Spring 2014 - New England Eye Center
advertisement

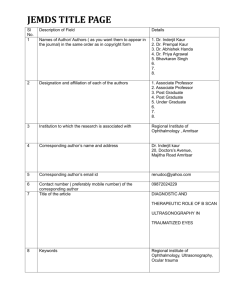
Spring 2014 THE TUFTS EYE ALUMNI ASSOCIATION newsletter p. 5 ~ welcoming the volume 5 number 1 2014 New England Eye Center Graduation, June 13 This year’s NEEC resident and fellow commencement is Friday, June 13, 2014. Resident and fellow research presentations will begin at 12:30 pm. more beginning on page 2 Inaugural Moshe Lahav, MD, Lecture class of ’13 to TEAA The family of the late, beloved Tufts University ophthalmic pathologist and retinal surgeon Moshe Lahav has generously funded a new lectureship for the annual graduation program. Eli Peli, OD, has been chosen to speak. continued on page 2 Resident class of 2013 below, l to r W. Morton Grant Lecture Michelle Liang, MD Kavita Bhavsar, MD Laurel Vuong, MD Steven Williams, MD The 2014 W. Morton Grant Lecturer is Gullapalli N. Rao, MD. Dr. Rao is the Distinguished Chair of Eye Health, L V Prasad Eye Institute, India. continued on page 3 Alumni are cordially invited to attend the New England Eye Center graduation June 13, 2014 (right) Michael Cooper, MD, PhD, (center) recipient of the 2013 Residents’ Award for Teaching Excellence 1 2014 Resident and Fellow Graduation: June 13 Dr. Peli to deliver the first Lahav Lecture continued from p 1 “Dr. Lahav was a committed physician and scientist who was also blessed with a human touch; his patients and colleagues loved him and he helped many people during the course of his life. The Lahav family hopes the lecture fund will contribute to the advancement of knowledge in the field of ophthalmology with a focus on the role of pathology, while recognizing the human impact of medicine.” The Lahav lecturer will be someone who embodies the personal attributes that Dr. Lahav projected as a physician, teacher and researcher here at Tufts. We are delighted to announce that the first lecturer will be Dr. Eli Peli, MSc, OD. Dr. Peli has been caring for visually impaired patients as the Director of the Vision Rehabilitation Service at Tufts Medical Center since 1983. He earned a BSc in Electrical Engineering and a MSc in Biomedical Engineering from the Technion Israel Institute of Technology. He then came to Boston where he received his OD degree from the New England College of Optometry. He is Adjunct Professor of Ophthalmology at Tufts University School of Medicine. Dr. Peli is also the Moakley Scholar in Aging Eye Research at Schepens Eye Research Institute, and Professor of Ophthalmology at Harvard Medical School. Dr. Peli will lecture on “Driving with Low Vision.” In memory of Moshe Lahav, MD Moshe Lahav, MD, died in 1998, having long battled pulmonary disease which never diminished his productivity or love of life. A specialist in vitreoretinal diseases and an ophthalmic pathologist, Dr. Lahav directed the diagnostic and experimental pathology laboratory at New England Eye Center for 17 years. Moshe Lahav was born in Tel Aviv, Israel, on November 10, 1939. In 1966, upon graduating medical school at Hebrew University, he received the Tabori Prize for Ophthalmology. This inspired him to pursue his studies in ophthalmology, ultimately traveling to the United States for residency and fellowship at Yale University. He became Chief Resident at Yale in 1972. He was a fellow in ophthalmic pathology at the Armed Forces Institute of Pathology, and he joined the Yale faculty in 1974. That same year he returned to Israel where he worked as a Senior Physician and the director of the Diagnostic and Experimental Eye Pathology Laboratory at the Hadassah Medical Center in Jerusalem. He returned to the United States in 1979, invited to establish the eye pathology laboratory at the Massachusetts Eye and Ear Infirmary. In 1981, he joined the department of ophthalmology at the Tufts University School of Medicine and became chief of ophthalmology at the Boston Veterans Administration Medical Center. He was appointed Professor of Ophthalmology at Tufts University School of Medicine in 1988. Thereafter he served as an ophthalmologist and director of the retina service at New England Medical Center and chief of ophthalmology at the Boston Veterans Administration Medical Center. A prolific contributor to the ophthalmic literature, Dr. Lahav’s early research concerned eye pathology. Case reports and series of important diseases provided significant insights relating clinical findings with pathology. One interesting project involved the use of methoxyflurane, an anesthetic. Clinicians noticed white dots in the eyes of patients who had undergone surgery. Dr. Lahav’s research established that these white dots were oxylate crystals formed by the breakdown of the anesthetic. As a result of this work, use of this anesthetic was discontinued. 2 Dr. Lahav was a distinguished surgeon. In a number of later articles he reported techniques developed for improving retinal surgery, as well as a model of retinal degeneration in vitro. He anticipated by a decade the local delivery of steroids to the eye for neovascular disease of the retina and choroid. Among his numerous research publications in the 1980s and 1990s in well regarded ophthalmology journals, a case record published in the prestigious New England Journal of Medicine stands out as a particular achievement. Moshe loved travel, music, dance, and hosting parties. His annual Halloween events are legendary. In addition, he was a talented artist who loved to paint and draw. Dr. Lahav is remembered as a creative researcher, a gifted pathologist, an excellent clinician whose patients hold in the highest regard to this day, and the compassionate and enthusiastic teacher of scores of ophthalmology residents at Yale and Tufts. His kindness and generosity, sense of humor and courage touched patients, staff and colleagues. W. Morton Grant Lecturer will be Gullapalli N. Rao, MD Continued from page 1 Dr. Rao is Chairman, Hyderabad Eye Institute, India, and Founder of the L.V. Prasad Eye Institute. Dr. Rao received his basic medical education in Guntur, Andhra Pradesh, and completed his postgraduate training in ophthalmology at the All India Institute for Medical Sciences, New Delhi. He came to the United States in 1974, where he was trained first at Tufts University School of Medicine in Boston, and later at the University of Rochester School of Medicine, where he served on the faculty until 1986. He then returned to India to establish the well-known L V Prasad Eye Institute. The Institute is considered to be among the top eye institutes in the world and is renowned for its innovative models of eye care delivery. His areas of specialization include diseases of the cornea, eye banking and corneal transplantation, community eye health, eye care policy and planning. He has published over 250 papers in national and international journals, and has contributed several book chapters. From 2004-2008, he served as President and CEO of the International Agency for the Prevention of Blindness, in which role he led VISION 2020: The Right to Sight, the global initiative to eliminate avoidable blindness by the year 2020. He is currently Chair of the International Centre for Eye Care Education (ICEE) and continues to be actively involved in global and national advocacy for eye care development. Dr. Rao will lecture on “Global Blindness: Eye Care in the Neglected Communities.” Dr. Seddon publishes important new findings in Nature Genetics Director of the Tufts MC Ophthalmic Epidemiology and Genetics Service Johanna M. Seddon, MD, ScM, fel ’77, res ’80 and her research team recently published “Rare variants in CFI, C3 and C9 are associated with high risk of advanced age-related macular degeneration” in Nature Genetics, November 2013 volume 45 number 11. The authors sequenced the exons of 681 genes within all reported AMD loci and related pathways in 2,493 cases and controls to define the role of rare variants in advanced age-related macular degeneration (AMD) risk. Testing each gene for increased or decreased burden of rare variants in cases compared to controls revealed that 7.8% of AMD cases compared to 2.3% of controls are carriers of rare missense CFI variants (odds ratio (OR) = 3.6; P = 2 × 10−8) with a predominance of dysfunctional variants in cases 3 compared to controls. Individual variants tested for association with disease demonstrated significant association with rare missense alleles in genes other than CFI. Genotyping in 5,115 independent samples confirmed associations with AMD of an allele in C3 encoding p.Lys155Gln (replication P = 3.5 × 10−5, OR = 2.8; joint P = 5.2 × 10−9, OR = 3.8) and an allele in C9 encoding p.Pro167Ser (replication P = 2.4 × 10−5, OR = 2.2; joint P = 6.5 × 10−7, OR = 2.2). Finally, the authors show that the allele of C3 encoding Gln155 results in resistance to proteolytic inactivation by CFH and CFI. These results implicate loss of C3 protein regulation and excessive alternative complement activation in AMD pathogenesis, informing both the direction of effect and mechanistic underpinnings of AMD. To date, Seddon’s team has found half of the known genes related to this common visually threatening disorder and their pioneering discoveries of modifiable risk factors have changed the management of this disease worldwide. Cynthia Mattox, MD, FACS, was elected Vice President/President-elect to the American Glaucoma Society (AGS), for the 2015-2016 term. AGS has more than 1,000 glaucoma specialists globally from 17 different countries and is dedicated to sharing clinical and scientific information for the benefit of patients, colleagues, fellows and residents. Dr. Mattox, previously AGS’s Patient Care Committee Chair, will be the first female Vice President/President-elect since the society’s inception in 1985. New attendings will join NEEC on or around September 1, 2014. Alan Lowinger, MD f ’14 (photo p. 8) is currently a glaucoma fellow in the combined NEEC/OCB fellowship program. Dr. Lowinger will initially be working in both the glaucoma and comprehensive ophthalmology services in Boston, as well as in our satellite offices. He completed his ophthalmology residency at California Pacific Medical Center. Laurel Vuong, MD r’13 (group photo p. 1) completed her residency at New England Eye Center and fellowship at Emory University. She will join Drs. Hedges and Athappilly in the neuro-ophthalmology service. Kamden Kopani, MD f’14 (photo p. 8) is completing a cornea fellowship at New England Eye Center and will join the faculty of the cornea service here. Sylvia Yoo, MD, completed her eye residency at Jules Stein Eye Institute and a pediatric ophthalmology fellowship at Johns Hopkins. She will join the NEEC pediatric eye service. Felipe Tolentino, MD, Has Retired from Ophthalmic Practice Fel Tolentino is an icon in the retina community. He has practiced retina in the Boston area for nearly 50 years, first with the Schepens Retina Associates and, for the past 11 years, at the New England Eye Center. Dr. Tolentino’s academic reputation was built on his superlative surgical skills and his ability to take on some of the most difficult cases. He wrote landmark papers on diabetic vitrectomy and new techniques of scleral buckling. Beyond his surgical skills, his bedside manner and aplomb under the most difficult circumstances allowed him to build an international practice. Patients who could fly anywhere for their retina care flew to Boston to see Fel. Over the past 20 years, Fel and his wife Flora spent a great deal of their time and money to build a free standing eye center in the native country of the Philippines. This eye hospital has become one of the most reputable deliverer of eye care in South Asia. In addition, Fel helped to start a local organization to combat blindness called Restoring Sight International. Dr. Tolentino’s dedication to his patients, practice, profession and the international community stands as an inspiration to us all. 4 THE TUFTS EYE ALUMNI ASSOCIATION 2013 New England Eye Center Graduation The New England Eye Center Graduation 2013 took place on Friday, June 28, 2013. Richard L. Abbott, MD, delivered The W. Morton Grant Lecture. Dr. Abbott is the Thomas W. Boyden Endowed Chair in Ophthalmology at the University of California San Francisco, Health Sciences Professor, Cornea and External Diseases Service. An expert in the political economy of ophthalmology, Dr. Abbot presented a timely, informative contribution to the audience’s understanding of risk management. Dr. Abbott was graduated from Tufts University with a Bachelor of Science degree before commencing his medical education and ophthalmology career. Tufts Alumni Speakers were Stefanie L. Davidson, MD res ’03 and Howard S. Weiss, MD, MPH TUSM ’85, res ’89. Dr. Davidson, a member of the Division of Pediatric Ophthalmology at the Children’s Hospital of Philadelphia and Assistant Clinical Professor of Ophthalmology with the University of Pennsylvania and Scheie Eye Institute spoke on “The Impact of Pediatric Vision Problems in Adulthood.” Dr. Weiss, active in clinical practice and academics at Walter Reed, Georgetown University and Washington Hospital Center, and in cataract and glaucoma research, spoke on “How to Learn New Surgical Procedures During Practice.” (Left) The electrophysiology laboratory at New England Eye Center is to be dedicated to the late Samuel Sokol, PhD. The plaque honoring Dr. Sokol, to be installed in the electrophysiology lab in pediatric ophthalmology in the Floating Hospital, is presented by Tom Hedges to Sam’s wife Heather. Sam’s career is described in the Newsletter 4:1, p. 4, “Samuel Sokol, PhD: 40 years at Tufts.” http://www.neec.com/Pages/Alumni/newsletter/v4n2_TEAA_W inter_2012.pdf. His obituary appears in the Newsletter 4:2, p.5. https://www.neec.com/Pages/Alumni/newsletter/v4n1_TEAA_S pring_2012.pdf Drs. Duker and Krishnan present the Preefer Award to Steven Williams, MD Millie Commodore, Kate Peterson, graduating cornea fellow Elvia Canseco, MD, Michael Raizman, MD, graduating cornea fellow Jonathan Kahn, MD, Jen Shields 5 and Minerva Bien-Aime Graduate residents: where they are now Steven Williams, MD West Coast Retina San Francisco, CA Kavita Bhavsar, MD Vitreous Retina Macula Consultants of New York, NY Laurel Vuong, MD Atlanta, GA Drs. Hung, Krishnan, graduating glaucoma fellows David Diaz, MD, and Mehul Nagarsheth, MD, Drs. Mattox, Hsu and Liang Michelle Liang, MD New England Eye Center, Boston, MA Graduate fellows : where they are now Hyung Cho, MD Retina Georgia Retina, Sandy Springs, GA Darin Goldman, MD Retina Retina Group of Florida Fort Lauderdale, FL Jonathan Kahn, MD Cornea Madison Ophthalmology. New York, NY Elvia Canseco, MD Cornea Drs. Witkin, Duker, graduating retina fellows Hyung Cho, MD, and Darin Goldman, MD, Drs. Rogers, Baumal, and Waheed Houston, TX Mehul Nagarsheth, MD Glaucoma Eye Consultants of PA, Wyomissing PA David Diaz, MD Glaucoma University of Vermont, Shelburne, VT Catherine Cox, MD Oculoplastics Oakland Medical Center, Oakland, CA Jordana Fein, MD Medical Retina New England Eye Center, Boston, MA Graduating oculopalastics fellow Catherine Cox, MD, with Dr. Kapadia Photo right top, Kendrew Caporal and Jean McGeary, RN; lower, Lisa Samborski, Sue Grant and Kara Waldron 6 THE TUFTS EYE ALUMNI ASSOCIATION NEW ENGLAND EYE CENTER RESIDENTS 1st year Bradley Hansen, MD Kendra Klein, MD Residents in Ophthalmology at the New England Eye Center 2013-14 Kirsten Dunbar, MD Kirstin Tawse, MD Nora Muakkasa, MD Gregory Lee, MD Joseph Ho, MD 7 3rd year Residents in Ophthalmology at the New England Eye Center 2013-14 Lauren Branchini, MD 2nd year Claudia Bartolini, MD Jen Renz, MD Kevin Sitko, MD Avneet Sodhi, MD THE TUFTS EYE ALUMNI ASSOCIATION Alan Lowinger, MD Kamden Kopani, MD Lauren Taney, MD Madina Falcone, MD David Lally, MD glaucoma cornea medical retina oculoplastics retina Fellows in Ophthalmology at the New England Eye Center 2013-14 Michelle Liang, MD Brendon Sumich, MD Shlomit Sandler, MD Michael Tibbetts, MD MarissaWeber, MD Roger Goldberg, MD retina cornea glaucoma medical retina retina retina , A volunteer attending’s experience Sharewood Eye Clinic Grows, Doubles Its Clinic Schedule by Yvonne Tsai, M.D. Sharewood has been a delightful experience for me — the medical students are enthusiastic, eager to learn, inquisitive about the clinical aspects of what they have learned in the classroom. Since leaving my fellowship training at Manhattan Eye and Ear in 1987, I have been in solo practice. I realize how much I miss a teaching hospital experience. Sharewood gives me the chance to pay it forward — give the medical students and residents some practical knowledge in ophthalmology as well as to offer medical care to the local citizens of Malden. I feel that the students and residents are getting a valuable exposure to their future careers by volunteering at Sharewood and that physicians already in practice benefit as well by seeing that they really do enjoy what they do! I wish that this type of program had been available back when I was in medical school or residency training. The Sharewood Project, under the auspices of the Tufts University School of Medicine, provides a range of free and unscheduled health services to the uninsured and underserved in the city of Malden. Sharewood is operated by medical students under the supervision of volunteer physicians, with assistance from other affiliated health care professionals and translators. The program is located at The First Church in Malden Center, and is funded solely through donations and fundraising. The Vision Center of the Sharewood Project offers diagnoses for visual abnormalities. A monthly clinic session has been conducted by students who are interested in ophthalmology, under the administrative supervision of Thomas R. Hedges, MD. Trial frames and loose lenses have filled eye glass prescriptions. Medical students and other interested volunteers learn to use the indirect ophthalmoscope and slit lamp for dilated retinal examination, as well as other ophthalmic instruments including the lensometer, applanation tonometer, and direct ophthalmoscope. The diagnosis of visual disorders is performed under the supervision of a volunteer ophthalmologist and resident. The Sharewood Project’s Vision Center is 8 a unique opportunity for students of any level — undergraduate to clinical fellowship — to gain exposure and to hone skills. Alex Legocki, now a second year medical student at Tufts University, was elected to coordinate the eye clinic of Sharewood in AY 201213. The eye clinic was then in its fourth year, with an established infrastructure and ongoing challenges, and the opportunity to lay a deeper foundation to sustain the project. The challenges included acquiring equipment and ensuring an adequate staff of volunteer ophthalmologists to supervise. Alex applied for a Tufts School of Medicine Student Council Award aimed to fund an indirect ophthalmoscope. Combined with a contribution from the Tufts Ophthalmology Interest Group, the Student Council Award granted Sharewood this critical piece of equipment. Toward the recruitment of volunteers, Alex wrote a memorandum of outreach that the executive committee of the New England Ophthalmological Society NEOS generously communicated to its membership, resulting in enlisting no fewer than seven ophthalmologists from Massachusetts and New Hampshire. Of these to date, Dr. Yvonne Tsai, Dr. Matthew Lazzara, Dr. Michael Raizman, and Dr. Macie Himmel have served as attendings for the grateful students of Sharewood’s eye service. On his experience as Sharewood’s Eye Clinic coordinator, Alex reflects, “I gained valuable clinical and technical skills and developed connections throughout the ophthalmology field.” Coordinators of Sharewood serve one year, during their first year as Tufts medical students. Following Alex Legocki’s term, Pamela Sherwood (her name a coincidence) and Steven Young took the reins as Sharewood coordinator and ophthalmology clinic coordinator respectively in January 2014. They are enthusiastic about continuing the growth enabled by the strengthening of the infrastructure under their predecessors. Both Pam and Steve had previous experience working in ophthalmology clinics prior to starting medical school, and are looking to further develop their skills. They have implemented a more efficient clinic intake and have started involving more graduate and medical students in the clinic. Starting in April of 2014, Sharewood will begin holding ophthalmology clinics twice a month. Additionally, they are working with the Sharewood IT team to incorporate ophthalmology into its electronic medical record system. Recruiting ophthalmologists and eye residents to volunteer service in the clinic remains a priority. Pamela has taken on the effort to contact and build strong relationships between Sharewood and community ophthalmologists. Recently John Liu, a third year medical student at Tufts who previously coordinated the Sharewood ophthalmology clinic, arranged contact between the new coordinators and the Massachusetts Society of Eye Physicians and Surgeons, to reinforce the successful effort via NEOS to encourage volunteering. For his part, each month Steven reaches out to the residents at Tufts Medical Center. Many of them have taken time in their crowded schedules to spend an evening at Sharewood. Among them are former TUSM students who had volunteered at Sharewood, to whom returning as residents to teach holds special meaning. “We have been lucky to have had such amazing volunteers come and share their passionate knowledge about the field with us. Our clinical skills in ophthalmology have benefited tremendously from their presence here at Sharewood.” Goals now include building new partnerships with charitable organizations or start-ups to develop the scope of service and innovative technology at Sharewood. For example, Warby Parker sells prescription frames at low cost, through which it funds Vision Spring to provide eyeglasses to people who cannot afford prescription spectacles. Another lead, from Dr. Yvonne Tsai, involves a start-up out of MIT that is working on a vision technology mobile app that may be useful to pilot at the clinic. The excellent contribution and progress of Sharewood rely on continuing volunteer efforts, and your opportunity to serve awaits. Please do not hesitate to sign up for one evening of participation. You may well decide that the Sharewood experience is one to which you will wish to make the time to return. Please contact Pamela.sherwood@tufts.edu or Steven_K.Young@tufts.edu to volunteer, discuss a donation of equipment, or for further information. 9 COS opens at Continued from p. 11 New England Eye Center Upon the opening of COS, New England Eye Center administrative director Linnea Olsson observed, “The Comprehensive Ophthalmology Service will allow us to better serve patient needs for both urgent and routine comprehensive ophthalmology care. It will be much easier to accommodate new patients who wish to come to New England Eye Center, with faster appointment times. We believe that the structure of COS will greatly enhance our residency training program. The optometry department has been relocated to Biewend 11, and our optometrists and technicians as well as physicians are very excited about the beautiful new space and equipment! “Many people have worked hard on the planning and set-up of the new area. Drs. Jordana Fein and Dru Krishnan have spent countless hours conceptualizing and organizing how COS will run, and I would like to particularly acknowledge the contributions of Dr. Cynthia D’Auria, Chris Kiernan, Bianca Cardona, Nathan Knowles, Meredith Dunbar, Jean McGeary, Amanda Bruce, and our unsung hero of logistics, David Schultz!” The establishment of the COS will enable the NEEC and the Tufts Department of Ophthalmology to grow, and represents the strength and foresight that will serve us through many years of change and challenges in the future of eye care. situation ensues and we grow our volume enough, we may have to address staffing and facilities expansion to keep up the pace, but that would not be a bad situation to be in.” Dr. Fein also observes that billing for emergency visits is now more consistent, with far fewer chances that billing for services might be overlooked. Tom Bigelow, manager of New England Eyewear, the optical dispensary of NEEC, adds his witness that patients are happier and better served. “Patients have reported to me that they are now getting appointments in a far more timely way. They’re very satisfied.” In addition to the full-time participation of Dr. Fein, COS is attended by Brooke Miller, MD, and Sergey Urman, MD as well as Dr. Lauren Taney and Dr. Michael Tibbets, our current medical retina fellows. Senior optometrist Cynthia D’Auria, OD, comments, “The Optometry Service is thrilled to be on the 11th floor working alongside the COS. It is refreshing to be in a new space with new equipment. The patient flow works well with the New England Eyewear optical shop just steps away to service our patients for their glasses and contact lens needs.” Pride in Tufts Medical History Thomas R. Hedges, MD, has been elected President of the Tufts Medical Alumni Association. Tom graduated from TUSM in 1975 and has been on the faculty of Tufts since 1981. He hopes to use his position to remind the Tufts medical alumni of the great history of this institution. For the eye alumni Tom would like to make us aware of Josef Igersheimer who was a professor at Tufts from 1939 to 1968. After escaping Nazi Germany he went to Turkey where he helped modernize ophthalmology there. In 1930 he came to the United States where he was welcomed by The Boston Dispensary and Tufts Medical School. Dr. Igersheimer, a student of Gonin, was one of the first to treat retinal detachments by closing breaks in the retina. He also performed one of the first corneal transplants, in Boston. 10 Josef Igersheimer, M.D. COS opens at New England Eye Center Continued from the back page The new service is organized and staffed in such a way as to facilitate the care and follow-up of patients presenting through emergency services and urgent consults, and, additionally, provide a dedicated area where patients with general ophthalmological needs may obtain convenient appointments and be seen in a timely way. Director of COS Dr. Fein describes the organization and operational system of COS as well as its advantages. “COS provides a service in which residents, under appropriate supervision, can participate in the care and follow-up of their own patients and develop the continuing relationship that is beneficial to both the patient as well as the educational need of the resident. The service provides a properly designated facility as well as a scheduled time, free from other responsibilities, during which the resident may see his or her patient. “The first year residents will begin to realize early in their training the advantages of independent, albeit supervised, management of patient care that previously had not been so available until the third year of training. The resident will be the patient’s doctor and both will benefit from the continuity of care and its efficient management.” Previously, emergency patients would be seen by the resident on call. However, due to the resident’s responsibility to the subspecialty service to which he or she was assigned, and lacking a designated time or place for a follow up visit, the patient would likely not then be followed by the original resident and so there would not be the long-term follow-up for the resident. “Now they have a dedicated time and place to see such patients. “At the same time in the past, patients who came to our eye center for routine examination or for undiagnosed problems would be given excellent care, but within a subspecialty unit. There was a degree of competition for the available facilities and provider time. This system resulted in longer waits for routine appointments, longer stays in the waiting room, and impinged teaching time. The system worked, but as an educational environment and comfortable patient experience it needed improvement.” In the planning, Dr. Fein explained, director of clinical services Nathan Knowles analyzed patient flow data and derived the number of appointment slots necessary to build into the system to accommodate emergency patients in COS. Currently four slots are reserved daily for emergency add-ons; the remainder are available for scheduling routine appointments and followups. COS also has the advantage of being located in the same area as our optometry service. This provides the advantage of the excellent teaching our experienced optometrists can provide, especially for refraction. The work distribution and teaching conduciveness in a resident-centered academic practice are arguably superior to other systems. Supervision and teaching are more uniform and dedicated. Patient care is standardized at the highest level. Patients benefit from a team effort and have the advantage of access to the very latest diagnostic and treatment protocols. “Such a system allows for the efficient delivery of the highest quality of care, it is really the state-of theart academic care structure. COS will operate at the same level of excellence as all of the subspecialty and adjunct services of our highly respected, worldclass tertiary referral center.” Thus far, patients are now getting appointments within weeks rather than months. “If the best Continued on p. 10 11 New England Eye Center Opens Comprehensive Ophthalmology Service Under Directorship of Jordana Fein, MD res ’12, fel ’13 Top to bottom, The culmination of years of planning and groundwork, the long-anticipated Comprehensive Ophthalmology Service (COS) of the New England Eye Center opened on Biewend 11 on January 13, 2014. The new service will contribute to the delivery of general ophthalmic care and the education of resident physicians. The service has been built from the experience of residents and attending physicians in treating patients at the New England Eye Center. Its mission and organization are thus informed by the inseparable collaboration between faculty and resident. When Dr. Jordana Fein started her residency at the NEEC in 2009, a “general” ophthalmology service had already been on the mind of Jay Duker, MD, chairman of the department. Such a service would provide for the needs of the emergency patients as well as routine eye exams. It would also be the service where residents, even in their first year, could have the substantial responsibility for care management, and the opportunity to follow patients from first presentation through the course of their care. The possibility was well discussed. While requiring the knowledge and supervision of the experienced attending physician, the delivery of patient care in all specialties is largely dependent on the work of the resident. Dru Krishnan, MD, director of residency training, shared his understanding that the founding of such a service as COS was key in addressing challenges of both resident education and expeditious delivery of eye care. Trained as resident at the NEEC, Dr. Krishnan understands the dynamic at the New England Eye Center, particularly the role of the house officer as trainee and patient care provider. It was during her own residency and fellowship, under the tutelage of Drs. Duker and Krishnan, that Dr. Fein made a commitment to the goal of establishing the COS. Drs. Duker and Krishnan had already begun the procedures for obtaining institutional approval and support, space acquisition and development, budgeting and organizational planning. Dr. Fein became the administrative coordinator who would see the plan to completion. Continued on p. 11 Photographs: Kathleen Warren 12 and the New England Eye Center Photography Department Jordana Fein, MD Brooke Miller. MD Sergey Urman, MD Cynthia D’Auria, OD