care and Anticoagulation After AF
Surgery
Ad et al developed a strict follow-up program designed to
adhere to the Heart Rhythm Society guidelines.30,65 In brief, it
consisted of a detailed AF registry that included a statistical
platform that interacted with an institutional database. The AF
registry tracked all patients’ preoperative, operative, and postoperative characteristics, as well as patients’ health-related
quality of life. Clinical information and algorithm-driven protocols served as a basis for recommendations to the referring
physicians. The clinical information collected included (1) patients’ self-reported rhythm, (2) current medications, (3) any
readmissions and cardiac intervention that had taken place
during the interim, and (4) the date of the last visit to the
cardiologist. Diagnostic (electrocardiography, Holter monitoring, 1-week monitoring, or pacemaker interrogation) rhythm
information and echocardiography were obtained. Then the
appropriateness of antiarrhythmic drugs and anticoagulation
was decided on, depending on the clinical algorithm.65 Incidentally, the authors recommended discontinuation of warfarin therapy whenever long-term monitoring confirmed rhythm
status and atrial contraction assured the absence of intra-atrial
stasis for a long period of time after surgery. However, Beukema and Sie recommend a more conservative approach with
respect to anticoagulation.54,56 Since reliable monitoring was
not always available and a low flow state could not be ruled out in
several patients, most of their patients were still on anticoagulant
therapy at long-term follow-up, including patients with bioprosthetic mitral valve replacement. It should also be emphasized that
the rate of recurrence of AF is not stable over time and that the
moment of AF reappearance is uncertain.54 Therefore, in the absence of strict continuous monitoring capabilities and the lack of a
clinical program with algorithm-driven treatment protocols, it is
probably best to maintain anticoagulation therapy despite its inherent inconveniences. This conservative approach constitutes the
rationale for our recommendation on postoperative anticoagulation therapy. There are new and less troublesome options than
warfarin for thromboembolism prophylaxis soon to be available
for many of these patients.66
O
ED
Pulmonary vein isolation procedure
EM
BA
results of their PV approach have been disappointing in patients with persistent or longstanding AF because freedom
from AF off drugs was achieved in only 32% at 6 months.15
Thus, we propose the following algorithm of surgical ablation,
which is based on the type of AF and the nature of underlying
cardiac abnormalities (Table 1): The recommended lesion set
ranges from PVs alone (as shown in Fig. 1) to a bi-atrial
complete Cox Maze lesion pattern (as shown in Fig. 2). In
between these extremes, PVs (in pairs or with a box lesion)
may be associated with connecting lines to the left atrial
appendage and the mitral valve annulus (PVI⫹ in Table 1,
also termed left atrial procedure and Fig. 2, A). The full Cox
Maze lesion set (CM in Table 1) should include the left
atrial procedure (Fig. 2, A) plus right atrial lines along the
sulcus terminalis and a line from the right atrial free wall to
the annulus of the tricuspid valve (Fig. 2, B), plus right atrial
isthmus ablation (Fig. 2, C). All procedures must include
exclusion or resection of the left atrial appendage. Based on
our review of the recent literature, we would recommend the
full modified Cox Maze III pattern (as shown in Fig. 2, A to
Fig. 2, C)64 for patients with persistent or long-standing AF.
Alternatively, the left atrial procedure (termed “PVI⫹” in
Table 1 and also shown in Fig. 2, A) may be used in these
patients on the surgeon’s judgement to shorten the operative time. The PVI procedure (as shown in Fig. 1) should be
confined to patients with lone paroxysmal AF and paroxysmal AF with nonmitral valve disease.
RECOMMENDATION
We recommend that oral anticoagulant therapy be continued following surgical AF ablation in patients with a
CHADS2 score ⱖ2 (Strong Recommendation, ModerateQuality Evidence).
We suggest that oral anticoagulant therapy be continued
following surgical AF ablation in patients who have undergone mechanical or bioprosthetic mitral valve replacement
(Conditional Recommendation, Low-Quality Evidence).
Values and preferences. These recommendations place
a high value on minimizing the risk of stroke and a lower
value in the utility of long-term monitoring to document
the absence of AF.
Conclusion
The Heart Rhythm Society Task Force on Catheter and
Surgical Ablation of Atrial Fibrillation suggests the following
Pagé et al.
Surgical Therapy
71
Cox Maze III ablation pattern
A. Left atrial lesions
MV
LAA
LPV
RPV
B. Right atrial lesions
External view
C. Right atrial lesions
Internal view
RAA
O
ED
RAA
TV
SVC
IVC
SVC
FO
CS
RSPV
IVC
R
G
RIPV
EM
BA
Figure 2. Cox Maze III ablation pattern. (A) Left-sided lesion set. The left atrium is shown as viewed from the right side by the surgeon through
an atriotomy in the Waterston’s groove. Ablation lines inside the left atrium (dotted lines) shown as they can be performed using various ablation
devices. Irrigated radiofrequency probes or cryosurgical probes are preferred. LAA indicates left atrial appendage excised. (B) Right-sided lesion
set. The right atrium is shown as viewed from the right side by the surgeon. The vertical dotted line indicates an ablation line in the right atrium
between the superior and inferior vena cavae; it can be performed with a bipolar radiofrequency probe or cryosurgical probe. An incision on the
central part of this line is made to open the right atrium. Additional lines are performed on the free wall until the right atrioventricular groove and
along the right atrial appendage. The double dotted line indicates isolation of the right pulmonary veins with radiofrequency energy. (C) Right-sided
lesion set (continued). The right atrium is shown open as viewed from the right side by the surgeon. Ablation lines (dark dotted lines) are
performed inside the right atrium. See text and reference 64 for details. CS, coronary sinus; FO, fossa ovalis; IVC, inferior vena cava; LAA, left
atrial appendage; LPV, left pulmonary veins; MV, mitral valve; RAA, right atrial appendage; RIPV, right inferior pulmonary vein; RPV, right pulmonary
veins; RSPV, right superior pulmonary vein; SVC, superior vena cava; TV, tricuspid valve.
indications for surgical treatment of AF: (1) symptomatic patients with AF undergoing other cardiac surgical procedures;
(2) selected asymptomatic patients with AF undergoing cardiac
surgery in whom the ablation can be performed with minimal
Table 1. Recommended type-specific surgical strategies*
Cardiac status or type of
atrial fibrillation
Lone atrial fibrillation
Mitral valve surgery
Aortic valve/CABG surgery
Paroxysmal
Persistent, mixed, or
continuous
PVI
PVI⫹
PVI
PVI⫹
Bi-atrial (CM) or PVI⫹
PVI⫹
CABG, coronary artery bypass grafting procedure; CM, lesion set mimicking the full Cox Maze III procedure including left atrial procedure (as in Fig.
2, A) plus right atrial lines along the sulcus terminalis and to the tricuspid valve,
plus right atrial isthmus ablation (as in Fig. 2, B); PVI, pulmonary vein isolation (see Fig. 1); PVI⫹, left atrial procedure consisting of pulmonary vein
isolation (in pairs or with a box lesion) and connecting lines to the left atrial
appendage and the mitral valve annulus (see Fig. 2, A).
* All procedures must include exclusion or resection of the left atrial appendage.
risk; and (3) symptomatic patients with AF who prefer a surgical approach, have experienced 1 or more failed attempts at
catheter ablation, or are not candidates for catheter ablation.30
We modified these recommendations to take into account the
recent data on the results of the various surgical options to treat
AF. It should also be recognized that all treatment options are
not available in all centres dealing with challenging cardiac
disorders. There may be significant differences in the experience and skills of the teams in various institutions. The quality
of evidence varies significantly with regard to the multiple aspects of surgical care in the field of AF. We therefore developed
the recommendations with respect to AF surgery, along with a
type-specific surgical algorithm shown in Table 1, to help surgeons select the most appropriate procedure based on the patient’s underlying cardiac status and pattern of AF.
References
1. Cox JL, Canavan TE, Schuessler RB, et al. The surgical treatment of atrial
fibrillation II. Intraoperative electrophysiologic mapping and description
72
Canadian Journal of Cardiology
Volume 27 2011
2. Garrey WE. Auricular fibrillation. Physiol Rev 1924;4:215-50.
3. Cox JL, Ad N, Palazzo T, et al. Current status of the maze procedure for
the treatment of atrial fibrillation. Semin Thorac Cardiovasc Surg 2000;
12:15-9.
4. Raanani E, Albage A, David T, Yau T, Armstrong S. The efficacy of the
Cox/maze procedure combined with mitral surgery: a matched control
study. Eur J Cardiothorac Surg 2001;19:438-42.
5. Prasad SM, Maniar HS, Camillo CJ, et al. The Cox maze III procedure
for lone atrial fibrillation: long-term efficacy in patients undergoing
lone versus concomitant procedures. J Thorac Cardiovasc Surg 2003;
126:1822-8.
6. McCarthy PM, Gillinov AM, Castle L, Chung M, Cosgrove D III. The
Cox-maze procedure: the Cleveland Clinic experience. Semin Thorac
Cardiovasc Surg 2000;12:25-9.
7. Schaff HV, Dearani JA, Daly RC, Orszulak TA, Danielson GK. Coxmaze procedure for atrial fibrillation: Mayo Clinic experience. Semin
Thorac Cardiovasc Surg 2000;12:30-7.
8. Arcidi JM Jr, Doty DB, Millar RC. The maze procedure: the LDS hospital
experience. Semin Thorac Cardiovasc Surg 2000;12:38-43.
9. Ballaux PKEW, Geuzebroek GSC, van Hemel NM, et al. Freedom from
atrial arrhythmias after classic maze III surgery: a 10-year experience.
J Thorac Cardiovasc Surg 2006;132:1433-40.
22. Gillinov AM, Svensson LG. Ablation of atrial fibrillation with minimally
invasive mitral surgery. Ann Thorac Surg 2007;84:1041-2.
23. Moten SC, Rodriguez E, Cook RC, et al. New ablation techniques for
atrial fibrillation and the minimally invasive cryo-maze procedure in patients with lone atrial fibrillation. Heart Lung Circ 2007;16(suppl 3):
S88-93.
24. Suwalski P, Suwalski G, Wilimski R, et al. Minimally invasive off-pump
video-assisted endoscopic surgical pulmonary vein isolation using bipolar
radiofrequency ablation—preliminary report. Kardiol Pol 2007;65:370-4.
25. Saltman AE. Minimally invasive surgery for atrial fibrillation. Semin Thorac Cardiovasc Surg 2007;19:33-8.
26. Beyer E, Lee R, Lam, BK. Point: Minimally invasive bipolar radiofrequency ablation of lone atrial fibrillation: early multicenter results. J Thorac Cardiovasc Surg 2009;137:521-6
27. Haissaguerre M, Jais P, Shah DC, et al. Spontaneous initiation of atrial
fibrillation by ectopic beats originating in the pulmonary veins. N Engl
J Med 1998;339:659-66.
28. Oral H. Mechanisms of atrial fibrillation: lessons from studies in patients.
Prog Cardiovasc Dis 2005;48:29-40.
29. ACC/AHA/ESC 2006 guidelines for the management of patients with
atrial fibrillation— executive summary: a report of the American College
of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice
Guidelines. J Am Coll Cardiol 2006;48:854-906. Available at: http://
content.onlinejacc.org. Accessed August 22, 2006.
R
G
10. Jessurun ER, van Hemel NM, Defauw JAMT, et al. Results of maze
surgery for lone paroxysmal atrial fibrillation. Circulation 2000;101:
1559-67.
21. Pruitt JC, Lazzara RR, Ebra G. Minimally invasive surgical ablation of
atrial fibrillation: the thoracoscopic box lesion approach. J Interv Card
Electrophysiol 2007;20:83-7.
O
ED
of the electrophysiologic basis of AFL and atrial fibrillation. J Thorac
Cardiovasc Surg 1991;101:406-26.
BA
11. Lönnerholm S, Blomström P, Nilsson L, et al. Effects of the maze operation on health-related quality of life in patients with atrial fibrillation.
Circulation 2000;101:2607-11.
12. Kosakai Y. Treatment of atrial fibrillation using the maze procedure: the
Japanese experience. Semin Thorac Cardiovasc Surg 2000;12:44-52.
EM
13. Shen J, Bailey MS, Damiano RJ. The surgical treatment of atrial fibrillation. Heart Rhythm 2009;6:S45-S50.
14. Wolf RK, Schneeberger EW, Osterday R, et al. Video-assisted bilateral
pulmonary vein isolation and left atrial appendage exclusion for atrial
fibrillation. J Thorac Cardiovasc Surg 2005;130:797-802.
15. Edgerton JR, Edgerton ZJ, Weaver T, et al. Minimally invasive pulmonary vein isolation and partial autonomic denervation for surgical treatment of atrial fibrillation. Ann Thorac Surg 2008;86:35-9.
16. McClelland JH, Duke D, Reddy R. Preliminary results of limited thoracotomy: new approach to treat atrial fibrillation. J Cardiovasc Electrophysiol 2007;18:1289-95.
30. Calkins H, Brugada J, Packer DL, et al; Heart Rhythm Society (HRS)
Task Force on Catheter Ablation of Atrial Fibrillation, European Heart
Rhythm Association (EHRA), European Cardiac Arrhythmia Society
(ECAS), American College of Cardiology (ACC), American Heart Association (AHA), and Society of Thoracic Surgeons (STS). Report of the
HRS/EHRA/ECAS expert consensus statement on catheter and surgical
ablation of atrial fibrillation: recommendations for personnel, policy, procedures and follow-up. Europace 2007;9:330-79.
31. Chua LY, Schaff HV, Orszulak TA, Morris JJ. Outcome of mitral valve
repair in patients with preoperative atrial fibrillation. J Thorac Cardiovasc
Surg 1994;107:408-11.
32. Quader MA, McCarthy PM, Gillinov AM, et al. Does preoperative atrial
fibrillation reduce survival after coronary artery bypass grafting? Ann Thorac Surg 2004;77:1514-22.
33. Ngaage DL, Schaff HV, Mullany CJ, et al. Does preoperative atrial fibrillation influence early and late outcomes of coronary artery bypass grafting?
J Thorac Cardiovasc Surg 2007;133:182-9.
17. Wudel JH, Chaudhuri P, Hiller JJ. Video-assisted epicardial ablation and
left atrial appendage exclusion for atrial fibrillation: extended follow-up.
Ann Thorac Surg 2008;85:34-8.
34. Ngaage DL, Schaff HV, Barnes SA, et al. Prognostic implications of preoperative atrial fibrillation in patients undergoing aortic valve replacement: is there an argument for concomitant arrhythmia surgery? Ann
Thorac Surg 2006;82:1392-9.
18. Yilmaz A, Van Putte BP, Van Boven WJ. Completely thoracoscopic bilateral pulmonary vein isolation and left atrial appendage exclusion for
atrial fibrillation. J Thorac Cardiovasc Surg 2008;136:521-2.
35. Ngaage DL, Schaff HV, Mullany CJ, et al. Influence of preoperative atrial
fibrillation on late results of mitral repair: is concomitant ablation justified? Ann Thorac Surg 2007;84:434-42.
19. Sirak J, Jones D, Sun B, et al. Toward a definitive, totally thoracoscopic
procedure for atrial fibrillation. Ann Thoracic Surgery 2008;86:1960-4.
36. Lim E, Barlow CW, Hosseinpour AR, et al. Influence of atrial fibrillation
on outcome following mitral valve repair. Circulation 2001;104(12 suppl
1):I59-I63.
20. Matsutani N, Takase B, Ozeki Y, et al. Minimally invasive cardiothoracic
surgery for atrial fibrillation: a combined Japan-US experience. Circ J
2008;72:434-6.
37. Obadia JF, el Farra M, Bastien OH. Outcome of atrial fibrillation after
mitral valve repair. J Thorac Cardiovasc Surg 1997;114:179-85.
Pagé et al.
Surgical Therapy
73
38. Geidel S, Ostermeyer J, Lass M, et al. Three years experience with monopolar and bipolar radiofrequency ablation surgery in patients with permanent atrial fibrillation. Eur J Cardiothorac Surg 2005;27:243-9.
53. Khargi K, Hutten BA, Lemke B, Deneke TH. Surgical treatment of
atrial fibrillation: a systematic review. Eur J Cardiothorac Surg 2005;
27:258-65.
39. Jessurun ER, van Hemel NM, Kelder JC, et al. Mitral valve surgery and
atrial fibrillation: is atrial fibrillation surgery also needed? Eur J Cardiothorac Surg 2000;17:530-7.
54. Beukema WP, Sie HT, Ramdat Misier AR, Delnoy PPHM, Wellens HJJ,
Elvan A. Intermediate to long-term results of radiofrequency modified
maze procedure as an adjunct to open-heart surgery. Ann Thorac Surg
2008;86:1409-14.
41. Sie HT, Beukema WP, Elvan A, Ramdat Misier AR. Long-term results of
irrigated radiofrequency modified maze procedure in 200 patients with
concomitant cardiac surgery: six years experience. Ann Thorac Surg 2004;
77:512-7.
42. Raanani E, Albage A, David T, Yau T, Armstrong S. The efficacy of the
Cox/Maze procedure combined with mitral surgery: a matched control
study. Eur J Cardiothorac Surg 2001;19:438-42.
43. Pasic M, Bergs P, Muller P, et al. Intraoperative radiofrequency maze
ablation for atrial fibrillation: the Berlin modification. Ann Thorac Surg
2001;72:1484-91.
44. Mohr FW, Fabricius AM, Falk V, et al. Curative treatment of atrial fibrillation with intraoperative radiofrequency ablation: short-term and midterm results. J Thorac Cardiovasc Surg 2002;123:919-27.
45. Raman J, Ishikawa S, Storer MM, Power JM. Surgical radiofrequency
ablation of both atria for atrial fibrillation: results of a multicenter trial.
J Thorac Cardiovasc Surg 2003;126:1357-66.
56. Beukema WP, Sie HT. General discussion. In: Beukema WP, Sie HT,
eds. Radiofrequency Ablation in the Treatment of Atrial Fibrillation: Cardiological and Surgical Perspectives [thesis]. Nigmegen, The Netherlands:
Universiteit van Nigmegen, 2010:243-76.
57. Kim JB, Kim HJ, Moon DH, et al. Long-term outcomes after surgery for
rheumatic mitral valve disease: valve repair versus mechanical valve replacement. Eur J Cardiothorac Surg 2010;37:1039-46.
58. Bando K, Kobayashi J, Kosakai Y, et al. Impact of Cox maze procedure on
outcome in patients with atrial fibrillation and mitral valve disease. J Thorac Cardiovasc Surg 2002;124:575-83.
59. Itoh A, Kobayashi J, Bando K, et al. The impact of mitral valve surgery
combined with maze procedure. Eur J Cardiothorac Surg 2006;29:1030-5.
60. Baek MJ, Na CY, Oh SS, et al. Surgical treatment of chronic atrial fibrillation combined with rheumatic mitral valve disease: effect of the cryomaze procedure and predictors for late outcome. Eur J Cardiothorac Surg
2006;30:728-36.
R
G
46. Jessurun ER, van Hemel NM, Defauw JJ, et al. A randomized study of
combining maze surgery for atrial fibrillation with mitral valve surgery.
J Cardiovasc Surg 2003;44:9-18.
55. Handa N, Schaff HV, Morris JJ. Outcome of valve repair and the Cox
maze procedure for mitral regurgitation and associated atrial fibrillation.
J Thorac Cardiovasc Surg 1999;118:628-35.
O
ED
40. Reston JT, Shuhaiber JH. Meta-analysis of clinical outcomes of mazerelated surgical procedures for medically refractory atrial fibrillation? Eur
J Cardiothorac Surg 2005;28:724-30.
BA
47. Doukas G, Samani NJ, Alexiou C, et al. Left atrial radiofrequency ablation
during mitral valve surgery for continuous atrial fibrillation. JAMA 2005;
294:2323-9.
EM
48. Filho CAC, Lisboa LAF, Dallan L, et al. Effectiveness of the maze procedure using cooled-tip radiofrequency ablation in patients with permanent
atrial fibrillation and rheumatic mitral valve disease. Circulation 2005;
112(suppl 1):20-5.
49. Akpinar B, Guden M, Sagbas E, et al. Combined radiofrequency modified
maze and mitral valve procedure through a port access approach: early and
mid-term results. Eur J Cardiothorac Surg 2003;24:223-30.
50. Deneke T, Khargi K, Grewe PH, et al. Efficacy of an additional maze
procedure using cooled-tip radiofrequency ablation in patients with
chronic atrial fibrillation and mitral valve disease: a randomized, prospective trial. Eur Heart J 2002;23:558-66.
51. de Lima G, Kalil RA, Leiria TLL, et al. Randomized study of surgery for
patients with permanent atrial fibrillation as a result of mitral valve disease.
Ann Thorac Surg 2004;77:2089-95.
52. Barnett SD, Ad N. Surgical ablation as treatment for the elimination of atrial
fibrillation: a meta-analysis. J Thorac Cardiovasc Surg 2006;131:1029-35.
61. Maltais S, Forcillo J, Bouchard D, et al. Long-term results following concomitant radiofrequency modified maze ablation for atrial fibrillation.
J Card Surg 2010;25:608-13.
62. Bando K, Kobayashi J, Hirata M, et al. Early and late stroke after mitral
valve replacement with a mechanical prosthesis: risk factor analysis of a
24-year experience. J Thorac Cardiovasc Surg 2003;126:358-64.
63. Cox JL, Ad N, Palazzo T. Impact of the maze procedure on the stroke rate
in patients with atrial fibrillation. J Thorac Cardiovasc Surg 1999;118:
833-40.
64. Yii M, Yap CH, Nixon I, Chao V. Modification of the Cox-maze III
procedure using bipolar radiofrequency ablation. Heart Lung Circ 2007;
16:37-49.
65. Ad N, Henry L, Hunt S, Stone L. The implementation of a comprehensive clinical protocol improves long-term success after surgical
treatment of atrial fibrillation. J Thorac Cardiovasc Surg 2010;139:
1146-52.
66. Cairns JA, Connolly S, McMurtry S, Stephenson M, Talajic M, CCS
Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: prevention of stroke and systemic
thromboembolism in atrial fibrillation and flutter. Can J Cardiol 2011;
27:74-90.
Canadian Journal of Cardiology 27 (2011) 74 –90
Society Guidelines
Canadian Cardiovascular Society Atrial Fibrillation
Guidelines 2010: Prevention of Stroke and Systemic
Thromboembolism in Atrial Fibrillation and Flutter
John A. Cairns, MD, FRCPC,a Stuart Connolly, MD, FRCPC,b
Sean McMurtry, MD, PhD, FRCPC,c Michael Stephenson, MD, FCFP,b
Mario Talajic, MD, FRCPC,d and the CCS Atrial Fibrillation Guidelines Committeee
From the University of British Columbia, Vancouver, British Columbia, Canada
b
McMaster University, 1280 Main Street West, Hamilton, Ontario, Canada
c
d
e
O
ED
a
University of Alberta, Edmonton, Alberta, Canada
Université de Montréal, Montréal, Québec, Canada
For a complete listing of committee members, see Gillis AM, Skanes AC. Canadian Cardiovascular Society Atrial Fibrillation Guidelines
2010: Implementing GRADE and Achieving Consensus. Can J Cardiol 2011;27:27-30.
ABSTRACT
RÉSUMÉ
L’incidence annuelle de l’accident vasculaire cérébral (AVC) attribuable à la fibrillation auriculaire (FA) est de 4.5 %, causant la mort
ou l’invalidité permanente dans plus de la moitié des cas. Cette incidence varie de moins de 1 % à plus de 20 % par année en fonction des
facteurs de risque: insuffisance cardiaque, hypertension, âge, diabète
et antécédents d’AVC ou d’ischémie cérébrale transitoire. Le risque
d’hémorragie majeure sous traitement avec les antagonistes de la
vitamine K varie entre 1 % et 12 % par année et s’avère lié à beaucoup
d’autres facteurs. L’index de CHADS2 et le score HAS-BLED sont utiles
pour la prédiction du risque d’AVC ou d’hémorragie. Le risque d’AVC
est réduit de 64% avec le traitement aux antagonistes de la vitamine
K et de 19% avec l’aspirine. Comparativement à l’aspirine, les antagonistes de la vitamine K réduisent ce risque de 39%. Le Dabigatran est
supérieur à la warfarine pour la prévention du risque d’AVC sans augmentation du risque de saignement majeur. Nous recommandons que
le risque d’AVC et de saignement majeur soit déterminé chez tous les
patients avec FA ou flutter auriculaire (paroxystique, persistant ou
permanent) et que la plupart reçoivent un traitement antithrom-
EM
BA
R
G
The stroke rate in atrial fibrillation is 4.5% per year, with death or
permanent disability in over half. The risk of stroke varies from under
1% to over 20% per year, related to the risk factors of congestive heart
failure, hypertension, age, diabetes, and prior stroke or transient ischemic attack (TIA). Major bleeding with vitamin K antagonists varies
from about 1% to over 12% per year and is related to a number of risk
factors. The CHADS2 index and the HAS-BLED score are useful schemata for the prediction of stroke and bleeding risks.
Vitamin K antagonists reduce the risk of stroke by 64%, aspirin
reduces it by 19%, and vitamin K antagonists reduce the risk of stroke
by 39% when directly compared with aspirin. Dabigatran is superior to
warfarin for stroke prevention and causes no increase in major bleeding. We recommend that all patients with atrial fibrillation or atrial
flutter, whether paroxysmal, persistent, or permanent, should be stratified for the risk of stroke and for the risk of bleeding and that most
should receive antithrombotic therapy. We make detailed recommendations as to the preferred agents in various types of patients and for
Received November 11, 2010. Accepted November 24, 2010.
Corresponding author: Dr John A. Cairns, GLD Health Care Centre,
Room 9113, 2775 Laurel St, Vancouver, BC, V5Z 1M9, Canada.
E-mail: jacairns@medd.med.ubc.ca
The disclosure information of the authors and reviewers is available from the CCS
on the following Web sites: www.ccs.ca and www.ccsguidelineprograms.ca.
This statement was developed following a thorough consideration of medical literature and the best available evidence and clinical experience. It represents the consensus of a Canadian panel comprised of multidisciplinary experts
on this topic with a mandate to formulate disease-specific recommendations.
These recommendations are aimed to provide a reasonable and practical approach to care for specialists and allied health professionals obliged with the
duty of bestowing optimal care to patients and families, and can be subject to
change as scientific knowledge and technology advance and as practice patterns
evolve. The statement is not intended to be a substitute for physicians using
their individual judgment in managing clinical care in consultation with the
patient, with appropriate regard to all the individual circumstances of the
patient, diagnostic and treatment options available and available resources.
Adherence to these recommendations will not necessarily produce successful
outcomes in every case.
0828-282X/$ – see front matter © 2011 Canadian Cardiovascular Society. Published by Elsevier Inc. All rights reserved.
doi:10.1016/j.cjca.2010.11.007
Cairns et al
Stroke Prevention in Atrial Fibrillation
75
Risk of Stroke
Risk factors and risk estimation schemes
by about 2.0% for each 1-point increase in CHADS2 score
(from 1.9% with a score of 0 to 18.2% with a score of 6). This
scheme was also evaluated in comparison with several others
among 2580 patients receiving aspirin in 6 prospective trials.15
The CHADS2 index identified increments in stroke risk similar to those identified in the prior validation and was better
than the other schema at discriminating medium- and highrisk patients. Although a recent systematic review16 of 12 risk
stratification schemes noted that none has been compared in a
single cohort of adequate size and diversity, the CHADS2 index
has appropriately become the favoured choice for determining
risk of stroke and guiding choice of antithrombotic therapy.13
The European Society of Cardiology (ESC) has recently
updated its guidelines for the management of AF17 and has
incorporated the new Birmingham 2009 schema (known by
the acronym CHA2DS2-VASc) for the prediction of stroke
risk.18 The schema was validated and compared with standard
criteria in a subset of 1577 patients documented in the Euro
Heart Survey on AF population. The schema is similar to the
CHADS2, but gives 2 points for age of 75 years or older and 1
point for age between 65 and 74 years, 1 point for vascular
disease (prior myocardial infarction, peripheral artery disease,
or aortic plaque), and 1 point for female sex. The ESC recommends that the widely used and easily remembered CHADS2
be applied first; only if the score is under 2 should the new
schema be applied to further grade risk of stroke in patients
at low risk. The degree of risk can be refined, and if any of
the additional risk factors embodied in the CHA2DS2-VASc
are present, the score will be increased and may influence the
physician to choose more potent antithrombotic management. Conversely, if the score remains at 0, the patient is
clearly at very low risk of stroke and may not require any
antithrombotic agent. The ESC recommends that a patient
EM
BA
R
G
In the 5 landmark randomized clinical trials of oral anticoagulants (OACs) among patients with nonvalvular atrial fibrillation (AF),1-6 most of whom had no previous stroke or TIA,
control subjects had a mean 4.5% annual incidence of stroke
(range, 3%-7%), over half of which resulted in death or permanent disability.7 The mean annual incidence of the composite of stroke or other systemic emboli was 5% (range, 3%7.4%). These subjects had no contraindications to warfarin
and no echocardiographic evidence of rheumatic valvular disease. The observed rates of stroke and other systemic embolism
were similar to those reported in earlier cohorts8 and likely are
representative of individuals in the general population with AF
and not receiving antithrombotic therapy. In the United
States, the annual risk of stroke attributable to AF is 1.5% in
the age group 50 to 59 years, rises to 23.5% in the age group 80
to 89 years, and overall is 15%.9
An overview of the randomized control trials of warfarin
therapy in AF7 determined that previous stroke or TIA, increasing age, history of hypertension, and diabetes were statistically significant multivariate predictors of stroke. Annual
stroke risk ranged from 0 (patients younger than 60 years) to
1.3% (patients younger than 80 years with no other risk factors) and to 11.7% (patients with prior stroke or TIA). A recent
systematic review10 examined the evidence identifying independent risk factors for stroke as reported in 7 studies selected
according to rigourously defined criteria. The absolute annual
risk of stroke varied 20 fold among patients grouped by various
risk factors. Independent risk factors for stroke were the same as
those previously identified7: stroke or TIA (relative risk [RR]
2.5), age (RR 1.5/decade), history of hypertension (RR 2.0),
and diabetes mellitus (RR 1.7). Female sex was an independent
risk factor in 3 of 6 cohorts, but coronary artery disease and clinical
congestive heart failure were not found to be independent risk
factors in any of these studies. Even though congestive heart failure
and reduced ejection fraction have been identified only as univariate risk factors,7,10-12 they are included in current risk classification schemes.13,14 The review10 emphasized a variety of shortcomings of the studies, including inconsistencies in definitions of some
of the risk factors, the use of antiplatelet therapies, and the stroke
outcomes (ischemic strokes only, all strokes, strokes plus other
systemic emboli, and strokes plus TIAs).
The CHADS2 index14 (see Table 1 for the components of
the acronym) assigns 1 point each for congestive heart failure,
hypertension, age 75 years or older, and diabetes mellitus and 2
points for a history of stroke or TIA (Table 1). The scheme was
validated and compared with 2 other schemes among 1733
Medicare beneficiaries aged 65 to 95 years who had been discharged from hospital with nonrheumatic AF and had not been
prescribed warfarin. The CHADS2 index was the most accurate predictor of stroke, with the annual stroke rate increasing
botique. Nos recommandations font état des agents antithrombotiques à favoriser dans les contextes cliniques de cardioversion,
maladie cardiaque athérosclérotique concomitante, procédures diagnostiques ou chirurgicales avec risque d’hémorragie majeure associée, et en cas d’AVC ou de saignement majeur. Les alternatives au
traitement antithrombotique sont brièvement discutées.
O
ED
the management of antithrombotic therapies in the common clinical
settings of cardioversion, concomitant coronary artery disease, surgical or diagnostic procedures with a risk of major bleeding, and the
occurrence of stroke or major bleeding. Alternatives to antithrombotic
therapies are briefly discussed.
Table 1. The CHADS2 score for estimating stroke risk in patients
with atrial fibrillation according to the presence of major risk factors
CHADS2 risk criteria
Score
C
H
A
D
S2
Congestive heart failure
Hypertension
Age ⬎75 years
Diabetes mellitus
(Prior) stroke or TIA
1
1
1
1
2
CHADS2 score
Adjusted stroke rate, %/y
(95% CI)
0
1
2
3
4
5
6
1.9 (1.2-3.0)
2.8 (2.0-3.8)
4.0 (3.1-5.1)
5.9 (4.6-7.3)
8.5 (6.3-11.1)
12.5 (8.2-17.5)
18.2 (10.5-27.4)
Data from Gage BF, et al.14
76
Canadian Journal of Cardiology
Volume 27 2011
heart failure are uncertain. The risk of stroke is also substantial
among patients with hypertrophic cardiomyopathy and AF.
These risks have not been rigourously evaluated, and antithrombotic therapies for patients with AF and thyrotoxicosis or
hypertrophic cardiomyopathy should be based on the presence
of validated stroke risk factors.9,13,17
Atrial flutter
There is a widespread perception that the risk of stroke is
less with atrial flutter than with AF. However, a retrospective
analysis of a large database of elderly hospitalized patients
found little difference in the risk ratios for atrial flutter (1.4)
and AF (1.6).25 By 8 years of follow-up, more than half the
patients with atrial flutter had developed AF, and these patients
were more likely to experience a stroke. The development of AF
was more likely among patients with congestive heart failure,
rheumatic heart disease, hypertension, and diabetes mellitus.
O
ED
Trials of Antithrombotic Therapies
Oral vitamin K antagonists and antiplatelet agents
An overview7 of the initial 5 randomized trials of oral vitamin K antagonists compared with no treatment found the incidence of ischemic stroke was reduced from 4.5% per year to
1.4% per year (relative risk reduction [RRR] 68%; 95% CI,
50%-79%; P ⬍ .001). The rate of major hemorrhage with
vitamin K antagonists was 1.3% per year vs 1% per year in
controls. The most recent meta-analysis of such trials26 in-
R
G
Figure 1. Randomized controlled trials (RCTs) of adjusted-dose warfarin (or other vitamin K antagonist in a small proportion of patients)
vs placebo or no treatment. Point estimates of the relative risk
reductions of stroke (ischemic plus hemorrhagic) with their associated 95% CIs are depicted for 5 trials of primary prevention and 1 of
secondary prevention. The overall relative risk reduction is 64% (95%
CI, 49%-74%). AFASAK, Atrial Fibrillation, ASpirin, AntiKoagulation;
SPAF, Stroke Prevention in Atrial Fibrillation; BAATAF, Boston Area
Anticoagulation Trial for Atrial Fibrillation; CAFA, Canadian Atrial
Fibrillation; SPINAF, Stroke Prevention in Nonrheumatic Atrial Fibrillation; EAFT, European Atrial Fibrillation Trial. Reprinted from
Hart RG et al26 with permission from Ann Intern Med.
Paroxysmal AF
EM
BA
with a score of 0 according to the CHA2DS2-VASc schema
should receive either aspirin or no antithrombotic therapy,
with the latter preferred; a patient with a score of 1 should
receive either aspirin or OAC, with the latter preferred; and
a patient with a score of 2 should receive OAC. This new
schema may eventually be useful for patient management,
but for the present, the CCS recommends ongoing use of
the CHADS2 schema.
The Stroke Prevention in Atrial Fibrillation (SPAF) trial6
found similar annual rates of ischemic stroke in patients with
“recurrent” (3.2%) and “chronic” (3.3%) AF. A report from
the Atrial Fibrillation Clopidogrel Trial With Irbesartan for
Prevention of Vascular Events-Warfarin (ACTIVE-W), based
on 1202 patients with paroxysmal AF and 5495 with persistent
or permanent AF, confirmed similar rates of thromboembolic
events.19 However, it is possible that the risk of stroke is less in
patients whose episodes of AF are brief (⬍1 day) and selfterminating.20 The short-term risk of stroke appears to be
higher in patients with recent-onset AF than in those with AF
that first occurred more than 1 to 2 years ago.21,22 Among AF
patients with prior stroke, the annual recurrence rate is about
12% without antithrombotic treatment.7,23 Several case series
reported recurrence rates of 0.1% to 1.3% per day during the
first 2 weeks following a cardioembolic stroke.24
Thyrotoxicosis and hypertrophic cardiomyopathy
The risk of stroke in patients with thyrotoxic AF is substantial, although the mechanism and the relative role of congestive
Figure 2. Randomized controlled trials (RCTs) of aspirin vs placebo or
no treatment. Point estimates of the relative risk reductions of stroke
(ischemic plus hemorrhagic) with their associated 95% CIs are depicted for 4 trials of primary prevention and 3 of secondary prevention. The overall relative risk reduction is 19% (95% CI, ⫺1% to 35%).
AFASAK, Atrial Fibrillation, ASpirin, AntiKoagulation; SPAF, Stroke
Prevention in Atrial Fibrillation; EAFT, European Atrial Fibrillation Trial;
ESPS, European Stroke Prevention Study; LASAF, Low-dose Aspirin,
Stroke, Atrial Fibrillation; UK-TIA, United Kingdom Transient Ischemic
Attack; JAST, Japan Atrial fibrillation Stroke Trial. Reprinted from Hart
RG et al26 with permission from Ann Intern Med.
Cairns et al
Stroke Prevention in Atrial Fibrillation
77
pidogrel might be noninferior to warfarin for the prevention of
stroke, while offering the advantages of less bleeding and
greater convenience. However, the ACTIVE-W trial32 found
the RR for the composite outcome of stroke, non– central nervous system embolus, myocardial infarction, and vascular
death was 1.44 (95% CI, 1.18-1.76; P ⫽ .0003) for the combination of clopidogrel plus aspirin (75 mg and 75-100 mg/d)
vs warfarin (INR 2-3). Somewhat surprisingly, the RR for major bleeding was 1.10 (95% CI, 0.83-1.45) with the combination.
It had also been expected that in patients not suitable for
warfarin therapy, the combination of aspirin and clopidogrel
might be more effective than aspirin alone. The ACTIVE-A
trial33 did find that after a mean of 3.6 years, the risk of major
vascular events was reduced by the combination (RR 0.89;
95% CI, 0.81-0.98; P ⫽ .01). However, major bleeding was
increased by the combination (2.0% vs 1.3% per year; RR
1.57; 95% CI, 1.29-1.92; P ⬍ .01).
O
ED
New non–vitamin-K-antagonist anticoagulants
Ximelagatran is an oral direct thrombin inhibitor with predictable and stable pharmacokinetics and relatively low potential for interactions with other drugs and with foods. Coagulation monitoring and dose adjustments are not required. This
agent was evaluated in 2 large trials employing noninferiority designs.34,35 In both, it was concluded that ximelagatran was noninferior to warfarin. The incidence of major bleeding was similar
with the 2 agents, but all bleeding was significantly less with ximelagatran. However, both studies found a 6-fold excess of patients with elevations of alanine aminotransferase to greater than 3
times the upper limit of normal, usually within the first 6 months.
The Food and Drug Administration did not approve the new
agent, having concluded that the more convenient dose and monitoring regimens and less total bleeding did not outweigh concerns
about hepatic toxicity and the inappropriately large noninferiority
margins.
Dabigatran is an oral direct thrombin inhibitor that is licensed for use in Canada and the United States. It was compared with warfarin in the Randomized Evaluation of LongTerm Anticoagulation Therapy (RE-LY) trial,36 in which
18,113 patients with AF (mean CHADS2⫽ 2.1) were randomized to dabigatran 110 mg twice daily, dabigatran 150 mg twice
daily, or warfarin (INR 2-3) and followed for a median of 2.0
years. The mean time in the therapeutic range for warfarin was
64%. Rates of discontinuation of therapy by 2 years were
16.6% for warfarin, 20.7% for dabigatran 110 mg, and 21.2%
for dabigatran 150 mg. Approximately 20% of subjects were
taking aspirin in addition to their study drug. The rates of the
principal outcome of all stroke (ischemic or hemorrhagic) or
non– central nervous system embolus were 1.69% per year
with warfarin, 1.53% per year with dabigatran 110 mg (RR
0.91; 95% CI, 0.74-1.11; P ⬍ .001 for noninferiority), and
1.11% per year with dabigatran 150 mg (RR 0.66; 95% CI,
0.53-0.82; P ⬍ .001 for superiority; Fig. 4). The RR of stroke
or systemic embolus for dabigatran 150 mg vs 110 mg was 0.73
(95% CI, 0.58-0.91; P ⫽ .005). The rates of major bleeding
were 3.36% per year with warfarin, 2.71% per year with dabigatran 110 mg (RR vs warfarin 0.8, P ⫽ .003), and 3.11% per
year with dabigatran 150 mg (RR vs warfarin 0.93, P ⫽ .31 and
RR vs dabigatran 110 mg 1.16, P ⫽ .052). The rates of the net
clinical benefit outcome (a composite of stroke, systemic em-
R
G
Figure 3. Randomized trials of adjusted-dose warfarin (or other vitamin K antagonist in a small proportion of patients) vs aspirin. Point
estimates of the relative risk reductions of stroke (ischemic or hemorrhagic) with their associated 95% CIs are depicted for 7 trials of
primary prevention and 1 of secondary prevention. The overall relative
risk reduction is 39% (95% CI, 19%-53%). AFASAK, Atrial Fibrillation,
ASpirin, AntiKoagulation; BAFTA, Birmingham Atrial Fibrillation Treatment of the Aged; Chinese ATAFS, Chinese Antithrombotic Therapy in
Atrial Fibrillation; EAFT, European Atrial Fibrillation Trial; PATAF, Prevention of Arterial Thromboembolism in Atrial Fibrillation; SPAF,
Stroke Prevention in Atrial Fibrillation. Reprinted from Hart RG et al27
with permission from Ann Intern Med.
EM
BA
cluded 1 additional trial (of secondary prevention of stroke)
and calculated an RRR of 64% (95% CI, 49% to 74%) for the
more clinically meaningful outcome of all stroke (ischemic or
hemorrhagic; Fig. 1). The absolute risk reduction (ARR) was
2.7% per year in primary prevention trials and 8.4% per year in
the only secondary prevention trial. There was an excess of
0.3% per year (P ⫽ not significant) of major extracranial hemorrhage with vitamin K antagonist therapy but a statistically
significant ARR of mortality of about 1.6% per year.
The overview included trials of aspirin vs no treatment26
and reported an RRR for all stroke of 19% (95% CI, 1% to
35%; Fig. 2), with an ARR of 0.8% per year in primary prevention trials and 2.5% per year in secondary prevention trials.
There were no significant differences in major extracranial
hemorrhage or mortality. An update of this overview27 assessed
trials of vitamin K antagonists vs aspirin and reported an RRR
for all stroke of 39% (95% CI, 19%-53%) in favour of vitamin
K antagonists (Fig. 3), equivalent to an ARR of about 0.9% per
year for primary prevention and 7% per year for secondary
prevention. There were no significant differences in major extracranial hemorrhage or mortality. The inclusion of 3 further
trials comparing vitamin K antagonists with other antiplatelet
agents did not importantly alter the findings.
Warfarin adjusted to an international normalized ratio
(INR) of 2 to 3 has been compared with various regimens of
lower-dose warfarin plus aspirin28 and to warfarin at lower
intensity and low fixed dose,29-31 but none of these regimens
was as effective. It had been expected that in patients suitable
for warfarin therapy, the combination of aspirin plus clo-
78
Canadian Journal of Cardiology
Volume 27 2011
EM
BA
R
G
bolism, pulmonary embolism, myocardial infarction, death, or
major bleeding) were 7.64% per year with warfarin, 7.09% per
year with dabigatran 110 mg (RR vs warfarin 0.92; 95% CI,
0.84-1.02), and 6.91% per year with dabigatran 150 mg (RR vs
warfarin 0.91; 95% CI, 0.82-1.00). Hence, in this group of
patients with clear indications for warfarin therapy, dabigatran
110 mg twice daily was associated with rates of stroke and
systemic embolism similar to those associated with warfarin,
but with a rate of major hemorrhage that was lower. Compared with warfarin, dabigatran 150 mg twice daily was
associated with lower rates of stroke and systemic embolism
and a similar rate of major hemorrhage. Compared with
dabigatran 110 mg, the 150-mg dose was associated with
lower rates of stroke and systemic embolus but a strong
trend toward more major hemorrhage.
The data for the comparative beneficial and harmful effects
of dabigatran vs warfarin among patients with AF are derived
only from RE-LY and a relatively small pilot study (Prevention
of Embolic and ThROmbotic events in patients with persistent
atrial fibrillation).37 However, RE-LY enrolled over 18,000
patients. The recommendations made by previous national
guidelines exercises have been based on a total of 2900 patients
in the randomized trials of warfarin vs control, 3990 patients in
the trials of aspirin vs control, and 3647 patients in the trials of
warfarin vs aspirin. The results of RE-LY and studies of other
newer anticoagulants, as they are published, must be taken into
account in all subsequent guidelines exercises.
Although dabigatran 110 mg twice daily was found to be as
effective as warfarin and caused less major bleeding, and dabigatran 150 mg twice daily was found to be more effective than
warfarin and with a similar risk of major bleeding, additional
considerations are necessary in arriving at sensible recommendations for use. The subjects all had at least 1 risk factor for
stroke (mean CHADS2 was 2.0), and patients with CrCl ⬍30
mL per minute and any condition that increased the risk of
bleeding were excluded. Dyspepsia was twice as common in the
dabigatran groups, gastrointestinal bleeding was more common, and patients receiving dabigatran discontinued study
therapy almost 50% more often in the first year of therapy than
O
ED
Figure 4. Cumulative hazard rates (y-axis) vs time in years (x-axis) for
the primary outcome of stroke (ischemic or hemorrhagic) or systemic
embolism, according to treatment group (dabigatran 150 mg twice
daily, dabigatran 110 mg twice daily, or warfarin [INR 2-3]). RR,
relative risk. Reprinted from Connolly SJ, et al36 with permission from
N Engl J Med, © Massachusetts Medical Society.
did those receiving warfarin. Although there was a trend to a
reduction of the composite clinical outcome in the dabigatran
groups, there was a trend to more frequent myocardial infarction with dabigatran, which was significant at the 150-mg dose.
There was no hint of greater hepatic toxicity with dabigatran
than with warfarin, but the total clinical experience extends to
only a mean of 2 years, and careful long-term follow-up data
are needed. Dabigatran tablets are much more costly than warfarin, but rigourous cost-effectiveness analyses will be needed
to assess total costs.
We recommend that when an OAC is indicated for stroke
prevention, most patients should receive dabigatran in preference to warfarin. Possible exceptions would include patients
with a propensity to dyspepsia, gastrointestinal bleeding, or
both and those at substantial risk of coronary events (see more
detailed discussion under the heading Coronary Artery Disease). The dose of 150 mg twice a day is preferable to 110 mg
twice a day, except in patients of low body weight, decreased
renal function, or at increased risk of major bleeding.
Idraparinux is a specific inhibitor of activated factor X,
which may be given in a fixed, weekly subcutaneous injection
without coagulation monitoring. This agent was compared
with vitamin K antagonists (INR 2-3) in the AMADEUS trial
of 4576 patients.38 The trial was stopped early because of excess
clinically relevant bleeding with idraparinux (19.7% vs 11.3%
per year, P ⬍ .0001), at which point idraparinux was noninferior for the principal outcome of all stroke or systemic embolism (hazard ratio 0.71; 95% CI, 0.39-1.30; P ⫽ .007). Elderly
patients and those with renal insufficiency were more at risk of
excess bleeding, but clearly at the dose regimen tested, idraparinux would not be a suitable alternative to vitamin K antagonist therapy in AF patients.
There are several available oral, direct-acting factor Xa inhibitor drugs that have proven effective and safe in studies of
deep venous thrombosis and offer promise in the setting of AF.
In the Apixaban Versus ASA to Reduce the Rate Of Embolic
Stroke (AVERROES) trial,39 apixaban (5 mg twice a day) was
compared with aspirin (81-324 mg daily) among patients with
AF at more than very low risk of stroke in whom vitamin K
antagonist therapy was unsuitable. The trial was terminated for
early efficacy in 2010. In the Apixaban for the Prevention of
Stroke in Subjects with Atrial Fibrillation (ARISTOTLE)
trial,40 apixaban (5 mg twice a day) is being compared with
warfarin (INR 2.5) among patients at somewhat higher risk of
stroke. The expected enrollment is 15,000 patients, with completion in 2010. In the Rivaroxaban Once daily oral direct
factor Xa inhibition Compared with vitamin K antagonism for
prevention of stroke and Embolism Trial in Atrial Fibrillation
(ROCKET-AF) trial,41 which enrolled over 14,000 patients,
rivaroxaban (20 mg/d) was compared to warfarin (INR 2.5)
among patients with AF at risk of stroke and suitable for warfarin therapy. Rivaroxiban was noninferior to warfarin for the
principal outcome of all stroke or systemic embolus.
Atrial flutter
Although there are no rigourous prospective data on the
incidence of stroke among patients with atrial flutter, nor are
there randomized trials of the value of anticoagulation, it is
generally recommended that patients with atrial flutter be risk
stratified and treated in the same manner as patients with
AF.9,13
Cairns et al
Stroke Prevention in Atrial Fibrillation
79
Clinical characteristic
Score
Hypertension
Abnormal renal or liver function (1 point each)
Stroke
Bleeding
Labile INRs
Elderly (eg, age ⬎65 yr)
Drugs or alcohol (1 point each)
1
1 or 2
1
1
1
1
1 or 2
Risk factor score
Major bleeds (%/y)
0
1
2
3
4
5
1.13
1.02
1.88
3.74
8.70
12.50
Data from Pisters R, et al.46
EM
BA
R
G
Risk of Hemorrhage
The efficacy of any antithrombotic therapy for the prevention of ischemic stroke must be balanced against the risk of
major hemorrhage, particularly cerebral hemorrhage, which is
often fatal. In each of the initial randomized trials of antithrombotic therapies, the principal outcome was the composite
of ischemic stroke or systemic embolus. Although hemorrhage
and the subsets of intracranial and intracerebral hemorrhage
were generally reported, the net benefit for major clinical outcomes was not always clear. More recent trials and overviews
have focused on the principal outcome of all stroke (ischemic
plus hemorrhagic) or systemic embolus, a more meaningful
outcome for patients and treating physicians. The incidence of
extracranial major hemorrhage (usually without long-term sequellae among survivors) can be subjectively compared to the
reduced incidence of all stroke in order to reach conclusions
about the net patient benefits of antithrombotic therapies.
The risk of hemorrhage depends on the specific antithrombotic agent (including dose and monitoring) and on a variety of
patient characteristics. The risks of hemorrhage are lowest with
either aspirin (75-325 mg/d) or clopidogrel (75 mg/d) alone,
higher when they are combined, higher still with dabigatran
110 mg twice a day, and highest with dabigatran 150 mg per
day and vitamin K antagonists, which carry similar risks. When
vitamin K antagonists are used, the bleeding risk depends on
the INR, the quality of monitoring, the duration of therapy
(the risk is higher during the initial few weeks of therapy), and
the stability of dietary and other factors that may alter the INR
at a given dose of the chosen agent. The risk of bleeding is likely
to be higher in common clinical practice than in the rigourous
setting of a clinical trial or a dedicated, expert anticoagulation
service.
For most patients who are candidates for warfarin, an INR
range of 2.0 to 3.0 with a target of 2.5 appears optimal.9,13 In
a large cohort of patients, the risk of ischemic stroke, severity of
stroke, and mortality rose sharply when INR fell to 1.5 to 1.9,
but the risk of intracranial hemorrhage did not rise until INR
values exceeded 3.9.42 A recent meta-analysis43 of studies that
assigned hemorrhagic and thromboembolic events in patients
taking anticoagulants to discrete INR ranges found that 44%
of hemorrhages occurred when INRs were above the therapeutic range, 48% of thromboembolic events took place when
INRs were below it, and the mean proportion of events that
occurred when the patient’s INR was outside the therapeutic
range was higher in the studies of shorter follow-up. Patients
with a previous TIA or minor stroke may benefit from a somewhat higher INR of 2.0 to 3.5, with a target of 3.0.13,17,44
Patients at higher risk of cerebral hemorrhage, particularly
those older than 75 years, may benefit from a somewhat lower
INR range of 1.6 to 2.5, with a target of 2.0,13 although protection against ischemic stroke drops off sharply when INRs
fall below this target.
The HEMORR2HAGES scheme45 was developed from 3
previously published prediction rules, a recent systematic review, and a formal literature search. The scheme allotted 2
points for a previously documented episode of bleeding and 1
point each for hepatic or renal disease, ethanol abuse, malignancy, age ⬎75 years, reduced platelet count or function, rebleeding risk, hypertension (uncontrolled), anemia, genetic
factors (CYP 2C19 SNPs), excessive falls (including neuropsychiatric disease), and stroke. When compared with the 3 earlier
prediction rules in a population of elderly patients with AF45
who were receiving warfarin, aspirin, or no antithrombotic
therapy, the new scheme provided good discrimination among
patients with an annual risk of hospitalization for hemorrhage
while receiving warfarin, which ranged from 1.9% to 12.3%.
The new ESC guidelines for management of AF46 suggest
the use of a new schema for the prediction of bleeding risk
(Table 2). It is based on the presence of hypertension, abnormal liver or renal function, history of stroke or bleeding, labile
INRs, elderly age (⬎65 years), and concomitant use of drugs
that promote bleeding or excess alcohol use (HAS-BLED is the
acronym)46 and was derived from the Euro Heart Survey on
AF. The proposed schema relies on fewer and more readily
obtained risk factors than earlier schemata do and performs at
least as well as the HEMOR2RHAGES schema in the prediction of bleeding events. Documentation of a HAS-BLED score
allows the clinician to assign the patient a risk of major bleeding
ranging from about 1% (score 0-1) to 12.5% (score 5) and can
be useful in decisions about the relative risks of stroke vs major
bleeding with various antithrombotic therapies. Patients at
high risk of major bleeding warrant caution in the use of antithrombotic therapies and closer monitoring and follow-up. We
suggest the use of this new schema as a simpler alternative to the
HEMOR2RHAGES schema.
O
ED
Table 2. The HAS-BLED score for estimating the risk of major
bleeding among AF patients
RECOMMENDATION
We recommend that all patients with AF or AFL (paroxysmal, persistent, or permanent) should be stratified using a predictive index for stroke (eg, CHADS2) and for the
risk of bleeding (eg, HAS-BLED) and that most patients
should receive antithrombotic therapy (Strong Recommendation, High-Quality Evidence).
We recommend that patients at very low risk of stroke
(CHADS2 ⫽ 0) should receive aspirin (75-325 mg/d)
(Strong Recommendation, High-Quality Evidence).
We recommend that patients at low risk of stroke
(CHADS2 ⫽ 1) should receive OAC therapy (either warfarin [INR 2 to 3] or Dabigatran) (Strong Recommendation,
80
Canadian Journal of Cardiology
Volume 27 2011
Overview of Thromboembolic Management
Elderly patients
CHADS2 = 0
CHADS2 = 1
CHADS2 ≥ 2
aspirin
OAC
OAC
Aspirin is a reasonable
alternave in some as
indicated by risk-benefit
Dabigatran is preferred OAC over warfarin in most paents.
Figure 5. A summary of our recommendations for thromboembolic
management guided by the CHADS2 score. See Tables 1 and 2 for
definitions of CHADS2 and HAS-BLED. OAC, oral anticoagulant.
R
G
High-Quality Evidence). We suggest, based on individual
risk-benefit considerations, that aspirin is a reasonable alternative for some (Conditional Recommendation, Moderate-Quality Evidence).
Advanced age (⬎75 years) has been consistently noted as a
risk factor for both ischemic stroke and major hemorrhage,
particularly intracranial. Hylek et al53 reported a series of 472
patients aged ⱖ65 years (153 patients aged ⱖ80 years), with
electrocardiogram-verified AF, newly started on warfarin at the
study institution, and managed by the on-site anticoagulation
clinic. Anticoagulation control was very good, with 56% of
person-time within the INR range of 2.0 to 3.0, 29% below
2.0, 11% within 3.0 to ⬍4.0, and only 2% ⱖ4.0. Even within
this optimized setting, the rate of major hemorrhage (100%
follow-up) was 7.2 per 100 patient-years (intracranial hemorrhage 2.5 per 100 patient-years). The incidence of major hemorrhage was 13.1% for patients aged ⱖ80 years vs 4.75% for
those ⬍80 years. The risk during the first 90 days of therapy
was 3 times that of the remainder of the year. The risk of major
hemorrhage was increased 20 times among patients with an
INR ⬎ 4.0. Most of the intracranial bleeds occurred in patients
aged ⱖ75 years. The rate of major hemorrhage was higher in
patients with higher CHADS2 scores. In contrast, the Birmingham Atrial Fibrillation Treatment of the Aged study54 found
that in patients aged ⬎75 years, warfarin was more efficacious
than aspirin in preventing all strokes (ischemic plus hemorrhagic) and did not cause more major extracranial hemorrhage
(1.4% per year with warfarin vs 1.6% per year with aspirin).
The lower bleeding risk may be attributable to more restrictive
patient selection for a clinical trial than for the Hylek survey
and to the fact that 40% of them had been taking warfarin
safely prior to entering the trial. A more recent cohort study
found an annual incidence of major extracranial bleeding of
1.3% with careful INR management.55 These observations
point to the challenges in choosing the optimal antithrombotic
therapy for very elderly patients in order to ensure a favourable
risk-benefit ratio.56 For those with no stroke risk factors other
than age ⱖ75 years, some guidelines have recommended consideration of aspirin in preference to warfarin.13 Nevertheless,
ischemic stroke, with its dire consequences, is relatively frequent, and the competing risk of intracranial hemorrhage with
warfarin may be acceptable. If warfarin is to be used, great care
must be taken to rigourously maintain the selected therapeutic
INR with frequent monitoring in the first 3 months and more
often than the “standard” monthly interval subsequently.
O
ED
Assess Thromboembolic
Risk (CHADS2) and
Bleeding Risk (HAS-BLED)
No anthromboc may be
appropriate in selected young
paents with no stroke risk
factors
Selected Clinical Settings
EM
BA
Values and preferences. This recommendation places
relatively greater weight on the absolute reduction of
stroke risk with both warfarin and dabigatran compared
with aspirin and less weight on the absolute increased risk
for major hemorrhage with an OAC compared with aspirin.
We recommend that patients at moderate risk of stroke
(CHADS2 ⱖ2 should receive OAC therapy (either warfarin
[INR 2-3] or Dabigatran) (Strong Recommendation,
High-Quality Evidence).
We suggest that when OAC therapy is indicated, most
patients should receive dabigatran in preference to warfarin.
In general, the dose of dabigatran 150 mg by mouth twice a
day is preferable to a dose of 110 mg by mouth twice a day
(exceptions discussed in text) (Conditional Recommendation, High-Quality Evidence).
Values and preferences. This recommendation places a
relatively high value on the greater efficacy of dabigatran
during a relatively short time of follow-up, particularly
among patients who have not previously received an OAC;
the lower incidence of intracranial hemorrhage; and its ease
of use—and less value on the long safety experience with
warfarin.
Figure 5 is a flow chart outlining our recommendations for
the choice of antithrombotic therapy.
Recent practice guidelines9,13 stress the importance of appropriate antithrombotic therapy for AF, and yet practice surveys indicate that rates of compliance range from rather
low47-51 to reasonably high.52
Cardioversion
Although the randomized trials have shown no improvement in major outcomes, including thromboembolism, with a
rhythm control strategy vs rate control, individual patients may
gain symptomatic benefit and even long-term freedom from
AF after electrical or pharmacologic cardioversion. The strongest predictor of initial and persistent success with cardioversion is short duration of the AF before cardioversion. In general, it may be expected that AF occurring in conjunction with
surgery (see accompanying article titled “Prevention and Treatment of Atrial Fibrillation Following Cardiac Surgery”57), viral
illness, alcohol excess, or in association with thyrotoxicosis or
pulmonary embolus has a high likelihood of reversion with
persistence of sinus rhythm if there has been resolution of the
precipitating cause. Successful and sustained reversion to sinus
Cairns et al
Stroke Prevention in Atrial Fibrillation
81
Stroke risk with cardioversion
Atrial flutter
Retrospective studies of patients with atrial flutter undergoing cardioversion suggest that the risk of thromboembolism
may not be importantly different from that for patients with
AF.68,69 Case series note a very low incidence of thromboemboli when patients with atrial flutter are adequately anticoagulated prior to cardioversion.69-71 It is generally recommended
that patients with atrial flutter who are to be cardioverted receive an anticoagulant regimen identical to that for patients
with AF.9,13,17
Emergency cardioversion
Emergency cardioversion may be required because of ischemia
or hemodynamic compromise in some situations and should not
be delayed, even if the AF has been present for more than 48 hours
and the patient is not already anticoagulated. In such a situation,
concomitant anticoagulation with unfractionated heparin (UFH)
or low molecular weight heparin (LMWH) may offer some benefit, but there are no published evaluations. (See accompanying
article titled “Management of Recent-Onset Atrial Fibrillation
and Flutter in the Emergency Department.”70)
EM
BA
R
G
Cardioversion is appropriate for selected patients with AF or
AFL,57,58 necessitating consideration of the possibility of associated thromboembolism. A well-designed prospective cohort
study reported a reduction of postcardioversion systemic embolism of from 5.3% to 0.8% among anticoagulated patients.59 These observations have been supported by several
published case series.13 Two more-recent studies reported remarkably similar incidences of cerebral embolization among
patients receiving OAC in the setting of electrical cardioversion.60,61 It is generally believed that a newly formed thrombus
will become organized and adherent to the left atrial wall
within 2 weeks of formation. Transesophageal echocardiography (TEE) reveals that in the majority of patients, thrombus
resolves, rather than simply becoming firmly adherent to the
wall of the left atrium or left atrial appendage.62 Accordingly, it
is generally recommended that documented systemic anticoagulation at therapeutic levels be instituted at least 3 weeks before
cardioversion.9,13 An analysis that pooled data from 32 studies
found that 98% of thromboembolic events occurred within 10
days of cardioversion of AF or flutter.63 However, evidence
exists that even after successful electrical cardioversion, atrial
contraction may not normalize for weeks when AF has been
present for some time,64,65 and therefore maintenance of anticoagulation for at least 4 weeks after cardioversion seems prudent.9,13 If AF or AFL persists or recurs after attempted cardioversion, or if symptoms suggest that the presenting AF or AFL
has been recurrent, antithrombotic therapy should be continued indefinitely with either aspirin or OAC as appropriate. If
normal sinus rhythm is achieved and sustained for 4 weeks, the
need for ongoing antithrombotic therapy depends on the risk
of stroke, and in difficult cases, the practitioner may require
expert consultative advice. There is no evidence that the incidence of thromboembolism is less with pharmacologic than
with electrical cardioversion,66,67 and accordingly, it is generally recommended that anticoagulant management should not
differ.13 New-onset AF is generally not thought to warrant
anticoagulation if cardioversion is undertaken within 48 hours
of its onset, based on case series showing an incidence of thromboembolism ⬍1%9,13,68,69 without OAC. Even when the duration of the current episode of AF is ⬍48 hours, if the
patient is at particularly high risk of stroke (eg, mechanical
valve, rheumatic heart disease, recent stroke, or TIA), it
would be appropriate to delay cardioversion to allow the
patient to receive OAC for 3 weeks before the procedure and
to continue indefinitely. Following attempted cardioversion, if AF persists or recurs or if symptoms suggest the
presenting AF or AFL has been recurrent, antithrombotic
therapy (OAC or aspirin) should be commenced and continued indefinitely. If normal sinus rhythm is achieved and
sustained, the need for ongoing antithrombotic therapy de-
pends on the risk of stroke. (See accompanying article titled
“Management of Recent-Onset Atrial Fibrillation and Flutter in the Emergency Department.”70)
O
ED
rhythm is associated with relatively young age and freedom
from underlying heart disease. Some patients have intolerable
symptoms and poor exercise tolerance during AF and may prefer attempted rhythm control to rate control. The rate of initial
success in restoring sinus rhythm is high, but in the contemporary Atrial Fibrillation Follow-up Investigation of Rhythm
Management (AFFIRM) trial, vigorous efforts to establish and
sustain sinus rhythm resulted in prevalences of only 82.5%,
73.3%, and 62.6% at 1, 3, and 5 years, respectively.58
RECOMMENDATION
We recommend that hemodynamically stable patients
with AF or AFL of ⱖ48 hours or uncertain duration for
whom electrical or pharmacologic cardioversion is planned
should receive therapeutic OAC therapy (warfarin [INR
2-3] or dabigatran) for 3 weeks before and at least 4 weeks
post-cardioversion.
Following attempted cardioversion,
If AF or AFL persists or recurs or if symptoms suggest
that the presenting AF or AFL has been recurrent, the patient should have antithrombotic therapy continued indefinitely (using either OAC or aspirin, as appropriate).
If sinus rhythm is achieved and sustained for 4 weeks,
the need for ongoing antithrombotic therapy should be determined on the basis of the risk of stroke, and in selected
cases expert consultation may be required (Strong Recommendation, Moderate-Quality Evidence).
We recommend that hemodynamically stable patients
with AF or AFL of known duration 48 hours may undergo
cardioversion without prior or subsequent anticoagulation.
However, if the patient is at particularly high risk of stroke
(eg, mechanical valve, rheumatic heart disease, recent
stroke, or TIA), cardioversion should be delayed, and the
patient should receive OAC for 3 weeks before and at least
4 weeks post-cardioversion.
Following attempted cardioversion,
If AF or AFL persists or recurs or if symptoms suggest
that the presenting AF or AFL has been recurrent, antithrombotic therapy (OAC or aspirin, as appropriate)
should be commenced and continued indefinitely.
If normal sinus rhythm is achieved and sustained for 4
weeks, the need for ongoing antithrombotic therapyshould
82
Canadian Journal of Cardiology
Volume 27 2011
Antithrombotic Strategies for Cardioversion of AF/AFL
Hemodynamically
unstable
Hemodynamically
stable
Urgent electrical
cardioversion
Pharmacological
or electrical
cardioversion
Anthromboc therapy
-In general, no prior or subsequent ancoagulaon is
required.
-If AF/AFL persists or recurs or if AF/AFL has been
recurrent, anthromboc therapy (aspirin or OAC)
should be iniated and connued indefinitely; if NSR is
ongoing, anthromboc therapy according to CHADS2
- early follow-up to review anthromboc strategy,
expert consultaon may be required)
1
Duraon > 48 hours or uncertain
or high-risk paents 1
Rate-control
Therapeuc OAC
for 3 weeks before
cardioversion
TEE-guided cardioversion
(OAC initiated with
heparin bridging)2
Anthromboc therapy
-OAC connued for 4 consecuve weeks.
-If AF/AFL persists or recurs or if AF/AFL has been recurrent,
anthromboc therapy (aspirin or OAC) should be connued
indefinitely; if NSR is ongoing, anthromboc therapy
according to CHADS2
-early follow-up to review anthromboc strategy, expert
O
ED
Known duraon < 48 hours
(and not high-risk paents1)
consultaon may be required
Paents at parcularly high risk of stroke (e.g. mechanical valve INR<2.5, rheumac heart disease, recent stroke/TIA, CHADS 2
≥ 3)
R
G
Figure 6. A summary of our recommended strategies for antithrombotic therapy in conjunction with cardioversion. CHADS2, please see Table 1;
INR, international normalized ratio; NSR, normal sinus rhythm; OAC, oral anticoagulant; TEE, transesophageal echocardiography; TIA, transient
ischemic attack.
EM
BA
be determined on the basis of the risk of stroke according to
CHADS2 score, and in selected cases expert consultation
may be required (Strong Recommendation, ModerateQuality Evidence).
We suggest that hemodynamically unstable patients
with AF or AFL who require emergency cardioversion be
managed as follows:
If the AF or AFL is of known duration 48 hours, the
patient may generally undergo cardioversion without prior anticoagulation. However, if the patient is at particularly high risk
of stroke (eg, mechanical valve, rheumatic heart disease, recent
stroke, or TIA), the patient should receive IV UFH or LMWH
before cardioversion if possible, or immediately thereafter if
even a brief delay is unacceptable, and then be converted to
OAC for at least 4 weeks post-cardioversion.
If the AF or AFL is of ⱖ48 hours or of uncertain
duration, we suggest the patient receive intravenous UFH
or LMWH before cardioversion if possible, or immediately
thereafter if even a brief delay is unacceptable. Such a patient should then be converted to OAC for at least 4 weeks
post-cardioversion.
Following attempted cardioversion, the guidelines for
subsequent antithrombotic therapy are identical to those for
the management of hemodynamically stable patients undergoing cardioversion (Conditional Recommendation, LowQuality Evidence).
Figure 6 is a flow chart outlining our recommendations for
antithrombotic therapy in conjunction with cardioversion.
Transesophageal echocardiography guidance
The potential role of TEE to rule out the presence of atrial
thrombi and the avoidance of anticoagulation was studied in
several case series. An overview of these studies71 reported that
patients with no atrial thrombus who then underwent electrical
cardioversion had an unacceptably high incidence of embolization by comparison with anticoagulated patients in separate
case series. It is generally accepted that the absence of thrombi
on TEE does not eliminate the requirement for a period of 4
weeks of anticoagulation following cardioversion.
The Assessment of Cardioversion Utilizing Echocardiography (ACUTE) was a multicentre randomized prospective of
trial of 1222 patients with AF of more than 2 days’ duration.60
Patients were assigned to therapy guided by TEE findings or to
conventional management. Patients assigned to TEE were anticoagulated at therapeutic levels (typically with UFH intravenously for 24 hours or warfarin [INR ⫽ 2-3] for 5 days) prior
to attempted cardioversion. If TEE showed no thrombus, the
patient underwent cardioversion and continued on anticoagulant therapy for 4 weeks. If thrombus was detected, warfarin
was given for 3 weeks, TEE was repeated, and if the thrombus
had resolved, cardioversion was performed and warfarin continued for 4 weeks. If thrombus was still detected after 3 weeks
of anticoagulation, no cardioversion was attempted, but warfarin was continued for 4 weeks further. The patients randomized to no TEE received warfarin for 3 weeks precardioversion
and a further 4 weeks post-cardioversion. There was no significant difference between the TEE and the no-TEE groups in
the rate of embolic events or prevalence of sinus rhythm. The
TEE group had fewer total hemorrhagic events, most of them
Cairns et al
Stroke Prevention in Atrial Fibrillation
83
RECOMMENDATION
We suggest that hemodynamically stable patients with
AF or AFL of ⱖ48 hours or of unknown duration may
undergo cardioversion guided by TEE (following the protocol from the Assessment of Cardioversion Utilizing Echocardiography trial as detailed in the text) (Conditional Recommendation, High-Quality Evidence).
EM
BA
R
G
Coronary Artery Disease
The clinician managing a patient with AF must often deal
with concomitant coronary artery disease in the settings of
primary prevention, stable coronary artery disease, an acute
coronary syndrome (ACS), or percutaneous coronary intervention (PCI). There is good evidence for the use of aspirin for
primary prevention,74,75 for aspirin or clopidogrel for stable
coronary artery disease,76 for aspirin supplemented by clopidogrel for up to 1 year following an ACS (with or without
PCI77-86) and for PCI (both elective83,84 and post-ACS80).
Warfarin alone or in combination with aspirin is less effective
than aspirin plus clopidogrel for patients post-PCI.81,82 There
is considerable evidence from randomized controlled trials,
that for primary prevention among patients at high risk of
coronary events, low-intensity warfarin (INR 1.5) is as effective as aspirin for the prevention of coronary events,87
and for secondary prevention following myocardial infarction, warfarin alone (INR 2.8-4.8)88 or warfarin (INR
2-2.5) plus aspirin (75-100 mg)89,90 is at least as efficacious
as aspirin alone in reducing subsequent coronary events.91
There has been no rigourous comparison of warfarin vs the
combination of aspirin and clopidogrel.
The benefits of antithrombotic therapies for the primary
prevention of coronary events must be balanced against the
risks of major bleeding attributable to both aspirin and vitamin
K antagonists. Although viewpoints vary, once the annual risk
of a coronary event exceeds 1% to 1.5%, antithrombotic therapy is likely to confer more benefit than harm.75,92 Among
patients with known coronary artery disease, ACS, or recent
PCI, the benefits of appropriate antithrombotic therapy
strongly outweigh the harms. Both aspirin and warfarin are
appropriate for the primary prevention of coronary events in
those patients at higher risk and for secondary prevention in
most patients with known coronary artery disease. Accordingly, when such patients also have AF or AFL, it seems rea-
sonable to choose the most appropriate antithrombotic therapy
for the prevention of stroke with the expectation that the chosen therapy will also be protective against coronary events. For
primary prevention of coronary events and for stable coronary
artery disease, when the risk of stroke is very low (CHADS2 ⫽
0), aspirin would be appropriate because of its lower bleeding
risk and greater ease of administration. When the risk of stroke
is higher (CHADS2 ⱖ1), warfarin would be appropriate, instead of aspirin.
In the setting of elective PCI, aspirin plus clopidogrel are
required for optimal prophylaxis against stent thrombosis. If
the patient also has AF with a risk of stroke that is very low to
low (CHADS2 ⱕ1), then aspirin plus clopidogrel would be
appropriate for a minimum of 1 month for a bare metal stent,
3 months for a sirolimus drug-eluting stent, or 6 months for a
paclitaxel drug-eluting stent; subsequently, CHADS2 ⫽ 0 patients might continue on aspirin alone, and CHADS2 ⫽ 1
patient might stay on aspirin plus clopidogrel or be switched to
warfarin. If the risk of stroke is higher (CHADS2 ⱖ 2), OAC is
required for adequate stroke prophylaxis. Hence, for optimal
prophylaxis against both stroke and coronary events, a period
of therapy with a combination of aspirin, clopidogrel, and
OAC (“triple antithrombotic therapy”) may be required, even
though the risk of bleeding is considerably increased by this
combination.93 Whereas the optimal duration of dual antiplatelet therapy post-PCI for patients without AF is up to 12
months, the duration of triple therapy in patients with AF is
uncertain and should be decided on the basis of balancing the
likely risks of a stent-related event vs the risk of bleeding. Those
patients at particularly high risk of bleeding should be considered for the use of a bare metal stent rather than a drug-eluting
stent, with the triple therapy continued for only 1 month.
Following an episode of ACS, aspirin plus clopidogrel appear optimal for up to 1 year. If the patient also has AF with a
risk of stroke that is very low to low (CHADS2 ⱕ1), then
aspirin plus clopidogrel would be appropriate for up to 1 year;
subsequently, CHADS2 ⫽ 0 patients might continue on aspirin alone, and CHADS2 ⫽ 1 patients might stay on aspirin plus
clopidogrel or be switched to warfarin. If the risk of stroke is
higher (CHADS2 ⱖ2), warfarin is required for adequate stroke
prophylaxis. Hence, for optimal prophylaxis against both
stroke and coronary events, a period of therapy with combination aspirin, clopidogrel, and warfarin may be required, as for
the patients with elective PCI. Whereas the optimal duration of
dual antiplatelet therapy post-ACS for patients without AF is
up to 12 months, the duration of triple therapy in patients with
AF should be decided based on balancing the likely risks of a
stent-related event vs the risk of bleeding. There are no randomized trials to guide the decisions, but it might be reasonable
to prescribe 1 month of triple therapy, followed by up to 1 year
of a combination of warfarin plus clopidogrel or warfarin plus
aspirin, followed by warfarin alone as suggested in other guidelines.91 The issues regarding antithrombotic therapies for patients with coronary artery disease plus AF have been extensively evaluated in recent evidence-based guidelines.9,13,84,86,93
In the RE-LY trial, although the net clinical benefit outcome (a composite of stroke, systemic embolism, pulmonary embolism, myocardial infarction, death, or major
bleeding) was in favour of dabigatran 150 mg (hazard ratio
0.91; 95% CI, 0.82-1.00; P ⫽ .04), there was a higher
incidence of myocardial infarction with dabigatran (hazard
O
ED
minor. Right or left heart thrombi were identified in 13.8% of
patients who underwent TEE. Of those patients with thrombi
detected, 88.2% had a thrombus in the left atrial appendage.
Among those patients with atrial thrombi detected, the value of
repeat TEE after the initial 3 weeks of anticoagulation is uncertain.72 The investigators subsequently reported the results
of a small randomized controlled trial which found no difference in safety outcomes between UFH and enoxaparin for the
acute anticoagulation phase.73 In centres where TEE is readily
available and the interpretations reliable, a TEE-guided management strategy may safely shorten the time to cardioversion
by comparison with standard anticoagulant regimens. The
cost-effectiveness of such an approach depends very much on
local and national patterns of practice and cost structures.
84
Canadian Journal of Cardiology
Volume 27 2011
Anthromboc Management of AF/AFL in CAD
Stable CAD
Recent ACS
PCI
Choose
anthromboc
based on stroke risk
Choose anthromboc
based on balance of risks
and benefits
Choose anthromboc
based on balance of risks
and benefits
CHADS2 = 0
CHADS2 ≥ 1
CHADS2 ≤1
CHADS2 ≥ 2
Aspirin
OAC*
monotherapy
aspirin +
clopidogrel
Triple anthromboc Rx
OAC 2 ≤1
CHADS
aspirin +
clopidogrel
CHADS2 ≥ 2
Triple anthromboc Rx
O
ED
* Warfarin is preferred OAC over dabigatran for paents at high risk of coronary events
Figure 7. A summary of our recommendations for antithrombotic management in settings of coronary artery disease. ACS, acute coronary
syndrome; CAD, coronary artery disease; CHADS2, see Table 1; OAC, oral anticoagulant; PCI, percutaneous coronary intervention.
RECOMMENDATION
We suggest that patients with AF or AFL who have stable
coronary artery disease should receive antithrombotic therapy selected on the basis of their risk of stroke (aspirin for
CHADS2 ⫽ 0 and OAC for CHADS2 ⱖ1). Warfarin is
preferred over dabigatran for those at high risk of coronary
events (Conditional Recommendation, Moderate-Quality
Evidence).
We suggest that patients with AF or AFL who have experienced ACS or who have undergone PCI should receive
EM
BA
R
G
ratio 1.38; 95% CI, 1.00-1.91; P ⫽ .048). There has not yet
been a trial of dabigatran to evaluate the agent for the primary or secondary prevention of coronary events. Given the
known benefits of warfarin for the reduction of coronary
events, which can be substantial in those patients at higher
risk, when OAC is indicated to prevent stroke in those who
have AF and are also at high risk of a coronary event (eg,
those without evidence of coronary artery disease whose
Framingham risk is ⱖ2% per year, those with stable coronary artery disease with high risk features, and those with or
ACS in recent months), it seems prudent to recommend
warfarin in preference to dabigatran.
Paent With AF undergoing Surgical or
Diagnosc Procedure With Major Bleeding Risk
Very Low to Moderate Stroke Risk*
High Stroke Risk**
Low Bleeding Risk
High Bleeding Risk
Low Bleeding Risk
High Bleeding Risk
Connue
anthromboc
(INR < 3 if warfarin)
Stop anthromboc
preprocedure
Reinstute when risk
of bleeding reduced
Connue OAC or
stop OAC and bridge
with UFH or LMWH
perioperavely
Stop OAC and
bridge
with UFH or LMWH
¶
perioperavely
* CHADS2 ≤ 2
* * mechanical valve, recent stroke or TIA, rheumac valve disease, CHADS2 ≥3
¶
stop 12 to 24 hours preprocedure, restart when hemostasis secure and bridge to therapeuc
OAC
Figure 8. A summary of our recommendations for management of antithrombotic therapies in patients undergoing surgical or diagnostic
procedures with a risk of major bleeding. AF, atrial fibrillation; CHADS2, see Table 1; INR, international normalized ratio; LMWH, low molecular
weight heparin; OAC, oral anticoagulant; TIA, transient ischemic attack; UFH, ultrafractionated heparin.
Cairns et al
Stroke Prevention in Atrial Fibrillation
85
Figure 7 is a flow chart outlining our recommendations
for the management of antithrombotic therapy in the setting of coronary artery disease.
EM
BA
R
G
Invasive Procedures
When a patient receiving an OAC or antiplatelet agent is
to undergo a surgical or diagnostic procedure that has a risk
of major bleeding, the risk of a thromboembolic event occurring while the antithrombotic agent is reduced or
stopped must be weighed against the goal of a reduced risk
of major bleeding.94,95 We suggest that such patients be
stratified as to their risk of stroke, which can range from
⬍1% to ⬎20% per year. If there is a very low to moderate
risk of stroke (CHADS2 ⱕ 2), the antithrombotic agent
should be discontinued before the procedure (aspirin or
clopidogrel for 7-10 days, warfarin for 5 days if the INR was
in the range of 2-3, and dabigatran for 2 days). Once postprocedure hemostasis is established (about 24 hours), the
antithrombotic therapy should be reinstated. If the risk of
bleeding from the procedure is low, the clinician might
choose to continue the antithrombotic agent uninterrupted.
On the other hand, if there is a particularly high risk of
stroke (eg, prosthetic valve, recent stroke or TIA, rheumatic
valve disease, CHADS2 ⱖ 3) or of other thromboembolism
(eg, Fontan procedure), some form of antithrombotic therapy should be continued until as close to the time of the
procedure as is judged to be safe in terms of the risk and
consequences of procedural bleeding, and it should be reinstated as soon as hemostasis is established post-procedure.
Consideration should be given to the risk of major bleeding
from the procedure in determining the antithrombotic regimen. It is likely that most potentially hemorrhagic dental
procedures, if undertaken with appropriate surgical skill and
the use of hemostatic mouthwash, can be done without discontinuing warfarin, provided the preoperative INR is under 3.0.96 Cataract extraction and minor dermatologic procedures may also be done without interrupting warfarin.95 A
randomized controlled trial is currently underway by a
group of Canadian investigators who are comparing the
strategies of uninterrupted warfarin vs bridging UFH or
LMWH in the mangement of patients having a cardiac arrhythmia device implanted.97
surgical or diagnostic procedure carrying a risk of major
bleeding be stratified by their risk of stroke:
If there is a very low to moderate risk of stroke (CHADS2
ⱕ2), patients should have their antithrombotic agent discontinued before the procedure (aspirin or clopidogrel for
7-10 days, warfarin for 5 days if the INR was in the range of
2-3, and dabigatran for 2 days). Once postprocedure hemostasis is established (about 24 hours), the antithrombotic
therapy should be reinstated (Conditional Recommendation, Low-Quality Evidence).
If there is a particularly high risk of stroke (eg, mechanical
valve, recent stroke or TIA, rheumatic valve disease,
CHADS2 ⱖ3) or of other thromboembolism (eg, Fontan
procedure), further consideration should be given to the risk
of major bleeding from the procedure:
If there is an acceptable perioperative bleeding risk (ie,
risk of stroke outweighs risk of bleeding), patients should
have OAC therapy continued perioperatively or have their
OAC discontinued before the procedure and be bridged
with LMWH or UFH perioperatively (Conditional Recommendation, Low-Quality Evidence).
If there is a substantial risk of major and potentially
problematic bleeding (ie, risk of bleeding and risk of stroke
are both substantial), patients should have their OAC
discontinued before the procedure, with LMWH or
UFH bridging until 12 to 24 hours preprocedure. Once
postprocedure hemostasis is established (about 24
hours), the OAC should be reinstated with LMWH or
UFH bridging (Conditional Recommendation, LowQuality Evidence).
O
ED
antithrombotic therapy selected on the basis of a balanced
assessment of their risks of stroke, of recurrent coronary
artery events, and of hemorrhage associated with the use of
combinations of antithrombotic therapies, which in patients at higher risk of stroke may include aspirin plus clopidogrel plus OAC (Conditional Recommendation, LowQuality Evidence).
RECOMMENDATION
We suggest that patients with AF or AFL who are receiving aspirin, clopidogrel, or OAC and are scheduled for a
Figure 8 is a flow chart outlining our recommendations for
the management of antithrombotic therapy in patients undergoing invasive procedures.
Stroke Management in Patients With AF
Among AF patients experiencing a stroke, the high rate of
recurrence suggested that there was some urgency in initiating
anticoagulation after the occurrence of embolic stroke. The
International Stroke Trial Collaborative Group randomized
18,451 patients with ischemic stroke within 24 hours of onset
to subcutaneous unfractionated heparin (5000 IU twice a day
or 12,500 IU twice a day), aspirin 300 mg per day, both, or
neither and maintained for 14 days or until prior hospital discharge.24 CT scan was performed to exclude intracranial hemorrhage when possible and was mandatory in comatose patients. Among the 3169 patients with AF, both doses of
heparin were significantly more effective for the prevention of
recurrent stroke of ischemic or unknown type but resulted in
significantly more symptomatic intracranial hemorrhage.
There was no significant difference among the regimens in the
rate of the composite outcome of recurrent stroke or symptomatic intracranial hemorrhage or in the rate of all-cause mortality. Patients with AF had a higher mortality than did patients
without AF (16.9% vs 7.5%), probably because of greater
mean age and larger cerebral infarcts. The rate of recurrence,
within 14 days, of stroke of ischemic or unknown type was
3.9% among patients with AF, considerably lower than that
reported in earlier studies but still higher than in patients with-
86
Canadian Journal of Cardiology
Volume 27 2011
not life threatening and occurs with an INR in the therapeutic range, once pathology is ruled out and if the
CHADS2 score is ⱖ2, it may be appropriate to reinstitute
the OAC, attempting to maintain a therapeutic INR.
RECOMMENDATION
We suggest that patients with AF or AFL who experience
hemorrhage while on OAC therapy be managed according
to the practice guidelines of the American College of Chest
Physicians103 (Conditional Recommendation, Low-Quality Evidence).
O
ED
Pharmacogenomics
Eventually, pharmacogenomic algorithms may allow more
rapid and safe determinations of initial warfarin dosage, particularly among patients whose warfarin requirements are particularly
low or high.104 For the present, routine genetic testing is not advised in the management of therapy with a vitamin K antagonist.
Alternatives to Antithrombotic Therapies
Rhythm control and stroke risk
An overview105 of the 5 trials that compared the strategies of rhythm vs rate control in AF found a mortality of
13.0% with rate control vs 14.6% with rhythm control
(odds ratio 0.87, P ⫽ .09). The rates of ischemic stroke and
major hemorrhage were similar. The AFFIRM trial58 is by
far the largest, mandated anticoagulation (INR 2.0-3.0) in
the rate-control group (85% maintained warfarin) and
strongly encouraged in the rhythm-control group, while allowing cessation at the physician’s discretion if sustained
sinus rhythm was achieved (70% maintained warfarin).
Ischemic stroke occurred at an annual rate of about 1% in each
group, and in most instances the patient was either off warfarin
or the INR was ⬍2.0. The authors concluded that continuous
anticoagulation is warranted in all patients with AF and 1 or
more risk factors for stroke, whether or not sinus rhythm appears to be restored and maintained, and this approach is recommended by consensus groups.9,13
Left atrial radiofrequency ablation is increasingly used as a
rhythm control approach to treat AF, raising questions about
the role of long-term OAC therapy in such patients.106 The
issues are the risk of dislodgement of left atrium thrombus
during the ablation procedure, bleeding in association with the
invasive procedure, creation of thrombogenic areas of left
atrium endothelial damage, and the risk of embolization during long-term follow-up. Recommendations are generally weak
and based on evidence of low or very low quality.106 TEE is
advised immediately preprocedure to ensure there is no important left atrium thrombus. In general, the procedure is performed with the patient adequately anticoagulated, either by
sustaining the preprocedure warfarin (usually allowing the
INR to fall to the lower end of the therapeutic range) or with
use of bridging LMWH both before and after the procedure. In
the latter case, UFH is given with access to the left atrium. The
UFH or LMWH are discontinued at the completion of the
procedure, and the sheath is removed when the ACT returns to
RECOMMENDATION
BA
R
G
out AF in this study. The results indicate that heparin is not
indicated in the acute management of embolic stroke among
patients with AF. Published guidelines for the management of
stroke in a patient with AF98-100 are based on extrapolations
from clinical trials97,101 and include recommendations for the
use of intravenous rtPA for selected patients within 3 hours of
onset. Patients who receive rtPA should not receive any antiplatelet or anticoagulant therapy for at least 24 hours subsequently. If there is no evidence of hemorrhage on urgent CT
scan, and yet the patient is not to receive fibrinolytic therapy,
the patient should begin aspirin 325 mg per day immediately
thereafter, with conversion to OAC after 14 days, or sooner if
the infarct size is small and the patient is normotensive. If the
clinical and computed tomography picture are consistent with
a TIA, then immediate heparin therapy may be acceptable. If
stroke occurs in a patient with AF or AFL who is already receiving anticoagulation, the drug should be stopped and intracranial hemorrhage should be excluded. If intracranial hemorrhage is present, the anticoagulation should be reversed, and
subsequent decisions to resume anticoagulation should be
made after reassessment of the risks of embolism and the risks
of recurrent intracranial hemorrhage. For those without intracranial hemorrhage, it would be reasonable to start aspirin 325
mg per day when the INR falls below 1.5 and to restart the
anticoagulant at day 14, or sooner if the infarct is small and the
patient is normotensive.98,99 If warfarin is chosen as the anticoagulant, meticulous attention should be given to maintenance of the INR in the range of 2 to 3. A double-blind randomized trial102 of LMWH vs aspirin (160 mg/d) among
patients with acute ischemic stroke and AF showed a trend to
more recurrent ischemic stroke in the LMWH group (odds
ratio 1.13; 95% CI, 0.57-2.24), supporting the strategy of early
administration of aspirin to such patients in preference to heparin.
EM
We recommend that patients with AF or AFL who experience a stroke be managed acutely according to the published guidelines of the American Heart and American
Stroke Associations100 (Strong Recommendation, Moderate-Quality Evidence).
Hemorrhage on OAC Therapy
The major determinants of OAC-induced bleeding are
the INR, patient characteristics, and the concomitant use of
drugs that interfere with hemostasis. The acute management
of hemorrhage in a patient receiving OAC requires a graded
response according to published guidelines,103 beginning
with the immediate measurement of the INR, stopping the
OAC, and assessment of the severity of hemorrhage. If there
is major bleeding, vitamin K may be given intravenously,
and if the bleeding is life threatening, vitamin K should be
accompanied by fresh frozen plasma, prothrombin complex
concentrate, or recombinant factor VIIa. If the INR is elevated and no explanatory pathology is found, it may be
appropriate to restart the OAC, attempting to maintain the
INR in the usual therapeutic range with intensified monitoring and attention to patient factors that can increase the
INR in the setting of a given dose of OAC. If the bleeding is
Cairns et al
Stroke Prevention in Atrial Fibrillation
87
Left atrial appendage-directed interventions
5. Petersen P, Boysen G. Letter to editor. N Engl J Med 1990; 323:482.
6. Stroke Prevention in Atrial Fibrillation Investigators. Stroke Prevention
in Atrial Fibrillation study: final results. Circulation 1991;84:527-39.
7. Atrial Fibrillation Investigators. Risk factors for stroke and efficiency of
antithrombotic therapy in atrial fibrillation: analysis of pooled data from
five randomized controlled trials. Arch Intern Med 1994;154:1449-57.
8. Wolf PA, Dawber TR, Thomas E Jr, et al. Epidemiologic assessment of
chronic atrial fibrillation and risk of stroke: the Framingham Study.
Neurology 1978;28:973-7.
9. Singer DE, Albers GW, Dalen JE, et al. Antithrombotic therapy in atrial
fibrillation. Chest 2008;133:546S-92S.
10. The Stroke Risk in Atrial Fibrillation Working Group. Independent
predictors of stroke in patients with atrial fibrillation: a systematic review.
Neurology 2007;69:546-54.
11. Stroke Prevention in Atrial Fibrillation Investigation. Prevention of
thromboembolism in atrial fibrillation: I. Clinical features of patients at
risk. Ann Intern Med 1992;116:1-5.
12. Stroke Prevention in Atrial Fibrillation Investigation. Prevention of
thromboembolism in atrial fibrillation: II. Echocardiographic features of
patients at risk. Ann Intern Med 1992;116:6-12.
13. Fuster V, Rydén LE, Cannon AS, et al. ACC/AHA/ESC guidelines for
the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on
Practice Guidelines and the European Society of Cardiology Committee
for Practice Guidelines. Circulation 2006;114:257-354.
EM
BA
R
G
A range of surgical procedures focused on curing AF have been
developed and reported during the past 20 years.107 Left atrial
appendage removal or occlusion may be done in an attempt to
lower the risk of thromboembolism as part of a Cox Maze procedure or as an adjunct to another cardiac surgical procedure. Only
case series are available in the literature, with levels of success very
specific to individual centres and the indications uncertain. The
long-term risk of stroke after such procedures appears to be low,
but the requirement for long-term OAC is unclear, and advice
should be provided by the expert centre conducting the arrhythmia surgery. A Canadian collaborative group is currently conducting a pilot study evaluating left atrial appendage occlusion in conjunction with various cardiac surgical procedures
(clinicaltrials.gov, NCT00908700). (See detailed discussion in the accompanying article titled “Surgical Therapy
for Atrial Fibrillation.”108)
Percutaneous closure of the left atrial appendage was evaluated in a randomized, noninferiority comparison of conventional warfarin vs the Watchman occluding device and subsequent discontinuation of warfarin.109 The composite primary
outcome (any stroke, cardiovascular or unexplained death, or
systemic embolism) at a mean of 18 months was nonsignificantly less in the Watchman group (RR ⫽ 0.62; 95% CI,
0.35-1.25), and the device was concluded to be noninferior to
conventional warfarin therapy. However, there were relatively
few events, the follow-up was short, there are substantial learning
curve considerations, and the antithrombotic regimen used with
the device was complex and changing. Additional, adequately
powered studies, particularly in patients at higher risk of stroke, are
needed for adequate assessment of this new technique.
4. Petersen P, Boysen G, Godtfredsen J, et al. Placebo-controlled, randomised trial of warfarin and aspirin for prevention of thromboembolic
complications in chronic atrial fibrillation: the Copenhagen AFASAK
study. Lancet 1989;i:175-9.
O
ED
a safe level. Parenteral anticoagulation is reinitiated within
hours of the sheath removal and maintained until therapeutic
anticoagulation is reestablished with warfarin or dabigatran,
which is continued for at least 3 months. Long-term OAC
should continue if AF recurs. In the presence of sustained normal sinus rhythm, OAC should be discontinued only if the
long-term risk of stroke is low (CHADS2 score ⬍2). (See further details in the accompanying article titled “Catheter Ablation of Atrial Fibrillation and Flutter.”106)
14. Gage BF, Waterman AD, Shannon W, et al. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA 2001;285:2864-70.
15. Gage BF, van Walraven C, Pearce L, et al. Selecting patients with atrial
fibrillation for anticoagulation: stroke risk stratification in patients taking
aspirin. Circulation 2004;110:2287-92.
16. Stroke Risk in Atrial Fibrillation Working Group. Comparison of 12 risk
stratification schemes to predict stroke in patients with nonvalvular atrial
fibrillation. Stroke 2008;39:1901-10.
Acknowledgements
The authors are grateful to Grant Stotts, MD, FRCPC, for
advice and liaison with the Canadian Stroke Network and to
Marie-Josee Martin and Jody McCombe for final transcription
of the manuscript. Administrative and technical support was
provided by the Canadian Cardiovascular Society.
17. Camm AJ, Kirchof P, Lip GYH, et al. Task Force for the Management of Atrial Fibrillation of the European Society of Cardiology
(ESC). Guidelines for the management of atrial fibrillation. Eur
Heart J 2010;31:2369-429. Available at http://www.escardio.org/
guidelines-surveys/esc-guidelines/GuidelinesDocuments/guidelinesafib-FT.pdf. Accessed December 15, 2010.
References
18. Lip GYH, Nieuwlaat R, Pisters R, Lane DR, Crijns HJGM. Refining
clinical risk stratification for predicting stroke and thromboembolism in
atrial fibrillation using a novel risk factor-based approach: the Euro Heart
Survey on Atrial Fibrillation. Chest 2010;137:263-72.
1. Boston Area Anticoagulation Trial of Atrial Fibrillation Investigators.
The effect of low-dose warfarin on the risk of stroke in patients with
nonrheumatic atrial fibrillation. N Engl J Med 1990;323:1505-11.
2. Connolly SJ, Laupacis A, Gent M, et al; for CAFA Study Coinvestigators. Canadian Atrial Fibrillation Anticoagulation (CAFA) study. J Am
Coll Cardiol 1991;18:349-55.
3. Ezekowitz MD, Bridgers SL, James KE, et al. Warfarin in the prevention
of stroke associated with nonrheumatic atrial fibrillation. N Engl J Med
1992;327:406-12.
19. Hohnloser SH, Pajitnev D, Pogue J, et al. Incidence of stroke in paroxysmal versus sustained atrial fibrillation in patients taking oral anticaogulation or combined antiplatelet therapy: an ACTIVE W substudy. J Am
Coll Cardiol 2007;50:2156-61.
20. Hart RG, Pearce LA, Rothbart RM, et al. for Stroke Prevention in Atrial
Fibrillation Investigators. Stroke with intermittent atrial fibrillation: incidence and predictors during aspirin therapy. J Am Coll Cardiol 2000;
35:183-7.
88
Canadian Journal of Cardiology
Volume 27 2011
21. Petersen P, Godtfredsen J. Embolic complications in paroxysmal atrial
fibrillation. Stroke 1986;17:622-6.
brillation: a randomised, open-label, non-inferiority trial. Lancet
2008;371:315-21.
22. Wolf PA, Kannel WB, McGee DL, et al. Duration of atrial fibrillation
and eminence of stroke: the Framingham Study. Stroke 1983;14:664-7.
39. A phase III study of apixaban in patients with atrial fibrillation
(AVERROES). ClinicalTrials.gov identifier: NCT00496769. Available
at: http://clinicaltrials.gov/ct2/show/NCT00496769. Accessed December 15, 2010.
24. Saxena R, Lewis S, Berge E, Sandercock PAG, Koustaal PJ; for International Stroke Trial Collaborative Group. Risk of early death and recurrent stroke and effect of heparin in 3169 patients with acute ischemic
stroke and atrial fibrillation in the International Stroke Trial. Stroke
2001;32:2333-7.
25. Biblo LA, Yuan Z, Quan KJ, Mackall JA, Rimm AA. Risk of stroke in
patients with atrial flutter. Am J Cardiol 2001;87:346-9.
26. Hart RG, Pearce LA, Aguilare MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation.
Ann Intern Med 2007;146:857-67.
27. Hart RG, Pearce LA, Aguilar MI. Adjusted-dose warfarin versus aspirin
for preventing stroke in patients with atrial fibrillation. Ann Intern Med
2007;147:590-2.
28. Stroke Prevention in Atrial Fibrillation Investigators. Warfarin versus
aspirin for prevention of thromboembolism in atrial fibrillation: Stroke
Prevention in Atrial Fibrillation II Study. Lancet 1994;343:687-91.
41. Randomized, double-blind study comparing once daily oral rivaroxaban with adjusted-dose oral warfarin for the prevention of stroke in
subjects with non-valvular atrial fibrillation. ClinicalTrials.gov identifier: NCT00403767. Available at: http://clinicaltrials.gov/ct2/show/
NCT00403767. Accessed December 15, 2010.
42. Hylek EM, Go AS, Chang Y, et al. Effect of intensity of oral anticoagulation on stroke severity and mortality in atrial fibrillation. N Engl J Med
2003;349:1019-26.
43. Oake N, Fergusson DA, Forster AJ, van Walraven C. Frequency of
adverse events in patients with poor anticoagulation: a meta-analysis.
Can Med Assoc J 2007;176:1589-94.
44. European Atrial Fibrillation Trial Study Group. Optimal oral anticoagulant therapy in patients with nonrheumatic atrial fibrillation and recent
cerebral ischemia. N Engl J Med 1995;333:5-10.
45. Gage BF, Yan Y, Milligan PE, et al. Clinical classification schemes for
predicting hemorrhage: results from the National Registry of Atrial Fibrillation (NRAF). Am Heart J 2006;151:713-9.
R
G
29. Gullov AL, Koefoed BG, Petersen P, et al. Fixed minidose warfarin and
aspirin alone and in combination vs. adjusted-dose warfarin for stroke
prevention in atrial fibrillation: Second Copenhagen Atrial Fibrillation,
Aspirin, and Anticoagulation Study. Arch Intern Med 1998;158:151321.
40. Apixaban for the prevention of stroke in subjects with atrial fibrillation
(ARISTOTLE). ClinicalTrials.gov identifier: NCT00412984. Available
at: http://clinicaltrials.gov/ct2/show/NCT00412984. Accessed December 15, 2010.
O
ED
23. EAFT (European Atrial Fibrillation Trial) Study Group. Secondary prevention in non-rheumatic atrial fibrillation after transient ischemic attack or minor stroke. Lancet 1993;342:1255-62.
BA
30. Pengo V, Zasso A, Barbero F, et al. Effectiveness of fixed minidose warfarin in the prevention of thromboembolism and vascular death in nonrheumatic atrial fibrillation. Am J Cardiol 1998;82:433-7.
EM
31. Hellemons BS, Langenberg M, Lodder J, et al. Primary prevention of
arterial thromboembolism in non-rheumatic atrial fibrillation in primary
care: randomized controlled trial comparing two intensities of coumarin
with aspirin. BMJ 1999;319:958-64.
32. ACTIVE Writing Group of the ACTIVE Investigators, Connolly S,
Pogue J, Hart R, et al. Clopidogrel plus aspirin versus oral anticoagulation for atrial fibrillation in the Atrial fibrillation Clopidogrel Trial with
Irbesartan for prevention of Vascular Events (ACTIVE W): a randomized controlled trial. Lancet 2006;367:1903-12.
33. ACTIVE Investigators. Effect of clopidogrel added to aspirin in patients
with atrial fibrillation. N Engl J Med 2009;360:2066-78.
34. Executive Steering Committee on behalf of the SPORTIF III Investigators. Stroke prevention with the oral direct thrombin inhibitor ximelagatran compared with warfarin for the prevention of thromboembolism
in patients with nonvalvular atrial fibrillation (SPORTIF III); a randomized trial. Lancet 2003;362:1691-98.
35. SPORTIF Executive Steering Committee for the SPORTIF V Investigators. Ximelagatran vs. warfarin for stroke prevention in patients with nonvalvular atrial fibrillation: a randomized trial. JAMA 2005;293:690-8.
36. Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin
in patients with atrial fibrillation. N Engl J Med 2009;361:1139-51.
37. Ezekowitz MD, Reilly PA, Nehmiz G, et al. Dabigatran with or without
concomitant aspirin compared with warfarin alone in patients with nonvalvular atrial fibrillation (PETRO Study). Am J Cardiol 2007;100:1419-26.
38. Amadeus Investigators. Comparison of idraparinux with vitamin K antagonists for prevention of thromboembolism in patients with atrial fi-
46. Pisters R, Lane DA, Nieuwlaat R, et al. A novel user-friendly score
(HAS-BLED) to assess 1-year risk of major bleeding in patients with
atrial fibrillation: the Euro Heart Survey. Chest 2010;138:1093-100.
47. Waldo AL, Becker RC, Tapson VF, Colgan KJ. Hospitalized patients
with atrial fibrillation and a high risk of stroke are not being provided
with adequate anticoagulation. J Am Coll Cardiol 2005;46:1729-36.
48. Rowan SB, Bailey DN, Bublitz CE, Anderson RJ. Trends in anticoagulation for atrial fibrillation in the U.S.: an analysis of the national ambulatory medical care survey database. J Am Coll Cardiol 2007;49:1561-5.
49. Glazer NL, Dublin S, Smith NL, et al. Newly detected atrial fibrillation
and compliance with antithrombotic guidelines. Arch Intern Med 2007;
167:246-52.
50. Simpson SR, Wilson C, Hannaford PC, Williams D. Evidence for age
and sex differences in the secondary prevention of stroke in Scottish
primary care. Stroke 2005;36:1771-5.
51. Hylek EM, D’Antonio J, Evans-Molina C, et al. Translating the results
of randomized trials into clinical practice: the challenge of warfarin candidacy among hospitalized elderly patients with atrial fibrillation. Stroke
2006;37:1075-80.
52. Nieuwlaat R, Capucci A, Lip GYH, et al. Antithrombotic treatment in
real-life atrial fibrillation patients: a report from the Euro Heart Survey
on Atrial Fibrillation. Eur Heart J 2006;27:3018-26.
53. Hylek EM, Evans-Molina C, Shea C, Henault LE, Regan S. Major
hemorrhage and tolerability of warfarin in the first year of therapy
among elderly patients with atrial fibrillation. Circulation 2007;115:
2689-96.
54. Mant J, Hobbs R, Roalfe A, et al; BAFTA investigators. Warfarin versus
aspirin for stroke prevention in an elderly community population with
atrial fibrillation (the Birmingham Atrial Fibrillation Treatment of the
Cairns et al
Stroke Prevention in Atrial Fibrillation
89
55. Poli D, Antonucci E, Grifoni E, et al. Bleeding risk during oral anticoagulation in patients older than 80 years. J Am Coll Cardiol 2009;54:
999-1002.
56. Wyse DG. Bleeding while starting anticoagulation for thromboembolism prophylaxis in elderly patients with atrial fibrillation. Circulation
2007;115:2684-6.
57. Mitchell LB, CCS Atrial Fibrillation Guidelines Committee. Canadian
Cardiovascular Society Atrial Fibrillation Guidelines 2010: prevention
and treatment of atrial fibrillation following cardiac surgery. Can J Cardiol 2011;27:91-7.
58. Wyse DG, Waldo AL, DiMarco JP, et al. A comparison of rate control
and rhythm control in patients with atrial fibrillation. N Engl J Med
2002;347:1825-33.
59. Bjerkelund CJ, Orning OM. The efficacy of anticoagulant therapy in
preventing embolism related to DC electrical conversion of atrial fibrillation. Am J Cardiol 1969;23:208.
60. Klein AL, Grimm RA, Murray RD, et al. Use of transesophageal echocardiography to guide cardioversion in patients with atrial fibrillation.
N Engl J Med 2001;344:1411-20.
72. Moreyra E, Finkelhor RS, Debul RD. Limitations of transesophageal
echocardiography in the risk assessment of patients before nonanticoagulated cardioversion from atrial fibrillation and flutter: an analysis of
pooled trials. Am Heart J 1995;129:71-5.
73. Klein AL, Jasper SE, Katz JF, et al. The use of enoxaparin compared to
unfractionated heparin for short-term antithrombotic therapy in atrial
fibrillation patients undergoing transoesophageal echocardiographyguided cardioversion: Assessment of Cardioversion Using Transoesophageal Echocardiography (ACUTE) II randomized multicentre study. Eur
Heart J 2006;27:2858-65.
74. Berger JS, Roncaglioni MC, Avanzini F, et al. Aspirin for the primary
prevention of cardiovascular events in women and men: a sex-specific
meta-analysis of randomized controlled trials. JAMA 2006;295:306-13.
75. Sanmuganathan PS, Ghaharamani P, Jackson PR, et al. Aspirin for the
primary prevention of coronary heart disease: safety and absolute benefit
related to coronary risk derived from meta-analysis of randomised trials.
Heart 2001;85:265-71.
76. CAPRIE Steering Committee. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE).
Lancet 1996;348:1329-39.
77. Yusuf S, Zhao F, Mehta S, et al. Effects of clopidogrel in addition to
aspirin in patients with acute coronary syndromes without ST-segment
elevation. N Engl J Med 2001;345:494-502.
R
G
61. Seidel K, Ramekaen M, Drogemuller A, et al. Embolic events in patients
with atrial fibrillation and effective anticoagulation: value of transesophageal echocardiography to guide direct-current cardioversion: final results of the Ludwigschafen Observational Cardioversion Study. J Am
Coll Cardiol 2002;39:1436-42.
71. Elhendy A, Gentile F, Khandheria BK, et al. Thromboembolic complications after electrical cardioversion in patients with atrial flutter. Am J
Med 2001;111:433-8.
O
ED
Aged Study, BAFTA): a randomized controlled trial. Lancet
2007;370:493-503.
62. Collins LJ, Silverman DI, Douglas PS, Manning WJ. Cardioversion of
nonrheumatic atrial fibrillation: reduced thromboembolic complications
with 4 weeks of precardioversion anticoagulation are related to atrial
thrombus resolution. Circulation 1995;92:160-3.
BA
63. Berger M, Schweitzer P. Timing of thromboembolic events after electrical cardioversion of atrial fibrillation or flutter: a retrospective analysis.
Am J Cardiol 1998;82:1545-7, A8.
EM
64. Manning WJ, Silverman DI, Keightly CS, et al. Transesophageal echocardiographically facilitated early cardioversion from atrial fibrillation
using short-term anticoagulation: final results of a prospective 4.5 year
study. J Am Coll Cardiol 1995;25:1354-61.
65. Padraig GO, Puleo PR, Bolli R, et al. Return of atrial mechanical function following electrical cardioversion of atrial dysrhythmias. Am Heart J
1990;120:353-9.
66. Lown B. Electrical reversion of cardiac arrhythmias. Br Heart J 1967;29:
469-89.
67. Goldman M. The management of chronic atrial fibrillation: indications
and method of conversion to sinus rhythm. Prof Cardiovasc Dis 1959;
2:465-79.
68. Weigner MJ, Caulfield TA, Danias PG, et al. Risk for clinical thromboembolism associated with conversion to sinus rhythm in patients with
atrial fibrillation lasting less than 48 hours. Ann Int Med 1997;126:
741-5.
69. Gallagher MM, Hennessy BJ, Edvardsson N, et al. Embolic complications of direct current cardioversion of atrial arrhythmias: association
with low intensity of anticoagulation at the time of cardioversion. J Am
Coll Cardiol 2002;40:926-33.
70. Stiell IG, Macle L, CCS Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: management of recent-onset atrial fibrillation and flutter in the emergency
department. Can J Cardiol 2011;27:38-46.
78. Sabatine MS, Cannon CP, Gibson CM, et al. Addition of clopidogrel to
aspirin and fibrinolytic therapy for myocardial infarction with ST-segment elevation. N Engl J Med 2005;352:1179-89.
79. Chen ZM, Jiang LX, Chen YP, et al. Addition of clopidogrel to aspirin in
45,852 patients with acute myocardial infarction: randomised placebocontrolled trial. Lancet 2005;366:1607-21.
80. Mehta SR, Yusuf S, Peters RJ, et al. Effects of pretreatment with clopidogrel and aspirin followed by long-tern therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet
2001;358:527-33.
81. Rubboli A, Milandri M, Castelvetri C, et al. Meta-analysis of trials comparing oral anticoagulation and aspirin versus dual antiplatelet therapy
after coronary stenting: clues for the management of patients with an
indication for long-term anticoagulation undergoing coronary stenting.
Cardiology 2005;104:101-6.
82. Leon MB, Baim DS, Popma JJ, et al. A clinical trial comparing three
antithrombotic-drug regimens after coronary stenting. N Engl J Med
1998;339:1665-71.
83. Bertrand ME, Rupprecht HJ, Urban P, Gershlick AH. Double-blind study
of the safety of clopidogrel with and without a loading dose in combination
with aspirin compared with ticlopidine in combination with aspirin after
coronary stenting: the clopidogrel aspirin stent international cooperative
study (CLASSICS). Circulation 2000;102:624-9.
84. Steinhubl SR, Berger PB, Mann JT, et al. Early and sustained dual antiplatelet therapy following percutaneous coronary intervention: a randomized controlled trial. JAMA 2002;288:2411-20.
85. Becker RC, Meade TW, Berger PB, et al. The primary and secondary
prevention of coronary artery disease. Chest 2008;133:776S-814S.
86. King SB, Smith SC, Hirshfeld JW, et al. 2007 focused update of the
ACC/AHA/SCAI guideline update for percutaneous coronary intervention. Circulation 2008;117:261-95.
90
Canadian Journal of Cardiology
Volume 27 2011
87. Medical Research Council’s General Practice Research Framework.
Thrombosis prevention trial: randomised trial of low-intensity oral anticoagulation with warfarin and low-dose aspirin in the primary prevention of ischaemic heart disease in men at increased risk. Lancet 1998;
351:233-41.
88. Smith P, Arneson H, Holme I. The effect of warfarin on mortality and
reinfection after myocardial infarction. N Engl J Med 1990;323:499-503.
89. Hurlen N, Abdelnoor M, Smith P, et al. Warfarin, aspirin or both after
myocardial infarction. N Engl J Med 2002;347:969-74.
90. Fiore LD, Ezekowitz MD, Brophy MT, et al. Department of Veterans
Affairs Cooperative Studies Program Clinical Trial comparing combined
warfarin and aspirin with aspirin alone in survivors of myocardial infarction:
primary results of the CHAMP study. Circulation 2002:105:557-63.
91. Anand SS, Yusuf S. Oral anticoagulants in patients with coronary artery
disease. J Am Coll Cardiol 2003;41:62S-9S.
100. Adams HP, del Zoppo G, Alberts MJ, et al. Guidelines for the early
management of adults with ischemic stroke. Stroke 2007;38:1655711.
101. Chen ZM, Sandercock P, Pan HC, et al. Indications for early aspirin
use in acute ischemic stroke: a combined analysis of 40,000 randomized patients from the Chinese Acute Stroke Trial and the International Stroke Trial: indications for early aspirin. Stroke 2000;31:
1240-9.
102. Berge E, Abdelnoor M, Nakstad PH, Sandset PM; on behalf of HAEST
Study Group. Low molecular-weight heparin versus aspirin in patients
with acute ischaemic stroke and atrial fibrillation: a double-blind randomised study. Lancet 2000;355:1205-10.
103. Schulman S, Beyth RJ, Kearon C, Levine MN. Hemorrhagic complications of anticoagulant and thrombolytic treatment. Chest 2008;133:
257S-98S.
104. International Warfarin Pharmacogenetics Consortium. Estimation of
the warfarin dose with clinical and pharmacogenetic data. N Engl J Med
2009;360:753-64.
93. Lip GYH, Huber K, Andreotti F, et al. Management of antithrombotic
therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous coronary intervention/stenting.
Throm Haemost 2010;103:13-28.
105. de Denus S, Sanoski CA, Carlsson J, Opolski G, Spinler SA. Rate vs.
rhythm control in patients with atrial fibrillation: a meta-analysis. Arch
Int Med 2005;165:258-62.
94. Kearon C, Hirsh J. Management of anticoagulation before and after
elective surgery. N Engl J Med 1997;336:1506-11.
106. Verma A, Macle L, Cox JL, Skanes AC, CCS Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society Atrial Fibrillation
Guidelines 2010: catheter ablation for atrial fibrillation/atrial flutter.
Can J Cardiol 2011;27:60-6.
107. Calkins H, Brugada J, Packer D, et al. HRS/EHRA/ECAS expert consensus statement on catheter and surgical ablation of atrial fibrillation:
recommendation for personnel, policy, procedures and follow-up. Europace 2007;9:335-79.
R
G
95. Douketis JD, Berger PB, Dunn AS, et al. The perioperative management
of antithrombotic therapy. Chest 2008;133:299S-339S.
O
ED
92. Becker RC, Meade TW, Berger PB, et al. The primary and secondary
prevention of coronary artery disease. Chest 2008;133:776S-814S.
96. Patatanian E, Fugate SE. Hemostatic mouthwashes in anticoagulated patients
undergoing dental extraction. Ann Pharmacotherapy 2006;40:2205-10.
BA
97. Birnie D, Healey JS, Krahn A, et al. Bridge or continue Coumadin for
device surgery: a randomized controlled trial rationale and design. Curr
Opin Cardiol 2008;24:82-7.
98. Albers GW, Amarenco P, Easton JD, Sacco RL, Teal P. Antithrombotic and
thrombolytic therapy for ischemic stroke. Chest 2008;133:630S-69S.
EM
99. Broderick J, Connolly S, Feldman E, et al. Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update.
Stroke 2007;38:2001-23.
108. Pagé P, CCS Atrial Fibrillation Guidelines Committee. Canadian Cardiovascular Society Atrial Fibrillation Guidelines 2010: surgical therapy.
Can J Cardiol 2011;27:67-73.
109. Holmes DR, Reddy V, Turi ZG, et al. Percutaneous closure of the left
atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: a randomized non-inferiority trial. Lancet
2009;374:534-42.
Canadian Journal of Cardiology 27 (2011) 91–97
Society Guidelines
Canadian Cardiovascular Society Atrial Fibrillation
Guidelines 2010: Prevention and Treatment of Atrial
Fibrillation Following Cardiac Surgery
L. Brent Mitchell, MD, FRCPC,a and the CCS Atrial Fibrillation Guidelines Committeeb
Libin Cardiovascular Institute of Alberta, Alberta Health Services and University of Calgary, Foothills Hospital, Calgary, Alberta, Canada
b
For a complete listing of committee members, see Gillis AM, Skanes AC. Canadian Cardiovascular Society Atrial Fibrillation Guidelines
2010: Implementing GRADE and achieving consensus. Can J Cardiol 2011;27:27-30.
RÉSUMÉ
Postoperative atrial fibrillation and atrial flutter (POAF) are the most
common complications of cardiac surgery that require intervention or
prolong intensive care unit and total hospital stay. For some patients,
these tachyarrhythmias have important consequences including patient discomfort/anxiety, hemodynamic deterioration, cognitive impairment, thromboembolic events including stroke, exposure to the
risks of antiarrhythmic treatments, longer hospital stay, and increased
health care costs. We conclude that prevention of POAF is a worthwhile exercise and recommend that the dominant therapy for this
purpose be -blocker therapy, especially the continuation of -blocker
therapy that is already in place. When -blocker therapy is contraindicated, amiodarone prophylaxis is recommended. If both of these therapies are contraindicated, therapy with either intravenous magnesium
or biatrial pacing is suggested. Patients at high risk of POAF may be
considered for first-line amiodarone therapy, first-line sotalol therapy,
or combination prophylactic therapy. The treatment of POAF may follow either a rate-control approach (with the dominant therapy being
-blocking drugs) or a rhythm-control approach. Anticoagulation
should be considered if persistent POAF lasts ⬎72 hours and at the
La fibrillation auriculaire (FA) et le flutter auriculaire postopératoires
sont les complications les plus courantes de la chirurgie cardiaque qui
nécessitent une intervention et prolonge la durée de séjour de l’unité
des soins intensifs ou hospitalier. Chez certains patients, ces tachyarythmies ont des conséquences importantes, citons entre autres
l’inconfort et l’anxiété, la détérioration hémodynamique, les troubles
cognitifs, les thromboembolies, l’accident vasculaire cérébral,
l’exposition aux effets secondaires des traitements antiarythmiques,
le séjour prolongé à l’hôpital et les coûts additionnels. Nous concluons
que la prévention de la FA postopératoire est un exercice qui en vaut
la peine et recommandons que le but premier du traitement soit le
traitement par -bloquant, particulièrement la continuation des -bloquants déjà administrés en préopératoire. Lorsque le traitement par
-bloquants est contre-indiqué, on recommande l’amiodarone en prophylaxie. Si ces deux traitements sont contre-indiqués, on suggère le
traitement soit à l’aide de magnésium intraveineux ou la stimulation
biauriculaire. Les patients à haut risque de FA postopératoire peuvent
être considérés pour le traitement de première intention à l’amiodarone,
le traitement de première ligne par sotalol ou la combinaison de
Incidence of Postoperative Atrial
Tachyarrhythmias
Given that atrial fibrillation (AF) and atrial flutter are facilitated by atrial trauma, atrial stretch, atrial ischemia, epicardial inflammation, hypoxia, acidosis, electrolyte disturbances, and the
refractoriness changes that accompany sympathetic nervous sys-
tem discharge and given that all of these factors are frequently
present immediately after cardiac surgical procedures, it is not
surprising that AF and atrial flutter are frequent complications of
these procedures. Indeed, atrial tachyarrhythmias are the most
common postoperative complications of cardiac surgery that require intervention or prolonged intensive care unit and total hos-
Received for publication November 11, 2010. Accepted November 12,
2010.
consensus of a Canadian panel comprised of multidisciplinary experts on this topic
with a mandate to formulate disease-specific recommendations. These recommendations are aimed to provide a reasonable and practical approach to care for specialists and allied health professionals obliged with the duty of bestowing optimal
care to patients and families, and can be subject to change as scientific knowledge
and technology advance and as practice patterns evolve. The statement is not
intended to be a substitute for physicians using their individual judgment in managing clinical care in consultation with the patient, with appropriate regard to all
the individual circumstances of the patient, diagnostic and treatment options available and available resources. Adherence to these recommendations will not necessarily produce successful outcomes in every case.
EM
R
G
BA
ABSTRACT
O
ED
a
Corresponding author: L. Brent Mitchell, MD, FRCPC, Libin Cardiovascular Institute of Alberta, Alberta Health Services and University of Calgary,
Foothills Hospital, 1403 29th St NW, Calgary, Alberta, Canada, T2N 2T9.
Tel.: ⫹1-403-944-1683; fax: ⫹1-403-944-2906.
E-mail: brent.mitchell@albertahealthservices.ca
The disclosure information of the authors and reviewers is available from the
CCS on the following Web sites: www.ccs.ca and www.ccsguidelineprograms.ca.
This statement was developed following a thorough consideration of medical
literature and the best available evidence and clinical experience. It represents the
0828-282X/$ – see front matter © 2011 Canadian Cardiovascular Society. Published by Elsevier Inc. All rights reserved.
doi:10.1016/j.cjca.2010.11.005
92
Canadian Journal of Cardiology
Volume 27 2011
pital stay.1-10 The incidence of POAF after cardiac surgery ranges
from ⬇30% for patients undergoing isolated coronary artery bypass graft (CABG) surgery to ⬇40% for patients undergoing valve
replacement or repair to ⬇50% of patients undergoing both procedures.11 Furthermore, there is evidence that the incidence of
POAF is increasing as older individuals with a higher prevalence of
atrial tachyarrhythmia risk factors are more commonly undergoing these procedures.2,8
The peak incidence of these atrial tachyarrhythmias is between postoperative days 2 and 4. Of the patients who develop
an atrial tachyarrhythmia, 70% do so before the end of the
fourth postoperative day and 94% do so before the end of the
sixth post hospital day.8
revealed a highly statistically significant heterogeneity assessment
P-value of ⬍.001, indicating that differences between the trials
preclude meaningful merging of their results. Much of the heterogeneity in the results of these trials was explained by the practice
in some trials of permitting preoperative withdrawal of preexisting
-blocker drug therapy in those patients randomized not to receive study -blocker drug therapy (-blocker therapy withdrawal–mandated trials) versus the practice in other trials of continuing
preexisting -blocker drug therapy in those patients randomized
not to receive study -blocker drug therapy (-blocker therapy
withdrawal–not mandated trials). In the -blocker therapy withdrawal–mandated trials, study -blocker drug therapy was associated with a large reduction in the probability of postoperative AF
(OR 0.30, 95% CI 0.22-0.40, P-value for effect ⬍.001, P-value
for heterogeneity of .06). In the -blocker therapy withdrawal–
not mandated trials, study -blocker drug therapy was associated
with a smaller reduction in the probability of postoperative AF
(OR 0.69, 95% CI 0.54-0.87, P-value for effect of .002, P-value
for heterogeneity of .72). This observation may relate to preoperative -blocker therapy withdrawal increasing the control group
probability of postoperative AF.26
The largest of the -blocker therapy withdrawal–not mandated trials, the Beta Blocker Length Of Stay (BLOS) trial,27 reported a post-hoc analysis28 indicating that, in patients receiving
preoperative nonstudy -blocker drug therapy, study metoprolol
therapy was associated with a decrease in postoperative AF (metoprolol group AF incidence 29.6%, placebo group AF incidence
40.1%, OR 0.63), while in patients not receiving preoperative
nonstudy -blocker drug therapy, study metoprolol therapy was
not associated with a decrease in postoperative AF (metoprolol
group AF incidence 38.5%, placebo group AF incidence 35.0%,
OR 1.16) (unadjusted P-value for interaction of .065). Furthermore, in patients not receiving preoperative nonstudy -blocker
drug therapy, study metoprolol therapy was associated with
greater acute reduction in heart rate (unadjusted P-value for interaction of .002), greater acute reduction in cardiac index (unadjusted P-value for interaction of .002), and an increase in total
hospital stay (unadjusted P-value for interaction of .002).
Current evidence suggests that the standard -blocker drugs
are equivalent with regard to their efficacy in the prevention of
postoperative AF after cardiac surgery. Nevertheless, one small,
nonrandomized, retrospective comparison of carvedilol versus
other -blocker drugs (mostly metoprolol or atenolol) suggested
that carvedilol prevented postoperative AF better than did the
others (relative risk 0.24, 95% CI 0.11-0.51, P ⬍ .05).26 This
possibility will need to be assessed in a comparative clinical trial.
Thus, the evidence for continuing preoperative -blocker drug
therapy after cardiac surgery for the prevention of postoperative AF is very strong. However, initiating -blocker
drug therapy just before or after cardiac surgery in patients
BA
R
G
Risk Factors for Postoperative Atrial
Tachyarrhythmias
Independent patient characteristics that predict the occurrence of atrial tachyarrhythmias after cardiac surgery include
prior AF episodes, older age, male gender, history of hypertension, requirement for an intraoperative balloon pump, requirement for prolonged ventilation (⬎24 hours), and withdrawal
of -blocker therapy.2-8,12,13 As in the general population,14
age has the highest predictive value. Operative variables reported to be atrial tachyarrhythmia risk factors include the
procedure performed (isolated CABG, valve repair/replacement, or both), the number of bypass grafts, the duration of
surgery, and the duration of aortic cross-clamp time.2,15-17
traitements prophylactiques. Le traitement d’une FA postopératoire
peut suivre soit une méthode de ralentissement de la fréquence ventriculaire (avec les -bloquants) ou une méthode de stabilisation du
rythme. Les anticoagulants devraient être considérés si la FA postopératoire dure plus de 72 heures et si elle est encore présente au
moment de prendre congé de l’hôpital. Le besoin continu de traitement d’une FA postopératoire (notamment l’anticoagulation) devra
être reconsidéré pour 6 à 12 semaines suivant la procédure
chirurgicale.
O
ED
point of hospital discharge. The ongoing need for any POAF treatment
(including anticoagulation) should be reconsidered 6-12 weeks after
the surgical procedure.
EM
Consequences of Postoperative Atrial
Tachyarrhythmias
Post cardiac surgery atrial tachyarrhythmias may be transient and cause little morbidity. However, for some patients
these tachyarrhythmias have important consequences including patient discomfort/anxiety, hemodynamic deterioration,
cognitive impairment, thromboembolic events including
stroke, exposure to the risks of arrhythmia treatments, longer
hospital stay, and increased health care costs.2,4,8,9,18-23 Linear
regression models indicate that postoperative atrial tachyarrhythmias are independently associated with an increase in the
duration of hospitalization and in health care costs.8,24
Prophylaxis of Postoperative Atrial
Tachyarrhythmias
Standard -blocker drug therapy
A recent meta-analysis of randomized controlled clinical trials
(RCTs) evaluating standard -blocker drug therapy (Table 1) for
the prevention of postoperative AF after cardiac surgery examined
31 RCTs involving 4452 patients.25 -Blocker drug therapy was
associated with a reduction in the probability of postoperative AF
with an odds ratio (OR) of 0.36, a 95% confidence interval (95%
CI) for this point estimate of 0.28-0.47, and a statistical significance level (P-value) of .001. Nevertheless, this meta-analysis also
Postoperative Atrial Fibrillation
Mitchell et al.
93
Table 1. Prophylactic therapies for the prevention of postoperative atrial tachyarrhythmias
Dosage*
Odds ratio†
Any in usual therapeutic dose (ie,
metoprolol 50 mg PO q12h or
q8h for at least 2 preoperative d, d
of surgery, and at least 6
postoperative d)
10 mg/kg/d (rounded to nearest 100
mg) divided into 2 daily PO dosages
for 6 preoperative d, d of surgery,
and 6 postoperative d44
0.39 (0.28-0.52)
Reactive airways disease,
decompensated CHF
Sinus bradycardia
AV block
Hypotension
Bronchospasm
0.61 (0.50-0.74)
Postoperative
amiodarone
900-1200 mg IV over 24 h beginning
within 6 h of surgery, then 400 mg
PO tid each of the next 4 d37
0.53 (0.39-0.71)
Magnesium
sulfate
1.5 g IV over 4 h first preoperative d,
immediately postoperatively, and
next 4 postoperative d.45 Other trials
have omitted the preoperative dosage
Right, left, or biatrial pacing for 3-4 d
postoperatively.46 Rate set to
overdrive sinus rate either manually
or using sensing algorithms
0.83 (0.65-1.06)
30%-50% reduction in the dosages
of other drugs with
antiarrhythmic or sinus/AV
nodal effects and warfarin will
be required
30%-50% reduction in the dosages
of other drugs with
antiarrhythmic or sinus/AV
nodal effects and warfarin will
be required
Renal failure
Sinus bradycardia
AV block
Hypotension
Torsade de pointes VT (rare)
Pulmonary toxicity (rare)
Sinus bradycardia
AV block
Hypotension
Torsades de pointes VT (rare)
Pulmonary toxicity (rare)
Hypotension (rare)
Sedation (very rare)
Respiratory depression
(very rare)
Diaphragmatic stimulation,
Increased myocardial
oxygen requirements,
? Increased infection rate
Preoperative
-blocker
Preoperative
amiodarone
Atrial pacing
Cautions
0.67 (0.54-0.84)
May increase atrial
tachyarrhythmias if pacing
continues in setting of sensing
malfunction
O
ED
Therapy
Adverse effects
R
G
AV, atrioventricular; CHF, congestive heart failure; VT, ventricular tachycardia.
* Dosages used in the randomized studies vary widely and the optimal dosages for this indication have not been established. The dosages provided are those used
in the largest positive trial of that therapy and are referenced to that study.
† The odds ratios provided are from meta-analyses of the studies of each prophylactic approach (not for the single study referenced for dosage). Comparisons of
the efficacies of various prophylactic approaches require randomized trials, which, for the most part, have not been performed. Accordingly, comparisons of the odds
ratios provided in the table should be avoided.
RECOMMENDATION
BA
who were not receiving preoperative -blocker drug therapy
for the purpose of preventing postoperative AF has less compelling support.
EM
We recommend that patients who have been receiving a
-blocker before cardiac surgery have that therapy continued through the operative procedure in the absence of the
development of a new contraindication (Strong Recommendation, High-Quality Evidence).
We suggest that patients who have not been receiving a
-blocker before cardiac surgery have -blocker therapy initiated just before or immediately after the operative procedure in the absence of a contraindication (Conditional Recommendation, Low-Quality Evidence).
Values and preferences. These recommendations place
a high value on reducing postoperative AF and a lower value
on adverse hemodynamic effects of -blockade during or
after cardiac surgery. It is also noted that inherent to a strategy of prophylaxis, a number of patients will receive
-blocker therapy without personal benefit.
0.50, 95% CI 0.43-0.59, P ⬍ .0001). This meta-analysis reported
that amiodarone therapy for the prevention of postoperative AF
was also associated with a reduction in postoperative ventricular
tachyarrhythmias (OR 0.39, 95% CI 0.26-0.58, P ⬍ .001), a
reduction in postoperative neurologic events (OR 0.53, 95% CI
0.30-0.92, P ⫽ .02), a reduction in the postsurgery hospital length
of stay (0.6 days: 95% CI 0.4-0.8 days, P ⬍ .0001), and a reduction in hospital costs (–$2527, 95% CI –$500 to –$5815, P ⫽ .1).
Another meta-analysis that included adverse events noted that
amiodarone therapy in this setting is also associated with an increase in postoperative bradycardia (OR 1.66, 95% CI 1.732.47).25 A meta-analytic comparison of the effects of amiodarone
therapy initiated preoperatively (6 studies, OR 0.50, 95% CI
0.30-0.63) versus that initiated intraoperatively or postoperatively
(8 studies, OR 0.48, 95% CI 0.37-0.63) showed no statistically significant difference in the prevention of postoperative AF (P ⫽ .86).30
In a small, direct-comparison RCT, amiodarone was reported
to be more effective for the prevention of postoperative AF after
cardiac surgery than standard -blockade (propranolol) (RR 0.53,
95% CI 0.37-0.93, P ⫽ .05).31 Similarly, amiodarone therapy
was suggested to be more effective than sotalol therapy for this
purpose, but the difference was not statistically significant in a small
trial of 160 patients (RR 0.77, 95% CI 0.54-1.12, P ⫽ .21).32
RECOMMENDATION
Amiodarone therapy
A recent meta-analysis of RCTs evaluating amiodarone therapy (Table 1) for the prevention of postoperative AF after cardiac
surgery examined 19 placebo-controlled RCTs involving 3295
patients.29 Compared to placebo, amiodarone therapy was associated with a reduction in the probability of postoperative AF (OR
We recommend that patients who have a contraindication to -blocker therapy before or after cardiac surgery be
considered for prophylactic therapy with amiodarone to
prevent postoperative AF (Strong Recommendation, HighQuality Evidence).
94
Canadian Journal of Cardiology
Volume 27 2011
Sotalol therapy
Overdrive atrial pacing
Trials of overdrive atrial pacing (Table 1) for the prevention of
postoperative AF have used multiple pacing configurations: right
atrial pacing, left atrial pacing, biatrial pacing, and Bachmann’s
bundle pacing. Overall, a meta-analysis of 14 RCTs involving
1885 patients showed that overdrive atrial pacing was associated
with a reduction in the incidence of postoperative AF from 35.3%
to 17.7% (OR 0.60, 95% CI 0.47-0.77, P ⬍ .001).25 Although
the P-value for heterogeneity was not statistically significant, there
was a trend to heterogeneity (P ⫽ .13) and the majority of the
benefit was seen in 10 trials involving 754 patients wherein biatrial
pacing was associated with a statistically significant reduction in
the incidence of postoperative AF (OR 0.44, 95% CI 0.31-0.64,
P ⬍ .001). Individual assessment of right atrial and of left atrial or
Bachmann’s bundle overdrive atrial pacing did not show a statistically significant result.
The Atrial Fibrillation Suppression Trial II (AFIST-II)
compared overdrive atrial septal pacing to amiodarone therapy
for the prevention of postoperative AF and reported that amiodarone therapy prevented AF better than did overdrive atrial
pacing (RR 0.50, 95% CI 0.30-0.82, P ⬍ .05).37
Accordingly, the quality of evidence to recommend overdrive
atrial pacing, in the absence of other prophylactic therapy, for the
prevention of postoperative AF after cardiac surgery is low but, when
used, the evidence favours biatrial overdrive pacing.
Intravenous magnesium therapy
BA
R
G
A recent meta-analysis of RCT evaluating sotalol therapy for
the prevention of postoperative AF after cardiac surgery examined
9 placebo-controlled RCTs involving 1382 patients.25 Compared
to placebo, sotalol therapy was associated with a reduction in the
probability of postoperative AF (OR 0.34, 95% CI 0.26 – 0.45,
P-value ⬍.001). More patients receiving sotalol had their therapy
withdrawn because of adverse effects than did patients receiving
placebo (6.0% versus 1.9%, respectively, P ⫽ .004).
The same meta-analysis of RCTs evaluating sotalol therapy
for the prevention of postoperative AF after cardiac surgery
examined 7 RCTs involving 1240 patients comparing sotalol
therapy to standard -blocker drug therapy.25 Compared to
standard -blocker drug therapy, sotalol therapy was associated
with a reduction in the probability of postoperative AF (OR
0.42, 95% CI 0.26-0.65, P-value ⬍.001). More patients receiving sotalol had their therapy withdrawn because of adverse
effects than did patients receiving standard -blocker drug
therapy but this difference was not statistically significant
(7.2% versus 4.8%, respectively, P ⫽ .25).
Thus, sotalol therapy for the prevention of postoperative AF
after cardiac surgery has been less well studied than has standard -blocker drug therapy. Nevertheless, it appears that sotalol therapy has greater efficacy for this purpose than does
standard -blocker drug therapy but may also have a greater
adverse effect profile in this setting.
postoperative AF than was intravenous magnesium (RR 0.53,
95% CI 0.36-0.80, P ⫽ .01). Another small trial of 105 patients found no significant difference in the efficacy of intravenous magnesium therapy versus sotalol therapy for this purpose
(RR 0.87, 95% CI 0.48-1.55).36
Thus, there is moderate evidence that intravenous magnesium therapy, particularly lower-dose therapy initiated before
cardiac surgery, will reduce the postoperative incidence of AF
after cardiac surgery. The major advantage of this approach is
that the therapy has a very low probability of being associated
with adverse effects in patients without renal dysfunction.
O
ED
Values and preferences. This recommendation places a
high value on minimizing the patient population exposed to
the potential adverse effects of amiodarone and a lower
value on data suggesting that amiodarone is more effective
than -blockers for this purpose.
EM
A recent meta-analysis of 7 RTCs involving 1234 patients
evaluating intravenous magnesium therapy (Table 1) for the
prevention of postoperative AF after cardiac surgery reported
that intravenous magnesium therapy was associated with a reduction in the incidence of postoperative AF from 26.7% to
20.0% (OR 0.66, 95% CI 0.51-0.87, P ⫽ .003) and with a
reduction of the postoperative length of hospital stay in 6 trials
involving 1136 patients by 0.29 days (95% CI 0.05-0.54 days,
P ⫽ .02).33 However, this meta-analysis also found significant
heterogeneity among the intravenous magnesium trials (P ⫽
.02) with patients receiving preoperative intravenous magnesium (as opposed to intraoperative or postoperative therapy
initiation) and patients receiving lower dosages of intravenous
magnesium (as opposed to moderate or higher dosages of magnesium) apparently receiving all of the benefit of therapy with respect
to a reduction in the postoperative incidence of AF. Most intravenous magnesium trials report no evident adverse effects of magnesium therapy in properly selected patients. Nevertheless, one trial
reported a higher probability of postoperative hypotension with
combination intravenous magnesium and propranolol therapy
than with propranolol therapy alone.34
Intravenous magnesium therapy has been compared to a
standard -blocker (propranolol) in a trial involving 134 patients.35 Propranolol was more effective for the prevention of
RECOMMENDATION
We suggest that patients who have a contraindication to
-blocker therapy and to amiodarone therapy before or after cardiac surgery be considered for prophylactic therapy to prevent
postoperative AF with intravenous magnesium (Conditional Recommendation, Moderate-Quality Evidence) or with biatrial pacing (Conditional Recommendation, Low-Quality Evidence).
Values and preferences. This recommendation places a
high value on preventing postoperative AF using more novel
therapies that are supported by lower quality data. A high value
is placed on the low probability of adverse effects from magnesium. The use of biatrial pacing needs to be individualized by
patient and institution, as the potential for adverse effects may
outweigh potential benefit based on local expertise.
Other interventions
Meta-analyses have not shown a potential role for the use of
digoxin (OR 0.97, 0.62-1.49, P ⫽ .88), calcium channel
blocker drugs (OR 0.73, 95% CI 0.48-1.12, P ⫽ .15),
Postoperative Atrial Fibrillation
Mitchell et al.
95
Combination therapy
RECOMMENDATION
We suggest that consideration be given to anticoagulation therapy if postoperative continuous AF persists for
⬎72 hours. This consideration will include individualized assessment of the risks of a thromboembolic event
and the risk of postoperative bleeding (Conditional Recommendation, Low-Quality Evidence).
EM
BA
R
G
Two small trials36,37 directly compared 2 apparently effective treatments for the prevention of POAF after cardiac surgery using a 2 ⫻ 2 factorial trial design to evaluate the utility of
combination prophylactic therapy.
Forlani et al36 randomized 207 patients to receive prophylactic sotalol, prophylactic intravenous magnesium,
both therapies, or neither therapy. The incidence of postoperative AF was statistically significantly reduced from 38.0%
in the neither-therapy group to 14.8% in the magnesium
therapy–alone group and to 11.8% in the sotalol therapy–
alone group. The incidence of postoperative AF was statistically significantly reduced even further by combined magnesium and sotalol to an astonishing 1.9%.
The AFIST-II37 randomized 160 patients to receive prophylactic atrial septal pacing, prophylactic amiodarone, both therapies, or neither therapy. The incidence of postoperative AF was
37.5% in the neither-therapy group. The incidence of postoperative AF was not reduced by atrial septal pacing (40.0%). The
incidence of postoperative AF was reduced to 28.5% in the amiodarone-treated group but this difference was not statistically significant (RR 0.79, 95% CI 0.48-1.29). Although the incidence of
postoperative AF was further reduced by combined amiodarone
and atrial septal pacing to 15.8%, this difference was not statistically significant relative to that achieved with amiodarone therapy
alone (RR 0.77, 95% CI, 0.49-1.22). These suggestions of no
difference are, of course, power-limited.
cardiac surgery is dominated by self-terminating but frequently recurrent atrial tachyarrhythmia episodes and resolution of this propensity in 6-12 weeks regardless of the
therapy used.38-40 Furthermore, the adrenergic discharge
state after cardiac surgery lessens the effectiveness of therapies that do not include -blockade.
There is an association between POAF and postoperative
cerebrovascular events2,3,8,20,21 and cognitive impairment19
after cardiac surgery. On the other hand, early anticoagulation therapy in this setting may predispose the postoperative
patient to delayed pericardial bleeding and cardiac tamponade.41 In recognition of this risk and in the absence of controlled trials of the optimum timing for the initiation of
anticoagulation therapy for patients with AF after cardiac
surgery, anticoagulation is recommended for patients with
prolonged (⬎72 hours) AF. Once initiated, anticoagulation
is usually continued for ⱖ6 weeks.
O
ED
propafenone (OR 0.73, 0.39-1.38, P ⫽ .97), or procainamide
(OR 0.51, 95% CI 0.25-1.04, P ⫽ .07) for the prevention of
postoperative AF after cardiac surgery.25
Newer interventions with promising preliminary results
not yet tested in larger patient populations include glucose/
insulin/potassium, preservation of the anterior cardiac fat
pad, N-3 fatty acids, HMG CoA reductase inhibitors, and
systemic steroids.
RECOMMENDATION
We suggest that patients at high risk of postoperative
AF receive prophylactic therapy to prevent postoperative
AF such as sotalol or combination therapy including ⱖ2
of a -blocker, amiodarone, intravenous magnesium, or
biatrial pacing (Conditional Recommendation, Low- to
Moderate-Quality Evidence).
Values and preferences. This recommendation recognizes that data confirming the superiority of combinations
of prophylactic therapies are sparse.
Treatment of postoperative atrial fibrillation
The treatment goals for AF and flutter that occur after
cardiac surgery are identical to those of AF and atrial flutter
that occur in other settings. These goals include prevention
of thromboembolic events, slowing of the ventricular response rate, and consideration of conversion to and maintenance of sinus rhythm. Nevertheless, postoperative physiology does have features that favour some therapeutic
strategies over others. The natural history of POAF after
Values and preferences. This recommendation places
a higher value on minimizing the risk of thromboembolic
events and a lower value on the potential for postoperative bleeding. Because the risk of postoperative bleeding
decreases with time, the benefit-to-risk ratio favours a
longer period without anticoagulation in the postoperative setting than that suggested in other settings.
Therapy for ventricular rate control for atrial tachyarrhythmias is usually required for patients who experience AF
after cardiac surgery. Nevertheless, cardiac surgery may also
predispose such patients to bradyarrhythmias after conversion of AF or atrial flutter secondary to sinus nodal, AV
nodal, or His-Purkinje system dysfunction. Accordingly,
the availability of back-up ventricular pacing is important.
As the postsurgical state includes adrenergic discharge,
-blocker therapy is often very effective for slowing of the
ventricular response rate to AF and flutter. Other therapeutic alternatives, used when -blocker therapy is ineffective,
poorly-tolerated, or contra-indicated, include a non-dihydropyridine calcium antagonist (diltiazem, verapamil) or
amiodarone. In this setting, therapy with digoxin is usually
insufficient.
RECOMMENDATION
We recommend that temporary ventricular epicardial
pacing electrode wires be placed at the time of cardiac surgery to allow for backup ventricular pacing as necessary
(Strong Recommendation, Low-Quality Evidence).
96
Canadian Journal of Cardiology
Volume 27 2011
RECOMMENDATION
We recommend that postoperative AF with a rapid ventricular response be treated with a -blocker, a non– dihydropyridine calcium antagonist, or amiodarone to establish
ventricular rate control. In the absence of a specific contraindication, the order of choice is as listed (Strong Recommendation, High-Quality Evidence).
Values and preferences. This recommendation places a
high value on the randomized controlled trials investigating
rate control as an alternative to rhythm control for AF,
recognizing that these trials did not specifically address the
postoperative period.
We suggest that postoperative AF may be appropriately
treated with either a ventricular response rate-control strategy or a rhythm-control strategy (Conditional Recommendation, Low-Quality Evidence).
Values and preferences. This recommendation places a
high value on the randomized controlled trials investigating
rate control as an alternative to rhythm control for AF, recognizing that these trials did not specifically address the postoperative period.
RECOMMENDATION
We recommend that, when anticoagulation therapy,
rate-control therapy, and/or rhythm-control therapy has
been prescribed for postoperative AF, formal reconsideration of the ongoing need for such therapy should be undertaken 6-12 weeks later (Strong Recommendation, Moderate-Quality Evidence).
Values and preferences. This recommendation reflects
the high probability that postoperative AF will be a selflimiting process that does not require long-term therapy.
EM
BA
R
G
Considerations related to the advantages, disadvantages,
and risks of conversion to and maintenance of sinus rhythm
for patients with sustained atrial tachyarrhythmias after cardiac surgery are similar to those in other settings. Nevertheless, because early recurrence of the atrial tachyarrhythmia is
common, ongoing antiarrhythmic drug therapy to prevent
atrial tachyarrhythmia recurrences is preferred over isolated
DC cardioversion provided that the patient is sufficiently
stable to proceed. Although intravenous ibutilide has been
proposed as a rapid-acting approach to pharmacologic cardioversion of atrial tachyarrhythmias after cardiac surgery,
this intervention was effective in ⬍50% of patients (with
the highest success rates in patients with atrial flutter) and
was associated with the precipitation of Torsades de pointes
ventricular tachycardia in ⬇2%-5% of postoperative patients.42 In addition, the short half-life of this agent also
translates into the absence of ongoing therapy to prevent
atrial tachyarrhythmia recurrences.
The overwhelming majority of patients with postoperative
atrial tachyarrhythmias will no longer be susceptible to atrial
tachyarrhythmia recurrences within 6-12 weeks after cardiac surgery. Accordingly, a rate-control strategy, as opposed to a rhythmcontrol strategy, has the advantage of not exposing the patient,
who by definition has structural heart disease, to the risks of Class
I or Class III antiarrhythmic drugs. No large randomized clinical
trial has evaluated the advantages, disadvantages, and risks of the
rate-control strategy versus the rhythm-control strategy for POAF.
One small randomized pilot study39 reported a statistically significant reduction in the duration of the postsurgical hospital stay in
patients developing postoperative AF who were assigned to a
rhythm-control approach versus a rate-control approach to treatment. Nevertheless, a retrospective evaluation43 suggested a statistically significant reduction in the duration of postsurgical hospital
stay in patients discharged in AF (after ventricular response rate
control and anticoagulation) compared to patients discharged in
sinus rhythm. Accordingly, the preferred approach remains unknown. Regardless of the approach chosen, therapy provided for
POAF can usually be withdrawn 6-12 weeks later.
RECOMMENDATION
O
ED
Values and preferences. This recommendation reflects
the relative ease of placement of epicardial temporary
pacing wires at the time of surgery as well as the potential
for significant morbidity associated with postoperative
bradycardia.
References
1. Andrews TC, Reinmold SC, Berlin JA, Antman EM. Prevention of supraventricular arrhythmias after coronary artery bypass surgery: a meta-analysis of
randomized control trials. Circulation 1991;84:III-236-44.
2. Creswell LL, Schuessler RB, Rosenbloom M, Cox JL. Hazards of postoperative atrial arrhythmias. Ann Thorac Surg 1993;56:539-49.
3. Fuller JA, Adams GG, Buxton B. Atrial fibrillation after coronary artery
bypass grafting. Is it a disorder of the elderly? J Thorac Cardiovasc Surg
1989;97:821-5.
4. Leitch JW, Thomson D, Baird DK, Harris PJ. The importance of age as a
predictor of atrial fibrillation and flutter after coronary artery bypass grafting. J Thorac Cardiovasc Surg 1990;100:338-42.
5. Crosby LH, Pifalo WB, Woll KR, Burkholder JA. Risk factors for atrial
fibrillation after coronary artery bypass grafting. Am J Cardiol 1990;66:
1520-2.
6. Hashimoto K, Ilstrup DM, Schaff HV. Influence of clinical and hemodynamic variables on risk of supraventricular tachycardia after coronary artery bypass. J Thorac Cardiovasc Surg 1991;101:56-65.
7. Frost L, Mølgaard H, Christiansen EH, et al. Atrial fibrillation and flutter
after coronary artery bypass surgery: epidemiology, risk factors and preventative trials. Int J Cardiol 1992;36:253-61.
8. Aranki SF, Shaw DP, Adams DH, et al. Predictors of atrial fibrillation
after coronary artery surgery: current trends and impact of hospital resources. Circulation 1996;94:390-7.
9. Khaja F, Parker JO. Hemodynamic effects of cardioversion in chronic
atrial fibrillation. Arch Intern Med 1972;129:433-40.
10. Wong DT, Cheng DCH, Kustra R, et al. Risk factors of delayed extubation, prolonged length of stay in the intensive care unit, and mortality in
patients undergoing CABG with fast track cardiac anesthesia: a new cardiac risk score. Anesthesiology 1999;91:936-44.
Postoperative Atrial Fibrillation
Mitchell et al.
97
11. Mitchell LB. Incidence, timing and outcome of atrial tachyarrhythmias
after cardiac surgery. In: Steinberg JS, ed. Atrial Fibrillation After Cardiac
Surgery. Kluwer Academic Publishers 2000:37-50.
29. Bagshaw SM, Galbraith PD, Mitchell LB, et al. Prophylactic amiodarone
for prevention of atrial fibrillation after cardiac surgery: a meta-analysis.
Ann Thorac Surg 2006;82:1927-37.
12. Abel RM, van Gelder HM, Pores IH, et al. Continued propranolol administration following coronary bypass surgery: antiarrhythmic effects.
Arch Surg 1983;118:727-31.
30. Buckley MS, Nolan PE, Slack MK, et al. Amiodarone prophylaxis for
atrial fibrillation after cardiac surgery: meta-analysis of dose response and
timing of initiation. Pharmacotherapy 2007;27:360-8.
13. Silverman NA, Wright R, Levitsky S. Efficacy of low-dose propranolol in
preventing postoperative supraventricular tachyarrhythmias. Ann Surg
1982;196:194-7.
31. Solomon AJ, Greenberg MD, Kilborn MJ, Katz NM. Amiodarone versus
a -blocker to prevent atrial fibrillation after cardiovascular surgery. Am
Heart J 2001;142:811-5.
14. Kannell WB, Abbott RD, Savage DD, McNamara PM. Epidemiologic
features of chronic atrial fibrillation: the Framingham Study. N Engl
J Med 1982;306:1018-22.
32. Mooss AN, Wurdeman RL, Sugimoto JT, et al. Amiodarone versus sotalol
for the treatment of atrial fibrillation after open heart surgery: the Reduction in Postoperative Cardiovascular Arrhythmic Events (REDUCE) trial.
Am Heart J 2004;148:641-48.
16. Roffman JA, Feldman A. Digoxin and propranolol in the prophylaxis of
supraventricular tachydysrhythmias after coronary bypass surgery. Ann
Thorac Surg 1981;31:496-501.
17. Ormerod OJM, McGregor CGA, Stone DL, Wisbey C, Petch MC. Arrhythmias after coronary bypass surgery. Br Heart J 1984;51:618-21.
18. Orlando JR, van Herick R, Aronow WS, Olson HJ. Hemodynamics and
echocardiograms before and after cardioversion of atrial fibrillation to
normal sinus rhythm. Chest 1979;76:521-6.
34. Solomon AJ, Berger AK, Trivedi KK, Hannan RL, Katz NM. The combination of propranol and magnesium does not prevent postoperative
atrial fibrillation. Ann Thorac Surg 2000;69:126-9.
35. Bert AA, Reinert SE, Singh AK. A -blocker, not magnesium, is effective
prophylaxis for atrial tachyarrhythmias after coronary artery bypass graft
surgery. J Cardiothorac Vasc Anesth 2001;15:204-9.
36. Forlani S, De Paulis R, de Notaris S, et al. Combination of sotalol and
magnesium prevents atrial fibrillation after coronary artery bypass grafting. Ann Thorac Surg 2002;74:720-6.
R
G
19. Stanley TO, Mackensen GB, Grocott HP, et al; Neurological Outcome
Research Group, CARE Investigators of the Duke Heart Center. The
impact of post-operative atrial fibrillation on neurocognitive outcome after coronary artery bypass graft surgery. Anesth Analg 2002;94:290-5.
33. Henyan NH, Gillespie EL, White CM, Kluger J, Coleman CI. Impact of
intravenous magnesium on post-cardiothoracic surgery atrial fibrillation
and length of hospital stay: a meta-analysis. Ann Thorac Surg 2005;80:
2402-6.
O
ED
15. Caretta Q, Mercanti CA, De Nardo D, et al. Ventricular conduction
defects after coronary artery bypass grafting: multivariate analysis of preoperative, intra-operative and postoperative variables. Eur Heart J 1991;
12:1107-11.
BA
20. Taylor GJ, Malik SA, Colliver JA, et al. Usefulness of atrial fibrillation as
a predictor of stroke after isolated coronary artery bypass grafting. Am J
Cardiol 1987;60:905-7.
21. Lynn GM, Stefanko K, Reed JF III, Gee W, Nicholas G. Risk factors for stroke
after coronary artery bypass. J Thorac Cardiovasc Surg 1992;104:1518-23.
EM
22. Coplen SE, Antman EM, Berlin JA. Efficacy and safety of quinidine therapy for maintenance of sinus rhythm after cardioversion: a meta-analysis
of randomized control trials. Circulation 1990;82:1106-16.
23. Flaker GC, Blackshear JL, McBride R, et al. Antiarrhythmic drug therapy
and cardiac mortality in atrial fibrillation. J Am Coll Cardiol 1992;20:
527-32.
24. Kowey PR, Stanowski A, Schnoor E. Impact of atrial fibrillation on duration of hospital stay and cost of coronary artery bypass surgery. Clin Res
1992;40A:365.
25. Burgess DC, Kilborn MJ, Keech AC. Interventions for prevention of
post-operative atrial fibrillation and its complications after cardiac surgery:
a meta-analysis. Eur Heart J 2006;27:2846-57.
26. Merritt JC, Niebauer M, Tarakji K, Hammer D, Mills RM. Comparison
of effectiveness of carvedilol versus metoprolol or atenolol for atrial fibrillation appearing after coronary artery bypass grafting or cardiac valve
operation. Am J Cardiol 2003;92:735-6.
27. Connolly SJ, Cybulski I, Lamy A, et al. Double-blind, placebo-controlled,
randomized trial of prophylactic metoprolol for reduction of hospital
length of stay after heart surgery: the -Blocker Length of Stay (BLOS)
study. Am Heart J 2003;145:226-32.
28. Crystal E, Thorpe KE, Connolly SJ, et al. Metoprolol prophylaxis increases length of hospital stay in patients not on pre-operative  blockers:
the -Blocker Length of Stay (BLOS) study. Heart 2004;90:941-2.
37. White CM, Caron MF, Kalus JS, et al. Atrial Fibrillation Suppression
Trial II Investigators. Intravenous plus oral amiodarone, atrial septal pacing, or both strategies to prevent postcardiothoracic surgery atrial fibrillation: the Atrial Fibrillation Suppression Trial II (AFIST II). Circulation
2003;108(Suppl II):II-200-6.
38. Kowey PR, Stebbins D, Igidbashian L, et al. Clinical outcome of patients
who develop PAF after CABG surgery. PACE 2001;24:191-3.
39. Lee JK, Klein GJ, Krahn AD, et al. Rate-control versus conversion strategy
in postoperative atrial fibrillation: a prospective, randomized pilot study.
Am Heart J 2000;140:871-7.
40. Danias PG, Caulfield TA, Weigner MJ, et al. Likelihood of spontaneous
conversion of AF to sinus rhythm. J Am Coll Cardiol 1998;31:588-92.
41. Meurin P, Weber H, Renaud N, et al. Evolution of the postoperative
pericardial effusion after day 15: the problem of late tamponade. Chest
2004;125:2182-7.
42. VanderLugt JT, Mattioni T, Denker S, et al. Efficacy and safety of ibutilide fumarate for the conversion of atrial arrhythmias after cardiac surgery.
Circulation 1999;100:369-75.
43. Solomon AF, Kouretas PC, Hopkins RA, et al. Early discharge of patients
with new-onset atrial fibrillation after cardiovascular surgery. Am Heart J
1998;135:557-63.
44. Mitchell LB, Exner DV, Wyse DG, et al. Prophylactic oral Amiodarone
for the Prevention of Arrhythmias that Begin Early After Revascularization, valve replacement, or repair (PAPABEAR): a randomized clinical
trial. JAMA 2005;294:3093-100.
45. Toramen F, Karabulut EH, Alhan HC, Dağdelen S, Tarcan S. Magnesium infusion dramatically decreases the incidence of atrial fibrillation
after coronary artery bypass surgery. Ann Thorac Surg 2001;72,1256-62.
46. Greenberg MD, Katz NM, Iuliano S, Tempestra BJ, Solomon AJ. Atrial
pacing for the prevention of atrial fibrillation after cardiovascular surgery.
J Am Coll Cardiol 2000;35:1416-22.